Heart failure (HF) is a leading cause of morbidity and mortality in the United States.[1] A chronically, disabling and debilitating condition, HF often results in hospital admission and subsequent readmission.[2] After hospitalization, nearly 25% of older adults with HF are discharged to skilled nursing facilities (SNFs) for rehabilitation due to difficulties with functioning independently.[3] Critically, patients with HF discharged to SNFs also show significantly higher rates of mortality.[2] Identifying factors that predict mortality among this important patient population, especially factors that could be addressed in the hospital setting, is an important step toward improving survivability among these patients.
The presence of suicidal ideation may be a useful clinical marker to identify which patients with HF who have been discharged to SNFs are at greater risk of mortality. Patients with HF frequently experience significant changes in health, function, and life stress during recovery, and have more limited access to social supports. They also commonly experience a myriad of psychiatric comorbidities (i.e., depression, post-traumatic stress disorder, and other psychiatric disorders),[4,5] and are at greater risk of chronic pain,[6] all of which are factors that increase risk for suicidal ideation[7] and mortality. Moreover, patients discharged to SNFs have a higher prevalence of cognitive impairment, physical illnesses and pain, functional impairment, feelings of social disconnectedness, and other factors that may increase the risk of suicidal ideation compared to individuals discharged to the community. And, risk for experiencing suicidal ideation is especially heightened among geriatric patients.[8] As a result, suicidal ideation may be a proxy for the severity of these factors, that all can indicate greater risk for mortality.
However, factors unique to suicidal ideation may also increase mortality risk among patients with HF discharged to SNFs. Patients experiencing suicidal thoughts are often highly distressed and overwhelmed by their life circumstances, and can be highly motivated to seek an escape from their problems. Perhaps as a result, there is some evidence that patients with suicidal thoughts may be less engaged in treatment and exhibit greater functional decline,[9] factors that can increase risk for mortality. As such, suicidal ideation could be a marker of increased mortality risk, and could indicate patients who might benefit from additional support and interventions to improve outcomes. This is a highly relevant question as mental health comorbidities can impact medical outcomes, but are often not an area of focus in medical decision-making contexts. However, whether the presence of suicidal ideation predicts increased risk of mortality apart from medical and psychiatric comorbidities in this important group is unknown. This is an important knowledge gap given the high comorbidity between medical issues and suicide ideation.[10,11]
The present study examined these important knowledge gaps by examining whether suicidal ideation was a marker of increased mortality risk in the 30- and 365-days following admission to a SNF. We conducted a secondary data analysis of a population of older veterans with HF discharged to SNFs within the Veterans Affairs (VA) system. Specifically, we sought to (1) describe demographic, psychiatric, and medical factors associated with suicide ideation among patients with HF upon admission to a SNF; and to (2) determine whether suicide ideation predicted mortality over 30-day and 365-day follow-up among those discharged to a SNF.
METHODS
Study Design and Population
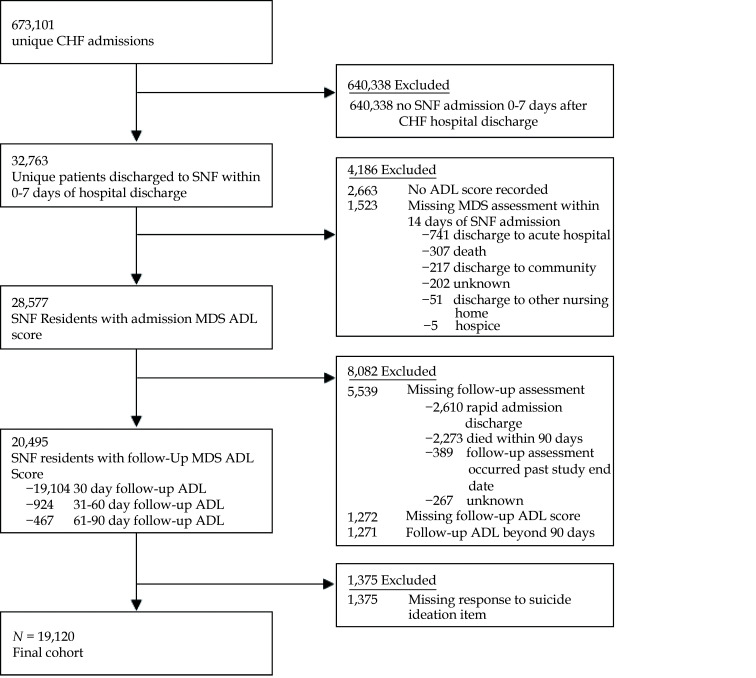
This was a retrospective cohort study derived from a national source population of 673,101 veterans across 129 VA Medical Centers who were admitted for treatment of HF at the index admission (i.e., had a primary HF diagnosis at the index admission) and subsequently discharged to a SNF. Thus, all Veterans included in this study were treated for HF during their index admission. Veterans at VAMCs which did not provide inpatient services were excluded. We linked Veterans Health Administration (VHA) electronic medical records and hospitalization claims to Minimum Data Set (MDS) version 3.0 assessments using unique Veterans Administration (VA) identifiers. The MDS is a federally mandated, standardized resident assessment for Medicare and Medicaid-certified Skilled Nursing Facilities (SNFs).[12] We derived information from MDS assessments administered at admission, which consist of health information and validated questionnaires including demographics, clinical conditions, functional status, mood and behavioral symptoms, and cognitive status. Information extracted from VHA records included data such as demographics, comorbidities, prior healthcare utilization, test results, claims data, and mortality.
