Abstract
Limited research has examined coronavirus disease 2019 (COVID-19)-related work stressors experienced by nursing home (NH) employees and how these stressors may impact employees’ decision to resign when taking organizational factors into account. Thus, the purpose of this study was to investigate whether quality of employer communication related to COVID-19 and staff preparedness to care for residents with COVID-19 can mediate the effects of COVID-19-related stressors on NH employees’ (N = 1,730) decision to resign. Results from path analyses indicate that higher quality of communication and more optimal preparedness mediated the relationship between COVID-19-related stressors and likelihood of resignation. Specifically, higher levels of COVID-19-related stressors were indirectly associated with reduced likelihood of resigning through the paths of more optimal communication and preparedness. Findings underscore the importance of effective employer communication during emergencies in NHs.
Keywords: long-term care workforce, turnover, direct care workforce, organizational supports, COVID-19, nursing homes, stress
Introduction
Nursing homes (NHs) have faced an unprecedented crisis due to the rapid spread of coronavirus disease 2019 (COVID-19)—a flu virus that is particularly challenging and potentially fatal for older adults and individuals with complex medical conditions. The pandemic has not only had a devastating impact on NH residents, but also negatively affected NH workers (e.g., nursing assistants) who were on the frontlines providing hands-on care. In fact, estimates indicate that since the beginning of the pandemic until early February 2021, more than 1.2 million COVID-19 cases occurred in long-term care facilities and more than 160,000 residents and staff at long-term care facilities have died from COVID-19, accounting for 36% of all coronavirus-related deaths nation-wide (The COVID Tracking Project, 2021).
The high COVID-19 infection rates and deaths among workers in NHs are not only likely due to their daily exposure to residents with COVID-19, but also because many reside in areas with high COVID-19 infection rates (Almeida et al., 2020). Their vulnerability to COVID-19-related infection and death is compounded by the challenges faced by many low-income workers (e.g., reliance on risky mass transportation, food insecurity, lack of childcare, and no paid sick leave). Furthermore, a large proportion of long-term care workers, including NH workers, are people of color who are more likely to have comorbidities (e.g., hypertension, diabetes) that are associated with increased risk of severe illness and mortality from COVID-19 (Greene & Gibson, 2021; Gross et al., 2020; Koma et al., 2020; Laurencin & McClinton, 2020).
In addition to threats to their physical health, health care workers have experienced a variety of other stressors as a result of the pandemic. Emerging work has begun to highlight the experiences of NH workers during the COVID-19 pandemic. White and colleagues (2021) conducted a qualitative study on the experiences of frontline NH staff and found the following emerging themes: fears of infecting themselves and their families, sincere empathy and concern for their residents, burnout due to increased workloads, staffing shortages, and the emotional burden of caring for residents facing significant isolation, illness, and death. In addition to severe work-related stressors and the likelihood of these stressors to have a spillover effect on workers’ private lives, NH workers are also likely to have been affected by the negative media coverage of residential care facilities during the pandemic. Allen and Ayalon (2021) analyzed the content of 54 articles from U.S. newspapers and found that the articles portrayed residential care as a shockingly dangerous setting and referred to it as a deceptive and problematic industry. Because of the exposure to these stressors, in addition to the intense pressure to care for COVID-19 patients, and the looming threat of COVID-19 to workers’ physical health, frontline workers’ mental health has also been negatively impacted during the pandemic (Kirzinger et al., 2020; Tomlin et al., 2020; Wu et al., 2020).
Research has recently begun to investigate factors that can support NH workers in these difficult times and mitigate some of the negative impact of the intense strain experienced during the pandemic. Research in this area has documented that organizational supports (e.g., support from a supervisor) can buffer some of the negative effects of increased NH employee workload and work-related stress experienced when caring for residents with COVID-19 (Blanco-Donoso et al., 2020). Furthermore, a qualitative study found that NH workers identified the presence (or lack) of organizational communication and teamwork as important factors influencing their ability to work under challenging circumstances during the pandemic (White et al., 2021). To our knowledge, these are the only two studies that have examined the relationship between work stress and organizational factors among NH workers during the COVID-19 pandemic.
In addition to this paucity of research examining the impact of organizational supports on work-related strain, there is essentially no research that has investigated how work-related stress and organizational supports, such as COVID-19-related communication provided by employers, may contribute to turnover, specifically work resignation, in NHs during the pandemic.
As a result of COVID-19, staff shortages in NHs were prevalent (U.S. Public Interest Research Group [PIRG] Education Fund, 2021). The investigation of factors associated with NH employee resignation during the pandemic is important because staffing levels and turnover impact the quality of care in NHs. For example, more optimal staffing levels (e.g., appropriate number of nursing assistants’ hours per resident) have been found to be associated with better NH quality outcomes (see Castle, 2008 for a review). Recent COVID-19-related research demonstrated that higher numbers of overall nursing and aid hours were associated with a reduced likelihood of experiencing an outbreak and fewer deaths in NHs that had at least one COVID case (Figueroa et al., 2020; Gorges & Konetzka, 2020). Furthermore, high staff turnover rates in NHs negatively affect resident health outcomes (e.g., higher odds of pressure ulcers) as well as resident and family satisfaction with care (Bishop et al., 2008; Trinkoff et al., 2013). Therefore, it is critical for the well-being of residents that NHs maintain optimal staffing levels and have low turnover rates, particularly during the pandemic. However, it is unknown which factors influence NH workers’ decision to resign from their job during the highly stressful times of the COVID-19 pandemic.
