Abstract
Since diabetes was first described over 3,000 years ago, clinicians and scientists alike have sought ever improving treatments en route to a cure. As we approach the 100th anniversary of insulin’s first therapeutic use, this article will recount the glorious history associated with research surrounding insulin’s isolation, purification, cloning, and subsequent modification. The discovery path we will relate tells the story of many relentless and passionate investigators pursuing ground-breaking research. The fruits of their labor include several Nobel Prizes, new technology, and, more importantly, ever improving treatments for one of humankind’s greatest medical scourges.
The Path to Insulin’s Discovery
Diabetes has plagued humans for millennia. The earliest reference may be found in Ebers papyrus, an Egyptian medical text written around 1550 BC, which gives a prescription for “the too great emptying of the urine.” Later, Aretaeus, an ancient Greek physician, described the disease as “a melting down of the flesh and bones into urine as though the aqueducts were opened wide … in whom thirst is extreme, mouth parched, body dry, and wasting progressive.” Aretaeus gave diabetes its name, which literally means “to pass through” (1).
As centuries and millennia passed, many small advances were made toward understanding the cause of diabetes, the most obvious being the recognition by many that the urine of those with diabetes tasted sweet. In 1815, Chevreul identified the cause of sweet urine to be a buildup of glucose, and diabetes research burst forth in earnest (2). In 1869, a German medical student, Paul Langerhans, discovered “islands” of tissue that differed from surrounding pancreatic tissue. These “islands” now bear his name, the islets of Langerhans (3). In 1889, Joseph von Mering and Oskar Minkowski proposed that the pancreas produced an external secretion aiding in digestion and an internal secretion controlling sugar equilibrium (4). In 1901, Eugene Opie from Johns Hopkins University reported evidence suggesting that the islets of Langerhans were the source of this internal secretion (5). These discoveries led many to attempt isolation of the mysterious internal secretion. Success depended on extracting scanty amounts of insulin from a sea of enzymatic tissue, a dilemma causing many to fail (2).
“Starvation” therapy became a mainstay for patients with diabetes near the turn of the twentieth century. Physicians like Allen and Joslin, and many others, noted that patients survived longer on restricted diets. To reduce carbohydrate content, Allen prescribed “thrice boiled vegetables” to his patients. He described diabetes treatment prior to 1912 as a “big, blooming, buzzing confusion,” and also wrote, “When there is deep seated damage to the pancreas, this can no more be cured by some magic herb than can a deformed limb” (6). Dr. Elliot P. Joslin was the first physician to specialize in diabetes. He is remembered for his meticulous record keeping and prolific writing. He would famously say, “Teaching is cheaper than nursing,” and he pioneered diabetes self-management education. He practiced a tireless 64 years in Boston from 1898 to 1962 and was perhaps the best eyewitness of the transmutation of diabetes (7). The austere and devoted guidance of physicians such as Allen and Joslin allowed many patients with diabetes to survive long enough for a miracle (8).
Banting, Best, Macleod, and Collip
On Saturday evening, 30 October 1920, while preparing a carbohydrate lecture for Ontario’s Western University, Frederick Banting read Moses Barron’s article, “The Relation of the Islets of Langerhans to Diabetes with Special Reference to Cases of Pancreatic Lithiasis” (9). Since physicians of the era were treating other hormone deficiencies, e.g., hypothyroidism, with animal thyroid extract, Banting was aware that similar attempts to treat diabetes with animal pancreatic extracts had failed. The common wisdom was that the pancreatic “internal secretion” was simply destroyed by the other pancreatic products, i.e., the digestive enzymes. Barron described autopsy findings that when stones obstruct the pancreatic duct to induce severe pancreatitis, those surviving the insult are left with islet tissue intact but that much of the exocrine tissue had degenerated. Banting’s thoughts raced for much of the night, and he awoke at 2:00 a.m. on 31 October 1920 inspired with an idea. That night he wrote in his notebook: “Diabetus - Ligate pancreatic ducts of dog. Keep dogs alive till acini degenerate leaving islets. Try to isolate the internal secretion of these to relieve glycosurea” (8). (The misspelled words “diabetus” and “glycosurea” are as Banting wrote them.)
