Summary
Few peculiarities have been observed in the etiology of coronavirus disease 2019 (COVID-19), one such being its greater prevalence in men than women partly due to the higher expressions of angiotensin-converting enzyme-2 (ACE2) in the male reproductive tissues. Recent scientific reports are in line with some of the evidence-based hypotheses in the initial phase of the COVID-19 pandemic, regarding the involvement of oxidative stress (OS) and oxidant-sensitive pathways in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection-mediated male reproductive disruptions. The seminal dissemination of SARS-CoV-2 or its components, testicular disruptions due to viral infection and oxidative damage in the testis have all been evidenced recently. High-dose of antioxidants, such as vitamin C, have been shown to be a useful treatment for COVID-19 patients, to alleviate systemic inflammation and OS. In addition, vitamin C is a major testicular antioxidant that neutralizes excess reactive oxygen species (ROS), prevents sperm agglutination, prevents lipid peroxidation, recycles vitamin E, and protects against DNA damage. Thus, the present review aims to discuss the mechanism of COVID-19-mediated male reproductive dysfunctions, based on the evidence available so far, and explore the possibility of using vitamin C in alleviating testicular OS and associated damage caused by COVID-19.
Keywords: COVID-19, Inflammation, Male infertility, Oxidative stress, SARS-CoV-2
Introduction
Coronavirus disease 2019 (COVID-19) was first identified in the Wuhan City, China, in December 2019 as a result of a newly emerged coronavirus (CoV), severe acute respiratory syndrome coronavirus (SARS), named as SARS-CoV-2. This lethal virus has infected 210 countries and territories worldwide [1]. As a result, the World Health Organization (WHO) retorted on 30 January, 2020 by declaring the novel coronavirus (2019-nCoV) epidemic a public health emergency of international concern (PHEIC), the sixth time since 2005 [2]. SARS-CoV-2, like other CoVs, is an RNA virus that is a member of the subfamily Orthocoronavirinae, the order Nidovirales, and the genus coronavirus. Coronaviruses are enclosed and have positive sense single-stranded RNA genomes ranging in size from 26 to 32 kb [3]. The electron microscopic appearance of the SARS-CoV-2 particle resembled that of a solar corona, with a diameter of 60 to 140 nm and spikes measuring approximately 9 to 12 nm. It is the eighth coronavirus to be identified as the cause of COVID-19 [4]. Recent research indicates that SARS-CoV-2 shares 79 % nucleotide identity with SARS-CoV and 51.8 % with middle-east respiratory syndrome-related coronavirus (MERS-CoV) [5], demonstrating a significant degree of genetic similarity between SARS-CoV-2, MERS-CoV, and SARS-CoV. This infection has a direct effect on the respiratory, digestive, and central neurological systems [4]. Men have been discovered to be more susceptible to this condition than women [6,7], and the underlying causes of this phenomena remain unknown.
Pathogenesis of SARS-CoV-2: ACE2 in male reproductive tissues
The angiotensin-converting enzyme-2 (ACE2) receptor facilitates the entrance of SARS-CoV-2 into host cells and consequently plays an important role in the pathogenesis of COVID-19. ACE2 expression has been detected in a variety of organs, including the gonads [8]. Cells expressing higher levels of ACE2 are, however, more susceptible to COVID-19 infection because the viral attachment to the ACE2 receptors allows it to enter and replicate within the cell [9]. The transmembrane protease serine-2 (TMPRSS2) is a key protease involved in the priming of the viral spike proteins with the target host cell receptor, and it is responsible for cleaving the ACE2 receptor in particular [9]. Evidence suggests that androgen receptor activity is required for the transcription of the TMPRSS2 gene. Given that both the androgen receptor and the ACE2 gene loci are located on chromosome X, it is possible that enhanced X-linked inheritance of genetic polymorphisms, as well as an increase in androgen activities, may explain why males are more vulnerable to SARS-CoV-2 infection [9]. Furthermore, the startling fact that testicles are among the bodily tissues with the highest ACE2 expression suggests that SARS-CoV-2 infections are associated with male reproductive dysfunctions [9]. The expression of ACE2 mRNA and protein in the seminiferous duct cells, spermatogonia, Leydig cells, and Sertoli cells is extremely high [8].
