Background:
The coronavirus-19 (COVID-19) pandemic has prompted a shift in health-care provision toward implementation of telemedicine. This study investigated demographic information on orthopaedic telemedicine utilization at a single academic orthopaedic institution in an effort to identify factors associated with telemedicine usage.
Methods:
Demographic and appointment data were collected from the electronic medical record during equivalent time periods prior to the onset of the COVID pandemic (pre-COVID) and during the COVID pandemic (peri-COVID). Multivariate analyses were performed to identify demographic and socioeconomic correlates of telemedicine utilization.
Results:
There was a significant increase in telemedicine visits between the eras of study, with significant differences in telemedicine usage in association with age, sex, marital status, English as the primary language, and insurance type (p < 0.001). Multivariate analyses found American Indian/Alaska Native (adjusted odds ratio [aOR] = 0.487, p = 0.004), Black/African American (aOR = 0.622, p < 0.001), Native Hawaiian/other Pacific Islander (aOR = 0.676, p = 0.003), and Asian (aOR = 0.731, p < 0.001) race to be significantly associated with decreased telemedicine usage. Additionally, male sex (aOR = 0.878, p < 0.001) and a non-commercial insurance plan (p < 0.001) were significantly associated with decreased telemedicine usage.
Conclusions:
Non-White race, non-commercial insurance plans, and male sex were associated with decreased telemedicine utilization. Further investigation is needed to characterize and better identify underlying factors contributing to disparities in telemedicine access and utilization.
Health-care disparities have been extensively identified in the United States, within both the general field of medicine and the specialty of orthopaedics1. Elderly patients (≥65 years) have been shown to be more likely to experience underdiagnosis and delayed diagnosis of multiple conditions such as cancer, infection, and metabolic disease when compared with younger patients2. Furthermore, multiple studies have found that racial/ethnic minorities undergo elective orthopaedic procedures as well as screening and treatment for osteoporosis at lower rates3,4. In addition, they experience longer wait times for radiographic imaging and have been shown to have higher morbidity and mortality rates following hip fracture3,4. An analysis of a nationwide database showed that insurance status and median ZIP-code income had a significant influence on the type of treatment patients received for calcaneal fractures5.
Telemedicine is a multidimensional, rapidly evolving modality that has been shown to be capable of improving access to quality cost-efficient health care for patients needing orthopaedic specialty services6. Multiple studies have found that telemedicine increases access to care for patients in remote locations7-12. By allowing orthopaedic providers to deliver care remotely, telemedicine has rapidly gained momentum as a potential solution to socioeconomic and geographical disparities in orthopaedic care13.
The coronavirus-19 (COVID-19) pandemic and the response that it has engendered have disrupted health-care systems around the world6. Initiatives such as telemedicine have been employed to limit this disruption and combat the spread of COVID-1914. The primary purpose of our study was to examine disparities in orthopaedic care during the COVID-19 pandemic. More specifically, our study was intended to provide demographic information on orthopaedic telemedicine utilization at a single academic orthopaedic institution and identify which characteristics are associated with telemedicine usage. Given telemedicine’s purported improvements in access to care for many populations, we hypothesized that significant disparities in telemedicine utilization would not be observed.
Materials and Methods
After obtaining approval from our institutional review board, we performed a retrospective review and extracted demographics and ambulatory care appointment data (dates, visit types, and insurance types) from electronic health records across our Department of Orthopedic Surgery. The demographic information consisted of age, race, ethnicity, primary language, marital status, and type of insurance. Queried ambulatory care appointments included new patient visits and follow-up visits.
Data were retrieved from comparable time periods designated as “pre-COVID” and “peri-COVID.” The “pre-COVID” period of study was defined as January 1, 2019, to December 23, 2019, while the “peri-COVID” period was defined as January 1, 2020, to December 23, 2020. Data were further stratified according to visit type (in-person office visit or telemedicine visit). All telemedicine visits were performed using an HIPAA (Health Insurance Portability and Accountability Act)-compliant video conferencing platform. For the purposes of the present study, we define telemedicine as communication with patients at a distance using audio and video content in real time to facilitate the provision of health care. Within the institution studied, all patients were at least offered a telemedicine visit across the period of study.
