Abstract
Resveratrol is a polyphenol that has been shown to possess many applications in different fields of medicine. This systematic review has drawn attention to the axis between resveratrol and human microbiota, which plays a key role in maintaining an adequate immune response that can lead to different diseases when compromised. Resveratrol can also be an asset in new technologies, such as gene therapy. PubMed, Cochrane Library, Scopus, Web of Science, and Google Scholar were searched to find papers that matched our topic dating from 1 January 2017 up to 18 January 2022, with English-language restriction using the following Boolean keywords: (“resveratrol” AND “microbio*”). Eighteen studies were included as relevant papers matching the purpose of our investigation. Immune response, prevention of thrombotic complications, microbiota, gene therapy, and bone regeneration were retrieved as the main topics. The analyzed studies mostly involved resveratrol supplementation and its effects on human microbiota by trials in vitro, in vivo, and ex vivo. The beneficial activity of resveratrol is evident by analyzing the changes in the host’s genetic expression and the gastrointestinal microbial community with its administration. The possibility of identifying individual microbial families may allow to tailor therapeutic plans with targeted polyphenolic diets when associated with microbial dysbiosis, such as inflammatory diseases of the gastrointestinal tract, degenerative diseases, tumors, obesity, diabetes, bone tissue regeneration, and metabolic syndrome.
Keywords: resveratrol, microbiota, microbiome, nutrition, bone regeneration, immune response, resveratrol supplementation, genic therapy, dentistry, thrombosis
1. Introduction
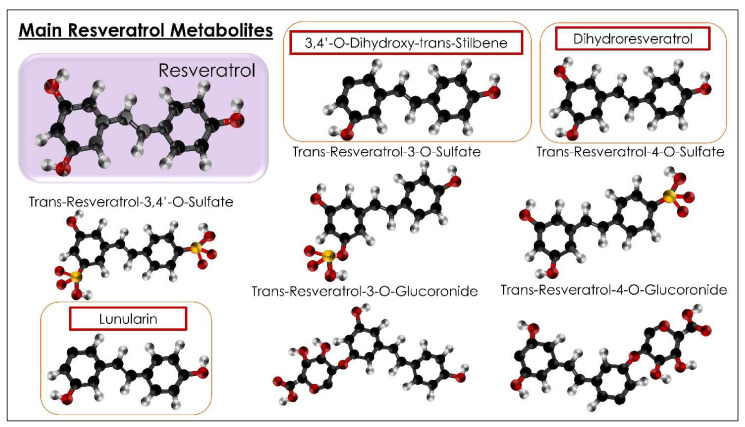
Nutrition is one of the most determinative factors of health [1]. Egyptian medicine, one of best-known of the ancient forms of medicine, held nutrition in high account for a purpose: the Egyptian diet was measured and balanced and was considered an art for health and healing. The basis of the diet was: flax, barley, spelt, as well as fruit and vegetables, among which red grapes were especially consumed. Above all, red grapes were widespread in the wealthy classes, who recognized their health and curative benefits [2]. Nutrition’s burden in pathologies, even if not exclusive, is costly for patients in terms of health, expectations, and quality of life. Some aliments (fruits, vegetables) have specific qualities (antioxidants, diuretic, hypoglycemic) in the nutrition sector. These can represent significant effects that implement and develop a high level of human health. One of these is resveratrol (RSV), which is, interestingly, considered as the “molecule of youth” [3,4]. RSV (C14H12O3: 3, 5, 4′-trihydroxy-trans-stilbene) is a powerful natural polyphenol of the phytoalexin family. RSV is present in the barks of some plants, seeds, nuts, peanuts, flowers, and fruits (fermented grapes, mulberry, red wine, blueberries) and in a particular plant called “Japan’s polygon” (Polygonum cuspidatum) [5]. It is found in the form of trans isomer and cis-resveratrol. The first is more stable and has higher bioactivity compared to the second one (six times more potent than cis). Trans-RSV remained stable for several months (protected from the lights and excepted in high pH buffers) [6,7,8]. The higher bioavailability of trans-RSV increases its antioxidant, anti-inflammatory, vasoprotective, anti-mutagenic, anti-proliferative, and anti-carcinogenic actions, making it more effective and longer-lasting [9]. RSV is not soluble in water; however, it is soluble in substances such as ethanol and dimethyl sulfoxide. RSV is known for its anti-inflammatory, antifungal, antioxidant, antithrombotic, anticoagulant, anticancer, and antiviral properties (MERS-CoV, pseudo-rabies, Zika, influenza, Dengue, COVID-19) [10,11,12,13,14,15]. RSV is a polyphenolic sirtuin activator (SIRT-1) that initiates the process of deacetylation of peroxisome proliferator-activated receptor-γ coactivator (PGC-1α), which activates protein phosphatase (PPRy). PPRY takes part in the genomic transcription of those genes that favor mitochondrial metabolism [5,7]. This natural polyphenol takes part in multiple metabolic processes by activating SITR1, which is present in many tissues, such as muscles, pancreas, and adipose tissues [16]. Microbiota (MB) and microbiome (MM) have a substantial difference in meaning (Figure 1) [16,17]. MB indicates all the microorganisms (bacteria, fungi, archaea, protozoa, and viruses) that live and colonize a specific environment in symbiosis, in physiological or pathological conditions. Recent studies estimate the presence of about 38,000 billion bacteria in the human body, mainly living in the intestinal tract. The dominant families (phyla) are Firmicutes and Bacteroidetes [18,19]. The MM instead indicates the totality of the genetic heritage present in the microbiota and the ability to manifest them [17]. The microbiome study has advanced with metagenomics, which is based on the isolation and genomic sequencing of the 16S rRNA gene, an RNA gene specific to each bacterium responsible for ribosomes production. Identifying these genes means tracing a single bacterial species through a computational analysis of microorganisms, which is also helpful for studying some pathologies dominated by specific families of microbial communities [18,20]. In particular, metagenomics allows us to study the interaction methods of various microorganisms with the environment (microbial ecology) and their precise role in the community [19]. The genome of microbial communities can be studied through a targeted technology: not only sequencing (metagenomics) but also through the transcriptome (transcriptomics), which quantifies the whole RNA that is transcribed by a genome (i.e., microarray technique), and the proteome (proteomics), which studies the whole set of proteins synthesized by mRNA (electrophoretic techniques, chromatographic techniques, mass spectrometry) [21,22]. The metabolome (metabolomics) is another innovative method of studying MM and MB. However, it is not considered an analytical method capable of tracing all the metabolites of a biological microorganism and interacting in metabolic processes [23,24,25]. More and more scientific evidence demonstrates how MB affects metabolic activity and the inflammatory state. MB is recognized as beneficial in compromised psychological states due to its influence on the hypothalamic–pituitary–adrenal axis and the serotoninergic system [23,26,27,28]. The human MB would also intervene in the development of the immune system in the first years of life and in the regulation of the adult immune system [24,29,30]. Eubiosis is mentioned in conditions of equilibrium, dysbiosis in the opposite case. The administration of antibiotics generates alterations in the MB and MM [17,20]. The onset of metabolic, cardiovascular, inflammatory, neurological, psychic, and oncological diseases is often related to dysbiotic conditions [26]. A recent study on the role of the oral microbiome, dysbiosis, and long COVID was performed by metagenomic sequencing using lingual swabs from SARS-CoV-2-infected patients [31,32,33,34,35,36,37,38]. In the oral MB of the patients with long COVID, bacteria such as Prevotella and Villanella predominated and are known to have inflammatory activity: Villanella strains stimulate IL-6 production, while Prevotella strains activate IL-23 and IL-1 and toll-like receptor 2 [4,39,40,41,42]. It was also found that the oral MB of patients with chronic asthenia syndrome and myalgic encephalomyelitis was comparable to that of patients with long COVID [43,44,45,46,47,48]. In both, Leptotrichia, Prevotella, and Fusobacteria phyla prevailed, all with inflammatory activities. All the results demonstrate that oral MB dysbiosis may have determined the clinical and symptomatic course of long COVID patients [49,50,51,52]. The latest studies confirm the ability of RSV to interact with intestinal MB and derivatives of their metabolism, such as short-chain fatty acids and intraluminal lipids, playing an essential role in improving the clinical aspects of the metabolic syndrome [16,53,54,55]. In particular, the metabolic syndrome (MS) is a recurrent disease worldwide, characterized by hyperlipidemia, abdominal obesity, insulin resistance, and hypertension, with consequent development of systemic inflammatory diseases, diabetes, coronary heart disease, stroke, and cancer [56,57,58]. Studies show that the oral administration of RSV, activating SIRT-1, influences both glucose metabolism and lipid metabolism, inhibiting their accumulation. RSV inhibits the process of the formation and accumulation of fat in the white adipose tissue, while, in glucose metabolism, it intervenes in several mechanisms [57,59]. Oral administration of RSV in humans improves insulin secretion and insulin resistance by protecting pancreatic β cells from oxidative stress, suppresses glucagon production after meals by improving insulin metabolism, and reduces fasting blood sugar and A1C hemoglobin [60,61]. In the liver, SIRT-1 acts on gluconeogenesis. In tissues where SIRT-1 is present, RSV controls the insulin responses of target cells. Therefore, RSV mimics the effects of a low-calorie diet, which improves cell turnover by slowing down the aging process [62,63,64]. Studies show that there could be an interaction between GM and RSV as if the intestinal microbiota would be the target of RSV, which regulates intestinal homeostasis in response to oxidation processes [65,66,67,68,69]. Most phenolic foods are absorbed in the colon, where they are metabolized by GM into low molecular weight phenolic compounds, such as phenolic acids, which are better absorbed from the intestinal tract to be then conveyed to the liver, where they undergo further biometabolizations (hydrolysis, reductions, and splits) and enter the circulatory system [70,71]. The rate, quantity, and type of metabolites are closely related to the MB variety of the colon. To date, three metabolites of RSV are known: dihydroresveratrol, 3,4′-dihydroxy-trans-stilbene, and 3,4′-dihydroxybibenzyl (lunularin) (Figure 1) [67]. The bioactivity of RSV metabolites could be more intense than RSV itself, and the antioxidant and anti-inflammatory bioactivity of dihydroresveratrol was detected both in vitro and in vivo [72,73,74,75].
Figure 1.
Summary of the RSV metabolites and the main molecules indicated for their antioxidant and anti-inflammatory bioactivity.
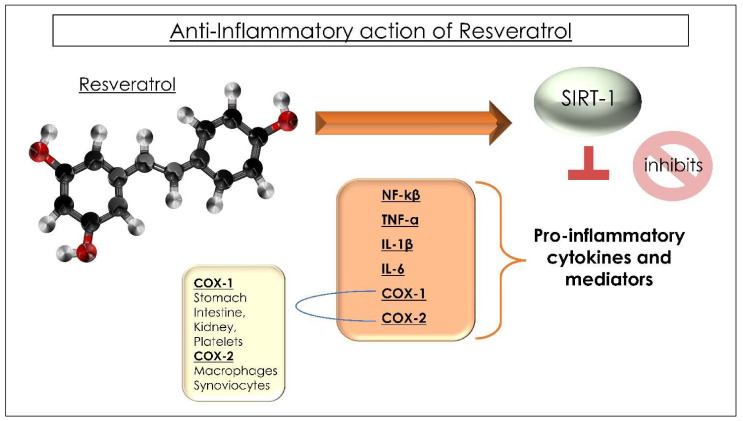
In turn, as for an interdependence relationship, the phenolic derivatives control the GM composition either for or against some microbial strains. Furthermore, it has been observed that some Lactobacilli are proven regulators of the immune system [4], and the qualities of Lactobacilli and Bifidobacteria modulate the gut microbiota. These microorganisms limit gut permeability and favor the immune system [46]. The non-metabolized phenols, together with other endogenous substances of the patient, act as prebiotics influencing the GM with antimicrobial activity and influencing bacterial adhesion to cell surfaces, for example, by favoring strains of Bifidobacterium and Lactobacillus or by inhibiting the growth of different species of Clostridia, Lachnospiraceae, and Enterococcus faecalis [70,76,77,78,79]. An opposite effect was obtained for Faecalibacterium prausnitzii, which was increased compared to the control group. The properties of the prebiotic RSV, which modifies the variability and composition of the intestinal MB, are also manifested in the decrease in the Firmicutes/Bacteroidetes ratio, which instead is increased in obese patients or patients with systemic diseases [80,81,82]. The metabolite dihydroresveratrol (Dh-RSV) comes from the RSV fermentation in the cecum, colon, and rectum by the MB, which acts as a drug in the human large intestine. Therefore, the beneficial effects are not only due to RSV but also due to the products of its metabolism [76,83,84,85,86]. The administration of RSV results in a reduced formation of Trimethylamine-N-oxide (TMAO), a metabolite of carnitine and choline, resulting from the digestion of red meat, egg yolk, and fatty cheeses and liver [87]. A high concentration of TMAO is considered a risk for heart attack and stroke because it activates platelet activity predisposing to thrombosis [87]. Probably, the traditional association that red wine with red meat-based meals acts as a cardiovascular prevention by limiting the production of TMAO has not been observed in white wine consumers or abstainers. Therefore, RSV interacting with the intestinal microbiota could be therapeutic in inflammatory bowel diseases with a systemic implication [81,88,89]. By decreasing the production of interleukin 1 (IL-1), IL-6, C-reactive protein (inflammatory markers), and the transcriptional activity of nuclear factor kappa B (NF-kB), which regulate inflammatory processes and immune responses, RSV reduces inflammation even in patients with cardiovascular diseases, showing improvements in hypertension, heart failure, and ischemic heart disease (Figure 2) [90]. The action of the RSV on the activation of SIRT-1 has also shown benefits on bone metabolism [91].
Figure 2.
Summary of the cytokines’ and mediators’ modulation correlated to the anti-inflammatory properties of RSV. The RSV is able to interact with the SIRT-1 pathway in order to inhibit the pro-inflammatory mediators’ cascade and the COX-1 and COX-2.
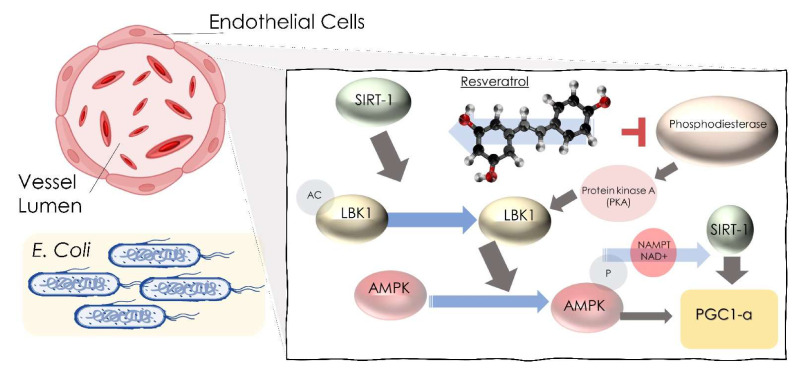
Some studies show that the concentration of alkaline phosphatase in serum and bone alkaline phosphatase was increased with the administration of RSV, while the values of serum calcium, osteocalcin (a specific marker of bone turnover), and procollagen did not decrease. In a study conducted on type 2 diabetic patients exposed to the risk of fracture, 500 mg/day of RSV was administered, and a reduced loss in bone density was encountered [92,93]. Better results were found in those patients who had lower values of calcium and 25-hydroxy vitamin D and in alcoholic beverage drinkers [91,94]. Some studies have shown how RSV stimulates the activity, and the differentiation processes of osteoblasts slow down the processes of osteoporosis, and, also, combined with platelet concentrates, such as concentrated growth factors (CGF), prevent osteonecrosis from bisphosphonates, in particular from zoledronic acid (ZOL) [95,96,97,98]. At the bone level, the administration of RSV also prevents osteomyelitis due to Staphylococcus Aureus by avoiding damage from the neutrophils, caused by the Panton–Valentine leukocidin toxin (PVL), and avoids the development of thrombosis [99,100]. RSV may reduce CNS injury caused by meningitic E. coli. In fact, in an in vivo study on mice, it was found that, in the presence of meningitic Escherichia coli, the RSV interacting with the lipid raft of the endothelial cells of the blood–brain barrier, blocking the signal cascade of extracellular signal-regulated protein kinase 1/2 and vascular endothelial growth factor-A (ERK1/2-VEGFA), prevented penetration and, therefore, infection of the central nervous system (CNS) and reduced the production of inflammatory cytokines (Figure 3) [101,102]. The antiviral action of RSV is also due to the activation of the intracellular signal of SIRT-1, which blocks viral infections by increasing their resistance [103]. As for COVID-19, studies show that RSV inhibits viral entry into the cell and its replication [4,36,104].
Figure 3.
Summary of the pathway correlated to the bacteria infection protective properties of RSV. RSV pathways are able to produce a signals cascade involving Sirtuin 1 [SIRT-1], adenosine monophosphate (AMP)-activated protein Kinase [AMPK] (blue arrow), liver-kinase B1 [LKB1] (grey arrow), and peroxisome proliferator-activated receptor-γ coactivator [PGC-1α].
On the other hand, in multiple sclerosis and hepatitis C, RSV administration worsens the clinical outcome [105,106,107]. Recent studies have suggested that RSV improves its stability when combined with glucan. Glucans, also called biological response modifiers, are present in the structure of yeasts, fungi, and algae’s cell walls. For more than half a century, glucan has been recognized as having an active role as a biological immunomodulator [108,109,110,111]. RSV in an aqueous solution with carboxymethyl-β-glucan inhibits the replication of human rhinoviruses (HRVs), responsible for the common cold both in the adult and pediatric population. Precisely, the lack of HRV’s replication seems to be associated with an RSV-induced low cytokine release [108]. Studies show how the use of nasal spray or aerosol with RSV and carboxymethyl-β-glucan has reduced the application of antihistamines and nasal decongestants in the allergic rhinitis common cold, improving symptoms such as cough, rhinorrhea, nasal congestion, sneezing, sore throat, and fever. They were also used as a prophylaxis in pediatric patients exposed to frequent respiratory infections [49,112,113]. An interesting study revealed an inhibitory effect of RSV at the minimum inhibitory concentration (sub-MIC) level on Streptococcus mutans and its cariogenic virulence, interfering with the synthesis of acids and their tolerance, on the synthesis of extracellular polysaccharides, on the composition of the biofilm, and on the potential of the virulence gene. For this reason, it could be considered as a product for prophylaxis in the development of dental caries [114,115,116,117]. RSV is considered an antitumor substance since it induces proapoptotic, antiproliferative, anti-inflammatory, and anti-angiogenic mechanisms. One of the main anti-tumor mechanisms of RSV seems to be related to the activation of TANK-binding kinase 1 (TBK1), whose insufficient activity would lead to autoimmune, neurodegenerative, or oncogenic diseases [69,118,119,120]. Many experimental studies recognize the immunomodulatory role and immune function of RSV [79,121,122,123]. RSV modulates innate and acquired immunity by interacting with different cellular targets. However, its properties appear to be conflicting. Its immune functions are dose-dependent: it induces immunosuppression in high doses, while it stimulates the immune system in low doses [124,125]. It intervenes in the immune system by activating macrophages, T cells, and natural killer (Nk) cells with an antioxidant effect, removing reactive oxygen species (ROS), inhibiting cyclooxygenases (Cox), and thus activating anti-inflammatory processes. As an immunomodulator, it inhibits the proliferation of spleen cells stimulated by Concanavaline A and interleukin-2 (Il-2) and blocks T lymphocytes and tumor necrosis factor-α (TNF-α) to produce Il-2 and interferon-gamma (Ifnγ) and macrophages to produce Il-12 [126,127,128]. The RSV bioavailability is rapidly reduced after oral administration, reducing its effects. In fact, traces of RSV are detected in plasma (5 ng/1) after 25 mg administration because 70% is absorbed by intestinal cells, and the remainder is rapidly metabolized [79,129]. As it is not water-soluble, if administered orally, about 30% is directly eliminated without being absorbed [130]. Therefore, to improve the bioavailability, new compounds have been formulated with adjuvants, nanoparticles, phospholipid complexes, and liposomes to evaluate the proper therapeutic dosage in pathological and inflammatory situations and for prophylaxis in physiological conditions [6]. RSV did not show any side effects when administered in the daily dose of 600 mg in chronic diseases and immunomodulatory disorders [104]. Our systematic review focuses on the influence of RSV on the gut microbiota (GM), bone metabolism, and the immune system.
2. Materials and Methods
The present systematic review has been performed in accordance to the principles of the PRISMA and International Prospective Register of Systematic Review Registry guidelines (n. 313242) [131]. PubMed, Cochrane Library, Scopus, Web of Science, and Google Scholar were searched to find papers that matched our topic dating from 1 January 2017 up to 18 January 2022, with English-language restriction. The search strategy was built by using a combination of words that matched the purpose of our investigation, whose primary focus is the effect of resveratrol on the microbiota; hence, the following Boolean keywords were used: (“resveratrol” and “microbio*”) (Table 1). Two independent reviewers (A.C., F.I.) working in duplicate evaluated all suitable trials with the following inclusion criteria: (1) studies only on human subjects; (2) open access studies that any other researchers can retrieve without any subscription; (3) studies that analyzed the link between resveratrol supplementation and the effects on the axis microbiota and immune system with a particular focus on oral and intestinal microbiota; studies that did not take into account the microbiota were excluded. Disagreements between the investigators regarding the article’s selection were adequately discussed and resolved by adjusting the inclusion and exclusion criteria.
Table 1.