SARS-CoV-2, inflammation, oxidative stress and male reproduction
Infection with SARS-CoV-2 in males results in acute stage hypogonadism, which can be deadly in certain circumstances [10,11]. Hypogonadism has been associated with elevated levels of pro-inflammatory cytokines, including interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), suggesting an exacerbated inflammatory response following SARS-CoV-2 infection [12]. Animal models infected with SARS-CoV and MERS-CoV have been shown to develop significant inflammatory and immunological responses as a result of the induction of a “cytokine storm”, which results in apoptosis, vascular leakage, and aberrant T cell and macrophage responses [13]. Patients with COVID-19 are likely to experience a cytokine storm as well, as previously stated in relation to genetic homology and clinical manifestations of the condition. When comparing the blood of COVID-19 patients to that of SARS patients, there was a significant increase in interleukin 1 (IL-1), interferon gamma (IFN-γ), interferon-inducible protein 10 (IP-10), monocyte chemoattractant protein 1 (MCP-1). According to this, there may be some differences between SARS and MERS in the pathophysiology of coronaviruses [4,14]. A putative repressed immune function has also been identified in COVID-19 patients who had hypoalbuminemia, lymphopenia, neutropenia, and decreased CD8+ T cell percentage [15,16], among other symptoms. According to recent findings, certain COVID-19 patients, despite testing negative for the viral nucleic acid, may nonetheless present with a high amount of inflammation in their bodies. Patients with COVID-19 may benefit from a clinical trial involving certolizumab pegol (a TNF blocker) in conjunction with other anti-viral medications, according to the findings of the study. Collectively, the findings suggest that inflammation is a significant characteristic of COVID-19 individuals' conditions. To this end, we postulate that COVID-19 pathophysiology is influenced by excessive inflammation, a suppressed immune system, and an activated cytokine storm, among other factors. In the early stages of coronavirus infection, dendritic cells and epithelial cells become activated and secrete a large number of pro-inflammatory cytokines and chemokines, including IL-1, IL-2, IFN-γ, TNF-α, CeC motif chemokine 3 (CCL3), CCL5, CCL2, and IP-10. The overproduction of these cytokines and anti-inflammatory chemokines contributes to the development of disease in this way [17,18]. It is believed that infection with coronaviruses causes a significant decrease in the production of IL-10, which is produced by T-helper-2 (Th2) cells [19]. Interestingly, people infected with COVID-19 occasionally have a considerably high level of IL-10 [4]. Whether this is a characteristic of the COVID-19 infection, or a side effect of medical treatment is still unclear. Inflammatory cells would die or be killed as a result of the increased apoptosis or necrosis of the affected cells, which would further fuel the inflammation. This would be followed by increased permeability of blood vessels and an abnormal accumulation of inflammatory monocytes, macrophages, and neutrophils in the affected organ [16,20]. As the immune system's ability to regulate itself is compromised, the “cytokine storm” is further exacerbated, resulting in potentially fatal implications for the patient. It is possible that coronaviruses are responsible for this pathology known as “cytokine storm”. Another study found that the deletion of the IFN-γ receptor or the depletion of inflammatory monocytes/macrophages resulted in a significant increase in the survival rate of coronaviruses in the host without a change in the viral load [21].
Increased OS is associated with cellular injury, organ failure, and mortality as a result of the fast release of free radicals and cytokines. Additionally, this virus has been found to produce orchitis, which can result in the production of OS, spermatogenic disturbances, and germ cell death, resulting in decreased sperm quality [22]. OS has been shown to impair testicular function at both the macro and micro levels, as seen by lipid peroxidation of sperm membranes and intracellular oxidative damage to spermatozoa, most notably sperm DNA fragmentation (SDF) [23–25]. Additionally, OS-induced SDF may be associated with miscarriage and infertility. Sperm chromatin is prone to OS-induced damage because of its indiscriminate protamination and poor compaction [26]. OS impairs spermiogenesis and results in spermatozoa with defective chromatin remodelling. Defective spermatozoa have a proclivity for initiating apoptotic pathways through caspase activation and mitochondrial free radical production. The radicals generated cause sperm lipid peroxidation and SDF [26]. Additionally, this may employ a major immunoinvasive technique similar to that described for SARS-CoV and influenza virus, namely inhibiting the host's cortisol stress response. In this regard, an intriguing observation is that SARS-CoV encodes specific amino acid sequences that can resemble host adrenocorticotropic hormone (ACTH), so triggering the formation of antibodies against the actual circulating ACTH. This ultimately results in the inhibition of the stress-induced cortisol increase [27]. This will disrupt the hypothalamo-pituitary adrenal (HPA) and hypothalamo-pituitary-gonadal (HPG) signaling pathway in stressful settings but will have no effect on testosterone or luteinizing hormone (LH) production [28]. As a result, it implies that SARS-CoV-2 infection also results in HPG-independent testosterone downregulation [29].
