Abstract
In studies that have reported device-based measures of sedentary time (ST) in people with chronic obstructive pulmonary disease (COPD), we explored if the monitor type and monitor wear time moderated the estimate of this measure. Five electronic databases were searched in January 2021. Studies were included if >70% of participants had stable COPD, and measures of ST (min/day) were collected using wearable technology. Meta-regression was used to examine the influence of moderators on ST, monitor type, and wear time. The studies identified were a total of 1153, and 36 had usable data for meta-analyses. The overall pooled estimate of ST (mean [95% CI]) was 524 min/day [482 to 566] with moderate heterogeneity among effect sizes (I2 = 42%). Monitor wear time, as well as the interaction of monitor wear time and monitor type, were moderators of ST (p < 0.001). The largest difference (−318 min; 95% CI [−212 to −424]) was seen between studies where participants wore a device without a thigh inclinometer for 24 h (and removed sleep during analysis) (675 min, 95% CI [589 to 752]) and studies where participants wore a device with a thigh inclinometer for 12 h only (356 min; 95% CI [284 to 430]). In people with COPD, the monitor wear time and the interaction of the monitor wear time and the monitor type moderated the estimate of ST.
Keywords: COPD, inclinometer, meta-analysis, sedentary time, systematic review
1. Introduction
Sedentary behaviour is defined as any behaviour undertaken during waking hours, in a seated or reclined posture, that requires low energy expenditure (i.e., <1.5 metabolic equivalents of tasks [METs] [1]. Common examples in older adults include television viewing, reading, completing crossword puzzles [1]. There is recognition that reducing sedentary time (ST) is an important lifestyle target for many clinical populations [2,3,4], including adults with chronic obstructive pulmonary disease (COPD) [5,6]. Specifically, in this population, increased ST has been linked with deleterious health outcomes such as a higher risk of cardiometabolic disease [7,8], and clinical trials are now reporting device-measured ST as an outcome of interest [9,10,11]. This review targets adults with chronic obstructive pulmonary disease (COPD), as this population is extremely sedentary [12] and is at greater risk of poor health outcomes due to pre-morbid health conditions [13] and engagement in prolonged, uninterrupted sitting [5,6].
The approach used to quantify ST in people with COPD differs considerably across studies [14]. That is, many studies have focused on measuring physical activity as the primary outcome and then have quantified daily inactivity (sitting, lying, and standing still) data as ST. This is achieved by downloading data collected with wearable devices and classifying the time during which movement was recorded as ‘physical activity’, and the time during which no movement was recorded as ‘ST’. That is, periods of physical inactivity are classified as ST [15]. This issue is overcome by using wearable devices that include an inclinometer on the thigh, which can separate inactivity into behaviour undertaken in seated or reclined posture (where the thigh is horizontal and should be classified as ST) from those undertaken when standing still (where the thigh is vertical and should be classified as light-intensity physical activity) [16].
Another factor that may have little influence on measures of physical activity but may produce large differences in the measure of ST is monitor wear time (e.g., 12 h vs. all waking hours). That is, in people with COPD, physical activity is most likely to occur during daylight hours, which will be captured over a 12 h sampling period (e.g., 07:00 to 19:00). In contrast, the time between sunset and going to bed for overnight sleep is very likely classified as ST (e.g., television viewing), and ceasing data collection in the early evening (e.g., 19:00) may mean ST will be grossly underestimated.
To explore these issues and provide information on the precision of measures of ST, we undertook a systematic review and meta-analyses to address the following research question: In studies that have reported on device-measured ST in people with COPD, does monitor type (i.e., with or without a thigh inclinometer) or monitor wear time moderate the estimate of this measure?
2. Methods
2.1. Study Selection
This study has been reported in accordance with the Preferred Reporting of Items for Systematic Review and Meta-analysis (PRISMA) guidelines [17] (File S1). Studies were included if >70% of the participants had stable COPD, and measures of ST (min/day) were collected using wearable technology (e.g., accelerometers, inclinometers). Studies published only as conference abstracts or in a language other than English were excluded.
2.2. Search Strategy
Studies were identified by searching five electronic databases: CINAHL, the Cochrane Library, EMBASE, (via OVID), PEDro (Physiotherapy Evidence Database), and PubMed from their inception to 7 January 2021. Reference lists (hand searches) from relevant papers were also screened. The search strategy used for PubMed was adapted for use in other databases (Figure S1).
The research question addressed in this systematic review was not included in the prospective registration of PROSPERO (CRD42019138106). The analyses presented in this paper constitute an additional analysis relating to the broad theme of sedentary behaviour and people with COPD.
Using Covidence software, [18] two review authors (FC and SW) independently screened titles, abstracts, and full papers as required to identify eligible studies. Disagreement was resolved by discussion or when needed by a third review author (KH).
2.3. Data Extraction
Data were extracted into Microsoft Excel database by one author (FC) and checked by another author (KH). Data were extracted on sample size, monitor type, monitor wear time and, where appropriate, the method to omit sleep time from analysis. That is, it was noted whether the study asked participants to: (i) wear the monitor for a standard hours period (12 h protocol), (ii) remove the monitor overnight so that sleep was not included in the estimate of ST (waking hours protocol) or, (iii) wear the monitor continuously and during analysis, data that appeared to be overnight sleep were omitted (24 h sleep removed protocol). Where studies had collected measures of ST before and after an intervention, only data collected prior to the intervention were included in our analysis. The mean and standard deviation (SD) of the estimate of ST was expressed in natural units (i.e., min/day). If the estimates were reported using other measures of central tendency and dispersion (e.g., median and interquartile range), online software was used to derive estimates of mean and SD [19]. In the case of missing data, study authors were contacted via email on a maximum of three occasions.
