Abstract
Chrozophora tinctoria (Euphorbiaceae) has been used as an emetic, anthelminthic, and cathartic agent in traditional medicine. We used gas chromatography-mass spectrometry (GC-MS) to characterize the composition of ethyl acetate (EAC) and dichloromethane (DCMC) fractions from the whole Chrozophora tinctoria plant. EAC and DCMC fractions were evaluated for acetylcholinesterase (AChE) inhibitory activity and acute toxicity. Their effects on intestinal propulsive movement and spasmogenic activity of the gastrointestinal tract (GIT) muscle were also assessed. The compounds detected in both fractions were mostly fatty acids, with about seven compounds in EAC and 10 in DCMC. These included pharmacologically active compounds such as imipramine, used to treat depression, or hexadecanoic acid methyl ester, an antioxidant. Both EAC and DCMC fractions inhibited acetylcholinesterase (AChE) activity with IC50 values of 10 µg and 130 µg, respectively. Both the fractions were found to be toxic in a dose-dependent manner, inducing emesis at 0.5 g or higher and lethargy and mortality from 3–5 g upwards. Similarly, both of the fractions showed laxative activity in metronidazole- and loperamide-induced constipation models. EAC relaxed the intestinal muscle at a lower dose (1 mg/mL) than DCMC. Similarly, the EAC extract showed a significant relaxation effect (EC50 = 0.67 ± 0.15 mg/mL) on KCL-induced contraction in rabbit jejunum as compared to DCMC (EC50 = 5.04 ± 0.05 mg/kg). The present study strongly supports the folklore that this valuable plant is a cathartic agent. Further work is required to isolate and validate the bioactive compounds that act as diarrheal agents in Chrozophora tinctoria.
Keywords: Chrozophora tinctoria, acetylcholinesterase inhibitor, laxative, acute toxicity, spasmogenic
1. Introduction
Constipation is a chronic disorder of the gastrointestinal tract (GIT) and is defined as bowel movements of fewer than three times per week. Clinically, constipation manifests with heterogeneous symptoms including difficulty in defecation, infrequent bowel movements, hard bowel, and the feeling of incomplete defecation [1]. Constipation is equally prevalent across the globe and affects all age groups almost equally. According to one estimate, constipation is reported in 2.5–39.6% of the world’s adult population [2], while in infants to adolescents, the prevalence is in the range of 0.5–26.9% [3]. Common contributing factors to constipation include insufficient dietary fiber and fluid intake, adverse effects of medications, decreased physical activity, hypothyroidism, and colorectal cancer-induced obstruction, which can be broadly attributed to either genetic predisposition or the socioeconomic status of the patients [4]. Different drugs are applied to improve complications of constipation, including Correctol, Senna, Exlax, and Gaviscon, but with limited benefits due to the associated adverse effects and treatment costs [5,6]. The primary approach to treat constipation involves regulation of GIT motility, for which several drugs have been introduced. For instance, cisapride was among the first developed prokinetic agents but was withdrawn later due it to its effect on increasing cardiac arrhythmias [7]. Another noteworthy example is a selective 5-hydroxytrptamine-4 (5-HT4) receptor antagonist, tegaserod, that is currently in practice to diminish constipation despite its role in causing coronary artery diseases and myocardial infarction [8,9].
The plant kingdom has served as a remarkable resource for extracts exhibiting prokinetic activity that diminish characteristics of constipation by improving intestinal motility, defecation frequency, and stool weight. Leaf extract from the perineal plant Ecklonia cava showed a prominent laxative effect on the loperamide-induced constipation model in SD rates in terms of stool recovery and GIT motility. This study confirmed that the underlying principle involved facilitation of GIT hormone secretion and augmenting the downstream signaling pathway of local muscarinic acetylcholine receptors (mAChRs) [10]. Leaf extract of Malva sylvestris has been shown to attenuate constipation induced in male Wistar rats by increasing gastric emptying and decreasing intestinal transit time via its stimulatory effect on mAChRs [11]. In addition to intestinal transit length, a significant increase in stool frequency, weight, and water content was also observed as a result of Ficus carica treatment [12]. Reports such as these have encouraged many researchers to investigate medicinal plants to look for therapeutic alternatives that offer no or fewer adverse effects compared to currently available drugs.
Chrozophora tinctoria, commonly known as ‘dyer’s croton’ or ‘turnsole’, belongs to the family Euphorbiaceae. It is an annual plant found in Africa, Europe, and Asia. In Pakistan, it is found in tropical and temperate regions [13]. Chrozophora species are traditionally used to cure mouth ulcers, skin disorders such as skin burns, fever, abdominal and joint pain, jaundice, menstrual problems, wounds, GIT worms, and migraine. Moreover, Chrozophora tinctoria is used as an emetic and cathartic and to treat warts [14]. In Ethiopia and Senegal, the seeds and leaves of the Chrozophora species are used as a laxative. In Nepal, the juice obtained from its fruit is used as a remedy for cough and cold [15]. The antibacterial activity of Chrozophora tinctoria leaves and stem was established by earlier workers [16]. In addition, Chrozophora tinctoria is used for producing natural dye [17].
The presence of arabinose, fructose, glucose, raffinose, sucrose, and ribose in Chrozophora tinctoria has been confirmed by HPLC [18]. It has been reported that flavonoids are abundantly prevalent in almost all species of the genus Chrozophora [19,20,21]. HPLC analysis of the methanolic extract of the aerial parts of Chrozophora tinctoria reported five flavonoid glycosides. These five flavonoid glycosides are apigenin 7-O-b-d-glucopyranoside, apigenin 7-O-b-d-[(6-pcoumaroyl)]-glucopyranoside, acacetin 7-O-rutinoside, quercetin 3-O-rutinoside, and apigenin 7-O-b-d-[6-(3,4dihydroxybenzoyl)]-glucopyranoside (Chrozophorine) [13]. Most of these flavonoids have therapeutic properties and especially antiviral activity [22,23]. Other compounds extracted from the ethanolic extract of Chrozophora tinctoria are kaempferol, kaempferol 3-O-(600-a-rhamnopyranosyl)-b-glucopyranoside, kaempferol 3-O-b-glucopyranoside, two phenolics, namely, methyl gallate and gallic acid, and one steroid, namely, b-sitosterol-3-O-b-glucopyranoside. There are 35 different flavonoids found in various species of the genus Chrozophora, which have anti-proliferative, antioxidant, antimicrobial, antipyretic, and anti-nociceptive properties [24]. The leaves of C. tinctoria possess antidiabetic and hepatoprotective properties [25]. Rutin present in Chrozophora has the ability to promote bone cell growth [26]. Here, we used gas chromatography-mass spectrometry to investigate the phytochemical profile of fractions taken from Chrozophora tinctoria and evaluate their laxative activity as novel treatment options for constipation.
2. Results
2.1. GC-MS
2.1.1. Composition of EAC
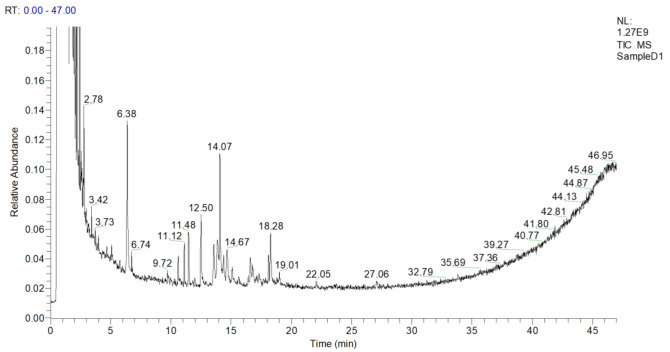
About seven compounds were tentatively identified through GC-MS. The GC-MS chromatogram demonstrated seven phytochemical constituents, as presented in Figure 1, Table 1 and Supplementary Table S1. These peaks were matched with the database of known components present in the GC-MS library. Compounds having a similarity index of more than 600 were recorded. GC-MS analysis of EAC showed the presence of many bioactive compounds at different retention times (min).
