Abstract
Cardiac hypertrophy, initiated by a variety of physiological or pathological stimuli (hemodynamic or hormonal stimulation or infarction), is a critical early adaptive compensatory response of the heart. The structural basis of the progression from compensated hypertrophy to pathological hypertrophy and heart failure is still largely unknown. In most cases, early activation of an inflammatory program reflects a reparative or protective response to other primary injurious processes. Later on, regardless of the underlying etiology, heart failure is always associated with both local and systemic activation of inflammatory signaling cascades. Cardiac macrophages are nodal regulators of inflammation. Resident macrophages mostly attenuate cardiac injury by secreting cytoprotective factors (cytokines, chemokines, and growth factors), scavenging damaged cells or mitochondrial debris, and regulating cardiac conduction, angiogenesis, lymphangiogenesis, and fibrosis. In contrast, excessive recruitment of monocyte-derived inflammatory macrophages largely contributes to the transition to heart failure. The current review examines the ambivalent role of inflammation (mainly TNFα-related) and cardiac macrophages (Mφ) in pathophysiologies from non-infarction origin, focusing on the protective signaling processes. Our objective is to illustrate how harnessing this knowledge could pave the way for innovative therapeutics in patients with heart failure.
Keywords: inflammation, TNFα, resident macrophages, monocyte-derived macrophages, adaptive cardiac remodeling, heart failure, aging
1. Introduction to Short-Term Adaptive Cardiac Remodeling and Transition to Heart Failure
Clinical studies have clearly established that any abnormal change in left ventricular (LV) geometry (concentric (thickening) or eccentric (dilation)) is associated with an increased risk of cardiovascular disease [1]. Cardiac hypertrophy, initiated by a variety of physiological or pathological stimuli (hemodynamic or hormonal stimulation or infarction), is a critical early adaptive compensatory response of the heart [2]. Development of either physiological or pathological hypertrophy depends both on the nature of upstream stimuli and associated signaling mechanisms as well as the duration of cardiac stress [3]. Concentric hypertrophy (elevated h/r geometric parameter: diastolic wall thickness to radius ratio, associated with an increase in heart weight) has been described as an early adaptive response to maintain a normal systolic function [4], as recently illustrated in Flamant et al. [5]. The ability of the myocardium to successfully compensate for and adapt to environmental stress ultimately determines whether the heart will decompensate and fail or conversely maintain preserved function [2]. Age, gender, increased blood pressure and body mass index are key clinical risk factors of dynamic worsening. Data in humans regarding the development of LV geometric pattern over time are relatively scarce. However, there is substantial evidence for a potential temporal sequence of transient concentric hypertrophy evolving over the long term toward eccentric hypertrophy, dilation, and the development of heart failure (HF) [6,7], as already suggested in animal studies [5].
Physiological hypertrophy (during development, pregnancy, or endurance training) is totally reversible, characterized by mild heart growth (10–20% higher than that of a normal heart), absence of fetal gene program reactivation, an increase in individual cardiomyocyte growth in both length and width, angiogenesis, and the absence of apoptosis and interstitial fibrosis [8]. In contrast, chronic cardiac hypertrophy will eventually progress into HF, arrhythmia, and sudden death, following associated induction of apoptotic and fibrotic responses and the disruption of coordinated tissue growth with angiogenesis [9,10,11,12]. Adaptative concentric LV hypertrophy is also observed during aging, even in apparently healthy individuals [13]. Moreover, the left atrium enlarges and increases in volume roughly 50% between the third and eighth decade [14], predisposing elderly subjects to atrial fibrillation (AF).
Of note, physical exercise has a protective effect on the heart, and endurance training improves cardiac performance in hypertensive rats by converting pathologic hypertrophy into a more physiologic hypertrophy associated with lower apoptosis and fibrosis and higher angiogenesis [15,16].
In case of HF, the heart is unable to pump the blood efficiently due to ineffective muscle contraction (systolic HF) or relaxation or filling abnormalities (diastolic HF). Based on the ejection fraction, HF patients can be classified into two major groups. Patients with impaired systolic function are categorized in HF with reduced ejection fraction (HFrEF), whereas patients with diastolic dysfunction, often characterized by normal systolic function, are classified in HF with preserved EF (HFpEF). HFpEF has emerged as a critical health problem. Its prevalence increases with aging, obesity, diabetes, and hypertension. For example, in the setting of normal aging, HFpEF is promoted by an impairment of ventricular compliance due to the expansion of myocardial fibrosis, and disturbances of calcium homeostasis in hypertrophied cardiomyocytes, leading to a delayed relaxation [17]. In these elderly patients, the contribution of atrial contraction to ventricular filling is enhanced but atrial contractility is impaired, increasing the risk of the development of HF [18].
In most cases, early activation of an inflammatory program reflects a reparative or protective response to other primary injurious processes [19]. Later on, regardless of underlying etiology, HF is always associated with both local and systemic activation of inflammatory signaling cascades [19,20,21]. The structural basis of the progression from well-compensated hypertrophy to pathological hypertrophy and HF is still largely unknown [22]. Therefore, a better understanding of cellular mechanisms elicited during early remodeling is necessary to prevent the progression to HF or favor recovery [23,24]. To achieve this goal, there is accumulating evidence that advances in understanding the role of inflammation in tissue remodeling are essential [25].The current review examines the ambivalent role of inflammation (mainly TNFα-related) and cardiac macrophages (Mφ) in pathophysiologies related to hypertension, aortic stenosis, genetic cardiomyopathies, and sepsis or aging, with a special focus on related protective signaling processes.
2. Cardiac Remodeling, HF, and Inflammation
The link between HF and inflammation was first recognized in 1990 by Levine [26]. Since then, proinflammatory cytokines have emerged as determinant factors for initiating, integrating, and maintaining the myocardial response to stress [2], and there is evidence of an ongoing inflammatory response in all the manifestations of clinical HF [27]. For example, activation of the NLRP3 inflammasome is important for severe pressure overload-induced myocardial remodeling [28]. Inhibition of NLRP3 signaling reverses transverse aortic constriction (TAC)-induced pathological remodeling by attenuating hypertrophy, inflammation, and fibrosis via inhibition of calcineurin and MAPK activities, thereby improving contractile function [29]. Similarly, with age, high levels of oxidative stress and associated tissue damage (including cell death and fibrosis) trigger an inflammatory response, which importantly contributes to atrial and ventricular remodeling [30,31,32,33].
The prevailing concept has long been that inflammation, like one of its master regulator tumor necrosis factor alpha (TNFα), is harmful and precipitates transition from early cardiac remodeling to HF. In support for this concept, dysregulated cytokines expression (sustained and excessive), e.g., cardiac targeted TNFα overexpression, is sufficient to produce injury and provoke overt cardiac decompensation [34,35,36,37,38,39]. Elevated levels of TNFα have been associated with HF [26,27,40,41,42] and a progressive increase in serum TNFα correlated with disease progression (according to the New York Heart Association classification) [43,44]. By using TNFα-knockout mice, Sun et al. have demonstrated that, in the pressure-overload TAC model, TNFα contributes to adverse cardiac remodeling [45]. Accordingly, a series of multicenter clinical trials have been conducted in HF patients using compounds that trap TNFα, comprising infliximab, an antibody directed to TNFα, and etanercept, a soluble recombinant receptor of TNFα. Surprisingly, outcomes were disappointing, leading at best to no benefit, and at worst to HF worsening [46,47,48,49]. This highlighted the revisited cytokine hypothesis of a long-term deleterious but potentially beneficial short-term impact of inflammation [43,49,50]. In fact, a growing body of evidence supports the notion that short-term low-level expression of pro-inflammatory molecules is beneficial and acts as an early warning system (review in Mann [2] and Sacks [51]). This literature reporting beneficial effects of inflammation in the early stages of cardiac injury offers novel insights [52,53]. Interestingly, clinical studies have suggested the potential adaptive role of TNFα in early cardiac remodeling showing that myocardial TNFα gene expression is significantly higher in patients with compensated aortic stenosis than in patients with decompensated stenosis [54] and that elevation of circulating TNFα is associated with concentric left ventricular remodeling [55].
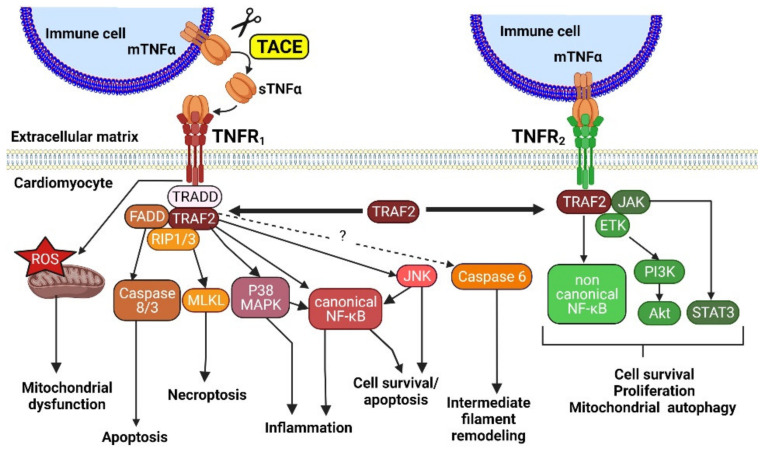
Figure 1 illustrates some of TNFα signaling pathways.
Figure 1.
TNFα downstream signaling pathways mediated by the two receptors, TNFR1 and TNFR2. sTNFα, soluble tumor necrosis factor α; mTNFα, membranous tumor necrosis factor α; TACE, tumor necrosis factor α converting enzyme; TNFR1, Tumor necrosis factor receptor 1; TNFR2, tumor necrosis factor receptor 2; TRADD, TNFR1-associated death domain; FADD, fas-associated protein with death domain; RIP1/3, receptor interacting protein 1/3; ROS, reactive oxygen species; MLKL, mixed lineage kinase domain like pseudokinase; MAPK, mitogen-activated protein kinase; JNK, c-Jun N-terminal kinases; TRAF2, TNFR-associated factor 2; JAK, Janus kinase; ETK, epithelial and endothelial tyrosine kinase; PI3K, phosphoinositide 3 kinase; Akt, protein kinase B; STAT3, signal transducer and activator of transcription 3.
Since its discovery in 1975, the pro-inflammatory cytokine TNFα has been a subject of intense study [56]. TNFα is primarily produced by immune system cells, but also by all cell types in the heart, including cardiomyocytes. TNFα signals through two distinct membrane receptors, TNFR1 and TNFR2 [57]. TNFα exists as a membrane-bound form protein (mTNFα) that can be cleaved by a TNFα-converting enzyme (TACE) and released from cells as a soluble form of TNFα, sTNFα (Figure 1). The biological effects of sTNFα and mTNFα are not identical, with sTNFα and mTNFα preferentially activating TNFR1 and TNFR2, respectively [58]. Both receptors require the recruitment of adaptor molecules to initiate signaling, such as TNFR1-associated death domain (TRADD) and ubiquitin ligases and TNFR associated factors (TRAFs). TNFR1 and TNFR2 not only function independently, but also can influence each other via cross-talk between the different signaling pathways. A key player in TNFR1- and TNFR2-induced signaling is the RING finger protein TRAF2, which is recruited to both receptors upon their stimulation [59]. TRAF2 mediates cross-talk between TNFR1 and TNFR2, dictating the outcome of TNFα stimulation [59,60] (Figure 1). Membranous TNFR1 and TNFR2 can also be shed via cleavage by TACE and soluble truncated forms of TNFR1 and TNFR2 may lower the concentration of TNFα available for binding to functional cells [61,62].
2.1. TNFα, Early Adaptive Remodeling and HF
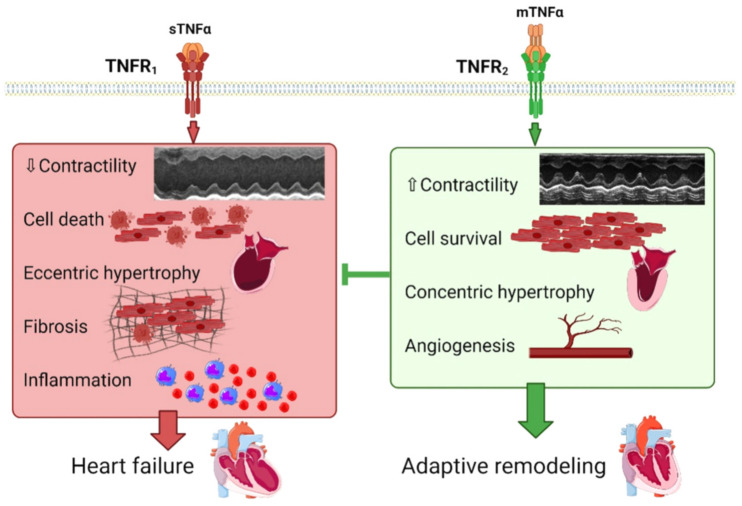
TNFα treatment has been shown to induce hypertrophy in isolated adult and neonatal cardiomyocytes, via ROS production, NFκB, MAPK and/or Akt signaling [63,64,65,66,67] (Figure 1). In line with this, TNFα overexpressing mice undergo ventricular hypertrophy, altered cardiac contractility and develop dilated cardiomyopathy [34,36,68,69], as illustrated in Figure 2.
Figure 2.
Physiopathological impact of TNFα signaling mediated by TNFR1 and TNFR2 on cardiac remodeling. sTNFα, soluble tumor necrosis factor α; mTNFα, membranous tumor necrosis factor α; TACE, tumor necrosis factor α converting enzyme; TNFR1, tumor necrosis factor receptor 1; TNFR2, tumor necrosis factor receptor 2. Macrophages are represented in blue and inflammatory monocytes in red (inflammation panel).
In TNFα overexpressing mice, disruption of TNFR1 limits cardiac hypertrophic remodeling and preserves cardiac function [68]. The remaining hypertrophic response observed after TNFR1 ablation was suggested to be driven by TNFR2 [68]. By contrast, disruption of TNFR2 exacerbates dilation and HF [68]. In accordance, whereas cardiac restricted overexpression of mTNFα favors concentric hypertrophy that does not evolve towards dilated cardiomyopathy after 24 weeks, cleavable TNFα overexpression elicits a dilated cardiac phenotype [70,71] (Figure 2). Thus, interaction between mTNFα and TNFR2 may contribute to the beneficial effect of TNFR1 KO. In contrast, the interaction between sTNFα and TNFR1 may relay the deleterious effects of TNFR2 KO (Figure 2). In mice overexpressing cleavable TNFα, TACE inhibition abrogates the LV dilation and results in an increase in LV wall thickness, mimicking the effects observed in mice with non-cleavable mTNFα [68]. This suggests that posttranslational processing of TNFα is responsible for the dilated cardiac phenotype in mice with targeted cardiac overexpression of TNFα [70,71]. In addition, by using global KO mice or AAV9-mediated troponin C targeted deletion in cardiomyocytes, a recent study by Miao et al. demonstrates that transmembrane TNFα (mTNFα) attenuates pressure-overload TAC cardiac hypertrophy via TNFR2 [72] and suggests that preventing mTNFα cleavage by targeting the TNFα converting enzyme (TACE) rather than inhibiting TNFα signaling might be a valuable approach in HF [73]. TNFα signaling contributes to in vivo β-AR-mediated cardiac remodeling in a receptor-specific manner [74]. Unopposed TNFR1 activation is pro-inflammatory, pro-hypertrophic, and promotes functional decline. However, co-activation of TNFR2 during β adrenergic stress is anti-inflammatory and counterbalances these deleterious effects [74]. As proposed by Higuchi et al. [68], the opposite effects of TNFR1 and TNFR2 on cardiac remodeling and HF progression could rely on their opposite regulation of Akt, a pro-survival kinase, potently inhibited by the TNFR1-induced second messenger ceramide [75], as illustrated in Figure 3.
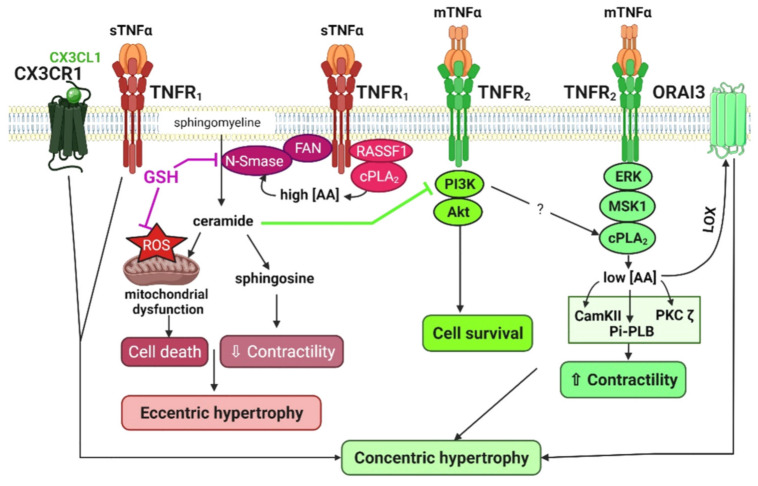
Figure 3.
Determinant role of lipid signaling in TNFα–induced regulation of contractility, cell survival and hypertrophy. Synergistic action of TNFα and CX3CL1 drives a concentric hypertrophic response. sTNFα, soluble tumor necrosis factor α; mTNFα, membranous tumor necrosis factor α; TACE, tumor necrosis factor α converting enzyme; TNFR1, tumor necrosis factor receptor 1; TNFR2, tumor necrosis factor receptor 2; CX3CL1, fractalkine; GSH, glutathione; ROS, reactive oxygen species; FAN, factor associated with neutral sphingomyelinase activation; N-Smase, neutral sphingomyelinase; RASSF1, ras association domain family member 1; cPLA2, cytosolic phospholipase A2; AA, arachidonic acid; LOX, lipoxygenase, PI3K, phosphoinosisitde 3 kinase; Akt, protein kinase B; ERK, extracellular signal-regulated kinase; MSK1, mitogen- and stress-activated kinase 1; CamKII, calmoduline kinase II; PKC, protein kinase C; Pi-PLB, phosphorylated phospholamban.
