Abstract
Introduction:
Cervical cancer is preventable and, in most cases, curable if identified at an early stage. Cervical cancer is the second leading cause of cancer-related mortality Ethiopia with screening accounting for only 0.8%. Furthermore, female students and young adults in colleges and universities’ have a high prevalence of genital HPV infection because of their risky sexual behavior, lack of knowledge on screening and very few students receive screening services. This study aimed to assess the Knowledge, attitudes, and practice toward cervical cancer screening and its associated factors among female college students in Dire Dawa City, Ethiopia.
Methods:
An institutional-based cross-sectional study was conducted using a multistage sampling technique from November to December 2020, among 730 female college students in Dire Dawa. Descriptive statistics and binary logistic regression were used to describe each variable and identify associations between the dependent and independent variables respectively. Adjusted odds ratio with 95% confidence interval and P-value <.05 used to determine the association.
Results:
The results showed, only 64 (9.3%) participants were knowledgeable, 413 (60.1%) had positive attitudes and 17 (2.5%) were screened in their lifetime. Age group, years of study, and history of cervical cancer practice were significantly associated with knowledge of cervical cancer screening. The year of study was based on cervical cancer smears and the number of screenings was significantly associated with attitude.
Conclusion:
This study showed that students’ knowledge of cervical cancer screening is low. Overall attitudes toward cervical cancer screening among female students were good, but only a small proportion of students had undergone cervical cancer screening. The most common reasons for the low screening practice were lack of information and undecided. There is a need to promote different campaigns for cervical cancer screening programs, in order to increase awareness.
Keywords: Cervical cancer screening, knowledge, attitude, practice, college and university, female students
Introduction
Cervical cancer is preventable and, in most cases, curable if identified at an early stage. Human papillomavirus (HPV) is a common sexually transmitted virus that causes cervical cancer. 1 Effective screening programs can significantly reduce the morbidity and mortality associated with this cancer. 2 Screening aims to detect precancerous changes, that, may lead to cancer if not treated. Women who are found to have abnormalities on screening require follow-up, diagnosis, and treatment, to prevent the development of cancer or to treat cancer at an early stage. HPV testing, cytology and visual inspection with acetic acid (VIA) are all recommended screening tests. Cryotherapy or loop electrosurgical excision can provide effective treatment. 3
Cervical cancer is a global public health problem with an estimated 569 847 cases and 311 365 deaths reported in 2018. It is the fourth most frequently diagnosed cancer and the fourth leading cause of cancer-related deaths in women. 4 More than 85% of the global burden occurs in developing countries, accounting for 13% of all female cancers and is a major cause of cancer-related deaths. It is also a major public health problem with new diagnosis cases of 530 232, and 275 008 deaths annually; with more than 85% of these deaths occurring in low- and middle-income countries including Ethiopia.5,6
A Study conducted in Tanzania and Nigeria Colleges and Universities showed that there is a low (<30%) level of knowledge, attitude, and practice toward cervical cancer screening.7,8 Similarly, a study conducted among female University Students at Kilimanjaro, Tanzania found that only 28.6% of participants had good knowledge and practiced cervical cancer screening. 7
A recent study conducted in Aksum, northern Ethiopia, Wollega, western Ethiopia, and Hawassa Universities, southern Ethiopia among female students showed that more than half of them had heard about cervical cancer, but their knowledge, attitude and practice toward cervical cancer screening were very low.9-12 Regarding attitude, a study conducted in Wollega University, western Ethiopia, identified that 55.9% of study participants had a negative attitude toward cervical cancer screening which was similar to the study conducted in Hawassa University, southern Ethiopia 44.7% of the respondents had a negative attitude toward cervical cancer screening.
