Abstract
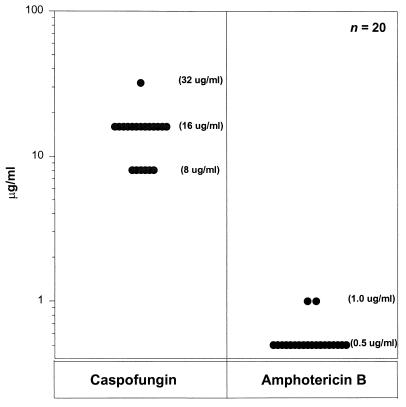
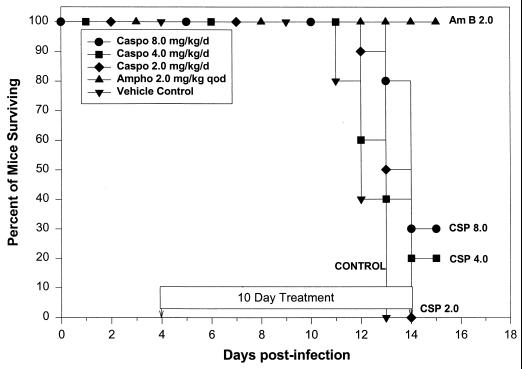
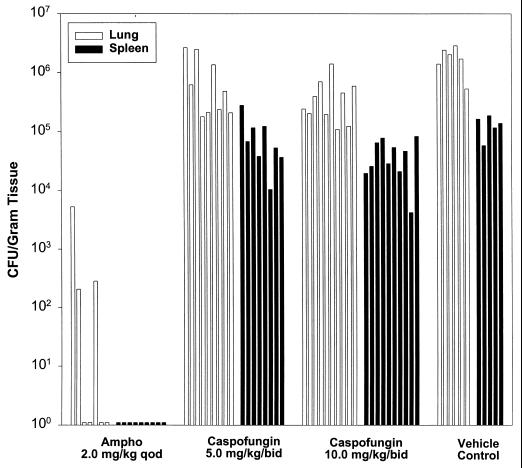
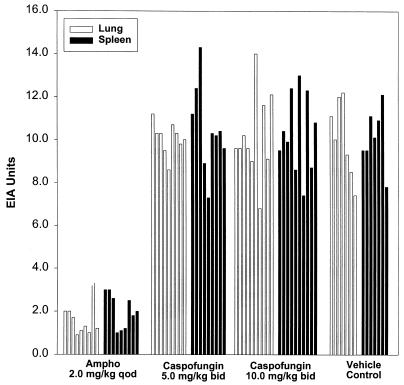
Twenty clinical isolates of Histoplasma capsulatum were tested for their in vitro susceptibilities to caspofungin in comparison to those to amphotericin B by following National Committee for Clinical Laboratory Standards guidelines for yeasts. The mean MICs were 16.6 μg/ml (range, 8 to 32 μg/ml) for caspofungin and 0.56 μg/ml (range, 0.5 to 1.0 μg/ml) for amphotericin B. Survival experiments used a 105 dose in a pulmonary challenge model with B6C3F1 mice. All mice that received amphotericin B at 2 mg/kg of body weight every other day (q.o.d.), 30% of mice that received caspofungin at 8 mg/kg/day, and 20% of mice that received caspofungin at 4 mg/kg/day survived to day 15, while mice that received caspofungin at 2 mg/kg/day and all control mice that received the vehicle died by day 14. Amphotericin B at 2 mg/kg q.o.d. markedly reduced the fungal burden in the lungs and spleens, as measured by Histoplasma antigen detection techniques and quantitative cultures, for each comparison. Caspofungin at 10 mg/kg twice a day (b.i.d.) did not reduce the fungal burden, as measured by antigen detection techniques, but slightly reduced the levels of fungi in both the lungs and spleens, as determined by quantitative cultures. Caspofungin at 5 mg/kg b.i.d. did not affect fungal burden. Overall, caspofungin had only a slight effect on survival or fungal burden.
