Abstract
Background and aims
The effect of internet-based psychological treatment for gambling problems has not been previously investigated by meta-analysis. The present study is therefore a quantitative synthesis of studies on the effects of internet-based treatment for gambling problems. Given that effects may vary according to the presence of therapist support and control conditions, it was presumed that subgroup analyses would elucidate such effects.
Methods
A systematic search with no time constraints was conducted in PsycINFO, MEDLINE, Web of Science, and the Cochrane Library. Two authors independently extracted data using a predefined form, including study quality assessment based on the Cochrane risk of bias tool. Effect sizes were calculated using random-effects models. Heterogeneity was indexed by Cochran’s Q and the I 2 statistics. Publication bias was investigated using trim and fill.
Results
Thirteen studies were included in the analysis. Random effects models at post-treatment showed significant effects for general gambling symptoms (g = 0.73; 95% CI = 0.43–1.03), gambling frequency (g = 0.29; 95% CI = 0.14–0.45), and amount of money lost gambling (g = 0.19; 95% CI = 0.11–0.27). The corresponding findings at follow-up were g = 1.20 (95% CI = 0.79–1.61), g = 0.36 (95% CI = 0.12–0.60), and g = 0.20 (95% CI = 0.12–0.29) respectively. Subgroup analyses showed that for general gambling symptoms, studies with therapist support yield larger effects than studies without, both post-treatment and at follow-up. Additionally, on general gambling symptoms and gambling frequency, there were lower effect sizes for studies with a control group compared to studies without a control group at follow-up. Studies with higher baseline severity of gambling problems were associated with larger effect sizes at both posttreatment and follow-up than studies with more lenient inclusion criteria concerning gambling problems.
Discussion and conclusions
Internet-based treatment has the potential to reach a large proportion of persons with gambling problems. Results of the meta-analysis suggest that such treatments hold promise as an effective approach. Future studies are encouraged to examine moderators of treatment outcomes, validate treatment effects cross-culturally, and investigate the effects of novel developments such as ecological momentary interventions.
Keywords: internet-based treatment, online therapy, e-therapy, meta-analysis, problem gambling, randomized controlled trial
Introduction
Gambling problems are maladaptive gambling behavior that disrupt personal, family and/or vocational pursuits (Hodgins & El-Guebaly, 2000). Prevalence studies indicate that between 0.7 and 6.5% of the adult population in Europe, Asia, North-America, and Oceania report gambling problems (Calado & Griffiths, 2016). Although symptom levels and type of gambling problems may change over time (DeFuentes-Merillas, Koeter, Schippers, & van den Brink, 2004; Nelson, Gebauer, LaBrie, & Shaffer, 2009; Slutske, Jackson, & Sher, 2003), some individuals experience chronic gambling problems for many years (Bilevicius, Edgerton, Sanscartier, Jiang, & Keough, 2020). Harms experienced by problem gamblers comprise financial problems, relationships disruption, emotional distress (e.g., shame, stigma), health problems (e.g., stress-related medical conditions, sedentary behavior impairing health), cultural harm (e.g., behaving at odds with cultural beliefs, reduced cultural connection), reduced educational/occupational performance (e.g., absenteeism), and criminal activity such as stealing money to gamble (Langham et al., 2016).
The psychological treatment modalities for problem gamblers with the strongest evidence base are cognitive behavior therapy (CBT), motivational interviewing (MI), and mindfulness interventions (Cowlishaw et al., 2012; Matheson et al., 2018; Maynard, Wilson, Labuzienski, & Whiting, 2018; Yakovenko, Quigley, Hemmelgarn, Hodgins, & Ronksley, 2015). CBT typically involves monitoring of gambling behavior, psychoeducation, and cognitive and behavioral strategies aiming to control behavior, learning problem-solving skills, coping strategies of dysphoric emotions, and relapse prevention (Raylu & Oei, 2010). Meta-analytic evidence supports the effectiveness of CBT, with good treatment response in terms of general symptoms (d = 1.82), gambling frequency (d = 0.78), and amount of money lost (d = 0.52) although the results at follow-up were inconclusive due to limited data (Cowlishaw et al., 2012).
MI explores and resolves ambivalence associated with behavioral change, and comprises several communication principles to facilitate this (Miller & Rollnick, 2012). Similar to CBT, MI has yielded significant short-term treatment effects in terms of amount of money lost and gambling frequency. However, long-term treatment effects were only maintained for the latter outcome (Yakovenko et al., 2015). Mindfulness interventions typically focus on being attentive of the present as opposed to the past or future, engaging a full, direct, and active awareness of experienced phenomena (Griffiths, Shonin, & Van Gordon, 2016). Mindfulness interventions have also yielded moderate to large effects for gambling symptoms, urges, and financial outcomes (Maynard et al., 2018). Moreover, meta-analyses have shown personalized feedback on gambling (Peter et al., 2019) and brief interventions (≤three sessions) to yield small, albeit significant, treatment effects (Quilty, Wardell, Thiruchselvam, Keough, & Hendershot, 2019), whilst face-to-face therapy yields better results than self-help approaches (Goslar, Leibetseder, Muench, Hofmann, & Laireiter, 2017).
Despite the wide range of effective treatment options, only about 10% of persons experiencing gambling problems seek treatment (Ladouceur, 2005). Desire to handle problems themselves, stigma, secrecy, shame, not acknowledging problems, practical issues (e.g. lack of availability, costs), concerns about treatment, uncertainty, and avoidance, pressure from others to continue gambling, and not wanting to give up benefits from gambling are some of the barriers that prevent persons experiencing gambling problems from engaging in treatment (Rockloff & Schofield, 2004; Suurvali, Cordingley, Hodgins, & Cunningham, 2009). Internet-based treatments, referring to exchanges via email or chat between client and therapist or web-based treatment programs, may overcome many of these barriers by: (i) increasing feelings of anonymity, (ii) encouraging openness and honesty, and (iii) overcoming practical barriers such as distance to treatment facilities, conflicts between treatment and other constraints on time including child care or paid work, cost of transportation to treatment facilities, and provision of treatment relevant to cultural or language needs (van der Maas et al., 2019). Other advantages of internet-based treatment are the ease of recruitment, the possibility to assess symptoms and to diagnose via the internet, the cost-effectiveness of such interventions, and the opportunity to integrate such treatments into regular clinical settings (Andersson & Titov, 2014).
Positive effects of internet-based treatment of addictions have been attested to in several narrative reviews (Chebli, Blaszczynski, & Gainsbury, 2016; Gainsbury & Blaszczynski, 2011; Giroux, Goulet, Mercier, Jacques, & Bouchard, 2017). Although two narrative reviews of the effects of internet-based treatment for gambling problems specifically have been published (Griffiths & Cooper, 2003; van der Maas et al., 2019), no quantitative review has so far been conducted. Mixed findings comprising positive (Carlbring & Smit, 2008; Casey et al., 2017) and nonsignificant (Luquiens et al., 2016; Cunningham, Godinho, & Hodgins, 2019) have also been reported. Accordingly, a meta-analysis was conducted to evaluate the effects of internet-based treatment of gambling problems, synthesizing both short-term and long-term effects across three main outcomes: general gambling symptoms, gambling frequency, and amount of money lost gambling.
A meta-analysis on psychological interventions for gambling problems showed larger effects for studies without a control condition compared to studies with one (Pallesen, Mitsem, Kvale, Johnsen, & Molde, 2005) which may be attributed to spontaneous recovery (Walker, 2005). There is also evidence of a better effect when therapist support (any direct contact between therapist and patients via emails, phone calls or other channels during therapy) is incorporated into internet-based interventions compared to treatment without this (Rash & Petry, 2016). Moreover, baseline severity of gambling problems has been shown to be inversely related to successful treatment (Merkouris, Thomas, Browning, & Dowling, 2016). Therefore, study design, therapist support, and baseline severity of gambling problems were examined as potential moderators of treatment effectiveness.
Methods
Registration and reporting
The meta-analysis was pre-registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020184582) and its procedures adhered to the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (Moher, Liberati, Tetzlaff, Altman, & Grp, 2009).
Inclusion criteria
The meta-analysis included randomized controlled trials (RCTs): (i) where adult participants with gambling problems were randomized to different treatment arms (with and without control group), and where the effects of internet-based interventions (exchanges via email or chat between client and therapist or web-based treatment programs) for gambling problems were investigated, (ii) written in English or a Scandinavian language, and (iii) published in a peer-reviewed journals. Gambling problems was operationalized as: (a) scoring above a set cut-off on a psychometric instrument assessing gambling problems, such as the South Oaks Gambling Screen (SOGS; Lesieur & Blume, 1987) or the Problem Gambling Severity Index (PGSI; Ferris & Wynne, 2001), (b) pathological gambling or gambling disorder diagnosis in line with DSM-IV (American Psychiatric Association, 1994) or (c) self-referral, or referral for problem gambling treatment by a health professional.