Therefore, additional research is needed to gain further insights into what factors can aid in preventing staff turnover during a pandemic. Prior research on NH staff turnover in the pre-COVID-19 era has led to the development of conceptual frameworks proposing a myriad of factors involved in an NH employee’s decision to resign from their job. These include sociodemographic characteristics (e.g., ethnicity), role-related characteristics (e.g., tenure), job characteristics (e.g., work schedule, work content, and job satisfaction), organizational characteristics (e.g., facility size, training, and quality of workplace supports), availability of jobs, and intent to leave (e.g., Castle et al., 2007; Temkin-Greener et al., 2020). Knowledge of organizational factors impacting job resignation is of relevance for NH leadership for the design of specific measures and interventions that can potentially prevent employee job resignation and reduce turnover in NHs, especially during times of crises such as a pandemic. Unfortunately, there is a lack of research on organizational factors that may have impacted job resignation among NH workers during the COVID-19 pandemic. More specifically, what remains unclear is whether the quality of COVID-19-related communication provided by employers is associated with workers’ preparedness to care for residents and how both factors may influence NH workers’ decision to resign from their job in the highly stressful work environment during a pandemic.
The Current Study
Using data from a sample of resigned and currently employed NH workers, the first aim of our study was to describe COVID-19-related stressors and to explore whether COVID-19-related stressors differed by resignation status (resigned vs. still employed). In this study, we operationalized COVID-19-related stressors by measuring overall COVID-19 work-related stress levels and the types and number of stressful work-related and non-work-specific challenges (e.g., lack of childcare) experienced due to COVID-19. The second aim of the study was to investigate whether high-quality employer communication regarding COVID-19 (an organizational support) can mediate the impact of COVID-19-related stressors on NH workers’ decision to resign by optimizing workers’ preparedness to care for residents with COVID-19. Figure 1 depicts the conceptual model for the second study aim. Past research indicates that open communication by NH leadership is linked to more optimal staff performance (Vogelsmeier & Scott-Cawiezell, 2011). Furthermore, lack of training and skills is associated with higher staff turnover in NHs (Temkin-Greener et al., 2020). Therefore, our central hypothesis was that, under circumstances of high work-related stress during the pandemic, if employer communication is qualitatively high, employees will feel more prepared to care for residents, and as a result will be less likely to resign. Thus, the intent of this part of the study was to test for serial mediation. Specifically, under the second study aim, we hypothesized the following relationships among study variables:
Figure 1.
Conceptual model with hypotheses.
Note. 1: (a) Higher levels of COVID-19-related stressors will be directly associated with less optimal preparedness, and (b) higher quality of employer communication will mediate the negative effects of COVID-19-related stressors on preparedness. 2: (a) Higher quality of employer communication will be directly associated with improved employee preparedness and with reduced likelihood of job resignation, and (b) higher quality of communication will be indirectly associated with a decreased likelihood of job resignation through improved employee preparedness. 3: (a) Higher levels of COVID-19-related stressors will be directly associated with an increased likelihood of job resignation, and (b) this negative effect will be mediated by both higher quality of employer communication associated improved employee preparedness and associated improved employee preparedness.
Hypothesis 1 (H1): (a) Higher levels of COVID-19-related stressors will be directly associated with less optimal preparedness, and (b) higher quality of employer communication will mediate the negative effects of COVID-19-related stressors on preparedness.
Hypothesis 2 (H2): (a) Higher quality of employer communication will be directly associated with improved employee preparedness and with reduced likelihood of job resignation, and (b) higher quality of communication will be indirectly associated with a decreased likelihood of job resignation through improved employee preparedness.
Hypothesis 3 (H3): (a) Higher levels of COVID-19-related stressors will be directly associated with an increased likelihood of job resignation, and (b) this negative effect will be mediated by both higher quality of employer communication and associated improved employee preparedness.
Method
Study Participants
One thousand eight hundred sixty-four NH workers completed a WeCare Connect™ (WCC) interview in May 2020. Of these 1,864 NH workers who were employed in May 2020, 263 resigned and the services of 134 were terminated between June and November 2020. Therefore, 1,467 NH workers were still employed at the end of November 2020. Only including those who resigned and who were still employed (N = 1,730), the resignation rate for NH workers in our study was 15%. The 263 employees who had resigned had been employed on average for about 1 year in May 2020. In contrast, the average length of employment of currently employed workers was about 2 years. About half of the participants in each of the two employment groups were certified nursing assistants (CNAs) and aides—51% in the resigned group and 44% in the still employed group were CNAs. About 20% in each group were registered nurses (RNs) or licensed practical nurses (LPNs), and the remaining were dietary and environmental service workers, therapists, and social workers.