Figure 1.
GC-MS chromatogram of the ethylacetate fraction of Chrozophora tinctoria. The numbers show the retention times of various compounds.
Table 1.
Bioactive compounds identified in the ethylacetate fraction (EAC) through GC-MS.
| Peak No. | Retention Time (min) | SI | RSI | Area % | Probability | Compound Name | Formula | Molecular Weight | Library |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.78 | 783 | 980 | 0.01 | 93.57 | Imipramine | C19H24N2 | 280 | nist_msms |
| 2 | 6.38 | 905 | 914 | 0.06 | 76.55 | Hexadecanoic acid, methyl ester | C17H34O2 | 270 | replib |
| 3 | 11.12 | 684 | 870 | 0.01 | 22.81 | 3,7,11,15-Tetramethyl-2-hexadecen-1-ol | C20H40O | 296 | MAINLIB |
| 4 | 12.50 | 865 | 889 | 0.02 | 48.69 | Pentadecanoic acid, 14-methyl-, methyl ester | C17H34O2 | 270 | MAINLIB |
| 5 | 14.07 | 846 | 866 | 0.07 | 80.32 | Hexadecanoic acid, ethyl ester | C18H36O2 | 284 | MAINLIB |
| 6 | 14.67 | 612 | 652 | 0.01 | 45.49 | Nonanoic acid, 9-(0-propylphenyl)- methyl ester | C19H30O2 | 290 | MAINLIB |
| 7 | 18.28 | 728 | 749 | 0.03 | 12.14 | 9,12,15-Octadecatrienoic acid, ethyl ester, (Z,Z,Z)- | C20H34O2 | 306 | replib |
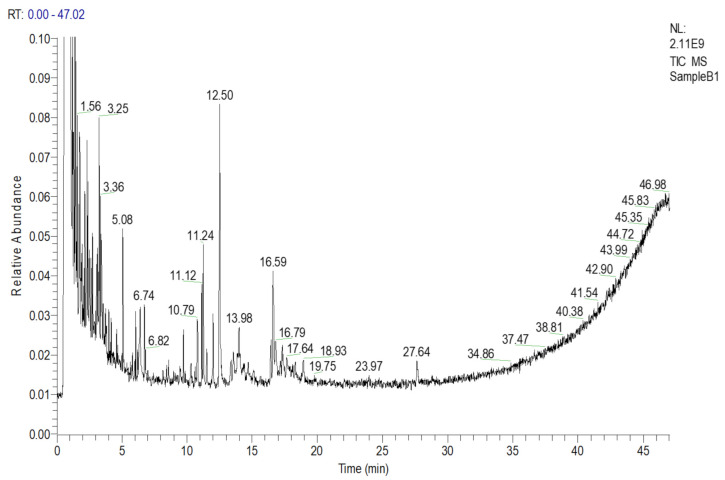
2.1.2. Composition of DCMC
Similarly, a total of 10 chemical compounds from the DCMC fraction were tentatively identified with a similarity index of more than 600, after matching the different retention times with the library, as shown in Figure 2 and Table 2.
Figure 2.
GC-MS chromatogram of the dichloromethane fraction (DCMC) of Chrozophora tinctoria. The numbers inside the chromatogram are the retention times of the compounds.
Table 2.
Bioactive compounds identified in DCMC through GC-MS.
| Peak No. | Retention Time (min) | SI | RSI | Area % | Probability | Compound Name | Formula | Molecular Weight | Library |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1.56 | 742 | 812 | 0.06 | 51.92 | Hydroperoxide, 1-ethyl butyl | C6H14O2 | 118 | MAINLIB |
| 2 | 3.25 | 657 | 722 | 0.04 | 40.54 | Silane, chlorodiisopropylmethyl- | C7H17ClSi | 164 | MAINLIB |
| 3 | 5.08 | 712 | 891 | 0.01 | 4.42 | 1-Hexadecene | C16H32 | 224 | MAINLIB |
| 4 | 10.79 | 686 | 757 | 0.01 | 26.35 | 3,7,11,15-Tetramethyl-2-hexadecen-1-ol | C20H40O | 296 | MAINLIB |
| 5 | 12.50 | 912 | 919 | 0.06 | 72.93 | Hexadecanoic acid, methyl ester | C17H3402 | 270 | MAINLIB |
| 6 | 13.98 | 728 | 893 | 0.03 | 6.03 | 1-Eicosanol | C20H42O | 298 | replib |
| 7 | 16.59 | 775 | 791 | 0.05 | 8.39 | 10-Octadecanoic acid, methyl ester | C19H36O2 | 296 | MAINLIB |
| 8 | 17.64 | 674 | 714 | 0.01 | 25.03 | 9,12,15-Octadecatrienoic acid, 2,3-bis[(trimethylsilyl)oxy]propyl ester, (Z,Z,Z)- | C27H52O4Si2 | 496 | replib |
| 9 | 18.93 | 651 | 675 | 0.01 | 6.21 | 17-Pentatriacontene | C35H70 | 490 | MAINLIB |
| 10 | 27.64 | 727 | 899 | 0.01 | 41.12 | 1,2-Benzenedicarboxylic acid, diisooctyl ester | C24H38O4 | 390 | replib |
2.2. Acetylcholinesterase Inhibitory Activity
Effect of EAC and DCMC
The EAC and DCMC fractions demonstrated AChE inhibition at various concentrations, as presented in Table 3. The percent inhibition of 1000 µg/mL EAC was 93.33 ± 1.53. The inhibitory concentration (IC50) of the EAC fraction was 10 µg/mL, showing good AChE inhibitory potential as compared to galantamine (IC50 = 5 µg/mL). Similarly, 1000 µg/mL of DCMC showed good enzyme inhibitory activity, with AChE inhibition of 68.33%.
Table 3.
Percent inhibition of acetylcholinesterase by EAC.
| Compound Name/Plant Name | Fraction | Concentration (µg/mL) | % AChE Inhibition | IC50 |
|---|---|---|---|---|
| Galantamine | Standard | 1000 | 95.67 ± 2.52 | 5.0 |
| 500 | 87.33 ± 2.52 | |||
| 250 | 82.67 ± 3.06 | |||
| 125 | 77.00 ± 3.00 | |||
| Chrozophora tinctoria | EAC | 1000 | 93.33 ± 1.53 | 10 |
| 500 | 87.33 ± 3.06 | |||
| 250 | 80.67 ± 2.08 | |||
| 125 | 73.00 ± 4.58 | |||
|
Chrozophora
tinctoria |
DCMC | 1000 | 68.33 ± 2.52 | 130 |
| 500 | 63.00 ± 3.61 | |||
| 250 | 57.67 ± 2.31 | |||
| 125 | 48.67 ± 2.08 |
Values are expressed as mean ± SEM. Statistical significance was determined using IC50 values through Biostata software.
2.3. Acute Toxicity
2.3.1. Acute Toxicity of EAC and DCMC
The acute toxicity parameters of EAC and DCMC are shown in Table 4. Doses up to 0.3 g/kg were safe and without any toxic symptoms; however, at a concentration of 0.5 g/kg and upward, emesis and diarrhea were noticed. Concentrations of 4 and 5 g/kg were found to be emetic and diarrheal with 25.0% mortality.
Table 4.
