Abstract
We reviewed articles published in 2019 and 2020 and identified and summarized the most impactful articles describing pediatric medical overuse. Articles were identified via a structured Medline search and manual table contents review of high-impact journals. Articles were scored by 3 independent raters according to strength of methods, magnitude of potential harm, and potential number of patients harmed using a standardized scoring rubric. Of 258 articles reviewed, 32 articles were discussed and the 10 most impactful were selected by consensus. This year’s review includes opportunities for higher-value utilization of blood products, antibiotics, surgical and other invasive procedures, and follow-up.
Medical overuse, or health care that provides no net benefit to patients, is associated with significant costs and potential harm to patients.1 It is a global problem, affecting both high- and low-income countries across a wide range of services.2 Data suggest that nearly 8% of the U.S. population receives low-value services in a given year,3 with one study finding 1 in 9 publicly insured children experience overuse each year.4 Consequently, methods for eliminating unnecessary health care practices have evolved,5,6 but significant barriers still exist that hinder de-implementation of low-value practices.7
Our annual updates8–11 are inspired by a similar adult medicine series,12–14 and aim to update pediatric providers about the most recent research highlighting areas of pediatric medical overuse. Our objective was to encourage continued focus on improving health care value by identifying and providing concise summaries of 10 articles describing potentially unnecessary or harmful practices in pediatrics.
METHODS
Methods were similar to our previous overuse reviews8–11 and consisted of 2 strategies of article collection: (1) a structured Medline search, and (2) a manual table of contents review of 8 high-impact journals. This year, to increase the potential impact of selected articles, we elected to review articles within a 2-year span rather than the usual annual review. We intend to continue 2-year reviews going forward, with the goal of providing readers with a more concise summary of the highest-quality articles.
Article Selection
The structured Medline review was performed by searching PubMed for articles published during the 2019 and 2020 calendar years containing the medical subject heading term “health services misuse” or “medical overuse,” as well as articles with titles or abstracts containing the words “unnecessary,” “inappropriate,” “overutilization,” or “overuse.” Articles containing the phrase “overuse injury” within the text, articles not comprising original research, and non-English articles were excluded. One author (N.M.) reviewed these titles and, when needed for clarity, abstracts, and excluded those not related to pediatric medical overuse.
Studies describing medical overuse may not all use the same descriptive terminology and inferring overuse is often subjective. Therefore, in an effort to capture a broader scope of articles describing overuse, we performed a manual table of contents review of the following 8 journals, which were divided among the authors: Annals of Emergency Medicine, Archives of Disease in Childhood, BMJ, JAMA, JAMA Pediatrics, Lancet, The New England Journal of Medicine, and Pediatrics. These journals were selected because they have historically delivered top overuse articles in our previous reviews, apart from Annals of Emergency Medicine, which was added to broaden our representation. Two authors reviewed each abstract, and articles describing original research pertaining to pediatric medical overuse were included for scoring.
Article Scoring
Articles identified in the structured Medline search and table of content reviews were scored using a rubric from previous years’ reviews composed of 3 categories: strength of methods, magnitude of potential harm, and potential number of patients harmed (Table 1). Strength of methods was based on the Oxford Centre for Evidence-based Medicine’s “Levels of Evidence.”15 Magnitude of potential harm included both severity and longevity of harm, similar to the Joint Commission on Accreditation of Healthcare Organizations’ patient safety event classification.16 The potential number of patients harmed category was scored according to the frequency of the clinical scenario and potential harm within the expected clinical environment.
TABLE 1.
Scoring Rubric
| Category | Score | Criteria |
|---|---|---|
| 1. Quality of methods | High | Randomized controlled trial (single or systematic review) |
| Medium | Cohort study (single or systematic review), poor-quality randomized controlled trial | |
| Low | Case-control, case series, cross-sectional, cohort with historical control, or poor-quality cohort study | |
| 2 Magnitude of potential harm | High | Profound impairment or life-threatening harm |
| Medium | Prolonged, nonsevere harm | |
| Low | Transient, nonsevere harm or costly | |
| 3 Number harmed | High | Common clinical scenario and common harm |
| Medium | Common clinical scenario and uncommon harm or uncommon clinical scenario and common harm | |
| Low | Uncommon clinical scenario and uncommon harm |
The articles were combined and divided among 6 authors with expertise in pediatric medicine (N.M., A.S., R.Q., T.H., J.M., and E.C.). Articles identified in the Medline search and table of contents review were scored by 2 and 3 authors, respectively. Before article scoring, each author scored the same 5 “practice articles,” which were discussed via conference call to standardize scoring. While scoring articles, authors flagged those that were either not related to pediatric overuse or those that were felt to be highly impactful. Articles flagged by 2 authors as not related to overuse were excluded. Articles flagged by 1 author as not related to pediatric overuse were adjudicated by each of 2 authors for exclusion (N.M. and E.C.). Top-scoring articles and articles flagged as highly impactful were combined and discussed via conference call, and the most impactful articles relating to pediatric medical overuse were selected by consensus based on strength of score and potential impact to practice. Interrater reliability was assessed by calculating an average intraclass correlation coefficient with corresponding 95% confidence interval (CI). Supplemental Table 2 summarizes the scoring rationale for the top 10 articles.
RESULTS
The structured Medline search identified 1839 articles, 89 (5%) of which pertained to pediatric medical overuse (Fig 1). The manual table of contents review included 9253 articles, 169 (1.8%) of which were deemed relevant to pediatric medical overuse (Fig 1). Raters reviewed a total of 258 articles (Supplemental Table 3). The average intraclass correlation coefficient (95% CI) was 0.73 (0.64–0.80), reflecting good interrater agreement.17 There were a total of 31 articles discussed by the pediatric authors: 22 highest-scoring articles and 9 additional articles which did not score as high but were rated as highly impactful (Supplemental Table 3). The 10 most impactful articles are summarized below.