More than 10 different categorizations of patient race and ethnicity were self-reported in both databases. For standardization, races were further grouped based on National Institutes of Health (NIH) guidelines, which include a minimum of 5 categories for race: White, Black/African American, Asian, Native Hawaiian/other Pacific Islander, and American Indian/Alaska Native15. Patients who declined notation of their race on their chart (“unknown or not reported”) and patients who reported “more than one race” were excluded from analysis based on a priori assessment. Ethnicity was categorized by NIH standards (Hispanic or Latino; not Hispanic or Latino). A third ethnicity category was incorporated to account for patients who did not have ethnicity noted in their charts or declined to report it (“unknown or not reported”).
Insurance plans were categorized as commercial, managed care, Medicaid, Medicare, or self-pay (out of pocket for the entire billed appointment). Marital status included the following designations: married, single, divorced, widowed, and other. Appointment data from all divisions, providers, and locations within the department’s orthopaedic practices were considered in the analysis.
Statistical Analysis
Analyses were performed using Stata 16 (StataCorp). A Shapiro-Wilk test was utilized and identified a nonparametric distribution of the collected data. For descriptive statistics, means for nonparametric continuous variables were compared using Wilcoxon rank sum tests. Comparisons across categorical variables were performed using Pearson chi-square analyses. For multivariate analyses, demographic and socioeconomic factors were entered a priori into a multiple logistic regression model. Multiple regression modeling was performed for the total population of individual patient visits across the 2 eras of study. Significance was determined by p < 0.05. Individual effect sizes were accompanied by 95% confidence intervals (CIs) for all statistical comparisons within the regression model.
Source of Funding
The research was supported by the Columbia University “Addressing Racism” Seed Grant, Fall 2020. The funding source did not play a role in the investigation.
Results
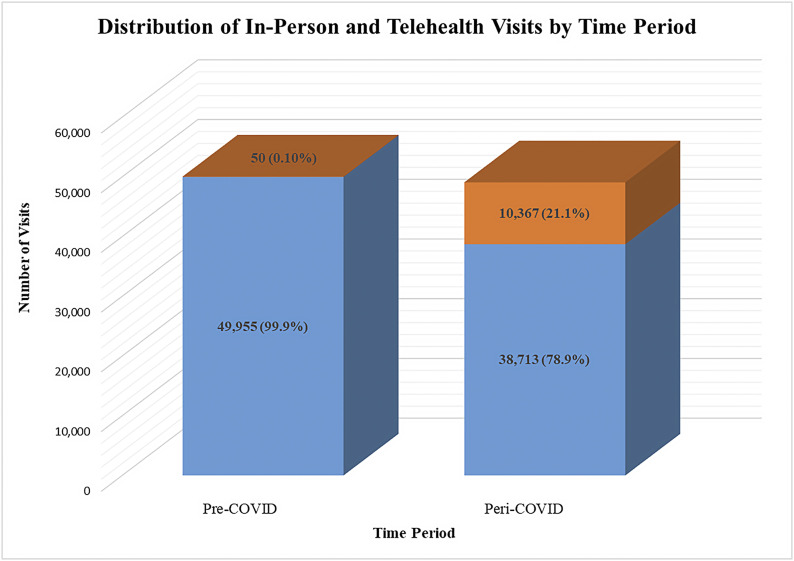
During the pre-COVID period (January 1, 2019, to December 23, 2019), there was a total of 50,005 orthopaedic ambulatory care episodes across 21,275 patients. Within the peri-COVID period (January 1, 2020, to December 23, 2020), there were 49,080 ambulatory care episodes across 19,447 patients. Comparisons of demographic data for unique patient visits between the pre-COVID and peri-COVID periods elicited significant differences in age (p = 0.0375), race (p < 0.001), ethnicity (p < 0.001), marital status (p < 0.001), primary language (p < 0.001), and type of insurance (p < 0.001) (Table I). During the pre-COVID period, 99.9% (n = 49,955) of the ambulatory care episodes were in-person office visits. This decreased to 78.9% during the peri-COVID period (Fig. 1). The pre- and peri-COVID eras of study differed significantly with respect to the proportion of in-person and telemedicine visits for new patient encounters as well as telemedicine visits for follow-up patient encounters (Table II).
