Abstract
Objective:
We examined users’ preferences for and engagement with text messages delivered as part of an emergency department (ED)-based intervention to improve antihypertensive medication adherence.
Methods:
We recruited ED patients with elevated blood pressure for a pilot randomized trial evaluating a medication adherence intervention with text messages. Intervention participants chose text content and frequency, received texts for 45 days, and completed a feedback survey. We defined engagement via responses to texts. We examined participant characteristics associated with text preferences, engagement, and feedback.
Results:
Participants (N=101) were 57% female and 46% non-White. Most participants (71%) chose to receive both reminder and informational texts; 94% chose reminder texts once per day and 97% chose informational texts three times per week. Median text message response rate was 56% (IQR 26–80%). Participants who were Black (p<0.01), had lower income (p=0.03), or had lower medication adherence (p<0.01) rated the program as more helpful and wanted additional functionalities for adherence support.
Conclusions and Practice Implications:
While overall engagement was modest, participants at risk of worse health outcomes expressed more value and interest in the program. Findings inform the design of text messaging interventions for antihypertensive medication adherence and support targeting vulnerable patients to reduce health disparities.
Keywords: Patient preference, patient engagement, text messages, behavioral intervention, hypertension, medication adherence, health disparities
1. Introduction
Nearly half of U.S. adults (108 million) have hypertension, and only about 1 in 4 of these adults have adequate blood pressure control using a threshold of <140/ 90mm Hg [1]. Recent data show both a rise in the prevalence of hypertension and a decrease in the prevalence of controlled blood pressure [2, 3]. Hypertension is associated with an increased risk of serious health problems including stroke, heart failure, and kidney disease [4]. Adherence to antihypertensive medications is necessary to achieve blood pressure control and reduce the risk of adverse events [5]. However, medication nonadherence is common [6, 7], and is thought to be a major contributor to worse blood pressure control in non-Hispanic Blacks compared to other racial groups [8–10]. Common barriers to antihypertensive medication adherence include beliefs about hypertension and its treatment, complexity and cost of medication regime, and competing priorities [11–13].
Text message-delivered interventions are a promising solution to improve antihypertensive medication adherence among all patients [14]. Text messages reach patients in their daily lives where self-care occurs and can provide adherence information, motivation, and reminders. These behavioral interventions are not intended to replace or undermine the patient-provider relationship [15], but rather complement it and provide adherence support in-between clinic visits. Although the digital divide persists with respect to Internet access and smartphone ownership [16], over 96% of U.S. adults own a mobile phone with text messaging capabilities, and texting is the most common mobile phone activity among all phone users [17, 18]. A growing number of studies are using text messages to target medication adherence; however, evidence for the efficacy of text messaging on clinical outcomes is mixed [19, 20]. One reason for the inconsistent results could be due to differences in patients’ preferences for and engagement with these interventions.
In general, there is strong support for the acceptance of text messaging interventions across a wide variety of patient populations [19, 21]; however, more nuanced information on patients’ preferences for how content is delivered and associations with participant characteristics is limited. Asking users about their preferences is critical to informing the types of design elements to include and the types of patients for whom the intervention may be best suited [22]. In addition, user engagement with the intervention can signify its potential to impact outcomes [23, 24], but few studies report on engagement with texting interventions, specifically for antihypertensive medication adherence. Among the studies reporting on engagement in other disease contexts, text message response rates vary widely which could be explainable by variation in participant-specific attributes [25].
Despite the potential for text message-delivered interventions to improve antihypertensive medication adherence, there is limited information on patients’ perspectives of these interventions. Notably, few studies have examined perspectives among racially diverse patients with hypertension, who stand to benefit considerably from such an intervention [8]. We sought to explore patients’ preferences for and engagement with text messages delivered as part of an emergency department (ED)-based behavioral intervention designed to support antihypertensive medication adherence. We examined patient characteristics associated with users’ preferences for, engagement with, and feedback on the text messages.
2. Methods
2.1. Study Design, Setting, and Eligibility
This study was conducted as part of a pilot randomized trial evaluating the effects of an ED-based behavioral intervention designed to improve antihypertensive medication adherence and blood pressure called the Vanderbilt Emergency Room Bundle (VERB) study. For these analyses, we use data from participants who were randomly assigned to the intervention.
Between February 25, 2016 and January 15, 2018, participants enrolled during an ED visit at Vanderbilt University Medical Center (VUMC) or the Veterans Affairs-Tennessee Valley Healthcare System (VA-TVHS), which are both located in Nashville, Tennessee. Eligible participants were adults between 21 and 84 years of age who were prescribed at least one antihypertensive medication, had an initial ED systolic blood pressure (SBP) ≥140 mm Hg, and were expected to be discharged from the ED rather than hospitalized, according to their ED attending physician. Eligible patients also had to have a phone with texting capability and be willing to receive text messages. Patients who sought care for conditions that contribute to elevated blood pressure (e.g., delirium tremens and acute stroke) were not eligible.
2.2. Procedure
The Vanderbilt University and VA-TVHS institutional review boards approved all study procedures. Research Assistants (RAs) performed initial eligibility screenings of all patients as they arrived in the ED via an electronic whiteboard. Potentially eligible patients were then approached in-person by RAs for additional screening within six hours of the start of ED care. After confirming eligibility and obtaining written informed consent, RAs administered enrollment surveys. All data were collected verbally by RAs, recorded on paper case report forms, and later entered into Research Electronic Data Capture (REDCap) [26].
