Abstract
Background
Latinx populations have experienced disproportionately high case rates of COVID-19 across the USA. Latinx communities in non-traditional migration areas may experience greater baseline day-to-day challenges such as a lack of resources for immigrants and insufficient language services. These challenges may be exacerbated by the COVID-19 pandemic.
Objective
This article describes the results of an initial community health needs assessment to better understand the prevention and care of COVID-19 infection in the Cincinnati Latinx community.
Methods
We used convergent mixed methods to examine barriers and facilitators to COVID-19 prevention and care for those with infection.
Results
Latinx adults ≥ 18 years old completed 255 quantitative surveys and 17 qualitative interviews. Overarching mixed methods domains included knowledge, prevention, work, challenges, and treatment. Quantitative results largely reinforced qualitative results (confirmation). Certain quantitative and qualitative results, however, diverged and expanded insights related to caring for COVID-19 infection among Latinx adults (expansion). There were infrequent contradictions between quantitative and qualitative findings (discordance). Primary barriers for the Latinx community during the COVID-19 pandemic included insecurities in food, jobs, housing, and immigration. Key facilitators included having trusted messengers of health-related information.
Conclusion
Public health interventions should be centered on community partnerships and the use of trusted messengers. Wraparound services (including resources for immigrants) are essential public health services. Close partnership with employers is essential as lack of sick leave and mask supplies were more frequent barriers than knowledge. These findings emerged from experiences during the COVID-19 pandemic but likely generalize to future public health crises.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-022-01294-7.
Keywords: Community, COVID-19, Health disparities, Latinx, Mixed methods
To date, the coronavirus disease 2019 (COVID-19) has infected > 269 million individuals worldwide [1]. A disproportionate number of COVID-19 infections, hospitalization, and deaths in the USA have occurred among racial and ethnic minorities [2, 3]. This has been true among Latinx individuals; areas with larger populations of Central American immigrants have had especially high COVID-19 incidence rates [4–6]. The national data suggest that such patterns are associated with social determinants of health including crowded housing, multigenerational households, frontline role within the workforce, lack of access to sick leave, and varying access to healthcare [7–11]. Previous study of COVID-19 knowledge and prevention behaviors among Latinx adults has been limited by a lack of data on information sources about COVID-19 [12] and by online data collection procedures that may limit the participation of low-income sub-populations of Latinx adults [13]. Additionally, evaluation of Latinx experiences of public health practices during the pandemic has been limited to either qualitative or quantitative methodology alone. Qualitative methods, in isolation, are less suited to establish prevalence of beliefs or behaviors. Quantitative methods, in isolation, lack the deeper context that can be elucidated about drivers of beliefs or behaviors [14]. Studies with limited community partner engagement, including across a metropolitan area, may leave meaningful local concerns unaddressed [12–14].
Latinx communities in non-traditional migration areas (i.e., areas outside of traditional Latinx immigrant locations such as Houston) have experienced rapid population growth [15] and may experience greater challenges such as limited social networks and insufficient Spanish language services [16]. These challenges have likely been exacerbated by the pandemic [17]. Cincinnati is a non-traditional migration city that 60,000 Latinx people call home [18]. The Latinx population in Cincinnati is growing at a rate of ~ 13% per year [19, 20]. In Cincinnati, between March and November 2020, Latinx individuals accounted for 18.6% of all COVID-19 cases despite representing just 3.7% of city residents [8, 21, 22]. During that same time period, 53% of all COVID-positive laboring mothers in area birth hospitals and 37% of all COVID-positive children requiring hospitalization at Cincinnati Children’s Hospital Medical Center (CCHMC) identified as Latinx [23].
Given this initial case burden, local hospitals and community and public health agencies came together to identify community concerns about gaps in COVID-19 prevention and access to care. Key convening groups of stakeholders included the Greater Cincinnati Latino Coalition or Apoyo Latino, led by co-author LG, and the Latino Health Collaborative (LHC), led by co-author CD. Apoyo Latino is a Cincinnati network of 67 agencies, advocates, and community leaders working to improve access to culturally competent services for Latinx families [24], while the LHC is a Cincinnati collective of 17 academic and community organizations seeking to advance the health of Latinx families [25]. From community concerns, stakeholders formulated a range of hypotheses, specifically that the Cincinnati Latinx community had limited access to education about COVID-19, a lack of available resources to meet basic needs (e.g., food, hygiene supplies), sick family members holding essential jobs, inadequate personal protective equipment (PPE) supplies, fear about sharing information due to undocumented status, and confusion about treatments. A multi-institution and community agency collaborative sought to test these hypotheses and design targeted public health messaging and basic need interventions (food, housing, etc.). The collaborative saw its work as relevant locally and potentially generalizable to other regions experiencing similar challenges.
This article describes our use of mixed methods (MM) [26] to better understand barriers and facilitators to prevention and care of COVID-19 infection among those in the Cincinnati Latinx Community. This work was guided by the National Institute on Minority Health and Health Disparities (NIMHD) Research Framework [21]. Within this framework, we were interested in examining four domains—behavioral, physical or built environment, sociocultural environment, and healthcare system—across four levels of influence: individual, interpersonal, community, and societal. Our primary objective was to evaluate barriers and facilitators to COVID-19 prevention and management. Therefore, we included specific questions about COVID-19 knowledge and prevention behaviors (masking, handwashing, physical distancing, quarantining, etc.). This work was done in collaboration with community partners for the purpose of immediate application and local action. Thus, this study was unique given the use of a mixed methods approach, complementing qualitative with quantitative findings, and given a commitment to consistent, meaningful community engagement throughout the research process.
Methods
Study Design
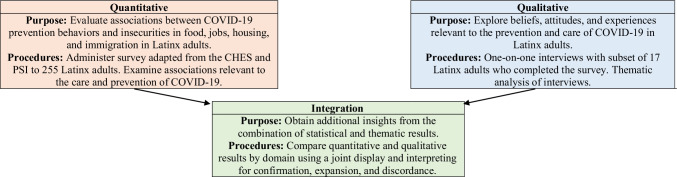
This study used a convergent MM design [27] (Fig. 1). Quantitative and qualitative data collection and analysis were conducted concurrently and independently. Integration or mixing analysis was conducted to determine the level of convergence and divergence of the findings. A convergent MM design was chosen because of its potential to help address the urgent problem of COVID-19 infection occurring within Cincinnati’s Latinx community at a time when the research team had limited access to vulnerable Latinx participants for data collection. The integrated insights from the convergent MM design had the potential to improve academic and community understanding faster than the pursuit of separate quantitative or qualitative analyses [28]. This study was reviewed and jointly approved as non-human subjects research by institutional review boards at our two academic medical centers.
Fig. 1.
Procedural diagram of convergent mixed methods study
Participants
Study inclusion criteria were self-identified Latinx (Hispanic or Latino/a) ethnicity, age ≥ 18 years, and residence within Greater Cincinnati. Participants completed quantitative surveys and semi-structured, qualitative interviews. Individuals who participated in qualitative interviews were nested among those completing quantitative surveys [29]. Recruitment, consent, surveys, and interviews were conducted in the participant’s preferred language (Spanish or English). Because the overarching goal of our study was to work with community partners to accelerate immediate and local action, and identify as many Latinx participants as possible, we opted to pursue convenience sampling. Previous study by co-author FJ has found that Latinx people in non-traditional migration areas like Cincinnati experience disparities in healthcare infrastructure and social support that vary by region and neighborhood [16]. To maximize the overlap of regions or neighborhoods with high Latinx populations and previously observed disparities, recruitment efforts were concentrated in the northern Hamilton County neighborhood of Springdale, the Price Hill and Westwood neighborhoods on the west side of Cincinnati, and the Norwood area in central Hamilton County in Ohio [16]. We also recruited participants from Covington, a city in Kenton County, Kentucky, located immediately south of Cincinnati—Covington has seen recent, rapid growth in its Latinx population [30, 31]. We used recruitment strategies, as pursued by Topmiller et al. and in collaboration with community partners, to enhance the likelihood of a representative sample of the Greater Cincinnati Latinx community through targeted recruitment at events in the aforementioned specific neighborhoods. Participants were also recruited at community agencies, churches, and food distribution events across the metropolitan area [16].