Acute toxicity of the ethyl acetate and dichloromethane fractions of Chrozophora tinctoria in pigeons.
| Sample | Dose (g).(mL)/kg | Emesis | Diarrhea | Lethargy | Mortality (%) |
|---|---|---|---|---|---|
| Total Number of Vomits | Total Number of Wet Stools | ||||
| Distilled water | 6 | 0.00 ± 0.00 | 0.00 ± 0.00 | - | 0.00 ± 0.00 |
| EAC | 0.3 | 0.00 ± 0.00 | 0.00 ± 0.00 | - | 0.00 ± 0.00 |
| 0.5 | 2.00 ± 0.82 | 0.00 ± 0.00 | - | 0.00 ± 0.00 | |
| 1 | 6.00 ± 2.65 * | 8.33 ± 4.51 | - | 0.00 ± 0.00 | |
| 2 | 6.67 ± 2.52 * | 10.00 ± 3.00 * | - | 0.00 ± 0.00 | |
| 3 | 8.00 ± 2.00 *** | 10.67 ± 3.06 ** | Less | 0.00 ± 0.00 | |
| 4 | 9.33 ± 1.53 *** | 12.33 ± 2.52 *** | More | 25.00 | |
| 5 | 11.00 ± 3.00 *** | 14.00 ± 4.00 *** | More | 25.00 | |
| DCMC | 0.3 | 0.00 ± 0.00 | 0.00 ± 0.00 | - | 0.00 ± 0.00 |
| 0.5 | 2.33 ± 0.58 | 0.00 ± 0.00 | - | 0.00 ± 0.00 | |
| 1 | 6.33 ± 1.53 * | 6.00 ± 3.00 | - | 0.00 ± 0.00 | |
| 2 | 7.00 ± 1.73 ** | 8.67 ± 2.08 | - | 0.00 ± 0.00 | |
| 3 | 9.67 ± 2.08 *** | 9.33 ± 2.52 * | Less | 0.00 ± 0.00 | |
| 4 | 10.00 ± 2.65 *** | 9.67 ± 4.04 * | More | 25.00 | |
| 5 | 11.33 ± 2.31 *** | 11.00 ± 1.00 ** | Most | 25.00 |
Values are expressed as mean ± SEM. Statistical significance was determined with one-way ANOVA followed by Tukey’s multiple comparison test (using Graph Pad Prism 6.01 software); * p ≤ 0.05 was considered statistically significant (** p ≤ 0.01, *** p ≤ 0.001).
2.3.2. Effect on Metronidazole-Induced Constipation
EAC and DCMC were both prokinetic against metronidazole-induced constipation, as presented in Table 5 and Table 6, respectively. The tested groups treated with EAC and metronidazole (Metro) demonstrated that the prokinetic effects of EAC were significantly (p < 0.001) inhibited, as shown in Table 6. The total number of stools, number of wet stools, and percent of wet stool were significantly (p < 0.001) diminished by metronidazole-treated groups as compared to EAC- and DW-tested groups.
Table 5.
Diarrheal/laxative activity of EAC.
| Samples | Dose g/kg mL/kg (PO) | First Stool/Latency Time (Minutes) | Total Number of Stools | Number of Wet Stools | Weight of Stool (Grams) | Percent Wet Stool (%) |
|---|---|---|---|---|---|---|
| EAC + DW | 1 | 28.00 ± 4.32 | 17.25 ± 3.30 | 8.75 ± 2.50 | 8.25 ± 1.71 | 50.41 ± 8.33 |
| 2 | 25.00± 1.83 | 19.00 ± 2.94 | 10.25 ± 1.71 | 10.50 ± 2.65 | 53.98 ± 4.89 | |
| 3 | 22.00 ± 1.83 | 21.00 ± 2.16 | 15.75 ± 1.89 | 12.25 ± 2.75 | 72.65 ± 6.64 | |
| Metronidazole (7 mg/kg) was administered (PO) 30 min before fraction/distilled water/castor oil | ||||||
| Distilled water (-ve control) | 6 | 73.33 ± 2.52 | 9.33 ± 2.52 | 0.00 ± 0.00 | 8.27 ± 1.96 | 0.00 ± 0.0 |
| Castor oil (+ve control) | 6 | 20.33 ± 2.52 *** | 22.00 ± 2.00 *** | 18.33 ± 1.53 *** | 18.67 ± 2.36 *** | 83.43 ± 2.23 *** |
| EAC + Metro | 1 | 35.33 ± 3.06 *** | 13.00 ± 3.00 | 5.00 ± 1.00 ** | 8.37 ± 1.03 | 38.65 ± 1.26 *** |
| 2 | 35.00 ± 2.00 *** | 16.67 ± 1.15 *** | 6.00 ± 2.00 *** | 10.17 ± 1.96 | 35.65 ± 9.85 *** | |
| 3 | 31.00 ± 1.73 *** | 18.00 ± 1.00 | 6.00 ± 2.00 *** | 10.90 ± 1.80 | 63.43 ± 3.33 *** | |
Data are presented as the mean ± SEM; one-way ANOVA followed by Dunnett’s test was applied to determine significance; p ≤ 0.05 was considered as significant (** p ≤ 0.01; *** p ≤ 0.001). EAC, ethyl acetate fraction of Chrozophora tinctoria; Metro, metronidazole; DW, distilled water; PO, per orally.
Table 6.
Diarrheal/laxative activity of DCMC.
| Samples | Dose g/kg mL/kg (PO) | First Stool/Latency Time (Minutes) | Total Number of Stools | Number of Wet Stools | Weight of Stool (Grams) | Percent Wet Stool (%) |
|---|---|---|---|---|---|---|
| DCMC + DW | 1 | 30.00 ± 2.94 | 16.25 ± 1.71 | 5.25 ± 1.71 | 10.10 ± 1.34 | 31.79 ± 8.13 |
| 2 | 28.75 ± 4.27 | 18.25 ± 2.06 | 7.00 ± 1.63 | 13.00 ± 2.16 | 38.31 ± 7.34 | |
| 3 | 27.50 ± 3.42 | 19.75 ± 2.99 | 9.00 ± 2.16 | 14.78 ± 3.03 | 45.18 ± 6.29 | |
| Metronidazole (7 mg/kg) was administered (PO) 30 min before fraction/distlled water/castor oil | ||||||
| Distilled water (-ve control) | 6 | 73.33 ± 2.52 | 9.33 ± 2.52 | 0.00 ± 0.00 | 8.27 ± 1.96 | 0.00 ± 0.00 |
| Castor oil (+ ve control) | 6 | 20.33 ± 2.52 *** | 22.00 ± 2.00 *** | 18.33 ± 1.53 *** | 18.67 ± 2.36 *** | 83.43 ± 2.23 *** |
| DCMC + Metro | 1 | 38.00 ± 3.00 *** | 12.00 ± 2.65 | 3.00 ± 1.00 | 7.30 ± 1.21 | 24.64 ± 4.03 *** |
| 2 | 39.67 ± 3.06 *** | 15.33 ± 1.53 ** | 5.33 ± 2.52 ** | 9.73 ± 1.42 | 33.93 ± 12.83 *** | |
| 3 | 39.33 ± 1.53 *** | 15.00 ± 1.73 | 5.00 ± 1.00 ** | 9.07 ± 1.17 | 33.33 ± 5.56 *** | |
Data are presented as mean ± SEM; one-way ANOVA followed by Dunnett’s test was done to determine statistical significance where p ≤ 0.05 was considered as statistically significant (** p ≤ 0.01; *** p ≤ 0.001). DCMC, dichloromethane fraction of Chrozophora tinctoria; Metro, metronidazole; DW, distilled water; PO, per orally/by orally.
