Abstract
Background: Nursing homes were particularly affected by the COVID-19 pandemic. The purpose of this study was to evaluate qualitatively and quantitatively with the use of a self-reported questionnaire as a tool for screening for mental disorders in nursing home staff. Methods: A multicenter epidemiological study was conducted in 12 nursing homes in France with 1117 nursing home staff eligible. Socio-demographic, occupational, and medical data were collected by anonymous self-reported questionnaire using validated scales to assess anxiety/depressive symptoms (HAD scale) and post-traumatic stress disorder (PCL-5). A total of 12 semi-structured interviews were conducted to assess acceptance and expectations for the use of the questionnaire. Results: The participation rate was 34.5%. Data from 373 questionnaires were included in the analysis. The questionnaire was well accepted by the participants and met their wishes for prevention action. The sample was 82% female. More than half reported a feeling of powerlessness and lack of time or staffing. The prevalence of anxiety symptoms was 22%, depressive symptoms 10%, and post-traumatic stress 7%. Conclusions: This study underlines the interest in screening for mental disorders by self-reported questionnaire and deploying preventive actions in the workplace to reduce stress and facilitate the reconciliation of family and working life in this context of the pandemic.
Keywords: nursing home staff, COVID 19 health crisis, mental disorders, screening, prevention, quantitative and qualitative study
1. Introduction
The year 2020 was marked by the emergence of COVID-19, responsible for a global pandemic. Between 1 March and 29 December 2020, the French Public Health Agency counted 64,068 Covid-19-related deaths in hospitals and facilities for the elderly, compared with an excess of 62,800 deaths from all causes and all places of death over the same period in 2020 compared with 2019 [1]. A total of 10,301 elderly people died in nursing homes between 1 March and 8 June 2020 [2]. Caregivers involved in the care of patients infected with COVID-19 are exposed to stressful situations, intense emotional load linked to the new conditions and organization of work, distress and, sometimes, death of patients and the suffering of families, which can jeopardize their psychological health. Previous studies highlighted the intense psychosocial stress to which nursing home staff are exposed and their links with impaired physical and psychological health [3,4,5,6].
Nursing home staff had to react to the influx of patients infected by COVID-19, presenting severe forms, leading to a dramatic increase in mortality in healthcare services and requiring strong mobilization of caregivers. The emergence of this new virus created a climate of anxiety, concern and uncertainty for healthcare providers and also for the general public [7].
As understanding of viruses and mechanisms of dissemination was poor at the beginning of the pandemic in 2020, the very mention of COVID-19 generated great anxiety. On a global scale, the WHO estimates that 30% to 50% of populations affected by the disaster have suffered from some form of psychological distress [8].
Mental health providers define trauma as a stressful occurrence outside the range of usual human experience that would be markedly distressing to almost anyone [9]. Exposure to traumatic and stressful events can lead to acute stress disorder and finally to post-traumatic stress disorder (PTSD) if symptoms persist [10]. PTSD is a trauma-related disorder that is characterized by the presence of at least one of four symptoms (intrusion, avoidance, negative mood, and cognitive changes), plus arousal and reactivity, for at least 1 month [11].
Numerous studies have demonstrated the presence of stress, anxiety disorder, depression, and post-traumatic stress disorder in many caregivers [8,12,13,14,15].
The French High Authority of Health published recommendations, validated on 7 May 2020, aimed at preventing and identifying occupational suffering in the health sector, with guidance in the context of the COVID-19 crisis [16]. Health professionals are in the first line in the management of the epidemic in healthcare facilities. Considering that humanity is undergoing the most severe pandemic since the Spanish flu, the current COVID-19 pandemic is very likely to promote PTSD, which commonly occurs during major disasters [17,18]. The French National Academy of Medicine, on 8 June 2020, recommended that special long-term attention be paid to the mental health of caregivers involved in the management of COVID-19, who should have a systematic medical examination and 3 years’ follow-up by preventive medicine doctors to identify “possible psychological symptoms that appeared after the acute phase of the health crisis” [15].
Currently, the medical follow-up of caregivers by the occupational health service is based on medical consultations [19]. Due to a lack of occupational physicians in healthcare institutions, systematic consultation would be very difficult to implement in the short term [20]. In this context, it is necessary to facilitate the identification and adapted psychological management of anxiety, depressive, and post-traumatic stress disorder in all staff (nursing and non-nursing) exposed during this pandemic.
The purpose of this study was to evaluate qualitatively and quantitatively the use of a self-reported questionnaire as a tool for screening for mental disorders in nursing home staff.
Study objectives were:
to evaluate the acceptance and expectations regarding screening by self-reported questionnaire;
to determine the prevalence of anxiety, depressive, and post-traumatic stress disorder in nursing home staff involved in the COVID-19 health crisis;
to identify occupational and medical factors associated with anxiety, depression, and post-traumatic stress disorder symptoms in order to adapt prevention actions.
2. Methods
2.1. Target Population
The target population was nursing home staff involved in the health crisis in the Saint-Etienne area.
Saint-Etienne is a city of 173,089 inhabitants located in the Loire department in France. A total of 72% of the population has a level of education equivalent to or lower than the baccalaureate. In 2019, the median income was 18,410 euros [21].
The directors of 24 nursing homes for the elderly were asked to include their staff, 12 of whom agreed. The participants received clear and comprehensible information on study objectives and procedures and were free to decline participation. A declaration was made to the CNIL data protection commission before starting the study.
- Inclusion criteria:
-
–Member of staff having worked in nursing homes for the elderly involved in the health crisis for at least 12 months.
-
–
- Exclusion criteria:
-
–Age under 18 years.
-
–
2.2. Measurements
In a first step, 12 semi-structured interviews (4 managers, 4 healthcare staff, 3 non-healthcare staff, 1 occupational physician) were conducted. The sample size was determined according to the empirical saturation principle [22]. The interview grid included questions on the acceptability of the questionnaire (theme 1), the conditions under which it was administered (theme 2), and the participants’ expectations regarding psychological care and preventive actions (theme 3). Eligible patients were provided with clearly understandable information on the study protocol and objectives. The information document specified that individual interviews would be recorded to facilitate transcription and that data would be anonymized.
In a second step, an anonymous self-administered questionnaire was provided online via a specific URL and QR code link for each nursing home and in paper format from 26 March to 31 May 2021. Self-administration time was approximately 15 min.
The questionnaire was developed using scientifically validated evaluation scales for anxiety, depression, and PTSD.
HAD scale for assessing anxiety and depression
The Hospital Anxiety and Depression Scale (HADS) is a self-administered questionnaire developed by Snaith and Zigmond in 1983 to detect and classify the severity of anxiety and depression [23]. It comprises 2 parts, with 7 questions each, relating to anxiety and depressive symptoms, respectively. Each answer is rated from 0 to 3, for a total score out of 42 and anxiety and depression scores out of 21 each. The French version of HADS has good reliability and discriminant validity; the internal consistency of the two scales is good. For anxiety, Cronbach’s alpha is 0.81, and for depression, 0.78 [24]. A meta-analysis showed a sensitivity of 82% and specificity of 74% [25]. In addition, in 2002, Bjelland et al. reported good sensitivity and specificity in the detection of anxiety and depressive disorders, in particular outside psychiatric settings [26]. In the present study, the main endpoint was anxiety symptoms, assessed on the French HADS. The Anxiety dimensions were rated on 3 levels: no symptoms (score ≤ 7), doubtful (8–10), and certain (≥ 11). A cut-off at 8 points defined clinical signs suggestive of anxiety disorder. A score of 11 was considered a threshold for each subcategory and was previously reported to be valid for defining the presence or absence of anxiety or depressive symptomatology [25,26].
PCL-5 scale to assess post-traumatic stress disorder.
The PCL-5 scale (PTSD Checklist for DSM-5) was created by Weathers et al. in 2013 and translated into French by Desbiendras [27,28]. It is a 20-item self-report questionnaire that assesses PTSD symptoms according to DSM-5 criteria. It is used to screen for PTSD, establish a provisional diagnosis of PTSD, and assess changes in symptomatology. Items are scored from 0 (“not at all”) to 4 (“extremely”). A cut-off value of 38 suggests the presence of PTSD [27].
Calculation of scores for each validated scale identified proven signs of these pathologies when above the threshold. A message interpreting the score with advice for medical evaluation and management was included at the end of the questionnaire.
