Abstract
Objectives
The aim of this study was to investigate factors associated with unplanned 30-day readmissions following a total knee arthroplasty (TKA), including association with post-hospital syndrome, patient enablement and transition from hospital to home.
Design, setting and participants
A cross-sectional written survey of public and private patients attending a 6-week follow-up appointment after TKA at one of four clinical services in the Australian Capital Territory (ACT) between 1 February 2018 and 31 January 2019. Multiple logistic regression analyses were used to measure associations between patient, hospital and transitional care factors with unplanned 30-day readmissions, while controlling for known confounders.
Results
Of the 380 participants who completed the survey (n=380, 54% of TKAs undertaken over the study period), 3.4% (n=13; 95% CI: 1.8 to 5.8) were subsequently readmitted within 30 days of discharge after a primary hospitalisation. Public patients were significantly more likely to be readmitted within 30 days compared with private patients (adjusted OR=6.31, 95% CI: 1.59 to 25.14, p=0.009), and patients who attended rehabilitation were significantly less likely to be readmitted within 30 days of discharge than those who did not (adjusted OR=0.16, 95% CI: 0.04 to 0.57, p=0.005). There were no associations between post-hospital syndrome or patient enablement and 30-day readmissions in this study.
Conclusion
Reasons underlying the difference in unplanned readmission rates for public versus private patients need to be explored, including differences in surgical waiting times and the consequences for impairment and disease complexity. Strategies to foster increased participation post-surgical rehabilitation programmes need to be developed as an avenue to mitigate the burden of unplanned 30-day readmissions on individuals and health systems.
Keywords: knee, health policy, quality in health care
Strengths and limitations of this study.
A survey, co-designed with clinicians and patients, examined associations between patient, hospital and transitional care factors and unplanned 30-day readmission following total knee arthroplasty in both public and private hospital settings.
This study is the first to use patient-reported responses to quantify the effect of hospital experience of pain, sleep and nutrition in unplanned 30-day readmissions following total knee arthroplasty.
A limitation of this study is that results were based on self-reported patient outcomes with no capacity to link them to hospital records for confirmation as well as the lack of information from those who declined the survey.
Introduction
Unplanned readmission rates are an indicator of health system performance.1 2 The rate of unplanned 30-day readmission for total knee arthroplasty (TKA) in Australian public hospitals was 2.6% in 2017–2018.3 In the USA, readmission rates have been used as an incentive to reduce readmission and drive improved practice.4 While there is no such programme in Australia, the economic burden of unplanned readmissions makes it a policy priority.3 5 6
The rate of knee replacement surgery has more than doubled over the past 15 years both in Australia and internationally7 with the highest rate of increase seen in the private sector.3 5 8 This growing demand has placed increased logistical and financial strain on the healthcare system, including associated unplanned 30-day readmissions.5 The most common condition-related causes of unplanned readmission following a TKA are surgical-site infection, arthrofibrosis, cellulitis, concomitant comorbidities and fluid and electrolyte imbalance.9 Other factors such as old age, revision procedure and acute length of hospital stay also increase the risk of unplanned 30-day readmissions.9 Beyond the complications as a cause of the readmission, there are patient factors related to the hospital stay that increase risk of readmission.10
Krumholz11 describes post-hospital syndrome as a period of vulnerability after discharge from the hospital which leaves a patient at increased risk of re-hospitalisation from conditions which are often unrelated to the original reason for admission. It is proposed that this acquired transient state might be due to patients’ experiences of pain, sleep deprivation and poor nutrition during their hospital stay.11 While this hypothesis is supported by evidence that increasing patient capacity for self-care is effective at reducing 30-day readmissions,10 as far as we are aware, post-hospital syndrome has not been quantified or measured as an independent variable in association with unplanned 30-day readmission.
Research examining unplanned 30-day readmissions has described a number of associated factors. These factors include: clinical and demographic characteristics12 13; a lack of access to primary care; the continuity and regularity of primary care14–16; and deficits in hospital discharge planning, which often focus on knowledge provision rather than patients’ capacity to implement this knowledge.10
The patient-enablement instrument is a tool used to measure a person’s knowledge and understanding of their health condition; confidence to manage their condition, health and life17; and their ability to source appropriate healthcare for their individual needs. While this measure has largely been examined in primary-care settings, its role in preventing unplanned hospital readmissions has not yet been explored.
The purpose of this study was to investigate factors associated with unplanned 30-day readmissions following a TKA, including aspects of hospital experiences, patient enablement and transition from hospital to home.
Methods
Study population
Consecutive patients over the age of 16 years, attending a 6-week follow-up appointment after undergoing TKA at one of four private and public clinical services between 1 February 2018 and 31 January 2019.
Patient and public involvement
Five people who had previously had an arthroplasty with a surgeon from one of the participating clinics completed the survey and provided feedback regarding its meaningfulness in relation to their experiences, and the length and readability of the survey.
