Abstract
Objective
The oral-cervical human papillomavirus (HPV) infection/cancer relationship is not well established. Oral-cervical HPV studies were reviewed to assess dual-site occurrence, HPV type concordance, and study quality/deficiencies.
Methods
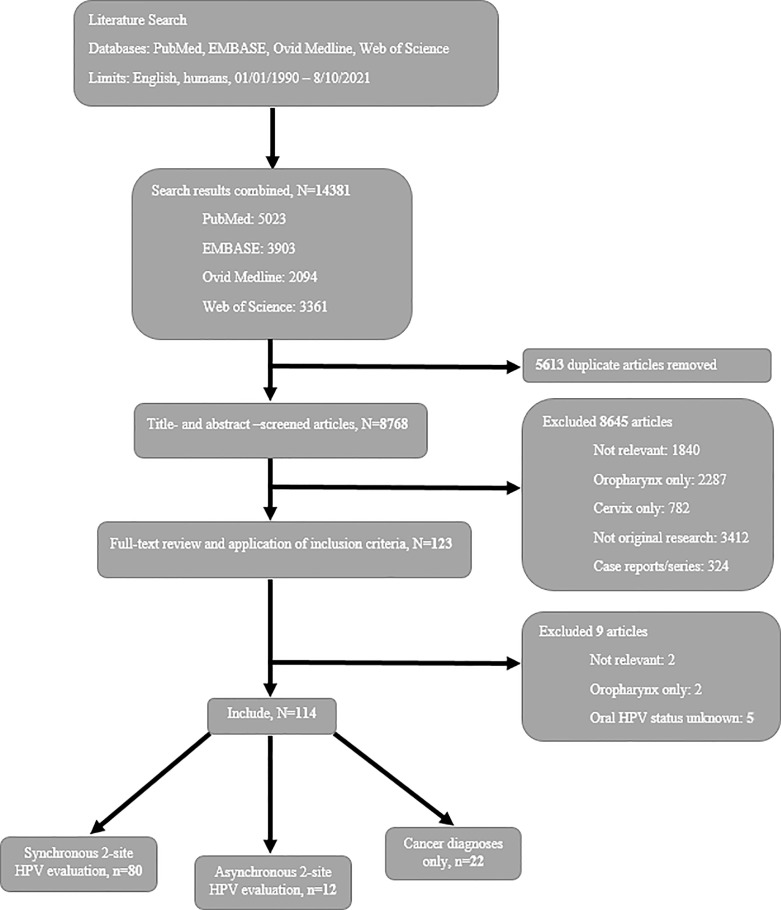
PubMed, EMBASE, Ovid Medline, and Web of Science were searched between 1/1/1990 and 8/10/2021 for studies investigating HPV infections/cancers and type concordance between the oral cavity/oropharynx and cervix. Dual-site and concordant HPV infection rates were summarized as percentages; cancer diagnoses studies were summarized using standardized incidence ratios (SIR). The Quality Assessment Tool for Quantitative Studies (QATQS) evaluated study methodology.
Results
One hundred fourteen papers were identified. Most were cross-sectional (n=79, 69%), involved synchronous dual-site HPV testing (n=80, 70%), did not report HPV type concordance (n=62, 54%), and achieved moderate methodological QATQS ratings (n=81, 71%). The overall dual-site infection rate averaged 16%; the HPV type concordance rate averaged 41%, among those dually-infected women. Most HPV-related cancer diagnoses studies reported increased secondary cancer risk, with SIRs generally ranging from 1.4 to 29.4 for secondary cervical cancer after primary oral cancer and from 1.4 to 6.3 for secondary oral cancer after primary cervical cancer.
Conclusion/Impact
Oral-cervical HPV infections/cancers remain understudied. Future research should use stronger methodologies and HPV concordance analyses to better understand oral-cervical HPV epidemiology.
Keywords: female, (human) papillomavirus (HPV) infection, oropharynx, cervix (uteri), cancer, epidemiology, systematic review
Introduction
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection (1). The virus exists in 200+ types—some more high risk (i.e., potentially malignant) than others (1). Various HPV types can infect the cervix, vagina, vulva, penis, anus, and/or oropharyngeal region, increasing the risk for the development of warts and/or cancers (1). Globally, about 630,000 incident cancers are HPV-related with most occurring in the oropharynx and cervix (1, 2). Oral HPV infections and cancer biology remain less understood than cervical HPV (3–7). Cervical HPV infection is clearly acquired through vaginal intercourse, whereas acquisition of oral HPV, potentially during orogenital sex, remains uncertain, especially in women (3, 4, 8, 9). Therefore, women are disproportionately burdened with the disease, amassing 90% of all HPV-related cancers (1).
HPV can be attributed to more than 70% of oropharyngeal cancers in the United States (US) (8, 10). In 2020, there were 98,412 new oropharyngeal cancer cases worldwide (11). High-risk HPV types (e.g., HPV16) account for a substantial proportion of oral HPV cases (3). HPV tends to infect the back of the oral cavity from the base of the tongue through the esophagus, including the oropharynx and tonsils (3, 9). However, there is no routine screening for oral HPV infection and methods are less-refined for oral HPV cancer detection, resulting in later stage diagnoses and more aggressive cancer treatments (3).
Approximately 604,127 women were diagnosed with cervical cancer worldwide in 2020 (11). Essentially all cervical cancers are HPV-related (10). HPV types 16 and 31/18/33 are the first and second most common type groupings routinely identified in advanced cervical infections and cancers, respectively (5). Slow disease progression and effective screening methods, including Papanicolaou (Pap) tests, allow for opportunities to detect and treat cervical abnormalities to reduce the risk for cancer development (12).
Results from studies of dual-site oral-cervical HPV infections/cancers are inconsistent. Investigating HPV status in both oral and cervical sites in women can aid in determining how HPV is transmitted (e.g., orogenital interaction, autoinoculation, unrelated events) (4). For example, oral-cervical HPV type concordance (i.e., same HPV type(s) in both sites) would suggest a transfer of infection across sites. Whereas HPV type discordance would suggest the infections were separate. Clarity in the oral-cervical HPV+ association could improve prevention, screening, and/or treatment approaches for both diseases, ultimately reducing HPV-related cancer rates overall.
Current systematic reviews on the topic of oral HPV infections and cervical cancers have only studied the infections independently of one another. This prohibits a complete assessment of HPV type concordance between the anatomical sites. The one meta-analysis that investigated oral and cervical HPV infections estimated an HPV concordance rate of 27% (4). However, the study was limited in publication years, databases, search terms, and oral HPV data collection methodologies, including just 10 studies, and without any quality assessment.
To date, there is no published comprehensive systematic review incorporating a quality assessment of the literature that examines the potential for both oral and cervical HPV infections in women. This systematic review aims to fill significant gaps in the HPV literature regarding oral and cervical dual-site and concordance rates of HPV. In summary, there is no consensus on whether oral and cervical HPV-related infections and/or cancers are more likely to be related or unrelated events. This systematic review aims to critically assess studies with participants who have at least one HPV-related oral and/or cervical infection/cancer diagnosis, comparing any HPV types across the two biological sites, to determine if there is a higher probability that any HPV types at the two sites had concordance.
Materials and Methods
Literature Search Strategy
A review of the literature was conducted in PubMed, EMBASE, Ovid Medline, and Web of Science databases using variations to the search terms oropharynx and cervix and human papillomavirus and infection or cancer. Searches were restricted to peer-reviewed papers published from January 1, 1990 to August 10, 2021. For example in PubMed, the following terms were used:
| Oropharynx: | [(head and neck) OR (oral) OR (oropharyngeal) OR (oropharynx) or (oropharyn*) OR (soft and palate) OR (esophagus) or (esophageal) or (esophag*) OR (hypopharynx) or (hypopharyngeal) or (hypopharyn*) OR (larynx) or (laryngeal) or (laryn*) OR (nasopharyngeal) OR (nasopharynx) or (nasopharyn*) Or (tonsil) or (tonsillar) or (tonsil*) OR (throat)] |
| Cervix: | [(Cervix) or (cervical) or (cerv*)] |
| Human papillomavirus: | [(hpv) or (human and papilloma and virus) or (papillomaviridae) or (human and papillomavirus)] |
| Infection or cancer: | [(cancer) or (cancerous) or (cancer*) OR (carcinoma) or (carcinom*) OR (neoplasia) OR (neoplasm) OR (neoplas*) OR (tumor) or (tumor*) or (tumorous) OR (dysplasia) OR (intra and epithelial and neoplasia) or (intra and epithelial and dysplasia) OR (mucosal and lesion) OR (infection) or (infect*) OR (malignancy) OR (malignant) or (malignan*) OR (precancerous and lesion) OR (pre and cancerous and lesion) OR (squamous and cell and carcinoma)] |
| Applied search filters: | Publication date from 1990/01/01 to 2021/08/10; Humans; English |
These search strategies were reproduced in each of the other three databases (Supplementary Table). Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines were used in this systematic review with respect to design and reporting.
Eligibility Criteria
Inclusion Criteria
Studies were eligible for inclusion if they: involved human subjects; investigated both person-specific anatomical sites of oral cavity/oropharynx and cervix for HPV synchronously (i.e., evaluated simultaneously) or asynchronously (i.e., evaluated at different times); and were full-text papers of original research written in English. Partner studies with both men and women were included if any HPV data pertaining to women could be independently differentiated from any HPV data presented on men. Studies including participants with a positive oral HPV test or any HPV-related oral cancer (i.e., non-tobacco/alcohol-related oral cancers) were included. Oral sites could range from the oral cavity to the esophagus (both potentially HPV-associated), including the oropharyngeal region with the base of the tongue and the tonsils (both HPV-related), as long as the original study authors had justified the sites to be at least possibly oral HPV-related (3, 9). All cervical abnormalities/cancers were assumed to be HPV-related since 95–99% of cervical cancer cases involve HPV (13).
Exclusion Criteria
Studies were excluded if they were not relevant to within-person HPV evaluation of both oral and cervical infections (e.g., both sites but in different people, wrong biological site or cancer or population), involved only HPV infections in the oral cavity/oropharynx or cervix, not original research (e.g., reviews, abstracts, letters, commentaries, meetings, protocols), or were case reports or series (i.e., N <10).
Data Collection, Categories, and Analyses
Data Extraction
Duplicate citations from the four databases were reviewed and removed. The remaining citations were divided equally, reviewed separately, and then summarized with data extraction by three study authors (KHJ, CBH, XZ). Any questions regarding inclusion were resolved by consensus among the three authors listed above.
Assessment of Risk of Bias and Quality of Studies
As described by Thomas et al., the Quality Assessment Tool for Quantitative Studies (QATQS) from the Effective Public Health Practice Project criteria was utilized to determine the quality of each included study (14). The assessment tool evaluates: 1) selection bias, 2) study design, 3) confounder adjustment, 4) blinding, 5) data collection methods, and 6) withdrawals and dropouts (14). All topics were evaluated for studies included in this systematic review, excluding blinding since all studies were observational in nature and no intervention or randomized control trial methods were considered for HPV evaluation in the oropharynx/oral cavity sites and/or cervix. Included papers were divided such that two authors (KHJ, CBH, or XZ) reviewed and scored the QATQS for each study independently. Each topic area evaluated received a rating of strong, moderate, or weak quality, dependent on topic-specific criteria. Studies attaining only moderate and/or strong quality topic ratings were classified as “strong”; studies with one weak quality topic rating were classified as “moderate” while studies with two or more weak quality topic ratings were classified as “weak” (14). The primary paper evaluator (KHJ, CBH, or XZ) compared the two-author ratings for inconsistencies. Discrepancies were discussed amongst authors and a consensus was reached.
Outcomes
Concurrent infections were defined as any HPV infection(s) occurring in both the oral cavity/oropharynx and cervix simultaneously due to synchronous site testing. If HPV infection was absent at either or both sites, then any infection was not considered concurrent. “Dual-site infections” were defined as any HPV infections occurring in both the oral cavity/oropharynx and cervix at different times due to asynchronous (i.e., non-simultaneous) testing of the two sites. Concordant infections were identified in women who shared at least one HPV type across oral and cervical sites at any time (synchronously or asynchronously) (Table 1).
Table 1.
Definitions and summary statistics for a 1990-2021 systematic review of oral-cervical human papillomavirus (HPV) infection/cancer rates in women.
| DEFINITIONS | CONCURRENT/DUAL-SITE INFECTIONS Any HPV type(s) in oropharynx/oral cavity and cervix, simultaneously (concurrent) or at varying times (dual-site) | CONCORDANT INFECTIONS At least one identical HPV type(s) in oropharynx/oral cavity and cervix, simultaneously or at varying times |
|---|---|---|
|
SYNCHRONOUS EVALUATIONS
HPV testing of oral and cervical anatomical sites at same time |
Average: 15% Range: 0-95% |
Average: 41% Range: 0-100% |
|
ASYNCHRONOUS EVALUATIONS
HPV testing of oral and cervical anatomical sites at varying times |
Average 26% Range: 2-100% |
Average: 39% Range 2-100% |
| OVERALL ESTIMATED AVERAGE | 16% | 41% |
Studies investigating oral-cervical cancer diagnoses from registry data were also considered. We included studies that examined the occurrence of cervical cancer after a primary diagnosis of HPV-related oral cancer and occurrence of HPV-related oral cancer after a primary diagnosis of cervical cancer. Infections were also included here, if documented accordingly in the registries/databases.
Categories
Eligible studies were divided into three categories based on the timing of HPV evaluation at both sites (i.e., synchronously, asynchronously, or cancer diagnoses). Synchronous HPV evaluation studies actively collected oral and cervical samples and tested them both for HPV DNA at the same visit (with one study testing oral samples within three weeks of cervical samples). Asynchronous HPV evaluation studies either HPV-tested the oral and cervical sites at separate visits or one anatomical site was previously diagnosed with a HPV-related cancer and the other anatomical site was actively tested for HPV infection during the study. Cancer diagnoses only studies relied on data from cancer registries or medical records to determine prior primary and secondary cancer diagnoses of the oral cavity/oropharyngeal region and cervix.
Statistical Analyses
When individual synchronous and asynchronous studies presented sufficient results, we summarized concurrent/dual-site infection data as percentages of women with any oral-cervical HPV infections at any time. HPV type concordance data was summarized as percentages of women with the same oral-cervical HPV type(s) at any time. Overall concurrent/dual-site and concordant oral-cervical HPV infection rates were determined by averaging respective individual study percentages (Table 1). For cancer diagnoses studies, we summarized the overall rates of secondary cervical and/or oral cancers (number of cases per 10,000 women) and reported the standardized incidence ratios (SIR) to indicate whether the age-adjusted observed cancer cases were higher than expected for individual study populations. Results were not pooled across studies but stated as ranges.
Results
A total of 8768 papers were identified through PubMed, EMBASE, Ovid Medline, and Web of Science databases after removing duplicates (Figure 1). Titles, abstracts, and full-text papers were screened, 8654 did not meet the eligibility criteria and subsequently were removed. Specifically, 1842 (21%) studies were not topic relevant, 3071 (35%) studies evaluated HPV only in the oropharynx/oral cavity [2289 (26%) studies] or cervix [782 (9%) studies], 5 (0.06%) studies did not relate oral cancers to HPV status, 3412 (39%) studies were not original research, and 324 (4%) studies were case reports or series. A total of 114 papers were included.
Figure 1.
Flow diagram of study selection for a systematic review of oral-cervical HPV infection/cancer epidemiology literature.
Most studies (n=80, 70%) (4, 15–93) evaluated oral and cervical sites with synchronous HPV testing; the remaining studies were divided between asynchronous evaluations (n=12, 11%) (94–105) and cancer diagnoses only (n=22, 19%) (106–127). Combining synchronous (4, 15–93) and asynchronous (94–105) study data, the overall estimate of oral and cervical dual-site HPV infections was 16% and the overall estimate of oral-cervical HPV type concordance among dually-infected women was 41% (Table 1). Among cancer diagnoses only studies (106–127), the incidence of a secondary cervical cancer diagnosis ranged from as few as 4.5/10,000 to as many as 192.5/10,000 women; the incidence of a secondary oral HPV-related cancer ranged from 1.0 to 45.8 per 10,000 women.
Synchronous Oral-Cervical HPV Testing (n=80)
Eighty studies synchronously evaluated HPV-related infections at both the oral and cervical sites (4, 15–93) (Table 2A). Cervical samples were collected by a variety of measures with most studies using swabs or a combination of methods; oral samples were collected mainly by rinses or swabs. HPV DNA detection was most often determined through polymerase chain reaction (PCR) (n=60, 75%) (4, 16–20, 24–29, 33–35, 38, 39, 42–49, 52–56, 61–65, 67–76, 78–89, 91–93).
Table 2A.