Database search indicators. No publication period limitations have been considered.
| Articles screening strategy | KEYWORDS: A: “resveratrol”; B: “microbio*”Boolean Indicators: (“A” AND “B”)Timespan: from January 2017 up to January 2022.Electronic Databases: PubMed, Cochrane Library, Scopus, Web of Science, and Google Scholar |
3. Results and Discussion
3.1. General Characteristics of the Articles Included
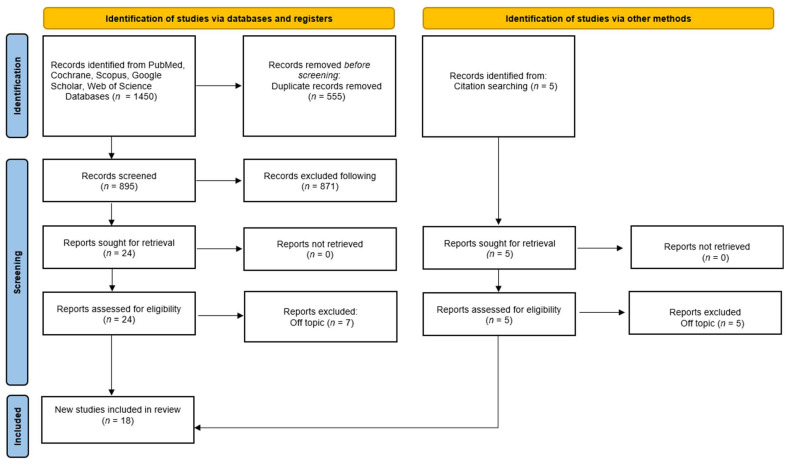
A total of 1450 publications were identified from the following databases, including Pubmed (441), Google Scholar (55), Scopus (408), Cochrane (0), and Web of Science (546), which led to 895 articles after removing duplicates (555). Five additional relevant papers were added by searching the reference list of eligible publications. A total of 871 publications were excluded by analysis of the title and abstract. The remaining 24 articles were successfully sought for retrieval and were added to the five papers found by reference list, leading to 29 publications that were assessed for eligibility by the authors. Eleven publications were excluded in the process because they were off-topic. A final number of 18 studies were included in the review for qualitative analysis (Figure 4).
Figure 4.
PRISMA flowchart diagram of the inclusion process [131].
3.2. Resveratrol and the Microbiota Modulation
In terms of RSV’s therapeutic potential and benefits, more and more research is finding evidence of RSV’s interaction with the human MM [70,88,132]. Because the totality of bacteria in the human body serves as one of the key regulators in maintaining the homeostasis of many systems in our body [133], alterations in the human MB resulting from RSV usage are also linked to metabolic changes [134]. Metabolic syndrome, which is associated with the development of type 2 diabetes and heart disease, is defined as the presence of three of the following metabolic changes in an individual: obesity or high blood pressure in the central nervous system, high blood glucose, and low serum high-density lipoprotein or high serum triglycerides [55]. RSV has been described as an effective supplement in reducing calories, a process that aids physical activity and insulin sensitivity, leading to increased energy consumption. RSV has also been described as inhibiting adipogenesis, presenting fat-lowering effects [63,135]. These data make RSV a multi-organ/anti-obesity supplement that is worth studying. Walker et al. conducted their study on white subcutaneous adipose tissue. Adipose tissue material obtained for biopsy from both groups was compared before and after RSV treatment, indicating that changes in the expression of genes and expression of gene pathways are inconsiderable; genes related to the mammalian target of rapamycin (mTOR) and SIRT-1 did not change [136]. SIRT-1 is vital in the mitochondria’s function and biogenesis, and repressing PPARγ in adipocytes causes lipolysis and fat loss [135,137]. Nevertheless, RSV in humans has not shown significant effects in weight loss, waist thinning, BMI, or in reducing adipose mass [138,139]. Korsholm et al. conducted their analysis in intracellular pathways, considering these analyses as unbiased and more generalized than the usual tests performed on blood (Table 2).
Table 2.
Reported RSV results in obese individuals with metabolic syndrome.
| Ref. | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [136] | Walker et.al 2018 |
A pilot randomized placebo-controlled clinical trial 30 days |
|
28 obese men with MS
|
No significant effect on insulin sensitivity or glucose homeostasis but during a 2-h oral GTT, post hoc analysis was seen a significant improvement in insulin sensitivity and glucose tolerance in Caucasian subject |
| [140] | Korsholm et.al 2017 |
A randomized placebo-controlled clinical trial 4 months |
A comprehensive metabolomic analysis of the changes caused in middle-aged men with MS by RSV | 66 obese men with MS
|
RSV supplementation reduces sulfated androgen precursors, at the same time lipid metabolism was affected and urinary derivates of aromatic amino acids reflect the composition of gut microbiota. |
| [132] | Most et.al 2017 |
A randomized double-blind placebo-controlled trial 12 weeks |
To evaluate the effect of combined EGCG–RSV supplementation on gut microbiota composition. If changing the composition of the microbiota brings EGCG–RSV improves lipid oxidation and mitochondrial oxidative capacity. |
42 obese men and women
|
EGCG–RSV supplementation reduced Bacteroidetes and tended to reduce Fecalibacterium in men. The composition of men’s baseline microbiota determined the increase in fat oxidation after EGCG–RSV supplementation. |
This biochemical analysis in adipose tissue found considerable increases in intracellular glycerol and free fatty acids in individuals treated with RSV. Six of the thirteen identified lipids experienced a slight increase in individuals of the hRSV group and a slight reduction in dehydroisoandrosterone sulfate (DHEA-S) and 4-androsten-3β, 17β-diol disulfate, which are steroid hormones, leading to the reduction in cholesterol [26]. In MS, a person’s high blood pressure is often present as a consequence of being overweight, and a reduction in cholesterol may bring good results in these cases, but treatment with RSV in humans has not provided satisfactory results either in diastolic or systolic blood pressure [10,141]. The mechanism by which RSV improves insulin sensitivity is already known: RSV activates AMPK [135], so RSV upregulates Act and insulin receptor substrate-1, which are insulin-signaling components [142,143]. RSV reduces the expression of adipokines and adiponectin, which regulate insulin sensitivity and retinol-binding protein 4 expression and resistin [144,145]. However, some studies have not found positive effects of RSV on insulin resistance and glucose homeostasis [138,146,147]. In contrast, other studies acknowledge that RSV does not affect glucose homeostasis and insulin resistance in healthy individuals but in individuals with middle insulin resistance, where it shows a mild action [26,148]. The primary site of postprandial glucose disposal is skeletal muscle [149], and this occurs through the insulin-activated glucose transporter GLUT4 [150,151]. GLUT4 translocation is reduced in insulin-resistant diabetic and prediabetic tissues [152]. Exercise and diet are the strategies that aim to lower postprandial blood glucose in cases of insulin resistance by improving glucose uptake into skeletal muscle cells [153,154]; the MM has an impact on metabolism during exercise [155], and athletes’ GM values differ from those of sedentary people [156]. The impact of the microbial catabolism of phenols on glucose metabolism, particularly in the postprandial period, insulin responses, and type 2 diabetes, was investigated in recent research [157] (Table 3). The effects of certain phenolic compounds on glucose metabolism and absorption by differentiated muscle cells of the human musculoskeletal cell line LHCN-M2 [158], which display typical muscle phenotypic markers, were investigated in detail. The activity of IVAS isovanillic acid-3-O-sulfate, a metabolite of the gut MM, was found to be the most effective in the study [157] (Table 3). IVAS 2 was discovered in plasma after eating berries or cyanidin-3-O-glucoside [159,160], although its biological functions are unknown. According to the findings, IVAS, 3-O-sulfated isovanillic acid enhanced glucose transport as a phase 2 conjugate of protocatechuic acid [161]. Protocatechuic acid acted according to a dose-dependent mechanism in the uptake of (deoxy) glucose in primary human muscle cells [162]. Human adipocytes increased the glucose uptake by mimicking insulin and thereby activating its receptor [163]. Protocatechuic acid and its metabolites may affect both pathways stimulating GLUT4 translocation in L6 myotubes [164]. The mechanism was dependent on PI3K signaling and GLUT4 translocation. IVAS also upregulated GLUT1 and activated Akt (Table 3). According to a study [157] (Table 4), the action of IVAS and IVA isovanillic acid (phenolic conjugate) likely occurs on the insulin receptor present on the surface of LHCN-M2 cells [165], and, because IVATS and insulin are structurally similar, there may be a mechanism of competition between the two molecules that is not yet well understood; this could be investigated in the future using molecular docking and mutagenesis studies. This research demonstrated that conjugated catabolites, derived from the action of the GM, affect glucose uptake and metabolism in LHCN-M2 human skeletal myotubes. Because skeletal muscle is responsible for 75% of postprandial glucose disposal [152], it will be critical to optimize systemic glucose metabolism and muscle function by regulating the insulin-stimulated glucose uptake in muscle cells via the GM [157]. In Caucasian subjects, the post hoc analysis performed 2 h oral GTT speaks of a change in results compared to non-Caucasian (Table 2). Glucose tolerance and insulin sensitivity, according to this study, were notably improved [136]. Using RSV brings about changes in the GM, altering the alpha and beta diversity. Specific taxa changes were also found in persons treated with RSV [136]. Most et al. conducted the study in two groups, polyphenols epigallocatechin-3-gallate (EGCG) and RSV (RES) in the first group and the placebo in the other group. This study compared how the usage of polyphenol supplementation affects the intestinal bacterial flora in both males and females (Table 3). The results showed that taking these supplements considerably reduced bacteroidetes in males but not in women (however, this could be due to women’s usage of oral contraceptives, which was not controlled before testing) [132]. According to some studies, polyphenols most likely act on the adhesion of microorganisms and stimulate the growth of commensal bacteria and inhibit pathogenic intestinal bacteria [74,81,166,167]. The selection of bacterial strains depends on their ability to adhere to epithelial cells, production of antimicrobial substances, and survival under simulated gastrointestinal conditions [168]. These characteristics can be studied by in vitro cellular models of the human colon, such as Caco-2, HT 29, T-84, and others. The co-culture of Caco-2/HT29-MTX seeded in the ratio of 9:1 (Caco-2: HT29-MTX) mimics the ratio of Goblet cells to absorptive epithelial cells in the healthy tract [80,167,169], including in the production of mucin. This glycoprotein may have a function in lactobacilli adhesion; in fact, it serves as a rich binding network and substrate for commensal microbiota [170]. Resveratrol improved Lactobacillus acidophilus adherence to mucin and HT-29 cells via changes in glycoprotein expression in a recent study [171]; nevertheless, issues remain concerning the physiological significance of the doses utilized in the model. According to the study [172], both L. gasseri and L. Plantarum in the presence of RSV adhered with high capacity to the in vitro Caco-2/HT29-MTX co-culture, demonstrating consistency with numerous in vivo Lactobacillus studies; these strains colonize the intestinal mucosa after oral administration, and, in particular, L. gasseri [173] and L. Plantarum [174] were consistently found in the feces. However, on the adhesion of any strain to the physiologically low concentrations of RSV (4.5, 2.25, and 1.125 g mL−1) utilized in bacterial suspension, no statistically significant findings (p 0.05) were found [172] (Table 4). RSV did not affect the strains examined in the panel, but it cannot be ruled out that it affects other strains. RSV raised Lactobacillus’s adhesion to mucin and HT-29 cells by up to 100 µg mL−1 in a recent study [171] despite questions about the relevance of the physiological concentrations used. This suggests that RSV is one of the tested polyphenols that is most efficacious in changing surface protein expression. According to several data, polyphenols have a specific lactobacillus strain and cell line-dependent activity [74]: Epigallocatechin boosted L. casei adhesion 3 to Caco-2 cells, while procyanidins B1 and B2 stimulated adhesion to HT-29 cells. Furthermore, epigallocatechin gallate improved L. acidophilus adherence to Caco-2 cells [74]. This study demonstrates that, while L. gausseri has higher adherence than L. Plantarum, the idea that RSV promotes bacterial adhesion cannot be verified because no statistically significant results were found on the lactobacilli tested [172]. RSV’s favorable effects on the MB and, as a result, on the prevention of noncommunicable illnesses, have only been established in vitro and in rodent models, so more research is required [172]. The binary capability of RSV has been demonstrated in a mice model by Qiao et al. [175], which revealed a selective inhibition of the gut growth of Enterococcus faecalis in favor of a growth of Lactobacillus and Bifidobacterium species. A secondary outcome was associated to an mRNA under-expression of Lpl, Scd1, Ppar-γ, Acc1, and Fas markers that are correlated to the fatty acid synthesis and adipogenesis/lipogenesis processes [175]. Korsholm et al. found changes in the urine, where many of the metabolites derived from aromatic amino acids are the product of MB (Table 2). Metabolites such as tyramine and phenol sulfate, along with homovanillate and tryptamine, as well as indolelactate, 2-hydroxyphenylacetate, and histidine, were changed in the RSV group [26]. Jarosova et al. provided new information on the metabolic process that makes stilbenoids more water-soluble by the human GM depending on their molecular structural properties (Table 4). All this is because the uniformity of stilbenoids varies in the different habitat of the colon. These phenolic compounds have significant biological effects on humans. Many of the most recent nutritional and epidemiological studies confirm these important effects, for example, the ability to defend against oxidative cellular stress and the suitability for the prevention of degenerative diseases affecting the cardiovascular system, neurological system, and even cancer [70]. There are two ways in which resveratrol has affected and modulated the intestinal microbiota: the first with its antimicrobial role, and the second by modifying the composition of this population [176,177]. Its antimicrobial role has been shown to be effective in both Gram-positive and Gram-negative bacteria, for example, the antimicrobial effect of resveratrol on E. coli occurs by inhibiting cell division (Z-ring formation) [178,179]. Hydrolysis (O-deglycosylations and ester hydrolysis), cleavage (C-ring cleavage, delactonization, demethylation), and reductions (dehydroxylation and double bond reduction) are the three major catabolic processes in microbial biotransformations [77]. In turn, phenolics appear to influence GM composition by favoring/disfavoring specific microbial strains, establishing a two-way connection between the GM and phenolics [65,81,180,181,182]. Chlorogenic acid, resveratrol, catechin, and some quercetin derivatives, for example, have been shown to increase the proportional representation of Bifidobacterium strains and, hence, have prebiotic-like effects [66,84,183,184,185]. Inoculation with resveratrol and some ellagitannins inhibited the growth of various Clostridia species, demonstrating antimicrobial activity [75,84,181,186]. Bacterial adhesion effects of procyanidin and chlorogenic acid have been observed by Lactobacillus strain adhesion augmentation to intestinal epithelial cells [80,187]. Regarding the composition of gut microbiota, Larrosa et al., concluded that Lactobacillus and Bifidobacterium were increased after the use of resveratrol, and the opposite happened with E. coli and Enterobacteria [181]. There is also evidence that confirms the positive role of resveratrol in maintaining gut barrier function and integrity [188]. The changes that resveratrol brings to the composition of gut microbiota are thought to be one of the main mechanisms of how it acts in the body; also, these changes are closely related to the course of metabolic disorders [189,190]. RSV has a strong congeniality with quinone reductase, by the continuous dissociation that reaches a level above 35 nM, so much so that it is possible to define RVS as one of the most potent inhibitors known so far, capable of regulating the cellular presence of antioxidant enzymes and assisting in cellular resistance to stress oxidation [191]. Its anti-inflammatory capacity remains as demonstrated by three pivotal factors: the decrease in tumor necrosis element alpha (TNF-α) and interleukin 1 beta (IL-1ß), amplification of interleukin 10 (IL-10), and reduction in the manifestation of prostaglandin E synthase-1 (PGES-1), cyclooxygenase-2 (COX-2), and inducible nitric oxide synthase (iNOS) [192,193]. RSV affects various metabolic elements and receptors that are responsible for oxidative stress. A study [194] investigating RVS’s effect on intestinal eubiota noted that, with the determination of the internal structure developed by stilbenoids, a reduction in the Firmicutes and Bacteroidetes ratio was produced, as well as a lowering in the Clostridium strains and the incidence in the Lachnospiraceae family. The antimicrobial effect of RVS has been demonstrated through its inoculation, which inhibits the growth of several species of Clostridia [75,84,181,186]. The total GM is made up of 90% Firmicutes and Bacteroidetes [195], and it is known that the increase in F/B in the human (and also mouse) GM is related to an increase in obesity and onset of disease [82,196]. RVS demonstrated to reduce this proportion [84,175,185]. Recent studies lead us to deduce that GM is one of the most important protagonists in cardiovascular diseases, passing through the meta-organismal pathways [197]. In fact, Chen et al. have developed some guidelines for in vitro screening of the mouse gut MM. The results demonstrate that the MB modulates bacterial growth [198]; moreover the cyclic peptides D, L-a of the microbiota are able to reform the intestinal microbioma itself. The GM bases its metabolism on choline, which, by producing trimethylamine (TMA), converts into trimethylamine-N-oxide (TMAO), which implements atherosclerosis by hepatic monooxygenases containing flavin (FMO), and it is known that TMAO has a significant function in cardiovascular disorders [199]. It is noted that TMAO is a product of fish and meat-based nutrition [200] and of the intestinal microbial metabolism of choline, carnitine, and betaine to trimethylamine (TMA). Furthermore, many species of bacteria elaborate that the synthesis of TMA has been developed with cultural methods, as well as those described here belonging to Firmicutes and Proteobacteria, and Actinobacteria [201]. Peptides administered orally daily can reduce the density of total cholesterol, and atherosclerotic plaques and RSV inhibit the synthesis of trimethylamine-N-oxide (TMAO), reducing the growth of TMA with the remodeling of the MM [202]. Intestinal bacteria through choline, carnitine, and TMA synthesize TMAO (Table 4) [203], which has been noted as a cause of cardiovascular disorders.
Table 3.
Effects of RSV and phenolic compounds on glucose uptake and metabolism in muscle cells, Lactobacillus adherence to intestinal epithelial cells, and S.Mutans cariogenic activity.
| Ref. | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [157] | Houghton et al. (2019) | Research in vitro | Investigate the impact of microbiota-derived phenolic metabolites on glucose uptake and metabolism in muscle cells in myotubes treated with insulin and glucose | LHCN-M2 myoblasts Flavanol conjugates, RSV conjugates, and phenolic sulfates, compounds from colonic microbiota metabolism |
Many of the compounds tested increased glucose absorption and metabolism, but most notablyisovanillic acid 3-O-sulfate (IVAS) by a dose-dependent mechanism through the GLUT 4 transporter and PI3K pathway IVAS also enhanced phosphorylation of Akt and upregulated GLUT1, GLUT4, and PI3K p85a proteins. |
| [172] | Jarosova et al. (2018) |
Research in vitro | RSV increases bacterial lactobacilli’s adhesion | Bacterial strains: L. plantarum, L. Gasseri L. fermentum, and L. brevis Caco-2 cell line, human epithelial intestinal cell lines at three physiologically low doses of 4.5, 2.25, and 1.125 g mL–1 of RSV There was no statistically significant difference in adhesion between any strains (p 0.05). |
No statistically significant result on the adhesion of any strain (p < 0.05) |
| [114] | Li et al. (2020) |
Research in vitro | Evaluate anticariogenic activity of RSV on S.Mutans | Bacterial strain S. Mutans UA159 RSV (0, 50, 100, 200, 400 μg/mL) |
RSV reduced the synthesis of water-soluble and water-insoluble polysaccharides and lowered acid production and tolerance at sub-MIC doses, compromising biofilm formation. Virulence factors were inhibited as concentrations of RSV increased (ldh, relA, gtfC, comDE). |
Table 4.
Reported RSV results in the colonic environment and GM.
| Ref. | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [70] | Jarosova et al. (2018) |
In vitro study 48 h study | To analyze the effectiveness of selected stilbenoids (batatasin III, oxyRSV, piceatannol, pinostilbene, RSV, thunalbene) in the colon To provide new data about the biotransformation of six stilbenoids by microbiota, depending on their structural molecular properties. |
In vitro fecal fermentation system fermentation medium Sodium phosphate buffer and reducing solution Stilbenoid preparation Fecal samples and ethics statement |
The stilbenoids vary their stability in a colonic environment. |
| [76] | Jaimes et.al 2019 |
In vitro study of fecal bacteria of 4 volunteer donors | To explore the effect of six stilbenoids (batatasin III, oxyRSV, piceatannol, pinostilbene, RSV, thunalbene) on the gut microbiota composition. To understand the impact of phenolic supplementation and favorable colonic conditions |
Fecal fermentation (FFM) system Set of six stilbenoid phenolics were fermented in vials via inoculation with human fecal bacteria obtained from four donors. 2 males and two females ages 23, 28 (volunteer Donors 1 and 3) and 26, 29 (volunteer Donors 2 and 4). Fermentation Medium |
The tested stilbenoidsmodulate the GM |
| [215] | Heng et.al 2021 |
In vitro study to identify the TMA inhibitors | To identify choline-degrading bacteria from healthy human feces and used for screening of trimethylamine (TMA)-lyase inhibitors To screen choline-degrading bacteria from healthy human feces |
Stool samples from healthy adult college students BSM supplemented with 50 mM choline |
The treatment with β-sitosterol and RSV decreased TMA level |
The whole process is assisted by micro inhibitors that prevent dietary choline or L-carnitine from converting into TMA, which becomes unable to attack the GM. Some researchers confirm that a particular inhibitor, 3,3-dimethyl-1-butanol (DMB), inhibits the microbial activity of choline TMA lyase [204]. In this experiment, Klebsiella and Escherichia were found to host three of the four potential pathways of production of TMA (choline, carnitine, and TMAO), so they have a significant role in the cycle of TMA in the human intestine (Table 4) [203]. Among the various positive effects of RSV, there are also the anti-cariogenic ones. This activity against S. Mutans has been the subject of studies, focusing on acid production, acid tolerance, gene expression, extracellular polysaccharide synthesis, virulence, and biofilm formation [114]. Dental caries is among the most frequent diseases of the oral cavity, and the action of S. Mutans mainly causes it. Several antimicrobial agents, including fluoride, have been utilized, but research is moving towards herbal products with minimal side effects. The synthesis of acid and LDH, an enzyme known to create lactic acid during glycolysis, was investigated in a study on the anti-cariogenic features of RSV. S. Mutans’ cariogenic activity is achieved through glycolysis and the LDH’s action [205]. According to a study by Li et al. [114], RSV reduces the acid production of S. Mutans to sub-MIC levels by suppressing bacterial glycolysis (Table 3). Furthermore, by adding 200 and 400 μg/mL RSV, the final pH values in the glycolytic pH drop test were above the critical pH value that determines the rate of demineralization and remineralization of tooth enamel [206]. RSV reduces the amount of S. Mutans at ph 5. Inhibitory activity of RSV on acid tolerance has been demonstrated using proton permeability and F-ATPase activity assays: this action appears to be due to the inhibition of F-ATPase activity, which is essential in maintaining the pH gradient across the membrane, which is related to acid tolerance [207]. The adhesion of S. Mutans occurs through water-soluble and insoluble extracellular polysaccharides (EPS), which act in the biofilm matrix’s formation [208,209]. According to the study [114], RSV reduces adhesion and biofilm formation by taking action on soluble and non-soluble polysaccharides, more so on insoluble ones; CLSM images demonstrate a looser and thinner biofilm and thus an inhibitory action on bacterial viability. This study (Table 4) also evaluated the S.Mutans’ transcriptional activity and virulence factors, including acid production and acid tolerance, synthesis, and polysaccharide formation. RSV caused lactate dehydrogenase (LDH) gene expression reduction in accordance with LDH activity assay and PCR; RelA gene expression, which encodes for guanosine tetra (penta)-phosphatesynthetase involved in oxidative stress and acid tolerance mechanisms [210], was also decreased. The activity of the gtfC gene encoding for GTCF, which is required for glucan synthesis in the biofilm, was also discovered to be altered, resulting in lower cariogenic activity in vivo [211,212]. RSV can repress the ComDE system of S. Mutans, generating a phenotype with a defective biofilm [213]. The ComDE system is a fundamental quorum, sensing the cell–cell communication system in the gene regulatory networks responsible for bacterial adaptation in biofilms [115,214]. Repression of this gene interferes with the internal communication quorum sensing mechanism in S. Mutans by inhibiting biofilm formation. According to this study, RSV might have anti-cariogenic effects, but the toxic effect in the oral cavity is still to be elucidated, so further studies are needed to understand its molecular mechanism.