Participants were randomized 1:1 to VERB or an active control group. VERB is a multicomponent behavioral intervention that included motivational interviewing, an educational toolkit, text messaging, and pharmacy resources all designed to help patients improve their antihypertensive medication adherence. Motivational interviews were conducted and recorded by trained RAs. Using a patient-centered approach, RAs used reflective listening and supportive communication to help participants identify a barrier to medication adherence; if a barrier was identified, it was included as part of the educational toolkit. The toolkit, motivational interviewing, and pharmacy resources were all provided while participants were in the ED. Participants received their first text message (a welcome text) while in the ED and then continued to receive text messages for 45 days after ED discharge. This study focuses on the text message component of the intervention.
Follow-up data were collected at 1-month and 3-months post-enrollment and included an in-person feedback survey that asked about the helpfulness of the intervention. Participants were compensated up to $50 for completing all the study measures; there was no compensation for receiving or responding to text messages.
2.3. Text Messages
Text messages were delivered through Knock, a patient text messaging syndication system developed at VUMC [27]. In addition to a welcome and closing message, participants chose to receive reminder and/or informational text messages. Reminder texts asked the participant if he/she had taken their medicine. Informational texts provided general tips and information about medication adherence and blood pressure. If participants chose to receive reminder texts, they were given the option to receive them either once or twice daily; they also specified the time(s) of day and days of the week to receive messages. If participants chose to receive informational text messages, they were given the option to receive them every three days or once per week and specified the time of day to receive the texts. Table 1 summarizes the types of text messages, example content, and options for frequency and timing.
Table 1.
VERB text message content, frequency, and options
| Type of message | Content | Frequency | Option to choose timing |
|---|---|---|---|
|
| |||
| Welcome Message | “Hello from your VERB Research Team: We are excited to get started - your help with this study is very important!” | Once, at enrollment | No |
| Reminder Messages | “Hello from your VERB Team: Have you taken your medicine today?” | Daily or twice daily | Yes |
| Informational Messages* | “Hello from your VERB Team with tips for taking medicine: Some pharmacies can do automatic refills or refill reminders - ask your pharmacist for programs that may work for you.” | Three times per week or weekly | Yes |
| “Hello from your VERB Team: Did you know that 3 out of 4 Americans say they do not always take their medicines correctly? Usually they say it’s because of more than one reason. Visit http://www.scriptyourfuture.org/faqs-2/ to learn more.” | |||
| “Hello from your VERB Team with tips for taking medicine: Sometimes it is helpful to have a ‘Plan B Routine’ for taking your medicines. Family and friends can also help with reminders to take medicine.” | |||
| End message | “Hello from your VERB Research Team: This is the last message - thank you for your important help with this study! We look forward to seeing you at the next study visit.” | Once, 5 minutes after last scheduled reminder or informational message | No |
Example message content
After January 4, 2017, functionality was developed to record confirmation of text message receipt. From that date going forward, text messages ended with a request for confirmation that read: “Reply with ‘Y’ to let us know you got this message. Thank you!” Knock was designed to register all acceptable responses to the request for confirmation, including “Y,” “yes,” “yeah,” “yep,” “1,” and “si” and was not case sensitive. If a participant responded with something other than an acceptable response, he/she received a text message that read: “Sorry, we didn’t understand that…could you respond with “Y” or “1” to let us know you received the message?” If multiple texts were delivered on the same day, a response to a specific text was only recorded if it was sent before another text was delivered. If a participant wanted to stop receiving text messages at any time, he/she could text “STOP.”
2.4. Baseline Measures
Demographics Characteristics.
We collected self-reported age, gender, race, education (years in school), income, and insurance.
Psychosocial Factors.
Participants completed self-reported measures of health literacy (Brief Health Literacy Screen [28]), numeracy (Subjective Numeracy Scale, 3-item version [29]), perceived health competence (Perceived Health Competence Scale-2 [30], and depressive symptoms (Patient Health Questionnaire-2) [31].
Medication Adherence.
Participants also completed self-reported measure of medication adherence (Adherence to Refills and Medications Scale-7 item version [32]).
Text Message Engagement.
We defined engagement as a response to the request for confirmation included at the end of the text messages. We calculated text message response rates by dividing each participant’s number of responses by the total number of texts he/she received.
Text Message Feedback.
Follow-up surveys included close-ended, yes/no items assessing the utility of the text messages and preferences for text message functionality. A Likert-type item assessed the helpfulness of the text messages. Response options ranged from 1 = “not at all” to 5 = “a lot” (Table 1).
2.5. Analyses
Statistical analyses were performed using R version 4.0.3. and IBM SPSS Statistics version 26. To describe patient characteristics, we used means and standard deviations (SD) for continuous variables and absolute/relative frequencies for discrete variables. We examined participant interactions with the text message intervention through three lenses: chosen text message type and frequency, text message engagement, and text feedback. For all analyses, statistical significance was determined to be achieved at the nominal α = 0.05 level (two-sided).
2.5.1. Chosen text message type and frequencies
We used frequencies and percentages to describe chosen text types (i.e., reminder and informational) and frequencies. We also used kernel density plots to examine the distribution in participants’ selected time of day to receive the texts based on their chosen text type and frequency. We used Mann–Whitney U tests or chi-square tests, as appropriate, to explore bivariate associations between participants’ characteristics and their chosen text types and text frequencies. Patient characteristics included demographics and clinical characteristics (age, gender, enrollment site [VUMC vs VA], race [Black vs White], education, income, insurance [private/work-related vs government]), baseline psychosocial factors (health literacy, numeracy, and perceived health competence), and baseline self-reported medication adherence. For race, specifically, we focused on comparisons between Black and White participants because there too few participants in the other race categories.
2.5.2. Text message engagement
We estimated the mean, median, and first/third quartiles of text message response rates. For all engagement analyses, we excluded the first 5 days to mitigate the impact of participants’ acclimation to the intervention (i.e., learning curve). Participants who withdrew after starting the intervention were coded as having a nonresponse from the day they withdrew through 45 days.