TNFα also impacts intermediate filament remodeling (Figure 1). TNFα has been reported to play a central role in end-stage HF in humans and mice, due to desmin (Des) cleavage by activated caspase 6 [76]. Des cleavage triggers aggregates formation, leading to intercalated disk destabilization, mitochondrial defects, cell death, and HF [77]. In TNFα overexpressing mice also expressing a caspase cleavage-resistant Des mutant (D263E), cardiac myocyte apoptosis was attenuated, LV wall thinning was prevented, and cardiac function was improved. This reveals an important role for Des cleavage in the development of TNFα-induced dilated cardiomyopathy and HF [77]. However, surprisingly, crossing the following two genetic HF models, namely TNFα overexpressing and Des−/− mice, results in a considerable rescue of the typical Des−/− extensive myocardial degeneration: mice display early cardiac hypertrophy, but prevention of adverse dilated remodeling and alteration of fractional shortening [78]. TNFα overexpression exerts a cardioprotective function through NF-κB-mediated cardiomyocyte ectopic expression of keratin 8 (K8) and keratin 18 (K18), two simple epithelia-specific intermediate filament (IF) proteins at the IDs [78]. The global nature of K8 and K18 ectopic protective induction was confirmed in stressed or failing cardiomyocytes by using experimental models of HF such as TAC or infarction, or in cardiomyocytes from human failing hearts, and associated with TNFα upregulation [78]. The mechanism of protection by TNFα through formation of a potential de novo alternative IF cytoskeletal system allowing to compensate for Des deficiency, could be through maintenance of mitochondrial function and intercalated disks integrity [78].
2.2. TNFR and NF-κB Signaling, Cell Survival and HF
NF-κB plays an essential role in cardiac remodeling and HF, essentially driven by two main pathways: the canonical pathway (involving p65, p50 and/or cRel protein members) and the non-canonical pathway (involving p52 and/or RelB) [79]. Activation of NF-κB relies on the nuclear translocation of homodimer or heterodimer forms of its members [79]. Increased activity and/or expression of NF-κB may participate in both cardioprotection (e.g., anti-apoptotic) [80,81], or in the development of heart diseases, as detailed in [79]. For example, the transition of cardiac hypertrophy to HF may be accompanied by NF-κB-mediated suppression of the sarcoplasmic reticulum Ca2+ ATPase 2 (SERCA2) transcription in ventricular myocytes [82]. NF-κB activation also mediates aging in the heart [83,84,85]. Different translocation patterns of NF-κB protein members were observed in aged murine models, but inhibition of NF-κB was generally suggested as protective [83,84,85]. In patients with valvular disease, higher NF-κB activity, higher TNFα levels, and more fibrosis characterized those with atrial fibrillation as compared to patients with sinus rhythm [86]. However, in other clinical studies, a loss of function mutation of NF-κB was considered either to confer susceptibility to left ventricular dysfunction [87], or to facilitate the onset of HF or worsen its prognosis [88]. These opposing findings suggest contrasting regulatory effects of the different NFkB members with complex outcomes.
TNFR1 is a death receptor, as its structure includes a death domain [60]. TNFR1 activates the canonical NF-κB pathway and the JNK/p38 MAP kinase pathway leading to either 1) inflammatory cytokines production or survival or 2) apoptosis or necroptosis, depending on receptor interacting protein 1/3 (RIP1/3) ubiquitination [60,80,89] (Figure 1). TNFR2 (lacking the death domain) can activate both the canonical NF-κB pathway (but to a lower extent as compared to TNFR1) and the non-canonical NF-κB pathway, mostly resulting in cell survival and proliferation [60]. A pro-survival signaling pathway termed the SAFE pathway (for survivor activating factor enhancement), involving TNFR2/STAT3 signaling, has also been identified to protect against MI [90]. The scaffolding protein TRAF2 may facilitate cytoprotective signaling downstream of both TNFR, playing a prosurvival key role to transduce activation of kinases and transcription factors [91,92,93] and promoting mitochondrial autophagy [94] (Figure 1).
2.3. TNFα, Contractile Function and HF
2.3.1. The Neutral Sphingomyelinase, a Determinant of TNFR1 Deleterious Signaling
Lipid signaling plays a determinant role in TNFα-induced regulation of cardiac remodeling, as illustrated in Figure 3.
TNFα is essentially considered as a cardio-depressant mediator [95,96,97]. It has been shown to induce oxidant stress [98], to cause a drop in glutathione (GSH) levels, and to increase ceramide production through neutral-sphingomyelinase (N-Smase) activation (enzyme that converts sphingomyelin to ceramide). These mechanisms precede and regulate its depressant effects [95,99,100].
In control cardiac myocytes, TNFR1-dependent responses are predominant, overwhelming TNFR2 signaling but seem to be under the yoke of TNFR2, acting as a limiting factor [101]. TNFα exerts a dual positive and negative action on cell fractional shortening and alters cell survival [101,102,103,104,105]. The negative inotropic effect exerted by TNFα is thought to be mediated by TNFR1 [57,101,106]. In cardiomyocytes, activation of the N-Smase mediates TNFα-induced apoptosis and negative contractile effect [99,100,102,107]. This TNFα depressant effect is reproduced by sphingosine and suppressed by a specific inhibitor of ceramidase (enzyme that converts ceramide to sphingosine) [107] (Figure 3).
Glutathione is the physiological inhibitor of the neutral sphingomyelinase [99]. Administration to rats of the GSH precursor N-acetylcysteine (NAC) abrogates TNFα-induced N-Smase activation, oxidative stress, and negative effects on contraction in isolated cardiomyocytes [102]. One can speculate that glutathione status determines the adverse effects of TNFα in cardiac failure and that TNFα antagonism may be achieved by glutathione supplementation. In agreement, NAC, given orally as a curative treatment, replenishes cardiac GSH content, normalizes serum TNFα, and prevents morphological and functional cardiac injuries in the hypertensive high salt/L-NAME rat model. Of note, the NAC effect likely derives both from GSH-induced N-Smase direct inhibition [99,108] and from GSH anti-oxidant action [99] (Figure 3).
Treatment with a neutralizing anti-TNFR1 antibody or the GSH precursor, NAC, favors the emergence of the TNFR2 signaling, driving a positive effect on cell fractional shortening [101]. Thus, NAC treatment is proving a valuable anti-inflammatory tool to neutralize TNFR1-dependent signaling [101,102] and promote the emergence of TNFR2 pathways. In contrast, neutralizing anti-TNFR2 antibodies exacerbates TNFα-induced ROS production, negative inotropic impact and cell death, arguing for a protective role of the TNFR2 pathway and a TNFR1 and TNFR2 signaling interplay [101].
2.3.2. The Cardiac cPLA2, a Determinant TNFR2 Protective Signaling Pathway: Involvement in β2-Adrenergic Signaling and Relationship with PI3Kinase Activity
Phospholipase A2 enzymes (PLA2s) catalyze the hydrolysis of the sn-2-fatty acyl ester bonds of membranous glycerophospholipids, leading to the liberation of lysophospholipids and free fatty acids including arachidonic acid (AA) [109,110].There is accumulating evidence for the determinant role of the cytosolic PLA2 (cPLA2)/AA pathway in cardiac TNFα signaling. AA activates N-Smase activity [111] (Figure 3). Thus, the TNFR1-induced negative contractile effect of TNFα is reproduced by high concentrations of AA [112]. In contrast, low concentrations of AA mediate TNFR2 signaling, leading to an improvement of the contractile function [108] (Figure 3). MacEwan’s group highlighted distinct regulations of the cPLA2 phosphorylation, proteolysis and activation by TNFR subtypes [113]. In addition, Mohamed et al. demonstrated the essential role of the RASSF1 (Tumor Suppressor Ras-Association Domain Family Protein 1A) adaptor protein in regulating downstream TNFα signaling via cPLA2 [103]. In adult rat cardiomyocytes, the study by Defer et al. identified a TNFR2-dependent activation of the cPLA2 together with the phosphorylation of ERK, MSK1, PKCζ, CAMKII, and phospholamban (Thr17 residue), leading to a positive action on calcium cycling and cell fractional shortening [101] (Figure 3).
Accumulating evidence highlights the cross-talk between inflammatory cytokines and sympathetic systems [61,114]. The sympathetic nervous system serves as one of the first mechanisms of compensation in response to cardiac injury. β-adrenergic receptor (β-AR) signaling defects are central features of human HF, with a selective decrease in β1-ARs number, and an impairment of the coupling of both β1-ARs and β2-ARs to Gs and adenylyl cyclase (AC) [115]. In a manner similar to TNFR2 signaling, the cPLA2 pathway has also been reported to play an important cardioprotective role in β2-AR signaling [116,117,118,119,120]. In homeostatic conditions, in embryonic chicks [117], and in adult rats [116] ventricular myocytes, β2-AR stimulation activates cPLA2/AA signaling, supporting calcium cycling and cell contraction. In the context of HF, the recruitment of the cPLA2 by β2-AR in the human heart has been evidenced in situations of altered β-AR (both β1-AR and β2-AR subtypes) coupling to AC/cAMP/PKA signaling [119]. Importantly, this suggested that cPLA2 signaling might compensate for impaired cAMP/PKA signaling occurring in aging or failing hearts [118,119]. In line with this, the group of Lipsius recently demonstrated that inhibition of PKA by phosphatidylinositol-3-kinase (PI3kinase) favors β2-AR stimulation of cPLA2 [121]. This study illustrates the potential association between cPLA2 signaling and activation of the PI3Kinase [121], a downstream target of β2-AR signaling initially identified by Xiao et al. [122] driving a strong cell survival signal in adult rat cardiomyocyte [123,124]. Similarly, the TNFR2 pathway has been associated not only with cPLA2 activation but also with PI3K stimulation [125]. Whether TNFR2-dependent activation of PI3Kinase favors cPLA2 signaling remains to be investigated.
By using cPLA2 knockout mice, the group of Bonventre and Force has shown that cPLA2 mitigates both normal and TAC-induced cardiac pathological hypertrophy, limiting growth factor IGF1 signaling, via AA-induced translocation to the membrane and activation of PKCζ and PDK1, pivotal players in cardiac hypertrophy [126,127]. However, cPLA2 metabolites have also been implicated as positive regulators of cardiac growth [128,129]. Concerning the TNFα signaling, the cPLA2 pathway also plays a role in modifications of Ca2+ handling remodeling that drive TNFα-protective hypertrophic and anti-apoptotic responses in hypertrophied cardiomyocytes [130,131] (Figure 3). Our group highlighted a TNFα/TNFR2-dependent signaling leading to ORAI3-dependent Ca2+ channel activation promoting early adaptive cardiac hypertrophy (ECH) and resistance to oxidative stress in rats subjected to isoproterenol infusion or abdominal aortic banding [130,131]. Of note, the regulation of ORAI3 by TNFα is detected in hypertrophied cardiomyocytes but not in normal counterparts. ORAI3-driven store-independent Ca2+ influx relies on cPLA2 activation [131], initial AA production and further AA metabolism via the lipoxygenase (LOX) pathway [131,132,133] (Figure 3). ORAI3 pharmacologic or molecular (siRNA) neutralization inhibits protective GSK3β phosphorylation, impairs early adaptive cardiac hypertrophy and accelerates HF [131].
2.4. Combined Signaling of TNFα with the CX3CL1 Chemokine
Unrelated to this previously identified TNFR2-ORAI3 pathway, our recent study shows that synergistic action of TNFα with the chemokine CX3CL1 promoted adaptive cardiac concentric hypertrophy in response to early β-AR chronic stimulation and limited transition toward eccentric dilated remodeling (low h/r geometric parameter) and HF [5]. This newly identified compensatory TNFα signaling relied on binding to TNFR1 (Figure 3). These results illustrated the protective role of the CX3CL1/CX3CR1 axis in early cardiac remodeling. Other studies have reported that CX3CL1 increases endothelial and smooth muscle cell migration and proliferation and acts as a proangiogenic factor that favors neovascularization [134]. Importantly, our results suggested the participation of TNFα, CX3CL1-cosecreting Mφ and their crosstalk with CX3CR1 expressing cardiomyocytes to delay HF [5].
3. Innate Immunity, Cardiac Remodeling and HF
Recent developments in the field of innate immunity have further advanced our understanding of the major role of inflammation in the pathogenesis of HF [27] or aging [135]. In particular, cardiac remodeling is a complex inflammatory syndrome where Mφ play a determinant role. Mφ reside in the tissue in the absence of injury and inflammation, but also play a major role following myocardial stress, where they can be protective or harmful [136,137]. Mφ influence tissue homeostasis, repair and regeneration in response to injury and modulating cardiac hypertrophy and HF [138,139,140]. These plastic cells adapt their physiology in response to cardiac and systemic stimuli. They are crucial in controlling and regulating the local tissue microenvironment, the matrix, oxygen content, acidification, and other molecular components (e.g., cytokines, growth factors, and chemokines) associated with micro-environmental shifts [141]. Mφ metabolism, including lipid metabolism, not only provides energy but also greatly influences Mφ phenotype and function, for example modulating signal transduction and gene regulation [142]. Dysregulation of lipid metabolism in Mφ is associated with various diseases [142].
Mφ have been extensively implicated in the inflammatory response to myocardial infarction (MI) [143]. A growing body of evidence suggests that they also play a critical role in the pathogenesis of chronic non-ischemic heart remodeling, e.g., after TAC [144,145,146,147].
Striking increases in the accumulation of recruited inflammatory Mφ in the heart within days to weeks following TAC, are linked to fibrosis and adverse LV remodeling [148,149]. In agreement, clodronate-induced Mφ depletion decreases infiltration of inflammatory Mφ and reduces LV hypertrophy in a model of hypertensive heart disease elicited by angiotensin II [150]. These studies are consistent with and further support the notion that inhibition of inflammatory signals is effective at preventing HF development after an increase in mechanical overload [28,147].
However, other studies have shown that the inflammatory response induced by the innate immune system can be physiological and results in the upregulation of cytoprotective responses that allow the heart to adapt to stress in the short term [2]. For instance, the study by Keck et al. points out inflammation arising from cardiac resident CD11b/c cells as a potential trigger of TNFR2- and ORAI3-dependent protective signaling pathways in cardiomyocytes, promoting early adaptive hypertrophy, improving resistance to oxidative stress, and delaying transition to HF, in response to TAC-induced pressure overload or β-adrenergic chronic infusion [131].
Therefore, cardiac Mφ are an emerging focus for therapeutic strategies aimed at strengthening adaptive responses, minimizing cardiomyocyte death, ameliorating pathological cardiac remodeling, and for treating HF [151].
4. Macrophages Subsets and Cardiac Remodeling
Metchnikov first described Mφ as phagocytic cells and key mediators in the phagocytosis theory in the late 1880′s [152] and received the Nobel prize in Physiology or Medicine for his work in 1908. Cardiac Mφ comprise 5–10% of total myocardial cells and are the most abundant leukocyte species in the heart [153,154]. In mice, their identification is based on “classical” surface markers (F4/80, CD64, CCR2, CX3CR1, MERTK, Ly6C, MHCII, CD206), novel markers (LYVE1 and TIMD4) or intracellular (CD68) molecule expression [155,156].
For years Mφ were thought to derive exclusively from circulating monocytes becoming tissue-resident after infiltration and differentiation [157]. We now know that many Mφ from embryonic origin integrate tissues prior to the onset of hematopoiesis [158,159]. Thus, cardiac tissue Mφ, either derive from embryonic origin independent of hematopoiesis (CCR2−/Ly6Clow/MHCIIlow/high) and persist in adultwood through in situ proliferation, or originate from monocyte infiltration (CCR2+/Ly6Chigh/MHCIIhigh) and replenish by circulating monocyte seeding [160]. Equivalent Mφ subpopulations (CCR2− and CCR2+) were identified in the human heart [161]. During aging, the number of fetal liver-derived cardiac resident Mφ decreases and a substantial pool of adult cardiac Mφ is replenished by Mφ derived from bone marrow or spleen monocytes, suggesting an age-associated decrease in the local self-renewal capacity of resident CCR2− Mφ [135,160,162].
Current knowledge gives clear evidence that the different cardiac Mφ populations are plastic, display various responses to injury, and differentially regulate repair processes. It thus appears that a timely planned targeting of specific subsets of Mφ will probably be necessary to achieve beneficial results in HF.
Strikingly, recent mapping and genetic depletion studies allowed to begin to decipher the functional roles of various Mφ populations and identify functions far beyond a phagocytic and immunologic role, e.g., maintaining mitochondrial function, facilitating cardiac conduction, and promoting coronary development and lymphangiogenesis [136,163].