Data Collection
Surveys were administered by a 10-member team of bilingual community health workers (CHWs) and students from July 2020 to September 2020. The quantitative surveys were done in person, over the phone, or via paper depending on participant social distancing preferences, taking 15–20 min to complete. Quantitative data were entered into a secured REDCap database. Spanish and English text was available for each question of the paper survey. Repeated check-ins were completed with the community groups Apoyo Latino and the LHC to ensure that CHWs collected participant data at a variety of events hosted in a variety of neighborhoods. All CHWs completed required CITI training for human subjects research and received training from co-author KJM on research methods, survey administration, and data integrity. Co-author SRH received additional training on qualitative interviewing. Data collection was supervised by co-author KJM through periodic check-ins with CHWs conducting surveys and interviews.
Measures
Quantitative Survey
Survey questions were adapted from the COVID-19 Household Environment Scale (CHES) [32] and the Pandemic Stress Index (PSI) (Appendix Table 1) [33, 34]. The CHES measures family functioning, conflict, and cohesion, while the PSI measures behavior changes and stress that individuals may have experienced during COVID-19. These scales were selected because of alignment with the relevant NIMHD domains of influence on which we framed our study. The survey consisted of 60 total items, with the actual number of items completed dependent on the participants’ previous responses using branching logic. Survey items were developed by co-authors KJM and ARLR and revised prior to data collection via an iterative feedback process with co-authors LG and CD (community partners) and YX (biostatistician). The survey also assessed health-related social needs experienced by respondents before and after March 2020. Specifically, insecurities in food, jobs, housing, and immigration were assessed via retrospective recall, with options of “Yes, before March”; “Yes, since March”; or “No, not before March and not after March.” Prompts included (1) food insecurity, “Please indicate if you are worried whether your food would run out before you got money to buy more”; (2) housing insecurity, “Housing problems such as overcrowding, roaches, utilities, mold, or lead that your landlord is not helping with?”; (3) eviction problems, “Being threatened with eviction or losing your home?”; (4) job insecurity, “Are you worried about losing your job/source of income due to COVID?” or “Did you lose your source of income because of COVID-19/coronavirus?”; and (5) immigration insecurity, “Were you concerned about deportation, detention, or family separation by United States immigration for yourself, a family member, or a community member.”
Qualitative Interviews
At the time of survey completion, participants were given the option to complete a semi-structured, qualitative interview at a separate time (Appendix Table 2). All interviews were done via phone by bilingual CHW and co-author SRH, recorded using Zoom. They lasted 10–40 min. Nine interviews were conducted in Spanish, eight in English. Interviews were pursued using a qualitative approach that employed open-ended questions to enable in-depth exploration of individual narratives [35–37]. Interviews began with an assessment of participant home and family life [38]. This laid necessary groundwork for discussing COVID-19-specific knowledge and beliefs [39]. COVID-19-specific questions were adapted from the COVID-19 Impact on Health and Wellbeing Survey [40] and were re-written to be open-ended and explore participant perspectives [41]. While this survey is yet to be validated, it was chosen because of its listing in both the National Institutes of Health (NIH) COVID-19 Office of Behavioral and Social Sciences Research data collection instruments and the National Institute of Environmental Health Sciences (NIEHS) Disaster Research Response Resources Portal [42, 43].
Data Analysis
Quantitative Analysis
Free-text survey responses were coded by co-authors KJM and ARLR (Appendix Table 3). To measure participant knowledge, free-text responses were coded for survey questions “What is COVID-19?”; “What are symptoms of COVID-19?”; and “How can you protect yourself and others from COVID-19?” Through a process of independent coding and resolving of differences through discussion and refinement [44, 45], co-authors KJM and ARLR derived three variables for analysis: knowledge of COVID-19, knowledge of COVID-19 symptoms, and knowledge of COVID-19 prevention (Appendix Table 3). For example, based on the question “What is COVID-19?”, we coded knowledge of COVID-19 as “Yes” if participants mentioned any of the following, “SARS,” “disease,” “virus,” “illness,” “germ,” “cold,” or “flu,” and coded knowledge of COVID-19 as “No” if participants did not mention any of the valid responses listed above or responded with any of the following responses: “bacteria,” “Chinese,” or “I don’t know.” In addition to knowledge of COVID-19 prevention, prevention behaviors were measured using the following survey questions “Do you wear a mask?”; “Have you practiced social distancing”; “Should you go to work if you have symptoms?”; and “Should you go to work if you are positive for COVID-19 but don’t have symptoms?” (Appendix Table 3). Descriptive statistics enumerated question response frequencies. We conducted a series of bivariate analyses examining associations between insecurities, information sources, and COVID-19-related knowledge and prevention behaviors using Chi-square or Fisher’s exact tests, as appropriate. Specifically, our insecurity analysis included an evaluation of associations between various insecurities (food, employment, housing problems, eviction treats, and immigration insecurity, each examined separately) and COVID-19-related knowledge and prevention behavior outcomes. In our analysis of information sources, we examined the association between a specific information source and the COVID-19-related knowledge and prevention behavior outcomes. In addition, we compared basic needs and immigration insecurity before and after the start of pandemic (March 2020), using McNemar’s test. All quantitative analyses were pursued using SAS® version 9.4.
Qualitative Analysis
Interviews were recorded and transcribed. Spanish interviews were transcribed in Spanish, translated into English for coding, and back-translated to verify translation accuracy [46, 47]. Data were analyzed by two academic coders (KJM and ARLR) and one community coder (CC) using Dedoose qualitative software to complete thematic analysis [48, 49]. Each coder completed repeated independent readings (familiarization) of the data for the first three interviews [50]. Familiarization was followed by team meetings to discuss emergent codes and reach agreement on a master codebook. Using the master codebook, each interview was then individually coded by two of the three coders, with each team member coding 11–12 interviews in total. Team meetings were held periodically to discuss coding and achieve consensus, identify themes, and develop an initial data report [51]. Memoing was used to document decisions made throughout coding [52, 53]. We conducted a member-checking process [54, 55] by soliciting feedback on preliminary findings from community stakeholders at a virtual (Zoom) forum. During the forum, stakeholders reviewed lists of themes and determined whether they made sense. We included their responses in the final results [56]. Salient quotes were identified for inclusion in this article by co-authors KJM and ARLR. Once qualitative themes were identified, we then examined themes in light of the NIMHD research framework as an additional layer of interpretation [21]. Within the NIMHD framework, qualitative themes were examined in four domains—behavioral, physical or built environment, sociocultural environment, and healthcare system—across four levels of influence: individual, interpersonal, community, and societal [21].
Integration
Integration was conducted to enhance validation and identify further insights through triangulation of quantitative and qualitative results [57, 58]. For each major domain (e.g., knowledge and prevention), we arrayed the main quantitative and qualitative findings in a joint display table to facilitate alignment [59]. Comparisons between quantitative and qualitative findings for each domain were interpreted in terms of three possible outcomes [59, 60]: (1) confirmation (when quantitative results reinforced qualitative results or vice versa), (2) expansion (when quantitative and qualitative results diverged and helped expand insights by addressing different or complementary findings), and (3) discordance (when quantitative and qualitative findings contradicted or disagreed with one another).
Results
Quantitative Survey Results
The 255 individuals completing the quantitative survey were 72.2% female (20% male, 7.8% missing) with a mean age of 36.5 (± 10.9) years old. Most had some knowledge of COVID-19 (> 85%) or its symptoms (92.2%). Most also pursued some prevention behaviors (98.4% masking, 96.1% social distancing, 98% not going to work if symptomatic, 95.3% not going to work if tested positive) or had some prevention knowledge (96.5%) (Table 1).
Table 1.