Description of methodology used in synchronous oral-cervical HPV evaluation papers (n=80).
| AUTHOR, YEAR (REFERENCE) | STUDY DESIGN STUDY NAME |
COUNTRY | PARTICIPANTS | SAMPLE COLLECTION METHOD | HUMAN PAPILLOMAVIRUS (HPV) DETECTION METHOD |
|---|---|---|---|---|---|
| Cervical/Oral | |||||
| SYNCHRONOUS | |||||
| Papers with sufficient concurrent* data | |||||
| Mosmann et al., 2021 (84) | Cross-sectional | Argentina | n=100 women (n=50 abnormal cervical cytology; n=50 normal cervical cytology) |
Cervical: Brush/swab Oral: Swab/scrape |
Polymerase Chain Reaction (PCR) |
| Paaso et al., 2021 (85) | Cross-sectional Finnish Family HPV Study |
Finland | n=21 women |
Cervical: Brush Oral: Brush |
PCR |
| Gilles et al., 2020 (86) | Cross-sectional | Belgium | n=44 human immunodeficiency virus (HIV)-positive women (n=22 women with perinatally infected HIV; n=22 with non-perinatal HIV) |
Cervical: Smear Oral: Rinse |
PCR |
| Nasioutziki et al., 2020 (87) | Cross-sectional | Greece | n=118 women with abnormal pap or high grade cervical intraepithelial neoplasia (CIN) |
Cervical: Spatula and brush Oral: Rinse |
PCR |
| Nemesio et al., 2020 (88) | Cross-sectional | Brazil | n=406 non-pregnant women with abnormal cervical cytology (n=323 with < CIN2; n=83 with ≥ CIN2) |
Cervical: Cytology and colposcopy biopsy Oral: Rinse |
PCR |
| Perez Quintanilla et al., 2020 (89) | Cross-sectional | Mexico | n=174 HIV+ women |
Cervical: Brush Oral: Brush |
PCR and reverse hybridization |
| Sricharoenchai et al., 2020 (90) | Cross-sectional | Thailand and Vietnam | n=192 HPV unvaccinated women (12-24 years old) (n=93 perinatally HIV+; n=99 HIV-) |
Cervical: Vaginal speculum exam Oral: Rinse |
Linear Array |
| Suehiro et al., 2020 (91) | Cross-sectional | Brazil | n=254 women (n=115 HIV+, n=139 HIV- women) |
Cervical: Brush and spatula Oral: Brush and rinse |
PCR and Multiplex Kit |
| Tewari, 2020 (93) | Cross-sectional | Ireland | n=235 women with abnormal cytology |
Cervical: Biopsy Oral: Rinse |
Cervical: Reverse hybridization Oral: PCR and reverse hybridization |
| Brouwer et al., 2019 (18) | Cross-sectional National Health and Nutrition Examination Survey (NHANES) 2003-2014 |
United States | n=10776 women with genital samples n=7102 women with oral samples |
Cervical: Swab Oral: Rinse |
PCR |
| Eggersmann et al., 2019 (17) | Cross-sectional | Germany | n=221 women |
Cervical: Smear Oral: Smear and Rinse |
PCR |
| Enerly 2019 (92) | Cross-sectional | Norway | n=312 girls (18-20 year olds) (n= 239 HPV vaccinated; n=73 HPV unvaccinated) |
Cervical: Brush Oral: Swab |
PCR and type specific hybridization |
| Kiwerska et al., 2019 (16) | Cross-sectional | Poland | n=197 women with previous history of cervical cancer or pre-cancerous lesions |
Cervical: Brush Oral: Swab |
PCR |
| Sehnal, 2019 (15) | Cross-sectional | Czech Republic | n=718 women (n=473 with high-grade cervical lesions; n=245 with low-grade/no cervical lesions) |
Cervical: Brush Oral: Rinse |
Linear Array |
| Cossellu et al., 2018 (25) | Cross-sectional | Italy | n=44 women with abnormal Pap smear (20-45 years old) |
Cervical: Swab Oral: Swab |
PCR |
| Grimm et al., 2018 (23) | Cross-sectional | Germany | n=73 women with cervical high grade squamous intraepithelial lesion (HSIL) |
Cervical: Swab Oral: Swab |
Linear Array and “PapilloCheck” |
| Thorsteinsson et al., 2018 (21) | Cross-sectional Study on HIV, cervical Abnormalities and infections in women in Denmark (SHADE) cohort |
Denmark | n=214 HIV+ women |
Cervical: Swab Oral: Swab |
PCR |
| Tuominen et al., 2018 (20) | Cross-sectional Finnish Family HPV Study |
Finland | n=39 women who recently gave birth |
Cervical: Scrape Oral: Scrape |
PCR |
| Vargas-Robles et al., 2018 (19) | Cross-sectional | Venezuela | n=111 women from the Amazonian area (12-53 years old) |
Cervical: Swab Oral: Swab |
PCR |
| Beachler et al., 2017 (73) | Cohort Costa Rica Vaccine Trial (CVT) |
Costa Rica | n=352 women (22-33 years old) |
Cervical: Not specified Oral: Rinse |
PCR |
| Oliveira et al., 2017 (27) | Cross-sectional | Brazil | n=76 women |
Cervical: Scrape Oral: Scrape/brush |
PCR |
| Woelber et al., 2017 (26) | Cross-sectional | Germany | n=235 women with abnormal cervical cytology (18-45 years old) |
Cervical: Swab Oral: Scrape |
PCR |
| Kedarisetty et al., 2016 (32) | Cross-sectional NHANES 2009-2012 |
United States | n=3463 women |
Cervical: Swab Oral: Rinse |
Cervical: Linear Array and “Digene HC2 HPV DNA” test Oral: PCR |
| Kero et al., 2016 (74) | Cohort Finnish Family HPV Study |
Finland | n=131 women |
Cervical: Brush/scrape Oral: Brush/scrape |
PCR |
| Loverro et al., 2016 (31) | Cross-sectional | Italy | n=35 transgendered individuals with cervix (14 female to male; 21 male to female) |
Cervical: Brush Oral: Brush |
Linear Array |
| Menezes et al., 2016 (75) | Cohort | India | n=65 women, HIV positive |
Cervical: Swab Oral: Swab |
PCR |
| Temizkan et al., 2016 (30) | Cross-sectional | Turkey | n=30 women with abnormal cervical cytology n=68 women with normal cervical cytology |
Cervical: Smear Oral: Brush |
None (cytology) |
| Uken et al., 2016 (29) | Cross-sectional | Germany | n=101 women with cervical dysplasia |
Cervical: Brush Oral: Brush |
PCR |
| Brouwer et al., 2015 (36) | Cross-sectional NHANES 2003-2012 |
United States | n=10407 women with genital samples n=5236 women with oral samples |
Cervical: Swab Oral: Rinse |
Cervical: Linear Array and multiplex assay Oral: PCR |
| Grun et al., 2015 (35) | Cross-sectional | Sweden | n=211 women (15-23 years old) |
Cervical: Swab Oral: Swab |
PCR |
| Skoczynski et al., 2015 (34) | Cross-sectional | Poland | n=152 pregnant women |
Cervical: Smear Oral: Smear |
PCR |
| Tatar et al., 2015 (33) | Cross-sectional | Hungary | n=149 women |
Cervical: Not specified Oral: Rinse/brush |
PCR |
| Ribeiro et al., 2014 (38) | Cross-sectional Recife Brazil Study |
Brazil | n=31 women |
Cervical: Swab/brush Oral: Swab/brush |
PCR |
| Lima et al., 2014 (41) | Cross-sectional | Brazil | n=200 women (n=100 HIV positive, n=100 HIV negative) |
Cervical: Brush Oral: Scraping/brush |
“Digene HC2 HPV DNA” test |
| Louvanto et al., 2014 (76) | Case-control Finnish Family HPV Study |
Finland | n=43 pregnant women with persistent cervical HPV infection (>24 months) n=52 pregnant women without cervical HPV infection |
Cervical: Scrape/brush Oral: Scrape/brush |
PCR |
| Mbulawa et al., 2014 (40) | Cross-sectional | South Africa | n=221 women (18-65 years old) |
Cervical: Not specified Oral: Brush |
Linear Array |
| Meyer et al., 2014 (39) | Cross-sectional | Germany | n=129 women |
Cervical: Smear/brush Oral: Smear and rinse |
PCR |
| Steinau et al., 2014 (37) | Cross-sectional NHANES |
United States | n=1812 women (18-59 years old) |
Cervical: Swab Oral: Rinse |
Linear Array |
| Adamopoulou et al., 2013 (47) | Cross-sectional | Greece | n=43 women |
Cervical: Scrape Oral: Rinse |
PCR |
| Lang Kuhs et al., 2013 (44) | Cross-sectional CVT |
Costa Rica | n=5838 women (22-29 years old) |
Cervical: Exfoliated Oral: Rinse |
PCR |
| Schlecht et al., 2013 (43) | Cross-sectional | United States | n=97 women (15-22 years old) |
Cervical: Brush Oral: Rinse |
PCR |
| Vogt et al., 2013 (42) | Cross-sectional | South Africa | n=34 women |
Cervical: Swab Oral: Rinse |
PCR |
| Du et al., 2012 (50) | Cross-sectional | Sweden | n=408 female youth (15-23 years old) |
Cervical: Swab Oral: Rinse |
Cervical: Multiplex array Oral: “Gentra Puregene Buccal Cell Kit” |
| Elasbali et al., 2012 (49) | Cross-sectional | Sudan | n=50 women (n=40/50 with cervical lesions; n=10/50 with no cervical lesions) |
Cervical: Scrape Oral: Scrape |
PCR |
| Zonta et al., 2012 (72) | Cross-sectional | Brazil | n=409 women inmates |
Cervical: Brush Oral: Brush |
PCR |
| Brown et al., 2011 (55) | Cross-sectional | Peru | n=184 female sex workers |
Cervical: Not specified Oral: Rinse |
PCR |
| Crawford et al., 2011 (54) | Cross-sectional | United Kingdom | n=100 women with abnormal cervical smear |
Cervical: Swab/brush Oral: Swab |
PCR |
| Matsushita et al., 2011 (52) | Cross-sectional | Japan | n=196 female sex workers (18-45 years old) |
Cervical: Scrape/smear Oral: Scrape |
PCR |
| Paaso et al., 2011 (77) | Cohort Finnish Family HPV Study |
Finland | n=323 women |
Cervical: Scrape Oral: Scrape |
Multiplex Kit |
| Ragin et al., 2011 (51) | Cross-sectional Epidemiologic Study of HEalth Risk (ESTHER) project |
United States | n=118 women |
Cervical: Brush Oral: Brush and/or rinse |
Linear Array |
| Termine et al., 2011 (4) | Cross-sectional | Italy | n=100 women with cervical HPV infection |
Cervical: Not specified Oral: Exam, rinse |
PCR |
| Termine et al., 2009 (56) | Cross-sectional | Italy | n=140 women with known cervical HPV status |
Cervical: Spatula and brush Oral: Brush |
PCR |
| Marais et al., 2008 (58) | Cross-sectional | South Africa | n=115 women with CIN1-CIN3 |
Cervical: Swab Oral: Swab |
Linear Array |
| Richter et al., 2008 (57) | Cross-sectional | South Africa | n=30 women, HIV-positive (22-64 years old) |
Cervical: Smear Oral: Brush |
Linear Array |
| Nordin et al., 2007 (61) | Cross-sectional | (Not specified - Swedish author group) | n=30 women (n=21/30 renal transplant carriers; n=9/30 healthy controls) |
Cervical: Brush Oral: Swab |
PCR |
| Passmore et al., 2007 (60) | Cross-sectional | South Africa | n=103 women (18-40 years old) |
Cervical: Swab Oral: Swab |
Linear Array |
| Ragin et al., 2007 (59) | Cross-sectional | Tobago | n=212 women (18-65 years old) |
Cervical: Brush Oral: Rinse |
Linear Array; nested PCR |
| Fakhry et al., 2006 (70) | Cross-sectional Women’s Interagency HIV Study |
United States | n=258 women (n=172 HIV positive, n=86 HIV negative) |
Cervical: Rinse Oral: Rinse |
PCR |
| Goncalves et al. 2006 (71) | Cross-sectional | Brazil | n=140 women (n=70/140 with clinical genital HPV lesions) |
Cervical: Smear Oral: Swab |
PCR |
| Canadas et al., 2004 (63) | Cross-sectional | Spain | n=188 women who practiced prostitution |
Cervical: Not specified (exfoliates) Oral: Not specified |
PCR |
| Smith et al., 2004 (62) | Cross-sectional | United States | n=577 pregnant women |
Cervical: Swab Oral: Rinse |
PCR |
| Scala et al., 2002 (64) | Cross-sectional | Italy | n=76 women treated for genital, anorectal, and perineal HPV lesions |
Cervical: Scrape Oral: Not specified |
PCR |
| Aaltonen et al., 2001 (67) | Cross-sectional | Finland | n=9 women with adult onset laryngeal papilloma patients |
Cervical: Scraping Oral: Rinse |
PCR |
| Marais et al., 2001 (65) | Cross-sectional | South Africa | n=81 women with CIN or squamous carcinoma of the cervix |
Cervical: Swab/brush and biopsy Oral: Swab |
PCR and enzyme-linked immunosorbent assay |
| Badaracco et al., 1998 (68) | Cross-sectional | Italy | n=29 women (21-48 years old) |
Cervical: Spatula Oral: Swab |
PCR |
| van Doornum et al., 1994 (78) | Cohort | Netherlands | n=162 women |
Cervical: Spatula Oral: Spatula |
PCR |
| van Doornum et al., 1992 (69) | Cross-sectional | Netherlands | n=111 women |
Cervical: Spatula Oral: Spatula |
PCR |
| Papers with insufficient concurrent* data | |||||
| Cranston et al., 2018 (24) | Cross-sectional within a randomized control trial AIDS Clinical Trials Group (ACTG) |
United States and Brazil | n=103 HIV-infected women |
Cervical: Swab Oral: Rinse |
PCR |
| Sohn et al., 2018 (22) | Cross-sectional | Thailand, Vietnam | n=93 adolescents HIV positive n=99 adolescents HIV negative (12-24 years) |
Cervical: Pap smear Oral: Rinse |
Linear Array |
| Ciccarese et al., 2017 (28) | Cross-sectional | Italy | n=46 women |
Cervical: Brush Oral: Brush |
PCR |
| Kero et al., 2014 (79) | Cohort Finnish Family HPV Study |
Finland | n=46 women |
Cervical: Scrape/brush Oral: Brush |
PCR |
| da Mota Vasconcelos Brasil et al., 2013 (46) | Cross-sectional | Brazil | n=31 women |
Cervical: Brush Oral: Brush |
PCR |
| Herrero et al., 2013 (45) | Cross-sectional CVT |
Costa Rica | n=5840 women (18-25 years old) |
Cervical: Collection of exfoliated cells Oral: Rinse |
PCR |
| Schlecht et al., 2012 (48) | Cross-sectional | United States | n=645 young women (12-19 years old) |
Cervical: Brush Oral: Rinse |
PCR |
| Kero et al., 2011 (53) | Cross-sectional Finnish Family HPV Study |
Finland | n=128 pregnant women (third trimester) |
Cervical: Brush Oral: Brush |
PCR |
| Sarkola et al., 2009 (80) | Cohort Finnish Family HPV Study |
Finland | n=178 women (n=78 pregnant women, n=100 non-pregnant women) |
Cervical: Scrape Oral: Scrape |
PCR |
| D’Souza et al., 2007 (81) | Cohort Women’s Interagency HIV Study |
United States | n=199 women (n=136 HIV positive, n=63 HIV negative) |
Cervical: Rinse Oral: Rinse |
PCR |
| Rintala et al., 2005 (82) | Cohort Finnish Family HPV Study |
Finland | n=76 women |
Cervical: Scrape/brush Oral: Scrape/brush |
PCR |
| Winer et al., 2003 (83) | Cohort | United States | n=603 women, university students |
Cervical: Swab Oral: Brush |
PCR |
| Chatterjee et al., 2001 (66) | Cross-sectional | India | n=27 cervical samples from female prostitutes, n=69 oral samples from female prostitutes |
Cervical: Smear Oral: Swab |
Deoxyribonucleic acid hybridization (Vira type; Digene Diagnostics) |
*Concurrent refers to the synchronous occurrence of any HPV type(s) in both the cervix and oral cavity/oropharynx.
Overall rates of cervical HPV+ and oral HPV+ cases varied by study (Table 3A). Almost all studies found higher rates of cervical HPV+ than oral HPV+ (n=76/80, 95%) (4, 15–19, 21–67, 69–79, 81–84, 86–93). On average, 53% of women were HPV+ in the cervix; an average of 15% of women were HPV+ in the oral cavity/oropharyngeal region. Most papers included high-risk HPV type results from DNA genotyping (n=74/80, 93%) (4, 15–29, 31–33, 35–37, 39–45, 47–66, 68–70, 72–93) with 82% (n=61/74) (4, 15–26, 29, 31, 33, 35–37, 40, 42, 44, 45, 47–52, 54–62, 65, 66, 69, 70, 72, 74–79, 81, 83–93) reporting exact HPV types observed.
Table 3A.
