Abstract
Background
Idiopathic pulmonary fibrosis (IPF) is a chronic progressive lung disease with high morbidity and limited treatment options. Type 2 diabetes mellitus (T2DM) is a common comorbid illness among patients with IPF and is often treated with metformin, the first-line agent in the management of T2DM. There is growing evidence demonstrating metformin’s anti-fibrotic properties; however, there is little real-world clinical data regarding its potential effectiveness in IPF. This study aims to evaluate the clinical benefit of metformin in patients with IPF and T2DM.
Methods
This nationwide cohort study used de-identified administrative claims data from OptumLabs® Data Warehouse to identify 3599 adults with IPF and concomitant T2DM between January 1, 2014 and June 30, 2019. Two cohorts were created: a cohort treated with metformin (n = 1377) and a cohort not treated with metformin (n = 2222). A final 1:1 propensity score-matched cohort compared 1100 patients with IPF and T2DM receiving metformin to those with both diagnoses but not receiving metformin; matching accounted for age, sex, race/ethnicity, residence region, year, medications, oxygen use, smoking status, healthcare use, and comorbidities. Outcomes were all-cause mortality (primary) and hospitalizations (secondary).
Results
Among 2200 patients with IPF and T2DM included in this matched analysis, metformin therapy was associated with a reduction in all-cause mortality (hazard ratio [HR], 0.46; 95% confidence interval [CI], 0.36–0.58; p < 0.001) and hospitalizations (HR, 0.82; 95% CI, 0.72–0.93; p = 0.003) compared to patients not receiving metformin.
Conclusions
Among patients with IPF and T2DM, metformin therapy may be associated with improved clinical outcomes. However, further investigation with randomized clinical trials is necessary prior to metformin’s broad implementation in the clinical management of IPF.
Keywords: Idiopathic pulmonary fibrosis, Interstitial lung disease, Metformin, Type 2 diabetes mellitus, Mortality, Hospitalization
Background
Idiopathic pulmonary fibrosis (IPF) is a chronic progressive interstitial lung disease with high morbidity, mortality, and limited treatment options [1, 2]. Many therapies have been investigated as potential treatment options for IPF, but most have been ineffective [3–7] and, in some cases, harmful [8–10]. Currently, only two medications are approved by the U.S. Food and Drug Administration (FDA) for IPF: the anti-fibrotic agents nintedanib and pirfenidone, which were approved in 2014 based on phase 3 clinical trials demonstrating slowed decline in lung function in patients with IPF [11, 12]. Subsequent pooled analyses [13–16] and observational studies [17, 18] suggested that their use reduces the risk of hospitalizations and improves mortality. Yet, only between 25 and 60% of patients with IPF are prescribed these anti-fibrotic medications [19–22]. Many factors contribute to their limited use including high costs (estimated at $100,000 per year) [23], side effects, uncertainty regarding IPF diagnosis, and treatment deferral for presumed stable disease [19, 24]. Thus, additional therapies are needed to improve the health outcomes and reduce the risk of death among patients with IPF.
Type 2 diabetes mellitus (T2DM) is a common chronic health condition that is present in many patients with IPF [17]. Metformin is the first-line glucose-lowering medication in the management of T2DM [25]. In addition to metformin’s anti-glycemic control, there is accumulating evidence demonstrating anti-neoplastic [26–30], anti-aging [31–34], and anti-fibrotic properties [35–40]. Regarding its potential anti-fibrotic effect, initial in vivo studies showed that metformin reduced TGFβ1-induced fibrosis in human bronchial fibroblasts [41]. Several subsequent in vitro studies in murine models of bleomycin-induced lung fibrosis showed that mice treated with metformin after bleomycin exposure had decreased profibrotic markers [37, 38] as well as reduced histological [35–40] and radiological [40] signs of lung fibrosis compared to mice not receiving metformin. While these laboratory findings are intriguing, the concentrations and relative doses used in the cellular and rodent models were quite high, raising questions as to whether metformin would have similar impact on fibrosis in people with T2DM and IPF.
Beyond these pre-clinical findings, there is a paucity of clinical data regarding metformin’s effectiveness in patients with IPF. In fact, current evidence is limited to two studies. The first is a single post hoc analysis of three phase 3 clinical trials of pirfenidone where Spagnolo et al. investigated the effect of metformin on the clinical benefit of patients with IPF [42]. Metformin did not significantly impact clinical outcomes, including forced vital capacity (FVC) decline, 6-min walking distance (6MWD) decline, and death. However, this study was limited in its applicability and interpretation given the very small number of patients with metformin use (n = 71; 11.4%) and lack of formal power analysis. The second study is a retrospective study where Lambert et al. evaluated for significance of cardiovascular drugs on disease progression and survival in patients with idiopathic pulmonary fibrosis [43]. Metformin was again found to have no significant impact on IPF progression (demonstrated by annual FVC and diffusing capacity of the lungs for carbon monoxide (DLCO) decline) or survival. However, this study was also limited by its very small number of patients receiving metformin (n = 28).
Given the overall rarity of IPF, we chose to utilize a large healthcare claims database to enhance patient population diversity and size. To date, this study represents the only observational cohort analysis that evaluates for clinical benefit of metformin in patients with IPF in real-world practice. This nationwide cohort study sought to compare the risk of all-cause mortality among patients with IPF and concomitant T2DM receiving metformin to those not receiving metformin. In secondary analysis, the risk of hospitalizations was compared between IPF patients with and without metformin use.
Methods
Data source
We conducted a retrospective cohort study of de-identified administrative claims data from OptumLabs® Data Warehouse (OLDW), which is a large U.S. healthcare database containing information of enrollees in private and Medicare Advantage health plans [44]. Enrollees differ in age, race, ethnicity, incomes, and geographic location with representation from all 50 states. Per the Health Insurance Portability and Accountability Act of 1996 [45], institutional review board approval was not required since completely de-identified patient data was used.
Study population
The study population consisted of adults (≥ 18 years old) with IPF included in OLDW between January 1, 2014, and June 30, 2019. The diagnosis of IPF was established using either International Classification of Diseases, 9th edition (ICD-9) or International Classification of Diseases, 10th edition (ICD-10) codes for IPF or claims for ant-fibrotic medications present in medical and pharmacy claims, respectively. Patients were required to have either a single inpatient claim or two outpatient claims for IPF, as previously detailed by Dempsey et al. [17]. All patients were required to have 6 months of continuous enrollment in the health plan. The index date was defined as the first claims evidence of IPF after the 6-months enrollment criterion was met. Patients were also required to have a diagnosis of T2DM which was established using validated Healthcare Effectiveness Data and Information Set (HEDIS) criteria (an ICD-9 or ICD-10 billing code for T2DM, the use of insulin or oral anti-hyperglycemic agent, and either a single inpatient claim or two outpatient claims for T2DM) [46]. We excluded patients with invalid demographic data and type 1 diabetes mellitus (T1DM), defined as an ICD-9 or ICD-10 billing code for T1DM.