Fig. 1.
Distribution of in-person (blue) and telemedicine (orange) visits by time period.
TABLE I.
Demographics of Individual Patient Visits by Era
| Characteristic | Pre-COVID Era (N= 21,275) | Peri-COVID Era (N = 19,447) | P Value |
|---|---|---|---|
| Mean age (SD*) (yr) | 47.96 (24.3) | 47.46 (24.5) | 0.0375 |
| Female (no. [%]) | 11,804 (55.48) | 10,878 (55.94) | 0.357 |
| Race (no. [%]) | <0.001 | ||
| White | 17,010 (79.95) | 15,494 (79.67) | |
| Black/African American | 2,471 (11.61) | 2,919 (15.01) | |
| Asian | 1,124 (5.28) | 773 (3.97) | |
| American Indian/Alaska Native | 51 (0.24) | 62 (0.32) | |
| Native Hawaiian/other Pacific Islander | 619 (2.91) | 199 (1.02) | |
| Ethnicity (no. [%]) | <0.001 | ||
| Hispanic or Latino | 3,001 (14.11) | 2,683 (13.80) | |
| Not Hispanic or Latino | 14,773 (69.44) | 14,040 (72.20) | |
| Unknown or not reported | 3,501 (16.46) | 2,724 (14.01) | |
| Primary language English (no. [%]) | 19,633 (92.28) | 12,878 (66.22) | <0.001 |
| Marital status (no. [%]) | <0.001 | ||
| Single | 10,184 (47.87) | 9,491 (48.80) | |
| Married | 8,456 (39.75) | 7,655 (39.36) | |
| Divorced | 730 (3.43) | 766 (3.94) | |
| Widowed | 901 (4.24) | 787 (4.05) | |
| Other | 1,004 (4.72) | 748 (3.85) | |
| Insurance (no. [%]) | <0.001 | ||
| Commercial | 2,429 (11.42) | 6,644 (34.16) | |
| Managed care | 14,215 (66.82) | 5,214 (26.81) | |
| Medicare | 2,299 (10.81) | 5,423 (27.89) | |
| Medicaid | 2,255 (10.60) | 2,116 (10.88) | |
| Self-pay | 77 (0.36) | 50 (0.26) |
SD = standard deviation.
TABLE II.
Distribution of All Patient Encounter Types by Era
| Visit Type | Pre-COVID Era (N = 50,005) | Peri-COVID Era (N = 49,080) | P Value |
|---|---|---|---|
| New patient encounters (no.) | 23,765 | 17,851 | 0.064 |
| In-person visit (no. [%]) | 23,763 (99.99) | 13,515 (75.71) | 0.042 |
| Telemedicine (no. [%]) | 2 (0.01) | 4,336 (24.29) | <0.001 |
| Follow-up patient encounters (no.) | 26,240 | 31,229 | 0.0982 |
| In-person visit (no. [%]) | 26,192 (99.82) | 25,198 (80.69) | 0.813 |
| Telemedicine (no. [%]) | 48 (0.18) | 6,031 (19.31) | <0.001 |
There were 50 orthopaedic telemedicine visits during the pre-COVID period compared with 10,367 during the peri-COVID period. Patients utilizing telemedicine during the pre-COVID period were, on average, younger than those using it in the peri-COVID period (mean and standard deviation, 22.1 ± 4.29 years versus 43.6 ± 22.6 years, p < 0.001). Additionally, there were significant differences in patient sex, primary language, marital status, and type of insurance (p < 0.001 for all) between pre- and peri-COVID telemedicine users (Table III).
TABLE III.
