Abstract
Background
the Mediterranean Lifestyle index (MEDLIFE) was developed as a questionnaire to capture adherence to an overall Mediterranean healthy lifestyle. The reliability of the MEDLIFE as an independent questionnaire must be evaluated prior its use in research studies.
Objective
to assess the inter-method reliability of the MEDLIFE as a short and independent research tool.
Design
the 28-item MEDLIFE questionnaire and a 142-item validated questionnaire (full-Q) from which we derived the 28-items MEDLIFE (MEDLIFE-derived) were administered simultaneously to 196 adults (mean age 41.4 ± 9.2 y) living in Madrid, Spain. The reliability was assessed by Kappa (k) statistics, intra-class correlation coefficients (ICC) and limits of agreement (LOA).
Results
overall correlation between the two instruments was 0.626. MEDLIFE had an acceptable ability to rank participants by MEDLIFE-derived from full-Q (ICC = 0.544). Absolute agreement showed very good concordance for 10.7% of the items evaluated; good to moderate concordance for most items, and fair concordance for 32.1% of the items. Intake of sweets, processed meats, low-fat dairy products and cereals were overestimated by MEDLIFE. About 38%, 15%, 12% and 10% of participants who scored 1-point for those items in MEDLIFE also scored 1-point in the MEDLIFE-derived respectively. Bland Altman’s analysis showed that LOA ranged from −4.66 to 7.45 (mean = 1.40).
Conclusion
the MEDLIFE is a valid instrument to measure overall adherence to the Mediterranean lifestyle in middle age adults from a Spanish population, and could be used as an independent questionnaire in clinical and epidemiological studies for such population. Its generalizability and predictive validity for clinical outcomes remains to be investigated.
Keywords: Reliability, Mediterranean diet, Dietary index, Lifestyle, Questionnaire
Keywords: Fiabilidad, La dieta mediterránea, Índices dietéticos, Estilo de vida, Cuestionario
Resumen
Antecedentes
el índice de estilo de vida mediterráneo (MEDLIFE) fue desarrollado como un cuestionario para recoger la adherencia a un estilo de vida saludable mediterráneo. La fiabilidad del MEDLIFE como cuestionario independiente debe ser evaluada antes de su uso en estudios de investigación.
Objetivo
evaluar la fiabilidad inter-método del MED-LIFE como herramienta de investigación corta e independiente.
Diseño
cuestionario corto del MEDLIFE de 28 ítems y un cuestionario largo validado de 142 ítems, del cual se derivó posteriormente el cuestionario del MEDLIFE de 28 ítems (MEDLIFE-derivado), se administraron simultáneamente a 196 adultos (edad media 41,4 ± 9,2 años) con residencia en Madrid, España. La fiabilidad se evaluó mediante el coeficiente kappa de Cohen, el coeficiente de correlación intraclase (CCI) y el límite de acuerdo (LOA).
Resultados
el grado de correlación entre los dos instrumentos fue 0,626. El MEDLIFE tuvo una capacidad aceptable para clasificar a los participantes mediante el MEDLIFE-derivado (ICC = 0,544). El grado de acuerdo absoluto (coeficiente kappa) mostró muy buena concordancia para el 10,7% de los ítems evaluados; de buena a moderada para la mayoría de los ítems, y razonable para el 32,1% de los ítems. La ingesta de dulces, carnes procesadas, productos lácteos bajos en grasa y cereales se sobreestimó por el MEDLIFE. El 38%, 15%, 12% y 10% de los participantes que obtuvieron 1 punto para esos ítems en el MEDLIFE también obtuvieron 1 punto en el MEDLIFE-derivado, respectivamente. El análisis de Bland Altman mostró un rango de LOA de −4,66 a 7,45 (media = 1,40).
Conclusión
el MEDLIFE es un instrumento válido para medir la adherencia global al estilo de vida mediterráneo en adultos de mediana edad de una población española, y podría ser utilizado como cuestionario independiente en estudios clínicos y epidemiológicos para tal población. Su generalización y validez predictiva para los parámetros clínicos debe ser investigada.
Introduction
Several dietary indices have emerged during the last decade as an integrated measure of a healthy eating pattern and an alternative method to assess diet-disease relations1,2. One of these healthy eating patterns is the Mediterranean diet (MD), which has been consistently shown to protect against the development of chronic diseases3–5. In epidemiological research, a number of indices have been developed to study compliance with the traditional MD6, such as the Mediterranean Diet Score (MDS)7,8, Mediterranean Adequacy Index (MAI)9, MedDiet Score10, MEDAS11, and relative Mediterranean Diet (rMED)12, among others.
After those indices were created, the Mediterranean Diet Foundation’s International Scientific Committee updated the recommendations in 2010 to include other traditional Mediterranean lifestyle behaviors, such as resting patterns, social structures, consumption of seasonal and diverse foods, and other healthy culinary techniques13,14.
In order to address these Mediterranean lifestyle-behaviors altogether, we recently described the development of MEDLIFE (MEDiterranean LIFEstyle)15, a new index that incorporates those revised recommendations. MEDLIFE was developed with the aim of strengthening the evidence of a protective effect of the Mediterranean lifestyle on health-related diseases and potentially support new recommendations into public health policies. Unlike prior indices, the MEDLIFE includes additional emerging lifestyle-factors beyond diet that have been also associated with cardiovascular outcomes namely sociability, sleep and rest, and conviviality16–19, and new dietary components and eating behaviors (e.g. water as the main beverage).
Nevertheless, assessing the reliability of indices is an essential before an essential step before its use in epidemiological studies. While most of currently available dietary indices have been developed for epidemiological research and have been assessed as for their construct and content validity11,20–24, only few have been further developed to independent tools or short questionnaires for utilization in clinical settings11,25 .
We previously reported the construct and content validity of MEDLIFE15. The objective of this study was to assess the inter-method reliability of a 28-items MEDLIFE questionnaire as an independent tool by comparing its performance against a validated full block 142-items questionnaire.