Comparator groups
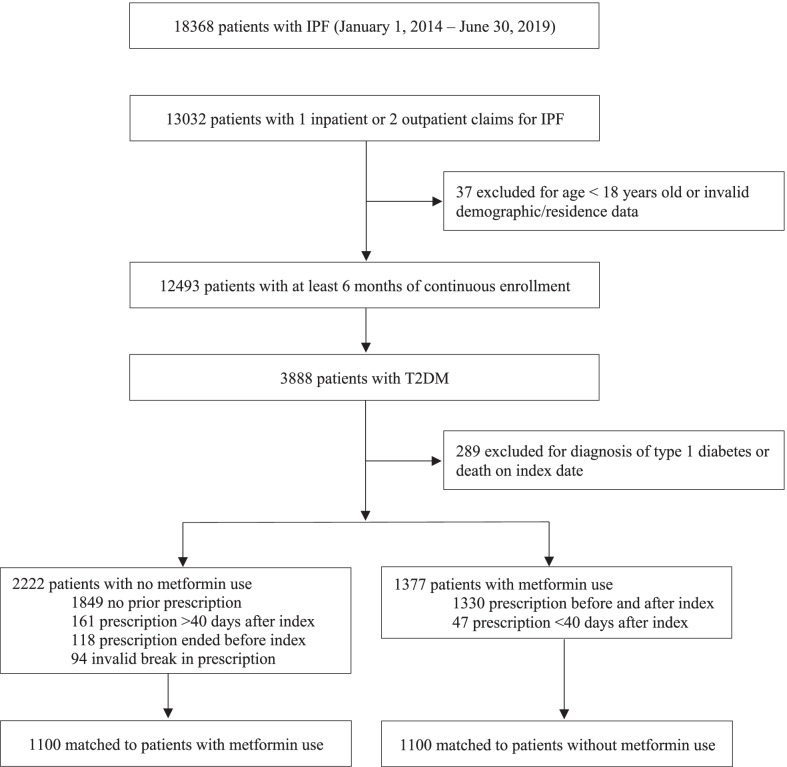
Patients with IPF were divided into those treated with metformin and those not treated with metformin, as seen in Fig. 1. The metformin-treated group included patients with a claim for metformin (any dose) any time prior to the index date and up until 40 days after the index date (to account for patients who started metformin after their index date). A 40-day window period was chosen because it was the median number of days (interquartile range 17, 78) to first metformin fill after index date. Most patients in the metformin-treated group had pharmacy claims for metformin that preceded their index date (1330/1377; 96.6%). Patients whose metformin prescription began > 40 days after the index date were placed in the comparator group and censored at time of treatment initiation (161/2222; 7.2%). The comparator group included those who had no prior prescription for metformin (1849/2222; 83.2%), those who discontinued metformin prior to index date (118/2222; 5.3%), and those who had an invalid break in prescription (94/2222; 4.2%).
Fig. 1.
Flow diagram of OptumsLab® cohort creation. IPF idiopathic pulmonary fibrosis, T2DM Type 2 diabetes mellitus, T1DM Type 1 diabetes mellitus
Patients were then matched 1:1 on age, sex, race, residence region, year, medications (see “Independent variables” section), oxygen use, smoking status, healthcare use (see “Independent variables” section), and comorbidities (cardiac arrhythmia, congestive heart failure, chronic pulmonary disease, depression, hypertension, obesity, pulmonary circulation disorder, renal failure, rheumatoid arthritis, and valvular disease). As in our previous studies, we used oxygen use as a measure for disease severity matching since lung functions measures are not available in this dataset [17].
Independent variables
Comorbidities diagnosed in the 6 months prior to index date were identified using ICD-9 and ICD-10 diagnostic codes associated with medical claims. Comorbidity burden was evaluated using the Elixhauser sum of conditions [47]. Healthcare use including hospitalizations, primary care office visits, and pulmonologist office visits were captured by medical claims in the 6 months preceding the index date. Medication use (specifically oral corticosteroids, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), statins, sodium-glucose co-transporter-2 (SGLT2) inhibitors, insulin, dipeptidyl peptidase-4 (DPP4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, sulfonylureas, glitazones, and anti-fibrotics) was defined as having filled a prescription within 6 months prior to the index date. Oxygen use was identified using Healthcare Common Procedure Coding System indicating oxygen supplies during the 6 months prior to index date.
Follow up
Patients were followed until the end of the study period (June 30, 2019), end of enrollment in health insurance plan, death, start of first prescription fill for metformin (for untreated cohort) or metformin discontinuation (for treated cohort) which was defined as no prescription fill 30 days after the end supply.
Study outcomes
Primary outcome was all-cause mortality. Secondary outcome was all-cause hospitalizations.
Statistical analysis
We used propensity score matching to balance the differences in baseline characteristics between those receiving metformin and those not receiving metformin. A propensity score was estimated using logistic regression based on age, sex, race, residence region, year, medications (see “Independent variables” section), oxygen use, smoking status, healthcare use (see “Independent variables” section), and comorbidities (cardiac arrhythmia, congestive heart failure, chronic pulmonary disease, depression, hypertension, obesity, pulmonary circulation disorder, renal failure, rheumatoid arthritis, and valvular disease). Specifically, we used one-to-one nearest-neighbor caliper matching to match patients based on the logit of the propensity score [48]. We evaluated the standardized difference to assess the balance of covariates after matching, and a standardized difference ≤ 10% was considered acceptable [49]. When balance was not achieved through propensity score matching, we controlled for the unbalanced variable in the analysis. We then used Cox proportional hazard regression to compare mortality and hospitalizations in the matched cohort between patients on metformin and those not on metformin.
Falsification endpoint analysis was performed with one endpoint selected: fracture. Corresponding ICD-9 and ICD-10 diagnostic codes are listed in Table 1.
Table 1.
Diagnosis codes
| Diagnosis | ICD-9 | ICD-10 |
|---|---|---|
| Idiopathic pulmonary fibrosis | 516.31 | J84.112 |
| Diabetes mellitus, type 2 | 250. × 0, 250. × 2 | E11.xxx, O24.1xx |
| Diabetes mellitus, type 1 | 250. × 1, 250. × 3 | E10.xxx |
| Fracture | 733.1x, 733.8x, 733.93, 733.94, 733.95, 733.96, 733.97, 733.98, 800–829 | M48.4x, M80.8x, M81.8, M83.3x-6x, S02.x, S12.x, S22.x, S32.x, S42.x, S52.x, S62.x, S72.x, S82.x, S92.x |
ICD-9 International Classification of Diseases, 9th edition; ICD-10 International Classification of Diseases, 10th edition
For a sensitivity analysis, we used inverse probability treatment weighting (IPTW) instead of propensity score matching to repeat the main analysis. A weight of 1/propensity score was used for patients receiving metformin and 1/(1-propensity score) for those not receiving metformin.
All analyses were conducted using SAS 9.4 (SAS Institute Inc.) and Stata version 15.1 (StataCorp).
Results
Characteristics of the patient population
A total of 18,368 patients were examined for eligibility. There were 3599 (19.6%) patients with IPF and concomitant T2DM who met eligibility criteria and were included in the study. A total of 1377 (38.2%) were treated with metformin upon cohort entry. Of these 1377 patients, 1100 were 1:1 propensity score matched to patients with IPF and T2DM that had not received metformin, as seen in Fig. 1. The baseline clinical characteristics were well balanced between the groups with standardized differences < 10%, as shown under Table 2.