In the context of the COVID-19 health crisis, socio-occupational and medical factors associated with these mental pathologies were sought on the basis of questions included in the questionnaire:
Socio-occupational factors: age, gender, family situation, job, working hours, seniority.
- Experience of the COVID crisis:
-
○Difficulties in reconciling family and working life;
-
○Feelings of inadequate protection against COVID-19 infection risk;
-
○Feelings of concern about the risk of transmission of COVID-19 for residents, for relatives, for their own health, for colleagues and superiors;
-
○Feelings of difficulties in accompanying residents with COVID-19 or their families
-
–due to lack of equipment;
-
–due to lack of communication within the facility;
-
–due to a feeling of dehumanization of care
-
–due to lack of time;
-
–due to a feeling of powerlessness;
-
–
-
○Feelings of difficulties in accompanying residents with COVID-19 or their families;
-
○Confrontation with the deaths of COVID-19 residents and emotional effects;
-
○Feeling of a traumatic work-related event during the health crisis.
-
○
- Medical factors:
-
○History of anxiety disorder;
-
○History of depressive syndrome;
-
○Psychotropic treatment;
-
○Work stoppage in the last 12 months;
-
○Duration of the work stoppage;
-
○Feeling of a traumatic work-related event during the health crisis.
-
○
Perceived stress related to personal and educational life was assessed on a visual analog scale (VAS) [29], with a cut-off at 7 points defining clinical signs of stress.
The collection of information on vaccination in our study was not foreseen in the methodology developed in July 2020 due to a lack of information on the availability of a vaccine for staff in 2021.
2.3. Analysis
Qualitative evaluation comprised transverse and comparative analysis of thematic content. Quantitative evaluation included descriptive analysis of sociodemographic, occupational, and medical characteristics. Univariate analysis assessed the association between anxiety, depression, and PTSD symptoms and sociodemographic, occupational, and medical factors. Chi2 and Fisher tests were applied as appropriate. The significance threshold was set at 5%. As the prevalence of the events (anxiety, depression, or PTSD) were high, odds ratios would not provide a good estimate of relative risk, rather, the log-linked binomial model was applied, using the PROC GENMOD procedure in the SAS statistical package ((SAS Institute Inc., SAS Campus Drive, Cary, NC 27513, USA, version 9.4) with the DIST = BINOMIAL and LINK = LOG options. Multivariable analyses were performed for each outcome (anxiety, depression, PTSD), variables with a p-value ≤ 0.05 in the univariate step were included in a multivariate model by a descending procedure, and variables with p-values < 0.05 remained in the model.
3. Results
3.1. Pilot Work: Qualitative Assessment
3.1.1. Theme 1: Questionnaire Acceptability
Half of the respondents were positive about the acceptability of the questionnaire and underlined its interest.
“I found the questionnaire easy to fill out, and the questions were quite clear.”
“It was the first time that we were concerned about nursing home staff. I have never seen studies like this in social and medical establishments.”
“I think it can be a good way indeed to reach more people.”
3.1.2. Theme 2: Questionnaire Administration Conditions
The methods of distributing the questionnaire online via a poster with QR codes or in paper format varied according to the institution. Anonymous distribution and the setting up of collection boxes facilitated participation and thus adherence. However, placing the ballot box in the office of a member of the hierarchy can be a hindrance to participation.
“So there were two modes of distribution. Indeed, the questionnaires were made available as paper questionnaires at the entrance where all the professionals pass by, there was also a box where they could be left.” “There were a few stapled sheets of paper, placed on the supervisor’s desk, I believe, which were handed out during relief. (…) And it was to be filled out and put in a cardboard box.”
“Online it was proposed to people who have direct access to the Internet here.”
3.1.3. Theme 3: Expectations Regarding Psychological Care and Implementation of Preventive Actions
Some participants emphasized the individual usefulness of this questionnaire as a source of questioning and expression of the experience of working conditions and the state of psychological health, and the collective usefulness of this questionnaire for collecting collective data with a view to proposing preventive actions.
“We have difficulties in our job. It’s an overload of work… a lack of staffing…”
“In this moment of crisis, it was still nice to know that we were being listened to through a questionnaire. It was to be heard but it was also to write down our feelings on paper.”
“It’s like I said: the questionnaire is fine, but there must be things put in place behind it.”
“When you give meaning to an action, the result is different afterwards and that’s why we have to follow up this survey.”
According to this qualitative assessment, the questionnaire was well accepted by the participants and met their wishes for prevention action.
3.2. Quantitative Results
3.2.1. Sociodemographic, Occupational, and Medical Characteristics
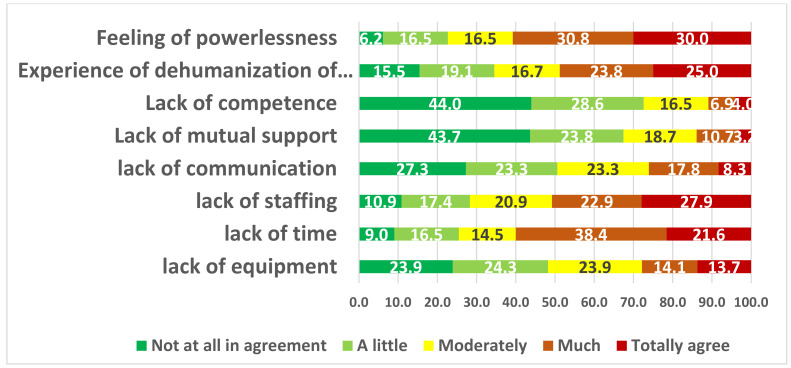
Out of 1117 eligible subjects, 386 working in 12 nursing homes participated in the study (participation rate: 34.5%). As shown in Table 1, 373 of the completed questionnaires could be included in the analysis. The sample size data was 373. The sample was 82% female (N = 306), and 70.7% of the participants (N = 263) lived in couples. More than two-thirds were caregivers. More than three-quarters worked 35 h per week or more. Mean age was 41.7 years [SD = 11.7]. Mean seniority was 11.9 years [SD = 9.3 years], and mean length of service in the present nursing home was 9.6 years [SD = 9]. As shown in Table 1, the prevalence was higher for anxiety symptoms (21%) than for depressive symptoms (10%) or PTSD (7%). A total of 8% of the subjects interviewed were taking a psychotropic treatment, two-thirds for less than a year. More than half of the respondents had taken time off work, half of whom for 2 weeks or more; 18% indicated a reason for being off work related to mental pathology. Nearly three-quarters of the employees interviewed expressed difficulties in caring for residents infected with COVID-19 and their families, related to a feeling of lack of time, powerlessness, lack of personnel, a perceived dehumanization of care, and, less frequently, perceived lack of equipment and communication within the facility (Figure 1).
Table 1.
Socio-occupational and medical characteristics.
| Medical Factors | n | % | Occupational Factors | n | % | ||
|---|---|---|---|---|---|---|---|
| History of anxiety disorder (n = 366) | No | 298 | 81.4 | Difficulties in reconciling family and working life (n = 367) | No | 169 | 46.1 |
| Yes | 68 | 18.6 | Yes | 198 | 53.9 | ||
| History of depressive syndrome (n = 367) | No | 325 | 88.6 | Feeling of inadequate protection against COVID-19 infectious risk (n = 366) | No | 219 | 59.8 |
| Yes | 42 | 11.4 | Yes | 147 | 40.2 | ||
| Proven symptoms of anxiety (n = 373) | No | 294 | 78.8 | Feeling of concern about the risk of transmission of COVID-19 (n = 365) | No | 23 | 6.3 |
| Yes | 79 | 21.2 | Yes | 342 | 93.7 | ||
| Proven symptoms of depression (n = 373) | No | 337 | 90.3 | For residents (n = 370) | No | 94 | 25.4 |
| Yes | 36 | 9.7 | Yes | 276 | 74.6 | ||
| Symptoms of post-traumatic stress disorder (n = 373) | No | 346 | 92.8 | For relatives (n = 370) | No | 54 | 14.6 |
| Yes | 27 | 7.2 | Yes | 316 | 85.4 | ||
| Taking a psychotropic treatment (n = 363) | No | 332 | 91.5 | For your own health (n = 370) | No | 186 | 50.3 |
| Yes | 31 | 8.5 | Yes | 184 | 49.7 | ||
| If taking a psychotropic treatment, since when? (n = 31) | Less than 3 months | 3 | 9.7 | For colleagues and superiors (n = 392) | No | 223 | 60.4 |
| Between 3 and 6 months | 5 | 16.1 | Yes | 146 | 39.6 | ||
| Between 6 months and 1 year | 13 | 41.9 |
Feeling of difficulties in accompanying residents with COVID-19 or their families
(n = 366) |
No | 103 | 28.1 | |
| More than 1 year | 10 | 32.3 | Yes | 263 | 71.9 | ||
| Work stoppage in the last 12 months (n = 365) | No | 177 | 48.5 | Have you been confronted with the deaths of COVID-19 residents? (n = 370) | No | 103 | 27.8 |
| Yes | 188 | 51.5 | Yes | 267 | 72.2 | ||
| If yes, what duration of work stoppage? (n = 183) | [1–7 days] | 51 | 27.9 | If Yes, were you emotionally affected? (n = 265) | No | 32 | 12.1 |
| [8–14 days] | 42 | 23.0 | |||||
| [15–29 days] | 55 | 30.0 | Yes | 233 | 87.9 | ||
| More than 30 days | 35 | 19.1 | |||||
Figure 1.
