Abstract
Introduction: Poor physical performance has been shown to be a good predictor of complications in some pathologies. The objective of our study was to evaluate, in patients with colorectal neoplasia prior to surgery, physical performance and its relationship with postoperative complications and in-hospital mortality, at 1 month and at 6 months. Methods: We conducted a prospective study on patients with preoperative colorectal neoplasia, between October 2018 and July 2021. Physical performance was evaluated using the Short Physical Performance Battery (SPPB) test and hand grip strength (HGS). For a decrease in physical performance, SPPB < 10 points or HGS below the EWGSOP2 cut-off points was considered. Nutritional status was evaluated using subjective global assessment (SGA). The prevalence of postoperative complications and mortality during admission, at 1 month, and at 6 months was evaluated. Results: A total of 296 patients, mean age 60.4 ± 12.8 years, 59.3% male, were evaluated. The mean BMI was 27.6 ± 5.1 kg/m2. The mean total SPPB score was 10.57 ± 2.07 points. A total of 69 patients presented a low SPPB score (23.3%). Hand grip strength showed a mean value of 33.1 ± 8.5 kg/m2 for men and 20.7 ± 4.3 kg/m2 for women. A total of 58 patients presented low HGS (19.6%). SGA found 40.2% (119) of patients with normal nourishment, 32.4% (96) with moderate malnutrition, and 27.4% (81) with severe malnutrition. Postoperative complications were more frequent in patients with a low SPPB score (60.3% vs. 38.6%; p = 0.002) and low HGS (64.9% vs. 39.3%, p = 0.001). A low SPPB test score (OR 2.57, 95% CI 1.37–4.79, p = 0.003) and low HGS (OR 2.69, 95% CI 1.37–5.29, p = 0.004) were associated with a higher risk of postoperative complications after adjusting for tumor stage and age. Patients with a low SPPB score presented an increase in in-hospital mortality (8.7% vs. 0.9%; p = 0.021), at 1 month (8.7% vs. 1.3%; p = 0.002) and at 6 months (13.1% vs. 2.2%, p < 0.001). Patients with low HGS presented an increase in mortality at 6 months (10.5% vs. 3.3%; p = 0.022). Conclusions: The decrease in physical performance, evaluated by the SPPB test or hand grip strength, was elevated in patients with colorectal cancer prior to surgery and was related to an increase in postoperative complications and mortality.
Keywords: physical performance, malnutrition, cancer, oncology, colorectal, surgery
1. Introduction
Colorectal cancer is the second most deadly and third most commonly diagnosed cancer in the world, and its global incidence and mortality are likely to increase in the coming decades. Surgery is the priority approach in most cases, especially in the early stages [1].
The oncological process and the surgery itself involve an inflammation process that leads to a metabolic stress response [2,3]. Patients with cancer present a degree of malnutrition due to their own underlying disease that conditions greater morbidity and mortality [4]. In addition, during surgery, a hypermetabolic response is produced with great catabolism, which leads to a nutritional and immune deficit [5]. In the response to this stress situation, the nutritional status and functional reserve are particularly relevant.
The prevalence of frailty in cancer patients undergoing colorectal surgery was 22.7% in a recent study [6]. Some studies have observed that a poor functional performance in the preoperative period is associated with higher postoperative morbidity [7], whereas an improvement in functional performance is related to a decrease in postoperative complications [8].
One of the most used tools for assessing functional capacity is the Short Performance Battery Test (SPPB). The SPPB is an effective tool for the assessment of physical function, developed by Guralnik [9]. This tool combines measurements of balance (standing, tandem, and semi-tandem), gait (4 m gait speed), strength, and endurance (rising from chair). Its score correlates significantly with institutionalization and mortality. It is validated to detect frailty and has high reliability in predicting disability [10].
On the other hand, about 35% of patients undergoing colorectal surgery are moderately to severely malnourished before surgery [11]. Malnutrition significantly affects the evolution of the surgical process with an unfavorable impact on the gastrointestinal tract, the endocrinological and immune systems, and cardiorespiratory function; delays wound healing, which implies an increase in morbidity, mortality, and hospital stay, with a consequent increase in health care costs [12].
As far as we know, the influence of preoperative physical performance using the SPPB and hand grip strength on postoperative complications and mortality in patients undergoing colorectal cancer has not been investigated.
Our hypothesis is that poor preoperative physical performance evaluated by the SPPB test and HGS in these patients is associated with postoperative complications and mortality regardless of nutritional status.
Hence, the aim of the present study was to evaluate the impact of preoperative physical performance evaluated by SPPB test and HGS on postoperative complications and mortality in patients undergoing colorectal cancer surgery.