Study design
A cross-sectional survey was conducted in the Australian Capital Territory (ACT) between 1 February 2018 and 31 January 2019 at all private and public sites undertaking lower limb joint replacement services. Data were collected retrospectively at the 6-week follow-up appointment post surgery for both total knee and hip replacement (THA). The responses for patients having undergone elective TKA are presented in this paper.
Instrument
The ACT Transition from Hospital to Home Survey was developed and piloted by researchers at the Australian National University, Canberra Hospital, Academic Unit of General Practice ACT Health, Capital Health Network, Health Care Consumer Association ACT and people who had previously experienced either TKA or THA.18 The 50-item survey was designed to measure patients’ experiences in hospital and transition to home across six domains: (1) Patient demographic characteristics and comorbidities; (2) Post-hospital syndrome; (3) Medication enablement; (4) Patient enablement; (5) Transition to general practice; and (6) Pre-hospital and post-hospital information and pre-surgical/post-surgical rehabilitation
Co-morbidities
Morbidity was assessed with the validated 18-item Functional Comorbidity Index which is used to predict functional status rather than mortality.19
Post-hospital syndrome
Fifteen items within three domains covering patients’ experiences of sleep, pain and diet in hospital were designed to measure post-hospital syndrome.
Medication enablement
Three items measured medication enablement in terms of patients’ knowledge and ability to manage their medications following discussions with healthcare providers derived from a previous study in general practice nurse consultations.20 The internal consistency of this scale was established (α=0.80) in the pilot study (unpublished results).
Patient enablement
This is the internationally validated six-item Patient Enablement Instrument21 used primarily in primary-care research.
Transition to general practice
Ten items assessing patients’ relationships with their general practitioner (GP) in terms of continuity of care, regularity of care, healthcare planning, patients’ understanding of when to see their GP following discharge and access to care. These questions were refined as a result of the pilot study to eliminate covariance and repetition.
Interaction with the recommended rehabilitation programme
Referral and attendance to outpatient physiotherapy rehabilitation post discharge was examined with one item.
Data collection
The paper surveys were distributed by reception staff at patients’ 6-week postoperative consultation. Staff were given a protocol and suggested wording to use when providing the survey. An information sheet about the study was provided to patients and anonymity guaranteed. Patients were not required to include their name or identifying information on the survey. This ensured that patients understood that participation or non-participation did not affect the care they received and that completed surveys were confidential to clinical staff. Completion of the survey implied written consent and this was agreed and approved by the local ethics committee. Surveys were deposited in a sealed box in the waiting room and collected by the researcher at regular intervals.
Data analysis
Completed survey data were collated and descriptive and inferential statistics used. Variables were described using summary statistics and frequencies. Some variables were grouped to create new variables and others, for example, body mass index (BMI), were converted to categorical variables for analysis. The primary outcome of interest was self-reported 30-day readmission to hospital following discharge, categorised as a binary variable (yes/no). Age, sex, living situation, country of origin, education, self-rated health, comorbidities, post-hospital syndrome (experiences of sleep, diet and pain), experiences of family practice (access, continuity, planning, regularity), medication enablement and patient enablement were separate independent variables.
An exploratory factor analysis (EFA) with orthogonal varimax rotation was undertaken to explore the relationship between variables which described post-hospital syndrome. The modes/themes which had an eigenvalue of >1 were retained and the internal consistency of the modes which emerged was examined using Cronbach’s alpha. The suitability of the data for an EFA was confirmed with a Kaiser-Meyer-Olkin criteria and Bartlett’s test.
Prior to analysis, variable independence was established. Ordinal variables were examined using Spearman’s correlation coefficient and categorical variables using the χ² test and OR. If a strong correlation (>0.6) or a significant association (p≤0.2) existed between two eligible variables, only one of these was retained for inclusion in the final analysis.
Univariate logistic regression analysis was conducted for each independent variable and the dependent variable (unplanned 30-day readmission). Univariate logistic regression was conducted on each individual comorbidity item, and then for the total comorbidity score.
To further eliminate potential confounding, two multiple logistic regression models were run—one including eligible individual variables from within the Functional Comorbidity Index, Medication Enablement questions and the Patient Enablement Instrument; and a second including total scores.
The full multiple logistic regression model included eight variables. These were public or private hospital; upper gastrointestinal disease; self-rated health; given an information package or checklist before surgery; usual waiting time to see GP; attendance at recommended rehabilitation or physiotherapy; and living status. The reduced model included ‘public or private hospital’ and ‘attendance at recommended rehabilitation or physiotherapy’. Only risk factors with p values≤0.25 were included in the multiple logistic regression analyses. Logistic regression with backward stepwise selection was used to choose risk factors for the multivariable model. A significance level of 0.25 was required to allow a risk factor into the model, and a significance level of 0.25 was required for a risk factor to stay in the model. The adjusted OR and its 95% CI were calculated for each risk factor in the presence of others in the final model. Both the models were adjusted for age and sex.
