Abstract
Objectives:
Sleep is a vital component for overall health and well-being, and it plays an essential role in social, physical, psychological, and cognitive health. This study aimed to appraise the sleep quality in medical and science students during the COVID-19 pandemic.
Methods:
This questionnaire-based cross sectional study was conducted in the Department of Physiology, College of Medicine, King Saud University, Riyadh, Saudi Arabia, during September-December 2020. In this study, a validated self-administered electronic questionnaire was distributed to 1000 students, 782 (78.2%) of whom completed the study. The selection of students was based on using the stratified random sampling. The Pittsburgh Sleep Quality Index (PSQI) instrument scale was used to assess the sleep quality among medical and general sciences students.
Results:
Out of 782 respondents, 410 (52.4%) were medical students, and 372 (47.6%) were science students, including Physics, Chemistry, Mathematics, Statistics, Botany, and Zoology. Among the medical students, 143 (34.9%) were in pre-clinical years (1st and 2nd), while 266 (64.9%) of them were in clinical years (3rd, 4th, and 5th). Among all medical and general sciences students, it was found that 669 (85.5%) had poor sleep quality with a mean PSQI global score (mean 8.356) among them 336 (50.2%) were medical, and 333 (49.8%) were science students. Science students’ sleep quality was poorer (mean 8.78) than their medical counterparts (mean= 7.93).
Conclusion:
The COVID-19 pandemic has a significant negative impact on students’ mental health and sleep quality. Both medical and general science students showed alarming levels of sleep deprivation and concerning low sleep quality during the COVID-19 pandemic. The sleep deprivation among students may be due to the sudden change of pedagogy in education driven by the COVID-19 pandemic. Sleep quality is quite a critical issue to be evaluated and addressed nationally and globally.
Keywords: Sleep health, Science students, Medical students, Pittsburgh Sleep Quality Index, COVID-19
INTRODUCTION
The “Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection, also known as COVID-19 pandemic”, has developed an alarming unique circumstance worldwide.1 The pandemic has flipped the education equation for students, which may have affected their psychological and learning behaviors.2 In March 2020, several preventive control measures were implemented to control the spread of COVID-19 worldwide, including Saudi Arabia. These measures included an entire country lock-down for several months to combat the spread of the virus. Universities and schools were closed, students switched to virtual classes and were allowed to attend the campus for their practical lessons. This swift shift changes the regular sleep pattern and remaining activities of life.2
Sleep medicine is an essential medical discipline3 and has been considered in the scientific field for many years. Poor sleep quality is one of the most common problems in modern times. The prevalence of sleep deprivation is increasing among people in both developing and modern societies.4,5 The quantity and quality of sleep play an essential part in individuals’ social, physical, and mental well-being.6 Sleep is a necessary and energizing body behavior that contributes to normal physiological and psychological functions, and it is difficult to change once compromised.7 The literature highlights the importance of sleep for overall health, memory, and higher cognitive consolidations.8
Impaired sleep quality is seen in university students9 and affects the students’ academic performance,10 which is a significant concern for students, universities, and overall countries. This emphasizes the importance of assessing the sleep quality of university students, especially in the stressful situation during the COVID-19 pandemic. The present study aimed to evaluate and compare the sleep quality among medical and general science students during the COVID-19 pandemic.
METHODS
Study design and settings
“This questionnaire-based cross sectional study was conducted in the Department of Physiology, College of Medicine, King Saud University, Riyadh, Saudi Arabia,” during September-December 2020.
Selection of Students and Data Collection
In this study, medical and science students at College of Medicine, College of Science, King Saud University, Riyadh, Saudi Arabia, were invited. The Science College includes the following divisions: Statistics, Mathematics, Zoology, Physics, Chemistry, Biochemistry, Botany, Microbiology, Astronomy, Geology, and Geophysics. The students’ emails and specialties were obtained from the Deanship of Admission and Registration Affairs office. The corroborated “self-administered electronic questionnaire” was circulated through email to the students after being selected randomly. We employed the power formula to calculate the sample size.
