Abstract
Background and aims
Consensus in acknowledging compulsive buying-shopping disorder (CBSD) as a distinct diagnosis has been lacking. Before research in this area can be advanced, it is necessary to establish diagnostic criteria in order to facilitate field trials.
Methods
The study consisted of the following phases: (1) operationalization of a broad range of potential diagnostic criteria for CBSD, (2) two iterative rounds of data collection using the Delphi method, where consensus of potential diagnostic criteria for CBSD was reached by an international expert panel, and (3) interpretation of findings taking into account the degree of certainty amongst experts regarding their responses.
Results
With respect to diagnostic criteria, there was clear expert consensus about inclusion of the persistent and recurrent experience of (a) intrusive and/or irresistible urges and/or impulses and/or cravings and/or preoccupations for buying/shopping; (b) diminished control over buying/shopping; (c) excessive purchasing of items without utilizing them for their intended purposes, (d) use of buying-shopping to regulate internal states; (e) negative consequences and impairment in important areas of functioning due to buying/shopping; (f) emotional and cognitive symptoms upon cessation of excessive buying/shopping; and (g) maintenance or escalation of dysfunctional buying/shopping behaviors despite negative consequences. Furthermore, support was found for a specifier related to the presence of excessive hoarding of purchased items.
Conclusions
The proposed diagnostic criteria can be used as the basis for the development of diagnostic interviews and measures of CBSD severity.
Keywords: compulsive buying-shopping disorder, compulsive buying, diagnostic criteria, Delphi study, behavioral addiction, impulse control disorder
Introduction
Described for well over 100 years of clinical history, excessive and dysfunctional preoccupations, impulses, urges, cravings and/or behaviors associated with buying or shopping are linked to significant clinical distress and impairment in social, occupational, financial and other important areas of functioning (Black, 2007; Dell'Osso, Allen, Altamura, Buoli, & Hollander, 2008; Lejoyeux & Weinstein, 2010; Müller, Brand, et al., 2019). In 1899, Emil Kraepelin first mentioned the “pathological propensity to buy” alongside kleptomania and “acquisitiveness” (Kraepelin, 1899). He named the phenomenon “oniomania” and considered it an impulse control disorder characterized by uncontrolled shopping and spending, with unremitting delay in payments, accumulation of debts, and the inability to disengage cognitively or to apprehend the negative consequences of buying excesses (Kraepelin, 1909). To date, various other terms can be found in the literature, e.g., compulsive buying (McElroy, Keck, Pope, Smith, & Strakowski, 1994), pathological buying (Müller, Trotzke, Mitchell, de Zwaan, & Brand, 2015), shopping addiction (Lo & Harvey, 2012) and, more recently, buying-shopping disorder (BSD; Kyrios et al., 2018; Müller, Brand, et al., 2019) or compulsive buying-shopping disorder (CBSD; WHO, 2019). The latter term is used in the coding tool of the 11th revision of the International Classification of Diseases (ICD-11) where the phenomenon is currently mentioned as an example for “other specified impulse control disorders” (WHO, 2019). CBSD refers to both, disordered acquisition of consumer goods by paying for them and the activity of looking for things to buy without necessarily purchasing them (e.g., “window shopping”, browsing shopping websites on the internet, or failing to buy due to financial challenges) (Bloch & Richins, 1983). Nowadays, with an ever-growing online retail market, excessive dysfunctional browsing through shopping websites should not be overlooked as it represents a specific feature of CBSD in the modern context (Müller, Steins-Loeber, et al., 2019; Rose & Dhandayudham, 2014; Trotzke, Starcke, Müller, & Brand, 2015). In the following, we will use the term CBSD to be consistent with the ICD-11 coding tool.
Over the past three decades, the public health importance of CBSD has become apparent. Population-based prevalence estimates of about 5% suggest that it is a prevailing condition within different cultural settings (Koran, Faber, Aboujaoude, Large, & Serpe, 2006; Maraz, Griffiths, & Demetrovics, 2016; Müller et al., 2015; Otero-López & Villardefrancos, 2014). In recent years, the negative consequences (e.g., distress, impairment) and underlying psychological and neuropsychological mechanisms of CBSD have emerged from various studies (Black, Shaw, & Allen, 2016; Claes, Luyckx, Vogel, Verschueren, & Müller, 2018; Granero, Fernández-Aranda, Baño, et al., 2016; Kyrios et al., 2018; Moulding, Duong, Nedeljkovic, & Kyrios, 2017; Trotzke, Brand, & Starcke, 2017). Despite this, CBSD is not included in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (APA, 2013) or ICD-11 (WHO, 2019) as an independent mental disorder. According to some researchers, the conceptualization as a formal diagnosis was not justified based on the relative lack of published scientific literature, particularly in terms of neurobiology and genetics (Grant & Chamberlain, 2016; Grant et al., 2014).
Nonetheless, continual research and discourse has maintained interest in establishing diagnostic criteria for buying and shopping problems, as has the inclusion of disorders such as gambling disorder, gaming disorder and hoarding disorder in the DSM-5 and ICD-11 (Fontenelle & Grant, 2014; Grant & Chamberlain, 2016; Grant et al., 2014; Mann, Fauth-Bühler, Higuchi, Potenza, & Saunders, 2016; Potenza, Higuchi, & Brand, 2018). While “CBSD” is considered to be an example in the residual ICD-11 category “other specified impulse control disorders” (category 6C7Y) (WHO, 2019), some researchers suggest that CBSD is better classified as an “other specified disorder due to addictive behaviors” (Brand, Rumpf, Demetrovics, et al., 2020; Granero, Fernández-Aranda, Mestre-Bach, et al., 2016; Müller, Brand, et al., 2019; Potenza et al., 2018). Excessive buying is also mentioned as a core feature of hoarding disorder (i.e., “repetitive urges or behaviors related to amassing or buying items”) in the ICD-11 (WHO, 2019) and as one form of excessive acquisition within the hoarding disorder specifier “with excessive acquisition” in the DSM-5 (APA, 2013). Moreover, “engaging in unrestrained buying sprees” is considered a symptom of borderline personality disorder and manic/hypomanic episodes in the DSM-5 (APA, 2013).
While McElroy et al. (1994) proposed operational criteria to diagnose compulsive buying more than 25 years ago, these were marked as preliminary and were developed to mirror the DSM-III-R (APA, 1987) diagnostic criteria for obsessive-compulsive, impulse control (particularly pathological gambling) and substance use disorders. The criteria focused on the importance of maladaptive preoccupations with buying or shopping, along with related impulses and behaviors that cause marked distress or interference, and which are not experienced exclusively during hypomanic or manic episodes. The criteria were widely used and stimulated research, but their clinical utility, reliability and validity were never specified nor evaluated systematically.
As with other mental disorders (First, Reed, Hyman, & Saxena, 2015; Grant & Chamberlain, 2016), there is no doubt that the clarification of diagnostic criteria for CBSD is crucial for the advancement of research on the topic, health care and appropriate health policy (Hollander & Allen, 2006; Müller, Brand, et al., 2019). One methodological approach that has been used in other areas of diagnostic uncertainty is the Delphi process. This approach was originally known as a method for forecasting, but has since been used in many other areas, including mental health settings (Castro-Calvo et al., 2021; Donohoe, Stellefson, & Tennant, 2012; Jorm, 2015; Yücel et al., 2019). It uses a systematic progression of repeated rounds of voting to determine expert consensus for a problem where precise information is lacking (Häder & Häder, 2000; Jorm, 2015). Experts are repeatedly asked to rate proposed criteria in iterative rounds until an a priori defined consensus (mostly percent agreement) is reached among them (Diamond et al., 2014; Häder, 2014). Alternatively, a pre-defined number of rounds can be conducted (Diamond et al., 2014; Häder, 2014). After each round, criteria that did not reach consensus are presented in a subsequent round for re-rating together with structured, summarized feedback about the ratings given by the same panel in the previous round (Häder & Häder, 2000).
The Delphi method offers several advantages that are of relevance for the current study, particularly diversity and anonymity. Diversity refers to a procedure synthesizing opinions from a heterogeneous group of experts in order to reach a consensus that may represent a better estimate than the consensus of a small, homogeneous expert group (Jorm, 2015; Surowiecki, 2004). Anonymity refers to the fact that participants of the panel do not know the identity of other experts, which enables each to make an independent decision, without being influenced by the dominance of other experts in the field, public opinions, socio-cultural standards or academic peer pressure (Häder, 2014). In the present study, the Delphi process was applied to garner the collective views of international expert researchers and clinicians and to draft diagnostic criteria for CBSD. Such proposed diagnostic criteria could then be validated in future field trials and used as the basis for the development of structured diagnostic interviews and measures of CBSD severity.
Methods
The current study consisted of the following phases: (1) operationalization of a broad range of potential diagnostic criteria for CBSD, based on previous literature and clinical experience, (2) two iterative rounds of data collection using the Delphi method, where consensus of potential diagnostic criteria for CBSD was reached by the expert panel, and (3) interpretation of findings by accounting for the degree of certainty amongst experts regarding their answers. Conducting two rounds was pre-specified in order to minimize attrition bias. According to the literature and the authors' experience with Delphi studies, larger panels and more items included in the survey are related to high attritions rates from the 2nd to 3rd round (Gargon, Crew, Burnside, & Williamson, 2019; Häder, 2014; Häder & Häder, 2000).
