Abstract
Amphotericin B is the only recognized antifungal used in the treatment of mucormycosis. In this study, we evaluated various combinations of amphotericin B, fluconazole, and trovafloxacin or ciprofloxacin in the treatment of murine pulmonary mucormycosis. The combination of fluconazole and a quinolone has a marked effect on the outcome of murine pulmonary mucormycosis. Even though we did not optimize therapy with the drugs, these experiments suggest that azoles, especially fluconazole, in combination with either trovafloxacin or ciprofloxacin were effective in the treatment of this aggressive mycosis in the mouse model.
Mucormycosis is an uncommon but extremely aggressive and destructive fungal infection (6). Despite the introduction of several new antifungal drugs over the past decade, options for the treatment of mucormycosis remain limited. Amphotericin B has been the mainstay of medical therapy for this condition, but morbidity and mortality remain high. Surgical intervention is widely perceived to be instrumental in achieving a successful outcome in many forms of mucormycosis (4, 5). Whether alternative drugs will help to arrest the infection remains to be determined. Little work with newer antifungal compounds, including the new formulations of amphotericin B, has been done in experimental models of mucormycosis, but some case reports have been published detailing some of the newer agents (2, 3).
We have previously shown the value of combinations of various compounds for the treatment of murine invasive candidiasis, including combinations of quinolone antibiotics and amphotericin B or azole antifungals (7). We have also demonstrated the potential for azole antifungal drugs to be useful in the therapy of mucormycosis (1). In this study, we have evaluated the efficacy of amphotericin B, the quinolones trovafloxacin and ciprofloxacin, and fluconazole in the treatment of murine pulmonary mucormycosis.
Outbred male ICR mice, each weighing approximately 20 g, were housed in treatment groups of 10 per large cage. They were provided food and water ad libitum.
Rhizopus oryzae was maintained on Sabouraud agar slants at 4°C and was subcultured onto a fresh Sabouraud agar slant and incubated for 48 h at 35°C prior to use in an experiment (1).
Conidia were harvested by flooding the slant with sterile water, agitating the culture tube, and filtering the suspension through gauze on ice. The conidia were counted, washed in cold sterile water, and resuspended in physiologic buffered saline at a concentration of 4 × 107/ml.
Mice were given cortisone acetate (10 mg/mouse) by intraperitoneal injection 72 and 24 h prior to being infected with R. oryzae. Mice were lightly anesthetized with halothane and held in an upright position. Fifty microliters of conidial suspension was placed on the nares of the mouse, and the mouse was held upright for 2 to 3 min following aspiration of the fungi. They were then returned to their cages.
Treatment was begun 24 h following infection with the regimens noted for each experiment and was continued for 10 consecutive days. Amphotericin B was obtained from Sigma as the deoxycholate suspension and was prepared fresh daily in sterile water. Fluconazole and trovafloxacin were obtained as powders from Pfizer, Inc., and were prepared fresh daily in sterile water. Ciprofloxacin was obtained as the injectable compound from the pharmacy. Groups of 10 mice/treatment regimen were used. Amphotericin B was administered by intraperitoneal injection once daily, and fluconazole and the quinolones were given by oral gavage twice daily.
Mice were observed twice daily, and dead mice were removed from the cages. Moribund mice (those unable to eat or drink) were removed from the cage and sacrificed with CO2. Mortality was recorded for 30 days.
Kaplan-Meier plots were created, and survival times were evaluated according to the log-rank statistic (SPSS for Windows). Significance was defined as P < 0.05.
The efficacy of amphotericin B, fluconazole, and trovafloxacin when used alone or in combination in the treatment of murine pulmonary mucormycosis is shown in Fig. 1. All untreated mice died by day 21. Mice treated with either trovafloxacin (80 mg/kg of body weight twice daily) or fluconazole (80 mg/kg of body weight twice daily) alone also had survival not significantly different from that of controls: 0% at day 23 and 20% at day 30. In contrast, mice treated with amphotericin B (1 mg/kg of body weight per day) or the combination of fluconazole and trovafloxacin had increased survival at day 30: 90 and 50%, respectively (P < 0.002 for amphotericin B compared to control, trovafloxacin, or fluconazole and P = 0.03 for the fluconazole and trovafloxacin combination compared to control). There was no statistical difference in the effect of amphotericin B with the combination regimen (P = 0.07). Median survival times (MSTs) are shown in Table 1.
FIG. 1.