Likelihood ratio tests and Hosmer-Lemeshow goodness of fit test were used to check the fit of the final model. The receiver operator characteristic (ROC) curve was plotted to check the specificity and sensitivity of the predicted model.
Stata/IC v.15.1 (StataCorp) was used to perform all statistical analyses.22
Missing data
The criteria used for acceptability of non-response to all survey questions was 10% or lower including for medication and patient enablement scale.23–25 Missing data for individual variables within the medication and patient enablement scales were imputed to equal the median value of non-missing data.26–29
Results
Of the 1069 people invited to participate, 827 (77%) completed the overall survey.
Of all surgeries, 380 received a TKA and of these 13 were readmitted within 30 days. Participant demographics are presented in table 1. Private patients accounted for 65% of the total population (247 private patients and 133 public patients). This represented 44% of all private patients and 96% of all public patients who had a TKA during the study period which represents 54% of all TKAs. Fifty-seven per cent of those who underwent knee surgery were women. The mean age was 67.4 with a SD 0.5 years (age range 44.8–91.0 years). Mean BMI was 31.5 kg/m2 with most having a BMI of >30 (58%). Most participants were non-indigenous (99%). There were three people of Aboriginal and/or Torres Strait Islander origin, none of whom was readmitted. There were proportionally more private patients aged 65–84 years (63%) compared with public (53%), whereas proportionally more public patients were in the 45–64 age group (44% compared with 35%). The proportion of women within the public cohort was greater than private (67% compared with 57%). A higher proportion of public patients lived alone (31% compared with 23%).
Table 1.
Characteristics of participants who underwent total knee arthroplasty with an unplanned 30-day readmission (n) as a proportion of all participants (N)
| Variable | Public n/N | Private | Total | |
| N=133 n/N |
N=247 n/N |
N=13/380 (%)* |
||
| Age | 45–64 | 1/55 | 1/79 | 2/134 (2) |
| 65–84 | 4/33 | 2/145 | 10/211 (5) | |
| >85 years | 0/4 | 0/5 | 0/9 | |
| Gender | Male | 1/21 | 1/97 | 3/139 (2) |
| Female | 7/86 | 3/129 | 2/55 (5) | |
| Other | 0/0 | 0/2 | 0/2 | |
| Language | Other than English at home | 0/21 | 1/14 | 2/49 (4) |
| Only speaks English | 1/12 | 1/106 | 11/320 (3) | |
| Living status | Lives alone | 7/40 | 0/55 | 2/95 (2) |
| Lives with someone | 1/45 | 4/189 | 11/273 (4) | |
| BMI calculations | BMI (mean) | 31.5 | ||
| 18.5–24.4 | 1/7 | 0/22 | 1/31 (3) | |
| 24.5–30 | 1/34 | 1/43 | 2/129 (2) | |
| >30 | 7/74 | 3/109 | 10/220 (5) | |
| Indigenous status | Aboriginal | 0/1 | 0/0 | 0/1 |
| Torres Strait Islander | 0/1 | 0/1 | 0/2 | |
| Both | 0/0 | |||
| Neither | 9/104 | 2/99 | 13/315 (4) | |
| Education | No school certificate or other qualifications | 0/9 | 0/11 | 0/22 |
| School or intermediate certificate | 1/8 | 1/40 | 6/87 (7) | |
| Year 12 or leaving certificate | 1/17 | 1/32 | 1/27 (4) | |
| Trade/apprenticeship | 0/10 | 1/17 | 1/30 (3) | |
| Certificate/diploma | 2/23 | 0/50 | 1/38 (3) | |
| University degree or higher | 1/17 | 1/68 | 2/95 (2) |
*Missing values for age: 26, Gender: 24, Language: 11, Living status: 6, BMI: 36, Indigenous status: 62, Education: 16.
†Missing value for readmission for age: 1.
BMI, body mass index.
Post-hospital syndrome EFA
The results of the EFA are reported in table 2. Three modes/themes with acceptable internal consistency emerged. First, diet, which was described by responses to two questions: ‘Did you feel your dietary requirements were met in hospital?’ and ‘Overall, how would you rate the quality of the food in hospital?’ The second theme was pain, which was also explained by two questions: ‘How would you describe the general level of pain you experienced?’ and ‘When you left hospital, how would you rate your pain out of 10?’ The third was sleep which was explained by ‘Did you feel well rested when you left the hospital?’ and ‘How would you rate the quality of sleep in the hospital?’
Table 2.
