Abstract
Introduction: Telemedicine interventions are gradually being used in primary health care to help patients with type 2 diabetes receive ongoing medical guidance. The purpose of this study was to analyze the effectiveness of using telemedicine in primary health care for the management of patients with type 2 diabetes. Methods: A systematic search was conducted from database inception to August 2021 in nine databases, including PubMed, Web of Science, Cochrane Library, EMBASE, EBSCO, CNKI, Wanfang Data, VIP, and CBM. Data extraction and quality assessment were performed for studies that met the inclusion criteria. The meta-analysis was performed using Review Manager 5.4 (Cochrane) and Stata v.16.0SE (College Station, TX, USA). Results: A total of 32 articles were included in this study. Analysis showed a reduction in glycated hemoglobin, fasting glucose, and postprandial glucose after the telemedicine intervention. Systolic blood pressure and self-efficacy improved significantly, but there was no significant improvement in weight, lipid metabolism, or diabetes awareness. Subgroup analysis based on the duration of intervention showed significant improvement in glycated hemoglobin at 6 months of intervention. Conclusions: Telemedicine interventions may help patients with type 2 diabetes to effectively control blood glucose and improve self-management in primary health care. There is only moderate benefit, and the benefit may not be sustained beyond 6 months. However, the evidence for the improvement in lipid metabolism is insufficient and further studies are needed.
Keywords: telemedicine, type 2 diabetes, primary health care, meta-analysis
1. Introduction
The International Diabetes Federation 2021 reported that the number of people with diabetes mellitus (DM) has reached 533 million worldwide and is expected to reach 783 million worldwide by 2045. The prevalence rate is as high as 12.2% [1], of which type 2 diabetes (T2DM) [2] accounts for 90%. During the COVID-19 pandemic, the vulnerability of people with diabetes to public health emergencies became even more pronounced, with at least a two-fold increase in the risk of serious illness or mortality [3]. Telemedicine is a branch of e-health that uses communication networks to deliver healthcare services and health education to patients across regions [4]. Telemedicine is a viable alternative for patients seeking medical guidance for a chronic condition such as diabetes that requires repeated consultations with a physician, and without the risk of COVID-19 infection [5]. At the same time, telemedicine can provide patients with opportunities to connect and learn online and expand access to care through self-management and diabetes education [6]. It also allows for the involvement of both patients and the healthcare team to provide solutions to the patient’s needs [7]. Globally, the vast majority of people with T2DM are treated in primary health care settings [8]. Primary care is seen as the ideal point for making lifestyle changes [9]. Many countries have identified primary care telemedicine as a future development priority [10,11]. Therefore, this study aimed to analyze the effectiveness of telemedicine in primary health care for patients with T2DM.
Most previous studies on telemedicine for diabetes focused on the effect of telemedicine on the ability to self-manage diabetes [12], the impact of certain interventions on T2DM self-management [13] that are not specific to the primary health care setting [14], and other specific aspects [15]. Although there have been published reviews of the effectiveness of telemedicine research [16,17] on diabetes, there is a lack of analysis of all the potential outcomes and the impact of telemedicine interventions on patients with type 2 diabetes. In addition, telemedicine has grown rapidly in recent years and new research has emerged, thus requiring an updated review. Therefore, this study systematically reviewed the literature on telemedicine and evaluated the effectiveness of telemedicine technology for diabetes self-management with health outcomes among type 2 diabetes within the primary health care setting.
2. Methods
The meta-analysis was performed based on the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18].
2.1. Search Strategy
The search was conducted in PubMed, Web of Science, Cochrane Library, EMBASE, EBSCO, CNKI, Wanfang Data, VIP, and CBM using a combination of subject terms, free terms, and MeSH terms from the time of database inception to 31 January 2021. Search terms included “type 2 diabetes”, “telemedicine”, “mobile health”, “primary health care”, and “community health services”. The review was registered prospectively (PROSPERO CRD42021299095). The list of search strategies is shown in detail in Appendix A. To prevent omissions, a snowball search was conducted for references of included articles and relevant reviews to supplement the relevant literature. No language restrictions were placed on the search terms.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria for articles were as follows: (a) patients ≥18 years of age with T2DM; (b) since telemedicine is defined as the remote collection of records and transmission of patient data via telecommunications systems to healthcare providers for analysis and decision-making [19], email, smartphone, phone, SMS and text messages, web-based platforms, and hybrid forms (video calls and text messages) were included, without any face-to-face contact by a healthcare practitioner during the intervention; (c) improving one or more areas of diabetes self-management through telehealth; (d) control group using conventional treatment; (e) randomized controlled trial.
Exclusion criteria were (a) duplicate publications, (b) inaccessibility of full texts or extracted data, (c) studies without clinical data (abstract presentations, case reports, review articles, case-control, pilot studies, or study protocols), and (d) special populations such as children and pregnant women with T2DM.
2.3. Literature Screening and Data Extraction
Two researchers screened titles and abstracts that met the requirements based on the inclusion criteria, and when disagreements arose, a third researcher was consulted. If applicable, the disagreements were recorded to ensure a final consensus among the three reviewers. The literature searches were managed using EndNote X9 (Thomson ResearchSoft; Stanford, CT, USA).
Two researchers independently extracted relevant data from the included studies using a self-designed form, including information on the author, year of publication, country, intervention method, and outcomes of both protocols in each of the clinical studies. In multiple-group studies, only telemedicine interventions and the conventional treatment groups were selected for comparison. For studies that could not be extracted or for which data were missing, attempts were made to contact the authors to obtain the data.
2.4. Methodological Quality Evaluation
The methodological quality of the included studies was independently evaluated by two investigators using the Critical Appraisal Skills Program (CASP) [20]. This list consists of 11 entries with three results: “yes”, “unclear”, and “no”. Disagreements, if any, were resolved through discussion with a third investigator or with the entire team.
2.5. Risk Bias Evaluation
Two researchers used Risk of Bias from the Cochrane Handbook for Systematic Review of Interventions 5.1.0 (2019) [21] to independently evaluate risk bias in the included studies. Bias included random sequence generation, allocation concealment, blinding of subjects and intervention providers, blinding of outcome evaluators, incomplete outcome data, selective reporting, and other sources of bias. Disagreements, if any, were resolved by discussion with a third author or by a discussion with the entire team.
2.6. Statistical Analysis
Meta-analysis was conducted using Review Manager 5.4 (Cochrane Collaboration, Oxford, UK) and Stata v.16.0SE (College Station, TX, USA) in this study. Continuous data were used with a mean and standard deviation as effect measures and estimates (MD) and 95% confidence intervals (CI) were given for each effect measure. We used the chi-square test (p < 0.01, statistically significant difference) and I2 to assess the heterogeneity between studies. When I2 < 50%, it indicated that there was no significant heterogeneity among studies, so a fixed-effect model was used; when I2 > 50%, it indicated that there was significant heterogeneity among studies, and a random-effects model was used. Sensitivity analysis was performed using a case-by-case exclusion approach to assess the stability of the study results. The presence of publication bias was assessed by a funnel plot and Egger and Begg tests when ≥10 studies were included with a two-sided significance level (p < 0.05, difference statistically significant). Subgroup analysis was used to observe the differences between intervention times.
3. Results
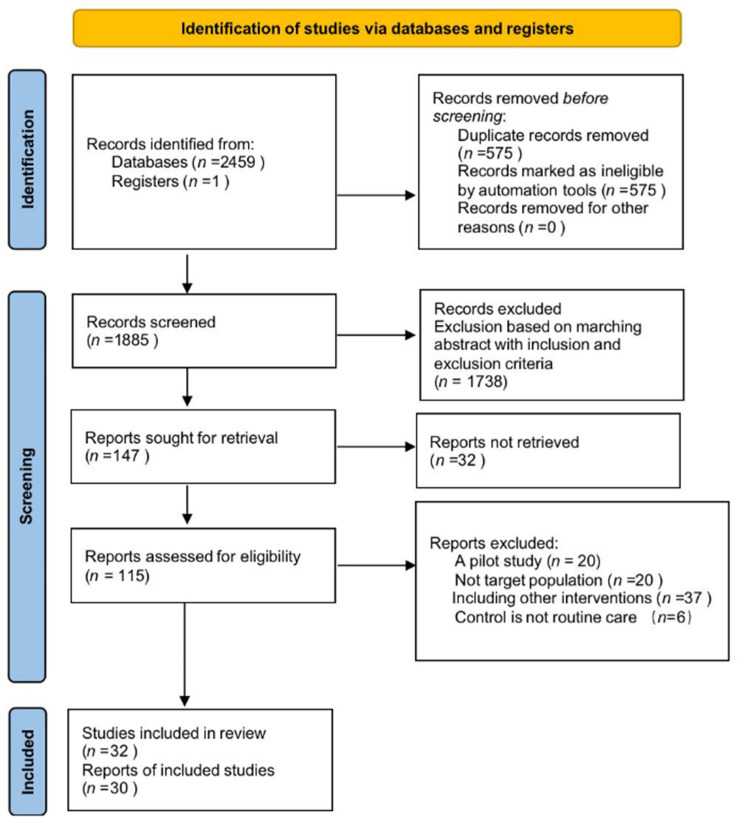
A total of 2460 articles were obtained through the search. After de-duplication, 1885 articles remained. After screening the titles and abstracts, a total of 147 studies were eligible. The PRISMA flow chart depicts the process of the literature screening (Figure 1).
Figure 1.
Flow diagram of preferred reporting items for systematic reviews and meta-analyses.
3.1. Characteristics of Included Studies
Among the 32 included studies [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53], 14 were from the United States, 3 from China, 2 from Spain, 2 from Australia, 2 from India, and 1 each from Australia, Iran, the United Kingdom, Slovenia, Sub-Saharan Africa, Canada, Belgium, Norway, Poland, and Italy. The studies ranged from 3 to 24 months of intervention between 2009 and 2021. Telemedicine in these studies used a variety of platforms to communicate and deliver the interventions, including cell phones (17.5%), Internet (17.5%), text messaging (27.5%), apps (20%), glucose-monitoring devices (12.5%), and tablets (5%). Some studies used a health belief model (13.3%), a trans-theoretical model of behavior change (26.7%), motivational interviewing (26.7%), social cognitive theory (13.3%), or chronic disease health management (20%) as part of the intervention. Intervention providers included physicians (18.9%), nurses (32.4%), allied health professionals (health education providers 5.5%; diabetes educators 2.7%; registered dietitians 2.7%; community workers 2.7%; telephone counselors 2.7%), and school research teams (32.4%). In addition, the content of routine care provided varied across studies, but in the majority of these studies, routine care provided general diabetes management. The details are shown in Table 1 and Table 2.