Another inclusion criterion was that the study reported at least one of the following outcomes: (a) general gambling symptoms, (b) gambling frequency, and (c) amount of money lost gambling. No limits were set in terms of publication year. Also, no criteria were set in terms of the period for reporting follow-up data. Studies were excluded if they: (a) did not include at least one of the three aforementioned outcomes, and (b) did not contain sufficient information for effect size calculation (e.g., reported no group pre-post means and/or standard deviations). In case of insufficient data, information requests were sent to authors via email. As pre-registered, the meta-analysis planned to include both RCTs and pre-post intervention studies. However, pre-post intervention studies were excluded based on journal reviewer feedback, representing a post hoc deviation from the original protocol.
Coding of studies
Raw data included in the meta-analysis were coded independently by two of the authors using pilot-tested forms. Each study was coded in line with the Problem/Population, Intervention, Comparison, and Outcome (PICO) characteristics: (i) participant characteristics (age, sex, diagnosis, and method for diagnosis), (ii) intervention characteristics (type, number of sessions, administration mode/with or without therapist support), and (iii) control/comparators (if present and type), and (iv) outcome variables. The studies were further coded for publication year, design, sample size, time for follow-up and information about handling of missing data.
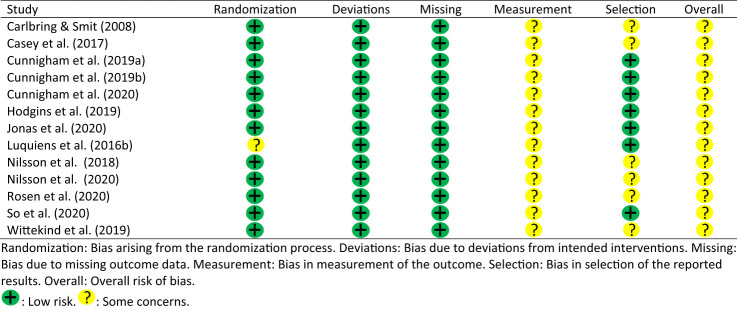
Risk of bias of the included studies
In order to evaluate risk of bias of the included studies, the updated Cochrane risk of bias tool (RoB 2) was used (Sterne et al., 2019). The tool has five domains for risk of bias assessment: (1) bias arising from the randomization process, (2) bias due to deviations from intended interventions, (3) bias due to missing outcome data, (4) bias in measurement of the outcome, and (5) bias in selection of the reported result. The risk of bias evaluations for each domain are: “low risk of bias”, “some concerns”, or “high risk of bias”. Based on the evaluations on the five dimensions, studies are assigned an overall risk of bias categorization comprising: “low risk of bias”, “some concerns”, or “high risk of bias”. Here, “low risk of bias” is indicated by “low risk of bias” evaluations for all domains. Also, “some concerns” is denoted by “some concerns” evaluations on at least one domain and the absence of a “high risk of bias” evaluation in any domain. Finally, “high risk of bias” is indicated by a “high risk of bias” evaluation in at least one domain. Risk of bias for each study was coded independently by two authors for the five domains across 13 studies yielding a total of 65 domains or items of potential (dis)agreement.
Statistical analysis
For each study and outcome category, Hedges’ g with corresponding 95% confidence interval (95% CI) was calculated. Hedges’ g was preferred over Cohen’s d as the former effect size corrects for small sample bias (Hedges, 1981). For studies with follow-up, data from the final assessment were used and compared to the control condition or to pre-treatment data. Results across studies were synthesized with a random-effects model where the between-study variance was estimated based on the DerSimonian and Laird (1986) procedure. This procedure is the most common approach weighing studies with the inverse of their variance and assumes that different studies estimate different, albeit related, intervention effects.
For studies with control groups, the effect sizes were calculated based on the post-treatment scores. For studies with more than one treatment arm, but without a control group, a within-group (pre-post, pre-follow-up) effect size was calculated. In the latter case, the correlation coefficient between the same measures over time was by default set to 0.50, in line with general recommendations (Follmann, Elliott, Suh, & Cutler, 1992). Although only RCTs were included, some RCTs had no control condition (e.g., two active treatment conditions or lacked a control condition at follow-up). In these cases, the effect sizes were calculated based on the change from baseline to post-treatment or follow-up. Consequently, subgroup analyses comparing effect sizes calculated based on designs with or without a control condition were therefore deemed appropriate.
Cases were collapsed (Cunningham, Hodgins et al., 2019, 2020; Hodgins, Cunningham, Murray, & Hagopian, 2019) where different treatment arms did not yield significant different results. For studies with several treatment conditions and one control group (Luquiens et al., 2016; Casey et al., 2017; Jonas et al., 2020), the effect size was calculated based on the most extensive internet-based treatment condition (e.g., more active, extensive and personalized content) with the rationale of not underestimating the treatment potential of such interventions for gambling problems. When combining results from more than one outcome within the same outcome category from the same study, setting the correlation between outcomes to the default (r = 1.00) used in most meta-analytic software overestimates the standard error (Borenstein, Hedges, Higgins, & Rothstein, 2009). To correct for this, the correlation between the outcomes was set to 0.70 in line with another meta-analysis (Bjørseth et al., 2021).
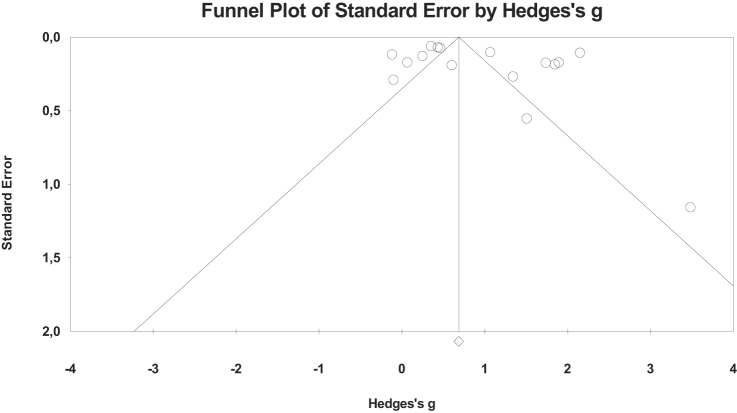
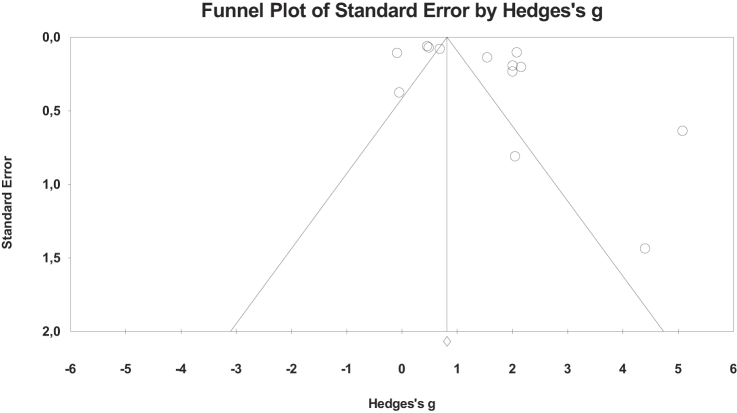
Between-study heterogeneity was assessed using Cochran’s Q. Also, the I 2-statistic was calculated. I 2 reflects the proportion of variation in observed effects that is due to variation in true effects (Borenstein, Higgins, Hedges, & Rothstein, 2017). I 2 values of 0.25, 0.50 and 0.75 are regarded as small, medium, and large, respectively (Higgins & Thompson, 2002). If the meta-analysis included at least 10 studies (Sterne et al., 2011) funnel plots (available in appendix) were generated in order to investigate if the overall effect sizes were influenced by publication bias. Publication bias is visually depicted by an asymmetric funnel plot where studies with small sample sizes and small effects are typically lacking (Harbord, Egger, & Sterne, 2006). The funnel plots were supplemented by the Duval and Tweedie’s (2000) trim and fill procedure which removes and imputes studies in order to make the funnel plot symmetric and subsequently recalculates an ‘unbiased’ overall effect size and 95% CI.
In order to estimate the robustness of the findings, Orwin’s Fail-safe N (Orwin, 1983) was calculated based on the number of studies with zero effects that would be needed to bring the overall effect down to a trivial level of g = 0.20, which is considered a small effect (Cohen, 1988). In cases of significant between-study heterogeneity, subgroup analyses was conducted. The subgroup analyses was based on the recommended (Borenstein et al., 2009) mixed effects model consisting of a random-effects model within subgroups pooling tau across groups as well as a fixed-effect model across subgroups. The subgroups were a priori determined and comprised studies with or without a control condition and studies with or without therapist support. A post hoc moderator, baseline severity of gambling problems (DSM-based diagnosis or PGSI ≥8 vs. studies with more lenient criteria), was also investigated. All analyses were conducted using Comprehensive Meta-Analysis 3.0 (Biostat Inc., 2014). Power analyses (Hedges & Pigott, 2004) for the moderator analyses were conducted setting alpha to 0.05 (two-tailed) and based on small (g = 0.20), medium (g = 0.50) and large (g = 0.80) effect sizes and the different subgroup variances.