Causes of difficulties accompanying residents infected with COVID-19 and their families.
3.2.2. Factors Associated with Anxiety Symptoms
As shown in Table 2, on univariate analysis, anxiety symptoms were associated with:
Difficulties in balancing family and working life (PR = 2.7 [1.7–4.3]).
- Medical factors:
-
–History of anxiety disorder (PR = 3.1 [2.2–4.5]);
-
–History of depressive disorder (PR = 2.8 [1.9–4.1]);
-
–Psychological/psychiatric care (PR = 2.3 [1.5–3.6]);
-
–Work stoppage related to mental health condition (PR = 2.0 [1.1–3.6]).
-
–
- Occupational factors:
-
–Feeling of inadequate protection against COVID-19 infection (PR = 1.8 [1.2–2.6]);
-
–Concern about the risk of transmission of COVID-19 for one’s own health (PR = 1.6 [1.1–2.3]), or for one’s colleagues or superiors (PR = 1.6 [1.1–2.4]);
-
–Feeling of difficulty in accompanying residents infected with COVID-19 or their families due to lack of equipment (PR = 1.2 [0.5–2.6]), lack of time (PR = 6.7 [0.9–47.5]), or perceived powerlessness (PR = 2.8 [0.7–10.5]);
-
–High level of occupational stress (PR = 8.7 [3.6–20.9]) or personal stress (PR = 5 [3.1–8.0]);
-
–Perceived traumatic event at work during the health crisis (PR = 2.3 [1.5–3.6]) or at home during the health crisis (PR = 1.8 [1.2–2.7]).
-
–
Table 2.
Factors associated with anxiety symptoms, depressive symptoms, and Post-Traumatic Stress Disorder after univariate analysis.
| Proven Symptoms of Anxiety | Proven Symptoms of Depression | Signs of Post-Traumatic Stress Disorder | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | ||||||||||||||
| n | % | n | % | PR | CI | n | % | n | % | PR | CI | n | % | n | % | PR | CI | ||
| Difficulties in reconciling family and working life | No | 19 | 24.1 | 150 | 52.1 | 1 **** | - | 8 | 22.9 | 161 | 48.5 | 1 ** | - | 6 | 22.2 | 163 | 47.9 | 1 ** | - |
| Yes | 60 | 75.9 | 138 | 47.9 | 2.7 | 1.7–4.3 | 27 | 77.1 | 171 | 51.5 | 2.9 | 1.3–6.2 | 21 | 77.8 | 177 | 52.1 | 3.0 | 1.2–7.2 | |
| Feeling of inadequate protection against COVID 19 infectious risk in the workplace | No | 36 | 45.6 | 183 | 63.8 | 1 *** | - | 17 | 48.6 | 202 | 61.0 | 1 | - | 12 | 44.4 | 207 | 61.1 | 1 | - |
| Yes | 43 | 54.4 | 104 | 36.2 | 1.8 | 1.2–2.6 | 18 | 51.4 | 129 | 39.0 | 1.6 | 0.8–2.9 | 15 | 55.6 | 132 | 38.9 | 1.9 | 0.9–3.9 | |
| Feeling of concern about the risk of transmission of COVID-19 to residents | No | 14 | 17.7 | 80 | 27.5 | 1 | - | 4 | 11.1 | 90 | 27.0 | 1 * | - | 3 | 11.1 | 91 | 26.5 | 1 | - |
| Yes | 65 | 82.3 | 211 | 72.5 | 1.6 | 0.9–2.7 | 32 | 88.9 | 244 | 73.0 | 2.7 | 0.9–7.5 | 24 | 88.9 | 252 | 73.5 | 2.7 | 0.8–8.8 | |
| Feeling of concern about the risk of transmission of COVID-19 for your own health | No | 31 | 39.2 | 155 | 53.3 | 1 * | - | 16 | 44.4 | 170 | 50.9 | 1 | - | 11 | 40.7 | 175 | 51.0 | 1 | - |
| Yes | 48 | 60.8 | 136 | 46.7 | 1.6 | 1.1–2.3 | 20 | 55.6 | 164 | 49.1 | 1.3 | 0.7–2.4 | 16 | 59.3 | 168 | 49.0 | 1.5 | 0.7–3.1 | |
| Feeling of concern about the risk of transmission of COVID-19 for colleagues and superiors | No | 38 | 48.1 | 185 | 63.8 | 1 * | - | 15 | 42.9 | 208 | 62.3 | 1 * | - | 12 | 44.4 | 211 | 61.7 | 1 | - |
| Yes | 41 | 51.9 | 105 | 36.2 | 1.6 | 1.1–2.4 | 20 | 57.1 | 126 | 37.7 | 2.0 | 1.1–3.8 | 15 | 55.6 | 131 | 38.3 | 1.9 | 0.9–4.0 | |
| Feeling of difficulties in accompanying residents with COVID-19 or their families due to lack of equipment | Not at all in agreement | 12 | 20.7 | 49 | 24.9 | 1 * | - | 4 | 13.8 | 57 | 25.2 | 1 | - | 4 | 18.2 | 57 | 24.5 | 1 | - |
| A little | 10 | 17.2 | 52 | 26.4 | 0.8 | 0.4–1.8 | 7 | 24.1 | 55 | 24.3 | 1.7 | 0.5–5.6 | 6 | 27.3 | 56 | 24.0 | 1.5 | 0.4–5.0 | |
| Moderately | 12 | 20.7 | 49 | 24.9 | 1.0 | 0.5–2.0 | 6 | 20.7 | 55 | 24.3 | 1.5 | 0.4–5.1 | 3 | 13.6 | 58 | 24.9 | 0.8 | 0.2–3.2 | |
| Much | 16 | 27.6 | 20 | 10.1 | 2.2 | 1.2–4.2 | 7 | 24.1 | 29 | 12.8 | 3.0 | 0.9–9.4 | 7 | 31.8 | 29 | 12.4 | 3.0 | 0.9–9.4 | |
| Totally agree | 8 | 13.8 | 27 | 13.7 | 1.2 | 0.5–2.6 | 5 | 17.2 | 30 | 13.3 | 2.2 | 0.6–7.6 | 2 | 9.1 | 33 | 14.2 | 0.9 | 0.2–4.5 | |
| Feeling of difficulties in accompanying residents with COVID-19 or their families due to lack of communication within the facility | Not at all in agreement | 17 | 28.8 | 52 | 26.8 | 1 | - | 9 | 30.0 | 60 | 26.9 | 1 | - | 3 | 13.0 | 66 | 28.7 | 1 * | - |
| A little | 13 | 23.7 | 46 | 23.7 | 0.9 | 0.5–1.7 | 3 | 10.0 | 56 | 25.1 | 0.4 | 0.1–1.4 | 3 | 13.0 | 56 | 24.3 | 1.2 | 0.2–5.6 | |
| Moderately | 16 | 22.2 | 43 | 22.2 | 1.1 | 0.6–2.0 | 10 | 33.3 | 49 | 22.0 | 1.3 | 0.6–3.0 | 10 | 43.5 | 49 | 21.3 | 3.9 | 1.1–13.5 | |
| Much | 10 | 18.0 | 35 | 18.0 | 0.9 | 0.5–1.8 | 7 | 23.3 | 38 | 17.0 | 1.2 | 0.5–3.0 | 7 | 30.5 | 38 | 16.5 | 3.6 | 0.9–13.1 | |
| Totally agree | 3 | 5.1 | 18 | 9.3 | 0.6 | 0.2–1.8 | 1 | 3.3 | 20 | 9.0 | 0.4 | 0.1–2.7 | 0 | 0 | 21 | 9.1 | - | - | |
| Feeling of difficulties in accompanying residents with COVID-19 or their families due to a feeling of dehumanization of care | Not at all in agreement | 6 | 10.7 | 33 | 16.8 | 1 | - | 4 | 13.8 | 35 | 15.7 | 1 | - | 1 | 4.4 | 38 | 16.6 | 1 * | - |