2.4. Statistical Analysis
Included studies were coded and grouped accordingly to the moderator variables (i.e., monitor type and monitor wear time) into six groups: (i) monitor type: had a thigh inclinometer; wear time: 12 h; (ii) monitor type: had a thigh inclinometer; wear time: waking hours; (iii) monitor type: had a thigh inclinometer; wear time: 24 h with sleep removed; (iv) monitor type: no thigh inclinometer; wear time: 12 h; (v) monitor type: no thigh inclinometer; wear time: waking hours; (vi) monitor type: no thigh inclinometer; wear time: 24 h sleep removed. We analysed the data using random-effects, 3-level meta-analytic model via the package metafor [20] in the R statistical platform was used to account for dependencies of effects, namely, sampling variance of individual effects (level 1), as well as variance of effects within (level 2) and between (level 3) studies. The main and interaction effects of wear time and monitor type were estimated within random effects, meta-regression framework in which the null hypothesis is that the overall pooled effect is the same for all levels of the covariate [21].
3. Results
3.1. Study Selection and Grouping
The search yielded a total of 1153 records, of which 127 (11%) were duplicates. Of the remaining 1026 records, 765 (75%) were excluded during the title and abstract screening, and 208 (20%) were excluded following a full-text review (Figure 1). The Cohen’s Kappa for agreement regarding the inclusion of the studies between the two review authors was 0.98.
Figure 1.
Flow of studies through the review.
Of the remaining 53 studies, 36 reported data in a way that could be used in the meta-analyses. Of these, 25 (69%) were observational, and 11 (31%) were interventional studies. Regarding monitor type, 33% (n = 12) of the studies used a monitor that included a thigh inclinometer and was attached to the hip, upper arm, lumbar spine, or ankle. Regarding monitor wear time, 44% of studies (n = 16) used a 12 h protocol, 25% (n = 9) using a waking hours protocol, and 31% (n = 11) used a 24 h protocol.
All studies in this review measured physical activity as a primary outcome. Thirteen (36%) studies also described ST as a primary outcome, and the others reported ST as a secondary outcome.
3.2. Characteristics of Participants
The characteristics of 36 studies are presented in Table 1. Studies were conducted in Australia [6,9,10,11,22,23], Austria [24], Brazil [5,12,25,26,27,28,29,30,31,32,33,34,35,36,37], Canada [38], Germany [39]. Greece [40], Japan [41], Korea [42], the Netherlands [43,44], Portugal [45,46], Saudi Arabia [47], Sweden [48], United Kingdom [49], and the United States of America [50,51]. The total number of participants across 36 studies was 3914 (56% males), and the mean ± SD for age was 67 ± 8 years. The (mean ± SD) forced expiratory volume in one second (FEV1) ranged between 24 ± 9% and 85 ± 28% predicted, with the sample size of the included studies ranging between 10 and 941 participants.
Table 1.
Characteristics of included studies.
| Study (Publication Year) | Total Sample Size | Age, Year | Males, N (Y%) | FEV1, % Predicted | Device | Time over which Participants were Instructed to Wear the Device | Minimum Daily wear Time to be Included in Analyses | Minimum Number of Days Data Needed to be Available to be Included in Analyses | Days Used in Data Analyses |
|---|---|---|---|---|---|---|---|---|---|
| Studies which used a monitor with a thigh inclinometer and a 12 h protocol | |||||||||
| Breyer (2010) [24] | 60 | 60 ± 9 | 27 (45) | 46 ± 18 | DAM | 3 days | 12 h | 3 days | Weekend days were excluded |
| Cani (2019) [25] |
59 | O2: 68 ± 8 C: 67 ± 8 |
O2: 21 (79) C: Not recorded |
O2: 25 ± 7 C: 24 ± 9 |
DAM | 2 days | 12 h | 2 days | All days included |
| Kawagoshi (2013) [41] | 26 | 77 ± 6 | 26 (100) | 53 ± 26 | A-MES | 7 days | 12 h | 2 days | All days included |
| Munari (2018) [31] | 115 | 66 ± 8 | 75(68) | 35 ± 16 | DAM | Not reported | 12 h | 2 days | All days included |
| Pitta (2005) [12] |
50 | 64 ±7 | 36 (72) | 43 ± 18 | DAM | 2 days | 12 h | 2 days | All days included |
| Pitta (2005) [33] |
13 | 61 ±8 | 10 (77) | 33 ± 10 | DAM | 1 day | 12 h | 1 day | All days included |
| Pitta (2009) [32] |
80 | A: 63 ± 7 B: 66 ± 8 |
A: 21 (53) B: 18 (45) |
A: 48 ± 17 B: 46 ± 17 |
DAM | 2 days | 12 h | 2 days | All days included |
| Probst (2011) [34] | 40 | Ix: 65 ± 10 C: 67 ± 7 |
21 (52) | Ix: 39 ± 14 C: 40 ± 13 |
DAM + SWA | 2 days | 12 h | 2 days | Weekend days were excluded |
| Studies that used a monitor without a thigh inclinometer and a 12 h protocol | |||||||||