Exploratory factor analysis and emerging variables
| Factor | Eigenvalue | Difference | Proportion | Cumulative |
| Factor 1 | 2.53 | 0.85 | 0.18 | 0.18 |
| Factor 2 | 1.69 | 0.42 | 0.12 | 0.30 |
| Factor 3 | 1.27 | 0.12 | 0.09 | 0.39 |
| Bartlett test of sphericity p=0.000 | ||||
| Kaiser-Meyer-Olkin=0.62 | ||||
| Variable | Factor 1 | Factor 2 | Factor 3 |
| Did you feel your dietary requirements were met in hospital? | 0.88 | 0.01 | 0.10 |
| Overall, how would you rate the quality of the food in hospital? | 0.86 | 0.01 | 0.09 |
| How would you describe the general level of pain you experienced? | −0.02 | 0.83 | 0.10 |
| When you left hospital, how would you rate your pain out of 10? | 0.04 | 0.75 | 0.09 |
| Did you feel well rested when you left the hospital? | 0.20 | 0.18 | 0.75 |
| How would you rate the quality of sleep in the hospital? (poor) | 0.30 | 0.18 | 0.67 |
The highlighted bold values respresent factor loading which are the correlation coefficient indicating the variance explained by the variable on the factor. Values 0.7 or greater are retained and highlighted in this table.
Floor and ceiling effects were observed for patient enablement due to a large number of participants reporting being either fully enabled or not enabled at all. To address this, the variable was dichotomised around the mean where ‘less enabled’ was ≤6.5 and ‘more enabled’ was >6.5 in line with previous studies using this instrument.28 30 Sixty per cent of participants (n=212/357) reported that they were less enabled to manage their health after their stay in the hospital.
Multiple logistic regression analysis
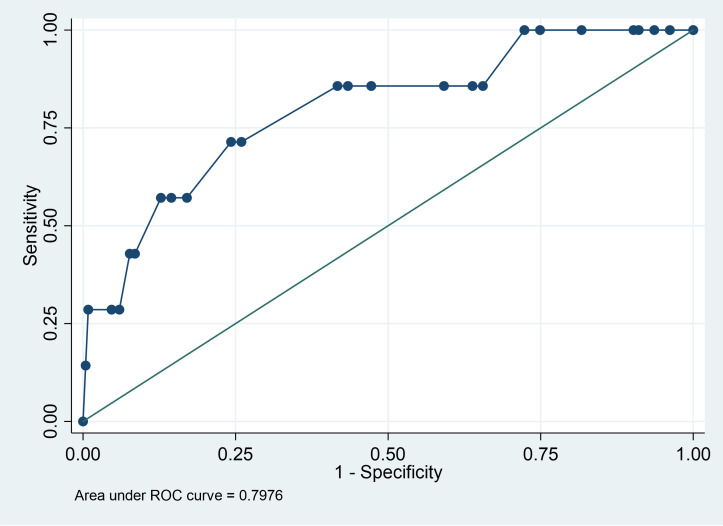
The results of univariate analysis are presented in online supplemental table 1. The area under the curve (AUC) was 0.80 (95% CI: 0.66 to 0.94) indicating high overall accuracy of the logistic model (80%) (figure 1). The area under the ROC curve is interpreted as the probability that a subject with unplanned 30-day readmission is given a higher probability of the outcome by the logistic model than a randomly chosen subject without unplanned 30-day readmission. An AUC value of 0.50 indicates that the model has no discriminatory ability (the diagonal line corresponds to random change). The Pearson χ² goodness of fit test statistic is 11.64 and since p=0.7682, we conclude that there is no evidence against the model fitting the data well.
Figure 1.
Receiver operator characteristic (ROC) curve.
bmjopen-2021-053831supp001.pdf (49.5KB, pdf)
Eight variables were eligible for inclusion in the multiple logistic regression analysis. Due to the wide CI for stroke, this variable was eliminated from the full model. Of these, ‘public or private status’ and ‘rehabilitation attendance’ were retained for the reduced model as they were the only variables to retain significance after stepwise removal of the other variables in the full model. The results of the multiple regression analysis are reported in table 3.
Table 3.
Results of multiple logistic regression analysis examining the association between patient, hospital and transition to general practice factors associated with unplanned 30-day readmission to hospital
| Relevant variables | Full model* | Reduced model† (n=328) | ||||
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Public or private | 3.44 | 0.70 to 16.89 | 0.12 | 6.31 | 1.59 to 25.14 | 0.009 |
| Comorbidity | ||||||
| Upper gastrointestinal disease | 0.43 | 0.06 to 2.96 | 0.39 | – | – | – |
| Living status | 0.27 | 0.03 to 2.45 | 0.25 | – | – | – |
| Self-rated health | 0.39 | 0.14 to 1.13 | 0.08 | – | – | – |
| Information package | 0.56 | 0.05 to 4.04 | 0.65 | – | – | – |
| Attended info session | 0.80 | 0.16 to 7.07 | 0.79 | – | – | – |
| Waiting time to see GP | 0.60 | 0.23 to 1.58 | 0.30 | – | – | – |
| Attendance to rehabilitation | 0.21 | 0.05 to 0.96 | 0.04 | 0.16 | 0.04 to 0.57 | 0.005 |
*Full model included public or private hospital; upper gastrointestinal disease; self-rated health; given an information package or checklist before surgery; usual waiting time to see GP; attendance to recommended rehabilitation or physiotherapy; and living status.
