Abstract
Injuries in low-income and middle-income countries are prevalent and their number is expected to increase. Death and disability after injury can be reduced if people reach healthcare facilities in a timely manner. Knowledge of barriers to access to quality injury care is necessary to intervene to improve outcomes. We combined a four-delay framework with WHO Building Blocks and Institution of Medicine Quality Outcomes Frameworks to describe barriers to trauma care in three countries in sub-Saharan Africa: Ghana, South Africa and Rwanda. We used a parallel convergent mixed-methods research design, integrating the results to enable a holistic analysis of the barriers to access to quality injury care. Data were collected using surveys of patient experiences of injury care, interviews and focus group discussions with patients and community leaders, and a survey of policy-makers and healthcare leaders on the governance context for injury care. We identified 121 barriers across all three countries. Of these, 31 (25.6%) were shared across countries. More than half (18/31, 58%) were predominantly related to delay 3 (‘Delays to receiving quality care’). The majority of the barriers were captured using just one of the multiple methods, emphasising the need to use multiple methods to identify all barriers. Given there are many barriers to access to quality care for people who have been injured in Rwanda, Ghana and South Africa, but few of these are shared across countries, solutions to overcome these barriers may also be contextually dependent. This suggests the need for rigorous assessments of contexts using multiple data collection methods before developing interventions to improve access to quality care.
Keywords: Health services research, Health policy, Health systems, Health systems evaluation, Traumatology
Summary box
Injury is a major cause of death globally, especially in low-income and middle-income countries.
For patients who have been injured, timely access to quality care is essential for reducing death and disability, but still people experience barriers causing delays in accessing healthcare with detrimental consequences.
By using a four-delays framework and multiple data collection methods, we uncovered 121 barriers to injury care access in Rwanda, South Africa and Ghana. Thirty-one barriers were common across all three countries, whilst many barriers were only present in one or two countries.
Most barriers were specific to individual countries suggesting they are context-specific. Solutions to improve access to injury care may therefore not necessarily be transferable across multiple countries.
To capture multiple barriers required the use of multiple data collections methods which indicates the importance of using mixed methods when assessing access to injury care.
Introduction
In low-income and middle-income countries (LMICs), injuries account for more deaths than tuberculosis, malaria and HIV combined; indeed 90% of injury deaths occur in LMICs.1 Injury is currently the leading killer among people in the economically productive age.2 Injury-associated mortality is expected to rise, with projections that road traffic accidents will be the third leading cause of death by 2030.2 Non-fatal injuries are also important and common, with 1 billion people (15% of the global population) sustaining an injury in 2013 that warranted healthcare.1 Reducing deaths from injury is a key Sustainable Development Goal (SDG 3.6) as is providing Universal Health Coverage (SDG 3.8).3
For patients who have been injured, timely access to quality care is essential for reducing death and disability. Access within the Golden Hour or the Lancet Commission on Global Surgery’s 2-hour target have been accepted by many trauma experts as the appropriate window for injured patients to reach a healthcare facility that can treat them.4 5 However, many injured people in LMICs take longer than 2 hours to reach a healthcare facility6 and our study on external injury deaths in South Africa found 36% of deaths were avoidable if barriers to access to care were reduced.6 We have also found that barriers to access to care are experienced at multiple stages throughout the healthcare journey.7 8
Developing healthcare systems that provide timely and quality care for the injured requires an acknowledgement that these are complex adaptive systems, with positive and negative interactions which may be context dependent.9 These differences and interactions may vary depending on, for example, countries’ development status; the political, governance and finance contexts for health; sociocultural contexts, individual factors (eg, personal wealth and education) and experiences (eg, previous interactions with the healthcare services); and healthcare service factors (eg, whether the necessary building blocks for health are present and whether quality care is provided).10 11 To develop systems that match the needs of the injured patients requires a thorough understanding of the barriers to access to quality care. However, few studies have collected such data and even fewer have done so using multiple methods.12
Barriers to accessing quality care have been described using the four-delay framework, adapted from the three delays framework previously used to improve maternal healthcare.13 14 Delay 1, seeking care, occurs from the point of injury to taking the decision to go to care; Delay 2, reaching care, is from the decision to seek care being made to arriving at formal healthcare; Delay 3, receiving care, is from arrival at the first formal healthcare facility to receiving definitive treatment; and Delay 4, remaining in quality care, is from discharge from acute care to rehabilitation to optimal function. In order to maximise ability to improve equitable access to quality trauma care, it is necessary to understand the barriers to access to quality care that occur at each and every delay stage. In addition, to assess whether barriers are shared across or experienced differently in countries with different socio-cultural characteristics, healthcare systems, and levels of economic development, requires employing similar methods to assess barriers in different settings. Assessing barriers across multiple countries or contexts may suggest where these are shared and thus, where solutions might be transferable across settings. As far as we are aware, no studies have aimed to compare, across countries, the barriers to timely access to quality care after injury.