We used logistic regression to examine variations in response rate. Specifically, we examined whether there was a time trend in the odds of responding over the 45-day intervention. The time-trend analysis used generalized estimating equations (GEE) to fit the model under a working independence correlation structure to account for repeated outcome measures and utilized a restricted cubic spline on time with knots at 15, 25, and 35 days (based on the first, second, and third quartiles of days post-baseline). To test the presence of a non-constant time trend, a robust Wald test was conducted.
We used simple linear regression to examine bivariate associations between patient characteristics and response rate. To account for missing data, we employed multiple imputation via chained equations with M = 300 iterations; standard errors and percentile-based 95% confidence intervals were formed based on B = 100 bootstrap replicates per imputation iteration, and results aggregated using the procedures suggested by Schomaker et al. [33]. Wald testing was conducted based on estimated covariance matrices from this procedure.
2.5.3. Text message feedback
We used means and SDs or frequencies and percentages, as appropriate, to describe patient feedback. We used Mann–Whitney U tests, Spearman’s rho, or chi-square tests, as appropriate, to explore bivariate associations between participants’ characteristics and their feedback.
3. Results
3.1. Patient characteristics
Figure 1 includes a consort diagram showing the flow of participants through enrollment, allocation, and those included in each type of analysis. Of the 111 participants randomized to receive the intervention, 10 were excluded because they were ineligible. The mean age of the remaining 101 intervention participants was 52.9 years (SD: 13.2); 57% were female and 43% were Black. The median reported annual income was $39.6K (IQR: 19.6, 75.0), and mean years of education was 14.2 years (SD: 2.9 years) (Table 2). Engagement was analyzed among the 63 intervention participants who were enrolled and randomized after January 4, 2017, when the functionality to respond to the text messages become available. Descriptive statistics on this subset of participants were similar to the larger sample (Table 2). Lastly, of the 101 intervention participants invited to complete a follow-up survey, 71 did so. We report participants’ feedback at their longest exposure to VERB based on available feedback data (i.e., 11 at 1 month and 61 at 3 months). Patient characteristics of those who provided feedback were generally similar to the larger sample and are reported in Table 2.
Figure 1.
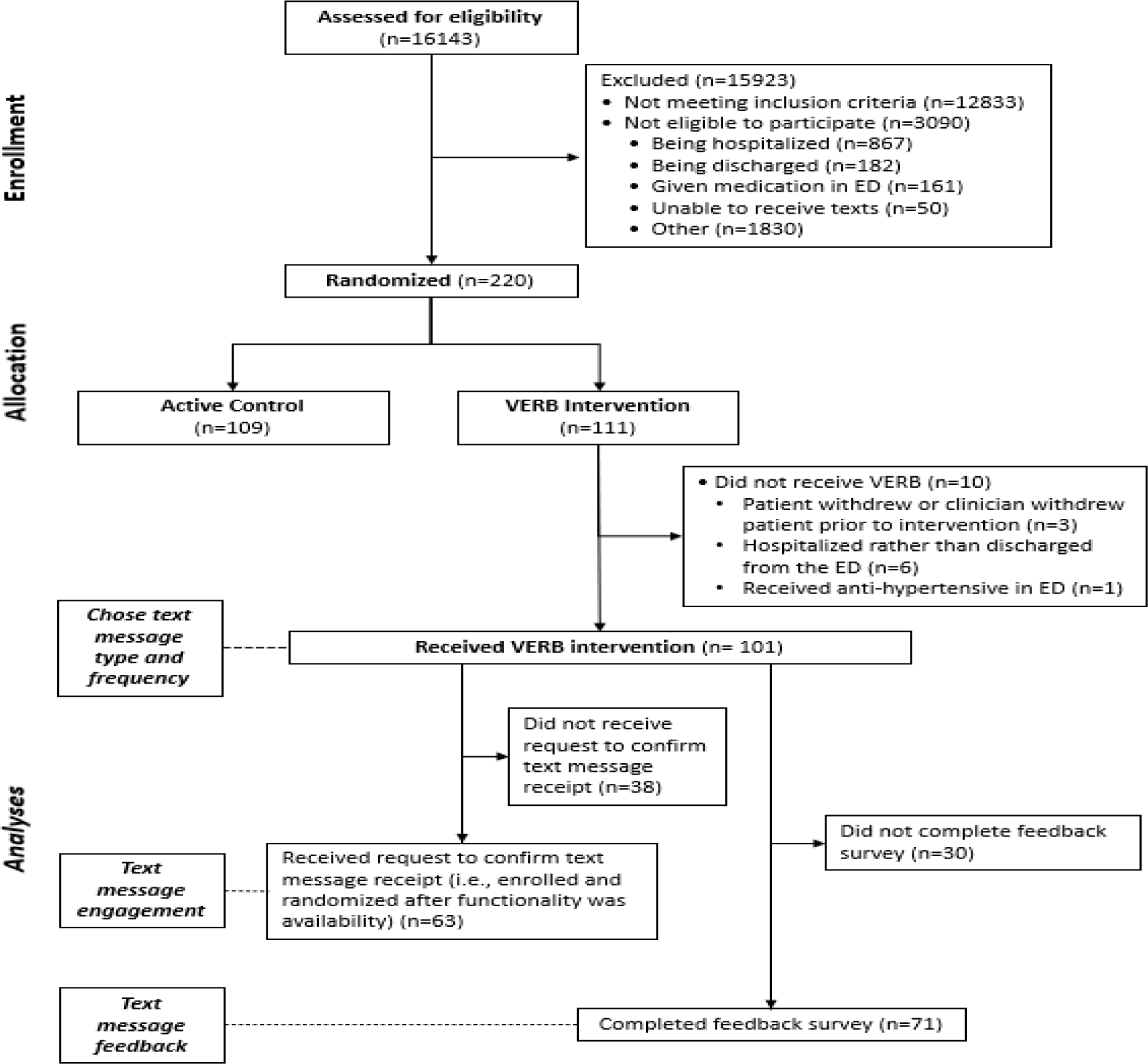
Consort Flow Diagram
Table 2.