Veterans with HF admissions between October 1, 2010 and September 30, 2015 were identified via ICD-9 codes from VHA electronic records and hospitalization claims. Discharges to SNFs were identified via the MDS. Among veterans who had multiple SNF stays, the first SNF stay was sampled. Veterans were excluded from the sample if they had a record of long-term (custodial) care conversion (i.e., MDS assessment beyond 90 days), incomplete data (e.g., missing two or more MDS assessments), or were being transferred directly from a SNF, as the purpose of this project was to examine new SNF admission due to HF. They were also excluded if they received hospice care services before, during, or following hospital discharge, established via VA fee basis files and CMS hospice data. To maximize the sample size, patients who met these criteria and had an MDS assessment within two weeks of admission were included in analyses. After applying these criteria, the final sample consisted of 19,120 Veterans. This study was approved by the Institutional Review Board at the Providence VA Medical Center.
Depressive Symptoms and Suicide Ideation
Depressive symptoms and suicidal ideation were measured using the Patient Health Questionnaire-9 (PHQ-9),[13,14,15] which was derived from Section D of the MDS version 3.0 SNF admission assessment. The PHQ-9 is a 9-item self-report measure that screens for the presence and severity of cognitive, affective, and somatic depressive symptoms. Patients reported the frequency each symptom was experienced in the past two weeks ranging from 0 (“not at all”) to 3 (“nearly every day”). The item that assesses recent suicidal ideation (“Thoughts that you would be better off dead, or thoughts of hurting yourself in some way?”) was dichotomized (e.g., presence (1) or absence (0) of ideation) for inclusion in analyses. Cutpoints resulting from the total score of all items correspond to endorsement of mild (5–9), moderate (10–14), moderately severe (15–20), and severe (> 20) depression (seeTable 1). For multivariate analyses, we included a total composite depression severity score derived from summing only items 1–8 were summed to create a composite total depression severity score. The suicide ideation item was excluded from this total depression score to minimize redundancy in models.
Table 1. Demographic and clinical characteristics in the full sample and as a function of suicide ideation at baseline.
| Total cohort
(n = 19,120) |
No SI
(n = 18,745) |
SI
(n = 375) |
SMD | P | |
| Data are presented as n (%) or mean ± SD unless other indicated. PHQ-9 scores were calculated including the suicide item.* Skilled nursing facility admission date was used as the reference. ADL: activities of daily living; CHF: coronary heart failure; EF: ejection fraction; SI: suicide ideation; SNF: skilled nursing facility; PHQ-9: patient health questionnaire-9. | |||||
| Age | 77.5 ± 10.2 | 77.5 ± 10.26 | 79.8 ± 10.22) | 0.23 | < 0.0001 |
| Gender | 588 (3.1%) | 572 (3.1%) | 16 (4.3%) | −0.06 | 0.1772 |
| Race/Ethnicity | 0.29 | < 0.0001 | |||
| White | 15,149 (79.4%) | 14,815 (79.30%) | 334 (86.67%) | ||
| Black | 3037 (15.9%) | 3011 (15.57%) | 26 (7.36%) | ||
| Other | 364(1.9%) | 356 (1.99%) | 8 (3.22%) | ||
| Hispanic | 529 (2.8%) | 523 (2.88%) | 6 (2.30%) | ||
| Missing | 41 (0.25%) | 39 (0.25%) | 2 (0.46%) | ||