Table 1.
Characteristics of telemedicine studies.
| Author (Year) Country |
Interveners | Intervention Basis | Intervention Method | Routine Group | Intervention Time; Frequency | Primary Outcome | Secondary Outcome | Intervention Method | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Education | Feedback | Counseling | Goals | Prompt | Motivation | Monitoring | ||||||||
| Stephen Agboola (2016) USA [22] |
Health literacy concepts, the transtheoretical model of behavior change | SMS, pedometers (monitoring and uploading data) | Reminder telephone calls for those participants who did not upload their activity data after 5 consecutive days, and usual care. | 6 months; 2 text messages daily |
Mean step counts (collected by the wireless pedometers) | HbA1c, weight, physical activity stage of change questionnaire, usability and satisfaction | Y | Y | Y | Y | Y | |||
| Daniel J. Amante (2021) USA [39] |
AADE National Standards for Diabetes Self-Management Education curriculum | SMBG, the Livongo Care Team of CDEs would contact participants by their preferred communication method (either phone call or text message) within 3 min of receiving an abnormal SMBG notification from the Smart Cloud. | Usual care | 6 months; within 3 min after receiving the abnormal SMBG notification |
Changes in HbA1c during each time period | Diabetes Treatment Satisfaction Questionnaire (DTSQ) | Y | Y | ||||||
| Charlene C. Quinn (2011) USA [50] |
Doctor | Mobile diabetes management software application and a web portal | Usual care | 12 months; real time based on feedback |
HbA1c | Patient Health Questionnaire-9 (PHQ), Diabetes Distress Scale, Self-Completion Patient Outcome Instrument, diabetes complications (blood pressure, lipid levels) | Y | Y | Y | |||||
| Daren R. Anderson (2010) Spain [34] |
EHR nurses | Telephonic disease management | Usual care | 12 months; patients were called weekly, bi-weekly, or monthly depending on their risk stratification. |
HbA1c | BMI, SBP, DBP, and LDL | Y | Y | ||||||
| Rade Iljaž (2017) Slovenia [46] |
Health-care providers | e-Diabetes application: upload data and send automatic alerts via simple email and text messages | Usual care | 12 months; data were recorded every two weeks. These reminders were sent if a user had not entered body weight, blood pressure, physical activity, and diet data within 2 weeks of the deadline or not completed the COOP-WONCA questionnaire within 8 weeks. |
Change from baseline of HbA1c at 1 year | HbA1c at 6 months, BMI, COOP-WONCA Questionnaire, blood lipids, SBP, DBP | Y | Y | Y | |||||
| Ramachandran Vinitha (2019) India [43] |
Health education SMS | Usual care | 24 months; 2–3 educatory text messages per week |
HbA1c | FPG, 2hPG, lipid parameters, weight, waist circumference, blood pressure, physical activity, quality of life and dietary aspects, acceptability of text messages | Y | ||||||||
| Samuel N. Forjuoh (2014) USA [51] |
a. CDSMP(chronic disease self-management program); b. PDA(diabetes self-care software); c. a combination of both interventions (CDSMP + PDA) | Usual care | 12 months; enter every day |
HbA1c | BMI and Blood pressure, along with several self-management behavioral measures (e.g., foot care) | Y | ||||||||
| Deborah A. Greenwood (2015) USA [27] |
Diabetes educators | In-home tablet computer: telehealth remote monitoring system | Usual care | 6 months; every day |
HbA1c | Diabetes Knowledge Test (DKT), Summary of Diabetes Self-Care Activities (SDSCA), Diabetes Empowerment Scale short form (DES-SF) | Y | Y | Y | |||||
| Jing Kang (2021) China [44] |
Doctor, nurse | WeChat app | Usual care | 3 months; twice a week |
FBG, PBG, BMI, blood glucose, TIR, and blood pressure | Y | Y | Y | Y | |||||
| Maryam Peimani (2016) Iran [42] |
Social cognitive theory | a. Tailored SMS group; b. non-tailored SMS group | Usual care | 3 months; 7 messages per week |
HgA1C levels, FBS, lipid profile, BMI, Self-Care Inventory (SCI), Diabetes Management Self-Efficacy Scale (DMSES) | Y | Y | Y | ||||||
| Paul C. Tang (2013) USA [29] |
Nurse-led, multidisciplinary health team | Universal models of behavior change, motivational interviewing techniques, Chronic Care Model | The PAMF Online-mediated Personalized Health Care Program, which couples a multidisciplinary diabetes care management team with an EHR-integrated Online Disease Management (ODM) system | Usual care | 12 months; periodically uploading data |
HbA1c | Blood pressure, LDL, 10-year Framingham cardiovascular risk, satisfactionand psychosocial well-being | Y | Y | Y | ||||
| Payal Agarwal (2019) Canada [33] |
Transtheoretical Model of Behavior Change | BlueStar mobile app: customized, evidence-based messages are delivered in real time based on information uploaded by patients. | Usual care | 3 months; every day |
HbA1c | Patient-reported outcomes measures (PROMs), patient-reported experience measures (PREMs), EuroQol-5D (EQ-5D), Problem Areas in Diabetes (PAID), The Summary of Diabtes Self-Care Activities Measure (SDSCA-6), availability | Y | Y | Y | |||||
| Gretchen A. Benson (2019) USA [38] |
Registered dietitian nutritionist (RDN) | Health Belief Model, Transtheoretical Model | Phone coaching intervention: medical nutrition therapy (MNT), combined with pharmacotherapy | No intervention | 12 months; intervention calls generally lasted about 30 min, with a specific call frequency tailored to patient preferences. |
The composite number of diabetes optimal care goals met | BMI, LDL, Morisky scale | Y | Y | Y | ||||
| Maria Magdalena Bujnowska-Fedak (2011) Poland [37] |
Nurse | Telehome monitoring system | Usual care | 6 months; upload data at least once a week and receive a text message if you exceed the alarm line. |
Regular glucometry, HbA1c, blood cell count, erythrocyte sedimentation rate, cholesterol balance, body mass index, creatinine concentration, urine analysis, blood serum electrolytes, blood pressure | Quality of life, doctor–patient communication, sense of control over the disease | Y | Y | ||||||
| Claudio Dario (2017) Italy [23] |
Telehealth service: Patients were equipped at home with a glucometer and a gateway for data transmission to a Regional eHealth Center (ReHC). | Usual care | 12 months; every day |
HRQoL: SF-20 questionnaire | HbA1c, outpatient, emergency, hospitalization rates, bed days of hospital care, Hospital Anxiety and Depression Scale (HADS) | Y | ||||||||
| Addie L. Fortmann (2017) USA [47] |
Culturally appropriate DSME curriculum | Dulce Digital participants received up to motivational, educational, and/or call-to-action SMS. | Usual care | 6 months; two to three messages a day were sent at study start, with frequency tapering over 6 months. |
HbA1c and lipids (TC, LDL, HDL, and TG), SBP, DBP, body weight and height, self-report items, feasibility, acceptability | Y | Y | Y | ||||||
| Heidi Holmen, MSc (2014) Norway [31] |
GPs, health providers | a. Few Touch Application (FTA): diabetes diary app; b. the FTA with health counseling (FTA-HC): increase health counseling | Usual care | 12 months | HbA1c | Health Education Impact Questionnaire (heiQ), Short-Form 36v2 Health Survey (SF-36), Center for Epidemiologic Studies Depression Scale (CES-D) | Y | Y | Y | Y | ||||
| Yanmei Wang (2019) China [41] |
Nurse | Mobile application: health monitoring, health guide, gealth advice, follow-up | Usual care | 6 months; patients upload data on a daily basis and the nurses evaluate them 2 to 3 days a week. |
Glycemic control compliance rate, self-management ability of patients with diabetes, questionnaire on disease awareness, rehospitalization rate and number of hospital visits | Y | Y | Y | Y | Y | ||||
| Sarah H. Wild (2016) UK [49] |
Nurse | Telemonitoring and glycemic control | Usual care | 9 months; one fasting and one nonfasting blood glucose at least twice weekly and BP and weight measured at least weekly |
HbA1c | Ambulatory systolic, DBP, weight, anxiety, depression, quality of life, self-efficacy, self-reported physical activity, self-reported exercise tolerance, self-reported alcohol intake, diabetes knowledge | Y | Y | ||||||
| I Odnoletkova (2016) Belgium [28] |
Nurse | COACH Program: an update of the best practice guidelines for the management of type 2 diabetes, motivational interviewing techniques and software program use | Usual care | 6 months; an average of 5 times over 6 months, each time 10–45 min |
HbA1c | TC, LDL, HDL, TG, blood pressure, BMI, self-perceived health status, diabetes-specific emotional distress, satisfaction, annual healthcare utilization | Y | Y | Y | Y | ||||
| Heather M. Young (2020) USA [30] |
Nurse | Motivational interviewing | Wearable tracking device (Basis Peak, then Garmin VivoSmart Heart Rate), telephone | Usual care | 9 months; conference call every 2 weeks for 3 months, real-time data upload |
Diabetes self-efficacy (Diabetes Empowerment Scale [DES]–Short Form) | Depression severity (Patient Health Questionnaire-9 (PHQ-9), physical function, emotional distress, anxiety, Perceived Stress Scale (PSS) | Y | Y | Y | Y | |||
| Elizabeth G. Eakin (2014) Australia [35] |
Telephone counselor | Motivational interviewing, social cognitive theory | Telephone counseling | Usual care | 18 months; 4 initial weekly calls, fortnightly calls for 5 months, monthly calls for 12 months |
Weight, accelerometer-derived MVPA, HbA1c | Dietary energy intake, diet quality, waist circumference, fasting blood lipid levels, blood pressure | Y | Y | Y | Y | |||
| Roslyn A. Stone (2010) USA [53] |