Questionnaire development
A questionnaire to assess the views of the expert panel about CBSD was developed by the study team (AM, NML, PT, MK, KA, DF). Given that the terminology and classification of CBSD are still controversially debated, the broader term “buying-shopping disorder” was used throughout the questionnaire (instead of “compulsive buying-shopping disorder”). Such a term is also consistent with DSM-5 (APA, 2013) terminology for other disorders such as hoarding disorder and gambling disorder. The items of the questionnaire were developed based on (a) relevant literature on CBSD, (b) clinical and research experience of the authors and (c) DSM-5 criteria for other disorders (e.g., gambling, gaming, hoarding, obsessive compulsive, impulse control disorders). Individual items were then reviewed by the study team using an agnostic approach to the nature of CBSD as an impulse control, obsessive-compulsive spectrum, mood disorder or behavioral addiction. Furthermore, we erred on the side of overinclusion to capture a broad range of items in order to allow the expert panel to make decisions about their inclusion or exclusion.
The final survey for the first round of the Delphi process consisted of 91 questions, including 37 suggested diagnostic criteria grouped into the following six different domains: (1) preoccupations/obsessions/impulses, (2) craving/emotion regulation, (3) loss of control/self-control, (4) tolerance, (5) withdrawal, and (6) negative consequences. For the purpose of assessing divergent validity, four out of the 37 criteria were filler items that encompassed key features of other DSM-5 mental disorders (e.g., posttraumatic stress disorder) or aspects that were likely irrelevant diagnostically (e.g., “upsetting memories of buying/shopping events”). The importance of each criterion with regard to the diagnosis of CBSD was rated by the experts (i.e., “How important do you think…”) using a 4-point scale (1 = irrelevant, 2 = peripheral, 3 = important, 4 = essential) which allowed dichotomizing of answers into agreement (i.e., important and essential) and disagreement (i.e., irrelevant and peripheral). Further, participants could indicate whether they were uncertain about the importance of a potential diagnostic criterion (i.e., “I don't know”).
We also included items regarding other aspects of CBSD formatted as “yes”, “no” or “I don't know”. Respondents who answered “yes” to those filter questions were then asked subsequent open-ended questions. For example, if the filter question “Do you think a frequency item (i.e., number of buying-shopping episodes) is needed for the diagnosis of buying-shopping disorder?” was answered with “yes”, the attached open-ended item was “How many buying/shopping episodes should occur during a certain period of time (e.g., 1 per week, 2 per week, other)?”. Other filter questions asked whether CBSD should be considered a distinct mental disorder and, if “yes”, how it should be classified and labeled.
The survey further comprised three items referring to potential differential diagnoses of CBSD (e.g., “Excessive buying/shopping does not occur exclusively during a period of mania/hypomania.”) and four items concerning potential specifiers (e.g., “predominantly offline vs. predominantly online”), including one filler item (“with vs. without binge eating disorder”).
To evaluate the quality of responses, participants were asked several times to indicate how certain they were about their answers using a 5-point scale (response format: 1 = not at all sure, 2 = uncertain, 3 = neither certain nor uncertain, 4 = certain, 5 = absolutely sure). Further, participants could suggest missing or additional information about potential diagnostic criteria or other aspects of CBSD by answering open-ended questions throughout the survey (e.g., “Are there any other characteristics that are missing?”, “Please indicate whether you would add any diagnostic criterion/characteristic that has not been listed here but should be included.”).
Sociodemographic information relating to participants and their relevant expertise (i.e., English proficiency, age, gender, profession, field of work, country of work; how many years they had been assessing or treating individuals with CBSD; how many individuals they had assessed or treated in the past 12 months) was collected. Finally, participants were asked to indicate their own perceived degree of expertise in the field of CBSD (“How would you describe your level of knowledge and experience related to buying-shopping disorder?”, response format: 1 = none, 2 = a little, 3 = a moderate amount, 4 = quite a bit, 5 = a great deal; or “I don't know”).
Consensus rules
Consensus regarding the importance of an item was reached when ≥75% of the entire expert panel and ≥75% of the subsample of self-identified master experts either agreed (i.e., important and essential ratings were collapsed) or disagreed (i.e., irrelevant and peripheral ratings were collapsed) on the same item. Seventy-five percent was chosen as an appropriate cut-off based on previous recommendations (Häder, 2014; Häder & Häder, 2000).
Expert panel recruitment
A literature search was conducted using four databases (PubMed, PubPsych, Scopus, Web of Science). The following keywords were searched to identify experts in the area of CBSD from a variety of disciplines (Donohoe et al., 2012; Häder, 2014): compulsive buying, pathological buying, buying disorder, BSD, addictive buying, shopping addiction, shopping disorder, impulsive buying and oniomania. Consistent with previous studies using a similar approach (Addington, McKenzie, Norman, Wang, & Bond, 2013), the first and last authors of the publications were invited via email to participate in the study to achieve expert panel diversity.
The first round of the Delphi process
The first round of the Delphi process was open from December 2018 until March 2019. Participants were presented with the questionnaire described above. In line with the total design method, three reminders were sent if participants did not respond to the invitation (Dillman, 1978; Donohoe et al., 2012).
The second round of the Delphi process
The second round of the Delphi process was open from August 2019 until November 2019. Items for which consensus had been reached in the first round (i.e., ≥75% of the entire expert panel and ≥75% of the subsample of master experts) were not presented in the second round (Diamond et al., 2014; Häder, 2014). Participants were asked to rerate the diagnostic suitability of items for which consensus was not reached in the first round. Anonymous feedback was presented regarding the distribution of all experts' responses (i.e., entire expert panel) from the first round (e.g., “9% answered irrelevant, 41% answered peripheral, 34% answered important, 16% answered essential”). Additional potential diagnostic criteria that were suggested by participants in the first round (i.e., responses to open-ended questions) were carefully evaluated by the study team (AM, NML, PT, MK, KA, DF) and included in the second round if they did not duplicate items from the first round and were not covered by other included criteria. Criteria proposed by different experts which referred to the same aspect were collapsed into a single item, worded in a way that was consistent with other items of the survey, and highlighted as new items. Items were not included if they were too specific or vague or if they were not within the scope of the study. The most frequent answers to the open-ended questions from the first round (e.g., “If you believe that buying-shopping disorder is a distinct psychiatric diagnosis, what should it be called?”) were categorized in a drop-down list and participants were asked to choose a single option from the lists (e.g., “What should it be called: shopping addiction OR buying-shopping disorder OR compulsive buying disorder?).
The final survey for the second round consisted of 79 questions: 22 items suggesting potential diagnostic criteria for CBSD, eight items referring to specific other aspects of CBSD (e.g., frequency item), 32 items asking how certain the experts were about their answers, four open-ended questions (e.g., “If you wish to add any further comments, please use the space provided below.”), five items referring to differential diagnoses of CBSD, and another eight items concerning potential specifiers of a CBSD diagnosis. Consensus criteria were the same as in the first round of the Delphi process.
Statistical analysis
Statistical analyses were conducted using SPSS version 26 (IBM Corp., Armonk, NY, USA). For all items that were based on 4-point (i.e., items suggesting diagnostic criteria) or 5-point scales (certainty ratings to evaluate the quality of responses) we report means, standard deviations (SD), medians (Md) and interquartile ranges (IQR). Furthermore, frequencies and percentages are listed for each answer (e.g., irrelevant, peripheral, important, essential). Responses to items inquiring about the importance of diagnostic criteria were then dichotomized in order to calculate frequencies and percentages of agreement (i.e., important and essential) or disagreement (i.e., irrelevant and peripheral) with the suggested criteria, as described above.
Ethics
To recruit international experts and allow for timely responses, the Delphi study was conducted using an online survey created with SoSci Survey version 3.2.00 (SoSci Survey GmbH, Munich, Germany). Experts in the field of CBSD (see below for expert panel recruitment) were invited via personalized emails to participate in the study entitled “Development of diagnostic criteria for buying-shopping disorder using the Delphi method”. An information statement at the beginning of the survey included the aims of the study and the academic, confidential and anonymous nature of the survey in accordance with the principles of the Declaration of Helsinki and the EU data protection regulations. Before commencing the survey, participants provided digital informed consent. Compensation for study participation was not provided. Ethical approval was obtained from the review board of the Hannover Medical School, Germany (No. 8081-BO-K-2018).
