Abstract
It is now well established that ischemia/reperfusion (I/R) injury is associated with the compromised recovery of cardiac contractile function. Such an adverse effect of I/R injury in the heart is attributed to the development of oxidative stress and intracellular Ca2+-overload, which are known to induce remodeling of subcellular organelles such as sarcolemma, sarcoplasmic reticulum, mitochondria and myofibrils. However, repeated episodes of brief periods of ischemia followed by reperfusion or ischemic preconditioning (IP) have been shown to improve cardiac function and exert cardioprotective actions against the adverse effects of prolonged I/R injury. This protective action of IP in attenuating myocardial damage and subcellular remodeling is likely to be due to marked reductions in the occurrence of oxidative stress and intracellular Ca2+-overload in cardiomyocytes. In addition, the beneficial actions of IP have been attributed to the depression of proteolytic activities and inflammatory levels of cytokines as well as the activation of the nuclear factor erythroid factor 2-mediated signal transduction pathway. Accordingly, this review is intended to describe some of the changes in subcellular organelles, which are induced in cardiomyocytes by I/R for the occurrence of oxidative stress and intracellular Ca2+-overload and highlight some of the mechanisms for explaining the cardioprotective effects of IP.
Keywords: ischemia-reperfusion injury, subcellular remodeling, ischemic preconditioning, cardioprotection, oxidative stress, intracellular Ca2+-overload
1. Introduction
Although myocardial ischemia due to a partial or complete blockage of the coronary artery is known to induce marked changes in cardiac function and metabolism, as well as the ultrastructural integrity of cardiomyocytes [1,2], the pathophysiological mechanisms that lead to contractile dysfunction and derangement of cardiac structure are not fully understood. While coronary reflow to the ischemic heart is helpful for the recovery of contractile function, reperfusion after a certain period of prolonged ischemia exacerbates damage to the heart [3,4,5,6,7,8]. Two major abnormalities, namely intracellular Ca2+-overload and oxidative stress, are considered to play a critical role in cardiac contractile dysfunction subsequent to ischemia/reperfusion (I/R) or hypoxia–reoxygenation injury. In this regard, the beneficial effects of Ca2+-antagonists [9,10] and Na+-H+ exchange inhibitors [11,12,13,14] support the role of intracellular Ca2+-overload [15,16,17,18,19,20,21], whereas the beneficial effects of antioxidants [4,5] suggest the role of oxidative stress in the pathophysiology of ischemia–reperfused hearts. It is pointed out that alterations in the function of different subcellular organelles such as sarcolemma (SL), sarcoplasmic reticulum (SR), myofibrils and mitochondria due to I/R injury have been demonstrated to be associated with depression in cardiac contractile activity, the development of intracellular Ca2+-overload and the occurrence of oxidative stress [4,5]. It is also known that repeated episodes of brief ischemia followed by reperfusion, which is referred as ischemic preconditioning (IP), attenuates subcellular organelle remodeling due to subsequent I/R [22,23]. This review is designed to examine the information regarding the effects of IP on the development of oxidative stress and intracellular Ca2+-overload with respect to the modification of subcellular defects due to I/R injury [4,5]. In particular, some of the mechanisms of beneficial action of IP on molecular and functional changes for Ca2+-handling by subcellular organelles will be described in hearts subjected to I/R injury. Furthermore, the effects of IP on some factors, such as inflammatory cytokines and proteolytic activities, as well as the nuclear factor erythroid factor 2 (Nrf2) signal transduction pathway, which are known to modulate subcellular defects due to I/R injury, will be outlined. The generation of reactive oxygen species (ROS) and subsequent oxidative stress is known to increase apoptosis [24], necrosis [24,25], inflammation [24] and impair mitochondrial function [26,27]. In fact, IP has been demonstrated to attenuate the I/R-induced defects [28,29,30,31]. Thus, it can be seen that the generation of ROS has marked detrimental impacts on cardiomyocyte function and that IP may provide protection against oxidative stress. Therefore, the focus of this review is on the protective effects of IP on the I/R-induced defects in the heart.
2. Alterations in Cardiac SL and SR Ca2+-Transporting Activities Due to I/R
In order to understand the importance of the beneficial actions of IP with respect to Ca2+-homeostasis in cardiomyocytes, it is necessary to describe the impact of I/R on the Ca2+-handling properties of the two major subcellular organelles, namely SL and SR. It has become evident that ROS and other oxidant molecules are involved in the genesis of intracellular Ca2+-overload, myocardial cell damage and subsequent contractile dysfunction due to I/R injury [3,4,5,32]. Electron paramagnetic resonance spectroscopic studies have revealed the generation of ROS during reperfusion of the ischemic heart [33,34,35]. Dysregulation of cardiomyocyte Ca2+-movements in response to excessive ROS generation and the inability of cardiomyocytes to scavenge ROS by endogenous antioxidant systems (a state of oxidative stress) results in the development of intracellular Ca2+-overload subsequent to I/R injury [36,37,38,39]. Since SL Ca2+-channel density has been reported to decrease due to hypoxia/regeneration and myocardial ischemia [40,41], or when SL membranes are treated with oxyradicals [42], this mechanism cannot be seen to account for the occurrence of intracellular Ca2+-overload, as it would decrease Ca2+-influx. On the other hand, the activities of both SL Na+-Ca2+ exchange and the SL Ca2+-pump have been observed to be markedly reduced subsequent to hypoxia or I/R injury [43,44,45], as well as when heart membrane preparations are exposed to oxyradicals [46,47,48,49]; these alterations would decrease in Ca2+-efflux and have been suggested to produce intracellular Ca2+-overload. Other SL activities, such as Na+-K+-ATPase, Ca2+/Mg2+ ecto-ATPase and superficial store of Ca2+ [49,50,51,52,53,54,55,56,57,58,59] are also affected by ROS and oxidant molecules and are considered to increase Ca2+-influx in the cell indirectly. It should be noted that the actions of ROS as well as I/R injury on the SL Na+-Ca2+ exchange, Na+-K+-ATPase and Ca2+/Mg2+ ecto-ATPase seem to depend on the type of oxyradical generating system and the time of exposure to these interventions [37,48,49,60,61,62]. It should be noted that several other SL defects are also known to occur in hearts subjected to I/R or exposure of heart membranes to oxyradicals and oxidant molecules; these include SL Ca2+ transporters [63,64,65,66], ATP-receptors, β-adrenoceptors, G-proteins, adenylyl cyclase, phospholipases, as well as alterations in membrane permeability [67,68,69,70,71,72,73,74,75,76,77,78,79,80] and loss of dystrophin [81,82]. From these observations, it is evident that the increase in the formation of ROS and oxidants in ischemic hearts upon reperfusion may induce a number of different and complex defects in the SL membrane for modifying Ca2+-fluxes, but on balance would result in the development of intracellular Ca2+-overload in cardiomyocytes. It should also be mentioned that oxidative stress generated due to I/R injury has been shown to cause alterations in excitation–contraction coupling as well as induce cardiac arrhythmias, heart dysfunction and myocardial cell damage [83,84,85,86,87,88,89].
Changes in SR Ca2+- transporting activities are also known to occur under conditions of I/R as well as upon exposure of the heart to different oxidant molecules. In this regard, a reduced ability of cardiac SR Ca2+-uptake due to oxyradicals has been attributed to attenuation of Ca2+-stimulated ATPase activities [90,91,92]. A progressive loss of Ca2+-release channels has also been observed following exposure of the SR to ROS [93], but this may not represent the status of Ca2+-release from SR under the in vivo situations for oxidative stress. The rotenone-insensitive NADH cytochrome C reductase activity of the cardiac SR has also been reported to be reduced in response to oxyradicals and has been linked to SR lipid peroxidation [57]. Although ATP-dependent Ca2+-uptake and Ca2+-stimulated ATPase activities of skeletal muscle SR are depressed by ROS, this effect was suggested to be due to the inhibition of the sulfhydryl groups of the Ca2+-pump ATPase rather than membrane lipid peroxidation [94,95]. Interestingly, activated neutrophils, which are known to suppress the contractile force development of the heart [96], are considered to decrease the SR Ca2+-pump activities due to the generation of oxidants [97]. Overall, these alterations due to I/R injury can be seen to contribute to the occurrence of intracellular Ca2+-overload in cardiomyocytes. It is therefore clear that several subcellular Ca2+-handling proteins can be targeted as mechanisms for defects in SL and SR Ca2+-handling activities and inducing intracellular Ca2+-overload due to I/R injury. Furthermore, it should also be pointed out that cardiac dysfunction due to I/R injury is not limited to defects in SL and SR membranes but to other subcellular organelles such as the mitochondria, myofibrils and extracellular matrix, which are also affected in inducing myocardial abnormalities [4,5,20,21,22,23,32].
3. Subcellular Modification Due to Ischemic Preconditioning
It has been demonstrated that IP limits the infarct size, and attenuates necrosis, apoptosis as well as cardiac dysfunction due to I/R injury [98,99,100,101,102,103]. These beneficial effects of IP are reported to be mediated through the activation of adenosine receptors [99] and protein kinase C activity [101,104,105,106,107], as well as due to reduced phospholipase activities [108] and the attenuation of TNF-α levels [109].
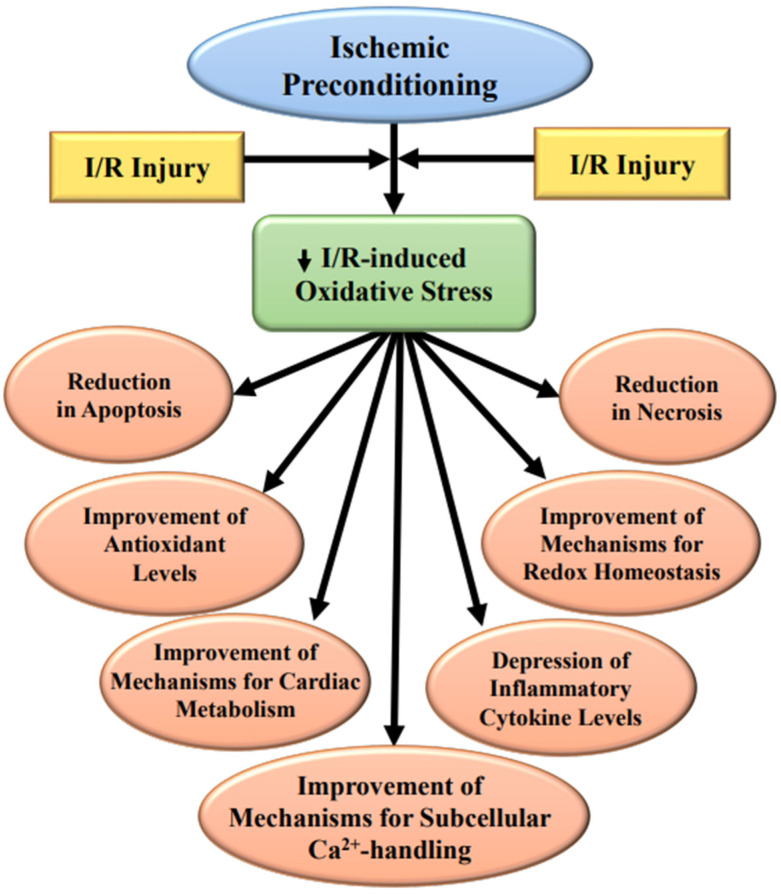
The glycocalyx is particularly susceptible to I/R injury, as it is the first to be exposed to ROS, but IP has been shown to provide partial protection [110]. Furthermore, IP attenuates the cleavage of myofilament troponin I by matrix metalloprotease 2 (MMP-2) [111] upon decreasing its release and activation due to I/R injury. It is pointed out that the activation and release of MMP-2 are directly correlated with cardiac dysfunction due to I/R injury [111,112], and these alterations have been suggested to be due to the formation of hydroxy radicals and peroxynitrite, which have been shown to cause myofibril damage [113]. IP has also been observed to be protect the cytoskeleton from I/R-induced damage due to the activation of the ROS-p38 MAPK-HSP 27 pathway that initiates actin filament polymerization, as well as increases the stability of the contractile apparatus [114,115,116]. It is therefore evident that IP induces cardioprotective actions against the I/R-induced abnormalities by reducing the development of oxidative stress and associated defects. Some of the parameters affected by IP in ischemic–reperfused hearts are depicted in Figure 1.
Figure 1.
Alterations in some ischemia–reperfusion induced (I/R) parameters in hearts subjected to ischemic preconditioning.
3.1. Protection of the SL Defects
There are a variety of receptors and ion channels/pumps located in the SL membrane that are considered to influence cardiomyocyte function through the activation of downstream signal transduction processes and are affected by I/R injury, and thus may serve as targets for providing cardioprotection in IP. For example, the activation of several different receptor types, including adenosine receptors [117], angiotensin II receptors [102,118,119], α1- adrenoceptor [120,121] and opioid receptors [122,123], have been shown to be involved in the initiation of cardioprotective mechanisms in response to IP. During ischemia, there is an increase in the cardiomyocyte concentration of Na+ due to the exchange with protons via the activation of the SL Na+-H+ exchanger (NHE), which causes the activation of the SL Na+-Ca2+ exchanger in reverse mode, resulting in an increase in the intracellular Ca2+-concentration [124]; thus, the inhibition of NHE has been observed to attenuate intracellular Ca2+-overload [125]. The beneficial actions of IP have been suggested to involve a reduction in the activation of NHE.