Results of the synchronous oral-cervical HPV evaluation papers (n=80).
| AUTHOR, YEAR (REFERENCE) | RESULTS, n=# of women unless otherwise noted | OVERALL QUALITY§ | |||
|---|---|---|---|---|---|
| Any Cervical Human Papillomavirus (HPV)+ or Oral HPV+ Infections | Concurrent† Oral-cervical HPV Infections | Concordant‡ Oral-cervical HPV Infections | High Risk (HR)-HPV Infections | ||
| SYNCHRONOUS | |||||
| Papers with sufficient concurrent data | |||||
| Mosmann et al., 2021 (84) |
Cervical: n=18/100 (18%) (n=12 normal cervical cytology; n=6 abnormal cervical cytology) Oral: n=14/100 (14%) (n=9 normal cervical cytology; n=5 abnormal cervical cytology) |
n=5/100 (5%) (n=3 normal cervical cytology; n=2 abnormal cervical cytology) | n=3/5* (60%) |
Cervical: n=11/18* Oral: n=10/14* |
Moderate |
| Paaso et al., 2021 (85) |
Cervical: n=5/21 (24%) Oral: n=8/21 (38%) |
n=2/21 (10%) | n=0/2 (0%) |
Cervical: n=0/5* Oral: n=3/8* |
Moderate |
| Gilles et al., 2020 (86) |
Cervical: n=11/36 (31%), (n=6 perinatal human immunodeficiency virus (HIV); n=5 non-perinatal HIV) Oral: n=1/36 (3%), (n=1 perinatal HIV) |
n=1/36 (3%), (n=1 perinatal HIV) | n=1/1 (100%) |
Cervical: n=11/11* Oral: n=1/1* |
Moderate |
| Nasioutziki et al., 2020 (87) |
Cervical: 88/118 (75%) Oral: n=3/118 (3%) |
Aggregate data only* | Aggregate data only* | Cervical= 74/118* Oral= 3/3* |
Moderate |
| Nemesio et al., 2020 (88) |
Cervical: n=251/401 (63%) Oral: n=16/406 (4%) |
n=10/16 (63%) | n=9/10 (90%) |
Cervical: n=251/251* Oral: n=16/16* (only HR HPV types tested) |
Moderate |
| Perez Quintanilla et al., 2020 (89) |
Cervical: n=168/174 (97%) Oral: n=161/174 (93%) |
n=155/174 (89%) | n ≤ 39/155 (25%) Bar graph description* |
Cervical: n=158/168* Oral: n=145/161* |
Moderate |
| Sricharoenchai, 2020 (90) |
Cervical: n=57/192 (30%) (n=34/93 perinatally HIV+; n=23/99 HIV-) Oral: n=8/192 (4%) (n=5/93 perinatally HIV+; n=3/99 HIV-) |
Bar graph description (combined sites) | Bar graph description (combined sites)* |
Cervical: n=57/192* Oral: n=8/192* (only HR HPV types tested) |
Moderate |
| Suehiro et al., 2020 (91) |
Cervical: n=103/254 (41%) (n=51/115 HIV+; n=53/139 HIV-) Oral: n=30/254 (12%), (n=17/115 HIV+; n=13/139 HIV-) |
n=15/30 (50%) (n=8/17 HIV+; n=7/13 HIV-) | n=0/15 (0%) |
Cervical: n=56/103* Oral: n=12/30* |
Moderate |
| Tewari, 2020 (93) |
Cervical: n=223/223 (100%) Oral: n=22/223 (10%) |
n=21/22 (95%) | n=6/21* (29%) | Bar graph description* | Moderate |
| Brouwer et al., 2019 (18) |
Cervical: n=2542/10776 (24%) Oral: n=282/7102 (4%) |
Aggregate data only* | n=66 | Bar graph description* | Moderate |
| Eggersmann et al., 2019 (17) |
Cervical: n=144/221 (65%) Oral: n=1/221 (0.5%) |
n=1/221 (0.5%) | . |
Cervical: n=68/114* Oral: n=0/1 |
Moderate |
| Enerly et al. 2019 (92) |
Cervical: n=122/312 (39%) (n=92/239 HPV vaccinated; n=30/73 HPV unvaccinated) Oral: n=4/312 (1.3%) (n=3/239 HPV vaccinated; n=1/73 HPV unvaccinated) |
n=4/312 (1.3%) | n=2/4* (50%) |
Cervical: n=60/312* (n=46/239 HPV vaccinated; n=14/73 HPV unvaccinated) Oral: n=1/312* |
Weak |
| Kiwerska et al., 2019 (16) |
Cervical: n=197/197 (100%) Oral: n=39/197 (20%) |
n=39/197 (20%) | n=17/39 (44%) |
Cervical: n=212/280 infections* Oral: n=30/52 infections* |
Moderate |
| Sehnal et al., 2019 (15) |
Cervical: n=448/714 (63%) Oral: n=10/438 (2%) |
n=6/437 (1.4%) | n=5/6* (83%) |
Cervical: n=416/448* Oral: n=10/10* |
Moderate |
| Cossellu et al., 2018 (25) |
Cervical: n=36/43 (84%) Oral: n=9/44 (20%) |
n=7/44 (16%) | n=1/7* (14%) | Bar graph description* | Moderate |
| Grimm et al., 2018 (23) |
Cervical: n=69/73 (95%) Oral: n=3/73 (4%) |
n=3/73 (4%) | n=3/3* (100%) |
Cervical: n=69/73* Oral: n=3/3* |
Moderate |
| Thorsteinsson et al., 2018 (21) |
Cervical: n=108/214 (50%) Oral: n=12/214 (6%) |
n=0 (0%) | N/A |
Cervical: n=60/108* Oral: n=8/12* |
Moderate |
| Tuominen, 2018 (20) |
Cervical: n=9/39 (23%) Oral: n=13/39 (33%) |
n=4/39 (10%) | n=2/4* (50%) |
Cervical: n=7/9* Oral: n=11/13* |
Moderate |
| Vargas-Robles et al., 2018 (19) |
Cervical: n=66/91 (73%) Oral: n=6/18 (33%) |
Aggregate data only* | Aggregate data only* |
Cervical: n=60/66* Oral: n=3/6* |
Moderate |
| Beachler et al., 2017 (73) |
Cervical: Year 4: n=223/350 (64%) infections (n=144/350 women, 41%); Year 6: n=40/223 (18%) infections Oral: Year 4: n=82/350 (23%) infections (n=66/350 women, 19%); Year 6: n=14/82 (17%) infections |
Year 4: n=47/82 (57%) infections Year 6: n=3/47 (6%) infections |
Year 4: n=31/47 (66%) infections Year 6: n=0/31 (0%) infections |
Cervical: Year 4: n=131/223 infections; Year 6: n=26/131 infections Oral: Year 4: n=47/82 infections; Year 6: n=7/47 infections |
Strong |
| Oliveira et al., 2017 (27) |
Cervical: n=7/76 (9%) Oral: n=4/76 (5%) |
n=1/76 (1%) | n=0/1 (0%) |
Cervical: n=3/7 Oral: n=0/4 |
Weak |
| Woelber et al., 2017 (26) |
Cervical: n=207/223 (93%) Oral: n=6/135 (4%) |
n=6/135 (4%) | n=3/6* (50%) |
Cervical: n=135/235* Oral: n=6/6* |
Moderate |
| Kedarisetty et al., 2016 (32) |
Cervical: n=1586/3463 (46%) Oral: n=141/3463 (4%) |
n=107/3463 (3%) | n=41/107 (38%) |
Cervical: n=337/1586 Oral: n=22/141 |
Moderate |
| Kero et al., 2016 (74) |
Cervical: Baseline: n=25/131 (19.1%) 2 month (mo): n=14/105 (13%) 12 mo: n=51/114 (45%) 24 mo: n=60/101 (59%) 36 mo: n=56/101 (55%) 72 mo: n=10/45 (22%) Follow up: 13.3-59.4% Oral: Baseline: n=25/131 (19.1%) 2 mo: n=23/105 (22%) 12 mo: n=24/115 (21%) 24 mo: n=27/100 (27%) 36 mo: n=15/101 (15%) 72 mo: n=6/58 (10%) Follow up: 10.3-27.0% |
Among 15 concordant couples: Baseline: n=2/15 (13%) 2 mo: n=0/15 (0%) 12 mo: n=2/15 (13%) 24 mo: n=5/15 (33%) 36 mo: n=1/15 (7%) 72 mo: n=1/15 (7%) |
Among 15 concordant couples: Baseline: n=1/15* (7%) 2 mo: n=0/15 (0%) 12 mo: n=2/15* (13%) 24 mo: n=3/15* (20%) 36 mo: n=0/15 (0%) 72 mo: n=1/15* (7%) |
Among 15 concordant couples: Cervical: Baseline: n=2/3* 2 mo: n=0/0 12 mo: n=6/8* 24 mo: n=9/10* 36 mo: n=7/7* 72 mo: n=3/3* Oral: Baseline: n=3/6* 2 mo: n=6/6* 6 mo: n=5/5* 12 mo: n=3/3* 24 mo: n=7/7* 36 mo: n=1/1* 72 mo: n=3/3* |
Moderate |
| Loverro et al., 2016 (31) |
Cervical: n=2/22 (9%) Oral: n=0/35 (0%) |
n=0 (0%) | N/A |
Cervical: n=1/2* Oral: N/A |
Moderate |
| Menezes et al., 2016 (75) |
Cervical: Baseline: n=26/50 (52%); Follow up: n=17/41 (41%) Oral: Follow up: n=5/38 (13%) |
n=4 infections/38 women | . |
Cervical: Baseline: n=24/50*; Follow up: n=16/41* Oral: Follow up: n=5/38* |
Moderate |
| Temizkan et al., 2016 (30) |
Cervical: n=30/98 (31%) Oral: n=3/98 (3%) |
n=3/98 (3%) | . | . | Weak |
| Uken et al., 2016 (29) |
Cervical: n=101/101 (100%) Oral: n=3/101 (3%) |
n=3/101 (3%) | n=2/3* (67%) |
Cervical: n=58/101* Oral: n=1/3* |
Moderate |
| Brouwer et al., 2015 (36) |
Cervical: n=1791/10407 (17%) Oral: n=196/5236 (4%) |
n=116/3940 (3%) | n=45/116 (39%) | Bar graph description* | Moderate |
| Grun et al., 2015 (35) |
Cervical: n=134/211 (64%) Oral: n=4/200 (2%) |
n=4/200 (2%) | . |
Cervical: Vaccinated: n=48/94; Not vaccinated: n=26/40* Oral: n=4/4* |
Moderate |
| Skoczynski et al., 2015 (34) |
Cervical: n=24/152 (16%) Oral: n=19/152 (13%) |
n=14/152 (9%) | . | . | Moderate |
| Tatar, 2015 (33) |
Cervical: n=33/40 (83%) Oral: n=8/40 (20%) |
n=7/40 (18%) | n=5/7* (71%) |
Cervical: n=25/33* Oral: n=4/8* |
Moderate |
| Ribeiro et al., 2014 (38) |
Cervical: n=18/31 (58%) Oral: n=17/31 (55%) |
n=12/31 (38%) | n=7/12 (58%) | . | Moderate |
| Lima et al., 2014 (41) |
Cervical: n=86/200 (43%) Oral: n=13/200 (7%) |
n=6/200 (3%) | . |
Cervical: n=77/86 Oral: n=9/86 |
Moderate |
| Louvanto et al., 2014 (76) |
Cervical: Persistent cases: n=43/43 (100%); Controls: n=0/52 (0%) Oral: Persistent cases: n=13/43 (30%); Controls: n=11/51 (22%) |
n=13/94 (14%) cases and controls | . |
Cervical: n=43/43* Oral: Cases: n=13/13* |
Strong |
| Mbulawa et al., 2014 (40) |
Cervical: n=121/219 (55%) Oral: n=15/221 (7%) |
Aggregate data provided | Aggregate data provided |
Cervical: aggregate genital data provided* Oral: not separated by sex* |
Moderate |
| Meyer et al., 2014 (39) |
Cervical: n=70/129 (54%) Oral: n=7/129 (5%) |
n=4/129 (3%) | n=1/4* (25%) |
Cervical: n=94 infections/70 women Oral: n=3/7 |
Moderate |
| Steinau et al., 2014 (37) | n=1812 total Cervical: 42.7% population prevalence Oral: 3.8% population prevalence |
3% population prevalence | 6.4% same strain* | Bar graph description* | Moderate |
| Adamopoulou et al., 2013 (47) |
Cervical: n=26/43 (60%) Oral: n=19/43 (44%) |
n=18/43 (42%) | n= 15/18* (83%) |
Cervical: n=17/26* Oral: n=14/19* |
Moderate |
| Lang Kuhs et al., 2013 (44) |
Cervical: n=1953/5838 (33%) Oral: n=101/5838 (2%) |
n=35/5838 (0.6%) | . |
Cervical: . Oral: n=57/101* |
Moderate |
| Schlecht et al., 2013 (43) |
Cervical: n=57/97 (59%) Oral: n=11/97 (11%) |
n=8/97 (8%) | n=0/8 (0%) |
Cervical: n=38/57 Oral: n=4/11 |
Moderate |
| Vogt et al., 2013 (42) |
Cervical: n=31/34 (91%) Oral: n=4/34 (12%) |
n=4/34 (12%) | n=2/4* (50%) |
Cervical: n=25/31* Oral: n=1/4* |
Moderate |
| Du et al., 2012 (50) |
Cervical: n=129/174 (74%) Oral: n=37/401 (9%) |
n=22/174 (13%) | n=20/22* (91%) |
Cervical: n=113/129* Oral: n=20/24* |
Weak |
| Elasbali et al., 2012 (49) |
Cervical: n=40/50 (80%) Oral: n=1/50 (2%) |
n=1/50 (2%) | . |
Cervical: n=16/40* Oral: n=1/1* |
Moderate |
| Zonta et al., 2012 (72) |
Cervical: n=27/409 (7%) Oral: n=23/27 (85%) |
n=18/27 (67%) | n=1/18* (6%) |
Cervical: n=10/27* Oral: n=22/23* |
Moderate |
| Brown et al., 2011 (55) |
Cervical: n=121/184 (66%) Oral: n=14/184 (8%) |
n=10/184 (5%) | . |
Cervical: n=27/121* Oral: n=4/14* |
Moderate |
| Crawford et al., 2011 (54) |
Cervical: n=96/100 (96%) Oral: n=92/100 (92%) |
n=88/100 (88%) | . |
Cervical: n=198/245* infections Oral: n=197/226* infections |
Moderate |
| Matsushita et al., 2011 (52) |
Cervical: n=103/196 (53%) Oral: n=12/196 (6%) |
n=6/196 (3%) | n=2/6* (33%) |
Cervical: n=84/103* Oral: n=10/12* |
Moderate |
| Paaso et al., 2011 (77) |
Cervical: Baseline: n=54 infections/323 women 12-mo: n=106 infections/281 women 24-mo: n=146 infections/261 women 36-mo: n=138 infections/260 women Oral: n=0/316 (0%) |
n=0 (0%) | N/A |
Cervical: Baseline: n=42/54 infections* 12-mo: n=86/106 infections* 24-mo: n=132/146 infections* 36-mo: n=133/138 infections* Oral: N/A |
Strong |
| Ragin et al., 2011 (51) |
Cervical: n=37/110 (34%) Oral: n=12/118 (10%) |
n=5/110 (5%) | n=1/5* (20%) |
Cervical: n=20/37* Oral: n=5/12* |
Weak |
| Termine et al., 2011 (4) |
Cervical: n=98/98 (100%) Oral: n=14/98 (14%) |
n=14/98 (14%) | n=3/14 (21%) | Among concurrent cases: Cervical: n=10/14* Oral: n=3/14* |
Moderate |
| Termine et al., 2009 (56) |
Cervical: n=76/140 (54%) Oral: n=2/140 (1%) |
n=2/140 (1%) | n=0/2* (0%) |
Cervical: n=38 infections/76 women* Oral: n=2/2* |
Moderate |
| Marais et al., 2008 (58) |
Cervical: n=98/109 (90%) Oral: n=28/105 (27%) |
n=25/99 (25%) | n=5/25 (20%) (detected by sequencing, not linear array) |
Cervical: n=190/216* infections Oral: n=10/33* infections |
Moderate |
| Richter et al., 2008 (57) |
Cervical: n=29/30 (97%) Oral: n=6/30 (20%) |
n=6/30 (20%) | n=3/6* (50%) |
Cervical: n=13/16* Oral: n=2/6* |
Moderate |
| Nordin et al., 2007 (61) |
Cervical: n=2/30 (7%) Oral: n=0/30 (0%) |
n=0 (0%) | N/A |
Cervical: n=1/2* Oral: N/A |
Weak |
| Passmore et al., 2007 (60) |
Cervical: n=92/103 (89%) Oral: n=22/91 (24%) |
n=4/91 (4%) | n=4/4* (100%) |
Cervical: n=68 infections/92 women* Oral: n=4 infections/22 women* |
Moderate |
| Ragin et al., 2007 (59) |
Cervical: n=75/212 (35%) Oral: n=14/212 (7%) |
n=7/212 (3%) | n=1/7* (14%) |
Cervical: n=43/75* Oral: n=3/14* |
Weak |
| Fakhry et al., 2006 (70) |
Cervical: n=479 infections/234 women Oral: n=69 infections/241 women |
n=37/221 (17%) | n=14/37* (38%) |
Cervical: n=224/479* infections Oral: n=30/69* infections |
Moderate |
| Goncalves et al., 2006 (71) |
Cervical: n=70/140 (50%) Oral: n=29/140 (21%) |
n=26/140 (19%) | . | . | Moderate |
| Canadas et al., 2004 (63) |
Cervical: n=52/187 (28%) Oral: n=15/188 (8%) |
n=7/188 (4%) | n=3/7* (43%) |
Cervical: n=41/65 infections Oral: n=4/15 infections |
Moderate |
| Smith et al., 2004 (62) |
Cervical: n=165/577 (29%) Oral: n=14/577 (2%) |
n=6/577 (1%) | n=0/6 (0%) |
Cervical: n=104/577* Oral: n=9/577* |
Moderate |
| Scala et al., 2002 (64) |
Cervical: n=22/76 (29%) Oral: n=2/76 (3%) |
n=2/76 (3%) | . | n=8/10 (not separated by site) | Moderate |
| Aaltonen et al., 2001 (67) |
Cervical: n=5/9 (55%) Oral: n=0/9 (0%) |
n=0 (0%) | N/A | . | Moderate |
| Marais et al., 2001 (65) |
Cervical: n=81/81 (100%) Oral: n=2/28 (7%) |
n=2/28 (7%) | n=0/2 (0%) |
Cervical: n=35/81* Oral: n=2/28* |
Moderate |
| Badaracco et al., 1998 (68) |
Cervical: n=8/24 (33%) Oral: n=11/29 (38%) |
n=4/24 (17%) | n=3/4* (75%) |
Cervical: n=6/8 Oral: n=7/11 |
Moderate |
| van Doornum et al., 1994 (78) |
Cervical: Baseline: n=25/162 (15%); Follow up: n=59/99 infections (60%) in 110 women Oral: Baseline: n=0/162 (0%); Follow up: n=1/110 (1%) |
n=0 (0%) | N/A |
Cervical: Baseline: n=22/25* Oral: Follow up: n=1/1* |
Moderate |
| van Doornum et al., 1992 (69) |
Cervical: n=15/111 (14%) Oral: n=0/111 (0%) |
n=0 (0%) | N/A |
Cervical: n=12/15* Oral: N/A |
Moderate |
| Papers with insufficient concurrent data | |||||
| Cranston et al., 2018 (24) |
Cervical: n=65/103 (63%) Oral: n=115/575 (includes males and females) (20%) |
. | Aggregate data only |
Cervical: n=42/65* Oral: n=109 infections/115 people* (includes males and females) |
Moderate |
| Sohn et al., 2018 (22) |
Cervical: n=98/192 (51%) Oral: n=18/190 (9%) |
. | . |
Cervical: n=69/98* Oral: n=9/18* |
Moderate |
| Ciccarese et al., 2017 (28) |
Cervical: n=31/46 (67%) Oral: n=17/46 (37%) |
. | . |
Cervical: n=12/31 Oral: n=3/17 |
Moderate |
| Kero et al., 2014 (79) |
Cervical: Baseline: n=8/46 (17%), Follow up: n=10/46 (22%) Oral: Baseline: n=3/46 (7%), Follow up: n=4/41 (10%) |
. | . |
Cervical: Baseline: n=0/8*, Follow up: n=9/10* Oral: Baseline: n=3/3*, Follow up: n=3/4* |
Strong |
| da Mota Vasconcelos Brasil et al., 2013 (46) |
Cervical: n=18/31 (58%) Oral: n=17/31 (55%) |
. | . | . | Moderate |
| Herrero et al., 2013 (45) |
Cervical: Baseline: n=511/5832 (9%); Year 4: n=280/5834 (5%) Oral: Year 4: n=157/2924 (5%) |
. | . |
Cervical: Year 4: n=280/5843* Oral: Year 4: n=57/5834 |
Moderate |
| Schlecht et al., 2012 (48) |
Cervical: n=345/645 (53%) Oral: n=126/645 (20%) |
. | . |
Cervical: n=208 infections/345 women* Oral: n=17 infections/126 women* |
Moderate |
| Kero et al., 2011 (53) |
Cervical: n=24/128 (19%) Oral: n=22/128 (17%) |
. | . |
Cervical: n=19/24 Oral: n=18/22 |
Moderate |
| Sarkola et al., 2009 (80) |
Cervical:
Baseline: n=31/178 (17%) 36 mo: n=24/178 (13%) (Aggregate data and bar graph description provided for additional follow-up mo) Oral: Baseline: n=33/178 (19%) 6mo: n=43/178 (24%) (Aggregate data bar graph description provided for additional follow-up mo) |
. | . |
Cervical:
Baseline: n=31/178 36 mo: n=24/178 (Aggregate data and bar graph description provided for additional follow-up mo) Oral: Baseline: n=33/178 6mo: n=43/178 (Aggregate data and bar graph provided for additional follow-up mo) |
Strong |
| D’Souza et al., 2007 (81) |
Cervical: Baseline: n=116/182 (64%); Follow up: n=110/182 (60%) Oral: Baseline n=35/182 (19%); Follow up: n=36/182 (20%) |
. | . |
Cervical: Baseline: n=82/116*; Follow up: n=90/110* Oral: Baseline n=21/35*; Follow up: n=21/36* |
Strong |
| Rintala et al., 2005 (82) |
Cervical: n=10/76 (13%) to n=19/76 (25%) Oral: n=6/76 (8%) to n=26/76 (34%) (Ranges presented; data aggregately reported for baseline to 24-mo follow-up) |
. | . |
Cervical: n=10/76 (13%) to n=19/76 (25%) Oral: n=6/76 (8%) to n=26/76 (34%) (Ranges presented; bar graph description and aggregate data reported for baseline - 24-mo follow-up) |
Moderate |
| Winer et al., 2003 (83) |
Cervical: Incident cases: n=88/444 (20%) Oral: n=5/2619 samples (0.2%) from 529 women |
. | . | Aggregate data and bar graph description* | Moderate |
| Chatterjee et al., 2001 (66) |
Cervical: n=17/27 (63%) Oral: n=20/69 (29%) |
. | . |
Cervical: n=17/17* Oral: n=20/20* |
Moderate |
N/A, Not applicable; ., No information provided; *HPV types listed in paper; † :Concurrent refers to the synchronous dual-site occurrence of any HPV type(s) in both the cervix and oral cavity/oropharynx; ‡ Concordant refers to infections with at least one identical HPV type across sites, synchronously or asynchronously; ¶ :HR-HPV types included 16, 18, 31, 33, 34, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, and 70; §: Study quality assessed though the Quality Assessment Tool for Quantitative Studies (QATQS) from the Effective Public Health Practice Project.