Histoplasmosis is an important cause of progressive infection in immunocompromised individuals and those with underlying chronic lung disease. New compounds with fungicidal properties are desirable in patients with histoplasmosis to achieve a more rapid response, avoid resistance, and reduce toxicity associated with other agents. Cyclic hexapeptide compounds, which include the echinocandins, have been found to have potent antifungal activity. By specifically targeting the fungal cell wall enzyme 1,3-β-d-glucan synthase, these agents offer a fungicidal alternative to the azoles, while they avoid the toxicity associated with amphotericin B. By disrupting this enzyme, which is important in cell wall development, the osmotic balance is compromised, causing lysis in the cell (15).
The echinocandins were derived from fermentation products of Zalerion arboricola. Individual echinocandin compounds differ in various side chains (4). The semisynthetic echinocandins (L733560, L705589, L731373) are water soluble and have demonstrated efficacy for the treatment of aspergillosis, candidiasis, and Pneumocystis carinii infections (1, 3, 14, 15, 16). In addition, caspofungin (Merck Research Laboratories, Rahway, N.J.) has been shown to have activity in vitro against both Candida species and Aspergillus fumigatus and in vivo against Candida species (2, 9, 10, 13, 17), as well as possible efficacy in vitro against Cryptococcus neoformans when acting in synergy with amphotericin B or fluconazole (8). The purpose of this study was to evaluate caspofungin for its effect on survival and fungal burden in a pulmonary challenge model of histoplasmosis.
MATERIALS AND METHODS
In vitro susceptibility.
Suspensions of 20 different clinical isolates of Histoplasma capsulatum var. capsulatum yeasts were grown for 4 days on brain heart infusion (BHI) agar containing 5% sheep blood and were adjusted to a density equal to that of a no. 5 McFarland standard at 530 nm. Each suspension was diluted in RPMI 1640 medium and was added to the drug dilutions. Amphotericin B (Bristol-Myers Squibb, Princeton, N.J.) and caspofungin (Merck Research Laboratories) were diluted in dimethyl sulfoxide. Both drugs were tested at 10 concentrations of doubling dilutions. Broth macrodilution suspensions were incubated at 37°C and were read at 120 to 144 h by visual inspection. A Candida parapsilosis strain, ATCC 90018, was used as a control to ensure that the activities of the dilutions of amphotericin B fell in the expected range. The MIC was defined as the dilution at which there was no visible growth (18).
Pulmonary challenge model of histoplasmosis.
All procedures with animals were done in a class II hood. Infected animals were housed in isolation containment at the Indiana University Laboratory Research Facility. Six-week-old B6C3F1 mice (Jackson) were anesthetized with 4.5% halothane for 5 min at an oxygen flow rate of 0.9 liter/min. A 20-gauge plastic cannula (Becton Dickinson) was passed into the trachea to the bifurcation, and 25 μl of phosphate-buffered saline (pH 7.2) containing the inoculum of H. capsulatum yeast was administered. The yeast phase of a single clinical isolate of H. capsulatum (isolate IU-CT), maintained for the purpose of murine model experiments, was grown in HMM (19) medium in a 37°C incubator with shaking at 150 rpm for 48 h. The yeast culture was centrifuged and was washed with Hank's balanced salt solution–20 mM HEPES. The inoculum was adjusted with a hemacytometer. For survival studies, an inoculum of 105 yeasts in 25 μl was used. Fungal burden studies used a 104 inoculum in the same volume.
Antifungal treatment.
Treatment began at day 4 after infection and continued for 10 days. For the survival study, mice received caspofungin at 8, 4, and 2 mg/kg of body weight intraperitoneally (i.p.) once daily; doses were based on toxicity and pharmacokinetic data for mice and other published reports on caspofungin. Mice received amphotericin B in the form of Fungizone at a dose of 2 mg/kg i.p. every other day. Control mice were treated with the drug vehicle alone. Animals that survived to day 15 were killed. For the fungal burden study, mice received caspofungin at 10 and 5 mg/kg i.p. twice daily (b.i.d.). As in the survival study, mice received amphotericin B at a dose of 2 mg/kg i.p. every other day (q.o.d.) and control mice were treated with vehicle alone. Mice were killed 1 week after the completion of 10 days of treatment. Both lung and spleen tissues were then assessed for fungal burden by quantitative culture and antigen detection techniques.
