Abstract
Background:
The COVID-19 pandemic interrupted the delivery of face-to-face pain services including pain management programmes in the United Kingdom with considerable negative impact on patients with chronic musculoskeletal pain. We aimed to develop and implement a remotely delivered pain management programme (PMP) using video-conferencing technology that contains all the core components of a full programme: the ‘virtual PMP’ (vPMP). By reporting on the process of this development, we endeavour to help address the paucity of literature on the development of remote pain management programmes.
Methods:
The vPMP was developed by an inter-disciplinary group of professionals as a quality improvement (QI) project. The Model for Improvement Framework was employed with patient involvement at the design phase and at subsequent improvements. Improvement was measured qualitatively with frequent and repeated qualitative data collection leading to programme change. Quantitative patient demographic comparisons were made with a patient cohort who had been on a face-to-face PMP pathway.
Results:
Sixty-one patients on the PMP waiting list were contacted and 43 met the criteria for the programme. Fourteen patients participated in three vPMP cycles. Patient involvement and comprehensive stakeholder consultation were essential to a robust design for the first vPMP. Continued involvement of patient partners during the QI process led to rapid resolution of implementation problems. The most prominent issues that needed action were technical challenges including training needs, participant access to physical and technological resources, participant fatigue and concerns about adequate communication and peer support.
Conclusion:
This report demonstrates how a remotely delivered PMP, fully in line with national guidance, was rapidly developed and implemented in a hospital setting for patients with chronic musculoskeletal pain. We also discuss the relevance of our findings to the issues of cost, patient experience, patient preferences and inequities of access in delivering telerehabilitation for chronic pain.
Keywords: Telehealth, telemedicine, chronic musculoskeletal pain, pain management programmes, virtual
Introduction
Chronic pain creates a major healthcare burden throughout the world. A recent review concluded that over 40% of the UK population are affected by chronic pain. 1 Inter-disciplinary pain management programmes (PMPs), based on the principles of cognitive behavioural intervention and goal directed rehabilitation, are designed with the aim of reducing the impact of chronic pain and increasing activity levels. The British Pain Society (BPS) has published Guidelines for Pain Management Programmes in Adults 2 to advise what constitutes a PMP, its position within care pathways for people with chronic pain and desirable content for programmes.
As the COVID-19 pandemic took hold in the United Kingdom, pressures on the wider healthcare system saw a change in chronic pain service provision throughout the country. At the host institution for this project, where PMPs have been running for over 25 years by an inter-disciplinary professional group, the pain and musculoskeletal (MSK) rehabilitation programmes were stood down as face-to-face treatment sessions delivered to patients in groups became prohibitive. The detrimental effect that long waiting times have on the physical and mental health of chronic pain patients is recognised. 3 Moreover, patients whose care was affected by the pandemic were faced with the uncertainty of whether they would be able to access any intervention in the foreseeable future. There is evidence that the conditions imposed by the COVID pandemic have affected people with persistent pain disproportionately, with increased symptoms, and greater effects on mood and physical activity. 4 In May 2020, recognising these factors, we set out to rapidly design and implement a remotely delivered PMP with live interactive sessions: the ‘virtual pain management programme’ (vPMP) using video-conferencing technology.
A recent rapid review of PMPs delivered via video-conferencing 5 identified three papers up until April 2020 and determined that video-conferencing for PMPs was feasible, but there was little guidance on how to develop and deliver these. In this article, we describe how this goal was achieved at our institution, using a quality improvement (QI) approach and service user involvement.
Methods
The inter-disciplinary pain management and rehabilitation team, supported by operational management, made the decision to move to delivering a remote PMP and set themselves a target of designing and beginning its delivery within 4 weeks. A core design and implementation group of professionals including medical staff, occupational therapists, physiotherapists and psychologists were assembled to achieve this goal. Two implementation leads (D.W., physiotherapist and H.P., physiotherapist) were appointed to coordinate the roll out of the vPMP. A data collection team was also formed to complete the evaluation tasks.
Participation criteria for the vPMP were agreed as: (1) reliable Internet access at home, (2) possession of a laptop or tablet for video sessions, (3) access to a quiet and confidential place for session participation, (4) no sensory difficulties that would affect ability to take part in a video-conferencing session and (5) no uncontrolled seizures or faints. These criteria were required in addition to the criteria already in place for a face-to-face PMP.
Pre-programme design phase
Delivery of a remote programme was a completely new experience for the team. However, there is vast collective experience in delivering face-to-face programmes in the host institution with all core members of the group having at least 5 years of experience in running programmes for adults that were fully in line with BPS guidance. Specifically, the face-to-face programme content has included all of the core elements of graded activation, cognitive therapy methods, graded exposure, methods to enhance acceptance, mindfulness and psychological flexibility, skills training and activity management, physical exercise and relevant patient education as a package of interventions by psychologists, physiotherapists, occupational therapists and nurses.
From the inception of the project, there was consensus in the core design group on four basic principles:
The vPMP will be an adaptation of the face-to-face version of the PMP. As such, it will consist of interactive, real-time video-conferencing–based sessions rather than delivered using pre-recorded material.
