Abstract
Renal cell carcinoma (RCC) associated with anaplastic lymphoma kinase (ALK) gene rearrangements (ALK-RCC) is currently considered an “emerging or provisional” tumor entity by the last World Health Organization classification published in 2016. Although several studies assessing ALK-RCC’s clinical and histological characteristics have been published in recent years, only a few publications have evaluated the activity of ALK inhibitors (ALK-i) in this subgroup of patients. Considering the well-recognized efficacy of this evolving class of targeted therapies in other ALK-positive tumors, we conducted a systematic review to evaluate the reported activity of ALK-i in the ALK-RCC subtype. MEDLINE was searched from its inception to 7 January 2022 for case reports and case series on adult metastatic ALK-RCC patients treated with ALK-i whose therapeutic outcomes were available. A virtual cohort of ALK-RCC patients was created. Our results showed a favorable activity of first- and second-generation ALK-i in pretreated ALK-RCC patients in terms of either radiological response or performance status improvement. We hope that the present work will prompt the creation of large, multi-institutional clinical trials to confirm these promising early data.
Keywords: renal cell carcinoma, ALK, ALK inhibitors, ALK-RCC, systematic review
1. Introduction
1.1. Rationale
In the last decade, the increasing knowledge in molecular pathology and the genetics of renal cancer has led to the identification of new potential subtypes of renal cell carcinoma (RCC) [1], as demonstrated by the recognition of several “emerging or provisional” renal tumor entities in the “WHO classification of tumors of the urinary system and male genital organs” published in 2016 [2]. However, although these novel subtypes may appear to be distinct tumor entities, further studies on morphology, immunohistochemistry, and molecular biology are needed to define their diagnostic criteria and assess their clinical outcomes [2].
RCC associated with anaplastic lymphoma kinase (ALK) gene rearrangements (ALK-RCC) is a novel renal cancer entity, currently considered as “emerging or provisional” [2]. ALK is a receptor protein kinase that plays a physiologic role in the nervous system’s development. It is encoded by the ALK gene located on the 2p23 chromosome [3]. ALK rearrangements with other fusion partners have been described in various malignancies, such as anaplastic large-cell lymphoma (ALCL), non-small cell lung cancer (NSCLC), anaplastic thyroid carcinoma, and others [4]. ALK-RCC accounts for less than 1% of all RCC subtypes [5]. However, a growing number of publications assessing the clinical presentation and histological characteristics of patients affected by ALK-RCC have been published in recent years (Figure 1) [1,6], mainly as case reports and case series [5].
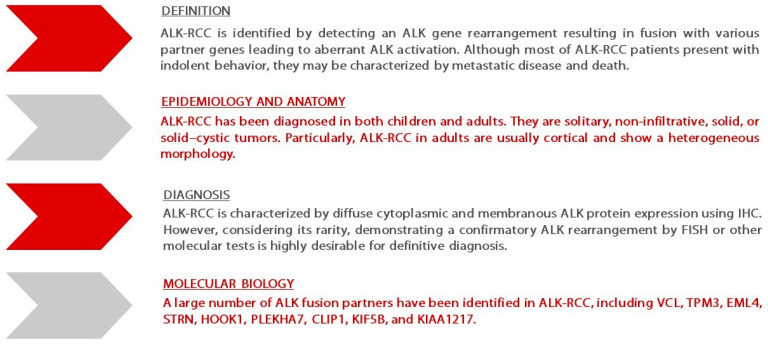
Figure 1.
Summary of ALK-RCC features adapted from the “GUPS update on renal neoplasia”—Ref. [6]. Abbreviations: ALK—anaplastic lymphoma kinase; ALK-RCC—renal cell carcinoma associated with ALK gene rearrangements; CLIP1—cytoskeleton-associated proteins-Gly domain containing linker protein 1; EML4—echinoderm microtubule-associated protein-like 4; FISH—fluorescence in situ hybridization; GUPS—Genitourinary Pathology Society; HOOK1—hook microtubule tethering protein 1 kinase; IHC—immunohistochemistry; KIF5B—kinesin family member 5B; PLEKHA7—Pleckstrin homology domain containing A7; STRN—striatin calmodulin-binding protein; TPM3—tropomyosin 3; VCL—vinculin.
Nowadays, the development of ALK inhibitors (ALK-i) has changed the treatment landscape of cancer patients with ALK alterations, as demonstrated by the dramatic and often prolonged responses to treatment achieved in patients affected by metastatic NSCLC [7]. In contrast, the activity of ALK-i in ALK-RCC patients has been reported in only a few publications. To the best of our knowledge, the impact of ALK-i on this population has never been reviewed.
1.2. Objectives
We conducted a systematic review according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (see Supplementary Material A) [8], aiming to evaluate the reported activity of ALK-i in ALK-RCC patients published in the scientific literature.
2. Methods
2.1. Eligibility Criteria
We included case reports and case series on adult patients affected by ALK-RCC who were treated with ALK-i. Only papers written in English or European languages were considered. The case series had to provide single descriptions of the reported cases to be included in the review. Letters to the editor providing single-case descriptions were also eligible if all the previous criteria were satisfied. All the references of the included studies were later hand-searched for additional eligible publications to include. On the contrary, case reports and case series on patients affected by ALK-RCC not treated with ALK-i were excluded, as well as narrative or systematic reviews on this topic.
2.2. Information Sources
We searched the electronic PubMed database from its inception to 7 January 2022 to identify all relevant papers. No research filters for case reports/case series or language limits were applied. All the results derived from the literature search were uploaded to a reference management software.
2.3. Search Strategy
The search strategy for eligible publications was established through a discussion among the authors. The following syntax was used: “(ALK OR ALK-rearranged) AND (renal cancer OR kidney cancer OR renal cell carcinoma* OR renal cell cancer OR renal)”.
2.4. Selection Process
The literature search was conducted independently by two of the authors. A two-stage study selection process was used. Firstly, all titles and abstracts were initially screened for potential relevance. Secondly, full texts of results deemed eligible were retrieved and further assessed for eligibility. Agreement of both authors was required for exclusion at both stages. A consultation with a third author was required to resolve disagreements on study selection by consensus. The authors achieved a complete consensus on publications to include in the systematic review before starting with data collection.
2.5. Data Collection Process
Two authors developed a data-charting template using Microsoft Excel to extract the variables of the included studies. They independently extracted the data and discussed the results in an interactive process. A third author verified all the extracted data.
2.6. Data Items
The variables extracted from the included papers were divided into three groups: study characteristics, patient characteristics, and exposure characteristics. The variables of the first group were: first author, publication date, journal of publication, type of study, and number of patients reported. The variables of the second group were: age, gender, presenting symptoms and signs, tumor staging, histotype of RCC, metastatic sites, type of ALK alteration, and previous surgical and medical treatments. Lastly, the variables of the third group were: type of ALK-i with the related therapeutic outcome described in terms of either best response according to the response evaluation criteria in solid tumors (RECIST) or survival (if available).
2.7. Study Risk of Bias Assessment
A tool proposed by Murad et al. to evaluate the methodological quality of case series and case reports was used to assess the risk of bias of publications included in the systematic review [9]. This tool considers eight different questions categorized in four domains: selection, ascertainment, causality, and reporting. A binary response (yes = 1 and no = 0) was assigned to every question and then an aggregate score was formulated for every publication [9].
2.8. Effect Measures
Variables extracted from eligible publications were described using numbers and proportions for categorical variables, and mean, standard deviation, median, and interquartile range for continuous variables.
2.9. Synthesis Methods
We reported aggregated data obtained from the included studies. Due to the limited sample size, no inferential or predictive statistics analyses were performed.