Patient characteristics at enrollment
| Characteristic | Participants included in each analysis | ||
|---|---|---|---|
|
| |||
| Chosen text type and frequency | Text message engagement | Text message feedback | |
| N=101 | N=63 | N=71 | |
|
| |||
| M ± SD or n (%)* | |||
|
| |||
| Age, years | 52.9 ± 13.2 | 53.7 ± 14.5 | 54.2 ± 12.3 |
| Gender, male | 43 (43) | 28 (44) | 29 (41) |
| Enrollment Site, VUMC | 93 (92) | 55 (87) | 64 (90) |
| Race | |||
| White | 53 (53) | 35 (56) | 40 (56) |
| Black | 43 (43) | 26 (41) | 28 (39) |
| Other race(s) | 3 (3) | 0 (0) | 2 (3) |
| Unknown/not reported | 2 (2) | 2 (3) | 1 (1) |
| Education, years | 14.2 ± 2.9 | 14.5 ± 2.6 | 14.1 ± 2.9 |
| Annual Household Income, USD in thousands; Median (IQR) | 39.6 (19.6, 75.0) | 35.0 (20.0, 73.8) | 36.0 (18.0, 80.0) |
| Health Insurance | |||
| Government | 44 (44) | 30 (47.6) | 27 (38) |
| Private | 51 (50) | 30 (47.6) | 41 (58) |
| Uninsured | 5 (5) | 2 (3.2) | 3 (4) |
| Unknown/not reported | 1 (1) | 1 (16) | 0 (0) |
| Health Literacy (BHLS) | 13.3 ± 2.5 | 13.0 ± 2.7 | 13.3 ± 2.4 |
| Numeracy (SNS) | 12.8 ± 4.2 | 12.7 ± 4.4 | 12.7 ±4.3 |
| Perceived Health Competence (PHCS-2) | 7.7 ± 1.9 | 7.9 ± 2.0 | 7.8 ± 1.9 |
| Patient Health Questionnaire (PHQ-2) | 1.65 ± 1.79 | 1.59 ± 1.76 | 1.62 ± 1.78 |
| Medication Adherence (ARMS-7) | 25.0 ± 3.0 | 25.1 ± 3.0 | 25.2 ± 3.1 |
USD, United States Dollars; BHLS, Brief Health Literacy Scale (possible score range: 3–15); SNS, Subjective Numeracy Scale (possible score range: 1–6); VUMC, Vanderbilt University Medical Center; PHCS-2, Perceived Health Competence Scale (possible score range: 2–10); PHQ-2, Patient Health Questionnaire (possible score range: 0–6); ARMS-7, Adherence to Refills and Medications Scale (possible score range: 7–28)
unless otherwise noted
3.2. Chosen text message type and frequencies
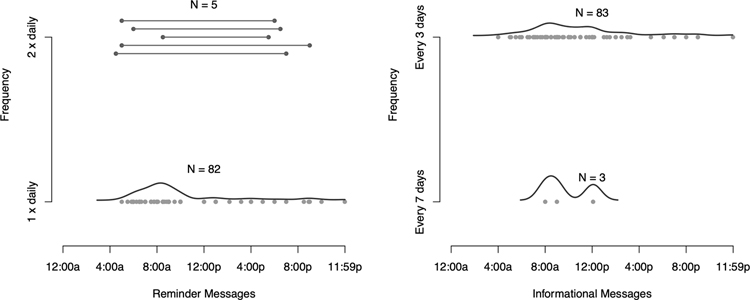
When provided the option to receive reminder messages, 86% (87/101) of participants chose this option. The majority (94%; 82/87) chose to receive these messages daily whereas only 6% (5/87) chose to receive them twice daily. Similarly, 85% (86/101) chose to receive the informational messages; 97% (83/86) chose to receive these messages every 3 days, whereas only 4% (3/86) chose to get them weekly. Seventy-one percent (72/101) chose to receive both reminder and informational messages. There was wide variation in participants’ selected time to receive their messages for either type of text (times ranged from 3:30am-11:59pm) (Figure 2); however, more popular times were between 7:00am and 10:00am.
Figure 2.
Distribution in participants’ selected time of day to receive the texts based on their chosen text type and frequency. For participants who chose to receive reminder texts twice per day (N=5), the dot on either end of the line represents each of their selected times.
Younger age was associated with choosing to receive informational messages (p=0.009). Otherwise, we did not detect associations between chosen text message type or frequency and participants’ gender, race, enrollment site, education, income, insurance, health literacy, numeracy, perceived health competence, depressive symptoms, or medication adherence.
3.2. Text message engagement
Three participants withdrew during the first three weeks of the intervention and were coded as having a nonresponse from the time they withdrew through 45 days. We estimated the mean subject-specific response rate to text messages as 53% (SD 32%; median 56%; IQR 26%−80%) over 45 days. We found evidence of a non-constant time trend; participants’ predicted response rate decreased over time (p=0.015). Specifically, the response rate appeared to decrease slightly from approximately 75% to 60% until around 25 days and then stabilized (Figure 3).
Figure 3.