Eighty-three percent of all synchronous testing studies (n=67/80, Table 3A) (4, 15–21, 23, 25–27, 29–44, 47, 49–52, 54–65, 67–78, 84–93) provided some form of data on concurrent oral-cervical HPV+ cases. Concurrent oral and cervical HPV infection rates could be calculated for most, but not all, of these studies (n=59/67, 88%) (4, 15–17, 20, 21, 23, 25–27, 29–39, 41–44, 47, 49–52, 54–65, 67–72, 76–78, 84–89, 91–93). The calculated concurrent rates ranged from 0% to 95%, depending on the study. On average, 15% of women had HPV infections occurring concurrently in both sites. Most rates of concurrent oral and cervical HPV infections were ≤10% (n=39/59, 66%) (15, 17, 20, 21, 23, 26, 27, 29–32, 34–37, 39, 41, 43, 44, 49, 51, 52, 55, 56, 59–65, 67, 69, 77, 78, 84–86, 92). Only four studies (7%) (54, 72, 89, 93) had concurrent oral and cervical HPV infection rates over 65%.
Among the 67 studies identifying concurrent oral and cervical HPV+ cases, 70% (n=47/67) (4, 15, 16, 18–20, 23, 25–27, 29, 32, 33, 36–40, 42, 43, 47, 50–52, 56–60, 62, 63, 65, 68, 70, 72–74, 84–93) determined concordance in oral-cervical HPV types (Table 3A). For studies reporting overall rates (n=40/47, 85%) (4, 15, 16, 20, 23, 25–27, 29, 32, 33, 36–39, 42, 43, 47, 50–52, 56–60, 62, 63, 65, 68, 70, 72, 84–86, 88, 89, 91–93), concordance in oral and cervical HPV infection types ranged from 0% to 100%, with an average of 41% of the women having infections of the same type in both sites. More than half of the studies had oral-cervical HPV type concordance rates of <50% (n=23/40, 58%) (4, 16, 25, 27, 32, 36, 37, 39, 43, 51, 52, 56, 58, 59, 62, 63, 65, 70, 72, 85, 89, 91, 93), yet seven studies reported concordance rates of >80% (15, 23, 47, 50, 60, 86, 88).
Asynchronous Oral-Cervical HPV Testing (n=12)
Twelve studies evaluated HPV-related infections of the oral cavity/oropharynx and cervix asynchronously (94–105) (Table 2B). Most studies sampled women with cervical infections for oral HPV (n=7/12, 58%) (95, 96, 98, 100, 101, 103, 105). Cervical HPV data collection usually relied on medical records (94–96, 98, 100–105) while at least some oral samples were actively evaluated for HPV during the study (94–105). Oral HPV sampling methodology used a buccal (brush) sample (95, 98, 101, 103), biopsied lesions (96, 97, 102, 104), or a gargle/rinse sample (94, 99, 100, 105). Cervical and oral HPV DNA was often detected by PCR (94–96, 100–105).
Table 2B.
Description of methodology used in asynchronous oral-cervical HPV evaluation papers (n=12).
| AUTHOR, YEAR (REFERENCE) | STUDY DESIGN | COUNTRY | PARTICIPANTS | SAMPLE COLLECTION METHOD | HUMAN PAPILLOMAVIRUS (HPV) DETECTION METHOD | NOTE/“FOLLOW UP TIMING” | |
|---|---|---|---|---|---|---|---|
| Cervical/Oral sample type | Cervical intraepithelial neoplasia (CIN)- cervical cancer/Oral cancer diagnosis data source | ||||||
| ASYNCHRONOUS | |||||||
| Papers with sufficient dual-site** data | |||||||
| Sanchez-Siles et al., 2020 (105) | Cohort | Spain | n=100 women (n=50 with HPV-related cervical intraepithelial neoplasia (CIN), n=50 without CIN) |
Cervical: Not specified Oral: Rinse |
Cervical: Hospital database Oral: N/A |
PCR |
Cervical: Not specified Oral: Baseline |
| Christensen et al., 2019 (104) | Case-control | Denmark | n=417 women with oropharyngeal squamous cell carcinoma |
Cervical: N/A Oral: Tumor specimens |
Cervical: Cancer registry Oral: Cancer registry |
PCR |
Cervical: Cancer history timing not specified, noted to be before oral cancer Oral: Cancer diagnosed 2000-2014 |
| Rietbergen et al., 2018 (102) | Cross-sectional | Netherlands | n=308 women with invasive squamous cell carcinoma of the oropharynx |
Cervical: N/A Oral: Biopsy |
Cervical: Pap smears from pathology database Oral: Cancer registry |
PCR |
Cervical: Various years specified Oral: Treated 2000-2015 |
| Lupato et al., 2017 (99) | Cross-sectional | Italy | n=253 women (18-35 years old) |
Cervical: Self-report from Papanicolaou (Pap) smear Oral: Rinse |
Cervical: N/A Oral: N/A |
Not specified |
Cervical: Current infections and Pap history (timing not specified) Oral: Baseline |
| Visalli et al., 2016 (100) | Cross-sectional | Italy | n=125 (n=100 women with pre-existing HPV genital lesions, n=25 healthy controls) |
Cervical: Medical record Oral: Rinse |
Cervical: N/A Oral: N/A |
PCR |
Cervical: Not specified Oral: Baseline |
| Marques et al., 2015 (101) | Cross-sectional | Brazil | n=43 women with CIN2, CIN3, and invasive cervical carcinoma |
Cervical: N/A Oral: Brush |
Cervical: Self-report from Pap Smear; Colposcopy Oral: N/A |
PCR |
Cervical: 1-6 months before baseline Oral: Baseline |
| Peixoto et al., 2011 (103) | Cross-sectional | Brazil | n=100 women with history of cervical HPV infection |
Cervical: Histology Oral: Swab/scrape/brush/biopsy |
Cervical: N/A Oral: N/A |
PCR |
Cervical: Not specified Oral: Baseline |
| Saini et al., 2010 (98) | Cross-sectional | Malaysia | n=70 women previously diagnosed with cervical cancer |
Cervical: N/A Oral: Swab |
Cervical: Medical records Oral: N/A |
“Digene HC2 HPV DNA” test |
Cervical: Not specified, undergoing active treatment Oral: Baseline |
| Sánchez-Vargas et al., 2010 (95) | Cross-sectional | Mexico | n=46 women with a CIN diagnosis <6 months |
Cervical: N/A Oral: Swab |
Cervical: Histology Oral: N/A |
PCR |
Cervical: <6 months from baseline Oral: Baseline |
| Premoli-De-Percoco, 1998 (97) | Cross-sectional | Not Specified | n=50 women with oral squamous cell carcinoma |
Cervical: Swab Oral: Biopsy |
Cervical: N/A Oral: Medical records |
Non-radioactive DNA probes (Oligoprobe source, Polar Brewing Co.) |
Cervical: Baseline Oral: Cancer history timing not specified |
| Kellokoski et al., 1992 (96) | Cross-sectional | Finland | n=334 women |
Cervical: Biopsy Oral: Biopsy |
Cervical: N/A Oral: N/A |
Southern Blot Hybridization and PCR |
Cervical: Medical histories starting in 1981 Oral: Baseline (no year, publication date 1992) |
| Papers with insufficient dual-site** data | |||||||
| D’Souza et al., 2014 (94) | Cross-sectional | United States | n=104 women total (n=17/104 women were patients with HPV-positive oropharyngeal squamous cell cancer (OPC); n=87/104 were women partners of male patients with HPV-positive OPC) |
Cervical: N/A Oral: Rinse |
Cervical: Self-report, medical records Oral: Patients-previously diagnosed; partners-oral screening evaluation by oncologist |
PCR |
Cervical: Previous cancer history disclosed at study baseline without date Oral: Baseline |
**Dual-site refers to the asynchronous occurrence of any HPV type(s) in both the cervix and oral cavity/oropharynx.
N/A: not applicable sample collection method, meaning a site specific sample was collected or a site specific cancer diagnosis was provided.
Half of the asynchronous studies (n=6/12, 50%) showed that more women were HPV+ in the cervix than in the oral cavity/oropharynx (98–101, 103, 105) while essentially the other half (n=5/12, 42%) found the opposite (94, 96, 97, 102, 104). Most asynchronous studies (n=9/12, 75%) provided some data regarding the high-risk HPV types (94–101, 105) (Table 3B), tending to only specify when high-risk oral HPV was found (n=5/9, 56%) (94, 95, 98, 99, 101). Due to HPV assessments occurring at different times, studies rarely (n=4/9, 44%) reported both the specific high-risk oral and cervical HPV types found at the person level (96, 97, 100, 105).
Table 3B.
Results of the asynchronous oral-cervical HPV evaluation papers (n=12).
| AUTHOR, YEAR (REFERENCE) | RESULTS, n=# of women unless otherwise noted | OVERALL QUALITY§ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Any Cervical Human Papillomavirus (HPV)+ or Oral HPV+ Infections | Dual-site†† oral-cervical HPV infections | Concordant‡ dual-site oral-cervical infections | High Risk (HR)-HPV Infections | ||||||
| ASYNCHRONOUS | |||||||||
| Papers with sufficient dual-site data | |||||||||
| Sanchez-Siles et al., 2020 (105) |
Cervical: n=50/100 (50%) Oral: n= 13/100 (13%), (n=7/50 with cervical intraepithelial neoplasia (CIN), n=6/50 without CIN) |
n=7/50 (14%) | n=1/50 (2%) |
Cervical: n=62/93* infections Oral: n=12/16* infections |
Strong | ||||
| Christensen et al., 2019 (104) |
Cervical: n=72/343 (21%) Oral: n=203/417 (49%) |
n=42/343 (12%) | . | . | Strong | ||||
| Rietbergen et al., 2018 (102) |
Cervical: n=16/224 (7%) Oral: n=70/308 (23%) |
n=9/224 (4%) | . | . | Moderate | ||||
| Lupato et al., 2017 (99) |
Cervical: n=11/90 (12%) Oral: n=10/253 (4%) |
n=1/90 (1.1%) | . |
Cervical: . Oral: HR-HPV cases not separated by sex* |
Moderate | ||||
| Visalli et al., 2016 (100) |
Cervical: n=100/125 (80%) Oral: n=26/125 (21%) |
n=24/125 (19%) | . |
Cervical: n=58/100* Oral: bar graph description * |
Moderate | ||||
| Marques et al., 2015 (101) |
Cervical: n=43/43 (100%) Oral: n=1/43 (2%) |
n=1/43 (2%) | . |
Cervical: . Oral: n=0/1 |
Moderate | ||||
| Peixoto et al., 2011 (103) |
Cervical: n=100/100 (100%) Oral: n=81/100 (81%) |
n=81/100 (81%) | . | . | Moderate | ||||
| Saini et al., 2010 (98) |
Cervical: n=70/70 (100%) Oral: n=4/70 (6%) |
n=4/70 (6%) | . |
Cervical: . Oral: n=4/4 |
Moderate | ||||
| Sánchez-Vargas et al., 2010 (95) |
Cervical: n=43/43 (100%) Oral: n=43/43 (100%) |
n=43/43 (100%) | . |
Cervical: . Oral: n=15/43* |
Moderate | ||||
| Premoli-De-Percoco et al., 1998 (97) |
Cervical: n=28/50 (56%) Oral: n=35/50 (70%) |
n=23/50 (46%) | n=23/23* (100%) |
Cervical: n=28/28* Oral: n=35/35* |
Moderate | ||||
| Kellokoski et al., 1992 (96) |
Cervical: n=14/272 (5%) Oral: Southern Blot Hybridization (SBH): n=42/272 (15%); Polymerase chain reaction (PCR): n=25/85 (29%) |
n=14/272 (5%) | n=2/14* (14%) | Controls: Cervical: n=12/25* Oral: n=6/25* |
Moderate | ||||
| Papers with insufficient dual-site data | |||||||||
| D’Souza et al., 2014 (94) |
Cervical: n=11/104 (11%) Oral: n=13/104 (13%) |
. | . |
Cervical: . Oral: n=11/104 |
Moderate | ||||
.: No information provided; *:HPV types listed in paper; †† Dual-site refers to the asynchronous occurrence of any HPV type(s) in both the cervix and oral cavity/oropharynx; ‡ Concordant refers to infections with at least one identical HPV type across sites, synchronously or asynchronously; ¶ HR-HPV types included 16, 18, 31, 33, 34, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, and 70; §: Study quality assessed though the Quality Assessment Tool for Quantitative Studies (QATAS) from the Effective Public Health Practice Project.
Most asynchronous studies (n=11/12, 92%) differentiated between women with and without dual-site oral and cervical HPV infections at any time (95–105) (Table 3B). One woman (2%) to as many as all (100%) women asynchronously tested positive for HPV in both the oral cavity/oropharynx and cervix. The overall dual-site oral and cervical HPV+ infection rate estimate was 26% (95–105). On average, when women had (pre)existing cervical infections (95, 98, 100, 101, 103, 105), almost twice as many were dually-infected with HPV in the oral cavity/oropharynx (avg.: 37%, range: 2-100%) as compared to women with (pre)existing oral HPV infections who were also cervical HPV+ (avg.: 21%, range: 4-46%) (97, 102, 104). Women without a known, prior oral or cervical HPV infection were not as likely to be dually HPV infected at both sites, with rates ranging from 1.1-5% (96, 99).
Among studies where women were known to be dually-infected with oral and cervical HPV, 27% (n=3/11) measured concordance in HPV types across both sites at any time (96, 97, 105). On average, 39% of asynchronous oral and cervical infections within women had an HPV type in common (96, 97, 105) (Table 3B). Women who had an HPV+ oral cancer and a cervical HPV infection present had the greatest concordance in oral-cervical HPV types (100%) (96, 97, 105). Rates of concordant oral-cervical HPV types were lower in studies where not all women had prior HPV-related infections (2-14%) (96, 97, 105).
Cancer Diagnoses Only (Primary Oral/Cervical, Secondary Cervical/Oral, n=22)
Twenty-two retrospective studies focused on the diagnosis of a secondary cervical or oral cancer after a primary cancer diagnosis of oral or cervical cancer (106–127) (Table 2C). Although we specifically included studies focused on HPV-related oral cancers, the sites of oral cancers varied across studies (e.g., some studies included oropharynx, oral cavity and pharynx, some only included oropharyngeal, and some vaguely defined HPV-related head and neck sites). Five studies examined the risk of a secondary cervical cancer after a primary diagnosis of oral cancer (113, 120–123). Half of the studies (n=11/22, 50%) examined the risk of a secondary oral cancer diagnosis after a primary diagnosis of a cervical cancer (n=6) (106–108, 111, 115, 116) or a cervical intraepithelial neoplasia (CIN) (n=5) (109, 110, 118, 124, 125). Six studies investigated the risk of a secondary cervical and/or oral cancer after a primary diagnosis of an oral and/or cervical cancer (112, 114, 117, 119, 126, 127). Most studies utilized data from country or state level cancer registries to monitor disease surveillance (n=15/22, 68%) (106–118, 124, 126); three studies conducted medical chart reviews (120, 121, 123); four studies collected at least some data from institutional or provincial tumor registries (119, 122, 125, 127).