| Furlanetto (2017) [6] | 101 | 66 (62–72) median (IQR) | 58 (57) | 41(30–50) | SWA + Dynaport | 2 days | 12 h | 2 days | Weekend days were excluded |
| Gulart (2018) [26] | 59 | 65 ± 9 | 45 (76) | 35 ± 13 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Gulart (2020) [27] | 53 | 64 ± 9 | 37 (70) | 38 ± 14 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Gulart (2020) [28] | 61 | 65 ± 9 | 47 (77) | 35 ± 13 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Karloh (2016) [37] | 38 | 65 ± 7 | 22 (58) | 41 ± 15 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Machado (2019) [29] | 270 | G1: 67 ± 8 G2: 67 ± 8 G3: 68 ± 9 C: 67 ± 7 |
G1:25 (74) G2:35 (63) G3:59 (80) C: 33 (31) |
G1: 47 ± 16 G2: 43 ± 16 G3: 42 ± 16 C: 50 ± 14 |
SWA | 2 days | ≥10 h | 2 weekdays | Weekend days were excluded |
| Morita (2018) [30] | 145 | 65 (60–73) median (IQR) | 67 (46) | 45 ± 15 | Dynaport move-monitor | 2 days | 12 h | 2 days | All days included |
| Schneider (2018) [35] | 137 | 66 ± 8 | 75 (56) | 46 (31–54) IQR | SWA | 2 days | ≥10 h | 2 weekdays | All days included |
| Studies that used a monitor without a thigh inclinometer and a waking hours protocol | |||||||||
| Alyami (2018) [47] | 34 | 62 ± 5 | 34(100) | 46 ± 16 | SAM | 8 days | ≥10 h | ≥5 days | All days included |
| Bernard (2018) [38] | 941 | 57 ± 15 | 519(55) | 85 ± 28 | Actical | 7 days | ≥8 h | ≥4 days | All days included |
| Cruz (2014) [45] |
16 | 66 ± 11 | 11(69) | 70 ± 23 | Actigraph | 7 days | ≥8 h | ≥5 days | All days included |
| Cruz (2016) [46] |
32 | 67 ± 8 | 27(84) | 67 ± 20 | Actigraph | 4 weekdays | ≥8 h | 4 days | Weekend days were excluded |
| Eliason (2011) [48] | 44 | Mild COPD: 64 ± 6 Moderate COPD: 64 ± 8 Severe COPD: 63 ± 8 |
16(36) | Not recorded | Actigraph | 7 days | ≥8 h | ≥3 days | All days included |
| Geidl (2019) [39] |
326 | 58 ± 6 | 174 (68) | 54 ± 18 | Actigraph | 7 days | ≥10 h | ≥5 days | All days included |
| Larson (2014) [50] | 49 | Ix: 71 ± 8 Ix: 72 ± 9 C: 71 ± 8 |
41(84) | Ix: 61 ± 20 Ix: 54 ± 17 C: 56 ± 17 |
Actigraph | 7 days | ≥10 h | ≥3 days | All days included |
| Park (2013) [42] |
224 | 70 ± 9 | 114(51) | Actigraph | 7 days | ≥10 h | ≥4 days | All days included | |
| Vasilopoulou (2018) [40] | 147 | Ix: 67 ± 10 Ix: 67 ± 7 C: 64 ± 8 |
Ix: 44(94) Ix: 38(76) C: 37(74) |
Ix: 50 ± 22 Ix: 52 ± 17 C: 52 ± 21 |
Actigraph | Not recorded | ≥8 h | ≥4 days | All days included |
| Studies that used a monitor with a thigh inclinometer and 24 h sleep removed protocol | |||||||||
| Cheng (2020) [22] | 69 | 74 ± 9 | 33 (48) | 55 ± 15 | ActivPAL | 7 days | ≥10 h | ≥4 days | All days included |
| Hill (2020) [11] |
11 | 72 ± 9 | 5 (45) | 28 ± 26 | ActivPAL | 5 to 7 days | ≥10 h | ≥3 days | All days included |
| Mesquita (2017) [43] | 90 | 67 ± 8 | 54 (60) | 47 ± 9 | MOX and CAM | ≥7 days | ≥10 h | 5 days | All days included |
| Mesquita (2017) [44] | 125 | 67 ± 4 | 69 (55) | 50 ± 9 | MOX | ≥7 days | ≥10 h | 5 days | All days included |
| Studies that used a monitor without a thigh inclinometer and a 24 h sleep removed protocol | |||||||||
| Holland (2017) [9] | 160 | Ix: 69 ± 13 Ix: 69 ± 10 |
Ix: 48 (60) Ix: 51 (64) |
52 ± 19 49 ± 19 |
SWA | 7 days | ≥10 h | ≥4 days | Yes 1 w/e day included |
| Lewis (2016) [6] |
24 | 75 ± 8 | 18(75) | 54 ± 23 | SWA + Actigraph | 7 days | ≥12 h | 6 days | All days included |
| Loprinzi (2015) [51] | 10 | 70 ± 10 | 4(40) | 68 ± 48 | Actigraph | 7 days | ≥10 h | 4 days | All days included |
| McNamara (2014) [23] | 50 | COPD + PC: 73 ± 11 COPD: 70 ± 8 |
COPD + PC: 11 (44) COPD: 12 (48) |
51 ± 17 54 ± 11 |
SWA | 9 days | >85% wear time | 3 days | All days included |
| Orme (2019) [49] |
109 | 66 ± 7 | 67 (61) | 76 ± 18 | Actigraph | 7 days | ≥10 h | ≥4 days | All days included |
| Schneider (2018) [36] | 45 | 66 ± 8 | 25 (55) | 46 ± 20 | SWA | 7 days | 24 h (3 groups: 8 h; 12 h; period awake) |
7 days | All days included |
| Wootton (2017) [10] | 101 | Ix: 69 ± 8 C: 68 ± 9 |
Ix: 38(61) C: 24(62) |
Ix: 42 ± 15 C: 43 ± 15 |
SWA | 7 days | ≥12 h | ≥3 days primary analysis ≥4 days secondary analysis |
No (primary analysis); 1 w/e day included (secondary analysis) |
Data are mean ± SD unless otherwise stated, A-MES: Activity Monitor and Evaluation System; C: control group; CAM: CIRO Activity Monitor; COPD + PC: chronic obstructive pulmonary disease + physical comorbidity; DAM: DynaPort Activity Monitor; FEV1% pred: forced expiratory volume in 1 s expressed as a percent predicted; Ix: intervention group; MOX: Mobile Only Accelerometer; O2: oxygen; SAM: Stepwatch Activity Monitor; SWA: SenseWear Armband.