Results
Participant flow
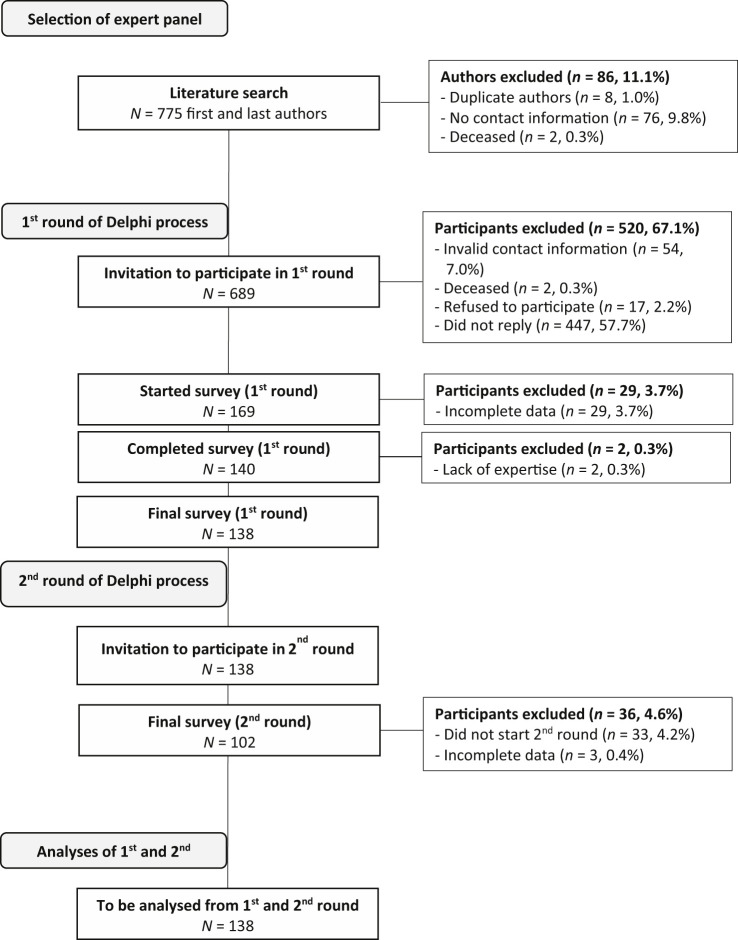
The participant flow is detailed in Fig. 1. The literature search resulted in 775 first or last authors in the field of CBSD. Eighty-six authors (11.1%) were removed from this list due to duplicate author names, missing contact information, or because authors were deceased. Consequently, invitations to participate in the study were emailed to 689 experts of which 54 could not be contacted (i.e., invalid contact information), 2 had deceased, 17 refused to participate and 445 did not reply. From the remaining 169 consenters who started round 1, 140 completed the survey (20.3% gross response rate/22.1% net response rate of invited participants). In addition, data from two participants had to be excluded due to self-identified lack of expertise in the CBSD field (i.e., the item “How would you describe your level of knowledge and experience related to buying-shopping disorder?” was answered with “none”). The final round 1 sample for data analysis consisted of 138 experts from 35 countries. They were subsequently invited to take part in the second round of the study, which was completed by 102 experts from 26 countries (response rate 73.9% of invited participants for the 2nd round).
Fig. 1.
Participant flow for round 1 and 2
Sample characteristics
Sample characteristics are presented in Table 1. Those participants who responded to the question “How would you describe your level of knowledge and experience related to buying-shopping disorder?” with “a great deal” were categorized as self-identified “master experts” in order to define a subdivision of greater self-perceived expertise and knowledge (Dalkey, Brown, & Cochran, 1969; Michael Häder, 2014). Analyses were performed for the entire expert panel as well as for the subgroup of master experts separately.
Table 1.
Sociodemographics and level of expertise of the experts in round 1 and 2
| Round 1 | Round 2 | |||
| Total expert panel | Subgroup of master experts | Total expert panel | Subgroup of master experts | |
| Gender | N = 137 | n = 35 | N = 102 | n = 27 |
| Male, n (%) | 76 (55.5) | 23 (65.7) | 56 (54.9) | 16 (59.3) |
| Female, n (%) | 61 (44.5) | 12 (34.3) | 46 (45.1) | 11 (40.7) |
| Age, mean (SD) | N = 129 | n = 32 | N = 98 | n = 26 |
| 49.34 (11.19) | 54.31 (11.67) | 49.11 (11.31) | 52.65 (10.61) | |
| Country of work (including multiple answers) | N = 138 | n = 34 | N = 101 | n = 25 |
| United States of America, n (%) | 25 (18.1) | 9 (26.5) | 15 (14.9) | 5 (20.0) |
| Germany, n (%) | 20 (14.5) | 3 (8.8) | 19 (18.8) | 3 (12.0) |
| Italy, n (%) | 11 (8.0) | 2 (5.9) | 6 (5.9) | 2 (8.0) |
| Spain, n (%) | 10 (7.2) | 3 (8.8) | 9 (8.9) | 3 (12.0) |
| France, n (%) | 8 (5.8) | 1 (2.9) | 6 (5.9) | 1 (4.0) |
| United Kingdom, n (%) | 7 (5.1) | 2 (5.9) | 4 (4.0) | 1 (4.0) |
| Australia, n (%) | 7 (5.1) | 1 (2.9) | 7 (6.9) | 1 (4.0) |
| Brazil, n (%) | 6 (4.3) | 2 (5.9) | 5 (5.0) | 2 (8.0) |
| The Netherlands, n (%) | 6 (4.3) | 2 (5.9) | 5 (5.0) | 2 (8.0) |
| Other, n (%)a,b | 38 (27.5) | 9 (26.5) | 25 (24.8) | 5 (20.0) |
| Proficiency in English | N = 138 | n = 35 | N = 102 | n = 27 |
| Elementary proficiency, n (%) | 2 (1.4) | 1 (2.9) | 2 (2.0) | 1 (3.7) |
| Limited working proficiency, n (%) | 9 (6.5) | - | 7 (6.9) | - |
| Professional working proficiency, n (%) | 47 (34.1) | 13 (37.1) | 36 (35.3) | 10 (37.0) |
| Full professional proficiency, n (%) | 37 (26.8) | 6 (17.1) | 27 (26.5) | 4 (14.8) |
| Native or bilingual proficiency, n (%) | 43 (31.2) | 15 (42.9) | 30 (29.4) | 12 (44.4) |
| Area of profession | N = 138 | n = 35 | N = 102 | n = 27 |
| Psychology, n (%) | 67 (48.8) | 10 (28.6) | 53 (52.0) | 10 (37.0) |
| Medicine, n (%) | 43 (31.2) | 18 (51.4) | 32 (31.4) | 12 (44.4) |
| Public health, n (%) | 2 (1.4) | - | 1 (1.0) | - |
| Social work, n (%) | 1 (0.7) | - | 1 (1.0) | - |
| Consumer research, n (%) | 20 (14.5) | 7 (20.0) | 10 (9.8) | 5 (18.5) |
| Other, n (%) | 5 (3.6) | - | 5 (4.9) | - |
| Field of work: clinical context | N = 130 | n = 31 | N = 95 | n = 23 |
| Yes, n (%) | 74 (56.9) | 23 (74.2) | 59 (62.1) | 18 (78.3) |
| No, n (%) | 56 (43.1) | 8 (25.8) | 36 (37.9) | 5 (21.7) |
| Knowledge/experience related to BSD | N = 138 | n = 35 | N = 102 | n = 27 |
| None, n (%) | - | - | - | - |
| A little, n (%) | 10 (7.2) | - | 7 (6.9) | - |
| A moderate amount, n (%) | 40 (29.0) | - | 28 (27.5) | - |
| Quite a bit, n (%) | 53 (38.4) | - | 40 (39.2) | - |
| A great deal, n (%) | 35 (25.4) | 35 (100) | 27 (26.5) | 27 (100) |
| Years of treating/assessing individuals | N = 133 | n =32 | N = 99 | n = 24 |
| with BSD, mean (SD) | 7.27 (8.40) | 13.19 (8.78) | 7.59 (8.36) | 12.50 (8.54) |
| Treated/assessed individuals with BSD in the past 12 months | N = 135 | n = 34 | N = 101 | n = 27 |
| Never, n (%) | 65 (48.1) | 10 (29.4) | 44 (43.6) | 7 (25.9) |
| Rarely: less than once per month, n (%) | 30 (22.2) | 6 (17.6) | 24 (23.8) | 5 (18.5) |
| Sometimes: a couple of times a month, n (%) | 23 (17.0) | 6 (17.6) | 18 (17.8) | 4 (14.8) |
| Often: about once a week, n (%) | 13 (9.6) | 8 (23.5) | 11 (10.9) | 7 (25.9) |
| Very frequently: multiple times per week, n (%) | 4 (3.0) | 4 (11.8) | 4 (4.0) | 4 (14.8) |
Note: BSD = buying-shopping disorder.
Other countries round 1 (total expert panel): Canada (n = 5), Turkey (n = 5), Switzerland (n = 3), Denmark (n = 2), China (n = 2), all n = 1: Africa, Austria, Belgium, Ecuador, Hungary, Iceland, India, Iran, Israel, Lebanon, Luxemburg, Norway, Poland, Portugal, Russia, Singapore, South Korea, Thailand, Taiwan, The United Arab Emirates, several countries (undefined).
Other countries round 1 (subsample of master experts): Turkey (n = 2), all n = 1: Austria, Canada, Denmark, Israel, Lebanon, Luxemburg, Poland.