Results
Literature search
The literature search was conducted by initial identification of relevant search words, among others by consulting a previous review on this topic (van der Maas et al., 2019). Relevant studies were then identified through searches in the following literature bases: PsycINFO, MEDLINE, Web of Science and the Cochrane library. The search covered the period to July 31, 2020. A supplementary search was conducted on May 1, 2021. It comprised different combinations of words reflecting gambling problems, such as ‘gambling disorder’, ‘gambling problems’ and ‘gambling addict’*, combined with terms related to treatment, such as ‘intervention’, ‘treatment’ and ‘therapy’, further combined with words related to internet, such as ‘online’, ‘web’ and ‘internet’. A comprehensive overview of search words used can be found in appendix. To ensure validity and to avoid errors, screening of potential studies was conducted independently by two authors. In case of disagreement, a third author was consulted, and the disagreement resolved through discussion. A total of 5,230 papers were initially identified. Based on title and abstract, 5,185 articles were excluded. After removal of duplicates, 45 papers remained where full text versions of all were thoroughly screened. Of these, 32 did not meet the inclusion criteria. A flow chart of the literature screening process is shown in Fig. 1.
Fig. 1.
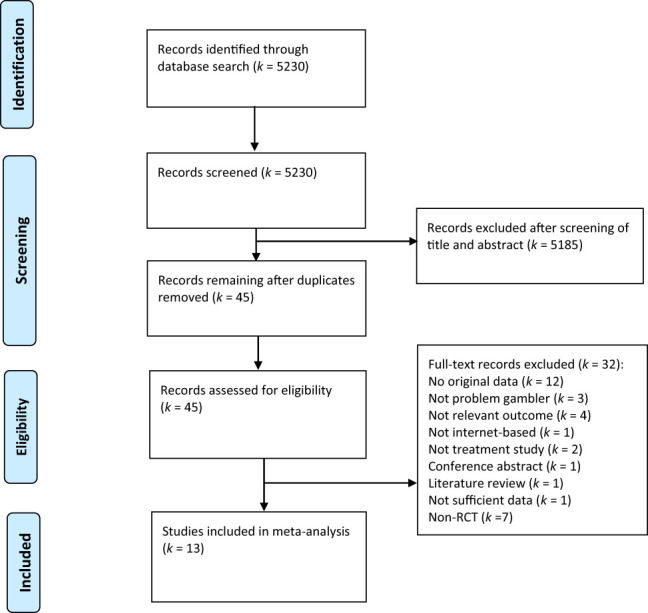
Flow chart of the literature search
Characteristics of the included studies
Table 1 provides an overview of the characteristics of the included studies. Of the 13 included studies, five were conducted in USA/Canada, three in Sweden, two in Germany, and one each from Australia, France, and Japan. Nine studies had a control condition whereas four had no control condition (e.g., two active treatments). The studies comprised a total of 2,183 participants with 1,587 in treatment groups and 596 in control groups. In two of the studies, participants fulfilled criteria for pathological gambling based on the DSM-IV (American Psychiatric Association, 1994). In ten studies participants scored above a cut-off score on a relevant diagnostic problem gambling instrument, or the group had an elevated mean score on the PGSI (Ferris & Wynne, 2001) or the SOGS (Lesieur & Blume, 1987). Finally, in one study, participants were self-referred.
Table 1.
Overview of study characteristics
| Study | Sample | Intervention | Contrast/control | Outcome | Missing data procedure | Data available at last follow-up | |||
| Age; M (SD) | Sex (%♂) | Country | Diagnostic procedure | ||||||
| Carlbring and Smit (2008) | 31.9 (9.8) | 94% | Sweden | DSM-IV (computerized screening interview) |
I-CBT (motivational interviewing, open-ended questions evoking change and CBT-techniques based on Hodgins (2002) and Ladouceur and Lachance (2006)) N = 34; eight sessions Therapist support was provided comprised feedback on homework assignments by email and a weekly telephone call |
Waitlist
N = 32 (at post, not at follow-up) |
NODS | LOCF | 36 months |
| Casey et al. (2017) | 44.4 | 41% | Australia | DSM-IV (online checklist) |
I-CBT (increased awareness of factor related to gambling behaviour, identifying and challenging thinking errors, imaginal exposure, relaxation, problem solving, dealing with negative emotions, relapse prevention). N = 60, six sessions. I-MFS (monitor gambling behavior, feedback on progress, supportive measures). N = 59, 6 sessions. No therapist support was provided |
Waitlist
N = 55 (at post only) |
GSAS SOGS GUS GRSEQ GRCS Frequency gambling Money spent |
Multilevel modelling | None |
| Cunningham, Hodgins et al. (2019) | 40.5 | 43% | USA/Canada | PGSI≥3 (self-report) |
I-CBT (based on self-help booklets by Hodgins (2002)). N = 102, optional no. sessions I-CBT + mood gym (internet intervention for mental health distress targeting depression and anxiety) N = 112, optional number of sessions No therapist support was provided |
Not applicable | NODS Frequency gambling |
Maximum likelihood | 6 months |
| Cunningham, Godinho et al. (2019) | 36.5 (10.9) | 45% | USA/Canada | PGSI≥5 3 (self-report) |
I-CBT (based on Hodgins, Fick, Murray, and Cunningham (2013)). N = 151, optional number of sessions No therapist support was provided |
No intervention
N = 170 (at post and follow-up) |
GSAS NODS Frequency gambling |
Maximum likelihood | 6 months |
| Cunningham et al. (2020) | 39.0 | 50% | USA/Canada | PGSI≥3 (self-report) |
I-CBT (based on self-help booklets by Hodgins (2002)). N = 143, optional number of sessions I-CBT+ alcohol feedback (comparative feedback on alcohol use) N = 139, optional number of sessions No therapist support was provided |
Not applicable | NODS Frequency gambling |
Maximum likelihood | 6 months |
| Hodgins et al. (2019) | 46.7 | 53% | USA/Canada | PGSI≥3 (self-report) |
I-CBT (self-assessment activities and behavioural and cognitive strategies for reducing and quitting gambling) N = 95, optional number of sessions No therapist support was provided |
Check Your Gambling (personalized feedback on gambling and advice on how to reduce/stop) N = 92, one session (at post and follow-up) |
NODS Frequency gambling Money lost |
Maximum likelihood | 12 months |
| Jonas et al. (2020) | 33.5 (11.5) | 72% | Germany | Self-referral |
Eclectic (clarifying situation, activating resources, establishing coping resources, diary of gambling behavior, develop control strategies, enhancing quality of life, evaluating pro and cons of gambling, gaining overview on debts developing emergency kits for high-risk situations, feed on diary and exercises. N = 54, optional number of sessions Therapist support was provided and comprised a 50 min admission chat, weekly feedback on diary/exercises and a 30-min concluding chat E-mail counselling (describe gambling, impact on life, reasons for stopping, feedback on how to cope, interaction based on solution-focused approach and motivational interviewing) N = 54, optional number of sessions Therapist support was provided and comprised time-lagged message exchanges |
Waitlist
N = 57 (at post but not at follow-up) |
PGSI Frequency gambling |
Multiple imputation | 12 months |
| Luquiens et al. (2016) | 34.7 (10.1) | 92% | France | PGSI≥5 (self-report) |
E-mailed I-CBT (based on Ladouceur and Lachance (2006). N = 14, six sessions Therapist support was provided and comprised weekly emails by psychologist with personalized guidance I-CBT self-help book (based on Ladouceur and Lachance 2006) N = 44, six sessions PNT (feedback on gambling category and prevalence information of category) N = 65, one session |
Waitlist
N = 65 (at post and follow-up). |
PGSI Frequency gambling Money lost |
Completers only | 3 months |
| Nilsson et al. (2018) | 36.8 | 89% | Sweden | PGSI≥8 (self-report) |
I-CBT (strategies handling cognitions and cravings, behavioral activation and functional analysis, motivation enhancement and psychoeducation). N = 8, ten sessions I-BCT (functional analysis, behavioral activation, strategies for handling gambling cognition and psychoeducation) N = 10, ten sessions Therapist support was provided for both conditions and comprised weekly counselling for 15 min |
Not applicable | NODS Money lost |
Bayesian Markov chain Monte Carlo | 6 months |
| Nilsson et al. (2020) | 35.6 (11.8) | 82% | Sweden | PGSI≥8 (self-report) |
I-CBT (psychoeducation, behavioral analysis, motivation enhancement, behavioral activation, cognitive restructuring, goalsetting, economic recovery, communication skills training, relapse prevention, repetition) N = 68, 10 sessions I-BCT (psychoeducation, behavioral analysis, motivation enhancement, behavioral activation, cognitive restructuring, goalsetting, economic recovery, communication skills training, reinforce positive behaviors, relapse prevention, repetition) N = 68, ten sessions Therapist support was provided for both conditions, comprising weekly counselling for 15 min |
Not applicable | NODS ICS Money lost |
Intent-to-treat | 12 months |
| Rosen et al. (2020) | 32.5 | 87% | USA | PGSI≥3 (self-report) |
Brief advise intervention (feedback regarding problem gambling, risk factors for development of problems, suggested ways to reduce risk) N = 51, one session No therapist support was provided |
Referral to treatment (informed about local resources to seek help) N = 51 (at post and follow-up) | ATGS-8 Frequency gambling Money spent |
Not applicable | 1 month |
| So et al. (2020) | 36.3 | 79% | Japan | PGSI≥3 (self-report) |
I-CBT (personalized feedback, monitoring, goalsetting, message about triggers, coping with urges, message about cognitive distortion) N = 96, 28 sessions No therapist support was provided |
Assessment only
N = 101, two sessions (at post only) |
PGSI GSAS Gambling frequency |
Multiple imputation | None |
| Wittekind et al. (2019) | 35.2 | 75% | Germany | SOGS≥1 (self-report) |
Approach bias modification (push all gambling related pictures – avoidance, pull all neutral picture – approach with computer mouse) N = 66, one session No therapist support was provided |
Sham (pushing and pulling were independent of picture content) N = 65, one session (at post only) |
PG-YBOCS | Multivariate imputation by chained equations | None |
ATGS-8: Attitudes Towards Gambling Scale-8. GRCS: Gambling Related Cognitions Scale. GRSEQ: Gambling Refusal Self-Efficacy Questionnaire. GSAS: Gambling Symptom Assessment Scale. GUS: Gambling Urge Scale. I-BCT: Internet behavioral couple therapy. I-CBT: Internet cognitive behavioral therapy. I-MFS: Internet based monitoring, feedback and support. ICS: Inventory of Consequences of Gambling for the Gambler and Concerned Significant Others. LOCF: Last observation carried forward. NODS: NORC Diagnostic Screening for Gambling Disorders. PG-YBOCS: Yale Brown Obsessive Compulsive Scale adapted for pathological gambling. PGSI: Problem Gambling Severity Index. PNT: Personalized normative feedback. SOGS: South Oaks Gambling Screen.