We combined the four-delay, the WHO building block, and the Institute of Medicine (IoM) Quality frameworks to describe barriers to trauma care in three countries in sub-Saharan Africa with differing levels of development, socio-cultural and healthcare contexts. We used a convergent parallel mixed-methods study design to appraise barriers to access to quality care after injury in these countries to enable holistic understanding within and across the countries.
Approach
Study countries
The study was conducted in Ghana, Rwanda and South Africa. One rural and one urban area in each country was purposively selected to allow feasibility while being as representative of the general population as possible.
Ghana is a lower-middle-income country, with an estimated population of 30.4 million people (2019), life expectancy of 63.8 years, and 7.56% of deaths and 7.24% of disability-adjusted life-years (DALYs) are estimated to be due to trauma.15 Inequality in Ghana is high,15 as is out of pocket (OOP) health expenditure (37.69% of total health expenditure is OOP).15 Tamale Metropolitan Area and Yendi Municipal District were the urban and rural study areas chosen; both are in the north of Ghana.
Rwanda is a low income country of 12.6 million people, with a life expectancy of 68.7 years; 9% of all deaths and 10% of DALYs are due to trauma.15 Community-Based Health Insurance was introduced in 1999/2000 to enable citizens in rural populations and the informal sector to access healthcare.16 Despite this, the health system is still challenged with deficiencies and inequalities.17 This study was conducted in the metropolitan area of the capital, Kigali, and the rural area of Burera.
South Africa is an upper-middle-income country, with a population of 60.1 million and a life expectancy of 62.0 years. Injuries are estimated to be responsible for 10% of deaths and 11% of DALYs.18 Interpersonal violence is seven times higher and road traffic collisions are double the global rate. Access to healthcare is inequitable with 86% of the population served by the public sector which has a disproportionately low proportion of the human resources for health.19
Conceptual frameworks
On appraising the literature on frameworks for conceptualising access to quality healthcare, we did not find a developed framework that suited our aims exhaustively. However, three frameworks we considered would, in combination, comprehensively cover the dimensions of access to quality healthcare for injured people in LMICs. These were: the four-delay framework to access to care as described above,14 20 the IoM framework for quality healthcare,21 and the WHO health systems building blocks.22 The IoM’s framework for quality healthcare conceptualises quality of care as effective, safe, efficient, timely, patient centred, and equitable. The WHO building blocks include leadership/governance, financing, medicines and equipment, information, human resources, and service delivery. Data collection and analyses were based on the domains in these frameworks.
Parallel convergent research design
The same methodologies were employed in each country. Data on barriers to equitable access of quality care were collected between June 2020 and May 2021 by trained local researchers. Desired numbers of participants for each methodology were determined by previous experience of numbers required to produce reliable results.20 23 Due to COVID-19, these numbers were not achieved for all methodologies, and the actual numbers recruited are seen in table 1. For the workshops, up to 30 participants were desired; slightly more were invited with the expectation of drop-outs. For the qualitative interviews, in each country we aimed to recruit 10 participants in both the urban and rural areas. We used a purposeful sampling strategy to ensure a relatively equal number of patients from each area in each study country. Our approach aimed to gain rich understandings of participants’ experiences of injury, with the interview schedule designed to be in-depth with open-ended questions.