| Dementia | 5904 (30.9%) | 5772 (30.8%) | 132 (35.2%) | 0.09 | 0.0673 |
| Elixhauser co-morbidity index | 4.9 (2.8%) | 4.9 (2.80%) | 4.9 (2.95%) | 0.01 | 0.8480 |
| Chronic lung disease | 8392 (43.9%) | 8229 (43.9%) | 163 (43.8%) | −0.01 | 0.6247 |
| Diabetes | 9806 (51.3%) | 9627 (51.4%) | 179 (47.7%) | −0.07 | 0.4585 |
| Diabetes with Complications | 5529 (28.9%) | 5440 (29.0%) | 89 (23.7%) | −0.12 | 0.0253 |
| Hypothyroidism | 2791 (14.6%) | 2743 (14.6%) | 48 (12.8%) | −0.05 | 0.2541 |
| Chronic kidney disease | 1840 (9.6%) | 1020 (5.4%) | 23 (6.1%) | −0.10 | 0.5591 |
| Liver disease | 1043 (5.5%) | 1206 (5.49%) | 25 (5.75%) | 0.03 | 0.8142 |
| Tumor history | 3323 (17.4%) | 3276 (17.5%) | 47 (12.5%) | −0.14 | 0.0124 |
| Obesity | 4084 (21.4%) | 4018 (21.4%) | 66 (17.6%) | −0.10 | 0.0728 |
| Weight loss | 1835 (9.6%) | 1795 (9.6%) | 40 (10.7%) | 0.04 | 0.4777 |
| Anemia | 7359 (38.5%) | 7208 (38.5%) | 151 (40.3%) | 0.04 | 0.4748 |
| Alcohol use disorder | 1515 (7.9%) | 1488 (7.9%) | 27 (7.2%) | −0.03 | 0.6003 |
| Substance use disorder | 742 (3.9%) | 725 (3.9%) | 17 (4.5%) | 0.03 | 0.5087 |
| Psychosis | 3014 (15.8%) | 2923 (15.6%) | 91 (24.3%) | 0.22 | < 0.0001 |
| Depression | 4592 (24.0%) | 4453 (23.8%) | 139 (37.1%) | 0.29 | < 0.0001 |
| ED admissions year before hospitalization | 3.1 (3.9%) | 3.1 (3.91%) | 3.1 (4.23%) | −0.00 | 0.9549 |
| EF (%) in year before hospitalization | 43.5 (15.0%) | 43.51 (14.96%) | 43.8 (14.73%) | 0.02 | 0.9536 |
| Ejection fraction categories | 0.11 | 0.4078 | |||
| 0−40%, reduced | 4920 (25.7%) | 4832 (25.8%) | 88 (23.5%) | ||
| 40%−50%, borderline | 2828 (14.8%) | 2771 (14.8%) | 57 (15.2%) | ||
| > 50%, Preserved | 5195 (27.2%) | 5100 (27.2%) | 95 (25.3%) | ||
| 99%, Missing | 6177 (32.3%) | 6042 (32.2%) | 135 (36.0%) | ||
| Length of stay of index heart failure admission | 10.5 (9.2%) | 10.5 (9.2%) | 10.1 (8.7%) | −0.05 | 0.6213 |
| Health care cost year before hospitalization | 30,705 (38,283) | 30,730 (38,192) | 29,472 (42,565) | −0.03 | 0.1509 |
| Depressive symptoms (PHQ-9) | 1.70 | < 0.0001 | |||
| Minimal | 14754 (78.5%) | 14693 (78.5%) | 61 (16.4%) | ||
| Mild | 3064 (15.8%) | 2952 (15.8%) | 112 (30.1%) | ||
| Moderate | 908 (4.4%) | 821 (4.4%) | 87 (23.4%) | ||
| Severe | 368 (1.4%) | 256 (1.4%) | 112 (30.1%) | ||
| Inpatient admissions one year prior to index CHF admission | 2.07 (1.78%) | 2.07 (1.77%) | 2.00 (1.81%) | −0.04 | 0.4882 |
| ADL score at admission | 16.0 (5.1%) | 16.0 (5.1%) | 16.4 (5.1%) | 0.10 | 0.0665 |
| Cognitive impairment | 0.43 | < 0.0001 | |||
| Intact | 10,366 (54.2%) | 10,233 (54.6%) | 133 (35.5%) | ||
| Mild | 5591 (29.3%) | 5440 (29.0%) | 151 (40.3%) | ||
| Modest | 2846 (14.9%) | 2766 (14.8%) | 80 (21.3%) | ||
| Severe | 307 (1.6%) | 296 (1.6%) | 11 (2.9%) | ||
| Outcomes | |||||
| Post 30 day mortality* | 1091 (5.7%) | 1042 (5.6%) | 49 (13.1%) | 0.26 | < 0.0001 |
| Post 365 day mortality* | 8095 (42.3%) | 7894 (42.1%) | 201 (53.6%) | 0.23 | < 0.0001 |
Mortality Outcomes
All-cause mortality was the outcome of interest and was measured in the VHA Vital Status File The VHA Vital Status File combines mortality data from several federal sources and has been previously validated.[11] Two separate time-to-event variables were created: 30- and 365-days after the day of admission to the SNF.