The weighted mean age across all studies was 37.9 years and 63% of the participants were male. Ten studies provided data for inclusion in follow-up analyses, where final follow-up ranged from one month to 36 months with a weighted mean of 8.3 months. All studies provided outcome data for general gambling symptoms, of which 10 also provided such data at follow-up. Eight studies reported data on gambling frequency post-treatment and seven reported such data at follow-up. Money lost was reported by five studies post-treatment and at follow-up, respectively.
Interventions in the included studies
The 13 included studies comprised a total of 22 interventions. Of these, 13 were based on CBT, of which four included feedback/support from a therapist. In one study, CBT was combined with interventions targeting unhealthy alcohol use and mental distress, respectively. Seven CBT-based interventions did not provide therapist assistance or any additional treatment components. Two interventions were based on personalized normative feedback, and one was based on monitoring, feedback, and support. One intervention was based on one session of brief advice. Additionally, one intervention was based on an eclectic approach encompassing elements from CBT, MI, and a solution-focused approach with therapist support. Two interventions comprised behavioral couple therapy, one consisted of simple advice via emails, and one was based on avoidance-learning related to gambling stimuli. The number of treatment sessions ranged from a single session to 28 sessions with a weighted mean of 9.9. In five studies, participants could log into the treatment program as often as they wanted. See Table 1.
Risk of bias of the included studies
The two reviewers disagreed on 12 of 65 items resulting in a concordance rate of 82%. Consensus was reached on the 12 discrepant items through discussion. Overall, all studies were evaluated as having some concerns. Across the five risk of bias criteria, studies were assessed as either low risk (45 of 65) or having some concerns (20 of 65). More specifically, all studies were evaluated as having low risk on deviations from intended interventions, as well as missing outcome data, and some concerns on outcome measurement. Additionally, one study (Luquiens et al., 2016) had some concerns regarding the randomization process and six studies (Carlbring & Smit, 2008; Casey et al., 2017; Nilsson, Magnusson, Carlbring, Andersson, & Gumpert, 2018; Nilsson, Magnusson, Carlbring, Andersson, & Hellner, 2020; Rosen, Weinstock, & Peter, 2020; Wittekind et al., 2019) were evaluated as having some concerns pertaining to selective reporting of results. The final risk of bias assessment is presented in Fig. 2.
Fig. 2.
Risk of bias judgement of the included studies
Power analyses for moderator analyses
Eleven moderator analyses were conducted. Expecting a small difference between subgroups (g = 0.20), the power varied between 0.05 and 0.26. Expecting a moderate subgroup difference (g = 0.50), the power varied between 0.19 and 0.91, of which two of 11 analyses yielded a power of 0.80 or above. In the cases of large subgroup differences (g = 0.80), the power varied between 0.40 and 1.0 where seven of 11 analyses yielded a power of 0.80 or higher.
Results at post-treatment
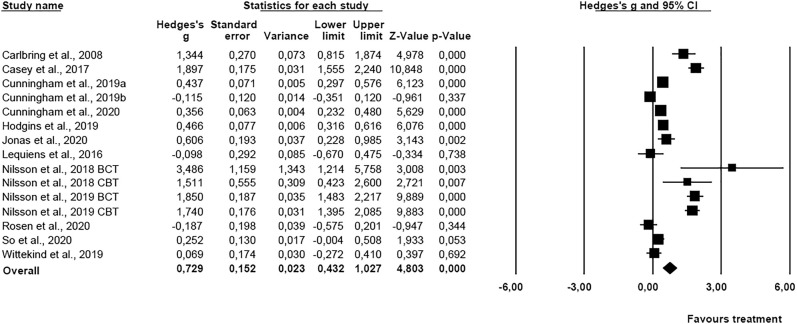
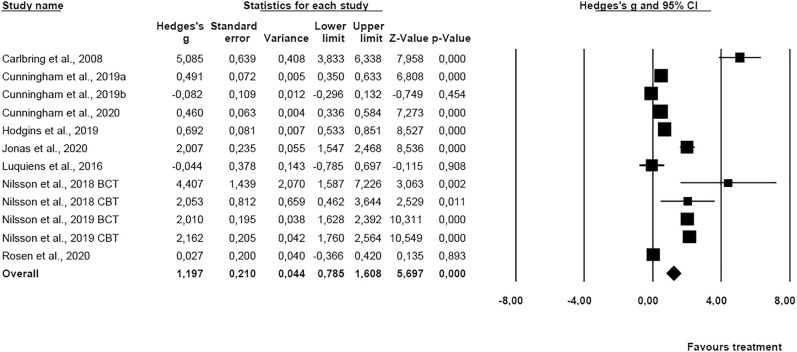
Results for symptoms at post-treatment (13 studies; N = 2,183) showed an overall effect size of g = 0.73 (95% CI = 0.43–1.03). See Fig. 3. Cochran’s Q was 243.96 (df = 14, P < 0.01) indicating significant heterogeneity, and the I 2 was 94.26. The funnel plot was not symmetric, and Duval and Tweedie’s trim and fill procedure yielded an adjusted overall effect size of 0.60 (95% CI = 0.29–0.90). Orwin’s Fail-safe N showed that 23 studies with zero effect size would be needed to bring the overall effect size down to a trivial level (g = 0.20). Due to the heterogeneity, subgroup analysis comparing studies with (k = 9) and without control groups (k = 6) were conducted. The difference between subgroups was significant (Q bet = 4.95, df = 1, P < 0.05) showing lower overall effect for studies with a control condition (g = 0.47, 95% CI = 0.07–0.87) than studies without a control condition (g = 1.23, 95% CI = 0.69–1.77).
Fig. 3.
Forest plot of the results for general symptoms at post-treatment
There was still significant heterogeneity within both subgroups (with: Q = 122.46, df = 8, P < 0.01, I 2 = 93.47; without: Q = 115.12, df = 5, P < 0.01, I 2 = 95.66. Also, subgroup analysis comparing studies with therapist support (k = 7) with studies without therapist support (k = 8) was conducted. The difference between subgroups was significant (Q bet = 9.95, df = 1, P < 0.01) indicating that studies with therapist support yielded a larger overall effect size (g = 1.23, 95% CI = 0.82–1.64, P < 0.01) compared to studies without therapist support (g = 0.39, 95% CI = 0.08–0.71, P < 0.05) at post-treatment. However, there were still significant heterogeneity within both subgroups (with: Q = 54.43, df = 6, P < 0.01, I 2 = 93.44; without: Q = 106.71, df = 7, P < 0.01, I 2 = 93.44). Studies with higher baseline severity of gambling problems were associated with a larger (Q bet = 99.68, df = 1, P < 0.01) effect size (k = 6, g = 1.76, 95% CI = 1.50–2.01) than studies with more lenient inclusion criteria (k = 9, g = 0.24, 95% CI = 0.09–0.39). There was still significant heterogeneity in the latter group (Q = 32.94, df = 8, P < 0.01, I 2 = 75.72).
