Abstract
Introduction
Advanced hepatocellular carcinoma (HCC) with macrovascular invasion (MVI) has the worst prognosis among all phenotypes. This trial aims to evaluate whether treatment with durvalumab, alone or in combination with tremelimumab, plus particle therapy is a safe and synergistically effective treatment in patients with advanced HCC and MVI.
Methods and analysis
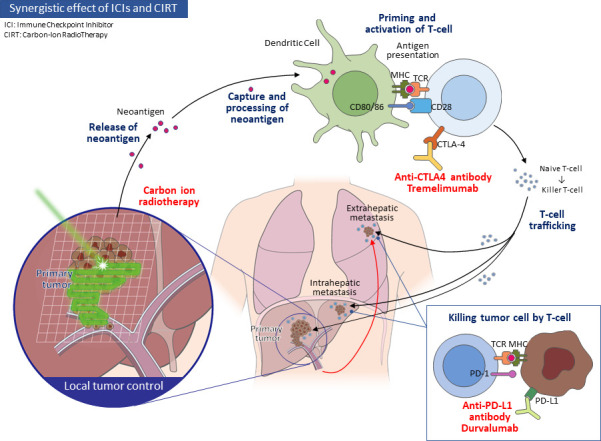
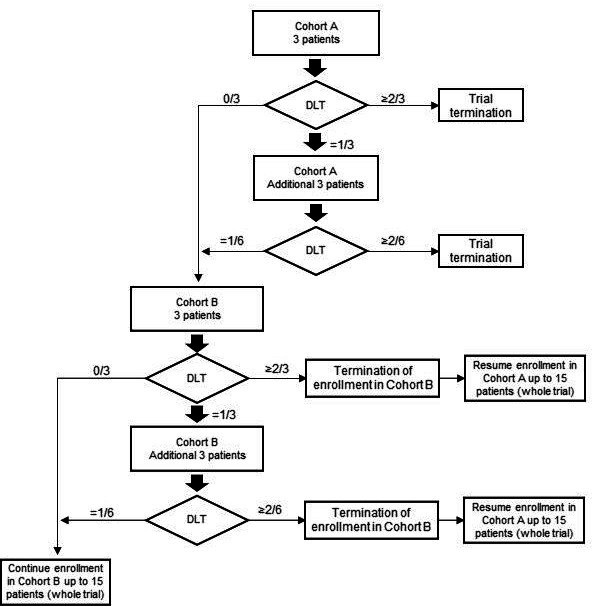
This phase Ib, multicentre (two sites in Japan), open-label, single-arm, investigator-initiated clinical trial will assess durvalumab monotherapy in combination with particle therapy (cohort A) and that of durvalumab plus tremelimumab in combination with particle therapy (cohort B) for patients with advanced HCC with MVI. Cohort A will receive 1500 mg durvalumab every 4 weeks. Cohort B will receive 1500 mg durvalumab every 4 weeks in principle and 300 mg tremelimumab only on day 1 of the first cycle. Carbon-ion radiotherapy will be administered after day 8 of the first cycle. The primary endpoints are rates of any and severe adverse events, including dose-limiting toxicities (DLTs); secondary endpoints are overall survival, 6-month survival, objective response, 6-month progression-free survival and time to progression. Patients are initially enrolled into cohort A. If cohort A treatment is confirmed to be tolerated (ie, no DLT in three patients or one DLT in six patients), the trial proceeds to enrol more patients into cohort B. Similarly, if cohort B treatment is confirmed to be tolerated (ie, no DLT in three patients or one DLT in six patients), a total of 15 patients will be enrolled into cohort B.
Ethics and dissemination
This study was approved by the ethics committees of the two participating institutions (Chiba University Hospital and National Institutes for Quantum (approval number: 2020040) and Radiological Science and Technology, QST Hospital (approval number: C20-001)). Participants will be required to provide written informed consent. Trial results will be reported in a peer-reviewed journal publication.
Trial registration number
jRCT2031210046.
Keywords: hepatobiliary tumours, radiation oncology, hepatology
Strengths and limitations of this study.
This trial is a multicentre, investigator-initiated study assessing a promising combination treatment in patients with advanced hepatocellular carcinoma with macrovascular invasion.