The Na+-K+-ATPase (sodium pump) is known to play an important role in the maintenance of the membrane potential and cation transport across the SL membrane [126]; specifically, Na+-K+-ATPase activity directly maintains intracellular Na+ and K+ concentrations as well as indirectly maintains intracellular Ca2+-concentration [127]. The α subunit of Na+-K+-ATPase is the catalytic domain and occurs in three isoforms: α1 is the most abundant but with a lower affinity for cardiac glycosides, as compared to the α2 and α3 subunits [128], while the β-subunit (also three isoforms) confers SL localization and insertion into the SL membrane. I/R has been reported to diminish Na+-K+-ATPase activity [129] and contribute to cardiac dysfunction. Thus, Na+-K+-ATPase can be considered as a viable mechanism for cardioprotection due to IP. In this regard, a reduction of the intracellular Ca2+-concentration has been reported to be due to the IP-induced preservation of Na+-K+-ATPase activity in the I/R hearts [52]. It should be mentioned that the Na+-K+-ATPase is considered to play a signaling function [130,131,132,133,134] and may act as a receptor transducing humoral signal [134]. Since ouabain activates several pathways that are involved in cardioprotection by IP, it has been suggested that protection against I/R injury by IP may involve the activation of the Na+-K+-ATPase/cSrc receptor complex and the subsequent stimulation of the key signaling mediators [135,136]. The reduction of infarct size due to IP is also considered to be due to Na+-K+-ATPase-mediated opening of the cardiac SL K+-ATP channels [137] and the subsequent reduction on the intracellular Ca2+-concentration, although these effects have been suggested to involve the mitochondrial K+-ATP channels [138].
It is pointed out that cardiac SL K+-ATP channels and the mitochondrial K+-ATP channels have been extensively studied in the cardioprotective effects of IP. Although it is now generally believed that the mitochondrial K+-ATP channels play a more significant role in the beneficial effects of IP, the SL K+-ATP channels have increased in importance for inducing the harmful effects of oxidative stress [139]. Earlier observations have revealed that the beneficial actions of IP may involve the SL K+-ATP channels because they are in an open state when exposed to ROS and this correlated well with the cytoprotective properties [140,141,142,143]. Subsequent studies demonstrated that the SL K+-ATP channels appear to act as an effector of IP and facilitated in improving functional recovery. This proposition was evident when the cardioprotective effects induced by the activation of the SL K+-ATP were observed in the stress period, but not during IP. On the other hand, by using isolated adult rat cardiomyocytes and an isoflurane-induced protection technique, both SL and mitochondrial K+-ATP channels were observed to participate in the IP-induced cardioprotection [144].
It should also be mentioned that the beneficial actions of IP have been reported to be lost in a cardiac specific Kir 6.2 (the pore subunit of SL K+-ATP channels) knockout mouse model [145]. It has also been shown that activated SL K+-ATP channels are important in preventing cardiomyocyte apoptosis and mitochondrial damage during oxidative stress, as inhibition of SL K+-ATP channels promoted oxidative stress-induced apoptosis. Mitochondrial Ca2+-loading has been reported to be markedly increased upon the inhibition of SL K+-ATP channel in cultured HL-1 and neonatal cardiomyocytes [146]. Taken together, it is evident that reduction in oxidative stress-induced alterations of the SL membrane plays an important role in cardioprotection by IP.
3.2. Protection for the SR Defects
Under conditions of I/R and/or oxidative stress marked changes in SR Ca2+-transport are associated with increase in the cytosolic Ca2+ level and decreasing ATP causing damage to the cell [147,148,149,150]. Decreases in the SR Ca2+-cycling protein mRNA levels due to I/R have also been demonstrated; however, IP has been shown to attenuate these changes by preventing the development of intracellular Ca2+ overload and thereby maintaining SR function [151,152]. It should be mentioned that ROS exert direct effects on SERCA 2 (SR Ca2+-stimulated-ATPase) by decreasing its activity and causing an increase in the SL Na+-Ca2+ exchanger (NCX) activity. These observations indicate that redox-dependent SR Ca2+ depletion may be partly affected by a reciprocal regulation of SERCA 2 and NCX [153]. Furthermore, the modification of –SH groups under conditions of oxidative stress have also been shown to compromise Ca2+-stimulated ATPase activity [154]. On the other hand, the oxidation of the –SH groups of SR ryanodine receptors (RyRs) are an important mechanism of IP for attenuating the I/R-induced intracellular Ca2+-overload [155].
3.3. Protection of the Mitochondrial Defects
There is a wealth of information available in the literature regarding the role of mitochondrial alterations in IP-induced cardioprotection in I/R hearts. [37,156,157,158]. The mitochondria are of particular interest because of their involvement in cell apoptosis and ROS generation. The major mechanism of cardioprotection related to this organelle is the closing of mitochondrial permeability pores and subsequent maintenance of the inner membrane potential and energy production [15,159]. As already mentioned, the mitochondrial K+-ATP channel acts not only as an effecter of IP, but also as a trigger, suggesting that its activation is required for both IP as well as during exposure to oxidative stress [153]. Of note, unlike the SL K+-ATP channel, the mitochondrial K+-ATP channel has been reported to primarily have an effect on the infarct size [153]. Pharmacological preconditioning of the rat heart with diazoxide results in the opening of the mitochondrial K+-ATP channel, which protects against ischemia-induced ventricular arrhythmias [160]. ROS released from the mitochondria during IP causes the opening of the mitochondrial K+-ATP channels, which is protective [161]. It is thus apparent that mitochondrial K+-ATP channels play an important role in IP-induced cardioprotection against I/R injury. On the other hand, donors of nitroxyl (the one-electron reduced form of nitric oxide) have been shown to provide protection against I/R injury in a manner similar to IP [162], with the translocation of PKCε to the mitochondria, but without the activation of the mitochondrial K+-ATP channels [163].
During IP, the mitochondria also undergo other modifications. In this regard, IP increases the expression level of manganese superoxide dismutase (MnSOD) via the formation of NFκB and activator protein-1 (AP-1) [164]. The increased production of oxyradicals may impair mitochondrial function, as an increase in the production of ATP has been observed in preconditioned hearts [165]. Although the ROS-induced opening of the mitochondrial permeability transition pore (mPTP) results in a further release of ROS [5,166,167], IP prevents the mPTP from opening and attenuates the burst of the ROS and the subsequent oxidative stress [5,166]. It has also been suggested that IP may cause a gradual activation of mitochondrial function that may avoid the ROS bursts and occurrence of mitochondrial Ca2+ overload [168].
It needs to be emphasized that complex I (NADH ubiquinone oxidoreductase) is the point of entry of the electron into the mitochondria and is a major site of ROS generation [168,169]. An increase in the NADH/NAD+ redox balance has been shown to inhibit the opening of the mPTP [169,170]. IP and NO∙ have both been observed to inhibit complex I activity and thus diminish ROS generation [169]. Interestingly, the inhibition of complex II has been reported to open the mitochondrial K+-ATP channel and result in cardioprotection [169,171]. Glyceraldehyde 3-phosphate dehydrogenase has also been observed to be inhibited by IP [172,173]. This action results in the accumulation of fructose-1,6-bisphosphate, which has been reported to improve glycolytic flux and functional recovery in post-ischemic myocardium [174]. Furthermore, lactate, which is known to accumulate in the ischemic heart, was observed to be markedly reduced in IP [174]. These findings demonstrated that IP can inhibit glycolysis and thereby prevent acidosis [169]. It should also be mentioned that the translocation of hexokinase from the cytosol to the mitochondrial compartment has been shown to occur in IP, which attenuates cytochrome c release and ROS production [175,176]. Overall, it is becoming clear that oxidative stress generated by the mitochondria may result in mitochondrial Ca2+-overload and the impairing of their function. These mitochondrial defects are attenuated by IP through the participation of diverse mechanisms.
3.4. Evidence for Attenuation of I/R-Induced SL and SR Defects by IP
While the aforementioned has described the IP-induced cardioprotection of subcellular organelle defects due to I/R, we have earlier examined some of the SL and SR mechanisms for cardioprotection induced by IP. Specifically, the effects of IP on Na+-K+-ATPase mRNA levels, protein contents and activity have been reported. Based on the analysis of information in our paper [52], while I/R attenuated Na+-K+-ATPase mRNA and protein levels as well as the activity, IP reduced the I/R-induced changes, demonstrating that cardioprotection due to IP involves maintenance of Na+-K+-ATPase. Table 1 shows the effect of IP (three cycles of 10 min ischemia/10 min reperfusion) on Na+-K+-ATPase activity and Na+-K+-ATPase isoform (α1, α2, α3) protein contents and mRNA levels in the I/R hearts [52]. In addition, we also explored the effects of IP on the Ca2+-handling properties of hearts subjected to a prolonged period of I/R. From the data in Table 2 showing SR Ca2+-release and Ca2+-uptake activities, as well as SR Ca2+-stimulated ATPase activity in preischemic, ischemic and ischemic–reperfused control and preconditioned hearts, it has been suggested that IP prevents cardiac contractile dysfunction by protecting SR Ca2+ movements in cardiomyocytes [151]. In addition, the protective effect of IP on SR gene expression in the I/R hearts is shown in Table 3 [152]. Based on the information in our papers [151,152], it is thus also evident that the beneficial actions of IP have been attributed, in part, to protecting SR Ca2+ movements by reducing the development of I/R-induced oxidative stress in cardiomyocytes. These earlier findings provide evidence that an attenuation of the I/R-induced defects in both the SL and the SR can be considered as important mechanisms for the beneficial actions of IP-induced cardioprotection.
Table 1.
Effect of ischemic preconditioning on Na+-K+-ATPase activities, protein contents and mRNA levels.
| Control | IP | I/R | IP + I/R | |
|---|---|---|---|---|
| Na+-K+-ATPase activity (µmol Pi/mg/h) | 15.0 ± 0.6 | 14.8 ± 0.8 | 11.3 ± 0.7 * | 15.4 ± 0.7 # |
| Protein content (arbitrary units) | ||||
| Na+-K+-ATPase α1 | 15.7 ± 1.3 | 15.0 ± 2.1 | 11.2 ± 1.4 * | 13.2 ± 1.8 |
| Na+-K+-ATPase α2 | 7.3 ± 1.8 | 7.1 ± 1.3 | 2.1 ± 1.5 * | 6.2 ± 1.1 # |
| Na+-K+-ATPase α3 | 2.3 ± 0.2 | 2.2 ± 0.5 | 0.8 ± 0.4 * | 1.4 ± 0.5 # |
| mRNA expression levels (% of control arbitrary units) | ||||
| Na+-K+-ATPase α1 | 100 | 140 ± 11 * | 79 ± 3 * | 95 ± 2 |
| Na+-K+-ATPase α2 | 100 | 90 ± 5 | 51 ± 4 * | 78 ± 4 # |
| Na+-K+-ATPase α3 | 100 | 100 ± 20 | 32 ± 5 * | 61 ± 12 # |
Ischemic preconditioning was 3 cycles of 10 min ischemia/10 min reperfusion. Values for Na+-K+-ATPase activity are means ± 12–18 hearts in each group. For Western blot determination of protein contents, each protein sample was a collection of three hearts. Northern blot analysis was conducted using 18S mRNA level as internal standard and each value is the mean ±SE of 6 hearts/group. Control value is taken as 100% for each gene under different condition. * p < 0.05 vs. control. # p < 0.05 vs. I–R. Data are based on the analysis of information in our paper Elmoselhi et al. [52]. IP = ischemic preconditioning; I/R = ischemia/reperfusion.
Table 2.
SR Ca2+-release and -uptake activities and SR Ca2+-stimulated ATPase activity in preischemic, ischemic and ischemic–reperfused control and preconditioned hearts.
| SR Ca2+-Release (nmol/mg/15 s) | Preischemia | Postischemia | Reperfusion |
|---|---|---|---|
| Control | 17.5 ± 5.1 | 2.0 ± 0.5 # | 2.5 ± 0.5 # |
| Precondition | 6.7 ± 5.2 * | 7.3 ± 2.2 * | 11.2 ± 4.5 * |
| SR Ca2+-uptake (nmol/mg/min) | |||
| Control | 70.8 ± 8.1 | 8.0 ± 1.1 # | 9.5 ± 2.0 # |
| Precondition | 38.6 ± 6.4 * | 28.3 ± 3.7 * | 24.5 ± 1.5 * |
| SR Ca2+-stimulated ATPase activity (nmol Pi/mg/min) | |||
| Control | 199.8 ± 28.4 | 102.0 ± 20.4 @ | 65.5 ± 13.4 @ |
| Precondition | 201.4 ± 16.9 | 203.5 ± 26.4 ! | 146.1 ± 19.6 ! |
The SR Ca2+-release is the EGTA-induced Ca2+-release from Ca2+-loaded SR vesicles; Ca2+-uptake is the oxalate-supported Ca2+-uptake in SR vesicles in the presence of ruthenium red. Values are means ±SE of 6 different preparations for each time point for each group. * p < 0.05 vs. corresponding control value. # p < 0.05 vs. preischemic group. Ca2+-stimulated ATPase activity was calculated from the difference between values in the presence and absence of 10 µM Ca2+. ! p < 005 compared with respective control value. @ p < 0.05 compared with preischemic control value. Data are based on the analysis of information in our paper Osada et al. [151].
Table 3.
Effect of ischemic preconditioning on SR gene expression and relative protein contents in the I–R hearts.
| A: mRNA Expression Levels (% of Control Arbitrary Units) |
IP | I/R | IP + I/R |
|---|---|---|---|
| RyR | 68.2 ± 4.4 * | 35.7 ± 4.2 * | 72.1 ± 4.7 *,# |
| SERCA | 76.9 ± 4.9 * | 70.8 ± 2.4 * | 90.3 ± 3.4 *,# |
| PLB | 74.1 ± 3.2 * | 40.6 ± 3.6 * | 67.5 ± 4.8 *,# |
| Calsequestrin | 100 ± 3.5 | 50.8 ± 4.5 * | 71.8 ± 6.4 *,# |
|
B: Relative protein content
(% of control arbitrary units) |
|||
| RyR | 73.4 ± 8.2 * | 51.7 ± 9.1 # | 923 ± 8.6 * |
| SERCA | 101.1 ± 18.1 | 45.4 ± 2.2 # | 81.2 ± 17.1 * |
| PLB | 118.1 ± 19.2 | 100.3 ± 18.3 | 105.5 ± 19.4 |
| Calsequestrin | n.d. | n.d. | n.d. |
Ischemic preconditioning was 3 cycles of 5 min ischemia/5 min reperfusion. (A) Northern blot analysis was conducted using 18S mRNA level as internal standard. (B) Determination of protein contents was conducted by Western blot analysis. Each value is the mean ± SE of 6 hearts/group in the case of mRNA analysis and 6 different SR preparations in the case of analysis of protein contents. Values are expressed as a percentage of control values. Control value is taken as 100% for each gene/protein under different condition. * p < 0.05 vs. control. # p < 0.05 vs. I–R. Data are based on the analysis of information in our papers Osada et al. [151] and Temsah et al. [152]. IP = ischemic preconditioning; I/R = ischemia/reperfusion; RyR = ryanodine receptor; SERCA = sarcoendoplasmic reticulum calcium transport ATPase; PLB = phospholamban; n.d., not determined.