Other countries round 2 (total expert panel): Canada (n = 4), Turkey (n = 4), Switzerland (n = 2), Denmark (n = 2), all n = 1: Africa, Belgium, China, Ecuador, Hungary, Iceland, Israel, Luxemburg, Portugal, Russia, Singapore, The United Arab Emirates, Thailand.
Other countries round 2 (subsample of master experts): all n = 1: Canada, Denmark, Israel, Luxemburg, Turkey.
About one third of participants reported working either in the United States or Germany. On average, participants judged their English language skills as very good, ranging from professional to native proficiencies. Most participants reported working in the field of psychology, followed by medicine, and consumer research. More than half of the expert panel and about three quarters of the master experts were working in a clinical context (e.g., clinical psychology, psychiatry, psychotherapy, psychosomatic medicine). The total expert panel had assessed, treated or investigated CBSD for 7.5 years on average, while the self-identified master subset of experts reported experience with CBSD of 13 years on average. Almost half of the entire expert panel had not seen clients with CBSD during the past year. In round 1, 35.3% of master experts admitted that they had seen a patient with CBSD at least once per week, compared to only 12.6% of the total expert panel. In round 2, 40.7% of master experts and 14.9% of the total panel had seen those patients.
Results of the Delphi process
Classification and terminology
Results with respect to classification and terminology of CBSD are listed in Table 2. In the first round, consensus that CBSD should be considered a distinct mental health disorder was not reached as the cut-off for agreement was missed narrowly in the total expert panel (74%). However, in the second round, both the total and the master expert group reached threshold for agreement on the recognition of CBSD as a separate mental disorder. In the first round, the entire expert panel favored the classification of CBSD as a disorder due to addictive behavior with most master experts voting for the categorization as an impulse control disorder. In the second round, both the entire panel, as well as the subsample of master experts, consented for the classification of CBSD as a disorder due to addictive behavior.
Table 2.
Classification and terminology of CBSD
| Round 1 | Round 2 | |||
| Total expert panel | Subgroup of master experts | Total expert panel | Subgroup of master experts | |
| Do you think BSD is a distinct psychiatric diagnosis? | N = 123 | n = 32 | N = 101 | n = 27 |
| Yes, n (%) | 91 (74.0) | 28 (87.5) | 83 (82.2) | 24 (88.9) |
| No, n (%) | 32 (26.0) | 4 (12.5) | 18 (17.8) | 3 (11.1) |
| How should BSD be classified? | N = 89 | n = 28 | N = 80 | n = 24 |
| Impulse control disorder, n (%) | 32 (36.0) | 13 (46.4) | 19 (23.8) | 7 (29.2) |
| Disorder due to addictive behaviors, n (%) | 48 (53.9) | 11 (39.3) | 59 (73.8) | 16 (66.7) |
| Obsessive compulsive disorder, n (%) | 5 (5.6) | 2 (7.1) | 2 (2.5) | 1 (4.2) |
| Other, n (%) | 4 (4.5) | 2 (7.1) | – | – |
| What should BSD be called? | – | – | N = 83 | n = 24 |
| Compulsive buying disorder, n (%) | – | – | 46 (55.4) | 16 (66.7) |
| Buying-shopping disorder, n (%) | – | – | 32 (38.6) | 6 (25.0) |
| Shopping addiction, n (%) | – | – | 5 (6.0) | 2 (8.3) |
Note: BSD = buying-shopping disorder.
In the first round, experts were asked to respond to an open-ended question about the proposed name of the disorder. A variety of terms were suggested from which the following most common names were presented to participants in the second round: shopping addiction, buying-shopping disorder, compulsive buying disorder. In round 2, experts then mostly agreed on “compulsive buying disorder” as the preferred term (55.4% of round 2 participants; 66.7% of round 2 master experts).
Characteristics of CBSD grouped into the predefined domains
A detailed description of experts' importance ratings in round 1 and 2 of the Delphi process is provided in the Supplementary Table S1. Below, we focus on criteria that obtained experts' consensus.
Preoccupations/obsessions/impulses
Experts agreed on the importance of the following characteristics of CBSD in the first round: “preoccupations”, “inability to stop thinking about buying/shopping” and “repetitive impulses to buy/shop”. In the second round, consensus was reached on the importance of “obsessions” and “repetitive intrusive thoughts” in CBSD. The item “upsetting memories of buying/shopping events in the context of BSD” was included for means of divergent validity. Experts rejected this filler item in the second round.
2. Craving/emotion regulation
In the first round, consensus was reached with regard to the importance of “strong or irresistible desire to buy/shop”, “irresistible urge to engage in buying/shopping activities”, “craving for the high while buying/shopping”, “buying/shopping disorder is used to generate positive emotions” and “buying/shopping is used to regulate negative emotions”. The filler item “buying/shopping is used to send a message to others” was rejected. Following the suggestions of some experts in the first round, the item “craving for relief from negative internal states” was included in the second round and obtained high consensus level.
3. Loss of control/self-control
In the first round, the items “loss of control/self-control”, “spending much more time buying/shopping than intended”, “buying many more things or spending more than necessarily needed/intended” and “repeated unsuccessful efforts to reduce or control buying/shopping” were endorsed. In the second round, agreement was reached on “buying many more things than can be afforded”, “buying/shopping something on the spur of the moment” and “repeated unsuccessful efforts to stop thinking about buying/shopping”.
4. Tolerance
None of the proposed tolerance criteria were endorsed or rejected in the first round. For means of divergent validity, the filler item “to experience desired excitement or relief from negative feelings more and more diverse things need to be bought” was listed in the first round. It was rejected by the master subgroup but not by the total expert panel. However, this item was rejected by both the total panel and the master subgroup in the second round. No consensus was reached on any of the other items, whereas a trend towards refusal was observed (see Table S1).
5. Withdrawal
In the first round, agreement was reached on the criterion “reduction or cessation of buying/shopping results in emotional symptoms: e.g., anxiety, restlessness, agitation, impatience, sadness, irritability, dysphoria, uncertainty, insecurity, anger, sustained tension”. As expected, the filler item “reduction or cessation of buying/shopping results in psychotic symptoms: e.g., delusion, hallucinations, disorganized speech” was rejected. In the second round, the criterion “reduction or cessation of buying/shopping results in cognitive symptoms: e.g., increasing worries, rumination, distractibility, cognitive constriction on shopping/buying, attentional biases towards shopping/buying stimuli” was accepted.
6. Negative consequences
In the first round, negative consequences such as “clinically significant distress”, “negative feelings e.g., shame, guilt, embarrassment, regret”, “impairment in social life e.g., familial discord, jeopardizing relationships”, “impairment in other important areas of functioning e.g., everyday activities and hobbies, daily responsibilities”, “financial difficulties including indebtedness, bankruptcy” and “lying to others about buying/shopping alone/in secret, hiding bought goods” were accepted. In the second round, further consensus was reached on the consequences “impairment in occupational areas e.g., risking career opportunities” and “loss of interest in other life activities and hobbies”. The consequence “delinquency e.g., deceptions, embezzlement, theft or other illegal behaviors” was rejected.
Other phenomenological characteristics of CBSD
In response to suggestions by some experts in the first round (i.e., answers to open-ended questions), the second round included additional items regarding phenomenological aspects of CBSD that did not fit into the six domains described above. The importance ratings for those items are also shown in the Supplementary Table S1.
Experts demonstrated high agreement levels on the criterion “maintenance or escalation of buying/shopping despite negative consequences (e.g., clinically significant distress, negative feelings, impairment in social life, impairment in other important areas of functioning, financial difficulties, lying to others about buying/shopping)” (agreement: total experts 96.1%, master experts 92.6%). They further rated “buying items without utilizing them for their intended purposes” as an important diagnostic criterion of CBSD (agreement: total experts 75.2%, master experts 77.8%). In contrast, no consensus was reached about the importance of “the average proportion of income spent per month on buying items” and “returning purchased items without utilizing them”.
Differential diagnoses
Importance ratings for potential differential diagnoses for CBSD are also presented in the Supplementary Table S1. In the first round, consensus was reached for the differentiation of excessive buying/shopping in the context of CBSD from “mania/hypomania” and “organic psychosyndrome”. In the second round, agreement emerged that “psychosis” should further be considered as a differential diagnosis. Following the suggestions of some experts, “excessive buying/shopping exclusively during a period of dopaminergic medication” and “acquisition of purchased or free items as a result of hoarding disorder” were added as potential differential diagnoses in the second round. While no consensus was reached on those items, it should be noted that the total expert panel approved “dopaminergic medication” as a differential diagnosis (agreement 83.1%), whereas the subsample of master experts did not (agreement 73.9%).
The second round included two additional questions about the co-occurrence of CBSD in the context of other disorders using a “yes/no” format. Experts agreed that “a diagnosis of buying-shopping disorder can co-occur in the context of hoarding disorder” (77.5% of the total expert panel, 75% of the master group). Likewise, experts highly agreed that “a diagnosis of buying-shopping disorder can co-occur in the context of borderline and/or other personality disorders” (88.5% of the total expert panel, 85.2% of the master group).
