Abstract
Introduction
Adequate water intake is a low-cost and effectively non-invasive strategy for individual health outcomes. We aimed to demonstrate the efficacy of water intake intervention in intensive-labor and static-type workplaces.
Method
Smart drinking cups were provided to the participants, and a built-in application (App) associated with the cup was downloaded on their phones. The App collected and recorded the amount of drinking water consumed by the participants set reminders for drinking water and drinking water health education information. We assessed the data, including the amount of and time interval between water intake, sedentary time, the degree of physical and psychological importance of oneself, self-satisfaction, and physical fitness.
Results
After the intervention, water intake in the two companies significantly increased during the reminder period compared with the non-reminder period. A significant increase was noted in week 3 in the amount of water intake by the participants after using the App, and the total sedentary time considerably decreased. Furthermore, the interval between water consumption decreased compared with the preintervention interval. The systolic and diastolic blood pressure decreased in the participants working at the static-type and intensive-labor workplaces after the intervention, respectively. The participants ' lower limb muscle performance also improved significantly, and the emphasis on self-care was significantly improved.
Conclusions
The health-promoting effects of the water intake wellness intervention were akin to the butterfly effect. Besides significantly increasing water intake, the intervention improved other health behaviors, thereby benefiting physical and mental health. Hence, promoting water consumption in workplaces till it becomes a habit may benefit the employees.
Keywords: water intake, health outcomes, public health, butterfly effect, health promotion
Highlights
What do We Already Know About This Topic?
Of the various nutrients necessary for good health, water is essential for various physiological processes.
How Does Your Research Contribute to the Field?
The health-promoting effects of the water intake wellness intervention were akin to the butterfly effect.
What Are Your Research’s Implications Towards Theory, Practice, or Policy?
Promoting water consumption in workplaces till it becomes a habit may benefit the employees.
Introduction
Promotion of physical and psychological health and well-being of employees in a workplace is a critical issue in the field of public health. A workplace should intend to ensure that employees spend more time at work than other places and participate more in wellness programs.1,2 In the previous decade, workplace health promotion has emerged as a popular strategy for health and cost benefits. Workplace health promotion programs (WHPPs) aim to improve lifestyle and consequently improve health and work-related outcomes. 3 In addition to promoting physical and mental health (such as reducing depression and anxiety) and increasing physical activity, WHPPs also increase workplace productivity and decrease the number of days of sick leave taken by employees.4-6 In addition, WHPPs can effectively improve employee productivity, working energy, and job satisfaction, as well as decrease absenteeism, enhance a sense of community, health behaviors, and overall well-being.7-9 Employees participating in WHPPs reduce their health risks and serve as health promotion advocates. 10 Furthermore, WHPPs also efficiently promote cancer prevention and decrease the incidence of heart diseases. 11 Using smart phone-based application (App) software as the supporting material for reminding employees at the workplace to drink water, this study aimed to provide an overview of the effectiveness of health promotion interventions at the workplace on physical and mental health outcomes related to physical fitness and self-satisfaction. Digital health interventions, including smart mobile phone pushing notification are currently commonly used in many areas. Digital health is increasingly providing opportunities for older adults and their family caregivers to educate, engage, and share health information across digital platforms. 12 Nonetheless, studies implementing interventions in the workplace designed to manipulate health-related behaviors have often demonstrated well-being status improvements and further reductions in absenteeism and improved presenteeism among participants. 13 Modern equipment, such as digital interventions and applications, may have a positive impact on health-related outcomes in the workplace. Some reviews have shown the importance of promoting physical activity, weight management, and implementing nutritional workplace interventions at workplaces.14-16 Nutrition-based suggestions are easy to implement and have been effective in the management of various health conditions. There are six general categories of nutrients essential for maintaining normal functions of the human body: carbohydrates, lipids, proteins, vitamins, minerals, and water. 17 Water does not provide energy; however, it plays a variety of important physiological roles. It is essential for metabolism, cellular homeostasis, cell-membrane integrity and transportation, temperature regulation, and cardiovascular functions. 18 In humans, water is always in a dynamic equilibrium, and inadequate fluid intake will influence the hydration status of a body and may interfere with cognition and state of consciousness. 19 Minor changes in knowledge, attitudes, and expected performance may result in significant changes in motivations and behaviors. The interactions between these variables may produce a potential model of unlimited behavioral changes, that is, “Butterfly effect.” This theory can be used to explain mental health and specific health behaviors in which a specific minor change extends to many other changes. 20 Employees are mostly sedentary during work. In addition to insufficient physical activity, their water intake is also below the recommended level, resulting in many adverse effects due to water deficiency, ranging from fatigue, 18 poor metabolism, dry and cracked lips and dry eyes 21 to joint pain, asthma and allergy,22,23 and even cardiovascular disease.24,25 Therefore, how to increase water intake in employees is an important issue.
Because water intake plays a key role in body hydration and is cost-effective, non-invasive, and low-risk to health outcomes, this study hypothesized that the use of an App to remind employees who worked in two different styles of workplaces to stay hydrated could effectively promote their physical fitness, physiological health, self-satisfaction, and degree of self-importance.
Method
Study Subjects and Recruitment
The methods proposed by Hanbury et al were referenced in this study to recruit employees for participation and to discover health problems in working environments. 26 To start, 86 workplaces that were registered in the 2021 Taipei Health Workplace Assessment were used as the target base. Then, 2 workplaces were selected based on the result of the sampling questionnaire survey showing that the employees of these two were taking the least amount of water (A Company: 586 ± 318.5 mL/at work; B Company; 512 ± 298.3 mL/at work). Next, depth interviews were conducted with the supervisors, site health management nurses, and relevant personnel of the two companies, in which the topics covered employees’ diet, water intake, and exercise habit, alongside the use of questionnaires to collect information about employees’ healthy lifestyle habits. The result showed that employees commonly had problems of imbalanced diet, insufficient water intake below the recommended amount, and insufficient exercise. In consideration of the opinions of the supervisors and site health management nurses that a water intake program is a more favorable one because it is easier to implement and has less impact on employees’ work, this study therefore focused on the intervention in employees with a problem of insufficient water intake. Based on this, the experimental design aimed to remind employees to take water via smart drinking cups and record the amount of consumed water to increase their water intake. Afterward, employees of the two companies who were found insufficient in water intake were screened to see whether they were willing to participate in the program. At this stage, 83 employees were screening out from company A and another 85 were from company B. Besides individual’s will, other inclusion criteria are as follows: (1) Weekly vegetable and fruit intake below 3 to 4 times (included) a week and no more than the amount of a bowl in each time; (2) No habit of regular exercise (defined by an aggregate time of 150 minutes of medium exertion exercise in a week, and at least 10 minutes in each time that induces an increase in heart beat and breath rhythm); (3) An average of 4 to 6 hours of sedentary seating at work daily with only one time of physical activity out of seat in every 1 to 2 hours; (4) Low awareness or satisfaction to personal physical and psychological health. In the end, 30 subjects were selected from each company; thus, the final number of participants in the experiment was 60, and the power = .945. The characteristics of the participants are listed in Table 1.