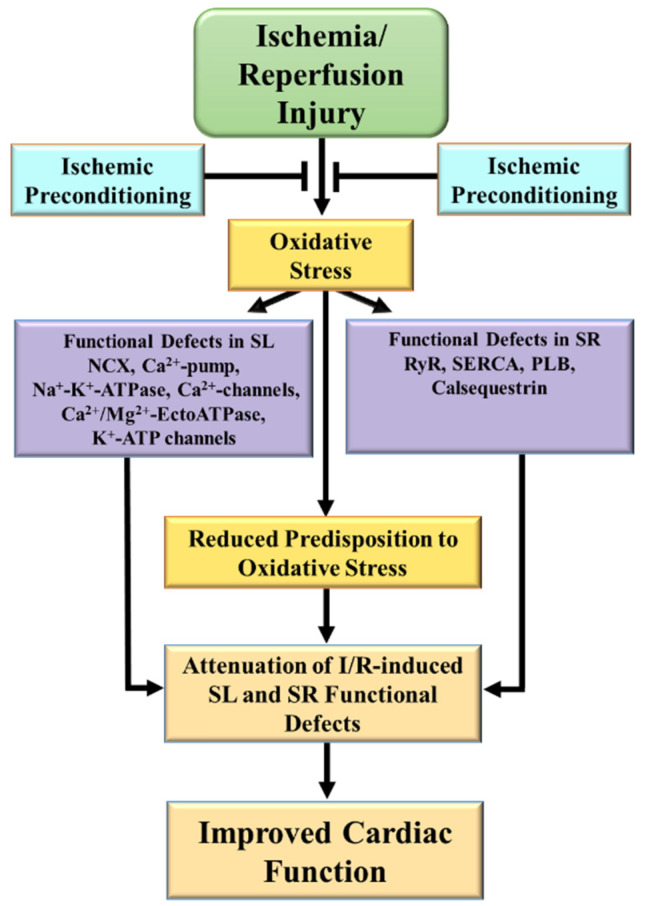
It should be pointed out that the expression and activities of different SL and SR proteins are altered in I/R, which are attenuated by IP [22,23,78,79,108,177], some of which are presented in Table 1 and Table 3. Figure 2 summarizes the functional defects of the SL and SR due to the oxidative stress induced by I/R, and that IP attenuates these defects associated with improved recovery of cardiac function.
Figure 2.
Functional defects the sarcolemma and sarcoplasmic reticulum membrane compartments due to ischemia/reperfusion and protective effects of ischemic preconditioning. SL = sarcolemma; SR = sarcoplasmic reticulum; NCX = Na+-Ca2+-exchanger; RyR = ryanodine receptor, SERCA = sarcoendoplasmic reticulum calcium transport ATPase; PLB = phospholamban; I–R = ischemia–reperfusion.
4. Modification of I/R-Induced Defects in Signal Transduction
Reperfusion of the ischemic heart is vital to restore cardiac function, reduce infarct size and salvage the viable myocardium [127]. From the aforementioned, it is evident that cardiac dysfunction due to I/R injury is multifaceted and complex and that there are several different elements that can modulate intracellular Ca2+-concentration and subsequent I/R injury. Some of these factors include the production of inflammatory cytokines, the activation of proteases as well as Nrf2 signal transduction. By virtue of their ability to influence intracellular Ca2+-concentration, it is possible that an attenuation of the I/R-induced increases in inflammatory cytokines and proteolytic activity, as well as the regulation of Nrf2 signaling processes, may serve as important mechanisms in IP-induced cardioprotection. These aspects are briefly described in the following sections.
4.1. Role of Inflammatory Cytokines in IP-Induced Cardioprotection
The inflammatory cytokines, TNF-α, IL-1 and IL-6, are known to influence cardiomyocyte Ca2+-handling and subsequent cardiac dysfunction in I/R injury [178,179,180,181], and thus may be important targets/mechanisms for cardioprotection due to IP. Both myocardial macrophages and cardiomyocytes produce TNFα, which depresses the heart function and induces cardiomyocyte apoptosis [182]. It is now established that the inflammatory cytokines mimic IP when given as a single episode before prolonged ischemia [183]; indeed, inflammatory cytokines may induce late preconditioning [184]. Late IP of the myocardium has been reported to alter the expression of genes that are involved in the inflammatory response. In this regard, not only is the gene for MMP9 upregulated, but also the gene for TNFα is upregulated in the late phase of IP [185]. Interestingly, the classic IP antagonist, 5-hydroxydecanoate, has been reported to abolish TNFα-mediated IP [186]. IP has been shown to decrease postischemic myocardial TNFα, which may represent the distal effector mechanism of preconditioning [187]. The influence of IP on TNFα and cardioprotection has been further demonstrated by the observation that the IP-mediated reduction in infarct size is associated with a reduction in circulating TNFα levels in a rat model of I–R injury [188].
It is pointed out that while the adverse effects of IL-1 in I–R are known to be due to the activation of superoxide dismutase and cardiac remodeling, IL-1 has been shown to be cardioprotective in IP [189]. On the other hand, IL-6 is a pleiotropic cytokine that protects against cardiac I/R injury following pharmacological preconditioning and IP [190,191,192]. The beneficial actions of IL-6 in IP have been suggested to be mediated through an IL-6/STAT3-dependent mechanism [193]; in fact, IL-6-mediated late preconditioning via JAK–STAT signaling results in the upregulation of iNOS and COX-2 and the development of cardioprotection [194]. In addition, IL-6 has also been reported to protect mitochondrial energetics and function [181].
4.2. Impact of IP on the Activation of Proteolysis
Proteases play an important role in the degradation of misfolded or malfunctional proteins, as well as in the routine turnover of the extracellular matrix and other subcellular organelles, and thus are essential in the maintenance of cell homeostasis [3,195,196]. Proteases are basally active, and their activity is regulated through a number of factors including their transcription, translation, chaperone molecules and the presence of endogenous inhibitors. However, in different pathophysiological conditions, including I/R, there is a dysregulation of proteases that results in a substantial increase in the activities of several effector proteases, including calpain, matrix metalloproteinases (MMP) and cathepsins [195]. Since these proteases are significantly altered in I/R, it is thus likely that IP may exert beneficial effects with respect to an attenuation of their highly activated state [127]. In this regard, IP, which is known to attenuate oxidative stress as well as intracellular Ca2+-overload has also been reported to diminish the I/R-induced activation of calpain and MMP [197]. Thus, it can be suggested that oxidative stress, either directly or indirectly as a consequence of intracellular Ca2+-overload, may both play a key role in the activation of proteolytic activities subsequent to I/R [197]. It should be mentioned that LonP1 is considered an essential mitochondrial protease that is critical for the maintenance of mitochondrial proteostasis and protection against cell stress [198]. Interestingly, IP was shown to induce a twofold increase in LonP1, which protected the heart against I/R injury, and it was thus suggested that the upregulation of LonP1 mitigated cardiac injury by preventing oxidative damage as well as through preserving mitochondrial redox balance [198].
4.3. Role of Nrf2 Signal Transduction in IP-Induced Cardioprotection
Nrf2 is a transcription factor that controls cellular defense responses [199], particularly in the regulation of the expression of antioxidant and detoxification genes [199,200,201]. Nrf2 is known to protect cardiomyocytes against oxidative stress by increasing endogenous antioxidants [202,203]. Indeed, the Nrf2/antioxidant response element plays a central role in the protective effect against oxidative and apoptotic damage [204,205]. Specifically, as a transcription factor, Nrf2 triggers the production of many phase II detoxifying and antioxidant enzymes through the activation of heme-oxygenase 1 and NADPH quinone oxidoreductase gene expression, which protect cells under conditions of oxidative stress [206,207,208] and provides cellular protection against different toxins [206,209,210,211]. In fact, several studies have shown that the activation of Nrf2 and the subsequent upregulation of antioxidant enzyme gene expression is an important mechanism of cardioprotection due to ischemic/hypoxic preconditioning, and that low concentrations of ROS may be an essential signal for the protective process [212,213,214,215]. Furthermore, Nrf2 has also been reported to modulate intracellular Ca2+ levels [216], and thus cardioprotection against I/R injury due to the activation of Nrf2 has recently been explored for clinical applicability [199]. In addition, the role of Nrf2 signal transduction in the protective actions of IP has also been examined [212,217]. Indeed, the Nrf2/antioxidant response element pathway activation may be of importance in IP [218]. In Nrf2 knockout mice, an increase in infarct size in response to I/R has been reported, as well as a reduced cardioprotective effect of IP [219]. The activation of PKC is known to be triggered by IP [219]. In this regard, polymyxin B, an inhibitor of PKC, blocked the membrane translocation of PKCδ and PKCε during IP that was also associated with an inhibition of Nrf2 nuclear accumulation, as well as a reduction in the cardioprotective effects of IP [219]. It was thus suggested that the activation of PKC induces the translocation of Nrf2 and the upregulation of endogenous antioxidant defenses in IP, and that specific PKC isoforms may target Nrf2 to exert cardioprotection [219].
5. Conclusions
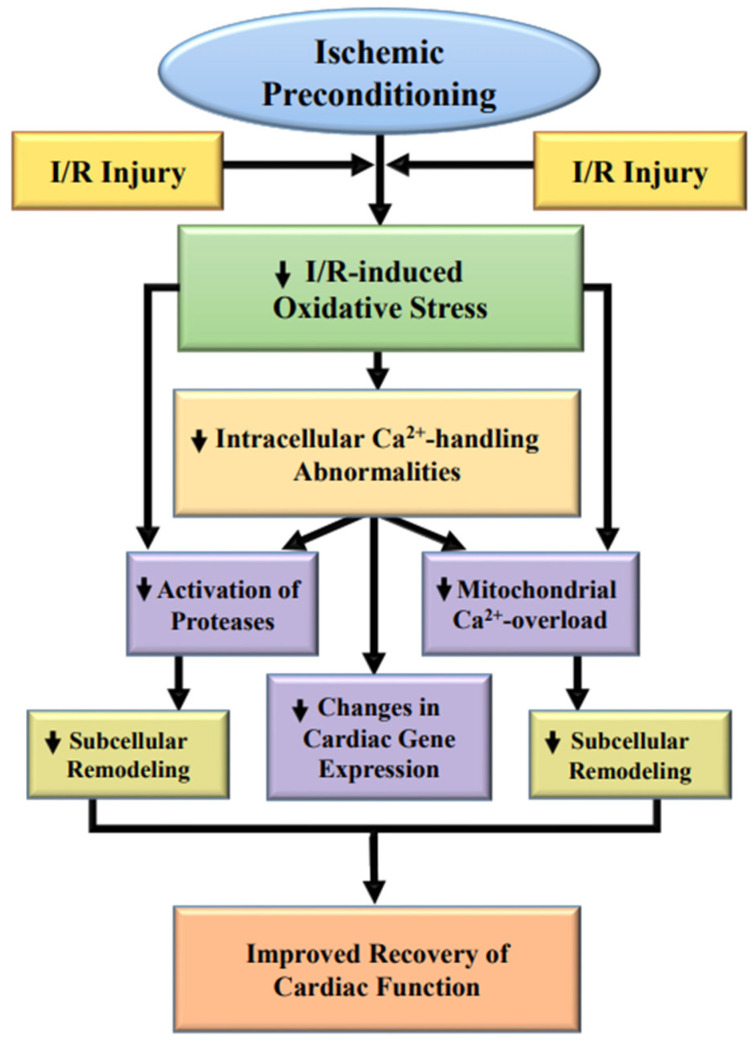
From the foregoing discussion, it is evident that IP-induced cardioprotection is associated with the reduction of I/R-induced oxidative stress and the subsequent depression in the development of intracellular Ca2+-overload in the I/R heart. A schematic representation of some critical events in eliciting improved cardiac function due to IP in the I/R hearts is given in Figure 3. It is also evident that I–R induces a wide variety of defects in subcellular organelles, both at the functional and molecular level. Although oxidative stress can be seen to produce adverse effects on subcellular organelles or subcellular remodeling through the development of intracellular Ca2+-overload, oxidative stress can directly cause subcellular and molecular abnormalities. While the initial functional changes occur rapidly under conditions of oxidative stress, the delay in functional recovery of the ischemic heart upon reperfusion may be due to alterations in the gene expression levels of SL and SR proteins, including those for other subcellular organelles such as the mitochondria, myofibrils and extracellular matrix. On the other hand, IP attenuates the occurrence of intracellular Ca2+-overload and oxidative stress in the I/R hearts, and thus reduces the I/R-induced subcellular remodeling and cardiac dysfunction. In addition, attenuation of proteolysis, but activation of Nrf2-mediated signal transduction, can also be considered as one of the important mechanisms of beneficial action of IP-induced cardioprotection. However, the translation of experimental interventions to clinical therapies remains to be a challenge.
Figure 3.
Proposed cardioprotective mechanisms of ischemic preconditioning for improving cardiac function in hearts subjected to ischemia/reperfusion (I/R) injury.
Acknowledgments
Infrastructural support for this project was provided by the St. Boniface Hospital Albrechtsen Research Centre. We would also like to thank Andrea Opsima for typing this manuscript.