Another study conducted at Adama University, Ethiopia revealed that only 2.2% of patients were screened in their lifetime, which was similar to the study conducted at Aksum University, Ethiopia where only 17.2% were screened. Surprisingly none of the study participants had been screened for cervical cancer in a study conducted at Wollega University.11-14 Furthermore, College and university students and young adults have a high prevalence of genital Human Papilloma Virus infection because of their risky sexual behavior, lack of knowledge on screening, and very few students receive screening services, and misconceptions about susceptibility. 15
In Ethiopian College and University female students’ age, year of study, and school category were significantly associated with knowledge of cervical cancer screening.10,15 -17 For instance, a study at Adama University showed that the level of knowledge about cervical cancer was associated with attitudes toward cervical cancer screening. Those with good knowledge had a more positive attitude, but the level of knowledge was not significantly associated with practice. 14
In Ethiopian policy, health education should be strengthened generally and for specific target populations through mass media, community leaders, religious and cultural leaders, professional associations, schools and other social organizations to inculcate attitudes and knowledge benefits of screening for cervical cancer; encouraging the awareness and development of health-promoting life-styles and attention to personal hygiene and a healthy environment; enhancing awareness of common communicable and nutritional diseases and the means for their prevention. The weakness of primary health-care (PHC) systems has represented a challenge to the achievement of the targets of disease control programs (DCPs) despite the availability of substantial development assistance for health, in resource-poor settings. Since 2005, Ethiopia has embraced a diagonal investment approach to strengthen its PHC systems and concurrently scale-up its DCPs. 18
Although there is limited evidence in this regard among most female college and university students in the world, no study has been conducted on female students of college and university in Dire Dawa City. This study was therefore tasked with assessing the knowledge, attitude, and practice toward cervical cancer screening and its associated factors among female college and university students in Dire Dawa City.
Methodology
Study area, period, and design
An institution-based cross-sectional study was conducted from November 15 to December 15, 2020, in 8 Colleges and 2 Universities in Dire Dawa City, Eastern Ethiopia.
Participants
All Colleges and Universities in Dire Dawa City registered as regular in the 2019/2020 academic years were included; those female students who were critically ill at the time of data collection were excluded from the study.
Sample size and sampling procedure
The sample size was obtained based on the following assumption: P-value from the previous study level of knowledge about cervical cancer screening of 25.36%, on attitude of 61.24% and on the prevalence of cervical cancer screening of 14.83%, 19 with 95% CI, a margin of error—0.05, multiplies with designing effect 2 and 5% non-response rate which makes a total of 730. A multistage sampling technique was used in this study. First, all Colleges and Universities in Dire Dawa City were identified by name. The sample size was proportionally allocated to each selected department for each academic year based on their class size. Using the student list obtained from the office of the registrar as a sampling frame the students were selected using a simple random sampling method.
Data collection
Data were collected using a structured self-administered questionnaire prepared in English. Three data collectors who had a Diploma in Nursing were involved in the study, and 1 BSc Nurse supervised the data collection. Training was given to both data collectors and supervisors on the objective of the study, on each part of the questionnaire, and on issues related to confidentiality.
Measurements
Knowledge assessment: assessed using 10 questions, the score was computed by giving “1” for students who correctly answered and “0” for those who did not. After the responses were summed and a total score was obtained for each respondent so they were considered “knowledgeable” if the percent score of 60% or more and “not knowledgeable” if less than 60%. 12
Attitude assessment: This was assessed using questions on a Likert scale. Questions on the Likert scale had positive and negative responses ranging from strongly disagree, disagree = 2, neutral = 3, agree = 4, and strongly agree = 5. The responses were summed up and a total score was obtained for each respondent. The mean score of 27.5 was calculated and those who scored the mean and above the mean score were considered as positive attitudes and scores below the mean indicated a negative attitude toward cervical cancer screening. 14 The highest score was 35 and the lowest score was 7.
Practice assessment: those respondents who screened for cervical cancer VIA test at least once in life were considered to have screening practice. Those who were never screened were considered to have no screening practice. 10
Data analysis
Data were entered into Epi-data 3.5.1 and exported to SPSS version 25.0. Frequency and proportion were computed to describe the socio-demographic characteristics of the study population. Then, logistic regression was employed to assess the association between dependent and independent variables with 95% CI and P-value of .25 for bi-variate and finally P-value of .05 for multivariate regression was considered to be statistically significant.
Quality control
To ensure the validity of the study, an appropriate size and representative type of study unit were selected; data collectors and supervisors were selected based on their educational background and they were trained. Pre-testing was conducted on 5% of Haramaya University prior to the data collection process. Based on the pre-test, the questionnaires were revised and edited with the necessary modifications. Data were checked for completeness, clarity, and consistency.