The trial is designed to investigate both safety (primary endpoints) and synergistic efficacy (secondary endpoints).
Although this study is designed to assess the performance of immune checkpoint inhibitors (ICIs) followed by carbon-ion radiotherapy (C-ion RT), the order of ICI and C-ion RT treatment requires further investigation.
Introduction
Hepatocellular carcinoma (HCC) accounts for the majority of liver cancer cases and remains to have a poor prognosis because most cases are diagnosed at the advanced stage.1 2 Recently, liver cancer ranks as the fourth most common cause of cancer-related death and as the sixth most frequently diagnosed cancer. Systemic therapies for advanced HCC have improved dramatically in the last decade. Previously, molecular target agents were the major treatment options for advanced HCC, but the impact on prognosis was limited.3–7 Nowadays, combination immunotherapy is becoming the mainstream of systemic therapy for advanced HCC. In fact, in a global randomised phase III trial, atezolizumab plus bevacizumab was shown to significantly improve both overall survival (OS) and progression-free survival (PFS), compared with the effects of sorafenib.8 Several clinical trials on combination immunotherapy are underway, and further improvement of prognosis is strongly expected.9
Durvalumab is a selective and high-affinity human immunoglobulin G1 monoclonal antibody that blocks PD-L1 binding to PD-1 and CD80.10 Tremelimumab, which is a monoclonal immunoglobulin G2 antibody targeting cytotoxic T lymphocyte-associated antigen 4 (CTLA4), prevents the normal downregulation of T cells and prolongs T cell action, thereby enhancing immune function.11 Combining anti-PD-1/PD-L1 with anti-CTLA4 therapies was shown to provide additive antitumour activity through its action on the antitumour T cell response by multiple immune checkpoint blockade.12 The combination of two immune checkpoint inhibitors (ICIs) has already been demonstrated to have clinical efficacy in several malignancies.13–17 For advanced HCC, durvalumab plus tremelimumab showed tolerability and promising clinical activity, based on the results of a global phase II trial (Study 22).18 Patients treated with a single priming dose of tremelimumab 300 mg added to durvalumab every 4 weeks (ie, T300 D regimen) achieved a median OS of 18.7 months. Including the other arms, such as durvalumab alone, tremelimumab alone and 75 mg of tremelimumab for four doses with durvalumab every 4 weeks (T75+D), this phase II study demonstrated acceptable safety profiles and no new adverse events (AE). Very recently, the results of a phase III trial (A Randomized, Open-label, Multi-center Phase III Study of Durvalumab and Tremelimumab as First-line Treatment in Patients with advanced Hepatocellular Carcinoma [HIMALAYA]) reported durvalumab plus tremelimumab significantly prolonged OS compared with sorafenib.19
Focusing on the disease state of advanced HCC, variations of disease progression can be divided into macrovascular invasion (MVI), which is unique to HCC, and extrahepatic metastasis, as in other malignant tumours.20 The presence of MVI is known to be an extremely poor prognostic factor that leads to progressive malignant disease severity and to deterioration of liver function. Surgical resection of tumours that include MVI and local control of MVI by transarterial chemoembolisation, hepatic arterial infusion chemotherapy or radiation therapy had been previously reported to improve the prognosis of patients with advanced HCC with MVI.20–26 However, these treatment strategies have not become common because of several reasons. First, in the majority of cases in which MVI is present, the tumour is not localised and metastatic lesions have often spread to both the liver and extrahepatic organs. Second, the procedures to remove or control MVI require sufficient skill and experience. In addition, all treatments that attempt to remove or control MVI are highly invasive and require extremely well-maintained liver function and general performance status. Development of innovative treatments that target this specific phenotype of advanced HCC is imperative.