Procedures
In April 2020, the study team formed a partnership with WCC to investigate the impact of COVID-19 on the long-term services and supports (LTSS) workforce. WCC is a program/service utilized by 165 aging services providers at 1,000+ locations around the United States. WCC is an innovative employee engagement and management system that supports organizations in better understanding staff members’ challenges with onboarding, training, supervisory relationships, job fit, expectations, and the physical and organizational environment. WCC staff reach out and get ongoing feedback from new and existing employees, as well as from employees who resign, and inform the appropriate people in an organization of any employee-related issues to facilitate continuous quality improvement. To obtain data on the impact of COVID-19 in LTSS settings, WCC—for the month of May 2020—added questions designed by the study team to their employee interview battery. The questions assessed employees’ overall stress and specific types of COVID-19-related stressful work and non-work-specific challenges experienced, as well as perceptions of the quality of organizational communication around COVID-19 and workers’ perceived preparedness to care for residents with COVID-19. At the end of November 2020, we obtained the employment status—using a 6-month look back period—of NH employees who had answered the COVID-19-related questions in May 2020. Then, we determined which of the workers who were employed in May 2020 had either resigned or were terminated, as well as which employees remained employed over the 6-month period from June to November 2020. The study was approved by the internal review board of the researchers’ institution (IRB No. 2020174).
Measures
NH worker characteristics.
Single items were used to assess worker position and work tenure in years. We formed a variable called direct care staff (1 = yes, 0 = no) based on positions. CNAs and aides were categorized as direct care workers and all other workers as non–direct care workers. Furthermore, based on the follow-up in respect to employment status, employees were categorized as resigned or not (1 = yes, 0 = no).
COVID-19-related stressors: COVID-19-related overall stress level and challenges.
To obtain an indicator of general stress level, we used one item asking participants to rate how stressed they felt overall as an employee during the COVID-19 pandemic on a scale from 1 to 5 (“Overall, how stressed do you feel as an employee during this COVID-19 pandemic?” 1 = not stressed at all; 5 = extremely stressed). To assess stressful work-related challenges, participants were presented with a list of five challenges asking them to indicate which COVID-19-related work challenges caused them stress when caring for residents, including lack of personal protective equipment (i.e., N95 masks and gowns), lack of organizational protocols/guidance to care for residents, increased workload demands, increased risk of transmission to/from residents, and understaffing. Similarly, to assess stressful non-work-specific challenges, participants were presented with a list of five challenges asking them to indicate which stressful non-work-specific challenges they faced due to COVID-19, including lack of childcare, lack of transportation, separation from family members, managing the personal needs and demands of family, and experiencing financial hardship. We calculated two challenge indicators—one for work-related challenges and one for non-work-specific challenges—by adding the number of stressful challenges experienced in each of the two challenge domains.
Perceived quality of organizational/employer communication around COVID-19.
We used two items to assess the quality of organizational communication around COVID-19. The first item asked participants to rate their organization’s communication with them regarding how to protect themselves and their family during the COVID-19 pandemic (“How would you rate your organization’s communication with you regarding how to protect yourself and your family during the COVID-19 pandemic?” 1 = does not keep us informed at all; 5 = keeps us fully informed); the other item asked participants to rate the quality of their organization’s communication with them regarding how to care for residents and protect them during the COVID-19 pandemic (“How would you rate your organization’s communication with you regarding how to care for residents and protect them during the COVID-19 pandemic?” 1 = does not keep us informed at all; 5 = keeps us fully informed). Scores on the two items were summed to obtain one indicator of quality of employer communication. Cronbach’s alpha for the two-item scale was .91.
Worker’s perceived preparedness to care for residents during COVID-19.
To gauge worker preparedness, we utilized one item asking participants to rate overall how prepared they felt to care for a resident with known or suspected COVID-19 (“Overall, how prepared are you to care for a resident/patient/client with known or suspected COVID-19?” 1 = not prepared at all; 5 = extremely prepared).
Data Analysis Plan
Descriptive and bivariate analyses (chi-square analyses and independent-samples t tests) comparing current employees with those who resigned during the 6 months after May 2020 were run on all study variables. To examine the mediating roles of quality of communication and preparedness on likelihood of job resignation in the relationship between COVID-19-related stressors and resignation, three separate path analytic models, using observed variables, were run. Our indicators of COVID-19-related stressors (the overall stress rating, the number of stressful work-related challenges, and the number of stressful non-work-specific challenges) were examined in separate models. In all three path analyses, we obtained direct and indirect effects to examine the effects of COVID-19-related stressors, quality of communication, and preparedness on likelihood of job resignation while controlling for direct care worker status and length of employment. IBM SPSS AMOS Version 25 for structural equation modeling (SEM) was used to estimate the serial mediation (Hayes, 2017), based on our hypothesized conceptual model (Figure 1) of quality of communication and job preparedness in the association between COVID-19-related stressors on job resignation. Assessment of direct and indirect effects followed published guidelines (Hayes, 2017; Lee, 2020; Preacher & Hayes, 2008; Yu et al., 2020; Zhao et al., 2010). User-defined estimands and bootstrapping analysis were used to identify the directional relationships among the two proposed mediators. Bootstrapping, a nonparametric resampling technique with replacement that can mitigate issues surrounding low power and non-normality (e.g., Bollen & Stine, 1990), was used to derive 95% bias-corrected confidence intervals with 5,000 bootstrapped resamples (Preacher & Hayes, 2008; Zhao et al., 2010). Bootstrapping methods require no missing data; thus, multiple imputation based on regression was used to address cases of missing data. Several fit indices were evaluated to assess model fit, including the chi-square statistics, chi-square ratio (χ2/df), the comparative fit index (CFI), and the root mean square error of approximation (RMSEA).