Ethical clearance
Ethical clearance was obtained from the Research and Ethics Committee of the Dire Dawa University. A formal cooperative letter was written for each college and university. After obtaining permission from the College and University departments to participate in the study, written consent was obtained from each study subject. The participants’ privacy was maintained. They were informed that there were no incentives or harms to their participation in this study. Finally, participants’ identities were kept anonymous during data collection and analysis.
Results
Socio-demographic characteristics of respondents
Among the 730 female students who participated in the study, 687 participants with complete responses had an overall response rate of 94.1%. The age range of the participants was 15 to 30 years with a mean age of 20.5 (±3 SD). The majority of 456 (66.4%) of the respondents were in the age group of 20 to 24 years. Regarding religion, 333 (48.5%) of the study participants were Orthodox followed by 274 (39.9%) of Muslim religion followers. Interims of College and University distribution, 207 (30.1%) respondents from Rift Valley University and 175 (25.5%) respondents from Ethio-Italian College.
The study distribution of study by year was 123 (17.9%) in the first year, 207 (30.1%) in the second year, 240 (34.9%) in the third year, 101(14.7%) in the fourth year, and 16(2.3%) in the fifth year. In terms of department 207(30.1%) respondents were from Business administration and 175 (25.5%) from Business department. Approximately 140 (20.4%) students were married (Table 1).
Table 1.
Socio-demographic characteristics of respondents on assessment of knowledge, attitude and practice toward cervical cancer screening and associated factors among college and university female students in Dire Dawa Administration, Ethiopia, 2021.
| Variables | Frequency | Percent (%) |
|---|---|---|
| Age group | ||
| 15-19 | 203 | 29.5 |
| 20-24 | 456 | 66.4 |
| 25-30 | 28 | 4.1 |
| Religion | ||
| Orthodox | 333 | 48.5 |
| Muslim | 274 | 39.9 |
| Catholic | 30 | 4.4 |
| Protestant | 48 | 7.0 |
| Adventist | 2 | 0.3 |
| Marital status | ||
| Married | 140 | 20.4 |
| Single | 547 | 79.6 |
| Department | ||
| Business Administration | 207 | 30.1 |
| Business | 175 | 25.5 |
| Information Technology | 106 | 15.4 |
| Accounting | 94 | 13.7 |
| Accounting and Finance | 40 | 5.8 |
| Bsc Nurse | 26 | 3.8 |
| Bsc Nurse | 23 | 3.3 |
| Construction Technology and Mgt | 16 | 2.3 |
Knowledge about cervical cancer screening
A total of 580 (84.4%) respondents had heard about cervical cancer. Of those who had heard about cervical cancer, a higher proportion 347 (50.5%) and 312 (45.4%) knew about its prevention and treatment respectively. This indicates that more than half of the respondents knew about the prevention methods and believed that cervical cancer was cured at an early stage. Moreover 467 (68.0%) of the respondents had heard of cervical cancer smears. Among those who had heard about cervical cancer, 313 (66.4%) were in the 20 - 24-year age group.
Among those who had heard of cervical cancer, 312 (53.2%) were from news media and 142 (24.2%) were from health workers.
Attitude about cervical cancer screening
Two hundred forty-one (35.1%) of the respondents agreed that cervical cancer is a killer if not detected early, and 240 (34.9%) of the respondents were neutral (Table 2).
Table 2.
Attitude of college and university female students toward cervical cancer screening in Dire Dawa Administration, Ethiopia, 2021.