Table 1.
A summary of methods for the study
| Data sources | Setting | Achieved no of participants | Methodological approach | Analysis approach |
| Workshops to capture and prioritise existing barriers from multiple stakeholder groups. | Kigali, Rwanda; Tamale, Ghana; Cape Town, South Africa |
Rwanda: 34 Ghana: 31 South Africa: 34 |
Consensus process with small working groups and plenary discussion | Identified priorities were de-duplicated by the whole investigator team and presented under each Delay. |
| Interviews and focus group discussions with injured persons to capture their experiences of barriers. | Both of an urban and a rural setting in each study country* | Around 10 interviews in rural and 10 in urban areas in each country, depending on saturation. Ghana=25 interviews South Africa=20 Interviews Rwanda=20 interviews Between 4 and 11 participants in each focus group |
Qualitative | Thematic analysis |
| Focus group discussions with community leaders to capture their experiences and perceptions of barriers | Both of an urban and a rural setting in each study country* | Between 4 and 9 participants in each focus group) | Qualitative | Thematic analysis |
| I-PAHC and O-PAHC surveys with injured persons to capture their experiences of quality of care provided by in or outpatient facilities | Both of an urban and a rural setting in each study country* | Rwanda: I-PAHC 36 O-PAHC 24 Ghana:
South Africa:
|
Descriptive quantitative analysis | The percentage score for each question and experiential quality category was calculated.24 |
| Governance survey with policy makers or trauma care providers or leaders to assess the policy and governance context for trauma | National surveys | Five from Rwanda, 5 from South Africa and 11 from Ghana |
Descriptive qualitative analysis | Each of the 10 principles of governance developed by Siddiqi et al and related questions were assigned scores.25 |
*Urban and rural settings were: Kigali (urban) and Burera (rural) in Rwanda; Tamale (urban) and Yendi (rural) in Ghana; and Khayelitsha (urban) and Worcester (rural) in South Africa.
I-PAHC, Inpatient Assessment of Healthcare; O-PAHC, Outpatient Users Assessment of Healthcare.
We also aimed to undertake one focus group discussion in both the urban and rural areas, with up to eight participants desired for each discussion. Ideal numbers for the Inpatient Assessment of Healthcare and Outpatient Users Assessment of Healthcare surveys are larger than our sample size, but this was not feasible to achieve in our study.24 Nevertheless, the IQR of responses was narrow even with our smaller sample size. Likewise, fewer participants were invited to complete the governance survey than in other studies, and the results from this should be taken as indicative only.25
Data were analysed separately by in-country research teams, with support from the central investigator team (JCB, JD, MLO, AI and AMAL). The results were then discussed, compared and integrated during a 2-day investigator meeting held in Tamale, Ghana in May 2021. A summary of the methods for this study is presented in table 1 and the full description is available in online supplemental appendix 1.
bmjgh-2021-008256supp001.pdf (419.6KB, pdf)
Patient and public involvement
Participants were not directly involved in planning the study methodologies in all countries. However, the design of the study was based on prior stakeholder engagement in Rwanda.20 Additionally, community leaders were consulted prior to the study and agreed to research being done in their community and results will be disseminated to communities via community leaders.
Synthesis of results
The results were presented, discussed and integrated during the 2 day investigator’s meeting in Ghana in May 2021, with the aims of identifying barriers shared across all countries, those unique to individual countries, and the delay stages (all and predominant) at which barriers act.
First, the results from each of the methods for each country were presented to generate a list of all barriers found using all methods in all countries, categorised by the IoM quality and health system building block domains. Barriers were captured as yes (y) if present; no (n) if it was mentioned but described as not a barrier; and silent (s) if it was not mentioned at all. We included the ‘no—not a barrier’ responses, for completeness, given that in the qualitative work, some respondents actively stated that some issues that they are aware of in other countries are not an issue in their own. In each individual country, where there was a discordance between methods in whether a barrier was present or not, these barriers were assigned both ‘y and n’.