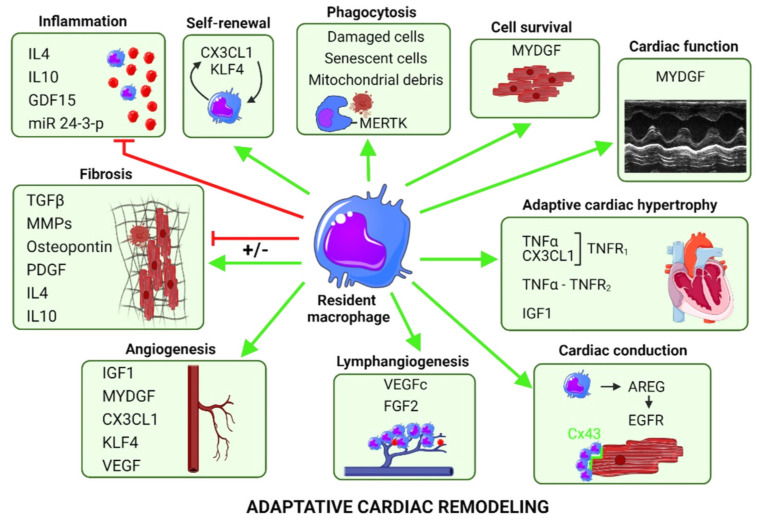
Figure 4 illustrates the impact of cardiac resident Mφ in adaptive cardiac remodeling.
Figure 4.
Induction of adaptive cardiac remodeling by resident CCR2− Ly6Clow macrophages. CCR2, C-C motif chemokine receptor 2; Ly6C, lymphocyte antigen 6 complex; IL4, interleukin 4; IL10, interleukin 10; GDF15, growth differentiation factors 15; CX3CL1, fractalkine; KLF4, Kruppel-like factor 4; MERTK, myeloid-epithelial-reproductive tyrosine kinase; MYDGF, myeloid derived growth factor; IGF1, insulin-like growth factor-1; TGFβ, transforming growth factor β; MMPs, metalloproteinases; PDGF, platelet-derived growth factor; VEGF, vascular endothelial growth factor; FGF2, fibroblast growth factor 2; AREG, amphiregulin; EGFR, epidermal growth factor receptor; Cx43, connexin 43. Resident macrophages are represented in blue and inflammatory monocytes in red (inflammation and lymphangiogenesis panels). Positive (green line) and negative (red line) regulations.
4.1. Resident Mφ Are Requisite for the Adaptive Response to Pressure Overload or Hypertension
An increase in pressure overload (e.g., TAC model) triggers an early concentric hypertrophic response of the myocardium. Cardiac-resident Mφ with low expression of Ly6C, generally considered as predominantly anti-inflammatory, were identified as critical mediators of this adaptive response by cardiomyocytes [164] (Figure 4). In contrast, a consensus seems to indicate that recruited pro-inflammatory CCR2+ Mφ, rather than resident CCR2− Mφ, mediate pathological hypertrophy during the late phase of pressure overload [147,165,166].
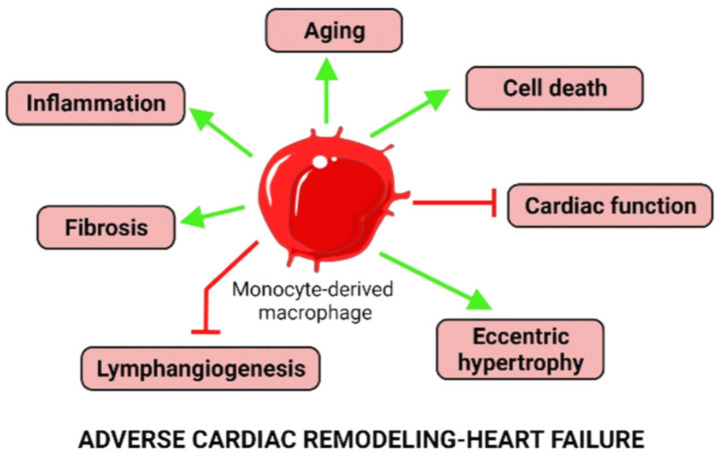
Global depletion of Mφ in the setting of hypertension worsens cardiac function but improves fibrosis suggesting dual protective and pathological functions of diverse Mφ populations [165,167,168,169]. Monocyte-derived Mφ (CCR2+) promote tissue damage and fibrosis in hypertension [170,171], as illustrated in Figure 5.
Figure 5.
Induction of heart failure by monocyte-derived CCR2+ Ly6Chigh macrophages. CCR2, C-C motif chemokine receptor 2; Ly6C, lymphocyte antigen 6 complex. Positive (green line) and negative (red line) regulations. Monocyte-derived inflammatory macrophage represented in red.
In contrast, a potential protective role of self-renewing resident-Mφ (CCR2−) has emerged from recent studies [137,156,169,172,173] (Figure 4).
4.1.1. Protective Growth Factor Secretion by Resident Mφ
IGF1
Adaptive cardiomyocyte growth allows the myocardium to withstand hypertensive stress. Fate-mapping approaches, genetic ablation of resident Mφ or specific deletion of IGF1 in resident Mφ recently highlighted that the ability of the heart to adapt to hypertension is dependent on local IGF1 produced by resident Mφ [169]. Selective reduction of resident Mφ abolishes adaptive cardiomyocyte growth and leads to adverse remodeling (fibrosis), dilation, and severe cardiac dysfunction [128,129]. Of note, IGF1 was also previously identified as a potential mediator of the proangiogenic properties of embryonic-derived Mφ [174] (Figure 4).
In a mouse model of chronic dilated cardiomyopathy harboring a causative human mutation of the troponin T2 gene, Wong et al. demonstrate that CCR2− Mφ, that interact with neighboring cardiomyocytes through focal adhesion complexes, sense mechanical stretch. This triggers their activation through a transient receptor potential vanilloid 4 (TRPV4)-dependent pathway and enhances their growth-factor expression, notably IGF1 [175]. This mechanism supports the determinant early protective role of CCR2− Mφ in adaptive remodeling, coronary angiogenesis, cardiac output maintenance, and mice survival [175]. Wong et al. confirmed the CCR2− Mφ-induced adaptive protection in a TAC model [175].
AREG/EGFR
The group of Manabe elegantly demonstrated that Ly6Clow Mφ, upregulated in the TAC model, secrete amphiregulin (AREG), which directly induces hypertrophy of neonatal cardiomyocytes in vitro [164]. In addition, AREG, produced by resident Mφ, controls connexin-43 (Cx43) phosphorylation and localization in cardiomyocytes, and therefore regulates cardiac impulse conduction [176] (Figure 4). The involvement of EGFR, a low-affinity receptor for AREG, and activation of a MEK/ERK pathway is suggested by Sugita et al. [176]. Thus, AREG is proposed as a potential therapeutical target for the prevention of arrhythmogenicity and sudden death after right ventricle or acute β adrenergic stress [176]. Notably, Son et al. describe a decrease in LV Areg mRNA expression in patients who suffered sudden cardiac death [177]. This points out a new protective mechanism in addition to the direct capacity of resident Mφ to connect to cardiomyocytes through Cx43-containing gap junctions that influences propagation of electrical signals and contributes to cardiac conduction in the AV node, previously identified by Hulsman et al. [178,179,180] (Figure 4).
However, activation of the AREG/AKT/mTOR pathway by using a chronic treatment with a GABA2R agonist has been shown to increase MHCIIhigh vs. MHCIIlow Ly6Clow Mφ, and favor not only hypertrophy but also the development of cardiac fibrosis and the transition from concentric adaptive to eccentric remodeling. This suggested, in the long term, a potential participation of the pathway in cardiac decompensation and HF [181].
MYDGF
In contrast, some anti-hypertrophic inflammatory stimuli are beneficial and mediate adaptation to pressure overload [52]. By using the TAC model, the group of Wollert recently demonstrated that myeloid-derived growth factor (MYDGF), secreted by both CCR2high and CCR2low Mφ, attenuates LV hypertrophy and dysfunction via activation of the Pim1 proto-oncogene (PIM1) kinase and enhancement of SERCA2a expression [52,182]. Of note, MYDGF expression by both CCR2high and CCR2low subsets of Mφ is in line with the notion that these subsets exert distinct and partially overlapping functions [147,165,182,183]. MYDGF is a paracrine protein produced by bone marrow- and spleen- derived mononuclear monocytes and Ly6Clow cardiac Mφ, as initially demonstrated [184], but also by endothelial cells, as more recently suggested [185]. MYDGF reduces scar size and improves heart function after MI via the MAPK-STAT3 signaling pathways, favoring endothelial cell proliferation and angiogenesis and limiting cardiomyocytes apoptosis [184] (Figure 4). MYDGF also promotes post-MI heart regeneration in neonates and adults by favoring cardiomyocyte proliferation and expansion via the c-Myc/FoxM1 pathway [185]. MYDGF is a promising target to reverse cardiac remodeling and HF because, in mice models, recombinant MYDGF protein improves heart regeneration both in neonatal and adult heart after MI or TAC injury [182,184,185]. Of note, MYDGF levels are increased in both heart and plasma post-MI patients [184].
GDF15
GDF15 is a particularly interesting growth factor, described as protective in cardiovascular diseases. This cardiac-inducible factor is upregulated with aging or after various cardiovascular events linked to inflammation and oxidative stress [186] and is secreted by different cell types including cardiomyocytes and Mφ [187]. Exposure of Mφ to pro-inflammatory cytokines such as TNFα and TGFβ upregulates GDF15 expression [188]. Although GDF15 was reported to be induced in a pressure-overload murine model, its cardiac-specific overexpression antagonizes the hypertrophic response and the loss of ventricular performance [189]. GDF15 exerts anti-inflammatory effects by 1) limiting the recruitment of infiltrating pro-inflammatory cells through direct interference with chemokine signaling and integrin activation [190] and 2) promoting the M2 polarization of Mφ [191] (Figure 4). Chronic increase in circulating GDF15 levels have been reported both in HFpEF and HFrEF patients [187], and GDF15 has recently emerged as a strong and independent biomarker for identifying patients displaying HF with midrange or preserved EF with a worse prognosis [192].
VEGFc-d and FGF2
The lymphatic system has recently emerged as an important regulator of the interstitial fluid compartment, the immune cell transport and tissue remodeling during cardiac pathology and is under the control of Mφ populations [163,193,194]. A dysfunctional lymphatic system promotes exacerbation of chronic inflammation and long-term deterioration of cardiac function after MI [195]. Inversely, stimulation of lymphangiogenesis by VEGFc treatment after MI was found to reduce fibrosis and inflammation and to improve cardiac function [195]. A peculiar CCR2low FLT3low Mφ population (L+), that renews by in situ proliferation, and secretes pro-lymphangiogenic growth factors VEGFc-d and FGF2, has been identified in a TAC model and was shown to be associated with preservation of the lymphatic network during cardiac remodeling [163] (Figure 4). The lymphatic system’s ability to recruit and transport immune cells to drain lymph nodes during pressure overload depends on LYVE-1 expression on lymphatic endothelial cells, acting as a docking receptor for hyaluronic acid-coated leukocytes [163,195]. The reduction of CCR2-dependent monocyte recruitment during TAC using a CCR2 antagonist abrogates the loss of LYVE-1 on lymphatic endothelial cells, enhances L+ Mφ proliferation, reduces fibrosis, and improves cardiac function [163] (Figure 5).
In addition, VEGF secreted by resident Mφ is a well-known key mediator of angiogenesis, e.g., in response to TAC [172,173] (Figure 4).
We have recently performed a transcriptomic analysis comparing genes expressed by Mφ isolated from early compensated (ECH) or failing (HF) hearts [141]. Interestingly, we identified panels of hypertrophy-related genes selectively regulated in ECH Mφ (Rcan1, Pik3ip1) or HF Mφ (Adam22, Tet2, Map3k2, Sik1) and thus potentially associated with compensated or failing hypertrophy remodeling, respectively. In addition, ECH Mφ were characterized by an induction of Egfr mRNA expression, whereas HF Mφ displayed upregulated Igfbp4 (insulin-like growth factor binding protein 4), a negative regulator of IGF1 signaling [141]. Such genomic or proteomic approaches may constitute the basis for future, more in-depth studies to identify important Mφ-related pathways interfering in cardiac remodeling as well as to characterize biomarkers associated with early vs. late disease progression [141,196,197,198,199].
4.2. Protective Phagocytic Activity of Cardiac Mφ
Overwhelming evidence from both preclinical and clinical studies indicates bioenergetics insufficiency in HF [200]. Thus, mitochondrial dysfunction seems to be an important target for therapy to directly improve cardiac function [200]. Interestingly, cardiac Mφ regulate myocardial homeostasis through effects on mitochondrial homeostasis [201]. MERTK expression is associated with anti-inflammatory and phagocytic Mφ functions. A recent study recently described that defective mitochondria debris are routinely ejected from cardiomyocytes as particules whose elimination is ensured by resident MERTK+ Mφ, enabling to preserve metabolic stability and ventricular function [201] (Figure 4).
With aging, cardiac cells that express senescence markers and display a so-called senescence-associated secretory phenotype (SASP) accumulate in the myocardium, [202,203]. To maintain tissue homeostasis, the removal of senescent cells in a timely manner is crucial and pharmacological senolytic treatment using navitoclax has been shown to reduce hypertrophy and fibrosis in hearts from aged mice [204]. The SASP cells secrete a complex combination of growth factors such as GDF15, proteases, chemokines such as monocyte chemoattractant protein (MCP)-1, -2 and -4 and Mφ inflammatory protein (MIP)-1a and -3a, matrix metalloproteinases, and pro-inflammatory cytokines. They perpetuate a pro-inflammatory signaling loop and play a role in their own death, promoting the recruitment of immune cells, including Mφ which function collectively to clear the senescent cells (Figure 4). However, the immune response declines with age (“immunosenescence”), and, as a result, the clearance of senescent cells is impaired [205].
4.3. Protective Signals Favoring Proliferation of Resident Mφ
In the TAC model, resident Mφ initially proliferate and support angiogenesis in a KLF4-dependent manner [165]. This process has been proposed to be driven by renal CSF2 (colony stimulating factor 2) [164,165] (Figure 4).
In contrast, in response to β adrenergic-induced cardiac remodeling, our group recently reported that an early activation of the CX3CL1/CX3CR1 axis supported cardiac resident Mφ proliferation and delayed transition to HF [5] (Figure 4). This transient beneficial impact relied on the emergence of CX3CL1- and TNFα-cosecreting resident Mφ and their crosstalk with CX3CR1-expressing cardiomyocytes, leading to compensatory concentric hypertrophy [5]. Of note, CX3CL1 has also been previously described as a proangiogenic factor [134] (Figure 4).
4.4. Exosomes, Mir and Cardiac Mφ
Paracrine intercellular communications between cardiac cell types also occur via exosomes (secreted extravesicular vesicles) and the exchange of miRNAs (small noncoding RNAs that inhibit gene expression of complementary target genes at the posttranscriptional level). For example, Mφ exosome-derived miR-155 suppresses fibroblast proliferation, decreases collagen production promoting function alteration and cardiac rupture after MI [206]. It also favors pro-inflammatory Mφ polarization and cardiac monocyte infiltration inducing hypertrophy and failure in hypertensive models [207]. Mφ exosome-derived miR-21 drives pressure overload-induced cardiac fibrosis and dysfunction [208].
In contrast, recent literature highlights the concept that M2-exosomes-derived miR-24-3p targets the TNFα superfamily member Tnfsf10 (TRAIL) to reduce myocardial injury after sepsis, improving cardiac function [209] (Figure 4).
Promising results from preclinical studies point out treatments with miRNAs or antagomir deliveries as new potential therapeutic approaches to limit HF. For example, the use of a specific miR-21 antagomir allowed researchers to achieve indefinite cardiac allograft survival abrogating chronic allograft vasculopathy. Treatment with MiR-21 antagomir also led to a reprogramming of Mφ metabolism, with a shift toward oxidative phosphorylation, resulting in an increase in M2-like Mφ [210]. Similarly, miR-21 antagomir was shown to limit inflammation and attenuate histological and echocardiographic effects of experimental autoimmune myocarditis [211].
4.5. Immune Response and Fibrosis in Aging and Myocardial Diseases
Fibrosis may reflect activation of reparative or maladaptive processes. Because the adult mammalian heart has negligible regenerative capacity, death of a large number of cardiomyocytes results in reparative fibrosis, a process that is critical for preservation of the structural integrity of the infarcted ventricle. Pathophysiologic stimuli, such as pressure overload, volume overload, metabolic dysfunction, and aging may cause interstitial and perivascular fibrosis in the absence of infarction [212]. The potential protective role of replacement fibrosis to maintain cardiac function during the first steps of aging has been documented in EMMPRIN−/− aged mice, (a matrix metalloprotease (MMP) inducer), that develop an aberrant extracellular matrix remodeling characterized by a loss of collagen deposition associated with a dilated cardiopathy as early as 12 months of age [213].
However, excessive cardiac fibrosis becomes a key driver of HF, a common pathophysiologic companion of most myocardial diseases, associated with systolic and diastolic dysfunction, aging, arrhythmogenesis, and adverse outcome [212].
For example, with aging and its associated evolution towards a low-grade oxygen environment, cardiomyocytes release pro-inflammatory cytokines and chemokines, stimulating an immune response. This leads to the increase in cardiac monocyte-derived CCR2+ Ly6Chigh Mφ [31,214,215], referred as “inflammaging” [31,162,216], promoting fibrosis (Figure 5).
Cardiac Mφ secrete stromal cell proteins and are directly involved in ECM remodeling by producing inflammatory cytokines, TGFβ, PDGF, osteopontin, MMPs, and their inhibitors. They actively participate in the process of transformation of quiescent fibroblasts to myofibroblasts [135,212,217,218]. Anti-inflammatory cytokines, e.g., IL4 mainly secreted by resident Mφ, are also associated with profibrogenic properties. In the TAC model, IL4 neutralization attenuates fibrotic changes [219]. IL4 may exert direct fibrogenic actions by stimulating collagen synthesis in cardiac fibroblasts through activation of STAT6 [220]. Data concerning IL10 are conflicting with reported anti- and pro-fibrogenic related effects. It has been suggested that the final impact of IL10 may depend on the balance between anti-inflammatory and pro-fibrotic actions. For example, during the resolution phase of injury, “resolving” Mφ can secrete IL10 that exerts protective roles against cardiac fibrosis [212].