Table 2.
Baseline characteristics of patients before and after propensity score matching
| No. (%) of patients | ||||||||
|---|---|---|---|---|---|---|---|---|
| Before propensity score matching | After propensity score matching | |||||||
| No metformin (n = 2222) | Metformin (n = 1377) | Std diff | p value | No metformin (n = 1100) | Metformin (n = 1100) | Std diff | p value | |
| Age, years | < 0.001 | 0.88 | ||||||
| Mean | 73.4 (9.4) | 72.2 (8.5) | – | 72.4 (9.4) | 72.5 (8.8) | – | ||
| Median (IQR) | 75 (68–82) | 73 (67–78) | – | 73 (67–80) | 74 (68–79) | – | ||
| Age group, years | < 0.001 | 0.63 | ||||||
| 18–54 | 89 (4.0) | 45 (3.3) | 0.0% | 48 (4.4) | 40 (3.6) | 0.0% | ||
| 55–64 | 278 (12.5) | 187 (13.6) | 3.2% | 155 (14.1) | 146 (13.3) | 0.0% | ||
| 65–74 | 729 (32.8) | 572 (41.5) | 18.1% | 419 (38.1) | 411 (37.4) | 0.6% | ||
| 75 + | 1126 (50.7) | 573 (41.6) | 0.0% | 478 (43.5) | 503 (45.7) | 0.0% | ||
| Sex | 0.02 | 0.73 | ||||||
| Female | 1042 (46.9) | 591 (42.9) | 0.0% | 511 (46.5) | 503 (45.7) | 2.0% | ||
| Male | 1180 (53.1) | 786 (57.1) | 8.0% | 589 (53.5) | 597 (54.3) | 0.0% | ||
| Race | 0.004 | 0.99 | ||||||
| White | 1332 (59.9) | 794 (57.7) | 7.9% | 645 (58.6) | 647 (58.8) | 0.0% | ||
| Black | 334 (15.0) | 170 (12.3) | 0.0% | 158 (14.4) | 151 (13.7) | 0.0% | ||
| Hispanic | 358 (16.1) | 263 (19.1) | 7.9% | 191 (17.4) | 193 (17.5) | 0.0% | ||
| Asian | 64 (2.9) | 60 (4.4) | 2.1% | 35 (3.2) | 34 (3.1) | 0.2% | ||
| Unknown | 134 (6.0) | 90 (6.5) | 0.0% | 71 (6.5) | 75 (6.8) | 0.8% | ||
| Insurance | 0.85 | 0.32 | ||||||
| Commercial | 245 (11.0) | 149 (10.8) | – | 135 (12.3) | 120 (10.9) | – | ||
| Medicare advantage | 1977 (89.0) | 1228 (89.2) | – | 965 (87.7) | 980 (89.1) | – | ||
| Census Region | 0.54 | 0.71 | ||||||
| Midwest | 535 (24.1) | 324 (23.5) | 0.0% | 243 (22.1) | 264 (24.0) | 0.0% | ||
| Northeast | 336 (15.1) | 200 (14.5) | 0.0% | 166 (15.1) | 156 (14.2) | 3.0% | ||
| South | 1167 (52.5) | 720 (52.3) | 0.0% | 600 (54.5) | 586 (53.3) | 0.9% | ||
| West | 184 (8.3) | 133 (9.7) | 4.8% | 91 (8.3) | 94 (8.5) | 0.0% | ||
| Year | 0.60 | 1.00 | ||||||
| 2014 | 392 (17.6) | 224 (16.3) | 0.0% | 187 (17.0) | 187 (17.0) | 2.0% | ||
| 2015 | 349 (15.7) | 204 (14.8) | 0.0% | 168 (15.3) | 171 (15.5) | 0.0% | ||
| 2016 | 416 (18.7) | 254 (18.4) | 0.0% | 217 (19.7) | 210 (19.1) | 1.7% | ||
| 2017 | 466 (21.0) | 288 (20.9) | 0.0% | 229 (20.8) | 229 (20.8) | 0.0% | ||
| 2018 | 409 (18.4) | 273 (19.8) | 3.6% | 202 (18.4) | 206 (18.7) | 0.0% | ||
| 2019* | 190 (8.6) | 134 (9.7) | 4.1% | 97 (8.8) | 97 (8.8) | 0.0% | ||
| Anti-fibrotics | 401 (18.0) | 391 (28.4) | 24.7% | < 0.001 | 260 (23.6) | 255 (23.2) | 0.0% | 0.80 |
| Baseline medications | ||||||||
| Steroids | 1009 (45.4) | 600 (43.6) | 0.0% | 0.28 | 505 (45.9) | 484 (44.0) | 2.0% | 0.37 |
| ACE inhibitor | 530 (23.9) | 469 (34.1) | 22.6% | < 0.001 | 344 (31.3) | 330 (30.0) | 1.7% | 0.52 |
| ARB | 558 (25.1) | 433 (31.4) | 14.1% | < 0.001 | 331 (30.1) | 322 (29.3) | 0.1% | 0.67 |
| Statins | 1296 (58.3) | 1005 (73.0) | 31.2% | < 0.001 | 756 (68.7) | 739 (67.2 | 0.0% | 0.44 |
| SGLT2 | 28 (1.3) | 50 (3.6) | – | < 0.001 | 13 (1.2) | 29 (2.6) | – | 0.01 |
| Insulin | 664 (29.9) | 248 (18.0) | 0.0% | < 0.001 | 231 (21.0) | 232 (21.1) | 0.0% | 0.96 |
| DPP4 | 229 (10.3) | 176 (12.8) | – | 0.02 | 143 (13.0) | 120 (10.9) | – | 0.13 |
| GLP-1 | 50 (2.3) | 63 (4.6) | – | 0.00 | 33 (3.0) | 42 (3.8) | – | 0.29 |
| Sulfonylureas | 483 (21.7) | 426 (30.9) | 21.0% | < 0.001 | 294 (26.7) | 294 (26.7) | 0.0% | 1.0 |
| Glitazones | 58 (2.6) | 71 (5.2) | – | 0.00 | 38 (3.5) | 51 (4.6) | – | 0.16 |
| HbA1c lab result | 0.00 | 0.04 | ||||||
| Mean (SD) | 6.9 (1.3) | 7.0 (1.2) | – | 6.9 (1.3) | 7.0 (1.2) | – | ||