Methods
Participants’ recruitment
Participants for this study included 196 adults who worked in public schools (teacher or staff) or were involved in the school environment (family members) from 6 control schools participating in the Program SI! Intervention, which aimed to promote healthy lifestyle habits in preschoolers. No intervention was undertaken on these schools26. Individuals who volunteered to participate had to be older than 18 years old, and were required to not be involved in any lifestyle-related intervention. Study questionnaires were administered by a trained dietitian. All participants gave written informed consent. The study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by the Regional Committee for Clinical Research Ethics (CEIC-R) of Madrid Area.
Assessment of lifestyle behaviors
Lifestyle assessment was completed using two instruments: the MEDLIFE 28-items questionnaire, and a full-length block 142-items questionnaire (full-Q) that has been previously validated and includes a food frequency questionnaire, a physical activity questionnaire and other questions related to lifestyle habits27–29. From the full-Q we derived the 28-items MEDLIFE, in order to later compare whether the same information provided by both instruments (MEDLIFE 28-items questionnaire and MEDLIFE-derived from the full-Q) by the same participant agreed.
28-items MEDLIFE
MEDLIFE was created based on the Mediterranean Food Guide pyramid proposed in 2010 by the Mediterranean Diet Foundation13,14. In brief, a total of 28 items were developed based on its recommendations and categorized into three blocks: (1) Mediterranean food consumption (15 items); (2) Mediterranean dietary habits (7 items); (3) Physical Activity, rest, social habits and conviviality (6 items). Each item was scored as 0 for not meeting the cutoff established for the item or 1 for meeting it, so that the complete MEDLIFE ranged from 0 to 28, with a higher value indicative of greater adherence to Mediterranean lifestyle (Table I).
Table I.
The Mediterranean Lifestyle index (MEDLIFE) questionnaire
| Items | Criteria for 1 point* |
|---|---|
| Block 1: Mediterranean food consumption | |
|
| |
| How many serving of pastries do you consume per week? (candy (1s = 1 unit or 50 g), chocolates (1 s = 30gr), biscuits (1 s = 4–6 units), nougat (“turrón”) (1s = 40 g)) |
≤ 2 s/week |
| How many servings of red meat do you consume per week? (Beef, pork, lamb (1 s = 100–150g)) | < 2 s/week |
| How many serving of processed meat do you consume per week? (Ham (1 s = 1 slice or 30 g), sausage, soft spicy sausage, bacon (1 s = 50 g), hamburger (1 s = 1 unit), liver (1 s = 100–150g), paté (1s = 25g)) |
≤ 1 s/week |
| How many eggs do you consume per week? (Eggs (1 egg)) | 2–4 s/week |
| How many serving of legumes do you consume per week? (Lentils, beans, peas, chickpeas (1 s = 1 plate or 150 g)) | ≥ 2/ week |
| How many servings of white meat do you consume per week? (Poultry, rabbit (1 s = 100–150 g)) | 2 s/ week |
| How many serving of fish or seafood portions do you consume per week? (White/fatty fish (1 s = 100–150 g), canned fish (1 s = 1 can or 50 g), seafood (1 s = 200g)) |
≥ 2/ week |
| How many potatoes do you consume per week? (Roasted/boiled potatoes, French fries (1 s = 150–200 g)) | ≤ 3 s/week |
| How many low-fat dairy products do you consume per day? (Skimmed dairy milk (1s = 200 ml milk, two yogurts, 1 portion soft cheese)) |
2 s/day |
| How many nuts and olives do you consume per day? (Walnuts, almonds, hazelnuts (1s = 1 handful or 30 g), olives (1 s = 10 units)) |
1–2 s/day |
| How many times do you use herbs, spices or garnish for cooking per day? (Onion, garlic, herbs (parsley, oregano)) |
≥ 1 s/day |
| How many pieces of fruit do you consume per day? (All fruit and fresh fruit-based juices (1 s = 150–200g)) | 3–6 s/day |
| How many servings of vegetables do you consume per day? (All vegetables except potatoes (1 s = 150–200 g)) | ≥ 2 s/day |
| How many tablespoons of olive oil do you consume per day (cooking or salad dressing)? (Olive oil, virgin olive oil (1s = 1Tablespoon)) |
≥ 3 s/day |
| How many servings of cereals do you consume per day? (White and whole-grain bread (1s = 40 g), cereals (1s = 1 plate rice, pasta or 40g breakfast cereals) and derivatives) |
3–6 s /day |
|
| |
| Block 2: Mediterranean dietary habits | |
|
| |
| Do you drink more than 6 glasses of water or at least one cup of tea per day? (Water or tea (1 s = 1 glass)) | Yes |
| Do you drink wine at mealtime every day? (White/red wine (1 s = 1 glass of wine)) | 1–2 s/ day |
| Do you limit added salt in meals? | Yes |
| Do you usually choose whole grain products? (bread, pasta, rice, breakfast cereals) | Yes |
| Do you consume snacks 2 or less times per week? (potatoes chips, tortilla chips, popcorn (1 s = 1 bag or 50 g)) | Yes |
| Do you usually limit nibbling between meals? | Yes |
| Do you limit intake of sugar in beverages? (including sugar-sweetened beverages) | Yes |
|
| |
| Block 3: Physical activity, rest, social habits and conviviality | |
|
| |
| Do you engage in physical activity (> 150min/week or 30 min/day)? (jogging, walk at a fast pace, dance, aerobics, gardening) |
Yes |
| Do you sleep siesta/nap? | Yes |
| How many hours do you sleep a day? (During weekdays) | 6–8 hour/day |
| How many hours do you spend watching TV per day? (During weekdays) | ≤ 1hour/day |
| How many hours do you spend going out with friends during the free time (e.g. weekends)? | ≥ 2hour/weekend |
| How many hours do you practice team sports per week? | ≥ 2hour/week |
0 points if these criteria were not met. s = serving
For this inter-method reliability study, we included the 28 items extracted from the full-Q. However, the 28-item MEDLIFE questionnaire administered to participants had four additional questions to address the seasonality and frugality included in the Mediterranean lifestyle pyramid that are not included in this analysis because this information was not assessed from the full-Q, and therefore comparison between the two tools was not possible (Supplementary material)
Full-length block 142-items questionnaire (full-Q)
Dietary intakes and habits were assessed using a semi-quantitative food frequency questionnaire (FFQ) previously validated in Spain30, capturing long-term intake during the year preceding the examination, and taking into account seasonal variations and differences between weekday and weekend patterns. The questionnaire was based on 136 food items, including specific questions about consumption of supplements and information on adherence to restrictive diets. Each food included in the questionnaire specified the serving size and offered nine options for frequency of consumption, from “never or almost never” to “more than six times a day”.