3.3. Resveratrol and Microbiota Modulation on the Immune Response
The MB invades and occupies the intestine from birth and is immediately conditioned by the type of birth, breastfeeding, and antibiotic intake [216]. The MB is the set of symbiotic microorganisms in symbiosis with the human body, and it is strongly regulated by food and microorganisms that regulate the bioavailability of many antioxidants [217]. Being in direct contact with the outside world, the oral MB is the first point of contact with everything we ingest. It has a defensive role of primary importance and acts as a sentinel against potential bacteria and viruses that can infiltrate and try to reach the respiratory tract, promoting infection [218]. The microbiota is a variable organ, modified by hormonal factors specific to the person or external factors, such as diet or probiotics [46,219]. However, if there is dysbiosis, the bacteria present are mostly pathological, and the “line of defense” is not strong enough to protect us from possible pathologies [220]. Pathogenic viruses and bacteria can prevail and inflame the tonsils, pharynx, and larynx, leading to pharyngotonsillitis, pharyngitis, tonsillitis, or halitosis oral candida [221]. Polyphenols can be an excellent help for available diseases, weight, and metabolism, helping to increase the risk for different diseases [222]. Plants synthesize RSV as one of the defense mechanisms, which regulates immunity and can play a role in the prevention and evolution of chronic inflammatory diseases as it interferes with the regulation of immune cells, the synthesis of pro-inflammatory cytokines, and gene expression [90]. RSV can directly damage bacterial, fungal, and viral cells, hitting specific targets within these microorganisms and slowing their growth [223]. RSV has antimicrobial activity: it is capable of recruiting and activating macrophages, neutrophils, and lymphocytes during infections [121]. It has an anti-inflammatory action, stimulating that of anti-inflammatory cytokines, reducing chronic inflammation: by activating SIRT-1, it inhibits the formation of inflammatory factors, which include NF-kB, which increases the production by the cells of the immune system of pro-inflammatory cytokines (such as TNF-α, IL-1β, IL-6) and COX (COX-1 and 2), which transforms arachidonic acid into inflammatory prostaglandins and thromboxanes. The anti-inflammatory function of RSV is mediated by SIRT-1 [121]. RSV also reduces oxidative stress and increases antioxidant molecules. These molecules, reducing the production of free radicals, are the inhibiting glutathione S-transferase (GST), glutathione peroxidase (Gpx), NQO1, catalase, and superoxide dismutase (SOD) [224]. Ramdani [225] demonstrated that RSV regulates RAS and ACE2, involved in SARS-CoV-2 disease, reducing inflammatory cytokines, activating the SIRT-1 and p53 signaling ways, and by increasing CTL and NK cells. The receptor for SARS-CoV-2 is the angiotensin-converting enzyme 2 (ACE-2). Inhibition of ACE reduces cardiovascular and renal diseases. Furthermore, ACE-2 can reduce the binding of the SARS-CoV 2 virus to human cells. RSV works by inhibiting ACE/ACE-2. RSV increases the activity of the angiotensin II converting enzyme receptor both in vivo and in vitro [226]. Cells with high ACE2 expression on their cell walls are an easy target for the SARS-CoV-2 virus [4]. RSV would have shown the potential to increase the expression of ACE-2, important in the role of the entry of SARS-CoV-2, and could intervene in the SARS-CoV-2 infection [227]. Research tells us that RSV is associated with carboxymethyl beta-glucan (CMG), which increases its solubility and blocks the SARS-CoV-2 virus replication in human nasal epithelial cells [228]. RSV could play an important role in the regulation of the renin–angiotensin system (RAS) and activation of ACE 2 [229]. RSV works by activating sirtuin 1 (SIRT-1) [230], which has a protective role in response to stress, inflammation, and the regulation of apoptosis [231]. The activation of SIRT-1 and superoxide dismutase (SOD) of RSV is associated with increased ACE2 function and decreased markers of inflammation. Therefore, the upregulation of ACE by the RSV could play an essential role in SARS [232]. RSV modulates inflammatory components and exercises immunoregulatory effects. The red wine polyphenols have a positive effect on bacteria, which cause problems with teeth and gums. The 2% RSV emulgel is very effective in improving gum health in orthodontics, reducing gingival inflammation [233]. In particular, RSV has inhibitory properties on the cariogenic virulence of Streptococcus mutans, reducing acid production and biofilm formation. The expression of the related virulence gene was also downregulated with increasing RSV concentrations. RSV, therefore, represents a promising anti-cariogenic agent, reducing the ability of bacteria to stick to teeth and gums [114]. In addition, there are studies on periodontitis, particularly on the inflammatory responses induced by Porphyromonas gingivalis in human gingival fibroblasts [234]. The mechanism by which RSV can increase antioxidant enzymes in our body is the activation of the Nrf-2 gene, involved in the synthesis of the antioxidant molecules listed above [235]. RSV is considered to be more potent than vitamin E, one of the most potent antioxidants known to date [236].
Liu et al. [237] (Table 5) analyzed antimicrobial peptides (AMP: α- and β-defensins, cathelicidin LL-37, and statins 5), which have antimicrobial and immunostimulant properties, an important defense mechanism of the innate immune system against invading microorganisms. The bactericidal activities of AMP are due to the formation of pores in bacterial cytoplasmic membranes. Furthermore, having a distinctly positive charge, AMPs enhance the initial electrostatic attraction to negatively charged lipid membranes and negatively charged acids on the surface of Gram-positive bacteria, for example, Staphylococcus aureus, a common opportunistic human colonizer that may cause life-threatening diseases, such as sepsis, endocarditis, and pneumonia. The sensitization of S. aureus to AMPs of the innate immune system can facilitate the eradication of S. aureus. RSV exhibits antibacterial effects and is a presumed inhibitor of ATP synthase in S. aureus. This indicates that ATP synthase inhibition can be used to sensitize S. aureus to the natural AMps of the innate immune system. The ATP synthase inhibitor is RSV. Inhibitors can be adjuvants for antibiotics [223]. The mosquito-borne (Aedes mosquitoes) disease caused by a flavivirus is DENV, and it is endemic to tropical climate areas of the world. DENV fever [238] is generally high and sudden, characterized by headache, myalgia, arthralgia, generalized lymphadenopathy, and rash after a brief apyrexia, and, in addition, coughing, sore throat, and runny nose. DENV can also cause fatal fever with bleeding diathesis and shock. Zainal et al. demonstrate that RSV has antiviral activity against DENV. RSV suppresses DENV replication by inhibiting the translocation of the high-mobility group box 1 (HMGB1), a DNA-binding protein from the nucleus. The RSV inhibits this migration and increases the interferon-stimulated genes’ (ISG) transcription by nuclear HMGB1 (Table 5). RSV inhibits the translocation of HMGB1 out of the nucleus, allowing pro-inflammatory genes to be downregulated during DENV infection [14]. Yang [101] examined the action of RSV in inhibiting meningitic invasion of meningitic E. coli in the blood–brain barrier (BBB). RSV inhibits bacterial penetration of BBB, reduces neuroinflammation and lethality, reducing the inflammatory cytokines and the upregulation of caveolin-1 (CAV-1), a class of rafts that is supposed to function in endothelial cells. RSV may prove to be important in the inhibition and management of E. coli meningitis and may alleviate E. coli-induced meningitic CNS injury (Table 2). Hwang and Lim [239] found that, in the Escherichia coli, is the AcrAB-TolC multi-drug efflux pump (Table 5). The E. coli AcrAB-TolC complex often transports toxic compounds out of the cells, and this pump has importance in drug resistance: in cases where there are high AcrAB levels, they are measured in the cases of multi-resistance of antibiotic-resistant strains, such as MRSA (methicillin-resistant Staphylococcus aureus). Efflux pump inhibitors (EPIs) are interesting molecules to test as potential adjuvants for antibiotic treatment because they hinder multidrug resistance in E. coli. The key goal of RSV is to stop bacterial growth. RSV significantly cut the activity of the AcrAB-TolC drug efflux complex, promoting the antibacterial activity of RSV in E. coli [239]. Cold is a communal viral infection (rhinoviruses (HRVs)) that causes inflammation of the nasal mucosa and pharynx (throat). Both sick and healthy carriers can transmit highly contagious colds. The common cold has mild symptoms but can be severe in children. According to the results of Baldassarre et al. [108], the solution with RSV plus carboxymethyl-β-glucan in the treatment of childhood colds reduces respiratory symptoms and relapses (significant reduction in sternutation and episodes of productive or non-productive cough). In children, RSV with CM-glucan can alleviate nasal problems and breathing difficulties, for example, allergic rhinitis and acute nasopharyngitis (Table 2). Based on the information mentioned in the above articles, having an intestinal microbiota composed of symbiotic microorganisms in balance with the immune system is of fundamental importance in order to be able to carry out an effective defense against external pathogens to which one may be exposed. Conversely, a condition of imbalance of the microbiota and of our immune system leads to a dysbiosis that negatively predisposes both innate and acquired immune defense, compromising it. Therefore, by virtue of the prebiotic role of RSV and the role of the stimulator of the immune system, it is possible to affirm its usefulness as a preventive and adjuvant factor of traditional antibiotic therapies against many diseases caused by pathogens. For the reasons we have analyzed, it can be said that RSV can undoubtedly be considered an excellent supplement to our everyday eating habits. The results derived from immunological research have undoubtedly generated increasing enthusiasm as RSV displays remarkable antibacterial and antiviral properties, which is why it will be necessary to continue the study on RSV given that it keeps our immune system in a state of alert activity and influences the intestinal microbiota (Table 5).
Table 5.
Included studies that focus on the immune-system–microbiota–resveratrol axis.
| Ref. | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [237] | Liu et al. (2020) | Clinical trial | RSV exhibits antibacterial effects against S. aureus. | Human antimicrobial peptides | RSV exhibits antibacterial effect sand is a presumed inhibitor of ATP synthase in S. aureus. |
| [14] | Zainal et al. (2017) | Randomized controlled trial | RSV in dengue virus infection | RSV | RSV suppresses DENV replication |
| [101] | Yang et al. (2021) | Randomized controlled trial | RSV attenuates Meningitic Escherichia coli-mediated blood–brain barrier disruption | Different doses of RSV (5, 10, 25, and 50 μM | RSV inhibited meningitic E. coli, protecting the integrity of the BBB and lethality |
| [239] | Hwang e Lim (2019) | Research letter | RSV controls Escherichia coli growth | AcrAB-TolC multidrug efflux pump in E. coli | RSV gives inhibition of the AcrAB-TolC pump in E. coli. RSV might act as an efflux pump inhibitor |
| [108] | Baldassarre et al. (2020) | Randomized double-blind trial | RSV with CM-glucan in infants with common cold | Solution containing RSV plus carboxymethyl-β-glucan | RSV and CM-glucan can alleviate nasal symptoms and respiratory complications, such as allergic coryza and acute nasopharyngitis. |
3.4. Resveratrol and Microbiota Implications on Preventing Thrombotic Complications
Regarding the protective effect of RSV, a natural polymeric compound contained in grapes, it has antibacterial mechanisms against Staphylococcus aureus (S. aureus), reducing the inflammatory response in infected tissues [99]. RSV is a potentially useful agent in preventing thrombotic infections caused by the S. aureus strains responsible for major infectious diseases, such as osteomyelitis [212]. S. aureus is a GRAM+ bacterium with a spherical and aerobic shape that gives rise to colonies in which the microorganisms form a cluster arrangement. It is a very virulent bacterium capable of causing several diseases. It usually colonizes the skin and mucous membranes, and an effective immune system can keep the microorganism under control. However, in immune deficiency, it can spread through the bloodstream and affect joints and bones by establishing osteomyelitis. S. aureus induces an inflammatory reaction in the host, leading to the excessive and rapid recruitment of inflammatory cells [240]. Following the lysis of neutrophils, which are found to be the target of PVL toxins produced by S. aureus, pro-inflammatory substances such as IL-6, IL-8, and TNF-α are released. These are responsible for thrombus formation when associated with osteomyelitis [241,242]. PVL is a toxin associated with the development of thrombosis in patients with osteomyelitis. It is made of two parts (LukS-PV and LukF-PV) that create beta-barrel pores. The lukS-PV component binds to the complement receptor C5aR, and both components then result in the insertion of the hydrophobic stalk into the target cell membrane. Once damaged by PVL, Neutrophils release prothrombotic cytokines, antimicrobial alpha-defensins (HPNs), myeloperoxidase (HOCL), and myeloperoxidase-modified proteins. RSV can inhibit these substances from damaged neutrophils [243,244]. Thrombotic problems can occur in those with a weakened immune system, and high levels of PVL can be seen in the context of bone infections [100]. The toxin secreted by S. aureus plays a central role in the development of thrombosis due to the interaction between PVL toxin, neutrophils, and platelets [99]. PVL induces neutrophil lysis and the release of HPNs and HOCL [100,245,246]. HPNs activate platelets [247], accompanied by the conformational change in the platelet fibrinogen receptor GPIIb/IIIa, which increases its affinity, inducing the formation of microparticles that induce thrombin generation and thus are essential in thrombus development [248]. There is a two-step mechanism in the development of osteomyelitis produced by Staphylococcus aureus that is determined by the activity of PVLs on platelets: A high number of neutrophils accumulate at the site of osteomyelitis, which is lysed by PVLs, inducing them to release HNPs or myeloperoxidase and subsequently activating platelets either directly or through lysine-presenting proteins. This mechanism causes thrombosis through platelet aggregation [248]. RSV can counteract the platelet activation effects of HOCL-modified proteins and inhibit neutrophil myeloperoxidase. Moreover, it blocks PVL-induced fibrinogen-platelet binding. RSV protects vessels from plaque formation and proliferation of smooth muscle tissue, stimulates nitric oxide production responsible for vasodilation, and inhibits platelet activation and aggregation, the first step in blood clot formation [249]. As a result, S. aureus is one of the microorganisms that might cause life-threatening complications. It is important to prevent its virulence. S. aureus has long been suspected of having its primary reservoir in the nasal cavity [250]. Recent studies, however, have shown that S. aureus is part of the oral MB in greater quantity than the nasal one [251]. S. aureus, in a 2008 study, was also found to be common in the oral cavity, with the prevalence ranging from approximately 33% in dental plaque to 47% in saliva [252]. In addition, it is recognized that the use of dental prostheses numerically elevates oral pathogens. In these cases, proper oral hygiene is recommended to avoid the establishment of distant or local infections [78,251]. Some oral diseases are caused by this microorganism, e.g., angular cheilitis, mumps, staphylococcal mucositis, failure of dental implants [253]. MRSA species have also been isolated in the oral cavity. These species are difficult to treat with classical antibiotics because of their resistance. They are very dangerous because they can have the gene for PVL, causing the previously reported disruptions [254]. Based on the information mentioned, we firmly believe that the oral condition of S. aureus colonization must be maintained at nonvirulent levels to avoid the establishment of the described diseases. RSV, as pointed out, aids in the maintenance of the oral MB.
3.5. Resveratrol and Microbiota Implications in Gene Therapy
Given its remarkable and important biochemical characteristics, in recent years, RSV has also been studied as an adjuvant in cutting-edge technology. Gene therapy is a modern approach that involves the manipulation of genetic material to treat specific diseases. This manipulation allows replacing a defective or mutated gene with a valid one or modifying an existing gene to change its function [255]. This technique involves modifying the gene responsible for the genetic disease and inserting it into a DNA vector. The vectors most commonly used to transport genetic material are viral vectors due to their efficiency in invading cells and introducing their genetic material [256]. The rationale for the procedure is to get the vector to transport the functioning gene into the target cell and have it integrated into the DNA to treat the disease. The inserted foreign genetic material must be stable in the host cell in order for the therapy to be successful [257]. This technique has proven efficacy in treating several hematological disorders using hemopoietic stem cells as target cells [258,259]. Transduction resistance of hematopoietic stem cells is the major problem of lentiviral vector-mediated gene therapy [260], previously attributed to inhibition by the proteasome, the absence of vector receptor [261], or a cell in a quiescence state [262]. The interferon-induced transmembrane (IFITM) family of proteins also have intrinsic defensive effects against pathogens that use cellular endosomes for entry and transport. In particular, IFITM3 limits the gene delivery efficiency mediated by vesicular stomatitis virus (VSV) in hematopoietic stem cells [263]. Further, mTOR inhibitor rapamycin can block this process pharmacologically, but this results in numerous immunosuppressive side effects [264,265]. A study by Ozog et al. proposed to investigate RSV as a viable component to enhance gene transport in hematopoietic stem cells [266]. Therefore, in this study, RSV and some of its synthetic cyclic compounds were examined to enhance the lentiviral vector-mediated gene delivery in this type of cells. The results showed that only a synthetic compound, CaraphenolA, a synthetic RSV cyclotrimer of a higher oxidation state, was able to enhance gene delivery [266]. Specifically, Caraphenol A substantially improved gene delivery through a mechanism that resolves the impediment by the IFITM2/3 to the vector. Notably, the modulation by this compound did not result in unusual integration or lineage disorders in vivo [266]. In addition to being a good asset in bioengineering [266], RSV can be used as an adjuvant in the treatment of hematological cancer disorders and other tumors [267,268]. In fact, several studies have shown that its anti-tumor activity acts on several levels. It indirectly decreases oxidative and inflammatory stress by minimizing reactive oxygen species, inhibits the phase I cytochrome P450 enzymes responsible for carcinogen activation, induces the death of malignant cells, and suppresses the proinflammatory signaling pathways linked to cancer progression [118,120,267,269]. Moreover, patients with cancerous hematological disorders are significantly immunosuppressed due to chemotherapies that encourage the development of opportunistic infections linked to alterations in the MB that make it pathogenic [270,271]. In addition, individuals treated with hematopoietic cell transplantation (HCT) may develop graft-versus-host disease (GvHD), which severely attacks the gut. Bacteria, particularly the GM, have recently been recognized as important in the success of HCT and the onset of GvHD [272]. In particular, the lack of MB is a risk factor for treatment-related mortality, including death from GvHD, infection, opportunistic illness, and organ failure after HCT [273]. Therefore, with the mechanisms previously discussed in this paper, we suspect that RSV may also have a role in controlling the GM in this cancer scenario.
3.6. Resveratrol and Microbiota Implications in Bone Regeneration
Based on the literature, RSV can promote the differentiation of bone cells and the release of angiogenic factors that result in better bone vascularization with a greater supply of nutrients and growth factors. This leads to bone formation [274,275]. Zhang et al. [276] showed that RSV associated with strontium ranelate (SrRn) induces osteogenic differentiation of mesenchymal stem cells (MSCc). This aspect was deduced by an increase in alkaline phosphatase (ALP) activity with an increase in the expression of the transcription factor runt-related transcription factor 2 (RUNX-2), osteocalcin (OCN), and collagen 1A1 (Col 1A1). Other studies report that RSV influences the osteogenic differentiation of MSCs because bone morphogenic protein-2 (BMP-2) activates SIRT-1. The latter increases the activity of ALP and human osteoprotegerin (OPG) [274,277,278]. The Notch signaling pathway, which RSV activates, favors the conversion of osteoblasts into osteocytes [279]. Furthermore, in the study of Zhang et al., RSV increases the expression of the nuclear factor of activated T cells 1, which is present (NFATc1; transcription factor for the differentiation of osteoclasts [280]); RSV has no effect on the expression of Matrix Metalloproteinase-9 (MMP-9; metalloproteinase involved in the destruction of the extracellular [281]) and Cathepsin K (CTSK; protease involved in the degradation of collagen and in the bone resorption phase [282]) [276]. Some studies show that RSV inhibits the action of osteoclasts by activating the Wnt/β–catenin pathway [283,284]. Several studies state that RSV causes an increase in vascularization and, consequently, bone formation [275,276]. In the study included in our review, the effect of RSV on human umbilical vein endothelial cells (HUVEC) was evaluated. It was noted that RSV promoted angiogenesis by increasing VEGFA, platelet–endothelial cell adhesion molecule (PECAM), and von Willebrand factor (vWF) [276].
In the work of Zhang et al. [276], the following aspects were analyzed:
the differentiating power of the RSV associated or not with SrRn on the MSCs;
the inhibitory effect of RSV on osteoclasts;
the angiogenesis effect of RSV associated or not with SrRn on HUVEC;
Formation of bone in rats. Bone defects were induced on the mandible of rats and then rehabilitated with 3D scaffolds (loaded with a mixture of RSV, SrRn, or both). Four groups of rats were evaluated: rats with scaffold only, rats with scaffold + RVS, rats with scaffold + SrRn, and rats with scaffold + (RVS + SrRn).
The results of this study show that [276]:
MSCs proliferate and differentiate with a high rate on scaffolds with SrRn, and the rate is higher than that on scaffolds alone and on RVS scaffolds;
on the scaffolds with RVS, SrRn, or both, there was a reduction in the number and size of osteoclasts compared to that observed in the group with only the scaffold;
RVS scaffolds have a more significant angiogenesis effect than SrRn or scaffold-only groups;
The micro-computed tomography (CT) analysis showed high bone formation in rats in which scaffolds with RVS and SrRn were implanted compared to the other two groups.
Another study [95] evaluates, through the in vitro analysis, the action of RSV associated with CGF on the differentiation and proliferation of human osteoblasts. Furthermore, the protection of RSV on osteoblastic cells treated with bisphosphonates was evaluated. The bisphosphonates administered on osteoblastic cells in vitro are Alendronate (AL) and ZOL. These drugs are administered in diseases, i.e., osteoporosis, metastatic bone cancer, and Paget’s disease. Bone regeneration can be compromised by prolonged use of these drugs, resulting in necrosis of the maxillary and mandibular bone tissue (osteonecrosis) [285,286,287].