Specifiers
As defined, there was no consensus on specifiers for CBSD (see Table S1). The filler item “with vs. without binge eating disorder” was rejected in the first round. The suggested specifier “with vs. without hoarding disorder” just missed consensus in the second round amongst the entire expert panel (74%), although 77.8% of the master subgroup approved this specifier.
Frequency and time criteria
The survey included some filter items formatted as “yes” or “no” to inquire about frequency and time criteria of CBSD. If those questions were answered with “yes”, subsequent open-ended questions or drop-down lists of potential answers were presented (see Method). In the first round, no agreement was reached with respect to frequency and time criteria for CBSD. In the second round, the question “Do you think a frequency item (i.e., number of buying/shopping episodes) is needed for the diagnosis of BSD?” was answered by 96 of the 102 experts from which only 64 of the total expert panel (66.7%) agreed. Likewise, only five of the 25 master experts voted for a frequency item. The subsequent question “If yes: How many buying/shopping episodes should occur during a certain period of time: 1 per week/2 per week/3 per week?” was answered by 32 of the 64 experts (including 5 master experts). Twenty-three experts of the total panel and four of the five included master experts selected the frequency criterion “1 per week”. Another question asked about the duration of CBSD symptoms: “How long should this criterion last: 3 months/6 months/1 year?”. Thirty-two of the 64 experts responded to this question with 18 participants voting for 6 months, 9 experts voting for 3months, and the remaining 5 experts for one year.
Ratings for the level of certainty
A detailed description of all certainty ratings can be found in Supplementary Tables S2 and S3. In the first round, most experts answered that they were either “certain” or “absolutely sure” about their answers (65.9–86.3%), with the exception of the time criterion (57.9%). As expected, the subsample of master experts reported high levels of certainty across items (“certain” or “absolutely sure”, 80–97.2%). The level of certainty in the second round was also demonstrated by most participants in the total panel (66.3–92.1%) and most master experts (74–95.7%) being either “certain” or “absolutely sure” about their answers, with the exception of responses for the frequency and time criteria, discussed below.
As mentioned above, the items of the domain tolerance were not included in further analyses due the lack of expert agreement regarding their importance. In the first round, only 65.9% of the total expert panel was either “certain” or “absolutely sure” about their answers regarding tolerance criteria (compared to 88.6% in the master group). In the second round, 73.3% of the total expert panel was either “certain” or “absolutely sure” about their responses (compared to 77.8% in the master group).
The level of certainty regarding the importance ratings for the four suggested specifiers in the first round was assessed with a single overall certainty question. In the total expert panel, 66.4% felt either “certain” or “absolutely sure” (compared to 82.8% in the master group) with their answer. In the second round, each suggested specifier was followed by a certainty rating. The results are shown in the Supplementary Table S3. Regarding their importance rating of the potential specifier “with vs. without hoarding disorder”, 79.3% of the total expert panel was either “certain” or “absolutely sure” about their responses (compared to 88.9% in the master group). In terms of the suggested specifier “with difficulty discarding vs. without difficulty discarding”, 70.9% of the total expert panel was either “certain” or “absolutely sure” about their responses (compared to 80.0% in the master group).
Discussion
This is the first study applying the Delphi technique to propose candidate diagnostic criteria for CBSD. The vast majority of experts agreed that CBSD should be recognized as a distinct psychiatric diagnosis, best classified as a disorder due to addictive behaviors. Most participants (round 2: 55.4%) preferred the term “compulsive buying disorder”, which may reflect the fact that it has been used since decades in the literature. However, 38.7% of the expert panel voted for “buying-shopping disorder” and a minority (6%) for “shopping addiction”. The term “buying-shopping disorder” reflects recent changes in consumer behavior by addressing both buying (i.e., purchasing) and shopping without purchasing (Bloch & Richins, 1983). With the growing online-retail market, shopping activities such as frequent and time-consuming searches for product-related information or simultaneous browsing of different shopping websites is a noticeable problem for many affected individuals (Müller, Brand, Mitchell, & de Zwaan, 2020; Rose & Dhandayudham, 2014). Overall, the classification of CBSD is still controversially debated. The same is also true for terminology. We use the CBSD terminology in this paper for consistency with current ICD-11 nomenclature, although our survey questions referred to “buying-shopping disorder” to maintain consistency with the most recent literature and with DSM-5 practices (cf. hoarding disorder, gambling disorder). Considering that 73.8% of the total expert panel (and 66.7% of master experts) stated that CBSD should be categorized as a disorder due to addictive behaviors, in our opinion, the broader term “buying-shopping disorder” should be viewed as an alternative expression to “compulsive buying disorder” or “compulsive buying-shopping disorder”. Nonetheless, discussions around future terminology will need to continue until there is general agreement.
Following collation of all the results, we developed a list of candidate criteria for CBSD (see Table 3). These criteria and the results are discussed next.
Table 3.
Proposed draft diagnostic criteria for compulsive buying-shopping disorder
|
|
|
|
| Specifier: With vs. without excessive hoarding of purchased items |
Consistent with McElroy et al. (1994), we chose the presence of “persistent and/or recurrent dysfunctional buying/shopping-related behaviors, thoughts and related phenomena” as the A criterion for CBSD. This criterion is specified in six subsections, taking into account the results of the importance and certainty ratings. In our opinion and that of the expert panel, the criterion A.1 “intrusive and/or irresistible urges and/or impulses and/or cravings and/or preoccupations for buying/shopping” is a key feature of CBSD. We decided to use the phrase “and/or” because it remains unclear if the presence of all of these aspects is required. On the one hand, some individuals with CBSD may present clinically with preoccupations or cravings, but not both. On the other hand, research highlights the importance of all these aspects in relation to CBSD (Kyrios et al., 2018; Trotzke et al., 2017).
Criterion A.2 “diminished control over buying/shopping” is also characteristic of excessiveness and problematic behavior. However, there are some critical issues regarding the delineation of this criterion, particularly with respect to the exact operationalization of 2a and 2b (i.e., number of purchases, affordability) or 2c (quantifying time). It was surprising that experts did not agree on frequency and/or time criteria or on the item “the average proportion of income spent per month on buying”, which would render a more precise description of required thresholds for the diagnosis of CBSD. However, greater frequencies of shopping/buying could rather be seen as simply indicators of severity. On their own, the individually operationalized “diminished control” items 2a-c may not add to the diagnosis of CBSD per se. If excessive buying/shopping causes substantial negative consequences (see below), there may be no reason for estimating the number of CBSD episodes. Severe CBSD episodes once every six weeks could be sufficient for a diagnosis because of the resulting harm to self or others. The relatively low level of experts' certainty with their responses on frequency items reflects the difficulty of defining a frequency threshold for CBSD and the questionable relevance of such an item for the diagnosis of CBSD (see Supplementary Tables S2 and S3). Nonetheless, future research needs to investigate frequency and period of excessive or uncontrolled buying/shopping or even browsing, inclusive of online browsing, amongst individuals with CBSD. Criterion A.3 reads “excessive purchasing of items without utilizing them for their intended purposes”, which was included as a criterion after the second round of data collection. Experts did agree it was a key feature of CBSD. This is in line with the literature and clinical experience indicating that CBSD should be considered if individuals frequently make unnecessary purchases without using them and, in fact, may return, throw, give away or forget them as soon as they are purchased (Christenson et al., 1994; Kellett & Bolton, 2009; McElroy et al., 1994; Schlosser, Black, Repertinger, & Freet, 1994). This might suggest that individuals with CBSD are “chasing” the purchase in the same way as individuals with gambling disorder chase the “win” (Granero, Fernandez-Aranda, Mestre-Bach, et al., 2016).
Criterion A.4, “the use of buying/shopping to regulate internal states”, refers to the functions associated with CBSD. In accordance with the experts' views and consistent with research on CBSD (e.g., Kellett & Bolton, 2009; Müller et al., 2012) and behavioral addictions (Brand et al., 2019), we differentiate between positive (i.e., gratification: generating or chasing positive mood) and negative (i.e., compensation: relieving negative mood) reinforcement properties of CBSD. In particular, while the complex association of CBSD with depression has been highlighted both as a precursor, consequence and vulnerability factor (Kyrios, McQueen, & Moulding, 2013), the reinforcing qualities of the short-lived euphoria following a purchase have also been emphasized (Miltenberger et al., 2003).
The criterion A.5, “persistent and recurrent dysfunctional buying/shopping symptoms result in negative consequences and impairment in important areas of functioning”, relates to the usual requirements that differentiate a clinical disorder from an excessive behavior (Stein et al., 2010). The negative consequences of CBSD, described consistently in the literature (e.g., Black, 2007; Christenson et al., 1994; Kellett & Bolton, 2009; McElroy et al., 1994; Müller, Brand, et al., 2019; Schlosser et al., 1994), were met with high agreement by the expert panel. It is noteworthy that the panel did not show accord on the item “buying/shopping preoccupations, obsessions, impulses or behaviors result in delinquency e.g., deceptions, embezzlement, theft or other illegal behaviors”. In treatment-seeking samples, the number of individuals who report legal problems due to inappropriate purchasing seems to be high (Vogel et al., 2019). However, there is still a lack of substantial empirical data regarding antisocial behavior related to CBSD and it may be more appropriate as a specifier rather than as a diagnostic criterion (Müller, Claes et al., 2020). While many clients may report for treatment after legal or interpersonal problems arise, future research would need to examine the breadth of such issues across CBSD.
