Abstract
Background
Achondroplasia, caused by a pathogenic variant in the fibroblast growth factor receptor 3 gene (FGFR3), leads to significant multisystem complications across the lifespan that may affect the health‐related quality of life (HRQoL) of individuals and families living with the condition.
Methods
The objective of this qualitative study was to describe the HRQoL of children and adolescents with achondroplasia and their caregivers. Thirty‐four caregivers and 12 adolescents from the United States and Spain participated in one of eight focus groups or completed an individual interview, which was audio‐recorded and transcribed. Thematic analysis of qualitative data was performed to identify commonly occurring themes pertaining to HRQoL.
Results
Caregivers and adolescents described challenges with physical functioning and medical complications due to achondroplasia. Key challenges included difficulties performing activities of daily living, issues of accessibility, bullying, or unwanted attention in public, and negative effects on self‐esteem. Caregivers were concerned about accessing appropriate medical care for their child, and also reported experiencing financial, relational, and emotional challenges in their families. Achondroplasia also affected individuals and their families in positive ways, including increasing empathy, receiving positive attention, and feeling supported by the achondroplasia community.
Conclusions
These findings underscore the importance of regular assessments of HRQoL and the provision of psychosocial support to affected children and families.
Keywords: achondroplasia, quality of life, skeletal dysplasia
This qualitative study describes the impact of achondroplasia on the health‐related quality of life (HR‐QoL) of affected children and adolescents and on caregivers. Many individuals with achondroplasia, as well as caregivers, experience daily challenges, and require ongoing adaptations related to the condition, but also report some positive aspects living with achondroplasia. These findings underscore the importance of regular psychosocial assessments and the provision of psychosocial support to affected children and families.

1. INTRODUCTION
Achondroplasia (OMIM 100800), the most common skeletal dysplasia, occurs in approximately 1/25,000 live births (Foreman et al., 2020) and is estimated to affect over 250,000 people worldwide (Horton et al., 2007; Pauli, 2019). Achondroplasia is caused by a gain‐of‐function mutation in the fibroblast growth factor receptor 3 (FGFR3) gene, leading to impaired endochondral bone growth (Horton et al., 2007). Clinical features include disproportionate short stature with narrow chest, short fingers and limbs, midface hypoplasia, macrocephaly with frontal bossing, abnormal spinal curvature, hypermobility in the knees and hips, hypotonia, and tibial bowing (Fredwall et al., 2020; Hoover‐Fong et al., 2021; Horton et al., 2007; Pauli, 2019). Individuals with achondroplasia face a range of medical issues over the lifespan, including foramen magnum stenosis and cervicomedullary compression, developmental motor milestone delays, ear infections, hearing loss, genu varum, spinal stenosis, chronic pain, and respiratory dysfunction (Fredwall et al., 2020; Hoover‐Fong et al., 2021; Horton et al., 2007; Pauli, 2019; Pfeiffer et al., 2021a, 2021b).
In addition to medical complications, achondroplasia can impact multiple domains of health‐related quality of life (HRQoL) in affected children (Alade et al., 2013; Ireland et al., 2011; Pfeiffer et al., 2021b; Witt et al., 2017; Witt et al., 2019), adolescents (Alade et al., 2013; Matsushita et al., 2019; Witt et al., 2017), and adults (Alade et al., 2013; Dhiman et al., 2017; Gollust et al., 2003; Mahomed et al., 1998; Matsushita et al., 2019; Witt et al., 2017; Yonko et al., 2021). Compared to individuals of average stature, individuals with achondroplasia consistently demonstrate lower HRQoL scores in physical domains (Alade et al., 2013; Dhiman et al., 2017; Gollust et al., 2003; Ireland et al., 2011; Mahomed et al., 1998; Matsushita et al., 2019; Pfeiffer et al., 2021b; Witt et al., 2017; Yonko et al., 2021). Some studies have also reported that individuals with achondroplasia score lower in social, emotional, and school‐related domains (Dhiman et al., 2017; Gollust et al., 2003; Pfeiffer et al., 2021b; Witt et al., 2017; Witt et al., 2019) compared to average stature individuals. Additionally, in one quantitative study, parents of children with achondroplasia reported significantly lower mental health scores compared to a reference population (Witt et al., 2019). A qualitative study of parents of children with achondroplasia aged 2–12 years found that the majority experienced worry or concern for their child, and that many felt stressed or overwhelmed, and described impacts on caregiver employment, family relationships, family activities, and social well‐being (Pfeiffer et al., 2021a). However, interventional programs provided by patient advocacy groups that are tailored specifically to the needs of individuals with achondroplasia and their families have been shown to improve HRQoL of participants compared to no change in HRQoL of nonparticipants (Witt et al., 2017).
It is important for clinicians and other stakeholders to understand current experiences within achondroplasia communities in order to improve the quality of care of affected individuals and to inform clinical practice guidelines (Savarirayan et al., 2021). Qualitative studies can provide more detailed insights into people's experiences compared to purely quantitative studies; moreover, utilizing focus groups enables participation from individuals who may be reluctant to partake in individual interviews, and the group interaction facilitates exploration on how and why people think the way they do (Kitzinger, 1995). The objective of this qualitative study was to better characterize how achondroplasia affects HRQoL for children and adolescents and their caregivers using concept elicitation focus groups and interviews. While previous studies have reported HRQoL in adolescents using quantitative measures, to our knowledge, no qualitative studies have described the experiences of adolescents from their own perspective. Additionally, we recruited participants from the United States (US) and Spain, two countries with divergent approaches to certain aspects of achondroplasia management (surgical limb lengthening is commonly practiced in Spain but rarely performed in the US), to examine country‐ and cultural‐specific similarities and differences in experiences with achondroplasia.
2. METHODS
2.1. Study design
This study consisted of four focus group discussions in both the US and Spain: adolescents (ages 13–17 years) with achondroplasia, and the caregivers of children/adolescents with achondroplasia aged 0–4, 5–12, and 13–17 years. As the type and severity of complications associated with achondroplasia differ across life stages (Hoover‐Fong et al., 2021), focus groups were segmented by age. Additionally, three one‐on‐one telephone interviews with US adolescents were conducted due to low attendance in the US adolescent focus group. While focus groups can be conducted with young children (Adler et al., 2019), it was not deemed appropriate for children under age 13 years to participate in this study given the complexity of the topics of interest and the planned duration of the sessions (outlined below); we, therefore, relied on caregiver reports to gain insight into the experiences of younger children. Focus groups and interviews were conducted by experienced qualitative researchers with study‐specific training.