In the study by Borsani et al. [95], the control group is represented by human osteoblastic cells in osteoblast growth medium. This study highlighted that:
CGF and RSV (10 μM) have an osteogenic effect and protect osteoblasts treated with ZOL;
OPG levels are found to be elevated in osteoblasts treated with RSV (10 μM) and ZOL or CGF associated with RSV (10 μM) and ZOL. Meanwhile, in the treatment with AL, there is no increase in OPG;
the treatment with CGF, RSV (10 μM), and AL or CGF, RSV (10 μM), and ZOL resulted in a significant increase in BMP-2 (inducer of osteogenesis [288]) levels but less than in osteoblasts treated with CGF and ZOL;
in osteoblastic cells treated with RSV, CGF, and ZOL, there is an increase in SIRT-1 and Col 1A1;
human osteoblastic cells treated with RSV (10 μM) deposited significant amounts of calcium, unlike the control group (human osteoblast cells in osteoblast mineralization medium).
Numerous literature studies state that the influence of RSV on osteogenic differentiation, proliferation of human osteoblasts, and endothelial cells depends on the dose of the drug [289,290,291].
In the study by Zhang et al. [276], the concentration of RSV released from the scaffolds was equal to 2.15 ± 0.16 µg/mL, while, in the study by Borsani et al. [95], it is stated that the concentration that determines an increase in the proliferation of osteoblasts without cytotoxic effects is equal to 10 µM.
By adopting a concentration of RSV equal to 25 μM, Ornstrup et al. [292] observed that this stilbenoid has an osteogenic action but reduces the proliferation of MSCs. Furthermore, different authors [289,290,293] described that, for a concentration of RSV between 0.1 μM and 2.5 μM, there is an increase in the proliferation of MSCs deriving from the human umbilical cord (hUC-MSCs), while proliferation is reduced to concentrations between 5 μM and 10 μM. Finally, high concentrations of RSV inhibit angiogenesis and HUVEC migration [294]. Our analysis shows that RSV has an osteogenic action as it induces the multiplication and differentiation of MSCs and plays an essential role in angiogenesis given by the proliferation of HUVEC. The action of RSV seems to be empowered by SrRn as the latter should play a key role in inhibiting osteoclastogenesis. This leads to a reduction in bone reabsorption in favor of bone deposition. Furthermore, RSV protects human osteoblasts treated with bisphosphonates. This appears to be potentiated by CGF, which contains autologous platelet-derived osteoinductive growth factors. Thus, the RSV appears to modulate the effects of the CGF. Table 6 summarizes the results obtained.
Table 6.
Reported RSV results in bone regeneration.
| Ref. | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [276] | Zhang et.al 2020 |
Research in vitro |
|
|
|
| [95] | Borsani et.al 2018 |
Research in vitro | The researchers wanted to see how CGFs and/or resveratrol affected the proliferation and differentiation of human osteoblasts, whether they were treated with bisphosphonates or not. | Osteoblast growth medium (OGM): control group OGM + RSV 10 µM OGM + AL 5 µM OGM + ZOL 5 µM OGM + AL 5 µM +RSV 10 µM OGM + ZOL 5 µM +RSV 10 µM OGM + CGF OGM + CGF + RSV 10 µM OGM + CGF + AL 5 µM OGM + CGF + ZOL 5 µM OGM + CGF + RSV 10 µM + AL 5 µM OGM + CGF + RSV 10 µM + ZOL 5 µM |
|
Numerous studies have shown that RSV increases the expression levels of SIRT-1 [274,295,296] even in rats in which an ovariectomy has been performed. This leads to thinking about the positive effect of RSV in the case of post-menopausal osteoporosis [297,298,299,300]. Therefore, RSV has been shown to activate SIRT-1, causing osteogenic MSCs differentiation and proliferation [274,277,301]. This leads to bone formation [298,302,303]. RSV also promotes the conversion of osteoblasts to osteocytes via the Notch pathway [279]. RSV appears to have a protective effect against osteoblastic cells treated in vitro with bisphosphonates [95], and the study by Zhai et al. demonstrates that RSV prevents steroid-induced osteonecrosis in a group of rabbits [96].
Other studies show that RSV inhibits the action of osteoclasts by activating the Wnt/β–catenin pathway [283,304]. Several studies state that RSV causes an increase in vascularization and, therefore, bone formation [275,302,305]. RSV increases osteoblast proliferation while inhibiting osteoclast differentiation [306,307], making it a promising candidate for research in dentistry and maxillofacial surgery [95,276,308,309,310,311]. Due to the minimal capacity to trigger an immune response, bone regeneration is currently carried out with autologous transplants [312]. The utilization of MSCs is a novel strategy, but it has a critical drawback: harvesting difficulty and poor long-term stability. Another option is to employ biomaterials; however, the clinical guidelines for doing so are currently unknown [313]. RSV, which is isolated from natural sources, triggers pathways that lead to osteoblastic development and differentiation [95,276,314]. As a result, administering RSV could be a viable therapeutic option for the processes of bone repair and defect restoration [315]. As demonstrated in the study by Zhang et al. [276], using RSV alone or combined with scaffolds can improve the clinical management of diseases such as osteonecrosis of the jaw caused by long-term bisphosphonate medication.
4. Conclusions
RSV has long been recognized for its anti-inflammatory, antifungal, antioxidant, antithrombotic, anticoagulant, antitumor, antiviral, and immune properties. Therefore, it can bring multiple beneficial effects to the body as it plays an essential role in preventing many pathologies by positively modulating the human GM. Its anti-inflammatory action is due to the activation of SIRT-1, which inhibits the formation of inflammatory factors, such as NF-kB, which stimulates the immune system to produce pro-inflammatory cytokines (such as TNF-α, IL-1β, IL-6) and cyclooxygenases (COX-1 and 2), thus reducing oxidative stress. In addition, the activation of the Nrf-2 gene, which is involved in synthesizing antioxidant molecules, enhances its antiphlogistic abilities. During an infectious process, RSV exerts its antimicrobial activity by recruiting and activating macrophages, neutrophils, and lymphocytes. In the oral cavity, RSV has inhibitory properties on the karyogenic virulence of Streptococcus mutans, reducing acid production and biofilm formation. Used as a nasal spray or aerosol, RSV combined with carboxymethyl-β-glucan has reduced the use of antihistamines and nasal decongestants in allergic rhinitis and the common cold, improving symptoms, such as cough, rhinorrhea, nasal congestion, sneezing, sore throat, and fever. At the level of bone metabolism, the study shows that RSV, by activating SIRT-1, promotes osteogenic proliferation by the differentiation of MSCs and angiogenetic proliferation because it stimulates the proliferation and migration of HUVECs. RSV associated with SrRn inhibits osteoclastogenesis by reducing bone resorption and promoting bone synthesis. RSV associated with CGF enhances its protective effects against osteonecrosis of the jaws, induced by taking bisphosphonates, by promoting osteoinductive processes and angiogenesis. Osteoblastic and angiogenetic activation are closely related to low doses of RSV administration. Due to its antioxidant and anti-inflammatory capacities, inhibiting cytochrome P450 phase I enzymes responsible for cancer activation, RSV can be used as an adjuvant in various tumor diseases. The activation of TANK-binding kinase 1 (TBK1), whose insufficient activity would lead to autoimmune, neurodegenerative, or oncogenic diseases, is one of the main anti-tumor mechanisms of RSV. Due to its biochemical characteristics, RSV has been studied in bioengineering for gene therapy. This technique is mainly used on hematological problems using hemopoietic stem cells as target cells.
The use of Carafenol A, an RSV cyclotrimer, facilitated the insertion of the gene into the predetermined sequence, activating the cellular mechanisms that eliminated the IFITM2/3 obstacle to the vector without creating lineage abnormalities in vivo. Recent scientific studies have validated the relevant role of polyphenols on MB and their influence on intestinal well-being. There is a clear interaction between GM and RSV as if the former were a target of the latter, regulating intestinal homeostasis in response to oxidation processes. The beneficial activity of RSV is evident by analyzing changes in the genetic expression of the host and the intestinal microbial community with its administration. Today, the four “omics” sciences: metagenomics, transcriptomics, proteomics, and metabolomics, allow us to study genomic sequencing, transcription, protein synthesis, and the composition of metabolites present in the biosystem.
The possibility of identifying individual microbial families and classifying the composition of the MB would allow us to customize preventive and therapeutic treatment plans with targeted polyphenolic diets when associated with microbial dysbiosis, such as inflammatory diseases of the gastrointestinal tract, degenerative diseases, tumors, obesity, diabetes, bone tissue regeneration, and metabolic syndrome in general.
Author Contributions
Conceptualization, A.D.I., A.M.I., G.D., F.L., A.S. (Antonio Scarano), D.H., Z.K., G.M.T., G.C., D.A., S.C., A.M., A.C., L.M., F.P., K.F., A.B.F. and F.I.; methodology, A.D.I., I.R.B., F.P., G.D., C.M., V.S., D.H., G.C., F.L., F.I., G.P., V.M., A.P., A.S. (Antonio Scarano), B.R., C.D.P., G.G., L.N., M.D.F. and L.M.; software, I.R.B., F.L., A.T., M.T.D., M.G.G., N.D.L., G.M.T., I.R.B., A.S. (Antonio Scarano), A.D.I., M.D.F., A.C., S.C., G.M. G.C., L.M., N.B., A.C., A.S. (Antonio Scarano) and F.I.; validation, F.I., F.L., A.M.I., I.R.B., G.P., V.S., G.G., F.P., C.M., A.S. (Alexandra Semjonova), N.B., V.S., A.C., F.P., G.P., A.P. and A.S (Antonio Scarano).; formal analysis, S.C., L.N., N.D.L., A.C., F.L., G.M.T., A.M., B.R., G.M. A.S. (Alexandra Semjonova), M.D.F. and A.D.I.; investigation, A.T., Z.K., M.T.D., M.G.G., G.M. G.D., A.D.I., F.L., S.C., G.C., A.C., C.D.P., A.S. (Antonio Scarano) and F.I.; resources, A.D.I., F.I., A.M.I., I.R.B., M.T.D., K.F., S.C., V.M., A.C., A.S. (Antonio Scarano), B.R. and G.M. data curation, F.I., F.L., K.F., A.B.F., L.N., G.G., A.S. (Antonio Scarano), G.M. A.M., A.S. (Alexandra Semjonova), M.D.F., K.F., A.B.F., V.S., A.C., F.P. and F.I.; writing original draft preparation, A.D.I., G.D., S.C., M.J., A.C., A.P., L.M., A.S. (Antonio Scarano), F.L., I.R.B., G.M., B.R., A.M.I. and F.I.; writing review and editing, F.I., F.L., I.R.B., N.B., G.M., A.D.I., A.S. (Antonio Scarano) and G.D.; visualization, F.L., A.S. (Antonio Scarano), F.I., G.D. and I.R.B.; supervision, F.I., F.L., N.B., A.P., I.R.B., Z.K., S.C., A.S. (Antonio Scarano) and A.C.; project administration, F.I., C.M., M.D.F., D.H., G.M.T., N.B., A.S. (Antonio Scarano), L.M., L.N., G.M., A.S. (Antonio Scarano), F.L., A.D.I., G.D., A.M.I. and N.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The present systematic review has been performed in accordance to the principles of the PRISMA and International Prospective Register of Systematic Review Registry guidelines (PROSPERO n. 313242).
Informed Consent Statement
Not applicable.
Data Availability Statement
All experimental data to support the findings of this study are available by contacting the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rapone B., Ferrara E., Montemurro N., Converti I., Loverro M., Loverro M.T., Gnoni A., Scacco S., Siculella L., Corsalini M., et al. Oral microbiome and preterm birth: Correlation or coincidence? A narrative review. Open Access Maced. J. Med. Sci. 2020;8:123–132. doi: 10.3889/oamjms.2020.4444. [DOI] [Google Scholar]
- 2.Inchingolo F., Santacroce L., Ballini A., Topi S., Dipalma G., Haxhirexha K., Bottalico L., Charitos I.A. Oral Cancer: A Historical Review. Int. J. Environ. Res. Public Health. 2020;17:3168. doi: 10.3390/ijerph17093168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orallo F. Trans-resveratrol: A magical elixir of eternal youth? Curr. Med. Chem. 2008;15:1887–1898. doi: 10.2174/092986708785132951. [DOI] [PubMed] [Google Scholar]
- 4.Inchingolo A.D., Inchingolo A.M., Bordea I.R., Malcangi G., Xhajanka E., Scarano A., Lorusso F., Farronato M., Tartaglia G.M., Isacco C.G., et al. SARS-CoV-2 Disease Adjuvant Therapies and Supplements Breakthrough for the Infection Prevention. Microorganisms. 2021;9:525. doi: 10.3390/microorganisms9030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad I. An Update on Pharmacological Relevance and Chemical Synthesis of Natural Products and Derivatives with Anti SARS-CoV-2 Activity. Chemistryselect. 2021;6:11502–11527. doi: 10.1002/slct.202103301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Venere D., Pettini F., Nardi G.M., Laforgia A., Stefanachi G., Notaro V., Rapone B., Grassi F.R., Corsalini M. Correlation between parodontal indexes and orthodontic retainers: Prospective study in a group of 16 patients. Oral Implantol. 2017;10:78–86. doi: 10.11138/orl/2017.10.1.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abba Y., Hassim H., Hamzah H., Noordin M.M. Antiviral Activity of Resveratrol against Human and Animal Viruses. Adv. Virol. 2015;2015:184241. doi: 10.1155/2015/184241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Santi C., Pietrabissa A., Spisni R., Mosca F., Pacifici G.M. Sulphation of resveratrol, a natural compound present in wine, and its inhibition by natural flavonoids. Xenobiotica. 2000;30:857–866. doi: 10.1080/004982500433282. [DOI] [PubMed] [Google Scholar]
- 9.Frémont L. Biological effects of resveratrol. Life Sci. 2000;66:663–673. doi: 10.1016/S0024-3205(99)00410-5. [DOI] [PubMed] [Google Scholar]
- 10.Liu F.-C., Tsai Y.-F., Tsai H.-I., Yu H.-P. Anti-Inflammatory and Organ-Protective Effects of Resveratrol in Trauma-Hemorrhagic Injury. Mediat. Inflamm. 2015;2015:e643763. doi: 10.1155/2015/643763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olas B., Wachowicz B. Resveratrol, a phenolic antioxidant with effects on blood platelet functions. Platelets. 2005;16:251–260. doi: 10.1080/09537100400020591. [DOI] [PubMed] [Google Scholar]
- 12.Grassi F.R., Rapone B., Scarano Catanzaro F., Corsalini M., Kalemaj Z. Effectiveness of computer-assisted anesthetic delivery system (STA™) in dental implant surgery: A prospective study. Oral Implantol. 2017;10:381–389. doi: 10.11138/orl/2017.10.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin S.-C., Ho C.-T., Chuo W.-H., Li S., Wang T.T., Lin C.-C. Effective inhibition of MERS-CoV infection by resveratrol. BMC Infect. Dis. 2017;17:144. doi: 10.1186/s12879-017-2253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zainal N., Chang C.-P., Cheng Y.-L., Wu Y.-W., Anderson R., Wan S.-W., Chen C.-L., Ho T.-S., AbuBakar S., Lin Y.-S. Resveratrol treatment reveals a novel role for HMGB1 in regulation of the type 1 interferon response in dengue virus infection. Sci. Rep. 2017;7:42998. doi: 10.1038/srep42998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santacroce L. The pivotal role of oral microbiota in health and disease. J. Biol. Regul. Homeost. AGENTS. 2020;34:733–737. doi: 10.23812/20-127-L-45. [DOI] [PubMed] [Google Scholar]
- 16.Asgary S., Karimi R., Momtaz S., Naseri R., Farzaei M.H. Effect of resveratrol on metabolic syndrome components: A systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 2019;20:173–186. doi: 10.1007/s11154-019-09494-z. [DOI] [PubMed] [Google Scholar]
- 17.Microbiota e microbioma: Quali sono le differenze? Microbioma.It. 2017. [(accessed on 16 February 2022)]. Available online: https://microbioma.it/gastroenterologia/microbiota-e-microbioma-quale-differenza/#:~:text=Microbiota%20si%20riferisce%20a%20una,%C3%A8%20in%20grado%20di%20esprimere.