Covariates
Demographic data (e.g., age, sex, race/ethnicity) were ascertained from VHA electronic medical records. Psychiatric and medical comorbidities from the year prior to SNF admission were drawn from VA coding data, and the number of comorbidities were summed to calculate the Elixhauser Comorbidity Index (ECI). Left ventricular ejection fraction (EF) values that were obtained from patient electronic medical record notes with an automated information extraction application using natural language processing algorithms validated for the VHA.[16] VA healthcare cost and utilization characteristics were extracted from VA administrative records. These characteristics included the number of emergency department visits, inpatient admissions, and healthcare costs in the year prior to index hospitalization, as well as the length of stay for the index HF admission.
Variables to index general and cognitive function from the MDS 3.0 admission assessment were also included as covariates in analyses. The 10 items from the MDS Activities of Daily Living (ADL) assessment (i.e., locomotion on/off unit, dressing, eating, personal hygiene; coded on a scale of 0 (independence) to 4 (total dependence)) were summed to create a total ADL score (higher scores indicate worse functional ability).[17] A Cognitive Function Scale was derived from Brief Inventory of Mental Status (BIMS) or Cognitive Performance Scale (CPS) scores,[12] depending on which method of assessment was completed. The highest level of impairment, “severely impaired” (3), includes individuals who did not complete the BIMS and have a CPS score of 5 or 6. Residents were assigned a value of “moderately impaired” (2) if they scored between a 0–7 on the BIMS or a 3 or 4 on the CPS. Residents with a BIMS score of 8–12 or a CPS score of 0–2 were considered “mildly impaired” (1). Residents were considered “cognitively intact” if they were able to complete the BIMS and scored between 13 and 15 (0).
Statistical Analysis
Baseline characteristics across suicide ideation groups (presence/absence of suicide ideation on SNF admission assessment) were compared using t-tests for continuous variables and chi-square tests for categorical variables to identify zero-order differences between groups of Veterans with and without suicidal ideation, and to inform selection of additional analytic covariates for mortality models. A Bonferroni correction (P < 0.0016) was employed to correct for multiple comparisons. Measures of variance (i.e., SD) were included across analyses.
Primary analyses examined whether suicidal ideation at admission predicted 30-day and 365-day mortality outcomes using Cox proportional hazards models. Initial inspection of model assumptions using Schoenfeld residuals indicated that the proportional hazards assumption was satisfied for the 30-day, but not the 365-day, model. Given these results, we chose to retain results of the Cox regressions, but interpreted our findings as a weighted average (rather than constant effect), consistent with recommendations from the literature.[18] For both outcomes, we computed one unadjusted and two adjusted models. Both adjusted models covaried for demographic, medical/psychiatric comorbidity, healthcare utilization, and function factors, and one model additionally adjusted for baseline depressive symptoms. In initial models, we included SNF facilities as a random effect to account for the impact of potential clustering across facilities in our analyses; however, this effect was nonsignificant across models, and therefore we report final results without this effect included for parsimony.
Software
All analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, NC) and stata/MP 16.0.
Data Availability
Data were obtained through a data use agreement with the U.S. Department of Veterans Affairs and cannot be made available publicly.
RESULTS
Population Characteristics
Characteristics of the overall population, representing data from 3,381 SNFs, are presented in Table 1. Veterans were predominantly male (97%) and White (80%), with an average age of 78 ± 10.2 years. Most patients had multiple medical comorbidities (ECI: 4.9 ± 2.8); the most common were diabetes, chronic lung disease, and anemia. Nearly a third of patients had a pre-existing dementia diagnosis. A total of 375 Veterans (0.5% of the population) endorsed recent suicidal thoughts at the baseline assessment.
Suicide Ideation
Several differences emerged when baseline characteristics were compared across Veterans with recent suicidal ideation versus without (see Table 1). Veterans with and without suicidal ideation showed similar rates of medical diagnoses and treatment utilization. However, veterans with suicide ideation were slightly older, more likely to be White, and less likely to be Black/African American. They were also more likely to have a diagnosis of a psychotic and depressive disorder noted in their medical record, and were more likely to have cognitive impairment across all categories of the BIMS (mild: P < 0.0001; moderate: P < 0.0001; severe: P < 0.0001) compared to veterans without suicidal ideation. Veterans with ideation also endorsed more severe depressive symptoms on the PHQ-9 (diagnostic codes used to capture key medical and psychiatric diagnoses for this sample are provided in Supplementary Table 1). These variables were included as additional analytic covariates in adjusted models. Veterans with ideation showed greater rates of mortality within 30 (13.1% vs. 5.6%, P < 0.0001) and 365 (53.6% versus 42.1%, P < 0.0001) days of admission.