Table 1.
Participant characteristics.
| Characteristics | Company A | Company B | |
|---|---|---|---|
| Total sample | 30 | 30 | |
| Age | |||
| 25–44 years | 16 | 12 | |
| 45–64 years | 14 | 18 | |
| Sex | |||
| Male | 11 | 18 | |
| Female | 19 | 12 | |
| Health status | |||
| Waist-to-hip ratio | Normal, 84.48% | Normal: 70.45% | |
| BMI | Standard value: 50.85% | Standard value: 63.64% | |
| Occupational characteristics | |||
| Working hours | 8 hours | ||
| Schedule | AM 09:00–12:00 PM 13:00–18:00 | ||
| Level of physical activity during work | Low | Low | |
| Work content | This company is a food company that mainly provides supporting services to retailers to deal with customer complaints, assist with inventory and sell food products when necessary | This company is a securities company that mainly operates buy and sale of finance stocks on computers | |
| Permission to drink water during work | Yes | ||
| Toilet access in the workplace | The toilet is far from the office | The toilet is close to the office, and the water dispenser is just outside the toilet | |
| Health problems present in the participating staff | 1. Blood pressure >120/80 mmHg: 49.15% 2. Blood pressure >140/80 mmHg: 16.95% 3. Body fat percentage in obesity: 68.42% 4. Drank >2 L of water every day: 22.2% |
1. Blood pressure >120/80 mmHg: 70.45% 2. Blood pressure >140/80 mmHg: 22.73% 3. Body fat percentage in obesity: 59.09% 4. Drank >2 L of water every day: 30.8% |
|
Note.
Waist-to-hip ratio: the definition for obesity is ≥.9 and ≥.85 in males and females, respectively.
BMI (body mass index): the standard value is defined as 18.5≦BMI<24.
Blood pressure: normal: <120/80 mmHg; prehypertension: 120/80 ≦ blood pressure <140/90 mmHg; hypertension: ≥140/90 mmHg.
Body fat percentage: The definition for obesity is ≥25% and ≥30% in men and women, respectively.
Questionnaire for Healthy Lifestyle Habits
In order to collect information on employees’ status of diet, water intake, and exercise, for the sake of good analysis results, the questionnaire used in this study was first jointly compiled and reviewed by experts in public health and rehabilitation in Taiwan then verified by the Department of Health, Taipei City Government. Five parts are included in this questionnaire: (1) Health management: including habits of measuring body weight and blood pressure regularly and reasons for sick leaves at work; (2) Dietary habit: including habits of consuming vegetables and water; (3) Physical activity: including exercise habit and length of remaining sedentary seating at work; (4) Self-awareness: including awareness and satisfaction to individual’s body weight, blood pressure, and physical and psychological health, as well as pressure index; (5) Employment information: including gender, age, levels of education, work location, time of shift, and work qualities. Please see Supplemental document for the details of the questionnaire.
Study Protocol
The wellness program was implemented as a water intake-based intervention over the course of 8 weeks. The participants were provided with an artificially intelligent smart drinking cup which could set a reminder for drinking water, and actively transmit the amount of water intake as well as drinking time to smart phones. The wellness program had three modules: the first one (week 1–2) did not involve a water-drinking reminder on the smart phone. The second module (week 3–5) involved turning on the reminder on the App. The last module (week 6–8) involved turning the reminder off. The App would record the amount of water intake in the three modules, and send employees reminders about drinking water in the second module.
Data collection methods included (1.) Water intake: A built-in mobile phone App for smart drinking cups was downloaded to record the water intake. (2.) Questionnaire surveys: including (a) Mean 1-day cumulative sedentary time (score 1: <2 hours; score 2: 2–4 hours; score 3: 4–6 hours; score 4: 6–8 hours; score 5: >8 hours. Cronbach’s ɑ was .83, indicating good reliability.); (b) Water intake interval (score 1: <30 minutes; score 2: 30 minutes–1 hour; score 3: 1–2 hours; score 4: >2 hours. Cronbach’s ɑ was .80, indicating good reliability.); (c) Psychological status survey of employees (score 0–10: the worst to the best), including the degree of “valuing” and “satisfaction” with one’s physical and psychological health. Cronbach’s ɑ was .60. (3) Physical fitness test: including (a) Measurements of blood pressure and weight. Two blood pressure measurements were taken from the left arm in a sitting position and after about 5 minutes of rest. An arm electronic blood pressure monitor (DB62 M, Goldon Smart Home Technology Corp, Hsinchu, Taiwan) was used and the mean of the two measurements was calculated for analysis, and weight was measured without shoes and heavy clothing; (b) Grip strength test of right hand, sit-up within 30 seconds and 60 seconds, and sit and reach test for flexibility. Countermovement jump was used for assessing lower extremity muscle strength. Participants were made to perform the modified Harvard step test for evaluating cardiovascular endurance. (4.) Health education: before the program started, the researchers explained the purpose of the study to subjects and provided brief health education, which included the importance of water intake and the risks of sedentary seating to health. Health education posters were made visible on announcement boards at work and near water dispensers, for the sake of unforcedly changing subjects’ habit and encouraging them to consume more water.
Data collected included the amount of drinking water, physical fitness test scores, and questionnaire answers at the baseline (at the start of the first module) and postintervention (at the end of the last module), which were compared to calculate the difference for each variable.
Data Analysis
Repeated measures two-way analysis of variance test was performed using and SPSS 20.0 (SPSS, Inc, Chicago, IL, USA). If the interaction was significant, post hoc analysis was performed using Tukey’s multiple comparison test to examine if there was any significant difference between A and B at each section and time point and between each section or time point in A and B. The significance level was α = .05.