Oblivious of those who had failed before him, Banting enthusiastically met J.J.R. Macleod, an expert in glucose metabolism at the University of Toronto, asking for support. Macleod was doubtful of the project but conceded a small lab space, some dogs, and a biochemistry student, Charles Best, to help begin the summer experiments. An uncomfortably hot lab, difficult surgeries, and flies only made the work more difficult. Many dogs died of infection, and among the survivors only a few ligations worked. Banting and Best endured disappointment, grueling work, and many setbacks. Their undaunted determination began to pay off when, on 30 July 1921, their islet-enriched pancreatic extract decreased the blood glucose of a diabetic dog. Professor Macleod was encouraged by their results and recruited a talented biochemist, James Collip, to aid in purifying the extract. The still impure insulin solutions, which took great time and effort to produce, were first tested on Leonard Thompson, a near-death 14-year-old boy whose appearance resembled a living skeleton. The first insulin injection, on 11 January 1922, recorded in Thompson’s medical record as “15 cc McCleod’s serum, 7 1/2 cc into each buttock” (with McLeod misspelled; Banting was not the best at that skill) resulted 1 week later in an “area of induration- circular- 7 1/2 cm in diameter- over the left buttock- center incised & softened.” Fortunately, on 23 January 1922, Leonard received the first of a series of shots (insulin with greater purity using a crystallization method Collip had worked out) that brought him back to health.
The Nobel Prize in Physiology or Medicine was awarded to Banting and Macleod on 26 February 1923 for their discovery of insulin. The magnitude of the discovery is symbolized by the fact that no other Nobel Prize has been awarded so promptly after a scientific advance. Banting shared half of his prize with Best, and Macleod, following suit, shared half of his prize with Collip. Thanks to the vested interest of Eli Lilly and the Connaught Laboratory in Toronto, insulin production became commercial and shortly thereafter was being used to treat diabetes around the world (10). See Fig. 1.
Figure 1.
Such was the infighting that developed among the four principal participants contributing to insulin’s first purification and use that no known photographs of the group exist. The closest to a group picture was taken in Victoria, Canada, on 25 June 1936. Shown are J.B. Collip, C.H. Best, F.N.G. Starr (widow of a Founding Fellow of the American College of Surgeons), and F.G. Banting. Numerous stories detailed in The Discovery of Insulin describe the many bitter disputes, prompting Lewellys Barker, a Canadian professor of medicine at Johns Hopkins University, to state at the 1923 dinner to celebrate the announcement of the Toronto group’s Nobel recognition that “in insulin, there is glory enough for all” (8). That sage counsel was not adopted by the protagonists. Photo credit: https://insulin.library.utoronto.ca/islandora/object/insulin%3AP10049.
Basic Research Advances
In the early 1920s, George Walden, working for Eli Lilly, and P.A. Shaffer, with Washington University’s School of Medicine, each independently developed isoelectric precipitation as a method for purifying insulin that has been used since. In 1935, H.C. Hagedorn and his associates found that adding protamine to insulin lengthened its duration, and, in 1936, D.A. Scott and A.M. Fisher showed that adding zinc did the same. These discoveries brought about neutral protamine Hagedorn insulin (NPH) and lente insulin, respectively, both of which improved glucose management for patients with diabetes starting in the early 1950s.
For patients with diabetes, insulin held the key to life, but for researchers it became a tool of discovery. As one of the first purified proteins available to the public, insulin fueled the work of three additional Nobel Prize discoveries. In 1958, Frederick Sanger received the prize in chemistry for determining the amino acid sequence of insulin. In 1964, Dorothy Hodgkin received the prize in chemistry for her contribution to the field of structural chemistry. Her capstone achievement was discerning the structure of insulin 5 years later. Most recently, Rosalyn Yalow received the 1977 prize in medicine/physiology for developing the radioimmunoassay (RIA) to measure insulin.
Hodgkin
Identifying the structure of insulin was Dorothy Hodgkin’s “north star” (11). Hodgkin’s lifelong study of insulin began in 1934 when the very first X-ray photographs of tiny insulin crystals were taken. In her words, it was “probably the most exciting moment in my life.” Thereafter, in the age before computers, she worked tirelessly over several years concluding that insulin (and other globulin proteins) conserved its three-dimensional structure, regardless of crystalline or soluble state. Since solving the full insulin structure was far beyond the technical capabilities at the time, she successfully identified the structure of penicillin and vitamin B12 in 4 and 8 years respectively. Her other works include determining the structures of cholesterol, lactoglobulin, ferritin, and tobacco mosaic virus. However, through all these years, she never lost faith that the structure of insulin would one day be solved. With the help of technical advances in the 1950s and 1960s, and a consortium of colleagues, the structure of insulin was finally revealed to the world in 1969—35 years after Hodgkin had taken the first X-ray photographs of the crystals (12). Dorothy Hodgkin was awarded the Nobel Prize in Chemistry in 1964 for the determination of the structures of penicillin and vitamin B12—and yet the work was inspired by insulin.