2. Materials and Methods
We conducted a prospective study on patients with a diagnosis of colorectal cancer, between October 2018 and July 2021. All the patients proposed for intervention at the Coloproctology Unit of the Hospital Regional Universitario de Malaga were evaluated. All assessed patients who signed the informed consent were included. Data about the type of neoplasm and tumor stage were collected.
2.1. Assessment of Nutritional Status
A nutritional assessment which included subjective global assessment (SGA) [13] was performed. The following anthropometric measures were obtained: weight, height, and BMI. Height was calculated at baseline with a stadiometer (Holtain Limited, Crymych, UK), and weight was calculated with a weighing scale adjusted to 0.1 kg (SECA 665, Hamburg, Germany). Brachial circumference was measured using a flexible and non-elastic tape. Fasting blood was collected from the pre-anesthetic study, including albumin and C-reactive protein (CRP).
Malnourished or at-risk patients received a nutritional intervention appropriate to routine clinical practice [2].
2.2. Physical Performance
The Short Physical Performance Battery (SPPB) test was used to measure physical performance [9]. The SPPB test comprises three items: standing balance, walking speed, and chair stands. Each item was evaluated on a scale from 0 (inability to complete) to 4 (best performance possible).
In accordance with previous studies [14,15,16], patients were classified into low physical performance-related risk (SPPB total score < 10) or no physical performance-related risk (SPPB total score ≥ 10).
Hand grip strength was measured using the dominant hand with a Jamar dynamometer (Asimow Engineering Co., Los Angeles, CA, USA). For this test, the patients were sat comfortably with the shoulder adducted, the forearm neutrally rotated, the elbow flexed to 90°, and the forearm and wrist in a neutral position. They were told to perform 3 consecutive contractions one minute apart from each other, and the mean value was calculated.
2.3. Clinical Outcomes
Data concerning postoperative complications [17] and mortality during admission, at 1 month, and at 6 months were collected.
2.4. Data Analysis
Quantitative variables were expressed as the mean ± standard deviation. Comparison between qualitative variables was conducted via a chi-square test, with Fisher correction if necessary. The quantitative variable distribution was assessed by the Kolmogorov–Smirnov test. Differences between quantitative variables were analyzed using Student’s t-test and, for variables not following a normal distribution, using non-parametric tests (Mann–Whitney or Kruskal–Wallis). We designed multivariate logistic regression models in which the dependent variable was the presence of postoperative complications, also controlling for sex, age, and stage of tumor. For calculations, significance was set at p < 0.05 for two tails. The data analysis was performed with the SPSS 22.0 program (SPSS Inc., Chicago, IL, USA, 2013).
2.5. Ethics
The Provincial Research Ethics Committee of Málaga approved the study and informed consent was obtained from all participants. The ethical principles included in the latest revision of the Declaration of Helsinki and good clinical practice standards were applied.
3. Results
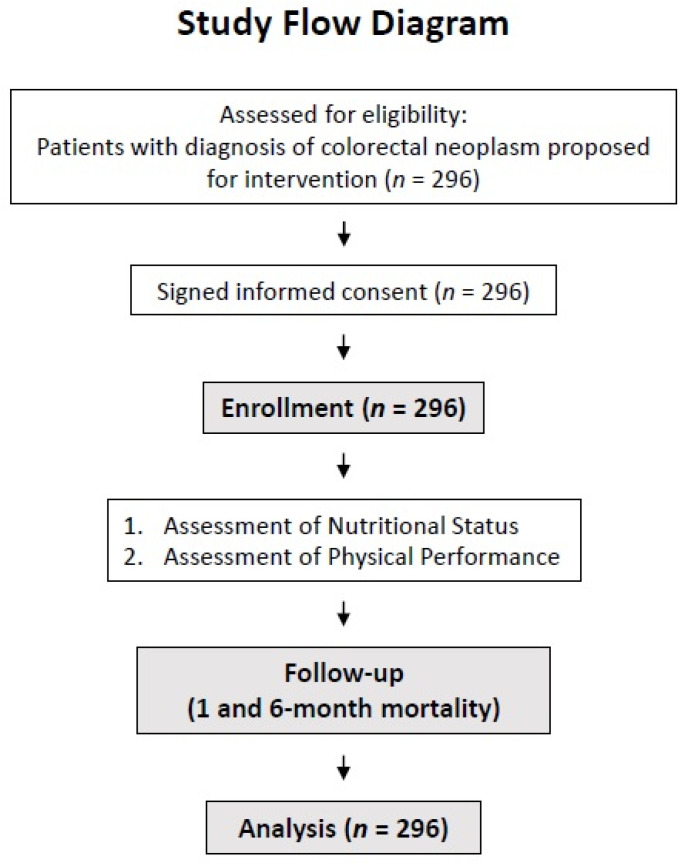
A total of 296 patients were evaluated (Figure 1). Their mean age was of 60.4 ± 12.8 years, and 59.3% of them were male. Their general features are displayed in Table 1.