Demographics of All Telemedicine Visits by Era
| Characteristic | Pre-COVID Era (N = 50) | Peri-COVID Era (N = 10,367) | P Value |
|---|---|---|---|
| Mean age (SD*) (yr) | 22.12 (4.29) | 43.62 (22.55) | <0.001 |
| Female (no. [%]) | 46 (92.00) | 5,835 (56.28) | <0.001 |
| Race (no. [%]) | 0.210 | ||
| White | 49 (98.00) | 8,944 (86.27) | |
| Black/African American | 1 (2.00) | 1,014 (9.78) | |
| Asian | 0 (0) | 320 (3.09) | |
| American Indian/Alaska Native | 0 (0) | 18 (0.17) | |
| Native Hawaiian/other Pacific Islander | 0 (0) | 71 (0.68) | |
| Ethnicity | 0.210 | ||
| Hispanic or Latino | 5 (10.0) | 950 (9.16) | |
| Not Hispanic or Latino | 28 (56.0) | 7,923 (76.43) | |
| Unknown or not reported | 17 (34.0) | 1,494 (14.41) | |
| Primary language English (no. [%]) | 50 (100.0) | 6,971 (67.24) | <0.001 |
| Marital status (no. [%]) | <0.001 | ||
| Single | 50 (100.0) | 5,264 (50.78) | |
| Married | 0 (0) | 4,091 (39.46) | |
| Divorced | 0 (0) | 415 (4.00) | |
| Widowed | 0 (0) | 239 (2.31) | |
| Other | 0 (0) | 358 (3.45) | |
| Insurance (no. [%]) | <0.001 | ||
| Commercial | 0 | 4,292 (41.40) | |
| Managed care | 49 (98.00) | 3,248 (31.33) | |
| Medicare | 0 (0) | 2,158 (20.82) | |
| Medicaid | 1 (2.00) | 648 (6.25) | |
| Self-pay | 0 (0) | 21 (0.20) |
SD = standard deviation.
Factors Associated with Telemedicine Utilization
On univariable analysis, non-White race was significantly associated with decreased telemedicine usage (p < 0.001), with the largest effect size seen with patients identifying as American Indian/Alaska Native (odds ratio [OR] = 0.317 [95% CI = 0.250 to 0.403], p < 0.001). Asian (OR = 0.661 [95% CI = 0.589 to 0.743], p < 0.001). Native Hawaiian/other Pacific Islander (OR = 0.543 [95% CI = 0.337 to 0.877], p = 0.012) and Black/African American (OR = 0.708 [95% CI = 0.662 to 0.759], p < 0.001) race were also associated with decreased telemedicine utilization but with comparatively lower effect sizes. Increasing age was negatively associated with telemedicine usage but with a relatively small effect size overall (OR = 0.992 [95% CI = 0.991 to 0.993] per year, p < 0.001). Additional significant negative correlates of telemedicine usage included male sex (OR = 0.911 [95% CI = 0.875 to 0.950], p < 0.001) and non-commercial insurance plans (p < 0.001). A managed care insurance plan was associated with the least telemedicine usage and had the highest effect size of all insurance types analyzed (OR = 0.321 [95% CI = 0.306 to 0.337], p < 0.001), followed by Medicaid (OR = 0.346 [95% CI = 0.317 to 0.377], p < 0.001), Medicare (OR = 0.635 [95% CI = 0.600 to 0.671], p < 0.001), and self-pay (0.407 [95% CI = 0.260 to 0.637], p < 0.001).
A multivariate regression analysis revealed non-White race to be significantly associated with decreased telemedicine usage (Table IV). Compared with White patients, the largest effect size was seen for American Indian/Alaska Native patients (adjusted odds ratio [aOR] = 0.487 [95% CI = 0.297 to 0.799, p = 0.004) and Black/African American patients (aOR = 0.622 [95% CI = 0.579 to 0.668], p < 0.001). Medicaid (aOR = 0.510 [95% CI = 0.465 to 0.559], p < 0.001) and Medicare (aOR = 0.812 [95% CI = 0.756 to 0.872], p < 0.001) were also associated with decreased telemedicine utilization, with the largest effect sizes of all insurance plans analyzed. Lastly, increasing age (aOR = 0.992 [95% CI = 0.991 to 0.994] per year, p < 0.001) and male sex (aOR = 0.878 [95% CI = 0.840 to 0.917], p < 0.001) were significantly associated with decreased telemedicine utilization as well (Table IV).