Results
Frequency and Bivariate Analyses.
Table 1 depicts frequencies and p values of the chi-square analyses for work-related and non-work-specific challenges by employment status. It appears that, among both resigned and current employees, increased risk of COVID-19 transmission, increased workload demands, and understaffing were the most frequently mentioned stressful work challenges. Furthermore, in both groups, separation from family members, managing personal needs and family demands, and experiencing financial hardship emerged as the top three stressful non-work-specific challenges faced by employees. Chi-square analyses examining each of the stressful work-related and non-work-specific challenges based on resignation status yielded only one statistically significant result: unexpectedly, employees who resigned after May 2020 were less likely to have reported lack of childcare as a challenge in May 2020. Furthermore, the average number for both stressful work-related and non-work-specific challenges was 1, with the number of challenges ranging from 0 to 5. The average overall stress level was 2.8. Independent-samples t tests identified no significant differences in the number of stressful work-related challenges, number of stressful non-work-specific challenges, and overall stress level based on resignation status (Table 1). However, independent-samples t-test results revealed that current employees had significantly higher mean scores on the two quality of communication indicators and the preparedness rating when compared with resigned employees (Table 1).
Table 1.
Chi-Square Analyses of COVID-19-Related Challenges and Independent t Tests for Study Variables by Employment Status.
| Predictor Variables | Resigned employees (n = 256) % (n) |
Current employees (n = 1,427) % (n) |
p |
|---|---|---|---|
| Work-related challenges | |||
| Lack of PPE | 19 (49) | 17 (238) | .34 |
| Lack of guidance/protocols to care for residents | 8 (21) | 9 (121) | .88 |
| Increased workload demands | 21 (53) | 24 (337) | .31 |
| Increased risk of COVID-19 transmission | 31 (79) | 28 (395) | .30 |
| Understaffing | 32 (82) | 30 (422) | .43 |
| Non-work-specific challenges | |||
| Lack of childcare | 6 (16) | 10 (153) | .03* |
| Lack of transportation | 2 (6) | 3 (41) | .65 |
| Separation from family members | 32 (83) | 35 (499) | .48 |
| Managing personal needs and family demands | 23 (60) | 27 (394) | .19 |
| Experiencing financial hardship | 26 (67) | 22 (309) | .10 |
| Mean | Mean | p | |
| Number of work-related challenges | 1.10 | 1.10 | .57 |
| Number of non-work-specific challenges | .91 | .97 | .36 |
| Overall perceived stress level | 2.75 | 2.83 | .40 |
| Perceived quality of communication regarding how to care for residents | 4.26 | 4.43 | .02* |
| Perceived quality of communication regarding how to protect yourself and family | 4.25 | 4.42 | .02* |
| Perceived level of preparedness | 3.95 | 4.21 | .00* |
Note. PPE = personal protective equipment; COVID-19 = coronavirus disease 2019.
p < .05.
Path Analyses
Because results from path analyses for each of the three indicators of COVID-19-related stressors were almost identical, we are summarizing the results combined for the three models tested. Direct effects and fit indices derived from each of the path analytic models are presented in Table 2. Each of the three models tested demonstrated adequate fit as indicated by the assessed indices. Table 3 presents the indirect effects of COVID-19-related stressors on quality of communication, preparedness, and job resignation. Figure 2 provides a summary of findings of path analyses, including hypothesized direct and indirect effects. In each of the three path analytic models, we controlled for direct care worker status and length of employment. Only length of employment was significantly related to job resignation status in each model: longer time employed was associated with a decreased likelihood to resign.
Table 2.
Unstandardized and Standardized Path Coefficients and Model Fit.