Author Contributions
Conceptualization, N.S.D.; writing—original draft preparation, P.S.T. and A.K.S.; responsibility for the final draft and the scientific background of the manuscript, N.S.D. and B.R. All authors approved the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jennings R.B., Reimer K.A. The cell biology of acute myocardial ischemia. Annu. Rev. Med. 1991;42:225–246. doi: 10.1146/annurev.me.42.020191.001301. [DOI] [PubMed] [Google Scholar]
- 2.Hearse D.J., Bolli R. Reperfusion induced injury: Manifestations, mechanisms, and clinical relevance. Cardiovasc. Res. 1992;26:101–108. doi: 10.1093/cvr/26.2.101. [DOI] [PubMed] [Google Scholar]
- 3.Bolli R., Marban E. Molecular and cellular mechanisms of myocardial stunning. Physiol. Rev. 1999;79:609–634. doi: 10.1152/physrev.1999.79.2.609. [DOI] [PubMed] [Google Scholar]
- 4.Dhalla N.S., Elmoselhi A.B., Hata T., Makino N. Status of myocardial antioxidants in ischemia-reperfusion injury. Cardiovasc. Res. 2000;47:446–456. doi: 10.1016/S0008-6363(00)00078-X. [DOI] [PubMed] [Google Scholar]
- 5.Dhalla N.S., Golfman L., Takeda S., Takeda N., Nagano M. Evidence for the role of oxidative stress in acute ischemic heart disease: A brief review. Can. J. Cardiol. 1999;15:587–593. [PubMed] [Google Scholar]
- 6.Piper H.M., Meuter K., Schafer C. Cellular mechanisms of ischemia-reperfusion injury. Ann. Thorac. Surg. 2003;75:S644–S648. doi: 10.1016/S0003-4975(02)04686-6. [DOI] [PubMed] [Google Scholar]
- 7.Marczin N., El-Habashi N., Hoare G.S., Bundy R.E., Yacoub M. Antioxidants in myocardial ischemia-reperfusion injury: Therapeutic potential and basic mechanisms. Arch. Biochem. Biophys. 2003;420:222–236. doi: 10.1016/j.abb.2003.08.037. [DOI] [PubMed] [Google Scholar]
- 8.Kim S.J., Depre C., Vatner S.F. Novel mechanisms mediating stunned myocardium. Heart Fail. Rev. 2003;8:143–153. doi: 10.1023/A:1023040718319. [DOI] [PubMed] [Google Scholar]
- 9.Simonovic N., Jakovljevic V., Jeremic J., Finderle Z., Srejovic I., Nikolic Turnic T., Milosavljevic I., Zivkovic V. Comparative effects of calcium and potassium channel modulators on ischemia/reperfusion injury in the isolated rat heart. Mol. Cell. Biochem. 2019;450:175–185. doi: 10.1007/s11010-018-3384-y. [DOI] [PubMed] [Google Scholar]
- 10.Huang Z., Li H., Guo F., Jia Q., Zhang Y., Liu X., Shi G. Egr-1, the potential target of calcium channel blockers in cardioprotection with ischemia/reperfusion injury in rats. Cell Physiol. Biochem. 2009;24:17–24. doi: 10.1159/000227809. [DOI] [PubMed] [Google Scholar]
- 11.Karmazyn M. NHE-1: Still a viable therapeutic target. J. Mol. Cell. Cardiol. 2013;61:77–82. doi: 10.1016/j.yjmcc.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Kandilci H.B., Richards M.A., Fournier M., Şimşek G., Chung Y.J., Lakhal-Littleton S., Swietach P. Cardiomyocyte Na+/H+ exchanger-1 activity is reduced in hypoxia. Front. Cardiovasc. Med. 2021;7:617038. doi: 10.3389/fcvm.2020.617038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kimura K., Nakao K., Shibata Y., Sone T., Takayama T., Fukuzawa S., Nakama Y., Hirayama H., Matsumoto N., Kosuge M., et al. Randomized controlled trial of TY-51924, a novel hydrophilic NHE inhibitor, in acute myocardial infarction. J. Cardiol. 2016;67:307–313. doi: 10.1016/j.jjcc.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Gazmuri R.J., Radhakrishnan J., Ayoub I.M. Sodium-hydrogen exchanger isoform-1 inhibition: A promising pharmacological intervention for resuscitation from cardiac arrest. Molecules. 2019;24:1765. doi: 10.3390/molecules24091765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dhalla N.S., Temsah R.M., Netticacadan T., Sandhu M.S. Calcium overload in ischemia/reperfusion injury. In: Sperelakis N., Kurachi Y., Terzic A., Cohen M., editors. Heart Physiology and Pathophysiology. 4th ed. Academic Press; San Diego, PA, USA: 2001. pp. 949–965. [Google Scholar]
- 16.Bompotis G.C., Deftereos S., Angelidis C., Choidis E., Panagopoulou V., Kaoukis A., Vassilikos V.P., Cleman M.W., Giannopoulos G. Altered calcium handling in reperfusion injury. Med. Chem. 2016;12:114–130. doi: 10.2174/1573406411666150928112420. [DOI] [PubMed] [Google Scholar]
- 17.Fauconnier J., Roberge S., Saint N., Lacampagne A. Type 2 ryanodine receptor: A novel therapeutic target in myocardial ischemia/reperfusion. Pharmacol. Ther. 2013;138:323–332. doi: 10.1016/j.pharmthera.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Dorado D., Ruiz-Meana M., Inserte J., Rodriguez-Sinovas A., Piper H.M. Calcium-mediated cell death during myocardial reperfusion. Cardiovasc. Res. 2012;94:168–180. doi: 10.1093/cvr/cvs116. [DOI] [PubMed] [Google Scholar]
- 19.Chen S., Li S. The Na+/Ca2+ exchanger in cardiac ischemia/reperfusion injury. Med. Sci. Monit. 2012;18:RA161–RA165. doi: 10.12659/MSM.883533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saini H.K., Dhalla N.S. Defective calcium handling in cardiomyocytes isolated from hearts subjected to ischemia-reperfusion. Am. J. Physiol. Heart Circ. Physiol. 2005;288:H2260–H2270. doi: 10.1152/ajpheart.01153.2004. [DOI] [PubMed] [Google Scholar]
- 21.He F., Wu Q., Xu B., Wang X., Wu J., Huang L., Cheng J. Suppression of Stim1 reduced intracellular calcium concentration and attenuated hypoxia/reoxygenation induced apoptosis in H9C2 cells. Biosci. Rep. 2017;37:BSR20171249. doi: 10.1042/BSR20171249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Müller B.A., Dhalla N.S. Mechanisms of the beneficial actions of ischemic preconditioning on subcellular remodeling in ischemic-reperfused heart. Curr. Cardiol. Rev. 2010;6:255–264. doi: 10.2174/157340310793566118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saini H.K., Machackova J., Dhalla N.S. Role of reactive oxygen species in ischemic preconditioning of subcellular organelles in the heart. Antioxid. Redox Signal. 2004;6:393–404. doi: 10.1089/152308604322899468. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez Rico C., Konate K., Josse E., Nargeot J., Barrère-Lemaire S., Boisguérin P. Therapeutic peptides to treat myocardial ischemia-reperfusion injury. Front. Cardiovasc. Med. 2022;9:792885. doi: 10.3389/fcvm.2022.792885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adameova A., Horvath C., Abdul-Ghani S., Varga Z.V., Suleiman M.S., Dhalla N.S. Interplay of oxidative stress and necrosis-like cell death in cardiac ischemia/reperfusion injury: A focus on necroptosis. Biomedicines. 2022;10:127. doi: 10.3390/biomedicines10010127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen C.L., Zhang L., Jin Z., Kasumov T., Chen Y.R. Mitochondrial redox regulation and myocardial ischemia-reperfusion injury. Am. J. Physiol. Cell Physiol. 2022;322:C12–C23. doi: 10.1152/ajpcell.00131.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang J., Li R., Wang C. The role of mitochondrial quality control in cardiac ischemia/reperfusion injury. Oxid. Med. Cell Longev. 2021;2021:5543452. doi: 10.1155/2021/5543452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zucchi R., Ronca F., Ronca-Testoni S. Modulation of sarcoplasmic reticulum function: A new strategy in cardioprotection? Pharmacol. Ther. 2001;89:47–65. doi: 10.1016/S0163-7258(00)00103-0. [DOI] [PubMed] [Google Scholar]
- 29.Sanada S., Komuro I., Kitakaze M. Pathophysiology of myocardial reperfusion injury: Preconditioning, postconditioning, and translational aspects of protective measures. Am. J. Physiol. Heart Circ. Physiol. 2011;301:H1723–H1741. doi: 10.1152/ajpheart.00553.2011. [DOI] [PubMed] [Google Scholar]
- 30.Jovanović A. Cardioprotective signalling: Past, present and future. Eur. J. Pharmacol. 2018;833:314–319. doi: 10.1016/j.ejphar.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 31.Caricati-Neto A., Errante P.R., Menezes-Rodrigues F.S. Recent advances in pharmacological and non-pharmacological strategies of cardioprotection. Int. J. Mol. Sci. 2019;20:4002. doi: 10.3390/ijms20164002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dhalla N.S., Temsah R.M., Netticadan T. Role of oxidative stress in cardiovascular diseases. J. Hypertens. 2000;18:655–673. doi: 10.1097/00004872-200018060-00002. [DOI] [PubMed] [Google Scholar]
- 33.Obal D., Dai S., Keith R., Dimova N., Kingery J., Zheng Y.T., Zweier J., Velayutham M., Prabhu S.D., Li Q., et al. Cardiomyocyte-restricted overexpression of extracellular superoxide dismutase increases nitric oxide bioavailability and reduces infarct size after ischemia/reperfusion. Basic Res. Cardiol. 2012;107:305. doi: 10.1007/s00395-012-0305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.He G. Electron paramagnetic resonance oximetry and redoximetry. Methods Mol. Biol. 2010;594:85–105. doi: 10.1007/978-1-60761-411-1_6. [DOI] [PubMed] [Google Scholar]
- 35.Khan M., Brauner M.E., Plewa M.C., Kutala V.K., Angelos M., Kuppusamy P. Effect of pulmonary-generated reactive oxygen species on left-ventricular dysfunction associated with cardio-pulmonary ischemia-reperfusion injury. Cell Biochem. Biophys. 2013;67:275–280. doi: 10.1007/s12013-011-9299-9. [DOI] [PubMed] [Google Scholar]
- 36.Saini-Chohan H.K., Dhalla N.S. Attenuation of ischemia-reperfusion-induced alterations in intracellular Ca2+ in cardiomyocytes from hearts treated with N-acetylcysteine and N-mercaptopropionylglycine. Can. J. Physiol. Pharmacol. 2009;87:1110–1119. doi: 10.1139/Y09-103. [DOI] [PubMed] [Google Scholar]
- 37.Kuznetsov A.V., Javadov S., Margreiter R., Grimm M., Hagenbuchner J., Ausserlechner M.J. The role of mitochondria in the mechanisms of cardiac ischemia-reperfusion injury. Antioxidants. 2019;8:454. doi: 10.3390/antiox8100454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang J.C., Lien C.F., Lee W.S., Chang H.R., Hsu Y.C., Luo Y.P., Jeng J.R., Hsieh J.C., Yang K.T. Intermittent hypoxia prevents myocardial mitochondrial Ca2+ overload and cell death during ischemia/reperfusion: The role of reactive oxygen species. Cells. 2019;8:564. doi: 10.3390/cells8060564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tappia P.S., Asemu G., Rodriguez-Leyva D. Phospholipase C as a potential target for cardioprotection during oxidative stress. Can. J. Physiol. Pharmacol. 2010;88:249–263. doi: 10.1139/Y10-019. [DOI] [PubMed] [Google Scholar]
- 40.Matucci R., Bennardini F., Sciammarella M.L., Baccaro C., Stendardi I., Franconi F., Giotti A. [3H]-nitrendipine binding in membranes obtained from hypoxic and reoxygenated heart. Biochem. Pharmacol. 1987;36:1059–1062. doi: 10.1016/0006-2952(87)90414-X. [DOI] [PubMed] [Google Scholar]
- 41.Nayler W.G., Dillon J.S., Elz J.S., McKelvie M. An effect of ischemia on myocardial dihydropyridine binding sites. Eur. J. Pharmacol. 1985;115:81–89. doi: 10.1016/0014-2999(85)90587-4. [DOI] [PubMed] [Google Scholar]
- 42.Kaneko M., Lee S.L., Wolf C.M., Dhalla N.S. Reduction of calcium channel antagonist binding sites by oxygen free radicals in rat heart. J. Mol. Cell. Cardiol. 1989;21:935–943. doi: 10.1016/0022-2828(89)90761-X. [DOI] [PubMed] [Google Scholar]
- 43.Dixon I.M., Eyolfson D.A., Dhalla N.S. Sarcolemmal Na+-Ca2+ exchange activity in hearts subjected to hypoxia reoxygenation. Am. J. Physiol. Heart Circ. Physiol. 1987;253:H1026–H1034. doi: 10.1152/ajpheart.1987.253.5.H1026. [DOI] [PubMed] [Google Scholar]
- 44.Conway S.J., Koushik S.V. Cardiac sodium–calcium exchanger: A double-edged sword. Cardiovasc. Res. 2001;51:194–197. doi: 10.1016/S0008-6363(01)00356-X. [DOI] [PubMed] [Google Scholar]
- 45.Javier Inserte J., Garcia-Dorado D., Ruiz-Meana M., Padilla F., Barrabés J.A., Pina P., Agulló L., Piper H.M., Soler-Soler J. Effect of inhibition of Na+/Ca2+ exchanger at the time of myocardial reperfusion on hypercontracture and cell death. Cardiovasc. Res. 2002;55:739–748. doi: 10.1016/s0008-6363(02)00461-3. [DOI] [PubMed] [Google Scholar]