The vPMP will remain faithful to the current BPS PMP guidelines 2 and not lose any of the core components outlined in this guidance.
The design will consider the viewpoints of all staff groups normally involved in running the face-to-face PMP.
The design will involve patients who have had experience of the face-to-face PMP.
The pre-programme design therefore included a staff consensus and a patient involvement exercise as well as infrastructure considerations for programme delivery. In parallel to delivery of the programme, the implementation leads for the vPMP explored the digitalisation of PMP patient-reported outcome measures (PROMs) during this project.
Review of existing literature
A systematic literature review of remotely delivered PMPs was conducted by three of the authors (G.B., A.G., H.P. and D.W.). 6 The purpose of which was to identify the variation in content of virtually delivered PMPs.
Staff consensus exercise
Opinions were sought internally from a range of staff groups normally involved in the delivery of the programmes including those with administrative and operational roles, as well as medical, nursing, occupational therapy, physiotherapy and psychology staff. Feedback was collected in planned one-to-one and team meetings.
Opinions of clinicians with experience in delivering programmes outside the organisation were included through participation by three of the authors (D.W., H.P. and M.P.) in the UK Physiotherapy Pain Association’s COVID-19 Response Webinar held on 29 May 2020. The webinar shared the experiences of clinicians and patients with both face-to-face and online pain management groups. 7 Key messages were summarised and agreed by the three physiotherapists independently and shared with the core design and implementation team.
Patient involvement
Eight patients who had had recent lived experience of participation in a PMP were approached to be involved in the design of the vPMP. The patient partners were required to have time and equipment for taking part in a 1-hour semi-structured telephone interview. All eight patients agreed to be involved. No material incentives were provided. The interviews were done on the telephone by two of the authors and members of the therapy team (G.B. and T.P.). Patients were asked open-ended questions about their viewpoints of a remotely delivered PMP followed by more specific questions relating to programme content, timetabling, online resources and technological support.
Infrastructure considerations
Access to sufficient hardware and physical space to conduct the programme sessions was imperative to its successful delivery. At the time of inception of the vPMP, sharing of IT facilities in open offices was the norm for the therapy team. A scoping exercise was undertaken to ascertain the additional resources required to conduct vPMP sessions effectively and in appropriate settings. These included facilities for working from home, additional IT equipment including laptops, webcams and headphones and on-site private office space. The team also considered the feasibility of moving away from paper-based, hand-filled PROMs data collection towards a system for digital data collection.
The first iteration of the programme design was finalised for the first cohort of patients in June 2020. One-to-one meetings with data collectors (for clinicians and patients) and minuted daily therapy team meetings were time tabled specifically for programme evaluation.
Real-time evaluation and QI
The Model for Improvement Framework 8 was used with rapid ‘plan, do, study act’ (PDSA) cycles to effect change. The aim of the project was to implement live, interactive, remotely delivered PMP interventions containing all core elements outlined in the BPS guidance. 2 Improvement delivery was measured using qualitative methods. Successful implementation was defined as full programme delivery with all sessions of the programme accessibly delivered to all participants without any reported concerns on technical or operational difficulties, clinical safety or information governance.
In a series of PDSA cycles, outputs from the qualitative evaluations generated improvement actions which would be implemented rapidly in the next programme after a team discussion. Where actions could be implemented immediately, this was done within the same programme. The actions were often put forward by the patients or clinicians themselves. The PDSA cycles were continued during the programmes until no new changes to the vPMP format were required.
Evaluations comprised qualitative data collection capturing patient and clinician experience. For both the patient and clinician data, a mix of semi-structured and open questions using specifically designed feedback forms was used to obtain as wide a variety of viewpoints as possible. All formally planned evaluations were completed by therapists not directly involved in the delivery of the programme to minimise bias. More detail on this is given below.
In addition to formal data collection, informal feedback to the core implementation group through clinician observations, one-to-one conversations and weekly multi-disciplinary team (MDT) meetings (a routine part of face-to-face programmes) were taken into consideration and influenced the PDSA cycles.
The formal data collection included the following.
Patient feedback
For individual feedback, patients were contacted by members of the therapy team not directly delivering the vPMP, by phone or video call to share their experience of the programme. This was carried out daily during the first programme and weekly during subsequent programmes. At the end the first vPMP, a patient focus group was held, facilitated by a physiotherapist (G.B.), in which all participants in the first programme agreed to take part and share their experience.
Clinician feedback
Individual clinicians shared their experience following each session of the programme during the first vPMP in written (e.g. email) or planned verbal 1:1 feedback. Staff feedback was also given within team meetings throughout the programmes. A clinician focus group was held in the week after the third vPMP by G.B. All 13 clinicians who delivered the first three programmes were invited and six participated (two physiotherapists, two occupational therapists, one psychologist and one therapy technician).