Quantitative COVID-19 survey results of Latinx participants
| Item | Yes | No | Missing | |||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||
| Knowledge of COVID-19 | 219 (85.9) | 34 (13.3) | 2 (0.8) | |||
| Knowledge of COVID-19 symptoms | 235 (92.2) | 18 (7.1) | 2 (0.8) | |||
| Knowledge of COVID-19 prevention | 246 (96.5) | 8 (3.1) | 1 (0.4) | |||
| I wear a mask | 251 (98.4) | 3 (1.2) | 1 (0.4) | |||
| I wear a mask | ||||||
| At home | 17 (6.7) | 238 (93.3) | - | |||
| At work | 172 (67.5) | 83 (32.5) | - | |||
| At the grocery store | 177 (69.4) | 78 (30.6) | - | |||
| Inside public places | 238 (93.3) | 17 (6.7) | - | |||
| Outside public places | 222 (87.1) | 33 (12.9) | - | |||
| I practice social distancing | 245 (96.1) | 8 (3.1) | 2 (0.8) | |||
| I should work if symptomatic | 2 (0.8) | 250 (98.0) | 3 (1.2) | |||
| I should work if I am positive for COVID but do not have symptoms | 8 (3.1) | 243 (95.3) | 4 (1.6) | |||
| My primary source of information about COVID-19 is: | ||||||
| National TV | 163 (63.9) | 92 (36.1) | - | |||
| Local TV | 120 (47.1) | 135 (52.9) | - | |||
| Local radio | 47 (18.4) | 208 (81.6) | - | |||
| National newspaper | 20 (7.8) | 235 (92.2) | - | |||
| Local newspaper | 16 (6.3) | 239 (93.7) | - | |||
| Social media | 146 (57.3) | 109 (42.7) | - | |||
| Family or friends | 119 (46.7) | 136 (53.3) | - | |||
| Community or religious groups | 94 (36.9) | 161 (63.1) | - | |||
| Health professionals | 58 (22.7) | 197 (77.3) | - | |||
| Local or national websites | 68 (26.7) | 187 (73.3) | - | |||
| Other sources | 22 (8.6) | 233 (91.4) | - | |||
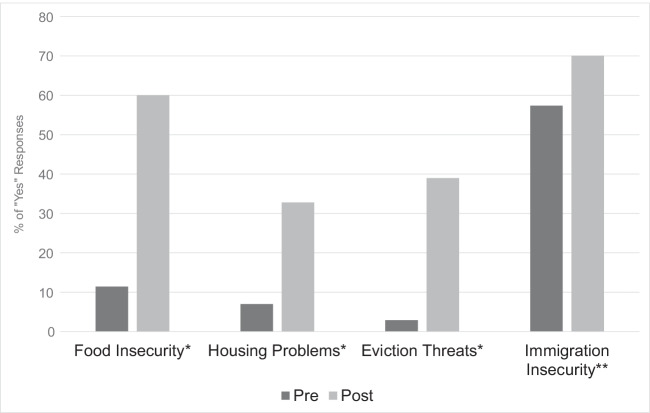
Both job and immigration insecurity were common among respondents after the onset of the pandemic. There was a significant increase in the proportion of participants reporting food or housing insecurities after March 2020 compared to before March 2020 (Fig. 2). Participants with job insecurity during the pandemic were more likely than those without job insecurity to experience food insecurity (73% vs. 39%, p < 0.0001), housing problems (44% vs. 14%, p < 0.0001), and eviction threats (55% vs. 9%, p < 0.0001). Similarly, participants with immigration insecurity during the pandemic were more likely than those not experiencing immigration insecurity to have food insecurity (72% vs. 43%, p < 0.0001), housing problems (50% vs. 13%, p < 0.0001), and eviction threats (58% vs. 13%, p < 0.0001). We did not observe any significant associations between these insecurities and COVID-related knowledge (Appendix Table 4) or prevention behaviors (Appendix Table 5).
Fig. 2.
Insecurities in food, housing, eviction, and immigration before vs. after March 2020. *p value < 0.0001; **p value = 0.20
The most used sources of health-related information were national TV (64%), social media (57%), local TV (47%), family/friends (47%), and community groups (37%) (Table 1). Most participants used 2–5 different sources of information; general knowledge and knowledge of symptoms varied by information source. Those who used social media had more general knowledge compared to those who did not use social media (90% vs. 82%, p = 0.046). Those who relied on family or friends for information had more general knowledge and knowledge about symptoms compared to those that did not rely on family or friends (94% vs. 80%, p = 0.001 for general knowledge, 98% vs. 88%, p = 0.003 for symptoms). Those who used health professionals as an information source had more symptoms knowledge than those who did not (100% vs. 91%, p = 0.02). There was a larger proportion of respondents with knowledge of COVID-19 symptoms among those who used websites as an information source compared to those who did not (98% vs. 91%, p = 0.03).
Qualitative Interview Results
Qualitative themes were knowledge, prevention, work, challenges, and treatment (Table 2).
Table 2.
Qualitative findings
| Themes | Sub-themes | Quotes | |
|---|---|---|---|
| Knowledge | Knowledge of… | Knowledge about COVID | “It is a very serious viral disease. Easily contacting or contracted, spread through maybe some droplets emanating from the mouth or maybe the nose. If you get it on your hand, you can spread it to other people through contact, and maybe on yourself from your hands onto your nose, lips and eyes. That’s what I know. It can be dangerous, and it can be fatal” |
| Knowledge alleviates fear about testing | “I have…heard on the news that right now…if you get seriously ill, don’t be afraid to go to the hospital because right now the police will not be asking if you are legal or if you have papers because some people are very sick and out of fear they don't go to the doctor. I keep hearing that you shouldn’t be afraid and that you should go to the doctor, that they shouldn’t be afraid if they are legal or non-legal…I realized that they do the test without asking any status or something like a legal document…now I can share that information with the rest of the community [so] that they can go get tested without any issues” | ||
| Lack of knowledge… | “I wish more information would be available to my Spanish speaking families. Everything being handed out is in English and there is a disconnect with what our families are going through….I go to grocery stores or…even at [a] place of work and…I see people walking in with the kids, no masks on stuff like that [and] you know some of them…don’t speak the language [and/or] they [are] probably like “Should I do it? Should I not?”…I think it’s the language…sadly I read on social media that cases for Hispanics…there [are] more of them than there is other races, and sometimes those are the places here” | ||
| Prevention | Facilitators to prevention | Individual social responsibility | “It is so they won’t spread the illness to other people or so they don’t bring the illness to the church [and] especially the community has many families and many kids. It is what I think this means to take care of others not just ourselves, for them and me and…especially the elderly” |
| Community-based PPE | “To prevent COVID we hardly go out on the street, we do not take the children to stores, to public places where there are many people. If we do take them, they wear masks and we try not to be too close together.” | ||
| Employer-based PPE | “They disinfect, they try, and everyone brings their own tools. They try to not use each other’s tools. They gave [PPE] to him. He has it there at work” | ||
| Barriers to prevention | Employer-based PPE | “Yes, he [her husband] needed it. He had to buy it, buy the gloves, mask [for himself]. He had to buy all of that” | |
| Barriers to social distancing | “And then people will say, “well just take the bus,” ok well what if they have five kids? Do they put all of the five kids on this public bus, that is you know 12 people sat in that chair within the hour?” | ||
| Work | Job insecurity | Going to work sick due to fear of losing job | “Because many get sick…They prefer silence,…because they know the company …makes you go get tested so you can bring the results and fill out the forms and all of that so you can rest. Well, if they lay you off, who is going to pay your bills? No one is going to pay you for 14, 10, 15 days, no one is going to pay…” |
| Job security | Sick leave | “My husband was giving sick leave. My brother lost his job…” | |
| Challenges | Economic challenges | Job and immigration insecurity | “Many people when they feel sick of a headache or fever…you tell the company “I can’t go to work because I have a fever,”…the company forces you to get a test and because many people are illegal, undocumented they don’t go to get tested…They prefer silence, to not say anything because they know the company asks for a test and makes you go get tested so you can bring the results and fill out the forms…Well, if they lay you off, who is going to pay your bills? No one is going to pay [and] that is why many people knowing the company asks for a bunch of papers prefer to not say anything.”…A lot of the undocumented men…have been going to work because they need to work. If they lose this job it will be too hard to get another…a lot of times they went to work despite having…symptoms [and] these ended up being hotspots for COVID cases” |
| Job and housing insecurity | “the concern of the entire Hispanic community is losing our job. In fact, as far as I know, several people lost their jobs, such as in restaurants, in hotels, and thank God I have mine, but I believe that losing a job and not being able to pay rent is more of a concern for the community” | ||
| Job and food insecurity | “The day when I don’t… have a job I would worry about not having food” | ||
| Immigration fear, insecurity, or uncertainty | “[Regarding barriers to accessing care] more than anything is the documentation, we are not legal…It is a fear because now that I went to the clinic … at the clinic they did a test and they did not ask me documentation, simply my identification from Guatemala so it is a fear that we have, but I went for a cough, not for a test but I realized that they do the test without asking any status or something like a legal document. So now I can share that information with the rest of the community that they can go get tested without any issues” | ||
| Family challenges | Switch to virtual | “Some of the technology is way beyond some of our parents because they’ve never been beyond or engrossed in it, or trained in it [and] a lot of them don’t have [it.] There’s a digital inequity. They don’t have the internet, and if they do they have it for their phone [they] don’t have the data plan that would allow their children to be on it for the whole day” | |
| Childcare or school stress | “Here at home they do not learn the same, that also worries me that being at home they do not learn the same as they are at the school being there with their teachers learning …The problem is that we Latinos have children. It is harder here to hire a baby-sitter and who will we leave our little one with? More than anything…My son, leaving him alone. I don’t know how he will react” | ||