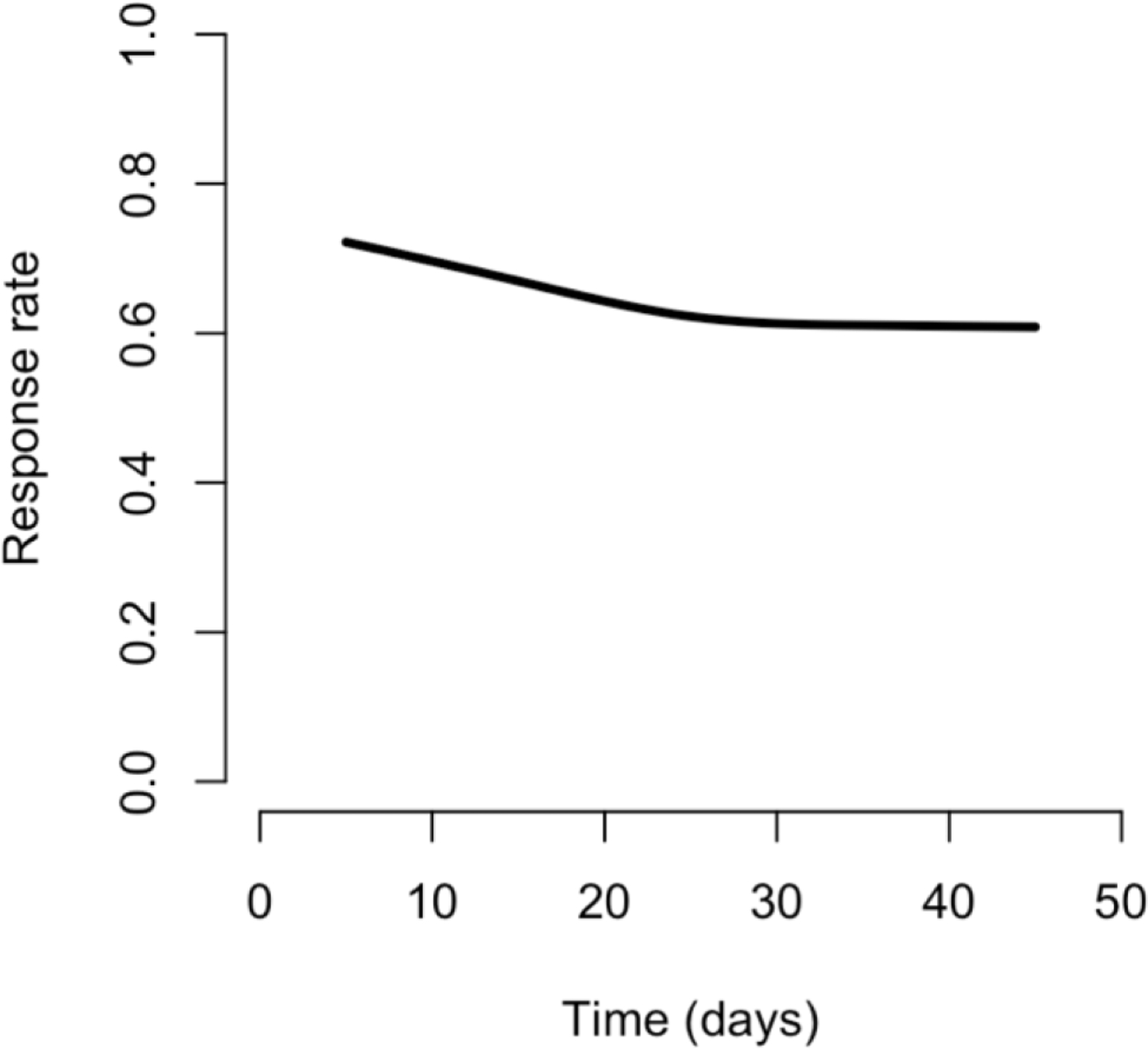
Model examining time-trend in predicted response rate including a restricted cubic spline (N=63)
We did not detect evidence of associations between response rate and participant age, race, enrollment site, education, income, insurance, health literacy, numeracy, perceived health competence, depressive symptoms, or medication adherence. However, compared to women, men had a 24% lower response rate (95% CI: [−38.8, −8.89]; p<0.01).
3.4. Text message feedback
Most of the 71 participants who provided feedback (75%) said they would not have chosen a personalized message instead of the pre-formatted messages (Table 3); however, responses to the remaining questions asking about additional text message functionalities were fairly split. Approximately half the sample wanted the option to: say whether they took their medicine (61%), continue getting reminder message until they responded whether they took their medicine (58%), track their progress with taking their medicines (50%), and share their adherence information with their doctor (59%).
Table 3.
Feedback Survey Items (N=71)
| Item format and Item Content | N (%) Yes |
|
| |
| Close ended (yes/no) | |
|
| |
| 1. If you could have had a completely personalized message, would you have chosen that instead of the pre-formatted messages? | 18 (25) |
| 2. Would you like to have the option to say whether you took your medicine? | 43 (61) |
| 3. If we added the ability to keep getting a reminder message until you let us know that you had taken your medicine, would you choose that option? | 41 (58) |
| 4. If we recorded the times when you responded that you had taken your medicine, would you like to see that information, to track your progress? | 35 (50) a |
| 5. If we recorded the times when you responded that you had taken your medicines, would you like to share that information with your doctor or nurses? | 42 (59) |
| 6. Would you recommend the messages that you received to your friends/family? | 62 (89)a |
| 7. Would you be interested in continuing the messages that you received? | 47 (67) a |
| Likert-type scale item | M (SD) |
| 8. Overall, on a scale of 1–5, where 1 is the messages are not helpful at all and 5 is “I found the messages very helpful,” how helpful were the messages to you? | 4.35 (1.23) |
1 person did not respond to item
Black race was associated with wanting nearly all the options for additional functionality, specifically, wanting the option to: say whether they took their medicine (p=0.02), track progress with taking medicines (p=0.03), and share adherence information with their doctor (p=0.03). Younger age was associated with wanting to share adherence information with their doctor (p=0.04). Lower income was associated with wanting the option to say whether they took their medicine (p=0.02). Lower health literacy was associated with wanting the option to say whether they took their medicine (p=0.03) and continuing to receive reminder messages (p=0.01). Being a VUMC patient was associated with wanting to track progress with taking medications (p=0.02). Lastly, lower baseline medication adherence was associated with wanting to continue to receive reminder messages (p=0.03).