TABLE IV.
Demographic and Socioeconomic Factors Associated with Likelihood of Telemedicine Usage
| Variable | Adjusted Odds Ratio (95% CI) | P Value |
|---|---|---|
| Age, per yr | 0.992 (0.991-0.994) | <0.001 |
| Sex | ||
| Female | 1 | Reference |
| Male | 0.878 (0.840-0.917) | <0.001 |
| Visit year | ||
| 2019 | 1 | Reference |
| 2020 | 216.2 (197.6-345.3) | <0.001 |
| Race | ||
| White | 1 | Reference |
| Black/African American | 0.622 (0.579-0.668) | <0.001 |
| Asian | 0.731 (0.646-0.828) | <0.001 |
| American Indian/Alaska Native | 0.487 (0.297-0.799) | 0.004 |
| Native Hawaiian/other Pacific Islander | 0.676 (0.523-0.873) | 0.003 |
| Insurance | ||
| Commercial | 1 | Reference |
| Managed care | 0.867 (0.823-0.913) | <0.001 |
| Medicare | 0.812 (0.756-0.872) | <0.001 |
| Medicaid | 0.510 (0.465-0.559) | <0.001 |
| Self-pay | 0.791 (0.487-1.29) | 0.344 |
Discussion
In this single-institution analysis of telemedicine utilization, our practice experienced a rapid increase in telemedicine usage, from <1% to >20% of all orthopaedic visits. This phenomenon was a likely consequence of the COVID-19 pandemic and restrictions requiring physical distancing. Further investigation of demographic factors associated with telemedicine utilization demonstrated non-White race, non-commercial insurance plans, and male sex to be significant negative correlates of telemedicine utilization. Although our analysis found increasing age be significantly associated with decreased telemedicine utilization, this finding may not have clinical relevance in our model given that the adjusted odds ratio for age was 0.992 per year. Nevertheless, our hypothesis that significant disparities in telemedicine utilization would not be observed was refuted.
The reasons for these disparities have been previously described as complex and multifactorial16. Whether measured by income, educational achievement, or occupation, differences in socioeconomic status are associated with large disparities in health status17. Although these disparities are largest for those living in poverty, gradients of disparity are seen across the socioeconomic spectrum18. Low socioeconomic status is an important determinant of access to health care19. Individuals with low incomes are more likely to be Medicaid recipients or uninsured, have poor-quality health care, and seek health care less often20-24. As it pertains to telemedicine, the “digital divide” in device ownership and broadband utilization between individuals with different financial statuses is a major barrier to the adoption of virtual care25. Video-conferencing abilities often require high-speed broadband connectivity, in contrast to the free simple wireless networking technology that has been made publicly available in many metropolitan areas26. While the present study did not independently evaluate the effect of socioeconomic status on telemedicine utilization, several prior studies have used insurance status as a surrogate for socioeconomic status27,28. Therefore, it is likely that socioeconomic status and telemedicine utilization are also similarly correlated.
Race continues to be a challenging factor to analyze when exploring health-care disparities as it is often subject to confounders such as access-related and socioeconomic factors26. Despite these confounding challenges noted in prior literature, our investigation identified non-White race as an independent negative predictor of telemedicine utilization. Within the orthopaedic literature, the relationship between race and health utilization has been studied by multiple authors. Nayar et al. found increased time to surgery and perioperative complications across non-White patients when adjusted for comorbidities, age, sex, and type of surgery29. In their study of shoulder arthroplasty, Best et al. found lower rates of anatomic and reverse total shoulder arthroplasty in Black patients compared with White patients independent of insurance status30. Zhang et al. used a national administrative database of total knee arthroplasties performed at high-volume hospitals and found that racial minorities not only had lower rates of total knee arthroplasty but also higher rates of adverse health outcomes associated with the procedure31. Provider referral patterns were suggested as one explanation for the disparities observed in the study, and it was suggested that patient education could help minimize the propagation of further disparities31.