Inclusion and Exclusion criteria
In this study, medical and science students at the “College of Medicine, College of Science, King Saud University, Riyadh” were invited. The participants with any previous known complaints of headache, anxiety, depression, sleep disturbances before the beginning of the COVID-19 pandemic were excluded from the study. The participants with a known history of chronic debilitating diseases, neurological, psychological disorders, and malignancy were excluded”.
Questionnaire
The survey questionnaire consisted of 17 items focused on assessing sleep quality using the “Pittsburgh Sleep Quality Index (PSQI) scale.” The survey included an introductory page for informed consent, whether to contribute or not in the study. The students were given an option by clicking on the required option to their responses. No reward was presented to the contributors, and information was kept confidential. We used valid and reliable instruments to assess the sleep quality using the “Pittsburgh Sleep Quality Index (PSQI) Scale.”11
Pittsburgh Sleep Quality Index (PSQI) Scale
PSQI is the most commonly rummage-sale instrument to assess sleep quality in the past month. It covers a wide range of gages relevant to sleep quality,10 including “subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction.” For the PSQI scale, the elements of PSQI were scored out of three, with the minimum score being 0 and the maximum score being 3, where lower values indicated better sleep quality.11 While the cut-off point for the overall Global PSQI score was five. The PSQI has been validated in many languages with acceptable psychometric properties12 and is frequently used in clinical and research settings.13 The PSQI has also been validated in college students as cited in,14-18 including medical students.19,20 The psychometric properties of the PSQI suggest that it is a valid measure of “sleep quality, with a strong reliability coefficient (Cronbach’s alpha) of 0.83 for its seven components. The overall PSQI global score correlation coefficient for test-retest reliability was (r=0.87). The survey was distributed through emails. Initially, 1000 students were included, 782 of whom completed the study; the final included sample size was n=782.
Ethical considerations
This study was approved by the “Institutional Review Board (IRB), Ethics Committee, College of Medicine Research Centre, King Saud University, Riyadh, Saudi Arabia,” approved the protocol (Ref #No.- E-20-5164).
Statistical Analysis
The findings were analyzed by using (SPSS) software version 26.0 for Mac20. All categorical variables, including “age, gender, and occupation status,” were reported using frequency and proportions. The numbers and percentages were calculated. The response score was presented using mean and standard deviation. The various variables were compared using Chi-square, ANOVA, post-turkey hoc, independent samples t-tests, and Wilcoxon rank-sum tests as appropriate. A p-value < 0.05 was considered as significant.
RESULTS
The total number of medical and science students included was 782, out of whom 410 (52.4%) were medical students, and 372 (47.6%) were science students, including Physics, Chemistry, Mathematics, Statistics, Botany, and Zoology. Among medical students, 143 (34.9%) were in pre-clinical years (1st and 2nd), while 266 (64.9%) of them were in clinical years 3rd, 4th, and 5th-year medical students (Table-I).
Table 1.
Sociodemographic characteristics of study subjects (n=782).
| Characteristics | N (%) |
|---|---|
| Age: | |
| 18-21 | 536 (68.5) |
| 22-25 | 244 (31.2) |
| >25 | 2 (0.3) |
| Gender | |
| Male | 271 (34.7) |
| Female | 511 (65.3) |
| Marital status | |
| Single | 777 (99.4) |
| Married | 5 (0.6) |
| Specialty | |
| Medical students | 410 (52.4) |
| Science students | 372 (47.6) |
| An academic year of medical students | |
| Pre-clinical years (1st, 2nd) | 143 (34.9) |
| Clinical years (3rd, 4th, 5th) | 266 (64.9) |
| Part-time job | |
| Yes | 17 (2.2) |
| No | 765 (97.8) |
| BMI | |
| Underweight (<18.5) | 105 (13.4) |
| Normal (18.5-24.9) | 458 (58.6) |
| Overweight (25-29.9) | 170 (21.7) |
| Obese (>30) | 49 (6.3) |
| Smoking status | |
| Yes | 61 (7.8) |
| No | 721 (92.2) |
Sleep quality among science and medical students
Table-II demonstrated that out of 782 participants, 669 (85.55%) had poor sleep quality (≥5 Global PSQI score), while only 113 students had good sleep quality (<5 Global PSQI score). Out of 410 medical students, 336 (81.95%) had poor sleep quality, and 74 (18.05%) had good sleep quality. While out of 372 science students, 333 (89.5%) had poor sleep quality, and 39 (10.5%) had good sleep quality. Overall, it was seen that the sleep quality of science students was poorer (Mean Global PSQI score= 8.78) than their medical counterparts (mean Global PSQI score= 7.93) (Table-II).