Quantitative culture.
At the time of killing, the lungs and spleens were harvested aseptically. The organs were weighed and ground in Ten Broeck tissue grinders containing 2.0 ml of RPMI 1640 medium. Organ homogenates were diluted and plated on BHI agar containing 10% sheep blood. The plates were incubated for 10 days at 30°C, and colony counts were determined.
Histoplasma antigen immunoassay.
Histoplasma antigen was measured in diluted organ homogenates (1:10 for spleen and 1:100 for lung) by enzyme immunoassay (7). The enzyme immunoassay units (EU) were determined by dividing the mean value obtained for each organ by 1.5 times the mean value for the negative controls. Results of ≥1.0 are considered positive.
Statistical analysis.
For each study, a Kaplan-Meier survival curve was generated for each treatment arm, and the survival curves were assessed by a log-rank test. A one-way analysis of variance was performed on the ranks of the antigen levels and quantitative cultures. Pairwise comparisons of each treatment group to the control group were adjusted by Dunnett's multiple comparison procedure. An overall significance level of alpha equal to 0.05 was used to test all hypotheses (6).
RESULTS
In vitro susceptibility.
Susceptibility to caspofungin and amphotericin B was determined by testing 20 patient isolates of H. capsulatum. The mean MICs were 16.6 μg/ml, with a range of 8 to 32 μg/ml, for caspofungin and 0.56 μg/ml, with a range of 0.5 to 1.0 μg/ml, for amphotericin B (Fig. 1). The MICs for the isolate used for this study (isolate IU-CT) were 0.5 μg/ml for amphotericin B and 8 μg/ml for caspofungin. The caspofungin MIC for the Candida parapsillosis susceptibility control strain, strain ATCC 90018, was 1 μg/ml, documenting that the drug possessed the expected antifungal activity.
FIG. 1.
MICs of caspofungin and amphotericin B for the yeast phase of 20 clinical isolates of H. capsulatum.
Effect of caspofungin on survival following infection with 105 Histoplasma yeasts.
All mice that received amphotericin B at 2 mg/kg q.o.d. survived to day 15 (Fig. 2). At day 13, mice that received caspofungin at 8 mg/kg/day began to die, and by day 15, only 30% of these mice remained alive. Mice that received caspofungin at 4 mg/kg/day started to die by day 12, and 20% remained alive at day 15. By day 13, half of the mice that received caspofungin at 2 mg/kg/day died, and the remaining mice died on day 14. The control mice started to die at day 11, and all had died by day 13. Wilcoxon's test for survival analysis showed a statistical difference among these survival curves (P < 0.0001).
FIG. 2.
Survival of mice receiving an inoculum of 105 H. capsulatum yeasts. The Wilcoxon test for survival showed a statistical difference among the survival curves (P < 0.0001). CSP or Caspo, caspofungin; Ampho or Am B, amphotericin B.
Fungal burden at day 20 following infection with 104 Histoplasma yeasts.
Mice were treated with a higher dose of caspofungin (10 mg/kg b.i.d.) because of the poor outcome of dosing at 8 mg/kg once daily in the survival experiment. The group treated with caspofungin at 10 mg/kg b.i.d. had a median of 3.14 × 105 CFU/g of organ weight for the lung tissue, whereas control mice had a median of 1.85 × 106 CFU/g (P = 0.0026) (Fig. 3; Table 1). The median colony count in the spleen tissue of caspofungin-treated mice was 3.68 × 104 CFU/g of organ weight, whereas that in the spleen tissue of control mice was 1.34 × 105 CFU/g (P = 0.0020). For mice treated with caspofungin at 5 mg/kg b.i.d., the median numbers of CFU per gram of organ weight were 4.80 × 105 for the lung and 5.97 × 104 for the spleen (P = 0.0602 and P = 0.1068 versus controls, respectively). Among the group of mice (n = 9) treated with amphotericin B at 2 mg/kg q.o.d., four of seven mice had sterile lung tissue cultures and nine of nine mice had sterile spleen tissue cultures. Quantitative culture results for both the lung (median = 0) and the spleen (median = 0) for the amphotericin B group were statistically lower than those for the controls (median for the lung, 1.85 × 106 CFU/g; median for the spleen, 1.34 × 105 CFU/g) (P < 0.0001 for each group).