A recent report by Falahieh et al. [30] has demonstrated the SARS-CoV-2-caused OS-induced negative impacts on semen parameters (including SDF) and OS markers in COVID-19 patients 14 and 120 days after diagnosis [30]. Holtmann and colleagues found that sperm concentration and motility were considerably lower in patients who had recovered from a mild kind of COVID-19 infection as compared to control subjects. In that study, 18 semen samples were collected from recovered men between the ages of 8 and 54 days after their symptoms had subsided, depending on their age [31]. Moghimi et al. have reported that infection with COVID-19 can result in spermatogenesis being disrupted. This disturbance occurs through the OS route, which then results in the induction of apoptosis. As OS biomarkers, the study indicated an increase in the generation of ROS and a decrease in the activity of glutathione reductase. The findings of the immunohistochemical and TUNEL assays revealed that the expression of ACE2 as well as the quantity of apoptotic cells were considerably higher in the COVID-19 group than in the control group [32].
Vitamin C and COVID-19: Possible remedy for male reproductive disruptions
From the above evidence, it is apparent that OS caused by SARS-CoV-2 infection results in the disruption of male reproductive systems during infection. Early usage of high-dose antioxidants, such as vitamin C, may prove to be a useful treatment for these patients in order to offset their negative effects. Clinical investigations have also shown that high-dose oral vitamin C can provide some protection against viral infection in some circumstances [34–37]. This regimen should therefore be included in the treatment of COVID-19 and utilized as a preventive precaution for susceptible populations, such as healthcare professionals who are at higher risk of exposure. It has been reported that vitamin C is advantageous to critical care management since it is a vital component of the cellular antioxidant system [33,34]. Cytokine storm has been found in both viral and bacterial infections [35], and it is associated with enhanced overall survival through a non-specific and general route. Because high doses of antioxidants have been shown to be effective in the prevention and management of OS, the results of three previous clinical studies involving a total of 146 patients with sepsis suggest that this approach may be applicable to COVID-19 in combination with intravenous high-dose vitamin C may be promising [36]. It has been demonstrated that dietary antioxidants (vitamin C and sulforaphane) can reduce OS-induced acute inflammatory lung damage [37].
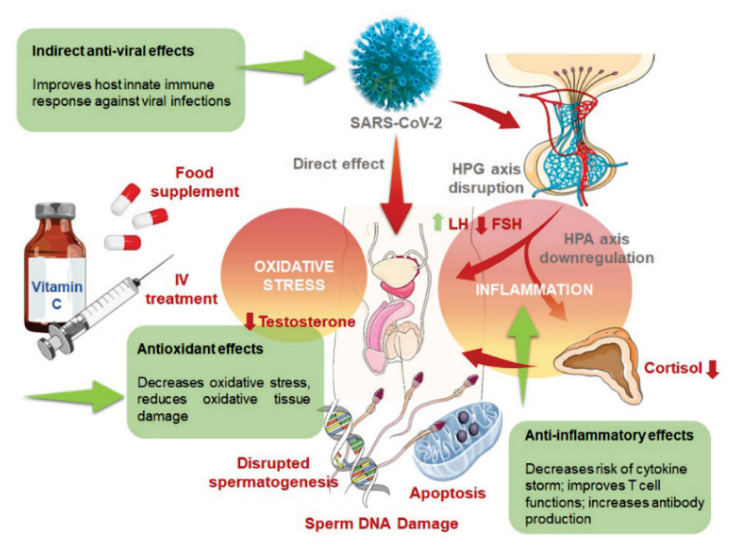
Considering the intricate role of OS in the COVID-19-mediated male infertility, therapeutic approaches targeting the mitigation of OS may possibly be effective [38]. Numerous antioxidants, essentially vitamin C, pentoxifylline, L-carnitine, arginine, zinc, and coenzyme Q10, are proven to be effective for ameliorating semen parameters in infertile men [39–43]. Vitamin C is highly effective in neutralizing ROS and preventing sperm agglutination, and it is considered to be a major antioxidant in the testis. It donates electrons to redox systems, prevents lipid peroxidation, recycles vitamin E, and protects against DNA damage caused by the hydrogen peroxide radical [44] all of which can contribute in protecting the testicular cells from oxidative damage and also in preventing SDF (Fig. 1). It has also been shown to enhance serum testosterone levels in mice after they have been exposed to OS [45]. Thus, including vitamin C in the treatment regime of COVID-19 patients may address the occurrence of primary hypogonadism in men. Additionally, oral vitamin C (e.g. 6 g daily) was found to be effective in reducing the likelihood of viral infection [46] or in alleviating symptoms [47]. Additionally, in China, high-dose intravenous vitamin C has been found to be effective in the treatment of 50 moderate to severe COVID-19 patients who were treated with success. Dietary dosages ranged from 10 g per day to 20 g per day and were administered over a period of 8–10 h. When patients are in critical condition, it is possible that an additional vitamin C bolus will be required. The oxygenation index was improving in real-time, and all of the patients were eventually treated