While radiotherapy for HCC has been mostly used in a palliative intent, with the emergence of particle therapy followed by stereotactic body radiotherapy (SBRT), it has become a viable treatment option for those not eligible for resection, transplant or radio frequency ablation but still with a localised disease.27–29 Compared with conventional photon radiotherapy and SBRT, particle radiation therapy, which includes both proton beam therapy and carbon-ion radiotherapy (C-ion RT), has been demonstrated to confer a unique dose distribution; its physical characteristics enable delivery of high radiation doses to the tumour and low doses to normal tissues.30 Compared with photons, charged particles have different depth–dose distributions and deposit majority of the dose at the Bragg peak, with little to no exit dose, thereby resulting in superior sparing of normal tissue. One particular advantage of particle radiation therapy for HCC is that irradiation can be confined to a localised area of tumour; this results in both high local control and minimal impact on liver function.31 Several reports have already confirmed the high local control rates and safety profile of both proton beam therapy and C-ion RT for HCC.29 32 Moreover, the possibility of local control of MVI in advanced HCC by particle radiation therapy has been suggested.33
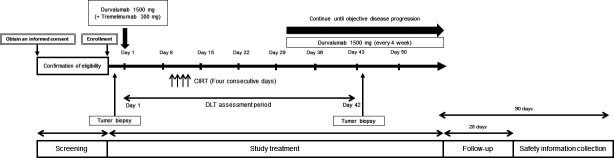
Radiation therapy, especially C-ion RT, is well known to mediate localised tumour killing and tumour microenvironment modification, thereby potentiating the effectiveness of ICIs.34–36 Because the combination of radiation and ICIs is expected to be a promising treatment, its impact on several advanced cancers is still being tested. In advanced HCC, several combination immunotherapies based on ICI are further developed.37 Among various treatments currently under development, we believe that C-ion RT combined with ICIs may lead to further breakthroughs for patients with advanced HCC and MVI using its powerful potential of local tumour control, immunosuppression and immunogenicity (figure 1).
Figure 1.
Study concept.
Methods and analysis
Objective
The aim of this study is to investigate the safety and synergistic effect of durvalumab with particle therapy and durvalumab plus tremelimumab combined with particle therapy in patients with advanced HCC and MVI (box 1).
Box 1. Study endpoints.
Primary endpoint
AEs/SAEs including DLTs.
Secondary endpoints
Overall survival.
6-month survival rate.
Objective response rate.
6-month progression-free survival rate.
Time to progression.
Study design and setting
This study is a non-blinded, single-arm, phase Ib trial that will be conducted at two institutions (Chiba University Hospital and National Institutes for Quantum and Radiological Science and Technology, QST Hospital) to assess the safety of durvalumab combined with particle therapy (cohort A) and durvalumab plus tremelimumab combined with particle therapy (cohort B) in patients with advanced HCC and MVI (figure 2). After providing consent, patients will undergo screening and assessment for study enrolment eligibility. Assessment of dose-limiting toxicity (DLT) will be for 42 days starting from the administration of durvalumab or durvalumab plus tremelimumab on day 1 of cycle 1. In both cohorts, if the investigators determined any potential clinical benefit, patients will continue to receive durvalumab every 4 weeks until clinical progression (ie, durvalumab q4W dosing period). In subjects who provide additional written informed consent, biopsy specimens will be obtained from the same liver tumour that is not irradiated with C-ion RT before and 42 days after the start of durvalumab or durvalumab plus tremelimumab administration on day 1 of cycle 1. Specimens will be stored appropriately and may be used for further studies if consent has been obtained from the subjects.
Figure 2.
Dosing schedule. DLT, dose-limiting toxicity. CIRT, carbon-ion radiotherapy
Trial resources
This study is funded by AstraZeneca. However, the sponsors are not involved in patient aggregation or analysis.
Eligibility and screening
Potential participants are screened by the principal investigator or one of the associate investigators, according to the eligibility criteria shown in box 2.
Box 2. Key eligibility criteria.
Inclusion criteria
Age ≥20 years at the time of study entry.
Eastern Cooperative Oncology Group performance status of 0 or 1.
Body weight >30 kg.
Adequately normal organ and marrow functions.
Life expectancy of at least 12 weeks.
Advanced HCC confirmed histologically or by the typical findings of a hypervascular tumour on CT or angiography.
Must not be eligible for locoregional therapy for unresectable HCC.
Child-Pugh A.
Patients who have been diagnosed with HCC with macrovascular invasion.
Patients with history of at least one prior systemic chemotherapy regimen, including atezolizumab/bevacizumab combination, sorafenib or lenvatinib, and were judged to be refractory or intolerant to standard therapy (excluded from the inclusion criteria in the expansion cohort).