| Median (IQR) | 6.6 (6.1–7.5) | 6.8 (6.2–7.5) | – | 6.6 (6.1–7.4) | 6.8 (6.2–7.5) | – | ||
| Primary care office visit | 1821 (82.0) | 1209 (87.8) | – | < 0.001 | 939 (85.4) | 964 (87.6) | – | 0.12 |
| Pulmonary office visit | 1237 (55.7) | 843 (61.2) | 11.3% | 0.00 | 652 (59.3) | 659 (59.9) | 0.7% | 0.76 |
| Baseline hospitalizations | < 0.001 | 0.92 | ||||||
| 0 | 1192 (53.6) | 925 (67.2) | 27.9% | 693 (63.0) | 701 (63.7) | 0.0% | ||
| 1 | 636 (28.6) | 326 (23.7) | 0.0% | 280 (25.5) | 277 (25.2) | 0.0% | ||
| 2 + | 394 (17.7) | 126 (9.2) | 0.0% | 127 (11.5) | 122 (11.1) | 0.8% | ||
| DME, oxygen | 1001 (45.0) | 587 (42.6) | 0.0% | 0.16 | 479 (43.5) | 473 (43.0) | 0.4% | 0.80 |
| Current smoker | 646 (29.1) | 395 (28.7) | 0.0% | 0.80 | 342 (31.1) | 321 (29.2) | 0.2% | 0.33 |
| Elixhauser comorbidity count | < 0.001 | 0.93 | ||||||
| Mean (SD) | 6.9 (3.1) | 5.8 (2.7) | – | 6.1 (2.7) | 6.1 (2.8) | – | ||
| Median (IQR) | 7 (5–9) | 6 (4–7) | – | 6 (4–8) | 6 (4–8) | – | ||
| Elixhauser conditions | ||||||||
| Cardiac arrhythmia | 905 (40.7) | 405 (29.4) | 0.0% | < 0.001 | 357 (32.5) | 364 (33.1) | 1.3% | 0.75 |
| Congestive heart failure | 941 (42.3) | 417 (30.3) | 0.0% | < 0.001 | 371 (33.7) | 376 (34.2) | 4.3% | 0.82 |
| Chronic pulmonary disease | 1525 (68.6) | 895 (65.0) | 0.0% | 0.02 | 737 (67.0) | 722 (65.6) | 0.0% | 0.50 |
| Depression | 368 (16.6) | 176 (12.8) | 0.0% | 0.00 | 160 (14.5) | 156 (14.2) | 0.0% | 0.81 |
| Hypertension | 1828 (82.3) | 1130 (82.1) | 0.0% | 0.88 | 916 (83.3) | 908 (82.5) | 1.4% | 0.65 |
| Obesity | 371 (16.7) | 227 (16.5) | 0.0% | 0.87 | 186 (16.9) | 183 (16.6) | 1.8% | 0.86 |
| Pulmonary circulation disorder | 512 (23.0) | 300 (21.8) | 0.0% | 0.38 | 250 (22.7) | 248 (22.5) | 1.9% | 0.92 |
| Renal failure | 764 (34.4) | 206 (15.0) | 0.0% | < 0.001 | 186 (16.9) | 203 (18.5) | 0.0% | 0.34 |
| Rheumatoid arthritis | 300 (13.5) | 167 (12.1) | 0.0% | 0.23 | 148 (13.5) | 143 (13.0) | 1.3% | 0.75 |
| Valvular disease | 575 (25.9) | 276 (20.0) | 0.0% | 0.00 | 239 (21.7) | 238 (21.6) | 0.0% | 0.96 |
SGLT2 sodium-glucose co-transporter-2, DPP4 dipeptidyl peptidase-4, GLP-1 glucagon-like peptide-1, DME durable medical equipment
*From January 1,2019–June 30, 2019
The mean ages of metformin-treated and untreated cohorts were 72.5 years (SD, 8.8) and 72.4 years (SD, 9.4), respectively. Men comprised 53.5% of the cohort untreated with metformin and 54.3% of the metformin-treated cohort. In the overall unmatched cohort, the percentage of patients with IPF that received an anti-fibrotic medication was 18.0% in the metformin-untreated cohort and 28.4% in the metformin-treated group. After 1:1 matching, the percentage of patients with IPF that received an anti-fibrotic medication was 23.6% in the metformin-untreated cohort and 23.2% in the metformin-treated group. The mean HbA1c was 6.9 (SD, 1.3) for the metformin-untreated cohort and 7.0 (SD, 1.2) for the metformin-treated cohort. The most prevalent comorbidities in the overall unmatched cohort were hypertension (82.2%), other chronic pulmonary conditions (67.2%), and congestive heart failure (37.7%). Mean durations of observation were 292.4 days (SD, 316.3) and 432.2 days (SD, 431.2) in the treated and untreated cohorts, respectively.
Association of metformin use with all-cause mortality
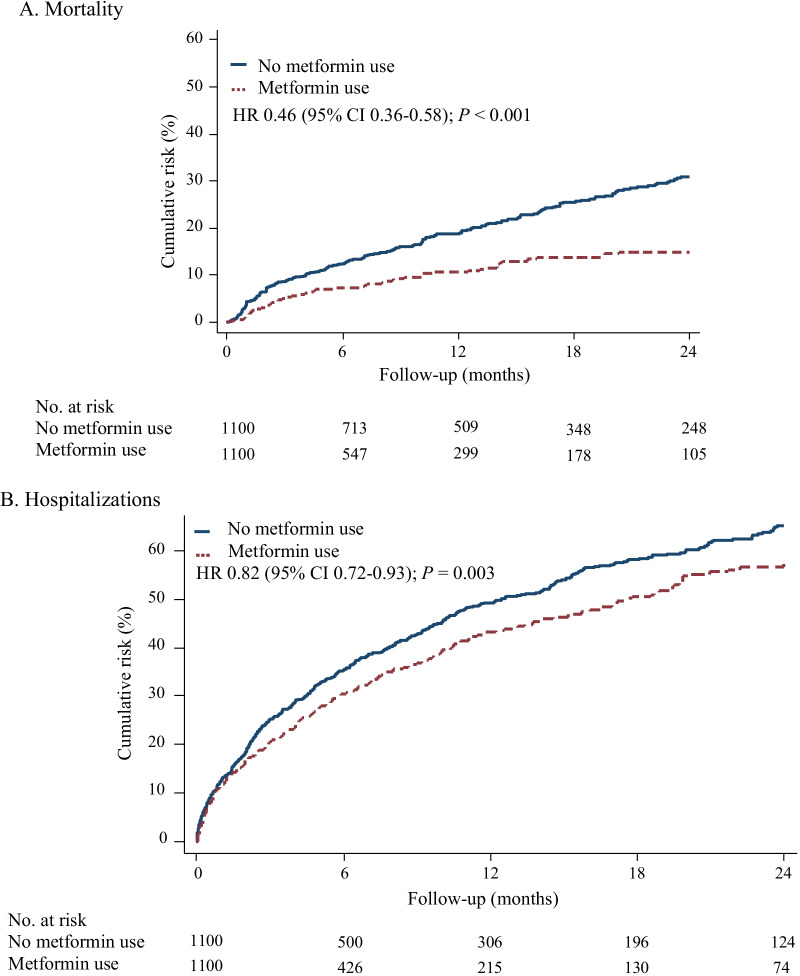
We next analyzed whether the use of metformin in patients with IPF and T2DM was associated with different all-cause mortality in the study population. Metformin use in the cohort diagnosed with both IPF and T2DM was associated with a significant decreased risk of all-cause mortality (hazard ratio [HR], 0.46; 95% confidence interval [CI], 0.36–0.58; p < 0.001) compared to patients with both diagnoses that were not receiving metformin, as shown in Fig. 2A and Table 3.