| Variables | Frequency | Percent (%) |
|---|---|---|
| Cervical cancer killer if not detecting early | ||
| Strongly disagree | 52 | 7.6 |
| Disagree | 74 | 10.8 |
| Neutral | 82 | 11.9 |
| Agree | 241 | 35.1 |
| Strongly agree | 238 | 34.6 |
| Cervical cancer is malignant in Ethiopia | ||
| Strongly disagree | 36 | 5.2 |
| Disagree | 65 | 9.5 |
| Neutral | 240 | 34.9 |
| Agree | 210 | 30.6 |
| Strongly agree | 136 | 19.8 |
| Taking a vaccine for cervical cancer is important | ||
| Strongly disagree | 19 | 2.8 |
| Disagree | 21 | 3.1 |
| Neutral | 183 | 26.6 |
| Agree | 201 | 29.3 |
| Strongly agree | 263 | 38.3 |
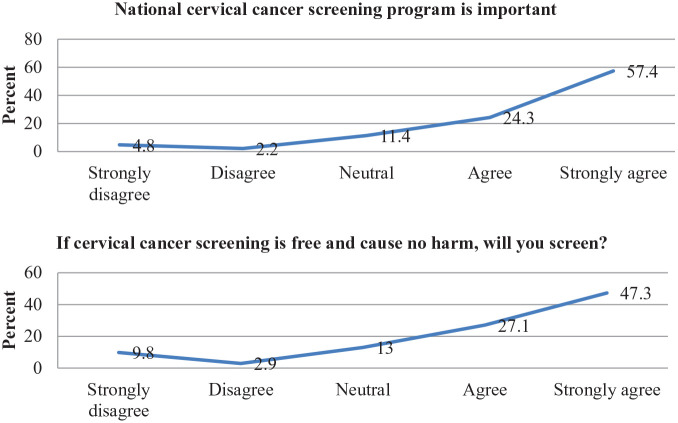
As shown below, 394 (57.4%) respondents perceived the national screening program as important. If the screening of cervical cancer was free and the procedure could not cause any harm, 263 (38.3%) of the respondents strongly agreed to be screened (Figure 1). A total of 430 (60.1%) participants had positive attitudes.
Figure 1.
Attitude of college and university female students toward cervical cancer screening in Dire Dawa Administration, Ethiopia, 2021.
Practice about cervical cancer screening
Only 17 (2.5%) patients were screened. Of those who were screened about 11 (64.7%) more than once, 9 (52.9%) were motivated by health practitioner advice, and 6 (35.3%) were motivated by friends and relations (Table 3). Reasons for not screening 294 (43.9%) participants said that I am not informed and 169 (25.2%) participants said I had not just decided.
Table 3.
Practice toward screening of cervical cancer Pap smear test among college and university female students in Dire Dawa Administration, Ethiopia, 2021.
| Variable | Frequency | Percent (%) |
|---|---|---|
| Have you ever screened for cervical cancer | ||
| Yes | 17 | 2.5 |
| No | 670 | 97.5 |
| How many times screened? | ||
| More than once | 11 | 64.7 |
| Once | 6 | 35.3 |
| Motivated for cervical cancer screen | ||
| Doctors/Health practitioners’ advice | 9 | 52.9 |
| Friends and relations | 6 | 35.3 |
| Self-motivated | 1 | 5.9 |
| When last time screening for cervical cancer | ||
| Within past three years | 11 | 64.7 |
| More than three years ago | 6 | 35.3 |
Association of knowledge about cervical cancer screening
In this study, 4 variables are significant by bi-variant, and of these, all 4 variables are significantly associated with disclosure by multiple logistic regression (P < .05). These 4 main factors included the following: age, year of study, and history of screening for cervical cancer were significantly associated with students’ knowledge toward cervical cancer screening. The age group of 15 to 19 years (OR = 0.1; 95% CI 0.02-0.39) was 10% less likely to be more knowledgeable than students with 25 to 30 years of age. Year 1 (OR = 26.39; 95% CI 3.39-205.9), year 2 (OR = 32.48; 95% CI 4.34-243.44), and year 3 (OR = 11.06; 95% CI 1.45-84.19) were more likely to be known as compared to the fourth year and above students. In addition, those students screened for cervical cancer (OR = 3.2; 95% CI 1.01-10.14) 3 times more likely to be known than students without a history of cervical cancer screening (Table 4).
Table 4.
Bivariate and multiple logistic regression of determinant factors of Knowledge toward cervical cancer screening among female students of college and university in Dire Dawa Administration, Ethiopia, 2021.