- 18.Metagenomica: Cos’è, Fasi Dell’analisi Metagenomica e Campi Applicative. [(accessed on 16 February 2022)]. Available online: https://www.microbiologiaitalia.it/didattica/metagenomica-cose-e-campi-applicativi/
- 19.Rapone B., Palmisano C., Ferrara E., Di Venere D., Albanese G., Corsalini M. The Accuracy of Three Intraoral Scanners in the Oral Environment with and without Saliva: A Comparative Study. Appl. Sci. 2020;10:7762. doi: 10.3390/app10217762. [DOI] [Google Scholar]
- 20.Maglione M., Bevilacqua L., Dotto F., Costantinides F., Lorusso F., Scarano A. Observational Study on the Preparation of the Implant Site with Piezosurgery vs. Drill: Comparison between the Two Methods in Terms of Postoperative Pain, Surgical Times, and Operational Advantages. BioMed Res. Int. 2019;2019:8483658. doi: 10.1155/2019/8483658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fiehn O., Kloska S., Altmann T. Integrated studies on plant biology using multiparallel techniques. Curr. Opin. Biotechnol. 2001;12:82–86. doi: 10.1016/S0958-1669(00)00165-8. [DOI] [PubMed] [Google Scholar]
- 22.Fiehn O. Combining Genomics, Metabolome Analysis, and Biochemical Modelling to Understand Metabolic Networks. Comp. Funct. Genomics. 2001;2:155–168. doi: 10.1002/cfg.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodacre R., Vaidyanathan S., Dunn W.B., Harrigan G.G., Kell D.B. Metabolomics by numbers: Acquiring and understanding global metabolite data. Trends Biotechnol. 2004;22:245–252. doi: 10.1016/j.tibtech.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Hasan M.R., Suleiman M., Pérez-López A. Metabolomics in the Diagnosis and Prognosis of COVID-19. Front. Genet. 2021;12:1358. doi: 10.3389/fgene.2021.721556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hyvärinen E., Savolainen M., Mikkonen J.J.W., Kullaa A.M. Salivary Metabolomics for Diagnosis and Monitoring Diseases: Challenges and Possibilities. Metabolites. 2021;11:587. doi: 10.3390/metabo11090587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Korsholm A.S., Kjær T.N., Ornstrup M.J., Pedersen S.B. Comprehensive Metabolomic Analysis in Blood, Urine, Fat, and Muscle in Men with Metabolic Syndrome: A Randomized, Placebo-Controlled Clinical Trial on the Effects of Resveratrol after Four Months’ Treatment. Int. J. Mol. Sci. 2017;18:554. doi: 10.3390/ijms18030554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Venere D., Corsalini M., Nardi G.M., Laforgia A., Grassi F.R., Rapone B., Pettini F. Obstructive site localization in patients with Obstructive Sleep Apnea Syndrome: A comparison between otolaryngologic data and cephalometric values. Oral Implantol. 2017;10:295–310. doi: 10.11138/orl/2017.10.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pacifici A., Pacifici L., Nuzzolese M., Cascella G., Ballini A., Santacroce L., Dipalma G., Aiello E., Amantea M., Saini R., et al. The alteration of stress-related physiological parameters after probiotics administration in oral surgeons with different degrees of surgical experience. Clin. Ter. 2020;171:e197–e208. doi: 10.7417/CT.2020.2214. [DOI] [PubMed] [Google Scholar]
- 29.Inchingolo F. Probiotics and EpiCor® in human health. J. Biol. Regul. Homeost. AGENTS. 2019;33:1973–1979. doi: 10.23812/19-543-L. [DOI] [PubMed] [Google Scholar]
- 30.Ceci S., Berate P., Candrea S., Babtan A.-M., Azzollini D., Piras F., Curatoli L., Corriero A., Patano A., Valente F., et al. The oral and gut microbiota: Beyond a short communication. Balneo PRM Res. J. 2021:405–411. doi: 10.12680/balneo.2021.471. [DOI] [Google Scholar]
- 31.Di Venere D., Nardi G.M., Lacarbonara V., Laforgia A., Stefanachi G., Corsalini M., Grassi F.R., Rapone B., Pettini F. Early mandibular canine-lateral incisor transposition: Case Report. Oral Implantol. 2017;10:181–189. doi: 10.11138/orl/2017.10.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malcangi G., Inchingolo A.D., Inchingolo A.M., Santacroce L., Marinelli G., Mancini A., Vimercati L., Maggiore M.E., D’Oria M.T., Hazballa D., et al. COVID-19 Infection in Children, Infants and Pregnant Subjects: An Overview of Recent Insights and Therapies. Microorganisms. 2021;9:1964. doi: 10.3390/microorganisms9091964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balzanelli M.G., Distratis P., Dipalma G., Vimercati L., Catucci O., Amatulli F., Cefalo A., Lazzaro R., Palazzo D., Aityan S.K., et al. Immunity Profiling of COVID-19 Infection, Dynamic Variations of Lymphocyte Subsets, a Comparative Analysis on Four Different Groups. Microorganisms. 2021;9:2036. doi: 10.3390/microorganisms9102036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rapone B., Ferrara E., Corsalini M., Converti I., Grassi F.R., Santacroce L., Topi S., Gnoni A., Scacco S., Scarano A., et al. The Effect of Gaseous Ozone Therapy in Conjunction with Periodontal Treatment on Glycated Hemoglobin Level in Subjects with Type 2 Diabetes Mellitus: An Unmasked Randomized Controlled Trial. Int. J. Environ. Res. Public Health. 2020;17:5467. doi: 10.3390/ijerph17155467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patano A., Cirulli N., Beretta M., Plantamura P., Inchingolo A.D., Inchingolo A.M., Bordea I.R., Malcangi G., Marinelli G., Scarano A., et al. Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:6056. doi: 10.3390/ijerph18116056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inchingolo A.D., Inchingolo A.M., Bordea I.R., Malcangi G., Xhajanka E., Scarano A., Lorusso F., Farronato M., Tartaglia G.M., Isacco C.G., et al. SARS-CoV-2 Disease through Viral Genomic and Receptor Implications: An Overview of Diagnostic and Immunology Breakthroughs. Microorganisms. 2021;9:793. doi: 10.3390/microorganisms9040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balzanelli M.G., Distratis P., Lazzaro R., Cefalo A., Catucci O., Aityan S.K., Dipalma G., Vimercati L., Inchingolo A.D., Maggiore M.E., et al. The Vitamin D, IL-6 and the eGFR Markers a Possible Way to Elucidate the Lung–Heart–Kidney Cross-Talk in COVID-19 Disease: A Foregone Conclusion. Microorganisms. 2021;9:1903. doi: 10.3390/microorganisms9091903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malcangi G., Inchingolo A.D., Inchingolo A.M., Piras F., Settanni V., Garofoli G., Palmieri G., Ceci S., Patano A., Mancini A., et al. COVID-19 Infection in Children and Infants: Current Status on Therapies and Vaccines. Children. 2022;9:249. doi: 10.3390/children9020249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vimercati L., De Maria L., Quarato M., Caputi A., Gesualdo L., Migliore G., Cavone D., Sponselli S., Pipoli A., Inchingolo F., et al. Association between Long COVID and Overweight/Obesity. J. Clin. Med. 2021;10:4143. doi: 10.3390/jcm10184143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Balzanelli M.G. Sars-CoV-2 Virus Infection May Interfere CD34+ Hematopoietic Stem Cells and Megakaryocyte–Erythroid Progenitors Differentiation Contributing to Platelet Defection towards Insurgence of Thrombocytopenia and Thrombophilia. Microorganisms. 2021;9:1632. doi: 10.3390/microorganisms9081632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Inchingolo A.D., Dipalma G., Inchingolo A.M., Malcangi G., Santacroce L., D’Oria M.T., Isacco C.G., Bordea I.R., Candrea S., Scarano A., et al. The 15-Months Clinical Experience of SARS-CoV-2: A Literature Review of Therapies and Adjuvants. Antioxidants. 2021;10:881. doi: 10.3390/antiox10060881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scarano A., Inchingolo F., Rapone B., Festa F., Rexhep Tari S., Lorusso F. Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. Int. J. Environ. Res. Public Health. 2021;18:2363. doi: 10.3390/ijerph18052363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Balzanelli M.G., Ballini A., Gargiulo Isacco C. Mesenchymal Stem Cells: The Secret Children’s Weapons against the SARS-CoV-2 Lethal Infection. Appl. Sci. 2021;11:1696. doi: 10.3390/app11041696. [DOI] [Google Scholar]
- 44.Charitos I.A., Prete R.D., Inchingolo F., Mosca A., Carretta D., Ballini A., Santacroce L. What we have learned for the future about COVID-19 and healthcare management of it? Acta Bio Med. Atenei Parm. 2020;91:e2020126. doi: 10.23750/abm.v91i4.10253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balzanelli M.G., Distratis P., Aityan S.K., Amatulli F., Catucci O., Cefalo A., De Michele A., Dipalma G., Inchingolo F., Lazzaro R., et al. An Alternative “Trojan Horse” Hypothesis for COVID-19: Immune Deficiency of IL-10 and SARS-CoV-2 Biology. Endocr. Metab. Immune Disord. Drug Targets. 2021;22:1–5. doi: 10.2174/1871530321666210127141945. [DOI] [PubMed] [Google Scholar]
- 46.Santacroce L., Inchingolo F., Topi S., Del Prete R., Di Cosola M., Charitos I.A., Montagnani M. Potential beneficial role of probiotics on the outcome of COVID-19 patients: An evolving perspective. Diabetes Metab. Syndr. 2021;15:295–301. doi: 10.1016/j.dsx.2020.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bordea I.R., Xhajanka E., Candrea S., Bran S., Onișor F., Inchingolo A.D., Malcangi G., Pham V.H., Inchingolo A.M., Scarano A., et al. Coronavirus (SARS-CoV-2) Pandemic: Future Challenges for Dental Practitioners. Microorganisms. 2020;8:1704. doi: 10.3390/microorganisms8111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Scarano A., Inchingolo F., Lorusso F. Environmental Disinfection of a Dental Clinic during the Covid-19 Pandemic: A Narrative Insight. [(accessed on 4 November 2020)]. Available online: https://www.hindawi.com/journals/bmri/2020/8896812/ [DOI] [PMC free article] [PubMed]
- 49.Santacroce L., Charitos I.A., Ballini A., Inchingolo F., Luperto P., De Nitto E., Topi S. The Human Respiratory System and its Microbiome at a Glimpse. Biology. 2020;9:E318. doi: 10.3390/biology9100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bellocchio L., Bordea I.R., Ballini A., Lorusso F., Hazballa D., Isacco C.G., Malcangi G., Inchingolo A.D., Dipalma G., Inchingolo F., et al. Environmental Issues and Neurological Manifestations Associated with COVID-19 Pandemic: New Aspects of the Disease? Int. J. Environ. Res. Public Health. 2020;17:8049. doi: 10.3390/ijerph17218049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Charitos I.A., Ballini A., Bottalico L., Cantore S., Passarelli P.C., Inchingolo F., D’Addona A., Santacroce L. Special features of SARS-CoV-2 in daily practice. World J. Clin. Cases. 2020;8:3920–3933. doi: 10.12998/wjcc.v8.i18.3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scarano A., Inchingolo F., Lorusso F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. Int. J. Environ. Res. Public Health. 2020;17:4624. doi: 10.3390/ijerph17134624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anhê F.F., Roy D., Pilon G., Dudonné S., Matamoros S., Varin T.V., Garofalo C., Moine Q., Desjardins Y., Levy E., et al. A polyphenol-rich cranberry extract protects from diet-induced obesity, insulin resistance and intestinal inflammation in association with increased Akkermansia spp. population in the gut microbiota of mice. Gut. 2015;64:872–883. doi: 10.1136/gutjnl-2014-307142. [DOI] [PubMed] [Google Scholar]
- 54.Nargeh H., Aliabadi F., Ajami M., Pazoki-Toroudi H. Role of Polyphenols on Gut Microbiota and ubiquitin-proteasome system in Neurodegenerative diseases. J. Agric. Food Chem. 2021;69:6119–6144. doi: 10.1021/acs.jafc.1c00923. [DOI] [PubMed] [Google Scholar]
- 55.Beilby J. Definition of Metabolic Syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Clin. Biochem. Rev. 2004;25:195–198. [Google Scholar]
- 56.Rapone B., Ferrara E., Corsalini M., Qorri E., Converti I., Lorusso F., Delvecchio M., Gnoni A., Scacco S., Scarano A. Inflammatory Status and Glycemic Control Level of Patients with Type 2 Diabetes and Periodontitis: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health. 2021;18:3018. doi: 10.3390/ijerph18063018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Walker J.M., Eckardt P., Aleman J.O., da Rosa J.C., Liang Y., Iizumi T., Etheve S., Blaser M.J., Breslow J.L., Holt P.R. The effects of trans-resveratrol on insulin resistance, inflammation, and microbiota in men with the metabolic syndrome: A pilot randomized, placebo controlled clinical trial. J. Clin. Transl. Res. 2018;4:122–135. doi: 10.18053/jctres.04.201802.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ballini A., Santacroce L., Cantore S., Bottalico L., Dipalma G., De Vito D., Saini R., Inchingolo F. Probiotics Improve Urogenital Health in Women. Open Access Maced. J. Med. Sci. 2018;6:1845–1850. doi: 10.3889/oamjms.2018.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frojdo S., Durand C., Pirola L. Metabolic Effects of Resveratrol in Mammals—A Link Between Improved Insulin Action and Aging. Curr. Aging Sci. 2008;1:145–151. doi: 10.2174/1874609810801030145. [DOI] [PubMed] [Google Scholar]
- 60.Crandall J.P., Oram V., Trandafirescu G., Reid M., Kishore P., Hawkins M., Cohen H.W., Barzilai N. Pilot Study of Resveratrol in Older Adults With Impaired Glucose Tolerance. J. Gerontol. A. Biol. Sci. Med. Sci. 2012;67:1307–1312. doi: 10.1093/gerona/glr235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Knop F.K., Konings E., Timmers S., Schrauwen P., Holst J.J., Blaak E.E. Thirty days of resveratrol supplementation does not affect postprandial incretin hormone responses, but suppresses postprandial glucagon in obese subjects. Diabet. Med. J. Br. Diabet. Assoc. 2013;30:1214–1218. doi: 10.1111/dme.12231. [DOI] [PubMed] [Google Scholar]
- 62.Dolinsky V.W., Dyck J.R.B. Calorie restriction and resveratrol in cardiovascular health and disease. Biochim. Biophys. Acta BBA-Mol. Basis Dis. 2011;1812:1477–1489. doi: 10.1016/j.bbadis.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 63.Quaglia E., Moscufo L., Corsalini M., Coscia D., Sportelli P., Cantatore F., De Rinaldis C., Rapone B., Carossa M., Carossa S. Polyamide vs silk sutures in the healing of postextraction sockets: A split mouth study. Oral Implantol. 2018;11:115–120. doi: 10.11138/orl/2018.11.2.115. [DOI] [Google Scholar]
- 64.Rapone B., Ferrara E., Santacroce L., Topi S., Gnoni A., Dipalma G., Mancini A., Di Domenico M., Tartaglia G.M., Scarano A., et al. The Gaseous Ozone Therapy as a Promising Antiseptic Adjuvant of Periodontal Treatment: A Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health. 2022;19:985. doi: 10.3390/ijerph19020985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tomás-Barberán F.A., Selma M.V., Espín J.C. Interactions of gut microbiota with dietary polyphenols and consequences to human health. Curr. Opin. Clin. Nutr. Metab. Care. 2016;19:471–476. doi: 10.1097/MCO.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 66.Carrera-Quintanar L., Roa R.I.L., Quintero-Fabián S., Sánchez-Sánchez M.A., Vizmanos B., Ortuño-Sahagún D. Phytochemicals That Influence Gut Microbiota as Prophylactics and for the Treatment of Obesity and Inflammatory Diseases. Mediat. Inflamm. 2018;2018:9734845. doi: 10.1155/2018/9734845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bode L.M., Bunzel D., Huch M., Cho G.-S., Ruhland D., Bunzel M., Bub A., Franz C.M., Kulling S.E. In vivo and in vitro metabolism of trans-resveratrol by human gut microbiota. Am. J. Clin. Nutr. 2013;97:295–309. doi: 10.3945/ajcn.112.049379. [DOI] [PubMed] [Google Scholar]
- 68.Rapone B., Corsalini M., Converti I., Loverro M.T., Gnoni A., Trerotoli P., Ferrara E. Does Periodontal Inflammation Affect Type 1 Diabetes in Childhood and Adolescence? A Meta-Analysis. Front. Endocrinol. 2020;11:278. doi: 10.3389/fendo.2020.00278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ávila-Gálvez M.Á., González-Sarrías A., Martínez-Díaz F., Abellán B., Martínez-Torrano A.J., Fernández-López A.J., Giménez-Bastida J.A., Espín J.C. Disposition of Dietary Polyphenols in Breast Cancer Patients’ Tumors, and Their Associated Anticancer Activity: The Particular Case of Curcumin. Mol. Nutr. Food Res. 2021;65:e2100163. doi: 10.1002/mnfr.202100163. [DOI] [PubMed] [Google Scholar]
- 70.Jarosova V., Vesely O., Marsik P., Jaimes J., Smejkal K., Kloucek P., Havlik J. Metabolism of Stilbenoids by Human Faecal Microbiota. Molecules. 2019;24:1155. doi: 10.3390/molecules24061155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ballini A., Gnoni A., Vito D.D., Dipalma G., Cantore S., Isacco C.G., Saini R., Santacroce L., Topi S., Scarano A., et al. Effect of probiotics on the occurrence of nutrition absorption capacities in healthy children: A randomized double-blinded placebo-controlled pilot study. Eur. Rev. Med. Pharmacol. Sci. 2019;23:8645–8657. doi: 10.26355/eurrev_201910_19182. [DOI] [PubMed] [Google Scholar]
- 72.Tsang S.W., Guan Y.-F., Wang J., Bian Z.-X., Zhang H.-J. Inhibition of pancreatic oxidative damage by stilbene derivative dihydro-resveratrol: Implication for treatment of acute pancreatitis. Sci. Rep. 2016;6:22859. doi: 10.1038/srep22859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dihydro-Resveratrol Ameliorates Lung Injury in Rats with Cerulein-Induced Acute Pancreatitis-Lin-2016-Phytotherapy Research—Wiley Online Library. [(accessed on 16 February 2022)]. Available online: https://onlinelibrary.wiley.com/doi/10.1002/ptr.5576. [DOI] [PubMed]
- 74.Bustos I., García-Cayuela T., Hernández-Ledesma B., Peláez C., Requena T., Martínez-Cuesta M.C. Effect of flavan-3-ols on the adhesion of potential probiotic lactobacilli to intestinal cells. J. Agric. Food Chem. 2012;60:9082–9088. doi: 10.1021/jf301133g. [DOI] [PubMed] [Google Scholar]
- 75.Etxeberria U., Fernández-Quintela A., Milagro F.I., Aguirre L., Martínez J.A., Portillo M.P. Impact of polyphenols and polyphenol-rich dietary sources on gut microbiota composition. J. Agric. Food Chem. 2013;61:9517–9533. doi: 10.1021/jf402506c. [DOI] [PubMed] [Google Scholar]
- 76.Jaimes J.D., Jarosova V., Vesely O., Mekadim C., Mrazek J., Marsik P., Killer J., Smejkal K., Kloucek P., Havlik J. Effect of Selected Stilbenoids on Human Fecal Microbiota. Molecules. 2019;24:744. doi: 10.3390/molecules24040744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Espín J.C., González-Sarrías A., Tomás-Barberán F.A. The gut microbiota: A key factor in the therapeutic effects of (poly)phenols. Biochem. Pharmacol. 2017;139:82–93. doi: 10.1016/j.bcp.2017.04.033. [DOI] [PubMed] [Google Scholar]
- 78.Contaldo M., Fusco A., Stiuso P., Lama S., Gravina A.G., Itro A., Federico A., Itro A., Dipalma G., Inchingolo F., et al. Oral Microbiota and Salivary Levels of Oral Pathogens in Gastro-Intestinal Diseases: Current Knowledge and Exploratory Study. Microorganisms. 2021;9:1064. doi: 10.3390/microorganisms9051064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ballini A., Dipalma G., Isacco C.G., Boccellino M., Di Domenico M., Santacroce L., Nguyễn K.C.D., Scacco S., Calvani M., Boddi A., et al. Oral Microbiota and Immune System Crosstalk: A Translational Research. Biology. 2020;9:131. doi: 10.3390/biology9060131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Volstatova T., Marsik P., Rada V., Geigerova M., Havlik J. Effect of apple extracts and selective polyphenols on the adhesion of potential probiotic strains of Lactobacillus gasseri R and Lactobacillus casei FMP. J. Funct. Foods. 2017;35:391–397. doi: 10.1016/j.jff.2017.06.005. [DOI] [Google Scholar]
- 81.Cueva C., Gil-Sánchez I., Ayuda-Durán B., González-Manzano S., González-Paramás A.M., Santos-Buelga C., Bartolomé B., Moreno-Arribas M.V. An Integrated View of the Effects of Wine Polyphenols and Their Relevant Metabolites on Gut and Host Health. Molecules. 2017;22:E99. doi: 10.3390/molecules22010099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Koliada A., Syzenko G., Moseiko V., Budovska L., Puchkov K., Perederiy V., Gavalko Y., Dorofeyev A., Romanenko M., Tkach S., et al. Association between body mass index and Firmicutes/Bacteroidetes ratio in an adult Ukrainian population. BMC Microbiol. 2017;17:120. doi: 10.1186/s12866-017-1027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ballini A., Santacroce L., Cantore S., Bottalico L., Dipalma G., Topi S., Saini R., De Vito D., Inchingolo F. Probiotics Efficacy on Oxidative Stress Values in Inflammatory Bowel Disease: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Endocr. Metab. Immune Disord.-Drug Targets. 2019;19:373–381. doi: 10.2174/1871530319666181221150352. [DOI] [PubMed] [Google Scholar]
- 84.Ozdal T., Sela D., Xiao J., Boyacioglu D., Chen F., Capanoglu E. The Reciprocal Interactions between Polyphenols and Gut Microbiota and Effects on Bioaccessibility. Nutrients. 2016;8:78. doi: 10.3390/nu8020078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ballini A., Signorini L., Inchingolo A.D., Saini R., Gnoni A., Scacco S., Cantore S., Dipalma G., Inchingolo F., Santacroce L. Probiotics May Improve Serum Folate Availability in Pregnant Women: A Pilot Study. Open Access Maced. J. Med. Sci. 2020;8:1124–1130. doi: 10.3889/oamjms.2020.5494. [DOI] [Google Scholar]
- 86.Signorini L., Ballini A., Arrigoni R., Leonardis F.D., Saini R., Cantore S., Vito D.D., Coscia M.F., Dipalma G., Inchingolo L.S., et al. Evaluation of a Nutraceutical Product with Probiotics, Vitamin D, plus Banaba Leaf Extracts (Lagerstroemia speciosa) in Glycemic Control. [(accessed on 28 November 2022)]. Available online: https://www.eurekaselect.com/187708/article. [DOI] [PubMed]