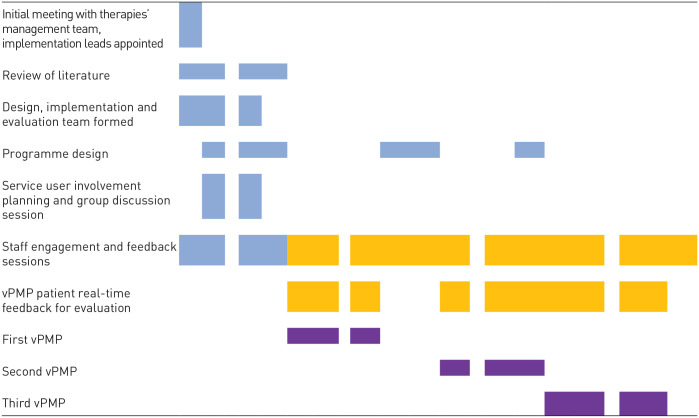
See Table 1 for the project timeline.
Table 1.
Timelines for planning (blue), implementation (purple) and evaluation (yellow).
| May | June | July | August | September | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| W1 | W2 | W3 | W4 | W5 | W6 | W7 | W8 | W9 | W10 | W11 | W12 | W13 | W14 | W15 | W16 | |
| ||||||||||||||||
vPMP: virtual pain management programme.
Analysis
For all the formally collected qualitative data, the data collectors and interviewers made detailed notes during the discussions. The interviews and meetings were not recorded. Inductive thematic analysis was undertaken based on the interviewer and data collector notes.
Quantitative data on patient demographics were analysed for normality using the Shapiro–Wilk test. Comparisons were made using the unpaired t-test for normally distributed data and the chi-square test for categorical data.
Project registration and participant consent
This project was submitted to the Trust’s Research and Development Project Evaluation Panel and was recommended to proceed as a service evaluation on 8 June 2020 (registration reference no. SE20.31). All participants were provided with a written information sheet on the project, and written informed consent was signed by all participants.
Results
Outputs from the pre-programme planning phase
We found no studies reported in the literature that used the BPS guidelines to support the design of vPMPs. 6
Learning points from internal and external experts in PMP delivery generated recommendations for both programme design and programme implementation.
The main points expressed at the PPA 2020 Webinar were that a new remotely delivered programme should:
Take steps to maintain peer support and sharing of experience among patients, for example, maintain group work using ‘breakout rooms’ and chat functions.
Have appropriate policies created for their safe conduct.
Train both patients and staff on the use of the online platform.
Allow extra time for technical issues and to ensure support to resolve these is available.
The following points emerged from discussions among PMP staff and were all implemented:
Development of a risk assessment document to support the management of a patient becoming unwell, particularly the management of joint dislocations in hypermobile patients during exercise sessions.
Adjustments in the programme code of conduct for vPMP participants, paying particular attention to maintaining confidentiality and establishing an appropriate virtual environment for video-conferencing.
Support for patients who do not have the skills to use the digital platform for the vPMP including an introductory skills tutorial session in the week prior to the vPMP.
Creating an electronic version of the programme patient educational material.
Training to boost staff competency in using video-conferencing technology: a competency framework was created, and a training package was developed on the use of the platform. A rota was established to allow clinicians to shadow each other enabling mutual learning and fast troubleshooting without interruption to the flow of the session.
Data collection on the reasons participants declined the vPMP, paying particular attention to inequities of access.
Patient involvement
Overall, former patients were enthusiastic about the range of practical sessions that could be conducted using the currently available technology. The following themes were extracted from interview notes:
Theme 1: The importance of peer support. Most participants believed that peer support is an essential part of PMPs. Shared experiences and ideas were thought to foster a sense of camaraderie which continued beyond the programme. There was concern that this may not happen naturally in a remotely delivered programme and suggestions were made about how this could be facilitated by staff early in the vPMP. Specifically proposed actions were ‘ice-breaking’ introductory sessions and use of ‘breakout rooms’ during video-conferencing to provide opportunities for less formal interactions and relationship building.
Theme 2: Individualised care and access to support. Two subthemes were identified in this context. The first was maintaining the 1:1 patient input from therapists. Retaining timetabled individual sessions was seen as essential across all disciplines to ensure personalised care and also allow sensitive issues to be addressed that would not be appropriate for a group environment. The second subtheme was access to the therapy team for support during the programme. Patients reported that ad hoc access to staff, as would be usual during the face-to-face programme, was important. They suggested that a support email address could be created for this purpose. It was highlighted that vPMP participants may also need to access support for the use of video-conferencing software.
Theme 3: Programme intensity. Participants felt that replicating the intensity of the face-to-face programme may be unrealistic. Two subthemes were identified in relation to programme intensity. The first was session intensity. A number of participants felt that video-conferencing sessions lasting 45–60 min would be more tiring compared to face-to-face sessions and this could lead to lapses in concentration. It was suggested that group sizes should not fall below four patients to enable a good group dynamic but should be limited to enable discussion, without becoming overwhelming. There was a wide range of suggestions for maximum group size going up to 15 patients. The second subtheme was the need for reflection time while on a novel programme delivered through video-conferencing. Participants suggested that gaps between sessions should be protected for time off-line. Some suggested that the programme could be longer in duration in order to cover all the content while reducing the frequency of sessions but they also recognised the counter argument that a longer, more spread-out programme may impact negatively on group cohesion and programme content.