Mortality Outcomes
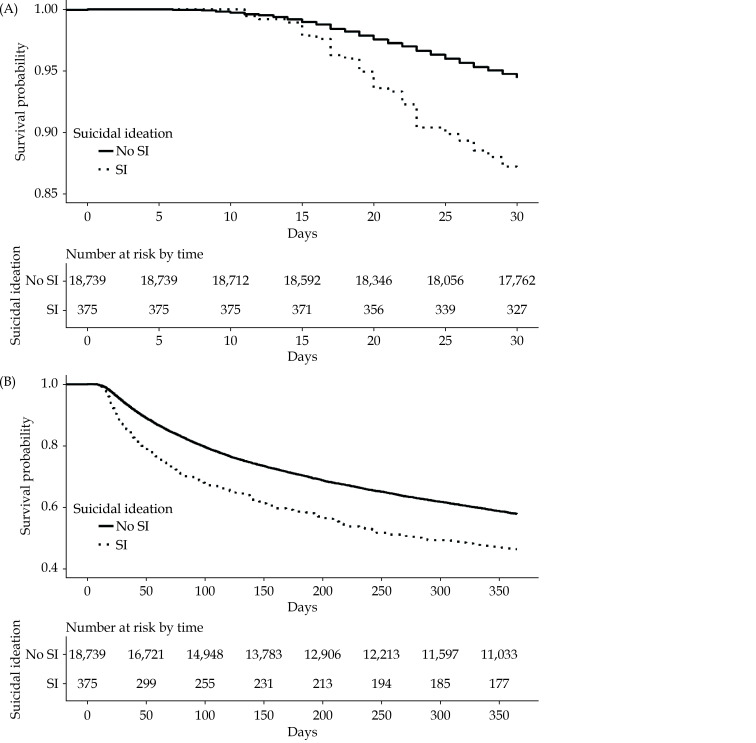
Unadjusted and adjusted HRs for outcomes are shown in Table 2, with patients without SI serving as the reference group. Mortality in the 30 days following baseline was significantly higher in the SI group across models (HR = 2.34, 95% CI: 1.75–3.11, P < 0.0001), even after adjusting for relevant covariates (HR = 2.10, 95% CI: 1.57–2.80, P < 0.0001) and depressive symptoms (HR = 1.51, 95% CI: 1.11–2.05, P = 0.01). Mortality in the 365-days after baseline was also significantly higher in the SI group (HR = 1.48, 95% CI: 1.29–1.67, P < 0.0001), including after adjusting for demographic and medical covariates (HR = 1.35, 95% CI: 1.17–1.55, P < 0.0001) and depressive symptoms (HR = 1.16, 95% CI: 1.002–1.34, P = 0.04). Kaplan-Meier curves for 30-day and 365-day event-free survivorship depicting increased mortality as a function of suicide ideation group are shown in Figures 1 and 2.
Table 2. Survival analyses for mortality within 30- and 365-days of SNF admission.
| Predictors | Hazard Ratio | 95% CI |
| PHQ-9: patient health questionnaire-9; SI: suicide ideation. | ||
| 30-day mortality | ||
| Unadjusted model | ||
| SI group (with SI) | 2.34 | (1.75, 3.11 ) |
| Adjusted models | ||
| SI group (with SI) Adjusted for relevant covariates | 2.10 | (1.57, 2.80 ) |
| SI group (with SI) Adjusted for relevant covariates and PHQ-9 depressive symptoms | 1.51 | (1.11, 2.05 ) |
| 365-day mortality | ||
| Unadjusted model | ||
| SI group (with SI) | 1.48 | (1.29, 1.67 ) |
| Adjusted models | ||
| SI group (with SI) Adjusted for relevant covariates | 1.35 | (1.17, 1.55 ) |
| SI group (with SI) Adjusted for relevant covariates
and PHQ-9 depressive symptoms |
1.16 | (1.002, 1.34 ) |
Figure 1.
Flow chart describing selection of sample from the broader MDS population.
ADL: activities of daily living; CHF: coronary heart failure; MDS: minimum data set; SNF: skilled nursing facility.
Figure 2.
Survival probability.
(A): Patients with and without suicidal thoughts in the 30-days following SNF admission; (B): patients with and without suicidal thoughts in the 365-days following SNF admission. SNF: skilled nursing facility.