- 87.Roberts A.B., Gu X., Buffa J.A., Hurd A.G., Wang Z., Zhu W., Gupta N., Skye S.M., Cody D.B., Levison B.S., et al. Development of a gut microbe–targeted nonlethal therapeutic to inhibit thrombosis potential. Nat. Med. 2018;24:1407–1417. doi: 10.1038/s41591-018-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Queipo-Ortuño M.I., Boto-Ordóñez M., Murri M., Gomez-Zumaquero J.M., Clemente-Postigo M., Estruch R., Cardona Diaz F., Andrés-Lacueva C., Tinahones F.J. Influence of red wine polyphenols and ethanol on the gut microbiota ecology and biochemical biomarkers. Am. J. Clin. Nutr. 2012;95:1323–1334. doi: 10.3945/ajcn.111.027847. [DOI] [PubMed] [Google Scholar]
- 89.Scarano A., Murmura G., Vantaggiato G., Lauritano D., Silvestre-Rangil J., Di Cerbo A., Lorusso F. Delayed Expansion of Atrophic Mandible (Deam): A Case Report. Oral Implantol. 2017;10:190–196. doi: 10.11138/orl/2017.10.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wahab A., Gao K., Jia C., Zhang F., Tian G., Murtaza G., Chen J. Significance of Resveratrol in Clinical Management of Chronic Diseases. Mol. J. Synth. Chem. Nat. Prod. Chem. 2017;22:1329. doi: 10.3390/molecules22081329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Asis M., Hemmati N., Moradi S., Nagulapalli Venkata K.C., Mohammadi E., Farzaei M.H., Bishayee A. Effects of resveratrol supplementation on bone biomarkers: A systematic review and meta-analysis. Ann. N. Y. Acad. Sci. 2019;1457:92–103. doi: 10.1111/nyas.14226. [DOI] [PubMed] [Google Scholar]
- 92.Bo S., Gambino R., Ponzo V., Cioffi I., Goitre I., Evangelista A., Ciccone G., Cassader M., Procopio M. Effects of resveratrol on bone health in type 2 diabetic patients. A double-blind randomized-controlled trial. Nutr. Diabetes. 2018;8:51. doi: 10.1038/s41387-018-0059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Scarano A., Noumbissi S., Gupta S., Inchingolo F., Stilla P., Lorusso F. Scanning Electron Microscopy Analysis and Energy Dispersion X-Ray Microanalysis to Evaluate the Effects of Decontamination Chemicals and Heat Sterilization on Implant Surgical Drills: Zirconia vs. Steel. Appl. Sci. 2019;9:2837. doi: 10.3390/app9142837. [DOI] [Google Scholar]
- 94.Acen E.L., Biraro I.A., Worodria W., Joloba M.L., Nkeeto B., Musaazi J., Kateete D.P. Impact of vitamin D status and cathelicidin antimicrobial peptide on adults with active pulmonary TB globally: A systematic review and meta-analysis. PLoS ONE. 2021;16:e0252762. doi: 10.1371/journal.pone.0252762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Borsani E., Bonazza V., Buffoli B., Nocini P.F., Albanese M., Zotti F., Inchingolo F., Rezzani R., Rodella L.F. Beneficial Effects of Concentrated Growth Factors and Resveratrol on Human Osteoblasts In Vitro Treated with Bisphosphonates. BioMed Res. Int. 2018;2018:4597321. doi: 10.1155/2018/4597321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhai J.-L., Weng X.-S., Wu Z.-H., Guo S.-G. Effect of Resveratrol on Preventing Steroid-induced Osteonecrosis in a Rabbit Model. Chin. Med. J. 2016;129:824–830. doi: 10.4103/0366-6999.178952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Simonet W.S., Lacey D.L., Dunstan C.R., Kelley M., Chang M.-S., Lüthy R., Nguyen H.Q., Wooden S., Bennett L., Boone T., et al. Osteoprotegerin: A Novel Secreted Protein Involved in the Regulation of Bone Density. Cell. 1997;89:309–319. doi: 10.1016/S0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 98.Recombinant human bone morphogenetic protein-2 stimulates osteoblastic maturation and inhibits myogenic differentiation in vitro. J. Cell Biol. 1991;113:681–687. doi: 10.1083/jcb.113.3.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Niemann S., Bertling A., Brodde M.F., Fender A.C., Van de Vyver H., Hussain M., Holzinger D., Reinhardt D., Peters G., Heilmann C., et al. Panton-Valentine Leukocidin associated with S. aureus osteomyelitis activates platelets via neutrophil secretion products. Sci. Rep. 2018;8:2185. doi: 10.1038/s41598-018-20582-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Löffler B., Hussain M., Grundmeier M., Brück M., Holzinger D., Varga G., Roth J., Kahl B.C., Proctor R.A., Peters G. Staphylococcus aureus Panton-Valentine Leukocidin Is a Very Potent Cytotoxic Factor for Human Neutrophils. PLoS Pathog. 2010;6:e1000715. doi: 10.1371/journal.ppat.1000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang R., Lv Y., Miao L., Zhang H., Qu X., Chen J., Xu B., Yang B., Fu J., Tan C., et al. Resveratrol Attenuates Meningitic Escherichia coli-Mediated Blood–Brain Barrier Disruption. ACS Infect. Dis. 2021;7:777–789. doi: 10.1021/acsinfecdis.0c00564. [DOI] [PubMed] [Google Scholar]
- 102.Pacifici L., Santacroce L., Dipalma G., Haxhirexha K., Topi S., Cantore S., Altini V., Pacifici A., Vito D.D., Pettini F., et al. Gender medicine: The impact of probiotics on male patients. Gend. Med. 2021;172:8–15. doi: 10.7417/CT.2021.2274. [DOI] [PubMed] [Google Scholar]
- 103.Côté C.D., Rasmussen B.A., Duca F.A., Zadeh-Tahmasebi M., Baur J.A., Daljeet M., Breen D.M., Filippi B.M., Lam T.K.T. Resveratrol activates duodenal SIRT-1 to reverse insulin resistance in rats through a neuronal network. Nat. Med. 2015;21:498–505. doi: 10.1038/nm.3821. [DOI] [PubMed] [Google Scholar]
- 104.Yang M., Wei J., Huang T., Lei L., Shen C., Lai J., Yang M., Liu L., Yang Y., Liu G., et al. Resveratrol inhibits the replication of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in cultured Vero cells. Phytother. Res. 2020;35:1127–1129. doi: 10.1002/ptr.6916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sato F., Martinez N.E., Shahid M., Rose J.W., Carlson N.G., Tsunoda I. Resveratrol Exacerbates Both Autoimmune and Viral Models of Multiple Sclerosis. Am. J. Pathol. 2013;183:1390–1396. doi: 10.1016/j.ajpath.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nakamura M., Saito H., Ikeda M., Hokari R., Kato N., Hibi T., Miura S. An antioxidant resveratrol significantly enhanced replication of hepatitis C virus. World J. Gastroenterol. WJG. 2010;16:184–192. doi: 10.3748/wjg.v16.i2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Goldoni R., Dolci C., Boccalari E., Inchingolo F., Paghi A., Strambini L., Galimberti D., Tartaglia G.M. Salivary biomarkers of neurodegenerative and demyelinating diseases and biosensors for their detection. Ageing Res Rev. 2022;76:101587. doi: 10.1016/j.arr.2022.101587. [DOI] [PubMed] [Google Scholar]
- 108.Baldassarre M.E., Di Mauro A., Labellarte G., Pignatelli M., Fanelli M., Schiavi E., Mastromarino P., Capozza M., Panza R., Laforgia N. Resveratrol plus carboxymethyl-β-glucan in infants with common cold: A randomized double-blind trial. Heliyon. 2020;6:e03814. doi: 10.1016/j.heliyon.2020.e03814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Francioso A., Cossi R., Fanelli S., Mastromarino P., Mosca L. Studies on Trans-Resveratrol/Carboxymethylated (1,3/1,6)-β-d-Glucan Association for Aerosol Pharmaceutical Applications. Int. J. Mol. Sci. 2017;18:967. doi: 10.3390/ijms18050967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chihara G., Maeda Y.Y., Hamuro J. Current status and perspectives of immunomodulators of microbial origin. Int. J. Tissue React. 1982;4:207–225. [PubMed] [Google Scholar]
- 111.Novak M., Vetvicka V. β-Glucans, History, and the Present: Immunomodulatory Aspects and Mechanisms of Action. J. Immunotoxicol. 2008;5:47–57. doi: 10.1080/15476910802019045. [DOI] [PubMed] [Google Scholar]
- 112.Miraglia Del Giudice M., Maiello N., Decimo F., Capasso M., Campana G., Leonardi S., Ciprandi G. Resveratrol plus carboxymethyl-β-glucan may affect respiratory infections in children with allergic rhinitis. Pediatr. Allergy Immunol. 2014;25:724–728. doi: 10.1111/pai.12279. [DOI] [PubMed] [Google Scholar]
- 113.Campanella V., Syed J., Santacroce L., Saini R., Ballini A., Inchingolo F. Oral probiotics influence oral and respiratory tract infections in pediatric population: A randomized double-blinded placebo-controlled pilot study. Eur. Rev. Med. Pharmacol. Sci. 2018;22:8034–8041. doi: 10.26355/eurrev_201811_16433. [DOI] [PubMed] [Google Scholar]
- 114.Li J., Wu T., Peng W., Zhu Y. Effects of resveratrol on cariogenic virulence properties of Streptococcus mutans. BMC Microbiol. 2020;20:99. doi: 10.1186/s12866-020-01761-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Li Y.-H., Tian X.-L., Layton G., Norgaard C., Sisson G. Additive attenuation of virulence and cariogenic potential of Streptococcus mutans by simultaneous inactivation of the ComCDE quorum-sensing system and HK/RR11 two-component regulatory system. Microbiology. 2008;154:3256–3265. doi: 10.1099/mic.0.2008/019455-0. [DOI] [PubMed] [Google Scholar]
- 116.Cantore S., Ballini A., De Vito D., Abbinante A., Altini V., Dipalma G., Inchingolo F., Saini R. Clinical results of improvement in periodontal condition by administration of oral probiotics. J. Biol. Regul. Homeost. Agents. 2018;32:1329–1334. [PubMed] [Google Scholar]
- 117.Ballini A., Cantore S., Saini R., Pettini F., Fotopoulou E.A., Saini S.R., Georgakopoulos I.P., Dipalma G., Gargiulo Isacco C., Inchingolo F. Effect of activated charcoal probiotic toothpaste containing Lactobacillus paracasei and xylitol on dental caries: A randomized and controlled clinical trial. J. Biol. Regul. Homeost. Agents. 2019;33:977–981. [PubMed] [Google Scholar]
- 118.Han Y., Jo H., Cho J.H., Dhanasekaran D.N., Song Y.S. Resveratrol as a Tumor-Suppressive Nutraceutical Modulating Tumor Microenvironment and Malignant Behaviors of Cancer. Int. J. Mol. Sci. 2019;20:925. doi: 10.3390/ijms20040925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Singh C.K., Ndiaye M.A., Ahmad N. Resveratrol and cancer: Challenges for clinical translation. Biochim. Biophys. Acta. 2015;1852:1178–1185. doi: 10.1016/j.bbadis.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jiang Z., Chen K., Cheng L., Yan B., Qian W., Cao J., Li J., Wu E., Ma Q., Yang W. Resveratrol and cancer treatment: Updates: Effects of resveratrol on cancer. Ann. N. Y. Acad. Sci. 2017;1403:59–69. doi: 10.1111/nyas.13466. [DOI] [PubMed] [Google Scholar]
- 121.Malaguarnera L. Influence of Resveratrol on the Immune Response. Nutrients. 2019;11:E946. doi: 10.3390/nu11050946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Isacco C.G., Ballini A., De Vito D., Inchingolo A.M., Cantore S., Paduanelli G., Nguyen K.C.D., Inchingolo A.D., Dipalma G., Inchingolo F. Probiotics in Health and Immunity: A First Step toward Understanding the Importance of Microbiota System in Translational Medicine. In: Franco-Robles E., Ramírez-Emiliano J., editors. Prebiotics and Probiotics—Potential Benefits in Nutrition and Health. IntechOpen; London, UK: 2020. [Google Scholar]
- 123.Isacco C.G., Ballini A., De Vito D., Nguyen K.C.D., Cantore S., Bottalico L., Quagliuolo L., Boccellino M., Di Domenico M., Santacroce L., et al. Rebalance the oral microbiota as efficacy tool in endocrine, metabolic, and immune disorders. Endocr. Metab. Immune Disord. Drug Targets. 2021;21:777–784. doi: 10.2174/1871530320666200729142504. [DOI] [PubMed] [Google Scholar]
- 124.Falchetti R., Fuggetta M.P., Lanzilli G., Tricarico M., Ravagnan G. Effects of resveratrol on human immune cell function. Life Sci. 2001;70:81–96. doi: 10.1016/S0024-3205(01)01367-4. [DOI] [PubMed] [Google Scholar]
- 125.Alesci A., Nicosia N., Fumia A., Giorgianni F., Santini A., Cicero N. Resveratrol and Immune Cells: A Link to Improve Human Health. Mol. Basel Switz. 2022;27:424. doi: 10.3390/molecules27020424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gao X., Xu Y.X., Janakiraman N., Chapman R.A., Gautam S.C. Immunomodulatory activity of resveratrol: Suppression of lymphocyte proliferation, development of cell-mediated cytotoxicity, and cytokine production. Biochem. Pharmacol. 2001;62:1299–1308. doi: 10.1016/S0006-2952(01)00775-4. [DOI] [PubMed] [Google Scholar]
- 127.Švajger U., Jeras M. Anti-inflammatory Effects of Resveratrol and Its Potential Use in Therapy of Immune-mediated Diseases. Int. Rev. Immunol. 2012;31:202–222. doi: 10.3109/08830185.2012.665108. [DOI] [PubMed] [Google Scholar]
- 128.Inchingolo A.D., Cazzolla A.P., Di Cosola M., Greco Lucchina A., Santacroce L., Charitos I.A., Topi S., Malcangi G., Hazballa D., Scarano A., et al. The integumentary system and its microbiota between health and disease. J. Biol. Regul. Homeost. Agents. 2021;35:303–321. doi: 10.23812/21-2supp1-30. [DOI] [PubMed] [Google Scholar]
- 129.Casu C., Mosaico G., Natoli V., Scarano A., Lorusso F., Inchingolo F. Microbiota of the Tongue and Systemic Connections: The Examination of the Tongue as an Integrated Approach in Oral Medicine. Hygiene. 2021;1:56–68. doi: 10.3390/hygiene1020006. [DOI] [Google Scholar]
- 130.Shaito A., Posadino A.M., Younes N., Hasan H., Halabi S., Alhababi D., Al-Mohannadi A., Abdel-Rahman W.M., Eid A.H., Nasrallah G.K., et al. Potential Adverse Effects of Resveratrol: A Literature Review. Int. J. Mol. Sci. 2020;21:E2084. doi: 10.3390/ijms21062084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Most J., Penders J., Lucchesi M., Goossens G.H., Blaak E.E. Gut microbiota composition in relation to the metabolic response to 12-week combined polyphenol supplementation in overweight men and women. Eur. J. Clin. Nutr. 2017;71:1040–1045. doi: 10.1038/ejcn.2017.89. [DOI] [PubMed] [Google Scholar]
- 133.Inchingolo F., Hazballa D., Inchingolo A.D., Malcangi G., Marinelli G., Mancini A., Maggiore M.E., Bordea I.R., Scarano A., Farronato M., et al. Innovative Concepts and Recent Breakthrough for Engineered Graft and Constructs for Bone Regeneration: A Literature Systematic Review. Materials. 2022;15:1120. doi: 10.3390/ma15031120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cardona F., Andrés-Lacueva C., Tulipani S., Tinahones F.J., Queipo-Ortuño M.I. Benefits of polyphenols on gut microbiota and implications in human health. J. Nutr. Biochem. 2013;24:1415–1422. doi: 10.1016/j.jnutbio.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 135.Lagouge M., Argmann C., Gerhart-Hines Z., Meziane H., Lerin C., Daussin F., Messadeq N., Milne J., Lambert P., Elliott P., et al. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT-1 and PGC-1alpha. Cell. 2006;127:1109–1122. doi: 10.1016/j.cell.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 136.Corsalini M., Di Venere D., Sportelli P., Magazzino D., Ripa M., Cantatore F., Cagnetta C., De Rinaldis C., Montemurro N., De Giacomo A., et al. Evaluation of prosthetic quality and masticatory efficiency in patients with total removable prosthesis: Study of 12 cases. Oral Implantol. 2018;11:230–240. [Google Scholar]
- 137.Picard F., Kurtev M., Chung N., Topark-Ngarm A., Senawong T., Machado de Oliveira R., Leid M., McBurney M.W., Guarente L. SIRT-1 promotes fat mobilization in white adipocytes by repressing PPAR-γ. Nature. 2004;429:771–776. doi: 10.1038/nature02583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Poulsen M.M., Vestergaard P.F., Clasen B.F., Radko Y., Christensen L.P., Stødkilde-Jørgensen H., Møller N., Jessen N., Pedersen S.B., Jørgensen J.O.L. High-dose resveratrol supplementation in obese men: An investigator-initiated, randomized, placebo-controlled clinical trial of substrate metabolism, insulin sensitivity, and body composition. Diabetes. 2013;62:1186–1195. doi: 10.2337/db12-0975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Arzola-Paniagua M.A., García-Salgado López E.R., Calvo-Vargas C.G., Guevara-Cruz M. Efficacy of an orlistat-resveratrol combination for weight loss in subjects with obesity: A randomized controlled trial. Obesity. 2016;24:1454–1463. doi: 10.1002/oby.21523. [DOI] [PubMed] [Google Scholar]
- 140.Grassi F.R., Grassi R., Rapone B., Gianfranco A., Balena A., Kalemaj Z. Dimensional changes of buccal bone plate in immediate implants inserted through open flap, open flap and bone grafting, and flapless technique. A CBCT randomized controlled clinical trial. Clin. Oral. Implant. Res. 2019;30:1155–1164. doi: 10.1111/clr.13528. [DOI] [PubMed] [Google Scholar]
- 141.Sahebkar A., Serban C., Ursoniu S., Wong N.D., Muntner P., Graham I.M., Mikhailidis D.P., Rizzo M., Rysz J., Sperling L.S., et al. Lack of efficacy of resveratrol on C-reactive protein and selected cardiovascular risk factors--Results from a systematic review and meta-analysis of randomized controlled trials. Int. J. Cardiol. 2015;189:47–55. doi: 10.1016/j.ijcard.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 142.Kang W., Hong H.J., Guan J., Kim D.G., Yang E.-J., Koh G., Park D., Han C.H., Lee Y.-J., Lee D.-H. Resveratrol improves insulin signaling in a tissue-specific manner under insulin-resistant conditions only: In vitro and in vivo experiments in rodents. Metabolism. 2012;61:424–433. doi: 10.1016/j.metabol.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 143.Kang L., Heng W., Yuan A., Baolin L., Fang H. Resveratrol modulates adipokine expression and improves insulin sensitivity in adipocytes: Relative to inhibition of inflammatory responses. Biochimie. 2010;92:789–796. doi: 10.1016/j.biochi.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 144.Costa C.D.S., Rohden F., Hammes T.O., Margis R., Bortolotto J.W., Padoin A.V., Mottin C.C., Guaragna R.M. Resveratrol upregulated SIRT-1, FOXO1, and adiponectin and downregulated PPARγ1-3 mRNA expression in human visceral adipocytes. Obes. Surg. 2011;21:356–361. doi: 10.1007/s11695-010-0251-7. [DOI] [PubMed] [Google Scholar]
- 145.Mercader J., Palou A., Bonet M.L. Resveratrol enhances fatty acid oxidation capacity and reduces resistin and Retinol-Binding Protein 4 expression in white adipocytes. J. Nutr. Biochem. 2011;22:828–834. doi: 10.1016/j.jnutbio.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 146.Thazhath S.S., Wu T., Bound M.J., Checklin H.L., Standfield S., Jones K.L., Horowitz M., Rayner C.K. Administration of resveratrol for 5 wk has no effect on glucagon-like peptide 1 secretion, gastric emptying, or glycemic control in type 2 diabetes: A randomized controlled trial. Am. J. Clin. Nutr. 2016;103:66–70. doi: 10.3945/ajcn.115.117440. [DOI] [PubMed] [Google Scholar]
- 147.Kjær T.N., Ornstrup M.J., Poulsen M.M., Stødkilde-Jørgensen H., Jessen N., Jørgensen J.O.L., Richelsen B., Pedersen S.B. No Beneficial Effects of Resveratrol on the Metabolic Syndrome: A Randomized Placebo-Controlled Clinical Trial. J. Clin. Endocrinol. Metab. 2017;102:1642–1651. doi: 10.1210/jc.2016-2160. [DOI] [PubMed] [Google Scholar]
- 148.Crandall J.P., Barzilai N. Exploring the promise of resveratrol: Where do we go from here? Diabetes. 2013;62:1022–1023. doi: 10.2337/db12-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lauritzen H.P.M.M., Schertzer J.D. Measuring GLUT4 translocation in mature muscle fibers. Am. J. Physiol. Endocrinol. Metab. 2010;299:E169–E179. doi: 10.1152/ajpendo.00066.2010. [DOI] [PubMed] [Google Scholar]
- 150.Mueckler M., Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol. Aspects Med. 2013;34:121–138. doi: 10.1016/j.mam.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cura A.J., Carruthers A. Role of monosaccharide transport proteins in carbohydrate assimilation, distribution, metabolism, and homeostasis. Compr. Physiol. 2012;2:863–914. doi: 10.1002/cphy.c110024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Saltiel A.R., Kahn C.R. Insulin signalling and the regulation of glucose and lipid metabolism. Nature. 2001;414:799–806. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- 153.Stanford K.I., Goodyear L.J. Exercise and type 2 diabetes: Molecular mechanisms regulating glucose uptake in skeletal muscle. Adv. Physiol. Educ. 2014;38:308–314. doi: 10.1152/advan.00080.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cheng C.-W., Villani V., Buono R., Wei M., Kumar S., Yilmaz O.H., Cohen P., Sneddon J.B., Perin L., Longo V.D. Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes. Cell. 2017;168:775–788.e12. doi: 10.1016/j.cell.2017.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Mach N., Fuster-Botella D. Endurance exercise and gut microbiota: A review. J. Sport Health Sci. 2017;6:179–197. doi: 10.1016/j.jshs.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Barton W., Penney N.C., Cronin O., Garcia-Perez I., Molloy M.G., Holmes E., Shanahan F., Cotter P.D., O’Sullivan O. The microbiome of professional athletes differs from that of more sedentary subjects in composition and particularly at the functional metabolic level. Gut. 2018;67:625–633. doi: 10.1136/gutjnl-2016-313627. [DOI] [PubMed] [Google Scholar]
- 157.Houghton M.J., Kerimi A., Mouly V., Tumova S., Williamson G. Gut microbiome catabolites as novel modulators of muscle cell glucose metabolism. FASEB J. 2019;33:1887–1898. doi: 10.1096/fj.201801209R. [DOI] [PubMed] [Google Scholar]
- 158.Zhu C.-H., Mouly V., Cooper R.N., Mamchaoui K., Bigot A., Shay J.W., Di Santo J.P., Butler-Browne G.S., Wright W.E. Cellular senescence in human myoblasts is overcome by human telomerase reverse transcriptase and cyclin-dependent kinase 4: Consequences in aging muscle and therapeutic strategies for muscular dystrophies. Aging Cell. 2007;6:515–523. doi: 10.1111/j.1474-9726.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 159.Pimpão R.C., Ventura M.R., Ferreira R.B., Williamson G., Santos C.N. Phenolic sulfates as new and highly abundant metabolites in human plasma after ingestion of a mixed berry fruit purée. Br. J. Nutr. 2015;113:454–463. doi: 10.1017/S0007114514003511. [DOI] [PubMed] [Google Scholar]