| Variables | Knowledge status | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Not knowledgeable (%) | Knowledgeable (%) | |||
| Marital status | ||||
| Married | 125 (18.2) | 15 (2.2) | 1.22 (0.66-2.25) | 1.25 (0.68-2.31) |
| Single | 498 (72.5) | 49 (7.1) | 1 | 1 |
| Age | ||||
| 15-19 | 197 (28.7) | 6 (0.9) | 0.18 (0.05-0.69) | 0.1 (0.02-0.39)** |
| 20-24 | 402 (58.5) | 54 (7.9) | 0.81 (0.27-2.4) | 0.68 (0.21-2.16) |
| 25-30 | 24 (3.5) | 4 (0.6) | 1 | 1 |
| Year of study | ||||
| 1 year | 108 (15.7) | 15 (2.2) | 16.11 (2.09-124.05) | 26.39 (3.39-205.9)** |
| 2 years | 177 (25.8) | 30 (4.4) | 19.66 (2.65-146.16) | 32.48 (4.34-243.44)** |
| 3 years | 222 (32.3) | 18 (2.6) | 9.41 (1.24-71.34) | 11.06 (1.45-84.19)** |
| ⩾ year 4 | 116 (16.9) | 1 (0.1) | 1 | 1 |
| History of Screened for CC | ||||
| Screened | 13 (1.9) | 4 (0.6) | 3.13 (0.99-9.9) | 3.2 (1.01-10.14)** |
| Not screened | 610 (88.8) | 60 (8.7) | 1 | 1 |
Note ** means that there is a significant association between dependent and independent variables.
Abbreviations: AOR, adjusted odds ratio; CC, cervical cancer; CI, confidence interval; COR, crude odds ratio.
Association of attitude about cervical cancer screening
First-year students (OR = 0.44; 95% CI 0.26-0.74) and students who heard about cervical cancer smear (OR = 0.71; 95% CI 0.51-0.98) were less likely to have a positive perception toward cervical cancer screening. Female students who were screened for cervical cancer had a more positive perception toward cervical cancer screening than female students who were screened more than once (OR = 30.00; 95% CI 1.47-611.8) (Table 5).
Table 5.
Bivariate and multiple logistic regression of determinant factors of attitude toward cervical cancer screening among female students of college and university in Dire Dawa Administration, Ethiopia, 2021.
| Variables | Attitude status | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Negative attitude (%) | Positive attitude (%) | |||
| Year of study | ||||
| 1 year | 68 (9.9) | 55 (8.0) | 0.4 (0.24-0.68) | 0.44 (0.26-0.74)** |
| 2 years | 79 (11.5) | 128 (18.6) | 0.81 (0.5-1.3) | 0.87 (0.53-1.41) |
| 3 years | 88 (12.8) | 152 (22.1) | 0.86 (0.54-1.38) | 0.91 (0.57-1.46) |
| ⩾ year 4 | 39 (5.7) | 78 (11.4) | 1 | 1 |
| Heard about cervical cancer | ||||
| Heard | 52 (7.6) | 55 (8.0) | 0.66 (0.43-0.99) | 0.76 (0.49-1.16) |
| Not heard | 222 (32.3) | 358 (52.1) | 1 | 1 |
| Heard about cervical cancer smear | ||||
| Not heard | 101 (14.7) | 119 (17.3) | 0.69 (0.5-0.96) | 0.71 (0.51-0.98)** |
| Heard | 173 (25.2) | 294 (42.8) | 1 | 1 |
| History of Screened for cervical cancer | ||||
| Screened | 10 (1.5) | 7 (1.0) | 0.46 (0.17-1.21) | 0.46 (0.17-1.23) |
| Not screened | 264 (38.4) | 406 (59.1) | 1 | 1 |
| No. of cervical cancer screen | ||||
| Once | 5 (29.4) | 6 (35.3) | 6.0 (0.52-69.74) | 30.00 (1.47-611.8)** |
| More than once | 5 (29.4) | 1 (5.9) | 1 | 1 |
Note ** means that there is a significant association between dependent and independent variables.
Abbreviations: AOR, adjusted odds ratio, CI, confidence interval; COR, crude odds ratio.
Association between cervical cancer screenings and socio-demographic characteristics
None of the socio-demographic characteristics were significantly associated with the practice of cervical cancer screening. However, one-year female students were less likely to utilize cervical cancer screening, than their counterparts (Table 6).
Table 6.