3. Results
3.1. Study Selection
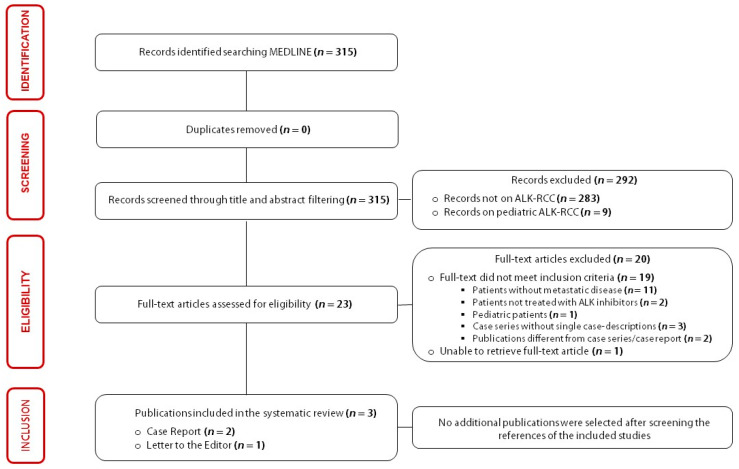
The literature search results and the identification process of papers included in the present systematic review are summarized using a PRISMA flow diagram in Figure 2.
Figure 2.
Flowchart of the results of literature search and identification process of included publications.
3.2. Study Characteristics
Three papers, published between 2018 and 2021, were included in this systematic review: two case reports and one letter to the editor. All the publications were written in English.
3.3. Results of Individual Studies
The results of single sources of evidence eligible for the present systematic review are described in Table 1.
Table 1.
Variables extracted from included publications.
| Study Characteristics | Patient Characteristics | Exposure Characteristics | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Author (Year of Publication) | Journal | Type of Study | Number of Cases | Age (Gender) | Initial Symptoms | Tumor Staging | Metastatic Sites | Hystotipe | ALK Alteration | Surgery | First-Line | Second-Line | Subsequent Lines | ALK-i | Outcome |
| Pal et al. (2018) [10] | Eur Urol. | LE | 3 | 66 (M) | Haematuria | Advanced | Brain—lung | ccRCC-pRCC | EML4-ALK | RN | Pazopanib | Savolitinib | Everolimus—nivolumab—cabozantnib | Alectinib | PR (9 mos)—AwD |
| - | - | - | - | 30 (F) | Excruciating hip—back pain | Advanced | Bone—lung—nodes | pRCC | EML4-ALK | RN | Savolitinib | - | - | Alectinib | PR (4 mos)—AwD |
| - | - | - | - | 85 (F) | Shortness of breath | Advanced | Lung | pRCC | EML4-ALK | No | CBDCA-Tax | - | - | Alectinib | PR (4 mos)—AwD |
| Zhou et al. (2020) [11] | Transl Androl Urol. | CR | 1 | 36 (F) | Follow up | Advanced | Nodes—lung | pRCC | ALK fusion partner not available | RN | Sunitinib | - | - | Crizotinib | PR (3 mos)—AwD |
| Varchetta et al. (2021) [12] | Recenti Prog Med. | CR | 1 | 44 (F) | NA | Advanced | Nodes—thyroid | NA | c.3512T > A | RN | Sunitinib | Sorafenib | Cabozantinib—bevacizumab—temsirolimus | Alectinib | PR (4 mos)—AwD |
Abbreviations: AwD—alive with disease; CBDCA—carboplatin; CR—case report; ccRCC—clear cell renal cell carcinoma; F—female; LE—letter to the editor; M—male; Mos—months; NA—not available; Tax—paclitaxel; pRCC—papillary renal cell carcinoma; PR—partial response; RN—radical nephrectomy.
3.4. Results of Syntheses
Data extracted from the selected papers allowed us to create a cohort of five patients affected by ALK-RCC treated with ALK-i, with available therapeutic outcomes (Table 2).
Table 2.
Results of quantitative analysis of variables extracted by included publications.
| Cohort | Staging | Treatments | |||
|---|---|---|---|---|---|
| Number of patients | 5 | Presence of metastases at diagnosis | Treatments before ALK-inhibitors | ||
| Median age (Range) | 44 (30—85) | Bone | 1 (20%) | Bevacizumab | 1 (20%) |
| Brain | 1 (20%) | Cabozantinib | 1 (20%) | ||
| Clinical presentation | Lymph-Nodes | 3 (60%) | Chemotherapy | 1 (20%) | |
| Lung | 4 (80%) | Everolimus | 1 (20%) | ||
| Initial symptoms | Thyroid | 1 (20%) | Nivolumab | 1 (20%) | |
| Back pain | 1 (20%) | Pazopanib | 1 (20%) | ||
| Hematuria | 1 (20%) | Histology and ALK alterations | Savolitinib | 2 (40%) | |
| Palpable mass | 2 (40%) | Sorafenib | 1 (20%) | ||
| Respiratory symptoms | 2 (40%) | Histological diagnosis | Sunitinib | 2 (40%) | |
| Weight loss | 1 (20%) | Papillary | 4 (80%) | Temsirolimus | 1 (20%) |
| No symptoms | 1 (20%) | Mixed Histology | 1 (20%) | Treatments with ALK-inhibitors | |
| ALK alterations | Alectinib | 4 (80%) | |||
| ALK-EML4 | 3 (60%) | Crizotinib | 1 (20%) | ||
| c.3512T > A | 1 (20%) | ||||
| Fusion partner not specified | 1 (20%) | Outcome | |||
| Partial disease | 4 (80%) | ||||
| Stable disease | 1 (20%) | ||||
The median age of the patients was 44 years (range: 30–85 years). The most frequent initial symptoms were a palpable mass in 40% of patients, respiratory symptoms (40%), back pain (20%), hematuria (20%), and weight loss (20%). Only one patient (20%) was asymptomatic at the time of diagnosis. All patients were affected by advanced RCC. The most common metastatic sites were lungs (80%), lymph nodes (60%), bones (20%), brain (20%), and thyroid (20%). The histological diagnosis was papillary RCC (PRCC) in 80% of cases and mixed histology RCC in 20% of patients. ALK alterations were detected with different procedures either in neoplastic tissue provided by biopsies of distant RCC metastases or circulating tumor DNA (ctDNA). In the case report published by Varchetta et al. [12], a genomic profiling test performed on a cell-block obtained by a lymph-node fine needle biopsy showed a pathogenic rearrangement (c.3512T > A) in the ALK gene. In the case report described by Zhou et al. [11], a rearrangement of the ALK gene with an unknown fusion partner was detected on a lung metastasis tissue through a FISH test performed due to ALK-positive results at the immunohistochemical analysis. In contrast, Pal et al. [10] detected in three patients a translocation between echinoderm microtubule-associated protein-like 4 (EML4) and ALK through a genomic profiling test performed on ctDNA. All patients received one or multiple lines of treatment before the administration of ALK-i: sunitinib in 40% of cases, savolitinib (40%), bevacizumab (20%), cabozantinib (20%), chemotherapy (20%), everolimus (20%), nivolumab (20%), pazopanib (20%), sorafenib (20%), and temsirolimus (20%). ALK-i administered to patients were alectinib in 80% of cases and crizotinib in 20% of cases. Concerning the assessment of ALK-i activity, 80% of patients achieved a radiological “partial response”, and 20% of patients were considered to have a “stable disease”. No patients were reported to have a progressive disease during ALK-i treatment. The mean progression-free survival (PFS) of ALK-i treated patients was 4.8 months (range: 3–9 months), despite the treatment still being ongoing in most cases at the time of publication.
3.5. Reporting Biases
We evaluated all the publications included in the review with the tool proposed by Murad et al. [9], assigning an aggregate score to every study (see Supplementary Material B).