2.3.3. Effect of Loperamide-Induced Constipation
The prokinetic activity of EAC and DCMC was significantly attenuated by loperamide (4 mg/kg), as presented in Table 7 and Table 8, respectively. Thus, the percent of wet stool with EAC doses of 1, 2, and 3 g/kg was significantly (p < 0.001) reduced from 63.03, 77.64, and 80.55% to 20.16, 43.30, and 62.02%, respectively. The latency time was also significantly (p < 0.001) delayed by the loperamide. A similar attenuation in the prokinetic effect of DCMC was observed against loperamide-induced constipation.
Table 7.
Diarrheal/laxative activity of EAC.
| Samples | Dose g/kg mL/kg (PO) | First Stool/Latency Time (Minutes) | Total Number of Stools | Number of Wet Stools | Weight of Stool (Grams) | Percent Wet Stool (%) |
|---|---|---|---|---|---|---|
| EAC + DW | 1 | 23.25 ± 2.50 | 14.75 ± 3.59 | 09 ± 2.16 | 10.05 ± 2.87 | 63.03 ± 13.97 |
| 2 | 21.5 ± 1.73 | 15.75 ± 1.71 | 12 ± 1.63 | 11.33 ± 3.21 | 77.64 ± 18.26 | |
| 3 | 19.75 ± 2.22 | 16 ± 2.45 | 13 ± 2.94 | 13 ± 2.45 | 80.55 ± 7.97 | |
| Loperamide hydrochloride (4 mg/kg) was administered (PO) 30 min before fractions/distilled water/castor oil. | ||||||
| Distilled water (-ve control) | 6 | 70.33 ± 2.52 | 8.33 ± 2.52 | 0.00 ± 0.00 | 7.50 ± 2.29 | 0.00 ± 0.00 |
| Castor oil (+ ve control) | 6 | 17.33 ± 2.52 *** | 16.67 ± 2.08 ** | 14.33 ± 1.53 *** | 15.07 ± 1.27 *** | 89.74 ± 2.78 *** |
| EAC + Lopr | 1 | 41.33 ± 3.21 *** | 11.00 ± 2.65 | 2.00 ± 1.00 | 8.43 ± 1.81 | 20.16 ± 13.10 *** |
| 2 | 40.33 ± 1.53 *** | 11.67 ± 3.06 | 5.00 ± 1.00 * | 9.23 ± 1.00 | 43.30 ± 2.90 *** | |
| 3 | 30.33 ± 1.53 *** | 9.67 ± 1.53 | 6.00 ± 1.00 ** | 9.20 ± 1.05 | 62.04 ± 1.86 *** | |
Data are represented as mean ± SEM. The data were analyzed by one-way ANOVA followed by Dunnett’s test using GraphPad prism version 6.01; p ≤ 0.05 was considered as significant (* p ≤ 0.05; ** p ≤ 0.01; *** p ≤ 0.001). EAC, ethyl acetate fraction of Chrozophora tinctoria; Lopr, loperamide hydrochloride; DW, distilled water, PO, per orally/by orally.
Table 8.
Diarrheal/laxative activity of DCMC.
| Samples | Dose g/kg mL/kg (PO) |
First Stool/Latency Time (Minutes) | Total Number of Stools | Number of Wet Stools | Weight of Stool (Grams) |
Percent Wet Stool (%) |
|---|---|---|---|---|---|---|
| DCMC + DW | 1 | 33.25 ± 3.50 | 15.00 ± 3.56 | 5.00 ± 2.83 | 8.62 ± 2.44 | 32.68 ± 12.27 |
| 2 | 30.25 ± 3.30 | 16.75 ± 2.22 | 7.25 ± 2.50 | 10.25 ± 2.55 | 42.16 ± 10.00 | |
| 3 | 28.25 ± 2.06 | 19.5 ± 2.52 | 9.25 ± 2.63 | 10.33 ± 1.79 | 46.79 ± 7.03 | |
| Loperamide hydrochloride (4 mg) was administered (PO) 30 min before of fractions/distilled water/castor oil. | ||||||
| Distilled Water (-ve control) | 6 | 70.33 ± 2.52 | 8.33 ± 2.52 | 0.00 ± 00 | 7.50 ± 2.29 | 0.00 ± 00 |
| Castor oil (+ ve control) | 6 | 17.33 ± 2.52 *** | 16.00 ± 2.00 ** | 14.33 ± 1.53 *** | 15.07 ± 1.27 *** | 89.74 ± 2.78 *** |
| DCMC + Lopr | 1 | 40.00 ± 2.65 *** | 10.33 ± 2.08 | 1.67 ± 0.58 | 8.20 ± 1.30 | 16.92 ± 7.95 ** |
| 2 | 37.00 ± 2.00 *** | 11.67 ± 1.53 | 3.67 ± 0.58 | 8.50 ± 0.62 | 30.00 ± 3.34 *** | |
| 3 | 33.67 ± 3.06 *** | 10.00 ± 1.00 | 6.00 ± 1.00 ** | 8.30 ± 0.79 | 35.45 ± 5.06 *** | |
Data are represented as mean ± SEM. The data were analyzed by one-way ANOVA followed by Dunnett’s test using GraphPad prism 6.01 version; p ≤ 0.05 was considered as significant (** p ≤ 0.01; *** p ≤ 0.001). DCMC, dichloromethane fraction of Chrozophora tinctoria; Lopr, loperamide hydrochloride; DW, distilled water; PO, per orally/by orally.
2.4. Gastrointestinal Motility (Charcoal Meal Method)
The charcoal meal transit of EAC and DCMC is presented in Table 9. The charcoal movement of EAC at 25, 50. and 100 mg/kg was 33.41, 53.97, and 75.20%, respectively. The effect of DCMC at the same doses was 31.50, 41.20, and 51.84%, respectively.
Table 9.
Percent intestinal transit of EAC and DCMC in the pigeons.
| Treatment | Dose mg/Kg (PO) | Total Length of Intestine (cm) | Total Distance Travelled by Charcoal Meal (cm) | % of Intestinal Transit |
|---|---|---|---|---|
| Castor oil | 4 mL | 88.9 ± 5.1 | 77.7 ± 5.1 | 87.60 ± 5.8 |
| Immodium | 6 | 92.3 ± 3.9 | 30.3 ± 6.8 | 32.7 ± 6.7 |
| DW | 4 mL | 90.9 ± 2.7 | 37.3 ± 2.8 | 41.15 ± 4.3 |
| EAC | 25 | 91.4 ± 2.3 | 30.5 ± 1.9 | 33.41 ± 2.5 |
| 50 | 71.9 ± 1.6 | 38.7 ± 1.3 | 53.97 ± 2.7 | |
| 100 | 73.7 ± 3.1 | 55.3 ± 1.9 | 75.2 ± 4.9 | |
| DCMC | 25 | 66.0 ± 2.0 | 20.8 ± 1.9 | 31.5 ± 3.7 |
| 50 | 85.4 ± 1.3 | 35.2 ± 2.1 | 41.2 ± 1.9 | |
| 100 | 76.4 ± 1.7 | 39.6 ± 1.3 | 51.84 ± 2.7 |
Data are represented as mean ± SEM. EAC, ethyl acetate fraction of Chrozophora tinctoria; DCMC, dichloromethane fraction of Chrozophora tinctoria; DW, distilled water; PO, per orally/by orally; %, percentage.