†Reduced model included variables public or private hospital and attendance to recommended rehabilitation or physiotherapy. Both the models were run when adjusting for age and sex.
GP, general practitioner.
The final multiple regression model included a sample size of 328 observations and the following factors remained significant. After controlling for age and sex, public patients were significantly more likely to be readmitted within 30 days compared with private patients (OR=6.31, 95% CI: 1.59 to 25.14, p=0.009), and patients attended rehabilitation were significantly less likely to be readmitted within 30 days of discharge than those who did not (OR=0.16, 95% CI: 0.04 to 0.57, p=0.005). After attempting to adjust for age and sex in a four-covariate reduced model, public patients (9/134, 6.7%) were significantly more likely (adjusted OR=6.31, 95% CI: 1.59 to 25.14, p=0.009) to be readmitted within 30 days compared with private patients (4/246, 1.6%) and patients attended rehabilitation (7/301, 2.3%) were significantly less likely (adjusted OR=0.16, 95% CI: 0.04 to 0.57, p=0.005) to be readmitted within 30 days of discharge than those who did not (6/39, 15.3 %).
Discussion
The aim of this study was to investigate factors associated with unplanned 30-day readmission in patients who underwent TKA. Of the 4% of patients who had an unplanned readmission, those who attended public hospitals and those who did not attend an outpatient rehabilitation programme were more likely to be readmitted to hospital within 30 days of discharge.
While the USA also has a similar 4% readmission rate following TKA,9 31–33 this is higher than that reported by the Australian Institute of Health and Welfare (AIHW).3 However, our results may reflect the true readmission rate more accurately as the AIHW only reports public hospital data and the majority of TKAs in Australia are performed in the private sector.
In our study, public patients were more likely to be readmitted within 30 days as compared with private patients. The majority of respondents (65%) had their TKA in the private sector, consistent with the higher proportion (80%) of TKA procedures performed in the private sector in the ACT.34 Our study has almost complete ascertainment from the public sector, and reasonable ascertainment from the private sector, supporting the robustness of our findings. The increased likelihood of readmission for public patients might be explained by several contributing factors such as socioeconomic status, longer waiting times resulting in increased impairment and disease complexity.35–40 The median waiting time for a TKA in 2018–2019 in the ACT public hospital system was 209 days with 8.2% of patients waiting more than 365 days.35 On the other hand, the median waiting time for Australian private patients was just 67 days during the same period.2 41 Therefore, waiting time may be an important mediating factor however association between the two may only be inferred and no causation can be implied.
Patients who have had to wait longer constitute 1.2% of all unplanned 30-day readmissions for elective surgical procedures in Australia.42 Patients who underwent TKA who waited longer than 6 months have been described as having significantly worse function and quality of life scores, as well as dissatisfaction rates which were mainly influenced by preoperative anxiety and depression.43 It is important to understand that surgical waiting times are only part of the waiting journey for patients in the public system. The mean waiting times recorded for Australian patients do not take into account the lengthy process of referral, specialist assessment and investigation.44 Addressing long waiting lists by using non-surgical exercise and education programmes are increasingly being implemented and the evidence for efficacy is strong.45 46
In our study, patients who attended rehabilitation were less likely to be readmitted within 30 days than those who did not. Previous research indicates that private patients are more likely to attend rehabilitation than public patients47 and that rehabilitation is associated with better physical function after TKA.45 However, we found no significant relationship between being a public or private patient and attendance at rehabilitation. Both groups in our sample had similar rehabilitation opportunities, except for the provision of hydrotherapy after 6 weeks indicating that public or private status was not a mediating factor for this finding.
This study showed no significant associations between general practice factors and unplanned 30-day readmissions. A recent study reported that timely and regular GP contact during the 2 years following transition from hospital to community care lowered the risk of emergency readmission to hospital in patients with cardiovascular disease.48 However, our results might reflect the nature of the health condition. This cohort included people having TKA as a treatment for severe pain for arthritis of the knee, which is quite different to other diseases in that the treatment is potentially definitive and is followed up by the surgeon.