DISCUSSION
This retrospective cohort study examined whether the presence of suicidal ideation is a marker of risk of 30-day and one year mortality among Veterans admitted to a SNF following HF hospitalization. While risk of negative health outcomes and mortality is disproportionately increased for HF patients who are discharged to SNFs following their hospitalizations,[2] research examining prognosis and related variables for outcomes following HF hospitalization has focused primarily on medical factors such as readmission, cardiac function recovery, and mortality. However, psychological factors and mental health variables also impact the medical health outcomes of cardiac patients,[19] and represent potentially malleable intervention targets that could lead to improved outcomes. Depression in particular has been linked to worse outcomes for a wide variety of medical conditions including cardiac conditions,[20] but significantly less is known about the relationship between medical outcomes and suicidal ideation in HF.
Rates of suicide ideation in this sample were lower than expected, with less than 1% of the sample endorsing any ideation. This finding is at odds with prior studies that have consistently found that patients with HF are at heightened risk of suicide.[21] For example, Bucy and colleagues (2017) evaluated a suicide risk management protocol for cardiac arrest survivors and found that systematic assessment of suicide risk showed that 15% of Veterans evaluated post-cardiac arrest endorsed suicidal ideation following hospital discharge and 9% of those with ideation were referred to receive expedited mental health services.[22] Furthermore, rates of suicidal ideation in older adults residing nursing homes have also been to be significantly higher (in the range of 5%-33%) than the rates endorsed in this sample.[9] Although it is possible that our patient population did truly endorse lower rates of ideation, these findings may suggest that more robust and focused assessment of depressive and ideation symptoms at admission among these patients is needed.
Despite the low rates of endorsement in this sample, our results showed an association between suicidal ideation and increased mortality. Suicide ideation predicted both short (e.g., within 30 days) and long-term (e.g., within 365 days) mortality. Effects for 30-day mortality were particularly robust, and persisted even after accounting for comorbid depressive symptoms, such that veterans who endorsed suicide ideation were more than twice as likely to die within 30 days of discharge to a SNF. Rates of medical comorbidities were similar in veteran patients with and without ideation, suggesting that thoughts about death and suicide at baseline uniquely contributed to mortality rates. Taken together, these results suggest that there is something unique about suicidal ideation that may lead to worse health outcomes and, in particular, short-term mortality risk within 30 days from discharge into a nursing facility.
These findings highlight the importance of screening and assessing suicide risk in HF patients. While this study did not explore mechanisms underlying this association, it is possible that patients who are endorsing a wish to die may engage in behaviors that work against their recovery, such as not following recovery or rehabilitation recommendations, not engaging fully in their own care, or withdrawing from social activities and relationships. Recovery from HF admission is a constellation of medication balance, increased physical activity, and dietary moderation. Neglecting any of these factors throughout the HF recovery process could be related to worse overall outcomes for patients and might be influenced by a patient’s suicide ideation. Research has found that patients with suicide ideation who are discharged from the hospital were more likely to be “suboptimal adherants” to medications compared to those without suicide ideation in prior reports.[23] Further research on the potential mechanisms driving the relationship between suicide ideation and mortality risk, especially in relationship to HF recovery, is needed.
Clinical Implications
Taken together, these results highlight the need for comprehensive assessment of suicide risk in cardiac patients, specifically in those discharged to SNF. The VHA has prioritized suicide risk screening at mental health contacts and outpatient clinic visits in primary care. Emphasizing this screening for veterans on entry to SNFs would allow providers to enhance care and address a factor that impacts patient engagement in their treatment and recovery process. Capturing suicide risk at key health care moments (e.g., at time of hospital discharge, during admission to SNFs, etc.), could identify the need for integrated treatment approaches to improve overall health, support the care transition and rehabilitation process, and reduce mortality. Using a relatively brief screening measure to identify the presence of ideation, such as the PHQ-9, as a routine assessment for patients hospitalized with HF may be a relatively quick means of assessing the presence of ideation. Comprehensively assessing suicide risk severity after this initial flag via a more detailed measure, such as the Columbia Suicide Severity Rating Scale,[24] and/or via the hospital’s Consultation and Liaison Team, would be critical next steps after a positive screen to identify the level of mental health care and supports the patient requires. There are numerous empirically supported interventions for suicide risk that could be provided to these patients. Brief cognitive behavioral therapy (BCBT) is one intervention that has been tested in veteran samples and shown to reduce suicide risk[25,26] in general veteran samples and in Veterans with chronic medical illnesses such as HF and chronic obstructive pulmonary disease.[26,27]
Nevertheless, there are likely a number of important considerations in implementing these screenings and follow-up procedures in this patient population, such as availability of hospital resources, provider burden, and impact on length of stay. Additional research examining the features of suicide risk that are most predictive of negative outcomes such as mortality is thus an important next step to guide these efforts. With a sufficient evidence base, these considerations can be brought to the forefront of policy discussions and efforts to develop a streamlined care pathway integrating assessment of mental health concerns such as suicide ideation into patient assessment and care planning in these settings.