The questionnaire also included items on physical activity based on the Spanish validated version27 of the Nurses’ Health Study (NHS) and Health Professionals’ Follow-up (HPFS) physical activity questionnaires28,29. It also included questions about resting and sedentary habits such as overall sitting time (h/day), time watching television (h/day), time in front of a computer (h/day), sleeping (h/day), and time socializing with friends (h/day), differentiating between a typical weekday and a typical weekend day.
Additionally, participants completed a questionnaire about socio-demographic characteristics including education level, income status, marital status, school affiliation, number of children, and number of family members.
The complete full-Q was used to extract the questions included in the 28-items of the MEDLIFE questionnaire, and to score participants on their degree of compliance to the Mediterranean recommendations.
Assessment of other covariates
Additionally, participants completed a questionnaire about socio-demographic characteristics including education level, income status, marital status, school affiliation, number of children, and number of family members.
Statistical analysis
As per statistical analysis plan, the distribution of collected variables is studied prior to applying any statistical tests. All variables presented a normal distribution and no transformations were made for the analyses. Participants’ characteristics were described using means (standard deviations) and proportions. Pearson correlation coefficients were calculated to evaluate the relationship between MEDLIFE and MEDLIFE-derived from the full-Q to establish relative validity. Absolute agreement between the MEDLIFE and MEDLIFE-derived was calculated by Cohen’s kappa to assess categorical agreement between each item of the MEDLIFE (0–1) and the one obtained by MEDLIFE derived from the full-Q and by intra class correlation (ICC) and limits of agreement (LOA) methods. Agreement between the two methods was further evaluated using graphical information as described by Bland and Altman31,32. With this method the arithmetic differences in the MEDLIFE and MEDLIFE-derived for each individual was plotted against the mean values of the 2 methods. Polynomial contrasts were used to determine P-linear trend for continuous variables. Chi square tests were used to determine P-linear trend for categorical variables.
Statistical analyses were conducted using STATA, version 12.0 (STATACORP, College Station, Texas, USA).
Results
Table II shows the baseline characteristics of the 196 participants in the validation study across tertiles of MEDLIFE. No differences on percentage of participation between participants regarding the school affiliation were found. Those in the higher tertile were more likely to be older, non-smokers and reporting higher family income.
Table II.
Demographic characteristics of study participants (n = 196) by tertile (tertile 1 = low; tertile 2 = medium; tertile 3 = high) of MEDLIFE1
| Overall (n = 196) |
Low (n = 71) |
Medium (n = 70) |
High (n = 55) |
P-trend | |
|---|---|---|---|---|---|
| Female | 166 (84.7) | 55 (77.5) | 64 (91.4) | 47 (85.5) | 0.168 |
| School affiliation | |||||
| Teacher | 75 (38.3) | 21 (29.6) | 33 (47.1) | 21 (38.2) | 0.132 |
| Parent | 59 (30.1) | 22 (31.0) | 18 (25.7) | 19 (34.5) | |
| School staff | 62 (31.6) | 28 (39.4) | 19 (27.1) | 15 (27.3) | |
| Age | 41.4 (9.0) | 40.6 (8.9) | 39.5 (8.8) | 44.8 (8.7) | 0.010 |
| BMI (Kg/m) | 24.1 (4.1) | 24.5 (4.5) | 23.9 (3.9) | 23.9 (3.6) | 0.383 |
| Household income, > 22,500 € | 115 (58.7) | 23 (32.9) | 27 (38.6) | 29 (53.7) | 0.022 |
| Education level, high* | 132 (67.3) | 54 (76.1) | 54 (77.1) | 45 (81.8) | 0.541 |
| Smoking | |||||
| Current smoker | 27 (13.8) | 14 (19.7) | 9 (13) | 4 (7.3) | 0.044 |
| Non-smoker/former | 168 (85.7) | 57 (80.3) | 60 (87.0) | 51 (92.7) | 0.044 |
| Self-perceived job strain (range 0–5 points) | 3.1 (1.1) | 3.1 (1.1) | 3.1 (1.1) | 3.2 (1.0) | 0.483 |
| Self-perceived overall stress in life (range 0–5 points) | 3.1 (1.0) | 3.1 (1.1) | 3.1 (1.1) | 3.1 (0.9) | 0.923 |
| Self-perceived healthy lifestyle | 135 (68.9) | 34 (47.9) | 52 (74.3) | 49 (89.1) | < 0.001 |
Values are mean and (standard deviation) or n and (percentage).
The polynomial contrast and chi square test were used to determine P-linear trend for continuous and categorical variables, respectively.
Education level was first classified according to the guidelines of the Instituto Nacional de Estadística (INE; www.ine.es) and then categorized into three bands according to the International Standard Classification of Education (ISCED; http://www.uis.unesco.org/Education/Pages/internationalstandard-classification-of-education.aspx, 2011): low (none or primary studies; ISDED 0–2), medium (completed high school; ISCED 3 or 4) and high (high qualification or completed university degree; ISCED 5 or 6).