In patients with cardiomyopathy, CCR2− Mφ seem to locate near the coronary vasculature, similarly to what has been reported for mice, whereas CCR2+ Mφ occupy fibrotic areas [161]. Cardiac-resident Mφ were reported to limit cardiac fibrosis in a pressure overload model [172] (Figure 4). Interestingly, Deniset et al. describe the pericardial cavity as an important source of resident Gata6+ Mφ that migrate into the heart, limit fibrosis of healthy myocardium, and improve functional cardiac recovery after ischemic injury, preventing detrimental repair caused by excessive fibrosis [221].
5. Future Directions
The overall analysis of the literature related to cardiac remodeling and transition to HF clearly outline the Janus nature of the inflammatory response, being either cytoprotective or detrimental, as well as the dynamic aspect of its impact. Therapeutic targeting of the NLRP3 inflammasome or of downstream IL1β signaling in patients with HF have been evaluated in clinical trials, making this pathway a promising target [222]. For example, the CANTOS study showed a significant reduction in HF-associated risk of hospitalization or HF-related mortality in patients treated with the IL1β inhibitor canakinumab [222,223]. In contrast, following the failure of global anti-TNFα strategies in HF patients, the development of novel classes of drugs selectively targeting TNFRs, e.g., selective blocking of sTNF/TNFR1 signaling which will preserve functional mTNF/TNFR2 signaling, or combination therapies using sTNF/TNFR1 antagonists together with TNFR2 agonists, might represent a novel superior therapeutic concept to treat a multitude of inflammatory and degenerative diseases including HF [224,225]. Supplementation in glutathione (with NAC) and/or inhibition of TACE activity might constitute additional valuable strategies to limit deleterious sTNF/TNFR1 signaling and promote TNFR2 pathways [72,73,101,108,226].
Cardiac Mφ are an emerging focus for therapeutic strategies aiming at strengthening adaptive responses, minimizing cardiomyocyte death, ameliorating pathological cardiac remodeling, and for treating HF [151]. Current knowledge clearly shows that the different cardiac Mφ populations are plastic, display various responses to injury, and differentially regulate inflammation and repair processes. Therapeutically, accumulating evidence indicates that strategies that will preserve or enhance the functions of CCR2− Mφ and/or limit infiltration of CCR2+ monocytes, may provide additive benefit to established medications for HF. However, from studies examining cardiac remodeling after infarction, it clearly appears that keeping a time-dependent balance in the work of different subtypes of immune cells is crucial for successful heart healing and remodeling. In fact, the maintenance of early inflammatory activity is as important as the subsequent promotion of resolution and repair mechanisms after infarction [227]. In keeping, a timely planned targeting of specific subsets of Mφ will probably be necessary to achieve beneficial results in all types of cardiac pathologies. In this context, recent studies suggest that achieving the optimal recruited monocyte/resident Mφ loading after cardiac injury represents a therapeutic opportunity that might be achieved by targeting the cardiac lymphatic system to spatiotemporally constrain the innate immune response [163,195].
Recent transcriptomic and single-cell RNA sequencing studies allowed an evaluation of the progressive reprogramming of Mφ during cardiac remodeling. This led to the uncovering of potential specific properties of Mφ isolated from early adaptive vs. late failing hearts and to identify clusters of phagocytes with distinct gene expression profiles among which some are characterized by a mixed expression of pro-inflammatory and anti-inflammatory marker-genes, further emphasizing oversimplification of Mφ categorization into M1 and M2 cells [141,196,227,228,229]. Early adaptive resident Mφ amplified in response to β-AR stimulation were characterized by an induction of anti-inflammatory, pro-phagocytic and pro-angiogenic gene markers [141]. There is accumulating evidence that growth factor secretion plays a cardinal role in their protective impact in cardiac remodeling [230,231]. One of the modern concepts is that metabolic reprogramming of immune cells is a major factor of immune modulation, with oxidative phosphorylation and glycolysis promoting anti- and pro-inflammatory profiles, respectively [232,233,234]. In response to β-AR stimulation, early adaptive resident Mφ were characterized by an enrichment in genes related to oxidative mitochondrial phosphorylation, glucose and fatty acid oxidation, lipophagy, and Arginine signaling [141]. In addition, combined transcriptomic and lipidomic results showed a typical lipid remodeling with induction of genes coding for enzymes potentially leading to AA production and eicosanoid signaling [141]. In contrast, HF Mφ presented with an enrichment in glycolysis genes [141]. Among the many avenues that are suggested, such overall analyses may constitute the basis for more in-depth studies to further identify important Mφ-related pathways interfering in cardiac remodeling and/or characterize biomarkers associated with early vs. late disease progression. Current approaches using Mφ as therapies have essentially been developed in preclinical models mainly for rheumatoid arthritis and cancer uses, but some seem promising [235]. Targeting Mφ polarization might lead to novel intervention strategies in HF.
Acknowledgments
C.P. is supported by grants from the Institute of Cardiometabolism and Nutrition (ICAN).
Abbreviations
LV: left ventricular; HF, heart failure; AF, atrial fibrillation; HFpEF, Heart failure with preserved function; HFrEF, heart failure with reduced function; TAC, transverse aortic constriction; sTNFα, soluble tumor necrosis factor α; mTNFα, membranous tumor necrosis fact α; TACE, tumor necrosis factor α converting enzyme; TNFR1, Tumor necrosis factor receptor 1; TNFR2, Tumor necrosis factor receptor 2; TRADD, TNFR1-associated death domain; FADD, Fas-associated protein with death domain; RIP1/3, Receptor interacting protein 1/3; ROS, Reactive oxygen species; MLKL, Mixed lineage kinase domain like pseudokinase; MAPK, Mitogen-activated protein kinase; JNK, c-Jun N-terminal kinases; TRAF2, TNFR-associated factor 2; JAK, Janus kinase; ETK, Epithelial and endothelial tyrosine kinase; PI3K, Phosphoinositide 3 kinase; Akt, proteine kinase B; GSK3β, glycogen synthase kinase 3 β; STAT3, Signal transducer and activator of transcription 3; CX3CL1, Fractalkine; GSH, Glutathione; ROS, Reactive oxygen species; FAN, Factor associated with neutral sphingomyelinase activation; N-Smase, Neutral sphingomyelinase; RASSF1, Ras Association Domain Family Member 1; cPLA2, cytosolic phospholipase A2; AA, Arachidonic acid; LOX, Lipoxygenase, PI3K, Phosphoinosisitde 3 kinase; Akt, Proteine kinase B; ERK, Extracellular signal-regulated kinase; MSK1, Mitogen- and stress-activated kinase 1; CamKII, Calmoduline kinase II; PKC, Protein kinase C; Pi-PLB, Phosphorylated phospholamban; SAFE; CCR2, C-C motif chemokine receptor 2; Ly6c, lymphocyte antigen 6 complex; Ly6c, lymphocyte antigen 6 complex; IL4, Interleukin 4; IL10, Interleukin 10; GDF15, growth differentiation factors 15; KLF4, Kruppel-like factor 4; MERTK, myeloid-epithelial-reproductive tyrosine kinase; MDGF, myeloid derived growth factor; IGF1, insulin-like growth factor-1; TGFβ, Transforming growth factor β; MMPs, metalloproteinases; PDGF, Platelet-derived growth factor; VEGF, Vascular endothelial growth factor; FGF2, fibroblast growth factor 2; AREG, Amphiregulin; EGFR, Epidermal Growth Factor receptor; Cnx43, Connexin 43.
Author Contributions
S.B., S.N., E.B. and C.P. participated in writing the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Verma A., Meris A., Skali H., Ghali J.K., Arnold J.M.O., Bourgoun M., Velazquez E.J., McMurray J.J.V., Kober L., Pfeffer M.A., et al. Prognostic Implications of Left Ventricular Mass and Geometry Following Myocardial Infarction: The VALIANT (VALsartan in Acute Myocardial INfarcTion) Echocardiographic Study. JACC Cardiovas. Imaging. 2008;1:582–591. doi: 10.1016/j.jcmg.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Mann D.L. Stress-Activated Cytokines and the Heart: From Adaptation to Maladaptation. Annu. Rev. Physiol. 2003;65:81–101. doi: 10.1146/annurev.physiol.65.092101.142249. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura M., Sadoshima J. Mechanisms of Physiological and Pathological Cardiac Hypertrophy. Nat. Rev. Cardiol. 2018;15:387–407. doi: 10.1038/s41569-018-0007-y. [DOI] [PubMed] [Google Scholar]
- 4.Sasayama S., Ross J., Franklin D., Bloor C.M., Bishop S., Dilley R.B. Adaptations of the Left Ventricle to Chronic Pressure Overload. Circ. Res. 1976;38:172–178. doi: 10.1161/01.RES.38.3.172. [DOI] [PubMed] [Google Scholar]
- 5.Flamant M., Mougenot N., Balse E., Le Fèvre L., Atassi F., Gautier E.L., Le Goff W., Keck M., Nadaud S., Combadière C., et al. Early Activation of the Cardiac CX3CL1/CX3CR1 Axis Delays β-Adrenergic-Induced Heart Failure. Sci. Rep. 2021;11:17982. doi: 10.1038/s41598-021-97493-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lieb W., Gona P., Larson M.G., Aragam J., Zile M.R., Cheng S., Benjamin E.J., Vasan R.S. The Natural History of Left Ventricular Geometry in the Community: Clinical Correlates and Prognostic Significance of Change in LV Geometric Pattern. JACC Cardiovasc. Imaging. 2014;7:870–878. doi: 10.1016/j.jcmg.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai R.V., Ahmed M.I., Marjan M., Aban I.B., Zile M.R., Ahmed A. Natural History of Concentric Left Ventricular Geometry in Community-Dwelling Older Adults without Heart Failure during Seven Years of Follow-Up. Am. J. Cardiol. 2011;107:321–324. doi: 10.1016/j.amjcard.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maillet M., van Berlo J.H., Molkentin J.D. Molecular Basis of Physiological Heart Growth: Fundamental Concepts and New Players. Nat. Rev. Mol. Cell Biol. 2013;14:38–48. doi: 10.1038/nrm3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haider A.W., Larson M.G., Benjamin E.J., Levy D. Increased Left Ventricular Mass and Hypertrophy Are Associated with Increased Risk for Sudden Death. J. Am. Coll. Cardiol. 1998;32:1454–1459. doi: 10.1016/S0735-1097(98)00407-0. [DOI] [PubMed] [Google Scholar]
- 10.Katz A.M. Maladaptive Growth in the Failing Heart: The Cardiomyopathy of Overload. Cardiovasc. Drugs Ther. 2002;16:245–249. doi: 10.1023/A:1020604623427. [DOI] [PubMed] [Google Scholar]
- 11.Heineke J., Molkentin J.D. Regulation of Cardiac Hypertrophy by Intracellular Signalling Pathways. Nat. Rev. Mol. Cell Biol. 2006;7:589–600. doi: 10.1038/nrm1983. [DOI] [PubMed] [Google Scholar]
- 12.Meng G., Liu J., Liu S., Song Q., Liu L., Xie L., Han Y., Ji Y. Hydrogen Sulfide Pretreatment Improves Mitochondrial Function in Myocardial Hypertrophy via a SIRT3-Dependent Manner. Br. J. Pharmacol. 2018;175:1126–1145. doi: 10.1111/bph.13861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakayama H., Nishida K., Otsu K. Macromolecular Degradation Systems and Cardiovascular Aging. Circ. Res. 2016;118:1577–1592. doi: 10.1161/CIRCRESAHA.115.307495. [DOI] [PubMed] [Google Scholar]
- 14.Van de Veire N.R., De Backer J., Ascoop A.-K., Middernacht B., Velghe A., Sutter J.D. Echocardiographically Estimated Left Ventricular End-Diastolic and Right Ventricular Systolic Pressure in Normotensive Healthy Individuals. Int. J. Cardiovasc. Imaging. 2006;22:633–641. doi: 10.1007/s10554-006-9082-y. [DOI] [PubMed] [Google Scholar]
- 15.Garciarena C.D., Pinilla O.A., Nolly M.B., Laguens R.P., Escudero E.M., Cingolani H.E., Ennis I.L. Endurance Training in the Spontaneously Hypertensive Rat: Conversion of Pathological into Physiological Cardiac Hypertrophy. Hypertension. 2009;53:708–714. doi: 10.1161/HYPERTENSIONAHA.108.126805. [DOI] [PubMed] [Google Scholar]
- 16.Feng L., Li G., An J., Liu C., Zhu X., Xu Y., Gao Y., Li J., Liu J., Yan J., et al. Exercise Training Protects Against Heart Failure Via Expansion of Myeloid-Derived Suppressor Cells Through Regulating IL-10/STAT3/S100A9 Pathway. Circ. Heart Fail. 2021;15:e008550. doi: 10.1161/CIRCHEARTFAILURE.121.008550. [DOI] [PubMed] [Google Scholar]
- 17.Sharma K., Kass D.A. Heart Failure with Preserved Ejection Fraction: Mechanisms, Clinical Features, and Therapies. Circ. Res. 2014;115:79–96. doi: 10.1161/CIRCRESAHA.115.302922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keller K.M., Howlett S.E. Sex Differences in the Biology and Pathology of the Aging Heart. Can. J. Cardiol. 2016;32:1065–1073. doi: 10.1016/j.cjca.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Hanna A., Frangogiannis N.G. Inflammatory Cytokines and Chemokines as Therapeutic Targets in Heart Failure. Cardiovasc. Drugs Ther. 2020;34:849–863. doi: 10.1007/s10557-020-07071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dick S.A., Epelman S. Chronic Heart Failure and Inflammation: What Do We Really Know? Circ. Res. 2016;119:159–176. doi: 10.1161/CIRCRESAHA.116.308030. [DOI] [PubMed] [Google Scholar]
- 21.Frangogiannis N.G. The Immune System and Cardiac Repair. Pharmacol. Res. 2008;58:88–111. doi: 10.1016/j.phrs.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hein S., Arnon E., Kostin S., Schönburg M., Elsässer A., Polyakova V., Bauer E.P., Klövekorn W.-P., Schaper J. Progression from Compensated Hypertrophy to Failure in the Pressure-Overloaded Human Heart: Structural Deterioration and Compensatory Mechanisms. Circulation. 2003;107:984–991. doi: 10.1161/01.CIR.0000051865.66123.B7. [DOI] [PubMed] [Google Scholar]
- 23.Balakumar P., Jagadeesh G. Multifarious Molecular Signaling Cascades of Cardiac Hypertrophy: Can the Muddy Waters Be Cleared? Pharmacol. Res. 2010;62:365–383. doi: 10.1016/j.phrs.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Crozatier B., Ventura-Clapier R. Inhibition of Hypertrophy, per Se, May Not Be a Good Therapeutic Strategy in Ventricular Pressure Overload: Other Approaches Could Be More Beneficial. Circulation. 2015;131:1448–1457. doi: 10.1161/CIRCULATIONAHA.114.013895. [DOI] [PubMed] [Google Scholar]
- 25.Shah S.J., Borlaug B.A., Kitzman D.W., McCulloch A.D., Blaxall B.C., Agarwal R., Chirinos J.A., Collins S., Deo R.C., Gladwin M.T., et al. Research Priorities for Heart Failure with Preserved Ejection Fraction: National Heart, Lung, and Blood Institute Working Group Summary. Circulation. 2020;141:1001–1026. doi: 10.1161/CIRCULATIONAHA.119.041886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levine B., Kalman J., Mayer L., Fillit H.M., Packer M. Elevated Circulating Levels of Tumor Necrosis Factor in Severe Chronic Heart Failure. N. Engl. J. Med. 1990;323:236–241. doi: 10.1056/NEJM199007263230405. [DOI] [PubMed] [Google Scholar]