Focus groups were conducted in three 90‐minute sessions organized around the following topics: (a) understand the impact of achondroplasia on affected individuals' and caregivers' lives; (b) obtain perceptions of the risk, benefits, and important aspects of treatments; and (c) understand the clinically meaningful change in height, proportionality, independence with activities of daily living, and meaningful change in scores of three HRQoL instruments (Pediatric Quality of Life Inventory (PedsQL™) (Varni et al., 2001), Quality of Life in Short Stature Youth (QoLISSY) (Bullinger et al., 2013) and Functional Independence Measure for Children (WeeFIM) (Slomine, 2011). The objective of this manuscript is to report the experiences of living with achondroplasia, which was primarily discussed in the first session. Data gathered in the second and third sessions were of interest for use in potential future studies; however, data from all sessions were included in this analysis.
2.2. Eligibility and recruitment
Participants resided in the US or Spain and were able to communicate fluently in the local language. Participants were ineligible if they (or their child with achondroplasia) had another unrelated condition or chronic illness which impacted HRQoL. Caregivers were defined as a primary caregiver to the individual with achondroplasia, and potentially included adoptive parents or grandparents. Only one caregiver with achondroplasia was permitted to participate in each of the caregiver focus groups, so that representation would be similar to the achondroplasia population with 20% of parents affected (Horton et al., 2007).
Recruitment was conducted through Global Perspectives. In Spain, participants were identified through the support organization Fundación ALPE Acondroplasia. In the US, participants were identified through a variety of sources, including Global Perspectives databases, a recruiter with close personal links to the community, and patient support groups willing to share the study announcement on social media.
2.3. Study procedures
A semi‐structured focus group discussion guide was developed based on consultation with five international clinical experts representing a range of specialties (clinical genetics, pediatrics, orthopedics) whose clinical experience with achondroplasia spanned 22–40 years. The discussion guide began with broad questions to elicit responses spontaneously, followed by specific questions based on impacts identified by the clinical experts. Examples of discussion guide topics and questions are provided in Table 1. The adolescent focus group discussion guide was also used for the individual Interviews.
TABLE 1.
Examples of discussion guide questions
| Topic | Caregiver discussion guides | Adolescent discussion guide |
|---|---|---|
| Physical impacts | In terms of any physical impacts, please can you describe how achondroplasia impacts physical functioning and say a little about how these impact your child's daily life? | In terms of any physical impacts, please can you describe how achondroplasia affects your physical functioning and say a little about how these impact your daily life? |
| Activities of daily living |
Ages 0–4 years: Does achondroplasia affect your child's ability to do activities appropriate for their age? Ages 5–17 years: Is your child able to manage their self‐care in relation to going to the toilet, washing, and dressing? (If no, do you think this will change?) |
Are you able to manage your own self‐care? (going to the toilet, washing, and dressing) |
| Social impacts | Have there been any social impacts for your child due to achondroplasia? (How is school life for your child? How do any challenges impact your child?) | Are you affected socially because you have achondroplasia? (How is school life for you? How do any challenges affect you?) |
| Medical care |
Tell me about your experiences with medical care for your child (Does your child have any routine follow‐up appointments related to achondroplasia? If so, how often?) (Do you have a medical provider who understands how to treat children with achondroplasia?) |
Tell me about your experiences with medical care (Do you have any routine follow‐up appointments related to achondroplasia? If so, how often?) (Do you have a medical provider who understands how to treat individuals with this condition?) |
| Impacts on family | Do you think there are specific impacts in having a child with achondroplasia on the family overall? | Not asked |
| Treatments | Before we discuss specific types of treatments, it would be useful to know in general what you think about medical treatment for this condition (Have your thoughts on this changed over time at all? If so, why? What led to this change?) | |
Note: Examples of probes, or potential follow‐up questions after spontaneous responses to the first question, are shown in parentheses. Due to the semi‐structured nature of guide, not all probes were asked directly and moderators could also ask other follow up questions according to the flow of the discussion. Note that this table provides several examples by topic only and does not show all possible probes included in the full discussion guide.
2.4. Analysis
Focus groups and interviews were audio recorded and transcribed verbatim. Spanish sessions were transcribed directly into English with review for accuracy by the bilingual moderators.
Thematic analysis, as described by Joffe and Yardley (2004) and based broadly on grounded theory (Glaser & Strauss, 1967), was the selected analytic approach to meet the research objectives. Initial codes were based on pre‐defined concepts and themes; analysts added data‐driven codes that emerged during the focus groups and interviews.
MAXQDA qualitative analysis software was used to help organize the data and code the transcripts (Software, 2020). The lead analyst reviewed several transcripts to develop a preliminary codebook. Two transcripts (one per country and representative of different age cohorts) were double coded independently by two analysts and compared. Discrepancies were discussed and addressed by modifying the organization of the codebook or clarifying code definitions. After the second inter‐coder exercise showed high agreement, one analyst coded the remaining transcripts. Before the codebook was finalized, a second analyst familiar with the dataset reviewed the results.
3. RESULTS
3.1. Sample description
Focus groups and interviews were conducted between August and October 2018. Participants included 34 caregivers (US n = 16, Spain n = 18) and 12 adolescents (US n = 6, Spain n = 6). Sample characteristics are provided in Tables 2 and 3. Children of caregivers were distributed across the age groups. In the US, all caregivers were female; in Spain, most caregivers were female (n = 14/18, 78%). All caregivers were biological or adoptive parents.
TABLE 2.