Most participants (89%) said they would recommend the messages to their family and friends and most (67%) reported interest in continuing to receive the messages. Younger age (p=0.04) was associated with recommending the messages. Younger age (p=0.002), Black race (p=0.03), lower health literacy (p=0.03), and lower medication adherence (p=0.049) were associated with interest in continuing the program. On average, participants rated the helpfulness of the messages 4.36 (SD 1.22) on the 1–5 Likert-type scale. Younger age (p=0.01), Black race (p=0.002), lower income (p=0.03), and lower baseline medication adherence (p=0.009) were associated with rating the messages as more helpful.
4. Discussion and conclusion
4.1. Discussion
We examined preferences for text message type and frequency, engagement, and feedback as part of an ED-based behavioral intervention for antihypertensive adherence. Most participants wanted to receive reminder and informational texts; reminder texts were more often chosen once versus twice daily, whereas informational texts were more often chosen every 3 days rather than weekly. Average response rate was relatively modest and gradually decreased over 45 days. We found few differences in chosen text type, frequencies, and engagement by patient characteristics; that is, participants tended to choose similar text types and frequencies and engage similarly irrespective of their characteristics. However, we observed patterns where participants who were Black, had lower socioeconomic status (SES), and had lower medication adherence wanted additional text message functionalities to support their adherence and rated the text messages as more helpful.
Text messages have been promoted as an ideal intervention modality for improving health among underserved groups considering they are a technology most patients already have and tend to appeal across age, SES, and cultures [14, 34]. To our knowledge, very few studies have included racially and socioeconomically diverse patients in text messaging interventions for antihypertensive support [35]. Based on our findings, patients who tend to experience more barriers to adherence and are at risk for worse outcomes expressed more interest and value in the text messages. These patients’ interest in the additional support and general acceptability of the program is encouraging and supports targeting these patients in future work involving text messages for promoting medication adherence [14, 34].
Preferences for the types of text messages received were fairly consistent across participants. Younger participants were more likely to choose informational messages than older participants, which may reflect lower rates of antihypertensive adherence among younger patients and a desire to improve understanding of medications [36]. Selected times to receive text messages was highly variable promoting tailoring of this text message feature. Although we only offered two frequency options for either type of text, informational texts were preferred less often and reminder texts more often. The text message frequency that optimally impacts outcomes is unclear and may vary on an individual basis. Understanding and tailoring the intervention to user preference is a starting place to help ensure the intervention appeals to the user and may help facilitate engagement [19, 37].
User engagement with the text messages was relatively modest. In similar interventions, response rates to text messages vary widely [25] which could be due to differences in the types of responses elicited and registered. As part of a recent 12-month text messaging intervention for diabetes medication adherence, the median response rate to text messages was 91% [37]; messages asked participants to respond if they had taken all of their diabetes medication that day and any response to the text was registered. In our study, we asked participants to confirm if they received a message and only acceptable responses were registered. Asking to confirm receipt may not have been as engaging to participants as asking about their adherence, which could have led to lower response rates. Notably, of all the patient characteristics we examined, gender was the only characteristic associated with engagement. Males had both lower response rates than females, consistent with digital tool engagement in other studies [38]. We did not detect associations with factors associated with engagement in other texting interventions, such as age and depression [39, 40]. Although more engagement with an intervention is typically presumed to be better for patient outcomes, there is a growing literature on effective or meaningful engagement [24, 41]; that is, rather than simply promote more engagement, it may be more valuable to establish the level of engagement needed to achieve benefit, which could vary by individual users. More research that explores engagement alongside patient outcomes is needed to help understand effective engagement and its implications.
This study has several limitations. We focused on participants’ perspective of text messages that were delivered as part of a larger behavioral intervention; therefore, it is possible receiving the other components may have impacted feedback and engagement with the text messages. In addition, participants only received the text messages for 45 days; although the information is helpful for informing future interventions, the data may not be representative of how participants would respond if the intervention period were longer. Although timing of text messages was tailored to participants’ preferences, content was not tailored, possibly resulting in lower engagement rates. With any technology-delivered intervention, there is the potential for technical issues and glitches; it is possible some of the acceptable responses to the request for confirmation were not recognized by the system and therefore missed. This study recruited patients who were treated in the ED with high blood pressure and discharged to home in a specific region in middle Tennessee. Therefore, we acknowledge that the findings may not be generalizable to other patient populations or patients in other locations. In addition, there may have been self-selection bias among our sample considering patients unwilling or unable to respond to text messages would have been ineligible to participate in the study, those who agreed to participate may have been more amenable to receiving texts, and those who agreed to complete the feedback survey may have been more likely to provide positive responses.
4.2. Conclusion
Our findings provide a thorough assessment of users’ perspectives of text messages to support antihypertensive medication adherence delivered as part of an ED-based behavioral intervention. Overall, in this diverse population of patients recruited from an acute care setting, engagement assessed by response to text messages was modest across participants and decreased gradually over the 45-day intervention period. However, participants who were Black, had low SES, or had worse medication adherence were more likely to rate the program as helpful, wanted to continue the text messages, and wanted additional text functionalities to support their adherence.