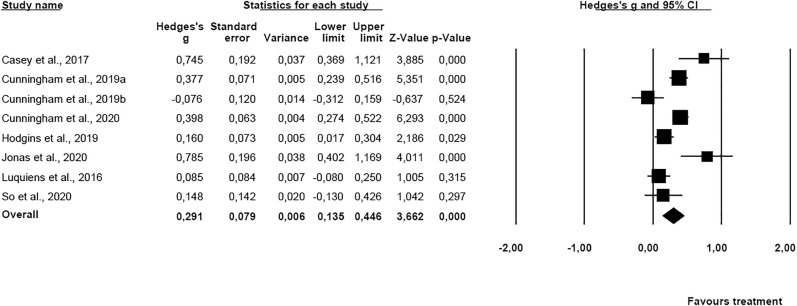
For gambling frequency at post-treatment (k = 8; N = 1,730), a significant overall effect size of g = 0.29 (95% CI = 0.14–0.45) was found (see Fig. 4). Cochran’s Q was 35.63 (df = 7, P < 0.01) showing significant heterogeneity, and the I 2 was 80.35. Orwin’s Fail-safe N showed that only three studies with zero effect size would be needed to bring the overall effect size down to a trivial level (g = 0.20). Subgroup analysis comparing studies with (k = 6) and without control groups (k = 2) were conducted. The difference between subgroups was however not significant (Q bet = 0.84, df = 1, P > 0.05). Neither were there effect size differences (Q = 0.14, df = 1, P = 0.71) between studies with therapist support (k = 2) and studies without therapist support (k = 6), nor between (Q = 3.34, df = 1, P > 0.05) studies with higher baseline severity of gambling problems (k = 1) and studies (k = 7) employing more lenient inclusion criteria.
Fig. 4.
Forest plot of the results for gambling frequency at post-treatment
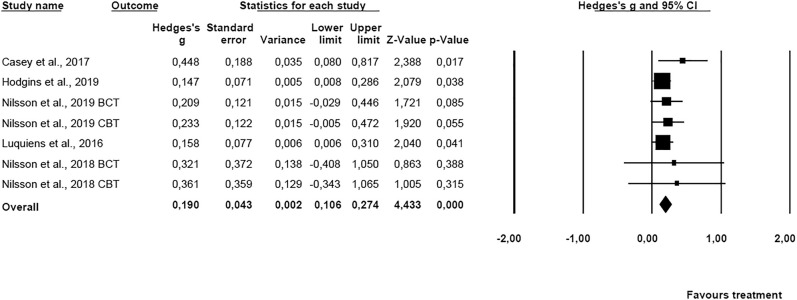
In terms of amount of money lost gambling at post-treatment (five studies; N = 515), the analysis yielded an overall significant effect of g = 0.19 (95% CI = 0.11–0.27) which is depicted in Fig. 5. Cochran’s Q was 2.94 (df = 6, P = 0.82) showing no heterogeneity across the effect sizes whereas I 2 was 0.00.
Fig. 5.
Forest plot of the results for money lost at post-treatment
Results at follow-up
Results for general gambling symptoms at follow-up (k = 10; N = 1,195) showed an overall effect size of g = 1.20 (95% CI = 0.79–1.61). See Fig. 6. Cochran’s Q was 264.17 (df = 11), P < 0.01 indicating significant heterogeneity, and the I 2 was 95.84. The funnel plot was asymmetric, and Duval and Tweedie’s trim and fill procedure resulted in adjustment of the overall effect size to 0.76 (95% CI = 0.34–1.18). Orwin’s Fail-safe N showed that 24 studies with zero effect size would be needed to bring the overall effect size down to a trivial level (g = 0.20). Subgroup analysis comparing results of studies with a control condition (k = 4) to those without (k = 8) showed lower effects in the former (g = 0.162, 95% CI = −0.558–0.882) compared to the latter group (g = 1.885, 95% CI = 1.318–2.453), with a Q bet of 13.56 (df = 1, P < 0.01). Significant heterogeneity remained in both subgroups (Q = 36.97, df = 3, P < 01, I 2 = 91.89 and Q = 206.15, df = 7, P < 0.01, I 2 = 96.60).
Fig. 6.
Forest plot of the results for general symptoms at follow-up
Regarding therapist support, the effect size in the subgroup of studies (k = 7) with therapist support had a larger overall effect size (g = 2.03, 95% CI = 1.62–2.44, P < 0.01) than the subgroup of studies without therapist support (k = 5, g = 0.33, 95% CI = −0.02–0.68, P > 0.05) with a Q bet of 38.15 (df = 1, P < 0.01). However, heterogeneity was significant in both subgroups (with: Q = 55.94, df = 6, P < 0.01, I 2 = 89.28; without: Q = 37.30, df = 4, P < 0.01, I 2 = 89.27). Baseline severity of gambling problems was also significant (Q bet = 40.36, df = 1, P < 0.01). Here, studies with higher baseline severity (k = 5) were associated with a larger effect size (g = 2.56, 95% CI = 2.02–3.10) than studies (k = 7) with more lenient inclusion criteria (g = 0.51, 95% CI = 0.18–0.84) concerning gambling problems. There was significant heterogeneity within both groups (higher severity: Q = 23.68, df = 4, P < 0.01, I 2 = 83.11; less stringent inclusion criteria: Q = 82.57, df = 6, P < 0.01, I 2 = 92.73).
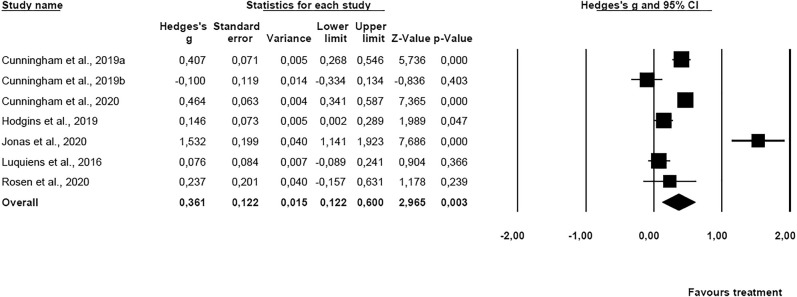
Regarding gambling frequency at post-treatment (k = 7; N = 1,461), a significant overall effect size of g = 0.36 (95% CI = 0.12–0.60) was found (see Fig. 7). Cochran’s Q was 70.05 (df = 6, P < 0.01) showing significant heterogeneity, and the I 2 was 91.43. Orwin’s Fail-safe N showed that four studies with zero effect would suffice to bring the overall effect size down to a trivial level (g = 0.20). Subgroup analysis comparing studies with a control condition (k = 4) to studies without a control condition (k = 3) showed lower effects in the former (g = 0.081, 95% CI = −0.170–0.332) compared to the latter group (g = 0.693, 95% CI = 0.407–0.979), with a Q bet of 9.93 (df = 1, P < 0.01). There was still significant heterogeneity within the group without control conditions (Q = 28.87, df = 2, P < 01, I 2 = 93.07). Also, subgroup analysis comparing the effect size across studies with therapist support (k = 2) to studies without therapist support (k = 5) showed no significant difference in terms of overall effect size between subgroups (Q bet = 2.52, df = 1, P = 0.11). Subgroup analysis for baseline severity of gambling problems on gambling frequency outcome was not possible because all studies belonged to the more lenient inclusion criteria.
Fig. 7.
Forest plot of the results for gambling frequency at follow-up
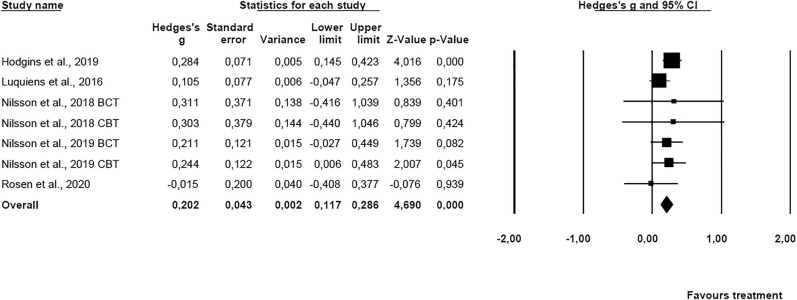
For amount of money lost gambling at follow-up (five studies; N = 443), the results showed a significant overall effect size of g = 0.20 (95% CI = 0.12–0.29). Figure 8 depicts the forest plot. Cochran’s Q was 4.37 (df = 5, P = 0.63) and I 2 was 0.00 indicating lack of heterogeneity. Orwin’s Fail-safe N showed that one study with zero effect would suffice to bring the overall effect size down to a trivial level (g = 0.20).
Fig. 8.
Forest plot of the results for money lost at follow-up
Discussion
The effect size for general gambling symptoms was large, suggesting that online interventions have a substantial impact from pre-treatment to post-treatment and at follow-up. For gambling frequency and amount of money lost gambling, small but significant effects were found post-treatment and at follow-up.
The meta-analysis by Goslar et al. (2017) comparing face-to-face treatment with self-help treatment reported large effects for the former treatment on general gambling symptoms (g = 1.15), and moderate effects on gambling frequency (g = 0.74) as well as amount of money lost gambling (g = 0.67). Compared to face-to-face treatment effects, the present meta-analysis suggests that internet-based treatment overall has a smaller but substantial effect on general gambling symptoms post-treatment. However, on gambling frequency and amount of money lost gambling, the findings of Goslar et al. (2017) suggest that face-to-face therapy is more effective than internet-based interventions. Compared to self-help treatments (e.g., written material or self-help workbooks) which yielded effect sizes for general gambling symptoms (g = 0.30), gambling frequency (g = 0.12), and amount of money lost gambling (g = 0.13) (Goslar et al., 2017), the present findings suggest that internet-based interventions are associated with better outcomes.