Multiple studies have discussed a host of behavioral and social factors, such as patient preferences and expectations, that may play a role in influencing a patient’s decision to seek medical care as well as their overall health perception24,32,33. For example, compared with Whites, African Americans have been shown to be more likely to rely on self-care measures such as prayer and are less likely to consider interventions in analyses accounting for disease severity24,32,33. This explanation could also provide some rationale for the results observed in the present study if non-White minorities opted to forego telemedicine in favor of self-care measures or believed the severity of their disease or condition did not meet a threshold that would support the pursuit of telemedicine.
Another factor that has been reported to lead to lower utilization of orthopaedic care among African American patients is lower trust1. One study demonstrated lower trust in the health-care system among African Americans compared with Whites34. Among African Americans, trust was lower in the subgroup of patients who did not have a primary care physician in comparison with those who had an established relationship with a primary care provider34. For immigrant populations, concerns around confidentiality, privacy, and data security could also contribute to a hesitancy to use telemedicine in the setting of more recent governmental policies related to U.S. Immigration and Customs Enforcement (ICE)26. George et al. investigated perceptions of telemedicine in minority populations and noted that the physical absence of a physician or a specialist during their evaluation was a limiting factor in their trust in an examiner’s diagnosis35. Distrust in telemedicine among African Americans and immigrant populations could explain why we found non-White race to be a negative predictor of telemedicine utilization. With the rise of telemedicine implementation on the horizon for many large, urban medical centers, more patient-perception studies are needed to elucidate this possible confounder.
Despite the purported benefits of telemedicine in terms of providing care to a wider patient demographic, a more robust geographic catchment area of patients, and greater patient satisfaction when telemedicine is provided as an option, our investigation identified several disparities that merit further investigation to improve access to this evolving mode of health care in the face of the COVID-19 pandemic. There are a number of important ways that the present study expands on prior analyses previously published in the literature16,36,37. Not only did it identify disparities in orthopaedic care, it highlighted disparities in telemedicine use during a time period when telemedicine use increased significantly. In addition, it provides specific demographics associated with telemedicine use, which deserve further study.
There are several limitations of the present study. For example, the categories of “unknown or not reported” or “more than one race” were not included in the analysis of the demographic data, which may have skewed the relative weighting of variables within our multivariate analyses. Although insurance type was viewed as a surrogate for socioeconomic status, no socioeconomic data were collected. Therefore, conclusions pertaining to socioeconomic status and insurance type are inferred; no direct link was established. Also, the study is from a single, large, urban academic tertiary orthopaedic center. Thus, our findings may not be generalizable to other parts of the United States with dissimilar demographics, practice models (i.e., private practice, or rural or community practices), and medical specialties. Furthermore, there was a large difference in telemedicine usage from the pre-COVID era to the peri-COVID era that limits the ability to make statistical comparisons that are not potentially subject to type-1 error. Additionally, although telemedicine visits were widely offered to all patients during the pandemic, as hospital and regional policies on access to in-person services fluctuated and became less restrictive over time it remained up to the patients to decide whether they wanted an in-person or telemedicine visit. The significant differences observed in the distribution of telemedicine and in-person visits as a function of new and follow-up patient encounters must be viewed within the context of uniquely fluid and ever-changing restrictions during the pandemic. However, these differences are not the primary finding of the study; the results of the regression model to identify predictors of telemedicine usage were the main focus. Lastly, our investigation does not present or differentiate visits based on the severity of the chief complaints that traditionally prompt an orthopaedic visit. For more emergency issues (e.g., infection, fracture, or trauma) or problems predicated on detailed physical examination, an in-person office visit may offer the highest yield of information, allowing for coordination of subsequent surgical care; thus, these situations may not be appropriate for an evaluation with telemedicine.
In conclusion, significant disparities in orthopaedic care were observed despite an increase in telemedicine utilization during the COVID-19 pandemic. Non-White race, non-commercial insurance plans, and male sex were significantly associated with decreased telemedicine utilization. These disparities warrant further investigation to characterize and better identify underlying factors that contribute to telemedicine access and utilization in orthopaedic practices.
Footnotes
Investigation performed at the Department of Orthopedic Surgery, Columbia University Irving Medical Center, New York, NY
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A373).