and released from the hospital [48]. In fact, high-dose vitamin C has been clinically utilized for several decades, and a recent National Institutes of Health expert panel paper confirms unequivocally that this regimen (1.5 g/kg body weight) is safe and does not cause any significant side effects [49]. Vitamin C and other antioxidants are among the treatments now available to minimize COVID-19-associated acute respiratory distress syndrome (ARDS) [50,51]. This is due to the fact that developing effective vaccinations and antiviral medications takes time. Given the fact that high-dose vitamin C is considered to be safe, healthcare professionals should take note of this chance to expand their knowledge. It goes without saying that well-designed clinical investigations are required in order to explore the potential of vitamin C therapy in combination with standard treatment for COVID-19 male patients which will hold promise of addressing the viral infection as well as restoration of male reproductive functions.
Fig. 1.
Role of vitamin C in combating SARS-CoV-2 induced infection and projections of vitamin C mediated amelioration of male reproductive functions in COVID-19 patients. SARS-CoV-2 may adversely affect male reproductive functions either via direct viral infection of the testis and other male reproductive tissues, or via the systemic inflammation and OS-mediated disruptions of hormonal axes and damage to the male reproductive tissues. These ultimately impair spermatogenesis, steroidogenesis, induce germ cell apoptosis, SDF and overall reduction in semen quality. Vitamin C administration (either as food supplement or IV treatment) is effective in controlling the inflammatory and OS progression as well as improving the host immune response to COVID-19. Vitamin C, being a potent antioxidant and anti-inflammatory agent, is beneficial to male reproductive health. It prevents OS-induced testicular damage, SDF and also improves testosterone level, which project towards its possible therapeutic efficacy in ameliorating male reproduction in COVID-19 patients.
Conclusions
Vitamin C (ascorbic acid) is a water-soluble non-enzymatic highly potent antioxidant, which has been found effective against sepsis and elevated OS in COVID-19 patients. In severely ill COVID-19 patients, intravenous vitamin C administration in gram amounts have been shown to decrease mortality. COVID-19 has adverse impact upon male reproductive functions as well, mediated either by direct viral infestation in the reproductive tissues, via the chain of inflammatory reactions following systemic inflammation. Vitamin C, by the virtue of its pleiotropic physiological functions, mainly anti-inflammatory, antioxidant, and immuno-modulatory, may be a potent candidate to be included in the treatment regime for men with COVID-19. In physiological state, the seminal plasma vitamin C concentration is 10-fold higher as compared to serum, which is required to safeguard spermatozoa against endogenous oxidative damage by neutralizing the free radicals and preventing sperm agglutination. Vitamin C concentration in the seminal plasma has also been found to positively correlate with the percentage of morphologically normal spermatozoa and improved testosterone levels. It is also effective towards preventing DNA damage and thus may protect against the OS-mediated SDF in COVID-19 patients, too. Future research and clinical investigations should be undertaken to find the effectiveness of vitamin C in preventing or treating male reproductive disruptions induced by COVID-19.
Abbreviations
- ACE2
angiotensin-converting enzyme-2
- ARDS
acute respiratory distress syndrome
- ACTH
adrenocorticotropic hormone
- CCL
CeC motif chemokine
- CeC
chromo domain-containing protein
- CoQ10
coenzyme Q10
- COVID-19
coronavirus disease-19
- HPA
hypothalamo-pituitary adrenal
- HPG
hypothalamo-pituitary gonadal
- IFN
interferon
- IL
interleukin
- IP
interferon-inducible protein
- LH
luteinizing hormone
- MCP
monocyte chemoattractant protein
- MERS-CoV
Middle-East respiratory syndrome-related coronavirus
- nCoV
novel coronavirus
- ROS
reactive oxygen species
- SARS-CoV
severe acute respiratory syndrome coronavirus
- SDF
sperm DNA fragmentation
- TMPRSS2
transmembrane protease serine-2
- TNF
tumor necrosis factor
Footnotes
Conflict of Interest
There is no conflict of interest.