Figure 1.
Study flow diagram.
Table 1.
General features.
| n = 296 | ||
| Age (years) | mean ± SD (min–max) | 68.4 ± 10.2 (30–89) |
| Sex | n (%) | |
| Men | 175 (59.1) | |
| Women | 121 (40.9) | |
| Type of cancer | n (%) | |
| Colon | 180 (60.8) | |
| Rectum | 116 (39.2) | |
| Stage | n (%) | |
| I | 39 (13.1) | |
| II | 99 (33.5) | |
| III | 124 (41.9) | |
| IV | 34 (11.5) | |
| BMI (kg/m2) | mean ± SD (min–max) | |
| Men | 27.6 ± 5.1 (17.2–47.6) | |
| Women | 26.5 ± 5.3 (15.8–46.1) | |
| Surgical complications | n (%) | 131 (44.2) |
| Postoperative collection | 24 (18.3) | |
| Paralytic ileus | 23 (17.6) | |
| Surgical wound infection | 23 (17.6) | |
| Suture dehiscence | 16 (12.2) | |
| Febrile syndrome | 13 (9.9) | |
| Bleeding | 12 (9.2) | |
| Other | 20 (15.3) | |
| In-hospital exitus | n (%) | 8 (2.7) |
| 1-month exitus | n (%) | 9 (3) |
| 6-month exitus | n (%) | 14 (4.7) |
Abbreviations: BMI = body mass index; SD = standard deviation.
Colon cancer was the most frequent type of cancer (60.8%), while most of the patients were at stages II and III (75.4%).
The mean BMI was 27.6 ± 5.1 kg/m2. More than half of the patients (62.5%) were overweight, and 24.3% of them were obese.
The results of the functional tests are shown in Table 2. No significant differences were found in the SPPB total score between genders.
Table 2.
Short Physical Performance Battery (SPPB) test and hand grip strength.
| n = 296 | ||
| SPPB | ||
| Balance (points) | mean ± SD | 3.81 ± 0.48 |
| 4 m gait speed (points) | mean ± SD | 3.60 ± 0.83 |
| Sit to stand (points) | mean ± SD | 3.14 ± 1.14 |
| Total (points) | mean ± SD | 10.57 ± 2.07 |
| SPPB < 10 (low physical performance) | n (%) | 69 (23.3%) |
| SPPB ≥ 10 | n (%) | 227 (76.7%) |
| Hand grip strength | ||
| Men | mean ± SD (min–max) | 34.01 ± 8.57 (13.3–57.8) |
| Women | mean ± SD (min–max) | 21.03 ± 5.09 (10.6–34) |
| Low hand grip strength | n (%) | 58 (19.6%) |
| Normal hand grip strength | n (%) | 238 (80.4%) |
Abbreviations: SD = standard deviation.
After the categorization of patients according to their physical performance, 227 patients (76.7%) presented a normal score in the SPPB test (≥10), and 69 (23.3%) presented a low score (<10). The age of the low-SPPB group (73.1 ± 10 years) was significantly higher than that of the high-SPPB group (67.1 ± 9.9 years, p < 0.001), and a low SPPB score was more frequent in women (29.4% vs. 18.7%, p = 0.047). There were no significant differences in the type of cancer (colon or rectum, p < 0.257) or in the stage of tumor (p = 0.95). The high-SPPB group had a greater length of stay than the low-SPPB group (p = 0.018).
A total of 58 patients (19.6%) presented low hand grip strength, and 238 patients (80.4%) presented normal values.
Differences between the SPPB and hand grip strength groups are shown in Table 3.
Table 3.
Differences between the SPPB and hand grip strength groups.