Nurse | ACM + HT: home telemonitoring coupled with active medication management by a nurse practitioner | Monthly telephone calls from the study’s diabetes nurse educator | 6 months; patients upload data daily and nurses provide timely phone contact. |
HbA1c, blood pressure, weight, a fasting lipid panel | Medication regimen (dose), changes in the regimen (dose and date) | Y | Y | Y | |||||
| Yakun Feng (2016) China [52] |
Doctor, nurse | U-Healthcare: Patients upload data and doctors give feedback over the phone or on the web. | Usual care | 6 months; 2 times a week |
HbA1c, FPG, 2 hPG, TG, TC, HDL, LDL, BMI, SBP, DBP, BUN, Scr, AST, ALT, r-GT | Y | Y | Y | ||||||
| Leonard E. Egede (2021) USA [25] |
Nurse case manager, doctor | Web-based TACM intervention: the FORA 2-in-1 Telehealth System for diabetes to link a case manager to poorly controlled diabetics in real time. | Usual care | 6 months; patients upload data on a daily basis and nurses adjust patients’ medication weekly or biweekly under the supervision of doctors. |
BP, QOL: 12-item Short-Form Health Survey (SF-12) | Y | ||||||||
| María I. Rodríguez-Idígoras (2009) Spain [24] |
Doctor, nurse | Telemedicine system: possibility of sending the SMBG values of the patients to a web page via mobile SMS messages. The HCP had a password access to this web page to check the blood glucose values of the patients and if necessary send to them SMS messages with recommendations. | No intervention | 12 months; send text messages if necessary |
HbA1c | Blood glucose, TC, HDL, LDL, TG, BMI, SBP, DBP, and system adherence | Y | Y | Y | |||||
| A. Farmer (2021) Sub-Saharan Africa [48] |
Capability, opportunity, Motivation Behavior Model | SMS | Usual care | 12 months; three to four times a week |
HbA1c | Systolic blood pressure, Lipids, EuroQol 5-Dimension 3-Level (EQ-5D-3L), cardiovascular risk and the proportion of participants reaching treatment goals | Y | Y | Y | |||||
| Timothy Middleton (2021) Australia [40] |
SMS: personalized support and reminder programs based on text messages | Usual care | 12 months; two a week for the first two months; one per week in the third month; one per month after the fourth month |
All scheduled follow-up appointments | Overall clinic attendance, HbA1c, BMI, total cholesterol, triglycerides, diabetes self-management practices | Y | Y | Y | ||||||
| Made Rini Damayanti (2021) India [45] |
SMS | Usual care | 10 weeks; three times a day |
Diabetes Self-Care Activities Measure | Y | Y | Y | |||||||
| Ran Xu (2020) USA [36] |
Self-reported FBG data were collected by EpxDiabetes automated phone calls or text messages. | Usual care | 6 months; three times a week. |
HbA1c, FBG | Response rate, engagement rate | Y | Y | |||||||
| Ernest L. Carter (2011) USA [26] |
Nurse | Laptop, wireless scale, blood pressure cuff, glucometer: Upload biometric data, make action plans with nurses through video conferencing, and watch related health videos. | Usual care | 9 months; every two weeks. |
HbA1c, BMI, blood pressure, qualitative interview | Y | Y | |||||||
| Charlene C. Quinn (2016) USA [32] |
Doctor | Software application, glucose meter and glucose testing supplies: Upload blood glucose monitoring data, receive health education information, and check health files. | Usual care | 12 months; real time based on feedback |
HbA1c | Y | Y | Y | ||||||
HbA1c: glycated hemoglobin A; FBG: fast blood sugar; 2hPG: 2hr plasma glucose; BMI: body mass index; SBP: systolic pressure; DBP: diastolic pressure; HDL: high-density lipoprotein cholesterol; LDL: low density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides; BUN: blood urea nitrogen; AST: aspartate aminotransferases; ALT: alanine transaminase; Scr: serum creatinine; r-GT: gamma-glutamyltransferase; app: application; SMS: short message service; SMBG: self-monitoring of blood glucose.
Table 2.
Characteristics of telemedicine intervention.
| Author (Year) |
Diabetes Management | Diet | Exercise | Diabetes Complications (Eye, Foot) | Diabetes Symptoms (Hypoglycemia) | Medication Compliance | Other | Diabetes Managemen | Diet | Exercise | Diabetes Complications (Eye, Foot) | Diabetes Symptoms (Hypoglycemia) | Medication Compliance | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | |||||||||||||
| Stephen Agboola (2016) [22] |
Y | Y | Y | Y | Y | |||||||||
| Daniel J. Amante (2021) [39] |
Y | Y | Y | Y | ||||||||||
| Charlene C. Quinn (2011) [50] |
Y | Y | Y | Y | Y | Y | Y | |||||||
| Deborah A. Greenwood (2015) [27] |
Y | Y | Y | Y | Y | Y | ||||||||
| Jing Kang (2021) [44] |
Y | Y | Y | Y | Y | Psychological counselling | Y | Y | Y | |||||
| Maryam Peimani (2016) [42] |
Y | Y | Y | Y | Blood glucose monitoring | Y | ||||||||
| Paul C. Tang (2013) [29] |
Y | Y | Y | Y | Y | Y | ||||||||
| Yanmei Wang (2019) [41] |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Sarah H. Wild (2016) [49] |
Y | Y | Lifestyle change | Y | ||||||||||
| Heather M. Young (2020) [30] |
Y | Y | Y | Self-efficacy | Y | |||||||||
| Daren R. Anderson (2010) [34] |
Y | Y | Y | Y | Y | |||||||||
| Rade Iljaž (2017) [46] |
Y | Y | Y | Y | ||||||||||
| RamachandranVinitha (2019) [43] |
Y | Y | Y | Y | Y | Y | Y | |||||||
| Payal Agarwal (2019) [33] |
Y | Y | Y | Y | Y | Y | ||||||||
| Gretchen A. Benson (2019) [38] |
Y | Y | Y | |||||||||||
| Maria Magdalena Bujnowska-Fedak (2011) [37] |
Y | Y | Y | Y | ||||||||||
| Claudio Dario (2017) [23] |
Blood glucose monitoring | |||||||||||||
| Addie L. Fortmann (2017) [47] |
Y | Y | Y | Y | ||||||||||
| Yakun Feng (2016) [52] |
Y | Y | Y | Y | Y | Lifestyle and weight control | Y | |||||||
| Elizabeth G. Eakin (2014) [35] |
Y | Y | Y | Weight loss | Y | |||||||||
| Leonard E. Egede (2021) [25] |
Y | Y | Y | |||||||||||
| Roslyn A. Stone (2010) [53] | Y | Y | Y | |||||||||||
| María I. Rodríguez-Idígoras (2009) [24] |
Y | Blood glucose monitoring | Y | |||||||||||
| Heidi Holmen, MSc (2014) [31] |
Y | Y | Y | Y | ||||||||||
| I Odnoletkova (2016) [28] |
Y | Y | Y | Y | Y | Y | Y | Y | ||||||
| Samuel N. Forjuoh (2014) [51] |
Y | Y | Y | Y | Y | |||||||||
| Timothy Middleton (2021) [40] |
Y | Y | Y | Y | Y | |||||||||
| A. Farmer (2021) [48] |
Y | Y | Y | |||||||||||
| Made Rini Damayanti (2021) [45] |
Y | Y | Y | Y | Y | |||||||||
| Ran Xu (2020) [36] |
Y | Blood glucose monitoring | Y | |||||||||||
| Ernest L. Carter (2011) [26] | Y | Y | Y | Y | Y | Y | ||||||||
| Charlene C. Quinn (2016) [32] | Y | Y | Y | Y | Y | Y | Y | |||||||
3.2. Literature Quality Evaluation and Risk Bias
Through the CASP inventory [20], the methodological quality of the included articles was assessed, and the results are presented in Table 3. Most of the studies were rated as moderate quality. Due to the specificity of the intervention, the vast majority of studies were not blinded to interventionists or the subjects.
Table 3.
Critical Appraisal Skills Program (CASP) checklist on the included studies.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stephen Agboola et al. (2016) [22] | Y | Y | Y | Y | Y | L | Y | Y | ? | Y | ? |
| Daniel J. Amante et al. (2021) [39] | Y | Y | Y | Y | Y | L | Y | Y | N | Y | Y |
| Charlene C. Quinn et al. (2011) [50] | Y | Y | Y | ? | Y | S | Y | Y | N | Y | Y |
| Daren R. Anderson et al. (2010) [34] | Y | Y | Y | N | Y | S | Y | Y | N | Y | Y |
| Rade Iljaž et al. (2017) [46] | Y | Y | Y | ? | Y | S | Y | Y | N | Y | Y |
| RamachandranVinitha et al. (2019) [43] | Y | Y | ? | Y | Y | L | Y | Y | N | Y | Y |
| Samuel N. Forjuoh et al. (2014) [51] | Y | ? | Y | N | Y | S | Y | Y | N | Y | ? |
| Deborah A. Greenwood et al. (2015) [27] | Y | Y | Y | ? | Y | S | Y | Y | ? | Y | Y |
| Jing Kang et al. (2021) [44] | Y | N | ? | ? | Y | L | Y | Y | ? | Y | Y |
| Maryam Peimani et al. (2016) [42] | Y | Y | Y | N | N | L | Y | Y | ? | Y | Y |
| Paul C. Tang et al. (2013) [29] | Y | N | Y | ? | Y | S | Y | N | ? | Y | Y |
| Payal Agarwal et al. (2019) [33] | Y | Y | Y | ? | Y | S | Y | Y | Y | Y | ? |
| Gretchen A. Benson RDN et al. (2019) [38] | Y | Y | Y | ? | Y | N | Y | Y | ? | Y | Y |
| Maria Magdalena Bujnowska-Fedak et al. (2011) [37] | Y | N | ? | N | Y | S | Y | N | ? | Y | Y |
| Claudio Dario et al. (2017) [23] | Y | Y | Y | N | Y | S | Y | Y | ? | Y | Y |
| Addie L. Fortmann et al. (2017) [47] | Y | Y | ? | ? | Y | S | Y | N | ? | Y | Y |
| Heidi Holmen, MSc et al. (2014) [31] | Y | Y | Y | ? | Y | S | Y | Y | N | Y | ? |
| Yanmei Wang et al. (2019) [41] | Y | Y | Y | ? | Y | S | Y | N | ? | Y | Y |
| Sarah H. Wild et al. (2016) [49] | Y | Y | Y | Y | Y | S | Y | N | N | Y | Y |
| I Odnoletkova et al. (2016) [28] | Y | Y | Y | ? | Y | S | Y | Y | Y | Y | Y |
| Heather M. Young et al. (2020) [30] | Y | Y | Y | ? | Y | S | Y | N | ? | Y | Y |
| Elizabeth G. Eakin et al. (2014) [35] | Y | Y | ? | N | Y | S | Y | Y | N | Y | ? |
| Roslyn A. Stone et al. (2010) [53] | Y | Y | Y | ? | Y | L | Y | Y | N | Y | Y |
| Yakun Feng et al. (2016) [52] | Y | ? | Y | N | ? | S | Y | N | N | Y | Y |
| Leonard E. Egede et al. (2021) [25] | Y | Y | Y | ? | Y | S | Y | Y | ? | Y | Y |
| María I. Rodríguez-Idígoras et al. (2009) [24] | Y | Y | Y | ? | Y | N | Y | Y | N | Y | Y |
| A. Farmer et al. (2021) [48] | Y | Y | Y | Y | Y | L | Y | Y | Y | Y | Y |
| Timothy Middleton et al. (2021) [40] | Y | Y | Y | ? | Y | L | Y | Y | ? | Y | Y |
| Made Rini Damayanti et al. (2021) [45] | Y | Y | Y | N | Y | S | N | Y | Y | Y | Y |
| Ran Xu et al. (2020) [36] | Y | Y | Y | N | Y | S | Y | Y | ? | Y | Y |
| Ernest L. Carter et al. (2011) [26] | Y | Y | Y | ? | Y | L | Y | Y | N | Y | Y |
| Charlene C. Quinn et al. (2016) [32] | Y | Y | ? | N | Y | S | Y | N | ? | Y | Y |
?: Cannot tell; L: large; N: no; S: small; Y: yes.