Bivariate and multiple logistic regression of determinant between cervical cancer screening and socio-demographic characteristics among female students of college and university in Dire Dawa Administration, Ethiopia, 2021.
| Variables | Cervical cancer | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Practiced (%) | Not practiced (%) | |||
| Year of study | ||||
| 1 year | 6 (0.9) | 117 (17.0) | 0.51 (0.13-2.1) | 0.57 (0.14-2.34) |
| 2 year | 3 (0.4) | 207 (30.1) | 1.79 (0.36-9.01) | 1.97 (0.39-10.00) |
| 3 year | 5 (0.7) | 240 (34.9) | 1.24 (0.29-5.27) | 1.30 (0.30-5.54) |
| ⩾ year 4 | 3 (0.4) | 117 (17.0) | 1 | 1 |
| Marital status | ||||
| Married | 2 (0.3) | 138 (20.1) | 1.9 (0.44-8.61) | 1.96 (0.45-8.82) |
| Single | 15 (2.2) | 532 (77.4) | 1 | 1 |
Abbreviations: AOR, adjusted odds ratio, CI, confidence interval; COR, crude odds ratio.
Discussion
Basic knowledge of cervical cancer screening is key to reducing maternal deaths secondary to cervical cancer. The results of this study showed that the majority 68.0% of respondents had heard of cervical cancer smears. Most of the respondents (85.7%) were unaware of the procedures used to screen cervical cancer. Among those who had heard about cervical cancer smears 7.3% said HPV testing, 4.5% visual inspection with acetic acid (VIA). Regarding the frequency of screening, about 42.2% of respondents said every year, 2.4% once every 2 years. This finding is lower than the study done in Addis Ababa University, Ethiopia, which reported that 87.7% of respondents heard about cervical cancer smears, 1.17% did not know any methods, 87.5%, and 74.4% said Pap smear and VIA; frequency of screening about 30% said every year, and 13.4% once in 2 years. 15 This difference shows that students’ knowledge of cervical cancer screening methods in the current study was lower. This difference is due to the fact that there were female students other than the health science department in the current study but the other study was only on health science students.
The overall knowledge status of cervical cancer screening was 64 (9.3%) of respondents who were knowledgeable. This is lower when compared with similar studies conducted in female university students at Kilimanjaro; Tanzania, and Sub-Saharan Africa of UK University, where 32.3% and 31.7% were knowledgeable toward cervical cancer screening.7,20 This gap may be due to differences in the nature of the population, prevalence of the disease, availability of services and information on cervical cancer screening. However, at Addis Ababa University only 12 (5.9%) respondents were knowledgeable about cervical cancer screening. 15 This difference indicates the inaccessibility of screening services in this area.
According to this study, there were significant associations between age group, year of study, and history of cervical cancer screening toward knowledge of cervical cancer screening. Age group of 15 to 19 years (OR = 0.18; 95% CI 0.05-0.69). The sample from the age group of 15 to 19-year students in College and University were 18% less likely to be knowledgeable about cervical cancer screening compared to the 25 to 30 years old age group. This may indicate that, as age increased the knowledge status also increased.
Moreover, year 1 (OR = 26.39; 95% CI 3.39-205.9), year 2 (OR = 32.48; 95% CI 4.34-243.44), and year 3 students (OR = 11.06; 95% CI 1.45-84.19) were more likely knowledgeable compared to the fourth year and above students. This finding is unexpected and requires further study. However, it could be as a result of the fact that, when the year of study increased or as the students stay in the college or university longer they became negligent.
In addition, students screened for cervical cancer (OR = 3.2; 95% CI 1.01-10.14) were more likely knowledgeable than students who did not have a history of cervical cancer screening. This may indicate that, students’ level of knowledge increased when they were screened for cervical cancer.
A positive attitude toward cervical cancer screening is crucial for detecting precancerous changes, which, if not treated, may lead to cancer. Overall attitude status on cervical cancer screening is 413 (60.1%) have a positive attitude. This result is higher than the similar study done in Hawassa and Wolega University, which is 55.3% 12 and 44.1%. 11 The same as in the current study, Mizan Tepi University 61.4% of respondents had a positive attitude. 21 While a study was done at Adama University 71.7% of respondents had a positive attitude toward cervical cancer screening. 13 This may be due to the different in the nature of population and accessibility of health-related information’s.
The finding of this study indicated that there were significant differences in the attitude of respondents toward cervical cancer screening among the different years of study, heard about cervical cancer smear, screened for cervical cancer with multivariate logistic regression analysis. Students who heard about cervical cancer smear (OR = 0.71) were less likely to have a positive attitude toward cervical cancer screening than their counterpart. Moreover, students who are once screened for cervical cancer (OR = 30.00) had a more positive perception toward cervical cancer screening. In addition, year 1 students (OR = 0.44) are less likely to have a positive attitude toward cervical cancer screening than fourth and fifth-year students. This indicated that as the year of study increased the positive perception toward cervical cancer screening also increased.