Contributor Information
Richard A. Ruberto, Email: rar2210@cumc.columbia.edu.
Eric A. Schweppe, Email: easchweppe@gmail.com.
Rifat Ahmed, Email: ra2998@cumc.columbia.edu.
Hasani W. Swindell, Email: hwillswindell23@gmail.com.
Christopher A. Cordero, Email: cc4258@cumc.columbia.edu.
Nathan S. Lanham, Email: nathanscottlanham@gmail.com.
References
- 1.Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(Suppl 1):S13-7. [DOI] [PubMed] [Google Scholar]
- 2.Rothschild JM, Bates DW, Leape LL. Preventable medical injuries in older patients. Arch Intern Med. 2000. Oct 9;160(18):2717-28. [DOI] [PubMed] [Google Scholar]
- 3.Adelani MA, O’Connor MI. Perspectives of Orthopedic Surgeons on Racial/Ethnic Disparities in Care. J Racial Ethn Health Disparities. 2017. Aug;4(4):758-62. [DOI] [PubMed] [Google Scholar]
- 4.Ali I, Vattigunta S, Jang JM, Hannan CV, Ahmed MS, Linton B, Kantsiper ME, Bansal A, Srikumaran U. Racial Disparities are Present in the Timing of Radiographic Assessment and Surgical Treatment of Hip Fractures. Clin Orthop Relat Res. 2020. Mar;478(3):455-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zelle BA, Morton-Gonzaba NA, Adcock CF, Lacci JV, Dang KH, Seifi A. Healthcare disparities among orthopedic trauma patients in the USA: socio-demographic factors influence the management of calcaneus fractures. J Orthop Surg Res. 2019. Nov 12;14(1):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lanham NS, Bockelman KJ, McCriskin BJ. Telemedicine and orthopaedic surgery: The Covid-19 pandemic and our new normal. JBJS Rev. 2020. Jul;8(7):e2000083. [DOI] [PubMed] [Google Scholar]
- 7.Aarnio P, Lamminen H, Lepistö J, Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5(1):62-6. [DOI] [PubMed] [Google Scholar]
- 8.Wallace P, Haines A, Harrison R, Barber J, Thompson S, Jacklin P, Roberts J, Lewis L, Wainwright P; Virtual Outreach Project Group. Joint teleconsultations (virtual outreach) versus standard outpatient appointments for patients referred by their general practitioner for a specialist opinion: a randomised trial. Lancet. 2002. Jun 8;359(9322):1961-8. [DOI] [PubMed] [Google Scholar]
- 9.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016. Sep 8;16(1):483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blank E, Lappan C, Belmont PJ, Jr, Machen MS, Ficke J, Pope R, Owens BD. Early analysis of the United States Army’s telemedicine orthopaedic consultation program. J Surg Orthop Adv. 2011. Spring;20(1):50-5, https://pubmed.ncbi.nlm.nih.gov/21477534/. Accessed 2020 Dec 27. [PubMed] [Google Scholar]
- 11.Rogers FB, Ricci M, Caputo M, Shackford S, Sartorelli K, Callas P, Dewell J, Daye S. The use of telemedicine for real-time video consultation between trauma center and community hospital in a rural setting improves early trauma care: preliminary results. J Trauma. 2001. Dec;51(6):1037-41. [DOI] [PubMed] [Google Scholar]
- 12.Clegg A, Brown T, Engels D, Griffin P, Simonds D. Telemedicine in a rural community hospital for remote wound care consultations. J Wound Ostomy Continence Nurs. 2011. May-Jun;38(3):301-4. [DOI] [PubMed] [Google Scholar]
- 13.Abbott DE, Voils CL, Fisher DA, Greenberg CC, Safdar N. Socioeconomic disparities, financial toxicity, and opportunities for enhanced system efficiencies for patients with cancer. J Surg Oncol. 2017. Mar;115(3):250-6. [DOI] [PubMed] [Google Scholar]
- 14.Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020. Apr 2;6(2):e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NOT-OD-15-089: Racial and Ethnic Categories and Definitions for NIH Diversity Programs and for Other Reporting Purposes. Accessed 2020. Dec 28. https://grants.nih.gov/grants/guide/notice-files/not-od-15-089.html [Google Scholar]
- 16.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020. Oct 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socioeconomic status. Epidemiology. 1997. Jan;8(1):42-7. [DOI] [PubMed] [Google Scholar]