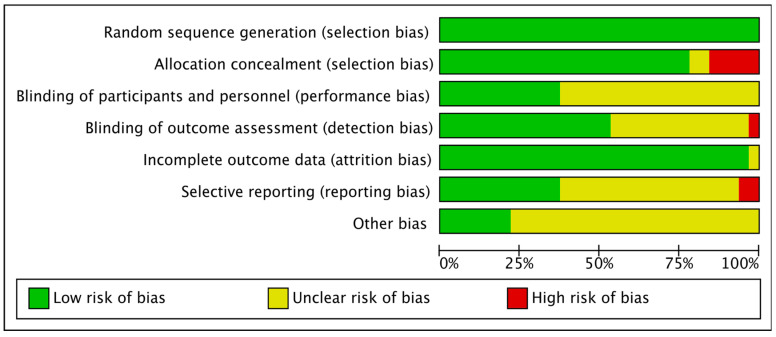
All studies had clear reporting of sequence generation and were therefore considered to be low risk. Because there was no apparent allocation concealment, five [29,37,44,51,52] studies were rated as high risk. Twenty [23,24,25,27,28,29,31,33,34,35,36,37,44,45,46,47,50,51,52,53] studies were also rated as unclear bias because they were not blinded to interventionists or subjects. One [42] study was rated as high risk because it was not blinded to the outcome evaluator. Two [26,32] studies were rated as high bias risk because of incomplete outcome data. Figure 2 and Figure 3 show the results of the risk bias.
Figure 2.
Overall summary of risk of bias in the included studies.
Figure 3.
Risk of bias in the included studies. +: Low risk of bias; -: High risk of bias; ?: Unclear risk of bias.
3.3. Results of the Meta-Analysis
3.3.1. Primary Results (Effect on HbA1c)
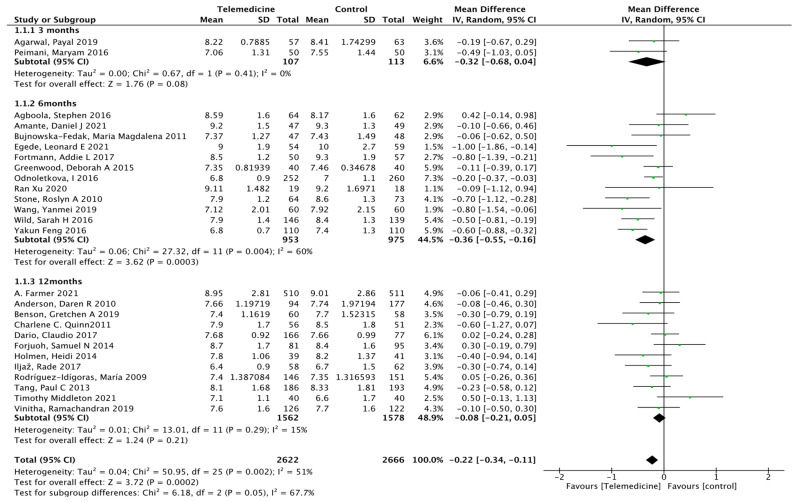
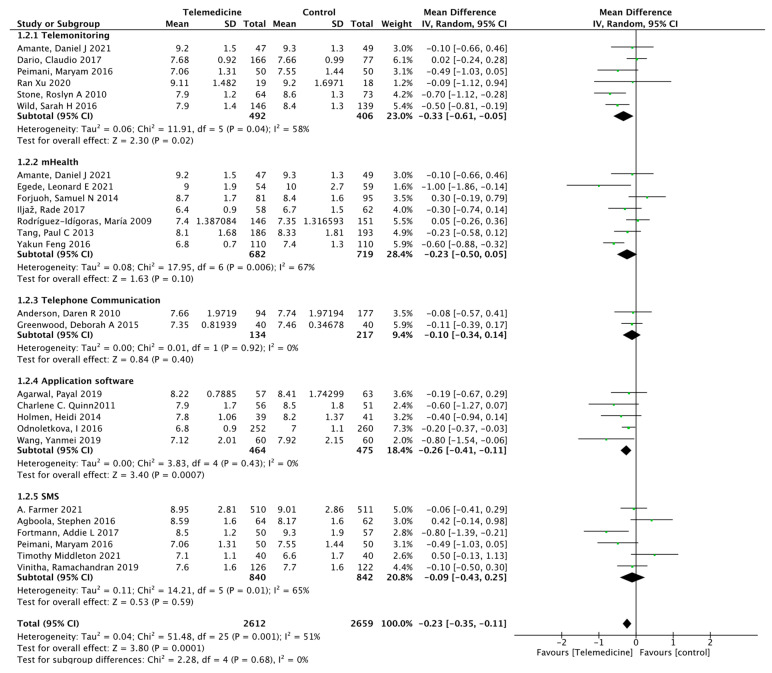
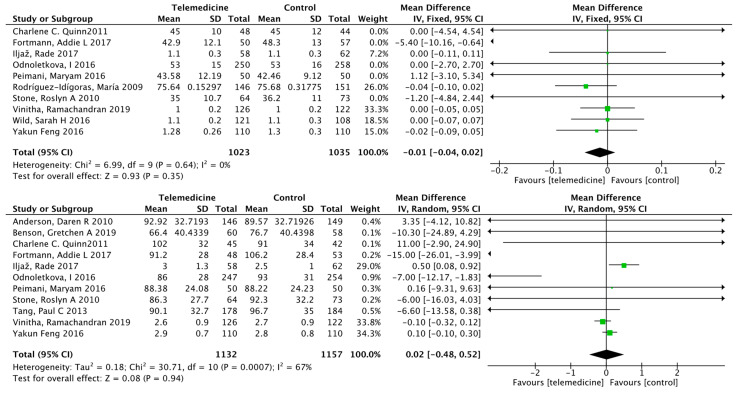
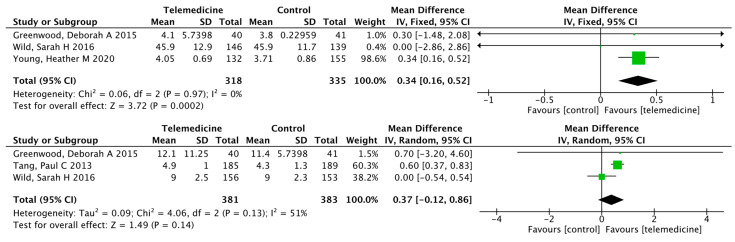
Twenty-six studies [22,23,24,25,27,28,29,31,33,34,36,37,38,39,40,41,42,43,46,47,48,49,50,51,52,53] reported HbA1c outcomes at different intervention times. There were 2622 cases in the intervention group and 2666 cases in the control group. The results showed a statistically significant reduction in glycated hemoglobin levels in the intervention group compared to that in the control group (MD: −0.22, 95% CI [−0.34, −0.11], p < 0.0001; I2 = 51%, Figure 4). According to the time of intervention, subgroup analysis showed that in the mid-term intervention [22,25,27,28,36,37,39,41,47,49,52,53] (6–11 months) (MD: −0.36, 95% CI [−0.55, −0.16], p = 0.0003; I2 = 60%), glycated hemoglobin was reduced in the intervention group, but in the short-term intervention [33,42] (3–5 months), glycated hemoglobin did not change significantly (MD: −0.32, 95% CI [−0.68, 0.04], p = 0.08; I2 = 0%), and it may be diluted in the long-term intervention [23,24,29,31,34,38,40,43,46,48,50,51] (more than 12 months) (MD: −0.08, 95% CI [−0.21, 0.05], p = 0.21; I2 = 15%), as the results also did not change significantly. According to the means of intervention, subgroup analysis showed that in telemonitoring intervention [23,36,39,42,49,53] (MD: −0.33, 95% CI [−0.61, −0.05], p = 0.02; I2 = 58%, Figure 5) and application software [28,31,33,50] (MD: −0.26, 95% CI [−0.41, −0.11], p = 0.0007; I2 = 0%,), glycated hemoglobin was reduced in the intervention group, with statistically significant difference. However, in the three intervention methods of m-Health [24,25,29,39,46,51,52] (MD: −0.23, 95% CI [−0.50, 0.05], p = 0.10; I2 = 67%), telephone communication [27,34] (MD: −0.10, 95% CI [−0.34, 0.14], p = 0.40; I2 = 0%), and SMS [22,40,42,43,47,48] (MD: −0.09, 95% CI [−0.43, 0.25], p = 0.59; I2 = 65%), the results showed that these three intervention methods were superior to conventional nursing, but they are not significant. Both p = 0.637 obtained from Begg’s rank correlation test and p = 0.213 from Egger’s linear regression method suggested no significant publication bias. The funnel plot is shown in Figure S1.
Figure 4.
Subgroup analysis showed higher HbA1c reduction at 6 months of intervention.
Figure 5.
Subgroup analysis showed higher HbA1c reductions in patients with remote monitoring and application interventions.