In the next stage, all barriers assigned ‘y’ were collated to show where barriers were shared across all three countries. The investigators then divided into three country-based teams to discuss which delay stage or stages these barriers affected, and the predominant delay stage. These results were presented in the plenary discussion among the investigators until consensus was reached on all the delay stages that barriers affected, and the predominant delay that they affected across all countries.
In total, using all data collection methods in the three countries, 121 barriers in accessing injury care were identified across all countries (online supplemental appendix 2). The domains with the largest number of barriers were the WHO building block of service delivery (37/121=30.6%) and leadership and governance (21/121=17.4%).
In Ghana, 83 out of the 121 barriers (68.6%) were identified (‘y’). Out of these, 58 (58/83=69.9%) barriers were identified using one method, 22 (22/83=26.5%) using two methods, and one (1/83=1.2%) using three methods. For two barriers, there was disagreement (“y and n”) between methods. Thirty (30/121=24.8%) barriers were not mentioned using any method in Ghana and were given an ‘s’. In South Africa, 74 barriers (71/121=58.7%) were identified; 51 (51/74=68.9%) using one method, 20 (20/74=27.0%) using two methods and three barriers (3/74=4.1%) using three different methods. Thirty-six barriers (36/121=29.8%) were not identified using any method in South Africa and given a ‘s’. In Rwanda, 62 (62/121=51.2%) barriers were identified with disagreement for five barriers (‘y’ and ‘n’). Forty-three barriers (43/62=69.4%) were identified using one method, 13 barriers (13/62=21.0%) were identified using two different methods and one of the barriers (1/62=1.6%) using three methods. Forty-one barriers (41/121=33.9%) were not identified using any method in Rwanda and noted as ‘s’.
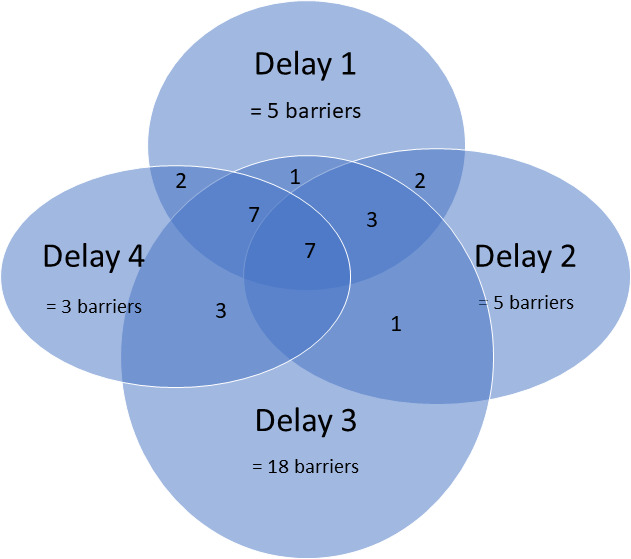
Out of all the 121 barriers identified, 31 (31/121=25.6%) were present in all three study countries using at least one data collection method (table 2), 49 (49/121=40.5%) were present in only two countries and 41 (41/121=33.9%) were only present in one. Figure 1 shows the number of consensus barriers (n=31) in each delay and overlapping delays. The majority of the shared barriers came under the WHO building blocks of governance (n=7) and service delivery (n=8).
Table 2.