4. Discussion
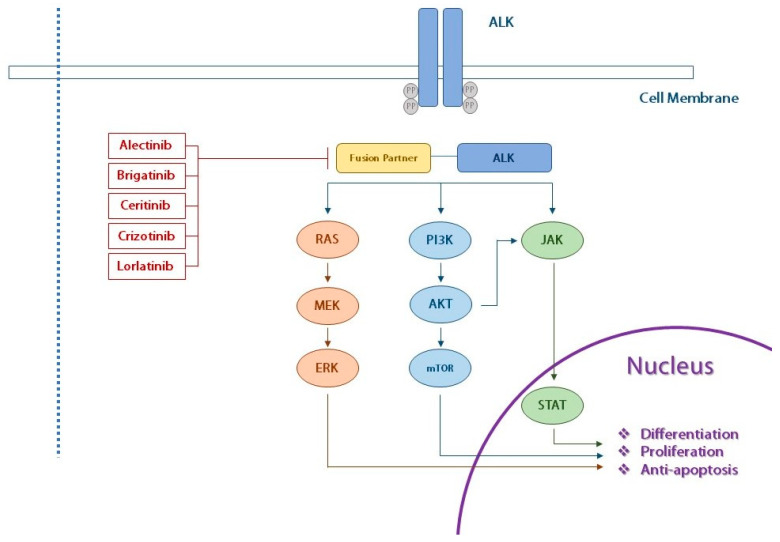
In recent years, the increasing understanding of RCC genetics has led to the identification of potential new renal tumor entities [1], classified as “emerging or provisional” in the recent “WHO classification of tumors of the urinary system and male genital organs”, including the ALK-RCC subtype [2]. ALK is a receptor protein kinase belonging to the superfamily of insulin receptors and encoded by the ALK gene located on the 2p23 chromosome [3]. The role of ALK in tumorigenesis was initially shown in ACLC by Morris et al. in 1994 [13]. Several mechanisms may cause ALK hyperactivation, such as translocations involving the kinase domain of the protein, point mutations, and gene amplification resulting in the pathological activation of pathways contributing to the cell acquisition of malignant phenotypes [3]. In particular, the phosphorylation of ALK results in the activation of downstream signaling pathways which can promote cell proliferation and differentiation, such as the Janus kinase (JAK)/signal transducer and activator of transcription (STAT), phosphatidylinositol-3-kinase (PI3K)/protein kinase-B (AKT)/mammalian target of rapamycin (mTOR), and rat sarcoma virus (RAS)/mitogen-activated protein kinase (MAPK) pathways (Figure 3) [14,15].
Figure 3.
Illustration of ALK fusion oncogene with main downstream signaling pathways. Abbreviations: ALK—anaplastic lymphoma kinase; ERK—extracellular signal-regulated kinase; JAK—Janus kinase; mTOR—mammalian target of rapamycin; MEK—mitogen-activated protein kinase; PI3K—phosphatidylinositol 3-kinase; PP—pyrophosphate; AKT—protein kinase B; RAS—rat sarcoma virus; STAT—signal transducer and activator of transcription.
Nowadays, different ALK alterations have been detected in several solid tumors such as ACLC, inflammatory myofibroblastic tumors, neuroblastomas, and NSCLC [4]. In parallel, the identification of ALK-positive tumors prompted the creation of a new class of targeted therapy, named ALK-i. Crizotinib was the first ALK-i drug approved in the setting of metastatic NSCLC. Subsequently, second-generation ALK-i (alectinib, brigatinib, and ceritinib) and, recently, a third-generation ALK-i (lorlatinib) have been introduced in the same clinical setting [16]. All these agents have shown an undeniable efficacy in patients affected by ALK-positive advanced NSCLC, thus revolutionizing the treatment landscape in this subgroup of patients [17].
Despite a lack of encouraging results, the activity of crizotinib has already been evaluated in the field of RCC treatment in recent years, due to its ability to inhibit the mitogen-activated protein kinase (MET). Indeed, an increased expression of MET has been implicated in either tumor angiogenesis or the development of resistance to anti-vascular endothelial growth factor (VEGF) therapies [18]. In 2019, Michaelson et al. published the results of a phase Ib study aimed to evaluate the combination of axitinib and crizotinib in advanced solid tumors and metastatic RCC, showing a manageable safety profile and evidence of modest antitumor activity for this combination [19]. Concomitantly, the genomic characterization of PRCC led to the identification of molecular alterations in the MET gene [20], suggesting the opportunity to investigate the effects of the MET inhibitors (including crizotinib) also in this RCC subtype. In 2017, Schoffski et al. published the results of a single cohort of patients affected by advanced PRCC treated with crizotinib enrolled in the CREATE trial [21]. Patients were divided into two subgroups depending on the presence of MET alterations. Only a small proportion of patients achieved durable responses, independent from the presence of MET alterations [21]. In 2021, Pal SK et al. published the results of the SWOG 1500 trial, which compared the standard of care (SoC), represented by sunitinib, with the other MET kinase inhibitors, including crizotinib, in metastatic PRCC patients [22]. The assignment to the crizotinib group was halted after a prespecified futility analysis. The final results showed that cabozantinib determined a significantly longer PFS in comparison to SoC and other MET inhibitors [22].
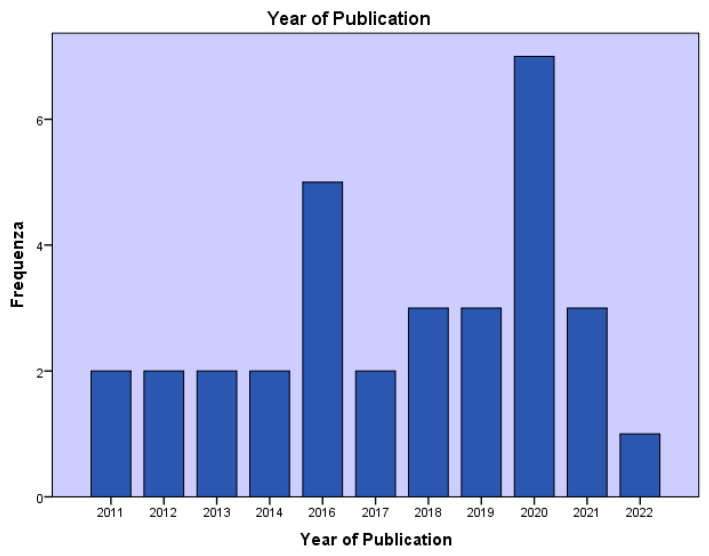
ALK-RCC accounts for less than 1% of all renal neoplasms [5]. It was described for the first time in 2010 [23]. Since then, a growing number of publications assessing the clinical presentation and histological characteristics of patients affected by ALK-RCC have been published (Figure 4) [6]. Indeed, approximately forty ALK-RCC cases have been reported (Table 3) in both adults and children, aged between 6 and 85 years [24]. Although most of the ALK-RCC patients present with an indolent behavior, they may be characterized by metastatic disease and death, as documented in about 25% of reported cases [6]. ALK-RCC are solitary tumors, generally not associated with any syndrome [25]. Concerning the gross pathological features, they are solid or solid–cystic tumors showing white-grey to yellow and variegated cut surfaces and can originate either from the medulla or the cortex [26]. The most frequent translocations reported in ALK-RCC patients are the fusion of the vinculin (VCL) and ALK, typically in young patients with the sickle cell trait [27], the TPM3–ALK and EML4–ALK fusions in tumors characterized by papillary, solid, and mucinous cribriform components. Furthermore, striatin (STRN) and ALK translocation typically appear in tumors with papillary, solid, tubular, and mucinous cribriform structures associated with psammoma bodies [28].
Figure 4.
Number of publications on ALK-RCC based on the year of publication.
Table 3.