3.3.2. Secondary Results
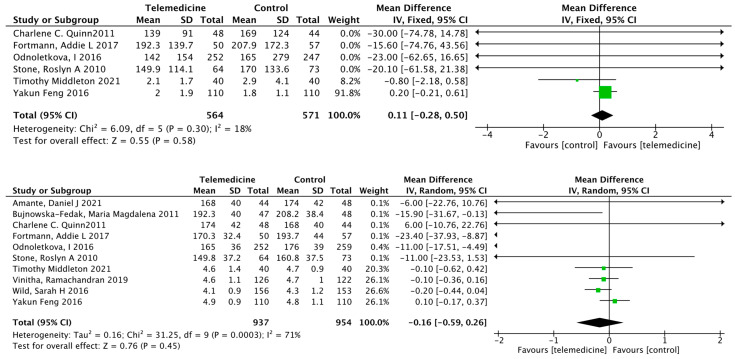
Impact on Fasting Blood Glucose
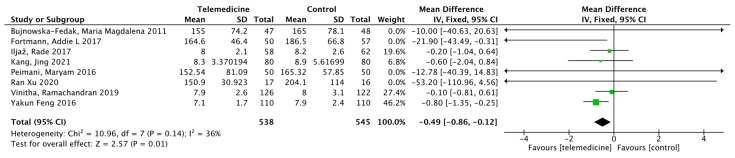
Eight studies [36,37,42,43,44,46,47,52] reported the results of fasting blood glucose (FBG). There were 538 cases in the intervention group and 545 cases in the control group, and the duration of intervention ranged from 3 to 24 months. Meta-analysis showed a statistically significant reduction in FBG levels in the intervention group compared to that in the control group (MD: −0.49, 95% CI [−0.86, −0.12], p = 0.01; I2 = 36%, Figure 6).
Figure 6.
Mean difference in the changes in FBG levels for telemedicine and usual care interventions.
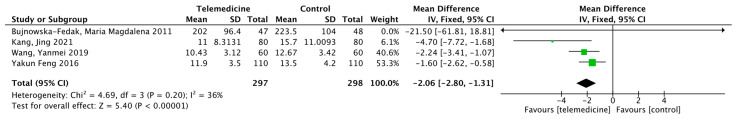
Effects on Postprandial Blood Glucose
Four studies [37,41,44,52] reported the results of post-prandial blood glucose (PBG). There were 297 cases in the intervention group and 298 in the control group, and the duration of the intervention ranged from 3 to 6 months. Meta-analysis showed a statistically significant difference in reduced PBG levels in the intervention group compared to that in the control group (MD: −2.06, 95% CI [−2.80, −1.31], p < 0.00001; I2 = 36%, Figure 7).
Figure 7.
Mean difference in the changes in PBG levels for telemedicine and usual care interventions.
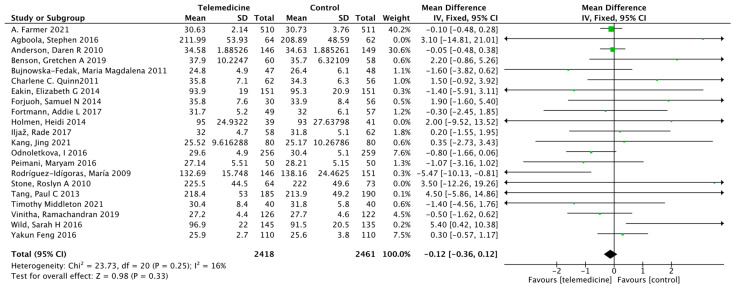
Effect on Body Weight
Nineteen studies [22,24,28,29,31,34,35,37,38,40,43,44,46,47,48,49,50,52,53] reported the results of body weight. The duration of intervention ranged from 3 to 24 months in 2418 cases in the intervention group and 2461 cases in the control group. Meta-analysis showed no significant difference in body weight between the intervention and control groups (MD: −0.12, 95% CI [−0.36, 0.12], p = 0.33; I2 = 16%, Figure 8). Begg’s rank correlation test yielded p = 0.319 and Egger’s linear regression method yielded p = 0.506, both suggesting no significant publication bias. The funnel plot is shown in Figure S2.
Figure 8.
Mean difference in the changes in weight levels for telemedicine and usual care interventions.
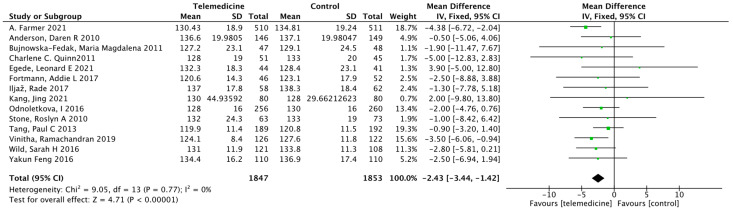
Effect on Systolic Blood Pressure
Thirteen studies [25,28,29,34,43,44,47,48,49,50,53] reported the results of systolic blood pressure. There were 1847 cases in the intervention group and 1853 cases in the control group, and the duration of the intervention ranged from 3 to 24 months. Meta-analysis showed that systolic blood pressure improved in the intervention group compared to that in the control group, with a statistically significant difference (MD: −2.43, 95% CI [−3.44, −1.42], p < 0.00001; I2 = 0%, Figure 9). Begg’s rank correlation test yielded p = 0.155 and Egger’s linear regression method yielded p = 0.191, both suggesting no significant publication bias. The funnel plot is shown in Figure S3.
Figure 9.
Mean difference in the changes in SBP levels for telemedicine and usual care interventions.
Effects on High-Density Lipoprotein, Low-Density Lipoprotein, Triglycerides, and Total Cholesterol
Ten studies [24,28,42,43,46,47,49,50,52,53] reported high-density lipoprotein (HDL) results, 11 studies [24,28,29,34,42,43,46,47,50,53] reported low-density lipoprotein (LDL) results, 6 studies [28,40,47,50,52] reported triglyceride (TG) results, and 10 studies [28,29,34,38,42,43,46,47,50,52,53] reported total cholesterol (TC) results. All four results were not significantly different (Figure 10). For HDL, Begg’s rank correlation test yielded p = 0.371 and Egger’s linear regression method yielded p = 0.238. For LDL, Begg’s rank correlation test yielded p = 1.000 and Egger’s linear regression method yielded p = 0.266. The above suggested no significant publication bias. The funnel plots are shown in Figures S4 and S5.
Figure 10.
Mean difference in the changes in HDL, LDL, TG, and TC levels for telemedicine and usual care interventions.
Effects on Self-Efficacy, Diabetes Knowledge, Physical Health, and Mental Health
There were three separate outcomes reporting self-efficacy, diabetes knowledge, physical health, and mental health, in which only self-efficacy improved in the intervention group compared to the control group (MD: 0.34, 95% CI [0.16, 0.52], p = 0.0002; I2 = 0%; Figure 11).
Figure 11.
Mean difference in the changes in self-efficacy, diabetes knowledge, physical health, and mental health levels for telemedicine and usual care interventions.
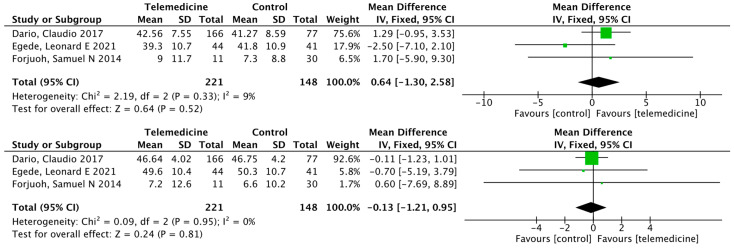
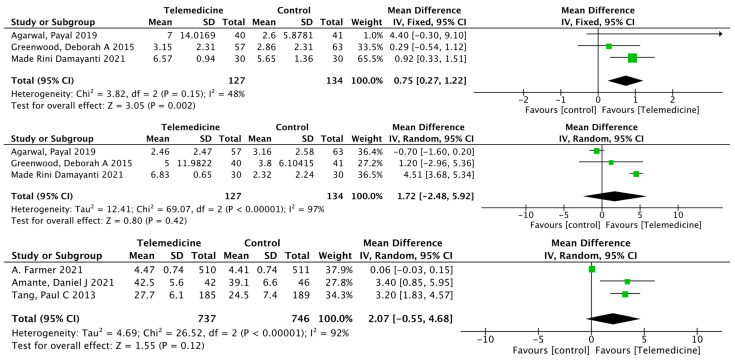
Effects on Exercise, Foot Care, and Satisfaction
There were three separate outcomes reporting exercise, foot care, and satisfaction, in which only exercise improved in the intervention group compared to the control group (MD: 0.75, 95% CI [0.27, 1.22], p = 0.002; I2 = 48%; Figure 12).
Figure 12.
Mean difference in the changes in exercise, foot care, and satisfaction levels for telemedicine and usual care interventions.
4. Discussion
This study confirms the effectiveness of various telemedicine interventions applied in primary health care. Meta-analysis showed that despite high heterogeneity, telemedicine interventions can improve patients’ metabolic control more than conventional controls over 6 months, as is supported in other meta-analyses [54,55,56]. However, we did not find any significant effect on lipid metabolism such as body weight, HDL, TG, or TC, which is different from the results of several previous studies [55,57,58]. This may be because, on the one hand, most of the study interventions focused on the improvement of patients’ blood glucose, and fewer studies provided a full range of interventions on patients’ diet, exercise, and diabetes knowledge. One the other hand, lipid control in diabetic patients is mainly dependent on the use of drugs [59], so there is no difference between the two.
4.1. Blood Sugar Control
The results of the study showed that the telemedicine intervention resulted in a significant decrease in clinical glycated hemoglobin levels, with a mean decrease of 0.1% to 0.32%. HbA1c concentrations effectively reflected the patients’ average blood glucose levels over the previous 8–12 weeks. Thus, the reduction in HbA1c concentrations reflects the positive impact of telemedicine on the long-term care of patients with T2DM. In the subgroup analysis regarding duration, the intervention group showed lower HbA1c than the conventional group only when the intervention duration was 6 months. In contrast, there was no significant improvement in glycosylated hemoglobin at short-term (3 months) or long-term (12 months) intervention times. This may be because T2DM is a slow-treating chronic disease and the HbA1c level reflects the average blood glucose over 2–3 months [60]. Therefore, there was no significant improvement in glycated hemoglobin for the short-term intervention, which is consistent with other studies [61,62]. In addition, the small number of studies of short-term interventions included in the articles of this study may be somewhat biased, and hence, more and higher quality studies may be needed for further evaluation. The decline in benefit at 12 months of intervention may be related to the patient’s response to the intervention, which is consistent with the results of other studies [63,64]. Therefore, in studies of long-term interventions, patient engagement declines with the duration of the intervention, and continuous monitoring and individualized reminders are important to maintain the continuity of the intervention.