2.5. Spasmolytic Activity
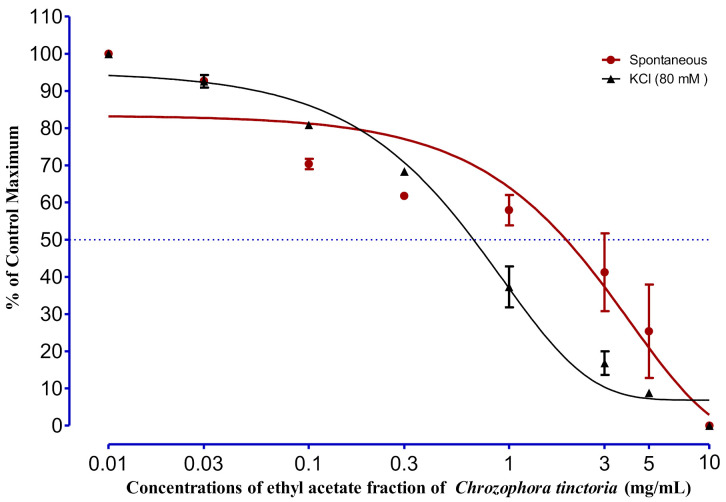
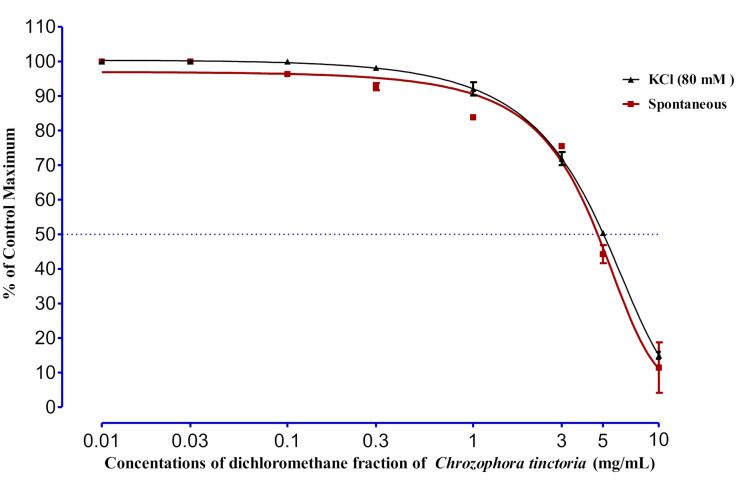
Significant relaxations in the spontaneous responses were noted at a concentration of 1 mg/mL; however, complete relaxation in spontaneous responses was detected at a concentration of 10 mg/mL with EC50 of 2.11 ± 1.20 mg/mL. In the case of KCL-induced (80 mM) contraction, the relaxing effect of EAC started gradually from 0.1 and 0.3 mg and showed a complete relaxing effect at 10 mg/mL, with an EC50 value of 0.67 ± 0.15 mg/mL (Figure 3). The effect of DCMC on spontaneous rabbit jejunal preparation is described in Figure 4. Different concentrations were tested, as shown in the figure; significant results were shown by 3, 5, and 10 mg/kg, with EC50 equal to 4.71 ± 0.26 mg/kg. In the same way, the 3-, 5-, and 10-mg/kg concentrations of DCMC had a relaxing effect on KCL-induced (80 mM) contraction in rabbit’s jejunum, with an EC50 value of 5.04 ± 0.05 mg/kg.
Figure 3.
The effect of EAC on spontaneous and KCL-induced (80 mM) contraction of rabbit jejunum. Rabbit jejunum muscle was relaxed in a dose-dependent manner. EC50 values were calculated from curve fitting in GraphPad prism 6.01. Each point represents the mean ± SEM of grouped data.
Figure 4.
The effect of DCMC on spontaneous and KCL-induced (80 mM) contraction of rabbit jejunum. Rabbit jejunum muscle was relaxed in a dose-dependent manner. EC50 values were calculated from curve fitting in GraphPad prism 6.01. Each point represents the mean ± SEM of grouped data.
3. Discussion
Constipation is a worldwide problem that is equally prevalent in all age groups. Different pharmacological and non-pharmacological paradigms are available for relieving the symptoms of constipation. Among the pharmacological approaches, various allopathic and herbal-based therapeutic options are practiced. Even though the allopathic system offers various synthetic and semisynthetic molecules for the treatment of constipation, numerous side effects are attributed to those approaches. Therefore, the search for a safe, effective, and affordable therapeutic agent for constipation is a challenge to current medical science. In this study, the prokinetic effect of Chrozophora tinctoria fractions was investigated to establish pharmacological grounds for the potential use of these fractions in constipation therapy.
AChE is a key enzyme found in the blood and nervous system, mediating various important physiological functions. The principal role of this enzyme is the cessation of nerve impulses at cholinergic synapses by breaking down the neurotransmitter acetylcholine into choline and acetic acid. The inhibition of acetylcholinesterase is a promising strategy against Parkinson disease, myasthenia gravis, ataxia, senile dementia, and Alzheimer disease [27]. Phytochemicals derived from other plants have shown inhibitory action against acetylcholinesterase [28]. The EAC fraction of Chrozophora tinctoria significantly inhibited AchE, with an IC50 of 10 µg/mL. AChE inhibition implies blockade of ACh degradation, resulting in a higher concentration of ACh. This availability of ACh will result in a prolonged interaction with the muscarinic and nicotinic receptors, maintaining the impulse. Ach is bioavailable in various conformational isomers (gauche and anti-gauche forms), which is the reason behind its interaction with both cholinergic receptors. The cholinergic response will promote diarrhea through its intracellular signaling pathways. The laxative effect of Chrozophora tinctoria might be related to the cholinergic action of the tested fractions. The laxative activity of both fractions was studied in metronidazole- (7 mg/kg) and loperamide hydrochloride- (4 mg/kg) induced constipated pigeons. The prokinetic potential of the tested fractions was attenuated by loperamide more significantly than metronidazole. The prokinetic effect of the Chrozophora tinctoria fractions was further confirmed by the charcoal meal propulsion in the intestine of pigeons. Both of the fractions demonstrated significant (p ≤ 0.05) propulsion of charcoal in the animal intestine.
Contraction of intestinal smooth muscle results from periodic depolarization. Thus, depolarization in intestinal smooth muscle is usually attributed to the release of calcium ions, either from intracellular stores or through the influx of calcium to the inside of the tissue through voltage-gated calcium channels. KCL in high doses is considered a depolarizer, which may trigger cellular calcium influx. Therefore, a relaxing effect in KCL-induced contraction usually indicates that the test substance induces calcium channel blockade [29]. This experiment was conducted to investigate the direct effects of EAC and DCMC on rabbit jejunum. The antispasmodic effect of EAC on the smooth muscles of the jejunum was detected at a concentration of 1 mg/mL. Similarly, the spasm induced in rabbit’s jejunum by KCL (80 mM) was relaxed by EAC completely at 10 mg/mL. Similarly, at a concentration of 3 mg/kg the DCMC exhibited a relaxing effect on KCL-induced (80 mM) contraction in rabbit’s jejunum with an EC50 value of 5.04 ± 0.05 mg/kg. It was deduced that the relaxing effect with EC50 2.11 ± 1.20 mg/mL of EAC and an EC50 value of 5.04 ± 0.05 mg/kg of DCMC may have been due to the inhibition of voltage-gated calcium channels. Furthermore, it also implies that EAC was more potent than DCMC. The tested fractions were also investigated for acute toxicity on pigeons. The animal model used in this study is considered a paradigm for the induction of emesis [30], as compared to other emesis models, such as mice and rats, which are usually not as responsive. The acute toxicity study confirmed that the plant fractions used in this study induce emesis, a potential side effect of EAC and DCMC. Strikingly, the tested plant fractions are also anthelmintic as dead worms were observed in the stool passed by animals used in this study. The spasmolytic effect can be a contributing factor to the anthelmintic action of Chrozophora tinctoria. A further molecular-level study is needed to elaborate on the underlying mechanisms of the EAC and DCMC fractions.