- 160.de Ferrars R.M., Czank C., Zhang Q., Botting N.P., Kroon P.A., Cassidy A., Kay C.D. The pharmacokinetics of anthocyanins and their metabolites in humans. Br. J. Pharmacol. 2014;171:3268–3282. doi: 10.1111/bph.12676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Czank C., Cassidy A., Zhang Q., Morrison D.J., Preston T., Kroon P.A., Botting N.P., Kay C.D. Human metabolism and elimination of the anthocyanin, cyanidin-3-glucoside: A (13)C-tracer study. Am. J. Clin. Nutr. 2013;97:995–1003. doi: 10.3945/ajcn.112.049247. [DOI] [PubMed] [Google Scholar]
- 162.Ho G.T.T., Kase E.T., Wangensteen H., Barsett H. Phenolic Elderberry Extracts, Anthocyanins, Procyanidins, and Metabolites Influence Glucose and Fatty Acid Uptake in Human Skeletal Muscle Cells. J. Agric. Food Chem. 2017;65:2677–2685. doi: 10.1021/acs.jafc.6b05582. [DOI] [PubMed] [Google Scholar]
- 163.Scazzocchio B., Varì R., Filesi C., Del Gaudio I., D’Archivio M., Santangelo C., Iacovelli A., Galvano F., Pluchinotta F.R., Giovannini C., et al. Protocatechuic acid activates key components of insulin signaling pathway mimicking insulin activity. Mol. Nutr. Food Res. 2015;59:1472–1481. doi: 10.1002/mnfr.201400816. [DOI] [PubMed] [Google Scholar]
- 164.Yamamoto N., Ueda M., Kawabata K., Sato T., Kawasaki K., Hashimoto T., Ashida H. Artemisia princeps Extract Promoted Glucose Uptake in Cultured L6 Muscle Cells via Glucose Transporter 4 Translocation. Biosci. Biotechnol. Biochem. 2010;74:2036–2042. doi: 10.1271/bbb.100305. [DOI] [PubMed] [Google Scholar]
- 165.Wong C.C., Akiyama Y., Abe T., Lippiat J.D., Orfila C., Williamson G. Carrier-mediated transport of quercetin conjugates: Involvement of organic anion transporters and organic anion transporting polypeptides. Biochem. Pharmacol. 2012;84:564–570. doi: 10.1016/j.bcp.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 166.Parkar S.G., Stevenson D.E., Skinner M.A. The potential influence of fruit polyphenols on colonic microflora and human gut health. Int. J. Food Microbiol. 2008;124:295–298. doi: 10.1016/j.ijfoodmicro.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 167.Laparra J.M., Sanz Y. Interactions of gut microbiota with functional food components and nutraceuticals. Pharmacol. Res. 2010;61:219–225. doi: 10.1016/j.phrs.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 168.Makinen K., Berger B., Bel-Rhlid R., Ananta E. Science and technology for the mastership of probiotic applications in food products. J. Biotechnol. 2012;162:356–365. doi: 10.1016/j.jbiotec.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 169.Volštátová T., Havlík J., Doskočil I., Geigerová M., Rada V. Effect of hydrolyzed milk on the adhesion of Lactobacilli to intestinal cells. Sci. Agric. Bohem. 2015;46:21–25. doi: 10.1515/sab-2015-0012. [DOI] [Google Scholar]
- 170.Carrière V., Lesuffleur T., Barbat A., Rousset M., Dussaulx E., Costet P., de Waziers I., Beaune P., Zweibaum A. Expression of cytochrome P-450 3A in HT29-MTX cells and Caco-2 clone TC7. FEBS Lett. 1994;355:247–250. doi: 10.1016/0014-5793(94)01199-0. [DOI] [PubMed] [Google Scholar]
- 171.Celebioglu H.U., Delsoglio M., Brix S., Pessione E., Svensson B. Plant Polyphenols Stimulate Adhesion to Intestinal Mucosa and Induce Proteome Changes in the Probiotic Lactobacillus acidophilus NCFM. Mol. Nutr. Food Res. 2018;62:1700638. doi: 10.1002/mnfr.201700638. [DOI] [PubMed] [Google Scholar]
- 172.Jarosova V., Doskocil I., Volstatova T., Havlik J. Adhesive Property of Different Strains of Lactobacilli in The Presence of Resveratrol. Sci. Agric. Bohem. 2018;49:291–296. doi: 10.2478/sab-2018-0036. [DOI] [Google Scholar]
- 173.Fujiwara S., Seto Y., Kimura A., Hashiba H. Establishment of orally-administered Lactobacillus gasseri SBT2055SR in the gastrointestinal tract of humans and its influence on intestinal microflora and metabolism. J. Appl. Microbiol. 2001;90:343–352. doi: 10.1046/j.1365-2672.2001.01251.x. [DOI] [PubMed] [Google Scholar]
- 174.Johansson M.L., Nobaek S., Berggren A., Nyman M., Björck I., Ahrné S., Jeppsson B., Molin G. Survival of Lactobacillus plantarum DSM 9843 (299v), and effect on the short-chain fatty acid content of faeces after ingestion of a rose-hip drink with fermented oats. Int. J. Food Microbiol. 1998;42:29–38. doi: 10.1016/S0168-1605(98)00055-5. [DOI] [PubMed] [Google Scholar]
- 175.Qiao Y., Sun J., Xia S., Tang X., Shi Y., Le G. Effects of resveratrol on gut microbiota and fat storage in a mouse model with high-fat-induced obesity. Food Funct. 2014;5:1241–1249. doi: 10.1039/c3fo60630a. [DOI] [PubMed] [Google Scholar]
- 176.Dao T.-M.A., Waget A., Klopp P., Serino M., Vachoux C., Pechere L., Drucker D.J., Champion S., Barthélemy S., Barra Y., et al. Resveratrol increases glucose induced GLP-1 secretion in mice: A mechanism which contributes to the glycemic control. PLoS ONE. 2011;6:e20700. doi: 10.1371/journal.pone.0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wang P., Wang J., Li D., Ke W., Chen F., Hu X. Targeting the gut microbiota with resveratrol: A demonstration of novel evidence for the management of hepatic steatosis. J. Nutr. Biochem. 2020;81:108363. doi: 10.1016/j.jnutbio.2020.108363. [DOI] [PubMed] [Google Scholar]
- 178.Paulo L., Ferreira S., Gallardo E., Queiroz J., Domingues F. Antimicrobial activity and effects of resveratrol on human pathogenic bacteria. World J. Microbiol. Biotechnol. 2010;26:1533–1538. doi: 10.1007/s11274-010-0325-7. [DOI] [Google Scholar]
- 179.Hwang D., Lim Y.-H. Resveratrol antibacterial activity against Escherichia coli is mediated by Z-ring formation inhibition via suppression of FtsZ expression. Sci. Rep. 2015;5:10029. doi: 10.1038/srep10029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Dueñas M., Muñoz-González I., Cueva C., Jiménez-Girón A., Sánchez-Patán F., Santos-Buelga C., Moreno-Arribas M.V., Bartolomé B. A survey of modulation of gut microbiota by dietary polyphenols. BioMed Res. Int. 2015;2015:850902. doi: 10.1155/2015/850902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Larrosa M., Yañéz-Gascón M.J., Selma M.V., González-Sarrías A., Toti S., Cerón J.J., Tomás-Barberán F., Dolara P., Espín J.C. Effect of a low dose of dietary resveratrol on colon microbiota, inflammation and tissue damage in a DSS-induced colitis rat model. J. Agric. Food Chem. 2009;57:2211–2220. doi: 10.1021/jf803638d. [DOI] [PubMed] [Google Scholar]
- 182.Ding S., Jiang H., Fang J. Regulation of Immune Function by Polyphenols. J. Immunol. Res. 2018;2018:1264074. doi: 10.1155/2018/1264074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Tzounis X., Vulevic J., Kuhnle G., George T., Leonczak J., Gibson G., Kwik-Uribe C., Spencer J. Flavanol monomer-induced changes to the human faecal microflora. Br. J. Nutr. 2007;99:782–792. doi: 10.1017/S0007114507853384. [DOI] [PubMed] [Google Scholar]
- 184.Impact of Tart Cherries Polyphenols on the Human Gut Microbiota and Phenolic Metabolites in vitro and in vivo|Elsevier Enhanced Reader. [(accessed on 23 March 2022)]. Available online: https://reader.elsevier.com/reader/sd/pii/S0955286317307143?token=2A314BA6B8CF02782E277EE45A17808518FD0D141F0B6C889A40B967CF1D3B155C2F1FE12044543A057B4C1CFCBB9107&originRegion=eu-west-1&originCreation=20220323095057. [DOI] [PubMed]
- 185.Catinean A., Neag M.A., Muntean D.M., Bocsan I.C., Buzoianu A.D. An overview on the interplay between nutraceuticals and gut microbiota. PeerJ. 2018;6:e4465. doi: 10.7717/peerj.4465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bialonska D., Kasimsetty S.G., Schrader K.K., Ferreira D. The effect of pomegranate (Punica granatum L.) byproducts and ellagitannins on the growth of human gut bacteria. J. Agric. Food Chem. 2009;57:8344–8349. doi: 10.1021/jf901931b. [DOI] [PubMed] [Google Scholar]
- 187.Saura-Calixto F., Pérez-Jiménez J., editors. Non-Extractable Polyphenols and Carotenoids. Royal Society of Chemistry; London, UK: 2018. [Google Scholar]
- 188.Ling K.-H., Wan M.L.Y., El-Nezami H., Wang M. Protective Capacity of Resveratrol, a Natural Polyphenolic Compound, against Deoxynivalenol-Induced Intestinal Barrier Dysfunction and Bacterial Translocation. Chem. Res. Toxicol. 2016;29:823–833. doi: 10.1021/acs.chemrestox.6b00001. [DOI] [PubMed] [Google Scholar]
- 189.Sung M.M., Kim T.T., Denou E., Soltys C.-L.M., Hamza S.M., Byrne N.J., Masson G., Park H., Wishart D.S., Madsen K.L., et al. Improved Glucose Homeostasis in Obese Mice Treated With Resveratrol Is Associated With Alterations in the Gut Microbiome. Diabetes. 2016;66:418–425. doi: 10.2337/db16-0680. [DOI] [PubMed] [Google Scholar]
- 190.Schroeder B.O., Bäckhed F. Signals from the gut microbiota to distant organs in physiology and disease. Nat. Med. 2016;22:1079–1089. doi: 10.1038/nm.4185. [DOI] [PubMed] [Google Scholar]
- 191.Buryanovskyy L., Fu Y., Boyd M., Ma Y., Hsieh T., Wu J.M., Zhang Z. Crystal structure of quinone reductase 2 in complex with resveratrol. Biochemistry. 2004;43:11417–11426. doi: 10.1021/bi049162o. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Sánchez-Fidalgo S., Cárdeno A., Villegas I., Talero E., de la Lastra C.A. Dietary supplementation of resveratrol attenuates chronic colonic inflammation in mice. Eur. J. Pharmacol. 2010;633:78–84. doi: 10.1016/j.ejphar.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 193.Leláková V., Šmejkal K., Jakubczyk K., Veselý O., Landa P., Václavík J., Bobáľ P., Pížová H., Temml V., Steinacher T., et al. Parallel in vitro and in silico investigations into anti-inflammatory effects of non-prenylated stilbenoids. Food Chem. 2019;285:431–440. doi: 10.1016/j.foodchem.2019.01.128. [DOI] [PubMed] [Google Scholar]
- 194.Edwards C.A., Havlik J., Cong W., Mullen W., Preston T., Morrison D.J., Combet E. Polyphenols and health: Interactions between fibre, plant polyphenols and the gut microbiota. Nutr. Bull. 2017;42:356–360. doi: 10.1111/nbu.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Healey G.R., Murphy R., Brough L., Butts C.A., Coad J. Interindividual variability in gut microbiota and host response to dietary interventions. Nutr. Rev. 2017;75:1059–1080. doi: 10.1093/nutrit/nux062. [DOI] [PubMed] [Google Scholar]
- 196.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 197.Heianza Y., Ma W., Manson J.E., Rexrode K.M., Qi L. Gut Microbiota Metabolites and Risk of Major Adverse Cardiovascular Disease Events and Death: A Systematic Review and Meta-Analysis of Prospective Studies. J. Am. Heart Assoc. 2017;6:e004947. doi: 10.1161/JAHA.116.004947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Chen P.B., Black A.S., Sobel A.L., Zhao Y., Mukherjee P., Molparia B., Moore N.E., Aleman Muench G.R., Wu J., Chen W., et al. Directed remodeling of the mouse gut microbiome inhibits the development of atherosclerosis. Nat. Biotechnol. 2020;38:1288–1297. doi: 10.1038/s41587-020-0549-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gersh B.J., Sliwa K., Mayosi B.M., Yusuf S. Novel therapeutic conceptsThe epidemic of cardiovascular disease in the developing world: Global implications. Eur. Heart J. 2010;31:642–648. doi: 10.1093/eurheartj/ehq030. [DOI] [PubMed] [Google Scholar]
- 200.Brunt V.E., Gioscia-Ryan R.A., Casso A.G., VanDongen N.S., Ziemba B.P., Sapinsley Z.J., Richey J.J., Zigler M.C., Neilson A.P., Davy K.P., et al. Trimethylamine-N-Oxide Promotes Age-Related Vascular Oxidative Stress and Endothelial Dysfunction in Mice and Healthy Humans. Hypertension. 2020;76:101–112. doi: 10.1161/HYPERTENSIONAHA.120.14759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Romano K.A., Vivas E.I., Amador-Noguez D., Rey F.E. Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. MBio. 2015;6:e02481. doi: 10.1128/mBio.02481-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Chen M., Yi L., Zhang Y., Zhou X., Ran L., Yang J., Zhu J., Zhang Q., Mi M. Resveratrol Attenuates Trimethylamine-N-Oxide (TMAO)-Induced Atherosclerosis by Regulating TMAO Synthesis and Bile Acid Metabolism via Remodeling of the Gut Microbiota. MBio. 2016;7:e02210–e02215. doi: 10.1128/mBio.02210-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Jameson E., Doxey A.C., Airs R., Purdy K.J., Murrell J.C., Chen Y. Metagenomic data-mining reveals contrasting microbial populations responsible for trimethylamine formation in human gut and marine ecosystems. Microb. Genom. 2016;2:e000080. doi: 10.1099/mgen.0.000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Wang Z., Roberts A.B., Buffa J.A., Levison B.S., Zhu W., Org E., Gu X., Huang Y., Zamanian-Daryoush M., Culley M.K., et al. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell. 2015;163:1585–1595. doi: 10.1016/j.cell.2015.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Fitzgerald R.J., Adams B.O., Sandham H.J., Abhyankar S. Cariogenicity of a lactate dehydrogenase-deficient mutant of Streptococcus mutans serotype c in gnotobiotic rats. Infect. Immun. 1989;57:823. doi: 10.1128/iai.57.3.823-826.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Dawes C. What is the critical pH and why does a tooth dissolve in acid? J. Can. Dent. Assoc. 2003;69:722–724. [PubMed] [Google Scholar]
- 207.Xu X., Zhou X.D., Wu C.D. The tea catechin epigallocatechin gallate suppresses cariogenic virulence factors of Streptococcus mutans. Antimicrob. Agents Chemother. 2011;55:1229–1236. doi: 10.1128/AAC.01016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Pires J.G., Zabini S.S., Braga A.S., de Cássia Fabris R., de Andrade F.B., de Oliveira R.C., Magalhães A.C. Hydroalcoholic extracts of Myracrodruon urundeuva All. and Qualea grandiflora Mart. leaves on Streptococcus mutans biofilm and tooth demineralization. Arch. Oral Biol. 2018;91:17–22. doi: 10.1016/j.archoralbio.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 209.Koo H., Jeon J.G. Naturally occurring molecules as alternative therapeutic agents against cariogenic biofilms. Adv. Dent. Res. 2009;21:63–68. doi: 10.1177/0895937409335629. [DOI] [PubMed] [Google Scholar]
- 210.Liu C., Worthington R.J., Melander C., Wu H. A new small molecule specifically inhibits the cariogenic bacterium Streptococcus mutans in multispecies biofilms. Antimicrob. Agents Chemother. 2011;55:2679–2687. doi: 10.1128/AAC.01496-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Yamashita Y., Bowen W.H., Burne R.A., Kuramitsu H.K. Role of the Streptococcus mutans gtf genes in caries induction in the specific-pathogen-free rat model. Infect. Immun. 1993;61:3811–3817. doi: 10.1128/iai.61.9.3811-3817.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Wu S., Huang J. Resveratrol alleviates Staphylococcus�aureus pneumonia by inhibition of the NLRP3 inflammasome. Exp. Ther. Med. 2017;14:6099–6104. doi: 10.3892/etm.2017.5337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Suntharalingam P., Cvitkovitch D.G. Quorum sensing in streptococcal biofilm formation. Trends Microbiol. 2005;13:3–6. doi: 10.1016/j.tim.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 214.Kaur G., Balamurugan P., Princy S.A. Inhibition of the Quorum Sensing System (ComDE Pathway) by Aromatic 1,3-di-m-tolylurea (DMTU): Cariostatic Effect with Fluoride in Wistar Rats. Front. Cell. Infect. Microbiol. 2017;7:313. doi: 10.3389/fcimb.2017.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Heng X., Liu W., Chu W. Identification of choline-degrading bacteria from healthy human feces and used for screening of trimethylamine (TMA)-lyase inhibitors. Microb. Pathog. 2021;152:104658. doi: 10.1016/j.micpath.2020.104658. [DOI] [PubMed] [Google Scholar]
- 216.Lin L., Zhang J. Role of intestinal microbiota and metabolites on gut homeostasis and human diseases. BMC Immunol. 2017;18:2. doi: 10.1186/s12865-016-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Rinninella E., Raoul P., Cintoni M., Franceschi F., Miggiano G.A.D., Gasbarrini A., Mele M.C. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7:14. doi: 10.3390/microorganisms7010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hills R.D., Pontefract B.A., Mishcon H.R., Black C.A., Sutton S.C., Theberge C.R. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients. 2019;11:1613. doi: 10.3390/nu11071613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Inchingolo F., Dipalma G., Cirulli N., Cantore S., Saini R.S., Altini V., Santacroce L., Ballini A., Saini R. Microbiological results of improvement in periodontal condition by administration of oral probiotics. J. Biol. Regul. Homeost. Agents. 2018;32:1323–1328. [PubMed] [Google Scholar]
- 220.Stecher B. The Roles of Inflammation, Nutrient Availability and the Commensal Microbiota in Enteric Pathogen Infection. Microbiol. Spectr. 2015;3:3. doi: 10.1128/microbiolspec.MBP-0008-2014. [DOI] [PubMed] [Google Scholar]
- 221.Patano A., Di Venere D., Ceci S., Berate P., Candrea S., Babtan A.-M., Azzollini D., Piras F., Curatoli L., Corriero A., et al. Essential oils utility implications in symptomatic Burning Mouth Syndrome. Balneo PRM Res. J. 2021;12:381–385. doi: 10.12680/balneo.2021.466. [DOI] [Google Scholar]
- 222.Thursby E., Juge N. Introduction to the human gut microbiota. Biochem. J. 2017;474:1823–1836. doi: 10.1042/BCJ20160510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Vestergaard M., Ingmer H. Antibacterial and antifungal properties of resveratrol. Int. J. Antimicrob. Agents. 2019;53:716–723. doi: 10.1016/j.ijantimicag.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 224.Mehta J., Rayalam S., Wang X. Cytoprotective Effects of Natural Compounds against Oxidative Stress. Antioxidants. 2018;7:147. doi: 10.3390/antiox7100147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ramdani L.H., Bachari K. Potential therapeutic effects of Resveratrol against SARS-CoV-2. Acta Virol. 2020;64:276–280. doi: 10.4149/av_2020_309. [DOI] [PubMed] [Google Scholar]
- 226.Kim E.N., Kim M.Y., Lim J.H., Kim Y., Shin S.J., Park C.W., Kim Y.-S., Chang Y.S., Yoon H.E., Choi B.S. The protective effect of resveratrol on vascular aging by modulation of the renin–angiotensin system. Atherosclerosis. 2018;270:123–131. doi: 10.1016/j.atherosclerosis.2018.01.043. [DOI] [PubMed] [Google Scholar]
- 227.Junior A.G., Tolouei S.E.L., Dos Reis Lívero F.A., Gasparotto F., Boeing T., de Souza P. Natural Agents Modulating ACE-2: A Review of Compounds with Potential against SARS-CoV-2 Infections. Curr. Pharm. Des. 2021;27:1588–1596. doi: 10.2174/1381612827666210114150607. [DOI] [PubMed] [Google Scholar]
- 228.Frari V., Capuano F., Micera A., Greco F., Salvinelli F. The potential role of trans-resveratrol/carboxymethylated (1.3/1.6)-β-d-glucan minimizing symptoms and improve healing after functional endoscopic sinus surgery. Eur. Rev. Med. Pharmacol. Sci. 2020;24:12395–12399. doi: 10.26355/eurrev_202012_24034. [DOI] [PubMed] [Google Scholar]
- 229.Gutiérrez S., Morán A., Martínez-Blanco H., Ferrero M.A., Rodríguez-Aparicio L.B. The Usefulness of Non-Toxic Plant Metabolites in the Control of Bacterial Proliferation. Probiotics Antimicrob. Proteins. 2017;9:323–333. doi: 10.1007/s12602-017-9259-9. [DOI] [PubMed] [Google Scholar]
- 230.Zordoky B.N.M., Robertson I.M., Dyck J.R.B. Preclinical and clinical evidence for the role of resveratrol in the treatment of cardiovascular diseases. Biochim. Biophys. Acta. 2015;1852:1155–1177. doi: 10.1016/j.bbadis.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 231.Hsu C.-P., Odewale I., Alcendor R.R., Sadoshima J. SIRT-1 protects the heart from aging and stress. Biol. Chem. 2008;389:221–231. doi: 10.1515/BC.2008.032. [DOI] [PubMed] [Google Scholar]
- 232.Clark D., Tuor U.I., Thompson R., Institoris A., Kulynych A., Zhang X., Kinniburgh D.W., Bari F., Busija D.W., Barber P.A. Protection against recurrent stroke with resveratrol: Endothelial protection. PLoS ONE. 2012;7:e47792. doi: 10.1371/journal.pone.0047792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Gingivitis Effectiveness of Emulgel Containing 2% Resveratrol in Orthodontic Patients: An 8-Week Randomized Clinical Trial—PubMed. [(accessed on 16 February 2022)]; doi: 10.1155/2021/6615900. Available online: https://pubmed.ncbi.nlm.nih.gov/33859693/ [DOI] [PMC free article] [PubMed]
- 234.Chin Y.-T., Cheng G.-Y., Shih Y.-J., Lin C.-Y., Lin S.-J., Lai H.-Y., Whang-Peng J., Chiu H.-C., Lee S.-Y., Fu E., et al. Therapeutic applications of resveratrol and its derivatives on periodontitis. Ann. N. Y. Acad. Sci. 2017;1403:101–108. doi: 10.1111/nyas.13433. [DOI] [PubMed] [Google Scholar]
- 235.Ma Q. Role of Nrf2 in Oxidative Stress and Toxicity. Annu. Rev. Pharmacol. Toxicol. 2013;53:401–426. doi: 10.1146/annurev-pharmtox-011112-140320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Vaiserman A., Koliada A., Zayachkivska A., Lushchak O. Nanodelivery of Natural Antioxidants: An Anti-aging Perspective. Front. Bioeng. Biotechnol. 2020;7:447. doi: 10.3389/fbioe.2019.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Liu L., Beck C., Nøhr-Meldgaard K., Peschel A., Kretschmer D., Ingmer H., Vestergaard M. Inhibition of the ATP synthase sensitizes Staphylococcus aureus towards human antimicrobial peptides. Sci. Rep. 2020;10:11391. doi: 10.1038/s41598-020-68146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Phan D.Q., Nguyen L.D.N., Pham S.T., Nguyen T., Pham P.T.T., Nguyen S.T.H., Pham D.T., Pham H.T., Tran D.K., Le S.H., et al. The Distribution of Dengue Virus Serotype in Quang Nam Province (Vietnam) during the Outbreak in 2018. Int. J. Environ. Res. Public Health. 2022;19:1285. doi: 10.3390/ijerph19031285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Hwang D., Lim Y.-H. Resveratrol controls Escherichia coli growth by inhibiting the AcrAB-TolC efflux pump. FEMS Microbiol. Lett. 2019;366:fnz030. doi: 10.1093/femsle/fnz030. [DOI] [PubMed] [Google Scholar]