4.2. Self-Management
Good self-management can significantly reduce the occurrence and progression of T2DM complications [65]. In this study, we evaluated the patients’ self-management abilities based on results of FBG and PBG, and the results showed that the blood glucose level was reduced in the intervention group compared to the control group, as is supported in other meta-analyses [66]. Moreover, significant improvements in self-efficacy occurred in the intervention group. Ten of these studies [22,29,30,33,35,38,39,40,42,47], combined with theoretical models, improved the self-management ability of patients with T2DM by providing them with knowledge about blood glucose monitoring, diet, and exercise, and by providing them with timely personalized message reminders through the data obtained. However, since the number of each study is limited, it is not possible to determine whether there are interactions between different telemedicine technologies (e.g., text messaging, smartphones). Most research trials reported on glycosylated hemoglobin concentrations, and only a small number of study trials reported on other aspects regarding diabetes management (FBG, postprandial glucose, lipid metabolism, self-management ability, etc.). Therefore, great care should be taken in interpreting the results of other secondary outcomes. The meta-analysis also showed that telemedicine strategies were associated with other clinical benefits of glycemic control and that telemedicine measures contributed to improved self-management abilities, including systolic blood pressure and diabetes self-efficacy, in patients with T2DM.
4.3. Telemedicine
In the study by Natalie Robson et al. [67], phone-based telehealth interventions had the greatest impact on the self-management of people with type 2 diabetes. In the study of Puikwan A. Lee et al. [68], although the results of meta-analysis showed that telemedicine intervention was better than usual care, it was impossible to judge which intervention method would benefit patients the most. The results of this study showed that telemedicine intervention was superior to conventional care. In the subgroup analysis of different intervention methods, only remote monitoring and application software intervention significantly improved HbA1c in the intervention group, whereas there were no significant differences in mobile medicine, telephone communication, or SMS remote intervention. Interventions delivered through remote monitoring had the greatest impact on type 2 diabetes-related outcomes, followed by app interventions, M-Health, telephone counseling, and SMS interventions. At the same time, there was significant heterogeneity among individual studies, which may have been caused by the different methods and applications of telemedicine intervention. Therefore, it is difficult to determine which interventions are most effective in managing type 2 diabetes. A total of five [22,29,33,39,48] studies assessed patient engagement or perception of telemedicine in this review. Although these studies reported widespread patient acceptance of telemedicine interventions, only three studies formally tested subjects’ satisfaction. Meta-analysis results showed that although the satisfaction of the intervention group was better than that of the control group, the difference was not statistically significant. At the same time, high-frequency and short-term interventions [25,41,47,53] can significantly improve the hemoglobin of patients. However, the effectiveness of the intervention decreases with the duration of the intervention, so the next step that should be considered is how to maintain a high level of patient compliance during prolonged intervention. Only one study [48] reported the costs associated with the intervention and no cost-benefit analysis was performed, making it impossible to draw firm conclusions about the cost-effectiveness of telemedicine interventions in type 2 diabetes.
In response to the ongoing COVID-19 pandemic, telemedicine has seen incremental growth [69], with one study [44] reporting improved patient glycemic control during the COVID-19 pandemic with telemedicine-based patient interventions using an app. We believe this number is too small to draw firm conclusions about telemedicine in diabetes care in the context of COVID-19. Although telemedicine can provide benefits to patients, many problems remain in its future development. For example, the professional and ethical challenges posed by telemedicine may affect both patients and physicians [70]. Patients’ trust in telemedicine interventions may be reduced due to untimely phone calls or incorrect text messages. Moreover, patient compliance decreased with the prolongation of intervention time. In addition, in most countries the cost of telehealth interventions is borne by the patient, which can lead to low patient acceptance. Therefore, future research should explore a convenient and timely telemedicine system, improve the quality of intervention, and increase patient acceptance through the training of intervention teams, as well as maintain a certain frequency of intervention to increase patient compliance, ensure government funding to reduce telemedicine costs, and accelerate telemedicine adoption.
5. Limitations and Strengths
First, the study found high heterogeneity in some outcomes, and the high heterogeneity may have been due to differences in telemedicine interventions, subjects, the timing of interventions, interventionists, and intervention frequency. Second, because we found a small number of studies reporting diabetes self-management ability, the findings are inconclusive regarding the effectiveness of self-management and require large sample testing and further investigation. Third, there are fewer studies with long-term follow-up, and the findings may contain only short-term effects of improving T2DM and lack evaluation of long-term effects (development of complications, mortality, etc.). In addition, the cost-effectiveness of the intervention becomes uncertain as the duration of the intervention increases. Fourth, the nature of the intervention led to the fact that most of the studies were not blinded to the interventionists or subjects. Fifth, the inclusion of studies from different countries resulted in significant differences in baseline primary health care systems. For example, government-funded telemedicine services are common in primary health care in the United States and Europe [71], but in some developing countries, especially South Africa, even basic services are not available due to low government budgets [72]. This may affect the compliance of patients. Sixth, because the term “telemedicine” is very nonspecific, conclusions may not be generalizable. Finally, we identified slight missing corners in some of the funnel plots, which may have been caused by the presence of small sample sizes and low-quality studies in our included studies. However, the Egger and Begg tests revealed that there was no significant publication bias in the included studies, and sensitivity analyses did not show any significant change in the effect values of the study results. Therefore, this does not affect our conclusions.
This meta-analysis has multiple strengths. First, we assessed the quality of evidence for all included articles using the CASP [20] method. Second, we did not restrict the search language, so articles in all countries and languages were eligible for this study. Third, we strictly followed the recommendations of the meta-analysis evaluation method [73,74,75]. Fourth, we had no time limit on previous published articles, so no earlier published articles were missed.
The meta-analysis of this study supports that telemedicine interventions can be effective in improving glycemic control in patients with T2DM in primary health care. This information is critical for decision-makers to develop interventions based on desired outcomes and to maximize the use of resources in the primary health care setting.
6. Conclusions
The results of this study suggest that compared with non-telemedicine care, telemedicine intervention in primary health care may improve glycemic control and self-management in patients with type 2 diabetes. In particular, the six-month intervention period was most effective, and interventions with remote monitoring or apps were most effective. Therefore, telemedicine interventions are an effective supplement to traditional face-to-face counseling in primary health care settings, and telemedicine can provide convenience for homebound patients with T2DM who do not have timely access to medical resources. The next step should focus on assessing the acceptability and feasibility of telemedicine implementation on a large scale and whether it is effective in reducing healthcare costs.
Acknowledgments
The authors would like to thank the School of Nursing of Yangzhou University, the Yangzhou Commission of Health, and the Affiliated Hospital of Yangzhou University.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19074173/s1, Figure S1: Funnel plot evaluating publication bias with regard to HbA1c change for all studies; Figure S2: Funnel plot evaluating publication bias with regard to wieght change for all studies; Figure S3. Funnel plot evaluating publication bias with regard to SBP change for all studies; Figure S4. Funnel plot evaluating publication bias with regard to HDL change for all studies; Figure S5. Funnel plot evaluating publication bias with regard to LDL change for all studies
Appendix A. Search Strategies
(((((((Mobile Health) OR (Health, Mobile)) OR (mHealth)) OR (Telehealth)) OR (eHealth)) OR (“Telemedicine”[Mesh])) AND ((((“Primary Health Care”[Mesh]) OR ((((((Care, Primary Health) OR (Health Care, Primary)) OR (Primary Healthcare)) OR (Healthcare, Primary)) OR (Primary Care)) OR (Care, Primary))) OR (“Community Health Services”[Mesh])) OR ((((((((((((Health Services, Community) OR (Community Health Service)) OR (Health Service, Community)) OR (Service, Community Health)) OR (Services, Community Health)) OR (Community Health Care)) OR (Care, Community Health)) OR (Health Care, Community)) OR (Community Healthcare)) OR (Community Healthcares)) OR (Healthcare, Community)) OR (Healthcares, Community)))) AND ((“Diabetes Mellitus, Type 2”[Mesh]) OR (((((((((((((((((((((((((((((((Diabetes Mellitus, Noninsulin-Dependent) OR (Diabetes Mellitus, Ketosis-Resistant)) OR (Diabetes Mellitus, Ketosis Resistant)) OR (Ketosis-Resistant Diabetes Mellitus)) OR (Diabetes Mellitus, Non Insulin Dependent)) OR (Diabetes Mellitus, Non-Insulin-Dependent)) OR (Non-Insulin-Dependent Diabetes Mellitus)) OR (Diabetes Mellitus, Stable)) OR (Stable Diabetes Mellitus)) OR (Diabetes Mellitus, Type II)) OR (NIDDM)) OR (Diabetes Mellitus, Noninsulin Dependent)) OR (Diabetes Mellitus, Maturity-Onset)) OR (Diabetes Mellitus, Maturity Onset)) OR (Maturity-Onset Diabetes Mellitus)) OR (Maturity Onset Diabetes Mellitus)) OR (MODY)) OR (Diabetes Mellitus, Slow-Onset)) OR (Diabetes Mellitus, Slow Onset)) OR (Slow-Onset Diabetes Mellitus)) OR (Type 2 Diabetes Mellitus)) OR (Noninsulin-Dependent Diabetes Mellitus)) OR (Noninsulin Dependent Diabetes Mellitus)) OR (Maturity-Onset Diabetes)) OR (Diabetes, Maturity-Onset)) OR (Maturity Onset Diabetes)) OR (Type 2 Diabetes)) OR (Diabetes, Type 2)) OR (Diabetes Mellitus, Adult-Onset)) OR (Adult-Onset Diabetes Mellitus)) OR (Diabetes Mellitus, Adult Onset))).
Author Contributions
A.Z. and J.W. contributed to study concept and design; A.Z. and X.W. contributed to the data extraction; A.Z., S.Z. and Z.Z. screened the articles; A.Z. and J.W. discussed the themes of the review and contributed to the analysis and interpretation of the data; A.Z. contributed to the drafting of the manuscript; J.W., Z.G. and X.W. contributed to the critical revision of the manuscript for important intellectual content; C.W. contributed to the language editing. All authors have read and agreed to the published version of the manuscript.