FIG. 3.
Quantitative culture results for lungs and spleens from mice killed on day 20 following infection with an inoculum of 104 H. capsulatum yeasts. Each bar represents one animal.
TABLE 1.
Results of antigen detection and quantitative culture in the lungs and spleen of mice infected with 104 yeasts and killed on day 20 postinfection
| Drug (concn [mg/kg]) | No. of mice | Median antigen level (EU)
|
Median quantitative culture result (CFU/g of organ weight)
|
||
|---|---|---|---|---|---|
| Lung | Spleen | Lung | Spleen | ||
| Amphotericin B (2.0) | 9 | 1.3 (<0.0001)a | 2.0 (<0.0001) | 0b (<0.0001) | 0b (<0.0001) |
| Caspofungin (10.0) | 10 | 9.6 (0.9981) | 10.2 (0.9960) | 3.14 × 105 (0.0026) | 3.68 × 104 (0.0020) |
| Caspofungin (5.0) | 9 | 10.3 (0.9860) | 10.3 (0.9330) | 4.80 × 105 (0.0602) | 5.97 × 104 (0.1068) |
| Untreated control | 7 | 10.0 | 10.1 | 1.85 × 106 | 1.34 × 105 |
Values in parentheses are P values.
The lungs of four of seven mice were sterile, while the spleens of nine of nine mice were sterile.
Fungal burden was also assessed by an antigen detection technique. Mice treated with caspofungin at 10 mg/kg b.i.d. (n = 10) had median lung antigen levels of 9.6 EU and median spleen antigen levels of 10.2 EU (Fig. 4 and Table 1). The antigen levels in both lung and spleen homogenates were 10.3 EU for mice treated with caspofungin at 5 mg/kg b.i.d. (n = 9). In the group treated with amphotericin B at 2 mg/kg q.o.d. (n = 9), the median antigen level in the lung was 1.3 EU (P < 0.0001) and that in the spleen was 2.0 EU (P < 0.0001), whereas the median antigen levels in the lungs and spleens of the untreated mice (n = 7) were 10.0 and 10.1 EU, respectively.
FIG. 4.
Histoplasma antigen concentrations in lungs and spleens from mice following infection with an inoculum of 104 H. capsulatum yeasts. Each bar represents one animal. The order of the animals in this figure is identical to that in Fig. 3 except for the cultures for the vehicle control mice; cultures were not evaluable for the lung from one animal and the spleens from two animals.
DISCUSSION
The murine model used in this study was created to establish a model with a mode of pathogenesis that resembles that which occurs in patients with histoplasmosis. By varying the severity of the exposure (infecting inoculum), in addition to modifying the immune status of the host, this model is useful in evaluating the efficacies of new antifungal compounds (5). Animals develop a pulmonary infection followed by hematogenous dissemination throughout the body. This model has been used to study other new antifungal agents (5) and to assess the immune response to infection with H. capsulatum.