Table II.
Distribution of responses to different items of PSQI.
| PSQI elements | Mean ± SD | Valid 0 N (%) | Valid 1 N (%) | Valid 2 N (%) | Valid 3 N (%) |
|---|---|---|---|---|---|
| Sleep Quality | 1.431±0.088 | 105 (13.4) | 338 (43.2) | 236 (30.2) | 103 (13.2) |
| Sleep Latency | 2.09 ± 1.137 | 118 (15.1) | 119 (15.2) | 121 (15.5) | 424 (54.2) |
| Sleep Duration | 1.42 ± 0.990 | 197 (25.2) | 153 (19.6) | 341 (43.6) | 91 (11.6) |
| Sleep Efficiency | 0.055 ± 0.905 | 523 (66.9) | 134 (17.1) | 76 (9.7) | 49 (6.3) |
| Disturbance | 1.06 ± 0.499 | 72 (9.2) | 590 (75.4) | 118 (15.1) | 2 (0.3) |
| Daytime Dysfunction | 1.54 ± 0.871 | 95 (12.1) | 271 (34.7) | 312 (39.9) | 104 (13.3) |
| Global PSQI score | 8.34± 3.456 | Minimum | Maximum | ||
| 0 | 18 | ||||
Sleep quality of medical students in relation to the academic year
Among the respondent medical students, 143 (34.9%) were in pre-clinical years (1st and 2nd), while 266 (64.9%) of them were in clinical years (3rd-5th). Table-IV shows that subjective sleep quality, sleep duration, and daytime dysfunction were poorer among pre-clinical students than clinical students (Table-III, IV).
Table IV.
Association between the academic year of medical students and PSQI score
| PSQI elements | Pre-clinical years Mean ± SD | Clinical years Mean ± SD | t-test | Significance level. |
|---|---|---|---|---|
| Subjective Sleep Quality | 1.52 ± 0.94 | 1.34 ± 0.86 | 1.973 | 0.049 |
| Sleep Latency | 1.85 ± 1.24 | 1.94 ± 1.17 | 0.729 | 0.466 |
| Sleep Duration | 1.52 ± 1.03 | 1.21 ± 0.96 | 3.048 | 0.002 |
| Habitual Sleep Efficiency | 0.63 ± 0.90 | 0.58 ± 0.93 | 0.527 | 0.598 |
| Disturbance | 0.98 ± 0.48 | 0.95 ± 0.45 | 0.581 | 0.562 |
| Daytime Dysfunction | 1.59 ± 0.87 | 1.42 ± 0.85 | 1.992 | 0.047 |
| Global PSQI | 8.30 | 7.76 | 1.506 | 0.133 |
Table III.
Association between medical and general science and PSQI score.
| PSQI elements | Medical students Mean ± SD | Science students Mean ± SD | t-test | Significance level. |
|---|---|---|---|---|
| Subjective Sleep Quality | 1.40 ± 0.89 | 1.46 ± 0.87 | -0.867 | 0.386 |
| Sleep Latency | 1.91 ± 1.2 | 2.29 ± 1 | -4.737 | 0.000 |
| Sleep Duration | 1.31 ± 0.99 | 1.53 ± 0.98 | -3.047 | 0.002 |
| Habitual Sleep Efficiency | 0.60 ± 0.92 | 0.51 ± 0.89 | 1.345 | 0.179 |
| Disturbance | 0.96 ± 0.47 | 1.18 ± 0.51 | -6.350 | 0.000 |
| Daytime Dysfunction | 1.48 ± 0.86 | 1.62 ± 0.88 | -2.212 | 0.027 |
| Global PSQI | 7.93 | 8.78 | -3.440 | 0.001 |
Sleep quality in relation to demographic factors
Out of the selected cases with poor sleep quality (≥5 PSQI score), 32.1% were males, and 67.9% were females. The majority of the respondents, i.e., 58.6%, had normal BMI, 21.7% overweight, 13.4% underweight, and 6.3% obese. It was found that sleep disturbance and daytime dysfunction were poorer in students with higher BMI ranges.