Table III shows the absolute agreement by kappa statistics between each component of the MEDLIFE and MEDLIFE-derived from full-Q. Very good concordance (k = 0.81–1) was observed for ‘limit salt in meals’, ‘nibbling’ and ‘nap’ (10.7% of the items). Good (k = 0.61–0.80) to moderate (k = 0.41–0.60) agreement was found for most of the items evaluated (21.4%) such as wine, moderate consumption of red meat, legumes, fruit and olive oil consumption) and fair (0.21–0.40) for 32.1% of the items. Sweets, processed meats, low fat dairy products and cereals were overestimated by MEDLIFE. From the participants who obtained 1-point for those items in the MEDLIFE, only 38%, 15%, 12% and 10 % respectively achieved 1-point as well in the MEDLIFE-derived from full-Q (item 1, 3, 9, and 15).
Table III.
Absolute agreement between lifestyle variables measures by MEDLIFE and MEDLIFE derived from full questionnaire
| MEDLIFE |
||||||||
|---|---|---|---|---|---|---|---|---|
| Criteria for 1 point | YESa | Of whom YES in MEDLIFE derivedb |
NOa | Of whom NO in MEDLIFE derivedc |
kappa | |||
| Total MEDLIFE | 0–28 | N | N | (%) | N | N | (%) | |
| Sweets | ≤ 2 s/week | 116 | 44 | (37.9) | 80 | 78 | (97.5) | 0.312 |
| Red meat | < 2 s/week | 83 | 56 | (67.5) | 113 | 107 | (94.7) | 0.643 |
| Processed meat | ≤ 1 s/week | 80 | 12 | (15.0) | 116 | 102 | (87.9) | 0.033* |
| Eggs | 2–4 s/week | 136 | 133 | (97.8) | 60 | 37 | (61.7) | 0.656 |
| Legumes | ≥ 2/ week | 90 | 80 | (88.9) | 106 | 73 | (68.9) | 0.567 |
| White meat | 2 s/ week | 99 | 79 | (79.8) | 97 | 40 | (41.2) | 0.211 |
| Fish/seafood | ≥ 2/ week | 148 | 147 | (99.3) | 48 | 7 | (14.6) | 0.194 |
| Potatoes | ≤ 3 s/week | 164 | 107 | (65.2) | 32 | 27 | (84.4) | 0.300 |
| Low fat dairy products | 2 s/day | 49 | 6 | (12.2) | 147 | 140 | (95.2) | 0.099 |
| Nuts and olives | 1–2 s/day | 37 | 16 | (43.2) | 159 | 147 | (92.5) | 0.394 |
| Herbs, spices and garnish | ≥ 1 s/day | 157 | 101 | (64.3) | 39 | 33 | (84.6) | 0.330 |
| Fruit | 3–6 s/day | 84 | 53 | (63.1) | 112 | 95 | (84.8) | 0.489 |
| Vegetables | ≥ 2 s/day | 132 | 127 | (96.2) | 64 | 17 | (26.6) | 0.274 |
| Olive oil | ≥ 3 s/day | 129 | 88 | (68.2) | 67 | 51 | (76.1) | 0.407 |
| Cereals | 3–6 s /day | 82 | 8 | (9.8) | 114 | 111 | (97.4) | 0.081 |
| Water or teas | 6–8 s/day or ≥ 3 s/ week | 139 | 69 | (49.6) | 57 | 44 | (77.2) | 0.207 |
| Wine | 1–2 s/ day | 11 | 7 | (63.6) | 185 | 184 | (99.5) | 0.724 |
| Limit salt in meals | Yes | 119 | 112 | (94.1) | 77 | 75 | (97.4) | 0.905 |
| Preference of whole grain products | yes / > 25g/day | 86 | 64 | (55.8) | 110 | 103 | (93.6) | 0.694 |
| Snacks | ≤ 2 s/week | 170 | 159 | (93.5) | 26 | 16 | (61.5) | 0.542 |
| Limit nibbling between meals | Yes | 113 | 106 | (93.8) | 83 | 80 | (96.4) | 0.896 |
| Limit sugar in beverages (including sugar-sweetened beverages) |
Yes | 144 | 83 | (57.6) | 52 | 44 | (84.6) | 0.319 |
| Physical activity (> 150min/week or 30 min/day) |
Yes | 122 | 97 | (79.5) | 74 | 42 | (56.8) | 0.370 |
| Siesta/Nap | Yes | 85 | 82 | (96.5) | 111 | 102 | (91.9) | 0.876 |
| Hours’ Sleep | 6–8 hour/day | 160 | 160 | (100) | 36 | 19 | (52.8) | 0.646 |
| TV hours | < 1hour/day | 115 | 113 | (98.3) | 81 | 63 | (77.8) | 0.783 |
| Go out with friends | ≥ 2hour/weekend | 174 | 163 | (93.7) | 22 | 14 | (63.6) | 0.541 |
| Collective sports | ≥ 2hour/week | 47 | 38 | (80.9) | 149 | 114 | (76.5) | 0.482 |
Number (N) of participants scoring 1 point in MEDLIFE (YES) or scoring 0 points in the MEDLIFE (NO).
MEDLIFE derived: MEDLIFE derived from the full FFQ. Number of participants (percentage) from those who scored 1 point (YES) in MEDLIFE and scored as well 1-point in the MEDLIFE derived from the full-Q.
MEDLIFE derived from the full FFQ. Number of participants (percentage) from those who scored 0 point (NO) in MEDLIFE and scored as well 0-point in the MEDLIFE derived from the full-Q.
p > 0.05; all other kappa values are statistically significant at p < 0.0001 except for low-fat dairy products (p = 0.034).