4. Materials and Methods
4.1. Chemicals and Solvents
The chemicals/drugs used in the present study were Maxolon® (Valeant Pharmaceutical International, Inc., Karachi, Pakistan), Gravinate® (The Searle company (PVT) LTD, Karachi, Pakistan), Imodium® (ASPIN Pharma PVT. LTD, Karachi, Pakistan), Flagyl® (Sanofi Aventis (PVT) LTD, Pakistan), Copper Sulphate (Nenza pharmaceuticals (PVT) LTD, Peshawar, KPK, Pakistan), Cisplatin (Pfizer Laboratories LTD, Karachi, Pakistan), Magnesium Sulphate (Nenza Pharmaceuticals (PVT) LTD, Pakistan), castor oil (Karachi Pharmaceuticals Laboratory, Karachi, Pakistan), gum acacia (Shreeji Pharma International), normal saline (Shahzeb Pharmaceutical, Haripur, KPK, Pakistan), methanol (Master Chemical Supplier, Karachi, Pakistan), and ethyl acetate (Master Chemical Supplier, Karachi, Pakistan).
4.2. Instruments
A rotary evaporator (Model RE-111, Bochi, Switzerland), 5-cc, 3-cc, and 1-cc syringes (Shifa disposable syringe), a drip set (Shifa drip set, Pakistan), water bath (Thermostatic controlled-STD/GMP), magnetic stirrer (H3760-S Digital magnetic stirrer), and analytical balance (Shimadzo analytical balance) were used.
4.3. Plant Collection and Identification
Mature Chrozophora tinctoria was collected from the Mohmand Agency, Khyber Pakhtunkhwa, Pakistan, and was authenticated by Dr. Sher Wali, Assistant Professor, Department of Botany, Islamia College Peshawar. The identified plant specimen was given a voucher number (CT-Bot-11082017) and deposited in the Herbarium, Department of Botany, Islamia College Peshawar. The collected plant was washed with clean water to remove dirt, and was dried at room temperature by spreading it in a single layer on blotting paper. After drying, the plant was cut into fine pieces and was powdered using an electric grinder.
4.4. Extraction and Fractionation
Extraction and fractionation of the desired fractions were performed according to the literature with some modifications [31,32]. Maceration in methanol was carried out for a total of 10 kg of powdered plant with random shaking for several days followed by filtration through Whatmann filter paper No 1. The filtrate was concentrated by a rotary evaporator to obtain a crude methanolic extract. The dried crude methanolic extract was dissolved in distilled water and then n-hexane was added. After shaking in a separating funnel, the n-hexane fraction was obtained and concentrated by a rotary evaporator. Similarly, dichloromethane, ethyl acetate, and n-butanol fractions were obtained. This method is called solvent–solvent fractionation. Their order of fractionation was from n-hexane then dichloromethane, ethyl acetate, and n-butanol, respectively. DCMC and EAC fractions were used for further activities [31,32].
4.5. Gas Chromatography-Mass Spectrometry (GC-MS)
To identify different phytochemicals present in EAC and DCMC fractions, the samples were subjected to GC-MS. The samples were checked using a Thermo Scientific (DSQ-II) GC. The GC device was furnished with a 30-m-long TR-5MS capillary column and a 0.25-µm-thick film and had 0.25 mm of internal diameter. Helium was used as a carrier gas with a flow rate of 1 mL/min. The injection device was run in a split mode at 250 °C. The sample was injected, 1 µL at a time, with an initial oven temperature of 50 °C that was maintained for 2 min followed by gradually elevating the temperature to 150 °C at a rate of 8 °C/min. Finally, the temperature was raised to 300 °C at a rate of 15 °C/min and maintained for 5 min [33,34].
4.6. Pharmacological Activities
4.6.1. Animals
Pigeons
Healthy pigeons were defined as those with normal stools (non-diarrheal and non-emetic), that were non-lethargic, and had no weight loss, no nasal dropping, no shedding or feather ruffling, and usual flying movement with regular feeding. Mature pigeons of both sexes were selected with weights in the range of 240–380 g. Animals were provided with standard food (locally available food; millet + wheat grains), fresh water, and a light/dark cycle for 12/12 h for 5–7 days. On the day of the experiment, the pigeons were weighed and health was assessed. Pigeons observed as unhealthy were removed from the experiment. After selection, animals were placed in separate cages to get individual data of each group [35]. Pigeons were held gently, and fractions were given orally by a feeding tube with the help of an assistant.
Rabbits
Healthy rabbits were defined as being active and alert with no wet nose, runny eyes, scabby ears, or sore spots on their feet, with normal feeding and feces. Mature male rabbits weighing 1.5–3 kg were selected for the experiment. Rabbits were served with standard food and fresh water for several days. On the day of the experiment, the rabbits were examined again and the healthy ones were subjected to cervical dislocation [36]. The abdomen of the animal was opened after cervical dislocation and about 1.5–2.5-cm slices of jejunum were detached and placed in Tyrode solution in Petri dishes with a continuous supply of carbogen gas (95% O2 and 5% CO2). The jejunum was then used for further experiments.
4.6.2. In Vitro Experiments
Acetylcholinesterase Assay
Increasing concentrations of EAC (125, 250, 500, 1000 µg/mL) and DCMC fractions were tested for AChE using a spectrophotometer according to the method of Ellman [37]. This method for assaying thiols is based on the principle that acetylthiocholine iodide is hydrolyzed by the respective enzyme-producing thiocholine, which reacts with 5,5′-dithiobis-2-nitrobenzoic acid (DTNB) (Ellman’s reagent). The final products of the second reaction are 5-thio-2 nitrobenzoate and 2-nitrobenzoate-5-mercaptothiocholine. The absorption of the former product is measured by a spectrophotometer (412 nm). The positive control, galantamine, was prepared in the same concentrations as EAC. The test and control solutions were incubated at 37 °C for 20 min. The enzyme inhibition was calculated from the absorption rate with a change in time [37,38].
The percent inhibition was calculated as
| Enzyme inhibition (%) = 100 − percent enzyme activity |
| Percent enzyme activity (%) = 100 × V/Vmax |
where (Vmax) is an enzyme activity in the absence of an inhibitor.
4.6.3. In Vivo Experiments
Acute Toxicity
Acute toxicity of EAC and DCMC was established according to an available protocol with slight modifications [39]. The pigeons were divided into two groups (n = 8). One group received a fraction while the negative control group received distilled water only (6 mL/kg, PO). Each fraction was administered orally with 0.3, 0.5, 1, 2, 3, 4, and 5 g/kg as a single dose using a feeding tube to different groups. All the animals were observed for toxic symptoms, i.e., diarrhea, emesis, lethargy, and motility, for about 72 h [39].