Theme 4: Access to resources. Maintaining access to physical written resources, gym facilities and exercise equipment was important to patients, and it was observed that these would not be accessible in the home environment. Paper-based resources such as technology guides, timetables and introductions to therapists were identified as essential for successful preparation. Sending information in advance was recommended.
First vPMP design
Table 2 summarises the outputs from the pre-programme design work and how they influenced the first vPMP. Based on the pre-programme design work, a consensus was reached to have five to six patients per programme. We planned three consecutive programmes over a 10- to 12-week period. Each programme was planned to be 3 weeks in duration (same as the face-to-face PMPs) maintaining individual sessions for 1:1 work mirroring the timetables of face-to-face PMPs. An evaluation week was planned after the first programme for interim data analysis and implementation of actions for QI. The first vPMP timetable was drawn up with days starting at 09:30 and ending at 16:30, Monday to Thursday (4 days per week). We planned to revisit the need for the vPMP after running three programmes considering the external environment with respect to the COVID pandemic.
Table 2.
First programme design table.
| Output from pre-programme design | Source | Implemented changes |
|---|---|---|
| Optimising the patients’ home environment for participation | Patient involvement exercise | • Written material for the programme was sent to participants in advance to allow preparation time. • Patients were asked to brainstorm adaptations to exercises within their home such as household items that can be used instead of gym equipment. |
| Interactive peer support | Patient involvement exercise PPA Webinar |
• A video-conferencing software with ‘breakout rooms’ was sought to facilitate interaction in small groups. • Each educational talk utilised the ‘breakout room’ function. • A virtual coffee morning session was introduced to facilitate participant interactions early in the programme. |
| Overcoming technical challenges | Patient involvement exercise | • Patients encouraged to seek troubleshooting support in the virtual coffee morning session. • All written materials including personal timetables and information packs were sent in advance to patients by email at least 1 week prior to the start of the programme. • Frequently asked questions (FAQs) on video-conferencing were created. • A specific email was created for patients to use to access staff and ask for any support. |
| Protecting staff communication time | Internal expert staff opinions | • Virtual meetings were left open for clinicians to be able to debrief with each other. |
| Training for staff | 1:1 Staff feedback | • Opportunities for shadowing and peer support provided within the programme for staff members to observe each other in the use of video-conferencing technology. • Drop-in training to address skill gaps was organised for staff. • FAQ sheets created for staff. |
Participants
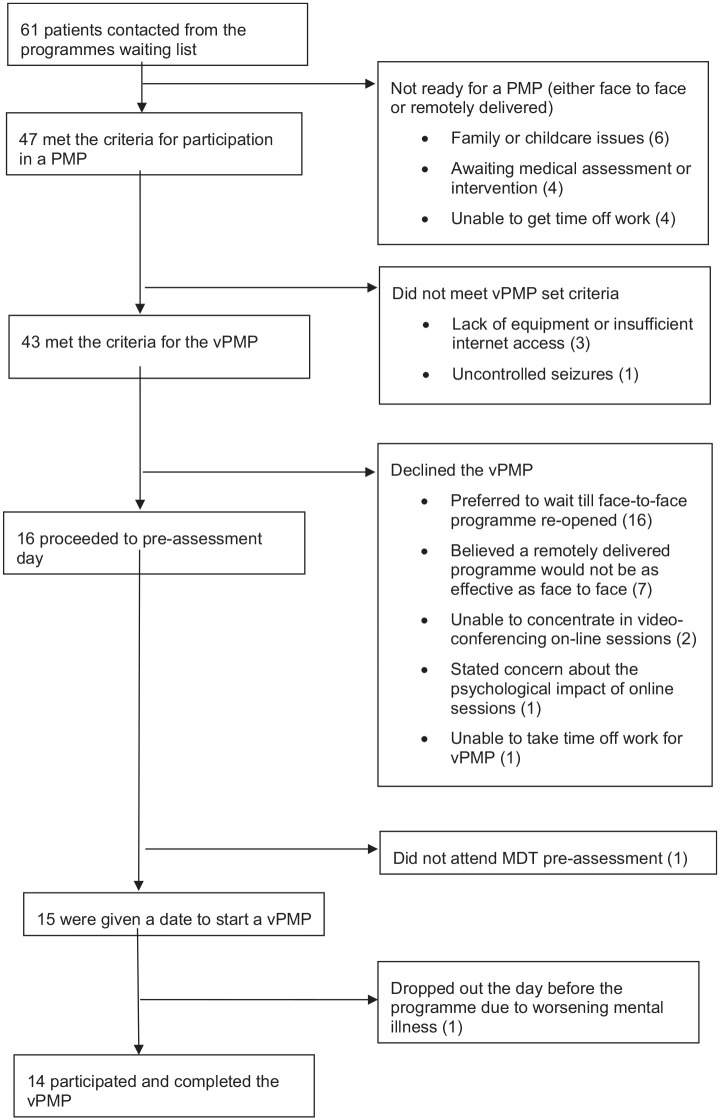
Sixty-one patients from programme waiting lists were called by a member of the therapy team and invited to consider participation on the vPMP. A checklist was completed at the time of the telephone call to ensure that patients met the vPMP criteria. Of the 61 people who were contacted, 43 met the criteria for the vPMP. Twenty-seven declined, 16 were enrolled on the programme and 14 completed it (see flow chart in Figure 1). Once 16 participants were enrolled, no more patients from the waiting list were contacted. Two patients did not attend the programme following enrolment.