- 27.Mann D.L. Innate Immunity and the Failing Heart: The Cytokine Hypothesis Revisited. Circ. Res. 2015;116:1254–1268. doi: 10.1161/CIRCRESAHA.116.302317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suetomi T., Willeford A., Brand C.S., Cho Y., Ross R.S., Miyamoto S., Brown J.H. Inflammation and NLRP3 Inflammasome Activation Initiated in Response to Pressure Overload by Ca2+/Calmodulin-Dependent Protein Kinase II δ Signaling in Cardiomyocytes Are Essential for Adverse Cardiac Remodeling. Circulation. 2018;138:2530–2544. doi: 10.1161/CIRCULATIONAHA.118.034621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao M., Zhang J., Xu Y., Liu J., Ye J., Wang Z., Ye D., Feng Y., Xu S., Pan W., et al. Selective Inhibition of NLRP3 Inflammasome Reverses Pressure Overload-Induced Pathological Cardiac Remodeling by Attenuating Hypertrophy, Fibrosis, and Inflammation. Int. Immunopharmacol. 2021;99:108046. doi: 10.1016/j.intimp.2021.108046. [DOI] [PubMed] [Google Scholar]
- 30.Li H., Hastings M.H., Rhee J., Trager L.E., Roh J.D., Rosenzweig A. Targeting Age-Related Pathways in Heart Failure. Circ. Res. 2020;126:533–551. doi: 10.1161/CIRCRESAHA.119.315889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meschiari C.A., Ero O.K., Pan H., Finkel T., Lindsey M.L. The Impact of Aging on Cardiac Extracellular Matrix. Geroscience. 2017;39:7–18. doi: 10.1007/s11357-017-9959-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J., Xia S., Kalionis B., Wan W., Sun T. The Role of Oxidative Stress and Inflammation in Cardiovascular Aging. BioMed Res. Int. 2014;2014:615312. doi: 10.1155/2014/615312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Izzo C., Vitillo P., Di Pietro P., Visco V., Strianese A., Virtuoso N., Ciccarelli M., Galasso G., Carrizzo A., Vecchione C. The Role of Oxidative Stress in Cardiovascular Aging and Cardiovascular Diseases. Life. 2021;11:60. doi: 10.3390/life11010060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kubota T., McTiernan C.F., Frye C.S., Slawson S.E., Lemster B.H., Koretsky A.P., Demetris A.J., Feldman A.M. Dilated Cardiomyopathy in Transgenic Mice with Cardiac-Specific Overexpression of Tumor Necrosis Factor-Alpha. Circ. Res. 1997;81:627–635. doi: 10.1161/01.RES.81.4.627. [DOI] [PubMed] [Google Scholar]
- 35.Bryant D., Becker L., Richardson J., Shelton J., Franco F., Peshock R., Thompson M., Giroir B. Cardiac Failure in Transgenic Mice with Myocardial Expression of Tumor Necrosis Factor-Alpha. Circulation. 1998;97:1375–1381. doi: 10.1161/01.CIR.97.14.1375. [DOI] [PubMed] [Google Scholar]
- 36.Sivasubramanian N., Coker M.L., Kurrelmeyer K.M., MacLellan W.R., DeMayo F.J., Spinale F.G., Mann D.L. Left Ventricular Remodeling in Transgenic Mice with Cardiac Restricted Overexpression of Tumor Necrosis Factor. Circulation. 2001;104:826–831. doi: 10.1161/hc3401.093154. [DOI] [PubMed] [Google Scholar]
- 37.Franco F., Thomas G.D., Giroir B., Bryant D., Bullock M.C., Chwialkowski M.C., Victor R.G., Peshock R.M. Magnetic Resonance Imaging and Invasive Evaluation of Development of Heart Failure in Transgenic Mice with Myocardial Expression of Tumor Necrosis Factor-Alpha. Circulation. 1999;99:448–454. doi: 10.1161/01.CIR.99.3.448. [DOI] [PubMed] [Google Scholar]
- 38.Machida Y., Kubota T., Kawamura N., Funakoshi H., Ide T., Utsumi H., Li Y.Y., Feldman A.M., Tsutsui H., Shimokawa H., et al. Overexpression of Tumor Necrosis Factor-Alpha Increases Production of Hydroxyl Radical in Murine Myocardium. Am. J. Physiol. Heart Circ. Physiol. 2003;284:H449–H455. doi: 10.1152/ajpheart.00581.2002. [DOI] [PubMed] [Google Scholar]
- 39.Engel D., Peshock R., Armstong R.C., Sivasubramanian N., Mann D.L. Cardiac Myocyte Apoptosis Provokes Adverse Cardiac Remodeling in Transgenic Mice with Targeted TNF Overexpression. Am. J. Physiol. Heart Circ. Physiol. 2004;287:H1303–H1311. doi: 10.1152/ajpheart.00053.2004. [DOI] [PubMed] [Google Scholar]
- 40.Meldrum D.R. Tumor Necrosis Factor in the Heart. Am. J. Physiol. 1998;274:R577–R595. doi: 10.1152/ajpregu.1998.274.3.R577. [DOI] [PubMed] [Google Scholar]
- 41.Dutka D.P., Elborn J.S., Delamere F., Shale D.J., Morris G.K. Tumour Necrosis Factor Alpha in Severe Congestive Cardiac Failure. Br. Heart J. 1993;70:141–143. doi: 10.1136/hrt.70.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matsumori A., Yamada T., Suzuki H., Matoba Y., Sasayama S. Increased Circulating Cytokines in Patients with Myocarditis and Cardiomyopathy. Br. Heart J. 1994;72:561–566. doi: 10.1136/hrt.72.6.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Torre-Amione G., Kapadia S., Benedict C., Oral H., Young J.B., Mann D.L. Proinflammatory Cytokine Levels in Patients with Depressed Left Ventricular Ejection Fraction: A Report from the Studies of Left Ventricular Dysfunction (SOLVD) J. Am. Coll. Cardiol. 1996;27:1201–1206. doi: 10.1016/0735-1097(95)00589-7. [DOI] [PubMed] [Google Scholar]
- 44.Seta Y., Shan K., Bozkurt B., Oral H., Mann D.L. Basic Mechanisms in Heart Failure: The Cytokine Hypothesis. J. Card. Fail. 1996;2:243–249. doi: 10.1016/S1071-9164(96)80047-9. [DOI] [PubMed] [Google Scholar]
- 45.Sun M., Chen M., Dawood F., Zurawska U., Li J.Y., Parker T., Kassiri Z., Kirshenbaum L.A., Arnold M., Khokha R., et al. Tumor Necrosis Factor-Alpha Mediates Cardiac Remodeling and Ventricular Dysfunction after Pressure Overload State. Circulation. 2007;115:1398–1407. doi: 10.1161/CIRCULATIONAHA.106.643585. [DOI] [PubMed] [Google Scholar]
- 46.Mann D.L., McMurray J.J.V., Packer M., Swedberg K., Borer J.S., Colucci W.S., Djian J., Drexler H., Feldman A., Kober L., et al. Targeted Anticytokine Therapy in Patients with Chronic Heart Failure: Results of the Randomized Etanercept Worldwide Evaluation (RENEWAL) Circulation. 2004;109:1594–1602. doi: 10.1161/01.CIR.0000124490.27666.B2. [DOI] [PubMed] [Google Scholar]
- 47.Chung E.S., Packer M., Lo K.H., Fasanmade A.A., Willerson J.T. Anti-TNF Therapy against Congestive Heart Failure Investigators Randomized, Double-Blind, Placebo-Controlled, Pilot Trial of Infliximab, a Chimeric Monoclonal Antibody to Tumor Necrosis Factor-Alpha, in Patients with Moderate-to-Severe Heart Failure: Results of the Anti-TNF Therapy against Congestive Heart Failure (ATTACH) Trial. Circulation. 2003;107:3133–3140. doi: 10.1161/01.CIR.0000077913.60364.D2. [DOI] [PubMed] [Google Scholar]
- 48.Anker S.D., Coats A.J.S. How to RECOVER from RENAISSANCE? The Significance of the Results of RECOVER, RENAISSANCE, RENEWAL and ATTACH. Int. J. Cardiol. 2002;86:123–130. doi: 10.1016/S0167-5273(02)00470-9. [DOI] [PubMed] [Google Scholar]
- 49.Mann D.L. Inflammatory Mediators and the Failing Heart: Past, Present, and the Foreseeable Future. Circ. Res. 2002;91:988–998. doi: 10.1161/01.RES.0000043825.01705.1B. [DOI] [PubMed] [Google Scholar]
- 50.Mann D.L. The Effect of Tumor Necrosis Factor-Alpha on Cardiac Structure and Function: A Tale of Two Cytokines. J. Card. Fail. 1996;2:S165–S172. doi: 10.1016/S1071-9164(96)80073-X. [DOI] [PubMed] [Google Scholar]
- 51.Sack M. Tumor Necrosis Factor-Alpha in Cardiovascular Biology and the Potential Role for Anti-Tumor Necrosis Factor-Alpha Therapy in Heart Disease. Pharmacol. Ther. 2002;94:123–135. doi: 10.1016/S0163-7258(02)00176-6. [DOI] [PubMed] [Google Scholar]
- 52.Hajjar R.J., Leopold J.A. Inflammation and Heart Failure: Friend or Foe? Circulation. 2021;144:1241–1243. doi: 10.1161/CIRCULATIONAHA.121.056628. [DOI] [PubMed] [Google Scholar]
- 53.Adamo L., Rocha-Resende C., Prabhu S.D., Mann D.L. Reappraising the Role of Inflammation in Heart Failure. Nat. Rev. Cardiol. 2020;17:269–285. doi: 10.1038/s41569-019-0315-x. [DOI] [PubMed] [Google Scholar]
- 54.Vanderheyden M., Paulus W.J., Voss M., Knuefermann P., Sivasubramanian N., Mann D., Baumgarten G. Myocardial Cytokine Gene Expression Is Higher in Aortic Stenosis than in Idiopathic Dilated Cardiomyopathy. Heart. 2005;91:926–931. doi: 10.1136/hrt.2004.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Norton G.R., Peterson V.R., Robinson C., Norman G., Libhaber C.D., Libhaber E., Gomes M., Sareli P., Woodiwiss A.J. Independent of Left Ventricular Mass, Circulating Inflammatory Markers Rather than Pressure Load Are Associated with Concentric Left Ventricular Remodelling. Int. J. Cardiol. 2019;274:342–347. doi: 10.1016/j.ijcard.2018.09.059. [DOI] [PubMed] [Google Scholar]
- 56.Carswell E.A., Old L.J., Kassel R.L., Green S., Fiore N., Williamson B. An Endotoxin-Induced Serum Factor That Causes Necrosis of Tumors. Proc. Natl. Acad. Sci. USA. 1975;72:3666–3670. doi: 10.1073/pnas.72.9.3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Torre-Amione G., Kapadia S., Lee J., Bies R.D., Lebovitz R., Mann D.L. Expression and Functional Significance of Tumor Necrosis Factor Receptors in Human Myocardium. Circulation. 1995;92:1487–1493. doi: 10.1161/01.CIR.92.6.1487. [DOI] [PubMed] [Google Scholar]
- 58.Grell M., Douni E., Wajant H., Löhden M., Clauss M., Maxeiner B., Georgopoulos S., Lesslauer W., Kollias G., Pfizenmaier K., et al. The Transmembrane Form of Tumor Necrosis Factor Is the Prime Activating Ligand of the 80 KDa Tumor Necrosis Factor Receptor. Cell. 1995;83:793–802. doi: 10.1016/0092-8674(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 59.Borghi A., Verstrepen L., Beyaert R. TRAF2 Multitasking in TNF Receptor-Induced Signaling to NF-ΚB, MAP Kinases and Cell Death. Biochem. Pharmacol. 2016;116:9. doi: 10.1016/j.bcp.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 60.Gough P., Myles I.A. Tumor Necrosis Factor Receptors: Pleiotropic Signaling Complexes and Their Differential Effects. Front. Immunol. 2020;11:585880. doi: 10.3389/fimmu.2020.585880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schumacher S.M., Naga Prasad S.V. Tumor Necrosis Factor-α in Heart Failure: An Updated Review. Curr. Cardiol. Rep. 2018;20:117. doi: 10.1007/s11886-018-1067-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zee K.J.V., Kohno T., Fischer E., Rock C.S., Moldawer L.L., Lowry S.F. Tumor Necrosis Factor Soluble Receptors Circulate during Experimental and Clinical Inflammation and Can Protect against Excessive Tumor Necrosis Factor Alpha In Vitro and In Vivo. Proc. Natl. Acad. Sci. USA. 1992;89:4845–4849. doi: 10.1073/pnas.89.11.4845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yokoyama T., Nakano M., Bednarczyk J.L., McIntyre B.W., Entman M., Mann D.L. Tumor Necrosis Factor-Alpha Provokes a Hypertrophic Growth Response in Adult Cardiac Myocytes. Circulation. 1997;95:1247–1252. doi: 10.1161/01.CIR.95.5.1247. [DOI] [PubMed] [Google Scholar]
- 64.Sekiguchi K., Li X., Coker M., Flesch M., Barger P.M., Sivasubramanian N., Mann D.L. Cross-Regulation between the Renin-Angiotensin System and Inflammatory Mediators in Cardiac Hypertrophy and Failure. Cardiovasc. Res. 2004;63:433–442. doi: 10.1016/j.cardiores.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 65.Higuchi Y., Otsu K., Nishida K., Hirotani S., Nakayama H., Yamaguchi O., Matsumura Y., Ueno H., Tada M., Hori M. Involvement of Reactive Oxygen Species-Mediated NF- κ B Activation in TNF- α -Induced Cardiomyocyte Hypertrophy. J. Mol. Cell. Cardiol. 2002;34:233–240. doi: 10.1006/jmcc.2001.1505. [DOI] [PubMed] [Google Scholar]
- 66.Nakamura K., Fushimi K., Kouchi H., Mihara K., Miyazaki M., Ohe T., Namba M. Inhibitory Effects of Antioxidants on Neonatal Rat Cardiac Myocyte Hypertrophy Induced by Tumor Necrosis Factor-Alpha and Angiotensin II. Circulation. 1998;98:794–799. doi: 10.1161/01.CIR.98.8.794. [DOI] [PubMed] [Google Scholar]
- 67.Condorelli G., Morisco C., Latronico M.V.G., Claudio P.P., Dent P., Tsichlis P., Condorelli G., Frati G., Drusco A., Croce C.M., et al. TNF-Alpha Signal Transduction in Rat Neonatal Cardiac Myocytes: Definition of Pathways Generating from the TNF-Alpha Receptor. FASEB J. 2002;16:1732–1737. doi: 10.1096/fj.02-0419com. [DOI] [PubMed] [Google Scholar]
- 68.Higuchi Y., McTiernan C.F., Frye C.B., McGowan B.S., Chan T.O., Feldman A.M. Tumor Necrosis Factor Receptors 1 and 2 Differentially Regulate Survival, Cardiac Dysfunction, and Remodeling in Transgenic Mice with Tumor Necrosis Factor-Alpha-Induced Cardiomyopathy. Circulation. 2004;109:1892–1897. doi: 10.1161/01.CIR.0000124227.00670.AB. [DOI] [PubMed] [Google Scholar]
- 69.Li Y.Y., Feng Y.Q., Kadokami T., McTiernan C.F., Draviam R., Watkins S.C., Feldman A.M. Myocardial Extracellular Matrix Remodeling in Transgenic Mice Overexpressing Tumor Necrosis Factor Alpha Can Be Modulated by Anti-Tumor Necrosis Factor Alpha Therapy. Proc. Natl. Acad. Sci. USA. 2000;97:12746–12751. doi: 10.1073/pnas.97.23.12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dibbs Z.I., Diwan A., Nemoto S., DeFreitas G., Abdellatif M., Carabello B.A., Spinale F.G., Feuerstein G., Sivasubramanian N., Mann D.L. Targeted Overexpression of Transmembrane Tumor Necrosis Factor Provokes a Concentric Cardiac Hypertrophic Phenotype. Circulation. 2003;108:1002–1008. doi: 10.1161/01.CIR.0000085203.46621.F4. [DOI] [PubMed] [Google Scholar]
- 71.Diwan A., Dibbs Z., Nemoto S., DeFreitas G., Carabello B.A., Sivasubramanian N., Wilson E.M., Spinale F.G., Mann D.L. Targeted Overexpression of Noncleavable and Secreted Forms of Tumor Necrosis Factor Provokes Disparate Cardiac Phenotypes. Circulation. 2004;109:262–268. doi: 10.1161/01.CIR.0000109642.27985.FA. [DOI] [PubMed] [Google Scholar]
- 72.Miao K., Zhou L., Ba H., Li C., Gu H., Yin B., Wang J., Yang X.-P., Li Z., Wang D.W. Transmembrane Tumor Necrosis Factor Alpha Attenuates Pressure-Overload Cardiac Hypertrophy via Tumor Necrosis Factor Receptor 2. PLoS Biol. 2020;18:e3000967. doi: 10.1371/journal.pbio.3000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dittrich G.M., Heineke J. TNF-α Signaling: TACE Inhibition to Put out the Burning Heart. PLoS Biol. 2020;18:e3001037. doi: 10.1371/journal.pbio.3001037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Garlie J.B., Hamid T., Gu Y., Ismahil M.A., Chandrasekar B., Prabhu S.D. Tumor Necrosis Factor Receptor 2 Signaling Limits Beta-Adrenergic Receptor-Mediated Cardiac Hypertrophy In Vivo. Basic Res. Cardiol. 2011;106:1193–1205. doi: 10.1007/s00395-011-0196-6. [DOI] [PubMed] [Google Scholar]
- 75.Chan T.O., Tsichlis P.N. PDK2: A Complex Tail in One Akt. Sci. STKE. 2001;2001:pe1. doi: 10.1126/stke.2001.66.pe1. [DOI] [PubMed] [Google Scholar]
- 76.Capetanaki Y., Papathanasiou S., Diokmetzidou A., Vatsellas G., Tsikitis M. Desmin Related Disease: A Matter of Cell Survival Failure. Curr. Opin. Cell Biol. 2015;32:113–120. doi: 10.1016/j.ceb.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Panagopoulou P., Davos C.H., Milner D.J., Varela E., Cameron J., Mann D.L., Capetanaki Y. Desmin Mediates TNF-Alpha-Induced Aggregate Formation and Intercalated Disk Reorganization in Heart Failure. J. Cell Biol. 2008;181:761–775. doi: 10.1083/jcb.200710049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Papathanasiou S., Rickelt S., Soriano M.E., Schips T.G., Maier H.J., Davos C.H., Varela A., Kaklamanis L., Mann D.L., Capetanaki Y. Tumor Necrosis Factor-α Confers Cardioprotection through Ectopic Expression of Keratins K8 and K18. Nat. Med. 2015;21:1076–1084. doi: 10.1038/nm.3925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bartekova M., Radosinska J., Jelemensky M., Dhalla N.S. Role of Cytokines and Inflammation in Heart Function during Health and Disease. Heart Fail. Rev. 2018;23:733–758. doi: 10.1007/s10741-018-9716-x. [DOI] [PubMed] [Google Scholar]