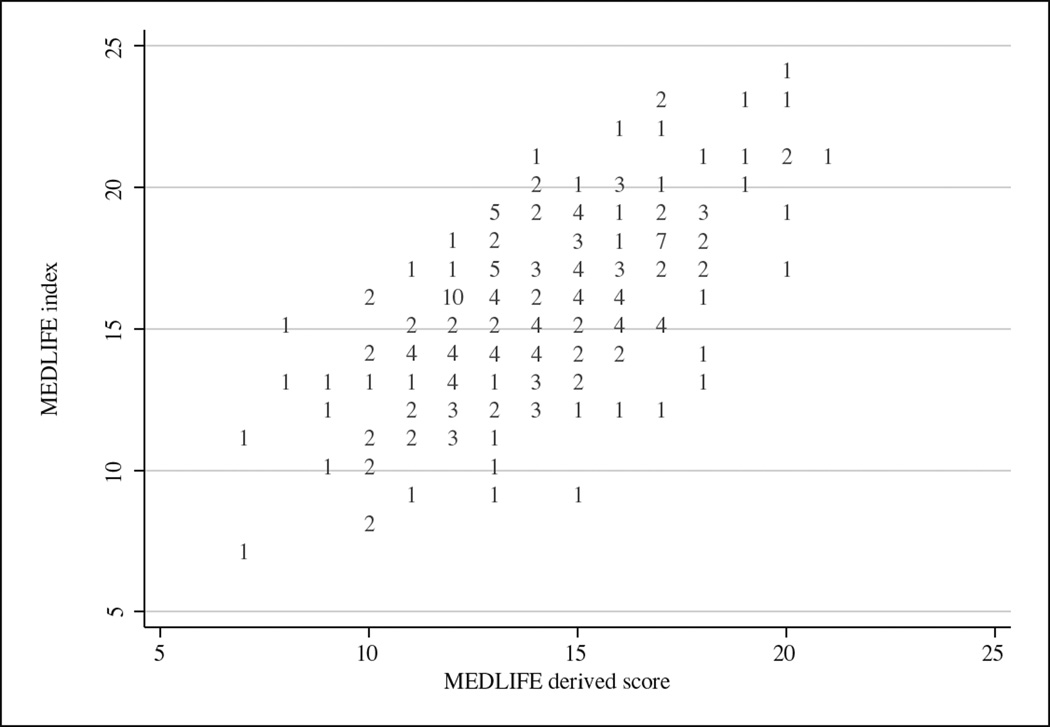
Correlation between the two instruments was 0.626. No difference by sex was observed. Consistency between both methods was assessed by ICC. A value of 0.544 (95% CI, 0.3–0.7) was calculated, suggesting that MEDLIFE has an adequate ability to rank participants by MEDLIFE-derived. Correlations between MEDLIFE and MEDLIFE individual blocks was 0.494 for MD food frequency consumption, 0.717 for MD dietary habits, and 0.663 for physical activity, rest, social habits, and conviviality. The MEDLIFE overestimated MEDLIFE-derived (15.7 ± 3.2 vs 14.1 ± 2.8, respectively) (Figure 1). In the classification analysis 52.1 % of the participants were classified in the same tertile by both instruments whereas only 7.1% were classified in the opposite tertile.
Fig. 1.
Scatter plot of MEDLIFE by MEDLI-FE derived score (numbers of plot indicate repeat values).
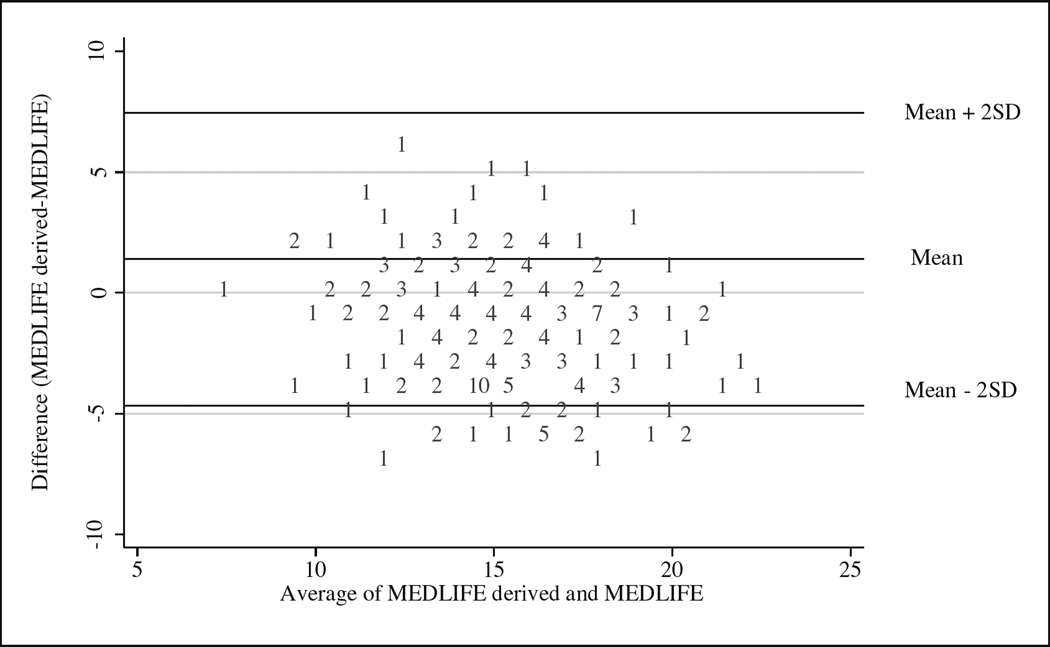
Despite the extensive use of correlation analyses to validate dietary assessment methods, correlation coefficients provide only limited measure of the level of agreement between two measurements31,32. Therefore, we calculated Limits of Agreement (LOA) and showed a Bland-Altman graphic (Figure 2). LOA mean was 1.40 and the range was −4.66 to 7.45, indicating an acceptable concordance despite the overestimation bias.