| B | SE | β | p | χ2 | df | χ2/df | CFI | RMSEA | |
|---|---|---|---|---|---|---|---|---|---|
| Overall stress | 7.73 | 4 | 1.93 | .996 | .023 | ||||
| Stress → Communication | −.30 | .03 | −.21 | <.001** | |||||
| Stress → Preparedness (H1a) | −.07 | .02 | −.09 | <.001** | |||||
| Communication → Preparedness (H2a) | .35 | .01 | .61 | <.001** | |||||
| Communication → Resignation (H2a) | −.004 | .01 | −.02 | .490 | |||||
| Preparedness → Resignation | −.03 | .01 | −.09 | .006** | |||||
| Stress → Resignation (H3a) | −.01 | .01 | −.05 | .064 | |||||
| Covariate: Direct care worker → Resignation | .02 | .02 | .03 | .210 | |||||
| Covariate: Length of employment → Resignation | −.006 | .02 | −.07 | .002** | |||||
| Work challenges | 4.86 | 4 | 1.21 | .999 | .011 | ||||
| Work challenges → Communication | −.61 | .02 | −.42 | <.001** | |||||
| Work challenges → Preparedness (H1a) | −.08 | .02 | −.10 | <.001** | |||||
| Communication → Preparedness (H2a) | .33 | .01 | .59 | <.001** | |||||
| Communication → Resignation (H2a) | −.01 | .01 | −.03 | .368 | |||||
| Preparedness → Resignation | −.03 | .01 | −.08 | .013* | |||||
| Work challenges → Resignation (H3a) | −.01 | .03 | −.02 | .372 | |||||
| Covariate: Direct care worker → Resignation | .02 | .02 | .03 | .206 | |||||
| Covariate: Length of employment → Resignation | −.006 | .002 | −.08 | <.001** | |||||
| Non-work challenges | 10.02 | 4 | 2.51 | .994 | .030 | ||||
| Non-work challenges → Communication | −.23 | .04 | −.13 | <.001** | |||||
| Non-work challenges → Preparedness (H1a) | −.02 | .02 | −.02 | .21 | |||||
| Communication → Preparedness (H2a) | .36 | .01 | .63 | <.001** | |||||
| Communication → Resignation (H2a) | −.01 | .01 | −.03 | .413 | |||||
| Preparedness → Resignation | −.03 | .01 | −.08 | .014* | |||||
| Non-work challenges → Resignation (H3a) | −.01 | .01 | −.04 | .091 | |||||
| Covariate: Direct care worker → Resignation | .03 | .02 | .03 | .187 | |||||
| Covariate: Length of employment → Resignation | −.006 | .002 | −.08 | <.001** |
Note. CFI = comparative fit index; df = degrees of freedom; RMSEA = root mean square error of approximation; H = hypothesis.
p < .05,
p <.01.
Table 3.
Indirect Effects of Stress on Work Resignation Through Communication and Preparedness.
| 95% bootstrap bias-corrected CI | |||||
|---|---|---|---|---|---|
| Mediation Paths | Coefficient | SE | Lower limit | Upper limit | p |
| Overall stress | |||||
| Stress → Communication → Preparedness (H1b) | −.103 | .014 | −.126 | −.081 | <.001** |
| Communication → Preparedness → Resignation (H2b) | −.010 | .004 | −.017 | −.003 | .012* |
| Stress → Communication → Preparedness → Resignation (H3b) | .003 | .001 | .001 | .005 | .010* |
| Work challenges | |||||
| Work challenges → Communication → Preparedness (H1b) | −.202 | .015 | −.229 | −.177 | <.001** |
| Communication → Preparedness → Resignation (H2b) | −.010 | .001 | −.016 | −.002 | .017* |
| Work challenges communication → Preparedness → Resignation (H3b) | .006 | .002 | .002 | .010 | .016* |
| Non-work challenges | |||||
| Non-work challenges → Communication → Preparedness (H1b) | −.081 | .017 | −.109 | −.052 | <.001** |
| Communication → Preparedness → Resignation (H2b) | −.010 | .004 | −.016 | −.002 | .017* |
| Non-work challenges communication → Preparedness → Resignation (H3b) | .002 | .001 | .001 | .004 | .008** |
Note. CI = confidence interval; H = hypothesis.
p < .05,
p <.01.
Figure 2.
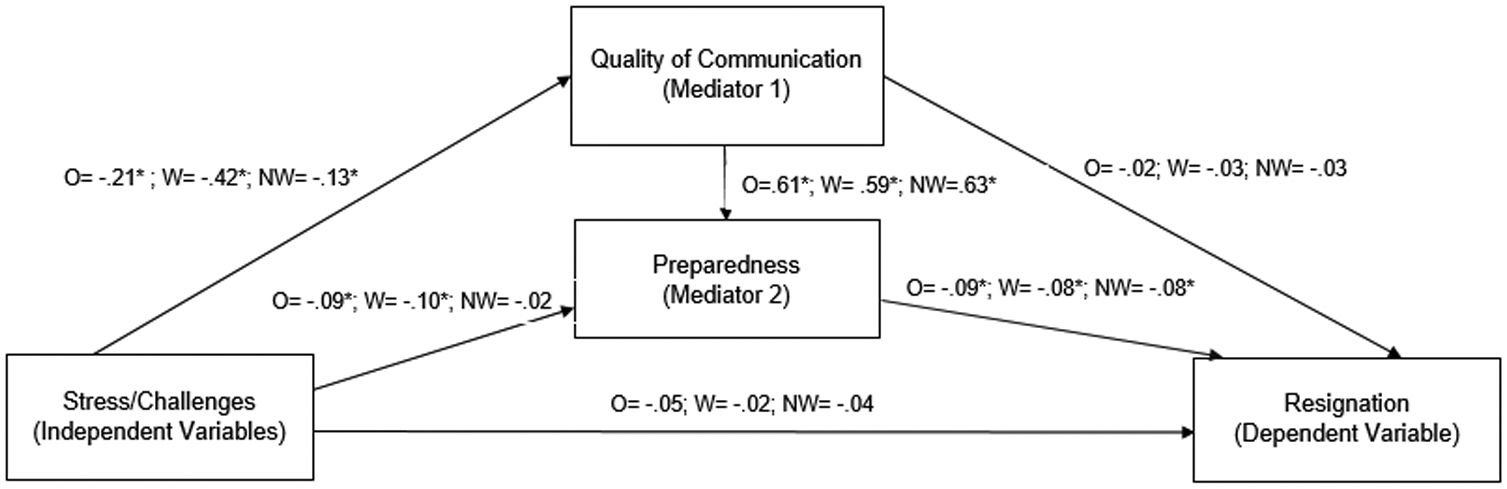
Serial mediation results.