Laxative Activity
Pigeons were divided into eight groups (n = 8). A white, plastic base was provided in the cages for stool collection and examination. Groups 1, 2, and 3 were administered distilled water and 1-g, 2-g, and 3-g doses of the fraction, respectively. Group 4 was given distilled water (6 mL/kg) and group 5, castor oil (6 mL/kg P.O). Groups 6, 7, and 8 were given 1 g, 2 g, and 3 g of the fractions, respectively. Constipation was induced in all the groups except groups 1, 2, and 3s by administering metronidazole (7 mg/kg) and loperamide hydrochloride (6 mg/kg). After 30 min, the first stool time/latency time (min), number of stools, number of wet stools, and weight of stool (g) were recorded and the percent effect was calculated as follows:
Charcoal Meal Treatment
Pigeons were divided into five groups (n = 8). Constipation was induced in all the groups by loperamide hydrochloride. Group 1 was given distilled water (2 mL) and group 2 was served with castor oil while groups 3, 4, and 5 received fractions with a concentration of 25, 50, and 100 mg/kg, respectively. After 30 min, 2 mL of charcoal meal (a solution of 10% charcoal and 5% gum acacia) was given orally to each pigeon. The animals were then provided food and water, and, after 30 min, they were sacrificed. Then, the whole intestine, starting from the pylorus region up to the ileocecal junction, was removed from the pigeons and was placed on white paper parallel to a ruler. The distance travelled by the charcoal marker was measured and expressed as percent intestinal transit [40]. The percent effect was calculated as follows:
Spasmolytic Activity
The spasmolytic activity of the fractions was assessed according to earlier reported studies [36]. Briefly, the abdomen of the rabbit was opened after cervical dislocation and about 1.5–2.5-cm slices of jejunum were detached and placed in Tyrode solution in Petri dishes with a continuous supply of carbogen gas (95% O2 and 5% CO2). The mesentery was removed from the separated jejunum tissue and was fixed in the organ bath containing Tyrode solution at a retained temperature of 37 ± 1 °C. After this, the tissue was stabilized in the organ bath for about 20–30 min. The stable tissue with spontaneous response was taken as a baseline control, which is a positive control. The relaxing effect of the tested plant extract was compared.
Then, the effect of the fractions on spontaneous activity of the jejunum preparation was carried out at different concentrations, i.e., 0.01, 0.03, 0.1, 0.3, 3.0, 5.0, and 10 mg/mL, at an interval of 1 to 2 min in a cumulative manner, and the effect was noted. The effect of the fractions was also tested against KCL-induced contraction.
4.7. Ethical Approval
The study was approved by the ethical board of the Department of Pharmacy, Abdul Wali Khan University, Mardan, Pakistan. The ethical approval no. is EC/PhM/AWKUM-871D.
4.8. Statistical Analysis
Data are expressed as the mean. One-way ANOVA followed by Dunnett’s test was applied. The concentration–response curve was plotted using Graph Pad Prism for Windows 6.0 (Graph Pad Software, San Diego, CA, USA).
5. Conclusions
Fractions prepared from Chrozophora tinctoria exhibited prominent laxative and spasmogenic activities. The laxative effects were observed by AChE inhibition and the charcoal meal assay. Possible side effects from the plant extracts are nausea and vomiting. The current study strongly supports the folklore of Chrozophora tinctoria as a potential cathartic to be used in constipation treatment, although further molecular studies are needed to establish the underlying pharmacology.
Acknowledgments
We are thankful to all the institutions associated with the authors for providing resources.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules27072143/s1, Supplementary Table S1: Chemical structure of the compounds identified in DCMC and EAC fractions.
Author Contributions
Conceptualization, A.A.S. and A.I.; methodology, N.M.; software, N.M.; validation, A.A.S.; A.I. and N.M.; formal analysis, A.A.S.; investigation, A.A.S.; resources, A.I.; data curation, N.M.; writing—original draft preparation, A.A.S.; writing—review and editing, S.L.B.; A.-H.E. and M.J.; visualization, A.I.; supervision, A.I.; project administration, A.I.; funding acquisition, A.I.; S.L.B. and M.J. All authors have read and agreed to the published version of the manuscript.
Funding
We appreciate the Higher Education Commission of Pakistan and King Abdullah University of Science and Technology for their support.
Institutional Review Board Statement
The study was approved by the ethical board of the Department of Pharmacy, Abdul Wali Khan University, Mardan, Pakistan. The ethical approval no. is EC/PhM/AWKUM-871D.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data such as the source files associated with these findings are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the fractions are available from the author (Ayaz Ali Sher).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prichard D.O., Bharucha A.E. Recent advances in understanding and managing chronic constipation. F1000Research. 2018;7:1640. doi: 10.12688/f1000research.15900.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Werth B. Epidemiology of constipation in adults: Why estimates of prevalence differ. J. Epidemiol. Res. 2019;5:37. doi: 10.5430/jer.v5n1p37. [DOI] [Google Scholar]
- 3.Levy E., Lemmens R., Vandenplas Y., Devreker T. Functional constipation in children: Challenges and solutions. Pediatr. Health Med. Ther. 2017;8:19–27. doi: 10.2147/PHMT.S110940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forootan M., Bagheri N., Darvishi M. Chronic constipation: A review of literature. Medicine. 2018;97:e10631. doi: 10.1097/MD.0000000000010631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vilanova-Sanchez A., Gasior A.C., Toocheck N., Weaver L., Wood R.J., Reck C.A., Wagner A., Hoover E., Gagnon R., Jaggers J., et al. Are Senna based laxatives safe when used as long term treatment for constipation in children? J. Pediatr. Surg. 2018;53:722–727. doi: 10.1016/j.jpedsurg.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Wintola O.A., Sunmonu T.O., Afolayan A.J. The effect of Aloe ferox Mill. In the treatment of loperamide-induced constipation in Wistar rats. BMC Gastroenterol. 2010;10:95. doi: 10.1186/1471-230X-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altabas K., Bilić A., Jurčić D., Dorosulić Z., Mihanović M., Šunić-Omejc M., Restek-Petrović B., Tolj N. The efficacy of cisapride vs. placebo and diet in patients with chronic constipation. Coll. Antropol. 2003;27:197–204. [PubMed] [Google Scholar]
- 8.Luthra P., Camilleri M., Burr N.E., Quigley E.M.M., Black C.J., Ford A.C. Efficacy of drugs in chronic idiopathic constipation: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2019;4:831–844. doi: 10.1016/S2468-1253(19)30246-8. [DOI] [PubMed] [Google Scholar]