Fig. 2.
Bland-Altman plot indicating the mean difference between indices obtained from the full-Q and the corresponding to MEDLIFE vs the mean of the two indices.
Discussion
Validating an instrument designed to capture lifestyle behaviors is essential before it can be applied and extended to the general population. Few studies have verified the inter-method reliability of the indices assessing adherence to the MD11,24,25, with most studies being limited to contrasting the indices against the FFQ validity, and therefore establishing construct and content validity only. In addition, most of the indices have not been developed to be used as an independent tool in clinical or epidemiological research.
The present study was conducted to evaluate the validity of a short 28 item-questionnaire assessed by comparing it to a full, 147-item, questionnaire that included validated FFQ, physical activity questionnaire, and other questions related to traditional Mediterranean lifestyle33. Of the 28 items evaluated, nearly 60% (16 items) had an absolute agreement from very good to moderate (kappa = 0.41–1). Only three items had a poor agreement (kappa < 0.2), namely dairy products, cereals and processed meats. These results agree with the findings from several studies assessing the validity of dietary indices that supported that some specific foods (dairy products and meats) tend to show poor correlations with the dietary indices34–38. Indeed, this issue was detected during content validation of the MEDLIFE15, where these items showed a weaker correlation (dairy products ρ- = 0.11, cereals = 0.17, and processed meats = 0.18). It is likely though that the intrinsic limitations of the FFQ as a dietary assessment tool, could explain the lack of agreement in the present external validation study: The limitation to measure diet accurately seems to matter more when classifying foods into a single food category, especially because arbitrary decisions are made. These subjective choices vary between studies for specific food groups, specifically dairy foods (low-fat dairy products vs. whole fat) and cereals (whole vs. refined). Likewise, portion size and the type of processed meat are also difficult to assess. To help overcome this limitation, MEDLIFE contains specific questions on low-fat dairy products (item 9) and distinguishes between refined and whole-grain cereal products (items 15 and 19). Additionally, the lack of awareness about standard food portions and serving sizes in the general population and the different serving sizes listed in the MEDLIFE and FFQ-items could also explain some of the discrepancies for some items (e.g. for cereals, in MEDLIFE (item 15) one serving of white and whole grain bread is 40 g, for rice and pasta is one plate, and for breakfast cereals is 40 g whereas in the FFQ the serving size of white and whole grain bread is 75g, for rice and pasta is 60 g dried, before cooking, and for breakfast cereals is 30g).
In general, agreement results (kappa values) indicated a correct classification for more than half of the participants evaluated. This allows for the identification of individuals or populations with poorer adherence that could benefit from lifestyle education interventions, enhancing the efficiency of public health strategies.
Furthermore, the present study evaluated the correlation of the final composite score between both instruments showing a moderate-to-good correlation (r = 0.626, p < 0.05). These estimators of validity are comparable, or better in some instances, to those obtained in other studies11,24,25,39,40, for example MEDAS11 (r = 0.52 between the questionnaire and the FFQ), DQI-R39 (r = 0.66 between 1 week diet record and FFQ), MEDFICTS25 (r = 0.50 by block correlations except for total fat intake (r = 0.30)), and Spanish dietary history and the mean of seven 24-hour recalls r = 0.5340. In addition, when analyzing MEDLIFE by blocks, a high correlation was obtained for Mediterranean dietary habits (0.717) and social and physical activity patterns (0.663), but lower for the food frequency consumption (0.494). MEDLIFE’s questions about usual diet consumption may be more easily and accurately collected than the frequencies and portion sizes of a long list of foods in a FFQ, which could explain the lower correlation for the food frequency consumption.
Despite the accepted use of correlations to assess reliability in the analysis of dietary validation methods, its used could be misleading as they provide a limited measure of the level of agreement between two measurements31. Using an alternative graphical approach, we showed that the MEDLIFE limits of agreement (LOA) on a Bland and Altman plot were within a correct range and similar to previously validated instruments11,41–44. ICC also indicated moderate agreement (0.54) between both methods, which also compares to that of other dietary indices11,40.
The MEDLIFE, apart from being designed as a potentially easy and user-friendly independent research tool, comprises consumption of specific foods as well as other lifestyle behaviors items that belong to the traditional Mediterranean lifestyle. Yet, some of the items that we included in MEDLIFE were difficult to formulate because they have not been assessed accurately, or at all, in previous epidemiological studies. In our study, we aimed to include some of the new recommendations of the MD pyramid related to seasonality and frugality of the foods as well as conviviality, such as eating in company or the time spent having meals, which are unique cultural aspects of the Mediterranean culture. Thus, we included 4 additional items to the previous 28-items (supplementary material) but could not assess the validity of those 4 questions because they have not been included in the full-Q from which we extracted the MEDLIFE-derived to assess the validity between both instruments. Despite including three diverse groups of participants (teachers, school staff, and families) to enhance representation of the sample, more than half of the final sample had a high educational level, which could carry some bias and limit generalizability. Therefore, validating MEDLIFE in populations with lower educational levels would add further value to the applicability and optimal performance of the questionnaire. Another limitation is that the MD pyramid recommendations are targeted to a healthy adult population and may not apply to the specific needs of children, pregnant women, or people with certain health conditions. MEDLIFE should be then adapted and validated for special populations before further applications. Finally, we did not measure any biomarker in this population, therefore its predictive validity to assess clinical endpoints it is another step that should be tested in future studies.
A unique feature of the MEDLIFE that is worth highlighting is that this is the first index to measure the Mediterranean lifestyle as a whole by incorporating other traditional healthy lifestyle and cultural elements pointed out by international committees in the MD pyramid. In addition, most of the dietary indices have been developed with epidemiological purposes (derived from detailed FFQ, with complex scoring cutoffs) and unlikely the MEDLIFE its application in the general population as an independent tool to capture adherence to a healthy diet is not possible. The fact that the MEDLIFE relies on scoring positively or negatively on the different recommendations for compliance to the Mediterranean lifestyle avoids classifications or scoring based on the distribution of any particular population. The practical benefits of the MEDLIFE as a short and user-friendly structure could enhance its applications as an educational tool to promote the Mediterranean pattern or as a clinical tool to evaluate adherence.