Caspofungin demonstrated limited antifungal activity in vitro and limited efficacy in this pulmonary challenge model. Survival was not significantly prolonged in groups of mice that received doses of caspofungin of 4 or 8 mg/kg/day. Amphotericin B at 2 mg/kg q.o.d. completely prevented death during the course of the study, confirming the results presented in our earlier reports (5). Also, while amphotericin B markedly reduced the fungal burden in the lungs and spleens, caspofungin given at higher doses (10 mg/kg b.i.d.) than those used in the survival experiment lowered the quantitative culture colony counts only by 0.5 log. While this effect may not be clinically significant, it does suggest that caspofungin has some activity against H. capsulatum. Poor efficacy was not caused by inadequate dosing, as administration of a single i.p. dose of 1 mg/kg to mice yields peak levels in blood of 3 μg/ml and trough levels in blood of 0.3 μg/ml (12). On the basis of caspofungin's linear pharmacokinetics and its accumulation with repeated dosing, 10 mg/kg b.i.d. should yield peak concentrations above 60 μg/ml and trough levels above 6 μg/ml. Caspofungin was given i.p., which excludes poor absorption as a cause for failure. Furthermore, others found caspofungin dosed at 5 to 10 mg/kg/day to be effective against histoplasmosis (11). One other study showed caspofungin to be an effective treatment for histoplasmosis. In that report, caspofungin reduced the fungal burden and the rate of mortality following an intravenous challenge with the mould phase of H. capsulatum (11). Use of the yeast phase in our study rather than the mould phase should not account for the differences observed between the two studies. The mould phase transforms to the yeast phase within 48 h of infection, supporting the assumption that outcome relates more to the activity of caspofungin to the yeast phase than to the mould phase of the organism. The MIC for the isolate used in that study was 0.25 μg/ml. The MIC for the isolate used in our model was 8 μg/ml. We have found that the MICs for the yeast and mould phases varied only slightly in studies with amphotericin B and itraconazole (unpublished data), but similar studies have not been conducted with caspofungin. While the higher MIC for our strain is an obvious difference between the two studies, MICs were 8 μg/ml or higher for all 20 isolates tested in our susceptibility study, suggesting that our findings are likely broadly applicable.
Perhaps the different outcomes observed in these two studies could be explained, in part, by the different routes of infection, the different infecting strains of H. capsulatum, and/or the different strains of mice that were used. Additional experiments that evaluate each of these factors would be required to establish the reasons for the different outcomes of these two studies. Should caspofungin show promise in ongoing clinical trials that evaluate other fungal pathogens, further studies to assess its potential in histoplasmosis should be considered in view of the discrepancy of the finding of our study compared to that of the study of Graybill et al. (11).
ACKNOWLEDGMENT
This work was supported by a grant from Merck Research Laboratories using a model developed in a project sponsored by the U.S. Department of Veterans' Affairs.
REFERENCES
- 1.Abruzzo G K, Flattery A M, Gill C J, Kong L, Smith J G, Krupa D, Pikounis V B, Kropp H, Bartizal K. Evaluation of water-soluble pneumocandin analogs L-733560, L-705589, and L-731373 with mouse models of disseminated aspergillosis, candidiasis, and cryptococcosis. Antimicrob Agents Chemother. 1995;39:1077–1081. doi: 10.1128/aac.39.5.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartizal K, Gill C J, Abruzzo G K, Flattery A M, Kong L, Scott P M, Smith J G, Leighton C E, Bouffard A, Dropinski J F, Balkovec J. In vitro preclinical evaluation studies with the echinocandin antifungal MK-0991 (L-743,872) Antimicrob Agents Chemother. 1997;41:2326–2332. doi: 10.1128/aac.41.11.2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartizal K, Scott T, Abruzzo G K, Gill C J, Pacholok C, Lynch L, Kropp H. In vitro evaluation of the pneumocandin antifungal agent L-733560, a new water-soluble hybrid of L-705589 and L-731373. Antimicrob Agents Chemother. 1995;39:1070–1076. doi: 10.1128/aac.39.5.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouffard F A, Zambias R A, Dropinski J, Balkovec J M, Hammond M L, Abruzzo G, Bartizal K, Marrinan J, Kurtz M B, McFadden D, Nollstadt K, Powles M A, Schmatz D M. Synthesis and antifungal activity of novel cationic pneumocandin Bo derivatives. J Med Chem. 1994;37:222–225. doi: 10.1021/jm00028a003. [DOI] [PubMed] [Google Scholar]