DISCUSSION
The present study findings during this critical time of COVID-19 pandemic and online teaching situation spotlight the sleeping health of college students, especially medical and science students, concerning the increasing demands of online teaching. The present study results reveal that 85.5% of the students had poor sleep quality with a mean PSQI global score (8.356) among them, 50.2% were medical, and 49.8% were science students. Sleep is a physiological process and is essential to normal body functions. Medical and science students are the most vulnerable groups to sleep deprivation and poor sleep quality. Their depleting state has become a global concern since its consequences adversely affect academic life and personal peace.21 As per various studies, medical students suffer from significant sleep issues, resulting in lower sleep duration.
Fig.1.
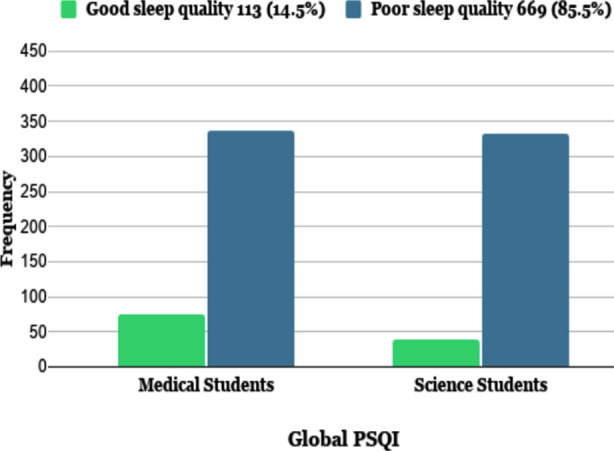
Global PSQI score for medical and science students.
Multiple factors are affecting sleep deprivations.22 This study has incorporated tests based on the data collected through PSQI interpretation concerning various differentiations and factors.22 The results acquired concerning the quality of sleep based on the difference of gender reflect that females are prone to suffer from sleep deprivation more than males. It demonstrates the need for measures to promote sleep awareness programs with gender-specific motives and attempts. And these findings are consistent with the literature.23
Another factor taken into consideration is the impact of BMI on sleep quality. The difference was found among obese or overweight respondents with issues like daytime dysfunction and disturbance. Even different studies also suggest that a higher weight can be associated with poor sleep quality.
This study investigates the sleep quality among science students in the gulf region. There is a deficit of international literature concerning science students’ sleep quality. While among medical students, according to a study conducted at King Saud Bin Abdulaziz University, medical students suffer from poor sleep quality due to the extensive academic workload, clinical responsibilities, stressful work environment, and an extremely challenging lifestyle.23 We found that the COVID-19 online teaching situation had contributed to a pronounced increase in the percentage of poor sleep quality among medical students in Saudi Arabia. A study conducted among medical students in King Saud University published in 2012 reported that only 36.3% of the students had poor sleep quality24 in contrast with our findings in the same college during the COVID-19 pandemic, which reported that 81.95% of medical students suffered from poor sleep quality. These percentages are alarming and rarely presented in the literature; it may be due to the increasing demands of online teaching and perhaps the psychological stress during the COVID-19 pandemic. On an international scope, a study in Pakistan showed that 67.3% of medical students and 50.4% of non-medical students were classified as poor sleepers.25
The assessment of sleep quality among medical students based on their academic year suggests that students in pre-clinical years have issues concerning subjective sleep quality, daytime dysfunction, and sleep duration. In other studies, the students in pre-clinical years face significant problems compared to others. As per a study conducted in a university in Brazil, the 1st and 2nd-year students suffered majorly due to adverse subjective sleep quality that is influenced due to the transition to medical curriculum and study schedule. It also highlighted the need for interventions among pre-clinical students to enhance their overall sleep quality.20
To sum up, sleep disturbances among university students show an alarming new trend with unbearable consequences on the mental health of university students.26 Moreover, during COVID 19 pandemic, sleep disturbances were reported in students26 and healthcare workers.27 It is quite a critical issue and is essential to develop a positive environment while offering substantial support. Various measures such as counseling facilities, providing academic guidance, and promoting positive sleep patterns could benefit. Also, with collaborative efforts, this situation can be improved to pursue a healthy, productive future.28
Study strengths and limitations
This sufficient sample size study compares sleep disturbance among university students during the COVID-19 pandemic. This study reported some interesting findings. However, this study has some limitations. First, the cross-sectional design limited the causality relationship interpretation, that COVID-19 is associated with sleep disturbance among university students. Second, our sample was restricted to King Saud University only. It would have been more appropriate to collect the data from other universities to extend our findings to the general population.