3.3. Meta-Analysis
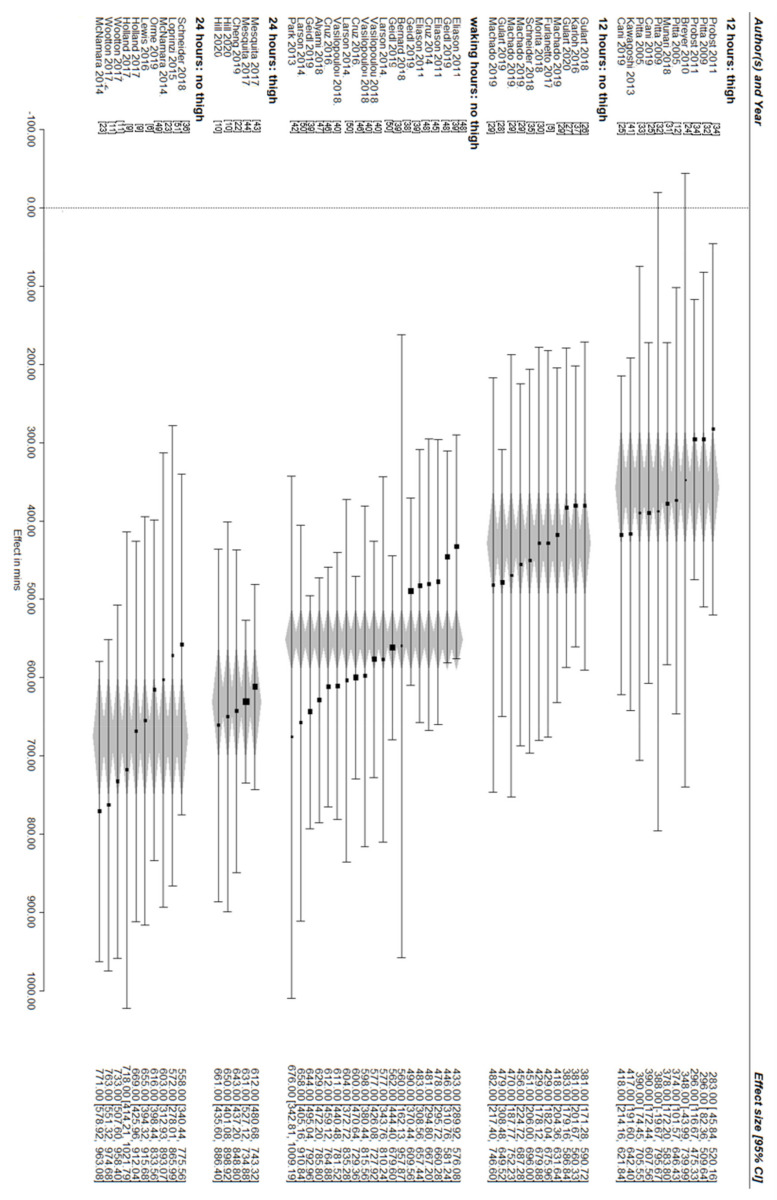
The overall pooled estimate of ST was 524 min/day (95% CI [482 to 566]), with a moderate amount of heterogeneity among effect sizes (I2 = 42%). Established guidelines for the interpretation of the proportion of total variance in effect estimates that is due to heterogeneity rather than sampling error are as follows: 0–40% = might not be important; 30–60% = may represent moderate heterogeneity; 50–90% = may represent substantial heterogeneity; and 75–100% = considerable heterogeneity [52]. Wear time (F (2,53)) = 26.23, p < 0.001 but not monitor type alone, (F (1,55)) = 2.21, p = 0.14) were meaningful moderators of the overall pooled estimate of ST. In terms of wear time, there was a stepwise reduction in ST between studies that used 24 h sleep removed protocol (651 min, 95% CI [599 to 703]), a waking hours protocol (551 min, 95% CI [512 to 590]) and a 12 h protocol (396 min, 95% CI [346 to 445]). For monitor type, the difference between no thigh inclinometer (545 min, 95% CI [494 to 596]) and thigh inclinometer (478 min, 95% CI [404 to 552]) was statistically inconsequential. When considering the interaction between wear time and monitor type, the highest ST was recorded by those studies that used ST in a 24 h sleep removed protocol and a device without a thigh inclinometer (675 min, 95% CI [598 to 752]), and the smallest ST was recorded by those studies which used a 12 h protocol and a device with thigh inclinometer (357 min 95% CI [284 to 430]) and the remaining estimates are between these quantities and are as follows: 12 h protocol and a device without a thigh inclinometer (429 min 95% CI [361 to 496]); waking hours protocol with a device without a thigh inclinometer (551 min 95% CI [512 to 590]); 24 h protocol with a device with a thigh inclinometer (631 min 95% CI [561 to 702]) (Figure 2) (Supplementary Material File S2: meta-analysis output file; Table S1 Data final).
Figure 2.
Forest plot of estimates of sedentary time with studies grouped according to wear time and monitor type. Data are represented as mean [95% confidence interval]. The grey diamonds represent the pooled 95% confidence interval for that category.
4. Discussion
This systematic review with meta-analyses is the first to report the range of methodologies used by studies that collected device-based measures of ST in people with COPD. The main findings were that studies in this area used highly disparate approaches to measure ST and that monitor wear time and the interaction of monitor wear time and monitor type influenced the estimate of ST.