Although more than half of the patients who were readmitted had high scores for post-hospital syndrome, there was no significant association with 30-day readmission. The hypothesis of post-hospital syndrome describes a transient state resulting in consequences, including a higher risk of readmission.11 Brownlee et al49 found that post-hospital syndrome was an independent predictor of readmission within 30 days of discharge in a large cohort of surgical patients. While other studies have attempted to determine the impact of post-hospital syndrome through linked hospital records data,49 50 this study is the first to use patient-reported responses to quantify the effect of hospital experience (of pain, sleep and nutrition) on unplanned 30-day readmissions.
There are limitations to this study. The main limitation was that there were fewer readmissions than anticipated and the study may have been insufficiently powered for detecting the associations being tested. The results were based on anonymous self-reports; hence there was no capacity to link them to hospital data to establish actual readmission time frames, length of hospital stay, reasons for readmission or previous admission history. However, our primary endpoint was 30-day readmission and we believe that the self-reported data were accurate. The response rate is only an estimation based on joint replacement activity in the ACT. It assumes that all patients returning for their 6-week follow-up appointment were invited to participate. We do not know whether the reception staff invited all patients, or only some. The lack of information about non-responders is another limitation of this study. More non-responders may have been readmitted and it is possible that they may have been sicker than responders, which would also influence the readmission rate. Also, as the ACT has a relatively high socioeconomic demographic the findings from this study may not apply to other less affluent areas.
Our data do not allow us to understand why rehabilitation was not accessed. It is possible that patients who were frailer did not feel able to participate and perhaps they were the patients who were readmitted. However, a range of patient and provider-based factors have been recognised as affecting the rehabilitation pathway chosen by patients, such as preoperative preferences, previous experiences, perceived benefits, clinical status post-surgery, as well as insurance provider and hospital business model.51 This association needs clarification.
It is not known if the rate of readmission can be reduced given the significant comorbidities of the patients who underwent TKA sample.
Conclusion
This study was undertaken to explore the factors impacting unplanned 30-day readmission after TKA. These results have implications for policy and for practice. An over-representation of public patients in the readmitted cohort is important. It is possible that the consequences of extended periods of delay to surgery among patients on the public waiting list may be an important factor. Therefore, it is essential to shorten waiting times and prioritise medical need when dealing with public patients. Clinicians should also place emphasis on the importance of attending rehabilitation after a TKA as an effective way to reduce 30-day readmission. Further investigation of how the pre-surgical patient journey can be better optimised to reduce readmission rates is warranted.
Supplementary Material
Acknowledgments
We wish to thank Orthopaedics ACT and Dr Michael Gross from Canberra Hip and Knee Replacement for their support with this project. We would like to acknowledge Professor Art Sedrakyan, Professor of Population Health Sciences, Weill Cornell Medical College, for his conceptual support in the early establishment of this research project; and Associate Professor Alice Richardson, Lead, Statistical Support Network, Australian National University.
Footnotes
Twitter: @JaneODes
Contributors: MC: data collection, analysis, drafting and finalising of manuscript. DP: data collection and analysis, significant contributions to final manuscript. CP: survey development, significant contributions to final manuscript. AP: data collection, significant contributions to final manuscript. NG: survey development, significant contributions to final manuscript. KD: survey development, significant contributions to final manuscript. DC: survey development, contributions to final manuscript. PS: survey development, significant contributions to final manuscript. JD: study conception and survey design, data collection, supervised data analysis, significant contributions to final manuscript, and responsible for the overall content as the guarantor.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was obtained from the Australian Capital Territory Health (ETHLR.17.207), Calvary Healthcare Bruce (45–2017) and the Australian National University (2017/798) Human Research Ethics Committees. All participants provided written informed consent to participate in this study.
References
- 1.Bureau of Health Information . Spotlight on measurement: return to acute care following hospitalisation, spotlight on readmissions Sydney (NSW). BHI, 2015. [Google Scholar]
- 2.Dixit SK, Sambasivan M. A review of the Australian healthcare system: a policy perspective. SAGE Open Med 2018;6:205031211876921. 10.1177/2050312118769211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Institute of Health and Welfare . Admitted patient care 2017–18: Australian hospital statistics. Health services series No. 90. Cat. no. HSE 225. Canberra: AIHW, 2019. [Google Scholar]
- 4.McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation 2015;131:1796–803. 10.1161/CIRCULATIONAHA.114.010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ackerman IN, Bohensky MA, Zomer E, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord 2019;20:90. 10.1186/s12891-019-2411-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med 2000;160:1074–81. 10.1001/archinte.160.8.1074 [DOI] [PubMed] [Google Scholar]
- 7.Losina E, Thornhill TS, Rome BN, et al. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 2012;94:201–7. 10.2106/JBJS.J.01958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Private Healthcare Australia . Pre-budget submission 2017–18, 2017. Available: https://static.treasury.gov.au/uploads/sites/1/2017/06/C2016-052_Private-Healthcare-Australia.pdf [Accessed 4 Jun 2020].