| A little | 7 | 12.5 | 41 | 20.9 | 0.9 | 0.3–2.6 | 4 | 13.8 | 44 | 19.7 | 0.8 | 0.2–3.0 | 2 | 8.7 | 46 | 20.1 | 1.6 | 0.2–17.3 | |
| Moderately | 7 | 12.5 | 35 | 17.9 | 1.1 | 0.4–2.9 | 2 | 6.9 | 40 | 17.9 | 0.5 | 0.1–2.4 | 4 | 17.4 | 38 | 16.6 | 3.7 | 0.4–31.8 | |
| Much | 19 | 33.9 | 41 | 20.9 | 2.1 | 0.9–4.7 | 9 | 31.0 | 51 | 22.9 | 1.5 | 0.5–4.2 | 4 | 17.4 | 56 | 24.4 | 2.6 | 0.3–22.4 | |
| Totally agree | 17 | 30.4 | 46 | 23.5 | 1.8 | 0.8–4.1 | 10 | 34.5 | 53 | 23.8 | 1.5 | 0.5–4.6 | 12 | 52.2 | 51 | 22.3 | 7.4 | 1.1–54.9 | |
| Feeling of difficulties in accompanying residents with COVID-19 or their families due to lack of time | Not at all in agreement | 1 | 1.7 | 22 | 11.2 | 1 * | - | 1 | 3.3 | 22 | 9.8 | 1 | - | 2 | 8.7 | 21 | 9.1 | 1 | - |
| A little | 6 | 10.3 | 36 | 18.3 | 3.3 | 0.4–25.7 | 4 | 13.3 | 38 | 16.9 | 2.2 | 0.2–18.5 | 2 | 8.7 | 40 | 17.2 | 0.5 | 0.1–3.6 | |
| Moderately | 6 | 10.3 | 31 | 15.7 | 3.7 | 0.5–29.0 | 3 | 10.0 | 34 | 15.1 | 1.9 | 0.2–16.9 | 3 | 13.0 | 34 | 14.7 | 0.9 | 0.2–5.2 | |
| Much | 29 | 50.0 | 69 | 35.0 | 6.8 | 1.0–47.4 | 14 | 46.7 | 84 | 37.3 | 3.3 | 0.5–23.7 | 10 | 43.5 | 88 | 37.9 | 1.2 | 0.3–5.0 | |
| Totally agree | 16 | 19.8 | 39 | 19.8 | 6.7 | 0.9–47.5 | 8 | 26.7 | 47 | 20.9 | 3.3 | 0.4–25.2 | 6 | 26.1 | 49 | 21.1 | 1.2 | 0.3–5.8 | |
| Feeling of difficulties in accompanying residents with COVID-19 or their families due to a feeling of powerlessness | Not at all in agreement | 2 | 3.4 | 14 | 7.0 | 1 *** | - | 0 | 0 | 16 | 6.9 | - | - | 0 | 0 | 16 | 6.7 | - | |
| A little | 2 | 3.4 | 41 | 20.4 | 0.4 | 0.1–2.4 | 3 | 10.0 | 40 | 17.4 | 1 | - | 1 | 4.4 | 42 | 17.7 | |||
| Moderately | 6 | 10.2 | 37 | 18.4 | 1.1 | 0.3–5.0 | 3 | 10.0 | 40 | 17.4 | 1.0 | 0.2–4.7 | 2 | 8.7 | 41 | 17.3 | |||
| Much | 22 | 37.3 | 58 | 28.9 | 2.2 | 0.6–8.4 | 8 | 26.7 | 72 | 31.3 | 1.4 | 0.4–5.1 | 5 | 21.7 | 75 | 31.7 | |||
| Totally agree | 27 | 45.8 | 51 | 25.4 | 2.8 | 0.7–10.5 | 16 | 53.3 | 62 | 27.0 | 2.9 | 0.9–9.5 | 15 | 65.2 | 63 | 26.6 | |||
| History of anxiety disorder | No | 46 | 58.2 | 252 | 87.8 | 1 **** | - | 23 | 63.9 | 275 | 83.3 | 1 ** | - | 16 | 59.3 | 282 | 83.2 | 1 ** | - |
| Yes | 33 | 41.8 | 35 | 12.2 | 3.1 | 2.2–4.5 | 13 | 36.1 | 55 | 16.7 | 2.5 | 1.3–4.6 | 11 | 40.7 | 57 | 16.8 | 3.0 | 1.5–6.2 | |
| History of depressive disorder | No | 58 | 73.4 | 267 | 92.7 | 1 **** | - | 25 | 69.4 | 300 | 90.6 | 1 *** | - | 16 | 59.3 | 309 | 90.9 | 1 **** | - |
| Yes | 21 | 26.6 | 21 | 7.3 | 2.8 | 1.9–4.1 | 11 | 30.6 | 31 | 9.4 | 3.4 | 1.8–6.4 | 11 | 40.7 | 31 | 9.1 | 5.3 | 2.6–10.7 | |
| Psychotropic treatment | No | 58 | 73.4 | 269 | 93.4 | 1 **** | - | 25 | 69.4 | 302 | 91.2 | 1 *** | - | 18 | 66.7 | 309 | 90.9 | 1 *** | - |
| Yes | 21 | 26.6 | 19 | 6.6 | 3.0 | 2.0–4.3 | 11 | 30.6 | 29 | 8.8 | 3.6 | 1.9–6.7 | 9 | 33.3 | 31 | 9.1 | 4.1 | 2.0–8.5 | |
| Psychological/psychiatric care | No | 65 | 82.3 | 267 | 94.0 | 1 ** | - | 29 | 80.6 | 303 | 92.7 | 1 * | - | 19 | 70.4 | 313 | 93.1 | 1 **** | - |
| Yes | 14 | 17.7 | 17 | 6.0 | 2.3 | 1.5–3.6 | 7 | 19.4 | 24 | 7.3 | 2.6 | 1.2–5.4 | 8 | 29.6 | 23 | 6.9 | 4.5 | 2.2–9.4 | |
| Work stoppage related to mental health condition | No | 25 | 69.4 | 126 | 84.6 | 1 * | - | 9 | 50.0 | 142 | 85.0 | 1 *** | - | 11 | 73.3 | 140 | 82.3 | 1 | - |
| Yes | 11 | 30.6 | 23 | 15.4 | 2.0 | 1.1–3.6 | 9 | 50.0 | 25 | 15.0 | 4.4 | 1.9–10.3 | 4 | 26.7 | 30 | 17.7 | 1.6 | 0.5–4.8 | |
| Level of occupational stress in the last 3 months | light | 5 | 6.5 | 97 | 34.6 | 1 **** | - | 4 | 11.4 | 98 | 30.4 | 1 **** | - | 6 | 23.1 | 96 | 29.0 | 1 * | - |
| moderate | 20 | 26.0 | 113 | 40.4 | 3.1 | 1.2–7.9 | 5 | 14.3 | 128 | 39.8 | 0.9 | 0.3–3.5 | 5 | 19.2 | 128 | 38.7 | 0.6 | 0.2–2.0 | |
| high | 52 | 67.5 | 70 | 25.0 | 8.7 | 3.6–20.9 | 26 | 74.3 | 96 | 29.8 | 5.4 | 2.0–15.1 | 15 | 57.7 | 107 | 32.3 | 2.1 | 0.8–5.2 | |
| Level of personal stress in the last 3 months | light | 19 | 24.4 | 159 | 56.0 | 1 **** | - | 8 | 22.8 | 170 | 52.0 | 1 *** | - | 8 | 29.6 | 170 | 50.8 | 1 *** | - |
| moderate | 22 | 28.2 | 92 | 32.4 | 1.8 | 1.0–3.2 | 12 | 34.3 | 102 | 31.2 | 2.3 | 0.9–5.5 | 7 | 25.9 | 107 | 31.9 | 1.4 | 0.5–3.7 | |
| high | 37 | 47.4 | 33 | 11.6 | 5.0 | 3.1–8.0 | 15 | 42.9 | 55 | 16.8 | 4.8 | 2.1–10.7 | 12 | 44.4 | 58 | 17.3 | 3.8 | 1.6–8.9 | |
| Feeling of a traumatic work-related event during the health crisis | No | 27 | 34.2 | 174 | 60.6 | 1 **** | - | 18 | 50.0 | 183 | 55.4 | 1 | - | 11 | 40.7 | 190 | 56.0 | 1 | - |
| Yes | 52 | 65.8 | 113 | 39.4 | 2.3 | 1.5–3.6 | 18 | 50.0 | 147 | 44.6 | 1.2 | 0.7–2.3 | 16 | 59.3 | 149 | 44.0 | 1.8 | 0.8–3.7 | |
| Feeling of a traumatic event in personal life during the health crisis | No | 50 | 63.3 | 227 | 79.1 | 1 *** | - | 27 | 75.0 | 250 | 75.8 | 1 | - | 15 | 55.6 | 262 | 77.3 | 1 * | - |
| Yes | 29 | 36.7 | 60 | 20.9 | 1.8 | 1.2–2.7 | 9 | 25.0 | 80 | 24.2 | 1.1 | 0.5–2.1 | 12 | 44.4 | 77 | 22.7 | 2.5 | 1.2–5.1 | |
PR: Prevalence Ratio; CI: Confidence Interval; p-value: *: p < 0.05 **: 0.01 < p ≤ 0.05; ***: 0.001 < p ≤ 0.01; **** p ≤ 0.0001.