References
- 1.Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, Meng J, Zhu Z, Zhang Z, Wang J, Sheng J, Quan L, Xia Z, Tan W, Cheng G, Jiang T. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microb. 2020;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. 2019-nCoV outbreak is an emergency of international concern. 2020.
- 3.Banerjee A, Kulcsar K, Misra V, Frieman M, Mossman K. Bats and coronaviruses. Viruses. 2019;11:41. doi: 10.3390/v11010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94:e00127. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanley KE, Thomas E, Leaver M, Wells D. Coronavirus disease (COVID-19) and fertility: viral host entry protein expression in male and female reproductive tissues. Fertil Steril. 2020;1:33–43. doi: 10.1016/j.fertnstert.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roychoudhury S, Das A, Jha NK, Kesari KK, Roychoudhury S, Jha SK, Kosgi R, Choudhury AP, Lukac N, Madhu NR, Kumar D, Slama P. Viral pathogenesis of SARS-CoV-2 infection and male reproductive health. Open Biol. 2021;11:200347. doi: 10.1098/rsob.200347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, Leydig and Sertoli cells. Cells. 2020;9:920. doi: 10.3390/cells9040920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wambier CG, Goren A. SARS-COV-2 infection is likely to be androgen mediated. J Am Acad Dermatol. 2020;83:308–309. doi: 10.1016/j.jaad.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sengupta P, Dutta S. COVID-19 and hypogonadism: Secondary immune responses rule-over endocrine mechanisms. Hum Fertil (Camb) 2021:1–6. doi: 10.1080/14647273.2020.1867902. [DOI] [PubMed] [Google Scholar]
- 11.Giagulli VA, Guastamacchia E, Magrone T, Jirillo E, Lisco G, De Pergola G, Triggiani V. Worse progression of COVID-19 in men: Is testosterone a key factor? Andrology. 2021;9:53–64. doi: 10.1111/andr.12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maggio M, Basaria S, Ceda G, Ble A, Ling S, Bandinelli S, Valenti G, Ferrucci L. The relationship between testosterone and molecular markers of inflammation in older men. J Endocrinol Invest. 2005;28(11 Suppl Proc):116–119. [PubMed] [Google Scholar]
- 13.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Sem Imunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roychoudhury S, Das A, Sengupta P, Dutta S, Roychoudhury S, Choudhury AP, Fuzayel Ahmed AB, Bhattacharjee S, Slama P. Viral pandemics of the last four decades: pathophysiology, health impacts and perspectives. Int J Env Res Pub Health. 2020;17:9411. doi: 10.3390/ijerph17249411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, Li Y. The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. 2020;92:2188–2192. doi: 10.1002/jmv.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Oliveira Toledo SL, Nogueira LS, das Graças Carvalho M, Rios DRA, de Barros Pinheiro M. COVID-19: Review and hematologic impact. Clin Chim Acta. 2020;510:170–76. doi: 10.1016/j.cca.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung CY, Poon LL, Ng IH, Luk W, Sia S-F, Wu MHS, Chan K-H, Yuen K-Y, Gordon S, Guan Y, Peiris JSM. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J Virol. 2005;79:7819–7826. doi: 10.1128/JVI.79.12.7819-7826.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu H, Zhou J, Wong BH-Y, Li C, Chan JF-W, Cheng Z-S, Yang D, Wang D, Lee AC-Y, Li C, Yeung M-L, Cai J-P, Chan IH-Y, Ho W-K, To KK-W, Zheng B-J, Yao Y, Qin C, Yuen K-Y. Middle East respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J Infect Dis. 2016;213:904–914. doi: 10.1093/infdis/jiv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fehr AR, Channappanavar R, Jankevicius G, Fett C, Zhao J, Athmer J, Meyerholz DK, Ahel I, Perlman S. The conserved coronavirus macrodomain promotes virulence and suppresses the innate immune response during severe acute respiratory syndrome coronavirus infection. mBio. 2016;7:e01721–16. doi: 10.1128/mBio.01721-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T, Gerotziafas G, Dimopoulos MA. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95:834–847. doi: 10.1002/ajh.25829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Channappanavar R, Fehr AR, Vijay R, Mack M, Zhao J, Meyerholz DK, Perlman S. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microb. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu J, Qi L, Chi X, Yang J, Wei X, Gong E, Peh S, Gu J. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol Reprod. 2006;74:410–16. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li R, Yin T, Fang F, Li Q, Chen J, Wang Y, Hao Y, Wu G, Duan P, Wang Y, Cheng D, Zhou Q, Zafar MI, Xiong C, Li H, Yang J, Qiao J. Potential risks of SARS-Cov-2 infection on reproductive health. Reprod Biomed Online. 2020;41:89–95. doi: 10.1016/j.rbmo.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dutta S, Sengupta P. SARS-CoV-2 and male infertility: possible multifaceted pathology. Reprod Sci. 2021;28:23–26. doi: 10.1007/s43032-020-00261-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sengupta P, Dutta S. Does SARS-CoV-2 infection cause sperm DNA fragmentation? Possible link with oxidative stress. Eur J Contracep Reprod Health Care. 2020;25:405–406. doi: 10.1080/13625187.2020.1787376. [DOI] [PubMed] [Google Scholar]
- 26.Selvam MKP, Sengupta P, Agarwal A. Genetics of Male Infertility. Springer; 2020. Sperm DNA fragmentation and male infertility; pp. 155–172. [DOI] [Google Scholar]
- 27.Wheatland R. Molecular mimicry of ACTH in SARS-implications for corticosteroid treatment and prophylaxis. Med Hypoth. 2004;63:855–862. doi: 10.1016/j.mehy.2004.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Viau V. Functional cross-talk between the hypothalamic-pituitary-gonadal and-adrenal axes. J Neuroendocrinol. 2002;14:506–513. doi: 10.1046/j.1365-2826.2002.00798.x. [DOI] [PubMed] [Google Scholar]
- 29.Dutta S, Sengupta P. SARS-CoV-2 infection, oxidative stress and male reproductive hormones: can testicular-adrenal crosstalk be ruled-out? J Basic Clin Physiol Pharmacol. 2020:31. doi: 10.1515/JBCPP-2020-0205. [DOI] [PubMed] [Google Scholar]
- 30.Falahieh FM, Zarabadipour M, Mirani M, Abdiyan M, Dinparvar M, Alizadeh H, Paktinat S, Hosseinirad H. Effects of moderate COVID-19 infection on semen oxidative status and parameters 14 and 120 days after diagnosis. Reprod Fertil Dev. 2021;33:683–690. doi: 10.1071/rd21153. [DOI] [PubMed] [Google Scholar]
- 31.Holtmann N, Edimiris P, Andree M, Doehmen C, Baston-Buest D, Adams O, Kruessel J-S, Bielfeld AP. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil Steril. 2020;114:233–238. doi: 10.1016/j.fertnstert.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moghimi N, Eslami Farsani B, Ghadipasha M, Mahmoudiasl GR, Piryaei A, Aliaghaei A, Abdi S, Abbaszadeh H-A, Abdollahifar M-A, Forozesh M. COVID-19 disrupts spermatogenesis through the oxidative stress pathway following induction of apoptosis. Apoptosis. 2021;26:415–430. doi: 10.1007/s10495-021-01680-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Q, Gao Y, Ci X. Role of Nrf2 and its activators in respiratory diseases. Oxidat Med Cell Long. 2019:2019. doi: 10.1155/2019/7090534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nabzdyk CS, Bittner EA. Vitamin C in the critically ill-indications and controversies. World J Crit Care Med. 2018;7:52. doi: 10.5492/wjccm.v7.i5.