Exclusion criteria
Any unresolved NCI-CTCAE grade ≥2 toxicity from previous anticancer therapy, with the exception of alopecia, vitiligo and the laboratory values defined in the inclusion criteria.
Radiotherapy treatment to more than 30% of the bone marrow or with a wide field of radiation within 4 weeks of the first dose of the study drug.
Major surgical procedure, as defined by the investigator, within 28 days prior to the first dose of IP.
History of allogenic organ transplantation.
Active or prior documented autoimmune or inflammatory disorders.
History of another primary malignancy.
Prior or current brain metastases or spinal cord compression.
History of active primary immunodeficiency.
Patients coinfected with hepatitis B and C viruses or with hepatitis B and D viruses.
Current or prior use of immunosuppressive medication within 14 days before the first dose of durvalumab or tremelimumab.
Known allergy or hypersensitivity to any of the study drugs or any of the study drug excipients.
Prior radiotherapy involving the liver.
Renal failure requiring haemodialysis or peritoneal dialysis.
Presence of any severe cardiac disease.
Poorly controlled hypertension.
Serious and active infection, excluding hepatitis virus infection.
Persistent proteinuria of NCI-CTCAE version 5.0 grade ≥3; urine dipstick result of 3+ is allowed if protein excretion is <3.5 g/24 hours.
Arterial or venous thrombotic or embolic events, such as cerebrovascular accident, deep vein thrombosis or pulmonary embolism within 6 months before the start of the study medication.
Refractory pleural effusion or ascites.
History of hepatic encephalopathy within the past 12 months.
Treatment regimen
In cohort A, durvalumab 1500 mg will be administered every 4 weeks in principle. Particle therapy in the form of C-ion RT will be administered after day 8 of cycle 1 following the first dose of durvalumab on day 1. In cohort B, durvalumab 1500 mg will be administered every 4 weeks in principle, and tremelimumab 300 mg will be administered only on day 1 of cycle 1. Particle therapy in the form of C-ion RT will be administered after day 8 of cycle 1 following the first cycle of durvalumab plus tremelimumab. C-ion RT will be given after day 8 of cycle 1 following the first dose of durvalumab plus tremelimumab on day 1. The dose is 60 Gy (relative biological effectiveness) in four fractions per week. The target lesion of the particle therapy will be focused on an intrahepatic nodule with MVI. The clinical target volume margin will be 1 cm for the feeding nodule and 2 cm alongside the vessel for the MVI lesion. Internal motion will be compensated according to 4D-CT movement assessment. Interfractional margin will be set at 3 mm and combined with internal motion compensation to form a field-specific planning treatment volume. Study treatments will continue until disease progression, according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Prohibited concomitant treatments are described in the online supplemental table 1. Information on AEs occurring in the trial or obtained from other trials will be collected and responded to appropriately following the Good Clinical Practice in Japan (J-GCP). The trial team will provide treatment for the patients’ recovery and provide appropriate medical care.
bmjopen-2021-059779supp001.pdf (57KB, pdf)
Patient registration rules
In this modified 3+3 design (figure 3), three patients are initially enrolled into cohort A. If no DLT is observed in any of these subjects, the trial proceeds to enrol more subjects into cohort B, which regimen contains an additional drug, tremelimumab. If one subject develops a DLT in cohort A or B, three more subjects are enrolled into the same cohort. DLT occurrence in >1 of six subjects in either cohort suggests that the regimen is not tolerable. If cohort A turns out to be intolerable, then cohort B regimen will not be pursued. If cohort B treatment is confirmed to be tolerated (ie, no DLT in three patients or one DLT in six patients), enrolment of up to a total of 15 subjects to cohort B is continued. Development of DLTs in at least two subjects in cohort A will mean that the entire trial will be terminated. Occurrence of DLTs in at least two subjects in cohort B would suggest that tolerability is not confirmed, and the regimen of cohort B will be discontinued. In this case, additional patients up to a total of 15 will be enrolled in cohort A. Criteria for discontinuation of the trial treatment are described in online supplemental table 2.
Figure 3.