Although understanding how people with COPD spend their waking hours has been an area of interest for more than a decade, an in-depth exploration of the methodological considerations regarding the measurement of ST in this population is lacking. This is because the focus of studies that have explored the use of waking hours in COPD has almost exclusively been on participation in physical activity. Specifically, in 2021 a task force comprised of researchers and key industry partners reviewed the data from the US-based COPDGene study [53] and the EU-based IMI-JU PROactive [54], as well as studies from individual consortium members that had collected measures of physical activity in COPD [55]. Based on their review of these data, a standardised methodology was proposed to guide the collection of device-measured physical activity in future research [55]. Recommendations were made regarding a minimum acceptable daily wear time of >8 h. Notwithstanding the well-established health benefits of regular participation in physical activity during daily life [56,57], epidemiological data collected in the general adult population have demonstrated that total ST in prolonged uninterrupted bouts increased the risk of cardiometabolic disease [2,5,58]. Of note, in people with COPD, similar associations have reported that reducing ST is increasingly considered an outcome for intervention-based studies [23,43]. Of note, although all studies included in the current review reported physical activity as a primary outcome, ST was also described as a primary outcome in 13 (36%) of studies. This highlights the need to understand the methodological considerations associated with reporting this outcome.
Our study is the first to demonstrate that monitor wear time is a moderator of the estimate of ST. That is, the longer the wear time protocol, the greater was the estimation of ST. For example, the mean difference in ST between studies that asked participants to wear devices for 24 h (and removed sleep during analysis) and those that asked participants to wear devices for 12 h was −318 min; (95% CI [−370 to −266]). Constraining monitor wear time to 12 h, which was the methodology adopted by 44% of the included studies, markedly reduced the potential for the true representation of ST. Conversely, the monitor type was not a moderator of ST. This is likely to reflect the discrepancy across the different subgroups. That is, studies that used a monitor that included a thigh inclinometer represent 6% of the combined sample size, whereas those studies which used a monitor that did not include a thigh inclinometer have 94% of the combined sample size.
Our study demonstrated that the interaction between monitor type and monitor wear time moderated ST. The smallest estimate of ST (356 min/day) was derived from studies that used a 12 h wear time protocol and a device that included a thigh inclinometer. This is because these studies underestimated ST with their short wear time protocol of 12 h. By using these data from a thigh inclinometer, we were also able to correctly classify standing still as light intensity physical activity rather ST; therefore, the estimate was smaller. The largest estimate of ST (675 min/day) was derived from studies that captured all waking hours using a 24 h wear time protocol (and removed sleep during analysis) and used a monitor without a thigh inclinometer, which would have misclassified standing still (inactivity) as ST, so, therefore, it was a larger estimate.
This review found that some of the studies used different anatomical locations for inclinometers. Although 25 percent of the studies included in this review used a monitor that incorporated an inclinometer attached to the upper arm, in this location, the inclinometer can only separate lying down (where the arm is horizontal) from sitting (the arm is vertical). Studies in other clinical populations [59,60,61,62] and that had no-clinical populations [16,63] have found similar results indicating the monitors with thigh inclinometers are less likely to misclassify standing as ST.
Strengths and Limitations
The strengths of this systematic review include: the use of two independent assessors to determine study inclusion, multiple attempts to contact authors of studies to clarify their suitability for inclusion, accounting for dependency among effects in our statistical model (i.e., multiple effects from the same sample) and missing or unpublished outcome data. Nevertheless, we were unable to include data from all studies. We accept that the influence of monitor wear time may be less when ST is expressed as a percentage of total wear time. However, we were unable to perform a meta-regression on ST expressed as a percentage of total wear time as these measures were not consistently reported with dispersion measures. We also note that the Dynaport Activity Monitor (DAM) (McRoberts BV, The Hague, Netherlands) and the SenseWear Armband (Bodymedia Inc, SenseWear Professional, Pittsburgh, (USA) that were used in 15 (42%) studies included in the review are no longer commercially available. Finally, although the topic of this systematic review broadly falls within the scope of a larger program of research that was prospectively registered (PROSPERO; CRD42019138106 and Open Science Framework; httpps://bit.ly/3j8Dt3n; accessed on 27 August 2021).), the specific research questions addressed in this study review were not specifically stated in these documents [64].
5. Conclusions
This systematic review and meta-analysis demonstrated that when collecting measures of ST in people with COPD, monitor wear time and the interaction of the monitor wear time and monitor type influence the estimate. These data suggest a meaningful comparison of the estimate of ST between studies or between time-points within the study is only possible when both monitor type and monitor wear time have been standardised. These considerations may not be important when quantifying physical activity but highlight the unique nuances in measuring ST. Specifically, we recommend that ST is measured using monitors that use an inclinometer located on the thigh to allow standing (which is LIPA) and sitting (which is ST) to be separated and properly classified. Further, it seems most appropriate to measure ST over 24 h but ensure that sleep is removed during the analysis by asking participants to diarise sleep and/or the application of processing algorithms.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11071980/s1, File S1: PRISMA checklist; File S2: meta-analysis output file; Figure S1: PubMed search strategy; Table S1: Data final.