Yalow and Berson
The earliest method of measuring insulin relied on injecting insulin into animals and waiting for them to become hypoglycemic—a method far too imprecise for clinical use (13). Measuring insulin at physiological levels came with the advent of the RIA, a method that transformed the field of endocrinology.
Rosalyn Yalow and Solomon Berson, both from immigrant families in New York and educated in public schools, were extremely stubborn and bright. Yalow was the only woman in her class of 400 at The College of Engineering at University of Illinois, where she received master’s and doctoral degrees in nuclear physics (14). In her Nobel autobiography she wrote about her determination: “Through the years my mother has told me that it was fortunate that I chose to do acceptable things, for if I had chosen otherwise no one could have deflected me from my path” (15). Berson would claim that he received 109 medical school application rejection letters before finally being admitted to New York University’s School of Medicine, where he graduated at the top of his class (16). Neither of them had any formal postgraduate training in investigation, but they worked together successfully for 22 years, using radioisotopes to study blood volume, the effect of blood volume expanders, thyroid disease, and kinetics of iodine metabolism.
Using iodine-labeled insulin, Yalow and Berson noticed psychiatric ward patients who had previously received insulin (as a treatment for depression by inducing hypoglycemic seizures) cleared radioactivity slower than their counterparts. They concluded that an insulin-binding globulin or insulin-binding antibodies were responsible for this phenomenon. Their first manuscript, which laid the groundwork for developing the RIA, was initially rejected in 1955 by both Science and the Journal of Clinical Investigation. Reviewers could not believe a peptide as small as insulin could induce antibody formation. Undeterred, the pair soon realized they could use anti-insulin antibodies as the basis for a sensitive and specific assay. By adding a fixed amount of radiolabeled insulin to patient samples and watching how much bound to antibody, they could determine serum insulin levels. They received no resistance from reviewers when the landmark 1960 article “Immunoassay of Endogenous Plasma Insulin in Man” was submitted—it remains one of the most cited articles in Journal of Clinical Investigation history (14,16). The Nobel citation for Dr. Yalow reads, “Her methodology … made [a] triumphant journey far beyond her own field of research,” and went on, “Rarely have so many had so few to thank for so much.” Unfortunately, Berson died 5 years before the announcement of the 1977 Nobel Prize.
Sanger
When Frederick Sanger began his work on insulin, it was well-known that proteins had different amino acid compositions, activities, and properties. It was postulated by Francis Crick and others that genes had an important role in regulation of proteins, but the definitive link was missing (17). Sanger developed a method for sequencing a protein’s amino acid composition, and in 1955, insulin became the first to reveal its secret (18). Not only did Sanger’s success lead to sequencing many other proteins, but also his description that each protein has a unique, well-defined arrangement of amino acids provided circumstantial evidence for a genetic code. Sanger would later go on to develop techniques to sequence DNA and RNA.
This modest scientist wrote in his memoir, “Of the three main activities involved in scientific research, thinking, and talking, and doing, I much prefer the last and am probably best at it. I am all right at thinking but not much good at the talking. … Unlike most of my scientific colleagues, I was not academically brilliant” (19). The Nobel Prize selection committee recognized his brilliance twice, first in 1958 for “his work on the structure of proteins, especially that of insulin” and then in 1980 (chemistry) “for their [with Walter Gilbert] contributions concerning the determination of base sequences in nucleic acids.”