Sample characteristics: US
| Caregivers of ages 0–4 years (n = 6) | Caregivers of ages 5–12 years (n = 6) | Caregivers of ages 13–17 years (n = 4) | Adolescents ages 13–17 years (n = 6) a | |
|---|---|---|---|---|
| Sex of caregiver | ||||
| Male | 0 | 0 | 0 | — |
| Female | 6 | 6 | 4 | — |
| Caregivers with achondroplasia | 1 | 1 | 0 | — |
| Ethnicity (child) | ||||
| Caucasian | 5 | 6 | 4 | 4 |
| Asian b | 0 | 0 | 2 | 2 |
| Unknown | 1 | 0 | 0 | 0 |
| Education (caregiver) | ||||
| High school | 1 | 0 | 0 | — |
| Some college | 2 | 1 | 1 | — |
| Bachelor's degree | 2 | 4 | 2 | — |
| Master's degree | 1 | 1 | 1 | — |
| Employment (caregiver) | ||||
| Full time | 1 | 2 | 0 | — |
| Part time | 4 | 0 | 2 | — |
| Self employed | 0 | 1 | 2 | — |
| Stay at home | 0 | 3 | 0 | — |
| Student | 1 | 0 | 0 | — |
| Unemployed | 0 | 0 | 0 | |
| Marital status (caregiver) | ||||
| Married | 4 | 6 | 3 | — |
| Divorced/separated | 1 | 0 | 1 | — |
| Single | 1 | 0 | 0 | — |
| Sex of child | ||||
| Male | 4 | 5 | 3 | 4 |
| Female | 2 | 1 | 1 | 2 |
Includes two adolescents who completed telephone interviews and whose parents did not participate in the caregiver focus groups. Additionally, one adolescent whose mother participated in the focus groups completed a telephone interview.
Two adolescents were adopted from China by two US families.
TABLE 3.
Sample characteristics: Spain
| Caregivers of ages 0–4 years (n = 6) | Caregivers of ages 5–12 years (n = 6) | Caregivers of ages 13–17 years (n = 6) a | Adolescent ages 13–17 years (n = 6) a | |
|---|---|---|---|---|
| Sex of caregiver | ||||
| Male | 1 | 1 | 2 | — |
| Female | 5 | 5 | 4 | |
| Caregivers with achondroplasia | 0 | 1 | 1 | — |
| Ethnicity (child) | ||||
| Caucasian | 5 | 6 | 6 | 6 |
| Caribbean | 1 | 0 | 0 | 0 |
| Education (caregiver) | ||||
| High school | 1 | 1 | 3 | — |
| Technical/vocational | 1 | 1 | 3 | — |
| University diploma | 3 | 3 | 0 | — |
| Postgraduate degree | 1 | 1 | 0 | — |
| Employment (caregiver) | ||||
| Full time | 4 | 5 | 5 | — |
| Part time | 1 | 1 | 1 | — |
| Self employed | 0 | 0 | 0 | — |
| Stay at home | 0 | 0 | 0 | — |
| Student | 0 | 0 | 0 | — |
| Unemployed | 1 | 0 | 0 | |
| Marital status (caregiver) | ||||
| Married | 5 | 5 | 5 | — |
| Divorced/separated | 0 | 0 | 1 | — |
| Single | 1 | 1 | 0 | — |
| Sex of child | ||||
| Male | 3 | 4 | 2 | 4 |
| Female | 3 | 2 | 4 | 2 |
Sample comprises four parents and adolescents from the same family, two additional adolescents, and two additional parents.
Themes related to individuals' and caregivers' experiences, respectively, are illustrated in Figure 1 and Figure 2.
FIGURE 1.
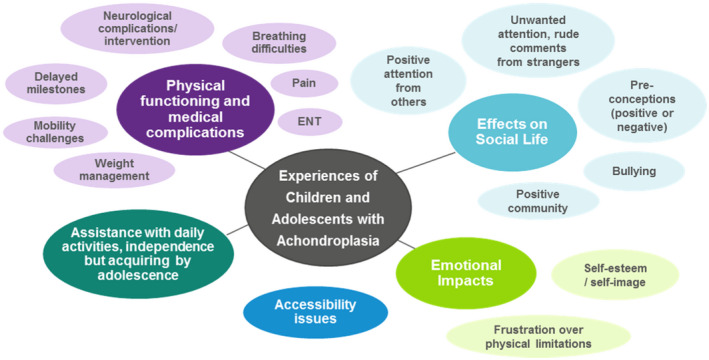
Themes and sub‐themes of experiences of children and adolescents with achondroplasia (ages 0–17 years). Bubble sizes are not reflective of frequency of mention
FIGURE 2.
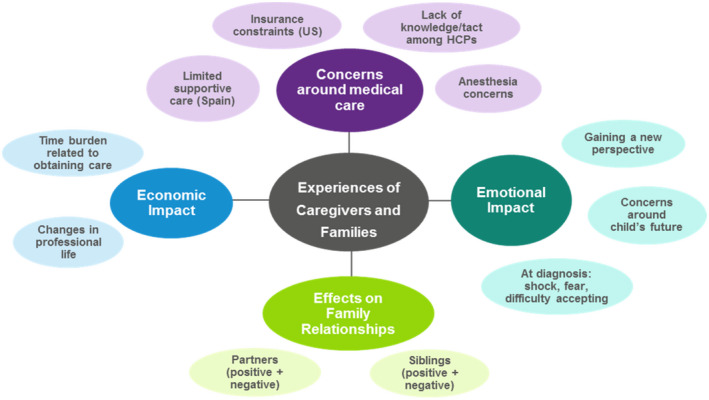
Themes and sub‐themes of caregivers' and families' experiences. Bubble sizes are not reflective of frequency of mention. HCPs, health care provider
3.2. Experiences of children and adolescents with achondroplasia, as reported by themselves and their caregivers
In describing results, we use the terms “children,” “adolescents,” or “individuals” to refer to, respectively, children, adolescents, or both children and adolescents with achondroplasia. The term “participants” applies to anyone who took part in focus groups or interviews directly, including the caregivers and adolescents with achondroplasia.
3.2.1. Physical functioning and related complications
All caregivers reported a delay in early physical developmental milestones, such as holding up the head, walking, crawling, and sitting up, and caregivers of all age groups discussed mobility limitations and challenges (e.g., balance issues that affect walking ability). Although all caregivers expected developmental delays, some expressed anxiety about delayed milestones. One caregiver shared, “…the doctors at [specialist center] kept saying ‘He's going to get there…’ I am looking at my…13‐month‐old who is not even sitting up, [thinking] ‘They're out of their mind. He's never going to do anything’….Then, all of a sudden, they do it.” Several caregivers noted how their children adapted movements to increase mobility, such as scooting with legs while not lifting up their head.
Participants reported physical complications of achondroplasia, such as stenosis/spinal compression, breathing and sleeping difficulties, pain, weight management, and otolaryngological issues. Spinal and neurological issues, such as kyphosis, foramen magnum compression, and stenosis, were noted for their severity and complexity, involving frequent medical appointments and surgical procedures, and were of particular concern to caregivers in their child's earlier years. Breathing and respiratory challenges of varying severity, including sleep apnea, hypopnea, and poor sleep quality, were frequently mentioned by caregivers, especially those of affected children aged 0–4 years.