Because educational interventions to achieve a simultaneous change in multiple health-related behaviors may be a better approach rather than only focusing on single behaviors45, the MEDLIFE could be used as an adaptable measure for researchers and policy-makers to identify key areas of concerns on which future intervention studies should focus.
In conclusion, the MEDLIFE is a reliable instrument to measure overall Mediterranean lifestyle in middle age adults from Spain that could be used as a short questionnaire in clinical and epidemiological studies. Its potential application as a predictive tool of health-related diseases and the generalization to other populations should be further explored in future studies.
Supplementary Material
Acknowledgments
The authors would like to thank the study participants, and the technical staff involved in the data collection, as well as the International SHE Foundation, intellectual owner of Program SI!.
Sources of support
Research Grant FISPI11/01885, Fondo de Investigación Sanitaria del Instituto de Salud Carlos III, Madrid, Spain (research grant PI11/01885). MSP was supported by a research fellowship from Fundación Alfonso Martín Escudero (FAME), Spain.
Footnotes
Conflict of interest
All authors declare no conflict of interest
Authorship
MSP developed the MEDLIFE, designed and coordinated the validation study, formulated the study question, conducted and designed the study and data collection, performed the statistical analysis, and interpreted and wrote the manuscript. JM interpreted data and contributed drafting the manuscript. GSB was responsible for the recruitment of participants, and data collection and interpretation of the results. PB was responsible for the recruitment of participants, and data collection. SP oversaw statistical analyses and helped draft the manuscript. JLP contribute to develop the MEDLIFE, oversaw the validation study, interpreted the results and helped draft the manuscript.
References
- 1.Patterson RE, Haines PS, Popkin BM. DIET QUALITY INDEX - CAPTURING A MULTIDIMENSIONAL BEHAVIOR. J Am Diet Assoc. 1994 Jan;94(1):57–64. doi: 10.1016/0002-8223(94)92042-7. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995 Oct;95(10):1103–1108. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 3.Estruch R, Ros E, Salas-Salvado J, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. New England Journal of Medicine. 2013 Apr 4;368(14):1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 4.Sotos-Prieto M, Angeles Zulet M, Corella D. Scientific evidence of the mediterranean diet effects in determining intermediate and final cardiovascular disease phenotypes. Medicina Clinica. 2010 Jan 23;134(1):22–29. doi: 10.1016/j.medcli.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 5.Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004 Apr;104(4):615–635. doi: 10.1016/j.jada.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Willett WC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid - a cultural model for healthy eating. Am J Clin Nutr. 1995 Jun;61(6):S1402–S1406. doi: 10.1093/ajcn/61.6.1402S. [DOI] [PubMed] [Google Scholar]
- 7.Trichopoulou A, Kourisblazos A, Wahlqvist ML, et al. Diet and overall survival in elderly people. British Medical Journal. 1995 Dec 2;311(7018):1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003 Jun 26;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 9.Alberti-Fidanza A, Fidanza F. Mediterranean Adequacy Index of Italian diets. Public Health Nutrition. 2004 Oct;7(7):937–941. doi: 10.1079/phn2004557. [DOI] [PubMed] [Google Scholar]
- 10.Schroder H, Marrugat J, Vila J, Covas MI, Elosua R. Adherence to the traditional Mediterranean diet is inversely associated with body mass index and obesity in a Spanish population. Journal of Nutrition. 2004 Dec;134(12):3355–3361. doi: 10.1093/jn/134.12.3355. [DOI] [PubMed] [Google Scholar]
- 11.Schroder H, Fito M, Estruch R, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011 Jun;141(6):1140–1145. doi: 10.3945/jn.110.135566. [DOI] [PubMed] [Google Scholar]
- 12.Buckland G, Gonzalez CA, Agudo A, et al. Adherence to the Mediterranean Diet and Risk of Coronary Heart Disease in the Spanish EPIC Cohort Study. American Journal of Epidemiology. 2009 Dec 15;170(12):1518–1529. doi: 10.1093/aje/kwp282. [DOI] [PubMed] [Google Scholar]
- 13.Bach-Faig A, Berry EM, Lairon D, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutrition. 2011 Dec;14(12):2274–2284. doi: 10.1017/S1368980011002515. [DOI] [PubMed] [Google Scholar]
- 14.Mediterranean Diet Pyramid: a lifestyle for today. 2015. Jun, http://dietame-diterranea.com/dietamed/piramide_INGLES.pdf .