- 18.Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991. Jun 8;337(8754):1387-93. [DOI] [PubMed] [Google Scholar]
- 19.Becker G, Newsom E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health. 2003. May;93(5):742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franks P, Clancy CM, Gold MR. Health insurance and mortality. Evidence from a national cohort. JAMA. 1993. Aug 11;270(6):737-41. [PubMed] [Google Scholar]
- 21.Becker G. Effects of being uninsured on ethnic minorities’ management of chronic illness. West J Med. 2001. Jul;175(1):19-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadley J, Steinberg EP, Feder J. Comparison of uninsured and privately insured hospital patients. Condition on admission, resource use, and outcome. JAMA. 1991. Jan 16;265(3):374-9. [PubMed] [Google Scholar]
- 23.Burstin HR, Lipsitz SR, Brennan TA. Socioeconomic status and risk for substandard medical care. JAMA. 1992. Nov 4;268(17):2383-7. [PubMed] [Google Scholar]
- 24.Swartz K. Dynamics of people without health insurance. Don’t let the numbers fool you. JAMA. 1994. Jan 5;271(1):64-6. [PubMed] [Google Scholar]
- 25.Vogels EA. Digital divide persists even as Americans with lower incomes make gains in tech adoption. Pew Research Center. Accessed 2020 Dec 27. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/ [Google Scholar]
- 26.Das LT, Gonzalez CJ. Preparing Telemedicine for the Frontlines of Healthcare Equity. J Gen Intern Med. 2020. Aug;35(8):2443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020. Jun 18;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swift E. Institute of Medicine (US) Committee on Guidance for Designing a National Healthcare Disparities, editor. Measuring the Effects of Socioeconomic Status on Health Care. Washington (DC): National Academies Press (US); 2002. [Google Scholar]
- 29.Nayar SK, Marrache M, Ali I, Bressner J, Raad M, Shafiq B, Srikumaran U. Racial Disparity in Time to Surgery and Complications for Hip Fracture Patients. Clin Orthop Surg. 2020. Dec;12(4):430-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Best MJ, Aziz KT, McFarland EG, Martin SD, Rue JPH, Srikumaran U. Worsening Racial Disparities in Patients Undergoing Anatomic and Reverse Total Shoulder Arthroplasty in the United States. J Shoulder Elbow Surg. 2021. Aug;30(8):1844-50. [DOI] [PubMed] [Google Scholar]
- 31.Zhang W, Lyman S, Boutin-Foster C, Parks ML, Pan TJ, Lan A, Ma Y. Racial and ethnic disparities in utilization rate, hospital volume, and perioperative outcomes after total knee arthroplasty. J Bone Joint Surg Am. 2016. Aug 3;98(15):1243-52. [DOI] [PubMed] [Google Scholar]
- 32.Ibrahim SA. Racial variations in the utilization of knee and hip joint replacement: an introduction and review of the most recent literature. Curr Orthop Pract. 2010. Mar;21(2):126-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.SooHoo NF. Zingmond DS Ko CY. Disparities in the utilization of high-volume hospitals for total knee replacement. J Natl Med Assoc. 2008. May;100(5):559-64. [DOI] [PubMed] [Google Scholar]
- 34.Halbert CH, Armstrong K, Gandy OH, Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006. Apr 24;166(8):896-901. [DOI] [PubMed] [Google Scholar]
- 35.George SM, Hamilton A, Baker R. Pre-experience perceptions about telemedicine among African Americans and Latinos in South Central Los Angeles. Telemed J E Health. 2009. Jul-Aug;15(6):525-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Talbot JA, Burgess AR, Thayer D, Parenteau L, Paluso N, Coburn AF. Patterns of telehealth use among rural Medicaid beneficiaries. J Rural Health. 2019. Jun;35(3):298-307. [DOI] [PubMed] [Google Scholar]
- 37.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018. Nov 27;320(20):2147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]