Participants frequently reported pain that limited physical functioning and stamina. Pain was also associated with sitting without back support and being unable to bend the knees when sitting in a chair due to leg shortness. Pain, with the back the most common site, was most often discussed in the adolescent focus groups, with one adolescent describing backaches that “happen every day…[and] last for like 20 minutes.”
Management of weight and maintaining physical activity were described as challenges, with parental awareness of the issue starting at their child's young age and continuing throughout adolescence. Adolescents with achondroplasia also acknowledged challenges with weight control and the consequences of weight gain (e.g., additional pressure on the back and legs, and having a more difficult time losing weight compared to people of average stature).
Caregivers and adolescents described some otologic issues, and placement of ear tubes was a common medical intervention. Caregivers tended to view this as less concerning than other medical issues, but two caregivers reported moderate deafness and hearing loss.
3.2.2. Challenges and difficulties in acquiring independence in activities of daily living
Caregivers discussed the challenges and the need for more assistance with activities of daily living than their other children or peers. Caregivers and adolescents most frequently mentioned needing assistance with toileting, such as undressing and wiping. Several caregivers felt it was important to encourage independence early in life to help children learn to adapt. For example, a caregiver in Spain explained, “She likes to feel that we are helping her, and I think that's a bad thing.” Another caregiver in Spain shared their reaction when requested for assistance: “With ‘Can you help me with [wiping] my bottom?’…I say, ‘Son, please. I'm still going to be doing this after you are married at this rate.’” Difficulties with performing tasks related to personal hygiene, such as not easily being able to reach sinks or shower heads to wash, were noted as a challenge; however, participants also noted improvements with age. Participants also discussed the challenge of independently dressing, especially pulling up pants.
3.2.3. Accessibility challenges and adaptations
All participants spoke of modifications and adaptations made at home to increase accessibility, although the cost and level of modification varied. For example, one family had completely renovated a bathroom to accommodate their young child with achondroplasia, while other families simply acquired footstools and strategically arranged things, like storing dishes in lower kitchen cabinets.
Caregivers discussed the frustration related to lack of accessibility experienced by the younger children: “…she cannot reach the light switch or the doorbell, so she starts crying.” By adolescence, as individuals become more independent and home adaptations are in place, most challenges of accessibility are outside of the home (e.g., public bathrooms, hotels, restaurants, and grocery stores) and involve issues such as reaching sinks, doorbells, and elevator buttons. One adolescent described specific challenges at school: “Sometimes our lockers are pretty high [and] they are actually a little bit out of my reach…and also the school sinks are very high, too, so it's a little difficult to wash my hands.” Furthermore, adolescents frequently mentioned impacts on their social activities in public domains, such as being excluded from theme park rides due to height requirements or difficulty seeing over the crowd at concerts.
3.2.4. Social impacts of achondroplasia
A range of social experiences was described, from negative ones such as receiving rude comments and being bullied, to positive ones such as being popular at school due to their unique size.
Caregivers of children across all age groups discussed challenges in keeping up with peers athletically and how their children's physical limitations could cause exclusion from activities. One parent explained, “He's the only one that's a little person …For his size, he does great, but he's always the last person, always behind …It's hard at this age.” Other social impacts were not being invited to participate in activities.
Social impacts in school appeared to be minimal for some, while others reported incidents of bullying. A caregiver shared their child's struggle with the transition to high school and how they were treated: “I'm having to face something new that is happening to me. They think I'm deaf. I'm short, but not deaf. They whisper and point their finger at me.” Two children were reported to have enrolled in a different school due to bullying. One adolescent described the impact of bullying: “It started in elementary school and died down a bit. It follows me here. It still hurts.” Nearly all participants spoke of an increase in attention when starting school, especially from younger students. One parent shared how a teacher helped their child with achondroplasia by addressing and discussing differences with other students.
Many caregivers discussed their child receiving unwanted or special attention in public: “Walking down the street, and nobody said anything mean, nobody was nasty, but that constant attention on him. You can't walk past a person without them noticing.” Caregivers reported their child receiving special or unwanted attention from strangers, having to cope with stares, comments, and even, in extreme cases, asking for photographs. One adolescent shared how this increased attention affects them: “You've had a bad day, for example, and you go somewhere and have to put up with people staring.… It annoys me.” Caregivers spoke of building up the children's self‐esteem and working on developing skills to handle these situations.
Some participants experienced special attention as positive or an advantage. One adolescent stated, “It makes me stand out a little more, people remember me.” A caregiver reported that, while their child does not mind the attention, they did not like patronizing comments. They explained, “I think it's different for a girl for some reason. …. Everybody thinks she's so cute and everybody stops her in the halls, ‘you're so cute, you're like a doll.’ She hates that part, but she doesn't mind the attention at all.”
Participants noted that individuals with achondroplasia are often subjected to preconceived perceptions. While these included positive preconceived notions, negative perceptions were also prevalent, as described by one adolescent: “…. first impressions for us with people are different….Sometimes people automatically have a prejudice against us and don't like us before they know our names….Or, people make fun of us before they ever meet us, while other people are just people in their minds.”
Due to their height, individuals with achondroplasia were perceived to be younger than their true age or less capable than average stature individuals. The height difference was especially confusing for average stature young children in primary school. A parent of an adolescent girl shared that “… people naturally tend to think of her as being younger or less capable…In some instances, they want to help more, which can be good or bad….I think it's harder for her peers or for adults to see her as the same age as her peers because of her height.”
Despite some challenges in their local communities, all participants mentioned having support systems, including family, friends, and community members. Nearly all participants spoke of the importance of the support, guidance, and information provided by local achondroplasia organizations. Caregivers of older children voiced positive feelings about support organizations and events organized by these foundations. One parent shared how their child felt about ALPE: “It's such a normal thing. It's like he has another large family; he says, ‘I've got my family and then I've got my ALPE family.’”
3.2.5. Emotional effects of living with achondroplasia
The negative emotional impacts of living with achondroplasia included hurt feelings, loss of self‐esteem, and frustration or anger. One caregiver described how their adolescent child struggles with achondroplasia: “She says ‘I know some children have cancer and other diseases, but I have the only condition that is funny, laughable, and people point out and make fun at you’….It's hard to live your daily life with a burden on you from the day you are born.” Adolescents discussed self‐esteem and the psychological impacts of having to deal with stares and unwanted attention from strangers in public: “…When people stare or make comments or call me a mean name or things, it makes me feel bad.”