4.3. Practice Implications
Medication nonadherence is a leading public health challenge for the US healthcare system [42]. Among patients with hypertension, specifically, nonadherence is a critical factor leading to worse blood pressure control and adverse outcomes [5]. In order to address this challenge, innovative solutions are needed that are scalable, low-cost, and acceptable to all patients, including those most at risk [43]. Text messaging interventions are a promising solution and evidence for their efficacy is growing, but more work is needed to optimize their implementation and impact [14]. Notably, over half of the participants in our study said they would want to share their text-reported adherence information with their doctor, which supports integrating these interventions as a supplement to clinical care. Our findings help inform the types and frequencies of text messages patients prefer to receive and support targeting racial/ethnic minorities and patients with low SES in text messaging interventions to help reduce health disparities.
Highlights.
Most participants (71%) wanted to receive both reminder and informational texts
Median text message response rate was 56% over 45 days and decreased over time
Patients at risk of worse health outcomes expressed more value and interest in texts
Funding:
Candace McNaughton received funding from the National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) (K23HL125670; R21HL140381), Veterans Health Administration Office of Rural Health (ORH-10808), and Pfizer. Lyndsay Nelson, Sunil Kripalani, and Christianne Roumie also received support from NIH/NHLBI (K12HL137943). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of Competing Interest:
All the authors declare that they have no relevant conflicts of interest.
Clinical trials registration:
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Centers for Disease Control and Prevention (CDC), Estimated hypertension prevalence, treatment, and control among U.S. adults, US Department of Health and Human Services, Atlanta, GA, 2018. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. (Accessed 01 December 2020). [Google Scholar]
- [2].Zhou Y, Jia L, Lu B, Gu G, Hu H, Zhang Z, Bai L, Cui W, Updated hypertension prevalence, awareness, and control rates based on the 2017 acc/aha high blood pressure guideline, J Clin Hypertens (Greenwich). 21 (2019) 758–765. 10.1111/jch.13564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD, Trends in blood pressure control among us adults with hypertension, 1999–2000 to 2017–2018, J Amer Med Assoc. 324 (2020) 1190–1200. 10.1001/jama.2020.14545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Centers for Disease Control and Prevention (CDC), High blood pressure symptoms and causes, 2017. https://www.cdc.gov/bloodpressure/about.htm. (Accessed 01 December 2020).
- [5].Krousel-Wood M, Thomas S, Muntner P, Morisky D, Medication adherence: A key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients, Curr Opin Cardiol. 19 (2004) 357–362. 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- [6].Vrijens B, Antoniou S, Burnier M, de la Sierra A, Volpe M, Current situation of medication adherence in hypertension, Front Pharmacol. 8 (2017) 100. 10.3389/fphar.2017.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Burnier M, Egan BM, Adherence in hypertension, Circ Res. 124 (2019) 1124–1140. 10.1161/CIRCRESAHA.118.313220. [DOI] [PubMed] [Google Scholar]
- [8].Ferdinand KC, Yadav K, Nasser SA, Clayton-Jeter HD, Lewin J, Cryer DR, Senatore FF, Disparities in hypertension and cardiovascular disease in blacks: The critical role of medication adherence, J Clin Hypertens (Greenwich). 19 (2017) 1015–1024. 10.1111/jch.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Schober DJ, Tate M, Rodriguez D, Ruppar TM, Williams J, Lynch E, High blood pressure medication adherence among urban, african americans in the midwest united states, J Racial Ethn Health Disparities. (2020). 10.1007/s40615-020-00819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ, Racial differences in blood pressure control: Potential explanatory factors, J Gen Intern Med. 23 (2008) 692–8. 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS, Barriers to and determinants of medication adherence in hypertension management: Perspective of the cohort study of medication adherence among older adults, Med Clin North Am. 93 (2009) 753–69. 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Al-Noumani H, Wu JR, Barksdale D, Sherwood G, AlKhasawneh E, Knafl G, Health beliefs and medication adherence in patients with hypertension: A systematic review of quantitative studies, Patient Educ Couns. 102 (2019) 1045–1056. 10.1016/j.pec.2019.02.022. [DOI] [PubMed] [Google Scholar]
- [13].Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB, Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting, J Clin Hypertens (Greenwich). 9 (2007) 179–86. 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Willcox JC, Dobson R, Whittaker R, Old-fashioned technology in the era of “bling”: Is there a future for text messaging in health care?, J Med Internet Res. 21 (2019) e16630. 10.2196/16630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bensadon BA, Maximizing treatment adherence: Physician-patient partnerships vs procedures, Hypertension. 63 (2014) e7. 10.1161/HYPERTENSIONAHA.113.02725. [DOI] [PubMed] [Google Scholar]
- [16].Pew Research Center, Digital divide persists even as lower-income americans make gains in tech adoption, 2019. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/. (Accessed 01 December 2020).
- [17].Pew Research Center, Mobile fact sheet, 2019. https://www.pewresearch.org/internet/fact-sheet/mobile/. (Accessed 01 December 2020).
- [18].Pew Research Center, Cell phone activities, 2015. https://www.pewresearch.org/internet/chart/cell-phone-activities/. (Accessed 01 December 2020).