| SPPB ≥ 10 (n = 227) Mean ± SD |
SPPB < 10 (n = 69) Mean ± SD |
p Value | Normal Hand Grip Strength (n = 238) Mean ± SD |
Low Hand Grip Strength (n = 58) Mean ± SD |
p Value | |
|---|---|---|---|---|---|---|
| Age (years) | 67 ± 9.9 | 73.2 ± 9.9 | <0.001 | 67 ± 10 | 74.3 ± 9.2 | <0.001 |
| BMI (kg/m2) | 26.9 ± 4.9 | 27.7 ± 6.3 | 0.29 | 27.5 ± 5.3 | 25.8 ± 5.1 | 0.033 |
| Hand grip strength (kg) | ||||||
| Men | 35.2 ± 7.7 | 25.4 ± 6.5 | <0.001 | 37.3 ± 6.1 | 21.8 ± 4 | <0.001 |
| Women | 22.7 ± 4.5 | 17.1 ± 4.2 | <0.001 | 22.6 ± 4 | 13.3 ± 1.6 | <0.001 |
| Brachial circumference (cm) | 28.8 ± 3.8 | 28.4 ± 4.8 | 0.49 | 29.1 ± 3.8 | 27 ± 4.6 | <0.001 |
| Albumin (g/dL) | 3.7 ± 0.5 | 3.5 ± 0.5 | 0.003 | 3.7 ± 0.4 | 3.5 ± 0.6 | 0.006 |
| CRP (mg/dL) | 7.7 ± 11.8 | 17.9 ± 26 | 0.003 | 7.1 ± 9 | 19.5 ± 29 | <0.001 |
| CRP/albumin ratio | 2.3 ± 3.9 | 6.7 ± 11.7 | 0.001 | 2 ± 2.7 | 7.4 ± 12.4 | <0.001 |
| Length of stay (days) | 11.1 ± 8.9 | 14.1 ± 9.4 | 0.018 | 11.2 ± 9.2 | 13.8 ± 8.1 | 0.058 |
Abbreviations: SPPB = Short Physical Performance Battery; SD = standard deviation; BMI = body mass index; CRP = C-reactive protein.
SGA found 40.2% (119) of patients with normal nourishment, 32.4% (96) with moderate malnutrition, and 27.4% (81) with severe malnutrition (59.8% with malnutrition or at risk). Malnourished patients presented a low SPPB score (28.3% vs. 15.4%, p = 0.011) and low dynamometry (24.4% vs. 11.8%, p = 0.007) more frequently.
Postoperative complications were more frequent in patients with a low SPPB score (60.3% vs. 38.6%; p = 0.002) and low hand grip strength (64.9% vs. 39.3%, p = 0.001). No difference was found in the frequency of postoperative complications or mortality in malnourished patients according to SGA (p = 0.86).
Multivariable logistic regression analyses showed that a low SPPB score and low hand grip strength were associated with a higher risk of postoperative complications after adjusting for confounding variables such as age, gender, and stage of tumor (Table 4).
Table 4.
Risk of presenting postoperative complications, adjusted for age, gender, and stage of tumor.
| Crude | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p Value | Odds Ratio | 95% CI | p Value | |||
| Lower | Upper | Lower | Upper | |||||
| Low SPPB | 2.37 | 1.35 | 4.17 | 0.003 | 2.52 | 1.35 | 4.70 | 0.004 |
| Low hand grip strength | 2.77 | 1.51 | 5.07 | 0.001 | 2.62 | 1.33 | 5.13 | 0.005 |
Abbreviations: SPPB = Short Physical Performance Battery; CI = confidence interval.
During hospital admission, eight patients (2.7%) died, increasing to nine (3%) one month after the intervention. After six months, 4.7% (14) of the patients were deceased.
An increased risk of mortality was found among patients with a low SPPB score and low hand grip strength (Table 5). No differences were found in mortality at any time according to malnutrition.
Table 5.
Relationship between low physical function and mortality.
| In-Hospital Mortality | 1-Month Mortality | 6-Month Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Low | p Value | Normal | Low | p Value | Normal | Low | p Value | |
| SPPB | 2 (0.9%) | 6 (8.7%) | 0.021 | 3 (1.3%) | 6 (8.7%) | 0.002 | 2 (2.2%) | 9 (13.1%) | <0.001 |
| Hand grip strength | 5 (2.1%) | 3 (5.3%) | 0.187 | 6 (2.5%) | 3 (5.3%) | 0.280 | 8 (3.3%) | 6 (10.5%) | 0.022 |
Abbreviations: SPPB = Short Physical Performance Battery.
4. Discussion
To our knowledge, this is the first study to evaluate the influence of preoperative physical performance using the SPPB and hand grip strength on postoperative complications and mortality in patients undergoing colorectal cancer surgery. Our main finding was that a low preoperative physical performance was frequent and was associated with postoperative complications and mortality.
The Short Physical Performance Battery (SPPB) is a useful, three-part assessment and well-established tool for evaluating physical performance [9,18]. It evaluates three physical measurements that include standing balance, walking speed, and chair stands. In this way, it assesses different aspects of physical performance and function of the lower extremities, making it an excellent tool to identify frailty in adults [19]. The SBBP has many advantages: it requires little training to carry it out, takes only a few minutes to complete, and can be performed in a small space. Further, the results are reproducible and sensitive to changes in functionality through time [20]. Previous studies showed a significant trend toward age-related functional decline, with some differences between men and women [20]. In our study, patients with a low SPPB score were older than those with SPPB > 10, but no significant differences were found in the SPPB total score between genders. Despite the obvious relationship between the loss of functional capacity and age, the permanence of the effect of a low SPPB score on clinical outcomes after adjusting the logistic regression for age reinforces the importance of the functional status of these patients.