For the youngest age group, 0–4 years, feelings of frustration appear to stem from physical limitations and the beginning of comparing their abilities to their peers. In Spain, caregivers reported that their children felt frustrated and angry when they were unable to reach items, such as door handles, light switches, and the intercom.
3.3. Decision‐making and perceptions of limb lengthening treatment
Among the Spanish adolescents, two had already undergone limb lengthening surgery, two were currently considering surgery, and two had decided not to have surgery. The two adolescents who had undergone limb‐lengthening surgery acknowledged the pain and challenges of recovery including the frequency of heparin injections, difficulty of wound dressings, and long period of limited mobility while recovering, including spending a year in a wheelchair and missing school. One adolescent spoke positively about the results of surgery, especially the gain in stature, and explained “I thought about it and said ‘Let's do it.’ But I have always known that I would have surgery since I was young.” A parent shared their child's rationale for the surgery: “My daughter's motto is that she prefers to spend three or four bad years of her life because of the lengthening, but then she enjoys it for the rest of her life.” The two adolescents who had completed the surgery reported greater independence in daily activities, such as the ability to reach items or maintain personal hygiene.
In the US groups, none of the participants or their children had undergone or considered undergoing limb lengthening surgery, which was generally perceived as intrusive, extremely painful, requiring a long recovery, and unnecessarily risky.
3.4. Experiences of caregivers and families
3.4.1. Concerns around access to appropriate medical care
Challenges and concerns regarding their child's medical care were the most discussed parental impact theme. Caregivers frequently mentioned a lack of confidence in providers, the challenge of accessing specialist care, and the economic burden of medical care.
In both countries, participants voiced concern about medical providers' lack of knowledge. Caregivers also reported a wide range of providers' efforts to gain or ensure they had appropriate knowledge and understanding of achondroplasia. Several caregivers voiced frustration with their pediatrician's lack of effort in learning more, for example: “He's almost 3 and I can't believe how they still don't know anything. [I'm thinking] ‘Can anyone Google this? I mean, I figured it out.” In Spain, two mothers shared experiences of medical providers suggesting termination in a tactless manner upon learning of the achondroplasia diagnosis in utero.
Participants reported concerns regarding the associated risks of anesthesia and the lack of knowledge and experience of anesthesiologists working with individuals with achondroplasia. A few caregivers voiced the need to question the anesthesiologist before the surgery to ensure they were aware of the potential complications of administering anesthesia to children with achondroplasia.
Many participants reported that access to care was a challenge. In Spain, caregivers reported having access to supportive care up to a certain age, though some reported struggling to get referrals to appropriate specialists. In the US, participants reported lack of access due to insurance constraints (not being covered) and location, with some reporting traveling hours to see specialists.
3.4.2. Economic impact
Caregivers discussed the indirect costs due to the amount of time needed to ensure their affected child received the necessary medical care, including time spent on the phone with insurance companies, getting second and third opinions from different providers, and attending frequent medical appointments.
Some caregivers reported modifying their work schedule or the need for flexibility to accommodate the numerous medical appointments required in the early years of achondroplasia. A few caregivers in the US discussed the challenge of finding competent care for their children so they can return to work, with two mothers choosing to stay home to care for their child. A caregiver in the US noted that, despite a desire to stay home, she returned to her work when her child with achondroplasia was born to ensure health insurance coverage.
3.4.3. Effects of achondroplasia on family relationships
Caregivers reported that having a child with achondroplasia could strain their marriage or partnership. Some caregivers discussed the challenges that arose specifically during the child's early years, with disagreements regarding treatment and supportive services or groups, while others noted stress arising from having a child who is in pain.
Caregivers discussed the negative and positive impacts of having a child with achondroplasia on the family. Some caregivers reported that siblings felt jealous and struggled with the amount of attention the child with achondroplasia received. Other participants remarked about the bond between siblings, reporting that their average stature children are protective of their sibling with achondroplasia. Caregivers also reported that having a child with achondroplasia strengthened the family bond.
3.4.4. Emotional effects on caregivers
Upon learning their child's diagnosis, caregivers most often reported feelings of denial and fear but also reported feeling guilt, shock, worry, isolation, grief, and anger. One caregiver described her initial denial: “I denied it until the labor. I was saying, ‘It doesn't matter if [the doctors] are eminences because they are wrong.’” Another explained their initial fear and how they adapted: “…from what the doctors told me at first, I was very terrified, honestly, and I was afraid that all these things were going to go wrong. I suppose part of it is getting used to the rhythm of raising a kid with achondroplasia. But now…we have medical issues sometimes, but they're not things that we can't handle.”
Caregivers discussed future concerns that they had for their children, most frequently mentioning medical issues and complications. A few caregivers voiced concerns about having to decide whether to pursue potential new drug treatments at a young age, with one explaining, “…What if she turns to me and tells me ‘Why didn't you try, mom?’ or the opposite, ‘[Why didn't you] embrace [my short stature]?’” Other future concerns were related to social impacts, romantic relationships, employment, and general worries about quality of life.
Caregivers also described positive emotional impacts of having a child with achondroplasia and shared how they learned to appreciate life in a different way, for example, “My life has changed. I am convinced that it's been for the better.”
4. DISCUSSION
This first qualitative study involving both children and adolescents with achondroplasia and their caregivers provides a rich narrative of the challenges of living with achondroplasia in the US and Spain. Although the physical impacts of achondroplasia noted by study participants, including delayed milestones, limitations in mobility and physical functioning, accessibility barriers and the need for assistance, adaptations, and accommodations, and medical complications, have been described previously in the literature (Alade et al., 2013; Hoover‐Fong et al., 2021; Ireland et al., 2011; Pfeiffer et al., 2021a; Thompson et al., 1999; Wigg et al., 2016), this study uniquely captured the frustration, anxiety, and unmet needs of patients and caregivers in addressing these physical challenges. While the negative social and emotional experiences of affected children and the burden on caregivers highlighted in previous studies were mirrored and expanded upon in our study findings, it was new to hear participants describe examples of positive attention received by children and adolescents with achondroplasia in social/school settings, and the ways in which having a child with achondroplasia can enhance familial bonds and the lives of caregivers. In concert, these study findings—voiced directly by individuals affected by achondroplasia and their caregivers—provide important context for understanding the complex and varied impacts of achondroplasia.