Additionally, previous meta-analyses (Cowlishaw et al., 2012; Gosslar et al., 2017) show larger treatment effects for general gambling symptoms than for gambling frequency and amount of money lost, which also was attested in the present meta-analysis. Whereas this suggests that gambling frequency and amount of money lost are more resistant to change, this finding may also reflect idiosyncratic characteristics of the two outcomes. General gambling symptoms are typically assessed with different screening instruments with inherent restrictions on scores and standard deviations. On the other hand, behavioral outcomes such as amount of money lost varies more between individuals, providing larger standard deviations and therefore smaller effect sizes. With regards to the latter, it has therefore been suggested that financial losses should be reported as a relative parameter (e.g., in relation to an individual’s income) rather than as an absolute parameter (Medeiros, Redden, Chamberlain, & Grant, 2018). The relative low effect size obtained for financial losses may also reflect that gamblers (e.g., at baseline) regularly underestimate their losses (Auer & Griffiths, 2017).
For general gambling symptoms and gambling frequency at follow-up, the subgroup analysis showed lower effect sizes in studies with control group compared to those without. This underlines the importance of including control groups as a means to correcting results for spontaneous recovery (Walker, 2005). The subgroup analyses further showed that studies with therapist support yielded larger effects than studies without such support on general gambling symptoms both post-treatment and at follow-up. This finding is in line with a literature review on the effects of psychological treatments for gambling problems (Rash & Petry, 2016) and suggests that therapist support may be a useful add-on to internet-based treatment of gambling problems.
In contrast to previous evidence (Merkouris et al., 2016), studies with higher baseline severity of gambling problems were associated with a better outcome regarding symptoms of gambling problems both at posttreatment and follow-up than studies employing more lenient inclusion criteria in terms of severity of gambling problems. This finding is in line with evidence from treatment studies on other addictions (Crits-Christoph et al., 2015; Tiet, Ilgen, Byrnes, Harris, & Finney, 2007), and suggests that those worse off at baseline have a larger treatment potential than those with less severe symptoms at baseline. It is also plausible that the studies with higher baseline severity of gambling problems have various unexplored study characteristics than those with more lenient inclusion criteria, and that these characteristics account for the subgroup differences (Tiet et al., 2007).
Although the moderators were significant in several of the subgroup analyses, there were still significant and high levels of heterogeneity within most subgroups. This implies that several factors not investigated in the present meta-analysis such as age, gambling severity, alcohol use, treatment compliance, employment status, ethnicity, gambling debts, personality traits, and action stage of change (Merkouris et al., 2016) may influence treatment outcomes. This denotes the importance of reporting how such factors are associated with treatment outcomes. Also, future studies are encouraged to examine treatment content and number of therapy sessions as potential moderators of treatment response as these factors have been suggested to affect outcome (Cowlishaw et al., 2012; Pallesen et al., 2005).
Methodical limitations
The included studies had some important limitations. As few studies had long follow-up time, uncertainty remains in terms of the lasting effects of treatments. While all studies included general gambling symptoms as an outcome, many did not report effects on gambling frequency and amount of money lost gambling. Future studies may better assess recovery by including measures of gambling frequency, amount of money lost gambling and other financial, health and social outcomes (Muggleton et al., 2021; Walker et al., 2006). It should also be noted that some studies had lenient inclusion criteria, below common cut-offs suggestive of gambling problems. In terms of bias of the included studies, the most noticeable limitations are that no study was based on probability sampling and that majority of the studies had a high attrition rate, as only three studies had a response rate above 80% at final assessment. Noticeably, all studies were conducted in Western Europe, North America, Australia, and Japan. Consequently, the generalizability of findings to other regions is uncertain.
A further limitation of the present meta-analysis is that grey literature was not included which may have led to an overestimation of the effects (Hopewell, McDonald, Clarke, & Egger, 2007). However, it has been argued that unpublished data are unlikely to have a significant impact on findings in meta-analyses (Schmucker et al., 2017) and that retrievable unpublished papers are not representative of unpublished literature in general (Higgins et al., 2019). Although significant, the findings related to gambling frequency and amount of money lost gambling show that few studies with zero findings would be needed to bring the results down to a trivial level. This suggests that findings for some of the outcomes are not stable.
Additionally, despite the high concordance rate of 82%, it is noteworthy that the updated Cochrane risk of bias tool (RoB 2) has been criticized for its complexity and poor agreement (Minozzi, Cinquini, Gianola, Gonzalez-Lorenzo, & Banzi, 2020). Importantly, as noted previously, consensus was reached on items of disagreement through discussion. Moreover, due to inconsistency in the reporting of outcomes of comorbid symptoms such as anxiety and depression across the included studies, they were not included in the present meta-analysis. Language restriction of inclusion of studies may also have limited the generalizability of the findings. Furthermore, because the effect sizes for studies with control conditions are based on comparisons at final measurement (posttreatment or follow-up), it is plausible that the results may have been biased in favor of studies with large between-condition differences at baseline. However, there is little reason to expect that the baseline differences yielded systematic bias across all studies (overall effect size). Finally, the power analyses for the moderator analyses show that, overall, they have low power when effect size differences between subgroups are small or moderate.
Conclusion
Internet-based treatments for gambling problems may overcome some of the obstacles (e.g., availability, costs, anonymity, and time) associated with face-to-face therapy for gambling problems. The current results suggest that internet-based treatment for gambling problems is effective, yielding high effects on general gambling symptoms, but small effects on gambling frequency and amount of money lost gambling. The treatment effects were upheld at follow-up. Still, the treatment field may advance further by for example employing mobile apps, which in addition, may provide ecological momentary interventions (Merkouris, Hawker, Rodda, Youssef, & Dowling, 2020).
Funding sources
The study was supported by the Norwegian Competence Center for Gambling and Gaming Research.
Authors’ contribution
SP and DS drafted the manuscript. SP conducted the analysis together with TH. DS, TH, IAL, MES, and SP coded the studies. All authors contributed critically to the text and all approved the final version of the manuscript.
Conflict of interests
DS, EKE, TH, TL, IAL, MES, and SP report no conflicts of interest. MDG’s university currently receives research funding from Norsk Tipping (the gambling operator owned by the Norwegian Government). MDG has also received funding for a number of research projects in the area of gambling education for young people, social responsibility in gambling and gambling treatment from Gamble Aware (formerly the Responsible Gambling Trust), a charitable body which funds its research program based on donations from the gambling industry. MDG regularly undertakes consultancy for various gaming companies in the area of social responsibility in gambling.
Appendix.