Results
This study included 60 participants who volunteered to participate in the workplace intervention program. A total of 30 participants, aged 25–64, were from an intensive-labor company, company A, and most of them had an education level of a bachelor’s degree and had no chronic disease. Another 30 participants, aged 25–64, were from a static-type company, company B, and most of them had an education level of a master’s degree and had no chronic diseases. All participants completed the 8-week intervention program, and the final pre–post analytic sample comprised 60 participates that had completed both baseline and postintervention measures for the wellness program.
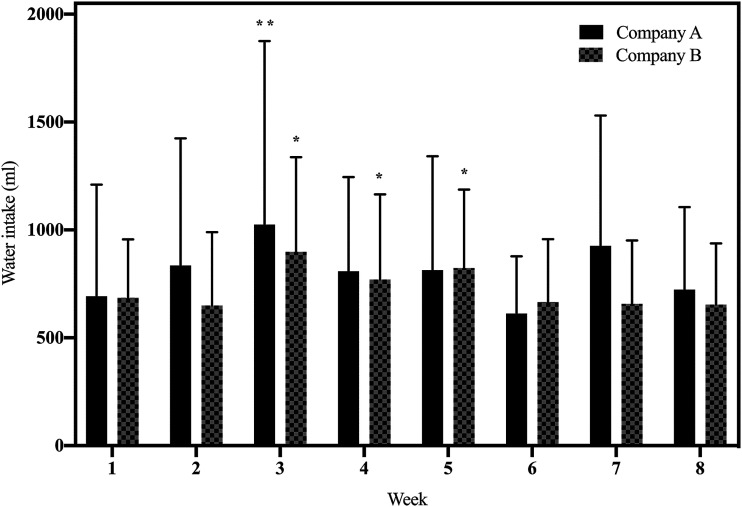
In company A, this study found that the average water intake in week 1–2 (first section), in which there was no phone-based water-drinking reminder was about 763.4 mL per day (Figure 1, week 1: average 691.9 mL; week 2: average: 834.8 mL). Furthermore, after turning the reminder of the App on in week 3–5 (second section), the amount of water intake in week 3 showed a significant increase compared with the baseline (1025.0 ± 849.9 vs. 691.9 ± 518.4 mL in week1, P < .01, Figure 1). And week 6–8 (last section), which involved turning the reminder off again had no significant difference compared with baseline. On the other hand, company B demonstrated different results as shown in Figure 1. After turned on the water intake reminder in the App in week 3-5, the amount of water intake showed statistically significant differences compared with those at baseline (897.8 ± 439.2 and 770.4 ± 394.1 and 822.6 ± 364.0 mL, respectively, P < .05 vs. 685.6 ± 270.5 mL in week 1, Figure 1). However, results in week 6–8 in which the reminder was turned off showed that the number of water intake dropped to that observed at baseline (lane 6, 7, 8 in Figure 1).
Figure 1.
Changes in drinking water intake between the employees of two companies in 8 weeks. The black bar represents company A, and the dotted bar represents company B; **, P < .01 vs. week 1 in company A; *, P < .05 vs. week1 in company B.
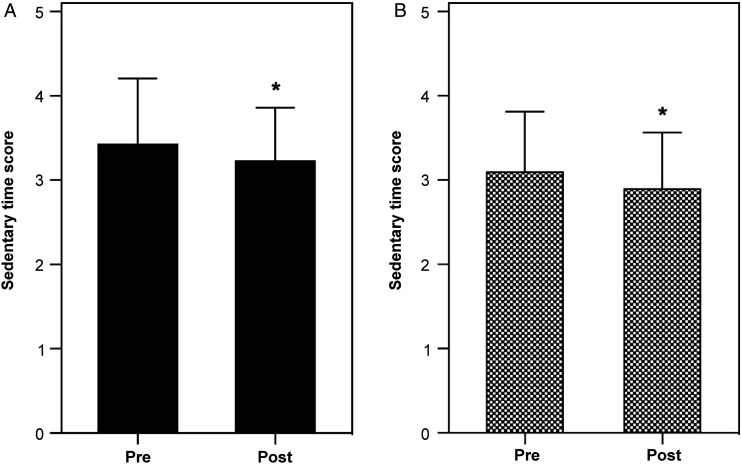
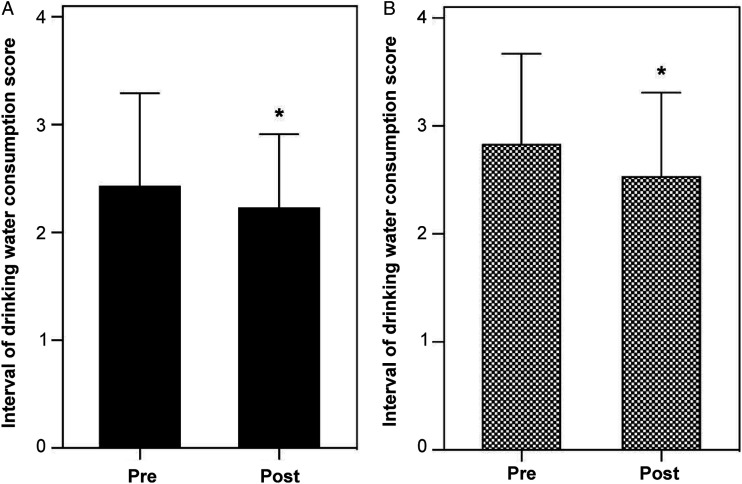
With regards to questionnaire result analysis, in terms of the sedentary time, we found that the continuous sitting interval time were significantly decreased after the water intake wellness program intervention was implemented in both the companies, compared with that pre-evaluation (Figure 2). Interestingly, after the 8-week water intake wellness program intervention, the water intake intervals in the two companies were significantly decreased (Figure 3).
Figure 2.
Questionnaire survey regarding sedentary time of the employees of companies A and B before (Pre) and after (Post) the water intake wellness intervention. (A) Representative company A (B) Representative company B. *, P < .05 in the Pre period.
Figure 3.
Questionnaire survey of water intake interval of the employees of companies A and B before (Pre) and after (Post) the water intake wellness intervention. (A) Representative company A (B) Representative company B. *, P < .05 in the Pre period.