Molecular Biology Revolution
Until the 1980s, consumer insulin had been isolated and purified from beef or pork pancreas. Sources were finite, and the demands were steadily increasing. Concerned, Eli Lilly held a conference in May of 1976 to discuss the issue. Three separate groups left the conference aspiring to clone human insulin (20). Programming bacteria to express the protein product from a foreign gene had never been done before. It would require inserting a foreign DNA into a bacterium and coercing it to turn it into protein. Three teams raced to be the first: a group of researchers from the University of California, San Francisco (UCSF), headed by Howard Goodman and William Rutter, a group from Harvard University headed by Walter Gilbert, and a group from Genentech/City of Hope headed by Herbert Boyer, Arthur Riggs, and Keiichi Itakura. The groups from Harvard and UCSF overcame hurdles to isolate insulin mRNA, which they used as a template to make complimentary DNA, but the Genentech/City of Hope group synthesized their DNA from scratch. While the Genentech/City of Hope’s innovative method faced several hurdles recently described (21), the approach ultimately allowed them to win the race and usher in the generation of recombinant DNA technology (22) (Fig 2). The groundwork laid by these groups is the basis for countless molecular feats including designer insulins that have gained wide commercial use today (20). In fact, with insulin leading the way, the work led to the biopharmaceutical industry of today with giants like Genentech, Biogen, and Amgen and countless others generating biological proteins for therapeutic use.
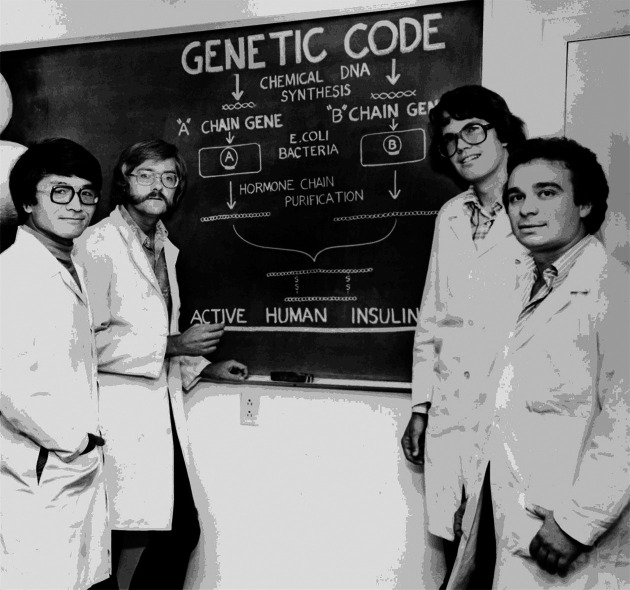
Figure 2.
The Genentech/City of Hope team that created artificial human insulin genes (A and B chains), inserted those constructs into bacteria, and then successfully created human insulin manufactured in a bacterial system. Shown left to right are K. Itakura, A. Riggs, D. Goeddel, and R. Crea (who worked with several others not shown). The work launched the biopharmaceutical industry and has provided countless benefits not only to those with diabetes but also to many others worldwide treated with other bioengineered proteins. And unlike the Toronto group, the Genentech/City of Hope team avoided the internal rancor. Photo reproduced with permission from the City of Hope.
The advent of recombinant human insulin resolved the problems of insulin shortage and immunogenicity, but the pharmacokinetic profile was still not ideal. There are many differences between the delivery of insulin from a healthy pancreas and the delivery of insulin from subcutaneous injection. Insulin produced by β-cells reaches the blood quickly and has a short duration of action. While fasting, blood insulin levels remain at a low basal rate, but after meals insulin levels quickly rise, keeping glucose levels within a narrow range. Subcutaneous regular insulin takes 15–30 min before producing an effect and wears off in a couple of hours. On the other hand, “basal” insulins last longer, but most still have a peak and are not well suited to mimic basal insulin levels. In an effort to resolve these differences, researchers have developed various short-acting and long-duration peak-less “designer” insulins in widespread use today. These insulins have subtle amino acid changes that change the way they are absorbed and can be made to act within minutes or last up to 24 h (23,24). And research into novel designer insulin molecules with better kinetics, the potential for glucose-responsive activity (25), and/or greater thermal resistance continues to be actively pursued.
Since they were developed in the late 1970s, insulin pumps offer a versatile alternative to long-acting basal insulins and have gained popularity among those with type 1 diabetes (26). Around the same time, home glucose monitors became available, and over the years they have gotten smaller and smarter. Subcutaneous glucose sensors are now widely used to provide real-time glucose readings, with semiclosed loop (insulin pump and glucose sensor) systems now gaining popularity with updates occurring with gratifying speed (27).