| Marital stressors | “One thing that came up recently was spousal abuse. [There] aren’t that many places where they can go, the females can go, for shelter…in the Latino culture… the man working is very important…provide for his family…. that tends to have consequences for the home environment…excessive drinking, short-tempered, verbal abuse …and eventually then physical blows against children and the spouse” | ||
| Treatment | Barriers to care | Distrust of health providers | “[Latinx] don’t want to go to the doctor. I [know a] few people [that say] ‘well you go to the doctor, they will, they will hurt [you.’ They] believe…conspiracy theories, that you will see a doctor [and] they will inject you [with] the virus…I think that a lot of it is the skepticism behind [seeing health professionals], the [belief] that God is going to keep you safe…and that Vicks VapoRub fixes everything [and] eating healthier will fix everything” |
| No PCP | “I know I am a patient, because my primary doctor speaks Spanish, but my husband doesn’t have anyone else, and my husband doesn’t have insurance and I believe he has been exposed” | ||
| Alternative treatment | “In myself, when [I got covid] … When I started, I was very cold and later I was a little hot, body aches, headaches, and a lot of chills. That was when I started. Later at night I made a home remedy, I do not know if you have heard of any home remedies, home remedy is a tea that we prepare here at home” | ||
| Facilitators to care | Family support | “I got my parents…a couple of sisters…a brother [and] friends [close by] that…help…to…go out and get stuff…if we were to go through [quarantine] we would get help…we have [also] helped when [other] people [in the community] get sick. Sometimes we have delivered fruit [and] leave it by the door and we call them to let them know [we have delivered fruit]. That is what we have done. Helping them by giving them food. Also, the community has offered to pay rent and bills if [needed.] If [everyone gets] sick, if all [of] the family is sick…they stay in quarantine and we offer to bring lunch and leave it at the door” | |
| Community or agency support | “I have the help and support of [a trusted community advocate] who [told me to] ‘go take the test, go do the test’ and if he did not pressure me, I wouldn’t have gone, but he pressured me to do so. [These advocates] have been a very important part of my life, they have helped me to get by with so many problems, mostly emotional, they are my psychologists…I want to thank all the organizations that are with us as a workers’ center…and all the people who are helping us by informing us about the disease with your time because we know that you are taking your time to help the community” | ||
| Church support | “The only other contact I have if things got bad would be to let my church know. We have a very strong support system at the church and I would let them know so if we needed to have someone bring food and other things they would be prepared to do that” | ||
Knowledge
There were two sub-themes: knowledge and lack of knowledge. Participants demonstrated a strong knowledge of COVID-19 disease, symptoms, and prevention. However, misinformation was a challenge due to language barriers and choices of health-related information. Participants suggested that correct information could lead to changed behavior such as choosing to get tested. One participant said:
I have…heard on the news that right now...if you get seriously ill, don’t be afraid to go to the hospital because…the police will not be asking if you are legal…I realized that they do the test without asking any status…now I can share that information with the rest of the community [so] that they can…get tested.
Prevention
There were two sub-themes: facilitators and barriers to prevention. Social responsibility was an example of a facilitator of masking, distancing, and handwashing. One participant said:
It is so they won’t spread the illness to other people or so they don’t bring the illness to the church [and] the community has many families and many kids. It is what I think this means to take care of others not just ourselves, for them and me and…the elderly.
Unique barriers to distancing included the need to take public transportation and care for family members. Limited access to PPE and the inability to distance at work were particularly challenging.
Work
There were two sub-themes: job insecurity and job security. Concerns about maintaining jobs and a stable income were ubiquitous. Many described going to work while sick instead of isolating due to concerns of being laid off or going without pay. One participant said:
Because many get sick…They prefer silence…because they know the company …makes you go get tested so you can bring the results and fill out the forms…so you can rest. Well, if they lay you off…no one is going to pay [the] bills.
Concerns over jobs were compounded by food and housing insecurities faced by participants during the pandemic.
Challenges
There were two sub-themes: economic and family challenges. Numerous participants endorsed economic challenges related to food and housing, often linked to jobs and providing for their families. Immigration insecurity was described as a reason for not seeking care or COVID-19 testing.
Participants described challenges of virtual schooling for children, a challenge compounded by language barriers. Several quotes depicted the agony of having to decide whether to leave a child alone to be able to meet a basic need. Participants also noted that pandemic stress worsened marital stress and/or domestic violence. One participant said:
In the Latino culture…the man working is very important…provide for his family…. that tends to have consequences for the home environment...excessive drinking, short-tempered, verbal abuse…and eventually then physical blows against children and the spouse.
Treatment
There were two sub-themes: barriers and facilitators to care. Participants described distrust of healthcare providers, trust in alternative therapies, and faith in God. Many participants described not having a primary care physician, with some noting this was due in part to language barriers and a lack of insurance. One participant said:
[Latinx] don’t want to go to the doctor. I [know a] few people [that say] ‘well you go to the doctor [and] they will hurt [you.’ They] believe…conspiracy theories, that you will see a doctor [and] they will inject you [with] the virus…I think that a lot of it is…skepticism behind [seeing health professionals]…the [belief] that God is going to keep you safe…and that Vicks VapoRub [and] eating healthier will fix everything.
Facilitators were described in the form of supportive relationships and social networks: family, community agencies, and church. Trusted advocates were described as key facilitators in multiple interviews given their ability to correct misinformation and address barriers to care or meeting basic needs (e.g., obtaining emergency food supply). One participant said:
I have the help and support of [a trusted advocate] who [told me to] go take the test…and if he did not pressure me, I wouldn’t have gone, but he pressured me to do so.
Many participants also endorsed the importance of their faith community for both emotional support and support of basic needs during the pandemic. Additionally, participants described the support they provided to others when they could, giving food, donations, and emotional support to their own family members and neighbors.
Interpretation of Qualitative Sub-themes by NIMHD Domains and Levels of Influence
All NIMHD domains and levels of influence were represented in qualitative sub-themes (Table 3). Our findings demonstrated eight total NIMHD domains and levels of influence, with frequent contributions to the sociocultural environment domain, healthcare system domain, community level of influence, and societal level of influence [21]. Sub-themes were observed at higher frequencies at the intersections of the physical/built environment domain and community level of influence, with sub-themes of employer-based PPE, church support, and job/housing insecurity.
Table 3.
NIMHD domains and levels of influence across qualitative sub-themes
| Levels of influence | |||||
|---|---|---|---|---|---|
| Individual | Interpersonal | Community | Societal | ||
| Domains of influence | Behavioral | Individual social responsibility (health behaviors, coping strategies) | Job and food insecurity (school/work functioning) |
Distrust of health providers (community functioning) Family support (community functioning) |
Sick leave (policies and laws) |
| Physical/built environment | Knowledge about COVID (personal environment) | Marital stressors (household environment) |
Employer-based PPE (community resources) Church support (community resources) Job and housing insecurity (community environment) |
Going to work sick due to fear of losing job (societal structure) | |
| Sociocultural environment | Job and immigration insecurity (response to discrimination) |
Knowledge alleviates fear about testing (social networks) Lack of knowledge… (social networks) |
Community-based PPE (community norms) Barriers to social distancing (local structural discrimination) |
Immigration fear, insecurity, or uncertainty (societal structural discrimination) Switch to virtual (societal structural discrimination) |
|
| Health care system |
No PCP (insurance coverage) Alternative treatment (treatment preferences) |
No PCP (patient–clinician relationship) Alternative treatment (medical decision-making) |
Community or agency support (availability of services) Childcare or school stress (safety net services) |
Community or agency support (quality of care) Sick leave (health care policies) |
|
Mixed Methods Results
Identification of quantitative results that aligned to each qualitative theme helped generate a joint display of the overarching MM domains: knowledge, prevention, work, challenges, and treatment (Table 4). The MM domains reflected the complex interplay and times conflict between the different levels of influences in the NIMHD framework (Table 3).
Table 4.