After 8 weeks, a physical examination was administrated to all subjects, and the findings were compared against the preintervention evaluation data. Table 2 showed that systolic blood pressure of the participants from company B had declined significantly (preintervention: 122.4 ± 19.4 mmHg, postintervention: 118.6 ± 15.1 mmHg, P < .05). With regards to diastolic pressure, in company A, the preintervention value of diastolic blood pressure was 69.3 ± 4.8 mmHg and significantly decreased to 67.2 ± 5.0 mmHg after 8 weeks. There was no significant change in the weight of the employees between the two companies.
Table 2.
Physiological and physical fitness data of the employees of companies A and B before and after the water intake wellness intervention.
| Company a (n = 30) | Company B (n = 30) | |||||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||||
| Pre | Post | P Value | Pre | Post | P Value | |
| SBP | 112.0 ± 10.6 | 109.7 ± 11.2 | .179 | 122.4 ± 19.4 | 118.6 ± 15.1 | .038* |
| DBP | 69.3 ± 4.8 | 67.2 ± 5.0 | .025* | 69.9 ± 13.2 | 69.4 ± 9.7 | .374 |
| BW | 69.5 ± 11.5 | 69.9 ± 10.6 | .200 | 63.7 ± 12.6 | 63.9 ± 12.7 | .126 |
| GSRH(kg) | 28.5 ± 5.8 | 29.3 ± 7.6 | .135 | 37.1 ± 9.5 | 36.7 ± 9.6 | .202 |
| SRT(cm) | 21.9 ± 7.8 | 22.8 ± 9.1 | .099 | 18.3 ± 12.4 | 23.3 ± 7.8 | .121 |
| 30sSU(time) | 15.0 ± 4.5 | 14.3 ± 5.6 | .074 | 19.4 ± 6.2 | 18.4 ± 5.6 | .085 |
| 60sSU(time) | 27.4 ± 9.5 | 28.2 ± 11.1 | .143 | 35.1 ± 10.6 | 33.0 ± 10.4 | .106 |
| CJ (cm) | 18.0 ± 2.1 | 20.4 ± 6.2 | .032* | 24.0 ± 4.6 | 25.4 ± 4.4 | .037* |
| MHST | 56.6 ± 6.9 | 54.8 ± 4.2 | .110 | 59.4 ± 14.1 | 57.5 ± 5.5 | .169 |
Note. Pre = preintervention; Post = postintervention; SBP = Systolic blood pressure (mmHg); DBP = Diastolic blood pressure (mmHg); BW = Body weight (kg); GSRH = Grip strength of right hand (kg); SRT = Sit and reach test (cm); 30sSU = 30s Sit-up(times); 60sSU = 60s Sit-up(times); CJ = Countermovement jump (cm); MHST = Modified Harvard step test; *P < .05.
Using objective measurement is a crucial tool to evaluate the effects of this intervention. The physical fitness evaluation aimed at assessing the strength and endurance of employees’ extremities and trunk muscles. From Table 2, it can be seen that the vertical jump height of employees from the two companies significantly increased after 8 weeks (company A: preintervention: 18.0 ± 2.1 cm, postintervention:20.4 ± 6.2 cm, P < .05; company B: preintervention: 24.0 ± 4.6 cm, postintervention: 25.4 ± 4.4 cm, P < .05).
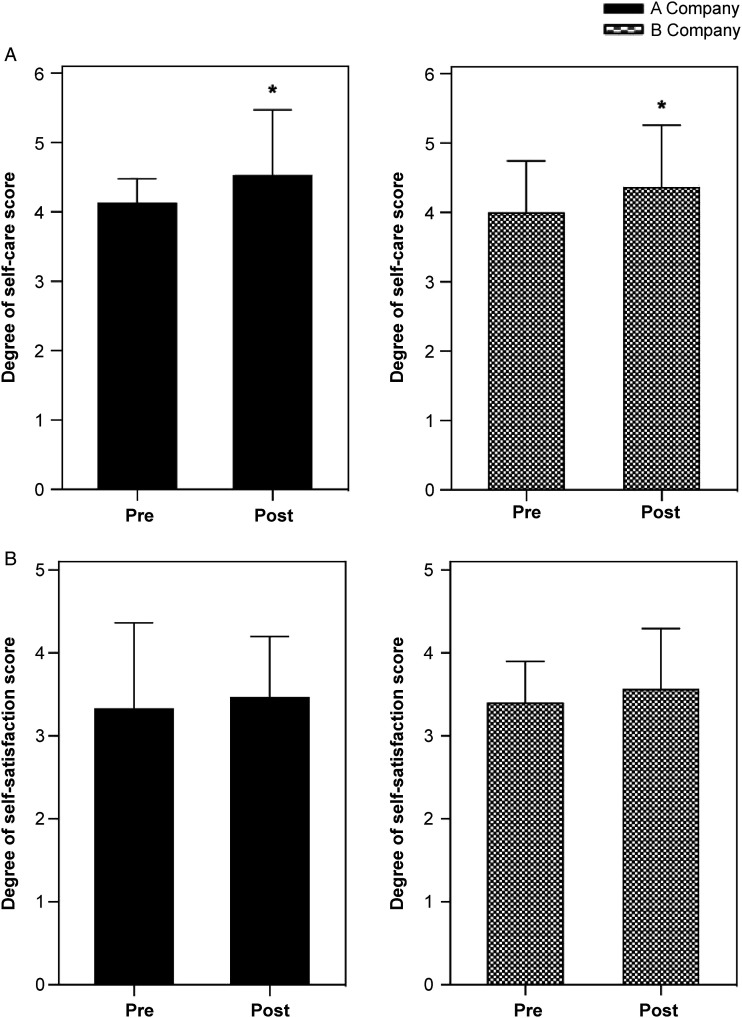
Health-related outcomes also include mental well-being. The data collected from both the pre- and post-intervention questionnaire were compared to show the difference in current valuing of “self-care” and “self-satisfaction” of one’s psychological health. After 8 weeks of the intervention, the valuing of self-care was significantly increased in both the companies and satisfaction of self-care also showed an increasing trend (Figure 4A). After the 8-week smart drinking cup intervention, the self-care value increased in the employees of both companies and they showed dissatisfaction with their health status (Figure 4B).
Figure 4.