Note. Standardized betas for direct effects: O = overall stress; W = work challenges; NW = non-work-related challenges. Significant indirect effects: (a) Stress/challenges → Communication preparedness (coefficients: O = −.103*, W = −.202*, NW = −.081*). (b) Communication → Preparedness → Resignation (coefficients: O = −.010*, W = −.010*, NW = −.010*). (c) Stress/challenges → Communication → Preparedness → Resignation (coefficients: O = .003*, W = .006*, NW = .002*).
Hypothesis 1a was partially confirmed. We found that higher overall COVID-19-related stress levels and number of stressful COVID-19-related work challenges were significantly directly associated with lower levels of preparedness. However, the number of stressful non-work-specific challenges experienced due to COVID-19 was not significantly directly associated with preparedness. Inspection of 95% bootstrap bias corrected confidence intervals revealed that the relationship between all three COVID-19-related stressors and job preparedness was significantly mediated by quality of organizational communication, indicating that higher quality of communication mediated the negative impact of COVID-19-related stressors on preparedness. Hypothesis 1b was thus confirmed.
Partially confirming Hypothesis 2a, we found a significant positive direct effect of quality of communication on preparedness, but no significant direct effect of quality of communication on resignation. Hypothesis 2b was confirmed as we found a significant negative indirect effect for quality of communication on job resignation, which was mediated by job preparedness Thus, higher quality of communication was associated with more optimal preparedness, which subsequently predicted a lower likelihood of job resignation.
Hypothesis 3a could not be confirmed as we did not find a significant direct association between COVID-19-related stressors and resignation. However, there was a significant positive indirect effect of COVID-19-related stressors on resignation. This indirect effect operated through the paths of communication quality and preparedness. Better quality communication was significantly associated with higher preparedness, and higher levels of preparedness were subsequently significantly associated with a reduced likelihood of resignation. Therefore Hypothesis 3b was confirmed.
Discussion
First, our study aimed to illustrate the types of COVID-19-related stressful work and non-work-specific challenges, along with overall work-related stress levels experienced by NH workers during the COVID-19 pandemic in early 2020. The stressful challenges endorsed by NH workers in our sample mirrored the findings of other recent studies where NH workers voiced infection concerns and increased work demands as major challenges (e.g., White et al., 2021). We also explored whether any stressful challenges experienced differed for currently employed when compared with resigned NH workers. We expected that workers who resigned over the 6 months following the data collection would have experienced more varied types of stressful challenges when compared with those who chose to stay on their job. However, with the exception of lack of childcare, we found no differences when comparing currently employed and resigned employees along challenges. Unexpectedly, resigned employees were less likely to report lack of childcare as a stressful challenge when compared with workers who had stayed employed 6 months after data collection.
Our other study aim was to determine whether quality of employer communication regarding COVID-19 could mediate the effects of COVID-19-related stressors on job resignation by optimizing workers’ preparedness to care for residents during COVID-19. Reviewing each of our specific hypotheses associated with our second study aim, we first found that overall COVID-19-related stress levels and number of stressful work challenges were associated with less optimal perceived preparedness to care for residents, but this did not hold true for the number of stressful non-work-specific challenges. Furthermore, as expected, better quality of communication mediated the negative effects of overall stress and amount of both types of stressful challenges on preparedness. This means that under highly stressful and challenging work conditions, workers felt more adequately prepared to care for residents during the pandemic when employer communication around COVID-19 was perceived as qualitatively better. As expected, better perceived preparedness was associated with remaining on the job, but, unexpectedly, worse quality of communication was not directly related to job resignation. However, the relationship between quality of communication and resignation was an indirect one operating through preparedness. This implies that while less optimal quality of communication by itself is not related to greater likelihood to resign one’s job, suboptimal communication leads to lower preparedness, which then is associated with greater likelihood of job resignation.
Our final set of predictions centered on testing our study conceptual model (Figure 1) in its entirety to learn how COVID-19-related work stressors were related to one’s decision to resign through the pathways of employer communication and employee perceived preparedness. We found that higher levels of COVID-19-related work stressors were indirectly associated with reduced likelihood of resigning through the paths of communication quality and preparedness: Higher quality of communication was associated with more optimal preparedness, which was subsequently associated with a reduced likelihood of leaving one’s job. In other words, when employer communication is inadequate, this will subsequently impact employees’ feelings of preparedness, which can increase the likelihood of job resignation during highly stressful times such as a pandemic. Hence, our study findings point to high-quality organizational communication and its associated enhanced preparedness of employees as key factors in preventing staff turnover during this pandemic. These findings add to recent research on organizational factors and work stressors conducted during the COVID-19 pandemic, which demonstrated that poor organizational communication made job performance more stressful (White et al., 2021) and that supportive supervisors could alleviate some of the workload-related stress (Blanco-Donoso et al., 2020). It is also likely that high quality of employer communication can have positive effects for worker well-being during a crisis like the COVID-19 pandemic as it has been suggested that frequent, unambiguous, and direct communication by leadership can support emotional well-being in health care workers (Scott-Cawiezell et al., 2004). Moreover, open communication—a type of communication that is characterized by all team members sharing their diverse perspectives—has been found to improve quality of performance in NHs (Vogelsmeier & Scott-Cawiezell, 2011). In terms of who can and should be responsible for enhancing quality of communication in the NH context, past research underscores the critical role of nurse leaders in facilitating communication (in addition to teamwork) among NH staff (Vogelsmeier & Scott-Cawiezell, 2011).