Schematic depiction of modified 3+3 design. DLT, dose-limiting toxicity.
bmjopen-2021-059779supp002.pdf (54.3KB, pdf)
Definition of DLT
DLT will be evaluated during the assessment period of the trial (ie, for 42 days starting from the administration of durvalumab on day 1 of cycle 1). Subjects who do not remain in the study up to this time for reasons other than DLT will be replaced with another subject who will receive the same dose level. Grading of DLTs will follow the guidelines provided in the Common Terminology Criteria for Adverse Events version 5.0. A DLT is defined as the occurrence of an AE that is at least possibly related with the treatment regimen. AEs that are at least possibly related with the treatment regimen will be designated as DLTs if they meet any of the criteria listed in online supplemental table 3. Any treatment-related toxicity that first occurs during the DLT assessment period must be followed up for resolution to determine if the event qualifies as a DLT, as specified in the DLT criteria.
bmjopen-2021-059779supp003.pdf (72.9KB, pdf)
Statistical methods and sample size determination
This study will employ a modified 3+3 design, and the number of subjects that will enable us to assess the safety and tolerability of the investigational regimen in the DLT population will be defined. We set the total number of subjects in this study, including the expansion cohort, at 15 based on the enrolment feasibility within the study period. The DLT analysis set will comprise all patients who will undergo DLT assessment or safety analyses. The frequencies of DLTs will be calculated for each cohort. For efficacy analyses, OS, 6-month survival rate, objective response rate, 6-month PFS rate and time to progression will be reported. No interim analysis will be conducted in this trial.
Data management, monitoring, safety and auditing
Data are accurately and appropriately recorded in the case report forms and will be managed appropriately following the J-GCP. Monitors ensure that the trial team is conducting the study per the study protocol and J-GCP. An audit will be conducted at the investigational site to confirm that the quality control of the trial is appropriately conducted.
Data monitoring committee
The data monitoring committee consists of clinical trial experts, including biostatisticians, who are not involved in this study. The committee will check the data obtained from the trial and evaluate the treatment cohort.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Ethics and dissemination
This study was approved by the ethics committee of two participating institutions (Chiba University Hospital and National Institutes for Quantum (approval number: 2020040) and Radiological Science and Technology, QST Hospital (approval number: C20-001)). All patients are required to give written informed consent to a member of the study team before inclusion in a phase Ib study of durvalumab with or without tremelimumab combined with particle therapy in advanced hepatocellular carcinoma patients with macrovascular invasion (DEPARTURE trial) (online supplemental file).
bmjopen-2021-059779supp004.pdf (124.4KB, pdf)
If the protocol is revised, the primary investigator will inform the trial team and obtain the institutional review board’s approval.
We will submit the trial results as the case study report on the Japan Registry of Clinical Trials. Trial results will be reported in a peer-reviewed journal publication. The authorship will be ascribed following the International Committee of Medical Journal Editors guidelines.
Protocol version
Protocol version 1.2, modified 2021.
Study status
The first subject of this study enrolled on 6th July, 2021. The study is ongoing.
Supplementary Material
Acknowledgments
The authors are grateful to the following people for their contributions to the data management: Satomi Nakamura, Ryoko Arai and Yuka Iwase.
Footnotes
Twitter: @hmaxi_MD
SO, KK and HM contributed equally.
Contributors: SO drafted the manuscript. SO, KK, HM, MW and AT designed the protocol. YO and YK performed the statistical analysis. SY, MN, TI, KO, KF, TI, TS, NF, RK, HK, KK, SK, MN, NK, TS, TK, RN, SN, RM, TC, TK, HH, HT and NK further aided in the assessment and revisions of the protocol and manuscript.
Funding: This work was supported by AstraZeneca (Osaka, Japan; grant number: ESR-19-20168).