Barriers present in all three study countries (n=31)
| Original framework | Category of barrier | Institute of medicine domain if relevant | Barrier | Consensus | |
| WHO Building blocks | Consensus—all delays | Consensus predominant delay | |||
| Leadership/ Governance |
Information on equitable access to trauma care collected | 1,2,3,4 | 3 | ||
| Road infrastructure. | 1, 2, 3, 4 | 2 | |||
| The ‘right’ hospital location. The ‘right’ acute care facility location—near to patients. | 1, 2, 3, 4 | 3 | |||
| Rehabilitation services —available and near to patients. | 4 | 4 | |||
| Ambulance transport availability | 1,2,3, | 2 | |||
| Geographical coverage of ambulance services | 1,2,3 | 2 | |||
| Facility infrastructure | 1, 2,3,4 | 3 | |||
| Health system finance | Equity | Budget equitably allocated | 1, 2, 3, 4 | 3 | |
| Cost of transport to get to hospital and between hospitals. (Cost of accessing ambulances) | 1,2,4 | 2 | |||
| Costs of getting to and receiving care at follow-up | 4 | 4 | |||
| Service delivery | Timely | Traditional healers and their interface with the health system. | 1,2,3 | 1 | |
| Available health facility targets for trauma care | 3, 4 | 3 | |||
| Organisation of facilities | 1,3,4 | 3 | |||
| Wait time at facilities | 1,3,4 | 3 | |||
| Clear referral processes (within facilities, between facilities and including discharge) | 1,3,4 | 3 | |||
| Follow-up system | 4 | 4 | |||
| Appropriate provision of services for the level of demand. | 1, 2, 3, 4 | 3 | |||
| Resources (beds, equipment, intensive care unit) | 1, 3, 4 | 3 | |||
| Patient centred | Pain control | 1, 3, 4 | 3 | ||
| Data collected on patient outcomes or satisfaction | 1,3 | 3 | |||
| Respectful care/attitudes of staff towards patients | 1,3,4 | 1 | |||
| Effective | Complications after injuries | 1,4 | 1 | ||
| Interfacility transfer | 1,2,3,4 | 3 | |||
| Information systems | Patient education—when to seek care. | 1, 4 | 1 | ||
| Patient education—where to seek care. | 1,2 | 1 | |||
| staff understanding of data to be collected and tools to do so | 3,4 | 3 | |||
| Ambulance divert systems | 2,3 | 3 | |||
| Workforce | Staff supervision | 2,3,4 | 3 | ||
| Medicine and equipment | Available medications/other treatment | 1,3,4 | 3 | ||
| Available equipment. | 3,4 | 3 | |||
| Miscellaneous | Bystander help | Bystander fear of injury | 1,2 | 2 | |
The darker shade of green the more delays the barrier influences.
Delay 1 yellow, delay 2 darker yellow, delay 3 lighter green and delay 4 darker green.
Figure 1.
Number of consensus barriers in each delay and overlapping delays.
Out of the barriers shared across all countries, 7 (23%) were related to all four delays, 12 (39%) were related to three delays and 9 (29%) were related to two delays. Only three (9%) barriers were related to only one delay. More than half of the shared barriers (18/31=58%) were classified as predominantly related to delay 3 (‘Delays to receiving quality care’), while five (16%) were predominately related to delay 1 (‘Delays in seeking care’) and five (16%) barriers were predominately related to delay 2 (‘Delays in reaching care’), respectively. There were three barriers (10%) that were predominantly related to delay 4 (‘Delays in remaining in care’).
For almost all shared barriers, we achieved consensus on which was the predominant delay to which the barrier belonged. However, for one barrier ‘Poor follow-up care’, this was difficult. The Ghana team felt very strongly this would affect delay 1 (seeking care) just as much or possibly more than delay 4 (remaining in care).
Reflections
In this mixed-method, multicountry study, we found several barriers to accessing quality injury care across multiple domains of delays, quality, outcomes and health system building blocks. Our findings show that access to quality trauma care is a complex health system problem and indicate that understanding the issue in a holistic manner is likely to be a prerequisite to improving access to quality care. Moreover, we collected data from three different countries in Sub-Saharan Africa with different income and development status and found only a small proportion of the total number of barriers identified in all countries were shared across countries. This indicates that these barriers may transcend contexts and that solutions for them might be transferable to other countries in this region. However, our findings on the large numbers of barriers that are limited to just one or two countries also indicate that issues limiting access to quality injury care are likely to be highly contextually dependent and it cannot be taken for granted that solutions developed in one country, or context, will be transferable to another. Of particular note were the barriers that were only experienced in one country, and which were likely therefore to be the most contextually determined. These were barriers related to violence and alcohol abuse in South Africa, seeking and receiving care from traditional healers in Ghana, and issues related to seeking care when injuries occur at night in Rwanda.