Figure 1.
Participants’ flow chart.
The characteristics of the 14 patients who participated and completed the first three vPMPs are shown in Table 3. To determine whether this small group was representative of the patients on the PMP waiting list, this group was compared to 100 consecutive patients deemed ready for a face-to-face PMP who had been added to the waiting list prior to the COVID pandemic in 2019.
Table 3.
Participant characteristics.
| Parameter | vPMP participants (n = 14) | PMP participants in 2019 (n = 100) |
|---|---|---|
| Age (years), mean (SD) | 37.6 (12), range = 19–56 | 39 (15.7), range = 18–81 |
| Gender | 13 Female and 1 male | 91 Female and 9 male |
| Most significant chronic pain problem | Persistent widespread pain 11 (with hypermobility 8) Axial spine pain 0 Complex regional pain syndrome 1 Joint pain without instability 2 |
Persistent widespread pain 68 (with hypermobility 49) Axial spine pain 18 Complex regional pain syndrome 7 (with hypermobility 2) Joint pain 7 |
PMP: pain management programme; SD: standard deviation.
Age in vPMP participants was normally distributed at alpha significance level 0.05 (p = 0.4). There was no difference in mean age (independent t-test, p = 0.75) or gender ratios (chi-square test, p = 0.99) between the vPMP participants and patients who were on the waiting list for a face-to-face PMP. In both groups, the commonest significant pain problem was persistent widespread pain and a similar proportion of these had been diagnosed with joint hypermobility.
Evaluation and improvement of vPMP programmes
A summary of these appears in Table 4. The actions were mostly put forward by the patients or clinicians themselves. The vPMP clinicians noted the limitations of video-conferencing technology during the evaluations, notably the challenges of picking up on non-verbal communication cues and sensing participants’ emotions. No solutions to this were identified.
Table 4.
Programme improvements table.
| Output from real-time evaluations | Source | Implemented changes |
|---|---|---|
| Optimising the patients’ home environment for participation | 1:1 Patient feedback 1:1 Staff feedback |
• Patients were signposted to the resources that had been sent in advance throughout the education talks. • Patients suggested adaptations to exercises within their home, using household items in place of exercise equipment, e.g. cans or rice bags for hand weights. Lists of these were created for participants in future programmes. • Physical exercises were demonstrated by therapists in a well-lit room. For group exercise classes, a second therapist stayed by the screen and offered advice and technique corrections for patients. |
| Interactive peer support | 1:1 Feedback with patients Patient focus group |
• A voluntary ‘open room’ session was introduced at the end of each day for participants to meet to reflect on the day. • Meeting rooms were left open after group sessions to allow participants to congregate virtually and reflect on sessions together in the virtual space. |
| Overcoming technical challenges | 1:1 Feedback with patients | • Paper copies of all written patient resources were posted in advance to patients who requested them as well as emailed materials. • FAQs on video-conferencing were used and updated iteratively after each programme. • Patients were provided with a central contact email checked regularly by clinicians involved in the vPMP for technology-related queries. • Arrangements were made for real-time assistance for those struggling to join sessions. |
| Programme intensity – avoiding ‘video-conferencing fatigue’ | 1:1 Feedback with patients | • Session scheduling was changed so that they were spread more evenly across the week (first vPMP planned Monday to Thursday, changed to Monday to Friday thereafter). • Session start times were adjusted to ensure there were regular breaks between group sessions and individual sessions (first vPMP onwards). |
| Protecting staff well-being and communication | 1:1 Staff feedback | • An optional weekly staff mindfulness session was introduced. • Daily MDT ‘huddles’ between clinicians on the programme were timetabled to allow for frequent communication of any changes. |
| Training for staff | 1:1 Staff feedback | • Drop-in training to address skill gaps was organised for staff. • A list of essential staff skills was complied, e.g. including how to place participants into break out rooms and how to share presentations on the screen, as a resource for future new staff. |
In parallel to the vPMP design, the implementation team created an electronic version of the previously used paper outcome measures booklet. A fully digitalised means of collecting PROMs was not immediately available. The electronic version that was faithful to the questionnaires’ original formatting was sent to patients by email with their pre-programme information 1 week prior to the start date of the programme. They were able to fill this in online and return it by email. One patient was unable to complete it digitally and was asked to print it out to complete by hand and then return a photo of the completed version. All the questionnaires were returned.