- 80.Gordon J.W., Shaw J.A., Kirshenbaum L.A. Multiple Facets of NF-ΚB in the Heart. Circ. Res. 2011;108:1122–1132. doi: 10.1161/CIRCRESAHA.110.226928. [DOI] [PubMed] [Google Scholar]
- 81.Regula K.M., Baetz D., Kirshenbaum L.A. Nuclear Factor-KappaB Represses Hypoxia-Induced Mitochondrial Defects and Cell Death of Ventricular Myocytes. Circulation. 2004;110:3795–3802. doi: 10.1161/01.CIR.0000150537.59754.55. [DOI] [PubMed] [Google Scholar]
- 82.Huang H., Joseph L.C., Gurin M.I., Thorp E.B., Morrow J.P. Extracellular Signal-Regulated Kinase Activation during Cardiac Hypertrophy Reduces Sarcoplasmic/Endoplasmic Reticulum Calcium ATPase 2 (SERCA2) Transcription. J. Mol. Cell. Cardiol. 2014;75:58–63. doi: 10.1016/j.yjmcc.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Forman K., Vara E., García C., Kireev R., Cuesta S., Acuña-Castroviejo D., Tresguerres J.A.F. Influence of Aging and Growth Hormone on Different Members of the NFkB Family and IkB Expression in the Heart from a Murine Model of Senescence-Accelerated Aging. Exp. Gerontol. 2016;73:114–120. doi: 10.1016/j.exger.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 84.Helenius M., Hänninen M., Lehtinen S.K., Salminen A. Aging-Induced up-Regulation of Nuclear Binding Activities of Oxidative Stress Responsive NF-KB Transcription Factor in Mouse Cardiac Muscle. J. Mol. Cell. Cardiol. 1996;28:487–498. doi: 10.1006/jmcc.1996.0045. [DOI] [PubMed] [Google Scholar]
- 85.Wang X., Li X., Ong H., Tan T., Park K.H., Bian Z., Zou X., Haggard E., Janssen P.M., Merritt R.E., et al. MG53 Suppresses NF-ΚB Activation to Mitigate Age-Related Heart Failure. JCI Insight. 2021;6:148375. doi: 10.1172/jci.insight.148375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Qu Y.-C., Du Y.-M., Wu S.-L., Chen Q.-X., Wu H.-L., Zhou S.-F. Activated Nuclear Factor-KappaB and Increased Tumor Necrosis Factor-Alpha in Atrial Tissue of Atrial Fibrillation. Scand. Cardiovasc. J. 2009;43:292–297. doi: 10.1080/14017430802651803. [DOI] [PubMed] [Google Scholar]
- 87.Mishra A., Srivastava A., Mittal T., Garg N., Mittal B. Role of Inflammatory Gene Polymorphisms in Left Ventricular Dysfunction (LVD) Susceptibility in Coronary Artery Disease (CAD) Patients. Cytokine. 2013;61:856–861. doi: 10.1016/j.cyto.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 88.Santos D.G.B., Resende M.F., Mill J.G., Mansur A.J., Krieger J.E., Pereira A.C. Nuclear Factor (NF) KappaB Polymorphism Is Associated with Heart Function in Patients with Heart Failure. BMC Med. Genet. 2010;11:89. doi: 10.1186/1471-2350-11-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chandrasekar B., Colston J.T., de la Rosa S.D., Rao P.P., Freeman G.L. TNF-Alpha and H2O2 Induce IL-18 and IL-18R Beta Expression in Cardiomyocytes via NF-Kappa B Activation. Biochem. Biophys. Res. Commun. 2003;303:1152–1158. doi: 10.1016/S0006-291X(03)00496-0. [DOI] [PubMed] [Google Scholar]
- 90.Lecour S., James R.W. When Are Pro-Inflammatory Cytokines SAFE in Heart Failure? Eur. Heart J. 2011;32:680–685. doi: 10.1093/eurheartj/ehq484. [DOI] [PubMed] [Google Scholar]
- 91.Evans S., Tzeng H.-P., Veis D.J., Matkovich S., Weinheimer C., Kovacs A., Barger P.M., Mann D.L. TNF Receptor–Activated Factor 2 Mediates Cardiac Protection through Noncanonical NF-ΚB Signaling. JCI Insight. 2018;3:e98278. doi: 10.1172/jci.insight.98278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Amgalan D., Chen Y., Kitsis R.N. Death Receptor Signaling in the Heart: Cell Survival, Apoptosis, and Necroptosis. Circulation. 2017;136:743–746. doi: 10.1161/CIRCULATIONAHA.117.029566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Guo X., Yin H., Li L., Chen Y., Li J., Doan J., Steinmetz R., Liu Q. Cardioprotective Role of Tumor Necrosis Factor Receptor-Associated Factor 2 by Suppressing Apoptosis and Necroptosis. Circulation. 2017;136:729–742. doi: 10.1161/CIRCULATIONAHA.116.026240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang K.-C., Ma X., Liu H., Murphy J., Barger P.M., Mann D.L., Diwan A. Tumor Necrosis Factor Receptor-Associated Factor 2 Mediates Mitochondrial Autophagy. Circ. Heart Fail. 2015;8:175–187. doi: 10.1161/CIRCHEARTFAILURE.114.001635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mehra V.C., Ramgolam V.S., Bender J.R. Cytokines and Cardiovascular Disease. J. Leukoc. Biol. 2005;78:805–818. doi: 10.1189/jlb.0405182. [DOI] [PubMed] [Google Scholar]
- 96.Prabhu S.D. Cytokine-Induced Modulation of Cardiac Function. Circ. Res. 2004;95:1140–1153. doi: 10.1161/01.RES.0000150734.79804.92. [DOI] [PubMed] [Google Scholar]
- 97.Yokoyama T., Vaca L., Rossen R.D., Durante W., Hazarika P., Mann D.L. Cellular Basis for the Negative Inotropic Effects of Tumor Necrosis Factor-Alpha in the Adult Mammalian Heart. J. Clin. Investig. 1993;92:2303–2312. doi: 10.1172/JCI116834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Suematsu N., Tsutsui H., Wen J., Kang D., Ikeuchi M., Ide T., Hayashidani S., Shiomi T., Kubota T., Hamasaki N., et al. Oxidative Stress Mediates Tumor Necrosis Factor-Alpha-Induced Mitochondrial DNA Damage and Dysfunction in Cardiac Myocytes. Circulation. 2003;107:1418–1423. doi: 10.1161/01.CIR.0000055318.09997.1F. [DOI] [PubMed] [Google Scholar]
- 99.Liu B., Andrieu-Abadie N., Levade T., Zhang P., Obeid L.M., Hannun Y.A. Glutathione Regulation of Neutral Sphingomyelinase in Tumor Necrosis Factor-Alpha-Induced Cell Death. J. Biol. Chem. 1998;273:11313–11320. doi: 10.1074/jbc.273.18.11313. [DOI] [PubMed] [Google Scholar]
- 100.Oral H., Dorn G.W., Mann D.L. Sphingosine Mediates the Immediate Negative Inotropic Effects of Tumor Necrosis Factor-Alpha in the Adult Mammalian Cardiac Myocyte. J. Biol. Chem. 1997;272:4836–4842. doi: 10.1074/jbc.272.8.4836. [DOI] [PubMed] [Google Scholar]
- 101.Defer N., Azroyan A., Pecker F., Pavoine C. TNFR1 and TNFR2 Signaling Interplay in Cardiac Myocytes. J. Biol. Chem. 2007;282:35564–35573. doi: 10.1074/jbc.M704003200. [DOI] [PubMed] [Google Scholar]
- 102.Cailleret M., Amadou A., Andrieu-Abadie N., Nawrocki A., Adamy C., Ait-Mamar B., Rocaries F., Best-Belpomme M., Levade T., Pavoine C., et al. N-Acetylcysteine Prevents the Deleterious Effect of Tumor Necrosis Factor-(Alpha) on Calcium Transients and Contraction in Adult Rat Cardiomyocytes. Circulation. 2004;109:406–411. doi: 10.1161/01.CIR.0000109499.00587.FF. [DOI] [PubMed] [Google Scholar]
- 103.Mohamed T.M.A., Zi M., Prehar S., Maqsood A., Abou-Leisa R., Nguyen L., Pfeifer G.P., Cartwright E.J., Neyses L., Oceandy D. The Tumour Suppressor Ras-Association Domain Family Protein 1A (RASSF1A) Regulates TNF-α Signalling in Cardiomyocytes. Cardiovasc. Res. 2014;103:47–59. doi: 10.1093/cvr/cvu111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Murray D.R., Freeman G.L. Tumor Necrosis Factor-Alpha Induces a Biphasic Effect on Myocardial Contractility in Conscious Dogs. Circ. Res. 1996;78:154–160. doi: 10.1161/01.RES.78.1.154. [DOI] [PubMed] [Google Scholar]
- 105.Pagani F.D., Baker L.S., Hsi C., Knox M., Fink M.P., Visner M.S. Left Ventricular Systolic and Diastolic Dysfunction after Infusion of Tumor Necrosis Factor-Alpha in Conscious Dogs. J. Clin. Investig. 1992;90:389–398. doi: 10.1172/JCI115873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Krown K.A., Yasui K., Brooker M.J., Dubin A.E., Nguyen C., Harris G.L., McDonough P.M., Glembotski C.C., Palade P.T., Sabbadini R.A. TNF Alpha Receptor Expression in Rat Cardiac Myocytes: TNF Alpha Inhibition of L-Type Ca2+ Current and Ca2+ Transients. FEBS Lett. 1995;376:24–30. doi: 10.1016/0014-5793(95)01238-5. [DOI] [PubMed] [Google Scholar]
- 107.Amadou A., Nawrocki A., Best-Belpomme M., Pavoine C., Pecker F. Arachidonic Acid Mediates Dual Effect of TNF-Alpha on Ca2+ Transients and Contraction of Adult Rat Cardiomyocytes. Am. J. Physiol. Cell Physiol. 2002;282:C1339–C1347. doi: 10.1152/ajpcell.00471.2001. [DOI] [PubMed] [Google Scholar]
- 108.Bourraindeloup M., Adamy C., Candiani G., Cailleret M., Bourin M.-C., Badoual T., Su J.B., Adubeiro S., Roudot-Thoraval F., Dubois-Rande J.-L., et al. N-Acetylcysteine Treatment Normalizes Serum Tumor Necrosis Factor-Alpha Level and Hinders the Progression of Cardiac Injury in Hypertensive Rats. Circulation. 2004;110:2003–2009. doi: 10.1161/01.CIR.0000143630.14515.7C. [DOI] [PubMed] [Google Scholar]
- 109.Adamy C., Le Corvoisier P., Candiani G., Kirsch M., Pavoine C., Defer N., Bourin M.C., Su J.B., Vermes E., Hittinger L., et al. Tumor Necrosis Factor Alpha and Glutathione Interplay in Chronic Heart Failure. Arch. Malad. Coeur Vaiss. 2005;98:906–912. [PubMed] [Google Scholar]
- 110.Leslie C.C. Cytosolic Phospholipase A2: Physiological Function and Role in Disease. J. Lipid Res. 2015;56:1386–1402. doi: 10.1194/jlr.R057588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ghosh M., Tucker D.E., Burchett S.A., Leslie C.C. Properties of the Group IV Phospholipase A2 Family. Prog. Lipid Res. 2006;45:487–510. doi: 10.1016/j.plipres.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 112.Jayadev S., Linardic C.M., Hannun Y.A. Identification of Arachidonic Acid as a Mediator of Sphingomyelin Hydrolysis in Response to Tumor Necrosis Factor Alpha. J. Biol. Chem. 1994;269:5757–5763. doi: 10.1016/S0021-9258(17)37526-9. [DOI] [PubMed] [Google Scholar]
- 113.Jupp O.J., Vandenabeele P., MacEwan D.J. Distinct Regulation of Cytosolic Phospholipase A2 Phosphorylation, Translocation, Proteolysis and Activation by Tumour Necrosis Factor-Receptor Subtypes. Biochem. J. 2003;374:453–461. doi: 10.1042/bj20030705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Murray D.R., Prabhu S.D., Chandrasekar B. Chronic Beta-Adrenergic Stimulation Induces Myocardial Proinflammatory Cytokine Expression. Circulation. 2000;101:2338–2341. doi: 10.1161/01.CIR.101.20.2338. [DOI] [PubMed] [Google Scholar]
- 115.Brodde O.E., Michel M.C. Adrenergic and Muscarinic Receptors in the Human Heart. Pharmacol. Rev. 1999;51:651–690. [PubMed] [Google Scholar]
- 116.Ait-Mamar B., Cailleret M., Rucker-Martin C., Bouabdallah A., Candiani G., Adamy C., Duvaldestin P., Pecker F., Defer N., Pavoine C. The Cytosolic Phospholipase A2 Pathway, a Safeguard of Beta2-Adrenergic Cardiac Effects in Rat. J. Biol. Chem. 2005;280:18881–18890. doi: 10.1074/jbc.M410305200. [DOI] [PubMed] [Google Scholar]
- 117.Pavoine C., Magne S., Sauvadet A., Pecker F. Evidence for a Beta2-Adrenergic/Arachidonic Acid Pathway in Ventricular Cardiomyocytes. Regulation by the Beta1-Adrenergic/Camp Pathway. J. Biol. Chem. 1999;274:628–637. doi: 10.1074/jbc.274.2.628. [DOI] [PubMed] [Google Scholar]
- 118.Pavoine C., Defer N. The Cardiac Beta2-Adrenergic Signalling a New Role for the CPLA2. Cell. Signal. 2005;17:141–152. doi: 10.1016/j.cellsig.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 119.Pavoine C., Behforouz N., Gauthier C., Le Gouvello S., Roudot-Thoraval F., Martin C.R., Pawlak A., Feral C., Defer N., Houel R., et al. Beta2-Adrenergic Signaling in Human Heart: Shift from the Cyclic AMP to the Arachidonic Acid Pathway. Mol. Pharmacol. 2003;64:1117–1125. doi: 10.1124/mol.64.5.1117. [DOI] [PubMed] [Google Scholar]
- 120.Magne S., Couchie D., Pecker F., Pavoine C. Beta(2)-Adrenergic Receptor Agonists Increase Intracellular Free Ca(2+) Concentration Cycling in Ventricular Cardiomyocytes through P38 and P42/44 MAPK-Mediated Cytosolic Phospholipase A(2) Activation. J. Biol. Chem. 2001;276:39539–39548. doi: 10.1074/jbc.M100954200. [DOI] [PubMed] [Google Scholar]
- 121.Pabbidi M.R., Ji X., Maxwell J.T., Mignery G.A., Samarel A.M., Lipsius S.L. Inhibition of CAMP-Dependent PKA Activates Β2-Adrenergic Receptor Stimulation of Cytosolic Phospholipase A2 via Raf-1/MEK/ERK and IP3-Dependent Ca2+ Signaling in Atrial Myocytes. PLoS ONE. 2016;11:e0168505. doi: 10.1371/journal.pone.0168505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jo S.-H., Leblais V., Wang P.H., Crow M.T., Xiao R.-P. Phosphatidylinositol 3-Kinase Functionally Compartmentalizes the Concurrent G(s) Signaling during Beta2-Adrenergic Stimulation. Circ. Res. 2002;91:46–53. doi: 10.1161/01.RES.0000024115.67561.54. [DOI] [PubMed] [Google Scholar]
- 123.Chesley A., Lundberg M.S., Asai T., Xiao R.P., Ohtani S., Lakatta E.G., Crow M.T. The Beta(2)-Adrenergic Receptor Delivers an Antiapoptotic Signal to Cardiac Myocytes through G(i)-Dependent Coupling to Phosphatidylinositol 3’-Kinase. Circ. Res. 2000;87:1172–1179. doi: 10.1161/01.RES.87.12.1172. [DOI] [PubMed] [Google Scholar]
- 124.Zhu W.Z., Zheng M., Koch W.J., Lefkowitz R.J., Kobilka B.K., Xiao R.P. Dual Modulation of Cell Survival and Cell Death by Beta(2)-Adrenergic Signaling in Adult Mouse Cardiac Myocytes. Proc. Natl. Acad. Sci. USA. 2001;98:1607–1612. doi: 10.1073/pnas.98.4.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yang S., Wang J., Brand D.D., Zheng S.G. Role of TNF–TNF Receptor 2 Signal in Regulatory T Cells and Its Therapeutic Implications. Front. Immunol. 2018;9:784. doi: 10.3389/fimmu.2018.00784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Haq S., Kilter H., Michael A., Tao J., O’Leary E., Sun X.M., Walters B., Bhattacharya K., Chen X., Cui L., et al. Deletion of Cytosolic Phospholipase A2 Promotes Striated Muscle Growth. Nat. Med. 2003;9:944–951. doi: 10.1038/nm891. [DOI] [PubMed] [Google Scholar]
- 127.Steinberg S.F. Cardiac Actions of Protein Kinase C Isoforms. Physiology. 2012;27:130–139. doi: 10.1152/physiol.00009.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kunapuli P., Lawson J.A., Rokach J.A., Meinkoth J.L., FitzGerald G.A. Prostaglandin F2alpha (PGF2alpha) and the Isoprostane, 8, 12-Iso-Isoprostane F2alpha-III, Induce Cardiomyocyte Hypertrophy. Differential Activation of Downstream Signaling Pathways. J. Biol. Chem. 1998;273:22442–22452. doi: 10.1074/jbc.273.35.22442. [DOI] [PubMed] [Google Scholar]
- 129.Lai J., Jin H., Yang R., Winer J., Li W., Yen R., King K.L., Zeigler F., Ko A., Cheng J., et al. Prostaglandin F2 Alpha Induces Cardiac Myocyte Hypertrophy In Vitro and Cardiac Growth In Vivo. Am. J. Physiol. 1996;271:H2197–H2208. doi: 10.1152/ajpheart.1996.271.6.H2197. [DOI] [PubMed] [Google Scholar]