Table 2C.
Description of methodology used in oral-cervical human papillomavirus (HPV)-related cancer diagnoses only papers (n=22).
| AUTHOR, YEAR (REFERENCE) | STUDY DESIGN REGISTRY NAME |
COUNTRY | PARTICIPANTS | PRIMARY CANCER DIAGNOSIS | DATA SOURCES | CANCER CONFIRMATION METHOD | TIME PERIOD |
|---|---|---|---|---|---|---|---|
| CANCER DIAGNOSES ONLY | |||||||
| Holstead et al., 2020 (122) | Cohort | United States | n= 155 diagnosed with oropharyngeal squamous cell carcinomas (OPSCC) n=26 women diagnosed with HPV-positive OPSCC |
Oral | Cancer registry (local) and medical records | Biopsy-proven | 2012-2014 |
| Larish et al., 2020 (123) | Cohort | United States | n=46 women diagnosed with HPV-positive OPSCC | Oral | Medical records | Not discussed HPV-positive: p16 staining or HPV DNA |
N/A |
| Loopik et al., 2020 (124) | Cohort | The Netherlands | n=89018 women diagnosed with cervical intraepithelial neoplasia (CIN) 3 n=89018 women with a benign dermal nevus were selected as control group |
Cervical (CIN3) | Histo and cytopathology registry (nationwide) | Histologically proven | 1990-2010 |
| Preti et al., 2020 (125) | Cohort | Italy | n=5595 patients surgically treated for high-grade CIN and had follow up times of at least 5 years | Cervical (High grade CIN) | Medical record with cancer registry (provincial) | Classification of Diseases (ICD) codes | 1992-2014 |
| Wang et al., 2020 (126) | Cohort Surveillance, Epidemiology, and End Results (SEER) |
United States | n=63,710 women diagnosed with an index P-HPV-associated cancer | Oral or Cervical |
Cervical: Cancer registry (state/nationwide) Oral: Cancer registry (state/nationwide) |
ICD codes and histology codes | 2000-2015 |
| Gazzaz et al., 2019 (127) | Cohort Alberta Health |
Canada | n=372 women diagnosed with OPSCC | Oral or Cervical | Cancer registry (provincial) | Not discussed | 1997-2015 |
| Papatla et al., 2019 (115) | Cohort SEER |
United States | n=21060 women with cervical squamous cell carcinoma |
Cervical |
Cervical: Cancer registry (state/nationwide) Oral: Cancer registry (state/nationwide) |
ICD codes | 1973-2014 |
| Suk et al., 2018 (117) | Cohort SEER |
United States | n=44011 women with cervical cancer n=15303 women with oropharyngeal cancer |
Oral or Cervical |
Cervical: Cancer registry (state/nationwide) Oral: Cancer registry (state/nationwide) |
ICD codes and histologically confirmed | 1973-2014 |
| Ebisch et al., 2017 (109) | Cohort PALGA |
Netherlands | n=89018 women with CIN3 | Cervical (CIN3) |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
Not discussed | 1990-2010 |
| Neumann et al., 2016 (114) | Cohort K2-France |
France | n=6049 women with potentially-HPV-related first cancers (n=4234 cervical cancer; n=502 head and neck cancer) | Oral or Cervical |
Cervical: Cancer registry (8 areas of France) Oral: Cancer registry (8 areas of France) |
ICD codes | 1989-2004 |
| Svahn et al., 2016 (118) | Cohort Danish Cancer Registry |
Denmark | n=101974 women with CIN3 (includes adenocarcinoma in situ) | Cervical (CIN3) |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
Pathology database matched | 1943-2012 |
| Jung et al., 2015 (113) | Cohort Korea Central Cancer Registry |
South Korea | n=11322 women diagnosed with primary head and neck cancer | Oral |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
ICD codes | 1993-2010 |
| Gaudet et al., 2014 (110) | Cohort British Columbia (BC) Cancer Agency Cervical Cancer Screening Program |
Canada | n=54320 women with CIN2 and CIN3 | Cervical (CIN2, CIN3) |
Cervical: Cancer registry (province-wide) Oral: Cancer registry (province-wide) |
ICD codes | 1980-2005 |
| Skinner et al., 2014 (119) | Retrospective cohort University of Texas (UT) MD Anderson Cancer Center |
United States | n=125 women with two or more HPV-related cancers | Oral or Cervical |
Cervical: Institutional tumor registry (UT MD Anderson Cancer Center) Oral: Institutional tumor registry (UT MD Anderson Cancer Center) |
Pathologically confirmed | 1949-2009 |
| Gan et al., 2013 (120) | Cohort | United States | n=2230 patients with confirmed squamous cell carcinoma of the oropharynx (SCCOP): oral cavity, oropharynx, hypopharynx, and/or larynx | Oral |
Cervical: Medical chart review Oral: Medical chart review |
Pathologically confirmed | 1995-2010 |
| Chen et al., 2012 (108) | Cohort Taiwan Cancer Registry |
Taiwan | n=52972 women with cervical cancer | Cervical |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
ICD codes | 1979-2008 |
| Biron et al., 2011 (121) | Cohort Alberta Health Services |
Canada | n=248 women with oropharyngeal squamous cell carcinoma | Oral |
Cervical: Medical chart review Oral: Medical chart review |
Pathologically confirmed | 1998-2008 |
| Chaturvedi et al., 2009 (107) | Cohort SEER |
Denmark, Sweden, Norway, Finland, United States | n=104760 cervical cancers (n=85109 squamous cell carcinoma; n=10280 adenocarcinoma) | Cervical |
Cervical: Cancer registry (multi-national combination) Oral: Cancer registry (multi-national combination) |
Histology codes | 1943-2002 |
| Rose Ragin et al., 2008 (116) | Cohort SEER |
United States | n=2618 women (19–97 years old) with cervical cancer | Cervical |
Cervical: Cancer registry (state/nationwide) Oral: Cancer registry (state/nationwide) |
ICD codes | 1973-2002 |
| Chaturvedi et al., 2007 (106) | Cohort SEER |
Denmark, Sweden, Norway, Finland, United States | n=104760 women diagnosed with cervical cancer | Cervical |
Cervical: Cancer registry (multi-national combination) Oral: Cancer registry (multi-national combination) |
Not discussed | 1943-2001 |
| Hemminki et al., 2001 (112) | Cohort Swedish Family Cancer Database |
Sweden | n=3366 women diagnosed with oral cancer n=17234 women diagnosed with cervical cancer |
Oral or Cervical |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
Histologically or cytological confirmed | 1958-1996 |
| Hemminki et al., 2000 (111) | Cohort Swedish Family Cancer Database |
Sweden | n=117830 women with in-situ cervical cancer n=17556 women with invasive cervical cancer |
Cervical |
Cervical: Cancer registry (nationwide) Oral: Cancer registry (nationwide) |
ICD codes | 1958-1996 |
Among women with a primary diagnosis of oral cancer, the number of secondary cervical cancers was lowest among medical record-based studies (122, 123), followed by provincial registries (121, 127), and highest among national studies (112, 113, 117, 120, 126). National studies reported that the incidence of a secondary cervical cancer ranged from 4.5-192.5 per 10,000 women (112, 113, 117, 120, 126) (Table 3C). The observed cases of a secondary cervical cancer were higher than expected in five studies with the SIR generally ranging from 1.4-29.4 (113, 117, 120, 121, 127). Interestingly, Gan et al. found that the SIR of a secondary cervical cancer was smaller among women diagnosed with HPV-related oral cancers (SIR range: 3.3-4.0) compared to women diagnosed with non-HPV-related oral cancers (SIR range: 8.3-12.8) (120). Two studies did not observe any differences between the numbers of observed and expected cases of a secondary cervical cancer among women who had a primary oral cancer (112, 126).
Table 3C.
Results of the oral-cervical human papillomavirus (HPV)-related cancer diagnoses only papers (n=22).
| AUTHOR, YEAR (REFERENCE) | RESULTS, number of cancer diagnoses | OVERALL QUALITY§ | |||
|---|---|---|---|---|---|
| Primary Diagnosis: Cervical | Primary Diagnosis: Oral | Secondary Diagnosis: Cervical | Secondary Diagnosis: Oral | ||
| CANCER DIAGNOSES ONLY | |||||
| Holstead et al., 2020 (122) | 26 | Cervical cancer: n=2 | Strong | ||
| Larish et al., 2020 (123) | 46 | Cervical cancer: n=1 Cervical intraepithelial neoplasia (CIN) 1-3: n=12 High risk HPV+: n=5 |
Strong | ||
| Loopik et al., 2020 (124) | 1797 | Oropharyngeal cancers: n=0 | Strong | ||
| Preti et al., 2020 (125) | 3184 | Oropharynx: n=5 Esophagus: n=1 |
Strong | ||
| Wang et al., 2020 (126) | 46,550 | 6,288 |
Among women who had potentially HPV-associated cancer: n=2,488 had secondary cervical cancer Standardized incidence ratio (SIR)=1.50 (1.44-1.56) Among women who had oral cancer: n=5 had secondary cervical cancer, SIR=1.53 (0.49-3.56) |
Among women who had potential HPV-associated cancer: n=695 had secondary oral cancer, SIR=2.29 (2.12-2.47) Among women who had cervical cancer: n=3 had secondary oral cancer SIR=3.88 (0.78-11.33) |
Strong |
| Gazzaz et al., 2019 (127) | 372 | History of cervical cancer (CC): n=33 SIR of CC: Age 25-39: 12.8 Age 40-54: 108.9 Age 55-69: 77.7 Age 70+: 23.9 |
Strong | ||
| Papatla et al., 2019 (115) | 21,060 | Oropharynx: n=4 Oral cavity and pharynx: n=72 SIR: 4.36 (95% confidence interval (CI)=1.19-11.15) |
Strong | ||
| Suk et al., 2018 (117) | 44,011 | 15,303 |
Primary Oropharyngeal cancer: Cervical: n=17 SIR: 1.6, P<0.05 |
Primary cervical cancer: Oropharyngeal: n=56 SIR: 1.4, P<0.05 |
Moderate |
| Ebisch et al., 2017 (109) | 89,018 | Oropharyngeal: n=13 SIR: 5.51 (95% CI=1.22-24.84) |
Strong | ||
| Neumann et al., 2016 (114) | 4234 | 502 |
Among primary head and neck:
Cervical: n=0/502 |
Among primary cervical:
head and neck: n=5/4234 SIR: 6.34 (95% CI=2.04-14.79) tongue and tonsil: n=0/4234 oral cavity: n=0/4234 larynx: n=4/4234 SIR: 8.85 (95% CI=2.38-22.65) |
Strong |
| Svahn et al., 2016 (118) | 101,974 |
Any Head and Neck Squamous Cell Carcinoma: n=189 (Strongly HPV associated: n=63/189; Base of tongue and tonsil: n=47/63; Other oropharynx: n=16/63) Hazard ratio (HR): 1.99 (95% CI=1.72-2.31) |
Strong | ||
| Jung et al., 2015 (113) | 11,322 |
Among those with primary oral cavity: Cervical: 3 years (yrs): n=36; 5 yrs: n=73 SIR:0.55 (95% CI=0.11-1.6) Among those with primary oropharynx: Cervical: 3 yrs: n=97; 5 yrs: n=133 SIR: 3.11 (95% CI=1.14-6.77) Among those with primary larynx: Cervical: 3 yrs: n=0; 5 yrs: n=12 SIR: 0.47 (95% CI=0.01-2.63) |
Strong | ||
| Gaudet et al., 2014 (110) | 54,320 | Head and neck: n=30 SIR: 0.61 (95% CI=0.21-1.38) |
Strong | ||
| Skinner et al., 2014 (119) | 85 | 17 |
Among those with primary head and neck cancer: Cervical: n=8 [NOTE: n=5 synchronous cancers at the cervix and head and neck sites] |
Among those with primary cervical cancer: Head and neck: n=63 |
Moderate |
| Gan et al., 2013 (120) | 2,230 |
Among those who had primary oropharynx cancer: Cervical: n=0 Among those who had primary non-oropharynx cancer: Cervical: n=1 |
Moderate | ||
| Chen et al., 2012 (108) | 52,972 | Oral/pharynx: n=37; SIR: 1.18 (95% CI=0.83-1.62) Salivary gland: n=4; SIR: 0.77 (95% CI=0.21-1.97) Nasopharynx and nasal cavity: n=34; SIR: 1.01 (95% CI=0.70-1.42) Esophagus: n=31; SIR: 2.55 (95% CI=1.74-3.63) Larynx: n=2; SIR: 0.67 (95% CI=0.08-2.43) |
Strong | ||
| Biron et al., 2011 (121) | 248 |
Cervical: n=20 SIR: 29.4 (95% CI=12.05-74.98) |
Strong | ||
| Chaturvedi et al., 2009 (107) | 104,760 | HPV-related cancer: n=1248 Tongue: n=28; SIR: 1.25 (95% CI=0.83-1.81) Mouth: n=60; SIR: 1.61 (95% CI=1.24-2.08) Pharynx: n=49; SIR: 2.06 (95% CI=1.53-2.73) Esophagus; n=89; SIR: 1.50 (95% CI=1.21-1.86) Larynx: n=48; SIR: 2.10 (95% CI=1.55-2.79) |
Strong | ||
| Rose Ragin et al., 2008 (116) | 2,618 | Oral Cavity: n=30 Oral cavity and pharynx SIR=1.7 (95% CI=1.3–2.2) Lip: n=4 Salivary gland: n=5 Oropharynx: n=12 (11 tonsil); |
Strong | ||
| SIR=2.7 (95% CI=1.4–4.7) Tonsils SIR=3.1(95% CI=1.5–5.5) Nasopharynx: n=2 Larynx: n=25; SIR=2.7 (95% CI=1.7–3.9) Hypopharynx: n=7 |
|||||
| Chaturvedi et al., 2007 (106) | 104,760 | Tongue: n=32; SIR: 1.18 (95% CI=0.81-1.67) Mouth: n=66; SIR: 1.48 (95% CI=1.15-1.89) Pharynx: n=52; SIR: 1.83 (95% CI=1.37-2.41) Esophagus: n=101; SIR: 1.42 (95% CI=1.16-1.73) Larynx: n=56; SIR 2.02 (95% CI=1.53-2.63) |
Strong | ||
| Hemminki et al., 2001 (112) | 17,234 | 3,366 |
Among those who had primary oral cancer:
Cervical cancer: n=8 SIR: 1.73 (95% CI=0.74-3.13) |
Among those who had primary cervical cancer:
Oral: n=33 SIR: 2.20 (95% CI=1.51-3.01) Esophagus: n=9 SIR: 1.67 (95% CI=0.76-2.94) |
Moderate |
| Hemminki et al., 2000 (111) | 117,830 | 17,556 |
Among primary
in situ
cervical: n=101 upper aerodigestive tract SIR=1.68 Among primary invasive cervical cancer: n=31 upper aerodigestive tract SIR=2.45 |
Strong | |
§Study quality assessed though the Quality Assessment Tool for Quantitative Studies (QATAS) from the Effective Public Health Practice Project.
Among women with a primary cervical cancer, one provincial-level registry found very few cases of secondary oral cancers (125). Nationally, studies that reported the incidence of a secondary oral/head and neck cancer ranged from 1.0-45.8 per 10,000 women (106–108, 110–112, 114–117, 126); one study had an incidence of zero for secondary oropharyngeal cancers (124) (Table 3C). The incidence rates varied due to differences in included oral cancer sites across studies. The observed cases of a secondary oral cancer were higher than expected in almost all national studies, including primary CIN3 cases, with the SIR ranging from 1.4-6.3 (106–109, 111, 112, 114–118, 126).
Quality Assessment
For the quality assessment of the 114 included papers based on the QATQS tool, 26 studies (23%) were classified as strong (73, 76, 77, 79–81, 104–111, 113–116, 118, 121–127), 81 studies (71%) were moderate (4, 15–26, 28, 29, 31–49, 52–58, 60, 62–72, 74, 75, 78, 82–91, 93–103, 112, 117, 119, 120), and 7 (6%) were weak (27, 30, 50, 51, 59, 61, 92) (Tables 3A–C). The most common component rated as weak was study design (n=79, 69%) (4, 15–72, 84–103); only a few studies used a case-control design (n=2, 2%) (76, 104) or cohort design (n=33, 29%) (73–75, 77–83, 105–127) with the majority being cross-sectional designs (n=79, 69%) (4, 15–72, 84–103). In addition, few studies randomly selected participants for inclusion from a comprehensive list of the target population (n=26, 23%) (18, 21, 24, 32, 34, 36, 37, 44, 45, 83, 92, 104, 108, 109, 111–113, 115–119, 121, 124, 126, 127). This contributed to most studies being classified as ‘moderate’ for selection bias (n=99, 87%) (4, 15–26, 28–33, 35–43, 46–49, 51–58, 60–77, 79–82, 84–91, 93–103, 105–107, 109–116, 118–123, 125). For data collection within synchronous and asynchronous HPV testing studies, some studies did not specify an HPV infection sample collection method, so the validity and reliability were unknown or they relied on self-reported HPV infections (n=10/92, 11%) (4, 33, 40, 55, 63, 64, 73, 94, 99, 101). For the last criteria, withdrawals and dropouts, few cohort studies described the number of and/or reasons for participants being lost-to-follow-up (n=8/33, 24%) (73, 74, 78–81, 83, 108).