Previously published cases of ALK-RCC.
| First Author | Journal | Year of Publication | Type of Study (Number of Cases) | Age (Gender) | Advanced Stage/Relapsed | Metastatic Sites | Hystotipe | ALK Translocation | Surgery | Medical Therapy |
|---|---|---|---|---|---|---|---|---|---|---|
| Debelenko et al. [23] | Mod Pathol. | 2011 | CS (6) | 16 (M) | No | Nodes | uRCC | VCL–ALK | RN | No |
| - | - | 2011 | - | 10 (F) | Yes | Nodes | RMC | VCL–ALK | RN | ChT |
| - | - | 2011 | - | 12 (M) | Yes | Lung | RMC | VCL–ALK | NA | NA |
| - | - | 2011 | - | 7 (F) | Yes | Lung | RPC | VCL–ALK | NA | NA |
| - | - | 2011 | - | 14 (M) | NA | - | RPC | VCL–ALK | NA | NA |
| - | - | 2011 | - | 6 (F) | No | - | uRCC | VCL–ALK | NA | NA |
| Mariño-Enríquez et al. [29] | Genes Chromosomes Cancer | 2011 | CR (1) | 6 (M) | No | - | RMC | VCL-ALK | RN | No |
| Sugawara et al. [30] | Cancer | 2012 | CS (2) | 36 (F) | No | - | uRCC | TPM3-ALK | RN | No |
| - | - | 2012 | - | 53 (F) | No | - | pRCC—ccRCC | EML4-ALK | RN | No |
| Sukov et al. [31] | Mod Pathol. | 2012 | CS (2) | 61 (M) | No | - | pRCC | NA | RN | No |
| - | - | 2012 | - | 59 (M) | No | - | pRCC | NA | RN | No |
| Lee C et al. [32] | Korean J Pathol. | 2013 | CR (1) | 44 (M) | No | - | RCC | NA | RN | No |
| Smith et al. [27] | Am J Surg Pathol. | 2014 | CR (1) | 6 (M) | No | - | RCC | VCL-ALK | RN | No |
| Ryan et al. [33] | Virchows Arch. | 2014 | CR (1) | 36 (M) | No | - | RCC | NA | RN | No |
| Kusano et al. [28] | Am J Surg Pathol. | 2016 | CS (2) | 33 (F) | Yes | Nodes | pRCC | STRN-ALK | RN | NA |
| - | - | 2016 | - | 38 (M) | Yes | Nodes—Liver | RCC | STRN-ALK | RN | Sunit. |
| Thorner et al. [34] | Pathol Res Pract. | 2016 | CR (1) | 12 (F) | Yes | Paraspinal mass—Soft tissue lesion | RCC | TPM3-ALK | RN | ALK-i |
| Cajaiba et al. [35] | Genes Chromosomes Cancer | 2016 | CR (1) | 16 (M) | NA | - | RCC | TPM3-ALK | NA | NA |
| - | - | 2016 | - | 6 (M) | NA | - | pRCC | VCL-ALK | NA | NA |
| - | - | 2016 | - | 16 (M) | NA | - | pRCC | VCL-ALK | NA | NA |
| - | - | 2016 | - | 6 (M) | NA | - | pRCC | VCL-ALK | NA | NA |
| - | - | 2016 | - | 16 (F) | NA | - | RCC | TPM3-ALK | NA | NA |
| - | - | 2016 | - | 14 (M) | NA | - | RCC | TPM3-ALK | NA | NA |
| Jeanneau et al. [36] | Pathol Res Pract. | 2016 | CR (1) | 40 (F) | No | - | RCC | VCL-ALK | RN | No |
| Cajaiba et al. [37] | Genes Chromosomes Cancer | 2016 | CR (1) | 16 (M) | No | - | pRCC | HOOK1-ALK | RN | NA |
| Yu et al. [38] | Histopathology | 2017 | CS (2) | 49 (M) | No | - | uRCC | TPM3-ALK | RN | No |
| - | - | 2017 | - | 52 (F) | No | - | pRCC | EML4-ALK | RN | No |
| Oyama et al. [39] | Pathol Int. | 2017 | CR (1) | 19 (F) | No | - | RCC | NA | RN | No |
| Bodokh et al. [40] | Cancer Genet. | 2018 | CR (1) | 55 (F) | No | - | RCC | TPM3-ALK | RN | No |
| Yang et al. [41] | Diagn Pathol. | 2019 | CR (1) | 58 (M) | No | - | RCC | TPM3-ALK | RN | No |
| Chen et al. [42] | Oncol Rep. | 2020 | CS (2) | 38 (M) | No | - | ccRCC | EML4-ALK | RN | No |
| - | - | 2020 | - | 59 (M) | NA | - | ccRCC | EML4-ALK | RN | NA |
| Woo et al. [43] | Yonsei Med J. | 2020 | CR (1) | 14 (M) | No | - | RCC | TPM3-ALK | RN | No |
| Hang et al. [44] | Virchows Archiv. | 2020 | CR (1) | 68 (F) | No | - | MA-like | PLEKHA7-ALK | PN | No |
| Zhu et al. [45] | Pathol Res Pract. | 2020 | CR (1) | 15 (F) | NA | - | pRCC | HOOK1-ALK | RN | NA |
| Kuroda et al. [46] | Mod Pathol. | 2020 | CS (12) | 33 (F) | No | - | uRCC | CLIP1-ALK | RN | No |
| - | - | 2020 | - | 51 (F) | No | - | MTSC-RCC | KIF5B-ALK | RN | No |
| - | - | 2020 | - | 25 (F) | No | - | MA-like | STRN-ALK | PN | No |
| - | - | 2020 | - | 48 (F) | No | - | RCC | STRN-ALK | PN | No |
| - | - | 2020 | - | 54 (M) | No | - | uRCC | TPM3-ALK | PN | No |
| - | - | 2020 | - | 56 (M) | No | - | uRCC | EML4-ALK | RN | No |
| - | - | 2020 | - | 42 (M) | No | - | RCC | STRN-ALK | RN | No |
| - | - | 2020 | - | 58 (F) | No | - | uRCC | TPM3-ALK | RN | No |
| - | - | 2020 | - | 43 (M) | No | - | RCC | KIAA1217-ALK | RN | No |
| - | - | 2020 | - | 40 (F) | No | - | RCC | EML4-ALK | PN | No |
| - | - | 2020 | - | 38 (M) | No | - | uRCC | TPM3-ALK | PN | No |
| - | - | 2020 | - | 68 (F) | No | - | MA-like | PLEKHA7-ALK | PN | No |
Abbreviations: ALK-i—ALK inhibitor; CR—case report; CS—case series; ChT—chemotherapy; ccRCC—clear cell renal cell carcinoma; CLIP1—cytoskeleton-associated proteins-Gly domain containing linker protein 1; EML—echinoderm microtubule-associated protein-like 4; F—female; HOOK1—hook microtubule tethering protein 1 kinase; KIF5B—kinesin family member 5B; M—male; MA-like—metanephric carcinoma-like; MTSC-RCC—mucinous tubular and spindle renal cell carcinoma; NA—not available; pRCC—papillary renal cell carcinoma; PN—partial nephrectomy; PLEKHA7—Pleckstrin homology domain containing A7; RN—radical nephrectomy; RCC—renal cell carcinoma; RMC—renal medullary carcinoma; Sunit.—sunitinib; STRN—striatin calmodulin-binding protein; TPM3—tropomyosin 3; uRCC—unclassified renal cell carcinoma; VCL—vinculin.
In addition, a few retrospective studies described ALK-RCC incidence in different populations. In 2012, Sukov et al. reported the results of the first single-institution retrospective study aiming to evaluate the frequency of ALK alterations in a large series of American adult patients affected by RCC. A cohort of 534 patients was analyzed, and a rearrangement of the ALK gene was detected in 2 patients (<1% of all patients), both affected by papillary RCC [31]. In the same year, Sugawara et al. described the results of a retrospective screening for ALK alterations of 355 renal tumors from Japanese patients, with the detection of two positive patients [30]. In 2013, Lee et al. reported the analysis’ results of a cohort of 829 resected RCC from Korean patients. Only one patient was diagnosed with ALK-RCC [32]. Three years later, Yu et al. reported data obtained through screening 477 resected RCC in the Chinese population, identifying only two patients with ALK alterations [40]. In 2019, Gorczynski et al. published the results of the analysis of 1019 renal tumors from Polish patients to evaluate ALK-RCC incidence, without any positive cases identified [47].