Fig. 2.
Kaplan–Meier curves displaying cumulative risk of mortality (A) and hospitalizations (B) among patients with idiopathic pulmonary fibrosis with and without metformin use
Table 3.
Cox proportional hazard regression comparing mortality and hospitalizations among patients with idiopathic pulmonary fibrosis with and without metformin use
| Rate per 100 (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Before propensity score matching | After propensity score matching | Hazard ratio (95% CI) | p value | |||
| No metformin (n = 2222) | Metformin (n = 1377) | No metformin (n = 1100) | Metformin (n = 1100) | |||
| Death | 25.1 (23.3, 27.1) | 10.5 (8.7, 12.5) | 20.6 (18.4, 23.2) | 10.5 (8.5, 12.8) | 0.46 (0.36, 0.58) | < 0.001 |
| Hospitalization | 76.1 (72.0, 80.6) | 55.12 (50.4, 60.3) | 64.3 (59.2, 69.9) | 57.8 (52.4, 63.8) | 0.82 (0.72, 0.93) | 0.003 |
Association of metformin use with hospitalizations
In a similar manner, we further sought to determine whether the use of metformin in patients with IPF and T2DM was associated with differing rates of hospitalization. Metformin use in this cohort was associated with a significant decreased risk of hospitalizations (HR, 0.82; 95% CI, 0.72–0.93; p = 0.003), as demonstrated in Fig. 2B and Table 3.
Falsification analysis and sensitivity analysis
We then performed falsification endpoint analysis to test for confounding. These results are depicted in Table 4 and confirm our findings (HR, 0.75; 95% CI, 0.45–1.21; p = 0.23). We also performed a sensitivity analysis using IPTW as seen in Table 5 which demonstrated similar results to our main analysis.
Table 4.
Falsification endpoint analysis
| Rate per 100 (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Before propensity score matching | After propensity score matching | Hazard ratio (95% CI) | p value | |||
| No metformin (n = 2222) | Metformin (n = 1100) | No metformin (n = 2222) | Metformin (n = 1100) | |||
| Fracture | 4.57 (3.81, 5.48) | 2.54 (1.75, 3.68) | 4.00 (3.05, 5.25) | 3.01 (2.05, 4.4) | 0.75 (0.45, 1.21) | 0.23 |
Table 5.
Sensitivity analysis using inverse probably treatment weighting
| Before propensity score matching | After propensity score matching | Hazard ratio (95% CI) | p value | |||
|---|---|---|---|---|---|---|
| No metformin (n = 2222) | Metformin (n = 1377) | No metformin (n = 2222) | Metformin (n = 1377) | |||
| Death | 25.1 (23.3, 27.1) | 10.5 (8.7, 12.5) | 22.5 (20.7, 24.6) | 11.6 (9.2, 14.7) | 0.46 (0.36, 0.58) | < 0.001 |
| Hospitalization | 76.1 (72.0, 80.6) | 55.12 (50.4, 60.3) | 70.8 (65.7, 76.3) | 63.4 (55.7, 72.3) | 0.81 (0.72, 0.92) | 0.001 |
Effects of cardiovascular disease and renal disease on treatment effects of metformin in IPF with T2DM
Finally, we assessed the potential differences in metformin effect based upon whether patients had coded cardiovascular and renal diseases including arrythmia, congestive heart failure (CHF), peripheral vascular disease (PVD) or renal disease. We did not observe any significant differences in the effects of metformin based on the presence or absence of these other coded diagnoses (Table 6).
Table 6.
Effects of cardiovascular and renal disease on treatment effects of metformin in IPF with T2DM
| Matched | Treated adjusted hazard ratio [95% CI] | p-value for interaction | ||
|---|---|---|---|---|
| No metformin (N = 1100) | Metformin (N = 1100) | |||
| Arrhythmia | 0.41 | |||
| Yes | 30.64 (25.52, 36.78) | 17.07 (12.70, 22.94) | 0.49 (0.34, 0.69) | |
| No | 16.80 (14.41, 19.57) | 7.67 (5.76, 10.21) | 0.42 (0.31, 0.60) | |
| CHF | 0.07 | |||
| Yes | 30.96 (26.05, 36.79) | 21.52 (16.21, 28.55) | 0.58 (0.41, 0.81) | |
| No | 16.04 (13.67, 18.83) | 6.64 (4.93, 8.96) | 0.39 (0.28, 0.55) | |
| PVD | 0.39 | |||
| Yes | 24.12 (18.95, 30.71) | 15.00 (10.05, 22.37) | 0.56 (0.35, 0.90) | |
| No | 19.76 (17.27, 22.59) | 9.43 (7.42, 11.98) | 0.44 (0.33, 0.58) | |
| Renal | 0.52 | |||
| Yes | 25.12 (19.42, 32.50) | 15.19 (9.90, 23.29) | 0.55 (0.33, 0.90) | |
| No | 19.72 (17.28, 22.49) | 7.32 (7.56, 12.08) | 0.44 (0.34, 0.58) | |
Discussion
Metformin therapy in patients with IPF and concomitant T2DM was observed to have a significant 54% reduction in all-cause mortality in this large nationwide claims-based dataset. This is striking and represents a far stronger effect than previously observed with anti-fibrotic therapy in a similar population, where anti-fibrotic agents reduced the risk of all-cause mortality by 23% [17]. Metformin was further associated with an 18% lower risk of hospitalization for any cause. In a similar population, the two FDA-approved anti-fibrotic medications only had a trend towards decreased hospitalization [18].
The anti-fibrotic medications nintedanib and pirfenidone are currently the only FDA approved medications with demonstrated clinical benefit in IPF, yet they are underutilized with these medications being prescribed in only about 25% to 60% of patients with IPF in various studies [19–22]. Their use is limited due to high cost (estimated in the U.S. at $100,000 per year) [23], adverse side effects, uncertainties regarding the diagnosis of IPF, and treatment deferral for presumed stable disease [19, 24]. In contrast however, metformin is affordable, widely available, and safe. It serves as the first-line agent in the management of T2DM [25] and is used to treat select patients with pre-diabetes [50] as well as an alternative agent in patients with gestational diabetes [51] and polycystic ovarian syndrome [52, 53].
There are laboratory investigations that provide some insights into the possible effectiveness of metformin in IPF. As previously mentioned, metformin has been shown to reduce lung fibrosis in murine models of bleomycin-induced lung fibrosis [35–40]. While the mechanism by which metformin reduces the development of lung fibrosis and accelerates its resolution is unknown, several hypotheses exist. The predominant hypothesis revolves around metformin-mediated stimulation of adenosine monophosphate-activated protein kinase (AMPK) [36, 38], which is a critical cellular energy sensor and regulator of cellular metabolism [54, 55]. AMPK protects cellular functions by converting cells to a catabolic state after metabolic stressors (i.e. hypoxia) interfere with adenosine triphosphate production [56, 57]. However other metformin-mediated signaling pathways have been implicated in the reduction of lung fibrosis including suppression of the pro-fibrotic cytokine insulin-like growth factor-1 (IGF-1) [40] and activation of BMP2-PPAR (bone morphogenetic protein-2-peroxisome proliferator-activated receptor) gamma that ultimately results in trans-differentiation of myofibroblasts to lipofibroblasts [39].