Discussion
After an expansive search of four databases for studies of dual-site oral and cervical HPV infections/cancers, we included 114 papers that evaluated the sites synchronously (n=80) (4, 15–93), asynchronously (n=12) (94–105), or by cancer diagnoses only (n=22) (106–127). This systematic review enhances the previous meta-analysis (4) by including more publication years, comprehensive search terms, databases, general oral HPV testing approaches, and formal study quality assessments of included studies using QATQS. We found that studies evaluating both oral and cervical HPV infections had cervical HPV+ rates that were higher than oral HPV+ rates.
The reporting of dual-site oral and cervical HPV infection rates was wide-ranging. On average, 15% of infections occurred concurrently in the oral cavity/oropharynx and cervix. Among concurrent oral-cervical HPV+ cases, HPV types were concordant across the two sites in an average of 41% of women. Asynchronous dual-site (oral-cervical) HPV infection rates also varied, spanning from 1.1% to 100%, with an average of 26% of study populations testing positive for both oral and cervical HPV at different times. Oral-cervical HPV type concordance was either very low (2%) or high (100%) for these asynchronously tested and dually-infected women, producing an average concordance rate of 39%. Combining synchronous and asynchronous oral-cervical HPV testing data, it was estimated that 16% of women were dually infected and 41% of the dually infected women had at least one concordant HPV type across sites. Most cancer diagnoses only studies reported an increased risk for a secondary cervical and/or oral cancer, resulting in incidence spanning 1.0-192.5/10,000 women. Regardless of timing, most studies were cross-sectional (n=79, 69%) (4, 15–72, 84–103) and therefore achieved an overall moderate rating with QATQS scoring criteria (n=81, 71%) (4, 15–26, 28, 29, 31–49, 52–58, 60, 62–72, 74, 75, 78, 82–91, 93–103, 112, 117, 119, 120).
Oral HPV infection can be especially difficult to detect which may explain the lower oral-cervical HPV type concordance rates or lack of significant findings in the reviewed studies. Saliva continuously rinses the mouth so it may aid in regional virus clearance, making oral HPV more transient than HPV infections at other sites. Most people clear oral HPV infections, often in as little as a few months, which means it can easily be missed (3). HPV detection in the oral cavity is not indicative of oropharyngeal cancer either. The virus tends to inhabit the oropharynx (e.g., tonsils), so if only buccal samples are being tested, HPV may go undetected. Rinsing or gargling within the oral cavity may only partially capture any HPV inhabiting the oropharyngeal region (3, 9, 99, 128). HPV testing materials were originally designed for cervical HPV; although repeatedly shown to be capable of HPV detection at other sites, materials might not be as effective at identifying oral HPV (94, 129). Many existing oral cancer diagnostic tests are questionable, lacking standard diagnostic protocols. New diagnostic approaches are evolving but are not yet validated (3). With the increase in oral HPV cancers, oral HPV sampling and testing methodology should improve over time.
Other reasons for non-significant findings within studies might be site-independent or biological in nature. Virus detection methods (e.g., assay, technique) vary in sensitivity levels and are often HPV type specific, so the chosen HPV test may not be able to detect the HPV type present, suggesting no infection (98–100, 103, 129–131). Poor or inappropriate sample collections at either site might also hinder a positive HPV result (98). HPV-infected, but otherwise healthy people can test negative for the virus and/or may develop HPV type-specific immunity at other uninfected mucosal sites (96, 98, 132). It is also biologically plausible for a cervical HPV+ woman to not be oral HPV+ given that cervical-oral HPV transmission between heterogeneous partners is common, but oral-oral HPV transmission is infrequent (94).
The current systematic review expands upon the narrowly-focused topic-related meta-analysis of 2010 (4) with the inclusion of additional oral-cervical HPV studies and their quality assessments. We identified a significant gap in the oral-cervical HPV literature with HPV type concordance between sites being understudied, highlighting the need for better HPV data collection and reporting efforts. HPV type was frequently missing. Synchronous studies usually provided HPV type data for one site and only HPV+/- status for the other site, despite data for both sites being collected concurrently. Asynchronous studies recruiting women with (pre)existing HPV conditions tended to only report basic HPV status for the secondary anatomical site. Cancer diagnoses only or registry-based studies did not collect any HPV type information. When HPV types were reported, data tended to be presented at aggregate levels with either totals or broad categories by anatomical site and/or HPV type (e.g., HPV+/- status only, HPV16/not HPV16, oncogenic/not oncogenic, groups of multiple HPV types).
Additional problems with vague data reporting were observed, irrespective of whether or not studies involved synchronous or asynchronous oral and cervical HPV testing or cancer diagnoses only. Many studies provided a general summary statement regarding the oral-cervical HPV relationship across sites with the corresponding statistics (e.g., odds ratios, (Cohen) kappa statistics, p-values). Enumeration of sub-sites of oral cancers made it difficult to calculate incidence consistently among cancer diagnoses only papers. Information on HPV type was represented as ranges or in bar graphs, which made it difficult to extract specific values and interpret results. Still others did not stratify oral HPV results by sex so cervical HPV data could not be cross-compared with respective oral samples in females.
Without specific HPV type information presented at the person-level for both the oral cavity/oropharynx and cervix, concurrent/dual-site versus concordant infections could not be elucidated. Additionally, not all dual-site HPV+ studies, especially asynchronous and cancer diagnoses only papers, discussed the potential for concurrent infections which made it difficult to determine if the identified oral and cervical HPV infections could be related. Few studies listed participant data individually, making it unclear if a participant had the same infection in both sites. In turn, oral-cervical HPV type concordance data was missing or could not be deduced for more than half of the papers (n=62/114, 54%) (17–19, 22, 24, 28, 30, 34, 35, 40, 41, 44–46, 48, 49, 53–55, 64, 66, 71, 75, 76, 79–83, 87, 90, 94, 95, 98–104, 106–127).
Lack of HPV type details also made it difficult to describe the oral-cervical HPV infection epidemiology more generally. About 10% of synchronous and asynchronous studies quantified the number of HPV infections (vs. HPV+ women) to account for multiple infections in women, which is an important detail to note, but complicated the estimation of the disease burden. More than 10% of synchronous and asynchronous studies did not discuss if any detected HPV types were high-risk. The interpretation of cancer diagnoses only papers could not be compared collectively with synchronous and asynchronous papers due to different effect estimates being used (i.e., SIR). Additionally, almost one-third of cancer diagnoses only papers (n=7/22, 32%) were missing SIR values (118–120, 122–125).
The current systematic review also had its limitations. Unpublished works and conference abstracts were excluded, potentially missing some information, however, we evaluated many peer-reviewed publications with broad search terms. Only papers written and published in English were included so there could be a lack of generalizability to international research. However, 94 international studies were captured with our search criteria (or 82.5% of all papers included in this systematic review were conducted outside the US). The inability to decipher the vagueness in oral cancer types (i.e., HPV vs. tobacco/alcohol related) and/or a lack of differentiation between HPV infection sites (e.g., oral-cervical data combined within multi-site results) potentially prevented some topic-relevant papers from being included in the current review. Regardless, studies had to justify oral cancers as potentially HPV-related to be included. Using strict review criteria, the current review included studies focused on HPV-related oral and cervical infections/cancers only, minimizing misclassification bias concerns. The systematic review also relied on literature-reported “oral HPV-related cancer” terminology to portray results. Inconsistent use of varying terms across publications impeded the summarization of results across studies. The standardized QATQS tool could not be fully utilized due to the topic-related nature of this systematic review relying only on observational studies.
To better understand the epidemiology of oral HPV transmission moving forward, data collection efforts need to be improved to include standardized reporting of HPV type data. Individual-level, site-specific HPV type data should be reported for every sample evaluated, especially when investigators are already using HPV DNA tests that provide such detailed information. Cancer diagnoses studies/registries should include a repository of HPV-evaluated bio-specimens such that site-specific HPV types can be identified. Broad categories, aggregated data, summary statistics, and analyses without stratum-specific results only provide an overview of a potential association of HPV infections/cancers across sites without being able to hone in on possible transmission routes which can only be divulged if HPV types are compared.
Detailed documentation of the timing of HPV site-specific sampling and evaluations are also needed to aid in determining concurrent HPV infections or the likelihood of an association between dual/multi-site HPV infections. Generation of a special access database to pool this person-level, site-specific HPV infection/cancer data would facilitate the additional analyses needed to understand the epidemiology of HPV transmission between sites. Better understanding site-specific HPV infection/cancer biology, including transmission routes, can further aid in preventing and minimizing future disease burdens.
In conclusion, few reviewed studies utilized strong epidemiological methodologies to determine HPV type concordance in dual-site oral and cervical infections. The results from this systematic review are inconclusive given the heterogeneity of included studies with wide-ranging oral-cervical HPV infection/cancer rates. Cervical HPV+ infection/cancer diagnoses tended to be more prevalent in women than oral HPV+ infections/cancers were. Given that these dual-site infection rates can vary significantly by female population and no oral HPV+ cancer screening approach exists, oral HPV+ cancer incidence may continue to increase unchecked. Additional studies identifying specific HPV infection types, both concurrently and over time, at multiple biological sites (especially oral and cervical, but also vaginal, vulval, penial, and anal) within women and men are needed to better understand how HPV is transmitted and determine any relationships between potentially HPV-related cancer sites. Pooling of these individual-level study results into a special access HPV database could facilitate future research investigations. From there, risk factors and populations with potentially increased oral and/or cervical HPV cancer risks could more easily be identified and incorporated into future public health prevention and control efforts, locally and globally, to reduce the HPV-related cancer burden in men and women.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author Contributions
All authors agree to be accountable for the content of the work. KJ: validation, formal analysis, investigation, data curation, writing-original draft, writing-review and editing, and project administration. CB: validation, formal analysis, investigation, data curation, writing-original draft, writing-review and editing, and visualization. XZ: validation, formal analysis, investigation, data curation, writing-original draft, and writing-review and editing. EP: conceptualization, methodology, resources, writing-review and editing, and supervision. All authors contributed to the article and approved the submitted version.
Funding
KJ (P01 CA229143-S1) and XZ (F99CA253745-01) both have National Cancer Institute (NCI) funding through the National Institutes of Health (NIH). CB is funded through The Ohio State University Comprehensive Cancer Center.
Conflict of Interest
EP receives grant funding through the university from Pfizer and Merck Foundation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.848628/full#supplementary-material
References
- 1. Szymonowicz KA, Chen J. Biological and Clinical Aspects of HPV-Related Cancers. Cancer Biol Med (2020) 17:864–78. doi: 10.20892/j.issn.2095-3941.2020.0370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide Burden of Cancer Attributable to HPV by Site, Country and HPV Type. Int J Cancer (2017) 141:664–70. doi: 10.1002/ijc.30716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Candotto V, Lauritano D, Nardone M, Baggi L, Arcuri C, Gatto R, et al. HPV Infection in the Oral Cavity: Epidemiology, Clinical Manifestations and Relationship With Oral Cancer. Oral Implantol (Rome) (2017) 10:209–20. doi: 10.11138/orl/2017.10.3.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Termine N, Giovannelli L, Matranga D, Caleca MP, Bellavia C, Perino A, et al. Oral Human Papillomavirus Infection in Women With Cervical HPV Infection: New Data From an Italian Cohort and a Metanalysis of the Literature. Oral Oncol (2011) 47:244–50. doi: 10.1016/j.oraloncology.2011.02.011 [DOI] [PubMed] [Google Scholar]
- 5. Bonde JH, Sandri MT, Gary DS, Andrews JC. Clinical Utility of Human Papillomavirus Genotyping in Cervical Cancer Screening: A Systematic Review. J Low Genit Tract Dis (2020) 24:1–13. doi: 10.1097/lgt.0000000000000494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shrestha AD, Neupane D, Vedsted P, Kallestrup P. Cervical Cancer Prevalence, Incidence and Mortality in Low and Middle Income Countries: A Systematic Review. Asian Pac J Cancer Prev (2018) 19:319–24. doi: 10.22034/apjcp.2018.19.2.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wheeler BS, Rositch AF, Poole C, Taylor SM, Smith JS. Patterns of Incident Genital Human Papillomavirus Infection in Women: A Literature Review and Meta-Analysis. Int J STD AIDS (2019) 30:1246–56. doi: 10.1177/0956462418824441 [DOI] [PubMed] [Google Scholar]
- 8. Berman TA, Schiller JT. Human Papillomavirus in Cervical Cancer and Oropharyngeal Cancer: One Cause, Two Diseases. Cancer (2017) 123:2219–29. doi: 10.1002/cncr.30588 [DOI] [PubMed] [Google Scholar]
- 9. Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M. HPV in Oropharyngeal Cancer: The Basics to Know in Clinical Practice. Acta Otorhinolaryngol Ital (2014) 34:299–309. [PMC free article] [PubMed] [Google Scholar]
- 10. Bruni L, Albero G, Serrano B, Mena M, Gomez D, Munoz J, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World (Accessed April 22, 2020). Summary Report 17 June 2019.
- 11. IARC . Cancer Today: Cancer Fact Sheets (2020). Available at: https://gco.iarc.fr/ (Accessed January 19, 2021).