Questionnaire survey regarding the values on self-care and self-satisfaction of the employees of companies A and B before (Pre) and after (Post) the water intake wellness intervention. (A) Representative self-care (B) Representative self-satisfaction. The black bar represents company A, and the dotted bar represents company B*, P < .05 in the Pre period.
Discussion
Improvement in healthy nutritional behavior and physical activity at the workplace is crucial to enhance the business performance and workers’ health condition. This study demonstrated that mobile device-delivered reminders regarding water intake and health education together had positive effects on the amount of water consumption in intensive-labor and static-type workplaces, decreased sedentary time and water intake interval, as well as decreased blood pressure. In addition, the vertical jump results that represented lower limb muscle strength were also found to be significantly improved.
One of the scopes of the Healthy People 2020 Objectives announced by the US is health promotion, which suggests that individual’s health awareness should be aroused so that they can practice healthy lifestyle. 27 Taking enough water every day is one of the most basic and simplest ways to promote health. Thus, individuals without underlying conditions shall take water to the level of daily recommendation in order to maintain metabolism. 28
Regarding water intake, the total water intake significantly increased when water-drinking reminders were turned on in the two companies. This proves the importance of the “reminder” function in health management plans. 29 Furthermore, the participants in intensive-labor company A had a significant increase in the average intake of water in week 3, which is when the reminder for water-drinking was turned on. Furthermore, the employees in static-type company B continuously showed an increase in the amount of water consumed in weeks 3–5. Surprisingly, irrespective of the type of company, the water intake of all participants dropped to the baseline after turned off the reminder. The results suggested that the participants in intensive-labor workplace had difficulty in getting water when the reminder was on. It might highly correlate with the working style and the long distance between their offices and their toilets. In the static workplace, people could increase the amount of drinking water because it was easily accessible in the indoor office when the mobile device delivered the notification. In addition, participants could not maintain positive significant improvements for targeted specific health behaviors without reminders. This result was similar to the results of the study done by Mainsbridge et al. 30 This is potentially means that employees need to integrate the concept into their daily workflow to create a high opportunity and strong motivation for the behavior change to occur. 31 Nowadays, several well-being programs fell short in communication and intervention interval which showed no obvious sufficient approaching for plan visibility. 32 Although the participants in company B increased the amount of water intake in weeks 3–5, the benefit effects could not persist after the intervention ended. A key element of the intervention was self-management, which relates to the active participation of an individual in a treatment or in ensuring health maintenance. This thus includes elements such as goal setting and action planning. If the employees could increase self-awareness and their knowledge regarding health practices and stimulate ownership and responsibility, they would be willing and able to improve their health behavior, which will ultimately result in improved health. 33
After 8 weeks of the intervention, the result of the questionnaire showed that the water intake intervals of the employees in both the companies were significantly decreased and water intake was effectively increased. This proved that long-term implementation of schemes to promote health information may indeed improve healthy lifestyle habits in employees. 34 Therefore, the health promotion schemes with smart reminder function and easily-accessible health education can be used more to improve water intake benefits and other health promotion behaviors. After the 8 weeks of water intake wellness intervention, we found that the average 1-day cumulative sedentary time was significantly decreased in employees from the two companies. This may be due to the overall increase in water intake and decrease in water intake interval, which encouraged employees to get up to fill up the water cup or increased the frequency of using the toilet, or increased the awareness on the improvement of self-care. Many papers pointed out that long-term sedentary work and lifestyle are potential health risk factors, and long sedentary time is positively correlated with obesity, metabolic syndrome, cardiovascular disease, and even decreased average life span.35,36 Furthermore, a long total sedentary time, even if it is noncontinuous, is positively correlated with waist circumference and body mass index.37,38 However, a slight increase in physical activity and number of steps can decrease weight, BMI, and blood pressure, and psychiatric problems and prevent cardiovascular disease. 39 Especially in people with long sedentary times, physical activity and health status have a significant linear relationship. 40 An increase in water intake has been proven to decrease hypertension. 41 Our study found that after 8 weeks of water intake wellness intervention, blood pressure in employees of static-type workplaces had significantly decreased, which coincides with the findings in past studies that blood pressure can be improved by a decrease in the time of remaining sedentary seating and an increase of water intake. Interestingly, the results of physical fitness tests of the both workplaces showed that there was an improvement in lower extremity strength, which is evidenced by an increase in performance of vertical jumps. Lengthy sedentary seating is positively correlated with low muscle mass (termed pre-sarcopenia), and a long time of seating may lead to a decrease in muscle mass, strength, and function.42-44 After the launch of the water intake program and the intervention of health education to the static-type workplace, the employees who were involved showed an improvement in their lower extremity strength, for which the reason might be that the employees had to go to the toilet more often because of higher water consumption, resulting in a decrease in time of remaining seating and an increase in frequency of standing and walking. In the intensive-labor workplace, on the other hand, the amount of subjects’ water intake increased only in the third week. Employees in this workplace do not need to move around while working unless they are requested to do so. Thus, the possible explanation for the increase in water intake might be that the intervention aroused the employees’ awareness of the importance of moving around and stretching during work hours. However, more studies are required to support this speculation. In the last few decades, the prevalence of common psychological disorders has continuously increased. Globally, there are around 29.2% of people suffering from psychiatric disorders.45,46 Previous studies pointed out that an increase in the water intake has slimming effects, and obesity and diabetes are correlated with psychiatric disorders,47-49 which is known as metabolic-mood syndrome. 50 Water can aid in signal transduction pathways and transport of nutrients to the brain, clear toxins and inflammatory substances, and provide an energy source for the brain. Therefore, increasing water intake can decrease psychological distress and anxiety.51,52 Under a high-pressure working state, it is easy to cause “workplace anxiety disorder” among workplace employees. The symptoms include feeling mental fatigue, depressed, or irritable at work, and having little interest in anything, including their physical health. 53 After the intervention of the drinking water program and instillation of health education knowledge, as the amount of water consumption and healthy behaviors increased, employees became more conscious of their physical and mental health and began to show dissatisfaction with their current condition.