- 9.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 2014;472:181–7. 10.1007/s11999-013-3030-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med 2014;174:1095–107. 10.1001/jamainternmed.2014.1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krumholz HM. Post-hospital syndrome-an acquired, transient condition of generalized risk. N Engl J Med 2013;368:100–2. 10.1056/NEJMp1212324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falster MO, Jorm LR, Douglas KA, et al. Sociodemographic and health characteristics, rather than primary care supply, are major drivers of geographic variation in preventable hospitalizations in Australia. Med Care 2015;53:436–45. 10.1097/MLR.0000000000000342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kossovsky MP, Sarasin FP, Perneger TV, et al. Unplanned readmissions of patients with congestive heart failure: do they reflect in-hospital quality of care or patient characteristics? Am J Med 2000;109:386–90. 10.1016/S0002-9343(00)00489-7 [DOI] [PubMed] [Google Scholar]
- 14.Einarsdóttir K, Preen DB, Emery JD, et al. Regular primary care lowers hospitalisation risk and mortality in seniors with chronic respiratory diseases. J Gen Intern Med 2010;25:766–73. 10.1007/s11606-010-1361-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cree M, Bell NR, Johnson D, et al. Increased continuity of care associated with decreased hospital care and emergency department visits for patients with asthma. Dis Manag 2006;9:63–71. 10.1089/dis.2006.9.63 [DOI] [PubMed] [Google Scholar]
- 16.Tsai C-L, Griswold SK, Clark S, et al. Factors associated with frequency of emergency department visits for chronic obstructive pulmonary disease exacerbation. J Gen Intern Med 2007;22:799–804. 10.1007/s11606-007-0191-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howie JG, Heaney DJ, Maxwell M, et al. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165–71. 10.1093/fampra/15.2.165 [DOI] [PubMed] [Google Scholar]
- 18.Desborough J, Doi S, Glasgow N. Examining the interface between acute and primary care: understanding unplanned 30-day readmissions, in Canberra health area research meeting. Canberra, Australia, 2017. [Google Scholar]
- 19.Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005;58:595–602. 10.1016/j.jclinepi.2004.10.018 [DOI] [PubMed] [Google Scholar]
- 20.Desborough J, Banfield M, Phillips C, et al. The process of patient enablement in general practice nurse consultations: a grounded theory study. J Adv Nurs 2017;73:1085–96. 10.1111/jan.13199 [DOI] [PubMed] [Google Scholar]
- 21.Hudon C, Fortin M, Rossignol F, et al. The patient enablement instrument-French version in a family practice setting: a reliability study. BMC Fam Pract 2011;12:71. 10.1186/1471-2296-12-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.StataCorp . Stata statistical software: release 16. College Station, TX: StataCorp LLC, 2019. [Google Scholar]
- 23.Foss AJ, Lamping DL, Schroter S, et al. Development and validation of a patient based measure of outcome in ocular melanoma. Br J Ophthalmol 2000;84:347–51. 10.1136/bjo.84.4.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desborough J, Bagheri N, Banfield M, et al. The impact of general practice nursing care on patient satisfaction and enablement in Australia: a mixed methods study. Int J Nurs Stud 2016;64:108–19. 10.1016/j.ijnurstu.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 25.Bowling A. Research methods in health: investigating health and health services: McGraw-hill education (UK), 2014. [Google Scholar]
- 26.Mercer SW, Jani BD, Maxwell M, et al. Patient enablement requires physician empathy: a cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract 2012;13:6. 10.1186/1471-2296-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desborough J, Bagheri N, Banfield M, et al. The impact of general practice nursing care on patient satisfaction and enablement in Australia: a mixed methods study. Int J Nurs Stud 2016;64:108–19. 10.1016/j.ijnurstu.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 28.Mercer SW, Jani BD, Maxwell M, et al. Patient enablement requires physician empathy: a cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract 2012;13:6. 10.1186/1471-2296-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mercer SW, Neumann M, Wirtz M, et al. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland--a pilot prospective study using structural equation modeling. Patient Educ Couns 2008;73:240–5. 10.1016/j.pec.2008.07.022 [DOI] [PubMed] [Google Scholar]
- 30.Desborough J, Banfield M, Parker R. A tool to evaluate patients' experiences of nursing care in Australian general practice: development of the patient enablement and satisfaction survey. Aust J Prim Health 2014;20:209–15. 10.1071/PY12121 [DOI] [PubMed] [Google Scholar]