In our results, a low SPPB score was correlated with a higher frequency of postoperative complications. In a Japanese study, it was found that a poor physical performance measured by the SPPB test can be predictive of postoperative pulmonary complications after lung resection surgery [21]. Similarly, an impaired preoperative physical performance determined by the SPPB has been associated with a worse postoperative outcome after cardiac surgery, pancreaticoduodenectomy, and lung and kidney transplant surgeries [14,15,16,21]. A systematic review [22] showed that physical performance tests, including the SPPB, seem to correlate significantly with survival, which is consistent with the results of our study.
Hand grip strength is often cited as an indirect measure of malnutrition and a reliable prognostic tool [23] and correlates well with fat-free mass [24]. Low hand grip strength is associated with aging, but regardless of this relationship, it has been shown to be a powerful predictor of disability, morbidity, and mortality, and, by itself, a good marker of frailty [25]. Along those lines, in the present study, we found that low preoperative HGS is a good predictor of postoperative complications and mortality, with results comparable to those found with the SPPB test.
In our sample, 62.5% of the patients were overweight, and 24.3% of them were obese, exceeding series previously described in similar patients [26]. Only 8.1% of the subjects were below the established cut-off points for a low BMI [27]. The presence of a high percentage of patients with impaired physical performance and a high prevalence of overweight suggests a significant presence of sarcopenic obesity, an entity that is difficult to diagnose without morphofunctional tests in patients in the early stages of the tumor. The presence of both obesity and sarcopenia leads to particularly bad clinical outcomes. A meta-analysis showed that the presence of sarcopenia was associated with an increased risk of complications after gastrointestinal tumor resection [28], and sarcopenic obesity has been specifically associated with a lower survival rate in several populations [28,29].
The prevalence of malnutrition in our study was high at 59.8%; this figure is similar to others previously found [4]. SGA has been used previously in patients with colorectal cancer, finding a prevalence between 35 and 40% [11,30]. A Japanese study found a prevalence of preoperative malnutrition of 23.6%, which was associated with postoperative complications, overall survival, and disease-free survival in colorectal cancer patients after radical resection surgery [31]. These findings were also corroborated by the results from a large population database from the United States [32].
A worse nutritional status is associated with worse functional walking capacity and hand grip strength [26], but some studies have shown that functional assessment techniques such as hand grip strength are independent predictors of clinical outcomes regardless of the diagnosis of malnutrition, so these techniques provide an additional predictive value. These results suggest that the use of malnutrition and physical performance tools in combination may be valuable in hospital settings [33]. Although the close relationship between malnutrition and postoperative outcomes seems evident, in our study, no relationship was found between the two. Although causal relationships cannot be established due to the study design, we postulate that this relationship was interfered with by the nutritional intervention performed in all patients with malnutrition or at risk [34].
Malnutrition and physical performance screening is not routinely practiced before surgery [26]. Our findings support the use of the SPPB and HGS to evaluate physical function in cancer patients in addition to malnutrition screening before colorectal cancer surgery.
An early awareness of impaired physical performance and nutritional status would allow an early onset of dietary, physical exercise, and, if needed, pharmacological interventions. Exercise prescription for diseases is becoming a standard practice worldwide, and several scientific reports highlight its growing role [35]. The introduction of a program of prehabilitation, including both nutritional and exercise interventions, seems to be justified. Thereby, there are studies that showed that exercise prehabilitation reduced postoperative complications in high-risk patients scheduled to undergo elective colon resection [36]. Likewise, a randomized controlled trial found that multimodal prehabilitation improves functional capacity before and after surgery, enhancing postoperative clinical outcomes [37]. Finally, a systematic review and meta-analysis showed that exercise, nutritional, and multimodal prehabilitation may reduce morbidity after abdominal surgery in patients with cancer [38].
Our study has several strengths: it was a prospective study with a considerable number of subjects and with long-term monitoring, using tools that can be easily used at the hospital and outpatient levels.
All the same, there are potential limitations in our study. It was a single-center, observational study; therefore, the results should be interpreted with caution, and causal links cannot be established. On the other hand, the SPPB can have a ceiling effect affecting patients with an optimal functional status [20]. In this study, 50% of the subjects had a full score on the SPPB, and the effect of the ceiling effect of the SPPB may be present. Finally, the fact of having a systematic nutritional intervention protocol may have influenced the results with a lack of association between malnutrition and clinical outcomes, compared to other studies.