FIGURE 1.
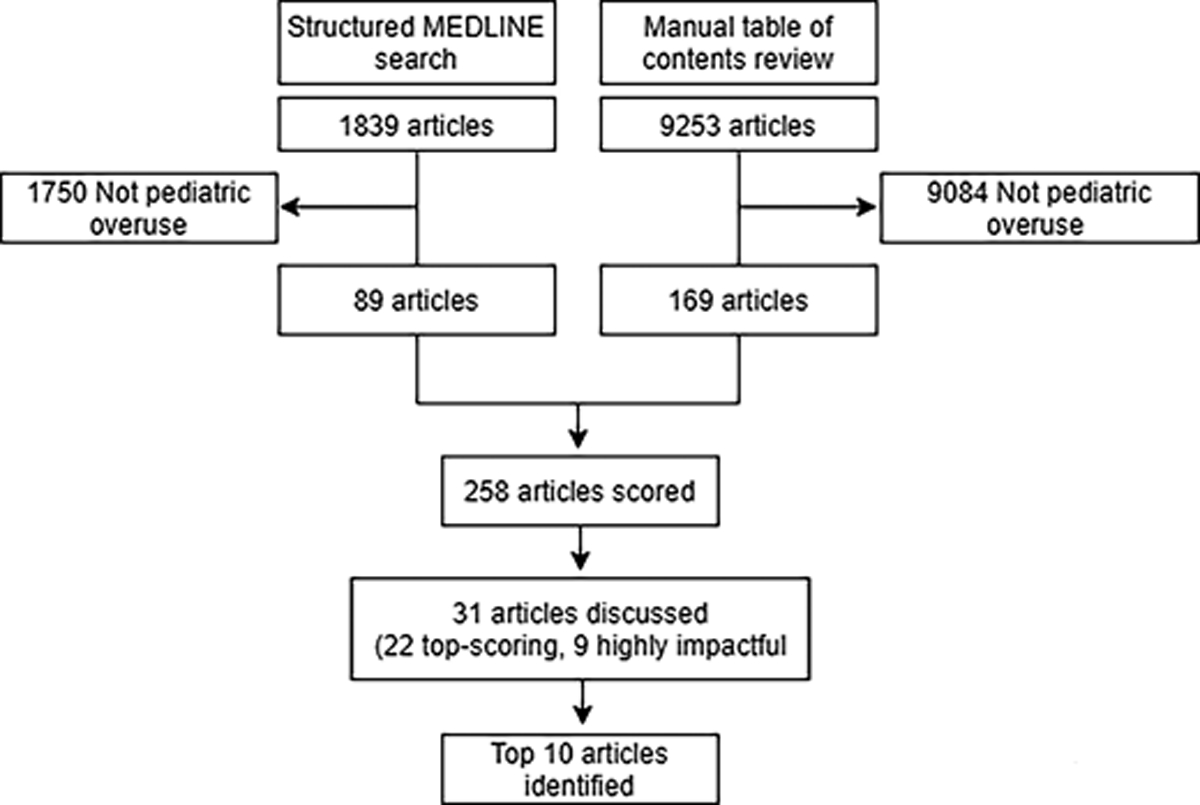
Flow diagram for selected overuse articles.
Use of a 25 000 Platelets Per Millimeter Transfusion Threshold Decreases Risk of Major Bleeding and Death18
Background
Preterm infants are at risk for intracranial hemorrhage. Neonatal providers have used a threshold of 50 000 platelets per milliliter based on a 1993 randomized controlled trial (RCT) that found no difference in outcomes between thresholds of 50 000 vs 150 000 per milliliter,19 but the effect of reserving transfusion for neonates with even lower platelet values has not been examined.
Findings
This multicenter RCT included 660 infants born <34 weeks gestation, randomized to a 50 000 platelets per milliliter or a 25 000 platelets per milliliter transfusion threshold.18 Infants who were transfused at a threshold of 50 000 platelets per millimeter had a higher rate of major bleeding or death within 28 days (26% vs 19%, odds ratio 1.57; 95% CI, 1.02 to 2.32) compared with infants transfused at a 25 000 platelets per millimeter threshold.
Limitations
In this study, cranial ultrasonography was done at the time of platelet transfusion consideration, whereas in clinical practice, these results will not always be readily available.
Implications
This RCT provides evidence that use of a 25 000 platelets per millimeter transfusion threshold may prevent harm to preterm infants without recent major bleeding.
Higher Thresholds for Neonatal Blood Transfusions Do Not Improve Survival Without Neurodevelopmental Impairment20
Background
Anemia of prematurity affects nearly every extremely low birth weight preterm infant (birth weight <1000 g), and the vast majority of these infants receive packed red blood cell transfusions in the first few weeks of life.21 Data suggest that transfusion thresholds vary, and higher transfusion thresholds may improve neurodevelopmental outcomes.22,23
Findings
This open-label trial randomized 1824 extremely low birth weight infants, with a gestational age between 22 and 29 weeks, to either the high- or low-hemoglobin threshold transfusion groups.20 Hemoglobin thresholds for transfusion were protocolized based on postnatal age and need for respiratory support, and ranged from 10 to 13 g/dL and 7 to 11 g/dL in the high- and low-threshold groups, respectively. There was no difference in the composite outcome of death or neurodevelopmental impairment in the high-versus low-threshold groups at 22 to 26 months of age, (50.1% vs 49.8%, respectively, adjusted risk ratio 1.00, 95% CI, 0.92 to 1.10). Notably, these findings are similar to those from a recently published, smaller European RCT.24
Limitations
Blinding was not feasible, and providers could choose to deviate from the transfusion algorithm, which happened in 3.5% (343 of 9679) cases, most of which (299 of 343, 87%) were in the lower-transfusion threshold group.