In contrast, anxiety symptoms were not significantly associated with gender (p = 0.8) and age (p = 0.4) and family situation (p = 0.3).
As shown in Table 3, on multivariate analysis, anxiety symptoms remained associated with
-
–
Feeling of inadequate protection against COVID-19 infection (PR = 1.4 [1.2–2.6]);
-
–
History of anxiety disorder (PR = 1.4 [1.2–1.6]);
-
–
Psychological/psychiatric care (PR = 1.4 [1.2–1.6]);
-
–
Level of high occupational stress in the last 3 months (PR = 5.0 [2.0–12.5]).
-
–
Level of high personal stress in the last 3 months (PR = 2.0 [1.2–3.4])
Table 3.
Factors associated with anxiety symptoms, depressive symptoms, and Post-Traumatic Stress Disorder after multivariate analysis.
| Experiencing a Traumatic Event in Personal Life (PR = 1.4 [1.2–1.6]) | Proven Symptoms of Anxiety | Proven Symptoms of Depression | Signs of Post-Traumatic Stress Disorder | ||||
|---|---|---|---|---|---|---|---|
| PR adj | 95% CI | PR adj | 95% CI | PR adj | 95% CI | ||
| Feeling of inadequate protection against COVID 19 infectious risk in the workplace | No | 1 **** | - | / | / | / | / |
| Yes | 1.4 | 1.2–1.6 | / | / | / | / | |
| History of anxiety disorder | No | 1 **** | - | / | / | / | / |
| Yes | 1.4 | 1.2–1.6 | / | / | / | / | |
| History of depressive disorder | No | / | / | 1 **** | - | 1 **** | - |
| Yes | / | / | 2.5 | 1.3–4.6 | 4.9 | 2.4–9.8 | |
| Psychological/psychiatric care | No | 1 **** | - | / | / | / | / |
| Yes | 1.4 | 1.2–1.6 | / | / | / | / | |
| Level of occupational stress in the last 3 months | light | 1 **** | - | 1 **** | - | / | / |
| moderate | 2.6 | 1.1–6.8 | 0.9 | 0.3–3.4 | |||
| high | 5.0 | 2.0–12.5 | 4.9 | 1.8–13.6 | / | / | |
| Level of personal stress in the last 3 months | light | 1 **** | - | / | / | / | / |
| moderate | 1.1 | 0.6–1.9 | / | / | / | / | |
| high | 2.0 | 1.2–3.4 | / | / | / | / | |
| Experiencing a traumatic event in personal life during the health crisis | No | 1 **** | - | / | / | 1 * | - |
| Yes | 1.4 | 1.2–1.6 | / | / | 2.2 | 1.1–4.4 | |
PR adj: adjusted Prevalence Ratio CI: Confidence Interval; *: p < 0.05; p-value: **** p ≤ 0.0001; variables with a p-value ≤ 0.05 in the univariate step were included in a multivariate model by a descending procedure and variables with p-values < 0.05 remained in the model.
3.2.3. Factors Associated with Depressive Symptoms
As shown in Table 2, on univariate analysis, depressive symptoms were associated with:
Difficulties in reconciling family and working life (PR = 2.9 [1.3–6.2]).
- medical factors:
-
–History of anxiety disorder (PR = 2.5 [1.3–4.6]);
-
–History of depressive disorder (PR = 3.4 [1.8–6.4]).
-
–
- Occupational factors:
-
–Concern about the risk of transmission of COVID-19 to residents (PR = 2.7 [0.9–7.5]), or to colleagues or superiors (PR = 2.0 [1.1–3.8]);
-
–High level of occupational stress (PR = 5.4 [2.0–15.1]) or personal stress (PR = 4.8 [2.1–10.7]).
-
–
In contrast, depressive symptoms were not significantly associated with gender (p = 0.8) and age (p = 0.8) and family situation (p = 0.9).
As shown in Table 3, on multivariate analysis, depressive symptoms remained associated with:
-
–
History of depressive disorder (PR = 2.5 [1.3–4.6]);
-
–
Level of high occupational stress in the last 3 months (PR = 4.9 [1.8–13.6]).
3.2.4. Factors Associated with Signs of PTSD
As shown in Table 2, on univariate analysis, signs of PTSD were associated with:
Difficulties in reconciling family and working life (PR = 3.0 [1.2–7.2]).
- Medical factors:
-
–History of anxiety disorders (PR = 3 [1.5–6.2]);
-
–History of depressive disorders (PR = 5.3 [2.6–10.7]).
-
–
- occupational factors:
-
–Perceived difficulty in accompanying residents infected with COVID-19 or their families, linked to lack of communication within the structure (PR = 3.6 [0.9–13.1]), or to perceived dehumanization of care (PR = 7.4 [1.1–54.9]);
-
–High level of occupational stress (PR = 2.1 [0.8–5.2]) or personal stress (PR = 3.8 [1.6–8.9]);
-
–Perceived traumatic event in the personal environment during the health crisis (PR = 2.5 [1.2–5.1]).
-
–
In contrast, depressive signs of PTSD were not significantly associated with gender (p = 0.7) and age (p = 0.8) and family situation (p = 0.7).
As shown in Table 3, on multivariate analysis, signs of PTSD remained associated with:
-
–
History of depressive disorder (PR = 4.9 [2.4–9.8]);
-
–
Experiencing a traumatic event in personal life (PR = 2.2 [1.1–4.4]).
Although the results of the univariate analysis show an association between difficulties in reconciling family/working life imbalance and anxiety symptoms, depressive symptoms, or PTSD, the association is not maintained after multivariate analysis. On the other hand, medical factors (such as a history of anxiety or depressive symptoms) and occupational factors (such as high occupational stress) remained associated with these pathologies after multivariate analysis in nursing home staff involved in the COVID-19 health crisis.
4. Discussion
During the pandemic, changes in working conditions in nursing homes and long-term care facilities have affected residents, their families, and health and social workers [30].
The use of a self-administered questionnaire to identify workers with impaired mental health is not a standard medical practice in occupational medicine. In a context of increasing workload for nursing home staff and a shortage of occupational physicians, this study provides a qualitative and quantitative assessment of a tool to detect mental health issues using a self-report questionnaire.
These screening methods could make it possible to identify mental disorders at an early stage with the potential effect of improving mental health and reducing the number of work stoppages.