Competing interests: SO has received honoraria from Bayer, Eisai, Eli Lilly and Chugai Pharma and research funding from Bayer, Eisai, Eli Lilly and AstraZeneca. NK has received honoraria from Bayer, Eisai, Eli Lilly and Chugai Pharma and research funding from Bayer, Eisai and Eli Lilly.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Villanueva A. Hepatocellular carcinoma. N Engl J Med 2019;380:1450–62. 10.1056/NEJMra1713263 [DOI] [PubMed] [Google Scholar]
- 2.Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nat Rev Dis Primers 2021;7:6. 10.1038/s41572-020-00240-3 [DOI] [PubMed] [Google Scholar]
- 3.Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–90. 10.1056/NEJMoa0708857 [DOI] [PubMed] [Google Scholar]
- 4.Cheng A-L, Kang Y-K, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 2009;10:25–34. 10.1016/S1470-2045(08)70285-7 [DOI] [PubMed] [Google Scholar]
- 5.Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017;389:56–66. 10.1016/S0140-6736(16)32453-9 [DOI] [PubMed] [Google Scholar]
- 6.Abou-Alfa GK, Meyer T, Cheng A-L, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med 2018;379:54–63. 10.1056/NEJMoa1717002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu AX, Kang Y-K, Yen C-J, et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 2019;20:282–96. 10.1016/S1470-2045(18)30937-9 [DOI] [PubMed] [Google Scholar]
- 8.Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 2020;382:1894–905. 10.1056/NEJMoa1915745 [DOI] [PubMed] [Google Scholar]
- 9.Cheng A-L, Hsu C, Chan SL, et al. Challenges of combination therapy with immune checkpoint inhibitors for hepatocellular carcinoma. J Hepatol 2020;72:307–19. 10.1016/j.jhep.2019.09.025 [DOI] [PubMed] [Google Scholar]
- 10.Stewart R, Morrow M, Hammond SA, et al. Identification and characterization of MEDI4736, an antagonistic anti-PD-L1 monoclonal antibody. Cancer Immunol Res 2015;3:1052–62. 10.1158/2326-6066.CIR-14-0191 [DOI] [PubMed] [Google Scholar]
- 11.Tarhini AA, Kirkwood JM. Tremelimumab (CP-675,206): a fully human anticytotoxic T lymphocyte-associated antigen 4 monoclonal antibody for treatment of patients with advanced cancers. Expert Opin Biol Ther 2008;8:1583–93. 10.1517/14712598.8.10.1583 [DOI] [PubMed] [Google Scholar]
- 12.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252–64. 10.1038/nrc3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015;373:23–34. 10.1056/NEJMoa1504030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med 2018;378:1277–90. 10.1056/NEJMoa1712126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Overman MJ, Lonardi S, Wong KYM, et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J Clin Oncol 2018;36:773–9. 10.1200/JCO.2017.76.9901 [DOI] [PubMed] [Google Scholar]
- 16.Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non-small-cell lung cancer. N Engl J Med 2019;381:2020–31. 10.1056/NEJMoa1910231 [DOI] [PubMed] [Google Scholar]
- 17.Baas P, Scherpereel A, Nowak AK, et al. First-Line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet 2021;397:375–86. 10.1016/S0140-6736(20)32714-8 [DOI] [PubMed] [Google Scholar]
- 18.Kelley RK, Sangro B, Harris W, et al. Safety, efficacy, and pharmacodynamics of tremelimumab plus durvalumab for patients with unresectable hepatocellular carcinoma: randomized expansion of a phase I/II study. J Clin Oncol 2021;39:2991–3001. 10.1200/JCO.20.03555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abou-Alfa GK, Chan SL, Kudo M, et al. Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (PTS) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. Journal of Clinical Oncology 2022;40:379. 10.1200/JCO.2022.40.4_suppl.379 [DOI] [Google Scholar]
- 20.Costentin CE, Ferrone CR, Arellano RS, et al. Hepatocellular carcinoma with macrovascular invasion: defining the optimal treatment strategy. Liver Cancer 2017;6:360–74. 10.1159/000481315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kokudo T, Hasegawa K, Matsuyama Y, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol 2016;65:938–43. 10.1016/j.jhep.2016.05.044 [DOI] [PubMed] [Google Scholar]