CONCLUSION
The COVID-19 pandemic has a negative impact on student’s mental health and sleep quality. The medical and science students showed alarming levels of sleep deprivation during the COVID-19 pandemic. The sleep deprivation among students may be due to the sudden change of pedagogy in education driven by the COVID-19 pandemic. The present study results may support implementing sleep education policies and academic counseling interventions to promote well-being in stressful conditions.
Author’s Contribution:
SAM, JMA, NFA: Research conceptualization, Manuscript writing.
WSA, AFA: Data collection, analysis, and literature review.
All authors have read and approved the manuscript and are responsible and accountable for the accuracy or integrity of the work.
Acknowledgments
We thank the “Researchers supporting project number (RSP- 2021/47), King Saud University, Riyadh, Saudi Arabia”. We thank May Ahmed Babaeer for her valid contribution in data collection and data-Analysis.
Footnotes
Conflicts of Interest: None.
REFERENCES
- 1.Meo SA, Bukhari IA, Akram J, Meo AS, Klonoff DC. COVID-19 vaccines:comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur Rev Med Pharmacol Sci. 2021;25(3):1663–669. doi: 10.26355/eurrev_202102_24877. doi:10.26355/eurrev_202102_24877. [DOI] [PubMed] [Google Scholar]
- 2.Meo SA, Abukhalaf AA, Alomar AA, Sattar K, Klonoff DC. COVID-19 Pandemic:Impact of Quarantine on Medical Students'Mental Wellbeing and Learning Behaviors. Pak J Med Sci. 2020;36(COVID19-S4):S43–S48. doi: 10.12669/pjms.36.COVID19-S4.2809. doi:10.12669/pjms.36.COVID19-S4.2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen NH, Hang LW, Lin CM. Sleep medicine in Taiwan. Sleep Biol Rhythms. 2016;14:11–19. doi: 10.1007/s41105-015-0007-9. doi:10.1007/s41105-015-0007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ. Sleep disturbances among medical students:A global perspective. J Clin Sleep Med. 2015;11:69–74. doi: 10.5664/jcsm.4370. doi:10.5664/jcsm.4370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shad R, Thawani R, Goel A. Burnout and Sleep Quality:A Cross-Sectional Questionnaire-Based Study of Medical and Non-Medical Students in India. Cureus. 2015;7:e361. doi: 10.7759/cureus.361. doi:10.7759/cureus.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawson HJ, Wellens-Mensah JT, Attah Nantogma S. Evaluation of Sleep Patterns and Self-Reported Academic Performance among Medical Students at the University of Ghana School of Medicine and Dentistry. Sleep Disord. 2019:1278579. doi: 10.1155/2019/1278579. doi:10.1155/2019/127Ↄ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayala EE, Berry R, Wiseman JS, Mason HR. A cross-sectional snapshot of sleep quality and quantity among US medical students. Acad Psychiat. 2017;41:664–672. doi: 10.1007/s40596-016-0653-5. [DOI] [PubMed] [Google Scholar]
- 8.Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiat Res. 2012;46:1618–1622. doi: 10.1016/j.jpsychires.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breath. 2014;18:257–63. doi: 10.1007/s11325-013-0874-8. doi:10.1007/s11325-013-0874-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozcan B, Acimis NM. Sleep Quality in Pamukkale University Students &its relationship with smartphone addiction. Pak J Med Sci. 2021;37(1):206–211. doi: 10.12669/pjms.37.1.3130. doi:10.12669/pjms.37.1.3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index:A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. doi:10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 12.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples:A systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Zailinawati A, Teng C, Chung Y, Teow T, Lee P, Jagmohni K. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64:108–118. [PubMed] [Google Scholar]