Data collection for evaluation and QI continued until the end of the third vPMP cycle. At this stage, no further new comments were being identified through staff or participant feedback and no new changes were being proposed to improve the quality of vPMP delivery.
Discussion
We have described the design and implementation of a remotely delivered, live, interactive PMP using video-conferencing technology within a QI framework. The rapid introduction of this programme was driven by the needs of patients with chronic MSK pain during the COVID-19 pandemic which had a significant impact on patients’ ability to access relevant healthcare. 9 Our report demonstrates the elements that were needed for successful full implementation, in a way that meets the needs and expectations of the immediate stakeholders and also remains faithful to the published guidance on delivering PMPs.
PMPs are complex interventions and adapting them to a remote version necessitated changes to all aspects of service delivery. This complexity created an imperative to engage all stakeholders in the design of the vPMP, and we included not only clinical staff of all grades and disciplines but also the pain and rehabilitation administrative staff and operational managers in the design of the project. Drawing on a diverse skill mix meant expertise was shared and the whole patient pathway was considered.
A major strength of this project was the involvement of patients with lived experience of chronic MSK pain and PMPs from inception despite the tight timescales. This made a significant and direct contribution to the pre-programme design. Previous participants in the PMP were enthusiastic about the prospect of a remotely delivered programme and, encouragingly, did not express any doubts about its feasibility. Some of the themes, such as fostering peer support, creating mechanisms for direct access to the therapy staff and finding imaginative ways to compensate for lack of gym and exercise equipment in the home environment, were carried through into the PDSA cycles during the remote programmes. With further input from programme participants, these evolved into concrete additions to future programmes. For example, ice-breaker sessions became part of the vPMP routine timetable, additional means of communicating within the inter-disciplinary team were incorporated into our way of working, and a list of what household items could be used for exercise sessions found its way into the vPMP standard materials for participants. During the programmes, the qualitative nature of the evaluations enabled the 14 vPMP patient participants to not only evaluate the programme but also to make active contributions to design change. In this way, the programme participants became active co-designers with the therapy team throughout this project. Demographic comparisons show that this group were representative of the patient population who are put on the PMP waiting list in terms of age, gender distribution and pain condition.
The external expertise, accessed through the PPA Webinar, chimed with the opinions of internal expert staff and also with patient partner views which gave strength to the team’s design proposals. Many of the issues that came up in the pre-programme preparation phase of this project are aligned with other researchers’ findings on telehealth for rehabilitation. These include patient concerns about losses in supportive peer relationships and patient–therapist relationships, 10 lack of resources encompassing both IT equipment and exercise equipment, unfamiliarity with video-communication systems and the need for clinician training and infrastructure investment. 5 During the project, we were able to resolve many of these issues with input from all staff engaged in PMP delivery and the patients. An important factor in finding these solutions was the selection of an appropriate software programme with functionalities that could meet patient and clinician needs. Teleconference fatigue emerged as an important finding early in this project and has been recognised as a negative consequence of using video-technology. 11 Adapting the programme timetable to spread the sessions over a longer time period improved this in subsequent programmes.
In starting a remotely delivered interactive programme, we found that some expected investment was needed in terms of the provision of IT equipment and need for access to private office space. There was also need for further investment that was relatively unexpected. This included the addition of a second physiotherapist or therapy technician in each group session to trouble-shoot technical difficulties or contact absent participants. It is recognised that additional costs of changing from face-to-face to remote services are often unreported, but they affect potential savings and are important to commissioning decisions. 12 Collecting digital PROMs via email was deemed to be a feasible method for future online programmes. We found that it requires an administrator to take on the role of managing this process. Patients were not asked directly for feedback on this method of data collection, although it is widely accepted that the completion of PROMs can be burdensome. 13
Telehealth is often put forward as a means of improving access to medical services by overcoming geographical barriers and reducing the need to travel for appointments. It also offers greater flexibility to patients, helping circumvent problems such as having to secure childcare 14 or taking time away from work. During this project, however, we found that having to rely solely on telehealth could create inequity in access to healthcare: we had to exclude patients with particular medical conditions, and there were patients who were not able to join the vPMP cohort due to lack of home IT equipment or Internet access. The required broadband speed for a group video-conferencing call 15 is 3 Mbps, and Ofcom reports that 5% of the UK population do not have access to these speeds. 16 While we did not explore these issues in further detail in this study, these findings point towards imbalances in access to digitalised health systems that reflect known socio-economic inequalities in accessing digital services. 17 Telemedicine, including the use of video-conferencing, relies on patients having additional skills and may disproportionately increase the burden of treatment on those who are less competent with newer technologies. 18 We also found that telehealth did not help circumvent childcare and work absence issues for high intensity interventions: five of our patients declined the programme due to childcare issues and altogether five patients declined due to inability to take time off work. Interestingly, one person confided that they felt they would have got the time off work for a face to face programme but could not do so for an on-line one.