5. Conclusions
Low physical performance, assessed by the SPPB and HGS, was elevated in colorectal cancer patients prior to surgery and was associated with postoperative complications and mortality. Assessing patients undergoing colorectal cancer surgery using the SPPB and HGS could help stratify patients at risk of postoperative complications and mortality. Therefore, consideration of preoperative countermeasures against impaired physical performance is necessary.
Acknowledgments
The authors would like to thank all the individuals who participated in this study for their willingness to collaborate. The authors are grateful for the grants received from SANCYD and Persan Farma, which allowed this study to be performed.
Author Contributions
Conceptualization, F.J.S.-T., M.G.-M., I.G.-P. and G.O.; formal analysis, F.J.S.-T. and G.O.; investigation, F.J.S.-T., M.J.T., I.G.-P., S.M.-V., J.A.T.-M., M.R.-L. and J.C.-C.; resources, J.S.-S. and G.O.; data curation, F.J.S.-T., M.G.-O. and N.P.; writing—original draft preparation, F.J.S.-T.; writing—review and editing, F.J.S.-T. and G.O.; supervision, G.O.; project administration, J.S.-S. and G.O.; funding acquisition, G.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by the 2019 research grants of SANCYD (Sociedad Andaluza de Nutrición Clínica y Dietética) and by an unrestricted grant from Persan Farma.
Institutional Review Board Statement
This study was approved by the Provincial Research Ethics Committee of Málaga (reference number #26072018), and informed consent was obtained from all participants. The ethical principles included in the latest revision of the Declaration of Helsinki and good clinical practice standards were applied.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sawicki T., Ruszkowska M., Danielewicz A., Niedźwiedzka E., Arłukowicz T., Przybyłowicz K.E. A Review of Colorectal Cancer in Terms of Epidemiology, Risk Factors, Development, Symptoms and Diagnosis. Cancers. 2021;13:2025. doi: 10.3390/cancers13092025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muscaritoli M., Arends J., Bachmann P., Baracos V., Barthelemy N., Bertz H., Bozzetti F., Hütterer E., Isenring E., Kaasa S., et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021;40:2898–2913. doi: 10.1016/j.clnu.2021.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Weimann A., Braga M., Carli F., Higashiguchi T., Hübner M., Klek S., Laviano A., Ljungqvist O., Lobo D.N., Martindale R., et al. ESPEN guideline: Clinical nutrition in surgery. Clin. Nutr. 2017;36:623–650. doi: 10.1016/j.clnu.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Martens E.A., Gonnissen H.K., Gatta-Cherifi B., Janssens P.L., Westerterp-Plantenga M.S. ESPEN practical guideline: Clinical nutrition in surgery. Clin. Nutr. 2021;40:4745–4761. doi: 10.1016/J.CLNU.2021.03.031. [DOI] [PubMed] [Google Scholar]
- 5.Horowitz M., Neeman E., Sharon E., Ben-Eliyahu S. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat. Rev. Clin. Oncol. 2015;12:213–226. doi: 10.1038/nrclinonc.2014.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsai H.-F., Liu C.-Y., Yang S.-H., Chiou A.-F. Factors Related to Frailty in Older Cancer Patients Undergoing Colorectal Surgery. Cancer Nurs. 2021 doi: 10.1097/NCC.0000000000001017. [DOI] [PubMed] [Google Scholar]
- 7.Lee L., Schwartzman K., Carli F., Zavorsky G.S., Li C., Charlebois P., Stein B., Liberman A.S., Fried G.M., Feldman L.S. The association of the distance walked in 6 min with pre-operative peak oxygen consumption and complications 1 month after colorectal resection. Anaesthesia. 2013;68:811–816. doi: 10.1111/anae.12329. [DOI] [PubMed] [Google Scholar]
- 8.Minnella E.M., Liberman A.S., Charlebois P., Stein B., Scheede-Bergdahl C., Awasthi R., Gillis C., Bousquet-Dion G., Ramanakuma A.V., Pecorelli N., et al. The impact of improved functional capacity before surgery on postoperative complications: A study in colorectal cancer. Acta Oncol. 2019;58:573–578. doi: 10.1080/0284186X.2018.1557343. [DOI] [PubMed] [Google Scholar]
- 9.Guralnik J.M., Simonsick E.M., Ferrucci L., Glynn R.J., Berkman L.F., Blazer D.G., Scherr P.A., Wallace R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- 10.Zugasti Murillo A., Casas Herrero Á. Frailty syndrome and nutritional status: Assessment, prevention and treatment. Nutr. Hosp. 2019;36:26–37. doi: 10.20960/NH.02678. [DOI] [PubMed] [Google Scholar]