Implications
Randomized data suggest that higher thresholds (hemoglobin of 10–13 g/dL) for packed red blood cell transfusions did not improve survival without neurodevelopmental impairment at 22 to 26 months of age.
Less Aggressive Treatment of Neonatal Hypoglycemia Did Not Affect Development25
Background
Prolonged hypoglycemia can be associated with brain injury, seizures, and death.26 To prevent these sequelae, at-risk infants are routinely screened for hypoglycemia. However, there is no consensus at what glucose value threshold providers should treat hypoglycemia.
Findings
This noninferiority RCT of 689 infants at 17 academic hospitals included infants aged ≥35 weeks with birth weight of ≥2000 g who had an indication for glucose screening.25 Infants were randomized to receive treatment when the glucose concentration was <36 mg/dL (lower threshold) or <47 mg/dL (traditional threshold). Blinded examiners conducted psychomotor (Bayley-III-NL) testing. Scores at 18 months of age were similar in both groups (mean scores [± SE], 102.9 ± 0.7 [cognitive] and 104.6 ± 0.7 [motor] in the lower-threshold group and 102.2 ± 0.7 [cognitive] and 104.9 ± 0.7 [motor] in the traditional-threshold group). Although fewer infants in the higher-threshold group had a hypoglycemic event (47% vs 57%, mean difference 10%, 95% CI, 2.2% to 17.0%) or a severe hypoglycemic episode (5% vs 10%, mean difference 4.2, 95% CI, 0.3 to 8.2), they were also subjected to increased interventions (eg, glucose monitoring, tube feeding, and intravenous glucose treatments).
Limitations
This study performed psychomotor testing at 18 months of life but did not evaluate cognitive outcomes at older ages.
Implications
A lower-treatment threshold for hypoglycemia (36 mg/dL) was not inferior to a higher threshold (47 mg/dL) with respect to cognitive and motor development at 18 months of age. More research is needed to understand the longer-term consequences of initiating treatment at lower glucose levels.
Antibiotic Prophylaxis is Not Necessary for Infants With Prenatal Urinary Tract Dilation27
Background
Urinary tract dilatation (UTD) is a common anomaly found during prenatal ultrasound evaluations, with up to 5% of fetuses affected.28 UTD may lead to an increased incidence of urinary tract infection (UTI) postnatally. Most cases of UTD are transient in nature, but some may indicate important obstructive conditions. Retrospective studies have suggested benefits to the use of continuous antibiotic prophylaxis in infants with prenatal diagnosis of UTD29; however, recent studies have questioned its effectiveness and benefit-to-harm ratio.30–32
Findings.
In this prospective cohort study, 428 infants diagnosed prenatally with UTD were enrolled over a 4-year period, of whom 278 (65%) had postnatally confirmed UTD.27 Continuous antibiotic prophylaxis was not initiated in any of the confirmed subjects with UTD. Renal ultrasounds were serially performed at 6, 12 and 24 months of life, and patients were monitored for development of a febrile UTI. During the first 2 years of life, 19 (7%) of the 278 children with postnatally confirmed UTD were diagnosed with UTI. Nine infants (47% of infants who developed UTI, 3% of the total cohort) were subsequently diagnosed with vesicoureteral reflux. Five patients presented with a second UTI, all of which had grades III or IV reflux.
Limitations.
The UTI rate in this cohort (7%) was lower than previous studies among similar infants treated with and without antibiotic prophylaxis (12%–14% vs 27%–33%, respectively).33,34 Additionally, renal scarring was not evaluated as an outcome.
Implications.
Routine antibiotic prophylaxis may not be necessary among patients with asymptomatic, postnatally confirmed UTD, though more safety data are needed.34
A Three-Day Course of Antibiotics is Sufficient to Treat Moderate and Severe Pneumonia in Developing Countries35
Background
Pneumonia remains one of the most common causes of pediatric mortality, particularly in low-resource settings.36 For patients from low-resource countries with pneumonia who present with retractions, the World Health Organization currently recommends a 5-day course of oral amoxicillin.37 However, this recommendation is not based on high-quality evidence and studies to inform treatment duration in low-resource settings are lacking.
Findings
This double-blind, noninferiority RCT in Malawi enrolled 3000 non-HIV–infected children with chest-indrawing pneumonia between the ages of 2 and 59 months, randomizing to a 3- or 5-day course of oral amoxicillin.35 The primary outcome was treatment failure by day 6. Treatment failure was a composite outcome defined as severe respiratory distress, oxygen saturation <90%, vomiting, antibiotic change or addition, persistent fever, or death. Noninferiority was defined as <50% higher treatment failure in the 3-day treatment group. Treatment failure was not significantly different between the 3- and 5-day treatment groups (5.9% vs 5.2%, respectively, adjusted difference, 0.7%, 95% CI, −0.9 to 2.4) and noninferiority criteria was met at days 6 and 14 of follow-up.
Limitations
This study may not be applicable to children with pneumonia in resource-rich countries, where diagnostic criteria for pneumonia are different. Additionally, it is difficult to distinguish viral and bacterial pneumonia and a portion of participants likely did not have bacterial pneumonia, limiting interpretation of the true effect of decreasing antibiotic treatment days for bacterial pneumonia.