Author Contributions
Conceptualization, K.H., V.C. and F.C.; methodology, K.H., F.C. and S.W.; software, D.F.G.; validation, K.H., V.C., F.C. and D.F.G.; formal analysis, D.F.G.; investigation, K.H. and F.C.; resources, D.F.G.; data curation, F.C., S.W. and K.H.; writing—original draft preparation, K.H. and F.C.; writing—review and editing, K.H., V.C., F.C., D.F.G. and S.W.; visualization, F.C. and K.H.; supervision, K.H.; project administration, K.H. and F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Detailed information on study data and analysis are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latima-Cheung A.E., Chastin S.F.M., Alternberg T.M., Chinapaw M.J.M., on behalf of SBRN Terminology Consensus Project Participants Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunstan D.W., Barr E.L., Healy G.N., Salmon J., Shaw J.E., Balkau B., Cameran A.J., Zimmet P.Z., Owen N. Television viewing time and mortality: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121:384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 3.Chomistek A.K., Manson J.E., Stefanick M.L., Lu B., Sands-Lincoln M., Going S.B., Garcia L., Allison M.A., Sims S.T., Lamonte M.J., et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the Women’s Health Initiative. J. Am. Coll. Cardiol. 2013;61:2346–2354. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tremblay M.S., Colley R.C., Saunders T.J., Healy G.N., Owen N. Physiological and health implications of a sedentary lifestyle. Appl. Physiol. Nutr. Metab. 2010;35:725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- 5.Furlanetto K.C., Donaria L., Schneider L.P., Lopes J.R., Ribeiro M., Fernandes K.B., Hernandes N.A., Pitta F. Sedentary Behavior Is an Independent Predictor of Mortality in Subjects With COPD. Respir. Care. 2017;62:579–587. doi: 10.4187/respcare.05306. [DOI] [PubMed] [Google Scholar]
- 6.Lewis L.K., Hunt T., Williams M.T., English C., Olds T.S. Sedentary Behavior in People with and without a Chronic Health Condition: How Much, What and When? AIMS Public Health. 2016;3:503–519. doi: 10.3934/publichealth.2016.3.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKeough Z., Cheng S.W.M., Alison J., Jenkins C., Hamer M., Stamakis E. Low leisure-based sitting time and being physically active were associated with reduced odds of death and diabetes in people with chronic obstructive pulmonary disease: A cohort study. J. Physiother. 2018;64:114–120. doi: 10.1016/j.jphys.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Park S.K., Larson J.L. The relationship between physical activity and metabolic syndrome in people with chronic obstructive pulmonary disease. J. Cardiovasc. Nurs. 2014;29:499–507. doi: 10.1097/JCN.0000000000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holland A.E., Mahal A., Hill C.J., Lee A.L., Burge A.T., Cox N.S., Moore R., Nicolson C., O’Halloran P., Lahham A. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax. 2017;72:57–65. doi: 10.1136/thoraxjnl-2016-208514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill K., Ng L.W.C., Cecins N., Formico V.R., Cavalheri V., Jenkins S.C. Effect of Using a Wheeled Walker on Physical Activity and Sedentary Time in People with Chronic Obstructive Pulmonary Disease: A Randomised Cross-Over Trial. Lung. 2020;198:213–219. doi: 10.1007/s00408-019-00297-2. [DOI] [PubMed] [Google Scholar]
- 11.Wootton S.L., Hill K., Alison J.A., Ng L.W.C., Jenkins S., Eastwood P.R., Hillman D.R., Jenkins C., Spencer L., Cecins N. Effects of ground-based walking training on daily physical activity in people with COPD: A randomised controlled trial. Respir. Med. 2017;132:139–145. doi: 10.1016/j.rmed.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Pitta F., Troosters T., Spruit M.A., Probst V.S., Decramer M., Gosselink R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2005;171:972–977. doi: 10.1164/rccm.200407-855OC. [DOI] [PubMed] [Google Scholar]
- 13.Sin D.D., Anthonisen N.R., Soriano J.B., Agust A.G. Mortality in COPD: Role of comorbidities. Eur. Respir. J. 2006;28:1245–1257. doi: 10.1183/09031936.00133805. [DOI] [PubMed] [Google Scholar]
- 14.Byrom B., Rowe D.A. Measuring free-living physical activity in COPD patients: Deriving methodology standards for clinical trials though a review of research studies. Contemp. Clin. Trials. 2016;47:172–184. doi: 10.1016/j.cct.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 15.Owen N., Healy G.N., Matthews C.E., Dunstan D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010;38:105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant P.M., Ryan C.G., Tigbe W.W., Granat M.H. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br. J. Sports Med. 2006;40:992–997. doi: 10.1136/bjsm.2006.030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Covidence Systematic Review Software. Veritas Health Innovation; Melbourne, Australia: 2020. Computer Program. [Google Scholar]
- 19.SPSS Statistics for Windows. IBM; Armonk, NY, USA: 2017. Version 25.0. Computer Program. [Google Scholar]
- 20.Viechtbauer W. Conducting meta-analyses in R with metafor package. J. Stat. Softw. 2010;36:1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 21.Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H. Introduction to Meta-Analysis. TJ International; Cornwall, UK: 2009. [Google Scholar]
- 22.Cheng S.W.M., Alison J.A., Stamatakis E., Dennis S., McKeough Z.J. Patterns and Correlates of Sedentary Behaviour Accumulation and Physical Activity in People with Chronic Obstructive Pulmonary Disease: A Cross-Sectional Study. COPD J. Chronic Obstr. Pulm. Dis. 2020;17:156–164. doi: 10.1080/15412555.2020.1740189. [DOI] [PubMed] [Google Scholar]
- 23.McNamara R.J., McKeough Z.J., McKenzie D.K., Alison J.A. Physical comorbidities affect physical activity in chronic obstructive pulmonary disease: A prospective cohort study. Respirology. 2014;19:866–872. doi: 10.1111/resp.12325. [DOI] [PubMed] [Google Scholar]