| Search terms and literature bases |
| Abbreviations: ‘ti’: title; ‘ab’: abstract; ‘kw’: keyword; ‘mp’ in MEDLINE include: title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms; ‘mp’ in PsycINFO includes: title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh; mesh: medical subject heading; ‘SCI-Expanded’: Science Citation Index Expanded; ‘SSCI’: Social Science Citation Index; ‘A&HCI’: Arts and Humanities Citation Index; ‘ESCI’: Emerging Sources Citation Index |
| The Cochrane Library |
| (gambling* OR “gambling problem*” OR “gambling patholog*” OR “gambling compuls*” OR “gambling addict*” OR “gambling disorder*”) AND (treatment* OR therap* OR intervention* OR CBT OR psychiatr* OR counsel* OR “e-therap*” OR etherap* OR “e-counsel*” OR ecounsel* OR cybercounsel* OR “cyber-counsel*” OR cybertherap* OR “cyber-therap*”) AND (internet* OR web* OR online* OR app* OR tablet* OR ipad*):ti,ab,kw (Word variations have been searched) |
| MEDLINE (Ovid) |
|
| PsycINFO (OvidSP) |
|
| Web of Science |
|
Funnel plot general symptoms post-treatment
Funnel plot general symptoms follow-up
References
- American Psychiatric Association . (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: American Psychiatric Association. [Google Scholar]
- Andersson, G. , & Titov, N. (2014). Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry , 13(1), 4–11. 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auer, M. , & Griffiths, M. D. (2017). Self-reported losses versus actual losses in online gambling: An empirical study. Journal of Gambling Studies , 33(3), 795–806. 10.1007/s10899-016-9648-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilevicius, E. , Edgerton, J. D. , Sanscartier, M. D. , Jiang, D. P. , & Keough, M. T. (2020). Examining gambling activity subtypes over time in a large sample of young adults. Addiction Research & Theory , 28(4), 305–313. 10.1080/16066359.2019.1647177. [DOI] [Google Scholar]
- Biostat Inc . (2014). Comprehensive meta-analysis, version 3.0 . Englewood, NJ: Biostat Inc. [Google Scholar]
- Bjørseth, B. , Simensen, J. O. , Bjørnethun, A. , Griffiths, M. D. , Erevik, E. K. , Leino, T. , & Pallesen, S. (2021). The effects of responsible gambling pop-up messages on gambling behaviors and cognitions: A systematic review and meta-analysis. Frontiers in Psychiatry , 11, 1670. 10.3389/fpsyt.2020.601800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein, M. , Hedges, L. V. , Higgins, J. P. T. , & Rothstein, H. R. (2009). Introduction to meta-analysis . Chichester: John Wiley & Sons. [Google Scholar]
- Borenstein, M. , Higgins, J. P. T. , Hedges, L. V. , & Rothstein, H. R. (2017). Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods , 8(1), 5–18. 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- Calado, F. , & Griffiths, M. D. (2016). Problem gambling worldwide: An update and systematic review of empirical research (2000–2015). Journal of Behavioral Addictions , 5(4), 592–613. 10.1556/2006.5.2016.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring, P. , & Smit, F. (2008). Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology , 76(6), 1090–1094. 10.1037/a0013603. [DOI] [PubMed] [Google Scholar]
- Casey, L. M. , Oei, T. P. S. , Raylu, N. , Horrigan, K. , Day, J. , Ireland, M. , & Clough, B. A. (2017). Internet-based delivery of cognitive behaviour therapy compared to monitoring, feedback and support for problem gambling: A randomised controlled trial. Journal of Gambling Studies , 33(3), 993–1010. 10.1007/s10899-016-9666-y. [DOI] [PubMed] [Google Scholar]
- Chebli, J. L. , Blaszczynski, A. , & Gainsbury, S. M. (2016). Internet-based interventions for addictive behaviours: A systematic review. Journal of Gambling Studies , 32(4), 1279–1304. 10.1007/s10899-016-9599-5. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Cowlishaw, S. , Merkouris, S. , Dowling, N. , Anderson, C. , Jackson, A. , & Thomas, S. (2012). Psychological therapies for pathological and problem gambling. Cochrane Database of Systematic Reviews , 11, Article No. CD008937. 10.1002/14651858.CD008937.pub2. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph, P. , Markell, H. M. , Gallop, R. , Gibbons, M. B. C. , McClure, B. , & Rotrosen, J. (2015). Predicting outcome of substance abuse treatment in a feedback study: Can recovery curves be improved upon? Psychotherapy Research , 25(6), 694–704. 10.1080/10503307.2014.994146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, J. A. , Godinho, A. , & Hodgins, D. C. (2019). Pilot randomized controlled trial of an online intervention for problem gamblers. Addictive Behavior Reports , 9, Article No. 100175. 10.1016/j.abrep.2019.100175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, J. A. , Hodgins, D. C. , Keough, M. , Hendershot, C. S. , Schell, C. , & Godinho, A. (2020). Online interventions for problem gamblers with and without co-occurring unhealthy alcohol use: Randomized controlled trial. Internet Interventions-the Application of Information Technology in Mental and Behavioural Health , 19, Article No. 100307. 10.1016/j.invent.2020.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, J. A. , Hodgins, D. C. , Mackenzie, C. S. , Godinho, A. , Schell, C. , Kushnir, V. , & Hendershot, C. S. (2019). Randomized controlled trial of an Internet intervention for problem gambling provided with or without access to an Internet intervention for co-occurring mental health distress. Internet Interventions-the Application of Information Technology in Mental and Behavioural Health , 17, Article No. 100239. 10.1016/j.invent.2019.100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFuentes-Merillas, L. , Koeter, M. W. J. , Schippers, G. M. , & van den Brink, W. (2004). Temporal stability of pathological scratchcard gambling among adult scratchcard buyers two years later. Addiction , 99(1), 117–127. 10.1111/j.1360-0443.2004.00601.x. [DOI] [PubMed] [Google Scholar]
- DerSimonian, R. , & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials , 7(3), 177–188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Duval, S. , & Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics , 56(2), 455–463. 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Ferris, J. , & Wynne, H. (2001). The Canadian problem gambling index . Final report. Ottawa: Canadian Centre on Substance Abuse. [Google Scholar]
- Follmann, D. , Elliott, P. , Suh, I. , & Cutler, J. (1992). Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology , 45(7), 769–773. 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- Gainsbury, S. , & Blaszczynski, A. (2011). A systematic review of Internet-based therapy for the treatment of addictions. Clinical Psychology Review , 31(3), 490–498. 10.1016/j.cpr.2010.11.007. [DOI] [PubMed] [Google Scholar]
- Giroux, I. , Goulet, A. , Mercier, J. , Jacques, C. , & Bouchard, S. (2017). Online and mobile interventions for problem gambling, alcohol, and drugs: A systematic review. Frontiers in Psychology , 8, Article No. 954. 10.3389/fpsyg.2017.00954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goslar, M. , Leibetseder, M. , Muench, H. M. , Hofmann, S. G. , & Laireiter, A. R. (2017). Efficacy of face-to-face versus self-guided treatments for disordered gambling: A meta-analysis. Journal of Behavioral Addictions , 6(2), 142–162. 10.1556/2006.6.2017.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths, M. , & Cooper, G. (2003). Online therapy: Implications for problem gamblers and clinicians. British Journal of Guidance & Counselling , 31(1), 113–135. 10.1080/0306988031000086206. [DOI] [Google Scholar]
- Griffiths, M. D. , Shonin, E. , & Van Gordon, W. (2016). Mindfulness as a treatment for gambling disorder: Current directions and issues. Journal of Gambling and Commercial Gaming Research , 1(1), 47–52. 10.17536/jgcgr.2016.004. [DOI] [Google Scholar]
- Harbord, R. M. , Egger, M. , & Sterne, J. A. C. (2006). A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Statistics in Medicine , 25(20), 3443–3457. 10.1002/sim.2380. [DOI] [PubMed] [Google Scholar]
- Hedges, L. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics , 6, 107–128. 10.2307/1164588. [DOI] [Google Scholar]
- Hedges, L. V. , & Pigott, T. D. (2004). The power of statistical tests for moderators in meta-analysis. Psychological Methods , 9(4), 426–445. 10.1037/1082-989X.9.4.426. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. , & Welch, V. A. (Eds.). (2019). Cochrane handbook for systematic reviews of interventions (2nd ed.). Chichester: John Wiley & Sons. [Google Scholar]
- Higgins, J. P. T. , & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine , 21(11), 1539–1558. 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Hodgins, D. (2002). Becoming a winner: Defeating problem gambling: A self-help manual for problem gamblers . Calgary: Calgary Regional Health Authority. [Google Scholar]
- Hodgins, D. C. , Cunningham, J. A. , Murray, R. , & Hagopian, S. (2019). Online self-directed interventions for gambling disorder: Randomized controlled trial. Journal of Gambling Studies , 35(2), 635–651. 10.1007/s10899-019-09830-7. [DOI] [PubMed] [Google Scholar]
- Hodgins, D. C. , & El-Guebaly, N. (2000). Natural and treatment-assisted recovery from gambling problems: A comparison of resolved and active gamblers. Addiction , 95(5), 777–789. 10.1046/j.1360-0443.2000.95577713.x. [DOI] [PubMed] [Google Scholar]
- Hodgins, D. C. , Fick, G. H. , Murray, R. , & Cunningham, J. A. (2013). Internet-based interventions for disordered gamblers: Study protocol for a randomized controlled trial of online self-directed cognitive-behavioural motivational therapy. BMC Public Health , 13. 10.1186/1471-2458-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopewell, S. , McDonald, S. , Clarke, M. J. , & Egger, M. (2007). Grey literature in meta-analyses of randomized trials of health care interventions. Cochrane Database of Systematic Reviews , 2, Article No. MR000010. 10.1002/14651858.MR000010.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas, B. , Leuschner, F. , Eiling, A. , Schoelen, C. , Soellner, R. , & Tossmann, P. (2020). Web-based Intervention and email-counseling for problem gamblers: Results of a randomized controlled trial. Journal of Gambling Studies , 36(4), 1341–1358. 10.1007/s10899-019-09883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladouceur, R. (2005). Controlled gambling for pathological gamblers. Journal of Gambling Studies , 21(1), 51–59. 10.1007/s10899-004-1923-9. [DOI] [PubMed] [Google Scholar]