Implications
Medical overuse occurs on a global scale. Providers who practice in low-resource countries can likely safely treat children with pneumonia with 3 days of oral amoxicillin. Shorter antibiotic courses can improve adherence,38 decrease costs,39 decrease likelihood of adverse events, and decrease antibiotic resistance.40
There Are Unclear Benefits of Adenotonsillectomy for Preschool-Aged Children With Obstructive Sleep Apnea41
Background
Obstructive sleep apnea (OSA) is increasingly used as an indication for adenotonsillectomy. The Childhood Adenotonsillectomy Trial demonstrated that, compared with watchful waiting, early adenotonsillectomy among school-aged children with OSA did not result in improved attention or executive function.42 However, it is not known whether adenotonsillectomy improves cognition or behavior for preschool-aged children.
Findings
Children aged 3 to 5 years with OSA were randomized to early adenotonsillectomy (surgery within 2 months of randomization; n = 99) versus routine adenotonsillectomy (waiting list for surgery >12 months; n = 91) in a multicenter RCT conducted at 3 Australian children’s hospitals.41 The primary outcome was a measure of cognitive functioning (brief intellectual ability score) assessed 12 months after randomization. Both groups demonstrated improvement in the primary outcome, and there was no statistically significant difference in the degree of improvement among the 2 groups (average baseline score, 12-month score: 449, 465 and 451, 463 for early versus routine adenotonsillectomy groups, respectively, P = .29). Statistically significant improvements in the early adenotonsillectomy group were measured for some secondary outcomes, including parent-reported child behavior and polysomnography.
Limitations
First, the extent to which the present findings might extrapolate to preschool-aged children with severe OSA is unclear because children with severe OSA were excluded from trial participation. Secondly, behavioral outcomes were measured by parent report and parents were not blinded to their child’s treatment allocation. Third, the measured improvements in polysomnography were small and their clinical significance uncertain.
Implications
Consistent with a previous RCT among school-aged children with OSA, this trial suggests early adenotonsillectomy does not improve cognition for preschool-aged children with mild to moderate OSA. The validity and importance of small differences in secondary outcomes require more study.
A De-Implementation Program Involving Provider Education and Audit/Feedback Lead to Sustained Improvements in Antibiotic Stewardship43
Background
Antibiotic overuse in respiratory illnesses is widespread and a common target for de-implementation. Efforts to reduce antibiotic prescriptions in the outpatient setting have had mixed results. The Dialogue Around Respiratory Illness Treatment program used a cluster-randomized, step-wedged design to assess the impact of a multicomponent intervention on antibiotic-prescribing by 57 clinicians across 19 primary care practices.43 The components included online tutorials, webinars, video vignette sessions, and prescribing feedback reports.
Findings
The Dialogue Around Respiratory Illness Treatment program resulted in sustained reductions in antibiotic prescribing for viral respiratory infections after each module and in the 2 to 8-month postintervention period (adjusted risk ratio [aRR] of 0.60, 95% CI, 0.51 to 0.70) compared with the preintervention period. The use of broad-spectrum antibiotics for streptococcal pharyngitis (aRR 0.66, 95% CI, 0.50 to 0.87) and sinusitis (aRR 0.59, 95% CI, 0.44 to 0.77) also decreased.
Limitations
It is unclear whether this intervention can be generalized to other specialties and clinical settings (this study included general pediatricians and nurse practitioners). Dissemination of this intervention is also limited to practices able to generate their own feedback reports.
Implications
De-implementation is central to improving health care value. This trial shows that a program involving comprehensive provider education, audit, and feedback can lead to sustained improvements in antibiotic stewardship for pediatric primary care practices.
Spontaneous Pneumothorax in Children Does Not Routinely Require Hospitalization or Chest Tubes44
Background
The most common treatment of primary spontaneous pneumothorax is a chest tube, which is painful, can result in complications, and requires hospitalization.45,46 Evidence from a historical cohort study suggests conservative management may be equally effective.47
Findings
A multicenter, noninferiority RCT at 39 hospitals in Australia and New Zealand included patients 14 to 50 years of age (mean age ± SD: 26.4 ± 8.7) with a first-time moderate to large pneumothorax on chest radiography, comparing chest tube placement versus conservative management.44 The noninferiority margin was set at −9 percentage points. Of the 131 patients in the intervention group, 98.5% had radiographic resolution of the pneumothorax within 8 weeks compared with 94.4% of the 125 patients in the conservative management group (risk difference 4.1%, 95% CI, −8.6% to 0.5%). Median time to radiographic resolution was 16 days in the intervention group and 30 days in the conservative management group (hazard ratio 0.49, 95% CI, 0.39 to 0.63). The rate of recurrence in the first 12 months was higher in the intervention group (16.8%) compared with the conservative management group (8.8%), (absolute risk difference 8.0%, 95% CI, 0.5 to 15.4). Nineteen (12%) patients in the intervention group had at least 1 serious adverse event compared with 6 (4%) of those in the conservative management group (relative risk 3.30, 95% CI, 1.37 to 8.10). Patients in the chest tube group were also more likely to progress to surgery, spent more days in the hospital, and were less likely to be satisfied with interventional management compared with conservative management.
Limitations
Patients and clinicians were not blinded to the trial-group assignment. Secondary analyses were not adjusted for multiple comparisons and therefore cannot be used to infer definitive treatment effects. The study was limited to patients aged >14 years, which represents the population for whom spontaneous pneumothoraces are most common, but results may not generalize to younger patients.48,49
Implications
This multicenter trial challenges the conventional management of patients with a spontaneous pneumothorax. Although chest tubes decreased time to resolution compared with observation, they increased rates of recurrence and adverse events. Routine chest tube use may not be necessary for patients without cardiopulmonary compromise from primary spontaneous pneumothorax.