Joint display of qualitative, quantitative, and mixed methods interpretation
| Qualitative domain | Sub-themes | Bivariate statistics | Quantitative synopsis | Data convergence label | Mixed methods interpretation | |
|---|---|---|---|---|---|---|
| Knowledge | Knowledge of… | Knowledge about COVID | n/a | Most (> 85%) of the participants had some knowledge of COVID or some knowledge of COVID symptoms | Confirmation | Descriptions of individual knowledge of understanding about COVID explain the findings of a high proportion of knowledge about COVID or COVID symptoms |
| Knowledge alleviates fear about testing | n/a | Most common sources of health-related information were national TV, social media, local TV, family/friends, community groups, with most participants using 2–5 difference sources | Expansion | Qualitative interviews demonstrate that for the common sources of health-related information (e.g., social media), correct information about COVID can allay fears | ||
| Lack of knowledge… | p = 0.06 | People who used social media had more knowledge of COVID vs. those who did not use social media | Confirmation | Participants describe obtaining health information from social media, in line with social media users demonstrating more knowledge about COVID in the surveys | ||
| Prevention | Facilitators to prevention | Individual social responsibility | n/a | Most (> 96%) of participants had prevention behaviors or prevention knowledge. Very few had neither | Confirmation | Feelings of individual responsibility for health help to explain findings of a high proportion of prevention behaviors among Latinx adults |
| Community-based PPE | n/a | 96% reported mask-wearing inside in public. 90% reported mask-wearing outside in public | Confirmation | High proportion of mask-wearing echoes adherence expressed during interviews | ||
| Employer-based PPE | n/a | 70% of participants reported mask-wearing at work | Discordance | Latinx adults describe consistent mask-wearing at work, incongruent to the proportion of participants reporting no mask-wearing at work, which may be explained by individuals working outside, e.g., construction | ||
| Barriers to prevention | ||||||
| Barriers to social distancing | n/a | Of the 44% that broke social distancing at least once a week, 40% did so to protect or care for a family or community member | Discordance | Latinx adults describe having to break social distancing frequently, incongruent to the proportion of participants describing practicing prevention behaviors | ||
| Work | Job insecurity | Going to work sick due to fear of losing job | n/a | 16% of Latinx had to break quarantine, usually to go to work or care for others | Expansion | Proportion of participants breaking medical isolation was clarified by descriptions of the need to work or to care for others |
| Job security | Sick leave | |||||
| Challenges | Economic challenges | Job and immigration insecurity | p < .0001 | Those with job insecurity are more likely to have immigration insecurity | Confirmation | Participants describe co-existing concerns about jobs and immigration, in line with associations observed in the quantitative surveys |
| Job and housing insecurity | p < .0001 | Latinx adults with job insecurity are more likely to have housing problems (overcrowding/cockroaches/mold) and eviction threats | Confirmation | Participants describe co-existing concerns about jobs and housing, in line with associations observed in the quantitative surveys | ||
| Job and food insecurity | p < .0001 | Those with job insecurity are more likely to have food insecurity | Expansion | Latinx adults with job concerns may also have concerns about food | ||
| Immigration fear, insecurity, or uncertainty | p < .0001 | Latinx adults with immigration insecurity are more likely to have food insecurity, housing problems (overcrowding/cockroaches/mold), and eviction threats | Expansion | Latinx adults with immigration concerns may also have concerns about food, housing, and eviction | ||
| Family challenges | Switch to virtual | p < 0.05 | Larger proportion having knowledge of COVID-19 symptoms in those who used websites as information source vs. those who did not | Expansion | Disparities in information about COVID symptoms for those able to use websites is one example of digital inequity that occurs because of elements such as Spanish language, access to internet, and digital education/literacy of adults and children | |
| Treatment | Barriers to care | Distrust of health providers | n/a | Low proportion (23%) of healthcare providers as trusted source of health-related information for Latinx adult participants | Confirmation | Participants describe distrust of healthcare providers in interviews, in line with low proportion of healthcare providers as trusted sources in quantitative surveys |
| No PCP | p < 0.05 | Larger proportion having knowledge of COVID-19 symptoms in those who used health professionals as information source vs. those who did not use health professionals | Expansion | Family or community advocates may help to address barriers to healthcare access, such as not having a primary care provider | ||
| Alternative treatment | n/a | Low proportion (10%) using alternative treatment over medical care if ill despite health providers not being a preferred source of information | Discordance | While there is distrust of health professionals in the Latinx community surveyed, the majority would seek medical care if ill | ||
| Facilitators to care | Family support | p < .001 | Larger proportion having knowledge of COVID-19 and COVID-19 symptoms in those who used family or friends as information source vs. those who did not | Expansion | Family and friends provide information about COVID-19 symptoms within a cultural context of helping others in the community | |
| Community or agency support | n/a | 1/3 of participants (37%) noted community or religious groups as their primary source of COVID-19 information | Expansion | Trusted community advocates are an important source of health-related information for Latinx participants | ||
| Church support | ||||||
Qualitative interviews confirmed quantitative survey findings suggestive of a strong knowledge base about COVID-19 and a preference for use of social media as an information source. Quantitative findings suggested that most participants received health-related information from multiple sources. Trusted sources providing correct information could allay fears. Quantitative findings illustrative of the central role family and friends played as information sources were expanded by qualitative interviews highlighting the importance of cultural context of helping others.
Feelings of individual social responsibility expressed during qualitative interviews reinforced quantitative survey findings of a high proportion of prevention behaviors. Yet, discordance was observed between participants describing consistent mask-wearing at work in interviews but reporting less mask-wearing at work in surveys. Similarly, many interviewed described challenges in distancing, frequently because of the need to care for someone in their family or community or because of the need to go to work. Concerns about jobs were described in tandem with concerns about immigration and housing, confirming and expanding associations identified via quantitative modeling.
Qualitative data expanded quantitative data in relation to the use of websites as a source of health-related information. However, interviews also highlighted the influence of limited Spanish language content, intermittent access to the Internet, and insufficient digital literacy. Distrust of healthcare providers expressed during interviews confirmed the low proportion of healthcare providers listed as a trusted source of information during surveys. Surveys showed a larger proportion having knowledge of COVID-19 symptoms among those using health professionals as an information source; this finding was expanded by interviews indicating that trusted messengers helped address barriers to healthcare access such as not having a primary care provider. While distrust of healthcare professionals was noted in surveys, interview participants frequently expressed that they would seek medical care if they felt ill, highlighting a degree of discordance.
Discussion
This MM study evaluated barriers and facilitators to prevention and care of COVID-19 infection within a Latinx community in a non-traditional migration area in the USA. All NIMHD domains and levels of influence (eight total) were demonstrated in study findings. Key identified MM domains related to knowledge, prevention, work, challenges, and treatment. Quantitative results largely reinforced qualitative results (confirmation). There were, however, certain quantitative and qualitative results that diverged and expanded insights related to addressing COVID-19 infection among Latinx adults (expansion). Finally, there were infrequent contradictions between quantitative and qualitative findings (discordance).
Our findings demonstrate eight total NIMHD domains and levels of influence, with frequent contributions to the healthcare system domain and the community level of influence [21]. Consistent with recent policy recommendations to address COVID-19 challenges among Latinx communities within the USA, existing partnerships between Cincinnati’s healthcare systems and Latinx community agencies created opportunities to listen and respond to local needs [61]. Since the submission of this study for peer review, we have leveraged study findings to examine barriers and facilitators for the prevention and care of COVID-19 infection among Latinx adults in the workplace and to develop a community-partnered COVID-19 vaccine education program pilot.
Job concerns were a central barrier identified in our study. Key job-related challenges included impediments to mask-wearing while on the job, work in essential industries, insufficient access to PPE, difficulties with social distancing, and limited workplace supports. Mask-wearing provides an interesting example. Discordant findings—interview participants who reported masking at work and survey participants who reported less masking at work—suggest that many had to make difficult choices. Indeed, it seems that many had to choose whether to protect oneself and family or go to work. Our findings are in line with previous study of jobs, immigration, and housing, highlighting these factors as major social determinants of health among Latinx adults [62]. In terms of Latinx individuals working in essential industries, the most common jobs worked by Latinx adults in the USA are in agriculture, cleaning and maintenance, construction, and service industries [63]. These industries were considered essential during the early phases of the pandemic, preventing many Latinx adults from following stay-at-home orders [64]. Moreover, many essential workers (including Latinx workers) did not receive adequate PPE in the first weeks of the pandemic, increasing potential for exposure, infection, and spread as they were among the first to re-enter the workplace even during lockdown [65]. As essential, often poorly protected workers, Latinx adults had a higher probability of becoming ill, a likelihood magnified by working indoors, in tight quarters, and in spaces with sub-optimal ventilation [64].