The criterion A.6, “the reduction or cessation of excessive buying/shopping results in negative emotional states and/or cognitive symptoms”, is likely related to potential withdrawal symptoms of CBSD. Those symptoms are often reported by clients with CBSD and have been described in the literature (e.g., Black, 2007; Christenson et al., 1994; Kellett & Bolton, 2009; McElroy et al., 1994; Müller, Brand, et al., 2019; Schlosser et al., 1994). It is interesting that physical symptoms of withdrawal (e.g., sweating, heart racing, tremor) were rejected by the experts, whereas emotional and cognitive symptoms were accepted. Future research will need to examine the differential aspects of various withdrawal symptoms. Again, we have used the phrase “and/or” because we assume that individuals with CBSD may experience emotional or cognitive withdrawal symptoms or both when reducing buying-shopping behavior.
The B criterion, “maintenance or escalation of dysfunctional buying/shopping behaviors despite negative consequences” was included in the second round in response to suggestions by some experts in the first round. The total panel and the master group strongly agreed on this criterion (96.1% and 92.6%, respectively). It is derived from the ICD-11 category “disorders due to substance use or addictive behaviors”, where the behavioral element “continuation or escalation of the behavior despite the occurrence of negative consequences” must be present to diagnose an addiction (WHO, 2019). In our opinion, the criterion is one that helps to delineate recreational buying/shopping from CBSD. Most consumers who have used buying and shopping in a way that results in distress or negative effects in important areas of functioning (see criteria A.5 and A.6) will likely recognize the potential risk for future harm and, therefore, adjust their shopping activities and purchasing behavior. Conversely, individuals with CBSD are perceived to ignore or neglect the negative effects of their consumptive patterns in favor of short-term gratification, pleasurable escape or compensation for emotional discomfort.
Criterion C, “the pattern of buying/shopping does not occur exclusively during a period of mania/hypomania”, and criterion D, “the pattern of buying/shopping is not better explained by the symptoms of another mental disorder (e.g., psychosis) or attributable to a medical condition (e.g., organic psychosyndrome)”, involve potential differential or exclusionary diagnoses. It is important to underline that the panel agreed that CBSD can co-occur in the context of hoarding disorder and borderline (or other) personality disorder. Such distinctions are common in both DSM-5 (APA, 2013) and ICD-11 (WHO, 2019).
Apparent from the Delphi process, experts were not in favor of specifiers. However, we would like to point out that the specifier “with vs. without hoarding disorder” very narrowly missed consensus by the total panel (74%) but the master group showed agreement above the threshold (77.8%). Prior research has shown that about one third of treatment seeking clients with CBSD suffer from hoarding of purchased items which is associated with a higher symptom severity for CBSD and worse treatment prognosis (Claes, Müller, & Luyckx, 2016; Frost, Steketee, & Tolin, 2011; Lawrence, Ciorciari, & Kyrios, 2014; Möllenkamp, de Zwaan, & Müller, 2015; Müller et al., 2008). A subtyping approach could be useful in defining treatment needs. On that basis, we chose to include the specifier “with vs. without excessive hoarding of purchased items” in the proposal so that it could be investigated in future trials.
The candidate criteria do not include a tolerance criterion because expert agreement was not reached on suggested characteristics (i.e., “increasingly amount of money needs to be spend/increasingly number of goods need to be bought/increasingly amount of time needs to be spend to experience desired excitement or relief from negative feelings”). According to experts' opinion, tolerance should not be seen as an indicator of CBSD, which is in contrast to the component model of addiction proposed by Griffiths (2009) and the level of agreement by participants that CBSD should be best classified as a disorder due to an addictive behavior. The lack of consensus might reflect the diversity of the expert panel which included clinical and non-clinical experts. In the context of our own clinical work, we have certainly seen clients who reported signs of tolerance as suggested in the current survey questionnaire. While we did not include a tolerance criterion, we recommend investigating the role of tolerance in CBSD in greater detail in future longitudinal and field trials.
Limitations
There are some methodological shortcomings that have to be considered when interpreting the current findings, including the potential selection bias and response rate (Donohoe et al., 2012). About one third of the expert panel was recruited from either Germany or the United States, with unknown exposure to dysfunctional buying patterns in minority groups. Therefore, experts' agreement on diagnostic criteria for CBSD may not necessarily be suitable for all cultures or minority groups. Our recruitment strategy to search databases and invite only first and last authors of CBSD-related publications might have led to an underrepresentation of clinicians in the expert panel. However, more than half of the entire expert panel and about three quarters of the master subgroup stated that they were working in a clinical context. In addition, there were differences in the professional background of participants (e.g., psychology versus medicine), which may have impacted on responses for various items (e.g., those that were biologically-oriented).
While the gross response rate of the first round (20.3%) appears low, it is in fact reasonable for a web-based Delphi study. Response rates from studies in the field of medicine with a comparable high number of distributed questionnaires ranged between 10% (Yap, Pilkington, Ryan, Kelly, & Jorm, 2014) and 44% (Malcolm, Knighting, Forbat, & Kearney, 2009). Panel retention across the two rounds of the current Delphi process was good with 74% of experts participating in the second round. In order to minimize attrition bias, we had predefined a number of two rounds, which may have limited the results. Possibly more subsequent rounds would have led to additional new relevant criteria suggested by the panel or to consensus regarding the agreement or disagreement with specifiers. With respect to importance ratings, the use of 4-point scales (i.e., omitting a neutral midpoint) as well as some of the response labels (e.g., 2 = peripheral) may reflect another limitation.
Strengths
One key advantage of the Delphi method is that it allows the involvement of a large number of experts from a particular field. The strength of evidence from this method depends on the participants' expertise, independence and diversity, and on the mechanism for coordinating and aggregating the panel's expertise (Diamond et al., 2014; Häder, 2014; Surowiecki, 2004). Compared to other Delphi studies in mental health research (Addington et al., 2013; Jorm, 2015), the current sample comprised a large number of international experts from different fields (e.g., psychology, medicine, consumer research) and from a broad range of different countries. This is a remarkable strength of the current investigation given the narrow scope of CBSD.
Having a subsample of master experts embedded within the participants' pool was a distinct advantage (Dalkey et al., 1969). All analyses were performed twice, first for the total expert panel and second for the subsample of experts with “a greater deal” of knowledge and experience related to CBSD. Moreover, consensus was only accepted if at least 75% agreed in both the total panel and the master group, which represents a rather strict criterion. Participants were also asked how certain they were about their responses in order to judge the quality of responses. In both rounds, the proportion of experts who felt uncertain about their answer was barely higher than 10%, except for one criterion item in the second round (discussed above). The rejection of all filler items indicates the validity and proficiency of selected experts.
Experts' consensus on suggested diagnostic criteria for CBSD should not be equated with the validity of those criteria. The proposed draft criteria must be regarded as a work in progress which forms the basis for the development of measurement and interview tools. While we argue for a descriptive approach by focusing on the behavioral and mental symptoms of CBSD, rather than on its underlying processes (Brand, Rumpf, King, Potenza, & Wegmann, 2020; Stein et al., 2010), we do not question the usefulness of psychobiological understandings for nosological decisions. Future studies – clinical, experimental, neuroimaging, genetic – should address the question of whether CBSD meets the following features of mental disorders: “a behavioral or psychological syndrome or pattern that occurs in an individual; the consequences of which are clinically significant distress or disability; not merely an expectable response to common stressors and losses; reflects an underlying psychobiological dysfunction; is not solely a result of social deviance or conflicts with society; has diagnostic validity using one or more sets of diagnostic validators; and has clinical utility” (Grant & Chamberlain, 2016, p. 2). Nonetheless, identifying a set of potential diagnostic criteria could lead to more exact etiological investigations by the mere fact that researchers could compare like with like across studies.
Conclusions
Based on collective views of international expert researchers and clinicians, we were able to propose candidate diagnostic criteria for CBSD. They can be used as the basis for the development of diagnostic interviews and measures of CBSD severity. The clinical utility, reliability, and validity of the proposed draft diagnostic criteria for CBSD should be addressed in future field studies.
Funding sources
The study was supported by the German Academic Exchange Service (DAAD, Project Related Personal Exchange, grant 57387119) from the budget of the Federal Ministry of Education and Research (BMBF) and by the Australia-Germany Joint Cooperation Scheme.
Conflicts of Interest
The authors declare no conflict of interest.
Authors' contribution
Study concept and design: AM, NL, MH, MK. Methodology – questionnaire development: AM, NL, PT, MK, MH, KA, DF. Methodology – Delphi method: NL, MH, AM. Statistical analysis: NL, DF, PT. Interpretation of the data: AM, NL, MK, PT, DF, KA, MH, MB. Supervision: AM, MH, MK. Obtained funding: AM, MK. Resources: MZ, MB, MK. Writing – original draft: AM, NL, PT, DF, KA, MK. Writing – review and editing: AM, NL, MK, DF, KA, PT, MB, MZ, MH.