This study adds to the sparse literature on the quality of life of caregivers of children and adolescents with achondroplasia. Similar to findings reported by Pfeiffer et al. (2021b), caregivers in the present study reported experiencing concern for their child's emotional and social well‐being, their child's ability to function independently, the health and safety of their child, and future implications. In addition, they reported challenges in navigating the medical system and seeking appropriate care, advocating for their child, and monitoring their child's health. This study demonstrates evidence of bureaucratic and physical barriers to accessing care for children with achondroplasia. Reasons for the challenges related to health care access differed between the two countries, reflecting the difficulties of two different healthcare systems. Caregivers in Spain reported difficulty accessing specialists after their child reached a certain age, while those in the US reported insurance and location constraints for accessing providers far from home. Moreover, this study provides a narrative description of caregivers' experiences with pediatricians and other specialists, highlighting lack of knowledge and experience with achondroplasia.
Our results demonstrate differences in preferences and practices across countries. In particular, the opposition to limb lengthening expressed by US caregivers, which was in contrast to broader acceptance in Spain, has not been described in previous research on this topic (Balci et al., 2015; Kim, Agashe, et al., 2012; Kim, Balce, et al., 2012; Leiva‐Gea et al., 2020). As new and less invasive treatment modalities become available (Legeai‐Mallet & Savarirayan, 2020; Savarirayan et al., 2019; Savarirayan et al., 2020), it will be important to understand how these treatments are perceived by caregivers in different countries and whether these treatments positively affect the quality of life, in terms of both physical and socio‐emotional functioning.
Our findings underscore the importance of routine psychosocial assessments and the provision of psychosocial support for those directly and indirectly impacted by achondroplasia. A number of instruments have been used to assess outcomes in individuals with achondroplasia (Hoover‐Fong et al., 2021); to date, the Quality of Life in Short Stature Youth (QoLISSY) and the Pediatric Quality of Life Inventory (PedsQL™) are the only outcome tools for children that have been demonstrated to be reliable and valid in a cross‐cultural context (Bloemeke et al., 2019). Participation in patient organizations has a positive impact on HRQoL, a finding that is consistent with those from other studies. (Pfeiffer et al., 2021a; Witt et al., 2017).
The main limitation of this study was a relatively small sample size located in two countries, which limits the generalizability of findings. However, our sample is diverse in terms of age and sex of individuals with achondroplasia and geographic regions within the United States. As we conducted only one focus group per age group in each country, it was not possible to assess data saturation; however, the themes and perspectives reported by the same age groups in different countries were similar and verified by the caregivers. The structure of focus groups made it difficult to accurately quantify the frequency of impacts; instead, we provided an indication of prevalence of experiences but focused primarily on qualitative descriptions of important concepts.
5. CONCLUSION
Study results provide a rich description of the multifaceted impacts of achondroplasia on the quality of life of affected children of varying ages and their families. Despite describing significant physical and socio‐emotional challenges of living with achondroplasia, individuals, and caregivers also discussed positive aspects of achondroplasia and highlighted the importance of an accepting and supportive community. Insights and themes from this study could be further explored in larger qualitative and quantitative studies.
CONFLICT OF INTEREST
R. Shediac, J. Quinn, and D. Kelly are employees and shareholders of BioMarin Pharmaceutical Inc. J. Hoover‐Fong has received consulting fees from BioMarin, Therachon, and Ascendis, and grants from BioMarin. K. Mohnike has received honoraria from Biomarin, Kyowa Kirin, and Novo Nordisk and is a consultant for QED and investigator for Biomarin and Pfizer. R. Savarirayan has received consulting fees and grants from BioMarin, and consulting fees from Ascendis, QED, and Pfizer.
AUTHOR CONTRIBUTIONS
R. Shediac, D. Kelly, J. Quinn, O. Moshkovich, and R. Ballinger were involved in the conception and design of the study. O. Moshkovich, R. Ballinger, H. Gerould, A. Williams, and M. A. Bellenger were involved in the acquisition and analysis of the data. R. Shediac, D. Kelly, J. Quinn, O. Moshkovich, R. Ballinger, J. Hoover‐Fong, K. Mohnike, and R. Savarirayan were involved in the interpretation of the data. All authors were involved in drafting and revising the manuscript.
ETHICS
The study was approved by a central institutional review board, Salus IRB (Austin, TX, USA). Informed consent was obtained for each participant prior to the focus groups; adolescent participants, who were consented to by their caregivers, also provided assent.
DATA AVAILaBILITY STATEMENT
The de‐identified individual participant data that underlie the results reported in this article (including text, tables, figures, and appendices) will be made available together with the research protocol and data dictionaries, for non‐commercial, academic purposes. Additional supporting documents may be available upon request. Investigators will be able to request access to these data and supporting documents via a data‐sharing portal beginning 6 months and ending 2 years after publication. Data associated with any ongoing development program will be made available within 6 months after approval of relevant product. Requests must include a research proposal clarifying how the data will be used, including proposed methods of data analysis. Research proposals will be evaluated relative to publicly available criteria available at www.BioMarin.com/patients/publication‐data‐request/ to determine if access will be given, contingent upon execution of a data access agreement with BioMarin Pharmaceutical Inc.
ACKNOWLEDGMENTS
We thank all study participants for their time and willingness to share their experiences and views.