- 24.Breyer M.K., Breyer-Kohansal R., Funk G.C., Dornhofer N., Spruit M., Wouters E., Wouters E.F.M., Burghuber O.C., Hartl S. Nordic walking improves daily physical activities in COPD: A randomised controlled trial. Respir. Res. 2010;11:112. doi: 10.1186/1465-9921-11-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cani K.C., Matte D.L., Silva I., Gulart A.A., Karloh M., Mayer A.F. Impact of Home Oxygen Therapy on the Level of Physical Activities in Daily Life in Subjects With COPD. Respir. Care. 2019;64:1392–1400. doi: 10.4187/respcare.06206. [DOI] [PubMed] [Google Scholar]
- 26.Gulart A.A., Munari A.B., Klein S.R., Santos de Silveira L., Mayer A.F. The Glittre-ADL Test Cut-Off Point to Discriminate Abnormal Functional Capacity in Patients with COPD. COPD J. Chronic Obstr. Pulm. Dis. 2018;15:73–78. doi: 10.1080/15412555.2017.1369505. [DOI] [PubMed] [Google Scholar]
- 27.Gulart A.A., Araujo C.L.P., Munari A.B., Santos K.D., Karloh M., Foscarini B.G., Dal Lago P., Mayer A.F. The minimal important difference for Glittre-ADL test in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2020;24:54–60. doi: 10.1016/j.bjpt.2018.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gulart A.A., Munari A.B., Klein S.R., Venancio R.S., Alexandre H.F., Mayer A.F. The London Chest Activity of Daily Living scale cut-off point to discriminate functional status in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2020;24:264–272. doi: 10.1016/j.bjpt.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Machado F.V.C., Schneider L.P., Fonseca J., Belo L.F., Bonomo C., Furlanetto K.C., Felcar J.M., Roderigues A., Franssen F.M.E., Spruit M.A. Clinical impact of body composition phenotypes in patients with COPD: A retrospective analysis. Eur. J. Clin. Nutr. 2019;73:1512–1519. doi: 10.1038/s41430-019-0390-4. [DOI] [PubMed] [Google Scholar]
- 30.Morita A.A., Silva L.K.O., Bisca G.W., Oliveira J.M., Hernandes N.A., Pitta F., Furlanetto K.C. Heart Rate Recovery, Physical Activity Level, and Functional Status in Subjects With COPD. Respir. Care. 2018;63:1002–1008. doi: 10.4187/respcare.05918. [DOI] [PubMed] [Google Scholar]
- 31.Munari A.B., Gulart A.A., Dos Santos K., Venancio R.S., Karloh M., Mayer A.F. Modified Medical Research Council Dyspnea Scale in GOLD Classification Better Reflects Physical Activities of Daily Living. Respir. Care. 2018;63:77–85. doi: 10.4187/respcare.05636. [DOI] [PubMed] [Google Scholar]
- 32.Pitta F., Breyer M.K., Hernandes N.A., Teixeira D., Sant’Anna T.J., Fontana A.D., Probst V.S., Brunetto A.F., Spruit M.A., Wouters E.F. Comparison of daily physical activity between COPD patients from Central Europe and South America. Respir. Med. 2009;103:421–426. doi: 10.1016/j.rmed.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 33.Pitta F., Troosters T., Spruit M.A., Decramer M., Gosselink R. Activity monitoring for assessment of physical activities in daily life in patients with chronic obstructive pulmonary disease. Arch. Phys. Med. Rehabil. 2005;86:1979–1985. doi: 10.1016/j.apmr.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 34.Probst V.S., Kovelis D., Hernandes N.A., Camillo C.A., Cavalheri V., Pitta F. Effects of 2 exercise training programs on physical activity in daily life in patients with COPD. Respir. Care. 2011;56:1799–1807. doi: 10.4187/respcare.01110. [DOI] [PubMed] [Google Scholar]
- 35.Schneider L.P., Furlanetto K.C., Rodrigues A., Lopes J.R., Hernandes N.A., Pitta F. Sedentary Behaviour and Physical Inactivity in Patients with Chronic Obstructive Pulmonary Disease: Two Sides of the Same Coin? COPD J. Chronic Obstr. Pulm. Dis. 2018;15:432–438. doi: 10.1080/15412555.2018.1548587. [DOI] [PubMed] [Google Scholar]
- 36.Schneider L.P., Furlanetto K.C., Hernandes N.A., Pitta F. Does wearing time of motion sensor interfere with the choice of physical activity in daily life outcomes of COPD patients? Fisioter. Pesqui. 2018;25:43–48. doi: 10.1590/1809-2950/16768425012018. [DOI] [Google Scholar]
- 37.Karloh M., Araujo C.L., Gulart A.A., Reis C.M., Steidle L.J., Mayer A.F. The Glittre-ADL test reflects functional performance measured by physical activities of daily living in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2016;20:223–230. doi: 10.1590/bjpt-rbf.2014.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bernard P., Hains-Monfette G., Atoui S., Moullec G. Daily Objective Physical Activity and Sedentary Time in Adults with COPD Using Spirometry Data from Canadian Measures Health Survey. Can. Respir. J. 2018;2018:9107435. doi: 10.1155/2018/9107435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geidl W., Carl J., Cassar S., Lehbert N., Mino E., Wittmann M., Wagner R., Schulz K., Pfeifer K. Physical Activity and Sedentary Behaviour Patterns in 326 Persons with COPD before Starting a Pulmonary Rehabilitation: A Cluster Analysis. J. Clin. Med. 2019;8:1346. doi: 10.3390/jcm8091346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vasilopoulou M., Papaioannou A.I., Kaltsakas G., Louvaris A., Chynkiamis N., Stavroula S., Kortianou E., Genimata S.A., Palamidas A., Kostikas K. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur. Respir. J. 2017;49:1602129. doi: 10.1183/13993003.02129-2016. [DOI] [PubMed] [Google Scholar]
- 41.Kawagoshi A., Kiyokawa N., Sugawara K., Takahashi H., Sakata S., Miura S., Sawamura S., Satake M., Shioya T. Quantitative assessment of walking time and postural change in patients with COPD using a new triaxial accelerometer system. Int. J. Chronic Obstr. Pulm. Dis. 2013;8:397–404. doi: 10.2147/COPD.S49491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park S.K., Richardson C.R., Holleman R.G., Larson J.L. Physical activity in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003–2006) Heart Lung. 2013;42:235–240. doi: 10.1016/j.hrtlng.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mesquita R., Meijer K., Pitta F., Azcuna H., Goetz Y.M.J., Essers J.M.N., Wouters E.F.M., Spruit M.A. Changes in physical activity and sedentary behaviour following pulmonary rehabilitation in patients with COPD. Respir. Med. 2017;126:122–129. doi: 10.1016/j.rmed.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 44.Mesquita R., Nakken N., Janssen D.J.A., van den Bogaart E.H., Delbressine J.M.L., Essers J.M.N., Meijer K., van Vliet M., de Vries G.J., Muris J.W. Activity Levels and Exercise Motivation in Patients With COPD and Their Resident Loved Ones. Chest. 2017;151:1028–1038. doi: 10.1016/j.chest.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 45.Cruz J., Brooks D., Marques A. Impact of feedback on physical activity levels of individuals with chronic obstructive pulmonary disease during pulmonary rehabilitation: A feasibility study. Chron. Respir. Dis. 2014;11:191–198. doi: 10.1177/1479972314552280. [DOI] [PubMed] [Google Scholar]