Previous studies have shown the value of early detection of mental illness in medical management and have shown that early identification of mental illness without appropriate medical management can be associated with increased injury [31,32]. The qualitative evaluation of this tool for screening for mental disorders underlines the interest, the acceptability of the modalities of taking the self-administered questionnaire, and the need to associate psychological support for the nursing home staff. The implementation literature emphasizes that it is important to create a positive climate for implementation [33]. Interest and acceptability are favorable criteria for the implementation of this tool for the identification of mental disorders.
The study showed the individual and collective interest in identifying employees with signs suggestive of anxiety, depression, and PTSD. It also underlined the personal and occupational factors associated with these pathologies in order to identify possible areas for prevention. According to the qualitative assessment, more than half of the participants accepted the questionnaire and found it interesting to complete.
Studies that examined mental health outcomes in healthcare workers before and during the COVID-19 outbreak found a significant increase in reported anxiety symptoms in the outbreak period compared to the non-outbreak period [34,35]. In the present study, the prevalence of anxiety disorder in nursing home staff was 21%, similar to previous reports. According to data from the French Public Health Agency, the prevalence of anxiety in the general French adult population was 23% in the first COVID wave, compared to 13.5% in 2017 [36]. A cross-sectional survey of 1422 Spanish health workers evaluated the prevalence of anxiety at 20.7% [37]. A systematic review of the literature with meta-analysis estimated the prevalence of anxiety in caregivers during COVID-19 as 25% [38]. A systematic review with meta-regression found a prevalence of anxiety of 25.8% in hospital caregivers managing patients affected by COVID-19 [39]. Another systematic review, including 12 studies, found a pooled anxiety prevalence of 23.2% in healthcare workers [40].
The prevalence of depressive disorder in the present study was consistent with data from the French Public Health Agency in 2011 in a sample of employees (7.11%) before the COVID-19 health crisis [41]. However, these findings were lower than those of studies focusing exclusively on healthcare workers. The systematic review of the literature with meta-analysis found a prevalence of depression of 22.8% in healthcare workers during the COVID-19 pandemic, however, the studies used a variety of self-report anxiety scales, and the use of some tests was associated with a significantly higher prevalence of anxiety than others [38]. A systematic review with meta-regression found a prevalence of 24.3% for depression in hospital healthcare workers caring for patients affected by COVID-19 [39]. A systematic review including 10 studies found a pooled depression prevalence of 22.8% [40]. A cross-sectional survey on 1422 Spanish healthcare workers evaluated the prevalence of depression at 15.2% [37]. The difference in the assessment of the prevalence of depression in our study may be because our sample included healthcare workers and non-healthcare workers and because working conditions differ between nursing homes for the elderly and hospitals.
The data collected by the French Public Health Agency in French employees before the beginning of the health crisis showed a prevalence of 2.3% in 2011, compared to 5–12% in the general American population [41,42]. Previous studies highlighted an important impact of the COVID-19 pandemic on the mental health of healthcare workers [43]. The prevalence of clinically relevant trauma-related symptoms ranged from 7.4% to 35% [44,45]. Our study estimated the prevalence of PTSD at 7%, lower than in a previous report of 13.2% in Chinese healthcare workers [46]. A multicenter observational cohort study of 9138 healthcare workers, carried out in a convenience sample of 18 healthcare institutions from 6 Autonomous Communities in Spain, showed a 22% prevalence of PTSD [47]. The differences in these results could be explained by different contagion rates and pressure on healthcare systems, different incidences of risk factors, and differences in access to psychological support [48]. Not all nursing homes experienced the crisis in the same way; for example, some had many patients infected with COVID but very few deaths, which may limit the psychological impact on staff. Strong support and team cohesion in the nursing homes may have reduced the effect of the stress induced by the health crisis.
In our study, anxiety symptoms, depressive symptoms were not significantly associated with gender, which is inconsistent with the data in the literature [44,49,50]. Moreover, anxiety symptoms and depressive symptoms were not significantly associated with age, whereas differences by age were reported, with younger Health Care Workers experiencing higher levels of anxiety and depressive symptoms compared to older age groups in the literature [14,51,52].
This study revealed factors associated with anxiety, depression, and PTSD and identified potential areas for prevention.
According to our study, the medical factors associated with anxiety disorders, depressive disorders, and PTSD were history of anxiety disorder and depressive disorder. These results are similar to those of previous studies. A multicenter, observational cohort study of 9138 healthcare workers reported that the higher the number of prior lifetime mental disorders, the more likely the presence of any current disorder [47]. Şahin et al. conducted a cross-sectional study of 939 healthcare workers during the COVID-19 pandemic in Turkey between 23 April and 23 May 2020. They showed that depression and anxiety symptoms were significantly greater in individuals with a history of psychiatric illness [53].
Our study also highlighted an association between exposure to modifiable occupational factors and the presence of anxiety, depression, or PTSD. There was an association between anxiety symptomatology and feelings of lack of time and of helplessness in caring for residents infected with COVID-19 or their families in this health crisis. Previous studies reported that nursing homes had difficulty organizing and managing material and human resources to respond to the pandemic [54]. This reorganization required nursing homes to make decisions on the safety of residents and employees, including protocols for isolation and evacuation and for screening people with symptoms or positive COVID-19 diagnosis, which increased stress levels.
Our study also highlighted an association between staff’s concern about transmitting infection, difficulties in supporting residents and their families, and mental illness. These results corroborate those in the literature. Previous studies showed an association between mental disorders and the high mental burden to which workers are exposed, excessive working hours, fear of contagion for themselves and their loved ones, lack of job resources, and the high degree of suffering of patients and their families [17,55,56,57].
High levels of stress and difficulties in balancing family and working life are modifiable factors that could be used as a basis for prevention measures. These findings are consistent with the literature.
Previous studies described the high levels of stress and pressure affecting nursing home employees (uncertainty, hopelessness, excess workload, and role conflicts), with a significant impact on their mental health [58,59]. In a study of 152 front-line nursing home staff, White et al., underlined the emotional burden of caring for residents experiencing distress, illness, and death [58]. Some employees commented on the fear and stress associated with possibly being infected and infecting family members. Spoorthy et al., in a review of the literature, highlighted the increased stress of health care personnel confronted with a health crisis and its association with anxiety and depressive disorders [60]. The authors underlined the positive effects of social support and psychological accompaniment of personnel confronted with the health crisis. Training in better stress management and a participatory approach to improving personal/working life could be proposed to nursing home staff.
Moreover, in line with the literature, our qualitative findings strongly suggest establishing psychological support services for providing adequate professional care for nursing home staff [61,62].
The use of this tool for the longitudinal medical follow-up of employees would allow the early identification of personnel requiring psychological care. The data in the literature underline the importance of encouraging the implementation of psychological support for staff involved in the health crisis. Nursing home staff are eager to receive psychological care [17,63,64]. Nursing home managers could use these results to implement human resources to promote psychological support for staff.
Study Strengths and Weaknesses
In this cross-sectional study, the identified factors were regarded as associated factors, which could be either causes or results of anxiety, depression disorders, and PTSD. The results should be generalized with caution since they were drawn from a non-randomized sample and the sample size was small, and the response rate was 34.5%. Furthermore, anxiety, depressive symptoms, and PTSD were identified not on clinical examination but on a validated scale. The collection method based on a self-administered questionnaire makes it possible to collect medical information and information on the experience of working conditions during a health crisis. The declarative nature of the information constitutes a potential bias in data classification. The controlled length of the questionnaire, its content, and presentation contributed to its completion.
Vaccination against COVID-19 may have had an effect on the prevalence of anxiety, depression, and Post-Traumatic Stress disorder in nursing home staff involved in the COVID-19 health crisis. According to Haddaden et al., a COVID-19 vaccination improved healthcare workers’ comfort and anxiety in caring for patients with COVID-19 and other illnesses likely explained by the high efficacy of vaccination in preventing symptomatic infection and critical illness [63]. The COVID-19 vaccination coverage of the sample was not known. However, the data from Santé Publique France, on 16 March 2021, showed that 20.8% of professionals working in retirement homes in the Loire had received a first dose of vaccine. It is estimated that 74.6% of the residents of retirement homes located in the Loire have received a first dose of the COVID-19 vaccine [64].
5. Conclusions
The questionnaire was well accepted by the participants and met their wishes for prevention actions. The study showed the interest in early detection of mental disorders by a self-report questionnaire in nursing home staff involved in the health crisis to optimize medical care. The survey showed that it is possible to encourage regular medical monitoring of professionals by using this kind of questionnaire. Moreover, the study highlighted possible lines of prevention based on better stress management and better reconciliation of family and working life for personnel involved in the health crisis. Future studies should clarify the long-term effects of the COVID-19 pandemic on the mental health of healthcare workers in nursing homes for the elderly.