Limitations
A first study limitation that needs to be acknowledged is that facilities using an employee management system such as WCC are likely NHs committed to quality improvement and may therefore not be representative of all NHs across the country in regard to how they communicated with and prepared workers during the pandemic. It is also likely that employees at WCC participating organizations may have experienced less COVID-19-related work stressors because of the better preparation and communication provided by these organizations that invest in performance improvement efforts and already focus on implementing practical solutions that help reduce turnover and improve retention. Related to this, our sample was a convenience sample of workers at NHs using this employee management system and not a random sample of NH workers across the United States. Therefore, generalizability of study findings is limited to NHs who are WCC customers. Furthermore, the WCC interview battery does not assess sociodemographic characteristics of employees. These variables, however, could contribute to how NH workers experienced the COVID-19 pandemic and their decision to resign from their job. Plus, some of these variables could be important ones to account for in predicting the likelihood of job resignation. Our analyses also did not account for job satisfaction that is another factor associated with workers’ decision to resign. In addition, we had mostly one-item indicators available for our major study variables and a two-item scale measuring quality of communication. We are thus unable to isolate which specific aspects of employer communication contributed to better preparedness in our sample of NH workers.
Conclusions and Implications
Despite its limitations, our study has practical implications for NH leadership regarding how to support workers during this and possibly future pandemics. First, high-quality communication is not only key for workers to feel able to care for the residents during the stressful time of this pandemic, but also for workers’ decision to remain on the job. NH leadership should train staff on how to care for residents during the pandemic and be as transparent as possible about the state of the organization during a pandemic. Many frontline nurse managers, who have direct supervisory responsibility for CNAs, have not received adequate training on the communication and coaching skills that are necessary to support and empower direct care staff. Nursing schools and other educational venues need to build this type of training into their curricula. NH providers also need to develop in-service training that strengthens the nurse managers’ knowledge and competencies around clear and consistent communication. Second, based on NH workers’ reports of what specific challenges they faced during the pandemic, there is a need for NHs to find strategies to solve issues resulting from understaffing, such as increased workload demands. Strategies that NH employers could use are staggering shifts and allowing workers to work flexible shifts. NHs may also consider how to strengthen the pipeline of workers by training new cohorts of workers to fill vacant positions. There is also a need for supportive/wraparound services for managing family needs and to help with financial hardships. Taken together, these efforts could not only support the delivery of high quality of care for NH residents, but also help to strengthen the NH workforce to counteract the devaluation of this important segment of the long-term care workforce, which has been particularly prevalent during the COVID-19 pandemic (McGilton et al., 2020). Implementation of such efforts, in particular those comprehensive in nature, by addressing communication, staffing shortages, and worker support can also further aid and put “into action” the now emerging more holistic view that NH leaders have gained of their employees to better support them instrumentally, emotionally, and morally.
Acknowledgments
We would like to thank David Gehm, president and CEO of Wellspring Lutheran Services, and Jon Golm, president of WeCare Connect™ and his team, for their collaboration on this study.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Aging in America, Inc.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Institutional Review Board and Approval Number
UMass Boston; No. 2020174.
HIPPA Identifiers
Not applicable.
References
- Allen LD, & Ayalon L (2021). “It’s pure panic”: The portrayal of residential care in American newspapers during COVID-19. The Gerontologist, 61(1), 86–97. 10.1093/geront/gnaa162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida B, Cohen MA, Stone RI, & Weller CE (2020). The demographics and economics of direct care staff highlight their vulnerabilities amidst the COVID-19 pandemic. Journal of Aging & Social Policy, 32(4–5), 403–409. 10.1080/08959420.2020.1759757 [DOI] [PubMed] [Google Scholar]
- Bishop CE, Weinberg DB, Leutz W, Dossa A, Pfefferle SG, & Zincavage RM (2008). Nursing assistants’ job commitment: Effect of nursing home organizational factors and impact on resident well-being. The Gerontologist, 48(Suppl. 1), 36–45. 10.1093/geront/48.Supplement_1.36 [DOI] [PubMed] [Google Scholar]
- Blanco-Donoso LM, Moreno-Jiménez J, Amutio A, Gallego-Alberto L, Moreno-Jiménez B, & Garrosa E (2020). Stressors, job resources, fear of contagion, and secondary traumatic stress among nursing home workers in face of the COVID-19: The case of Spain. Journal of Applied Gerontology, 40(3), 244–256. 10.1177/0733464820964153 [DOI] [PubMed] [Google Scholar]