The practice of cervical cancer screening among participants in this study was very low at 17 (2.5%); compared to studies done in College of Common wealth Dominica 10 (11.24%), 22 Dungu University which is 26 (8.7%), 23 and African American College students 77%. 24 This result was much lower than that of the current study. Approximately, 413 (60.1%) participants had a positive attitude but only 17 (2.5%) were screened. This could be because social desirability bias during data collection leads to a positive attitude. This could also be due to the lack of information on screening availability in the country.
In the current study 11 (64.7%) more than once screened, 9 (52.9%) were motivated by health practitioner advice, and 11 (64.7%) were screened within the past 3 years. Compared to studies conducted at Niger Delta University, Nigeria, 19.5%, 25 and Adama University, Ethiopia, 2.1% 13 of respondents had been screened once. At Addis Ababa University 40% of those who had undergone an examination had it within the past 3 years. 19 This discrepancy could be due to the time variation between our study and other studies. This means our study relatively conducted at the time when all concerned bodies gave attention for cervical cancer screening.
Limitation of the Study
First, the survey involved a sensitivity matter which may be subject to social desirability bias. Medical knowledge acquired through courses may create a gap between health science and non-health science students.
Conclusion
In general, there was a low level of knowledge, but most of the students had heard of cervical cancer. The study also revealed that age, year of study, and practice of cervical cancer screening were significantly associated with students’ knowledge. The overall attitude toward cervical cancer screening among female students was good but only a very small proportion of female students had undergone cervical cancer screening procedures. Moreover, years of study hearing about cervical cancer screening and practice of cervical cancer were significantly associated with attitudes toward cervical cancer screening. The most common reasons for the low practice of screening are, lack of information and undecided.
Acknowledgments
I would like to thank Dire Dawa University College of Medicine and Health Science Department of Public Health for giving me this chance. I would like to extend my deepest gratitude and appreciation to my advisors Mrs. Aliya Nuri (assistant professor) and Mr. Legesse Abera for their unreserved and all-rounded support important advice, close follow up and enriching comments in the development of this thesis.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration Of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: HT: was made substantial contributions from the inception of the research idea to proposal development, data collection, analysis and interpretation of data, and preparation of the manuscript. LA, AN: were made substantial contributions in the design, analysis of the study, and participated preparation of the manuscript for publication. All authors read and approved the final version of the manuscript.
Authors’ Information: HT: has MSC in General MPH, currently working as a data collector in Ethiopia Public Health Institute in Afar, Ethiopia. LA and AN: both have MSC in Reproductive Health, currently working as Lecturer in the Department of Midwifery in College of Medicine and Health Sciences in Dire Dawa University, Dire Dawa, Ethiopia
Availability of Data and Materials: Data related to this manuscript is available on the hand of corresponding author and will be obtained under a reasonable request.
Declarations: The study was conducted after getting ethical clearance from the ethical clearance committee of Dire Dawa University. Then data were collected after getting oral and written consent from all study participants after the provision of information on the purpose, procedures, potential risk and benefits. This encouraged the provision of accurate and honest responses. The participants were assured that they have full right to participate or withdraw from the study.