Supplementary Material
Acknowledgments
We wish to thank all experts who participated in the Delphi process and the reviewers for their thoughtful comments towards improving the manuscript. The study was supported by the German Academic Exchange Service (DAAD; PPP Programmes for Project Related Personal Exchange, grant 57387119) from the budget of the Federal Ministry of Education and Research (BMBF) and by the Australia-Germany Joint Cooperation Scheme.
References
- Addington, D. E., McKenzie, E., Norman, R., Wang, J., & Bond, G. R. (2013). Essential evidence-based components of first-episode psychosis services. Psychiatric Services, 64(5), 452–457. 10.1176/appi.ps.201200156. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1987). Diagnostic and statistical manual of mental disorders (vol. 3rd ed., revised). Washington, DC: American Psychiatric Press. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (vol. 5th ed.). Washington, DC: American Psychiatric Press. [Google Scholar]
- Black, D. W. (2007). A review of compulsive buying disorder. World Psychiatry, 6, 14–18. [PMC free article] [PubMed] [Google Scholar]
- Black, D. W., Shaw, M., & Allen, J. (2016). Five-year follow-up of people diagnosed with compulsive shopping disorder. Comprehensive Psychiatry, 68, 97–102. 10.1016/j.comppsych.2016.03.004. [DOI] [PubMed] [Google Scholar]
- Bloch, P., & Richins, M. L. (1983). Shopping without purchase: An investigation of consumer browsing behavior. Advances in Consumer Research, 10, 389–393. [Google Scholar]
- Brand, M., Rumpf, H.-J., Demetrovics, Z., Müller, A., Stark, R., King, D. L., …, & Potenza, M. N. (2020). Which conditions should be considered as disorders in the ICD-11 designation of “Other specified disorders due to addictive behaviors”? Journal of Behavioral Addictions. 10.1556/2006.2020.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, M., Rumpf, H.-J., King, D. L., Potenza, M. N., & Wegmann, E. (2020). Clarifying terminologies in research on gaming disorder and other addictive behaviors: Distinctions between core symptoms and underlying psychological processes. Current Opinion in Psychology, 36, 49–54. 10.1016/j.copsyc.2020.04.006. [DOI] [PubMed] [Google Scholar]
- Brand, M., Wegmann, E., Stark, R., Müller, A., Wölfling, K., Robbins, T. W., et al. (2019). The Interaction of Person-Affect-Cognition-Execution (I-PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neuroscience & Biobehavioral Reviews, 104, 1–10. 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Castro-Calvo, J., King, D. L., Stein, D., Brand, M., Carmi, L., Chamberlain, S. R., …, & Billieux, J. (2021). Expert appraisal of criteria for assessing gaming disorder: An international Delphi study. Addiction. 10.1080/14659890500114359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christenson, G. A., Faber, R. J., de Zwaan, M., Raymond, N. C., Specker, S. M., Ekern, M. D., …, & et al. (1994). Compulsive buying: Descriptive characteristics and psychiatric comorbidity. Journal of Clinical Psychiatry, 55(1), 5–11. [PubMed] [Google Scholar]
- Claes, L., Luyckx, K., Vogel, B., Verschueren, M., & Müller, A. (2018). Identity processes and clusters in individuals with and without pathological buying. Psychiatry Research, 267, 467–472. 10.1016/j.psychres.2018.06.003. [DOI] [PubMed] [Google Scholar]
- Claes, L., Müller, A., & Luyckx, K. (2016). Compulsive buying and hoarding as identity substitutes: The role of materialistic value endorsement and depression. Comprehensive Psychiatry, 68, 65–71. 10.1016/j.comppsych.2016.04.005. [DOI] [PubMed] [Google Scholar]
- Dalkey, N. C., Brown, B. B., & Cochran, S. (1969). The Delphi-method III: Use of selfratings to improve group estimates. Santa Monica, USA: RAND Corporation. [Google Scholar]
- Dell'Osso, B., Allen, A., Altamura, A. C., Buoli, M., & Hollander, E. (2008). Impulsive-compulsive buying disorder: Clinical overview. Australian and New Zealand Journal of Psychiatry, 42(4), 259–266. 10.1080/00048670701881561. [DOI] [PubMed] [Google Scholar]
- Diamond, I. R., Grant, R. C., Feldman, B. M., Pencharz, P. B., Ling, S. C., Moore, A. M., et al. (2014). Defining consensus: A systematic review recommends methodologic criteria for reporting of Delphi studies. Journal of Clinical Epidemiology, 67(4), 401–409. 10.1016/j.jclinepi.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Dillman, D. A. (1978). Mail and telephone surveys: The total design method. New York: John Wiley. [Google Scholar]
- Donohoe, H., Stellefson, M., & Tennant, B. (2012). Advantages and limitations of the e-Delphi technique: Implications for health education researchers. American Journal of Health Education, 43(1), 38–46. [Google Scholar]
- First, M. B., Reed, G. M., Hyman, S., & Saxena, S. (2015). The development of the ICD-11 clinical descriptions and diagnostic guidelines for mental and behavioural disorders. World Psychiatry, 14, 82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontenelle, L. F., & Grant, J. E. (2014). Hoarding disorder: A new diagnostic category in ICD-11? Revista Brasileira de Psiquiatria, 36(suppl 1), 28-39. 10.1590/1516-4446-2013-1269. [DOI] [PubMed] [Google Scholar]
- Frost, R. O., Steketee, G., & Tolin, D. F. (2011). Comorbidity in hoarding disorder. Depression and Anxiety, 28(10), 876–884. 10.1002/da.20861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargon, E., Crew, R., Burnside, G., & Williamson, P. R. (2019). Higher number of items associated with significantly lower response rates in COS Delphi surveys. Journal of Clinical Epidemiology, 108, 110–120. 10.1016/j.jclinepi.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granero, R., Fernández-Aranda, F., Baño, M., Steward, T., Mestre-Bach, G., del Pino-Gutiérrez, A., …, & Jiménez-Murcia, S. (2016). Compulsive buying disorder clustering based on sex, age, onset and personality traits. Comprehensive Psychiatry, 68, 1–10. 10.1016/j.comppsych.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Granero, R., Fernández-Aranda, F., Mestre-Bach, G., Steward, T., Baño, M., del Pino-Gutiérrez, A., …, & Jiménez-Murcia, S. (2016). Compulsive buying behavior: Clinical comparison with other behavioral addictions. Frontiers in Psychology, 7, 1–12. 10.3389/fpsyg.2016.00914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, J. E., Atmaca, M., Fineberg, N. A., Fontenelle, L. F., Matsunaga, H., Reddy, Y. C. J., …, & Stein, D. J. (2014). Impulse control disorders and “behavioural addictions” in the ICD-11. World Psychiatry, 13(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, J. E., & Chamberlain, S. R. (2016). Expanding the definition of addiction: DSM-5 vs. ICD-11. CNS Spectrums, 21(4), 300–333. 10.1017/S1092852916000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths, M. D. (2009). A ‘components’ model of addiction within a biopsychosocial framework. Journal of Substance Use, 10(4), 191–197. 10.1080/14659890500114359. [DOI] [Google Scholar]
- Häder, M. (2014). Delphi-Befragungen: Ein Arbeitsbuch [Delphi-survey: A workbook]. Wiesbaden: Springer. [Google Scholar]
- Häder, M., & Häder, S. (2000). Die Delphi-Technik in den Sozialwissenschaften. Methodische Forschungen und innovative Anwendungen [The Delphi method in social science. Methodological research and innovative applications]. Wiesbaden, Germany: Westdeutscher Verlag. [Google Scholar]
- Hollander, E., & Allen, A. (2006). Is compulsive buying a real disorder, and is it really compulsive? American Journal of Psychiatry, 163(10), 1670–1672. [DOI] [PubMed] [Google Scholar]
- Jorm, A. F. (2015). Using the Delphi expert consensus method in mental health research. Australian & New Zealand Journal of Psychiatry, 49(10), 887–897. 10.1177/0004867415600891. [DOI] [PubMed] [Google Scholar]
- Kellett, S., & Bolton, J. V. (2009). Compulsive buying: A cognitive-behavioural model. Clinical Psychology & Psychotherapy, 16(2), 83–99. 10.1002/cpp.585. [DOI] [PubMed] [Google Scholar]
- Koran, L., Faber, R. J., Aboujaoude, E., Large, M. D., & Serpe, R. T. (2006). Estimated prevalence of compulsive buying behavior in the United States. American Journal of Psychiatry, 163(10), 1806–1812. [DOI] [PubMed] [Google Scholar]
- Kraepelin, E. (1899). Psychiatrie: Ein Lehrbuch für Studierende und Ärzte. [A textbook for students and physicians] (6th ed.). Leipzig: Verlag Johann Ambrosius Barth. [Google Scholar]