- 15.Sotos-Prieto M, Moreno-Franco B, Ordovas JM, Leon M, Casasnovas JA, Penalvo JL. Design and development of an instrument to measure overall lifestyle habits for epidemiological research: the Mediterranean Lifestyle (MEDLIFE) index. Public Health Nutr. 2014 Jul;15:1–9. doi: 10.1017/S1368980014001360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Behrens G, Fischer B, Kohler S, Park Y, Hollenbeck AR, Leitzmann MF. Healthy lifestyle behaviors and decreased risk of mortality in a large prospective study of U.S. women and men. European Journal of Epidemiology. 2013;28(5):361–372. doi: 10.1007/s10654-013-9796-9. [DOI] [PubMed] [Google Scholar]
- 17.Laugero KD, Falcon LM, Tucker KL. Relationship between perceived stress and dietary and activity patterns in older adults participating in the Boston Puerto Rican Health Study. Appetite. 2011 Feb;56(1):194–204. doi: 10.1016/j.appet.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010 May;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burazeri G, Gofin J, Kark JD. Over 8 hours of sleep--marker of increased mortality in Mediterranean population: follow-up population study. Croat Med J. 2003 Apr;44(2):193–198. [PubMed] [Google Scholar]
- 20.Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index revised: a measurement instrument for populations. J Am Diet Assoc. 1999 Jun;99(6):697–704. doi: 10.1016/S0002-8223(99)00168-6. [DOI] [PubMed] [Google Scholar]
- 21.Miller PE, Mitchell DC, Harala PL, Pettit JM, Smiciklas-Wright H, Hartman TJ. Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutrition. 2011 Feb;14(2):306–313. doi: 10.1017/S1368980010001655. [DOI] [PubMed] [Google Scholar]
- 22.Toft U, Kristoffersen LH, Lau C, Borch-Johnsen K, Jorgensen T. The Dietary Quality Score: validation and association with cardiovascular risk factors: the Inter99 study. European Journal of Clinical Nutrition. 2007 Feb;61(2):270–278. doi: 10.1038/sj.ejcn.1602503. [DOI] [PubMed] [Google Scholar]
- 23.Taechangam S, Pinitchun U, Pachotikarn C. Development of nutrition education tool: healthy eating index in Thailand. Asia Pacific Journal of Clinical Nutrition. 2008;17:365–367. 2008. [PubMed] [Google Scholar]
- 24.Kris-Etherton P, Eissenstat B, Jaax S, et al. Validation for MEDFICTS, a Dietary Assessment Instrument for Evaluating Adherence to Total and Saturated Fat Recommendations of the National Cholesterol Education Program Step 1 and Step 2 Diets. J Am Diet Assoc. 2001;101(1):81–86. doi: 10.1016/S0002-8223(01)00020-7. [DOI] [PubMed] [Google Scholar]
- 25.Mochari H, Gao Q, Mosca L. Validation of the MEDFICTS dietary assessment questionnaire in a diverse population. J Am Diet Assoc. 2008 May;108(5):817–822. doi: 10.1016/j.jada.2008.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Penalvo JL, Santos-Beneit G, Sotos-Prieto M, et al. A cluster randomized trial to evaluate the efficacy of a school-based behavioral intervention for health promotion among children aged 3 to 5. BMC Public Health. 2013;13:656. doi: 10.1186/1471-2458-13-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martinez-Gonzalez MA, Lopez-Fontana C, Varo JJ, Sanchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005 Oct;8(7):920–927. doi: 10.1079/phn2005745. [DOI] [PubMed] [Google Scholar]
- 28.Chasan-Taber S, Rimm EB, Stampfer MJ, et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996 Jan;7(1):81–86. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994 Oct;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 30.de la Fuente-Arrillaga C, Ruiz ZV, Bes-Rastrollo M, Sampson L, Martinez-Gonzalez MA. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010 Sep;13(9):1364–1372. doi: 10.1017/S1368980009993065. [DOI] [PubMed] [Google Scholar]
- 31.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- 32.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999 Jun;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 33.Casasnovas JA, Alcaide V, Civeira F, et al. Aragon workers’ health study--design and cohort description. BMC Cardiovasc Disord. 2012;12:45. doi: 10.1186/1471-2261-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCullough ML, Feskanich D, Rimm EB, et al. Adherence to the Dietary Guidelines for Americans and risk of major chronic disease in men. Am J Clin Nutr. 2000 Nov;72(5):1223–1231. doi: 10.1093/ajcn/72.5.1223. [DOI] [PubMed] [Google Scholar]
- 35.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008 Nov;108(11):1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Lagiou P, Trichopoulos D, Sandin S, et al. Mediterranean dietary pattern and mortality among young women: a cohort study in Sweden. British Journal of Nutrition. 2006 Aug;96(2):384–392. doi: 10.1079/bjn20061824. [DOI] [PubMed] [Google Scholar]
- 37.Waijers PMCM, Feskens EJM, Ocke MC. A critical review of predefined diet quality scores. British Journal of Nutrition. 2007 Feb;97(2):219–231. doi: 10.1017/S0007114507250421. [DOI] [PubMed] [Google Scholar]
- 38.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014 Mar;144(3):399–407. doi: 10.3945/jn.113.183079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Newby PK, Hu FB, Rimm EB, et al. Reproducibility and validity of the Diet Quality Index Revised as assessed by use of a food-frequency questionnaire. Am J Clin Nutr. 2003 Nov;78(5):941–949. doi: 10.1093/ajcn/78.5.941. [DOI] [PubMed] [Google Scholar]
- 40.Guallar-Castillon P, Sagardui-Villamor J, Balboa-Castillo T, et al. Validity and reproducibility of a Spanish dietary history. PLoS One. 2014;9(1):e86074. doi: 10.1371/journal.pone.0086074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schroder H, Benitez Arciniega A, Soler C, Covas MI, Baena-Diez JM, Marrugat J. Validity of two short screeners for diet quality in time-limited settings. Public Health Nutr. 2012 Apr;15(4):618–626. doi: 10.1017/S1368980011001923. [DOI] [PubMed] [Google Scholar]
- 42.Rumawas ME, Dwyer JT, McKeown NM, Meigs JB, Rogers G, Jacques PF. The Development of the Mediterranean-Style Dietary Pattern Score and Its Application to the American Diet in the Framingham Offspring Cohort. Journal of Nutrition. 2009 Jun;139(6):1150–1156. doi: 10.3945/jn.109.103424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Panagiotakos DB, Pitsavos C, Stefanadis C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutrition Metabolism and Cardiovascular Diseases. 2006 Dec;16(8):559–568. doi: 10.1016/j.numecd.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Ambrosini GL, Mackerras D, de Klerk NH, Musk AW. Comparison of an Australian food-frequency questionnaire with diet records: implications for nutrition surveillance. Public Health Nutr. 2003 Jun;6(4):415–422. doi: 10.1079/PHN2002434. [DOI] [PubMed] [Google Scholar]
- 45.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006 Jul 4;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.