- 46.Kaneko M., Beamish R.E., Dhalla N.S. Depression of heart sarcolemmal Ca2+-pump activity by oxygen free radicals. Am. J. Physiol. Heart Circ. Physiol. 1989;256:H368–H374. doi: 10.1152/ajpheart.1989.256.2.H368. [DOI] [PubMed] [Google Scholar]
- 47.Kaneko M., Elimban V., Dhalla N.S. Mechanism for depression of heart sarcolemmal Ca2+ pump by oxygen free radicals. Am. J. Physiol. Heart Circ. Physiol. 1989;257:H804–H811. doi: 10.1152/ajpheart.1989.257.3.H804. [DOI] [PubMed] [Google Scholar]
- 48.Hata T., Kaneko M., Beamish R.E., Dhalla N.S. Influence of oxygen free radicals on heart sarcolemmal Na+-Ca2+ exchange. Coron. Artery Dis. 1991;2:397–407. doi: 10.1097/00019501-199105000-00014. [DOI] [Google Scholar]
- 49.Pratt R.D., Brickman C.R., Cottrill C.L., Shapiro J.I., Liu J. The Na/K-ATPase Signaling: From Specific Ligands to General Reactive Oxygen Species. Int. J. Mol. Sci. 2018;19:2600. doi: 10.3390/ijms19092600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaneko M., Singal P.K., Dhalla N.S. Alterations in heart sarcolemmal Ca2+-ATPase and Ca2+-binding activities due to oxygen free radicals. Basic Res. Cardiol. 1990;85:45–54. doi: 10.1007/BF01907013. [DOI] [PubMed] [Google Scholar]
- 51.Ostadal P., Elmoselhi A.B., Zdobnicka I., Lukas A., Elimban V., Dhalla N.S. Role of oxidative stress in ischemia-reperfusion-induced changes in Na+-K+-ATPase isoform expression in rat heart. Antioxid. Redox Signal. 2004;6:914–923. doi: 10.1089/ars.2004.6.914. [DOI] [PubMed] [Google Scholar]
- 52.Elmoselhi A.B., Lukas A., Ostadal P., Dhalla N.S. Preconditioning attenuates ischemia-reperfusion-induced remodeling of Na+-K+ATPase in hearts. Am. J. Physiol. Heart Circ. Physiol. 2003;285:H1055–H1063. doi: 10.1152/ajpheart.00865.2002. [DOI] [PubMed] [Google Scholar]
- 53.Liu J., Nie Y., Chaudhry M., Bai F., Chuang J., Sodhi K., Shapiro J.I. The redox-sensitive Na/K-ATPase signaling in uremic cardiomyopathy. Int. J. Mol. Sci. 2020;21:1256. doi: 10.3390/ijms21041256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu J., Lilly M.N., Shapiro J.I. Targeting Na/K-ATPase signaling: A new approach to control oxidative stress. Curr. Pharm. Des. 2018;24:359–364. doi: 10.2174/1381612824666180110101052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bogdanova A., Petrushanko I.Y., Hernansanz-Agustín P., Martínez-Ruiz A. “Oxygen Sensing” by Na,K-ATPase: These miraculous thiols. Front. Physiol. 2016;7:314. doi: 10.3389/fphys.2016.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaneko M., Panagia V., Paolillo G., Majumder S., Ou C., Dhalla N.S. Inhibition of cardiac phosphatidylethanolamine N-methylation by oxygen free radicals. Biochim. Biophys. Acta. 1990;1021:33–38. doi: 10.1016/0005-2736(90)90380-7. [DOI] [PubMed] [Google Scholar]
- 57.Kato K., Shao Q., Elimban V., Lukas A., Dhalla N.S. Mechanism of depression in cardiac sarcolemmal Na+-K+-ATPase by hypochlorous acid. Am. J. Physiol. Cell Physiol. 1998;275:C826–C831. doi: 10.1152/ajpcell.1998.275.3.C826. [DOI] [PubMed] [Google Scholar]
- 58.Shao Q., Matsubara T., Bhatt S.K., Dhalla N.S. Inhibition of cardiac sarcolemma Na+-K+ ATPase by oxyradical generating systems. Mol. Cell. Biochem. 1995;147:139–144. doi: 10.1007/BF00944794. [DOI] [PubMed] [Google Scholar]
- 59.Shattock M.J., Ottolia M., Bers D.M., Blaustein M.P., Boguslavskyi A., Bossuyt J., Bridge J.H., Chen-Izu Y., Clancy C.E., Edwards A., et al. Na+/Ca2+ exchange and Na+/K+-ATPase in the heart. J. Physiol. 2015;593:1361–1382. doi: 10.1113/jphysiol.2014.282319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Santacruz-Toloza L., Ottolia M., Nicoll D.A., Philipson K.D. Functional analysis of a disulfide bond in the cardiac Na+-Ca2+ exchanger. J. Biol. Chem. 2000;275:182–188. doi: 10.1074/jbc.275.1.182. [DOI] [PubMed] [Google Scholar]
- 61.Chakraborti S., Das S., Kar P., Ghosh B., Samanta K., Kolley S., Ghosh S., Roy S., Chakraborti T. Calcium signaling phenomena in heart diseases: A perspective. Mol. Cell. Biochem. 2007;298:1–40. doi: 10.1007/s11010-006-9355-8. [DOI] [PubMed] [Google Scholar]
- 62.Villa-Abrille M.C., Sidor A., O’Rourke B. Insulin effects on cardiac Na+/Ca2+ exchanger activity: Role of the cytoplasmic regulatory loop. J. Biol. Chem. 2008;283:16505–16513. doi: 10.1074/jbc.M801424200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Matsubara T., Dhalla N.S. Effect of oxygen free radicals on cardiac contractile activity and sarcolemmal Na+-Ca2+ exchange. J. Cardiovasc. Pharmacol. Ther. 1996;1:211–218. doi: 10.1177/107424849600100304. [DOI] [PubMed] [Google Scholar]
- 64.Matsubara T., Dhalla N.S. Relationship between mechanical dysfunction and depression of sarcolemmal Ca2+-pump activity in hearts perfused with oxygen free radicals. Mol. Cell. Biochem. 1996;160–161:179–185. doi: 10.1007/BF00240048. [DOI] [PubMed] [Google Scholar]
- 65.Aleksandrova E.A. Calcium- transporting systems and calcium regulation in cardiomyocytes. Usp. Fiziol. Nauk. 2001;32:40–48. [PubMed] [Google Scholar]
- 66.Matsubara T., Musat-Marcu S., Misra H.P., Dhalla N.S. Protective effect of vanadate on oxyradical-induced changes in isolated perfused heart. Mol. Cell. Biochem. 1995;153:79–85. doi: 10.1007/BF01075921. [DOI] [PubMed] [Google Scholar]
- 67.Musat S., Dhalla N.S. Alteration in cardiac sarcolemmal ATP receptors by oxyradicals. Ann. N. Y. Acad. Sci. 1996;793:1–12. doi: 10.1111/j.1749-6632.1996.tb33500.x. [DOI] [PubMed] [Google Scholar]
- 68.Persad S., Takeda S., Panagia V., Dhalla N.S. Beta-adrenoceptor-linked signal transduction in ischemic-reperfused heart and scavenging of oxyradicals. J. Mol. Cell. Cardiol. 1997;29:545–558. doi: 10.1006/jmcc.1996.0298. [DOI] [PubMed] [Google Scholar]
- 69.Persad S., Takeda S., Dhalla N.S. Alternations in beta-adrenoceptor mechanisms in hearts perfused with xanthine plus xanthine oxidase. J. Cardiovasc. Pharmacol. Ther. 1997;2:115–124. doi: 10.1177/107424849700200205. [DOI] [PubMed] [Google Scholar]
- 70.Persad S., Panagia V., Dhalla N.S. Role of H2O2 in changing beta-adrenoceptor and adenylyl cyclase in ischemia-reperfused hearts. Mol. Cell. Biochem. 1998;186:99–106. doi: 10.1023/A:1006823531286. [DOI] [PubMed] [Google Scholar]
- 71.Persad S., Dhalla N.S. Modification of beta-adrenoceptors and adenylyl cyclase in hearts perfused with hypochlorous acid. Can. J. Physiol. Pharmacol. 1998;76:961–966. doi: 10.1139/y98-112. [DOI] [PubMed] [Google Scholar]
- 72.Persad S., Elimban V., Kaila J., Dhalla N.S. Biphasic alterations in cardiac beta-adrenoceptor signal transduction mechanism due to oxyradicals. J. Pharmacol. Exp. Ther. 1997;282:1623–1631. [PubMed] [Google Scholar]
- 73.Persad S., Rupp H., Jindal R., Arneja J., Dhalla N.S. Modification of cardiac beta-adrenoceptor mechanisms by H2O2. Am. J. Physiol. Heart Circ. Physiol. 1998;274:H416–H423. doi: 10.1152/ajpheart.1998.274.2.H416. [DOI] [PubMed] [Google Scholar]
- 74.Persad S., Elimban V., Siddiqui F., Dhalla N.S. Alterations in cardiac membrane beta-adrenoceptors and adenylyl cyclase due to hypochlorous acid. J. Mol. Cell. Cardiol. 1999;31:101–111. doi: 10.1006/jmcc.1998.0847. [DOI] [PubMed] [Google Scholar]
- 75.Sato S., Sato N., Kudej R.K., Uechi M., Asai K., Shen Y.T., Ishikawa Y., Vatner S.F., Vatner D.E. β-adrenergic receptor signalling in stunned myocardium of conscious pigs. J. Mol. Cell. Cardiol. 1997;29:1387–1400. doi: 10.1006/jmcc.1997.0377. [DOI] [PubMed] [Google Scholar]
- 76.Haenen G.R., Veerman M., Bast A. Reduction of beta-adrenoceptor function by oxidative stress in the heart. Free Radic. Biol. Med. 1990;9:279–288. doi: 10.1016/0891-5849(90)90002-Z. [DOI] [PubMed] [Google Scholar]
- 77.Kaneko M., Chapman D.C., Ganguly P.K., Beamish R.E., Dhalla N.S. Modification of cardiac adrenergic receptors by oxygen free radicals. Am. J. Physiol. Heart Circ. Physiol. 1991;260:H821–H826. doi: 10.1152/ajpheart.1991.260.3.H821. [DOI] [PubMed] [Google Scholar]
- 78.Asemu G., Tappia P.S., Dhalla N.S. Identification of the changes in phospholipase C isozymes in ischemic-reperfused rat heart. Arch. Biochem. Biophys. 2003;411:174–182. doi: 10.1016/S0003-9861(02)00733-6. [DOI] [PubMed] [Google Scholar]
- 79.Asemu G., Dent M., Singal T., Dhalla N.S., Tappia P.S. Differential changes in phospholipase D and phosphatidate phosphohydralase activities in ischemia-reperfusion of rat heart. Arch. Biochem. Biophys. 2005;436:136–144. doi: 10.1016/j.abb.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 80.Munakata M., Stamm C., Friehs I., Zurakowski D., Cowan D.B., Cao-Danh H., McGowan F.X., Jr., del Nido P.J. Protective effects of protein kinase C during myocardial ischemia require activation of phosphatidyl-inositol specific phospholipase C. Ann. Thorac. Surg. 2002;73:1236–1245. doi: 10.1016/S0003-4975(01)03594-9. [DOI] [PubMed] [Google Scholar]
- 81.Askenasy N., Vivi A., Tassini M., Navon G., Farkas D.L. NMR spectroscopic characterization of sarcolemmal permeability during myocardial ischemia and reperfusion. J. Mol. Cell. Cardiol. 2001;33:1421–1433. doi: 10.1006/jmcc.2001.1404. [DOI] [PubMed] [Google Scholar]
- 82.Kyoi S., Otani H., Sumida T., Okada T., Osako M., Imamura H., Kamihata H., Matsubara H., Iwasaka T. Loss of intracellular dystrophin: A potential mechanism for myocardial reperfusion injury. Circ. J. 2003;67:725–727. doi: 10.1253/circj.67.725. [DOI] [PubMed] [Google Scholar]
- 83.Shah A.K., Bhullar S.K., Elimban V., Dhalla N.S. Oxidative stress as a mechanism for functional alterations in cardiac hypertrophy and heart failure. Antioxidants. 2021;10:931. doi: 10.3390/antiox10060931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hill M.F. Emerging role for antioxidant therapy in protection against diabetic cardiac complications: Experimental and clinical evidence for utilization of classic and new antioxidants. Curr. Cardiol. Rev. 2008;4:259–268. doi: 10.2174/157340308786349453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Siddall H.K., Yellon D.M., Ong S.B., Mukherjee U.A., Burke N., Hall A.R., Angelova P.R., Ludtmann M.H., Deas E., Davidson S.M., et al. Loss of PINK1 increases the heart’s vulnerability to ischemia-reperfusion injury. PLoS ONE. 2013;8:e62400. doi: 10.1371/annotation/94fd6502-4b2d-409c-8836-66fe6ebc03ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Morrey C., Brazin J., Seyedi N., Corti F., Silver R.B., Levi R. Interaction between sensory C-fibers and cardiac mast cells in ischemia/reperfusion: Activation of a local renin-angiotensin system culminating in severe arrhythmic dysfunction. J. Pharmacol. Exp. Ther. 2010;335:76–84. doi: 10.1124/jpet.110.172262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Goldhaber J.I., Qayyum M.S. Oxygen free radicals and excitation-contraction coupling. Antioxid. Redox. Signal. 2000;2:55–64. doi: 10.1089/ars.2000.2.1-55. [DOI] [PubMed] [Google Scholar]
- 88.Basu D.K., Karmazyn M. Injury to rat hearts produced by an exogenous free radical generating system. Study into the role of arachidonic acid and eicosanoids. J. Pharmacol. Exp. Ther. 1987;242:673–685. [PubMed] [Google Scholar]
- 89.Eley D.W., Korecky B., Fliss H. Dithiothreitol restores contractile function to oxidant-injured cardiac muscle. Am. J. Physiol. Heart Circ. Physiol. 1989;257:H1321–H1325. doi: 10.1152/ajpheart.1989.257.4.H1321. [DOI] [PubMed] [Google Scholar]
- 90.Manson N.H., Hess M.L. Interaction of oxygen free radicals and cardiac sarcoplasmic reticulum: Proposed role in the pathogenesis of endotoxin shock. Circ. Shock. 1983;10:205–213. [PubMed] [Google Scholar]
- 91.Rowe G.T., Manson N.H., Caplan M., Hess M.L. Hydrogen peroxide and hydroxyl radical mediation of activated leukocyte depression of cardiac sarcoplasmic reticulum. Participation of the cyclooxygenase pathway. Circ. Res. 1983;53:584–591. doi: 10.1161/01.RES.53.5.584. [DOI] [PubMed] [Google Scholar]