Author Contributions
Conceptualization, S.D., T.C., L.F., N.B. and C.P.; methodology, N.T., F.V., S.D., T.C., L.F., N.B. and C.P.; software, T.P., S.D., E.F. and C.P.; validation, N.T., F.V., T.P., S.D., E.F., T.C., L.F., N.B. and C.P.; format analysis, E.F.; investigation, N.T., F.V., T.P. and S.D.; resources, C.P.; data curation, N.T., F.V., T.P., S.D.; writing-review and editing, N.T., F.V., T.P., S.D., E.F., T.C., L.F., N.B. and C.P.; visualization, C.P.; supervision, N.B. and C.P.; project administration, T.C., L.F., N.B. and C.P.; funding acquisition, N.B. and C.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the CNSA (N° 0000 1260).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital Center of Saint-Etienne (IRBN1202020/CHUSTE, 22 October 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the confidentiality of participants.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.SPF COVID-19: Epidemiological Update of 31 December 2020. [(accessed on 9 March 2022)]. Available online: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-31-decembre-2020.
- 2.SPF COVID-19: Epidemiological update of 11 June 2020. [(accessed on 18 June 2020)]. Available online: https//maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-11-juin-2020.
- 3.Pélissier C., Fontana L., Fort E., Charbotel B. Subjective hardship and training by female staff working in direct contact with the elderly in nursing homes: A cross-sectional study. Psychol. Neuropsychiatr. Du Vieil. 2015;13:396–406. doi: 10.1684/pnv.2015.0572. [DOI] [PubMed] [Google Scholar]
- 4.Pelissier C., Fontana L., Fort E., Vohito M., Sellier B., Perrier C., Glerant V., Couprie F., Agard J.P., Charbotel B. Impaired mental well-being and psychosocial risk: A cross-sectional study in female nursing home direct staff. BMJ Open. 2015;5:e007190. doi: 10.1136/bmjopen-2014-007190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pelissier C., Fontana L., Fort E., Agard J.P., Couprie F., Delaygue B., Glerant V., Perrier C., Sellier B., Vohito M., et al. Occupational Risk Factors for Upper-limb and Neck Musculoskeletal Disorder among Health-care Staff in Nursing Homes for the Elderly in France. Ind. Health. 2014;52:334–346. doi: 10.2486/indhealth.2013-0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pélissier C., Charbotel B., Fassier J.B., Fort E., Fontana L. Nurses’ Occupational and Medical Risks Factors of Leaving the Profession in Nursing Homes. Int. J. Environ. Res. Public Health. 2018;15:1850. doi: 10.3390/ijerph15091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Hage W., Hingray C., Lemogne C., Yrondi A., Brunault P., Bienvenu T., Etain B., Paquet C., Gohier B., Bennabi D., et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encephale. 2020;46((Suppl. S3)):S73–S80. doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-CoV-2 pandemic. Psychol. Med. 2020;51:1773–1774. doi: 10.1017/S0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bisson J.I., Ehlers A., Pilling S., Dix P., Murphy A., Johnston J., Richards D., Turner S., Yule W., Jones C., et al. Post-Traumatic Stress Disorder (PTSD): The Management of PTSD in Adults and Children in Primary and Secondary Care. [(accessed on 22 December 2021)]. Available online: http://guidance.nice.org.uk/CG26.
- 10.Restauri N., Sheridan A.D. Burnout and Posttraumatic Stress Disorder in the Coronavirus Disease 2019 (COVID-19) Pandemic: Intersection, Impact, and Interventions. J. Am. Coll. Radiol. 2020;17:921–926. doi: 10.1016/j.jacr.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Compean E., Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2018;88:265–275. doi: 10.1016/j.pnpbp.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alwani S., Majeed M., Hirwani M., Rauf S., Saad S., Shah H., Hamirani F. Evaluation of Knowledge, Practices, Attitude and Anxiety of Pakistan’s Nurses towards COVID-19 during the Current Outbreak in Pakista. MedRxiv. 2020;14:707–712. doi: 10.1101/2020.06.05.20123703. [DOI] [Google Scholar]
- 13.Ornell F., Halpern S.C., Kessler F.H.P., Narvaez J.C.D.M. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad. Saude Publica. 2020;36:e00063520. doi: 10.1590/0102-311x00063520. [DOI] [PubMed] [Google Scholar]
- 14.Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Chin. J. Ind. Hyg. Occup. Dis. 2020;38:E001. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 15.Suivi Des Soignants Impliqués Dans La Prise En Charge de La COVID-19. 2020. [(accessed on 9 March 2022)]. Available online: http://www.academie-medecine.fr/wp-content/uploads/2020/06/20.6.8-Suivi-des-soignants-impliqu%C3%A9s-dans-la-Covid-ENG.pdf. [DOI] [PMC free article] [PubMed]
- 16.HAS Réponse Rapide Dans Le Cadre Du COVID-19—Souffrance Des Professionnels Du Monde de La Santé: Prévenir, Repérer, Orienter. 2020. [(accessed on 9 March 2022)]. Available online: https://www.has-sante.fr/upload/docs/application/pdf/2020-05/rr_souffrance_des_professionnels_du_monde_la_sante_version_cd_vdef_dlg_mel.pdf.
- 17.Cai H., Tu B., Ma J., Chen L., Fu L., Jiang Y., Zhuang Q. Psychological impacts and coping strategies of front-line medical staff during COVID-19 outbreak in Hunan, China. Med. Sci. Monit. 2020;26:e924171-1–e924171-16. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gold J.A. Covid-19: Adverse Mental Health Outcomes for Healthcare Workers. BMJ. 2020;369:m1815. doi: 10.1136/bmj.m1815. [DOI] [PubMed] [Google Scholar]
- 19.Le Suivi de L’état de Santé des Salariés. [(accessed on 9 March 2022)]. Available online: https://travail-emploi.gouv.fr/sante-au-travail/suivi-de-la-sante-au-travail-10727/article/le-suivi-de-l-etat-de-sante-des-salaries.
- 20.Marichalar P. La Médecine Du Travail sans Les Médecins? Une Action Patronale de Longue Haleine (1971–2010) Politix. 2010;3:27–52. doi: 10.3917/pox.091.0027. [DOI] [Google Scholar]
- 21.Insee Dossier Complet—Commune de Saint-Étienne (42218) [(accessed on 9 March 2022)]. Available online: https://www.insee.fr/fr/statistiques/2011101?geo=COM-42218#tableau-POP_G2.
- 22.Thietart R.-A. Méthodes de Recherche en Management. 4th ed. Dunod; Paris, France: 2014. [Google Scholar]
- 23.Zigmond A.S., Snaith R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 24.Bocéréan C., Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry. 2014;14:354. doi: 10.1186/s12888-014-0354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brennan C., Worrall-Davies A., McMillan D., Gilbody S., House A. The Hospital Anxiety and Depression Scale: A diagnostic meta-analysis of case-finding ability. J. Psychosom. Res. 2010;69:371–378. doi: 10.1016/j.jpsychores.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 26.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002;52:69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 27.Ashbaugh A.R., Houle-Johnson S.A., Herbert C., El-Hage W., Brunet A. Psychometric Validation of the English and French Versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) PLoS ONE. 2016;11:e0161645. doi: 10.1371/journal.pone.0161645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weathers F., Litz B., Keane T. PTSD Checklist for DSM-5 (PCL-5)-PTSD: National Center for PTSD. [(accessed on 9 March 2022)]; Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
- 29.Lesage F.-X., Chamoux A. Utilisation de l’échelle visuelle analogique (EVA) dans l’évaluation du stress au travail: Limites et perspectives. Revue de la littérature. Arch. Mal. Prof. L’environ. 2008;69:667–671. doi: 10.1016/j.admp.2008.06.013. [DOI] [Google Scholar]
- 30.D’Adamo H., Yoshikawa T., Ouslander J.G. Coronavirus Disease 2019 in Geriatrics and Long-Term Care: The ABCDs of COVID-19. J. Am. Geriatr. Soc. 2020;68:912–917. doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- 31.Auerbach R.P., Mortier P., Bruffaerts R., Alonso J., Benjet C., Cuijpers P., Demyttenaere K., Ebert D.D., Green J.G., Hasking P., et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018;127:623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pelissier C., Viale M., Berthelot P., Poizat B., Massoubre C., Tiffet T., Fontana L. Factors Associated with Psychological Distress in French Medical Students during the COVID-19 Health Crisis: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:12951. doi: 10.3390/ijerph182412951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirk J.W., Sivertsen D.M., Petersen J., Nilsen P., Petersen H.V. Barriers and facilitators for implementing a new screening tool in an emergency department: A qualitative study applying the Theoretical Domains Framework. J. Clin. Nurs. 2016;25:2786–2797. doi: 10.1111/jocn.13275. [DOI] [PubMed] [Google Scholar]
- 34.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li W., Frank E., Zhao Z., Chen L., Wang Z., Burmeister M., Sen S. Mental Health of Young Physicians in China During the Novel Coronavirus Disease 2019 Outbreak. JAMA Netw. Open. 2020;3:e2010705. doi: 10.1001/jamanetworkopen.2020.10705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.SPF La Santé Mentale des Français Face au Covid-19: Prévalences, Évolutions et Déterminants de L’anxiété au Cours des Deux Premières Semaines de Confinement (Enquête CoviPrev, 23–25 March et 30 March–1 April 2020) [(accessed on 16 December 2021)]. Available online: https://www.santepubliquefrance.fr/import/la-sante-mentale-des-francais-face-au-covid-19-prevalences-evolutions-et-determinants-de-l-anxiete-au-cours-des-deux-premieres-semaines-de-confi.