- Bollen KA, & Stine R (1990). Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology, 20, 115–140. 10.2307/271084 [DOI] [Google Scholar]
- Castle NG (2008). Nursing home caregiver staffing levels and quality of care: A literature review. Journal of Applied Gerontology, 27(4), 375–405. 10.1177/0733464808321596 [DOI] [Google Scholar]
- Castle NG, Engberg J, Anderson R, & Men A (2007). Job satisfaction of nurse aides in nursing homes: Intent to leave and turnover. The Gerontologist, 47(2), 193–204. 10.1093/geront/47.2.193 [DOI] [PubMed] [Google Scholar]
- The COVID Tracking Project. (2021). https://covidtracking.com/nursing-homes-long-term-care-facilities
- Figueroa JF, Wadhera RK, Papanicolas I, Riley K, Zheng J, Orav EJ, & Jha AK (2020). Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID-19 cases. The Journal of the American Medical Association, 324(11), 1103–1105. 10.1001/jama.2020.14709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorges RJ, & Konetzka RT (2020). Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. Journal of the American Geriatrics Society, 68(11), 2462–2466. 10.1111/jgs.16787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, & Gibson DM (2021). Workers at long-term care facilities and their risk for severe COVID-19 illness. Preventive Medicine, 143, Article 106328. 10.1016/j.ypmed.2020.106328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, & Nunez-Smith M (2020). Racial and ethnic disparities in population level COVID-19 mortality. Journal of General Internal Medicine, 35(10), 3097–3099. 10.1101/2020.05.07.20094250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press. [Google Scholar]
- Kirzinger A, Kearney A, Hamel L, & Brodie M (2020). KFF/The Washington post frontline health care workers survey. Kaiser Family Foundation. [Google Scholar]
- Koma W, Artiga S, Neuman T, Claxton G, Rae M, Kates J, & Michaud J (2020). Low-income and communities of color at higher risk of serious illness if infected with coronavirus. Kaiser Family Foundation. [Google Scholar]
- Laurencin CT, & McClinton A (2020). The COVID-19 pandemic: A call to action to identify and address racial and ethnic disparities. Journal of Racial and Ethnic Health Disparities, 7, 398–402. 10.1007/s40615-020-00756-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JK (2020). The effects of social comparison orientation on psychological well-being in social networking sites: Serial mediation of perceived social support and self-esteem. Current Psychology. 1–13. 10.1007/s12144-020-01114-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGilton KS, Escrig-Pinol A, Gordon A, Chu CH, Zúñiga F, Sanchez MG, Boscart V, Meyer J, Corazzini KN, Jacinto AF, Spilsbury K, Backman A, Scales K, Fagertun A, Wu B, Edvardsson D, Lepore MJ, Leun AYM, Siegel E, … Bowers B (2020). Uncovering the devaluation of nursing home staff during COVID-19: Are we fueling the next health care crisis?. Journal of the American Medical Directors Association, 21(7), 962–965. 10.1016/j.jamda.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Schenkman M, Moore L, Vojir C, Connolly RP, Pratt M, & Palmer L (2004). Exploring nursing home staff’s perceptions of communication and leadership to facilitate quality improvement. Journal of Nursing Care Quality, 19(3), 242–252. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H, Cen X, & Li Y (2020). Nursing home staff turnover and perceived patient safety culture: Results from a national survey. The Gerontologist, 60(7), 1303–1311. 10.1093/geront/gnaa015 [DOI] [PubMed] [Google Scholar]
- Tomlin J, Dalgleish-Warburton B, & Lamph G (2020). Psychosocial support for healthcare workers during the COVID-19 pandemic. Frontiers in Psychology, 11, Article 1960. 10.3389/fpsyg.2020.01960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkoff AM, Han K, Storr CL, Lerner N, Johantgen M, & Gartrell K (2013). Turnover, staffing, skill mix, and resident outcomes in a national sample of U.S. nursing homes. JONA: The Journal of Nursing Administration, 43(12), 630–636. 10.1097/NNA.0000000000000004 [DOI] [PubMed] [Google Scholar]
- U.S. Public Interest Research Group Education Fund. (2021). Nursing home safety during COVID: Staff shortages [Report]. https://uspirg.org/sites/pirg/files/reports/FINAL%201%3A28%20Nursing%20Home%20Report%20Staff%20Shortages.pdf
- Vogelsmeier A, & Scott-Cawiezell J (2011). Achieving quality improvement in the nursing home: Influence of nursing leadership on communication and teamwork. Journal of Nursing Care Quality, 26(3), 236–242. [DOI] [PubMed] [Google Scholar]
- White EM, Wetle TF, Reddy A, & Baier RR (2021). Front-line nursing home staff experiences during the COVID-19 pandemic. Journal of the American Medical Directors Association, 22(1), 199–203. 10.1016/j.jamda.2020.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu AW, Buckle P, Haut ER, Bellandi T, Koizumi S, Mair A, Øvretveit J, Power C, Sax H, Thomas EJ, Newman-Toker D, & Vincent C (2020). Supporting the emotional well-being of health care workers during the COVID-19 pandemic. Journal of Patient Safety and Risk Management, 25(3), 93–96. 10.1177/2516043520931971 [DOI] [Google Scholar]
- Yu Y, Yang X, Wang S, Wang H, Chang R, Tsamlag L, Zhang S, Xu C, Yu X, Cai Y, & Lau JT (2020). Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry, 20, Article 460. 10.1186/s12888-020-02870-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Lynch JG Jr., & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. 10.1086/651257 [DOI] [Google Scholar]