Strengths and Limitations
Results of this paper should be interpreted in the context of several limitations. First, while mortality was examined, data was not available on cause of death. Therefore, we are unable to determine whether increased mortality in those with suicidal ideation was due to suicide death or death from other medical causes. Moreover, our population was comprised predominantly of men, and thus additional research is needed to examine the extent to which our pattern of findings generalizes to women. Another important limitation was the availability of only one item in the dataset to assess suicide ideation. While the PHQ-9 is a well-established measure, and one commonly used in medical settings, it is used as a screening measure and lacks the depth required for comprehensive risk assessment. Razykov, et al.[28] examined PHQ-9 utility in assessing suicide risk among coronary artery disease patients and found that sensitivity and specificity of the PHQ-9 was low and recommended against using it as a screening measure in this patient group. The low base rates of suicidal ideation endorsement of this item found in this study also suggest that more comprehensive suicide risk assessment used to better understand the links between suicide ideation and mortality. Nevertheless, our data showed that endorsement of SI on item 9, even with these psychometric limitations, still has value for predicting all-cause mortality in coronary heart failure patients discharged to SNFs.
Nevertheless, despite these limitations, our study has important implications for understanding mortality risk among patients with HF. We leveraged a large, geographically diverse population of Veterans in analyses, and examined results of standardized assessments about suicidal ideation from the MDS. Our results indicated that patients with suicide ideation at their admission assessment were at greater risk of mortality in the 30- and 365-days following their admission, even after accounting for contributing effects of medical, psychiatric, and functioning factors. While additional research is needed to ascertain reasons why suicide ideation may predict increased mortality, these findings suggest that additional emphasis around early assessment of suicide ideation, and potentially brief psychiatric interventions to assist patients with these concerns, may have value in reducing all-cause mortality.
FUNDING
This work was funded by the U.S. Department of Veterans Affairs. Drs Rudolph, Wu, Erqou, Quach, Zullo and Ms Liang are supported by VA Health Services Research and Development Center of Innovation in Long Term Services and Supports (CIN 13–419). Dr. Zullo was also supported by National Institute on Aging grants R21AG061632, R01AG065722, RF1AG061221, and R01AG062492. Dr. Wu is partially supported by the VA HSRD Merit Reviews IRP 20-003 and IIR 14–293–2 for analyst time and resources to build and maintain the heart failure database. Dr. Primack is supported by HSRD merit awards HX002572 and HX002534. Dr. Bozzay is supported by NIMH R01MH124832. Dr. Madrigal was partially supported by the VA Office of Academic Affiliation Advanced Fellowship in Health Services Research. The content and views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
DISCLOSURES
Dr. Zullo received grant funding from Sanofi Pasteur paid directly to Brown University to support research on infections and vaccinations in U.S. nursing homes unrelated to the current study.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online.
ACKNOWLEDGMENTS
M.L.B., and J.M.P. conceptualized the initial research question and wrote the first draft of the manuscript, and J.A.L., and M.R.R., assisted in refining specific sections of the manuscript. L.J., Z.K., and A.R.Z. participated in data analyses and interpretation of results. J.A.R., C.M., R.C., S.E., W.W., and S.C. assisted with critical revision of the manuscript for important intellectual content. All authors provided final approval of the manuscript submitted.
References
- 1.van Riet EE, Hoes AW, Wagenaar KP, et al Epidemiology of heart failure: the prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur J Heart Fail. 2016;18:242–252. doi: 10.1002/ejhf.483. [DOI] [PubMed] [Google Scholar]
- 2.Allen LA, Hernandez AF, Peterson ED, et al Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung M, Yeh AY, Pressler SJ Heart failure and skilled nursing facilities: review of the literature. J Card Fail. 2012;18:854–871. doi: 10.1016/j.cardfail.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Freedland KE, Carney RM, Rich MW Effect of depression on prognosis in heart failure. Heart Fail Clin. 2011;7:11–21. doi: 10.1016/j.hfc.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sayers SL, Hanrahan N, Kutney A, et al Psychiatric comorbidity and greater hospitalization risk, longer length of stay, and higher hospitalization costs in older adults with heart failure. J Am Geriatr Soc. 2007;55:1585–1591. doi: 10.1111/j.1532-5415.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 6.Butchart A, Kerr EA, Heisler M, et al Experience and management of chronic pain among patients with other complex chronic conditions. Clin J Pain. 2009;25:293. doi: 10.1097/AJP.0b013e31818bf574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franklin JC, Ribeiro JD, Fox KR, et al Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017;143:187. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 8.Department of Veterans Affairs OoMHaSP. 2020 National Veteran Suicide Prevention Annual Report. 2020.