Increasing Respect for the β-Cell
And yet, designer insulins, insulin pumps, and real-time glucose sensors combined still do not provide glucose control comparable with that provided by β-cells. Insulin therapy causes hypoglycemia and other quality of life issues. Many have therefore focused on transplanting pancreatic islets to replace this population of endocrine cells. Islet transplants can abolish hyperglycemia and hypoglycemia and perhaps reverse complications whose pathogenesis is not yet well understood. Unfortunately, most islet transplants fail within a few years and the incumbent immunosuppressive medications have risks of their own (28). And to overcome the limited supply of pancreatic islets from cadaveric donors, many are now engaged in research to develop animal islets, e.g., from genetically manipulated pigs (29) or from induced pluripotent human stem cells (30) then genetically modified to resist immune destruction (31).
The paramount aim must be to prevent diabetes or cure it after it develops. Research focusing on the pathogenesis of both type 1 and type 2 diabetes will hopefully yield much needed insight.
As we rapidly approach the 100-year anniversary of the first insulin injection into a human being, many excellent reviews of the subject have recently been published (32–34). Insulin’s glorious story weaves together brilliance, serendipity, determination, unforeseen consequences, and countless people whose experiences lie on both sides of the needle. In Banting’s Nobel lecture, he stated, “Insulin is not a cure for diabetes; it is a treatment. It enables the diabetic to burn sufficient carbohydrates, so that proteins and fats may be added to the diet in sufficient quantities to provide energy for the economic burdens of life” (35). On 7 July 1980, Her Majesty Queen Elizabeth, The Queen Mother, lit the “Flame of Hope” just outside what was then Sir Frederick Banting’s London, Ontario, home and office where he awoke on 31 October 1920 with his idea to purify insulin (Fig. 3). It is no mistake that it is called the Flame of Hope and not an eternal flame, since the group that cures type 1 diabetes will be granted the great privilege of extinguishing the flame. Insulin’s noble saga continues, yet it begs us all to write its final chapter.
Figure 3.
Where it all began, and where it will end at some future date. One of this article’s authors (D.M.H.) at Banting’s London, Ontario, home where he awoke with his inspired dream, and where that dream can reach its goal when the Flame of Hope is extinguished.
Article Information
Acknowledgments. The authors acknowledge most informative discussions through the years with Grant Maltman, Curator of the Banting House National Historic Site; Michael Bliss (now deceased), author of The Discovery of Insulin; Stephen S. Hall, Arthur L. Carter Journalism Institute, NYU, author of Invisible Frontiers; and countless others who have shared stories of insulin’s remarkable history.
Funding. This piece was initiated when the authors were all supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health (NIH), and the Clinical Center, NIH, and was updated with funding support from NIH grants UC4DK116284-03 and U01DK104218-03, and by JDRF 5-COE-2020-967-M-N.
This article was written in a personal capacity and does not represent the opinions of the U.S. Food and Drug Administration, the Department of Health and Human Services, or the federal government.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Footnotes
References
- 1. Marwood SF. Diabetes mellitus--some reflections. J R Coll Gen Pract 1973;23:38–45 [PMC free article] [PubMed] [Google Scholar]
- 2. Raju TN. A mysterious something: the discovery of insulin and the 1923 Nobel Prize for Frederick G. Banting (1891-1941) and John J.R. Macleod (1876-1935). Acta Paediatr 2006;95:1155–1156 [DOI] [PubMed] [Google Scholar]
- 3. Sakula A. Paul Langerhans (1847-1888): a centenary tribute. J R Soc Med 1988;81:414–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Von Mering JMO. Diabetes mellitus nach Pankreasexstirpation. Naunyn Schmiedebergs Arch Exp Pathol Pharmakol 1890;26:371–387 [Google Scholar]
- 5. Opie EL. The relation oe diabetes mellitus to lesions of the pancreas. Hyaline degeneration of the islands oe Langerhans. J Exp Med 1901;5:527–540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allen MF. Diabetes and Its Treatment. New York, NY, Funk and Wagnalls Company, 1928 [Google Scholar]