We also found that while some barriers were seen using multiple data collection methods, many barriers were captured using just one of the data collection methods, showing the need to use a number of different methods when undertaking data collection to holistically understand access to quality injury care in LMICs. Most previous studies have addressed only one or two of the delay stages and used single methods, and are likely to have missed important barriers in access to care.12 Using different methods, we have shown some divergence in response regarding whether barriers are present or not, which adds to the understanding that single method studies or those with a focus on only one delay stage may not give a reliable picture of barriers in access to care. In a recent literature review by Whitaker et al12 Forty out of the 111 (40.5%) identified studies focused solely on barriers in delay 3, and only 3 studies (2.7%) focused on all three delays in access to care. Moreover, most of the studies were conducted in one country.12 We have found, as have others, that the majority of the shared barriers were related to delay 3,8 12 20 receiving care. However, using multiple methods, as we did in this study, ensures a broader array of barriers can be identified, and barriers occurring at delay 1 and delay 2 can also be seen as substantial contributors to delays in timely access of quality care for the injured. Similar findings have been seen in South Africa, where delays 1 and 2 contributed around 36% of avoidable mortality after injury.7 As our results show, barriers were not only around processes that would lead to effective clinical care, but also around the other quality outcomes of safety, timeliness, and patient-centred care; all issues that have been neglected in the global health agenda until recently.11
We have also shown that many barriers were experienced at multiple delay stages, exposing the intricacy of the effects of barriers on care-access. This is reflective of our previous findings in Rwanda20 which highlighted the complex and interconnected nature of barriers to health system access post injury.12 While this may make provision of solutions seem daunting, it could also be considered that improving one barrier that acts at multiple delays could improve several other delays, with a potentially synergistic or reinforcing effect.26 27 The same reasoning holds for multi-country interventions. For example, “Ambulance transport availability” is a barrier that was prioritised across all three countries in our study and which was found to act across multiple delays. This barrier influences the service user’s decision to seek care (delay 1) and their possibility to reach care (delay 2). Also, it influences delay 3 as we have defined interfacility transport as a third delay barrier after the patient has reached care. Additionally, this barrier influences patient’s decision to remain in care (delay 4). Hence improving ambulance transport availability is likely to have a substantial impact on timely access to quality care.
Ability to improve outcomes after injury in the countries included in this study and other LMICs will be limited if this is not a political priority. According to Shiffman and Smith there are four key components to achieving political priority in global health: actor power (the strengths of individuals and organisations concerned with the issue), ideas (the ways in which those involved with the issue understand and portray it), political context (the environments in which actors operate), and issue characteristics (features of the problem).28 We have found through our governance survey that some of these components are present in each country. For example, in Rwanda there is actor power and strong political commitment. The Rwanda Surgical Society made trauma a priority at their last general meeting in November 2019, which has hosted a national symposium on trauma care, and Rwanda has an Emergency Medical Services Strategic Plan,29 and a trauma registry capturing information on all trauma cases admitted to major referral hospitals in the country.30 31 However, without knowledge of issue characteristics, here, the barriers in accessing quality care for injuries, political will risks being poorly directed.
Conclusion
This mixed method multicountry study is one of the first of its kind showing there are multiple barriers in access to care for injuries in Rwanda, Ghana and South Africa. These three countries which have different development status and income levels had multiple barriers in access to injury care which shows that the issue is complex. Only a quarter of the barriers were shared across all three countries, suggesting the need for rigorous assessment in individual contexts using multiple data collection methods before developing interventions for improving access to quality care for injured patients.
Footnotes
Handling editor: Seye Abimbola
Twitter: @Mchantimah, @DrBarnabasAlay, @ORCID 0000-0003-0018-9096, @kathryn_chu_sa, @dr_staphy, @drjackoids
Collaborators: Equi-Trauma Collaborative: Maria Lisa Odland, Agnieszka Ignatowicz, Abdul-Malik Abdul-Latif, Justine Davies, Antonio Belli, Evangelos Balanikas, Anthony Howard, John Whitaker, Kathryn M. Chu, Karen Ferreira, Eyitayo O. Owolabi, Samukelisiwe Nyamathe, Stephen Tabriri, Bernard Appia Ofori, Sheba Mary Pognaa Kunfah, Mustapha Yakubu, Abebe Bekele, Barnabas Alyande, Pascal Nzasabimana and Jean-Claude Byiringiro.