- 130.Saliba Y., Keck M., Marchand A., Atassi F., Ouille A., Cazorla O., Trebak M., Pavoine C., Lacampagne A., Hulot J.S., et al. Emergence of Orai3 Activity during Cardiac Hypertrophy. Cardiovasc. Res. 2015;105:248–259. doi: 10.1093/cvr/cvu207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Keck M., Flamant M., Mougenot N., Favier S., Atassi F., Barbier C., Nadaud S., Lompré A.-M., Hulot J.-S., Pavoine C. Cardiac Inflammatory CD11b/c Cells Exert a Protective Role in Hypertrophied Cardiomyocyte by Promoting TNFR 2—and Orai3- Dependent Signaling. Sci. Rep. 2019;9:6047. doi: 10.1038/s41598-019-42452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Shuttleworth T.J. Selective Activation of Distinct Orai Channels by STIM1. Cell Calcium. 2017;63:40–42. doi: 10.1016/j.ceca.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Trebak M., Putney J.W. ORAI Calcium Channels. Physiology. 2017;32:332–342. doi: 10.1152/physiol.00011.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Skoda M., Stangret A., Szukiewicz D. Fractalkine and Placental Growth Factor: A Duet of Inflammation and Angiogenesis in Cardiovascular Disorders. Cytokine Growth Factor Rev. 2018;39:116–123. doi: 10.1016/j.cytogfr.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 135.Zhang S., Chen R., Chakrabarti S., Su Z. Resident Macrophages as Potential Therapeutic Targets for Cardiac Ageing and Injury. Clin. Transl. Immunol. 2020;9:e1167. doi: 10.1002/cti2.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alvarez-Argote S., O’Meara C.C. The Evolving Roles of Cardiac Macrophages in Homeostasis, Regeneration, and Repair. Int. J. Mol. Sci. 2021;22:7923. doi: 10.3390/ijms22157923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fujiu K., Wang J., Nagai R. Cardioprotective Function of Cardiac Macrophages. Cardiovasc. Res. 2014;102:232–239. doi: 10.1093/cvr/cvu059. [DOI] [PubMed] [Google Scholar]
- 138.Pinto A.R., Godwin J.W., Rosenthal N.A. Macrophages in Cardiac Homeostasis, Injury Responses and Progenitor Cell Mobilisation. Stem Cell Res. 2014;13:705–714. doi: 10.1016/j.scr.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 139.Frantz S., Nahrendorf M. Cardiac Macrophages and Their Role in Ischaemic Heart Disease. Cardiovasc. Res. 2014;102:240–248. doi: 10.1093/cvr/cvu025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.DeBerge M., Shah S.J., Wilsbacher L., Thorp E.B. Macrophages in Heart Failure with Reduced versus Preserved Ejection Fraction. Trends Mol. Med. 2019;25:328–340. doi: 10.1016/j.molmed.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nadaud S., Flamant M., Le Goff W., Balse E., Pavoine C. Transcriptomic and Lipidomic Mapping of Macrophages in the Hub of Chronic Beta-Adrenergic-Stimulation Unravels Hypertrophy-, Proliferation-, and Lipid Metabolism-Related Genes as Novel Potential Markers of Early Hypertrophy or Heart Failure. Biomedicines. 2022;10:221. doi: 10.3390/biomedicines10020221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yan J., Horng T. Lipid Metabolism in Regulation of Macrophage Functions. Trends Cell Biol. 2020;30:979–989. doi: 10.1016/j.tcb.2020.09.006. [DOI] [PubMed] [Google Scholar]
- 143.Andreadou I., Cabrera-Fuentes H.A., Devaux Y., Frangogiannis N.G., Frantz S., Guzik T., Liehn E.A., Gomes C.P.C., Schulz R., Hausenloy D.J. Immune Cells as Targets for Cardioprotection: New Players and Novel Therapeutic Opportunities. Cardiovasc. Res. 2019;115:1117–1130. doi: 10.1093/cvr/cvz050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ying X., Lee K., Li N., Corbett D., Mendoza L., Frangogiannis N.G. Characterization of the Inflammatory and Fibrotic Response in a Mouse Model of Cardiac Pressure Overload. Histochem. Cell Biol. 2009;131:471. doi: 10.1007/s00418-008-0541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Song X., Kusakari Y., Xiao C.-Y., Kinsella S.D., Rosenberg M.A., Scherrer-Crosbie M., Hara K., Rosenzweig A., Matsui T. MTOR Attenuates the Inflammatory Response in Cardiomyocytes and Prevents Cardiac Dysfunction in Pathological Hypertrophy. Am. J. Physiol. Cell Physiol. 2010;299:C1256–C1266. doi: 10.1152/ajpcell.00338.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chen B., Frangogiannis N.G. The Role of Macrophages in Nonischemic Heart Failure. JACC Basic Transl. Sci. 2018;3:245–248. doi: 10.1016/j.jacbts.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Patel B., Bansal S.S., Ismahil M.A., Hamid T., Rokosh G., Mack M., Prabhu S.D. CCR2+ Monocyte-Derived Infiltrating Macrophages Are Required for Adverse Cardiac Remodeling During Pressure Overload. JACC Basic Transl. Sci. 2018;3:230–244. doi: 10.1016/j.jacbts.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Damilano F., Franco I., Perrino C., Schaefer K., Azzolino O., Carnevale D., Cifelli G., Carullo P., Ragona R., Ghigo A., et al. Distinct Effects of Leukocyte and Cardiac Phosphoinositide 3-Kinase γ Activity in Pressure Overload–Induced Cardiac Failure. Circulation. 2011;123:391–399. doi: 10.1161/CIRCULATIONAHA.110.950543. [DOI] [PubMed] [Google Scholar]
- 149.Weisheit C., Zhang Y., Faron A., Köpke O., Weisheit G., Steinsträsser A., Frede S., Meyer R., Boehm O., Hoeft A., et al. Ly6C(Low) and Not Ly6C(High) Macrophages Accumulate First in the Heart in a Model of Murine Pressure-Overload. PLoS ONE. 2014;9:e112710. doi: 10.1371/journal.pone.0112710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tian Y., Luo J., Xu Q., Liu Y., Cai R., Zhou M.-S. Macrophage Depletion Protects against Endothelial Dysfunction and Cardiac Remodeling in Angiotensin II Hypertensive Mice. Clin. Exp. Hypertens. 2021;43:699–706. doi: 10.1080/10641963.2021.1945075. [DOI] [PubMed] [Google Scholar]
- 151.Lavine K.J., Pinto A.R., Epelman S., Kopecky B.J., Clemente-Casares X., Godwin J., Rosenthal N., Kovacic J.C. The Macrophage in Cardiac Homeostasis and Disease: JACC Macrophage in CVD Series (Part 4) J. Am. Coll. Cardiol. 2018;72:2213–2230. doi: 10.1016/j.jacc.2018.08.2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tauber A.I. Metchnikoff and the Phagocytosis Theory. Nat. Rev. Mol. Cell Biol. 2003;4:897–901. doi: 10.1038/nrm1244. [DOI] [PubMed] [Google Scholar]
- 153.Pinto A.R., Ilinykh A., Ivey M.J., Kuwabara J.T., D’Antoni M.L., Debuque R., Chandran A., Wang L., Arora K., Rosenthal N.A., et al. Revisiting Cardiac Cellular Composition. Circ. Res. 2016;118:400–409. doi: 10.1161/CIRCRESAHA.115.307778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ramos G.C., van den Berg A., Nunes-Silva V., Weirather J., Peters L., Burkard M., Friedrich M., Pinnecker J., Abeßer M., Heinze K.G., et al. Myocardial Aging as a T-Cell-Mediated Phenomenon. Proc. Natl. Acad. Sci. USA. 2017;114:E2420–E2429. doi: 10.1073/pnas.1621047114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Psarras S., Beis D., Nikouli S., Tsikitis M., Capetanaki Y. Three in a Box: Understanding Cardiomyocyte, Fibroblast, and Innate Immune Cell Interactions to Orchestrate Cardiac Repair Processes. Front. Cardiovasc. Med. 2019;6:32. doi: 10.3389/fcvm.2019.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Dick S.A., Macklin J.A., Nejat S., Momen A., Clemente-Casares X., Althagafi M.G., Chen J., Kantores C., Hosseinzadeh S., Aronoff L., et al. Self-Renewing Resident Cardiac Macrophages Limit Adverse Remodeling Following Myocardial Infarction. Nat. Immunol. 2019;20:29–39. doi: 10.1038/s41590-018-0272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Van Furth R., Cohn Z.A. The Origin and Kinetics of Mononuclear Phagocytes. J. Exp. Med. 1968;128:415–435. doi: 10.1084/jem.128.3.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Davies L.C., Taylor P.R. Tissue-Resident Macrophages: Then and Now. Immunology. 2015;144:541–548. doi: 10.1111/imm.12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Davies L.C., Rosas M., Jenkins S.J., Liao C.-T., Scurr M.J., Brombacher F., Fraser D.J., Allen J.E., Jones S.A., Taylor P.R. Distinct Bone Marrow-Derived and Tissue-Resident Macrophage Lineages Proliferate at Key Stages during Inflammation. Nat. Commun. 2013;4:1886. doi: 10.1038/ncomms2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Epelman S., Lavine K.J., Beaudin A.E., Sojka D.K., Carrero J.A., Calderon B., Brija T., Gautier E.L., Ivanov S., Satpathy A.T., et al. Embryonic and Adult-Derived Resident Cardiac Macrophages Are Maintained through Distinct Mechanisms at Steady State and during Inflammation. Immunity. 2014;40:91–104. doi: 10.1016/j.immuni.2013.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bajpai G., Schneider C., Wong N., Bredemeyer A., Hulsmans M., Nahrendorf M., Epelman S., Kreisel D., Liu Y., Itoh A., et al. The Human Heart Contains Distinct Macrophage Subsets with Divergent Origins and Functions. Nat. Med. 2018;24:1234–1245. doi: 10.1038/s41591-018-0059-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ma Y., Mouton A.J., Lindsey M.L. Cardiac Macrophage Biology in the Steady-State Heart, the Aging Heart, and Following Myocardial Infarction. Transl. Res. 2018;191:15–28. doi: 10.1016/j.trsl.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bizou M., Itier R., Majdoubi M., Abbadi D., Pichery E., Dutaur M., Marsal D., Calise D., Garmy-Susini B., Douin-Echinard V., et al. Cardiac Macrophage Subsets Differentially Regulate Lymphatic Network Remodeling during Pressure Overload. Sci. Rep. 2021;11:16801. doi: 10.1038/s41598-021-95723-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Fujiu K., Shibata M., Nakayama Y., Ogata F., Matsumoto S., Noshita K., Iwami S., Nakae S., Komuro I., Nagai R., et al. A Heart-Brain-Kidney Network Controls Adaptation to Cardiac Stress through Tissue Macrophage Activation. Nat. Med. 2017;23:611–622. doi: 10.1038/nm.4326. [DOI] [PubMed] [Google Scholar]
- 165.Liao X., Shen Y., Zhang R., Sugi K., Vasudevan N.T., Alaiti M.A., Sweet D.R., Zhou L., Qing Y., Gerson S.L., et al. Distinct Roles of Resident and Nonresident Macrophages in Nonischemic Cardiomyopathy. Proc. Natl. Acad. Sci. USA. 2018;115:E4661–E4669. doi: 10.1073/pnas.1720065115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sadoshima J. MRTF-A in Macrophages Mediates Pathological Hypertrophy. Cardiovasc. Res. 2022;118:cvab376. doi: 10.1093/cvr/cvab376. [DOI] [PubMed] [Google Scholar]
- 167.Kain D., Amit U., Yagil C., Landa N., Naftali-Shani N., Molotski N., Aviv V., Feinberg M.S., Goitein O., Kushnir T., et al. Macrophages Dictate the Progression and Manifestation of Hypertensive Heart Disease. Int. J. Cardiol. 2016;203:381–395. doi: 10.1016/j.ijcard.2015.10.126. [DOI] [PubMed] [Google Scholar]
- 168.Zandbergen H.R., Sharma U.C., Gupta S., Verjans J.W.H., van den Borne S., Pokharel S., van Brakel T., Duijvestijn A., van Rooijen N., Maessen J.G., et al. Macrophage Depletion in Hypertensive Rats Accelerates Development of Cardiomyopathy. J. Cardiovasc. Pharmacol. Ther. 2009;14:68–75. doi: 10.1177/1074248408329860. [DOI] [PubMed] [Google Scholar]
- 169.Zaman R., Hamidzada H., Kantores C., Wong A., Dick S.A., Wang Y., Momen A., Aronoff L., Lin J., Razani B., et al. Selective Loss of Resident Macrophage-Derived Insulin-like Growth Factor-1 Abolishes Adaptive Cardiac Growth to Stress. Immunity. 2021;54:2057–2071.e6. doi: 10.1016/j.immuni.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ishibashi M., Hiasa K., Zhao Q., Inoue S., Ohtani K., Kitamoto S., Tsuchihashi M., Sugaya T., Charo I.F., Kura S., et al. Critical Role of Monocyte Chemoattractant Protein-1 Receptor CCR2 on Monocytes in Hypertension-Induced Vascular Inflammation and Remodeling. Circ. Res. 2004;94:1203–1210. doi: 10.1161/01.RES.0000126924.23467.A3. [DOI] [PubMed] [Google Scholar]
- 171.Kuwahara F., Kai H., Tokuda K., Takeya M., Takeshita A., Egashira K., Imaizumi T. Hypertensive Myocardial Fibrosis and Diastolic Dysfunction: Another Model of Inflammation? Hypertension. 2004;43:739–745. doi: 10.1161/01.HYP.0000118584.33350.7d. [DOI] [PubMed] [Google Scholar]
- 172.Revelo X.S., Parthiban P., Chen C., Barrow F., Fredrickson G., Wang H., Yücel D., Herman A., van Berlo J.H. Cardiac Resident Macrophages Prevent Fibrosis and Stimulate Angiogenesis. Circ. Res. 2021;129:1086–1101. doi: 10.1161/CIRCRESAHA.121.319737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ismahil M.A., Prabhu S.D. Resident Macrophages in the Heart: Cardioprotective Under Pressure. Circ. Res. 2021;129:1102–1104. doi: 10.1161/CIRCRESAHA.121.320328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Leid J., Carrelha J., Boukarabila H., Epelman S., Jacobsen S.E.W., Lavine K.J. Primitive Embryonic Macrophages Are Required for Coronary Development and Maturation. Circ. Res. 2016;118:1498–1511. doi: 10.1161/CIRCRESAHA.115.308270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wong N.R., Mohan J., Kopecky B.J., Guo S., Du L., Leid J., Feng G., Lokshina I., Dmytrenko O., Luehmann H., et al. Resident Cardiac Macrophages Mediate Adaptive Myocardial Remodeling. Immunity. 2021;54:2072–2088.e7. doi: 10.1016/j.immuni.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sugita J., Fujiu K., Nakayama Y., Matsubara T., Matsuda J., Oshima T., Liu Y., Maru Y., Hasumi E., Kojima T., et al. Cardiac Macrophages Prevent Sudden Death during Heart Stress. Nat. Commun. 2021;12:1910. doi: 10.1038/s41467-021-22178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Son G.H., Park S.H., Kim Y., Kim J.Y., Kim J.W., Chung S., Kim Y.-H., Kim H., Hwang J.-J., Seo J.-S. Postmortem MRNA Expression Patterns in Left Ventricular Myocardial Tissues and Their Implications for Forensic Diagnosis of Sudden Cardiac Death. Mol. Cells. 2014;37:241–247. doi: 10.14348/molcells.2014.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hulsmans M., Clauss S., Xiao L., Aguirre A.D., King K.R., Hanley A., Hucker W.J., Wülfers E.M., Seemann G., Courties G., et al. Macrophages Facilitate Electrical Conduction in the Heart. Cell. 2017;169:510–522.e20. doi: 10.1016/j.cell.2017.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Harari E., Guo L., Smith S.L., Braumann R.E., Virmani R., Finn A.V. Heart-Resident Macrophages: Are They Involved in the Rhythm of Every Beat? J. Thorac. Dis. 2017;9:2264–2267. doi: 10.21037/jtd.2017.07.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Munshi N.V. Resident Macrophages: Near and Dear to Your Heart. Cell. 2017;169:376–377. doi: 10.1016/j.cell.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bu J., Huang S., Wang J., Xia T., Liu H., You Y., Wang Z., Liu K. The GABAA Receptor Influences Pressure Overload-Induced Heart Failure by Modulating Macrophages in Mice. Front. Immunol. 2021;12:670153. doi: 10.3389/fimmu.2021.670153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Korf-Klingebiel M., Reboll M.R., Polten F., Weber N., Jäckle F., Wu X., Kallikourdis M., Kunderfranco P., Condorelli G., Giannitsis E., et al. Myeloid-Derived Growth Factor Protects against Pressure Overload-Induced Heart Failure by Preserving Sarco/Endoplasmic Reticulum Ca2+-ATPase Expression in Cardiomyocytes. Circulation. 2021;144:1227–1240. doi: 10.1161/CIRCULATIONAHA.120.053365. [DOI] [PubMed] [Google Scholar]
- 183.Martini E., Kunderfranco P., Peano C., Carullo P., Cremonesi M., Schorn T., Carriero R., Termanini A., Colombo F.S., Jachetti E., et al. Single-Cell Sequencing of Mouse Heart Immune Infiltrate in Pressure Overload-Driven Heart Failure Reveals Extent of Immune Activation. Circulation. 2019;140:2089–2107. doi: 10.1161/CIRCULATIONAHA.119.041694. [DOI] [PubMed] [Google Scholar]