- 92.Okabe E., Hess M.L., Oyama M., Ito H. Characterization of free radical-mediated damage of canine cardiac sarcoplasmic reticulum. Arch. Biochem. Biophys. 1983;225:164–177. doi: 10.1016/0003-9861(83)90020-6. [DOI] [PubMed] [Google Scholar]
- 93.D’Oria R., Schipani R., Leonardini A., Natalicchio A., Perrini S., Cignarelli A., Laviola L., Giorgino F. The role of oxidative stress in cardiac disease: From physiological response to injury factor. Oxid. Med. Cell Longev. 2020;2020:5732956. doi: 10.1155/2020/5732956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zima A.V., Blatter L.A. Redox regulation of cardiac calcium channels and transporters. Cardiovasc. Res. 2006;71:310–321. doi: 10.1016/j.cardiores.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 95.Adameova A., Shah A.K., Dhalla N.S. Role of oxidative stress in the genesis of ventricular arrhythmias. Int. J. Mol. Sci. 2020;21:4200. doi: 10.3390/ijms21124200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Myers M.L., Webb C., Moffat M., McIver D., del Maestro R. Activated neutrophils depress myocardial function in the perfused rabbit heart. Can. J. Cardiol. 1991;7:323–330. [PubMed] [Google Scholar]
- 97.Ford D.A. Lipid oxidation by hypochlorous acid: Chlorinated lipids in atherosclerosis and myocardial ischemia. Clin. Lipidol. 2010;5:835–852. doi: 10.2217/clp.10.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yang J., Xu J., Tao L., Wang S., Xiang H., Tang Y. Synergetic protective effect of remote ischemic preconditioning and prolyl 4-hydroxylase inhibition in ischemic cardiac injury. Mol. Med. Rep. 2022;25:80. doi: 10.3892/mmr.2022.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Khaliulin I., Ascione R., Maslov L.N., Amal H., Suleiman M.S. Preconditioning or postconditioning with 8-Br-cAMP-AM protects the heart against regional ischemia and reperfusion: A role for mitochondrial permeability transition. Cells. 2021;10:1223. doi: 10.3390/cells10051223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hentia C., Rizzato A., Camporesi E., Yang Z., Muntean D.M., Săndesc D., Bosco G. An overview of protective strategies against ischemia/reperfusion injury: The role of hyperbaric oxygen preconditioning. Brain Behav. 2018;8:e00959. doi: 10.1002/brb3.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hausenloy D.J., Yellon D.M. Ischaemic conditioning and reperfusion injury. Nat. Rev. Cardiol. 2016;13:193–209. doi: 10.1038/nrcardio.2016.5. [DOI] [PubMed] [Google Scholar]
- 102.Nuñez R.E., Javadov S., Escobales N. Angiotensin II-preconditioning is associated with increased PKCε/PKCδ ratio and prosurvival kinases in mitochondria. Clin. Exp. Pharmacol. Physiol. 2017;44:1201–1212. doi: 10.1111/1440-1681.12816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shan D., Guo S., Wu H.K., Lv F., Jin L., Zhang M., Xie P., Wang Y., Song Y., Wu F., et al. Cardiac ischemic preconditioning promotes MG53 secretion through H2O2-activated protein kinase C-δ signaling. Circulation. 2020;142:1077–1091. doi: 10.1161/CIRCULATIONAHA.119.044998. [DOI] [PubMed] [Google Scholar]
- 104.Zeng H., Wang L., Zhang J., Pan T., Yu Y., Lu J., Zhou P., Yang H., Li P. Activated PKB/GSK-3βsynergizes with PKC-δ signaling in attenuating myocardial ischemia/reperfusion injury via potentiation of NRF2 activity: Therapeutic efficacy of dihydrotanshinone-I. Acta Pharm. Sin B. 2021;11:71–88. doi: 10.1016/j.apsb.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.De Marchi E., Baldassari F., Bononi A., Wieckowski M.R., Pinton P. Oxidative stress in cardiovascular diseases and obesity: Role of p66Shc and protein kinase C. Oxid. Med. Cell Longev. 2013;2013:564961. doi: 10.1155/2013/564961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Churchill E.N., Disatnik M.H., Mochly-Rosen D. Time-dependent and ethanol-induced cardiac protection from ischemia mediated by mitochondrial translocation of varepsilon PKC and activation of aldehyde dehydrogenase 2. J. Mol. Cell. Cardiol. 2009;46:278–284. doi: 10.1016/j.yjmcc.2008.09.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Apostolakis E., Baikoussis N.G., Papakonstantinou N.A. The role of myocardial ischaemic preconditioning during beating heart surgery: Biological aspect and clinical outcome. Interact. Cardiovasc. Thorac. Surg. 2012;14:68–71. doi: 10.1093/icvts/ivr024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Asemu G., Dhalla N.S., Tappia P.S. Inhibition of PLC improves postischemic recovery in isolated rat heart. Am. J. Physiol. Heart Circ. Physiol. 2004;287:H2598–H2605. doi: 10.1152/ajpheart.00506.2004. [DOI] [PubMed] [Google Scholar]
- 109.Zhang M., Xu Y.J., Saini H.K., Turan B., Liu P.P., Dhalla N.S. Pentoxifylline attenuate cardiac dysfunction and reduces TNF-α level in ischemia-reperfused heart. Am. J. Physiol. Heart Circ. Physiol. 2005;289:H832–H839. doi: 10.1152/ajpheart.00178.2005. [DOI] [PubMed] [Google Scholar]
- 110.Beresewicz A., Czarnowska E., Maczewski M. Ischemic preconditioning and superoxide dismutase protect against endothelial dysfunction and endothelium glycocalyx disruption in the postischemic guinea-pig hearts. Mol. Cell. Biochem. 1998;186:87–97. doi: 10.1023/A:1006867214448. [DOI] [PubMed] [Google Scholar]
- 111.Lalu M.M., Csonka C., Giricz Z., Csont T., Schulz R., Ferdinandy P. Preconditioning decreases ischemia/reperfusion-induced release and activation of matrix metalloproteinase-2. Biochem. Biophys. Res. Commun. 2002;296:937–941. doi: 10.1016/S0006-291X(02)02019-3. [DOI] [PubMed] [Google Scholar]
- 112.Cheung P.Y., Sawicki G., Wozniak M., Wang W., Radomski M.W., Schulz R. Matrix metalloproteinase-2 contributes to ischemia-reperfusion injury in the heart. Circulation. 2000;101:1833–1839. doi: 10.1161/01.CIR.101.15.1833. [DOI] [PubMed] [Google Scholar]
- 113.Rodrigo R., Castillo R., Cereceda M., Asenjo R., Zamorano J., Araya J. Non-hypoxic preconditioning of myocardium against postoperative atrial fibrillation: Mechanism based on enhancement of the antioxidant defense system. Med. Hypotheses. 2007;69:1242–1248. doi: 10.1016/j.mehy.2007.03.035. [DOI] [PubMed] [Google Scholar]
- 114.Guay J., Lambert H., Gingras-Breton G., Lavoie J.N., Huot J., Landry J. Regulation of actin filament dynamics by p38 map kinase-mediated phosphorylation of heat shock protein 27. J. Cell Sci. 1997;110:357–368. doi: 10.1242/jcs.110.3.357. [DOI] [PubMed] [Google Scholar]
- 115.Landry J., Huot J. Modulation of actin dynamics during stress and physiological stimulation by a signaling pathway involving p38 MAP kinase and heat-shock protein 27. Biochem. Cell Biol. 1995;73:703–707. doi: 10.1139/o95-078. [DOI] [PubMed] [Google Scholar]
- 116.Das D.K., Maulik N., Sato M., Ray P.S. Reactive oxygen species function as second messenger during ischemic preconditioning of heart. Mol. Cell. Biochem. 1999;196:59–67. doi: 10.1023/A:1006966128795. [DOI] [PubMed] [Google Scholar]
- 117.Singh L., Kulshrestha R., Singh N., Jaggi A.S. Mechanisms involved in adenosine pharmacological preconditioning-induced cardioprotection. Korean J. Physiol. Pharmacol. 2018;22:225–234. doi: 10.4196/kjpp.2018.22.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fryer R.M., Auchampach J.A., Gross G.J. Therapeutic receptor targets of ischemic preconditioning. Cardiovasc. Res. 2002;55:520–525. doi: 10.1016/S0008-6363(02)00316-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pachauri P., Garabadu D., Goyal A., Upadhyay P.K. Angiotensin (1-7) facilitates cardioprotection of ischemic preconditioning on ischemia-reperfusion-challenged rat heart. Mol. Cell. Biochem. 2017;430:99–113. doi: 10.1007/s11010-017-2958-4. [DOI] [PubMed] [Google Scholar]
- 120.Zhang J., Simpson P.C., Jensen B.C. Cardiac α1A-adrenergic receptors: Emerging protective roles in cardiovascular diseases. Am. J. Physiol. Heart Circ. Physiol. 2021;320:H725–H733. doi: 10.1152/ajpheart.00621.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Buchholz B., Annunzio D.V., Giani J.F., Siachoque N., Dominici F.P., Turyn D., Perez V., Donato M., Gelpi R.J. Ischemic postconditioning reduces infarct size through the α1-adrenergic receptor pathway. J. Cardiovasc. Pharmacol. 2014;63:504–511. doi: 10.1097/FJC.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 122.Headrick J.P., See Hoe L.E., Du Toit E.F., Peart J.N. Opioid receptors and cardioprotection—‘Opioidergic conditioning’ of the heart. Br. J. Pharmacol. 2015;172:2026–2050. doi: 10.1111/bph.13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fraessdorf J., Hollmann M.W., Hanschmann I., Heinen A., Weber N.C., Preckel B., Huhn R. Role of endogenous opioid system in ischemic-induced late preconditioning. PLoS ONE. 2015;10:e0134283. doi: 10.1371/journal.pone.0134283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Anzawa R., Seki S., Nagoshi T., Taniguchi I., Feuvray D., Yoshimura M. The role of Na+/H+ exchanger in Ca2+ overload and ischemic myocardial damage in hearts from type 2 diabetic db/db mice. Cardiovasc. Diabetol. 2012;11:33. doi: 10.1186/1475-2840-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhou R.H., Long C., Liu J., Liu B. Inhibition of the Na+/H+ exchanger protects the immature rabbit myocardium from ischemia and reperfusion injury. Pediatr. Cardiol. 2008;29:113–120. doi: 10.1007/s00246-007-9072-4. [DOI] [PubMed] [Google Scholar]
- 126.Ostadal P., Elmoselhi A.B., Zdobnicka I., Lukas A., Chapman D., Dhalla N.S. Ischemia-reperfusion alters gene expression of Na+-K+ ATPase isoforms in rat heart. Biochem. Biophys. Res. Commun. 2003;306:457–462. doi: 10.1016/S0006-291X(03)00986-0. [DOI] [PubMed] [Google Scholar]
- 127.Dhalla N.S., Saini H.K., Tappia P.S., Sethi R., Mengi S.A., Gupta S.K. Potential role and mechanisms of subcellular remodeling in cardiac dysfunction due to ischemic heart disease. J. Cardiovasc. Med. 2007;8:238–250. doi: 10.2459/01.JCM.0000263489.13479.68. [DOI] [PubMed] [Google Scholar]
- 128.Zahler R., Brines M., Kashgarian M., Benz E.J., Jr., Gilmore-Hebert M. The cardiac conduction system in the rat expresses the α2 and α3 isoforms of the Na+,K+-ATPase. Proc. Natl. Acad. Sci. USA. 1992;89:99–103. doi: 10.1073/pnas.89.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kim M.S., Akera T. O2 free radicals: Cause of ischemia-reperfusion injury to cardiac Na+-K+-ATPase. Am. J. Physiol. 1987;252:H252–H257. doi: 10.1152/ajpheart.1987.252.2.H252. [DOI] [PubMed] [Google Scholar]
- 130.Aizman O., Aperia A. Na,K-ATPase as a signal transducer. Ann. N. Y. Acad. Sci. 2003;986:489–496. doi: 10.1111/j.1749-6632.2003.tb07233.x. [DOI] [PubMed] [Google Scholar]
- 131.Shapiro J.I., Tian J. Signaling through the Na/K-ATPase: Implications for cardiac fibrosis. Am. J. Physiol. Heart Circ. Physiol. 2011;300:H29–H30. doi: 10.1152/ajpheart.01038.2010. [DOI] [PubMed] [Google Scholar]
- 132.Xie Z., Cai T. Na+-K+-ATPase-mediated signal transduction: From protein interaction to cellular function. Mol. Interv. 2003;3:157–168. doi: 10.1124/mi.3.3.157. [DOI] [PubMed] [Google Scholar]