- 11.Lohsiriwat V. The influence of preoperative nutritional status on the outcomes of an enhanced recovery after surgery (ERAS) programme for colorectal cancer surgery. Tech. Coloproctology. 2014;18:1075–1080. doi: 10.1007/s10151-014-1210-4. [DOI] [PubMed] [Google Scholar]
- 12.Parekh N.R., Steiger E. Percentage of Weight Loss as a Predictor of Surgical Risk: From the Time of Hiram Studley to Today. Nutr. Clin. Pract. 2004;19:471–476. doi: 10.1177/0115426504019005471. [DOI] [PubMed] [Google Scholar]
- 13.Detsky A.S., McLaughlin J.R., Baker J.P., Johnston N., Whittaker S., Mendelson R.A., Jeejeebhoy K.N. What is subjective global assessment of nutritional status? J. Parenter. Enter. Nutr. 1987;11:8–13. doi: 10.1177/014860718701100108. [DOI] [PubMed] [Google Scholar]
- 14.Dale W., Hemmerich J., Kamm A., Posner M.C., Matthews J.B., Rothman R., Palakodeti A., Roggin K.K. Geriatric assessment improves prediction of surgical outcomes in older adults undergoing pancreaticoduodenectomy: A prospective cohort study. Ann. Surg. 2014;259:960–965. doi: 10.1097/SLA.0000000000000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kato M., Saitoh M., Kawamura T., Iwata K., Sakurada K., Okamura D., Tahara M., Yuguchi S., Kamisaka K., Oura K., et al. Postoperative atrial fibrillation is associated with delayed early rehabilitation after heart valve surgery: A multicenter study. Phys. Ther. Res. 2019;22:E9957. doi: 10.1298/ptr.E9957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nastasi A.J., Bryant T.S., Le J.T., Schrack J., Ying H., Haugen C.E., Fernández M.G., Segev D.L., McAdams-DeMarco M.A. Pre-kidney transplant lower extremity impairment and transplant length of stay: A time-to-discharge analysis of a prospective cohort study. BMC Geriatr. 2018;18:246. doi: 10.1186/s12877-018-0940-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirchhoff P., Clavien P.-A., Hahnloser D. Complications in colorectal surgery: Risk factors and preventive strategies. Patient Saf. Surg. 2010;4:5. doi: 10.1186/1754-9493-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pavasini R., Guralnik J., Brown J.C., Di Bari M., Cesari M., Landi F., Vaes B., Legrand D., Verghese J., Wang C., et al. Short Physical Performance Battery and all-cause mortality: Systematic review and meta-analysis. BMC Med. 2016;14:215. doi: 10.1186/s12916-016-0763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abizanda P., Romero L., Sanchez-Jurado P., Atienzar-Núñez P., Esquinas-Requena J., Garcia-Nogueras I. Association between Functional Assessment Instruments and Frailty in Older Adults: The FRADEA Study. J. Frailty Aging. 2012;1:162–168. doi: 10.14283/jfa.2012.25. [DOI] [PubMed] [Google Scholar]
- 20.Bergland A., Strand B.H. Norwegian reference values for the Short Physical Performance Battery (SPPB): The Tromsø Study. BMC Geriatr. 2019;19:216. doi: 10.1186/s12877-019-1234-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuguchi S., Saitoh M., Oura K., Tahara M., Kamisaka K., Kawamura T., Kato M., Morisawa T., Takahashi T. Impact of preoperative frailty on regaining walking ability in patients after cardiac surgery: Multicenter cohort study in Japan. Arch. Gerontol. Geriatr. 2019;83:204–210. doi: 10.1016/j.archger.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Verweij N.M., Schiphorst A.H.W., Pronk A., Bos F.V.D., Hamaker M.E. Physical performance measures for predicting outcome in cancer patients: A systematic review. Acta Oncol. 2016;55:1386–1391. doi: 10.1080/0284186X.2016.1219047. [DOI] [PubMed] [Google Scholar]
- 23.Contreras-Bolívar V., Sánchez-Torralvo F.J., Ruiz-Vico M., González-Almendros I., Barrios M., Padín S., Alba E., Olveira G. GLIM criteria using hand grip strength adequately predict six-month mortality in cancer inpatients. Nutrients. 2019;11:2043. doi: 10.3390/nu11092043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torralvo F.J.S., Porras N., Fernandez J.A., Torres F.G., Tapia M.J., Lima F., Soriguer F., Gonzalo M., Martínez G.R., Olveira G. Normative reference values for hand grip dynamometry in Spain. Association with lean mass. Nutr. Hosp. 2018;35:98–103. doi: 10.20960/nh.1052. [DOI] [PubMed] [Google Scholar]