- 5.Connolly P, Wheat J, Schnizlein-Bick C, Durkin M, Kohler S, Smedema M, Goldberg J, Brizendine E, Loebenberg D. Comparison of a new triazole antifungal agent, Schering 56592, with itraconazole and amphotericin B for treatment of histoplasmosis in immunocompetent mice. Antimicrob Agents Chemother. 1999;43:322–328. doi: 10.1128/aac.43.2.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conover W J, Iman R L. Rank transformations as a bridge between parametric and nonparametric statistics. Am Stat. 1981;35:124–129. [Google Scholar]
- 7.Durkin M M, Connolly P A, Wheat L J. Comparison of radioimmunoassay and enzyme-linked immunoassay methods for detection of Histoplasma capsulatum var. capsulatum antigen. J Clin Microbiol. 1997;35:2252–2255. doi: 10.1128/jcm.35.9.2252-2255.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franzot S P, Casadevall A. Pneumocandin L-743,872 enhances the activities of amphotericin B and fluconazole against Cryptococcus neoformans in vitro. Antimicrob Agents Chemother. 1997;41:331–336. doi: 10.1128/aac.41.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graybill J R, Bocanegra R, Luther M, Fothergill A, Rinaldi M J. Treatment of murine Candida krusei or Candida glabrata infection with L-743,872. Antimicrob Agents Chemother. 1997;41:1937–1939. doi: 10.1128/aac.41.9.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Graybill J R, Najvar L K, Luther M F, Fothergill A W. Treatment of murine disseminated candidiasis with L-743,872. Antimicrob Agents Chemother. 1997;41:1775–1777. doi: 10.1128/aac.41.8.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graybill J R, Najvar L K, Montalbo E M, Barchiesi F J, Luther M F, Rinaldi M G. Treatment of histoplasmosis with MK-991 (L-743,872) Antimicrob Agents Chemother. 1998;42:151–153. doi: 10.1128/aac.42.1.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hajdu R, Thompson R, Sundelof J G, Pelak B A, Bouffard F A, Dropinski J F, Kropp H. Preliminary animal pharmacokinetics of the parenteral antifungal agent MK-0991 (L-743,872) Antimicrob Agents Chemother. 1997;41:2339–2344. doi: 10.1128/aac.41.11.2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krishnarao T V, Galgiani J N. Comparison of the in vitro activities of the echinocandin LY303366, the pneumocandin MK-0991, and fluconazole against Candida species and Cryptococcus neoformans. Antimicrob Agents Chemother. 1997;41:1957–1960. doi: 10.1128/aac.41.9.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurtz M B, Bernard E M, Edwards F F, Marrinan J A, Dropinski J, Douglas C M, Armstrong D. Aerosol and parenteral pneumocandins are effective in a rat model of pulmonary aspergillosis. Antimicrob Agents Chemother. 1995;39:1784–1789. doi: 10.1128/aac.39.8.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurtz M B, Douglas C, Marrinan J, Nollstadt K, Onishi J, Dreikorn S, Milligan J, Mandala S, Thompson J, Balkovec J M, Bouffard F A, Dropinski J F, Hammond M L, Zambias R A, Abruzzo G, Bartizal K, McManus O B, Garcia M L. Increased antifungal activity of L-733,560, a water-soluble, semisynthetic pneumocandin, is due to enhanced inhibition of cell wall synthesis. Antimicrob Agents Chemother. 1994;38:2750–2757. doi: 10.1128/aac.38.12.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmatz D M, Powles M A, McFadden D, Nollstadt K, Bouffard F A, Dropinski J, Liberator P, Anderson J. New semisynthetic pneumocandins with improved efficacies against Pneumocystis carinii in the rat. Antimicrob Agents Chemother. 1995;39:1320–1323. doi: 10.1128/aac.39.6.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vazquez J A, Lynch M, Boikov D, Sobel J D. In vitro activity of a new pneumocandin antifungal, L-743,872, against azole-susceptible and -resistant Candida species. Antimicrob Agents Chemother. 1997;41:1612–1614. doi: 10.1128/aac.41.7.1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waitz J A, Bartlett M S, Ghannoum M A, Espinel-Ingroff A, Lancaster M V, Odds F C, Pfaller M A, Rex J H, Rinaldi M G, Walsh T J, Galgiani J N. Reference method of broth dilution antifungal susceptibility testing of yeasts. 1997. pp. 1–29. . Approved standard M27-A. National Committee for Clinical Laboratory Standards, Wayne, Pa. [Google Scholar]
- 19.Worsham P L, Goldman W E. Selection and characterization of ura5 mutants of Histoplasma capsulatum. Mol Gen Genet. 1988;214:348–352. doi: 10.1007/BF00337734. [DOI] [PubMed] [Google Scholar]