- 184.Korf-Klingebiel M., Reboll M.R., Klede S., Brod T., Pich A., Polten F., Napp L.C., Bauersachs J., Ganser A., Brinkmann E., et al. Myeloid-Derived Growth Factor (C19orf10) Mediates Cardiac Repair Following Myocardial Infarction. Nat. Med. 2015;21:140–149. doi: 10.1038/nm.3778. [DOI] [PubMed] [Google Scholar]
- 185.Wang Y., Li Y., Feng J., Liu W., Li Y., Liu J., Yin Q., Lian H., Liu L., Nie Y. Mydgf Promotes Cardiomyocyte Proliferation and Neonatal Heart Regeneration. Theranostics. 2020;10:9100–9112. doi: 10.7150/thno.44281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Di Candia A.M., de Avila D.X., Moreira G.R., Villacorta H., Maisel A.S. Growth Differentiation Factor-15, a Novel Systemic Biomarker of Oxidative Stress, Inflammation, and Cellular Aging: Potential Role in Cardiovascular Diseases. Am. Heart J. Plus Cardiol. Res. Prac. 2021;9:100046. doi: 10.1016/j.ahjo.2021.100046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rochette L., Dogon G., Zeller M., Cottin Y., Vergely C. GDF15 and Cardiac Cells: Current Concepts and New Insights. Int. J. Mol. Sci. 2021;22:8889. doi: 10.3390/ijms22168889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Unsicker K., Spittau B., Krieglstein K. The Multiple Facets of the TGF-β Family Cytokine Growth/Differentiation Factor-15/Macrophage Inhibitory Cytokine-1. Cytokine Growth Factor Rev. 2013;24:373–384. doi: 10.1016/j.cytogfr.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 189.Xu J., Kimball T.R., Lorenz J.N., Brown D.A., Bauskin A.R., Klevitsky R., Hewett T.E., Breit S.N., Molkentin J.D. GDF15/MIC-1 Functions as a Protective and Antihypertrophic Factor Released from the Myocardium in Association with SMAD Protein Activation. Circ. Res. 2006;98:342–350. doi: 10.1161/01.RES.0000202804.84885.d0. [DOI] [PubMed] [Google Scholar]
- 190.Kempf T., Zarbock A., Widera C., Butz S., Stadtmann A., Rossaint J., Bolomini-Vittori M., Korf-Klingebiel M., Napp L.C., Hansen B., et al. GDF-15 Is an Inhibitor of Leukocyte Integrin Activation Required for Survival after Myocardial Infarction in Mice. Nat. Med. 2011;17:581–588. doi: 10.1038/nm.2354. [DOI] [PubMed] [Google Scholar]
- 191.Jung S.B., Choi M.J., Ryu D., Yi H.S., Lee S.E., Chang J.Y., Chung H.K., Kim Y.K., Kang S.G., Lee J.H., et al. Reduced Oxidative Capacity in Macrophages Results in Systemic Insulin Resistance. Nat. Commun. 2018;9:1551. doi: 10.1038/s41467-018-03998-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Mendez Fernandez A.B., Ferrero-Gregori A., Garcia-Osuna A., Mirabet-Perez S., Pirla-Buxo M.J., Cinca-Cuscullola J., Ordonez-Llanos J., Roig Minguell E. Growth Differentiation Factor 15 as Mortality Predictor in Heart Failure Patients with Non-Reduced Ejection Fraction. ESC Heart Fail. 2020;7:2223–2229. doi: 10.1002/ehf2.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Brakenhielm E., González A., Díez J. Role of Cardiac Lymphatics in Myocardial Edema and Fibrosis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2020;76:735–744. doi: 10.1016/j.jacc.2020.05.076. [DOI] [PubMed] [Google Scholar]
- 194.Brakenhielm E., Alitalo K. Cardiac Lymphatics in Health and Disease. Nat. Rev. Cardiol. 2019;16:56–68. doi: 10.1038/s41569-018-0087-8. [DOI] [PubMed] [Google Scholar]
- 195.Vieira J.M., Norman S., del Campo C.V., Cahill T.J., Barnette D.N., Gunadasa-Rohling M., Johnson L.A., Greaves D.R., Carr C.A., Jackson D.G., et al. The Cardiac Lymphatic System Stimulates Resolution of Inflammation Following Myocardial Infarction. J. Clin. Investig. 2018;8:3402–3412. doi: 10.1172/JCI97192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Stables M.J., Shah S., Camon E.B., Lovering R.C., Newson J., Bystrom J., Farrow S., Gilroy D.W. Transcriptomic Analyses of Murine Resolution-Phase Macrophages. Blood. 2011;118:e192–e208. doi: 10.1182/blood-2011-04-345330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ren Zongna; Yu Peng; Li Dandan; Li Zheng; Liao Yingnan; Wang Yin; Zhou Bingying; Wang Li Single-Cell Reconstruction of Progression Trajectory Reveals Intervention Principles in Pathological Cardiac Hypertrophy. Circulation. 2020;141:1704–1719. doi: 10.1161/CIRCULATIONAHA.119.043053. [DOI] [PubMed] [Google Scholar]
- 198.Wang J.J.-C., Rau C., Avetisyan R., Ren S., Romay M.C., Stolin G., Gong K.W., Wang Y., Lusis A.J. Genetic Dissection of Cardiac Remodeling in an Isoproterenol-Induced Heart Failure Mouse Model. PLOS Genet. 2016;12:e1006038. doi: 10.1371/journal.pgen.1006038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lau E., Cao Q., Lam M.P.Y., Wang J., Ng D.C.M., Bleakley B.J., Lee J.M., Liem D.A., Wang D., Hermjakob H., et al. Integrated Omics Dissection of Proteome Dynamics during Cardiac Remodeling. Nat. Commun. 2018;9:120. doi: 10.1038/s41467-017-02467-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Brown D.A., Perry J.B., Allen M.E., Sabbah H.N., Stauffer B.L., Shaikh S.R., Cleland J.G.F., Colucci W.S., Butler J., Voors A.A., et al. Expert Consensus Document: Mitochondrial Function as a Therapeutic Target in Heart Failure. Nat. Rev. Cardiol. 2017;14:238–250. doi: 10.1038/nrcardio.2016.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Nicolás-Ávila J.A., Lechuga-Vieco A.V., Esteban-Martínez L., Sánchez-Díaz M., Díaz-García E., Santiago D.J., Rubio-Ponce A., Li J.L., Balachander A., Quintana J.A., et al. A Network of Macrophages Supports Mitochondrial Homeostasis in the Heart. Cell. 2020;183:94–109.e23. doi: 10.1016/j.cell.2020.08.031. [DOI] [PubMed] [Google Scholar]
- 202.Tang X., Li P.-H., Chen H.-Z. Cardiomyocyte Senescence and Cellular Communications Within Myocardial Microenvironments. Front. Endocrinol. 2020;11:280. doi: 10.3389/fendo.2020.00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Rea I.M., Gibson D.S., McGilligan V., McNerlan S.E., Alexander H.D., Ross O.A. Age and Age-Related Diseases: Role of Inflammation Triggers and Cytokines. Front. Immunol. 2018;9:586. doi: 10.3389/fimmu.2018.00586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Anderson R., Lagnado A., Maggiorani D., Walaszczyk A., Dookun E., Chapman J., Birch J., Salmonowicz H., Ogrodnik M., Jurk D., et al. Length-Independent Telomere Damage Drives Post-Mitotic Cardiomyocyte Senescence. EMBO J. 2019;38:e100492. doi: 10.15252/embj.2018100492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Banerjee P., Kotla S., Reddy Velatooru L., Abe R.J., Davis E.A., Cooke J.P., Schadler K., Deswal A., Herrmann J., Lin S.H., et al. Senescence-Associated Secretory Phenotype as a Hinge Between Cardiovascular Diseases and Cancer. Front. Cardiovasc. Med. 2021;8:763930. doi: 10.3389/fcvm.2021.763930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wang C., Zhang C., Liu L., Xi A., Chen B., Li Y., Du J. Macrophage-Derived Mir-155-Containing Exosomes Suppress Fibroblast Proliferation and Promote Fibroblast Inflammation during Cardiac Injury. Mol. Ther. 2017;25:192–204. doi: 10.1016/j.ymthe.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Heymans S., Corsten M.F., Verhesen W., Carai P., van Leeuwen R.E.W., Custers K., Peters T., Hazebroek M., Stöger L., Wijnands E., et al. Macrophage MicroRNA-155 Promotes Cardiac Hypertrophy and Failure. Circulation. 2013;128:1420–1432. doi: 10.1161/CIRCULATIONAHA.112.001357. [DOI] [PubMed] [Google Scholar]
- 208.Ramanujam D., Schön A.P., Beck C., Vaccarello P., Felician G., Dueck A., Esfandyari D., Meister G., Meitinger T., Schulz C., et al. MicroRNA-21-Dependent Macrophage-to-Fibroblast Signaling Determines the Cardiac Response to Pressure Overload. Circulation. 2021;143:1513–1525. doi: 10.1161/CIRCULATIONAHA.120.050682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sun X., Liu Y., Wang J., Zhang M., Wang M. Cardioprotection of M2 Macrophages-Derived Exosomal MicroRNA-24-3p/Tnfsf10 Axis against Myocardial Injury after Sepsis. Mol. Immunol. 2022;141:309–317. doi: 10.1016/j.molimm.2021.11.003. [DOI] [PubMed] [Google Scholar]
- 210.Usuelli V., Ben Nasr M., D’Addio F., Liu K., Vergani A., El Essawy B., Yang J., Assi E., Uehara M., Rossi C., et al. MiR-21 Antagonism Reprograms Macrophage Metabolism and Abrogates Chronic Allograft Vasculopathy. Am. J. Transpl. 2021;21:3280–3295. doi: 10.1111/ajt.16581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Mirna M., Paar V., Topf A., Kraus T., Sotlar K., Aigner A., Ewe A., Watzinger S., Podesser B.K., Hackl M., et al. A New Player in the Game: Treatment with AntagomiR-21a-5p Significantly Attenuates Histological and Echocardiographic Effects of Experimental Autoimmune Myocarditis. Cardiovasc. Res. 2022;118:556–572. doi: 10.1093/cvr/cvab015. [DOI] [PubMed] [Google Scholar]
- 212.Frangogiannis N.G. Cardiac Fibrosis. Cardiovasc. Res. 2021;117:1450–1488. doi: 10.1093/cvr/cvaa324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Huet E., Gabison E., Vallee B., Mougenot N., Linguet G., Riou B., Jarosz C., Menashi S., Besse S. Deletion of Extracellular Matrix Metalloproteinase Inducer/CD147 Induces Altered Cardiac Extracellular Matrix Remodeling in Aging Mice. J. Physiol. Pharmacol. 2015;66:355–366. [PubMed] [Google Scholar]
- 214.Loredo-Mendoza M.L., Ramirez-Sanchez I., Bustamante-Pozo M.M., Ayala M., Navarrete V., Garate-Carrillo A., Ito B.R., Ceballos G., Omens J., Villarreal F. The Role of Inflammation in Driving Left Ventricular Remodeling in a Pre-HFpEF Model. Exp. Biol. Med. 2020;245:748–757. doi: 10.1177/1535370220912699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Chiao Y.A., Dai Q., Zhang J., Lin J., Lopez E.F., Ahuja S.S., Chou Y.-M., Lindsey M.L., Jin Y.-F. Multi-Analyte Profiling Reveals Matrix Metalloproteinase-9 and Monocyte Chemotactic Protein-1 as Plasma Biomarkers of Cardiac Aging. Circ. Cardiovasc. Genet. 2011;4:455–462. doi: 10.1161/CIRCGENETICS.111.959981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wagner J.U.G., Dimmeler S. Cellular Cross-Talks in the Diseased and Aging Heart. J. Mol. Cell. Cardiol. 2020;138:136–146. doi: 10.1016/j.yjmcc.2019.11.152. [DOI] [PubMed] [Google Scholar]
- 217.Chiao Y.A., Ramirez T.A., Zamilpa R., Okoronkwo S.M., Dai Q., Zhang J., Jin Y.-F., Lindsey M.L. Matrix Metalloproteinase-9 Deletion Attenuates Myocardial Fibrosis and Diastolic Dysfunction in Ageing Mice. Cardiovasc. Res. 2012;96:444–455. doi: 10.1093/cvr/cvs275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Aujla P.K., Kassiri Z. Diverse Origins and Activation of Fibroblasts in Cardiac Fibrosis. Cell Signal. 2021;78:109869. doi: 10.1016/j.cellsig.2020.109869. [DOI] [PubMed] [Google Scholar]
- 219.Kanellakis P., Ditiatkovski M., Kostolias G., Bobik A. A Pro-Fibrotic Role for Interleukin-4 in Cardiac Pressure Overload. Cardiovasc. Res. 2012;95:77–85. doi: 10.1093/cvr/cvs142. [DOI] [PubMed] [Google Scholar]
- 220.Peng H., Sarwar Z., Yang X.-P., Peterson E.L., Xu J., Janic B., Rhaleb N., Carretero O.A., Rhaleb N.-E. Profibrotic Role for Interleukin-4 in Cardiac Remodeling and Dysfunction. Hypertension. 2015;66:582–589. doi: 10.1161/HYPERTENSIONAHA.115.05627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Deniset J.F., Belke D., Lee W.-Y., Jorch S.K., Deppermann C., Hassanabad A.F., Turnbull J.D., Teng G., Rozich I., Hudspeth K., et al. Gata6+ Pericardial Cavity Macrophages Relocate to the Injured Heart and Prevent Cardiac Fibrosis. Immunity. 2019;51:131–140.e5. doi: 10.1016/j.immuni.2019.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wu J., Dong E., Zhang Y., Xiao H. The Role of the Inflammasome in Heart Failure. Front. Physiol. 2021;12:709703. doi: 10.3389/fphys.2021.709703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Everett B.M., Cornel J.H., Lainscak M., Anker S.D., Abbate A., Thuren T., Libby P., Glynn R.J., Ridker P.M. Anti-Inflammatory Therapy with Canakinumab for the Prevention of Hospitalization for Heart Failure. Circulation. 2019;139:1289–1299. doi: 10.1161/CIRCULATIONAHA.118.038010. [DOI] [PubMed] [Google Scholar]
- 224.Rolski F., Błyszczuk P. Complexity of TNF-α Signaling in Heart Disease. J. Clin. Med. 2020;9:3267. doi: 10.3390/jcm9103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Fischer R., Kontermann R.E., Pfizenmaier K. Selective Targeting of TNF Receptors as a Novel Therapeutic Approach. Front. Cell Dev. Biol. 2020;8:401. doi: 10.3389/fcell.2020.00401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Adamy C., Mulder P., Khouzami L., Andrieu-abadie N., Defer N., Candiani G., Pavoine C., Caramelle P., Souktani R., Le Corvoisier P., et al. Neutral Sphingomyelinase Inhibition Participates to the Benefits of N-Acetylcysteine Treatment in Post-Myocardial Infarction Failing Heart Rats. J. Mol. Cell. Cardiol. 2007;43:344–353. doi: 10.1016/j.yjmcc.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 227.Kologrivova I., Shtatolkina M., Suslova T., Ryabov V. Cells of the Immune System in Cardiac Remodeling: Main Players in Resolution of Inflammation and Repair After Myocardial Infarction. Front. Immunol. 2021;12:664457. doi: 10.3389/fimmu.2021.664457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Chaudhry F., Isherwood J., Bawa T., Patel D., Gurdziel K., Lanfear D.E., Ruden D.M., Levy P.D. Single-Cell RNA Sequencing of the Cardiovascular System: New Looks for Old Diseases. Front. Cardiovasc. Med. 2019;6:173. doi: 10.3389/fcvm.2019.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gladka M.M. Single-Cell RNA Sequencing of the Adult Mammalian Heart-State-of-the-Art and Future Perspectives. Curr. Heart Fail. Rep. 2021;18:64–70. doi: 10.1007/s11897-021-00504-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Vannella K.M., Wynn T.A. Mechanisms of Organ Injury and Repair by Macrophages. Annu. Rev. Physiol. 2017;79:593–617. doi: 10.1146/annurev-physiol-022516-034356. [DOI] [PubMed] [Google Scholar]
- 231.Walter W., Alonso-Herranz L., Trappetti V., Crespo I., Ibberson M., Cedenilla M., Karaszewska A., Núñez V., Xenarios I., Arroyo A.G., et al. Deciphering the Dynamic Transcriptional and Post-Transcriptional Networks of Macrophages in the Healthy Heart and after Myocardial Injury. Cell Rep. 2018;23:622–636. doi: 10.1016/j.celrep.2018.03.029. [DOI] [PubMed] [Google Scholar]
- 232.O’Neill L.A.J., Pearce E.J. Immunometabolism Governs Dendritic Cell and Macrophage Function. J. Exp. Med. 2016;213:15–23. doi: 10.1084/jem.20151570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Bertero E., Maack C. Metabolic Remodelling in Heart Failure. Nat. Rev. Cardiol. 2018;15:457–470. doi: 10.1038/s41569-018-0044-6. [DOI] [PubMed] [Google Scholar]
- 234.Batista-Gonzalez A., Vidal R., Criollo A., Carreño L.J. New Insights on the Role of Lipid Metabolism in the Metabolic Reprogramming of Macrophages. Front. Immunol. 2019;10:2993. doi: 10.3389/fimmu.2019.02993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ardura J.A., Rackov G., Izquierdo E., Alonso V., Gortazar A.R., Escribese M.M. Targeting Macrophages: Friends or Foes in Disease? Front. Pharmacol. 2019;10:1255. doi: 10.3389/fphar.2019.01255. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.