Limitations
As a rapidly implemented service improvement, our project had a number of limitations. The pre-programme patient involvement exercise and staff consensus work were not recorded or noted down verbatim. Instead, the facilitator and interviewers made detailed notes during interviews and focus groups. This has the potential to introduce confirmation bias as the data collector may consciously or subconsciously record comments and observations concordant with their own opinions. This was mitigated by the data collectors and analysers not being directly involved in the programme.
Although we involved patients with lived experience of chronic pain in the initial design of the vPMP project, we did not invite them to continue as part of the project team. This would have included being present in review meetings where we discussed patient and clinician feedback and generated real-time improvement actions. The need for rapid implementation of this programme, along with staff pressures meant that the team were not able to support the ongoing involvement of patient partners. We would acknowledge that such an approach would have aligned better with true co-production, 19 and we would recommend stronger patient partnerships in future work on remote programmes.
We did not use a quantitative measure for improvement. We recognise that we could have created a real-time log of reported problems and concerns to plot a run chart. However, the multiple avenues of data collection and the rapid nature of the changes, particularly during the first programme, made this impractical. We did reach a definitive quantitative end point at the end of the third vPMP, when comments and concerns had reached a saturation point and no further concerns with respect to the remote nature of the programme were being raised by either participants or clinicians.
As one of few PMPs with specific hypermobility pain management interest, our patient cohorts have a significant proportion of such patients. This is likely to be significantly lower in other PMPs. Therefore, certain aspects that needed additional consideration in our groups (e.g. joint subluxations and dislocations, and faints) may not be such an issue elsewhere.
Future considerations
Although remotely delivered psychological interventions have been shown to be effective in a number of settings including post-traumatic stress disorder (PTSD), 20 anxiety 21 and depression, 22 their non-inferiority compared to face-to-face treatment remains uncertain. Similarly, there is evidence for the effectiveness of remotely delivered exercise or exercise plus pain coping skills for people with chronic pain, but this does not support replacing usual care with remote delivery.23,24 The provision of virtual education has been shown to be feasible for patients with an MSK condition. 25
Over half of the patients on our PMP waiting list who met the criteria for the remote programme declined this intervention. We did not ask for a reason, but some explicitly stated that they did not believe it would be as effective as a face-to-face programme. In a qualitative study, Cranen et al. 10 explored the views of 25 adult chronic pain patients about potential telerehabilitation services. The patients placed higher value on face-to-face treatment, considering it more effective for both emotional support and feedback about the physical therapy aspects of the programme. None of the patients in this study expressed a preference for remotely delivered rehabilitation. If remotely delivered rehabilitation programmes are shown to be non-inferior to their face-to-face versions, both patient and clinician beliefs in respect to the effectiveness of this approach deserve further investigation.
The design of the vPMP was a pragmatic project, conducted at pace, in response to the COVID-19 pandemic. The provision of virtual programmes provided an opportunity to assess and rehabilitate patients in their home environment. Further research is required to determine how the use of remotely delivered services such as these can be integrated into a traditional face-to-face pathway beyond the COVID-19 pandemic. Future work should include a robust evaluation of outcomes, patient satisfaction and cost-effectiveness of remote programmes with both quantitative and qualitative methodology.
Conclusion
The COVID-19 pandemic has accelerated the provision and acceptability of telemedicine in all areas of healthcare including chronic pain management. 26 Despite the need and growing enthusiasm for telehealth, there is a paucity of evidence and expertise on remote PMPs.
This article demonstrates the feasibility of delivering a PMP using video-conferencing technology that is fully in line with current evidence-based guidelines. We have described the process of development using the Model for Improvement Framework with active patient involvement. Analysis of the data that we collected during this process also provides important findings related to cost, patient experience, patient preferences and inequities of access in delivering telerehabilitation.
Acknowledgments
The authors thank all of the patients and staff who contributed to the design and development of this project, embracing change in uncertain times. The authors also thank the RNOH Research and Innovation Centre and the pain and rehabilitation operational management teams especially Catherine Buckley and our co-ordinator Mrs Hemal Mehta for all of their support during this project.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Contributorship: H.C., A.G., A.L., G.M., H.P., M.P., W.R., D.W. and R.Z. were all involved in the development of the quality improvement project. G.B., T.P., D.W. and H.P. were involved in patient engagement. G.B., T.P. and C.M. collected and analysed the qualitative data. H.P., M.P. and R.Z. gathered and analysed quantitative data. D.W. wrote the first draft of the manuscript with A.G. and R.Z. All authors reviewed, edited and approved the final version of the manuscript. D.W. is listed as the first author and R.Z. as the last author. The remaining authors are listed in alphabetical order.
Ethical approval: This project was submitted to the Trust’s Research and Development Project Evaluation Panel. The project was classified and registered as a service evaluation (registration reference no. SE20.31).
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from the patients for their anonymised information to be published in this article.