- 31.Australian Commission on Safety and Quality in Health Care . Avoidable Hospital readmissions: report on Australian and international indicators, their use and the efficacy of interventions to reduce readmissions. Sydney: ACSQHC, 2019. [Google Scholar]
- 32.Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA 2012;308:1227–36. 10.1001/2012.jama.11153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown NM, Sheth NP, Davis K, et al. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty 2012;27:86–90. 10.1016/j.arth.2012.03.022 [DOI] [PubMed] [Google Scholar]
- 34.Pawlikowska TRB, Nowak PR, Szumilo-Grzesik W, et al. Primary care reform: a pilot study to test the evaluative potential of the patient enablement instrument in Poland. Fam Pract 2002;19:197–201. 10.1093/fampra/19.2.197 [DOI] [PubMed] [Google Scholar]
- 35.Australian Institute of health and welfare, 2018. Available: https://www.myhospitals.gov.au/hospital/810000082/the-canberra-hospital/waiting-times-elective-surgery-intended-procedure
- 36.Brennan SL, Lane SE, Lorimer M, et al. Associations between socioeconomic status and primary total knee joint replacements performed for osteoarthritis across Australia 2003-10: data from the Australian orthopaedic association national joint replacement registry. BMC Musculoskelet Disord 2014;15:356. 10.1186/1471-2474-15-356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desmeules F, Dionne CE, Belzile Étienne L, et al. The impacts of pre-surgery wait for total knee replacement on pain, function and health-related quality of life six months after surgery. J Eval Clin Pract 2012;18:111–20. 10.1111/j.1365-2753.2010.01541.x [DOI] [PubMed] [Google Scholar]
- 38.Desmeules F, Dionne CE, Belzile E, et al. The burden of wait for knee replacement surgery: effects on pain, function and health-related quality of life at the time of surgery. Rheumatology 2010;49:945–54. 10.1093/rheumatology/kep469 [DOI] [PubMed] [Google Scholar]
- 39.Keeney BJ, Koenig KM, Paddock NG, et al. Do aggregate socioeconomic status factors predict outcomes for total knee arthroplasty in a rural population? J Arthroplasty 2017;32:3583–90. 10.1016/j.arth.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCormack R, Michels R, Ramos N, et al. Thirty-day readmission rates as a measure of quality: causes of readmission after orthopedic surgeries and accuracy of administrative data. J Healthc Manag 2013;58:64–76. 10.1097/00115514-201301000-00011 [DOI] [PubMed] [Google Scholar]
- 41.Australian Institute of Health and Welfare . Admitted patient care 2015–16: Australian hospital statistics. Health services series no.75. Cat. no. HSE 185. Canberra: AIHW, 2017. [Google Scholar]
- 42.Australian Institute of Health and Welfare . Elective surgery waiting times 2017–18: Australian hospital statistics. Health services series no. 88. Cat. no. HSE 215. Canberra: AIHW, 2018. [Google Scholar]
- 43.Lizaur-Utrilla A, Martinez-Mendez D, Miralles-Muñoz FA, et al. Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int Orthop 2016;40:2303–7. 10.1007/s00264-016-3209-0 [DOI] [PubMed] [Google Scholar]
- 44.Curtis AJ, Russell COH, Stoelwinder JU, et al. Waiting lists and elective surgery: ordering the queue. Med J Aust 2010;192:217–20. 10.5694/j.1326-5377.2010.tb03482.x [DOI] [PubMed] [Google Scholar]
- 45.Skou ST, Roos EM. Good Life with osteoArthritis in Denmark (GLA:D): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord 2017;18:72. 10.1186/s12891-017-1439-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Skou ST, Roos EM, Laursen MB, et al. A randomized, controlled trial of total knee replacement. N Engl J Med Overseas Ed 2015;373:1597–606. 10.1056/NEJMoa1505467 [DOI] [PubMed] [Google Scholar]
- 47.Steven F, Shiner CW, Jane; Chia K. Evaluating the role of rehabilitation for lower limb joint replacement, deconditioning and cancer. Sydney: Department of Rehabilitation Medicine, St Vincent’s Hospital Sydney, Australia, (APHA) APHA. [Google Scholar]
- 48.Australian Institute of Health and Welfare . Transition between hospital and community care for patients with coronary heart disease: New South Wales and Victoria, 2012–2015. Cat. no. CDK 9. Canberra: AIHW, 2018. [Google Scholar]
- 49.Brownlee SA, Blackwell RH, Blanco BA, et al. Impact of post-hospital syndrome on outcomes following elective, ambulatory surgery. Ann Surg 2017;266:274–9. 10.1097/SLA.0000000000001965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sadatsafavi M, Lynd LD, Fitzgerald JM. Post-hospital syndrome in adults with asthma: a case-crossover study. Allergy Asthma Clin Immunol 2013;9:49. 10.1186/1710-1492-9-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buhagiar MA, Naylor JM, Simpson G, et al. Understanding consumer and clinician preferences and decision making for rehabilitation following arthroplasty in the private sector. BMC Health Serv Res 2017;17:415. 10.1186/s12913-017-2379-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053831supp001.pdf (49.5KB, pdf)
Data Availability Statement
Data are available upon reasonable request.