- 12. Sawaya GF, Smith-McCune K, Kuppermann M. Cervical Cancer Screening: More Choices in 2019. JAMA (2019) 321:2018–9. doi: 10.1001/jama.2019.4595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Burd EM. Human Papillomavirus and Cervical Cancer. Clin Microbiol Rev (2003) 16:1–17. doi: 10.1128/cmr.16.1.1-17.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thomas BH. A Process for Systematically Reviewing the Literature: Providing the Research Evidence for Public Health Nursing Interventions. Worldviews Evidence-Based Nurs (2004) 1:176–84. doi: 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- 15. Sehnal B, Zikan M, Nipcova M, Dusek L, Cibula D, Slama J. The Association Among Cervical, Anal, and Oral HPV Infections in High-Risk and Low-Risk Women. Eur J Obstet Gynecol Reprod Biol (2019) 4:1–5. doi: 10.1016/j.eurox.2019.100061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kiwerska K, Jozefiak A, Markowska J, Kedzia W, Jackowska J, Wierzbicka M. Oral-Genital Human Papillomavirus Infection in Polish Couples: Frequent Detection of HPV 42. BMC Infect Dis (2019) 19:122. doi: 10.1186/s12879-018-3645-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eggersmann TK, Sharaf K, Baumeister P, Thaler C, Dannecker CJ, Jeschke U, et al. Prevalence of Oral HPV Infection in Cervical HPV Positive Women and Their Sexual Partners. Arch Gynecol Obstet (2019) 299:1659–65. doi: 10.1007/s00404-019-05135-7 [DOI] [PubMed] [Google Scholar]
- 18. Brouwer AF, Eisenberg MC, Carey TE, Meza R. Multisite HPV Infections in the United States (NHANES 2003–2014): An Overview and Synthesis. Prev Med (2019) 123:288–98. doi: 10.1016/j.ypmed.2019.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vargas-Robles D, Magris M, Morales N, de Koning MNC, Rodriguez I, Nieves T, et al. High Rate of Infection by Only Oncogenic Human Papillomavirus in Amerindians. mSphere (2018) 3:1–13. doi: 10.1128/mSphere.00176-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tuominen H, Rautava S, Syrjanen S, Collado MC, Rautava J. HPV Infection and Bacterial Microbiota in the Placenta, Uterine Cervix and Oral Mucosa. Sci Rep (2018) 8:11. doi: 10.1038/s41598-018-27980-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thorsteinsson K, Storgaard M, Katzenstein TL, Ladelund S, Ronsholt FF, Johansen IS, et al. Prevalence of Cervical, Oral, and Anal Human Papillomavirus Infection in Women Living With HIV in Denmark - The SHADE Cohort Study. J Clin Virol (2018) 105:64–71. doi: 10.1016/j.jcv.2018.05.010 [DOI] [PubMed] [Google Scholar]
- 22. Sohn AH, Kerr SJ, Hansudewechakul R, Gatechompol S, Chokephaibulkit K, Dang HLD, et al. Risk Factors for Human Papillomavirus Infection and Abnormal Cervical Cytology Among Perinatally Human Immunodeficiency Virus-Infected and Uninfected Asian Youth. Clin Infect Dis (2018) 67:606–13. doi: 10.1093/cid/ciy144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grimm D, Woelber L, Prieske K, Schmalfeldt B, Kurti S, Busch CJ, et al. Comparison of PapilloCheck and Linear Array to Detect and Differentiate Human Papillomaviruses in Cervical and Tonsillar Smears From Females With Cervical Intraepithelial Lesions. Eur J Microbiol Immunol (2018) 8:107–11. doi: 10.1556/1886.2018.00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cranston RD, Cespedes MS, Paczuski P, Yang M, Coombs RW, Dragavon J, et al. High Baseline Anal Human Papillomavirus and Abnormal Anal Cytology in a Phase 3 Trial of the Quadrivalent Human Papillomavirus Vaccine in Human Immunodeficiency Virus-Infected Individuals Older Than 26 Years: ACTG 5298. Sex Transm Dis (2018) 45:266–71. doi: 10.1097/olq.0000000000000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cossellu G, Fedele L, Badaoui B, Angiero F, Farronato G, Monti E, et al. Prevalence and Concordance of Oral and Genital HPV in Women Positive for Cervical HPV Infection and in Their Sexual Stable Partners: An Italian Screening Study. PloS One (2018) 13:e0205574. doi: 10.1371/journal.pone.0205574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Woelber L, Breuer J, Meyer T, Vettorazzi E, Prieske K, Bohlmann I, et al. Oral Human Papillomavirus in Women With High-Grade Cervical Intraepithelial Neoplasia. J Low Genit Tract Dis (2017) 21:177–83. doi: 10.1097/lgt.0000000000000313 [DOI] [PubMed] [Google Scholar]
- 27. Oliveira LH, Santos LS, Silva CO, Augusto EF, Neves FP. Papillomavirus Infections in the Oral and Genital Mucosa of Asymptomatic Women. Braz J Infect Dis (2017) 21:88–91. doi: 10.1016/j.bjid.2016.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ciccarese G, Herzum A, Rebora A, Drago F. Prevalence of Genital, Oral, and Anal HPV Infection Among STI Patients in Italy. J Med Virol (2017) 89:1121–4. doi: 10.1002/jmv.24746 [DOI] [PubMed] [Google Scholar]
- 29. Uken RB, Brummer O, von Schubert-Bayer C, Brodegger T, Teudt IU. Oral HPV Prevalence in Women Positive for Cervical HPV Infection and Their Sexual Partners: A German Screening Study. Eur Arch Otorhinolaryngol (2016) 273:1933–42. doi: 10.1007/s00405-016-3953-1 [DOI] [PubMed] [Google Scholar]
- 30. Temizkan O, Aydogan B, Sanverdi I, Sakiz D, Arici B, Karaca K, et al. Prevalence of Abnormal Oral Cytology and Impact of Sexual Behavior in Women With Abnormal Cervical Cytology. Clin Exp Obstet Gynecol (2016) 43:388–92. doi: 10.12891/ceog2158.2016 [DOI] [PubMed] [Google Scholar]
- 31. Loverro G, Di Naro E, Caringella AM, De Robertis AL, Loconsole D, Chironna M. Prevalence of Human Papillomavirus Infection in a Clinic Sample of Transsexuals in Italy. Sex Transm Infect (2016) 92:67–9. doi: 10.1136/sextrans-2014-051987 [DOI] [PubMed] [Google Scholar]
- 32. Kedarisetty S, Orosco RK, Hecht AS, Chang DC, Weissbrod PA, Coffey CS. Concordant Oral and Vaginal Human Papillomavirus Infection in the United States. JAMA Otolaryngology– Head Neck Surg (2016) 142:457–65. doi: 10.1001/jamaoto.2016.0064 [DOI] [PubMed] [Google Scholar]
- 33. Tatar TZ, Kis A, Szabo E, Czompa L, Boda R, Tar I, et al. Prevalence of Human Papillomaviruses in the Healthy Oral Mucosa of Women With High-Grade Squamous Intra-Epithelial Lesion and of Their Partners as Compared to Healthy Controls. J Oral Pathol Med (2015) 44:722–7. doi: 10.1111/jop.12302 [DOI] [PubMed] [Google Scholar]
- 34. Skoczynski M, Gozdzicka-Jozefiak A, Kwasniewska A. The Prevalence of Human Papillomavirus Between the Neonates and Their Mothers. BioMed Res Int (2015) 2015:126417. doi: 10.1155/2015/126417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grun N, Ahrlund-Richter A, Franzen J, Mirzaie L, Marions L, Ramqvist T, et al. Oral Human Papillomavirus (HPV) Prevalence in Youth and Cervical HPV Prevalence in Women Attending a Youth Clinic in Sweden, a Follow Up-Study 2013-2014 After Gradual Introduction of Public HPV Vaccination. Infect Dis (Lond) (2015) 47:57–61. doi: 10.3109/00365548.2014.964764 [DOI] [PubMed] [Google Scholar]
- 36. Brouwer AF, Eisenberg MC, Carey TE, Meza R. Trends in HPV Cervical and Seroprevalence and Associations Between Oral and Genital Infection and Serum Antibodies in NHANES 2003-2012. BMC Infect Dis (2015) 15:575. doi: 10.1186/s12879-015-1314-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Steinau M, Hariri S, Gillison ML, Broutian TR, Dunne EF, Tong ZY, et al. Prevalence of Cervical and Oral Human Papillomavirus Infections Among US Women. J Infect Dis (2014) 209:1739–43. doi: 10.1093/infdis/jit799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ribeiro CMB, Ferrer I, de Farias ABS, Fonseca D, Silva IHM, Gueiros LAM, et al. Oral and Genital HPV Genotypic Concordance Between Sexual Partners. Clin Oral Investig (2014) 18:261–8. doi: 10.1007/s00784-013-0959-6 [DOI] [PubMed] [Google Scholar]
- 39. Meyer MF, Huebbers CU, Siefer OG, Vent J, Engbert I, Eslick GD, et al. Prevalence and Risk Factors for Oral Human Papillomavirus Infection in 129 Women Screened for Cervical HPV Infection. Oral Oncol (2014) 50:27–31. doi: 10.1016/j.oraloncology.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 40. Mbulawa ZZ, Johnson LF, Marais DJ, Coetzee D, Williamson AL. Risk Factors for Oral Human Papillomavirus in Heterosexual Couples in an African Setting. J Infect (2014) 68:185–9. doi: 10.1016/j.jinf.2013.10.012 [DOI] [PubMed] [Google Scholar]
- 41. Lima MD, Braz-Silva PH, Pereira SM, Riera C, Coelho AC, Gallottini M. Oral and Cervical HPV Infection in HIV-Positive and HIV-Negative Women Attending a Sexual Health Clinic in Sao Paulo, Brazil. Int J Gynaecol Obstet (2014) 126:33–6. doi: 10.1016/j.ijgo.2014.01.017 [DOI] [PubMed] [Google Scholar]
- 42. Vogt SL, Gravitt PE, Martinson NA, Hoffmann J, D'Souza G. Concordant Oral-Genital HPV Infection in South Africa Couples: Evidence for Transmission. Front Oncol (2013) 3(303):1–7. doi: 10.3389/fonc.2013.00303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schlecht NF, Rojas M, Lorde-Rollins E, Nucci-Sack A, Strickler HD, Burk RD, et al. Burden of Cervical, Anal, and Oral HPV in an Inner-City Pre-Vaccine Adolescent Population. J Urban Health (2013) 90:141–6. doi: 10.1007/s11524-012-9756-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lang Kuhs KA, Gonzalez P, Struijk L, Castro F, Hildesheim A, van Doorn LJ, et al. Prevalence of and Risk Factors for Oral Human Papillomavirus Among Young Women in Costa Rica. J Infect Dis (2013) 208:1643–52. doi: 10.1093/infdis/jit369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Herrero R, Quint W, Hildesheim A, Gonzalez P, Struijk L, Katki HA, et al. Reduced Prevalence of Oral Human Papillomavirus (HPV) 4 Years After Bivalent HPV Vaccination in a Randomized Clinical Trial in Costa Rica. PloS One (2013) 8:e68329. doi: 10.1371/journal.pone.0068329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. da Mota Vasconcelos Brasil C, Ribeiro CMB, Leão JC. Oral and Genital Human Herpesvirus 8 and Human Papillomavirus in Heterosexual Partners. J Oral Pathol Med (2013) 42:61–5. doi: 10.1111/j.1600-0714.2012.01184.x [DOI] [PubMed] [Google Scholar]
- 47. Adamopoulou M, Vairaktaris E, Nkenke E, Avgoustidis D, Karakitsos P, Sioulas V, et al. Prevalence of Human Papillomavirus in Saliva and Cervix of Sexually Active Women. Gynecol Oncol (2013) 129:395–400. doi: 10.1016/j.ygyno.2013.02.015 [DOI] [PubMed] [Google Scholar]
- 48. Schlecht NF, Burk RD, Nucci-Sack A, Shankar V, Peake K, Lorde-Rollins E, et al. Cervical, Anal and Oral HPV in an Adolescent Inner-City Health Clinic Providing Free Vaccinations. PloS One (2012) 7:e37419. doi: 10.1371/journal.pone.0037419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Elasbali AM, El Din AHS, Abdallah RAH, Ahmed HG. Cervical and Oral Screening for HR-HPV Types 16 and 18 Among Sudanese Women Cervical Lesions. Infect Agents Cancer (2012) 7:6. doi: 10.1186/1750-9378-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Du J, Nordfors C, Ahrlund-Richter A, Sobkowiak M, Romanitan M, Nasman A, et al. Prevalence of Oral Human Papillomavirus Infection Among Youth, Sweden. Emerg Infect Dis (2012) 18:1468–71. doi: 10.3201/eid1809.111731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ragin C, Edwards R, Larkins-Pettigrew M, Taioli E, Eckstein S, Thurman N, et al. Oral HPV Infection and Sexuality: A Cross-Sectional Study in Women. Int J Mol Sci (2011) 12:3928–40. doi: 10.3390/ijms12063928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Matsushita K, Sasagawa T, Miyashita M, Ishizaki A, Morishita A, Hosaka N, et al. Oral and Cervical Human Papillomavirus Infection Among Female Sex Workers in Japan. Jpn J Infect Dis (2011) 64:34–9. [PubMed] [Google Scholar]
- 53. Kero K, Rautava J, Syrjanen K, Grenman S, Syrjanen S. Human Papillomavirus Genotypes in Male Genitalia and Their Concordance Among Pregnant Spouses Participating in the Finnish Family HPV Study. J Sex Med (2011) 8:2522–31. doi: 10.1111/j.1743-6109.2011.02378.x [DOI] [PubMed] [Google Scholar]
- 54. Crawford R, Grignon AL, Kitson S, Winder DM, Ball SL, Vaughan K, et al. High Prevalence of HPV in Non-Cervical Sites of Women With Abnormal Cervical Cytology. BMC Cancer (2011) 11:473. doi: 10.1186/1471-2407-11-473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Brown B, Blas MM, Cabral A, Carcamo C, Gravitt PE, Halsey N. Oral Sex Practices, Oral Human Papillomavirus and Correlations Between Oral and Cervical Human Papillomavirus Prevalence Among Female Sex Workers in Lima, Peru. Int J STD AIDS (2011) 22:655–8. doi: 10.1258/ijsa.2011.010541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Termine N, Giovannelli L, Matranga D, Perino A, Panzarella V, Ammatuna P, et al. Low Rate of Oral Human Papillomavirus (HPV) Infection in Women Screened for Cervical HPV Infection in Southern Italy: A Cross-Sectional Study of 140 Immunocompetent Subjects. J Med Virol (2009) 81:1438–43. doi: 10.1002/jmv.21509 [DOI] [PubMed] [Google Scholar]
- 57. Richter KL, van Rensburg EJ, van Heerden WF, Boy SC. Human Papilloma Virus Types in the Oral and Cervical Mucosa of HIV-Positive South African Women Prior to Antiretroviral Therapy. J Oral Pathol Med (2008) 37:555–9. doi: 10.1111/j.1600-0714.2008.00670.x [DOI] [PubMed] [Google Scholar]
- 58. Marais DJ, Passmore JA, Denny L, Sampson C, Allan BR, Williamson AL. Cervical and Oral Human Papillomavirus Types in HIV-1 Positive and Negative Women With Cervical Disease in South Africa. J Med Virol (2008) 80:953–9. doi: 10.1002/jmv.21166 [DOI] [PubMed] [Google Scholar]
- 59. Ragin CC, Wheeler VW, Wilson JB, Bunker CH, Gollin SM, Patrick AL, et al. Distinct Distribution of HPV Types Among Cancer-Free Afro-Caribbean Women From Tobago. Biomarkers (2007) 12:510–22. doi: 10.1080/13547500701340384 [DOI] [PubMed] [Google Scholar]
- 60. Passmore JA, Marais DJ, Sampson C, Allan B, Parker N, Milner M, et al. Cervicovaginal, Oral, and Serum IgG and IgA Responses to Human Papillomavirus Type 16 in Women With Cervical Intraepithelial Neoplasia. J Med Virol (2007) 79:1375–80. doi: 10.1002/jmv.20901 [DOI] [PubMed] [Google Scholar]
- 61. Nordin P, Hansson BG, Hansson C, Blohme I, Larko O, Andersson K. Human Papilloma Virus in Skin, Mouth and Uterine Cervix in Female Renal Transplant Recipients With or Without a History of Cutaneous Squamous Cell Carcinoma. Acta Derm Venereol (2007) 87:219–22. doi: 10.2340/00015555-0235 [DOI] [PubMed] [Google Scholar]
- 62. Smith EM, Ritchie JM, Yankowitz J, Wang D, Turek LP, Haugen TH. HPV Prevalence and Concordance in the Cervix and Oral Cavity of Pregnant Women. Infect Dis Obstet Gynecol (2004) 12:45–56. doi: 10.1080/10647440400009896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Canadas MP, Bosch FX, Junquera ML, Ejarque M, Font R, Ordonez E, et al. Concordance of Prevalence of Human Papillomavirus DNA in Anogenital and Oral Infections in a High-Risk Population. J Clin Microbiol (2004) 42:1330–2. doi: 10.1128/jcm.42.3.1330-1332.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Scala M, Bonelli G, Gipponi M, Margarino G, Muzza A. Cryosurgery Plus Adjuvant Systemic Alpha2-Interferon for HPV-Associated Lesions. Anticancer Res (2002) 22:1171–6. [PubMed] [Google Scholar]
- 65. Marais DJ, Best JM, Rose RC, Keating P, Soeters R, Denny L, et al. Oral Antibodies to Human Papillomavirus Type 16 in Women With Cervical Neoplasia. J Med Virol (2001) 65:149–54. doi: 10.1002/jmv.2014 [DOI] [PubMed] [Google Scholar]
- 66. Chatterjee R, Mukhopadhyay D, Murmu N, Jana S. Prevalence of Human Papillomavirus Infection Among Prostitutes in Calcutta. J Environ Pathol Toxicol Oncol (2001) 20:113–7. doi: 10.1615/JEnvironPatholToxicolOncol.v20.i2.50 [DOI] [PubMed] [Google Scholar]
- 67. Aaltonen LM, Auvinen E, Dillner J, Lehtinen M, Paavonen J, Rihkanen H, et al. Poor Antibody Response Against Human Papillomavirus in Adult-Onset Laryngeal Papillomatosis. J Med Microbiol (2001) 50:468–71. doi: 10.1099/0022-1317-50-5-468 [DOI] [PubMed] [Google Scholar]
- 68. Badaracco G, Venuti A, Di Lonardo A, Scambia G, Mozzetti S, Benedetti Panici P, et al. Concurrent HPV Infection in Oral and Genital Mucosa. J Oral Pathol Med (1998) 27:130–4. doi: 10.1111/j.1600-0714.1998.tb01928.x [DOI] [PubMed] [Google Scholar]
- 69. van Doornum GJ, Hooykaas C, Juffermans LH, van der Lans SM, van der Linden MM, Coutinho RA, et al. Prevalence of Human Papillomavirus Infections Among Heterosexual Men and Women With Multiple Sexual Partners. J Med Virol (1992) 37:13–21. doi: 10.1002/jmv.1890370104 [DOI] [PubMed] [Google Scholar]
- 70. Fakhry C, D'Souza G, Sugar E, Weber K, Goshu E, Minkoff H, et al. Relationship Between Prevalent Oral and Cervical Human Papillomavirus Infections in Human Immunodeficiency Virus-Positive and -Negative Women. J Clin Microbiol (2006) 44:4479–85. doi: 10.1128/JCM.01321-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Goncalves AK, Giraldo P, Barros-Mazon S, Gondo ML, Amaral RL, Jacyntho C. Secretory Immunoglobulin A in Saliva of Women With Oral and Genital HPV Infection. Eur J Obstet Gynecol Reprod Biol (2006) 124:227–31. doi: 10.1016/j.ejogrb.2005.06.028 [DOI] [PubMed] [Google Scholar]
- 72. Zonta MA, Monteiro J, Santos G, Jr., Pignatari AC. Oral Infection by the Human Papilloma Virus in Women With Cervical Lesions at a Prison in Sao Paulo, Brazil. Braz J Otorhinolaryngol (2012) 78:66–72. doi: 10.1590/S1808-86942012000200011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Beachler DC, Lang Kuhs KA, Struijk L, Schussler J, Herrero R, Porras C, et al. The Natural History of Oral Human Papillomavirus in Young Costa Rican Women. Sex Transm Dis (2017) 44:442–9. doi: 10.1097/olq.0000000000000625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kero K, Rautava J, Louvanto K, Syrjanen K, Grenman S, Syrjanen S. Genotype-Specific Concordance of Oral and Genital Human Papillomavirus Infections Among Marital Couples Is Low. Eur J Clin Microbiol Infect Dis (2016) 35:697–704. doi: 10.1007/s10096-016-2589-9 [DOI] [PubMed] [Google Scholar]