It is important to emphasize that our current study only observes an association of metformin use with better clinical outcomes in patients with both IPF and T2DM and does not establish causality nor provide any information as to whether this agent has altered the course of the fibrotic disease itself. Claims-based analyses such as this cannot assess the impact of metformin on surrogate endpoints of fibrotic disease progression, like FVC decline, DLCO decline, or 6-min walk test. Instead, the current study provides significant initial insights into the clinically meaningful and patient-centric endpoints of mortality and hospitalizations. Indeed, metformin may reduce mortality and hospitalizations through its effects on cardiovascular disease, respiratory complications of lung fibrosis, or overall health of the patient. Alternatively, perhaps there is an interaction between the anti-fibrotic medications and metformin that potentiates each other’s effect—hence heightening the vast differences in observed outcomes. Metformin may offer cardiovascular protection to patients with IPF as it does in patients with T2DM [58–61]. In that light, it should be noted that cardiac disease is a common cause of death in patients with IPF, second only to respiratory failure [62, 63].
This study has several limitations. First, ICD billing codes were used to identify patients with IPF. IPF is difficult to diagnose and often requires multidisciplinary review for accurate diagnosis [64], so relying solely on billing codes for identification may result in inclusion of patients with erroneous diagnoses. However, we used the most accurate billing codes for IPF available for our review [65], a method that has been used previously in other studies [17, 22]. In addition, given the observational nature of this analysis, confounding factors cannot be completely eliminated, despite our rigorous statistical adjustments, falsification testing, and propensity score-matching. Our third limitation is due to cohort design as our treated cohort consisted of patients who filled a prescription for metformin. Unfortunately, in such a real-world analysis it is not possible to guarantee all patients reliably took the medication. Regardless, patients in our treated cohort consistently filled their prescriptions and those that did not refill metformin were excluded.
Conclusions
To our knowledge, this is the first real-world study assessing the clinical benefit of metformin in patients with IPF and T2DM. Several clinically relevant observations were gleaned from this U.S national, claims-based retrospective cohort analysis, most importantly that metformin therapy in patients with IPF and T2DM was associated with a significant reduction in all-cause mortality. While these results are intriguing, caution is encouraged. Specific recommendations for the clinical management of idiopathic pulmonary fibrosis will require further investigation, including randomized clinical trials that ideally delineate between cardiovascular protection, disease stabilization, and improvement in the course of fibrosis by utilizing objective measures such as pulmonary function testing and thoracic imaging.
Acknowledgements
The authors thank the members of the Mayo Clinic Division of Pulmonary and Critical Care for helpful discussions during the course of these investigations.
Abbreviations
- IPF
Idiopathic pulmonary fibrosis
- T2DM
Type 2 diabetes mellitus
- TGFβ1
Transforming growth factor-beta 1
- HR
Hazard ratio
- CI
Confidence interval
- U.S.
United States
- FDA
Federal Drug Administration
- FVC
Forced vital capacity
- 6MWD
6-Minute walking distance
- DLCO
Diffusing capacity of the lungs for carbon monoxide
- OLDW
OptumLabs® Data Warehouse
- ICD-9
International Classification of Diseases, Ninth Edition
- ICD-10
International Classification of Diseases, Tenth Edition
- HEDIS
Healthcare effectiveness data and information set
- T1DM
Type 1 diabetes mellitus
- ACE
Angiotensin-converting enzyme
- ARB
Angiotensin receptor blockers
- SGLT2
Sodium-glucose co-transporter-2
- DPP4
Dipeptidyl peptidase-4
- GLP-1
Glucagon-like peptide-1
- IPTW
Inverse probability treatment weighting
- SD
Standard deviation
- AMPK
Adenosine monophosphate-activated protein kinase
- IGF-1
Insulin-like growth factor
- BMP2-PPAR
Bone morphogenetic protein-2-peroxisome proliferator-activated receptor
Authors' contributions
AHL made substantial contributions to the conception, designed the work, and revised the manuscript. SRP and LRS performed the analyses and were involved in the interpretation of data. TTT, BTK, TMD, RGM, and AHL drafted and revised the manuscript. All authors approved the submitted version and have agreed to be personally accountable for their contributions. All authors read and approved the final manuscript.
Funding
AHL receives supported by a grant from Three Lakes Foundation (Grant No. TLF-1) and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. The sponsors of this study had no role in the design of the study, or collection, analysis, and interpretation of data, or in writing of the manuscript.
Availability of data and materials
The data underlying the results of this study are third party data owned by OptumLabs and contain sensitive patient information; therefore, the data is only available upon request. Interested researchers engaged in HIPAA compliant research may contact connected@optum.com for data access requests. The data use requires researchers to pay for rights to use and access the data.
Declarations
Ethics approval and consent to participate:
These studies were conducted in compliance with all relevant regulations and guidelines. The Mayo Clinic Institutional Review Board has reviewed the use of data from the OptumLabs® Data Warehouse, a large US database with de-identified administrative claims data for individuals enrolled in private and Medicare Advantage health plans. In compliance with the Health Insurance Portability and Accountability Act and the U.S. National Institutes of Health, this research represents the use of completely de-identified healthcare claims data. Accordingly, this research is deemed exempt from being considered human subjects research by both the Mayo Clinic Institutional Review Board and the NIH.
Consent for publication
Since all subjects have been completely de-identified, and only grouped summary data is shown, the need for additional informed consent for publication has also been waived by the Mayo Clinic Institutional Review Board. Furthermore, since all patients have been completely deidentified, it is impossible to recontact any of these individuals.