ORCID iD: Legesse Abera  https://orcid.org/0000-0003-3686-8445
https://orcid.org/0000-0003-3686-8445
References
- 1. Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers. 2016;2:16086. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Program on Cancer Control: Reproductive Health and Cervical cancer screening in developing countries: report of a WHO consultation in 2002; 2002. [Google Scholar]
- 3. Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321-346. [DOI] [PubMed] [Google Scholar]
- 4. Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8:e191-e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D. Human Papillomavirus and Related Diseases in the World. Summary report. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre); 2019;307. [Google Scholar]
- 6. Ifediora CO, Azuike EC. Knowledge and attitudes about cervical cancer and its prevention among female secondary school students in Nigeria. Trop Med Int Health. 2018;23:714-723. [DOI] [PubMed] [Google Scholar]
- 7. Joel H, Mduma D, Mawolle J, Rogathi J. Knowledge and Use of Cervical Cancer Screening Among University Female Students at Kilimanjaro. American Society of Clinical Oncology; 2019;2-2. [Google Scholar]
- 8. Agboeze J, Nwali M, Ezeani N. Cervical cancer screening knowledge and behavior among female undergraduate students in a Nigerian University. American Society of Clinical Oncology; 2018. doi:10.1200/jgo.18.69200 [Google Scholar]
- 9. Knowledge SHIMELEST, Attitude. Practice of Cervical Cancer Screening and Its Associated Factors Among Female Students in Hawassa. University College of Medicine and Health Science Hawassa: Addis Ababa University; 2015. [Google Scholar]
- 10. Gebregziabher D, Berhanie E, Birhanu T, Tesfamariam K. Correlates of cervical cancer screening uptake among female under graduate students of Aksum University, College of Health Sciences, Tigray, Ethiopia. BMC Res Notes. 2019;12:520-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tilahun T, Tulu T, Dechasa W. Knowledge, attitude and practice of cervical cancer screening and associated factors amongst female students at Wollega University, western Ethiopia. BMC Res Notes. 2019;12:518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tsegaye S, Mengistu D, Gultie T. Knowledge and attitude towards cervical cancer screening and associated factors among female Hawassa university college of medicine and health sciences students. MOJ Public Health. 2018;7:151-158. [Google Scholar]
- 13. Tadesse A. Knowledge, Attitude and Practice Towards Screening for Cervical Cancer Among Adama University Female Students. Addis Abeba University; 2015. [Google Scholar]
- 14. Kellogg C, Shu J, Arroyo A, et al. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Hum Vaccin Immunother. 2019;15:1760-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gamshe E, Demissie D. Knowledge cervical cancer and associated factors among female students in Addis Ababa University College Health Science in Addis Ababa, Ethiopia. EC Gynaecology. 2019;8:594-603. [Google Scholar]
- 16. Tesfaye Z, Gebreyohannes E, Bhagavathula A, Getaneh M, Tegegn H. Awareness and knowledge of human papillomavirus and cervical cancer among female medical and health science students at the university of Gondar. 2017. http://ascopubs.org/doi/full/10.1200/JGO.2017.009688 [Google Scholar]
- 17. Hailu H. Assessment of Knowledge and Attitude Towards Cervical Cancer and Screening Among Female Students at Menelik I Health Science College, Addis Ababa, Ethiopia. Addis Ababa University; 2015. [Google Scholar]
- 18. Assefa Y, Tesfaye D, Van Damme W, Hill P. Effectiveness and sustainability of a diagonal investment approach to strengthen the primary health-care system in Ethiopia. The Lancet. 2018;392(10156):1473-1481. [DOI] [PubMed] [Google Scholar]
- 19. Tariku R. Correlates of Knowledge on Cervical Cancer Among Female Students of College of Health Science. Addis Ababa University; 2016. [Google Scholar]
- 20. Ogbonna FS. Knowledge, attitude, and experience of cervical cancer and screening among Sub-Saharan African female students in a UK university. Ann Afr Med. 2017;16:18-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mulatu K, Motma A, Seid M, Tadesse M. Assessment of knowledge, attitude, and practice on cervical cancer screening among female students of Mizan Tepi University, Ethiopia, 2016. Cancer Biol Ther Oncol. 2017;1:1-5. [Google Scholar]
- 22. Akpo D, Deji P, Idiake V, Otohinoyi D, Medavarapu S. Cervical cancer: Knowledge, screening practices and vaccines among female medical students in the Commonwealth of Dominica. Arch Med. 2016;8:23-25. [Google Scholar]
- 23. Der E, Aduah R, Iddisa B, Awinboya G, Nakong N. The knowledge and acceptablity of cervical cancer screening amoung female students in University for Development Studies (UDS) Tamale Campus-Dungu. J Adv Med Med Res. 2018;27:1-9. [Google Scholar]
- 24. Staples J, W M. An educational intervention to improve HPV and cervical cancer knowledge among African American college students. Obstet Gynecol. 2017;130:45S. [DOI] [PubMed] [Google Scholar]
- 25. Kabelenga E, Mwanakasale V, Knowledge S. Knowledge, Attitude and Practices towards cervical cancer screening among female medical students at the Copperbelt University School of Medicine, Zambia. Asian Pac J Health Sci. 2018;5:89-96. [Google Scholar]