(A) Mice were infected with R. oryzae as described in the text and placed into the following treatment groups: untreated controls (■), trovafloxacin treated (▾), fluconazole treated (●), fluconazole plus trovafloxacin treated (▴), or amphotericin B treated (⧫). Significant positive effects on percent survival were seen in mice treated with amphotericin B or the combination of fluconazole plus trovafloxacin. (B) In the same experiment, mice were also treated with amphotericin B plus fluconazole plus trovafloxacin (□) or with amphotericin B plus trovafloxacin (○). The curves for single drug treatment are repeated for purposes of comparison and are the same as those depicted in Fig. 1A. The addition of one or two other drugs to amphotericin B resulted in no additional survival benefit or antagonism of amphotericin B.
TABLE 1.
MSTs with fluconazole, trovafloxacin, and amphotericin B
| Treatment group | MST (days)
|
||
|---|---|---|---|
| Expt 1 | Expt 2 | Expt 3 | |
| Control | 14 | 16 | 14 |
| Trovafloxacin | 11 | 16 | 15 |
| Fluconazole | 14 | 18 | 18 |
| Fluconazole + trovafloxacin | 23 | >30 | >30 |
| Amphotericin B | >30 | >30 | >30 |
| Amphotericin B + trovafloxacin | >30 | >30 | >30 |
| Amphotericin B + fluconazole + trovafloxacin | >30 | >30 | >30 |
In the same experiment, combinations of amphotericin B with trovafloxacin or amphotericin B plus trovafloxacin plus fluconazole were also evaluated. As shown in Table 1, survival rates of mice treated with amphotericin B plus trovafloxacin (70%) and with all three drugs (90%) were not statistically different from those with amphotericin B alone. The design of the experiment did not allow for determination of additive effects of the combinations compared to amphotericin B when used alone, since survival with amphotericin B at 1 mg/kg/day was 100%. Given survival of <100% in the combination groups, however, it is unlikely that an enhancement in efficacy exists when these other drugs are used with amphotericin B. Three similar experiments yielded identical results (data not shown).
The effects of low-dose amphotericin B in this model were evaluated in a separate set of experiments (Fig. 2). All untreated mice died by day 26, with an MST of 16 days (Table 1). All mice treated with trovafloxacin or fluconazole died by day 29 or 26, respectively, with MSTs of 16 and 18 days, respectively. Amphotericin B at 0.5 mg/kg/day was ineffective, with all mice dead by day 28 and an MST of 21 days (not significant compared to control). In contrast, as in the previous experiments, amphotericin B at 1 mg/kg/day was the most effective therapy, with 100% survival by day 30 and with MSTs of >30 days. Fluconazole plus trovafloxacin resulted in 80% survival by day 30 (MST of >30 days), and these drugs together with full-dose amphotericin B were similarly effective: 30-day survival of 90% (MST of >30 days). When mice were treated with fluconazole plus trovafloxacin plus amphotericin B at 0.5 mg/kg/day, 30-day survival was 90% and the MST was >30 days. Thus, amphotericin B did not antagonize the effects of the azole plus quinolone, but enhancement of the dual drug therapy by adding low-dose amphotericin B was not seen, perhaps because of the efficacy of the dual drug regimen. An additional experiment produced similar results.
FIG. 2.
Effects of treatment with low (suboptimal) doses of amphotericin B. Treatment groups were as follows: untreated controls (■), trovafloxacin treated (▾), fluconazole treated (●), fluconazole plus trovafloxacin treated (▴), low-dose amphotericin B at 0.5 mg/kg/day treated (▿), amphotericin B at 0.5 mg/kg/day plus fluconazole plus trovafloxacin treated (◊), or amphotericin B at 1 mg/kg/day treated (⧫). There were no differences in survival between mice treated with amphotericin B at 1 mg/kg/day and mice treated with fluconazole plus trovafloxacin or amphotericin B at 0.5 mg/kg/day plus fluconazole plus trovafloxacin. Note that the amphotericin B and amphotericin B plus fluconazole plus trovafloxacin groups overlap.
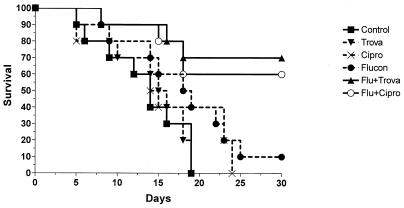
To determine whether the identity of the quinolone was important, an experiment using ciprofloxacin rather than trovafloxacin was done. In this experiment (Fig. 3), survival of mice treated with ciprofloxacin at 80 mg/kg twice daily by oral gavage was 0 by day 23 (MST of 14 days) compared to untreated mice (0% survival by day 18 [MST of 14 days]). Mice treated with fluconazole alone did not fare significantly differently from untreated controls: 10% survival by day 30 (MST of 18). In contrast, ciprofloxacin plus fluconazole resulted in 60% survival, with an MST of >30 days (P < 0.01 compared to control and ciprofloxacin alone and P < 0.05 compared to fluconazole alone).