ORCID iDs: Deborah Williams  https://orcid.org/0000-0003-2935-0621
https://orcid.org/0000-0003-2935-0621
Gregory Booth  https://orcid.org/0000-0003-3332-1890
https://orcid.org/0000-0003-3332-1890
Anthony Gilbert  https://orcid.org/0000-0003-2526-8057
https://orcid.org/0000-0003-2526-8057
References
- 1.Fayaz A, Croft P, Langford RM, et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 2016; 6: e010364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.British Pain Society. Guidelines for pain management programmes in adults, https://www.britishpainsociety.org/static/uploads/resources/files/pmp2013_main_FINAL_v6.pdf (2013, accessed 10 December 2020).
- 3.Lynch ME, Campbell F, Clark AJ, et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain 2008; 136(1–2): 97–116. [DOI] [PubMed] [Google Scholar]
- 4.Fallon N, Brown C, Twiddy H, et al. Adverse effects of COVID-19 related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Br J Pain 2020; 15: 357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walumbe J, Belton J, Denneny D. Pain management programmes via video conferencing: a rapid review. Scand J Pain 2020; 21(1): 32–40. [DOI] [PubMed] [Google Scholar]
- 6.Booth G, Williams D, Patel H, et al. What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review. Br J Pain. Epub ahead of print 13 June 2021. DOI: 10.1177/20494637211023074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Physiotherapy Pain Association. Online pain management groups, https://ppa.csp.org.uk/publications/ppa-webinar-online-pain-management-groups (accessed 30 May 2020).
- 8.Langley GL, Moen R, Nolan KM, et al. The improvement guide: a practical approach to enhancing organizational performance, 2nd edn. San Francisco, CA: Jossey-Bass, 2009. [Google Scholar]
- 9.Faculty of Pain Medicine of the Royal College of Anaesthetists. An update from the FPM and BPS to those waiting to access pain services 2020, https://fpm.ac.uk/update-fpm-and-bps-those-waiting-access-pain-services (accessed 8 May 2021).
- 10.Cranen K, Drossaert CH, Brinkman ES, et al. An exploration of chronic pain patients’ perceptions of home telerehabilitation services. Health Expect 2012; 15(4): 339–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiederhold BK. Connecting through technology during the coronavirus disease 2019 pandemic: avoiding ‘Zoom fatigue’. Cyberpsychol Behav Soc Netw 2020; 23(7): 437–438. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert AW, Billany JC, Adam R, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual 2020; 9(2): e000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bodart S, Byrom B, Crescioni M, et al. Perceived burden of completion of patient-reported outcome measures in clinical trials: results of a preliminary study. Ther Innov Regul Sci 2019; 53(3): 318–323. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez R, Sayed Y, Atassi S, et al. Why patients miss their appointments: a survey. Donn J Dentist Oral Hyg 2018; 4(2): 009–014. [Google Scholar]
- 15.System requirements for Zoom rooms, https://support.zoom.us/hc/en-us/articles/204003179-System-requirements-for-Zoom-Rooms (accessed 10 January 2021).
- 16.UK home broadband performance: the performance of fixed-line broadband delivered to UK residential customers, https://www.ofcom.org.uk/__data/assets/pdf_file/0038/194897/uk-home-broadband-performance.pdf (accessed 10 January 2021).
- 17.Yoon H, Jang Y, Vaughan PW, et al. Older adults’ Internet use for health information: digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol 2020; 39(1): 105–110. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert AW, Jones J, Jaggi A, et al. Use of virtual consultations in an orthopaedic rehabilitation setting: how do changes in the work of being a patient influence patient preferences? A systematic review and qualitative synthesis BMJ Open 2020; 10: e036197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf 2016; 25(7): 509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolton AJ, Dorstyn DS. Telepsychology for posttraumatic stress disorder: a systematic review. J Telemed Telecare 2015; 21(5): 254–267. [DOI] [PubMed] [Google Scholar]
- 21.Berryhill MB, Halli-Tierney A, Culmer N, et al. Videoconferencing psychological therapy and anxiety: a systematic review. Fam Pract 2018; 36(1): 53–63. [DOI] [PubMed] [Google Scholar]
- 22.Berryhill MB, Culmer N, Williams N, et al. Videoconferencing psychotherapy and depression: a systematic review. Telemed J E Health 2019; 25(6): 435–446. [DOI] [PubMed] [Google Scholar]
- 23.Adamse C, Dekker-Van Weering MG, van Etten-Jamaludin FS, et al. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare 2018; 24(8): 511–526. [DOI] [PubMed] [Google Scholar]
- 24.Bennell KL, Nelligan R, Dobson F, et al. Effectiveness of an Internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain. Ann Inter Med 2017; 166(7): 453–462. [DOI] [PubMed] [Google Scholar]
- 25.Warmington K, Flewelling C, Kennedy CA, et al. Telemedicine delivery of patient education in remote Ontario communities: feasibility of an Advanced Clinician Practitioner in Arthritis Care (ACPAC)-led inflammatory arthritis education program. Open Access Rheumatol 2017; 9: 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020; 161(5): 889–893. [DOI] [PMC free article] [PubMed] [Google Scholar]