Home Management Is As Effective as Primary Care Follow-Up for Patients with Distal Radius Buckle Fractures50
Background
Buckle fractures of the distal radius are the most common fractures in children.51 A removable splint is often used as treatment until the fracture heals, and complications are rare. There is variation in emergency department follow-up recommendations after discharge, including orthopedic follow-up, primary care provider follow-up, or, in some cases, home removal of the splint without provider reassessment.52
Findings
This noninferiority RCT at a pediatric emergency department in Canada evaluated the functionala recovery of children aged 5 to 17 years with distal radius buckle fractures who were splinted and received splint care instructions.50 Patients were randomized to home management or primary care follow-up in 1 to 2 weeks after the emergency department visit. The mean Activities Scale for Kids-38 score (scale: 0% to 100%)53 was 95.4% in the home management group compared with 95.9% in the primary care physician follow-up group in the intention-to-treat analysis (mean difference −0.5% (95% CI, −2.6 to 1.3). Compared with primary care provider follow-up, home management resulted in reduced health care costs (absolute difference −122 Canadian dollars, 95% CI, −169 to −75), fewer physician visits (12% vs 83%, absolute difference −71.5, 95% CI, −80.6 to −56.9), and fewer radiographs (3% vs 18%, mean difference −14.9, 95% CI, −26.0 to −4.5).
Limitations.
Participants were not blinded to the follow-up intervention. Most of the parents reported having completed postsecondary education; generalizability to other, less-educated populations is unclear.
Implications.
Additional primary care follow-up after emergency department management of distal radius buckle fractures may not be necessary in most cases. The alternative, home management, is associated with lower costs, less testing, and equivalent outcomes.
Children Who Are Young for Their School Grade Are More Likely to be Diagnosed with ADHD, Intellectual Disability, and Depression54
Background
Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed chronic pediatric conditions, with 9% of U.S. children receiving a diagnosis at some point in their lives.55 Previous studies have shown that younger relative age in the school year is associated with ADHD,56 raising the possibility of misdiagnosis of this condition. It is not known if the diagnoses of depression and intellectual disability are also associated with younger relative age.
Findings
This study followed a cohort of 1 042 106 children aged 4 to 16 years in the United Kingdom between 2017 and 2019.54 The authors used multivariable Cox proportional hazards regression modeling to determine the association between relative age and the incidence of ADHD, intellectual disability, and depression. Children who were in the youngest quarter for relative age had significantly higher odds of ADHD (adjusted hazard ratio [aHR], 1.36; 95% CI, 1.28 to 1.45), intellectual disability (aHR 1.30; 95% CI, 1.18 to 1.42), and depression (aHR, 1.31; 95% CI, 1.08 to 1.59) compared with those in the oldest quarter.
Limitations
The study controlled for socioeconomic status using the Index of Multiple Deprivation, but families facing additional stressors (eg, death in family, eviction) may choose to enroll children in school at younger relative ages. Thus, there may be unmeasured confounding that distorts the relationship between younger relative age and health outcomes.
Implications
The higher prevalence of ADHD, intellectual disability, and depression in children with younger relative age suggests the possibility of misdiagnosis of these conditions in this population. When considering diagnosis and treatment of ADHD, intellectual disability, and depression, providers should consider a child’s age relative to their peers.
DISCUSSION
We identified 10 of the most impactful articles related to pediatric overuse from 2019 to 2020. This year’s review includes opportunities to reduce blood product transfusions, unnecessary antibiotic use, surgical and invasive procedures, and primary care follow-up.
The review highlighted 4 articles addressing overuse in neonates: (1) hypoglycemia treatment thresholds, (2) blood and platelet transfusion thresholds, and (3) antibiotic prophylaxis for prenatal diagnosis of urinary tract dilation. Infants are at increased risk for medical overuse; their vulnerable nature and nonspecific presentations of serious conditions may lead to well-intentioned, but unnecessary, medical interventions.57 Preterm infants are particularly fragile, which can lead to closer monitoring, overtreatment, and excessive laboratory monitoring.58–62 Although the Choosing Wisely initiative identified 5 low-value practices in newborn medicine,63 the growing body of neonatal overuse literature suggests multiple additional targets for Choosing Wisely recommendations.58–60,64 By highlighting these practices, we hope to disseminate this literature and promote de-implementation efforts to improve the quality of care and clinical outcomes for this population.
A silver lining of the coronavirus disease 2019 pandemic may be that this abrupt, natural experiment has brought both high- and low-value65–67 During the pandemic, patients often faced a “watch and wait” reality for their medical care, whether because of reluctance to seek care, diminished access to care, or advice from their medical provider to delay care (eg, postponement of routine office visits or elective surgery).68 Articles that were highlighted in this review suggest that this watch and wait approach may be of higher value for patients with OSA, spontaneous pneumothorax, and buckle fracture. Future reflection and examination of health care value during the coronavirus disease 2019 pandemic may uncover additional opportunities for deimplementation.69 Hospitals also adapted their workflows, adopting practices to minimize patient exposure by increasing inpatient telemedicine use, reducing unnecessary laboratory testing and imaging, and decreasing unnecessary vital sign monitoring in stable patients.70,71 As the medical field emerges from the pandemic, it will be important to consider how recent momentum for high-value practices might be sustained.67,72,73
Our review is subject to several limitations. A degree of subjectivity exists for certain elements of the scoring rubric, which we sought to minimize via a practice scoring session. A degree of subjectivity also exists for the group discussion and selection of top 10 articles by consensus. Also, manual table of content review of high impact journals led to disproportionate representation from these journals and may have introduced bias. Our search may not have covered all relevant manuscripts related to overuse, as manuscripts may have been missed during manual review and not all manuscripts related to medical overuse contain similar verbiage, making search parameter selection difficult.