- 14.Deitch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in US college students. J Clin Sleep Med. 2016;12:1121–1129. doi: 10.5664/jcsm.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo S, Sun W, Liu C, Wu S. Structural validity of the Pittsburgh sleep quality index in Chinese undergraduate students. Frontiers Psychol. 2016;7:1126. doi: 10.3389/fpsyg.2016.01126. doi:10.3389/fpsyg.2016.01126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques D, Gomes AA, Meiavia A, Salgueiro A, Ribeiro CC, Dischler J. Reliability and initial validation of the Pittsburgh Sleep Quality Index, European Portuguese version:a preliminary study in a sample of higher education students. Sleep Med. 2013;14:e140. [Google Scholar]
- 17.Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh sleep quality index (PSQI) among Nigerian university students. Sleep Med. 2007;8:266–270. doi: 10.1016/j.sleep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Manzar MD, Moiz JA, Zannat W, Spence DW, Pandi-Perumal SR, BaHammam AS, et al. Validity of the Pittsburgh sleep quality index in Indian university students. Oman Med J. 2015;30:193. doi: 10.5001/omj.2015.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hashmi AM, Khawaja IS, Butt Z, Umair M, Naqvi SH, Ul-Haq J. The Pittsburgh sleeps quality index:Validation of the Urdu translation. J Coll Physicians Surg Pak. 2014;24:123–129. [PubMed] [Google Scholar]
- 20.Correa CdC, Oliveira FKd, Pizzamiglio DS, Ortolan EVP, Weber SAT. Sleep quality in medical students:a comparison across the various phases of the medical course. J Brasileiro de Pneumologia. 2017;43:285–294. doi: 10.1590/S1806-37562016000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IBM Support. using (SPSS) software version 26.0 for Mac. Available at: https://www.ibm.com/support/pages/downl oading-ibm-spss-statistics-26 . Cited date Oct 12, 2020.
- 22.Altun I, Cınar N, Dede C. The contributing factors to poor sleep experiences in according to the university students:A cross-sectional study. J Res Med Sci. 2012;17(6):557–561. [PMC free article] [PubMed] [Google Scholar]
- 23.Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. 2017;7(3):169–174. doi: 10.1016/j.jegh.2017.04.005. doi:10.1016/j.jegh.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Safhi MA, Alafif RA, Alamoudi NM, Alamoudi MM, Alghamdi WA, Albishri SF, Rizk H. The association of stress with sleep quality among medical students at King Abdulaziz University. J Family Med Prim Care. 2020;9(3):1662–1667. doi: 10.4103/jfmpc.jfmpc_745_19. doi:10.4103/jfmpc.jfmpc_745_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O'Halloran D, O'Boyle C, Doherty L. Poor Sleep Associated with Clinically Severe Obesity Is Independent of OSA Status. Obes Surg. 2021 Nov;31(11):4734–4740. doi: 10.1007/s11695-021-05588-3. doi:10.1007/s11695-021-05588-3. [DOI] [PubMed] [Google Scholar]
- 26.Nadeem A, Cheema MK, Naseer M, Javed H. Comparison of quality of sleep between medical &non-medical undergraduate Pakistani students. J Pioneer Med Sci. 2018;68:1465–1470. [PubMed] [Google Scholar]
- 27.Gruba G, Kasiak PS, Gębarowska J, Adamczyk N, Sikora Z, Jodczyk AM, et al. PaLS Study of Sleep Deprivation and Mental Health Consequences of the COVID-19 Pandemic among University Students:A Cross-Sectional Survey. Int J Environ Res Public Health. 2021;18(18):9581. doi: 10.3390/ijerph18189581. doi:10.3390/ijerph18189581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meo SA, Alkhalifah JM, Alshammari NF, Alnufaie WS. Comparison of Generalized Anxiety and Sleep Disturbance among Frontline and Second-Line Healthcare Workers during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18(11):5727. doi: 10.3390/ijerph18115727. doi:10.3390/ijerph18115727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basu M, Saha SK, Majumder S, Chatterjee S, Misra R. A Study on Sleeping Pattern among Undergraduate Medical Students of a Tertiary Care Teaching Hospital of Kolkata. Int J Med Pub Health. 2019;9:118–124. [Google Scholar]