We found that the presence or absence of employer-based PPE acted as either a barrier or a facilitator to the prevention of COVID-19 infection among Latinx adults. We also found that job security, e.g., ability to take sick leave, and job insecurity, e.g., needing to go to work sick due to a fear of losing one’s job, influenced Latinx participants’ decisions to work or not work while sick. These results suggest that respondents saw their employment situation as central to their COVID-19-related decision-making. We, therefore, suggest that public health crises are likely to benefit from close partnerships between employers and employees and with public health agencies and stakeholders. Since the submission of this study for peer review, we have extended the current study to examine the Latinx workplace, generating qualitative insights from both employers and their Latinx employees in our region. Preliminary findings from this study indicate challenges and opportunities of the workplace environment (e.g., ability to socially distance), workplace illness prevention (e.g., PPE incentives), and workplace supports (e.g., remote work and childcare). Collectively, our findings align with a previous study that looked specifically at Latinx farmworkers in North Carolina, highlighting tight working conditions and limited masking at work [12]. With respect to COVID-19, workplace culture and norms may be more of a challenge for Latinx adults than knowledge.
Infectious risks to essential workers are compounded by the propensity for Latinx families to live in larger, multigenerational households [66]. Our finding that 16% of Latinx adults had to break medical isolation or quarantine to work or care for others is consistent with previous study of ongoing challenges to prevention and care of COVID-19 infection among US Latinx adults [64]. While living with extended family members can decrease the cost of food, housing, and childcare, it can also increase infection risk and stand in the way of one’s ability to quarantine or isolate [64]. Such constraints are even more pronounced for Latinx families and households with undocumented members [67]. Previous study with Latinx community co-researchers in our setting has found that documentation status is a major challenge to accessing healthcare in our area [68]. These results imply that wraparound services including supports for undocumented immigrants in non-traditional migration areas such as ours are essential public health services.
Our quantitative survey found a high proportion of participants with immigration insecurity, with 57% reporting insecurity before March 2020 and 70% reporting insecurity after March 2020. Our results of immigration insecurity are higher than current national estimates [69]. Six years of population-representative data from the Pew Hispanic Center’s National Survey of Latinos show that between 2007 and 2018, fear of deportation remained relatively stable, with 53.5% of Latinx individuals reporting deportation fears in 2007, 55.0% in 2018, and 51.8% across the total study period [69]. While the Pew survey asked “Regardless of your own immigration or citizenship status, how much, if at all, do you worry that you, a family member, or a close friend could be deported?” [69], our immigration insecurity question asked about other types of immigration enforcement (e.g., detention, family separation) and included other individuals potentially impacted by immigration insecurity (e.g., community members). Our results may also reflect differences in immigration insecurity specific to the COVID-19 pandemic, e.g., fear of seeking COVID-19 testing or treatment due to fear of being reported as undocumented or fear of exposing an undocumented family member to deportation through reception of care for COVID-19 [70].
There were a variety of sources of COVID-19-related information used by respondents to both surveys and interviews. One-third of survey participants noted community or religious groups as their primary source of COVID-19 information, while support from community agencies and churches was found to be a facilitators of treatment and care among those interviewed. These results imply that trusted community advocates and organizations have an important role to play in delivering high-quality information about COVID-19 to Latinx community members. A recent qualitative study of Black and Latinx populations demonstrates that trusted messengers, fact-based information and transparent, consistent, and continued messaging all help to increase trust in the COVID-19 vaccine [61]. Another recent study also demonstrates the importance of culturally relevant interventions for Latinx individuals [71]. Previous work has identified core cultural values (e.g., familismo or a fundamental sense of family respect and loyalty), emphasizing the importance of relationships in one’s family and community [72]. For example, frequent and close communication with families has helped to reduce disparities in living kidney donor transplantation [73]. Our findings suggest that tailoring public health interventions and messages for cultural norms delivered through trusted messengers may be a valuable strategy. Care must also be paid to the digital divide [13]. Consistent with these suggestions, since submission of this manuscript, we have applied study findings to the development of a community-engaged COVID-19 vaccine education program pilot that leverages the knowledge, expertise, and relationships of trusted community messengers to address COVID-19 vaccine myths and hesitations among Latinx adults in our community.
It is important to note that our quantitative surveys showed a larger proportion having accurate knowledge of COVID-19 symptoms among those seeking information from health professionals. This finding was expanded by interviews indicating that family and community advocates helped address barriers to healthcare access, e.g., not having a primary care physician. Still, distrust of healthcare providers expressed during interviews confirmed the low proportion of healthcare providers listed as a trusted source of information during surveys. This is in line with work (including local work by co-author FJ) suggesting that Latinx individuals may distrust medical and public health institutions out of concern for immigration status [68, 74, 75]. While distrust of healthcare professionals was noted in surveys, many interview participants expressed that they would seek medical care if they felt ill. Many also noted that receipt of correct health-related information about COVID-19 allayed fears. Healthcare professionals may also be able to ensure that knowledge sought from other sources (e.g., the internet, social media) is accurate. A previous study using nationally representative data demonstrated that language proficiency and literacy may function as independent contributors of Latinx use of the internet for health-related information [76]. Our findings, in the context of previous studies, suggest that equitable access to trusted, accurate sources for information is critical. This has been true across pandemic phases. Now, accurate knowledge (built atop trust) can be applied to improve vaccine uptake [77].
This study is not without limitations. Because data was collected during the early months of the pandemic (July 2020 to September 2020), it is possible that results may have changed during later pandemic phases. Reporting biases of surveys and interviews on the part of participants (e.g., self-report bias, social desirability bias) may lead to results indicating that participants are engaging in preventive behaviors (e.g., social distancing, wearing PPE) when they are really not or vice versa. Demographic variables in our quantitative survey were limited to age and gender. We limited the number of demographic variables obtained given the previous findings that Latinx adults in the USA have a disproportionately high survey refusal rate [78], possibly as a function of privacy concerns and/or fear of US immigration. We also felt that knowledge of more detailed demographic characteristics was not central to our study’s primary focus on better understanding barriers and facilitators to prevention and care of COVID-19 infection among those in the Cincinnati Latinx community. To account for variability in geography and country of origin, we used community-partnered data collection approaches that were similar to those taken during previous Latinx studies in our setting [16]. While surveys were available to all participants in both Spanish and English, we did not keep track of whether individuals completed the survey in Spanish or English,or whether it was completed in person, over the phone, or via paper. This raises the possibility that we may have missed potential differences across language and/or method of survey administration. Because a very small number of participants had no prevention behaviors or lack of COVID-19 knowledge, it was not feasible to do more complex statistical modeling of survey results. While coding, team memos were incorporated into our thematic analysis, but the bilingual CHW who conducted all interviews did not memo or take field notes during interviews, raising the possibility of bias [79]. While our convergent MM design helped us to improve academic and community understanding faster than sequential analysis (e.g., first qualitative interviews, then quantitative surveys), the concurrent and independent collection and analysis of quantitative and qualitative data in our study did not allow us to incorporate qualitative findings into the adaptation of our quantitative instrument [27] [28], leading our survey to lack potentially important variables, e.g., family challenges and specific barriers to care such as distrust of healthcare providers. Our MM integration was also limited by a lack of quantitative questions targeting themes that were frequently coded in our qualitative analysis, e.g., school, childcare, and marital stress. This gap suggests that family stressors may be under-represented in quantitative surveys of emergent disparities in this pandemic and in other crises.
Conclusions
Latinx adults in US public health crises may experience greater challenges related to social determinants of health. Barriers for our Latinx community during the COVID-19 pandemic included insecurities in food, jobs, housing, and immigration. Facilitators included trusted messengers. Our results suggest that public health interventions should be centered on community partnerships and the use of trusted messengers, that wraparound services (including resources for immigrants) are essential public health services, and that close partnership with employers is critical. While these results emerged from experiences during COVID-19, we suspect that our findings and insights will generalize to other, and future, public health crises in the USA.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- CCHMC
Cincinnati Children’s Hospital Medical Center
- CHW
Community health worker
- COVID-19
Coronavirus disease 2019
- CHES
COVID-19 Household Environment Scale
- LHC
Latino Health Collaborative
- MM
Mixed methods
- NIEHS
National Institute of Environmental Health Sciences
- NIMHD
National Institute on Minority Health and Health Disparities
- NIH
National Institutes of Health
- PSI
Pandemic Stress Index
- PPE
Personal protective equipment
- USA
United States
Author Contribution
Drs. Martin and Rule conceptualized and designed the study, completed the qualitative and integrative analyses, drafted the initial manuscript, and reviewed and revised the manuscript.
Ms. Castano completed the qualitative analysis, reviewed and assisted in interpreting the analysis, and critically reviewed the manuscript for important intellectual content.