- 46.Cruz J., Brooks D., Marques A. Walk2Bactive: A randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron. Respir. Dis. 2016;13:57–66. doi: 10.1177/1479972315619574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alyami M.M., Jenkins S.C., Hill K. Walking-based activity and sedentary behavior in Saudi males with chronic obstructive pulmonary disease. Saudi Med. J. 2018;39:506–513. doi: 10.15537/smj.2018.5.22043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eliason G., Zakrisson A.B., Piehl-Aulin K., Hurtig-Wennlof A. Physical activity patterns in patients in different stages of chronic obstructive pulmonary disease. COPD J. Chronic Obstr. Pulm. Dis. 2011;8:369–374. doi: 10.3109/15412555.2011.605403. [DOI] [PubMed] [Google Scholar]
- 49.Orme M.W., Steiner M.C., Morgan M.D., Kingsnorth A.P., Esliger D.W., Singh S.J., Sherar L.B. 24-hour accelerometry in COPD: Exploring physical activity, sedentary behavior, sleep and clinical characteristics. Int. J. Chronic Obstr. Pulm. Dis. 2019;14:419–430. doi: 10.2147/COPD.S183029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Larson J.L., Covey M.K., Kapella M.C., Alex C.G., McAuley E. Self-efficacy enhancing intervention increases light physical activity in people with chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2014;9:1081–1090. doi: 10.2147/COPD.S66846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loprinzi P.D., Kane C., Sigler S., Brown K., Walker J.K. Free-living physical activity characteristics, activity-related air trapping and breathlessness, and utilization of transtheoretical constructs in COPD: A pilot study. Physiol. Behav. 2015;152:79–84. doi: 10.1016/j.physbeh.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 52.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analysis. BMJ. 2003;237:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bowler R., Allinder M., Jacobson S., Miller B., Tal-Singer R., Locantore N. Real-world use of rescue inhaler sensors, electronic symptom questionnaires and physical activity monitors in COPD. BMJ Open Respir Res. 2019;6:e000350. doi: 10.1136/bmjresp-2018-000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Demeyer H., Louvaris Z., Frei A., Rabinovich R.A., de Jong C., Gimeno-Santas E., Loeckx M., Buttery S.C., Rubio N., Van der Molen T., et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: A multicentre randomised controlled trial. Thorax. 2017;72:415–423. doi: 10.1136/thoraxjnl-2016-209026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Demeyer H., Mohan D., Burtin C., Vaes A., Heasley M., Bowler R., Casaburi R., Cooper C.B., Corriol-Rohou S., Frei A., et al. Objectively Measured Physical Activity in Patients with COPD: Recommendations from an International Task Force on Physical Activity. Chronic Obstr. Pulm. Dis. J. COPD Found. 2021;8:528. doi: 10.15326/jcopdf.2021.0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.M., Nieman D.C., Swain D.P., American College of Sports Medicine American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 57.Pate R.R., Pratt M., Blair S.N., Haskell W.L., Macera C.A., Bouchard C., Buchner D., Ettinger W., Heath G.W., King A.C., et al. American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.1995.03520290054029. [DOI] [PubMed] [Google Scholar]
- 58.Chau J.Y., Grunseit A., Midthjell K., Holmen T.L., Bauman A.E., van der Ploeg H.P. Cross-sectional associations of total sitting and leisure screen time with cardiometabolic risk in adults. Results from the HUNT Study, Norway. J. Sci. Med. Sport. 2014;17:78–84. doi: 10.1016/j.jsams.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 59.Peddle-McIntyre C.J., Cavalheri V., Boyle T., McVeigh J.A., Jeffery E., Lynch B.M., Vallance J.K. A Review of Accelerometer-based Activity Monitoring in Cancer Survivorship Research. Med. Sci. Sports Exerc. 2018;50:1790–1801. doi: 10.1249/MSS.0000000000001644. [DOI] [PubMed] [Google Scholar]
- 60.O’Brien C.M., Duda J.L., Kitas G.D., Veldhuijzen van Zanten J.S.C., Metsios G.S., Fenton S.A.M. Measurement of sedentary time and physical activity in rheumatoid arthritis: An ActiGraph and activPAL validation study. Rheumatol. Int. 2020;40:1509–1518. doi: 10.1007/s00296-020-04608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reid N., Daly R.M., Winkler E.A., Gardiner P.A., Eakin E.G., Owen N., Dunstan D.W., Healy G. Associations of Monitor-Assessed Activity with Performance-Based Physical Function. PLoS ONE. 2016;11:e0153398. doi: 10.1371/journal.pone.0153398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grant P.M., Dall P.M., Mitchell S.L., Granat M.H. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J. Aging Phys. Act. 2008;16:201–214. doi: 10.1123/japa.16.2.201. [DOI] [PubMed] [Google Scholar]
- 63.Kozey-Keadle S., Libertine A., Lyden K., Staudenmayer J., Freedson P.S. Validation of wearable monitors for assessing sedentary behavior. Med. Sci Sports Exerc. 2011;43:1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 64.Coll F., Cavalheri V., Gucciardi D.F., Wulff S., Hill K. In people with COPD, there is limited Evidence that Exercise Training Reduced Sedentary Time, and Behaviour Change Techniques are Poorly Reported: Systematic Review and Meta-analysis. Phys. Ther. 2021;101:pzab097. doi: 10.1093/ptj/pzab097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Detailed information on study data and analysis are available upon request from the corresponding author.