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fowler AA, III, Kim C, Lepler L, Malhotra R, Debesa O, Natarajan R, Fisher BJ, Syed A, DeWilde C, Priday A, Kasirajan V. Intravenous vitamin C as adjunctive therapy for enterovirus/rhinovirus induced acute respiratory distress syndrome. World J Crit Care Med. 2017;6:85–90. doi: 10.5492/wjccm.v6.i1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li J. Evidence is stronger than you think: A meta-analysis of vitamin C use in patients with sepsis. Crit Care. 2018;22:1–4. doi: 10.1186/s13054-018-2191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel V, Dial K, Wu J, Gauthier AG, Wu W, Lin M, Espey MG, Thomas DD, Ashby CR, Jr, Mantell LL. Dietary antioxidants significantly attenuate hyperoxia-induced acute inflammatory lung injury by enhancing macrophage function via reducing the accumulation of airway HMGB1. Int J Mol Sci. 2020;21:977. doi: 10.3390/ijms21030977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Izuka E, Menuba I, Sengupta P, Dutta S, Nwagha U. Antioxidants, anti-inflammatory drugs and antibiotics in the treatment of reproductive tract infections and their association with male infertility. Chem Biol Lett. 2020;7:156–165. [Google Scholar]
- 39.Imamovic Kumalic S, Pinter B. Review of clinical trials on effects of oral antioxidants on basic semen and other parameters in idiopathic oligoasthenoteratozoospermia. BioMed Res Int. 2014;2014:426951. doi: 10.1155/2014/426951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abad C, Amengual M, Gosálvez J, Coward K, Hannaoui N, Benet J, García-Peiró A, Prats J. Effects of oral antioxidant treatment upon the dynamics of human sperm DNA fragmentation and subpopulations of sperm with highly degraded DNA. Andrologia. 2013;45:211–216. doi: 10.1111/and.12003. [DOI] [PubMed] [Google Scholar]
- 41.Alahmar AT, Calogero AE, Sengupta P, Dutta S. Coenzyme Q10 improves sperm parameters, oxidative stress markers and sperm DNA fragmentation in infertile patients with idiopathic oligoasthenozoospermia. World J Men’s Health. 2021;39:346. doi: 10.5534/wjmh.190145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alahmar AT, Calogero AE, Singh R, Cannarella R, Sengupta P, Dutta S. Coenzyme Q10, oxidative stress, and male infertility: A review. Clin Exp Reprod Med. 2021;48:97. doi: 10.5653/cerm.2020.04175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alahmar AT, Sengupta P. Impact of coenzyme Q10 and selenium on seminal fluid parameters and antioxidant status in men with idiopathic infertility. Biol Trace Elem Res. 2021;199:1246–1252. doi: 10.1007/s12011-020-02251-3. [DOI] [PubMed] [Google Scholar]
- 44.Angulo C, Maldonado R, Pulgar E, Mancilla H, Córdova A, Villarroel F, Castro MA, Concha II. Vitamin C and oxidative stress in the seminiferous epithelium. Biol Res. 2011;44:169–180. [PubMed] [Google Scholar]
- 45.Sönmez M, Türk G, Yüce A. The effect of ascorbic acid supplementation on sperm quality, lipid peroxidation and testosterone levels of male Wistar rats. Theriogenology. 2005;63:2063–2072. doi: 10.1016/j.theriogenology.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 46.Kim TK, Lim H, Byun J. Vitamin C supplementation reduces the odds of developing a common cold in Republic of Korea Army recruits: randomised controlled trial. BMJ Mil Health. 2020 doi: 10.1136/bmjmilitary-2019-001384. [DOI] [PubMed] [Google Scholar]
- 47.Gorton HC, Jarvis K. The effectiveness of vitamin C in preventing and relieving the symptoms of virus-induced respiratory infections. J Manipul Physiol Ther. 1999;22:530–33. doi: 10.1016/s0161-4754(99)70005-9. [DOI] [PubMed] [Google Scholar]
- 48.Hoang BX, Shaw G, Fang W, Han B. Possible application of high-dose vitamin C in the prevention and therapy of coronavirus infection. J Glob Antimicrob Resist. 2020;23:256–262. doi: 10.1016/j.jgar.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Cancer Institute. High-dose vitamin C (PDQ®)–Health professional version. 2020. Available from: https://www.cancer.gov/about-cancer/treatment/cam/hp/vitamin-c-pdq.
- 50.Stárka L, Dušková M. Androgens in SARS-CoV-2 coronavirus infections. Physiol Res. 2021;70(Suppl 2):S145–S151. doi: 10.33549/physiolres.934724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knížatová N, Massanyi M, Roychoudhury S, Guha P, Greifova H, Tokarova K, Jambor T, Massanyi P, Lukáč N. Is there impact of the SARS-CoV-2 pandemic on steroidogenesis and fertility? Physiol Res. 2021;70(Suppl 2):S161–S175. doi: 10.33549/physiolres.934756. [DOI] [PMC free article] [PubMed] [Google Scholar]