Funding
Cadre Health Care Research Project of Jiangsu (BJ17011).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
All authors declare that there is no potential conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sun H., Saeedi P., Karuranga S., Pinkepank M., Ogurtsova K., Duncan B.B., Stein C., Basit A., Chan J.C.N., Mbanya J.C., et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022;183:109119. doi: 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saeedi P., Petersohn I., Salpea P., Malanda B., Karuranga S., Unwin N., Colagiuri S., Guariguata L., Motala A.A., Ogurtsova K., et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9 edition. Diabetes Res. Clin. Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 3.Hincapié M.A., Gallego J.C., Gempeler A., Piñeros J.A., Nasner D., Escobar M.F. Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J. Prim. Care Community Health. 2020;11:2150132720980612. doi: 10.1177/2150132720980612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sood S., Mbarika V., Jugoo S., Dookhy R., Doarn C.R., Prakash N., Merrell R.C. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. J. e-Health. 2007;13:573–590. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- 5.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for Physicians. Diabetes Metab. Syndr. 2020;14:273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shan R., Sarkar S., Martin S.S. Digital health technology and mobile devices for the management of diabetes mellitus: State of the art. Diabetologia. 2019;62:877–887. doi: 10.1007/s00125-019-4864-7. [DOI] [PubMed] [Google Scholar]
- 7.Ellahham S. Artificial Intelligence: The Future for Diabetes Care. Am. J. Med. 2020;133:895–900. doi: 10.1016/j.amjmed.2020.03.033. [DOI] [PubMed] [Google Scholar]
- 8.Seidu S., Cos X., Brunton S., Harris S.B., Jansson S.P.O., Mata-Cases M., Neijens A.M.J., Topsever P., Khunti K. A disease state approach to the pharmacological management of Type 2 diabetes in primary care: A position statement by Primary Care Diabetes Europe. Prim. Care Diabetes. 2021;15:31–51. doi: 10.1016/j.pcd.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Caro-Bautista J., Kaknani-Uttumchandani S., Garcia-Mayor S., Villa-Estrada F., Morilla-Herrera J.C., Leon-Campos A., Gomez-Gonzalez A.J., Morales-Asencio J.M. Impact of self-care programmes in type 2 diabetes mellitus population in primary health care: Systematic review and meta-analysis. J. Clin. Nurs. 2020;29:1457–1476. doi: 10.1111/jocn.15186. [DOI] [PubMed] [Google Scholar]
- 10.The King’s Fund The NHS Long-Term Plan Explained [EB/OL]. 23 January 2019. [(accessed on 1 February 2022)]. Available online: https://www.kingsfund.org.uk/publications/nhs-long-term-plan-explained?utm_source=TheKing%27sFundnewsletters%28mainaccount%29&utm_medium=email&utm_campaign=10222788_MKPUB_NHSlong-termplanlongread24012019&utm_content=btnbel.
- 11.Strive to Write a Healthy Chapter in Building a Socialist Modern Country in an All-Round Way [EB/OL]. 28 June 2021. [(accessed on 1 February 2022)]; Available online: http://www.nhc.gov.cn/wjw/mtbd/202106/3950e847c71f4d0c88bac4cc5b21ab8a.shtml.
- 12.So C.F., Chung J.W. Telehealth for diabetes self-management in primary healthcare: A systematic review and meta-analysis. J. Telemed. Telecare. 2018;24:356–364. doi: 10.1177/1357633X17700552. [DOI] [PubMed] [Google Scholar]
- 13.Salehi S., Olyaeemanesh A., Mobinizadeh M., Nasli-Esfahani E., Riazi H. Assessment of remote patient monitoring (RPM) systems for patients with type 2 diabetes: A systematic review and meta-analysis. J. Diabetes Metab. Disord. 2020;19:115–127. doi: 10.1007/s40200-019-00482-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang J., Yang H., Wang Z., Wang X., Wang Y., Yu X., Liu L. Self-management among type 2 diabetes patients via the WeChat application: A systematic review and meta-analysis. J. Clin. Pharm. Ther. 2021;46:4–16. doi: 10.1111/jcpt.13264. [DOI] [PubMed] [Google Scholar]
- 15.Lee S.W.H., Chan C.K.Y., Chua S.S., Chaiyakunapruk N. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: A systematic review and network meta-analysis. Sci. Rep. 2017;7:12680. doi: 10.1038/s41598-017-12987-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Udsen F.W., Hangaard S., Bender C., Andersen J., Kronborg T., Vestergaard P., Hejlesen O., Laursen S. The Effectiveness of Telemedicine Solutions in Type 1 Diabetes Management: A Systematic Review and Meta-analysis. J. Diabetes Sci. Technol. 2022:19322968221076874. doi: 10.1177/19322968221076874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hangaard S., Laursen S.H., Andersen J.D., Kronborg T., Vestergaard P., Hejlesen O., Udsen F.W. The Effectiveness of Telemedicine Solutions for the Management of Type 2 Diabetes: A Systematic Review, Meta-Analysis, and Meta-Regression. J. Diabetes Sci. Technol. 2021:19322968211064633. doi: 10.1177/19322968211064633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart L.A., Clarke M., Rovers M., Riley R.D., Simmonds M., Stewart G., Tierney J.F. Preferred Reporting Items for Systematic Review and Meta-Analyses of individual participant data: The PRISMA-IPD Statement. JAMA. 2015;313:1657–1665. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 19.American Telemedicine Association (ATA) Telehealth: Defining 21st Century Care. Telehealth Basics—ATA. 2019. 19 January 2021. [(accessed on 2 February 2022)]. Available online: https://www.americantelemed.org/resource/why-telemedicine/
- 20.Critical Appraisal Skills Program (CASP) CASP Checklists from Oxford. [(accessed on 20 September 2021)]. Available online: https://casp-uk.net/casp-tools-checklists/
- 21.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.-Y., Corbett M.S., Eldridge S.M., et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 22.Agboola S., Jethwani K., Lopez L., Searl M., O’Keefe S., Kvedar J. Text to Move: A Randomized Controlled Trial of a Text-Messaging Program to Improve Physical Activity Behaviors in Patients With Type 2 Diabetes Mellitus. J. Med. Internet Res. 2016;18:e307. doi: 10.2196/jmir.6439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dario C., Toffanin R., Calcaterra F., Saccavini C., Stafylas P., Mancin S., Vio E. Telemonitoring of Type 2 Diabetes Mellitus in Italy. Telemed. J. e-Health. 2017;23:143–152. doi: 10.1089/tmj.2015.0224. [DOI] [PubMed] [Google Scholar]
- 24.Rodríguez-Idígoras M.I., Sepúlveda-Muñoz J., Sánchez-Garrido-Escudero R., Martínez-González J.L., Escolar-Castelló J.L., Paniagua-Gómez I.M., Bernal-López R., Fuentes-Simón M.V., Garófano-Serrano D. Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol. Ther. 2009;11:431–437. doi: 10.1089/dia.2008.0114. [DOI] [PubMed] [Google Scholar]
- 25.Egede L.E., Dawson A.Z., Walker R.J., Garraci E., Knapp R.G. Randomized controlled trial of technology-assisted case management in low-income adults with type 2 diabetes: Effect on quality of life and blood pressure. J. Telemed. Telecare. 2021:1357633X211028491. doi: 10.1177/1357633X211028491. [DOI] [PubMed] [Google Scholar]
- 26.Carter E.L., Nunlee-Bland G., Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect. Health Inf. Manag. 2011;8:1b. [PMC free article] [PubMed] [Google Scholar]
- 27.Greenwood D.A., Blozis S.A., Young H.M., Nesbitt T.S., Quinn C.C. Overcoming Clinical Inertia: A Randomized Clinical Trial of a Telehealth Remote Monitoring Intervention Using Paired Glucose Testing in Adults With Type 2 Diabetes. J. Med. Internet Res. 2015;17:e178. doi: 10.2196/jmir.4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Odnoletkova I., Goderis G., Nobels F., Fieuws S., Aertgeerts B., Annemans L., Ramaekers D. Optimizing diabetes control in people with Type 2 diabetes through nurse-led telecoaching. Diabet. Med. 2016;33:777–785. doi: 10.1111/dme.13092. [DOI] [PubMed] [Google Scholar]
- 29.Tang P.C., Overhage J.M., Chan A.S., Brown N.L., Aghighi B., Entwistle M.P., Hui S.L., Hyde S.M., Klieman L.H., Mitchell C.J., et al. Online disease management of diabetes: Engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J. Am. Med. Inform. Assoc. 2013;20:526–534. doi: 10.1136/amiajnl-2012-001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young H.M., Miyamoto S., Dharmar M., Tang-Feldman Y. Nurse Coaching and Mobile Health Compared With Usual Care to Improve Diabetes Self-Efficacy for Persons With Type 2 Diabetes: Randomized Controlled Trial. JMIR mHealth uHealth. 2020;8:e16665. doi: 10.2196/16665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holmen H., Torbjørnsen A., Wahl A.K., Jenum A.K., Småstuen M.C., Arsand E., Ribu L. A Mobile Health Intervention for Self-Management and Lifestyle Change for Persons With Type 2 Diabetes, Part 2: One-Year Results From the Norwegian Randomized Controlled Trial RENEWING HEALTH. JMIR mHealth uHealth. 2014;2:e57. doi: 10.2196/mhealth.3882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn C.C., Shardell M.D., Terrin M.L., Barr E.A., Park D., Shaikh F., Guralnik J.M., Gruber-Baldini A.L. Mobile Diabetes Intervention for Glycemic Control in 45-to 64-Year-Old Persons With Type 2 Diabetes. J. Appl. Gerontol. 2016;35:227–243. doi: 10.1177/0733464814542611. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal P., Mukerji G., Desveaux L., Ivers N.M., Bhattacharyya O., Hensel J.M., Shaw J., Bouck Z., Jamieson T., Onabajo N., et al. Mobile App for Improved Self-Management of Type 2 Diabetes: Multicenter Pragmatic Randomized Controlled Trial. JMIR mHealth uHealth. 2019;7:e10321. doi: 10.2196/10321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson D.R., Christison-Lagay J., Villagra V., Liu H., Dziura J. Managing the space between visits: A randomized trial of disease management for diabetes in a community health center. J. Gen. Intern. Med. 2010;25:1116–1122. doi: 10.1007/s11606-010-1419-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eakin E.G., Winkler E.A., Dunstan D.W., Healy G.N., Owen N., Marshall A.M., Graves N., Reeves M.M. Living well with diabetes: 24-month outcomes from a randomized trial of telephone-delivered weight loss and physical activity intervention to improve glycemic control. Diabetes Care. 2014;37:2177–2185. doi: 10.2337/dc13-2427. [DOI] [PubMed] [Google Scholar]