- 22.Kokudo T, Hasegawa K, Yamamoto S, et al. Surgical treatment of hepatocellular carcinoma associated with hepatic vein tumor thrombosis. J Hepatol 2014;61:583–8. 10.1016/j.jhep.2014.04.032 [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Huang J, Chen M, et al. Transcatheter arterial chemoembolization (TACE) versus hepatectomy in hepatocellular carcinoma with macrovascular invasion: a meta-analysis of 1683 patients. J Cancer 2017;8:2984–91. 10.7150/jca.20978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ueshima K, Ogasawara S, Ikeda M, et al. Hepatic arterial infusion chemotherapy versus sorafenib in patients with advanced hepatocellular carcinoma. Liver Cancer 2020;9:583–95. 10.1159/000508724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munoz-Schuffenegger P, Barry A, Atenafu EG, et al. Stereotactic body radiation therapy for hepatocellular carcinoma with macrovascular invasion. Radiother Oncol 2021;156:120–6. 10.1016/j.radonc.2020.11.033 [DOI] [PubMed] [Google Scholar]
- 26.Finn RS, Zhu AX, Farah W, et al. Therapies for advanced stage hepatocellular carcinoma with macrovascular invasion or metastatic disease: a systematic review and meta-analysis. Hepatology 2018;67:422–35. 10.1002/hep.29486 [DOI] [PubMed] [Google Scholar]
- 27.Bujold A, Massey CA, Kim JJ, et al. Sequential phase I and II trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin Oncol 2013;31:1631–9. 10.1200/JCO.2012.44.1659 [DOI] [PubMed] [Google Scholar]
- 28.Hong TS, Wo JY, Yeap BY, et al. Multi-Institutional phase II study of high-dose Hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol 2016;34:460–8. 10.1200/JCO.2015.64.2710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yasuda S, Kato H, Imada H, et al. Long-Term results of high-dose 2-fraction carbon ion radiation therapy for hepatocellular carcinoma. Adv Radiat Oncol 2020;5:196–203. 10.1016/j.adro.2019.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malouff TD, Mahajan A, Krishnan S, et al. Carbon ion therapy: a modern review of an emerging technology. Front Oncol 2020;10:82. 10.3389/fonc.2020.00082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Apisarnthanarax S, Bowen SR, Combs SE. Proton beam therapy and carbon ion radiotherapy for hepatocellular carcinoma. Semin Radiat Oncol 2018;28:309–20. 10.1016/j.semradonc.2018.06.008 [DOI] [PubMed] [Google Scholar]
- 32.Shibuya K, Ohno T, Terashima K, et al. Short-Course carbon-ion radiotherapy for hepatocellular carcinoma: a multi-institutional retrospective study. Liver Int 2018;38:2239–47. 10.1111/liv.13969 [DOI] [PubMed] [Google Scholar]
- 33.Shiba S, Shibuya K, Kawashima M, et al. Comparison of dose distributions when using carbon ion radiotherapy versus intensity-modulated radiotherapy for hepatocellular carcinoma with macroscopic vascular invasion: a retrospective analysis. Anticancer Res 2020;40:459–64. 10.21873/anticanres.13974 [DOI] [PubMed] [Google Scholar]
- 34.Lee YH, Tai D, Yip C, et al. Combinational immunotherapy for hepatocellular carcinoma: radiotherapy, immune checkpoint blockade and beyond. Front Immunol 2020;11:568759. 10.3389/fimmu.2020.568759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iijima M, Okonogi N, Nakajima NI, et al. Significance of PD-L1 expression in carbon-ion radiotherapy for uterine cervical adeno/adenosquamous carcinoma. J Gynecol Oncol 2020;31:e19. 10.3802/jgo.2020.31.e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takahashi Y, Yasui T, Minami K, et al. Carbon ion irradiation enhances the antitumor efficacy of dual immune checkpoint blockade therapy both for local and distant sites in murine osteosarcoma. Oncotarget 2019;10:633–46. 10.18632/oncotarget.26551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roudi R, D'Angelo A, Sirico M, et al. Immunotherapeutic treatments in hepatocellular carcinoma; achievements, challenges and future prospects. Int Immunopharmacol 2021;101:108322. 10.1016/j.intimp.2021.108322 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059779supp001.pdf (57KB, pdf)
bmjopen-2021-059779supp002.pdf (54.3KB, pdf)
bmjopen-2021-059779supp003.pdf (72.9KB, pdf)
bmjopen-2021-059779supp004.pdf (124.4KB, pdf)