As a result, considering the growing attention to ALK-RCC and the well-recognized benefit of ALK-i in other ALK-positive tumors [48], we aimed to systematically revise the available literature to evaluate the activity of ALK-i in ALK-RCC patients. According to the inclusion criteria of the systematic review, only three publications were included that reported a single-case description of clinical and pathological features of adult ALK-RCC patients treated with ALK-inhibitors. Firstly, in 2018 Pal et al. showed the therapeutic outcomes of three advanced renal cancer patients treated with alectinib, a second-generation ALK-i [10]. All patients received multiple lines of treatment with different anticancer agents, including multi-target tyrosine kinase inhibitors (TKI) and immune checkpoint inhibitors (ICI). After being detected with ALK-EML4 translocations on ctDNA through a genomic profiling test, they started the treatment with alectinib. All patients achieved a radiological partial response with a concurrent improvement of performance status [10]. Secondly, in 2020, Zhou et al. reported the case of a young woman who had a progressive disease with pulmonary metastases after nephrectomy for a localized RCC [11]. The patient started a first-line treatment with sunitinib. After detecting an immunohistochemical ALK positivity, confirmed by a FISH test, the patient switched to a systemic therapy with crizotinib, achieving a radiological stable disease [11]. Thirdly, in 2021, Varchetta et al. described the case of a patient with relapsed renal cancer who received multiple lines of treatment, except for ICI due to a pre-existing severe rheumatic disease. After detecting an ALK rearrangement on neoplastic tissue, the patient started alectinib, achieving a radiological partial response [12]. Lastly, Thorner et al. reported the case of a twelve-year-old patient with a relapsed ALK-RCC who received an unspecified ALK-i for more than one year. The patient was still continuing the treatment at the time of publication [34]. However, the publication was not included in the review due to the pediatric age of the patient.
Despite the small number of publications available on ALK-RCC treated with ALK-i, several issues deserve to be discussed. Firstly, all ALK-RCC patients treated with ALK-i achieved a radiological response associated with improved performance status, although they all received previous systemic therapies [10,11,12]. Considering that most of the anticancer agents used today for the treatment of metastatic RCC are either targeted therapies directed at molecules involved in angiogenesis or ICI [49], promising results in terms of activity for ALK-i could open the way to a new class of anticancer agents for the treatment of patients affected by metastatic RCC. Four patients were treated with alectinib [10,12], a second-generation ALK-i, while only one patient received crizotinib [11]. In addition, considering the recent data on the efficacy of lorlatinib even in controlling the distant metastases localized in the central nervous system [50], it would have been interesting to evaluate its activity in ALK-RCC patients either after progression on a previous ALK-i or as a first-line treatment. In this direction, further promising results were published by Tao et al. [51]. They described the case report of an ALK-RCC patient who relapsed after complete resection of the tumor and, therefore, received first-line treatment with entrectinib, a selective TKI towards neurotrophic tyrosine receptor kinase (NTRK), ROS1, and ALK fusion. The patient maintained an excellent performance status throughout the treatment with a PFS of nineteen months [51].
Secondly, further questions are open on the procedures used to detect ALK alterations and their timing, considering the promising results provided by ALK-i. According to the International Society of Urological Pathology (ISUP), immunohistochemical screening with ALK antibody and the subsequent confirmation by fluorescence in situ hybridization (FISH) or sequencing methods is generally recommended [1]. In the case report published by Zhou et al., ALK rearrangement was detected on neoplastic tissue obtained by a biopsy of a lung metastasis through a FISH test performed after a positive result at the immunohistochemical analysis [11]. In the case report published by Varchetta et al., the ALK alteration was also detected on distant metastases through a genomic profiling test [12]. In contrast, in the three cases reported by Pal et al., the ALK-EML4 translocation was detected in ctDNA through a genomic profiling test, which showed the presence of ALK alterations associated with other mutations, not eligible for other targeted therapies [10]. ALK alterations in all these patients were not detected in specimens from primary RCC but only from distant metastases or ctDNA [10]. In this scenario, the available data on the concordance of ALK rearrangements between the primary lung tumor and metastases are encouraging. Indeed, in 2017 Hou et al. published a single-center study aimed to investigate the concordance of ALK rearrangements between lung adenocarcinoma and the paired metastatic lymph nodes [52]. The results showed a concordance rate of 98%, concluding that specimens provided from the primary tumor or the lymph-node metastases were equally suitable for ALK rearrangements’ detection [52]. These results were confirmed by a study published in the same year by Ma et al., where a high concordance of ALK status was found between the primary tumor and corresponding lymph node metastases [53]. Furthermore, considering that approximately 30% of tumor biopsy samples may be insufficient to perform ALK characterization, promising data are available on the role of circulating tumor cells as a surrogate to tissue for the detection of ALK alterations [54].
Lastly, these emerging data confirm that ALK is a compelling therapeutic target, as demonstrated by its role as an oncogenic driver in several tumor types of different lineages, including RCC. ALK fusions are extraordinarily versatile oncoproteins that can be targeted with several anticancer agents with a well-recognized efficacy [55]. Furthermore, in the “precision medicine” era where tumor-agnostic therapies represent a new revolutionary approach to cancer treatment [56], ALK-i are earning a potential role in the agnostic-setting of ALK-positive tumors. In this direction, it will be essential to know the final results of two ongoing trials, the CREATE trial [57] and the Alpha-T trial [58]. The former is a phase 2 trial designed to evaluate the antitumor activity of crizotinib across predefined tumor types in patients whose tumors are harboring specific alterations in ALK and/or MET [57]. The latter is a phase 2 trial aimed to evaluate the efficacy and safety of alectinib in participants with ALK-positive locally advanced or metastatic solid tumors other than lung cancer [58].
4.1. Future Directions
In the last two decades, the therapeutic scenario of metastatic RCC has been revolutionized, as evidenced by the dramatic improvement of the median survival of RCC patients from less than one year in the 1990s to over four years in the most recent trials [59]. The treatment landscape has evolved from interleukin 2 and interferon-alfa to targeted therapies such as vascular endothelial growth factor receptor inhibitors, mammalian target of rapamycin inhibitors, and ICI [49]. Nevertheless, a considerable effort is still necessary to transform the evolving knowledge in identifying novel RCC entities into more personalized treatments. Indeed, a greater understanding of RCC underlying biological processes is essential to develop future therapeutic agents [60]. For example, the detection of novel fusion genes involved in the development, growth, and survival of cancer cells could lead to the identification of new potential druggable targets for “precision medicine” approaches [61].
In this direction, initial evidence suggests that ALK-RCC patients might benefit from the treatment with ALK-i [60]. Nevertheless, it will be essential to evaluate the activity of ALK-i firstly in large, multi-institutional clinical trials for pretreated ALK-RCC patients. Once the activity of ALK-i has been demonstrated in pretreated patients, it would be of great clinical interest to test their efficacy against the available treatments in this subtype of patients. Indeed, the presence of ALK alterations could allow them to benefit from an evolving class of anticancer agents that have already demonstrated their efficacy in other tumor types.
In parallel, considering the potential efficacy of ALK-i in this RCC subtype, further data are necessary to describe the clinical and histological characteristics of ALK-RCC patients clearly. This would be important to select those patients who can benefit from molecular testing for ALK, in light of the cost and time-consuming procedures to screen all RCC patients at the diagnosis. According to the aforementioned larger case series, PRCC patients are more frequently carriers of ALK alterations than clear-cell RCC patients [30,31,32,40,47]. In addition, ALK testing represents a way to better classify some patients affected by RCC with unclassified histology (uRCC) that have no standard therapy. Indeed, the screening for ALK alterations in uRCC patients would be essential to allow these patients to be treated with a personalized treatment [62]. Lastly, the available data highlight heterogeneity in molecular testing for ALK alterations that could represent one of the explanations for the differences in ALK-RCC rates provided by the larger series published in recent years [62]. In this light, a consensus paper would be useful to provide recommendations for a test algorithm for renal cancer and the quality of the respective test approaches, like the one released regarding ALK testing in NSCLC [63].
4.2. Limitations
The main limitation of this systematic review lies in the extraction of data from case reports and case series. These two types of publications are at an increased risk of bias due to their intrinsic nature [9]. As a result, we decided to include case reports and case series in which a single case description was available.