CONCLUSIONS
This review of 2019 and 2020 articles highlights the importance of minimizing unnecessary care of the newborn and reconsidering current treatment thresholds and durations. We hope the articles and principles highlighted in this review will aid in the effort to remain focused on high-value care as our profession transitions out of the pandemic.
Supplementary Material
FUNDING:
Dr Wolf is funded through the National Center for Advancing Translational Sciences [KL2TR002648].
ABBREVIATIONS
- ADHD
attention-deficit/hyperactivity disorder
- aHR
adjusted hazard ratio
- aRR
adjusted risk ratio
- CI
confidence interval
- OSA
obstructive sleep apnea
- RCT
randomized controlled trial
- UTD
urinary tract dilation
- UTI
urinary tract infection
Footnotes
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Berwick DM, Hackbarth AD. Eliminating waste in U.S. health care. JAMA 2012;307(14):1513–1516 [DOI] [PubMed] [Google Scholar]
- 2.Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet 2017; 390(10090):156–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reid RO, Rabideau B, Sood N. Low-value health care services in a commercially insured population. JAMA Intern Med 2016;176(10):1567–1571 [DOI] [PubMed] [Google Scholar]
- 4.Chua KP, Schwartz AL, Volerman A, Conti RM, Huang ES. Differences in the receipt of low-value services between publicly and privately insured children. Pediatrics 2020;145(2):e20192325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parchman ML, Henrikson NB, Blasi PR, et al. Taking action on overuse: creating the culture for change. Healthc (Amst) 2017;5(4):199–203 [DOI] [PubMed] [Google Scholar]
- 6.Cheston CC, Vinci RJ. Overuse of continuous pulse oximetry for bronchiolitis: the need for deimplementation science JAMA 2020;323(15):1449–1450 [DOI] [PubMed] [Google Scholar]
- 7.Parchman ML, Palazzo L, Austin BT, et al. Taking action to address medical over-use: common challenges and facilitators. Am J Med 2020;133(5):567–572 [DOI] [PubMed] [Google Scholar]
- 8.Coon ER, Young PC, Quinonez RA, Morgan DJ, Dhruva SS, Schroeder AR. Update on pediatric overuse. Pediatrics 2017;139(2):e20162797. [DOI] [PubMed] [Google Scholar]
- 9.Coon ER, Young PC, Quinonez RA, Morgan DJ, Dhruva SS, Schroeder AR. 2017 update on pediatric medical overuse: a review. JAMA Pediatr 2018;172(5): 482–486 [DOI] [PubMed] [Google Scholar]
- 10.Coon ER, Quinonez RA, Morgan DJ, et al. 2018 Update on Pediatric Medical Over-use: A Review. JAMA Pediatr 2019;173(4): 379–384 10.1001/jamapediatrics.2018.5550 [DOI] [PubMed] [Google Scholar]
- 11.Money NM, Schroeder AR, Quinonez RA, et al. 2019 update on pediatric medical overuse: a systematic review. JAMA Pediatr 2020;174(4):375–382 [DOI] [PubMed] [Google Scholar]
- 12.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. 2016 update on medical overuse: a systematic review. JAMA Intern Med 2016;176(11):1687–1692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgan DJ, Dhruva SS, Coon ER, Wright SM, Korenstein D. 2017 update on medical overuse: a systematic review. JAMA Intern Med 2018;178(1):110–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan DJ, Dhruva SS, Coon ER, Wright SM, Korenstein D. 2018 update on medical overuse. JAMA Intern Med 2019; 179(2):240–246 [DOI] [PubMed] [Google Scholar]
- 15.The Centre for Evidence-Based Medicine. Levels of evidence Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-basedmedicine-levels-evidence-march-2009/. 2009. Accessed April 9, 2019
- 16.Hall A. JCAHO sentinel event alerts: a chance to enhance patient safety. Biomed Instrum Technol 2007;41(1):71–72 [DOI] [PubMed] [Google Scholar]
- 17.Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic 1981;86(2):127–137 [PubMed] [Google Scholar]
- 18.Curley A, Stanworth SJ, Willoughby K, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med 2019;380(3):242–251 [DOI] [PubMed] [Google Scholar]
- 19.Andrew M, Vegh P, Caco C, et al. A randomized, controlled trial of platelet transfusions in thrombocytopenic premature infants. J Pediatr 1993;123(2):285–291 [DOI] [PubMed] [Google Scholar]
- 20.Kirpalani H, Bell EF, Hintz SR, et al. Higher or Lower Hemoglobin Transfusion Thresholds for Preterm Infants. N EnglJ Med 2020;383(27):2639–2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howarth C, Banerjee J, Aladangady N. Red blood cell transfusion in preterm infants: current evidence and controversies. Neonatology 2018;114(1):7–16 [DOI] [PubMed] [Google Scholar]
- 22.Whyte RK, Kirpalani H, Asztalos EV, et al. PINTOS Study Group. Neurodevelopmental outcome of extremely low birth weight infants randomly assigned to restrictive or liberal hemoglobin thresholds for blood transfusion. Pediatrics 2009; 123(1):207–213 [DOI] [PubMed] [Google Scholar]
- 23.Guillén U, Cummings JJ, Bell EF, et al. International survey of transfusion practices for extremely premature infants. Semin Perinatol 2012;36(4):244–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franz AR, Engel C, Bassler D, et al. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth weight infants: the ETTNO randomized clinical trial. JAMA 2020;324(6):560–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Kempen AAMW, Eskes PF, Nuytemans DHGM, et al. Lower versus traditional treatment threshold for neonatal hypo-glycemia. N Engl J Med 2020;382(6): 534–544 [DOI] [PubMed] [Google Scholar]