- 133.Marck P.V., Pierre S.V. Na/K-ATPase Signaling and Cardiac Pre/Postconditioning with Cardiotonic Steroids. Int. J. Mol. Sci. 2018;19:2336. doi: 10.3390/ijms19082336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang L., Staehr C., Zeng F., Bouzinova E.V., Matchkov V.V. The Na,K-ATPase in vascular smooth muscle cells. Curr. Top. Membr. 2019;83:151–175. doi: 10.1016/bs.ctm.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 135.Pierre S.V., Yang C., Yuan Z., Seminerio J., Mouas C., Garlid K.D., Dos-Santos P., Xie Z. Ouabain triggers preconditioning through activation of the Na+,K+-ATPase signaling cascade in rat hearts. Cardiovasc. Res. 2007;73:488–496. doi: 10.1016/j.cardiores.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Belliard A., Gulati G.K., Duan Q., Alves R., Brewer S., Madan N., Sottejeau Y., Wang X., Kalisz J., Pierre S.V. Ischemia/reperfusion-induced alterations of enzymatic and signaling functions of the rat cardiac Na+/K+-ATPase: Protection by ouabain preconditioning. Physiol. Rep. 2016;4:e12991. doi: 10.14814/phy2.12991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Morita Y., Murakami T., Iwase T., Nagai K., Nawada R., Kouchi I., Akao M., Sasayama S. KATP channels contribute to the cardioprotection of preconditioning independent of anaesthetics in rabbit hearts. J. Mol. Cell. Cardiol. 1997;29:1267–1276. doi: 10.1006/jmcc.1996.0364. [DOI] [PubMed] [Google Scholar]
- 138.Imahashi K., Nishimura T., Yoshioka J., Kusuoka H. Role of intracellular Na+ kinetics in preconditioned rat heart. Circ. Res. 2001;88:1176–1182. doi: 10.1161/hh1101.092139. [DOI] [PubMed] [Google Scholar]
- 139.Slezak J., Tribulova N., Pristacova J., Uhrik B., Thomas T., Khaper N., Kaul N., Singal P.K. Hydrogen peroxide changes in ischemic and reperfused heart. Cytochemistry and biochemical and X-ray microanalysis. Am. J. Pathol. 1995;147:772–781. [PMC free article] [PubMed] [Google Scholar]
- 140.Gross G.J., Auchampach J.A. Blockade of ATP-sensitive potassium channels prevents myocardial preconditioning in dogs. Circ. Res. 1992;70:223–233. doi: 10.1161/01.RES.70.2.223. [DOI] [PubMed] [Google Scholar]
- 141.Tokube K., Kiyosue T., Arita M. Openings of cardiac KATP channel by oxygen free radicals produced by xanthine oxidase reaction. Am. J. Physiol. 1996;271:H478–H489. doi: 10.1152/ajpheart.1996.271.2.H478. [DOI] [PubMed] [Google Scholar]
- 142.Gross G.J., Fryer R.M. Sarcolemmal versus mitochondrial ATP-sensitive K+ channels and myocardial preconditioning. Circ. Res. 1999;84:973–979. doi: 10.1161/01.RES.84.9.973. [DOI] [PubMed] [Google Scholar]
- 143.Jovanovic A., Jovanovic S., Lorenz E., Terzic A. Recombinant cardiac ATP-sensitive K+ channel subunits confer resistance to chemical hypoxia-reoxygenation injury. Circulation. 1998;98:1548–1555. doi: 10.1161/01.CIR.98.15.1548. [DOI] [PubMed] [Google Scholar]
- 144.Marinovic J., Bosnjak Z.J., Stadnicka A. Distinct roles for sarcolemmal and mitochondrial adenosine triphosphate-sensitive potassium channels in isoflurane-induced protection against oxidative stress. Anesthesiology. 2006;105:98–104. doi: 10.1097/00000542-200607000-00018. [DOI] [PubMed] [Google Scholar]
- 145.Gumina R.J., Pucar D., Bast P., Hodgson D.M., Kurtz C.E., Dzeja P.P., Miki T., Seino S., Terzic A. Knockout of Kir6.2 negates ischemic preconditioning-induced protection of myocardial energetics. Am. J. Physiol. Heart Circ. Physiol. 2003;284:H2106–H2113. doi: 10.1152/ajpheart.00057.2003. [DOI] [PubMed] [Google Scholar]
- 146.Marinovic J., Ljubkovic M., Stadnicka A., Bosnjak Z.J., Bienengraeber M. Role of sarcolemmal ATP-sensitive potassium channel in oxidative stress-induced apoptosis: Mitochondrial connection. Am. J. Physiol. Heart Circ. Physiol. 2008;294:H1317–H1325. doi: 10.1152/ajpheart.00840.2007. [DOI] [PubMed] [Google Scholar]
- 147.Nakamura T., Hayashi H., Satoh H., Katoh H., Kaneko M., Terada H. A single cell model of myocardial reperfusion injury: Changes in intracellular Na+ and Ca2+ concentrations in guinea pig ventricular myocytes. Mol. Cell. Biochem. 1999;194:147–157. doi: 10.1023/A:1006919929104. [DOI] [PubMed] [Google Scholar]
- 148.Nayler W.G. The role of calcium in the ischemic myocardium. Am. J. Pathol. 1981;102:262–270. [PMC free article] [PubMed] [Google Scholar]
- 149.Nayler W.G., Panagiotopoulos S., Elz J.S., Daly M.J. Calcium-mediated damage during post-ischaemic reperfusion. J. Mol. Cell. Cardiol. 1988;20:41–54. doi: 10.1016/0022-2828(88)90331-8. [DOI] [PubMed] [Google Scholar]
- 150.Temsah R.M., Netticadan T., Chapman D., Takeda S., Mochizuki S., Dhalla N.S. Alterations in sarcoplasmic reticulum function and gene expression in ischemic-reperfused rat heart. Am. J. Physiol. 1999;277:H584–H594. doi: 10.1152/ajpheart.1999.277.2.H584. [DOI] [PubMed] [Google Scholar]
- 151.Osada M., Netticadan T., Tamura K., Dhalla N.S. Modification of ischemia-reperfusion-induced changes in cardiac sarcoplasmic reticulum by preconditioning. Am. J. Physiol. 1998;274:H2025–H2034. doi: 10.1152/ajpheart.1998.274.6.H2025. [DOI] [PubMed] [Google Scholar]
- 152.Temsah R.M., Kawabata K., Chapman D., Dhalla N.S. Preconditioning prevents alterations in cardiac SR gene expression due to ischemia-reperfusion. Am. J. Physiol. Heart Circ. Physiol. 2002;282:H1461–H1466. doi: 10.1152/ajpheart.00447.2001. [DOI] [PubMed] [Google Scholar]
- 153.Kuster G.M., Lancel S., Zhang J., Communal C., Trucillo M.P., Lim C.C., Pfister O., Weinberg E.O., Cohen R.A., Liao R., et al. Redox-mediated reciprocal regulation of SERCA and Na+-Ca2+ exchanger contributes to sarcoplasmic reticulum Ca2+ depletion in cardiac myocytes. Free Radic. Biol. Med. 2010;48:1182–1187. doi: 10.1016/j.freeradbiomed.2010.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kaplan P., Babusikova E., Lehotsky J., Dobrota D. Free radical-induced protein modification and inhibition of Ca2+-ATPase of cardiac sarcoplasmic reticulum. Mol. Cell. Biochem. 2003;248:41–47. doi: 10.1023/A:1024145212616. [DOI] [PubMed] [Google Scholar]
- 155.Zucchi R., Yu G., Galbani P., Mariani M., Ronca G., Ronca-Testoni S. Sulfhydryl redox state affects susceptibility to ischemia and sarcoplasmic reticulum Ca2+ release in rat heart. Implications for ischemic preconditioning. Circ. Res. 1998;83:908–915. doi: 10.1161/01.RES.83.9.908. [DOI] [PubMed] [Google Scholar]
- 156.Lotz C., Herrmann J., Notz Q., Meybohm P., Kehl F. Mitochondria and pharmacologic cardiac conditioning-at the heart of ischemic injury. Int. J. Mol. Sci. 2021;22:3224. doi: 10.3390/ijms22063224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Boengler K., Lochnit G., Schulz R. Mitochondria "THE" target of myocardial conditioning. Am. J. Physiol. Heart Circ. Physiol. 2018;315:H1215–H1231. doi: 10.1152/ajpheart.00124.2018. [DOI] [PubMed] [Google Scholar]
- 158.Vishwakarma V.K., Upadhyay P.K., Chaurasiya H.S., Srivasatav R.K., Ansari T.M., Srivastava V. Mechanistic pathways of ATP sensitive potassium channels referring to cardio-protective effects and cellular functions. Drug Res. 2019;69:365–373. doi: 10.1055/a-0806-7207. [DOI] [PubMed] [Google Scholar]
- 159.Cadenas S. ROS and redox signaling in myocardial ischemia-reperfusion injury and cardioprotection. Free Radic. Biol. Med. 2018;117:76–89. doi: 10.1016/j.freeradbiomed.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 160.Matejíková J., Kucharská J., Pintérová M., Pancza D., Ravingerová T. Protection against ischemia-induced ventricular arrhythmias and myocardial dysfunction conferred by preconditioning in the rat heart: Involvement of mitochondrial K(ATP) channels and reactive oxygen species. Physiol. Res. 2009;58:9–19. doi: 10.33549/physiolres.931317. [DOI] [PubMed] [Google Scholar]
- 161.Forbes R.A., Steenbergen C., Murphy E. Diazoxide-induced cardioprotection requires signaling through a redox-sensitive mechanism. Circ. Res. 2001;88:802–809. doi: 10.1161/hh0801.089342. [DOI] [PubMed] [Google Scholar]
- 162.Pagliaro P., Mancardi D., Rastaldo R., Penna C., Gattullo D., Miranda K.M., Feelisch M., Wink D.A., Kass D.A., Paolocci N. Nitroxyl affords thiol-sensitive myocardial protective effects akin to early preconditioning. Free Radic. Biol. Med. 2003;34:33–43. doi: 10.1016/S0891-5849(02)01179-6. [DOI] [PubMed] [Google Scholar]
- 163.Mancardi D., Pagliaro P., Ridnour L.A., Tocchetti C.G., Miranda K., Juhaszova M., Sollott S.J., Wink D.A., Paolocci N. HNO protects the myocardium against reperfusion injury, inhibiting the mPTP opening via PKCε activation. Antioxidants. 2022;11:382. doi: 10.3390/antiox11020382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Vanden Hoek T.L., Li C., Shao Z., Schumacker P.T., Becker L.B. Significant levels of oxidants are generated by isolated cardiomyocytes during ischemia prior to reperfusion. J. Mol. Cell. Cardiol. 1997;29:2571–2583. doi: 10.1006/jmcc.1997.0497. [DOI] [PubMed] [Google Scholar]
- 165.Fryer R.M., Eells J.T., Hsu A.K., Henry M.M., Gross G.J. Ischemic preconditioning in rats: Role of mitochondrial K(ATP) channel in preservation of mitochondrial function. Am. J. Physiol. Heart Circ. Physiol. 2000;278:H305–H3012. doi: 10.1152/ajpheart.2000.278.1.H305. [DOI] [PubMed] [Google Scholar]
- 166.Murphy E., Steenbergen C. What makes the mitochondria a killer? Can we condition them to be less destructive? Biochim. Biophys. Acta. 2011;1813:1302–1308. doi: 10.1016/j.bbamcr.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Penna C., Perrelli M.G., Pagliaro P. Mitochondrial pathways, permeability transition pore, and redox signaling in cardioprotection: Therapeutic implications. Antioxid. Redox Signal. 2013;18:556–599. doi: 10.1089/ars.2011.4459. [DOI] [PubMed] [Google Scholar]
- 168.Kussmaul L., Hirst J. The mechanism of superoxide production by NADH:ubiquinone oxidoreductase (complex I) from bovine heart mitochondria. Proc. Natl. Acad. Sci. USA. 2006;103:7607–7612. doi: 10.1073/pnas.0510977103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Stanley W.C., Recchia F.A., Lopaschuk G.D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 2005;85:1093–1129. doi: 10.1152/physrev.00006.2004. [DOI] [PubMed] [Google Scholar]
- 170.Fontaine E., Bernardi P. Progress on the mitochondrial permeability transition pore: Regulation by complex I and ubiquinone analogs. J. Bioenerg. Biomembr. 1999;31:335–345. doi: 10.1023/A:1005475802350. [DOI] [PubMed] [Google Scholar]
- 171.Wojtovich A.P., Brookes P.S. The endogenous mitochondrial complex II inhibitor malonate regulates mitochondrial ATP-sensitive potassium channels: Implications for ischemic preconditioning. Biochim. Biophys. Acta. 2008;1777:882–889. doi: 10.1016/j.bbabio.2008.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Nadtochiy S.M., Baker P.R., Freeman B.A., Brookes P.S. Mitochondrial nitroalkene formation and mild uncoupling in ischaemic preconditioning: Implications for cardioprotection. Cardiovasc. Res. 2009;82:333–340. doi: 10.1093/cvr/cvn323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Batthyany C., Schopfer F.J., Baker P.R., Durán R., Baker L.M., Huang Y., Cerveñansky C., Branchaud B.P., Freeman B.A. Reversible post-translational modification of proteins by nitrated fatty acids in vivo. J. Biol. Chem. 2006;281:20450–20463. doi: 10.1074/jbc.M602814200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yabe K., Nasa Y., Sato M., Iijima R., Takeo S. Preconditioning preserves mitochondrial function and glycolytic flux during an early period of reperfusion in perfused rat hearts. Cardiovasc. Res. 1997;33:677–685. doi: 10.1016/S0008-6363(96)00269-6. [DOI] [PubMed] [Google Scholar]
- 175.Zuurbier C.J., Eerbeek O., Meijer A.J. Ischemic preconditioning, insulin, and morphine all cause hexokinase redistribution. Am. J. Physiol. Heart Circ. Physiol. 2005;289:H496–H499. doi: 10.1152/ajpheart.01182.2004. [DOI] [PubMed] [Google Scholar]
- 176.Sun L., Shukair S., Naik T.J., Moazed F., Ardehali H. Glucose phosphorylation and mitochondrial binding are required for the protective effects of hexokinases I and II. Mol. Cell Biol. 2008;28:1007–1017. doi: 10.1128/MCB.00224-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Osada M., Netticadan T., Kawabata K., Tamura K., Dhalla N.S. Ischemic preconditioning prevents I/R-induced alterations in SR calcium-calmodulin protein kinase II. Am. J. Physiol. Heart Circ. Physiol. 2000;278:H1791–H1798. doi: 10.1152/ajpheart.2000.278.6.H1791. [DOI] [PubMed] [Google Scholar]