4.3. Conclusions
Although ALK-RCC is currently considered an “emerging or provisional” entity by the last WHO classification [2], several studies have been published in recent years assessing the clinical presentation and histological characteristics of ALK-RCC patients. In contrast, only a few publications have evaluated the activity of ALK-i in this subgroup of patients. By systematically revising the available literature, we demonstrated for the first time, to our knowledge, a favorable activity of first- and second-generation ALK-i in pretreated ALK-RCC patients in terms of either radiological response or performance status improvement. We hope that the present work will prompt the creation of large, multi-institutional clinical trials to confirm these promising early data to allow this subgroup of patients to benefit from a rapidly evolving class of targeted therapy that has already demonstrated its efficacy in other tumors.
5. Other Information
5.1. Registration and Protocol
The protocol was designed a priori and approved by all the authors. In addition, it was registered on the open science framework website https://osf.io/rx9hj/ (accessed on 23 February 2021).
5.2. Support
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
5.3. Competing Interests
The authors report no declarations of interest.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms23073995/s1.
Author Contributions
Conceptualization, G.M.I. and F.T.; methodology, G.M.I. and S.R.; data curation, S.R. and F.T.; writing—original draft preparation, G.M.I. and S.S.; writing—review and editing, S.R., F.T. and M.R.; visualization, S.S.; supervision, M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williamson S.R., Gill A.J., Argani P., Chen Y.-B., Egevad L., Kristiansen G., Grignon D.J., Hes O. Report from the International Society of Urological Pathology (ISUP) Consultation Conference on Molecular Pathology of Urogenital Cancers: III: Molecular Pathology of Kidney Cancer. Am. J. Surg. Pathol. 2020;44:e47–e65. doi: 10.1097/PAS.0000000000001476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moch H., Cubilla A.L., Humphrey P.A., Reuter V.E., Ulbright T.M. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur. Urol. 2016;70:93–105. doi: 10.1016/j.eururo.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 3.Gorczyński A., Prełowska M., Adam P., Czapiewski P., Biernat W. ALK-Positive Cancer: Still a Growing Entity. Future Oncol. 2014;10:305–321. doi: 10.2217/fon.13.184. [DOI] [PubMed] [Google Scholar]
- 4.Mano H. ALKoma: A Cancer Subtype with a Shared Target. Cancer Discov. 2012;2:495–502. doi: 10.1158/2159-8290.CD-12-0009. [DOI] [PubMed] [Google Scholar]
- 5.Kuroda N., Sugawara E., Kusano H., Yuba Y., Yorita K., Takeuchi K. A Review of ALK-Rearranged Renal Cell Carcinomas with a Focus on Clinical and Pathobiological Aspects. Pol. J. Pathol. 2018;69:109–113. doi: 10.5114/pjp.2018.76693. [DOI] [PubMed] [Google Scholar]
- 6.Trpkov K., Williamson S.R., Gill A.J., Adeniran A.J., Agaimy A., Alaghehbandan R., Amin M.B., Argani P., Chen Y.-B., Cheng L., et al. Novel, Emerging and Provisional Renal Entities: The Genitourinary Pathology Society (GUPS) Update on Renal Neoplasia. Mod. Pathol. 2021;34:1167–1184. doi: 10.1038/s41379-021-00737-6. [DOI] [PubMed] [Google Scholar]
- 7.Holla V.R., Elamin Y.Y., Bailey A.M., Johnson A.M., Litzenburger B.C., Khotskaya Y.B., Sanchez N.S., Zeng J., Shufean M.A., Shaw K.R., et al. ALK: A Tyrosine Kinase Target for Cancer Therapy. Cold Spring Harb Mol. Case Stud. 2017;3:a001115. doi: 10.1101/mcs.a001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PRISMA—Transparent Reporting of Systematic Reviews and Meta-Analyses. [(accessed on 16 February 2022)]. Available online: http://prisma-statement.org/
- 9.Murad M.H., Sultan S., Haffar S., Bazerbachi F. Methodological Quality and Synthesis of Case Series and Case Reports. BMJ Evid. Based Med. 2018;23:60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pal S.K., Bergerot P., Dizman N., Bergerot C., Adashek J., Madison R., Chung J.H., Ali S.M., Jones J.O., Salgia R. Responses to Alectinib in ALK-Rearranged Papillary Renal Cell Carcinoma. Eur. Urol. 2018;74:124–128. doi: 10.1016/j.eururo.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 11.Zhou S., Sun G., Wang J., Zhang H. Anaplastic Lymphoma Kinase (ALK) Rearrangement in Adult Renal Cell Carcinoma with Lung Metastasis: A Case Report and Literature Review. Transl. Urol. 2020;9:2855–2861. doi: 10.21037/tau-20-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varchetta V., Campanella C., Rossi M., Verzaro R., Vitale M., Soda G., Mancuso A. Identification of Anaplastic Lymphoma Kinase Fusion in Clear Cell Renal Carcinoma (ALK-TRCC): A Precision Oncology Medicine Case Report. Recenti. Prog. Med. 2021;112:14e–15e. doi: 10.1701/3525.35133. [DOI] [PubMed] [Google Scholar]
- 13.Morris S.W., Kirstein M.N., Valentine M.B., Dittmer K.G., Shapiro D.N., Saltman D.L., Look A.T. Fusion of a Kinase Gene, ALK, to a Nucleolar Protein Gene, NPM, in Non-Hodgkin’s Lymphoma. Science. 1994;263:1281–1284. doi: 10.1126/science.8122112. [DOI] [PubMed] [Google Scholar]
- 14.Bai R.Y., Ouyang T., Miething C., Morris S.W., Peschel C., Duyster J. Nucleophosmin-Anaplastic Lymphoma Kinase Associated with Anaplastic Large-Cell Lymphoma Activates the Phosphatidylinositol 3-Kinase/Akt Antiapoptotic Signaling Pathway. Blood. 2000;96:4319–4327. doi: 10.1182/blood.V96.13.4319. [DOI] [PubMed] [Google Scholar]
- 15.Camidge D.R., Doebele R.C. Treating ALK-Positive Lung Cancer—Early Successes and Future Challenges. Nat. Rev. Clin. Oncol. 2012;9:268–277. doi: 10.1038/nrclinonc.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gristina V., La Mantia M., Iacono F., Galvano A., Russo A., Bazan V. The Emerging Therapeutic Landscape of ALK Inhibitors in Non-Small Cell Lung Cancer. Pharmaceuticals. 2020;13:474. doi: 10.3390/ph13120474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NCCN Clinical Practice Guidelines in Oncology—Non-Small Cell Lung Cancer. [(accessed on 16 February 2022)]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
- 18.Ciamporcero E., Miles K.M., Adelaiye R., Ramakrishnan S., Shen L., Ku S., Pizzimenti S., Sennino B., Barrera G., Pili R. Combination Strategy Targeting VEGF and HGF/c-Met in Human Renal Cell Carcinoma Models. Mol. Cancer Ther. 2015;14:101–110. doi: 10.1158/1535-7163.MCT-14-0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michaelson M.D., Gupta S., Agarwal N., Szmulewitz R., Powles T., Pili R., Bruce J.Y., Vaishampayan U., Larkin J., Rosbrook B., et al. A Phase Ib Study of Axitinib in Combination with Crizotinib in Patients with Metastatic Renal Cell Cancer or Other Advanced Solid Tumors. Oncologist. 2019;24:1151–e817. doi: 10.1634/theoncologist.2018-0749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Albiges L., Guegan J., Le Formal A., Verkarre V., Rioux-Leclercq N., Sibony M., Bernhard J.-C., Camparo P., Merabet Z., Molinie V., et al. MET Is a Potential Target across All Papillary Renal Cell Carcinomas: Result from a Large Molecular Study of PRCC with CGH Array and Matching Gene Expression Array. Clin. Cancer Res. 2014;20:3411–3421. doi: 10.1158/1078-0432.CCR-13-2173. [DOI] [PubMed] [Google Scholar]