Shediac, R. , Moshkovich, O. , Gerould, H. , Ballinger, R. , Williams, A. , Bellenger, M. A. , Quinn, J. , Hoover‐Fong, J. , Mohnike, K. , Savarirayan, R. & Kelly, D. (2022). Experiences of children and adolescents living with achondroplasia and their caregivers. Molecular Genetics & Genomic Medicine, 10, e1891. 10.1002/mgg3.1891
REFERENCES
- Adler, K. , Salanterä, S. , & Zumstein‐Shaha, M. (2019). Focus group interviews in child, youth, and parent research: An integrative literature review. International Journal of Qualitative Methods, 18, 160940691988727. 10.1177/1609406919887274 [DOI] [Google Scholar]
- Alade, Y. , Tunkel, D. , Schulze, K. , McGready, J. , Jallo, G. , Ain, M. , Yost, T. , & Hoover‐Fong, J. (2013). Cross‐sectional assessment of pain and physical function in skeletal dysplasia patients. Clinical Genetics, 84(3), 237–243. 10.1111/cge.12045 [DOI] [PubMed] [Google Scholar]
- Balci, H. I. , Kocaoglu, M. , Sen, C. , Eralp, L. , Batibay, S. G. , & Bilsel, K. (2015). Bilateral humeral lengthening in achondroplasia with unilateral external fixators: Is it safe and does it improve daily life? The Bone & Joint Journal, 97‐b(11), 1577–1581. 10.1302/0301-620x.97b11.36037 [DOI] [PubMed] [Google Scholar]
- Bloemeke, J. , Sommer, R. , Witt, S. , Bullinger, M. , Nordon, C. , Badia, F. J. , González, F. L. , Leiva‐Gea, A. , Delgado Rufino, F. B. , Mayoral‐Cleries, F. , Romero‐Sanchiz, P. , Clamagirand Saiz, V. , Nogueira‐Arjona, R. , Mohnike, K. , & Quitmann, J. (2019). Cross‐cultural selection and validation of instruments to assess patient‐reported outcomes in children and adolescents with achondroplasia. Quality of Life Research, 28(9), 2553–2563. 10.1007/s11136-019-02210-z [DOI] [PubMed] [Google Scholar]
- Bullinger, M. , Quitmann, J. , Power, M. , Herdman, M. , Mimoun, E. , DeBusk, K. , Feigerlova, E. , Lunde, C. , Dellenmark‐Blom, M. , Sanz, D. , Rohenkohl, A. , Pleil, A. , Wollmann, H. , & Chaplin, J. E. (2013). Assessing the quality of life of health‐referred children and adolescents with short stature: Development and psychometric testing of the QoLISSY instrument. Health and Quality of Life Outcomes, 11, 76. 10.1186/1477-7525-11-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhiman, N. , Albaghdadi, A. , Zogg, C. K. , Sharma, M. , Hoover‐Fong, J. E. , Ain, M. C. , & Haider, A. H. (2017). Factors associated with health‐related quality of life (HRQOL) in adults with short stature skeletal dysplasias. Quality of Life Research, 26(5), 1337–1348. 10.1007/s11136-016-1455-7 [DOI] [PubMed] [Google Scholar]
- Foreman, P. K. , van Kessel, F. , van Hoorn, R. , van den Bosch, J. , Shediac, R. , & Landis, S. (2020). Birth prevalence of achondroplasia: A systematic literature review and meta‐analysis. American Journal of Medical Genetics. Part A, 182(10), 2297–2316. 10.1002/ajmg.a.61787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredwall, S. O. , Maanum, G. , Johansen, H. , Snekkevik, H. , Savarirayan, R. , & Lidal, I. B. (2020). Current knowledge of medical complications in adults with achondroplasia: A scoping review. Clinical Genetics, 97(1), 179–197. 10.1111/cge.13542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser, B. G. , & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for qualitative research. Aldine. [Google Scholar]
- Gollust, S. E. , Thompson, R. E. , Gooding, H. C. , & Biesecker, B. B. (2003). Living with achondroplasia in an average‐sized world: An assessment of quality of life. American Journal of Medical Genetics. Part A, 120A(4), 447–458. 10.1002/ajmg.a.20127 [DOI] [PubMed] [Google Scholar]
- Hoover‐Fong, J. , Cheung, M. S. , Fano, V. , Hagenas, L. , Hecht, J. T. , Ireland, P. , Irving, M. , Mohnike, K. , Offiah, A. C. , Okenfuss, E. , Ozono, K. , Raggio, C. , Tofts, L. , Kelly, D. , Shediac, R. , Pan, W. , & Savarirayan, R. (2021). Lifetime impact of achondroplasia: Current evidence and perspectives on the natural history. Bone, 146, 115872. 10.1016/j.bone.2021.115872 [DOI] [PubMed] [Google Scholar]
- Horton, W. A. , Hall, J. G. , & Hecht, J. T. (2007). Achondroplasia. The Lancet, 370(9582), 162–172. 10.1016/s0140-6736(07)61090-3 [DOI] [PubMed] [Google Scholar]
- Ireland, P. J. , McGill, J. , Zankl, A. , Ware, R. S. , Pacey, V. , Ault, J. , Savarirayan, R. , Sillence, D. , Thompson, E. M. , Townshend, S. , & Johnston, L. M. (2011). Functional performance in young Australian children with achondroplasia. Developmental Medicine and Child Neurology, 53(10), 944–950. 10.1111/j.1469-8749.2011.04050.x [DOI] [PubMed] [Google Scholar]
- Joffe, H. , & Yardley, L. (2004). Content and thematic analysis, in research methods for clinical and health psychology. SAGE. [Google Scholar]
- Kim, S. J. , Agashe, M. V. , Song, S. H. , Choi, H. J. , Lee, H. , & Song, H. R. (2012). Comparison between upper and lower limb lengthening in patients with achondroplasia: A retrospective study. Journal of Bone and Joint Surgery. British Volume (London), 94(1), 128–133. 10.1302/0301-620x.94b1.27567 [DOI] [PubMed] [Google Scholar]
- Kim, S. J. , Balce, G. C. , Agashe, M. V. , Song, S. H. , & Song, H. R. (2012). Is bilateral lower limb lengthening appropriate for achondroplasia?: Midterm analysis of the complications and quality of life. Clinical Orthopaedics and Related Research, 470(2), 616–621. 10.1007/s11999-011-1983-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzinger, J. (1995). Qualitative Research. Introducing Focus Groups. BMJ, 311(7000), 299–302. 10.1136/bmj.311.7000.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legeai‐Mallet, L. , & Savarirayan, R. (2020). Novel therapeutic approaches for the treatment of achondroplasia. Bone, 141, 115579. 10.1016/j.bone.2020.115579 [DOI] [PubMed] [Google Scholar]
- Leiva‐Gea, A. , Delgado‐Rufino, F. B. , Queipo‐de‐Llano, A. , Mariscal‐Lara, J. , Lombardo‐Torre, M. , & Luna‐Gonzalez, F. (2020). Staged upper and lower limb lengthening performing bilateral simultaneous surgery of the femur and tibia in achondroplastic patients. Archives of Orthopaedic and Trauma Surgery, 140(11), 1665–1676. 10.1007/s00402-020-03360-3 [DOI] [PubMed] [Google Scholar]