- 26.Shah PS, Kusuda S, Håkansson S, et al. International Network for Evaluation of Outcomes (iNEO) in Neonates Investigators. Neonatal outcomes of very preterm or very low birth weight triplets. Pediatrics 2018;142(6):e20181938. [DOI] [PubMed] [Google Scholar]
- 27.Pennesi M, Amoroso S, Bassanese G, Pintaldi S, Giacomini G, Barbi E. Frequency of urinary tract infection in children with antenatal diagnosis of urinary tract dilatation. Arch Dis Child 2020;105(3):260–263 [DOI] [PubMed] [Google Scholar]
- 28.May Llanas ME, Moreira Echeverría A, García Boente CV, et al. [Prenatal hydro-nephrosis: incidence, management and final diagnoses in 2003]. [Article in Spanish]. An Pediatr (Barc) 2004;61(6): 499–501 [DOI] [PubMed] [Google Scholar]
- 29.Braga LH, Mijovic H, Farrokhyar F, Pemberton J, DeMaria J, Lorenzo AJ. Antibiotic prophylaxis for urinary tract infections in antenatal hydronephrosis. Pediatrics 2013;131(1):e251–e261 [DOI] [PubMed] [Google Scholar]
- 30.Hewitt IK, Pennesi M, Morello W, Ronfani L, Montini G. Antibiotic prophylaxis for urinary tract infection-related renal scarring: a systematic review. Pediatrics 2017;139(5):e20163145. [DOI] [PubMed] [Google Scholar]
- 31.Dai B, Liu Y, Jia J, Mei C. Long-term antibiotics for the prevention of recurrent urinary tract infection in children: a systematic review and meta-analysis. Arch Dis Child 2010;95(7):499–508 [DOI] [PubMed] [Google Scholar]
- 32.Selekman RE, Shapiro DJ, Boscardin J, et al. Uropathogen resistance and antibiotic prophylaxis: a meta-analysis. Pediatrics 2018;142(1):e20180119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Braga LH, Farrokhyar F, D’Cruz J, Pemberton J, Lorenzo AJ. Risk factors for febrile urinary tract infection in children with prenatal hydronephrosis: a prospective study. J Urol 2015;193(5 Suppl): 1766–1771 [DOI] [PubMed] [Google Scholar]
- 34.Leigh J, Rickard M, Sanger S, Petropoulos J, Braga LH, Chanchlani R. Antibiotic prophylaxis for prevention of urinary tract infections in the first year of life in children with vesicoureteral reflux diagnosed in the workup of antenatal hydronephrosis: a systematic review. Pediatr Nephrol 2020;35(9):1639–1646 [DOI] [PubMed] [Google Scholar]
- 35.Ginsburg AS, Mvalo T, Nkwopara E, et al. Amoxicillin for 3 or 5 days for chest-indrawing pneumonia in Malawian children. N Engl J Med 2020;383(1):13–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015; 385(9966):430–440 [DOI] [PubMed] [Google Scholar]
- 37.Integrated Management of Childhood Illness: Chart Booklet Geneva: World Health Organization; 2014 [Google Scholar]
- 38.Nightingale R, Colbourn T, Mukanga D, et al. Non-adherence to community oral-antibiotic treatment in children with fast-breathing pneumonia in Malawi-secondary analysis of a prospective cohort study. Pneumonia (Nathan) 2016;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agarwal G, Awasthi S, Kabra SK, Kaul A, Singhi S, Walter SD. ISCAP Study Group. Three day versus five day treatment with amoxicillin for non-severe pneumonia in young children: a multicentre randomised controlled trial. BMJ 2004; 328(7443):791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.King C, Nightingale R, Phiri T, et al. Non-adherence to oral antibiotics for community paediatric pneumonia treatment in Malawi: a qualitative investigation. PLoS One 2018;13(10):e0206404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Waters KA, Chawla J, Harris MA, et al. Cognition after early tonsillectomy for mild OSA. Pediatrics 2020;145(2): e20191450. [DOI] [PubMed] [Google Scholar]
- 42.Marcus CL, Moore RH, Rosen CL, et al. Childhood Adenotonsillectomy Trial (CHAT). A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med 2013;368(25):2366–2376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kronman MP, Gerber JS, Grundmeier RW, et al. Reducing antibiotic prescribing in primary care for respiratory illness. Pediatrics 2020;146(3):e20200038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brown SGA, Ball EL, Perrin K, et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med 2020;382(5):405–415 [DOI] [PubMed] [Google Scholar]
- 45.Luketich JD, Kiss M, Hershey J, et al. Chest tube insertion: a prospective evaluation of pain management. Clin J Pain 1998;14(2):152–154 [DOI] [PubMed] [Google Scholar]
- 46.Filosso PL, Guerrera F, Sandri A, et al. Errors and complications in chest tube placement. Thorac Surg Clin 2017;27(1): 57–67 [DOI] [PubMed] [Google Scholar]
- 47.Stradling P, Poole G. Conservative management of spontaneous pneumothorax. Thorax 1966;21(2):145–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cashen K, Petersen TL. Pleural effusions and pneumothoraces. Pediatr Rev 2017;38(4):170–181 [DOI] [PubMed] [Google Scholar]
- 49.Gupta D, Hansell A, Nichols T, Duong T, Ayres JG, Strachan D. Epidemiology of pneumothorax in England. Thorax 2000;55(8):666–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Colaco K, Willan A, Stimec J, et al. Home management versus primary care physician follow-up of patients with distal radius buckle fractures: a randomized controlled trial. Ann Emerg Med 2021; 77(2):163–173 [DOI] [PubMed] [Google Scholar]