- 21.Schöffski P., Wozniak A., Escudier B., Rutkowski P., Anthoney A., Bauer S., Sufliarsky J., van Herpen C., Lindner L.H., Grünwald V., et al. Crizotinib Achieves Long-Lasting Disease Control in Advanced Papillary Renal-Cell Carcinoma Type 1 Patients with MET Mutations or Amplification. EORTC 90101 CREATE Trial. Eur. J. Cancer. 2017;87:147–163. doi: 10.1016/j.ejca.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Pal S.K., Tangen C., Thompson I.M., Balzer-Haas N., George D.J., Heng D.Y.C., Shuch B., Stein M., Tretiakova M., Humphrey P., et al. A Comparison of Sunitinib with Cabozantinib, Crizotinib, and Savolitinib for Treatment of Advanced Papillary Renal Cell Carcinoma: A Randomised, Open-Label, Phase 2 Trial. Lancet. 2021;397:695–703. doi: 10.1016/S0140-6736(21)00152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Debelenko L.V., Raimondi S.C., Daw N., Shivakumar B.R., Huang D., Nelson M., Bridge J.A. Renal Cell Carcinoma with Novel VCL-ALK Fusion: New Representative of ALK-Associated Tumor Spectrum. Mod. Pathol. 2011;24:430–442. doi: 10.1038/modpathol.2010.213. [DOI] [PubMed] [Google Scholar]
- 24.Argani P. Translocation Carcinomas of the Kidney. Genes Chromosomes Cancer. 2022;61:219–227. doi: 10.1002/gcc.23007. [DOI] [PubMed] [Google Scholar]
- 25.Cimadamore A., Cheng L., Scarpelli M., Massari F., Mollica V., Santoni M., Lopez-Beltran A., Montironi R., Moch H. Towards a New WHO Classification of Renal Cell Tumor: What the Clinician Needs to Know-a Narrative Review. Transl. Androl. Urol. 2021;10:1506–1520. doi: 10.21037/tau-20-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Siadat F., Trpkov K. ESC, ALK, HOT and LOT: Three Letter Acronyms of Emerging Renal Entities Knocking on the Door of the WHO Classification. Cancers. 2020;12:168. doi: 10.3390/cancers12010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith N.E., Deyrup A.T., Mariño-Enriquez A., Fletcher J.A., Bridge J.A., Illei P.B., Netto G.J., Argani P. VCL-ALK Renal Cell Carcinoma in Children with Sickle-Cell Trait: The Eighth Sickle-Cell Nephropathy? Am. J. Surg. Pathol. 2014;38:858–863. doi: 10.1097/PAS.0000000000000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kusano H., Togashi Y., Akiba J., Moriya F., Baba K., Matsuzaki N., Yuba Y., Shiraishi Y., Kanamaru H., Kuroda N., et al. Two Cases of Renal Cell Carcinoma Harboring a Novel STRN-ALK Fusion Gene. Am. J. Surg. Pathol. 2016;40:761–769. doi: 10.1097/PAS.0000000000000610. [DOI] [PubMed] [Google Scholar]
- 29.Mariño-Enríquez A., Ou W.-B., Weldon C.B., Fletcher J.A., Pérez-Atayde A.R. ALK Rearrangement in Sickle Cell Trait-Associated Renal Medullary Carcinoma. Genes Chromosomes Cancer. 2011;50:146–153. doi: 10.1002/gcc.20839. [DOI] [PubMed] [Google Scholar]
- 30.Sugawara E., Togashi Y., Kuroda N., Sakata S., Hatano S., Asaka R., Yuasa T., Yonese J., Kitagawa M., Mano H., et al. Identification of Anaplastic Lymphoma Kinase Fusions in Renal Cancer: Large-Scale Immunohistochemical Screening by the Intercalated Antibody-Enhanced Polymer Method. Cancer. 2012;118:4427–4436. doi: 10.1002/cncr.27391. [DOI] [PubMed] [Google Scholar]
- 31.Sukov W.R., Hodge J.C., Lohse C.M., Akre M.K., Leibovich B.C., Thompson R.H., Cheville J.C. ALK Alterations in Adult Renal Cell Carcinoma: Frequency, Clinicopathologic Features and Outcome in a Large Series of Consecutively Treated Patients. Mod. Pathol. 2012;25:1516–1525. doi: 10.1038/modpathol.2012.107. [DOI] [PubMed] [Google Scholar]
- 32.Lee C., Park J.W., Suh J.H., Nam K.H., Moon K.C. ALK-Positive Renal Cell Carcinoma in a Large Series of Consecutively Resected Korean Renal Cell Carcinoma Patients. Korean J. Pathol. 2013;47:452–457. doi: 10.4132/KoreanJPathol.2013.47.5.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ryan C., Mayer N., Cunningham J., Hislop G., Pratt N., Fleming S. Increased ALK1 Copy Number and Renal Cell Carcinoma-a Case Report. Virchows Arch. 2014;464:241–245. doi: 10.1007/s00428-013-1520-3. [DOI] [PubMed] [Google Scholar]
- 34.Thorner P.S., Shago M., Marrano P., Shaikh F., Somers G.R. TFE3-Positive Renal Cell Carcinomas Are Not Always Xp11 Translocation Carcinomas: Report of a Case with a TPM3-ALK Translocation. Pathol. Res. Pract. 2016;212:937–942. doi: 10.1016/j.prp.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Cajaiba M.M., Jennings L.J., Rohan S.M., Perez-Atayde A.R., Marino-Enriquez A., Fletcher J.A., Geller J.I., Leuer K.M.C., Bridge J.A., Perlman E.J. ALK-Rearranged Renal Cell Carcinomas in Children. Genes Chromosomes Cancer. 2016;55:442–451. doi: 10.1002/gcc.22346. [DOI] [PubMed] [Google Scholar]
- 36.Jeanneau M., Gregoire V., Desplechain C., Escande F., Tica D.P., Aubert S., Leroy X. ALK Rearrangements-Associated Renal Cell Carcinoma (RCC) with Unique Pathological Features in an Adult. Pathol. Res. Pract. 2016;212:1064–1066. doi: 10.1016/j.prp.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 37.Cajaiba M.M., Jennings L.J., George D., Perlman E.J. Expanding the Spectrum of ALK-Rearranged Renal Cell Carcinomas in Children: Identification of a Novel HOOK1-ALK Fusion Transcript. Genes Chromosomes Cancer. 2016;55:814–817. doi: 10.1002/gcc.22382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu W., Wang Y., Jiang Y., Zhang W., Li Y. Genetic Analysis and Clinicopathological Features of ALK-Rearranged Renal Cell Carcinoma in a Large Series of Resected Chinese Renal Cell Carcinoma Patients and Literature Review. Histopathology. 2017;71:53–62. doi: 10.1111/his.13185. [DOI] [PubMed] [Google Scholar]
- 39.Oyama Y., Nishida H., Kusaba T., Kadowaki H., Arakane M., Daa T., Watanabe D., Akita Y., Sato F., Mimata H., et al. A Case of Anaplastic Lymphoma Kinase-Positive Renal Cell Carcinoma Coincident with Hodgkin Lymphoma. Pathol. Int. 2017;67:626–631. doi: 10.1111/pin.12592. [DOI] [PubMed] [Google Scholar]