- 37.Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17:5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Santabárbara J., Bueno-Notivol J., Lipnicki D.M., Olaya B., Pérez-Moreno M., Gracia-García P., Idoiaga-Mondragon N., Ozamiz-Etxebarria N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107:110244. doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., Shohaimi S., Daneshkhah A., Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health. 2020;18:100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.SPF La Souffrance Psychique en Lien Avec le Travail Chez les Salariés Actifs en France entre 2007 et 2012, à Partir du Programme MCP. [(accessed on 16 December 2021)]. Available online: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-liees-au-travail/souffrance-psychique-et-epuisement-professionnel/la-souffrance-psychique-en-lien-avec-le-travail-chez-les-salaries-actifs-en-france-entre-2007-et-2012-a-partir-du-programme-mcp.
- 42.Troubles du Stress Post-Traumatique—INSERM, La Science Pour la Santé. [(accessed on 16 December 2021)]. Available online: https://www.inserm.fr/dossier/troubles-stress-post-traumatique/
- 43.Moitra M., Rahman M., Collins P.Y., Gohar F., Weaver M., Kinuthia J., Rouml W. Mental Health Consequences for Healthcare Workers During the COVID-19 Pandemic: A Scoping Review to Draw Lessons for LMICs. Front. Psychiatry. 2021;27:602614. doi: 10.3389/fpsyt.2021.602614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., et al. A Multinational, Multicentre Study on the Psychological Outcomes and Associated Physical Symptoms amongst Healthcare Workers during COVID-19 Outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang R., Hou T., Kong X., Wang G., Wang H., Xu S., Xu J., He J., Xiao L., Wang Y., et al. PTSD Among Healthcare Workers During the COVID-19 Outbreak: A Study Raises Concern for Non-Medical Staff in Low-Risk Areas. Front. Psychiatry. 2021;12:1064. doi: 10.3389/fpsyt.2021.696200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alonso Caballero J., Vilagut Saiz G., Mortier P., Ferrer M., Alayo I., Sanz F., Serra C., Group M.W. Mental Health Impact of the First Wave of COVID-19 Pandemic on Spanish Healthcare Workers: A Large Cross-Sectional Survey. Impacto en la salud mental del personal sanitario español de la primera ola de la pandemia COVID-19: Un amplio estudio transversal. Rev. Psiquiatr. Salud Ment. 2021;14:90–105. doi: 10.1016/j.rpsm.2020.12.001. [DOI] [Google Scholar]
- 48.Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic Stress in Healthcare Workers During COVID-19 Pandemic: A Review of the Immediate Impact. Front. Psychol. 2020;11:569935. doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu S., Yang L., Zhang C., Xu Y., Cai L., Ma S., Wang Y., Cai Z., Du H., Li R., et al. Gender Differences in Mental Health Problems of Healthcare Workers during the Coronavirus Disease 2019 Outbreak. J. Psychiatr. Res. 2021;137:393–400. doi: 10.1016/j.jpsychires.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Sio S., Buomprisco G., La Torre G., Lapteva E., Perri R., Greco E., Mucci N., Cedrone F. The Impact of COVID-19 on Doctors’ Well-Being: Results of a Web Survey during the Lockdown in Italy. Eur. Rev. Med. Pharmacol. Sci. 2020;24:7869–7879. doi: 10.26355/eurrev_202007_22292. [DOI] [PubMed] [Google Scholar]
- 51.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open. 2020;3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salman M., Raza M.H., Ul Mustafa Z., Khan T.M., Asif N., Tahir H., Shehzadi N., Hussain K. The Psychological Effects of COVID-19 on Frontline Healthcare Workers and How They Are Coping: A Web-Based, Cross-Sectional Study from Pakistan. medXriv. 2020;38:192–195. doi: 10.1101/2020.06.03.20119867. [DOI] [Google Scholar]
- 53.Sahin M.K., Aker S., Sahin G., Karabekiroglu A. Prevalence of Depression, Anxiety, Distress and Insomnia and Related Factors in Healthcare Workers During COVID-19 Pandemic in Turkey. J. Community Health. 2020;45:1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Palacios-Ceña D., Fernández-Peña R., Ortega-López A., Fernández-Feito A., Bautista-Villaécija O., Rodrigo-Pedrosa O., Arnau-Sánchez J., Lizcano-Álvarez Á. Long-Term Care Facilities and Nursing Homes during the First Wave of the COVID-19 Pandemic: A Scoping Review of the Perspectives of Professionals, Families and Residents. Int. J. Environ. Res. Public Health. 2021;18:10099. doi: 10.3390/ijerph181910099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blanco-Donoso L.M., Moreno-Jiménez J., Amutio A., Gallego-Alberto L., Moreno-Jiménez B., Garrosa E. Stressors, Job Resources, Fear of Contagion, and Secondary Traumatic Stress Among Nursing Home Workers in Face of the COVID-19: The Case of Spain. J. Appl. Gerontol. 2021;40:244–256. doi: 10.1177/0733464820964153. [DOI] [PubMed] [Google Scholar]
- 56.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing Mental Health Challenges Faced by Healthcare Workers during Covid-19 Pandemic. BMJ. 2020;368:1–4. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 57.Shanafelt T., Ripp J., Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 58.White E.M., Wetle T.F., Reddy A., Baier R.R. Front-Line Nursing Home Staff Experiences During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021;22:199–203. doi: 10.1016/j.jamda.2020.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mo S., Shi J. The Psychological Consequences of the COVID-19 on Residents and Staff in Nursing Homes. Work. Aging Retire. 2020;6:254–259. doi: 10.1093/workar/waaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spoorthy M.S., Pratapa S.K., Mahant S. Mental Health Problems Faced by Healthcare Workers Due to the COVID-19 Pandemic–A Review. Asian J. Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Caillet A., Coste C., Sanchez R., Allaouchiche B. Psychological Impact of COVID-19 on ICU Caregivers. Anaesth. Crit. Care Pain Med. 2020;39:717–722. doi: 10.1016/j.accpm.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Conti C., Fontanesi L., Lanzara R., Rosa I., Porcelli P. Fragile Heroes. The Psychological Impact of the COVID-19 Pandemic on Health-Care Workers in Italy. PLoS ONE. 2020;15:e0242538. doi: 10.1371/journal.pone.0242538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Haddaden M., Aldabain L., Patel N., Maharaj A., Saif A., Imam Z., Haas C.J. Health Care Workers Attitudes toward COVID-19 Vaccination and the Effect on Personal and Professional Life. J. Community Hosp. Intern. Med. Perspect. 2021;11:585–589. doi: 10.1080/20009666.2021.1951943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.COVID-19: Point Épidémiologique du 18 Mars 2021. [(accessed on 21 March 2022)]. Available online: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-18-mars-2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the confidentiality of participants.