- 25.Syddall H., Cooper C., Martin F., Briggs R., Sayer A.A. Is grip strength a useful single marker of frailty? Age Ageing. 2003;32:650–656. doi: 10.1093/ageing/afg111. [DOI] [PubMed] [Google Scholar]
- 26.Gillis C., Richer L., Fenton T.R., Gramlich L., Keller H., Culos-Reed S.N., Sajobi T.T., Awasthi R., Carli F. Colorectal cancer patients with malnutrition suffer poor physical and mental health before surgery. Surgery. 2021;170:841–847. doi: 10.1016/j.surg.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Cederholm T., Jensen G.L., Correia M.I.T.D., Gonzalez M.C., Fukushima R., Higashiguchi T., Baptista G., Barazzoni R., Blaauw R., Coats A.J., et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. J. Cachexia Sarcopenia Muscle. 2019;10:207–217. doi: 10.1002/jcsm.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prado C.M., Lieffers J.R., McCargar L.J., Reiman T., Sawyer M.B., Martin L., Baracos V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008;9:629–635. doi: 10.1016/S1470-2045(08)70153-0. [DOI] [PubMed] [Google Scholar]
- 29.Mintziras I., Miligkos M., Wächter S., Manoharan J., Maurer E., Bartsch D.K. Sarcopenia and sarcopenic obesity are significantly associated with poorer overall survival in patients with pancreatic cancer: Systematic review and meta-analysis. Int. J. Surg. 2018;59:19–26. doi: 10.1016/j.ijsu.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Barbosa L.R.L.S., Lacerda-Filho A., Barbosa L.C.L.S. Immediate preoperative nutritional status of patients with colorectal cancer: A warning. Arq. Gastroenterol. 2014;51:331–336. doi: 10.1590/S0004-28032014000400012. [DOI] [PubMed] [Google Scholar]
- 31.Song H.-N., Wang W.-B., Luo X., Huang D.-D., Ruan X.-J., Xing C.-G., Chen W.-Z., Dong Q.-T., Chen X.-L. Effect of GLIM-defined malnutrition on postoperative clinical outcomes in patients with colorectal cancer. Jpn. J. Clin. Oncol. 2022 doi: 10.1093/jjco/hyab215. [DOI] [PubMed] [Google Scholar]
- 32.Lee D.U., Fan G.H., Hastie D.J., Addonizio E.A., Suh J., Prakasam V.N., Karagozian R. The clinical impact of malnutrition on the postoperative outcomes of patients undergoing colorectal resection surgery for colon or rectal cancer: Propensity score matched analysis of 2011-2017 US hospitals. Surg. Oncol. 2021;38:101587. doi: 10.1016/j.suronc.2021.101587. [DOI] [PubMed] [Google Scholar]
- 33.Laur C.V., McNicholl T., Valaitis R., Keller H.H. Malnutrition or frailty? Overlap and evidence gaps in the diagnosis and treatment of frailty and malnutrition. Appl. Physiol. Nutr. Metab. 2017;42:449–458. doi: 10.1139/apnm-2016-0652. [DOI] [PubMed] [Google Scholar]
- 34.Williams D.G.A., Ohnuma T., Krishnamoorthy V., Raghunathan K., Sulo S., Cassady B.A., Hegazi R., Wischmeyer P.E. Impact of early postoperative oral nutritional supplement utilization on clinical outcomes in colorectal surgery. Perioper. Med. 2020;9:29. doi: 10.1186/s13741-020-00160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palermi S., Iacono O., Sirico F., Modestino M., Ruosi C., Spera R., De Luca M. The complex relationship between physical activity and diabetes: An overview. J. Basic Clin. Physiol. Pharmacol. 2021 doi: 10.1515/jbcpp-2021-0279. [DOI] [PubMed] [Google Scholar]
- 36.Berkel A.E.M., Bongers B.C., Kotte H., Weltevreden P., de Jongh F.H.C., Eijsvogel M.M.M., Wymenga M., Bigirwamungu-Bargeman M., van der Palen J., van Det M.J., et al. Effects of Community-based Exercise Prehabilitation for Patients Scheduled for Colorectal Surgery with High Risk for Postoperative Complications: Results of a Randomized Clinical Trial. Ann. Surg. 2021;275:e299–e306. doi: 10.1097/SLA.0000000000004702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barberan-Garcia A., Ubré M., Roca J., Lacy A.M., Burgos F., Risco R., Momblán D., Balust J., Blanco I., Martínez-Pallí G. Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann. Surg. 2018;267:50–56. doi: 10.1097/SLA.0000000000002293. [DOI] [PubMed] [Google Scholar]
- 38.Daniels S.L., Lee M.J., George J., Kerr K., Moug S., Wilson T.R., Brown S.R., Wyld L. Prehabilitation in elective abdominal cancer surgery in older patients: Systematic review and meta-analysis. BJS Open. 2020;4:1022–1041. doi: 10.1002/bjs5.50347. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.