Competing interests
There are no competing conflicts of interest for any of the authors with the content of this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: treatment of idiopathic pulmonary fibrosis. An update of the 2011 Clinical Practice Guideline. Am J Respir Crit Care Med. 2015;192(2):e3–19. doi: 10.1164/rccm.201506-1063ST. [DOI] [PubMed] [Google Scholar]
- 2.Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198(5):e44–e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 3.Martinez FJ, de Andrade JA, Anstrom KJ, King TE, Jr, Raghu G. Randomized trial of acetylcysteine in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2093–2101. doi: 10.1056/NEJMoa1401739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oldham JM, Ma SF, Martinez FJ, Anstrom KJ, Raghu G, Schwartz DA, et al. TOLLIP, MUC5B, and the response to N-acetylcysteine among individuals with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2015;192(12):1475–1482. doi: 10.1164/rccm.201505-1010OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King TE, Jr, Albera C, Bradford WZ, Costabel U, Hormel P, Lancaster L, et al. Effect of interferon gamma-1b on survival in patients with idiopathic pulmonary fibrosis (INSPIRE): a multicentre, randomised, placebo-controlled trial. Lancet. 2009;374(9685):222–228. doi: 10.1016/S0140-6736(09)60551-1. [DOI] [PubMed] [Google Scholar]
- 6.Daniels CE, Lasky JA, Limper AH, Mieras K, Gabor E, Schroeder DR. Imatinib treatment for idiopathic pulmonary fibrosis: randomized placebo-controlled trial results. Am J Respir Crit Care Med. 2010;181(6):604–610. doi: 10.1164/rccm.200906-0964OC. [DOI] [PubMed] [Google Scholar]
- 7.Raghu G, Brown KK, Costabel U, Cottin V, du Bois RM, Lasky JA, et al. Treatment of idiopathic pulmonary fibrosis with etanercept: an exploratory, placebo-controlled trial. Am J Respir Crit Care Med. 2008;178(9):948–955. doi: 10.1164/rccm.200709-1446OC. [DOI] [PubMed] [Google Scholar]
- 8.Raghu G, Anstrom KJ, King TE, Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366(21):1968–1977. doi: 10.1056/NEJMoa1113354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raghu G, Behr J, Brown KK, Egan JJ, Kawut SM, Flaherty KR, et al. Treatment of idiopathic pulmonary fibrosis with ambrisentan: a parallel, randomized trial. Ann Intern Med. 2013;158(9):641–649. doi: 10.7326/0003-4819-158-9-201305070-00003. [DOI] [PubMed] [Google Scholar]
- 10.Noth I, Anstrom KJ, Calvert SB, de Andrade J, Flaherty KR, Glazer C, et al. A placebo-controlled randomized trial of warfarin in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2012;186(1):88–95. doi: 10.1164/rccm.201202-0314OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.King TE, Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 12.Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 13.Fisher M, Nathan SD, Hill C, Marshall J, Dejonckheere F, Thuresson PO, et al. Predicting life expectancy for pirfenidone in idiopathic pulmonary fibrosis. J Manag Care Spec Pharm. 2017;23(3-b Suppl):S17–s24. doi: 10.18553/jmcp.2017.23.3-b.s17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nathan SD, Albera C, Bradford WZ, Costabel U, Glaspole I, Glassberg MK, et al. Effect of pirfenidone on mortality: pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir Med. 2017;5(1):33–41. doi: 10.1016/S2213-2600(16)30326-5. [DOI] [PubMed] [Google Scholar]
- 15.Richeldi L, Cottin V, du Bois RM, Selman M, Kimura T, Bailes Z, et al. Nintedanib in patients with idiopathic pulmonary fibrosis: Combined evidence from the TOMORROW and INPULSIS((R)) trials. Respir Med. 2016;113:74–79. doi: 10.1016/j.rmed.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Lancaster L, Crestani B, Hernandez P, Inoue Y, Wachtlin D, Loaiza L, et al. Safety and survival data in patients with idiopathic pulmonary fibrosis treated with nintedanib: pooled data from six clinical trials. BMJ Open Respir Res. 2019;6(1):e000397. doi: 10.1136/bmjresp-2018-000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dempsey TM, Sangaralingham LR, Yao X, Sanghavi D, Shah ND, Limper AH. Clinical effectiveness of antifibrotic medications for idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2019;200(2):168–174. doi: 10.1164/rccm.201902-0456OC. [DOI] [PubMed] [Google Scholar]
- 18.Kelly B, Thao V, Dempsey TM, Sangaralingham LR, Payne S, Limper AH. Anti-fibrotic therapy for idiopathic pulmonary fibrosis is associated with decreased mortality among hospitalized patients [abstract] Am J Respir Crit Care Med. 2020;201:A7798. [Google Scholar]
- 19.Maher TM, Molina-Molina M, Russell A-M, Bonella F, Jouneau S, Ripamonti E, et al. Unmet needs in the treatment of idiopathic pulmonary fibrosis-insights from patient chart review in five European countries. BMC Pulm Med. 2017;17(1):124. doi: 10.1186/s12890-017-0468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Culver D, Yow E, Neely M, Belperio J, Bender S, De Andrade J, et al. Characteristcs of patients with idiopathic pulmonary fibrosis (IPF) in the US: date from the IP-pro registry. Chest. 2018;154(4):397A–A398. doi: 10.1016/j.chest.2018.08.366. [DOI] [Google Scholar]
- 21.Flaherty K, De Andrade J, Lancaster L, Limb S, Lindell K, Nathan S, et al. Baseline characteristics of 1461 participants in the Pulmonary Fibrosis Foundation Patient Registry. Eur Respir J. 2018;52(suppl 62):PA2199. [Google Scholar]
- 22.Dempsey TM, Payne S, Sangaralingham L, Yao X, Shah ND, Limper AH. Adoption of the anti-fibrotic medications pirfenidone and nintedanib for patients with idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2021. [DOI] [PubMed]
- 23.Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. 2018;378(19):1811–1823. doi: 10.1056/NEJMra1705751. [DOI] [PubMed] [Google Scholar]
- 24.Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat. Respir Res. 2019;20(1):205. doi: 10.1186/s12931-019-1161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pharmacologic Approaches to Glycemic Treatment Standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S111–S124. doi: 10.2337/dc21-S009. [DOI] [PubMed] [Google Scholar]
- 26.Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009;137(2):482–488. doi: 10.1053/j.gastro.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bodmer M, Meier C, Krähenbühl S, Jick SS, Meier CR. Long-Term Metformin Use Is Associated With Decreased Risk of Breast Cancer. Diabetes Care. 2010;33(6):1304–1308. doi: 10.2337/dc09-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landman GWD, Kleefstra N, van Hateren KJJ, Groenier KH, Gans ROB, Bilo HJG. Metformin associated with lower cancer mortality in type 2 diabetes: ZODIAC-16. Diabetes Care. 2010;33(2):322–326. doi: 10.2337/dc09-1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, et al. Metformin and cancer risk in diabetic patients: a systematic review and meta-analysis. Cancer Prev Res (Phila) 2010;3(11):1451–1461. doi: 10.1158/1940-6207.CAPR-10-0157. [DOI] [PubMed] [Google Scholar]
- 30.Kamarudin MNA, Sarker MMR, Zhou J-R, Parhar I. Metformin in colorectal cancer: molecular mechanism, preclinical and clinical aspects. J Exp Clin Cancer Res. 2019;38(1):491. doi: 10.1186/s13046-019-1495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anisimov VN, Berstein LM, Egormin PA, Piskunova TS, Popovich IG, Zabezhinski MA, et al. Metformin slows down aging and extends life span of female SHR mice. Cell Cycle. 2008;7(17):2769–2773. doi: 10.4161/cc.7.17.6625. [DOI] [PubMed] [Google Scholar]