- 178.Zhang M., Xu Y.J., Saini H.K., Turan B., Liu P.P., Dhalla N.S. TNF-α as a potential mediator of cardiac dysfunction due to intracellular Ca2+-overload. Biochem. Biophys. Res. Commun. 2005;327:57–63. doi: 10.1016/j.bbrc.2004.11.131. [DOI] [PubMed] [Google Scholar]
- 179.Qian W., Zhao C., Li D., Dai R. Mechanism of interleukin-1 receptor antagonist protection against myocardial ischaemia/reperfusion-induced injury. Arch. Cardiovasc. Dis. 2018;111:545–554. doi: 10.1016/j.acvd.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 180.Wang H.Y., Liu X.Y., Han G., Wang Z.Y., Li X.X., Jiang Z.M., Jiang C.M. LPS induces cardiomyocyte injury through calcium-sensing receptor. Mol. Cell. Biochem. 2013;379:153–159. doi: 10.1007/s11010-013-1637-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Smart N., Mojet M.H., Latchman D.S., Marber M.S., Duchen M.R., Heads R.J. IL-6 induces PI 3-kinase and nitric oxide-dependent protection and preserves mitochondrial function in cardiomyocytes. Cardiovasc. Res. 2006;69:164–177. doi: 10.1016/j.cardiores.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 182.Meldrum D.R. Tumor necrosis factor in the heart. Am. J. Physiol. 1998;274:R577–R595. doi: 10.1152/ajpregu.1998.274.3.R577. [DOI] [PubMed] [Google Scholar]
- 183.Wojciechowska M., Zarębiński M., Pawluczuk P., Szukiewicz D. Decreased effectiveness of ischemic heart preconditioning in the state of chronic inflammation. Med. Hypotheses. 2015;85:675–679. doi: 10.1016/j.mehy.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 184.Wang Y.Y., Yin B.L. Pro-inflammatory cytokines may induce late preconditioning in unstable angina patients. Med. Hypotheses. 2006;67:1121–1124. doi: 10.1016/j.mehy.2006.04.060. [DOI] [PubMed] [Google Scholar]
- 185.Zubakov D., Hoheisel J.D., Kluxen F.W., Brändle M., Ehring T., Hentsch B., Frohme M. Late ischemic preconditioning of the myocardium alters the expression of genes involved in inflammatory response. FEBS. Lett. 2003;547:51–55. doi: 10.1016/S0014-5793(03)00667-7. [DOI] [PubMed] [Google Scholar]
- 186.Lecour S., Smith R.M., Woodward B., Opie L.H., Rochette L., Sack M.N. Identification of a novel role for sphingolipid signaling in TNFα and ischemic preconditioning mediated cardioprotection. J. Mol. Cell. Cardiol. 2002;34:509–518. doi: 10.1006/jmcc.2002.1533. [DOI] [PubMed] [Google Scholar]
- 187.Meldrum D.R., Dinarello C.A., Shames B.D., Cleveland J.C., Jr., Cain B.S., Banerjee A., Meng X., Harken A.H. Ischemic preconditioning decreases postischemic myocardial tumor necrosis factor-α production. Potential ultimate effector mechanism of preconditioning. Circulation. 1998;98:II214–II218. [PubMed] [Google Scholar]
- 188.Xiong J., Wang Q., Xue F.S., Yuan Y.J., Li S., Liu J.H., Liao X., Zhang Y.M. Comparison of cardioprotective and anti-inflammatory effects of ischemia pre- and postconditioning in rats with myocardial ischemia-reperfusion injury. Inflamm. Res. 2011;60:547–554. doi: 10.1007/s00011-010-0303-4. [DOI] [PubMed] [Google Scholar]
- 189.Maulik N., Engelman R.M., Wei Z., Lu D., Rousou J.A., Das D.K. Interleukin-1 α preconditioning reduces myocardial ischemia reperfusion injury. Circulation. 1993;88:II387–II394. [PubMed] [Google Scholar]
- 190.McGinnis G.R., Ballmann C., Peters B., Nanayakkara G., Roberts M., Amin R., Quindry J.C. Interleukin-6 mediates exercise preconditioning against myocardial ischemia reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2015;308:H1423–H1433. doi: 10.1152/ajpheart.00850.2014. [DOI] [PubMed] [Google Scholar]
- 191.Ma J., Qiao Z., Xu B. Effects of ischemic preconditioning on myocardium Caspase-3, SOCS-1, SOCS-3, TNF-α and IL-6 mRNA expression levels in myocardium IR rats. Mol. Biol. Rep. 2013;40:5741–5748. doi: 10.1007/s11033-013-2677-1. [DOI] [PubMed] [Google Scholar]
- 192.Hiasa G., Hamada M., Ikeda S., Hiwada K. Ischemic preconditioning and lipopolysaccharide attenuate nuclear factor-κB activation and gene expression of inflammatory cytokines in the ischemia-reperfused rat heart. Jpn. Circ. J. 2001;65:984–990. doi: 10.1253/jcj.65.984. [DOI] [PubMed] [Google Scholar]
- 193.Zuurbier C.J., Jong W.M., Eerbeek O., Koeman A., Pulskens W.P., Butter L.M., Leemans J.C., Hollmann M.W. Deletion of the innate immune NLRP3 receptor abolishes cardiac ischemic preconditioning and is associated with decreased Il-6/STAT3 signaling. PLoS ONE. 2012;7:e40643. doi: 10.1371/journal.pone.0040643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Dawn B., Xuan Y.T., Guo Y., Rezazadeh A., Stein A.B., Hunt G., Wu W.J., Tan W., Bolli R. IL-6 plays an obligatory role in late preconditioning via JAK-STAT signaling and upregulation of iNOS and COX-2. Cardiovasc. Res. 2004;64:61–71. doi: 10.1016/j.cardiores.2004.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Müller A.L., Hryshko L.V., Dhalla N.S. Extracellular and intracellular proteases in cardiac dysfunction due to ischemia-reperfusion injury. Int. J. Cardiol. 2013;164:39–47. doi: 10.1016/j.ijcard.2012.01.103. [DOI] [PubMed] [Google Scholar]
- 196.Batista-Almeida D., Martins-Marques T., Ribeiro-Rodrigues T., Girao H. The role of proteostasis in the regulation of cardiac intercellular communication. Adv. Exp. Med. Biol. 2020;1233:279–302. doi: 10.1007/978-3-030-38266-7_12. [DOI] [PubMed] [Google Scholar]
- 197.Singh R.B., Hryshko L., Freed D., Dhalla N.S. Activation of proteolytic enzymes and depression of the sarcolemmal Na+/K+-ATPase in ischemia-reperfused heart may be mediated through oxidative stress. Can. J. Physiol. Pharmacol. 2012;90:249–260. doi: 10.1139/y11-128. [DOI] [PubMed] [Google Scholar]
- 198.Venkatesh S., Li M., Saito T., Tong M., Rashed E., Mareedu S., Zhai P., Bárcena C., López-Otín C., Yehia G., et al. Mitochondrial LonP1 protects cardiomyocytes from ischemia/reperfusion injury in vivo. J. Mol. Cell. Cardiol. 2019;128:38–50. doi: 10.1016/j.yjmcc.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 199.Mata A., Cadenas S. The antioxidant transcription factor Nrf2 in cardiac ischemia-reperfusion injury. Int. J. Mol. Sci. 2021;22:11939. doi: 10.3390/ijms222111939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Xu B., Zhang J., Strom J., Lee S., Chen Q.M. Myocardial ischemic reperfusion induces de novo Nrf2 protein translation. Biochim. Biophys. Acta. 2014;1842:1638–1647. doi: 10.1016/j.bbadis.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ucar B.I., Ucar G., Saha S., Buttari B., Profumo E., Saso L. Pharmacological protection against ischemia-reperfusion injury by regulating the Nrf2-Keap1-ARE signaling pathway. Antioxidants. 2021;10:823. doi: 10.3390/antiox10060823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cheng L., Jin Z., Zhao R., Ren K., Deng C., Yu S. Resveratrol attenuates inflammation and oxidative stress induced by myocardial ischemia-reperfusion injury: Role of Nrf2/ARE pathway. Int. J. Clin. Exp. Med. 2015;8:10420–10428. [PMC free article] [PubMed] [Google Scholar]
- 203.Purdom-Dickinson S.E., Lin Y., Dedek M., Morrissy S., Johnson J., Chen Q.M. Induction of antioxidant and detoxification response by oxidants in cardiomyocytes: Evidence from gene expression profiling and activation of Nrf2 transcription factor. J. Mol. Cell. Cardiol. 2007;42:159–176. doi: 10.1016/j.yjmcc.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Taguchi K., Motohashi H., Yamamoto M. Molecular mechanisms of the Keap1-Nrf2 pathway in stress response and cancer evolution. Genes Cells. 2011;16:123–140. doi: 10.1111/j.1365-2443.2010.01473.x. [DOI] [PubMed] [Google Scholar]
- 205.Tkachev V.O., Menshchikova E.B., Zenkov N.K. Mechanism of the Nrf2/Keap1/ARE signaling system. Biochemistry. 2011;76:407–422. doi: 10.1134/S0006297911040031. [DOI] [PubMed] [Google Scholar]
- 206.Maldonado E., Rojas D.A., Urbina F., Solari A. The use of antioxidants as potential co-adjuvants to treat chronic chagas disease. Antioxidants. 2021;10:1022. doi: 10.3390/antiox10071022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Wang J., De-Qiong X., Hong D.Q., Zhang Q.Q., Zhang J. Attenuation of myocardial ischemia reperfusion injury by Geniposide preconditioning in diabetic rats. Curr. Res. Transl. Med. 2019;67:35–40. doi: 10.1016/j.retram.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 208.Yu L.M., Dong X., Xue X.D., Zhang J., Li Z., Wu H.J., Yang Z.L., Yang Y., Wang H.S. Protection of the myocardium against ischemia/reperfusion injury by punicalagin through an SIRT1-NRF-2-HO-1-dependent mechanism. Chem. Biol. Interact. 2019;306:152–162. doi: 10.1016/j.cbi.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 209.Radjendirane V., Joseph P., Lee Y.H., Kimura S., Klein-Szanto A.J., Gonzalez F.J., Jaiswal A.K. Disruption of the DT diaphorase (NQO1) gene in mice leads to increased menadione toxicity. J. Biol. Chem. 1998;273:7382–7389. doi: 10.1074/jbc.273.13.7382. [DOI] [PubMed] [Google Scholar]
- 210.Ku B.M., Joo Y., Mun J., Roh G.S., Kang S.S., Cho G.J., Choi W.S., Kim H.J. Heme oxygenase protects hippocampal neurons from ethanol-induced neurotoxicity. Neurosci. Lett. 2006;405:168–171. doi: 10.1016/j.neulet.2006.06.052. [DOI] [PubMed] [Google Scholar]
- 211.Refaie M.M.M., Shehata S., Ibrahim R.A., Bayoumi A.M.A., Abdel-Gaber S.A. Dose-dependent cardioprotective effect of hemin in doxorubicin-induced cardiotoxicity via Nrf-2/HO-1 and TLR-5/NF-κB/TNF-α signaling pathways. Cardiovasc. Toxicol. 2021;21:1033–1044. doi: 10.1007/s12012-021-09694-7. [DOI] [PubMed] [Google Scholar]
- 212.Shen Y., Liu X., Shi J., Wu X. Involvement of Nrf2 in myocardial ischemia and reperfusion injury. Int. J. Biol. Macromol. 2019;125:496–502. doi: 10.1016/j.ijbiomac.2018.11.190. [DOI] [PubMed] [Google Scholar]
- 213.Wang L., Tang Y., He H., Wei W. Liraglutide restores late cardioprotective effects of remote preconditioning in diabetic rats via activation of hydrogen sulfide and nuclear factor erythroid 2-related factor 2 signaling pathway. Acta Cir. Bras. 2021;36:e360207. doi: 10.1590/acb360207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Huang X.S., Chen H.P., Yu H.H., Yan Y.F., Liao Z.P., Huang Q.R. Nrf2-dependent upregulation of antioxidative enzymes: A novel pathway for hypoxic preconditioning-mediated delayed cardioprotection. Mol. Cell. Biochem. 2014;385:33–41. doi: 10.1007/s11010-013-1812-6. [DOI] [PubMed] [Google Scholar]
- 215.Yan Y.F., Chen H.P., Huang X.S., Qiu L.Y., Liao Z.P., Huang Q.R. DJ-1 mediates the delayed cardioprotection of hypoxic preconditioning through activation of Nrf2 and subsequent upregulation of antioxidative enzymes. J. Cardiovasc. Pharmacol. 2015;66:148–158. doi: 10.1097/FJC.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 216.Zhang X., Yu Y., Lei H., Cai Y., Shen J., Zhu P., He Q., Zhao M. The Nrf-2/HO-1 Signaling Axis: A Ray of Hope in Cardiovascular Diseases. Cardiol. Res. Pract. 2020;2020:5695723. doi: 10.1155/2020/5695723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wang H., Shi X., Cheng L., Han J., Mu J. Hydrogen sulfide restores cardioprotective effects of remote ischemic preconditioning in aged rats via HIF-1α/Nrf2 signaling pathway. Korean J. Physiol. Pharmacol. 2021;25:239–249. doi: 10.4196/kjpp.2021.25.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Cominacini L., Mozzini C., Garbin U., Pasini A., Stranieri C., Solani E., Vallerio P., Tinelli I.A., Fratta Pasini A. Endoplasmic reticulum stress and Nrf2 signaling in cardiovascular diseases. Free Radic. Biol. Med. 2015;88:233–242. doi: 10.1016/j.freeradbiomed.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 219.Zhang X., Xiao Z., Yao J., Zhao G., Fa X., Niu J. Participation of protein kinase C in the activation of Nrf2 signaling by ischemic preconditioning in the isolated rabbit heart. Mol. Cell. Biochem. 2013;372:169–179. doi: 10.1007/s11010-012-1458-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.