- 40.Bodokh Y., Ambrosetti D., Kubiniek V., Tibi B., Durand M., Amiel J., Pertuit M., Barlier A., Pedeutour F. ALK-TPM3 Rearrangement in Adult Renal Cell Carcinoma: Report of a New Case Showing Loss of Chromosome 3 and Literature Review. Cancer Genet. 2018;221:31–37. doi: 10.1016/j.cancergen.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 41.Yang J., Dong L., Du H., Li X.-B., Liang Y.-X., Liu G.-R. ALK-TPM3 Rearrangement in Adult Renal Cell Carcinoma: A Case Report and Literature Review. Diagn. Pathol. 2019;14:112. doi: 10.1186/s13000-019-0879-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen W., Li W., Bai B., Wei H. Identification of Anaplastic Lymphoma Kinase Fusions in Clear Cell Renal Cell Carcinoma. Oncol. Rep. 2020;43:817–826. doi: 10.3892/or.2020.7462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Woo C.G., Yun S.J., Son S.M., Lim Y.H., Lee O.J. Characteristics of Renal Cell Carcinoma Harboring TPM3-ALK Fusion. Yonsei Med. J. 2020;61:262–266. doi: 10.3349/ymj.2020.61.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hang J.-F., Chung H.-J., Pan C.-C. ALK-Rearranged Renal Cell Carcinoma with a Novel PLEKHA7-ALK Translocation and Metanephric Adenoma-like Morphology. Virchows Arch. 2020;476:921–929. doi: 10.1007/s00428-020-02752-5. [DOI] [PubMed] [Google Scholar]
- 45.Zhu Y., Liu N., Guo W., Pu X., Guo H., Gan W., Li D. ALK Rearrangement in TFE3-Positive Renal Cell Carcinoma: Alternative Diagnostic Option to Exclude Xp11.2 Translocation Carcinoma. Pathol. Res. Pract. 2020;216:153286. doi: 10.1016/j.prp.2020.153286. [DOI] [PubMed] [Google Scholar]
- 46.Kuroda N., Trpkov K., Gao Y., Tretiakova M., Liu Y.J., Ulamec M., Takeuchi K., Agaimy A., Przybycin C., Magi-Galluzzi C., et al. ALK Rearranged Renal Cell Carcinoma (ALK-RCC): A Multi-Institutional Study of Twelve Cases with Identification of Novel Partner Genes CLIP1, KIF5B and KIAA1217. Mod. Pathol. 2020;33:2564–2579. doi: 10.1038/s41379-020-0578-0. [DOI] [PubMed] [Google Scholar]
- 47.Gorczynski A., Czapiewski P., Korwat A., Budynko L., Prelowska M., Okon K., Biernat W. ALK-Rearranged Renal Cell Carcinomas in Polish Population. Pathol. Res. Pract. 2019;215:152669. doi: 10.1016/j.prp.2019.152669. [DOI] [PubMed] [Google Scholar]
- 48.Ross J.S., Ali S.M., Fasan O., Block J., Pal S., Elvin J.A., Schrock A.B., Suh J., Nozad S., Kim S., et al. ALK Fusions in a Wide Variety of Tumor Types Respond to Anti-ALK Targeted Therapy. Oncologist. 2017;22:1444–1450. doi: 10.1634/theoncologist.2016-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tran J., Ornstein M.C. Clinical Review on the Management of Metastatic Renal Cell Carcinoma. JCO Oncol. Pract. 2021;18:187–196. doi: 10.1200/OP.21.00419. [DOI] [PubMed] [Google Scholar]
- 50.Felip E., Shaw A.T., Bearz A., Camidge D.R., Solomon B.J., Bauman J.R., Bauer T.M., Peters S., Toffalorio F., Abbattista A., et al. Intracranial and Extracranial Efficacy of Lorlatinib in Patients with ALK-Positive Non-Small-Cell Lung Cancer Previously Treated with Second-Generation ALK TKIs. Ann. Oncol. 2021;32:620–630. doi: 10.1016/j.annonc.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 51.Tao J.J., Wei G., Patel R., Fagan P., Hao X., Bridge J.A., Arcila M.E., Al-Ahmadie H., Lee C.-H., Li G., et al. ALK Fusions in Renal Cell Carcinoma: Response to Entrectinib. JCO Precis. Oncol. 2018;2:1–8. doi: 10.1200/PO.18.00185. [DOI] [PubMed] [Google Scholar]
- 52.Hou L., Ren S., Su B., Zhang L., Wu W., Zhang W., Dong Z., Huang Y., Wu C., Chen G. High Concordance of ALK Rearrangement between Primary Tumor and Paired Metastatic Lymph Node in Patients with Lung Adenocarcinoma. J. Thorac. Dis. 2016;8:1103–1111. doi: 10.21037/jtd.2016.03.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ma W., Guo L., Shan L., Liu X., Lyu N., Ying J. Homogeneity and High Concordance of ALK Translocation in Primary Lung Adenocarcinoma and Paired Lymph Node Metastasis. Sci. Rep. 2017;7:10961. doi: 10.1038/s41598-017-11453-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ilié M., Mazières J., Chamorey E., Heeke S., Benzaquen J., Thamphya B., Boutros J., Tiotiu A., Fayada J., Cadranel J., et al. Prospective Multicenter Validation of the Detection of ALK Rearrangements of Circulating Tumor Cells for Noninvasive Longitudinal Management of Patients with Advanced NSCLC. J. Thorac. Oncol. 2021;16:807–816. doi: 10.1016/j.jtho.2021.01.1617. [DOI] [PubMed] [Google Scholar]
- 55.Cao Z., Gao Q., Fu M., Ni N., Pei Y., Ou W.-B. Anaplastic Lymphoma Kinase Fusions: Roles in Cancer and Therapeutic Perspectives. Oncol. Lett. 2019;17:2020–2030. doi: 10.3892/ol.2018.9856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Looney A.-M., Nawaz K., Webster R.M. Tumour-Agnostic Therapies. Nat. Rev. Drug Discov. 2020;19:383–384. doi: 10.1038/d41573-020-00015-1. [DOI] [PubMed] [Google Scholar]
- 57.CREATE: Cross-tumoral Phase 2 with Crizotinib (CREATE) [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01524926?cond=ALK+AND+renal+cancer&draw=2&rank=2.
- 58.A Home-Based Approach Study to Evaluate the Efficacy and Safety of Alectinib in Locally-Advanced or Metastatic ALK-Positive Solid Tumors (ALpha-T) [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04644315.
- 59.Albiges L., Tannir N.M., Burotto M., McDermott D., Plimack E.R., Barthélémy P., Porta C., Powles T., Donskov F., George S., et al. Nivolumab plus Ipilimumab versus Sunitinib for First-Line Treatment of Advanced Renal Cell Carcinoma: Extended 4-Year Follow-up of the Phase III CheckMate 214 Trial. ESMO Open. 2020;5:e001079. doi: 10.1136/esmoopen-2020-001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barthélémy P., Rioux-Leclercq N., Thibault C., Saldana C., Borchiellini D., Chevreau C., Desmoulins I., Gobert A., Hilgers W., Khalil A., et al. Non-Clear Cell Renal Carcinomas: Review of New Molecular Insights and Recent Clinical Data. Cancer Treat. Rev. 2021;97:102191. doi: 10.1016/j.ctrv.2021.102191. [DOI] [PubMed] [Google Scholar]
- 61.Pederzoli F., Bandini M., Marandino L., Ali S.M., Madison R., Chung J., Ross J.S., Necchi A. Targetable Gene Fusions and Aberrations in Genitourinary Oncology. Nat. Rev. Urol. 2020;17:613–625. doi: 10.1038/s41585-020-00379-4. [DOI] [PubMed] [Google Scholar]
- 62.Chen Y.-B., Xu J., Skanderup A.J., Dong Y., Brannon A.R., Wang L., Won H.H., Wang P.I., Nanjangud G.J., Jungbluth A.A., et al. Molecular Analysis of Aggressive Renal Cell Carcinoma with Unclassified Histology Reveals Distinct Subsets. Nat. Commun. 2016;7:13131. doi: 10.1038/ncomms13131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Von Laffert M., Schirmacher P., Warth A., Weichert W., Büttner R., Huber R.M., Wolf J., Griesinger F., Dietel M., Grohé C. ALK-Testing in Non-Small Cell Lung Cancer (NSCLC): Immunohistochemistry (IHC) and/or Fluorescence in-Situ Hybridisation (FISH)?: Statement of the Germany Society for Pathology (DGP) and the Working Group Thoracic Oncology (AIO) of the German Cancer Society e.V. (Stellungnahme Der Deutschen Gesellschaft Für Pathologie Und Der AG Thorakale Onkologie Der Arbeitsgemeinschaft Onkologie/Deutsche Krebsgesellschaft e.V.) Lung Cancer. 2017;103:1–5. doi: 10.1016/j.lungcan.2016.11.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.