There are limitations in this study. First, this study only targeted at the intensive-labor and static-type workplaces that were in the Healthy Workplace Program by the Ministry of Health and Welfare of Taiwan and that were selected by scholars who were also in the program. Hence, the results of this study cannot be generalized to all intensive-labor and static-type workplaces. In addition, it is theoretically unachievable to measure employees’ activity levels and psychological stress on a subjective basis, or to control their workload and working type to be equivalent, making the data collected in this study unjustifiable to be generalized outside of this study. Second, this study had no access to completely gather employees’ information about their daily routine, life style, and dietary behavior. This study was designed to provide detailed explanation about the method of intervention and to exclude employees who had underlying conditions and special exercise habit, but the fact is that influencing factors to individual’s physical data are beyond control. What could be done in this study is to include the controllable factors as many as possible in order to ensure the subjectivity of this study. Nevertheless, it is evidenced that insufficient water intake does harm to health, which is a common problem in workplaces.54-56 Also, due to the intense workload at workplaces, employees often forget to take water due to tight working schedules. Therefore, if there is a way to remind employees to take more water, even just a slight bit more, and with just very minor impacts on their work, it will still be a favorable choice to improve employees’ health in the long run.57-59。
If the health benefits of water consumption are promoted in a workplace and remind employees to drink water so that it becomes a habit, it will ultimately benefit both the workplace and its employees. These findings can be used as a reference for launching other health promotion programs in the future.
Conclusion
This study found out that, the use of smart drinking cups, along with easily-accessible health education, significantly increased the amount of water intake in the workplace and reduced the sedentary time of employees through the smart reminder function, which had positive effects on the physical fitness and blood pressure of employees. Therefore, if reminders about water intake can be sent to employees in a timely manner, and if they can be informed with the health benefits brought by drinking water regularly, combined with unforced health education, it may be possible to obtain other additional benefits in addition to enhancing employees' water intake.
Applying Research to Occupational Health Practice
A significant increase was observed in the amount of water intake by the study participants after the water-drinking reminder of the App was turned on, the total sedentary time was considerably decreased, and the interval between water consumption was found to decrease. Further, the systolic and diastolic blood pressure decreased in the participants working at the static-type and intensive-labor workplaces after the intervention, respectively. The participants' lower limb muscle performance also improved significantly, and the emphasis on self-care was significantly improved. Therefore, the health-promoting effects of the water intake wellness intervention were akin to the butterfly effect; it can also increase other health behaviors, thereby benefiting physical. If this research result could have applied to the workplace, that is, to provide employees with smart drinking cups with a “reminder” function, in addition to improving employee health, it is a win-win strategy for both employers and employees.
Supplemental Material
Supplemental Material, sj-pdf-1-inq-10.1177_00469580221085778 for Effectiveness of a Water Intake Program at the Workplace in Physical and Mental Health Outcomes by Yin Luo, Chia Chen, Kuo Jui Lin, Szu Kai Fu, Jyun Ru Chen and Chang-Chi Lai in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors thank Kuo-Wei Tseng and Jing-Ruei Lin for their excellent technical support in performing the experiments.
Author Contributions: CCL and KJL designed the experiments and drafted and revised the manuscript. YL
performed the main experimental work and was involved in drafting the manuscript. CCH contributed to data acquisition and analysis. SKF contributed to the conception and design of the study as well as to manuscript revision. All authors read and approved the manuscript. SKF and JRH confirm the authenticity of all the raw data.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported in part by the University of Taipei.
Ethical Approval: The study was submitted to the Institutional Review Board of University of Taipei and was determined as meeting the criteria for exemption of Institutional Review Board review. Review number: UT-IRB No. IRB-2017-038. Approval date: 2017.12.25.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Chang-Chi Lai https://orcid.org/0000-0003-0453-1207
References
- 1.Person AL, Colby SE, Bulova JA, Eubanks JW. (2010). Barriers to participation in a worksite wellness program. Nutrition Research and Practice, 4(2), 149–154. doi: 10.4162/nrp.2010.4.2.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altwaijri Y, Hyder S, Bilal L, Naseem MT, AlSaqabi D, AlSuwailem F. (2019). Evaluating the impact of a workplace wellness Program in Saudi Arabia: An intra-department study. J Occup Environ Med, 61(9), 760–766. doi: 10.1097/JOM.0000000000001656 [DOI] [PubMed] [Google Scholar]
- 3.Rongen A, Robroek SJW, van Lenthe FJ, Burdorf A. (2013). Workplace health promotion: A meta-analysis of effectiveness. Am J Prev Med, 44(4), 406–415. doi: 10.1016/j.amepre.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 4.Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. (2010). Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease--a systematic review. Scand J Work Environ Health, 36(3), 202–215. doi: 10.5271/sjweh.2891 [DOI] [PubMed] [Google Scholar]
- 5.Martin A, Sanderson K, Cocker F. (2009). Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health, 35(1), 7–18. doi: 10.5271/sjweh.1295 [DOI] [PubMed] [Google Scholar]
- 6.Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. (2009). Meta-analysis of workplace physical activity interventions. Am J Prev Med, 37(4), 330–339. doi: 10.1016/j.amepre.2009.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merrill RM, Aldana SG, Garrett J, Ross C. (2011). Effectiveness of a workplace wellness program for maintaining health and promoting healthy behaviors. J Occup Environ Med, 53(7), 782–787. doi: 10.1097/JOM.0b013e318220c2f4 [DOI] [PubMed] [Google Scholar]