- Mahomed, N. N. , Spellmann, M. , & Goldberg, M. J. (1998). Functional health status of adults with achondroplasia. American Journal of Medical Genetics, 78(1), 30–35. [DOI] [PubMed] [Google Scholar]
- Matsushita, M. , Kitoh, H. , Mishima, K. , Yamashita, S. , Haga, N. , Fujiwara, S. , Ozono, K. , Kubota, T. , Kitaoka, T. , & Ishiguro, N. (2019). Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcified Tissue International, 104(4), 364–372. 10.1007/s00223-019-00518-z [DOI] [PubMed] [Google Scholar]
- Pauli, R. M. (2019). Achondroplasia: A comprehensive clinical review. Orphanet Journal of Rare Diseases, 14(1), 1. 10.1186/s13023-018-0972-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer, K. M. , Brod, M. , Smith, A. , Gianettoni, J. , Viuff, D. , Ota, S. , & Charlton, R. W. (2021a). Assessing physical symptoms, daily functioning, and well‐being in children with achondroplasia. American Journal of Medical Genetics. Part A, 185(1), 33–45. 10.1002/ajmg.a.61903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer, K. M. , Brod, M. , Smith, A. , Gianettoni, J. , Viuff, D. , Ota, S. , & Charlton, R. W. (2021b). Assessing the impacts of having a child with achondroplasia on parent well‐being. Quality of Life Research, 30(1), 203–215. 10.1007/s11136-020-02594-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savarirayan, R. , Irving, M. , Bacino, C. A. , Bostwick, B. , Charrow, J. , Cormier‐Daire, V. , le Quan Sang, K. H. , Dickson, P. , Harmatz, P. , Phillips, J. , Owen, N. , Cherukuri, A. , Jayaram, K. , Jeha, G. S. , Larimore, K. , Chan, M. L. , Huntsman Labed, A. , Day, J. , & Hoover‐Fong, J. (2019). C‐type natriuretic peptide analogue therapy in children with achondroplasia. The New England Journal of Medicine, 381(1), 25–35. 10.1056/NEJMoa1813446 [DOI] [PubMed] [Google Scholar]
- Savarirayan, R. , Tofts, L. , Irving, M. , Wilcox, W. , Bacino, C. A. , Hoover‐Fong, J. , Ullot Font, R. , Harmatz, P. , Rutsch, F. , Bober, M. B. , Polgreen, L. E. , Ginebreda, I. , Mohnike, K. , Charrow, J. , Hoernschemeyer, D. , Ozono, K. , Alanay, Y. , Arundel, P. , Kagami, S. , … Day, J. (2020). Once‐daily, subcutaneous vosoritide therapy in children with achondroplasia: A randomised, double‐blind, phase 3, placebo‐controlled, multicentre trial. Lancet, 396(10252), 684–692. 10.1016/s0140-6736(20)31541-5 [DOI] [PubMed] [Google Scholar]
- Savarirayan, R. , Ireland, P. , Irving, M. , Thompson, D. , Alves, I. , Baratela, W. A. R. , Betts, J. , Bober, M. B. , Boero, S. , Briddell, J. , Campbell, J. , Campeau, P. M. , Carl‐Innig, P. , Cheung, M. S. , Cobourne, M. , Cormier‐Daire, V. , Deladure‐Molla, M. , Pino, M. , Elphick, H. , … Fredwall, S. O. (2021). International consensus statement on the diagnosis, multidisciplinary management and lifelong care of individuals with achondroplasia. Nature Reviews Endocrinology, 1–17. 10.1038/s41574-021-00595-x. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Slomine, B. (2011). Functional Independence measure for children. In Kreutzer J. S., DeLuca J., & Caplan B. (Eds.), Encyclopedia of clinical neuropsychology. Springer. 10.1007/978-0-387-79948-3_1607 [DOI] [Google Scholar]
- Software, V. (2020). MAXQDA. VERBI GmbH. [Google Scholar]
- Thompson, N. M. , Hecht, J. T. , Bohan, T. P. , Kramer, L. A. , Davidson, K. , Brandt, M. E. , & Fletcher, J. M. (1999). Neuroanatomic and neuropsychological outcome in school‐age children with achondroplasia. American Journal of Medical Genetics, 88(2), 145–153. [DOI] [PubMed] [Google Scholar]
- Varni, J. W. , Seid, M. , & Kurtin, P. S. (2001). PedsQL™4.0: Reliability and validity of the pediatric quality of life inventory™ version 4.0 generic core scales in healthy and patient populations. Medical Care, 39, 800–812. 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- Wigg, K. , Tofts, L. , Benson, S. , & Porter, M. (2016). The neuropsychological function of children with achondroplasia. American Journal of Medical Genetics. Part A, 170(11), 2882–2888. 10.1002/ajmg.a.37779 [DOI] [PubMed] [Google Scholar]
- Witt, S. , Kolb, B. , Bloemeke, J. , Mohnike, K. , Bullinger, M. , & Quitmann, J. (2019). Quality of life of children with achondroplasia and their parents—A German cross‐sectional study. Orphanet Journal of Rare Diseases, 14(1), 194. 10.1186/s13023-019-1171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt, S. , Rohenkohl, A. , Bullinger, M. , Sommer, R. , Kahrs, S. , Klingebiel, K. H. , Klingebiel, R. , & Quitmann, J. (2017). Understanding, assessing and improving health‐related quality of life of young people with achondroplasia—A collaboration between a patient organization and academic medicine. Pediatric Endocrinology Reviews, 15(Suppl 1), 109–118. 10.17458/per.vol15.2017.wrm.improvinghealthrelatedquality [DOI] [PubMed] [Google Scholar]
- Yonko, E. A. , Emanuel, J. S. , Carter, E. M. , & Raggio, C. L. (2021). Quality of life in adults with achondroplasia in the United States. American Journal of Medical Genetics Part A, 185(3), 695–701. 10.1002/ajmg.a.62018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The de‐identified individual participant data that underlie the results reported in this article (including text, tables, figures, and appendices) will be made available together with the research protocol and data dictionaries, for non‐commercial, academic purposes. Additional supporting documents may be available upon request. Investigators will be able to request access to these data and supporting documents via a data‐sharing portal beginning 6 months and ending 2 years after publication. Data associated with any ongoing development program will be made available within 6 months after approval of relevant product. Requests must include a research proposal clarifying how the data will be used, including proposed methods of data analysis. Research proposals will be evaluated relative to publicly available criteria available at www.BioMarin.com/patients/publication‐data‐request/ to determine if access will be given, contingent upon execution of a data access agreement with BioMarin Pharmaceutical Inc.