- 36.Xu R., Xing M., Javaherian K., Peters R., Ross W., Bernal-Mizrachi C. Improving HbA(1c) with Glucose Self-Monitoring in Diabetic Patients with EpxDiabetes, a Phone Call and Text Message-Based Telemedicine Platform: A Randomized Controlled Trial. Telemed. J. e-Health. 2020;26:784–793. doi: 10.1089/tmj.2019.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bujnowska-Fedak M.M., Puchała E., Steciwko A. The impact of telehome care on health status and quality of life among patients with diabetes in a primary care setting in Poland. Telemed. J. e-Health. 2011;17:153–163. doi: 10.1089/tmj.2010.0113. [DOI] [PubMed] [Google Scholar]
- 38.Benson G.A., Sidebottom A., Hayes J., Miedema M.D., Boucher J., Vacquier M., Sillah A., Gamam S., VanWormer J.J. Impact of ENHANCED (diEtitiaNs Helping pAtieNts CarE for Diabetes) Telemedicine Randomized Controlled Trial on Diabetes Optimal Care Outcomes in Patients with Type 2 Diabetes. J. Acad. Nutr. Diet. 2019;119:585–598. doi: 10.1016/j.jand.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 39.Amante D.J., Harlan D.M., Lemon S.C., McManus D.D., Olaitan O.O., Pagoto S.L., Gerber B.S., Thompson M.J. Evaluation of a Diabetes Remote Monitoring Program Facilitated by Connected Glucose Meters for Patients With Poorly Controlled Type 2 Diabetes: Randomized Crossover Trial. JMIR Diabetes. 2021;6:e25574. doi: 10.2196/25574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Middleton T., Constantino M., McGill M., D’Souza M., Twigg S.M., Wu T., Thiagalingam A., Chow C., Wong J. An Enhanced SMS Text Message-Based Support and Reminder Program for Young Adults With Type 2 Diabetes (TEXT2U): Randomized Controlled Trial. J. Med. Internet Res. 2021;23:e27263. doi: 10.2196/27263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y., Li M., Zhao X., Pan X., Lu M., Lu J., Hu Y. Effects of continuous care for patients with type 2 diabetes using mobile health application: A randomised controlled trial. Int. J. Health Plan. Manag. 2019;34:1025–1035. doi: 10.1002/hpm.2872. [DOI] [PubMed] [Google Scholar]
- 42.Peimani M., Rambod C., Omidvar M., Larijani B., Ghodssi-Ghassemabadi R., Tootee A., Esfahani E.N. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: A feasibility study. Prim. Care Diabetes. 2016;10:251–258. doi: 10.1016/j.pcd.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 43.Vinitha R., Nanditha A., Snehalatha C., Satheesh K., Susairaj P., Raghavan A., Ramachandran A. Effectiveness of mobile phone text messaging in improving glycaemic control among persons with newly detected type 2 diabetes. Diabetes Res. Clin. Pract. 2019;158:107919. doi: 10.1016/j.diabres.2019.107919. [DOI] [PubMed] [Google Scholar]
- 44.Kang J., Chen Y., Zhao Y., Zhang C. Effect of remote management on comprehensive management of diabetes mellitus during the COVID-19 epidemic. Prim. Care Diabetes. 2021;15:417–423. doi: 10.1016/j.pcd.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Damayanti M.R., Antari G.A.A., Nopriani N.L.P. Effect of a Ten-Week Short Message Service-Based Intervention on Self-Management of Type-2 Diabetes Patients in Bali, Indonesia. Nurse Media J. Nurs. 2021;11:177–186. doi: 10.14710/nmjn.v11i2.35257. [DOI] [Google Scholar]
- 46.Iljaž R., Brodnik A., Zrimec T., Cukjati I. E-healthcare for Diabetes Mellitus Type 2 Patients—A Randomised Controlled Trial in Slovenia. Zdr. Varst. 2017;56:150–157. doi: 10.1515/sjph-2017-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fortmann A.L., Gallo L.C., Garcia M.I., Taleb M., Euyoque J.A., Clark T., Skidmore J., Ruiz M., Dharkar-Surber S., Schultz J., et al. Dulce Digital: An mHealth SMS-Based Intervention Improves Glycemic Control in Hispanics With Type 2 Diabetes. Diabetes Care. 2017;40:1349–1355. doi: 10.2337/dc17-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farmer A., Bobrow K., Leon N., Williams N., Phiri E., Namadingo H., Cooper S., Prince J., Crampin A., Besada D., et al. Digital messaging to support control for type 2 diabetes (StAR2D): A multicentre randomised controlled trial. BMC Public Health. 2021;21:1907. doi: 10.1186/s12889-021-11874-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wild S.H., Hanley J., Lewis S.C., McKnight J.A., McCloughan L.B., Padfield P.L., Parker R.A., Paterson M., Pinnock H., Sheikh A., et al. Correction: Supported Telemonitoring and Glycemic Control in People with Type 2 Diabetes: The Telescot Diabetes Pragmatic Multicenter Randomized Controlled Trial. PLoS Med. 2016;13:e1002163. doi: 10.1371/journal.pmed.1002163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quinn C.C., Shardell M.D., Terrin M.L., Barr E.A., Ballew S.H., Gruber-Baldini A.L. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934–1942. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Forjuoh S.N., Bolin J.N., Huber J.C., Vuong A.M., Adepoju O.E., Helduser J.W., Begaye D.S., Robertson A., Moudouni D.M., Bonner T.J., et al. Behavioral and technological interventions targeting glycemic control in a racially/ethnically diverse population: A randomized controlled trial. BMC Public Health. 2014;14:71. doi: 10.1186/1471-2458-14-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Feng Y., Liu Y., Gang X., Sun L., Wang G., Sun C. The application of telemedicine in the integrated management of type 2 diabetes mellitus. Chin. J. Diabetes. 2016;24:439–442. [Google Scholar]
- 53.Stone R.A., Rao R.H., Sevick M.A., Cheng C., Hough L.J., Macpherson D.S., Franko C.M., Anglin R.A., Obrosky D.S., Derubertis F.R. Active care management supported by home telemonitoring in veterans with type 2 diabetes: The DiaTel randomized controlled trial. Diabetes Care. 2010;33:478–484. doi: 10.2337/dc09-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eberle C., Stichling S. Clinical Improvements by Telemedicine Interventions Managing Type 1 and Type 2 Diabetes: Systematic Meta-review. J. Med. Internet Res. 2021;23:12. doi: 10.2196/23244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haider R., Sudini L., Chow C.K., Cheung N.W. Mobile phone text messaging in improving glycaemic control for patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2019;150:27–37. doi: 10.1016/j.diabres.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 56.Timpel P., Oswald S., Schwarz P.E.H., Harst L. Mapping the Evidence on the Effectiveness of Telemedicine Interventions in Diabetes, Dyslipidemia, and Hypertension: An Umbrella Review of Systematic Reviews and Meta-Analyses. J. Med. Internet Res. 2020;22:e16791. doi: 10.2196/16791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Michaud T.L., Ern J., Scoggins D., Su D. Assessing the Impact of Telemonitoring-Facilitated Lifestyle Modifications on Diabetes Outcomes: A Systematic Review and Meta-Analysis. Telemed. J. e-Health. 2021;27:124–136. doi: 10.1089/tmj.2019.0319. [DOI] [PubMed] [Google Scholar]
- 58.Wang Y., Min J., Khuri J., Xue H., Xie B., Kaminsky L.A., Cheskin L.J. Effectiveness of Mobile Health Interventions on Diabetes and Obesity Treatment and Management: Systematic Review of Systematic Reviews. JMIR mHealth uHealth. 2020;8:e15400. doi: 10.2196/15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vergès B. Combination lipid therapy in type 2 diabetes mellitus. Expert Opin. Pharm. 2011;12:1393–1403. doi: 10.1517/14656566.2011.558503. [DOI] [PubMed] [Google Scholar]
- 60.American Diabetes Association Glycemic Targets: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44((Suppl. 1)):S73–S84. doi: 10.2337/dc21-S006. [DOI] [PubMed] [Google Scholar]
- 61.Hu Y., Wen X., Wang F., Yang D., Liu S., Li P., Xu J. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: A systematic review and meta-analysis of randomised controlled trials. J. Telemed. Telecare. 2019;25:402–413. doi: 10.1177/1357633X18776823. [DOI] [PubMed] [Google Scholar]
- 62.Yerrakalva D., Yerrakalva D., Hajna S., Griffin S. Effects of Mobile Health App Interventions on Sedentary Time, Physical Activity, and Fitness in Older Adults: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2019;21:e14343. doi: 10.2196/14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Faruque L.I., Wiebe N., Ehteshami-Afshar A., Liu Y., Dianati-Maleki N., Hemmelgarn B.R., Manns B.J., Tonelli M. Effect of telemedicine on glycated hemoglobin in diabetes: A systematic review and meta-analysis of randomized trials. CMAJ. 2017;189:E341–E364. doi: 10.1503/cmaj.150885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Su D., Zhou J., Kelley M.S., Michaud T.L., Siahpush M., Kim J., Wilson F., Stimpson J.P., Pagán J.A. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res. Clin. Pract. 2016;116:136–148. doi: 10.1016/j.diabres.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 65.Davies M.J., D’Alessio D.A., Fradkin J., Kernan W.N., Mathieu C., Mingrone G., Rossing P., Tsapas A., Wexler D.J., Buse J.B. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2018;41:2669–2701. doi: 10.2337/dci18-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De Groot J., Wu D., Flynn D., Robertson D., Grant G., Sun J. Efficacy of telemedicine on glycaemic control in patients with type 2 diabetes: A meta-analysis. World J. Diabetes. 2021;12:170–197. doi: 10.4239/wjd.v12.i2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Robson N., Hosseinzadeh H. Impact of Telehealth Care among Adults Living with Type 2 Diabetes in Primary Care: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Int. J. Environ. Res. Public Health. 2021;18:12171. doi: 10.3390/ijerph182212171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee P.A., Greenfield G., Pappas Y. The impact of telehealth remote patient monitoring on glycemic control in type 2 diabetes: A systematic review and meta-analysis of systematic reviews of randomised controlled trials. BMC Health Serv. Res. 2018;18:495. doi: 10.1186/s12913-018-3274-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mann D.M., Chen J., Chunara R., Testa P.A., Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020;27:1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stanberry B. Telemedicine: Barriers and opportunities in the 21st century. J. Intern. Med. 2000;247:615–628. doi: 10.1046/j.1365-2796.2000.00699.x. [DOI] [PubMed] [Google Scholar]
- 71.Mistry H. Systematic review of studies of the cost-effectiveness of telemedicine and telecare. Changes in the economic evidence over twenty years. J. Telemed. Telecare. 2012;18:1–6. doi: 10.1258/jtt.2011.110505. [DOI] [PubMed] [Google Scholar]
- 72.Kruk M.E., Freedman L.P. Assessing health system performance in developing countries: A review of the literature. Health Policy. 2008;85:263–276. doi: 10.1016/j.healthpol.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 73.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.