- 8.Soldano SK. (2016). Workplace wellness programs to promote cancer prevention. In Saunders WB. (Ed.) Seminars in oncology nursing (Vol. 32(3), pp. 281–290) Elsevier. doi: 10.1016/j.soncn.2016.05.008 [DOI] [PubMed] [Google Scholar]
- 9.Ott-Holland CJ, Shepherd WJ, Ryan AM. (2019). Examining wellness programs over time: Predicting participation and workplace outcomes. J Occup Health Psychol, 24(1), 163–179. doi: 10.1037/ocp0000096 [DOI] [PubMed] [Google Scholar]
- 10.Street TD, Lacey SJ. (2018). Employee perceptions of workplace health promotion programs: comparison of a tailored, semi-tailored, and standardized approach. Int J Environ Res Publ Health, 15(5), 881. doi: 10.3390/ijerph15050881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song Z, Baicker K. (2019). Effect of a workplace wellness program on employee health and economic outcomes: A randomized clinical trial. JAMA, 321(15), 1491–1501. doi: 10.1001/jama.2019.3307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quinn CC, Staub S, Barr E, Gruber-Baldini A. (2019). Mobile support for older adults and their caregivers: Dyad usability study. JMIR Aging, 2(1), Article e12276. doi: 10.2196/12276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howarth A, Quesada J, Silva J, Judycki S, Mills PR. (2018). The impact of digital health interventions on health-related outcomes in the workplace: A systematic review. Digital Health, 4(1), 2055207618770861. doi: 10.1177/2055207618770861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutchinson AD, Wilson C. (2012). Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int, 27(2), 238–249. doi: 10.1093/heapro/dar035 [DOI] [PubMed] [Google Scholar]
- 15.Weerasekara YK, Roberts SB, Kahn MA, LaVertu AE, Hoffman B, Das SK. (2016). Effectiveness of workplace weight management interventions: A systematic review. Current Obesity Reports, 5(2), 298–306. doi: 10.1007/s13679-016-0205-z [DOI] [PubMed] [Google Scholar]
- 16.Pereira MJ, Coombes BK, Comans TA, Johnston V. (2015). The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: a systematic review. Occup Environ Med, 72(6), 401–412. doi: 10.1136/oemed-2014-102678 [DOI] [PubMed] [Google Scholar]
- 17.Tungare S, Paranjpe AG. (2018). Diet and Nutrition to Prevent Dental Problems. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534248/ [PubMed] [Google Scholar]
- 18.Armstrong LE, Johnson EC. (2018). Water intake, water balance, and the elusive daily water requirement. Nutrients, 10(12), 1928. doi: 10.3390/nu10121928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Price A, Burls A. (2015). Increased water intake to reduce headache: learning from a critical appraisal. J Eval Clin Pract, 21(6), 1212–1218. doi: 10.1111/jep.12413 [DOI] [PubMed] [Google Scholar]
- 20.Resnicow K, Vaughan R. (2006). A chaotic view of behavior change: a quantum leap for health promotion. Int J Behav Nutr Phys Activ, 3(1), 25. doi: 10.1186/1479-5868-3-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker LB. (2019). Physiology of sweat gland function: the roles of sweating and sweat composition in human health. Temperature, 6(3), 211–259. doi: 10.1080/23328940.2019.1632145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim KB, &Kwak YS. (2019). Dehydration affects exercise-induced asthma and anaphylaxis. Journal of Exercise Rehabilitation, 15(5), 647. doi: 10.12965/jer.1938470.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Potter PC, Klein M, Weinberg EG. (1991). Hydration in severe acute asthma. Arch Dis Child, 66(2), 216–219. doi: 10.1136/adc.66.2.216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sengupta P. (2013). Potential health impacts of hard water. Int J Prev Med, 4(8), 866. PMID: 24049611 [PMC free article] [PubMed] [Google Scholar]
- 25.Watso JC, Farquhar WB. (2019). Hydration status and cardiovascular function. Nutrients, 11(8), 1866. doi: 10.3390/nu11081866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanbury A, Farley K, Thompson C. (2015). Cost and feasibility: an exploratory case study comparing use of a literature review method with questionnaires, interviews and focus groups to identify barriers for a behaviour–change intervention. BMC Health Serv Res, 15(1), 1–8. doi: 10.1186/s12913-015-0877-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parker R, Ratzan SC. (2010). Health literacy: a second decade of distinction for Americans. J Health Commun, 15(S2), 20–33. doi: 10.1080/10810730.2010.501094 [DOI] [PubMed] [Google Scholar]
- 28.Jéquier E, Constant F. (2010). Water as an essential nutrient: the physiological basis of hydration. Eur J Clin Nutr, 64(2), 115–123. doi: 10.1038/ejcn.2009.111 [DOI] [PubMed] [Google Scholar]
- 29.Wang MY, Shen MJ, Wan LH, et al. (2020). Effects of a comprehensive reminder system based on the Health Belief Model for patients who have had a stroke on health behaviors, blood pressure, disability, and recurrence from baseline to 6 months: a randomized controlled trial. J Cardiovasc Nurs, 35(2), 156–164. doi: 10.1097/JCN.0000000000000631 [DOI] [PubMed] [Google Scholar]
- 30.Mainsbridge CP, Cooley PD, Fraser SP, Pedersen SJ. (2014). The effect of an e-health intervention designed to reduce prolonged occupational sitting on mean arterial pressure. J Occup Environ Med, 56(11), 1189–1194. doi: 10.1097/JOM.0000000000000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pedersen SJ, Cooley PD, Mainsbridge C. (2014). An e-health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work, 49(2), 289–295. doi: 10.3233/WOR-131644 [DOI] [PubMed] [Google Scholar]
- 32.Pronk N. (2014). Best practice design principles of worksite health and wellness programs. ACSM's Health & Fit J, 18(1), 42–46. doi: 10.1249/FIT.0000000000000012 [DOI] [Google Scholar]
- 33.Hendriksen IJ, Snoijer M, de Kok BP, van Vilsteren J, Hofstetter H. (2016). Effectiveness of a multilevel workplace health promotion program on vitality, health, and work-related outcomes. J Occup Environ Med, 58(6), 575. doi: 10.1097/JOM.0000000000000747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pronk N. (2014). Best practice design principles of worksite health and wellness programs. ACSM's Health & Fit J, 18(1), 42–46. doi: 10.1249/FIT.0000000000000012 [DOI] [Google Scholar]
- 35.Brown WJ, Bauman AE, Owen N. (2009). Stand up, sit down, keep moving: turning circles in physical activity research? Br J Sports Med, 43(2), 86–88. doi: 10.1136/bjsm.2008.055285 [DOI] [PubMed] [Google Scholar]