- 240.Jin T., Bokarewa M., Foster T., Mitchell J., Higgins J., Tarkowski A. Staphylococcus aureus Resists Human Defensins by Production of Staphylokinase, a Novel Bacterial Evasion Mechanism. J. Immunol. 2004;172:1169–1176. doi: 10.4049/jimmunol.172.2.1169. [DOI] [PubMed] [Google Scholar]
- 241.Martin E., Cevik C., Nugent K. The role of hypervirulent Staphylococcus aureus infections in the development of deep vein thrombosis. Thromb. Res. 2012;130:302–308. doi: 10.1016/j.thromres.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 242.Sheikh H.Q., Aqil A., Kirby A., Hossain F.S. Panton-Valentine leukocidin osteomyelitis in children: A growing threat. Br. J. Hosp. Med. 2015;76:18–24. doi: 10.12968/hmed.2015.76.1.18. [DOI] [PubMed] [Google Scholar]
- 243.Volf I., Roth A., Cooper J., Moeslinger T., Koller E. Hypochlorite modified LDL are a stronger agonist for platelets than copper oxidized LDL. FEBS Lett. 2000;483:155–159. doi: 10.1016/S0014-5793(00)02104-9. [DOI] [PubMed] [Google Scholar]
- 244.Speth C., Brodde M.F., Hagleitner M., Rambach G., Van Aken H., Dierich M., Kehrel B.E. Neutrophils Turn Plasma Proteins into Weapons against HIV-1. PLoS ONE. 2013;8:e66073. doi: 10.1371/journal.pone.0066073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Colin D.A., Monteil H. Control of the Oxidative Burst of Human Neutrophils by Staphylococcal Leukotoxins. Infect. Immun. 2003;71:3724–3729. doi: 10.1128/IAI.71.7.3724-3729.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Niemann S., Ehrhardt C., Medina E., Warnking K., Tuchscherr L., Heitmann V., Ludwig S., Peters G., Löffler B. Combined Action of Influenza Virus and Staphylococcus aureus Panton–Valentine Leukocidin Provokes Severe Lung Epithelium Damage. J. Infect. Dis. 2012;206:1138–1148. doi: 10.1093/infdis/jis468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Quinn K.L., Henriques M., Tabuchi A., Han B., Yang H., Cheng W.-E., Tole S., Yu H., Luo A., Charbonney E., et al. Human Neutrophil Peptides Mediate Endothelial-Monocyte Interaction, Foam Cell Formation, and Platelet Activation. Arterioscler. Thromb. Vasc. Biol. 2011;31:2070–2079. doi: 10.1161/ATVBAHA.111.227116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Melki I., Tessandier N., Zufferey A., Boilard E. Platelet microvesicles in health and disease. Platelets. 2017;28:214–221. doi: 10.1080/09537104.2016.1265924. [DOI] [PubMed] [Google Scholar]
- 249.Kohnen S. Resveratrol Inhibits the Activity of Equine Neutrophil Myeloperoxidase by a Direct Interaction with the Enzyme. J. Agric. Food Chem. 2007;55:8080–8087. doi: 10.1021/jf071741n. [DOI] [PubMed] [Google Scholar]
- 250.Sakr A., Brégeon F., Mège J.-L., Rolain J.-M., Blin O. Staphylococcus aureus Nasal Colonization: An Update on Mechanisms, Epidemiology, Risk Factors, and Subsequent Infections. Front. Microbiol. 2018;9:2419. doi: 10.3389/fmicb.2018.02419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Azmi A.H., Adnan S.N.A., Ab Malik N. The Prevalence of Staphylococcus aureus in the Oral Cavity of Healthy Adults in Malaysia. Sains Malays. 2020;49:583–591. doi: 10.17576/jsm-2020-4903-13. [DOI] [Google Scholar]
- 252.Ohara-Nemoto Y., Haraga H., Kimura S., Nemoto T.K. Occurrence of staphylococci in the oral cavities of healthy adults and nasal oral trafficking of the bacteria. J. Med. Microbiol. 2008;57:95–99. doi: 10.1099/jmm.0.47561-0. [DOI] [PubMed] [Google Scholar]
- 253.McCormack M.G., Smith A.J., Akram A.N., Jackson M., Robertson D., Edwards G. Staphylococcus aureus and the oral cavity: An overlooked source of carriage and infection? Am. J. Infect. Control. 2015;43:35–37. doi: 10.1016/j.ajic.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 254.Martin M.V., Hardy P. Two cases of oral infection by methicillin-resistant Staphylococcus aureus. Br. Dent. J. 1991;170:63–64. doi: 10.1038/sj.bdj.4807419. [DOI] [PubMed] [Google Scholar]
- 255.Steffin D.H.M., Hsieh E.M., Rouce R.H. Gene Therapy. Adv. Pediatr. 2019;66:37–54. doi: 10.1016/j.yapd.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 256.Boulaiz H., Marchal J.A., Prados J., Melguizo C., Aránega A. Non-viral and viral vectors for gene therapy. Cell. Mol. Biol. 2005;51:3–22. [PubMed] [Google Scholar]
- 257.Alnasser S.M. Review on mechanistic strategy of gene therapy in the treatment of disease. Gene. 2021;769:145246. doi: 10.1016/j.gene.2020.145246. [DOI] [PubMed] [Google Scholar]
- 258.Thompson A.A., Walters M.C., Kwiatkowski J., Rasko J.E.J., Ribeil J.-A., Hongeng S., Magrin E., Schiller G.J., Payen E., Semeraro M., et al. Gene Therapy in Patients with Transfusion-Dependent β-Thalassemia. N. Engl. J. Med. 2018;378:1479–1493. doi: 10.1056/NEJMoa1705342. [DOI] [PubMed] [Google Scholar]
- 259.Biffi A., Montini E., Lorioli L., Cesani M., Fumagalli F., Plati T., Baldoli C., Martino S., Calabria A., Canale S., et al. Lentiviral hematopoietic stem cell gene therapy benefits metachromatic leukodystrophy. Science. 2013;341:1233158. doi: 10.1126/science.1233158. [DOI] [PubMed] [Google Scholar]
- 260.Villa N.Y., Bais S., Chan W.M., Meacham A.M., Wise E., Rahman M.M., Moreb J.S., Rosenau E.H., Wingard J.R., McFadden G., et al. Ex vivo virotherapy with myxoma virus does not impair hematopoietic stem and progenitor cells. Cytotherapy. 2016;18:465–480. doi: 10.1016/j.jcyt.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Amirache F., Lévy C., Costa C., Mangeot P.-E., Torbett B.E., Wang C.X., Nègre D., Cosset F.-L., Verhoeyen E. Mystery solved: VSV-G-LVs do not allow efficient gene transfer into unstimulated T cells, B cells, and HSCs because they lack the LDL receptor. Blood. 2014;123:1422–1424. doi: 10.1182/blood-2013-11-540641. [DOI] [PubMed] [Google Scholar]
- 262.Sutton R.E., Reitsma M.J., Uchida N., Brown P.O. Transduction of human progenitor hematopoietic stem cells by human immunodeficiency virus type 1-based vectors is cell cycle dependent. J. Virol. 1999;73:3649–3660. doi: 10.1128/JVI.73.5.3649-3660.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Alber D., Staeheli P. Partial inhibition of vesicular stomatitis virus by the interferon-induced human 9-27 protein. J. Interferon Cytokine Res. 1996;16:375–380. doi: 10.1089/jir.1996.16.375. [DOI] [PubMed] [Google Scholar]
- 264.Shi G., Ozog S., Torbett B.E., Compton A.A. mTOR inhibitors lower an intrinsic barrier to virus infection mediated by IFITM3. Proc. Natl. Acad. Sci. USA. 2018;115:E10069–E10078. doi: 10.1073/pnas.1811892115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Li J., Kim S.G., Blenis J. Rapamycin: One drug, many effects. Cell Metab. 2014;19:373–379. doi: 10.1016/j.cmet.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Ozog S., Timberlake N.D., Hermann K., Garijo O., Haworth K.G., Shi G., Glinkerman C.M., Schefter L.E., D’Souza S., Simpson E., et al. Resveratrol trimer enhances gene delivery to hematopoietic stem cells by reducing antiviral restriction at endosomes. Blood. 2019;134:1298–1311. doi: 10.1182/blood.2019000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Stokes III J. Optimum health and inhibition of cancer progression by microbiome and resveratrol. Front. Biosci. 2021;26:496–517. doi: 10.2741/4904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Arrigoni R., Ballini A., Santacroce L., Cantore S., Inchingolo A., Inchingolo F., Di Domenico M., Quagliuolo L., Boccellino M. Another look at dietary polyphenols: Challenges in cancer prevention and treatment. Curr. Med. Chem. 2021;29:1061–1082. doi: 10.2174/0929867328666210810154732. [DOI] [PubMed] [Google Scholar]
- 269.Whitlock N.C., Baek S.J. The anticancer effects of resveratrol: Modulation of transcription factors. Nutr. Cancer. 2012;64:493–502. doi: 10.1080/01635581.2012.667862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.van Vliet M.J., Tissing W.J.E., Dun C.A.J., Meessen N.E.L., Kamps W.A., de Bont E.S.J.M., Harmsen H.J.M. Chemotherapy treatment in pediatric patients with acute myeloid leukemia receiving antimicrobial prophylaxis leads to a relative increase of colonization with potentially pathogenic bacteria in the gut. Clin. Infect. Dis. 2009;49:262–270. doi: 10.1086/599346. [DOI] [PubMed] [Google Scholar]
- 271.Zwielehner J., Lassl C., Hippe B., Pointner A., Switzeny O.J., Remely M., Kitzweger E., Ruckser R., Haslberger A.G. Changes in human fecal microbiota due to chemotherapy analyzed by TaqMan-PCR, 454 sequencing and PCR-DGGE fingerprinting. PLoS ONE. 2011;6:e28654. doi: 10.1371/journal.pone.0028654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Staffas A., da Silva M.B., van den Brink M.R.M. The intestinal microbiota in allogeneic hematopoietic cell transplant and graft-versus-host disease. Blood. 2017;129:927–933. doi: 10.1182/blood-2016-09-691394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Taur Y., Jenq R.R., Perales M.-A., Littmann E.R., Morjaria S., Ling L., No D., Gobourne A., Viale A., Dahi P.B., et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. 2014;124:1174–1182. doi: 10.1182/blood-2014-02-554725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Li Y., Dånmark S., Edlund U., Finne-Wistrand A., He X., Norgård M., Blomén E., Hultenby K., Andersson G., Lindgren U. Resveratrol-conjugated poly-ε-caprolactone facilitates in vitro mineralization and in vivo bone regeneration. Acta Biomater. 2011;7:751–758. doi: 10.1016/j.actbio.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 275.Rutledge K.E., Cheng Q., Jabbarzadeh E. Modulation of Inflammatory Response and Induction of Bone Formation Based on Combinatorial Effects of Resveratrol. J. Nanomed. Nanotechnol. 2016;7:350. doi: 10.4172/2157-7439.1000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Zhang W., Shi W., Wu S., Kuss M., Jiang X., Untrauer J.B., Reid S.P., Duan B. 3D printed composite scaffolds with dual small molecule delivery for mandibular bone regeneration. Biofabrication. 2020;12:035020. doi: 10.1088/1758-5090/ab906e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Bäckesjö C.-M., Li Y., Lindgren U., Haldosén L.-A. Activation of SIRT-1 Decreases Adipocyte Formation During Osteoblast Differentiation of Mesenchymal Stem Cells. J. Bone Miner. Res. 2006;21:993–1002. doi: 10.1359/jbmr.060415. [DOI] [PubMed] [Google Scholar]
- 278.Yu H., de Vos P., Ren Y. Overexpression of osteoprotegerin promotes preosteoblast differentiation to mature osteoblasts. Angle Orthod. 2011;81:100–106. doi: 10.2319/050210-238.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Ji Y., Ke Y., Gao S. Intermittent activation of notch signaling promotes bone formation. Am. J. Transl. Res. 2017;9:2933–2944. [PMC free article] [PubMed] [Google Scholar]
- 280.Crotti T.N., Flannery M., Walsh N.C., Fleming J.D., Goldring S.R., McHugh K.P. NFATc1 regulation of the human β3 integrin promoter in osteoclast differentiation. Gene. 2006;372:92–102. doi: 10.1016/j.gene.2005.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Sundaram K., Nishimura R., Senn J., Youssef R.F., London S.D., Reddy S.V. RANK ligand signaling modulates the matrix metalloproteinase-9 gene expression during osteoclast differentiation. Exp. Cell Res. 2007;313:168–178. doi: 10.1016/j.yexcr.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 282.Raggatt L.J., Partridge N.C. Cellular and Molecular Mechanisms of Bone Remodeling. J. Biol. Chem. 2010;285:25103–25108. doi: 10.1074/jbc.R109.041087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Gao X., Ge J., Li W., Zhou W., Xu L. LncRNA KCNQ1OT1 promotes osteogenic differentiation to relieve osteolysis via Wnt/β-catenin activation. Cell Biosci. 2018;8:19. doi: 10.1186/s13578-018-0216-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Kim H.-Y., Yoon J.-Y., Yun J.-H., Cho K.-W., Lee S.-H., Rhee Y.-M., Jung H.-S., Lim H.J., Lee H., Choi J., et al. CXXC5 is a negative-feedback regulator of the Wnt/β-catenin pathway involved in osteoblast differentiation. Cell Death Differ. 2015;22:912–920. doi: 10.1038/cdd.2014.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Graves L.L., Bukata S.V., Aghazadehsanai N., Chang T.I., Garrett N.R., Friedlander A.H. Patients Receiving Parenteral Bisphosphonates for Malignant Disease and Having Developed an Atypical Femoral Fracture Are at Risk of Concomitant Osteonecrosis of the Jaw: An Evidence-Based Review. J. Oral Maxillofac. Surg. 2016;74:2403–2408. doi: 10.1016/j.joms.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 286.Lundberg A.P., Roady P.J., Somrak A.J., Howes M.E., Fan T.M. Zoledronate-Associated Osteonecrosis of the Jaw in a Dog with Appendicular Osteosarcoma. J. Vet. Intern. Med. 2016;30:1235–1240. doi: 10.1111/jvim.13980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Kharazmi M., Hallberg P., Warfvinge G., Michaëlsson K. Risk of atypical femoral fractures and osteonecrosis of the jaw associated with alendronate use compared with other oral bisphosphonates. Rheumatology. 2014;53:1911–1913. doi: 10.1093/rheumatology/keu286. [DOI] [PubMed] [Google Scholar]
- 288.Kobayashi M., Takiguchi T., Suzuki R., Yamaguchi A., Deguchi K., Shionome M., Miyazawa Y., Nishihara T., Nagumo M., Hasegawa K. Recombinant human bone morphogenetic protein-2 stimulates osteoblastic differentiation in cells isolated from human periodontal ligament. J. Dent. Res. 1999;78:1624–1633. doi: 10.1177/00220345990780100701. [DOI] [PubMed] [Google Scholar]
- 289.Safaeinejad Z., Kazeminasab F., Kiani-Esfahani A., Ghaedi K., Nasr-Esfahani M.H. Multi-effects of Resveratrol on stem cell characteristics: Effective dose, time, cell culture conditions and cell type-specific responses of stem cells to Resveratrol. Eur. J. Med. Chem. 2018;155:651–657. doi: 10.1016/j.ejmech.2018.06.037. [DOI] [PubMed] [Google Scholar]
- 290.Corsalini M., Di Venere D., Carossa M., Ripa M., Sportelli P., Cantatore F., De Rinaldis C., Di Santantonio G., Lenoci G., Barile G., et al. Comparative clinical study between zirconium-ceramic and metal-ceramic fixed rehabilitations. Oral Implantol. 2018;11:150–160. [Google Scholar]
- 291.LaFoya B., Munroe J.A., Albig A.R. A comparison of resveratrol and other polyphenolic compounds on Notch activation and endothelial cell activity. PLoS ONE. 2019;14:e0210607. doi: 10.1371/journal.pone.0210607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Ornstrup M.J., Harsløf T., Sørensen L., Stenkjær L., Langdahl B.L., Pedersen S.B. Resveratrol Increases Osteoblast Differentiation In Vitro Independently of Inflammation. Calcif. Tissue Int. 2016;99:155–163. doi: 10.1007/s00223-016-0130-x. [DOI] [PubMed] [Google Scholar]
- 293.Wang X., Ma S., Meng N., Yao N., Zhang K., Li Q., Zhang Y., Xing Q., Han K., Song J., et al. Resveratrol Exerts Dosage-Dependent Effects on the Self-Renewal and Neural Differentiation of hUC-MSCs. Mol. Cells. 2016;39:418–425. doi: 10.14348/molcells.2016.2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Wang Z., Wu Y., Wang J., Zhang C., Zhu M., Wang K., Li C., Xu Q., Kong D. The effect of resveratrol on modulation of endothelial cells and macrophages for rapid vascular regeneration from electrospun poly(ε-caprolactone) scaffolds. ACS Appl. Mater. Interfaces. 2017;9:19541–19551. doi: 10.1021/acsami.6b16573. [DOI] [PubMed] [Google Scholar]
- 295.Abed É., Delalandre A., Lajeunesse D. Beneficial effect of resveratrol on phenotypic features and activity of osteoarthritic osteoblasts. Arthritis Res. Ther. 2017;19:151. doi: 10.1186/s13075-017-1365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Sarubbo F., Esteban S., Miralles A., Moranta D. Effects of Resveratrol and other Polyphenols on SIRT-1: Relevance to Brain Function During Aging. Curr. Neuropharmacol. 2018;16:126–136. doi: 10.2174/1570159X15666170703113212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Guo D.-W., Han Y.-X., Cong L., Liang D., Tu G.-J. Resveratrol prevents osteoporosis in ovariectomized rats by regulating microRNA-338-3p. Mol. Med. Rep. 2015;12:2098–2106. doi: 10.3892/mmr.2015.3581. [DOI] [PubMed] [Google Scholar]
- 298.Mizutani K., Ikeda K., Kawai Y., Yamori Y. Resveratrol attenuates ovariectomy-induced hypertension and bone loss in stroke-prone spontaneously hypertensive rats. J. Nutr. Sci. Vitaminol. 2000;46:78–83. doi: 10.3177/jnsv.46.78. [DOI] [PubMed] [Google Scholar]
- 299.Feng J., Liu S., Ma S., Zhao J., Zhang W., Qi W., Cao P., Wang Z., Lei W. Protective effects of resveratrol on postmenopausal osteoporosis: Regulation of SIRT-1-NF-κB signaling pathway. Acta Biochim. Biophys. Sin. 2014;46:1024–1033. doi: 10.1093/abbs/gmu103. [DOI] [PubMed] [Google Scholar]
- 300.Lin Q., Huang Y., Xiao B., Ren G.-F. Effects of Resveratrol on Bone Mineral Density in Ovarectomized Rats. Int. J. Biomed. Sci. IJBS. 2005;1:76–81. [PMC free article] [PubMed] [Google Scholar]
- 301.Zhang P., Li Y., Du Y., Li G., Wang L., Zhou F. Resveratrol Ameliorated Vascular Calcification by Regulating Sirt-1 and Nrf2. Transplant. Proc. 2016;48:3378–3386. doi: 10.1016/j.transproceed.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 302.Dai Z., Li Y., Quarles L.D., Song T., Pan W., Zhou H., Xiao Z. Resveratrol enhances proliferation and osteoblastic differentiation in human mesenchymal stem cells via ER-dependent ERK1/2 activation. Phytomedicine. 2007;14:806–814. doi: 10.1016/j.phymed.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 303.Mizutani K., Ikeda K., Kawai Y., Yamori Y. Resveratrol stimulates the proliferation and differentiation of osteoblastic MC3T3-E1 cells. Biochem. Biophys. Res. Commun. 1998;253:859–863. doi: 10.1006/bbrc.1998.9870. [DOI] [PubMed] [Google Scholar]
- 304.Zhao X.-E., Yang Z., Zhang H., Yao G., Liu J., Wei Q., Ma B. Resveratrol Promotes Osteogenic Differentiation of Canine Bone Marrow Mesenchymal Stem Cells Through Wnt/Beta-Catenin Signaling Pathway. Cell. Reprogram. 2018;20:371–381. doi: 10.1089/cell.2018.0032. [DOI] [PubMed] [Google Scholar]
- 305.Tseng P.-C., Hou S.-M., Chen R.-J., Peng H.-W., Hsieh C.-F., Kuo M.-L., Yen M.-L. Resveratrol promotes osteogenesis of human mesenchymal stem cells by upregulating RUNX2 gene expression via the SIRT-1/FOXO3A axis. J. Bone Miner. Res. 2011;26:2552–2563. doi: 10.1002/jbmr.460. [DOI] [PubMed] [Google Scholar]
- 306.Lorusso F., Noumbissi S., Inchingolo F., Rapone B., Khater A.G.A., Scarano A. Scientific Trends in Clinical Research on Zirconia Dental Implants: A Bibliometric Review. Materials. 2020;13:5534. doi: 10.3390/ma13235534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Blair H.C., Athanasou N.A. Recent advances in osteoclast biology and pathological bone resorption. Histol. Histopathol. 2004;19:189–199. doi: 10.14670/HH-19.189. [DOI] [PubMed] [Google Scholar]
- 308.Adina S., Dipalma G., Bordea I.R., Lucaciu O., Feurdean C., Inchingolo A.D., Septimiu R., Malcangi G., Cantore S., Martin D., et al. Orthopedic joint stability influences growth and maxillary development: Clinical aspects. J. Biol. Regul. Homeost. Agents. 2020;34:747–756. doi: 10.23812/20-204-E-52. [DOI] [PubMed] [Google Scholar]
- 309.Coloccia G., Inchingolo A.D., Inchingolo A.M., Malcangi G., Montenegro V., Patano A., Marinelli G., Laudadio C., Limongelli L., Di Venere D., et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina. 2021;57:288. doi: 10.3390/medicina57030288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Inchingolo F., Tatullo M., Marrelli M., Inchingolo A.M., Tarullo A., Inchingolo A.D., Dipalma G., Podo Brunetti S., Tarullo A., Cagiano R. Combined occlusal and pharmacological therapy in the treatment of temporo-mandibular disorders. Eur. Rev. Med. Pharmacol. Sci. 2011;15:1296–1300. [PubMed] [Google Scholar]
- 311.Rapone B., Ferrara E., Santacroce L., Cesarano F., Arazzi M., Di Liberato L., Scacco S., Grassi R., Grassi F.R., Gnoni A., et al. Periodontal Microbiological Status Influences the Occurrence of Cyclosporine-A and Tacrolimus-Induced Gingival Overgrowth. Antibiotics. 2019;8:124. doi: 10.3390/antibiotics8030124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Sakkas A., Wilde F., Heufelder M., Winter K., Schramm A. Autogenous bone grafts in oral implantology—Is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant Dent. 2017;3:23. doi: 10.1186/s40729-017-0084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Rapone B., Converti I., Santacroce L., Cesarano F., Vecchiet F., Cacchio L., Scacco S., Grassi R., Grassi F.R., Gnoni A., et al. Impact of Periodontal Inflammation on Nutrition and Inflammation Markers in Hemodialysis Patients. Antibiotics. 2019;8:209. doi: 10.3390/antibiotics8040209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Gargiulo C., Inchingolo F., Nguyen K., Aityan S., van Pham H., Dipalma G., Ballini A., Strong D.M., Filgueira L., Tran T., et al. Aging and Metabolic Disorders, the Role of Molecular Mechanisms Leading to Bone Degeneration as a Possible Cause of Implant and Graft Loss: A Review. SignPost; New York, NY, USA: 2019. [Google Scholar]
- 315.Dimonte M., Inchingolo F., Minonne A., Arditi G., Dipalma G. Bone SPECT in management of mandibular condyle hyperplasia. Report of a case and review of literature. Minerva Stomatol. 2004;53:281–285. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All experimental data to support the findings of this study are available by contacting the corresponding author upon request.