- 7. Feudtner C. Bitter Sweet. Chapel Hill, NC, The University of North Carolina Press, 2003 [Google Scholar]
- 8. Bliss M. The Discovery of Insulin. Chicago, IL, University of Chicago Press, 1982 [Google Scholar]
- 9. Barron M. The relation of the islets of Langerhans to diabetes with special reference to cases of pancreatic lithiasis. Surg Gynecol Obstet 1920;31:437–448 [Google Scholar]
- 10. Discovery of insulin. Can Med Assoc J 1971;105:895–896 [PMC free article] [PubMed] [Google Scholar]
- 11. Howard JA. Dorothy Hodgkin and her contributions to biochemistry. Nat Rev Mol Cell Biol 2003;4:891–896 [DOI] [PubMed] [Google Scholar]
- 12. Blundell TL, Cutfield JF, Cutfield SM, et al. Atomic positions in rhombohedral 2-zinc insulin crystals. Nature 1971;231:506–511 [DOI] [PubMed] [Google Scholar]
- 13. Yalow RS, Berson SA. Immunoassay of endogenous plasma insulin in man. J Clin Invest 1960;39:1157–1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Friedman A. Remembrance: the Berson and Yalow saga. J Clin Endocrinol Metab 2002;87:1925–1928 [DOI] [PubMed] [Google Scholar]
- 15. Yalow RS. Radioimmunoassay: a probe for fine structure of biological systems, 1977. Accessed 26 September 2021. Available from https://www.nobelprize.org/prizes/medicine/1977/yalow/biographical/ [PubMed]
- 16. Kahn CR, Roth J. Berson, Yalow, and the JCI: the agony and the ecstasy. J Clin Invest 2004;114:1051–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stretton AO. The first sequence. Fred Sanger and insulin. Genetics 2002;162:527–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brown H, Sanger F, Kitai R. The structure of pig and sheep insulins. Biochem J 1955;60:556–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sanger F. Sequences, sequences, and sequences. Annu Rev Biochem 1988;57:1–28 [DOI] [PubMed] [Google Scholar]
- 20. Hall S. Invisible Frontiers. New York, NY, Oxford University Press, 1987 [Google Scholar]
- 21. Riggs AD. Making, cloning, and the expression of human insulin genes in bacteria: the path to Humulin. Endocr Rev 2021;42:374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goeddel DV, Kleid DG, Bolivar F, et al. Expression in Escherichia coli of chemically synthesized genes for human insulin. Proc Natl Acad Sci U S A 1979;76:106–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sharma AK, Taneja G, Kumar A, et al. Insulin analogs: glimpse on contemporary facts and future prospective. Life Sci 2019;219:90–99 [DOI] [PubMed] [Google Scholar]
- 24. Hirsch IB, Juneja R, Beals JM, Antalis CJ, Wright EE. The evolution of insulin and how it informs therapy and treatment choices. Endocr Rev 2020;41:733–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rege NK, Phillips NFB, Weiss MA. Development of glucose-responsive ‘smart’ insulin systems. Curr Opin Endocrinol Diabetes Obes 2017;24:267–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pickup J, Keen H. Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care 2002;25:593–598 [DOI] [PubMed] [Google Scholar]
- 27. Perkins BA, Sherr JL, Mathieu C. Type 1 diabetes glycemic management: insulin therapy, glucose monitoring, and automation. Science 2021;373:522–527 [DOI] [PubMed] [Google Scholar]
- 28. Bellin MD, Dunn TB. Transplant strategies for type 1 diabetes: whole pancreas, islet and porcine beta cell therapies. Diabetologia 2020;63:2049–2056 [DOI] [PubMed] [Google Scholar]
- 29. Dhanasekaran M, George JJ, Loganathan G, et al. Pig islet xenotransplantation. Curr Opin Organ Transplant 2017;22:452–462 [DOI] [PubMed] [Google Scholar]
- 30. Vantyghem MC, de Koning EJP, Pattou F, Rickels MR. Advances in β-cell replacement therapy for the treatment of type 1 diabetes. Lancet 2019;394:1274–1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Butler PC. Supplying insulin while evading immunity. N Engl J Med 2021;384:967–969 [DOI] [PubMed] [Google Scholar]
- 32. Sims EK, Carr ALJ, Oram RA, DiMeglio LA, Evans-Molina C. 100 years of insulin: celebrating the past, present and future of diabetes therapy. Nat Med 2021;27:1154–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lewis GF, Brubaker PL. The discovery of insulin revisited: lessons for the modern era. J Clin Invest 2021;131:e142239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Powers AC. Type 1 diabetes mellitus: much progress, many opportunities. J Clin Invest 2021;131:e142242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Banting FG. Diabetes and insulin, 1925. Accessed 26 September 2021. Available from https://www.nobelprize.org/prizes/medicine/1923/banting/lecture/