Ms. Geraghty, Ms. Horner, and Dr. McCann contributed to data collection, contributed to the manuscript, and approved the final manuscript.
Dr. Beck conceptualized and designed the study, reviewed and assisted in interpreting the results, contributed to the manuscript, and approved the final manuscript.
Dr. Xu conceptualized and designed the quantitative analysis, carried out the statistical analysis, and reviewed and revised the manuscript.
Ms. Gomez reviewed and assisted in interpreting the analysis and critically reviewed the manuscript for important intellectual content.
Drs. O’Dea, Jacquez, and Plano Clark reviewed and assisted in interpreting the analysis and critically reviewed the manuscript for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This work was undertaken with support from the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number 2UL1TR001425-05A1. Dr. Martin’s position was supported by the T32 HP10027 Ruth L. Kirschstein National Research Service Award (NRSA) in Primary Care Research.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johns Hopkins Center for Systems Science and Engineering (CSSE). Coronavirus COVID-19 global cases dashboard. Available at: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Accessed 14 Jan 2022.
- 2.Romano SD, Blackstock AJ, Taylor EV, et al. Trends in racial and ethnic disparities in COVID-19 hospitalizations, by region - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70:560–565. doi: 10.15585/mmwr.mm7015e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopez L, III, Hart LH, III, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325:719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 4.Martinez DA, Hinson JS, Klein EY, et al. SARS-CoV-2 positivity rate for Latinos in the Baltimore-Washington. DC region Jama. 2020;324:392–395. doi: 10.1001/jama.2020.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubin-Miller L, Alban C, Sullivan S, et al. COVID-19 racial disparities in testing, infection, hospitalization, and death: analysis of Epic patient data. Available at: https://www.ehrn.org/articles/covid-19-racial-disparities-in-testing-infection-hospitalization-death Accessed 14 Jan 2022.
- 6.Strully K, Yang TC, Liu H. Regional variation in COVID-19 disparities: connections with immigrant and Latinx communities in U.S. counties. Ann Epidemiol. 2021;53:56–62.e52. [DOI] [PMC free article] [PubMed]
- 7.Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cincinnati Health Department. Cincinnati COVID-19 case tracker. Available at: https://www.cincinnati-oh.gov/health/covid-19/cincinnati-covid-19-case-tracker/ Accessed 14 Jan 2022.
- 9.Chowkwanyun M, Reed AL, Jr. Racial health disparities and COVID-19 - caution and context. N Engl J Med. 2020;383:201–203. https://www.nejm.org/doi/full/10.1056/NEJMp2012910 [DOI] [PubMed]
- 10.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cervantes L, Martin M, Frank MG, et al. Experiences of Latinx individuals hospitalized for COVID-19: a qualitative study. JAMA Netw Open. 2021;4:e210684. doi: 10.1001/jamanetworkopen.2021.0684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quandt SA, LaMonto NJ, Mora DC, et al. COVID-19 pandemic among Latinx farmworker and nonfarmworker families in North Carolina: knowledge, risk perceptions, and preventive behaviors. Int J Environ Res Public Health. 2020;17. [DOI] [PMC free article] [PubMed]
- 13.Alsan M, Stanford FC, Banerjee A, et al. Comparison of knowledge and information-seeking behavior after general COVID-19 public health messages and messages tailored for Black and Latinx communities: a randomized controlled trial. Ann Intern Med. 2021;174:484–492. doi: 10.7326/M20-6141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jimenez ME, Rivera-Núñez Z, Crabtree BF, et al. Black and Latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Netw Open. 2021;4:e2117074–e2117074. doi: 10.1001/jamanetworkopen.2021.17074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PEW Research Center. Hispanics have accounted for more than half of total U.S. population growth since 2010. Available at: https://www.pewresearch.org/fact-tank/2020/07/10/hispanics-have-accounted-for-more-than-half-of-total-u-s-population-growth-since-2010/ Accessed 14 Jan 2022.
- 16.Topmiller M, Zhen-Duan J, Jacquez FJ, et al. Place matters in non-traditional migration areas: exploring barriers to healthcare for Latino immigrants by region, neighborhood, and community health center. J Racial Ethn Health Disparities. 2017;4:1214–1223. doi: 10.1007/s40615-016-0329-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page KR, Flores-Miller A. Lessons we've learned - COVID-19 and the undocumented Latinx community. N Engl J Med. 2021;384:5–7. doi: 10.1056/NEJMp2024897. [DOI] [PubMed] [Google Scholar]
- 18.Apoyo Latino. Latinos in Greater Cincinnati. Available at: http://cincinnatilatino.org/latinos-in-greater-cincinnati/ Accessed 14 Jan 2022.
- 19.Cincinnati USA Hispanic Chamber. A closer look at Latinos vs. our 11 peer metro areas. Did You Know…Hispanic Facts, Data, and Trivia. Available at: http://www.cincinnaticompass.org/docs/librariesprovider3/default-document-library/datadocuments/2015_hccusa_fun_facts.pdf?sfvrsn=2631c2c0_2.
- 20.United Way of Greater Cincinnati. The state of the community: a report on the socio-economic health of the greater Cincinnati region. The state of the community report. Available at: https://www.uwgc.org/docs/default-source/financial-reports/report_statecommunity2017.pdf?sfvrsn=2.
- 21.National Institute on Minority Health and Health Disparities. NIMHD research framework. Available at: https://www.nimhd.nih.gov/about/overview/research-framework.html Accessed 14 Jan 2022.
- 22.The Health Collaborative. COVID-19 data and research projects. Situational dashboard. Available at: https://www.cctst.org/covid19 Accessed 14 Jan 2022.
- 23.CCHMC Perinatal Institute. Available at: https://www.cincinnatichildrens.org/service/p/perinatal Accessed 14 Jan 2022.
- 24.Apoyo Latino: the Greater Cincinnati Latino Coalition. Available at: https://cincinnatilatino.org/ Accessed 10 Feb 2022.
- 25.Murdock J, Vaughn L. Latino Health Collaborative of Greater Cincinnati: university-community partnerships for better health for the Latino community. 2008. Available at: https://www.researchgate.net/publication/266818940_Latino_Health_Collaborative_of_Greater_Cincinnati_University-Community_Partnerships_for_Better_Health_for_the_Latino_Community Accessed 8 March 2022.
- 26.Creswell JW, Klassen AC, Plano Clark VL, et al. Best practices for mixed methods research in the health sciences. Available at: https://obssr.od.nih.gov/sites/obssr/files/Best_Practices_for_Mixed_Methods_Research.pdf Accessed 14 Jan 2022.
- 27.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 3rd ed: Sage; 2018.
- 28.Aultman J, Baughman KR, Ludwick R. A broader understanding of care managers' attitudes of advance care planning: A concurrent nested design. J Clin Nurs. 2018;27:3572–3582. doi: 10.1111/jocn.14531. [DOI] [PubMed] [Google Scholar]
- 29.Collins KMT, Onwuegbuzie AJ, Jiao QG. A mixed methods investigation of mixed methods sampling designs in social and health science research. J Mixed Methods Res. 2007;1:267–294.https://journals.sagepub.com/doi/abs/10.1177/1558689807299526
- 30.Holthaus D. On the ground: Covington's growing Latino community. Available at: https://nkythrives.com/features/latino.aspx Accessed 8 March 2022.
- 31.United States Census Bureau. QuickFacts: Covington, Kentucky. Available at: https://www.census.gov/quickfacts/fact/table/covingtoncitykentucky/PST045218 Accessed 8 March 2022.
- 32.Behar-Zusman V, Chavez JV, Gattamorta K, (In Preparation). Developing a measure of the impact of COVID-19 social distancing on household conflict and cohesion. Available at: https://elcentro.sonhs.miami.edu/research/measures-library/ches/ches-eng/index.html Accessed 14 Jan 2022. [DOI] [PMC free article] [PubMed]
- 33.Harkness A. The pandemic stress index. University of Miami. Available at: https://elcentro.sonhs.miami.edu/research/measures-library/psi/psi-english/index.html Accessed 14 Jan 2022.
- 34.Harkness A, Behar-Zusman V, Safren SA. Understanding the impact of COVID-19 on Latino sexual minority men in a US HIV hot spot. AIDS Behav. 2020. p. 1–7. [DOI] [PMC free article] [PubMed]
- 35.Macnaghten P, Myers G. Focus groups: the moderator's view and the analyst's view In: Gobo G, Gubrium J, Seale, Silverman D. eds. Qual Res Pract. 2004.