Contributors: JID and JCB led the overall study; JID, JCB and JW developed the concept for the study. JCB, AB, KC and ST—led each country component; PN, MY, SW, BAO, A-MA-L, KF, SMPK, EOO—conducted the data collection in each country; BA, EB, AH, A-MA-L, MLO, AI and all authors contributed to the analysis of results and the discussion meeting in Ghana; MLO, AI and JID led the write up of the manuscript; all other authors commented on iterations of the manuscript and agreed to its submission for publication. JD is the guarantor of this manuscript or JD accepts full responsibility for the conduct of this study and controlled the decision to publish.
Funding: Funding for this study was provided by the National Institute of Health Research, NIHR, award number 130036.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon a reasonable request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
The overall study was approved by University of Birmingham Research Ethics Committee, UK (ERN_20-00880). Data collection in each individual country was approved by appropriate Ethics Review Boards: Ghana Health Service Ethics Review Committee (GHS-ERC005/02/20); The Stellenbosch University Health Research Ethics Committee for South Africa (Reference: N20/01/010) and National Health Research Committee (NHRC/2020/PROT/044) for Rwanda. Additional approval was obtained from the Western Cape Department of Health (Reference: WC_202006_022) in South Africa, and in the other countries approval was sought from the respective hospitals before visiting the facilities. Participants gave informed consent to participate in the study before taking part.
References
- 1.Gosselin RA, Spiegel DA, Coughlin R, et al. Injuries: the neglected burden in developing countries. Bull World Health Organ 2009;87:246–46a. 10.2471/BLT.08.052290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations . Global indicator framework for the sustainable development goals and targets of the 2030 agenda for sustainable development. Available: https://unstats.un.org/sdgs/indicators/Global%20Indicator%20Framework%20after%202021%20refinement_Eng.pdf [Accessed 8 Jul 2021].
- 4.Meara JG, Greenberg SLM. The Lancet Commission on global surgery global surgery 2030: evidence and solutions for achieving health, welfare and economic development. Surgery 2015;157:834–5. 10.1016/j.surg.2015.02.009 [DOI] [PubMed] [Google Scholar]
- 5.Rogers FB, Rittenhouse KJ, Gross BW. The golden hour in trauma: dogma or medical folklore? Injury 2015;46:525–7. 10.1016/j.injury.2014.08.043 [DOI] [PubMed] [Google Scholar]
- 6.Pouramin P, Li CS, Busse JW, et al. Delays in hospital admissions in patients with fractures across 18 low-income and middle-income countries (INORMUS): a prospective observational study. Lancet Glob Health 2020;8:e711–20. 10.1016/S2214-109X(20)30067-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edem IJ, Dare AJ, Byass P, et al. External injuries, trauma and avoidable deaths in Agincourt, South Africa: a retrospective observational and qualitative study. BMJ Open 2019;9:e027576. 10.1136/bmjopen-2018-027576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fraser A, Newberry Le Vay J, Byass P, et al. Time-critical conditions: assessment of burden and access to care using verbal autopsy in Agincourt, South Africa. BMJ Glob Health 2020;5:e002289. 10.1136/bmjgh-2020-002289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ratnapalan S, Lang D. Health care organizations as complex adaptive systems. Health Care Manag 2020;39:18–23. 10.1097/HCM.0000000000000284 [DOI] [PubMed] [Google Scholar]
- 10.Pawson R, Greenhalgh J, Brennan C, et al. Do reviews of healthcare interventions teach us how to improve healthcare systems? Soc Sci Med 2014;114:129–37. 10.1016/j.socscimed.2014.05.032 [DOI] [PubMed] [Google Scholar]