- 75. Menezes LJ, Poongulali S, Tommasino M, Lin HY, Kumarasamy N, Fisher KJ, et al. Prevalence and Concordance of Human Papillomavirus Infection at Multiple Anatomic Sites Among HIV-Infected Women From Chennai, India. Int J STD AIDS (2016) 27:543–53. doi: 10.1177/0956462415587226 [DOI] [PubMed] [Google Scholar]
- 76. Louvanto K, Rautava J, Syrjanen K, Grenman S, Syrjanen S. The Clearance of Oral High-Risk Human Papillomavirus Infection Is Impaired by Long-Term Persistence of Cervical Human Papillomavirus Infection. Clin Microbiol Infect (2014) 20:1167–72. doi: 10.1111/1469-0691.12700 [DOI] [PubMed] [Google Scholar]
- 77. Paaso AE, Louvanto K, Syrjanen KJ, Waterboer T, Grenman SE, Pawlita M, et al. Lack of Type-Specific Concordance Between Human Papillomavirus (HPV) Serology and HPV DNA Detection in the Uterine Cervix and Oral Mucosa. J Gen Virol (2011) 92:2034–46. doi: 10.1099/vir.0.032011-0 [DOI] [PubMed] [Google Scholar]
- 78. Van Doornum GJ, Prins M, Juffermans LH, Hooykaas C, van den Hoek JA, Coutinho RA, et al. Regional Distribution and Incidence of Human Papillomavirus Infections Among Heterosexual Men and Women With Multiple Sexual Partners: A Prospective Study. Genitourin Med (1994) 70:240–6. doi: 10.1136/sti.70.4.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kero KM, Rautava J, Syrjanen K, Kortekangas-Savolainen O, Grenman S, Syrjanen S. Stable Marital Relationship Protects Men From Oral and Genital HPV Infections. Eur J Clin Microbiol Infect Dis (2014) 33:1211–21. doi: 10.1007/s10096-014-2061-7 [DOI] [PubMed] [Google Scholar]
- 80. Sarkola ME, Grenman SE, Rintala MA, Syrjanen KJ, Syrjanen SM. Effect of Second Pregnancy on Maternal Carriage and Outcome of High-Risk Human Papillomavirus (HPV). Experience From the Prospective Finnish Family HPV Study. Gynecol Obstet Invest (2009) 67:208–16. doi: 10.1159/000209204 [DOI] [PubMed] [Google Scholar]
- 81. D'Souza G, Fakhry C, Sugar EA, Seaberg EC, Weber K, Minkoff HL, et al. Six-Month Natural History of Oral Versus Cervical Human Papillomavirus Infection. Int J Cancer (2007) 121:143–50. doi: 10.1002/ijc.22667 [DOI] [PubMed] [Google Scholar]
- 82. Rintala MA, Grenman SE, Puranen MH, Isolauri E, Ekblad U, Kero PO, et al. Transmission of High-Risk Human Papillomavirus (HPV) Between Parents and Infant: A Prospective Study of HPV in Families in Finland. J Clin Microbiol (2005) 43:376–81. doi: 10.1128/jcm.43.1.376-381.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital Human Papillomavirus Infection: Incidence and Risk Factors in a Cohort of Female University Students. Am J Epidemiol (2003) 157:218–26. doi: 10.1093/aje/kwf180 [DOI] [PubMed] [Google Scholar]
- 84. Mosmann JP, Zayas S, Kiguen AX, Venezuela RF, Rosato O, Cuffini CG. Human Papillomavirus and Chlamydia Trachomatis in Oral and Genital Mucosa of Women With Normal and Abnormal Cervical Cytology. BMC Infect Dis (2021) 21:422. doi: 10.1186/s12879-021-06118-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Paaso A, Koskimaa HM, Welters MJP, Kero K, Rautava J, Syrjänen K, et al. Interferon-γ and IL-5 Associated Cell-Mediated Immune Responses to HPV16 E2 and E6 Distinguish Between Persistent Oral HPV16 Infections and Noninfected Mucosa. Clin Exp Dent Res (2021) 7:903–13. doi: 10.1002/cre2.396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gilles C, Buljubasic M, Konopnicki D, Manigart Y, Barlow P, Rozenberg S. Cervical, Anal and Oral Human Papillomavirus (HPV) Infection in Young Women: A Case Control Study Between Women With Perinatally HIV Infection and Women With Non-Perinatally HIV Infection. Eur J Obstet Gynecol Reprod Biol (2020) 244:114–9. doi: 10.1016/j.ejogrb.2019.11.022 [DOI] [PubMed] [Google Scholar]
- 87. Nasioutziki M, Chatzistamatiou K, Loufopoulos PD, Vavoulidis E, Tsampazis N, Pratilas GC, et al. Cervical, Anal and Oral HPV Detection and HPV Type Concordance Among Women Referred for Colposcopy. Infect Agent Cancer (2020) 15:22. doi: 10.1186/s13027-020-00287-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Nemesio I, Cury F, Longatto-Filho A, Fregnani JH, Musselwhite L, Vazquez F, et al. Identification of Human Papillomavirus in Oral Rinse Specimens From Women With and Without Cervical Intraepithelial Lesions. Sex Transm Infect (2020) 96:408–10. doi: 10.1136/sextrans-2019-054359 [DOI] [PubMed] [Google Scholar]
- 89. Pérez-Quintanilla M, Méndez-Martínez R, Vázquez-Vega S, Espinosa-Romero R, Sotelo-Regil R, Pérez-Montiel MD, et al. High Prevalence of Human Papillomavirus and European Variants of HPV 16 Infecting Concomitantly to Cervix and Oral Cavity in HIV Positive Women. PloS One (2020) 15:e0227900. doi: 10.1371/journal.pone.0227900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sricharoenchai S, Kerr SJ, Gatechompol S, Hansudewechakul R, Dang HLD, Tran DNH, et al. Prevalence of High-Risk Nonavalent Vaccine-Type Human Papillomavirus Infection Among Unvaccinated, Sexually Active Asian Female Adolescents With and Without Perinatally Acquired HIV Infection. Pediatr Infect Dis J (2020) 39:615–9. doi: 10.1097/inf.0000000000002659 [DOI] [PubMed] [Google Scholar]
- 91. Suehiro TT, Damke G, Damke E, de Azevedo Ramos PLR, de Andrade Pereira Silva M, Pelloso SM, et al. Cervical and Oral Human Papillomavirus Infection in Women Living With Human Immunodeficiency Virus (HIV) and Matched HIV-Negative Controls in Brazil. Infect Agent Cancer (2020) 15:31. doi: 10.1186/s13027-020-00301-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Enerly E, Flingtorp R, Christiansen IK, Campbell S, Hansen M, Myklebust T, et al. An Observational Study Comparing HPV Prevalence and Type Distribution Between HPV-Vaccinated and -Unvaccinated Girls After Introduction of School-Based HPV Vaccination in Norway. PloS One (2019) 14:e0223612. doi: 10.1371/journal.pone.0223612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Tewari P, Banka P, Kernan N, Reynolds S, White C, Pilkington L, et al. Prevalence and Concordance of Oral HPV Infections With Cervical HPV Infections in Women Referred to Colposcopy With Abnormal Cytology. J Oral Pathol Med (2021) 50:692–9. doi: 10.1111/jop.13172 [DOI] [PubMed] [Google Scholar]
- 94. D'Souza G, Gross ND, Pai SI, Haddad R, Anderson KS, Rajan S, et al. Oral Human Papillomavirus (HPV) Infection in HPV-Positive Patients With Oropharyngeal Cancer and Their Partners. J Clin Oncol (2014) 32:2408–15. doi: 10.1200/jco.2014.55.1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Sánchez-Vargas LO, Díaz-Hernndez C, Martinez-Martinez A. Detection of Human Papilloma Virus (HPV) in Oral Mucosa of Women With Cervical Lesions and Their Relation to Oral Sex Practices. Infect Agents Cancer (2010) 5(25):1–6. doi: 10.1186/1750-9378-5-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kellokoski JK, Syrjänen SM, Chang F, Yliskoski M, Syrjänen KJ. Southern Blot Hybridization and PCR in Detection of Oral Human Papillomavirus (HPV) Infections in Women With Genital HPV Infections. J Oral Pathol Med (1992) 21:459–64. doi: 10.1111/j.1600-0714.1992.tb00975.x [DOI] [PubMed] [Google Scholar]
- 97. Premoli-De-Percoco G, Ramirez JL, Galindo I. Correlation Between HPV Types Associated With Oral Squamous Cell Carcinoma and Cervicovaginal Cytology - An in Situ Hybridization Study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod (1998) 86:77–81. doi: 10.1016/s1079-2104(98)90153-6 [DOI] [PubMed] [Google Scholar]
- 98. Saini R, Khim TP, Rahman SA, Ismail M, Tang TH. High-Risk Human Papillomavirus in the Oral Cavity of Women With Cervical Cancer, and Their Children. Virol J (2010) 7:131. doi: 10.1186/1743-422x-7-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Lupato V, Holzinger D, Hofler D, Menegaldo A, Giorgi Rossi P, Del Mistro A, et al. Prevalence and Determinants of Oral Human Papillomavirus Infection in 500 Young Adults From Italy. PloS One (2017) 12:e0170091. doi: 10.1371/journal.pone.0170091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Visalli G, Curro M, Facciola A, Riso R, Mondello P, Lagana P, et al. Prevalence of Human Papillomavirus in Saliva of Women With HPV Genital Lesions. Infect Agents Cancer (2016) 11:6. doi: 10.1186/s13027-016-0096-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Marques AE, Barra GB, de Resende Oyama CN, Guerra EN. Low Rate of Oropharyngeal Human Papillomavirus Infection of Women With Cervical Lesions and Their Partners: New Data From Brazilian Population. J Oral Pathol Med (2015) 44:453–8. doi: 10.1111/jop.12252 [DOI] [PubMed] [Google Scholar]
- 102. Rietbergen MM, van Bokhoven A, Lissenberg-Witte BI, Heideman DAM, Leemans CR, Brakenhoff RH, et al. Epidemiologic Associations of HPV-Positive Oropharyngeal Cancer and (Pre)Cancerous Cervical Lesions. Int J Cancer (2018) 143:283–8. doi: 10.1002/ijc.31315 [DOI] [PubMed] [Google Scholar]
- 103. Peixoto AP, Campos GS, Queiroz LB, Sardi SI. Asymptomatic Oral Human Papillomavirus (HPV) Infection in Women With a Histopathologic Diagnosis of Genital HPV. J Oral Sci (2011) 53:451–9. doi: 10.2334/josnusd.53.451 [DOI] [PubMed] [Google Scholar]
- 104. Christensen JT, Gronhoj C, Zamani M, Brask J, Kjaer EKR, Lajer H, et al. Association Between Oropharyngeal Cancers With Known HPV and P16 Status and Cervical Intraepithelial Neoplasia: A Danish Population-Based Study. Acta Oncol (2019) 58:267–72. doi: 10.1080/0284186x.2018.1546059 [DOI] [PubMed] [Google Scholar]
- 105. Sánchez-Siles M, Remezal-Solano M, López-López AM, Camacho-Alonso F. Prevalence of Human Papillomavirus in the Saliva of Sexually Active Women With Cervical Intraepithelial Neoplasias. Med Oral Patol Oral Cir Bucal (2020) 25:e195–204. doi: 10.4317/medoral.23300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Chaturvedi AK, Engels EA, Gilbert ES, Chen BE, Storm H, Lynch CF, et al. Second Cancers Among 104,760 Survivors of Cervical Cancer: Evaluation of Long-Term Risk. J Natl Cancer Inst (2007) 99:1634–43. doi: 10.1093/jnci/djm201 [DOI] [PubMed] [Google Scholar]
- 107. Chaturvedi AK, Kleinerman RA, Hildesheim A, Gilbert ES, Storm H, Lynch CF, et al. Second Cancers After Squamous Cell Carcinoma and Adenocarcinoma of the Cervix. J Clin Oncol (2009) 27:967–73. doi: 10.1200/JCO.2008.18.4549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Chen CY, Lai CH, Lee KD, Huang SH, Dai YM, Chen MC. Risk of Second Primary Malignancies in Women With Cervical Cancer: A Population-Based Study in Taiwan Over a 30-Year Period. Gynecol Oncol (2012) 127:625–30. doi: 10.1016/j.ygyno.2012.09.004 [DOI] [PubMed] [Google Scholar]
- 109. Ebisch RMF, Rutten DWE, IntHout J, Melchers WJG, Massuger LFAG, Bulten J, et al. Long-Lasting Increased Risk of Human Papillomavirus–Related Carcinomas and Premalignancies After Cervical Intraepithelial Neoplasia Grade 3: A Population-Based Cohort Study. J Clin Oncol (2017) 35:2542–50. doi: 10.1200/JCO.2016.71.4543 [DOI] [PubMed] [Google Scholar]
- 110. Gaudet M, Hamm J, Aquino-Parsons C. Incidence of Ano-Genital and Head and Neck Malignancies in Women With a Previous Diagnosis of Cervical Intraepithelial Neoplasia. Gynecol Oncol (2014) 134:523–6. doi: 10.1016/j.ygyno.2014.07.088 [DOI] [PubMed] [Google Scholar]
- 111. Hemminki K, Dong C, Frisch M. Tonsillar and Other Upper Aerodigestive Tract Cancers Among Cervical Cancer Patients and Their Husbands. Eur J Cancer Prev (2000) 9:433–7. doi: 10.1097/00008469-200012000-00010 [DOI] [PubMed] [Google Scholar]
- 112. Hemminki K, Jiang Y, Dong C. Second Primary Cancers After Anogenital, Skin, Oral, Esophageal and Rectal Cancers: Etiological Links? Int J Cancer (2001) 93:294–8. doi: 10.1002/ijc.1319 [DOI] [PubMed] [Google Scholar]
- 113. Jung YS, Lim J, Jung KW, Ryu J, Won YJ. Metachronous Second Primary Malignancies After Head and Neck Cancer in a Korean Cohort (1993-2010). PloS One (2015) 10:e0134160. doi: 10.1371/journal.pone.0134160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Neumann F, Jegu J, Mougin C, Pretet JL, Guizard AV, Lapotre-Ledoux B, et al. Risk of Second Primary Cancer After a First Potentially-Human Papillomavirus-Related Cancer: A Population-Based Study. Prev Med (2016) 90:52–8. doi: 10.1016/j.ypmed.2016.06.041 [DOI] [PubMed] [Google Scholar]
- 115. Papatla K, Halpern MT, Hernandez E, Brown J, Benrubi D, Houck K, et al. Second Primary Anal and Oropharyngeal Cancers in Cervical Cancer Survivors. Am J Obstet Gynecol (2019) 221:478.e1–6. doi: 10.1016/j.ajog.2019.05.025 [DOI] [PubMed] [Google Scholar]
- 116. Rose Ragin CC, Taioli E. Second Primary Head and Neck Tumor Risk in Patients With Cervical Cancer–SEER Data Analysis. Head Neck (2008) 30:58–66. doi: 10.1002/hed.20663 [DOI] [PubMed] [Google Scholar]
- 117. Suk R, Mahale P, Sonawane K, Sikora AG, Chhatwal J, Schmeler KM, et al. Trends in Risks for Second Primary Cancers Associated With Index Human Papillomavirus-Associated Cancers. JAMA Netw Open (2018) 1:13. doi: 10.1001/jamanetworkopen.2018.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Svahn MF, Munk C, Jensen SM, von Buchwald C, Frederiksen K, Kjaer SK. Risk of Head-and-Neck Cancer Following a Diagnosis of Severe Cervical Intraepithelial Neoplasia: A Nationwide Population-Based Cohort Study in Denmark. Gynecol Oncol (2016) 142:128–32. doi: 10.1016/j.ygyno.2016.04.023 [DOI] [PubMed] [Google Scholar]
- 119. Skinner HD, Sturgis EM, Klopp AH, Ang KK, Rosenthal DI, Garden AS, et al. Clinical Characteristics of Patients With Multiple Potentially Human Papillomavirus-Related Malignancies. Head Neck (2014) 36:819–25. doi: 10.1002/hed.23379 [DOI] [PubMed] [Google Scholar]
- 120. Gan SJ, Dahlstrom KR, Peck BW, Caywood W, Li G, Wei Q, et al. Incidence and Pattern of Second Primary Malignancies in Patients With Index Oropharyngeal Cancers Versus Index Nonoropharyngeal Head and Neck Cancers. Cancer (2013) 119:2593–601. doi: 10.1002/cncr.28107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Biron VL, Cote DW, Seikaly H. Oropharyngeal Squamous Cell Carcinoma and Human Papillomavirus-Associated Cancers in Women: Epidemiologic Evaluation of Association. J Otolaryngol Head Neck Surg (2011) 40 Suppl 1:S65–9. [PubMed] [Google Scholar]
- 122. Holstead R, Rasul R, Golden A, Kamdar D, Ghaly M, Teckie S, et al. Identifying Patterns of Failure and Secondary Primary Malignancies in HPV-Related Oropharyngeal Squamous Cell Carcinomas. Future Oncol (2020) 16:199–207. doi: 10.2217/fon-2019-0673 [DOI] [PubMed] [Google Scholar]
- 123. Larish A, Yin L, Glaser G, Moore E, Bakkum-Gamez J, Routman D, et al. Human Papillomavirus-Associated Anogenital Pathology in Females With HPV-Positive Oropharyngeal Squamous Cell Carcinoma. Otolaryngol Head Neck Surg (2021) 164:369–74. doi: 10.1177/0194599820941499 [DOI] [PubMed] [Google Scholar]
- 124. Loopik DL, Ebisch RM, IntHout J, Melchers WJ, Massuger LF, Bekkers RL, et al. The Relative Risk of Noncervical High-Risk Human Papillomavirus-Related (Pre)Malignancies After Recurrent Cervical Intraepithelial Neoplasia Grade 3: A Population-Based Study. Int J Cancer (2020) 147:897–900. doi: 10.1002/ijc.32834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Preti M, Rosso S, Micheletti L, Libero C, Sobrato I, Giordano L, et al. Risk of HPV-Related Extra-Cervical Cancers in Women Treated for Cervical Intraepithelial Neoplasia. BMC Cancer (2020) 20:972. doi: 10.1186/s12885-020-07452-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Wang M, Sharma A, Osazuwa-Peters N, Simpson MC, Schootman M, Piccirillo JF, et al. Risk of Subsequent Malignant Neoplasms After an Index Potentially-Human Papillomavirus (HPV)-Associated Cancers. Cancer Epidemiol (2020) 64:101649. doi: 10.1016/j.canep.2019.101649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Gazzaz MJ, Jeffery C, O'Connell D, Harris J, Seikaly H, Biron V. Association of Human Papillomavirus Related Squamous Cell Carcinomas of the Oropharynx and Cervix. Papillomavirus Res (2019) 8:100188. doi: 10.1016/j.pvr.2019.100188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Rogers NL, Cole SA, Lan HC, Crossa A, Demerath EW. New Saliva DNA Collection Method Compared to Buccal Cell Collection Techniques for Epidemiological Studies. Am J Hum Biol (2007) 19:319–26. doi: 10.1002/ajhb.20586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Kim KY, Lewis JS, Jr., Chen Z. Current Status of Clinical Testing for Human Papillomavirus in Oropharyngeal Squamous Cell Carcinoma. J Pathol Clin Res (2018) 4:213–26. doi: 10.1002/cjp2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Sasagawa T, Minemoto Y, Basha W, Yamazaki H, Nakamura M, Yoshimoto H, et al. A New PCR-Based Assay Amplifies the E6-E7 Genes of Most Mucosal Human Papillomaviruses (HPV). Virus Res (2000) 67:127–39. doi: 10.1016/s0168-1702(00)00137-4 [DOI] [PubMed] [Google Scholar]
- 131. Gravitt PE, Peyton CL, Alessi TQ, Wheeler CM, Coutlée F, Hildesheim A, et al. Improved Amplification of Genital Human Papillomaviruses. J Clin Microbiol (2000) 38:357–61. doi: 10.1128/JCM.38.1.357-361.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Melbye M, Palefsky J, Gonzales J, Ryder LP, Nielsen H, Bergmann O, et al. Immune Status as a Determinant of Human Papillomavirus Detection and its Association With Anal Epithelial Abnormalities. Int J Cancer (1990) 46:203–6. doi: 10.1002/ijc.2910460210 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.