- Ladouceur, R. , & Lachance, S. (2006). Overcoming your pathological gambling: Workbook. New York: Oxford University Press. [Google Scholar]
- Langham, E. , Thorne, H. , Borwne, M. , Donaldson, P. , Rose, J. , & Rocloff, M. (2016). Understanding gambling related harm: A proposed definition, conceptual framework and taxonomy of harms. BMC Public Health , 16, Article No. 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesieur, H. R. , & Blume, S. B. (1987). The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry , 144(9), 1184–1188. 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Luquiens, A. , Tanguy, M. L. , Lagadec, M. , Benyamina, A. , Aubin, H. J. , & Reynaud, M. (2016). The efficacy of three modalities of internet-based psychotherapy for non-treatment-seeking online problem gamblers: A randomized controlled trial. Journal of Medical Internet Research , 18(2), e36. 10.2196/jmir.4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson, F. I. , Sztainert, T. , Lakman, Y. , Steele, S. J. , Ziegler, C. P. , & Ferentzy, P. (2018). Prevention and treatment of problem gambling among older adults: A scoping review. Journal of Gambling Issues , 39, 6–66. 10.4309/jgi.2018.39.2. [DOI] [Google Scholar]
- Maynard, B. R. , Wilson, A. N. , Labuzienski, E. , & Whiting, S. W. (2018). Mindfulness-based approaches in the treatment of disordered gambling: A systematic review and meta-analysis. Research on Social Work Practice , 28(3), 348–362. 10.1177/1049731515606977. [DOI] [Google Scholar]
- Medeiros, G. C. , Redden, S. A. , Chamberlain, S. R. , & Grant, J. E. (2018). How to measure monetary losses in gambling disorder? An evidence-based refinement. Psychiatry Research , 263, 220–224. 10.1016/j.psychres.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkouris, S. S. , Hawker, C. O. , Rodda, S. N. , Youssef, G. J. , & Dowling, N. A. (2020). Gambling less: Curb Your Urge: Development and usability testing of a smartphone-delivered ecological momentary intervention for problem gambling. International Gambling Studies, Advanced online publication. 10.1080/14459795.2020.1749293. [DOI] [Google Scholar]
- Merkouris, S. S. , Thomas, S. A. , Browning, C. J. , & Dowling, N. A. (2016). Predictors of outcomes of psychological treatments for disordered gambling: A systematic review. Clinical Psychology Review , 48, 7–31. 10.1016/j.cpr.2016.06.004. [DOI] [PubMed] [Google Scholar]
- Miller, W. R. , & Rollnick, S. (2012). Motivational interviewing: Helping people change (3rd ed.). New York: Guilford Press. [Google Scholar]
- Minozzi, S. , Cinquini, M. , Gianola, S. , Gonzalez-Lorenzo, M. , & Banzi, R. (2020). The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. Journal of Clinical Epidemiology , 126, 37–44. 10.1016/j.jclinepi.2020.06.015. [DOI] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Grp, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology , 62(10), 1006–1012. 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Muggleton, N. , Parpart, P. , Newall, P. , Leake, D. , Gathergood, J. , & Stewart, N. (2021). The association between gambling and financial, social and health outcomes in big financial data. Nature Human Behaviour , 5(3), 319–326. 10.1038/s41562-020-01045-w. [DOI] [PubMed] [Google Scholar]
- Nelson, S. E. , Gebauer, L. , LaBrie, R. A. , & Shaffer, H. J. (2009). Gambling problem symptom patterns and stability across individual and timeframe. Psychology of Addictive Behaviors , 23(3), 523–533. 10.1037/a0016053. [DOI] [PubMed] [Google Scholar]
- Nilsson, A. , Magnusson, K. , Carlbring, P. , Andersson, G. , & Gumpert, C. (2018). The development of an internet-based treatment for problem gamblers and concerned significant others: A pilot randomized controlled trial. Journal of Gambling Studies , 34(2), 539–559. 10.1007/s10899-017-9704-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson, A. , Magnusson, K. , Carlbring, P. , Andersson, G. , & Hellner, C. (2020). Behavioral couples therapy versus cognitive behavioral therapy for problem gambling: A randomized controlled trial. Addiction , 115(7), 1330–1342. 10.1111/add.14900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orwin, R. G. (1983). The Fail-Safe N for effect size in meta-analysis. Journal of Educational Studies , 8(2), 157–159. 10.2307/1164923. [DOI] [Google Scholar]
- Pallesen, S. , Mitsem, M. , Kvale, G. , Johnsen, B. H. , & Molde, H. (2005). Outcome of psychological treatments of pathological gambling: A review and meta-analysis. Addiction , 100(10), 1412. 10.1111/j.1360-0443.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- Peter, S. C. , Brett, E. I. , Suda, M. T. , Leavens, E. L. S. , Miller, M. B. , Leffingwell, T. R. , … Meyers, A. W. (2019). A meta-analysis of brief personalized feedback interventions for problematic gambling. Journal of Gambling Studies , 35(2), 447–464. 10.1007/s10899-018-09818-9. [DOI] [PubMed] [Google Scholar]
- Quilty, L. C. , Wardell, J. D. , Thiruchselvam, T. , Keough, M. T. , & Hendershot, C. S. (2019). Brief interventions for problem gambling: A meta-analysis. PloS One , 14(4), e0214502. 10.1371/journal.pone.0214502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash, C. J. , & Petry, N. (2016). Psychological treatments for gambling disorder. Psychological Research and Behavior Management , 7, 285–295. 10.2147/PRBM.S40883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raylu, N. , & Oei, T. P. (2010). A cognitive behavioural therapy programme for problem gambling: Therapist manual . London: Routledge. [Google Scholar]
- Rockloff, M. J. , & Schofield, G. (2004). Factor analysis of barriers to treatment for problem gambling. Journal of Gambling Studies , 20(2), 121–126. 10.1023/B:JOGS.0000022305.01606.da. [DOI] [PubMed] [Google Scholar]
- Rosen, L. A. , Weinstock, J. , & Peter, S. C. (2020). A randomized clinical trial exploring gambling attitudes, barriers to treatment, and efficacy of a brief motivational intervention among ex-offenders with disordered gambling. Journal of Forensic Sciences , 65(5), 1646–1655. 10.1111/1556-4029.14476. [DOI] [PubMed] [Google Scholar]
- Schmucker, C. M. , Blümle, A. , Schell, L. K. , Schwarzer, G. , Oeller, P. , Cabrera, L. , … Meerpohl, J. J. (2017). Systematic review finds that study data not published in full text articles have unclear impact on meta-analyses results in medical research. PloS One , 12(4), e0176210. 10.1371/journal.pone.0176210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske, W. S. , Jackson, K. M. , & Sher, K. J. (2003). The natural history of problem gambling from age 18 to 29. Journal of Abnormal Psychology , 112(2), 263–274. 10.1037/0021-843x.112.2.263. [DOI] [PubMed] [Google Scholar]
- So, R. , Furukawa, T. A. , Matsushita, S. , Baba, T. , Matsuzaki, T. , Furuno, S. , … Higuchi, S. (2020). Unguided chatbot-delivered cognitive behavioural intervention for problem gamblers through messaging app: A randomised controlled trial. Journal of Gambling Studies , Advanced online publication. 10.1007/s10899-020-09935-4. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. C. , Savovic, J. , Page, M. J. , Elbers, R. G. , Blencowe, N. S. , Boutron, I. , … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. Bmj-British Medical Journal , 366. 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. C. , Sutton, A. J. , Ioannidis, J. P. A. , Terrin, N. , Jones, D. R. , Lau, J. , … Higgins, J. P. T. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj-British Medical Journal , 343. 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- Suurvali, H. , Cordingley, J. , Hodgins, D. C. , & Cunningham, J. (2009). Barriers to seeking help for gambling problems: A review of the empirical literature. Journal of Gambling Studies , 25(3), 407–424. 10.1007/s10899-009-9129-9. [DOI] [PubMed] [Google Scholar]
- Tiet, Q. Q. , Ilgen, M. A. , Byrnes, H. F. , Harris, A. H. , & Finney, J. W. (2007). Treatment setting and baseline substance use severity interact to predict patients’ outcomes. Addiction , 102(3), 432–440. 10.1111/j.1360-0443.2006.01717.x. [DOI] [PubMed] [Google Scholar]
- van der Maas, M. , Shi, J. , Elton-Marshall, T. , Hodgins, D. C. , Sanchez, S. , Lobo, D. S. S. , … Turner, N. E. (2019). Internet-based interventions for problem gambling: Scoping review. JMIR Mental Health , 6(1), Article No. e65. 10.2196/mental.9419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, M. B. (2005). Problems in measuring the effectiveness of cognitive therapy for pathological gambling. Journal of Gambling Studies , 21(1), 79–92. 10.1007/s10899-004-1927-5. [DOI] [PubMed] [Google Scholar]
- Walker, M. , Toneatto, T. , Potenza, M. N. , Petry, N. , Ladouceur, R. , Hodgins, D. C. , … Blaszczynski, A. (2006). A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta consensus. Addiction , 101(4), 504–511. 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- Wittekind, C. E. , Bierbrodt, J. , Ludecke, D. , Feist, A. , Hand, I. , & Moritz, S. (2019). Cognitive bias modification in problem and pathological gambling using a web-based approach-avoidance task: A pilot trial. Psychiatry Research , 272, 171–181. 10.1016/j.psychres.2018.12.075. [DOI] [PubMed] [Google Scholar]
- Yakovenko, I. , Quigley, L. , Hemmelgarn, B. R. , Hodgins, D. C. , & Ronksley, P. (2015). The efficacy of motivational interviewing for disordered gambling: Systematic review and meta-analysis. Addictive Behaviors , 43, 72–82. 10.1016/j.addbeh.2014.12.011. [DOI] [PubMed] [Google Scholar]