- 9.Busti A.J., Murillo J.R., Cryer B. Tegaserod-induced myocardial infarction: Case report and hypothesis. Pharmacotherapy. 2004;24:526–531. doi: 10.1592/phco.24.5.526.33351. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.E., Choi Y.J., Lee S.J., Gong J.E., Lee Y.J., Sung J.E., Jung Y.S., Lee H.S., Hong J.T., Hwang D.Y. Antioxidant activity and laxative effects of tannin-enriched extract of Ecklonia cava in loperamide-induced constipation of SD rats. PLoS ONE. 2021;16:e0246363. doi: 10.1371/journal.pone.0246363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jabri M.A., Wannes D., Hajji N., Sakly M., Marzouki L., Sebai H. Role of laxative and antioxidant properties of Malva sylvestris leaves in constipation treatment. Biomed. Pharmacother. 2017;89:29–35. doi: 10.1016/j.biopha.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Lee H.Y., Kim J.H., Jeung H.W., Lee C.U., Kim D.S., Li B., Lee G.H., Sung M.S., Ha K.C., Back H.I., et al. Effects of Ficus carica paste on loperamide-induced constipation in rats. Food Chem. Toxicol. 2012;50:895–902. doi: 10.1016/j.fct.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Delazar A., Talischi B., Nazemiyeh H., Rezazadeh H., Nahar L., Sarker S.D. Chrozophorin: A new acylated flavone glucoside from Chrozophora tinctoria (Euphorbiaceae) Rev. Bras. Farmacogn. 2006;16:286–290. doi: 10.1590/S0102-695X2006000300002. [DOI] [Google Scholar]
- 14.Ahmed M.A., Mariod A.A., Hussein I.H., Kamal-Eldin A. Review: Biochemical composition and medicinal uses of Chrozophora genus. Inter. J. Pharm. Rev. Res. 2014;4:227–232. [Google Scholar]
- 15.Khare C.P. Indian Medicinal Plants: An Illustrated Dictionary. Springer; Berlin, Germany: 2007. p. 900. [Google Scholar]
- 16.Kader T.A. Effect of turnsoles Chrozophora tinctoria L. extracts on some pathological bacteria types. Anbar J. Agric. Sci. 2009;7:369–378. [Google Scholar]
- 17.Hashim O.K., Abou-zaid M.M., Abdel-Galil F.M., Saleh N.A.M. The flavonoids of Egyptian Chrozophora species. Biochem. Syst. Ecol. 1990;18:151–152. doi: 10.1016/0305-1978(90)90051-G. [DOI] [Google Scholar]
- 18.Ahmed F.A. Phytochemical studies on Chrozophora tinctoria (L.) Raf. growing naturally in South Sinai. Bull. Agric. Univ. Cairo. 2003;54:93–110. [Google Scholar]
- 19.Hawas U.W. Antioxidant activity of brocchlin carboxylic acid and its methyl ester from Chrozophora brocchiana. Nat. Prod. Res. 2007;21:632–640. doi: 10.1080/14786410701371124. [DOI] [PubMed] [Google Scholar]
- 20.Tabussum A., Riaz N., Saleem M., Ashraf M., Ahmad M., Alam U., Jabeen B., Malik A., Jabbar A. α-Glucosidase inhibitory constituents from Chrozophora plicata. Phytochem. Lett. 2013;6:614–619. doi: 10.1016/j.phytol.2013.08.005. [DOI] [Google Scholar]
- 21.Golkar P., Taghizadeh M., Jalali S.A.H. Determination of phenolic compounds, antioxidant and anticancer activity of Chrozophora tinctoria accessions collected from different regions of Iran. J. Food Biochem. 2019;43:e13036. doi: 10.1111/jfbc.13036. [DOI] [PubMed] [Google Scholar]
- 22.Ullah A., Munir S., Badshah S.L., Khan N., Ghani L., Poulson B.G., Emwas A.H., Jaremko M. Important flavonoids and their role as a therapeutic agent. Molecules. 2020;25:5243. doi: 10.3390/molecules25225243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Badshah S.L., Faisal S., Muhammad A., Poulson B.G., Emwas A.H., Jaremko M. Antiviral activities of flavonoids. Biomed. Pharmacother. 2021;140:111596. doi: 10.1016/j.biopha.2021.111596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sher A.A., Bakht J., Khan K. Antinociceptive, antipyretic and antimicrobial activities of Chrozophora tinctoria extracts. Indian J. Pharm. Sci. 2018;80:533–540. doi: 10.4172/pharmaceutical-sciences.1000388. [DOI] [Google Scholar]
- 25.Auda M.A., Saoudi M.H. Anti-diabetic activity and hepatoprotective effect of Chrozophora tinctoria (L.) Rafin leaves aqueous extract in STZ induced diabetic rats model. Am. J. Biomed. 2018;6:755–775. doi: 10.18081/2333-5106/018-12/755-775. [DOI] [Google Scholar]
- 26.Abdel-Naim A.B., Alghamdi A.A., Algandaby M.M., Al-Abbasi F.A., Al-Abd A.M., Eid B.G., Abdallah H.M., El-Halawany A.M. Rutin isolated from Chrozophora tinctoria enhances bone cell proliferation and ossification markers. Oxid. Med. Cell. Longev. 2018;2018:5106469. doi: 10.1155/2018/5106469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mukherjee P.K., Kumar V., Mal M., Houghton P.J. Acetylcholinesterase inhibitors from plants. Phytomedicine. 2007;14:289–300. doi: 10.1016/j.phymed.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Maya M., Sarada S. In vitro screening for anti-cholinesterase and antioxidant activity of methanolic extracts of Ayurvedic medicinal plants used for cognitive disorders. PLoS ONE. 2014;9:e86804. doi: 10.1371/journal.pone.0086804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali N., Shah I., Shah S.W.A., Ahmed G., Shoaib M., Junaid M., Ali W., Ahmed Z. Antioxidant and relaxant activity of fractions of crude methanol extract and essential oil of Artemisia macrocephala jacquem. BMC Complement. Altern. Med. 2013;13:96. doi: 10.1186/1472-6882-13-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanihata S., Igarashi H., Suzuki M., Uchiyama T. Cisplatin-induced early and delayed emesis in the pigeon. Br. J. Pharmacol. 2000;130:132–138. doi: 10.1038/sj.bjp.0703283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hartati S., Angelina M., Dewiyanti I., Meilawati L. Isolation and characterization compounds from hexane and ethyl acetate fractions of Peperomia pellucida L. J. Trop. Life Sci. 2015;5:117–122. doi: 10.11594/jtls.05.03.02. [DOI] [Google Scholar]
- 32.Bakht J., Tayyab M., Ali H., Islam A., Shafi M. Effect of different solvent extracted sample of Allium sativum (Linn) on bacteria and fungi. Afr. J. Biotechnol. 2011;10:5910–5915. doi: 10.5897/ajb11.232. [DOI] [Google Scholar]
- 33.Alam M., Uddin G., Siddiqui B.S., Sadat A., Khan A.A., Rauf A. Gas chromatography-mass spectrometry (GC-MS) analysis, antimicrobial, phytotoxic, insecticidal and leishmanicidal activities of fixed oil from Viburnum grandiflorum. Afr. J. Pharm. Pharmacol. 2014;8:1173–1179. doi: 10.5897/AJPP2014.4143. [DOI] [Google Scholar]
- 34.Shah Z., Badshah S.L., Iqbal A., Shah Z., Emwas A.H., Jaremko M. Investigation of important biochemical compounds from selected freshwater macroalgae and their role in agriculture. Chem. Biol. Technol. Agric. 2022;9:1–11. doi: 10.1186/s40538-021-00273-0. [DOI] [Google Scholar]
- 35.Muhammad N., Ullah S., Abu-Izneid T., Rauf A., Shehzad O., Atif M., Khan H., Naz H., Herrera-Calderon O., Khalil A.A., et al. The pharmacological basis of Cuscuta reflexa whole plant as an antiemetic agent in pigeons. Toxicol. Rep. 2020;7:1305–1310. doi: 10.1016/j.toxrep.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ali N., Ahmad B., Ali Shah S.W. Spasmogenic and spasmolytic activities of Onosma griffithii Vatke. Pak. J. Pharm. Sci. 2011;24:553–558. [PubMed] [Google Scholar]
- 37.Ellman G.L., Courtney K.D., Andres V., Featherstone R.M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 1961;7:88–95. doi: 10.1016/0006-2952(61)90145-9. [DOI] [PubMed] [Google Scholar]
- 38.Badshah S.L., Riaz A., Muhammad A., Çayan G.T., Çayan F., Duru M.E., Ahmad N., Emwas A.H., Jaremko M. Isolation, characterization, and medicinal potential of polysaccharides of Morchella esculenta. Molecules. 2021;26:1459. doi: 10.3390/molecules26051459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joshi C.S., Priya E.S., Venkataraman S. Acute and subacute toxicity studies on the polyherbal antidiabetic formulation Diakyur in experimental animal models. J. Health Sci. 2007;53:245–249. doi: 10.1248/jhs.53.245. [DOI] [Google Scholar]
- 40.Ullah I. Role of gastrointestinal motility/gastric emptying in cisplatin-induced vomiting in pigeon. Afr. J. Pharm. Pharmacol. 2012;6:2592–2599. doi: 10.5897/AJPP12.530. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data such as the source files associated with these findings are available from the corresponding author upon request.