- 36.Sagoe D. Precincts and prospects in the use of focus groups in social and behavioral science research. Qual Rep. 2012;17:1–16. [Google Scholar]
- 37.Yamane D. Narrative and religious experience. Sociol Relig. 2000;61:171–189. doi: 10.2307/3712284. [DOI] [Google Scholar]
- 38.Spradley JP. The ethnographic interview: Waveland Press; 2016.
- 39.Zayas LH, Gulbas LE. Processes of belonging for citizen-children of undocumented Mexican immigrants. J Child Fam Stud. 2017;26:2463–2474. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6141042/pdf/nihms-987348.pdf [DOI] [PMC free article] [PubMed]
- 40.Robledo C, Morrow J. COVID-19 impact on health and well-being survey. Available at: https://www.nlm.nih.gov/dr2/COVID_Impact_on_Health_Wellbeing_Eng.pdf Accessed 14 Jan 2022.
- 41.Mauthner M. Methodological aspects of collecting data from children: lessons from three research projects. Child Soc. 1997;11:16–28. doi: 10.1111/j.1099-0860.1997.tb00003.x. [DOI] [Google Scholar]
- 42.National Institutes of Health. COVID-19 research tools. Available at: https://www.nlm.nih.gov/dr2/COVID-19_BSSR_Research_Tools.pdf Accessed 14 Jan 2022.
- 43.National Institute of Environmental Health Sciences. COVID-19 impact on health and well-being survey. Available at: https://tools.niehs.nih.gov/dr2/index.cfm/resource/22126 Accessed 14 Jan 2022.
- 44.Ritchie J, Lewis J, Nicholls CM, et al. Qualitative research practice: a guide for social science students and researchers: sage; 2013.
- 45.White DR, McDermott J, Castelli M, et al. Better GP benchmarks: community survey results and proposals. Genet Program Evolvable Mach. 2013;14:3–29. doi: 10.1007/s10710-012-9177-2. [DOI] [Google Scholar]
- 46.Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1:185–216. doi: 10.1177/135910457000100301. [DOI] [Google Scholar]
- 47.Brelsford KM, Ruiz E, Beskow L. Developing informed consent materials for non-English-speaking participants: an analysis of four professional firm translations from English to Spanish. Clin trials (London, England) 2018;15:557–566. doi: 10.1177/1740774518801591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ: Br Med J. 2000;320:114. [DOI] [PMC free article] [PubMed]
- 49.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 50.Basu Roy U, Michel T, Carpenter A, et al. Community-led cancer action councils in Queens, New York: process evaluation of an innovative partnership with the Queens library system. Prev Chronic Dis. 2014;11:130176. [DOI] [PMC free article] [PubMed]
- 51.DeSantis L, Ugarriza DN. The concept of theme as used in qualitative nursing research. 2000;22:351–372. https://journals.sagepub.com/doi/abs/10.1177/019394590002200308 [DOI] [PubMed]
- 52.Hesse-Biber SN, Leavy P. The practice of qualitative research. 2. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 53.Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40:314–321. doi: 10.1111/j.1365-2929.2006.02418.x. [DOI] [PubMed] [Google Scholar]
- 54.Wade R, Jr, Shea JA, Rubin D, et al. Adverse childhood experiences of low-income urban youth. Pediatr. 2014;134:e13–20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- 55.Doyle S. Member checking with older women: a framework for negotiating meaning. Health Care Women Int. 2007;28:888–908. doi: 10.1080/07399330701615325. [DOI] [PubMed] [Google Scholar]
- 56.Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory into Practice. 2000;39:124–130. doi: 10.1207/s15430421tip3903_2. [DOI] [Google Scholar]
- 57.Carter N, Bryant-Lukosius D, DiCenso A, et al. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41:545–547. doi: 10.1188/14.ONF.545-547. [DOI] [PubMed] [Google Scholar]
- 58.Morse JM. Mixing qualitative methods. Los Angeles, CA: SAGE Publications Sage CA; 2009. [Google Scholar]
- 59.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs - principles and practices. Health Serv Res. 2013;48:2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moseholm E, Rydahl-Hansen S, Lindhardt B, et al. Health-related quality of life in patients with serious non-specific symptoms undergoing evaluation for possible cancer and their experience during the process: a mixed methods study. Qual Life Res. 2017;26:993–1006. doi: 10.1007/s11136-016-1423-2. [DOI] [PubMed] [Google Scholar]
- 61.Balasuriya L, Santilli A, Morone J, et al. COVID-19 vaccine acceptance and access among Black and Latinx communities. JAMA Netw Open. 2021;4:e2128575. [DOI] [PMC free article] [PubMed]
- 62.Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, et al. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;37:31. doi: 10.1186/s40985-016-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.U.S. Bureau of Labor Statistics. Labor force statistics from the current population survey. Available at: https://www.bls.gov/cps/tables.htm Accessed 14 Jan 2022.
- 64.Baquero B, Gonzalez C, Ramirez M, et al. Understanding and addressing Latinx COVID-19 disparities in Washington state. Health Educ Behav. 2020;47:845–849. doi: 10.1177/1090198120963099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Public Radio. What workers are saying at a meatpacking plant closed due to coronavirus outbreak. Available at: https://www.npr.org/2020/04/17/837511566/what-workers-are-saying-at-a-meatpacking-plant-closed-due-to-coronavirus-outbrea Accessed 6 March 2022.
- 66.Landale NS, Oropesa RS, Bradatan C. Hispanic families in the United States: family structure and process in an era of family change. Hispanics and the Future of America, 2006:138–178.
- 67.Hall M, Musick K, Yi Y. Living arrangements and household complexity among undocumented immigrants. Population and Development Review. 2019;45:81–101. https://onlinelibrary.wiley.com/doi/abs/10.1111/padr.12227
- 68.Jacquez F, Vaughn L, Zhen-Duan J, et al. Health care use and barriers to care among Latino immigrants in a new migration area. J Health Care Poor Underserved. 2016;27:1761–1778. doi: 10.1353/hpu.2016.0161. [DOI] [PubMed] [Google Scholar]
- 69.Asad AL. Latinos' deportation fears by citizenship and legal status, 2007 to 2018. Proc Natl Acad Sci U S A. 2020;117:8836–8844. doi: 10.1073/pnas.1915460117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kiester E, Vasquez-Merino J. A virus without papers: understanding COVID-19 and the impact on immigrant communities. J Migr Human Security. 2021;9:80–93. https://journals.sagepub.com/doi/abs/10.1177/23315024211019705
- 71.Ni L, De la Flor M, Wang Q, et al. Engagement in context: making meaning of the Latino community health engagement process. Publ Rela Rev. 2021;47:102036. https://www.sciencedirect.com/science/article/pii/S036381112100028X
- 72.Garza Y, Watts RE. Filial therapy and Hispanic values: common ground for culturally sensitive helping. J Couns Dev. 2010;88:108–113. doi: 10.1002/j.1556-6678.2010.tb00157.x. [DOI] [Google Scholar]
- 73.Gordon EJ, Lee J, Kang RH, et al. A complex culturally targeted intervention to reduce Hispanic disparities in living kidney donor transplantation: an effectiveness-implementation hybrid study protocol. BMC Health Serv Res. 2018;18:368. doi: 10.1186/s12913-018-3151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Macias Gil R, Marcelin JR, Zuniga-Blanco B, et al. COVID-19 pandemic: disparate health impact on the Hispanic/Latinx population in the United States. J Infect Dis. 2020;222:1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hill J, Rodriguez DX, McDaniel PN. Immigration status as a health care barrier in the USA during COVID-19. J Migr Health. 2021;4:100036. [DOI] [PMC free article] [PubMed]
- 76.Millar RJ, Sahoo S, Yamashita T, et al. Literacy skills, language use, and online health information seeking among Hispanic adults in the United States. Patient Educ Couns. 2020;103:1595–1600. doi: 10.1016/j.pec.2020.02.030. [DOI] [PubMed] [Google Scholar]
- 77.National Institutes of Health. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. Available at: https://obssr.od.nih.gov/wp-content/uploads/2020/12/COVIDReport_Final.pdf 14 Accessed Jan 2022.
- 78.Brown A. The unique challenges of surveying US Latinos. Available at: https://www.pewresearch.org/methods/2015/11/12/the-unique-challenges-of-surveying-u-s-latinos/ Accessed 6 March 2022.
- 79.Tufford L, Newman P. Bracketing in qualitative research. Qualitative Social Work. 2012;11:80–96.https://journals.sagepub.com/doi/abs/10.1177/1473325010368316
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.