- 51.Naranje SM, Erali RA, Warner WC Jr, Sawyer JR, Kelly DM. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop 2016;36(4):e45–e48 [DOI] [PubMed] [Google Scholar]
- 52.Dua K, Stein MK, O’Hara NN, et al. Variation among pediatric orthopaedic surgeons when diagnosing and treating pediatric and adolescent distal radius fractures. J Pediatr Orthop 2019;39(6): 306–313 [DOI] [PubMed] [Google Scholar]
- 53.Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the activities scale for kids. J Clin Epidemiol 2000;53(2):125–137 [DOI] [PubMed] [Google Scholar]
- 54.Root A, Brown JP, Forbes HJ, et al. Association of relative age in the school year with diagnosis of intellectual disability, attention-deficit/hyperactivity disorder, and depression. JAMA Pediatr 2019;173(11):1068–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported adhd diagnosis and associated treatment among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol 2018;47(2): 199–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Layton TJ, Barnett ML, Hicks TR, Jena AB. Attention deficit-hyperactivity disorder and month of school enrollment. N Engl J Med 2018;379(22):2122–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pursley DM, Zupancic JAF. Using neonatal intensive care units more wisely for at-risk newborns and their families. JAMA Netw Open 2020;3(6):e205693. [DOI] [PubMed] [Google Scholar]
- 58.Achten NB, Klingenberg C, Benitz WE, et al. Association of use of the neonatal early-onset sepsis calculator with reduction in antibiotic therapy and safety: a systematic review and meta-analysis. JAMA Pediatr 2019;173(11):1032–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sung SI, Lee MH, Ahn SY, Chang YS, Park WS. Effect of nonintervention vs oral ibuprofen in patent ductus arteriosus in preterm infants: a randomized clinical trial. JAMA Pediatr 2020; 174(8):755–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wickremasinghe AC, Kuzniewicz MW, McCulloch CE, Newman TB. Efficacy of subthreshold newborn phototherapy during the birth hospitalization in preventing readmission for phototherapy. JAMA Pediatr 2018;172(4):378–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Haidari ES, Lee HC, Illuzzi JL, Phibbs CS, Lin H, Xu X. Hospital variation in admissions to neonatal intensive care units by diagnosis severity and category. J Perinatol 2021;41(3):468–477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh N, Gray JE. Antibiotic stewardship in NICU: de-implementing routine CRP to reduce antibiotic usage in neonates at risk for early-onset sepsis. J Perinatol 2021;41(10):2488–2494 [DOI] [PubMed] [Google Scholar]
- 63.Ho T, Dukhovny D, Zupancic JA, Goldmann DA, Horbar JD, Pursley DM. Choosing wisely in newborn medicine: five opportunities to increase value. Pediatrics 2015;136(2):e482–e489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr 2018;8(1):1–6 [DOI] [PubMed] [Google Scholar]
- 65.Khullar D, Colla CH, Volpp KG. Imagining a world without low-value services: progress, barriers, and the path forward. Am J Manag Care 2021;27(4) [DOI] [PubMed] [Google Scholar]
- 66.Kim DD, Ollendorf DA, Neumann PJ, Fendrick AM. Crisis into opportunity: can COVID-19 help set a path to improved health care efficiency? Am J Manag Care 2020;26(9):369–370 [DOI] [PubMed] [Google Scholar]
- 67.Kevin MD. Seymann GB, Komsoukaniants A, Bouland D, Jenkins I. The silver linings playbook for COVID-19 Available at: https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html. 2020. Accessed March 26, 2021
- 68.Coon ER, Destino LA, Greene TH, Vukin E, Stoddard G, Schroeder AR. Comparison of as-needed and scheduled posthospitalization follow-up for children hospitalized for bronchiolitis: the bronchiolitis follow-up intervention trial (benefit) randomized clinical trial. JAMA Pediatr 2020;174(9): e201937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Elshaug A, Duckett S. Hospitals have stopped unnecessary elective surgeries and shouldn’t restart them after the pandemic Available at: https://theconversation.com/hospitals-have-stopped-unnecessary-elective-surgeries-and-shouldnt-restart-them-after-the-pandemic-136259. Accessed April 12, 2021
- 70.The Hospitalist. Jenkins I, Seymann G, Horman S, Bell J. Social distancing comes to the medicine wards Available at: https://www.the-hospitalist.org/hospitalist/article/220794/coronavirus-updates/social-distancing-comes-medicine-wards. 2020. Accessed April 21, 2021
- 71.Auerbach A, O’Leary KJ, Greysen SR, et al. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med 2020;15(8):483–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johansson M, Heath I. Can COVID-19 help us deal with the pandemic of defensive medicine? BMJ 2020;371: m4544. [DOI] [PubMed] [Google Scholar]
- 73.Gupta R, Simpson LA, Morgan DJ. Prioritizing high-value, equitable care after the COVID-19 shutdown: an opportunity for a health care renaissance. J Hosp Med 2021;16(2):114–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