- 36.Staal JB, De Rijk A, Houkes I, Heymans MW. (2013). Clinical interventions to reduce work disability in workers with musculoskeletal disorders or mental health problems. In Handbook of work disability (pp. 317–334). Springer. doi: 10.1007/978-1-4614-6214-9_20 [DOI] [Google Scholar]
- 37.Healy GN, Dunstan DW, Salmon J, et al. (2008). Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care, 31(4), 661–666. doi: 10.2337/dc07-2046 [DOI] [PubMed] [Google Scholar]
- 38.Biddle SJH, Bennie JA, De Cocker K, et al. (2019). Controversies in the science of sedentary behaviour and health: Insights, perspectives and future directions from the 2018 Queensland sedentary behaviour think tank. International Journal of Environmental Research and Public Health, 16(23), 4762. doi: 10.3390/ijerph16234762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yuenyongchaiwat K. (2016). Effects of 10,000 steps a day on physical and mental health in overweight participants in a community setting: A preliminary study. Braz J Phys Ther, 20(4), 367–373. doi: 10.1590/bjpt-rbf.2014.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Warburton DE, Nicol CW, Bredin SS. (2006). Health benefits of physical activity: the evidence. CMAJ (Can Med Assoc J), 174(6), 801–809. doi: 10.1503/cmaj.051351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jormeus A, Karlsson S, Dahlgren C, Lindström T, Nystrom FH. (2010). Doubling of water intake increases daytime blood pressure and reduces vertigo in healthy subjects. Clin Exp Hypertens, 32(7), 439–443. doi: 10.3109/10641961003686450 [DOI] [PubMed] [Google Scholar]
- 42.Reid N, Healy GN, Gianoudis J, et al. (2018). Association of sitting time and breaks in sitting with muscle mass, strength, function, and inflammation in community-dwelling older adults. Osteoporos Int, 29(6), 1341–1350. doi: 10.1007/s00198-018-4428-6 [DOI] [PubMed] [Google Scholar]
- 43.Gianoudis J, Bailey CA, Daly RM. (2015). Associations between sedentary behaviour and body composition, muscle function and sarcopenia in community-dwelling older adults. Osteoporos Int, 26(2), 571–579. doi: 10.1007/s00198-014-2895-y [DOI] [PubMed] [Google Scholar]
- 44.Sardinha LB, Santos DA, Silva AM, Baptista F, Owen N. (2015). Breaking-up sedentary time is associated with physical function in older adults. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 70(1), 119–124. doi: 10.1093/gerona/glu193 [DOI] [PubMed] [Google Scholar]
- 45.Murphy JM, Horton NJ, Laird NM, Monson RR, Sobol AM, Leighton AH. (2004). Anxiety and depression: A 40‐year perspective on relationships regarding prevalence, distribution, and comorbidity. Acta Psychiatr Scand, 109(5), 355–375. doi: 10.1111/j.1600-0447.2003.00286.x [DOI] [PubMed] [Google Scholar]
- 46.Olesen J, Leonardi M. (2003). The burden of brain diseases in Europe. Eur J Neurol, 10(5), 471–477. doi: 10.1046/j.1468-1331.2003.00682.x [DOI] [PubMed] [Google Scholar]
- 47.Muckelbauer R, Sarganas G, Grüneis A, Müller-Nordhorn J. (2013). Association between water consumption and body weight outcomes: A systematic review. Am J Clin Nutr, 98(2), 282–299. doi: 10.3945/ajcn.112.055061 [DOI] [PubMed] [Google Scholar]
- 48.Luppino FS, de Wit LM, Bouvy PF, et al. (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatr, 67(3), 220–229. doi: 10.1001/archgenpsychiatry.2010.2 [DOI] [PubMed] [Google Scholar]
- 49.Rasekhi H, Karandish M, Jalali MT, et al. (2015). Phylloquinone supplementation improves glycemic status independent of the effects of adiponectin levels in premonopause women with prediabetes: A double-blind randomized controlled clinical trial. J Diabetes Metab Disord, 14(1), 1. doi: 10.1186/s40200-014-0127-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mansur RB, Brietzke E, McIntyre RS. (2015). Is there a “metabolic-mood syndrome”? A review of the relationship between obesity and mood disorders. Neurosci Biobehav Rev, 52(1), 89–104. doi: 10.1016/j.neubiorev.2014.12.017 [DOI] [PubMed] [Google Scholar]
- 51.Stevenson EGJ, Ambelu A, Caruso BA, Tesfaye Y, Freeman MC. (2016). Community water improvement, household water insecurity, and women’s psychological distress: An intervention and control study in Ethiopia. PLoS One, 11(4), Article e0153432. doi: 10.1371/journal.pone.0153432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aihara Y, Shrestha S, Sharma J. (2016). Household water insecurity, depression and quality of life among postnatal women living in urban Nepal. J Water Health, 14(2), 317–324. doi: 10.2166/wh.2015.166 [DOI] [PubMed] [Google Scholar]
- 53.Haslam C, Atkinson S, Brown SS, Haslam RA. (2005). Anxiety and depression in the workplace: effects on the individual and organisation (a focus group investigation). J Affect Disord, 88(2), 209–215. doi: 10.1016/j.janxdis.2006.06.006 [DOI] [PubMed] [Google Scholar]
- 54.Moore M, Gould P, Keary BS. (2003). Global urbanization and impact on health. Int J Hyg Environ Health, 206(4–5), 269–278. doi: 10.1078/1438-4639-00223 [DOI] [PubMed] [Google Scholar]
- 55.Jury WA, Vaux H. (2005). The role of science in solving the world's emerging water problems. Proc Natl Acad Sci Unit States Am, 102(44), 15715–15720. 10.1073/pnas.0506467102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hunter PR, MacDonald AM, Carter RC. (2010). Water supply and health. PLoS Medicine, 7(11), Article e1000361. doi: 10.1371/journal.pmed.1000361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nakamura Y, Watanabe H, Tanaka A, Yasui M, Nishihira J, Murayama N. (2020). Effect of increased daily water intake and hydration on health in Japanese adults. Nutrients, 12(4), 1191. doi: 10.3390/nu12041191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goodman AB, Blanck HM, Sherry B, Park S, Nebeling L, Yaroch AL. (2013). Peer Reviewed: Behaviors and Attitudes Associated with Low Drinking Water Intake Among US Adults, Food Attitudes and Behaviors Survey, 2007. Preventing chronic disease, Vol. 10. doi: 10.5888/pcd10.120248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Daniels MC, Popkin BM. (2010). Impact of water intake on energy intake and weight status: a systematic review. Nutr Rev, 68(9), 505–521. doi: 10.1111/j.1753-4887.2010.00311.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-inq-10.1177_00469580221085778 for Effectiveness of a Water Intake Program at the Workplace in Physical and Mental Health Outcomes by Yin Luo, Chia Chen, Kuo Jui Lin, Szu Kai Fu, Jyun Ru Chen and Chang-Chi Lai in INQUIRY: The Journal of Health Care Organization, Provision, and Financing