- Kraepelin, E. (1909). Psychiatrie: Ein Lehrbuch für Studierende und Ärzte. [A textbook for students and physicians] (8th ed.). Leipzig: Verlag Johann Ambrosius Barth. [Google Scholar]
- Kyrios, M., McQueen, P., & Moulding, R. (2013). Experimental analysis of the relationship between depressed mood and compulsive buying. Journal of Behavior Therapy and Experimental Psychiatry, 44(2), 194–200. 10.1016/j.jbtep.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Kyrios, M., Trotzke, P., Lawrence, L., Fassnacht, D. B., Ali, K., Laskowski, N. M., et al. (2018). Behavioral neuroscience of buying-shopping disorder: A review. Current Behavioral Neuroscience Reports, 5, 263–270. 10.1007/s40473-018-0165-6. [DOI] [Google Scholar]
- Lawrence, L. M., Ciorciari, J., & Kyrios, M. (2014). Relationships that compulsive buying has with addiction, obsessive-compulsiveness, hoarding, and depression. Comprehensive Psychiatry, 55(5), 1137–1145. 10.1016/j.comppsych.2014.03.005. [DOI] [PubMed] [Google Scholar]
- Lejoyeux, M., & Weinstein, A. (2010). Compulsive buying. The American Journal of Drug and Alcohol Abuse, 36(5), 248–253. 10.3109/00952990.2010.493590. [DOI] [PubMed] [Google Scholar]
- Lo, H.-Y., & Harvey, N. (2012). Effects of shopping addiction on consumer decision-making: Web-based studies in real time. Journal of Behavioral Addictions, 1(4), 162–170. 10.1556/jba.1.2012.006. [DOI] [PubMed] [Google Scholar]
- Malcolm, C., Knighting, K., Forbat, L., & Kearney, N. (2009). Prioritisation of future research topics for children’s hospice care by its key stakeholders: A Delphi study. Palliative Medicine, 23, 398–405. 10.1177/0269216309104061. [DOI] [PubMed] [Google Scholar]
- Mann, K., Fauth-Bühler, M., Higuchi, S., Potenza, M., & Saunders, J. B. (2016). Pathological gambling: A behavioral addiction. World Psychiatry, 15(3), 297–298. 10.1002/wps.20356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maraz, A., Griffiths, M. D., & Demetrovics, Z. (2016). The prevalence of compulsive buying: A meta-analysis. Addiction, 111(3), 408–419. 10.1111/add.13223. [DOI] [PubMed] [Google Scholar]
- McElroy, S. L., Keck, P. E.,Jr., Pope, H. G.,Jr., Smith, J. M. R., & Strakowski, S. M. (1994). Compulsive buying: A report of 20 cases. Journal of Clinical Psychiatry, 55(6), 242–248. [PubMed] [Google Scholar]
- Miltenberger, R. G., Redlin, J., Crosby, R., Stickney, M., Mitchell, J., Wonderlich, S., …, & Smyth, J. (2003). Direct and retrospective assessment of factors contributing to compulsive buying. Journal of Behavior Therapy and Experimental Psychiatry, 34(1), 1–9. 10.1016/s0005-7916(03)00002-8. [DOI] [PubMed] [Google Scholar]
- Möllenkamp, M., de Zwaan, M., & Müller, A. (2015). Hoarding with and without excessive buying: Results of a pilot study. Psychopathology, 48(1), 56–59. 10.1159/000363389. [DOI] [PubMed] [Google Scholar]
- Moulding, R., Duong, A., Nedeljkovic, M., & Kyrios, M. (2017). Do you think that money can buy happiness? A review of the role of mood, materialism, self, and cognitions in compulsive buying. Current Addiction Reports, 4(3), 254–261. 10.1007/s40429-017-0154-y. [DOI] [Google Scholar]
- Müller, A., Brand, M., Claes, L., Demetrovics, Z., de Zwaan, M., Fernandes-Aranda, F., …, & Kyrios, M. (2019). Buying-shopping disorder – is there enough evidence to support its inclusion in ICD-11?. CNS Spectrums, 24(4), 374–379. 10.1017/S1092852918001323. [DOI] [PubMed] [Google Scholar]
- Müller, A., Brand, M., Mitchell, J.E., & de Zwaan, M. (2020). Internet-shopping disorder. In Faust, D., Faust, K., & Potenza, M. N. (Eds.), The oxford handbook of digital technologies and mental health (pp. 214–225). Oxford: Oxford University Press. [Google Scholar]
- Müller, A., Claes, L., Birlin, A., Georgiadou, E., Laskowski, N.M., Steins-Loeber, S., et al. (2020). Associations of buying-shopping disorder symptoms with identity confusion, materialism and socially undesirable personality features in a community sample. European Addiction Research. 10.1159/000511078. [DOI] [PubMed] [Google Scholar]
- Müller, A., Mitchell, J. E., Crosby, R. D., Cao, L., Johnson, J., Claes, L., et al. (2012). Mood states preceding and following compulsive buying episodes: An ecological momentary assessment study. Psychiatry Research, 200(2–3), 575–580. 10.1016/j.psychres.2012.04.015. [DOI] [PubMed] [Google Scholar]
- Müller, A., Müller, U., Silbermann, A., Reinecker, H., Bleich, S., Mitchell, J. E., et al. (2008). A randomized, controlled trial of group cognitive-behavioral therapy for compulsive buying disorder: Posttreatment and 6-month follow-up results. Journal of Clinical Psychiatry, 69, 1131–1138. [DOI] [PubMed] [Google Scholar]
- Müller, A., Steins-Loeber, S., Trotzke, P., Vogel, B., Georgiadou, E., & de Zwaan, M. (2019). Online shopping in treatment-seeking patients with buying-shopping disorder. Comprehensive Psychiatry, 94, 152120. 10.1016/j.comppsych.2019.152120. [DOI] [PubMed] [Google Scholar]
- Müller, A., Trotzke, P., Mitchell, J. E., de Zwaan, M., & Brand, M. (2015). The Pathological Buying Screener: Development and psychometric properties of a new screening instrument for the assessment of pathological buying symptoms. PloS One, 10(10), e0141094. 10.1371/journal.pone.0141094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otero-López, J. M., & Villardefrancos, E. (2014). Prevalence, sociodemographic factors, psychological distress, and coping strategies related to compulsive buying: A cross sectional study in Galicia, Spain. BMC Psychiatry, 14(101), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza, M. N., Higuchi, S., & Brand, M. (2018). Call for research into a wider range of behavioural addictions. Nature, 555(7694), 30. [DOI] [PubMed] [Google Scholar]
- Rose, S., & Dhandayudham, A. (2014). Towards an understanding of internet-based problem shopping behaviour: The concept of online shopping addiction and its proposed predictors. Journal of Behavioral Addictions, 3(2), 83–89. 10.1556/jba.3.2014.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser, S., Black, D. W., Repertinger, S., & Freet, D. (1994). Compulsive buying. General Hospital Psychiatry, 16, 205–2012. [DOI] [PubMed] [Google Scholar]
- Stein, D. J., Phillips, K. A., Bolton, D., Fulford, K. W. M., Sadler, J. Z., & Kendler, K. S. (2010). What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychological Medicine, 40(11), 1759–1765. 10.1017/s0033291709992261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surowiecki, J. (2004). The wisdom of crowds: Why the many are smarter than the few and how collective wisdom shapes business, economies, societies and nations . New York: Doubleday. [Google Scholar]
- Trotzke, P., Brand, M., & Starcke, K. (2017). Cue-reactivity, craving, and decision making in buying disorder: A review of the current knowledge and future directions. Current Addiction Reports, 4(3), 246–253. 10.1007/s40429-017-0155-x. [DOI] [Google Scholar]
- Trotzke, P., Starcke, K., Müller, A., & Brand, M. (2015). Pathological buying online as a specific form of internet addiction: A model-based experimental investigation. PloS One, 10(10), e0140296. 10.1371/journal.pone.0140296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel, B., Trotzke, P., Steins-Loeber, S., Schafer, G., Stenger, J., de Zwaan, M., …, & Müller, A. (2019). An experimental examination of cognitive processes and response inhibition in patients seeking treatment for buying-shopping disorder. PloS One, 14(3), e0212415. 10.1371/journal.pone.0212415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2019). International classification of Diseases updated 09/2019 (11th revision). Retrieved from https://icd.who.int/en/, January 15th, 2021. [Google Scholar]
- Yap, M. B. H., Pilkington, P. D., Ryan, S. M., Kelly, C. M., & Jorm, A. F. (2014). Parenting strategies for reducing the risk of adolescent depression and anxiety disorders: A Delphi consensus study. Journal of Affective Disorders, 156, 67–75. 10.1016/j.jad.2013.11.017. [DOI] [PubMed] [Google Scholar]
- Yücel, M., Oldenhof, E., Ahmed, S. H., Belin, D., Billieux, J., Bowden-Jones, H., …, & Verdejo-Garcia, A. (2019). A transdiagnostic dimensional approach towards a neuropsychological assessment for addiction: An international Delphi consensus study. Addiction, 114(6), 1095–1109. 10.1111/add.14424. [DOI] [PMC free article] [PubMed] [Google Scholar]