- [19].DeKoekkoek T, Given B, Given CW, Ridenour K, Schueller M, Spoelstra SL, Mhealth sms text messaging interventions and to promote medication adherence: An integrative review, J Clin Nursing. 24 (2015) 2722–35. 10.1111/jocn.12918. [DOI] [PubMed] [Google Scholar]
- [20].Xiong S, Berkhouse H, Schooler M, Pu W, Sun A, Gong E, Yan LL, Effectiveness of mhealth interventions in improving medication adherence among people with hypertension: A systematic review, Curr Hypertens Rep. 20 (2018) 86. 10.1007/s11906-018-0886-7. [DOI] [PubMed] [Google Scholar]
- [21].Schwebel FJ, Larimer ME, Using text message reminders in health care services: A narrative literature review, Internet Interv. 13 (2018) 82–104. 10.1016/j.invent.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Birnbaum F, Lewis D, Rosen RK, Ranney ML, Patient engagement and the design of digital health, Acad Emerg Med. 22 (2015) 754–6. 10.1111/acem.12692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zhang S, Hamburger E, Kahanda S, Lyttle M, Williams R, Jaser SS, Engagement with a text-messaging intervention improves adherence in adolescents with type 1 diabetes: Brief report, Diabetes Technol Ther. 20 (2018) 386–389. 10.1089/dia.2018.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Short CE, DeSmet A, Woods C, Williams SL, Maher C, Middelweerd A, Müller AM, Wark PA, Vandelanotte C, Poppe L, Hingle MD, Crutzen R, Measuring engagement in ehealth and mhealth behavior change interventions: Viewpoint of methodologies, J Med Internet Res. 20 (2018) e292. 10.2196/jmir.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nelson LA, Coston TD, Cherrington AL, Osborn CY, Patterns of user engagement with mobile- and web-delivered self-care interventions for adults with t2dm: A review of the literature, Curr Diab Rep. 16 (2016) 66. 10.1007/s11892-016-0755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Harris PA, Research electronic data capture (redcap)-planning, collecting and managing data for clinical and translational research, BMC Bioinformatics. 13 (2012) A15. https://doi.org/. [Google Scholar]
- [27].Coco J, Fabbri D, Knock: Hail lab https://www.vumc.org/hail-lab/knock.
- [28].Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S, Psychometric properties of the brief health literacy screen in clinical practice, J Gen Intern Med. 29 (2014) 119–26. 10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].McNaughton CD, Cavanaugh KL, Kripalani S, Rothman RL, Wallston KA, Validation of a short, 3-item version of the subjective numeracy scale, Med Decis Making. 35 (2015) 932–6. 10.1177/0272989X15581800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bachmann JM, Goggins KM, Nwosu SK, Schildcrout JS, Kripalani S, Wallston KA, Perceived health competence predicts health behavior and health-related quality of life in patients with cardiovascular disease, Patient Educ Couns. 99 (2016) 2071–2079. 10.1016/j.pec.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Kroenke K, Spitzer RL, Williams JB, The patient health questionnaire-2: Validity of a two-item depression screener, Med Care. 41 (2003) 1284–92. 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- [32].Kripalani S, Risser J, Gatti ME, Jacobson TA, Development and evaluation of the adherence to refills and medications scale (arms) among low-literacy patients with chronic disease, Value Health. 12 (2009) 118–23. 10.1111/j.1524-4733.2008.00400.x S1098-3015(10)60682-1 [pii]. [DOI] [PubMed] [Google Scholar]
- [33].Schomaker M, Heumann C, Bootstrap inference when using multiple imputation, Stat Med. 37 (2018) 2252–2266. 10.1002/sim.7654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mayberry LS, Lyles CR, Oldenburg B, Osborn CY, Parks M, Peek ME, Mhealth interventions for disadvantaged and vulnerable people with type 2 diabetes, Curr Diab Rep. 19 (2019) 148. 10.1007/s11892-019-1280-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Buis L, Hirzel L, Dawood RM, Dawood KL, Nichols LP, Artinian NT, Schwiebert L, Yarandi HN, Roberson DN, Plegue MA, Mango LC, Levy PD, Text messaging to improve hypertension medication adherence in african americans from primary care and emergency department settings: Results from two randomized feasibility studies, JMIR mHealth and uHealth. 5 (2017) e9. 10.2196/mhealth.6630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].van der Laan DM, Elders PJM, Boons C, Beckeringh JJ, Nijpels G, Hugtenburg JG, Factors associated with antihypertensive medication non-adherence: A systematic review, J Hum Hypertens. 31 (2017) 687–694. 10.1038/jhh.2017.48. [DOI] [PubMed] [Google Scholar]
- [37].Nelson LA, Spieker A, Greevy R, LeStourgeon LM, Wallston KA, Mayberry LS, User engagement among diverse adults in a 12-month text message-delivered diabetes support intervention: Results from a randomized controlled trial, JMIR Mhealth Uhealth. 8 (2020) e17534. 10.2196/17534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nouri SS, Adler-Milstein J, Thao C, Acharya P, Barr-Walker J, Sarkar U, Lyles C, Patient characteristics associated with objective measures of digital health tool use in the united states: A literature review, J Am Med Inform Assoc. 27 (2020) 834–841. 10.1093/jamia/ocaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Nelson LA, Mulvaney SA, Gebretsadik T, Ho YX, Johnson KB, Osborn CY, Disparities in the use of a mhealth medication adherence promotion intervention for low-income adults with type 2 diabetes, J Am Med Inform Assoc. (2015). 10.1093/jamia/ocv082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Turner CM, Coffin P, Santos D, Huffaker S, Matheson T, Euren J, DeMartini A, Rowe C, Batki S, Santos GM, Race/ethnicity, education, and age are associated with engagement in ecological momentary assessment text messaging among substance-using msm in san francisco, J Subst Abuse Treat. 75 (2017) 43–48. 10.1016/j.jsat.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, Merchant GC, Naughton F, Blandford A, Understanding and promoting effective engagement with digital behavior change interventions, Am J Prev Med. 51 (2016) 833–842. 10.1016/j.amepre.2016.06.015. [DOI] [PubMed] [Google Scholar]
- [42].Kleinsinger F, The unmet challenge of medication nonadherence, Perm J. 22 (2018) 18–033. 10.7812/TPP/18-033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Zullig LL, Gellad WF, Moaddeb J, Crowley MJ, Shrank W, Granger BB, Granger CB, Trygstad T, Liu LZ, Bosworth HB, Improving diabetes medication adherence: Successful, scalable interventions, Patient Prefer Adherence. 9 (2015) 139–149. 10.2147/PPA.S69651. [DOI] [PMC free article] [PubMed] [Google Scholar]