- 11.Kruk ME, Gage AD, Arsenault C, et al. High-Quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitaker J, O'Donohoe N, Denning M, et al. Assessing trauma care systems in low-income and middle-income countries: a systematic review and evidence synthesis mapping the three delays framework to injury health system assessments. BMJ Glob Health 2021;6:e004324. 10.1136/bmjgh-2020-004324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roder-DeWan S, Gupta N, Kagabo DM, et al. Four delays of child mortality in Rwanda: a mixed methods analysis of verbal social autopsies. BMJ Open 2019;9:e027435. 10.1136/bmjopen-2018-027435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Newsl Womens Glob Netw Reprod Rights 1991;36:22–4. [PubMed] [Google Scholar]
- 15.The World Bank . World bank open data, 2021. Available: https://data.worldbank.org/
- 16.Nyandekwe M, Nzayirambaho M, Kakoma JB. Universal health insurance in Rwanda: major challenges and solutions for financial sustainability case study of Rwanda community-based health insurance Part I. Pan Afr Med J 2020;37:55. 10.11604/pamj.2020.37.55.20376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ntakiyiruta G, Wong EG, Rousseau MC, et al. Trauma care and referral patterns in Rwanda: implications for trauma system development. Can J Surg 2016;59:35–41. 10.1503/cjs.008115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stats SA . Department: statistics South Africa, 2021. Republic of South Africa. Available: http://www.statssa.gov.za/
- 19.Stats SA. General household survey, 2019. Available: http://www.statssa.gov.za/publications/P0318/P03182019.pdf
- 20.Odland ML, Whitaker J, Nepogodiev D, et al. Identifying, prioritizing and visually mapping barriers to injury care in Rwanda: a multi-disciplinary Stakeholder exercise. World J Surg 2020;44:2903–18. 10.1007/s00268-020-05571-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute of Medicine . Six domains of health care quality. Available: https://www.ahrq.gov/talkingquality/measures/six-domains.html [Accessed 8 Jul 2021].
- 22.World Health Organisation . Monitoring the building blocks of health systems: a Handbook of indicators and their measurement strategies, 2010. Available: https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf
- 23.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753–60. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 24.Webster TR, Mantopoulos J, Jackson E, et al. A brief questionnaire for assessing patient healthcare experiences in low-income settings. Int J Qual Health Care 2011;23:258–68. 10.1093/intqhc/mzr019 [DOI] [PubMed] [Google Scholar]
- 25.Siddiqi S, Masud TI, Nishtar S, et al. Framework for assessing governance of the health system in developing countries: gateway to good governance. Health Policy 2009;90:13–25. 10.1016/j.healthpol.2008.08.005 [DOI] [PubMed] [Google Scholar]
- 26.Tapia-Conyer R, Gallardo-Rincón H, Saucedo-Martinez R. CASALUD: an innovative health-care system to control and prevent non-communicable diseases in Mexico. Perspect Public Health 2015;135:180–90. 10.1177/1757913913511423 [DOI] [PubMed] [Google Scholar]
- 27.World Health Organisation . Systems thinking for health systems strengthening, 2009. Available: https://apps.who.int/iris/bitstream/handle/10665/44204/9789241563895_eng.pdf;jsessionid=CE7C31FE990445C45152DA9F521E2CDF?sequence=1 [Accessed 25t Aug 2021].
- 28.Shawar YR, Shiffman J, Spiegel DA. Generation of political priority for global surgery: a qualitative policy analysis. Lancet Glob Health 2015;3:e487–95. 10.1016/S2214-109X(15)00098-4 [DOI] [PubMed] [Google Scholar]
- 29.Republic of Rwanda MoH . Emergency medical services strategic plan (2018-2024), 2018. Available: https://moh.prod.risa.rw/fileadmin/user_upload/Moh/Publications/Strategic_Plan/EMS_Strategic_Plan_2018-min.pdf
- 30.Rosenberg A, Ntirenganya F, Bagahirwa I, et al. First Rwanda national trauma symposium 2019: challenges and priorities. J Glob Health 2020;10:010201. 10.7189/jogh.10.010201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kearney AS, Kabeja LM, George N, et al. Development of a trauma and emergency database in Kigali, Rwanda. Afr J Emerg Med 2016;6:185–90. 10.1016/j.afjem.2016.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-008256supp001.pdf (419.6KB, pdf)
Data Availability Statement
Data are available upon a reasonable request.