- 9.Mezuk B, Rock A, Lohman MC, Choi M Suicide risk in long-term care facilities: A systematic review. Int J Geriatr Psychiatry. 2014;29:1198–1211. doi: 10.1002/gps.4142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Druss B, Pincus H Suicidal ideation and suicide attempts in general medical illnesses. Arch Intern Med. 2000;160:1522–1526. doi: 10.1001/archinte.160.10.1522. [DOI] [PubMed] [Google Scholar]
- 11.Pompili M, Forte A, Berman AL, Lamis DA. The association between physical illness/medical conditions and suicide risk. In: The International Handbook of Suicide Prevention. Wiley Online Library; 2016: 133–148.
- 12.Thomas KS, Dosa D, Wysocki A, Mor V The minimum data set 3.0 cognitive function scale. Med Care. 2017;55:e68. doi: 10.1097/MLR.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroenke K, Spitzer RL, Williams JB The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bélanger E, Thomas KS, Jones RN, et al Measurement validity of the patient-health questionnaire-9 in US nursing home residents. Int J Geriatr Psychiatry. 2019;34:700–708. doi: 10.1002/gps.5074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saliba D, DiFilippo S, Edelen MO, et al Testing the PHQ-9 interview and observational versions (PHQ-9 OV) for MDS 3.0. J Am Med Dir Assoc. 2012;13:618–625. doi: 10.1016/j.jamda.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Garvin JH, DuVall SL, South BR, et al Automated extraction of ejection fraction for quality measurement using regular expressions in Unstructured Information Management Architecture (UIMA) for heart failure. J Am Med Inform Assoc. 2012;19:859–866. doi: 10.1136/amiajnl-2011-000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wysocki A, Thomas KS, Mor V Functional improvement among short-stay nursing home residents in the MDS 3.0. J Am Med Inform Assoc. 2015;16:470–474. doi: 10.1016/j.jamda.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stensrud MJ, Hernán MA Why test for proportional hazards? JAMA. 2020;323:1401–1402. doi: 10.1001/jama.2020.1267. [DOI] [PubMed] [Google Scholar]
- 19.Adelborg K Neurological and psychiatric comorbidity in patients with heart failure: risk and prognosis. Dan Med J. 2018;65:B5429. [PubMed] [Google Scholar]
- 20.Liu RT, Hernandez EM, Trout ZM, et al Depression, social support, and long-term risk for coronary heart disease in a 13-year longitudinal epidemiological study. Psychiatry Res. 2017;251:36–40. doi: 10.1016/j.psychres.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Korkmaz H, Korkmaz S, Çakar M Suicide risk in chronic heart failure patients and its association with depression, hopelessness and self esteem. J Clin Neurosci. 2019;68:51–54. doi: 10.1016/j.jocn.2019.07.062. [DOI] [PubMed] [Google Scholar]
- 22.Bucy RA, Hanisko KA, Kamphuis LA, et al Suicide risk management protocol in post–cardiac arrest survivors: development, feasibility, and outcomes. Ann Am Thorac Soc. 2017;14:363–367. doi: 10.1513/AnnalsATS.201609-694BC. [DOI] [PubMed] [Google Scholar]
- 23.Baeza‐Velasco C, Olié E, Béziat S, et al Determinants of suboptimal medication adherence in patients with a major depressive episode. Depress Anxiety. 2019;36:244–251. doi: 10.1002/da.22852. [DOI] [PubMed] [Google Scholar]
- 24.Posner K, Brent D, Lucas C, et al. Columbia-suicide severity rating scale (C-SSRS). New York, NY: Columbia University Medical Center. 2008.
- 25.Rudd MD Brief cognitive behavioral therapy (BCBT) for suicidality in military populations. Military Psychology. 2012;24:592–603. doi: 10.1080/08995605.2012.736325. [DOI] [Google Scholar]
- 26.Rudd MD, Bryan CJ, Wertenberger EG, et al Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172:441–449. doi: 10.1176/appi.ajp.2014.14070843. [DOI] [PubMed] [Google Scholar]
- 27.Ecker AH, Johnson AL, Sansgiry S, et al Brief cognitive behavioral therapy reduces suicidal ideation in veterans with chronic illnesses. Gen Hosp Psychiatry. 2019;58:27–32. doi: 10.1016/j.genhosppsych.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Razykov I, Ziegelstein RC, Whooley MA, Thombs BD The PHQ-9 versus the PHQ-8—is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. J Psychosom Res. 2012;73:163–168. doi: 10.1016/j.jpsychores.2012.06.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data to this article can be found online.
Data Availability Statement
Data were obtained through a data use agreement with the U.S. Department of Veterans Affairs and cannot be made available publicly.