- 32.Anisimov VN, Berstein LM, Popovich IG, Zabezhinski MA, Egormin PA, Piskunova TS, et al. If started early in life, metformin treatment increases life span and postpones tumors in female SHR mice. Aging (Albany NY) 2011;3(2):148–157. doi: 10.18632/aging.100273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cabreiro F, Au C, Leung KY, Vergara-Irigaray N, Cochemé HM, Noori T, et al. Metformin retards aging in C. elegans by altering microbial folate and methionine metabolism. Cell. 2013;153(1):228–39. doi: 10.1016/j.cell.2013.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barzilai N, Crandall JP, Kritchevsky SB, Espeland MA. Metformin as a tool to target aging. Cell Metab. 2016;23(6):1060–1065. doi: 10.1016/j.cmet.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Choi SM, Jang AH, Kim H, Lee KH, Kim YW. Metformin reduces bleomycin–induced pulmonary fibrosis in mice. J Korean Med Sci. 2016;31(9):1419–1425. doi: 10.3346/jkms.2016.31.9.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sato N, Takasaka N, Yoshida M, Tsubouchi K, Minagawa S, Araya J, et al. Metformin attenuates lung fibrosis development via NOX4 suppression. Respir Res. 2016;17(1):107. doi: 10.1186/s12931-016-0420-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gamad N, Malik S, Suchal K, Vasisht S, Tomar A, Arava S, et al. Metformin alleviates bleomycin-induced pulmonary fibrosis in rats: pharmacological effects and molecular mechanisms. Biomed Pharmacother. 2018;97:1544–1553. doi: 10.1016/j.biopha.2017.11.101. [DOI] [PubMed] [Google Scholar]
- 38.Rangarajan S, Bone NB, Zmijewska AA, Jiang S, Park DW, Bernard K, et al. Metformin reverses established lung fibrosis in a bleomycin model. Nat Med. 2018;24(8):1121–1127. doi: 10.1038/s41591-018-0087-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kheirollahi V, Wasnick RM, Biasin V, Vazquez-Armendariz AI, Chu X, Moiseenko A, et al. Metformin induces lipogenic differentiation in myofibroblasts to reverse lung fibrosis. Nat Commun. 2019;10(1):2987. doi: 10.1038/s41467-019-10839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xiao H, Huang X, Wang S, Liu Z, Dong R, Song D, et al. Metformin ameliorates bleomycin-induced pulmonary fibrosis in mice by suppressing IGF-1. Am J Transl Res. 2020;12(3):940–949. [PMC free article] [PubMed] [Google Scholar]
- 41.Park CS, Bang BR, Kwon HS, Moon KA, Kim TB, Lee KY, et al. Metformin reduces airway inflammation and remodeling via activation of AMP-activated protein kinase. Biochem Pharmacol. 2012;84(12):1660–1670. doi: 10.1016/j.bcp.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 42.Spagnolo P, Kreuter M, Maher TM, Wuyts W, Bonella F, Corte TJ, et al. Metformin does not affect clinically relevant outcomes in patients with idiopathic pulmonary fibrosis. Respiration. 2018;96(4):314–322. doi: 10.1159/000489668. [DOI] [PubMed] [Google Scholar]
- 43.Lambert EM, Wuyt WA, Yserbyt J, De Sadeleer LJ. Statins: cause of fibrosis or the opposite? Effect of cardiovascular drugs in idiopathic pulmonary fibrosis. Respir Med. 2021;176:106259. [DOI] [PubMed]
- 44.Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: building a novel node in the learning health care system. Health Aff (Millwood) 2014;33(7):1187–1194. doi: 10.1377/hlthaff.2014.0038. [DOI] [PubMed] [Google Scholar]
- 45.Services USDoHH. Health Insurance Portability and Accountability Act of 1996 (HIPAA).
- 46.Assurance NCfQ. National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) 2020 Diabetes Mellitus Measures. 2020.
- 47.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 48.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–161. doi: 10.1002/pst.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.American Diabetes Association. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(Supplement 1):S32–S36. [DOI] [PubMed]
- 51.Nachum Z, Zafran N, Salim R, Hissin N, Hasanein J, Gam Ze Letova Y, et al. Glyburide versus metformin and their combination for the treatment of gestational diabetes mellitus: a randomized controlled study. Diabetes Care. 2017;40(3):332–7. doi: 10.2337/dc16-2307. [DOI] [PubMed] [Google Scholar]
- 52.Costello MF, Shrestha B, Eden J, Johnson NP, Sjoblom P. Metformin versus oral contraceptive pill in polycystic ovary syndrome: a cochrane review. Hum Reprod. 2007;22(5):1200–1209. doi: 10.1093/humrep/dem005. [DOI] [PubMed] [Google Scholar]
- 53.Moghetti P, Castello R, Negri C, Tosi F, Perrone F, Caputo M, et al. Metformin effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: a randomized, double-blind, placebo-controlled 6-month trial, followed by open, long-term clinical evaluation. J Clin Endocrinol Metab. 2000;85(1):139–146. doi: 10.1210/jcem.85.1.6293. [DOI] [PubMed] [Google Scholar]
- 54.Inoki K, Kim J, Guan KL. AMPK and mTOR in cellular energy homeostasis and drug targets. Annu Rev Pharmacol Toxicol. 2012;52:381–400. doi: 10.1146/annurev-pharmtox-010611-134537. [DOI] [PubMed] [Google Scholar]
- 55.Hardie DG, Ross FA, Hawley SA. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol. 2012;13(4):251–262. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Towler MC, Hardie DG. AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res. 2007;100(3):328–341. doi: 10.1161/01.RES.0000256090.42690.05. [DOI] [PubMed] [Google Scholar]
- 57.Marsin AS, Bertrand L, Rider MH, Deprez J, Beauloye C, Vincent MF, et al. Phosphorylation and activation of heart PFK-2 by AMPK has a role in the stimulation of glycolysis during ischaemia. Curr Biol. 2000;10(20):1247–1255. doi: 10.1016/S0960-9822(00)00742-9. [DOI] [PubMed] [Google Scholar]
- 58.UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):P854–865. [PubMed]
- 59.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 60.Roumie CL, Hung AM, Greevy RA, Grijalva CG, Liu X, Murff HJ, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2012;157(9):601–610. doi: 10.7326/0003-4819-157-9-201211060-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roussel R, Travert F, Pasquet B, Wilson PW, Smith SC, Jr, Goto S, et al. Metformin use and mortality among patients with diabetes and atherothrombosis. Arch Intern Med. 2010;170(21):1892–1899. doi: 10.1001/archinternmed.2010.409. [DOI] [PubMed] [Google Scholar]
- 62.Ley B, Collard HR, King TE., Jr Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183(4):431–440. doi: 10.1164/rccm.201006-0894CI. [DOI] [PubMed] [Google Scholar]
- 63.King TE, Jr, Albera C, Bradford WZ, Costabel U, du Bois RM, Leff JA, et al. All-cause mortality rate in patients with idiopathic pulmonary fibrosis Implications for the design and execution of clinical trials. Am J Respir Crit Care Med. 2014;189(7):825–31. doi: 10.1164/rccm.201311-1951OC. [DOI] [PubMed] [Google Scholar]
- 64.Moua T, Ryu JH. Obstacles to early treatment of idiopathic pulmonary fibrosis: current perspectives. Ther Clin Risk Manag. 2019;15:73–81. doi: 10.2147/TCRM.S160248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vu A, Vasireddy A, Moua T, Baqir M, Ryu JH. Clarifying the diagnosis of post-inflammatory pulmonary fibrosis: a population-based study. Eur Respir J. 2019;54(1):1900103. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying the results of this study are third party data owned by OptumLabs and contain sensitive patient information; therefore, the data is only available upon request. Interested researchers engaged in HIPAA compliant research may contact connected@optum.com for data access requests. The data use requires researchers to pay for rights to use and access the data.