FIG. 3.
Effect of ciprofloxacin in combination therapy with fluconazole and quinolones. Mice were treated as in previous experiments, with the exception that ciprofloxacin was substituted for trovafloxacin. The treatment groups were as follows: untreated controls (■), ciprofloxacin treated (▾), fluconazole treated (●), fluconazole plus ciprofloxacin treated (▴), and amphotericin B treated (⧫). No differences in survival were noted in mice treated with fluconazole and either trovafloxacin or ciprofloxacin.
Mucormycosis remains a formidable therapeutic challenge. Despite optimal therapy with amphotericin B, the fungus continues to cause extensive morbidity. Adjunctive surgical intervention is often required to gain control of the infection. Medical therapy with amphotericin B is the only recognized treatment option.
In all of the work performed with these drugs in the murine model of mucormycosis, fluconazole, trovafloxacin, and ciprofloxacin when used alone were inactive. Neither overall survival nor MSTs were significantly improved with these compounds. However, it is interesting that the combination of an azole with a quinolone demonstrated significant effects in prolonging survival of mice treated with these regimens. Addition of this combination had no effect in increasing survival of mice treated with amphotericin B, but this may be a function of finding the most appropriate dose of amphotericin B to demonstrate additive effects of various combinations of drugs. It is important to note that addition of fluconazole plus trovafloxacin to amphotericin B had no antagonistic effects, a potentially important observation given that amphotericin B remains as the cornerstone of drug therapy for mucormycosis. While one might argue that the antibacterial effects of the quinolones prevented deaths from bacterial superinfections, the lack of such a positive effect in mice treated with a quinolone and amphotericin B does not support this hypothesis.
Consistent with the experience in treating humans with mucormycosis, amphotericin B was very effective in prolonging survival in this model. Organ cultures were not done because of the problem of quantification of hyphal organisms. The degree of tissue homogenization has considerable impact on the numbers of CFU that can be recoverable from infected animals. Moreover, these experiments were designed primarily as a proof of principle. Further formal pharmacokinetic and pharmacodynamic studies are warranted to explore possibilities for the use of such combinations in treating humans with mucormycosis.
In conclusion, the results presented in this paper serve as initial evidence that combination therapy with fluconazole and the quinolone topoisomerase inhibitors have beneficial effects in prolonging survival in mice infected with R. oryzae. Additional work with more fungus-specific topoisomerase inhibitors and the newer azoles would be of interest.
Footnotes
Publication no. 017 from the Collaborative Medical Mycology Research Program (Section of Infectious Diseases, Department of Medicine, Boston Medical Center and Pfizer, Roerig Division).
REFERENCES
- 1.Goldani L Z, Sugar A M. Treatment of murine pulmonary mucormycosis with SCH 42427, a broad-spectrum triazole antifungal drug. J Antimicrob Chemother. 1994;33:369–372. doi: 10.1093/jac/33.2.369. [DOI] [PubMed] [Google Scholar]
- 2.Kocak R, Tetiker T, Kocak M, Baslamisli F, Zorludemir S, Gonlusen G. Fluconazole in the treatment of three cases of mucormycosis. Eur J Clin Microbiol Infect Dis. 1995;14:559–561. doi: 10.1007/BF02113443. [DOI] [PubMed] [Google Scholar]
- 3.Maury S, Leblanc T, Feuilhade M, Molina J M, Schaison G. Successful treatment of disseminated mucormycosis with liposomal amphotericin B and surgery in a child with leukemia. Clin Infect Dis. 1998;26:200–202. doi: 10.1086/517067. [DOI] [PubMed] [Google Scholar]
- 4.Nussbaum E S, Hall W A. Rhinocerebral mucormycosis: changing patterns of disease. Surg Neurol. 1994;41:152–156. doi: 10.1016/0090-3019(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 5.Peterson K L, Wang M, Canalis R F, Abemayor E. Rhinocerebral mucormycosis: evolution of the disease and treatment options. Laryngoscope. 1997;107:855–862. doi: 10.1097/00005537-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Sugar A M. Agents of mucormycosis and related species. In: Mandell G, Bennett J, Dolin R, editors. Principles and practice of infectious diseases. 5th ed. Philadelphia, Pa: Churchill Livingstone; 2000. pp. 2685–2695. [Google Scholar]
- 7.Sugar A M, Liu X-P, Chen R-J. Effectiveness of quinolone antibiotics in modulating the effects of antifungal drugs. Antimicrob Agents Chemother. 1997;41:2518–2521. doi: 10.1128/aac.41.11.2518. [DOI] [PMC free article] [PubMed] [Google Scholar]