Abstract
Objective:
Airway management during in-hospital cardiac arrest (IHCA) represents a fundamental component of resuscitative efforts, yet little is known about temporal trends in intubation during IHCA. Our objective was to investigate changes in IHCA airway management over time and in response to national guideline updates.
Design:
Observational cohort study of a prospectively collected database.
Setting:
Multicenter study of hospitals participating in the Get With The Guidelines®— Resuscitation registry from January 1, 2001 through December 31, 2018.
Subjects:
Adult patients who experienced an IHCA and did not have an invasive airway in place prior to the arrest.
Interventions:
The primary outcome was the rate of intra-arrest intubation from 2001-2018. We constructed multivariable regression models with generalized estimating equations to determine the annual adjusted odds of intubation. We also assessed the timing of intubation relative to the onset of pulselessness and other arrest measures. We used an interrupted time series analysis to assess the association between the 2010 Advanced Cardiac Life Support guideline update and intubation rates.
Measurements and Main Results:
166,849 patients from 797 hospitals were included. From 2001 to 2018, the percentage of patients intubated during an arrest decreased from 69% to 55% for all rhythms, 73% to 60% for nonshockable rhythms, and 58% to 36% for shockable rhythms (p<0.001 for trend for all 3 groups). The median time from onset of pulselessness to intubation increased from 5 minutes in 2001 (IQR 2-8 minutes) to 6 minutes in 2018 (IQR 4-10 minutes) (p<0.001 for trend). Following the 2010 guideline update, there was a downward step change and a steeper decrease over time in the rate of intubation as compared to the pre-intervention period (p <0.001).
Conclusions:
Endotracheal intubation rates during IHCA have decreased significantly over time, with a more substantial decline following the updated 2010 guideline that prioritized chest compressions over airway management.
Keywords: cardiac arrest, resuscitation, airway management, intubation, advanced cardiac life support
Introduction:
The timing and modality of advanced airway management during in-hospital cardiac arrest (IHCA) represents a high-stakes clinical decision given the elevated morbidity and mortality surrounding the event. Increasingly, both Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS) guidelines have prioritized chest compressions over airway management during resuscitative efforts (1). In 2010, the longstanding “airway, breathing, compressions” sequence of BLS resuscitation changed to “compressions, airway, breathing,” and the ACLS algorithm was similarly streamlined to emphasize the importance of chest compressions (1,2). Amidst this paradigm shift, specific airway management recommendations did not change and have remained relatively open-ended, with guidelines stating that either a bag-mask or an advanced airway (including supraglottic and endotracheal tubes) can be used (3).
Despite these flexible airway guidelines, endotracheal intubation remains the most common airway management technique employed in the IHCA setting (4). While potential benefits of intubation include optimization of oxygenation, improved gas exchange, and some protection from pulmonary aspiration of gastric contents, intubation can lead to a prolonged interruption in chest compressions and may interfere with evidence-based interventions during the arrest (4). While randomized trials comparing intubation to alternative airway management techniques in the out-of-hospital cardiac arrest setting have yielded variable results, no randomized trial has been performed in the IHCA setting (5–7). Further, the highest quality IHCA observational data suggest poorer survival in patients who are intubated relative to those who are not (8,9).
This study seeks to evaluate temporal trends in intubation and its timing during IHCA. Our goal is to further understand changes in intra-arrest airway management over time and in response to guideline changes, and to contextualize the timing of these airway decisions within the broader scope of the cardiac arrest. By evaluating these trends, we hope to inform future studies and policy recommendations.
Materials and Methods:
Study Design:
We used data prospectively collected from the Get With The Guidelines®— Resuscitation registry. This registry is a large quality-improvement initiative sponsored by the American Heart Association that collects data on IHCA in hospitals throughout the United States. Details of the registry’s design, data input, and quality assurance have been described elsewhere (10). Hospitals participating in the registry submit clinical information regarding the medical history, hospital care, and outcomes of consecutive patients hospitalized for cardiac arrest using an online, interactive case report form and Patient Management Tool™ (IQVIA, Parsippany, New Jersey). IQVIA is the data collection coordination center for the American Heart Association/American Stroke Association Get With The Guidelines® programs. The registry contains data from years 2000 until 2018. The year 2000, the first year of the data registry, contains relatively few recorded arrests and was excluded. Entries from January 1, 2001 through December 31, 2018 were thus used for this study.
Ethics Approval
All participating institutions were required to comply with local regulatory and privacy guidelines and, if required, to secure Institutional Review Board approval. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule. IQVIA (Parsippany, New Jersey) served as the registry coordinating center. The University of Pennsylvania served as the data analytic center and granted the opportunity to prepare the data for research purposes. This analysis was designated as exempt from review by the University of California, Los Angeles Institutional Review Board (#19-001424) due to the deidentified, publicly available nature of the data.
Study Population
We included adult patients (18 years or older) who experienced an in-hospital index pulseless cardiac arrest requiring chest compressions. We limited the analysis to arrests that occurred in the emergency department or hospital inpatient setting (including operating and procedural areas) and excluded hospital visitors and employees, as well as arrests that occurred in pediatric areas of the hospital. Patients were also excluded if they already had an invasive airway in place at the beginning of the cardiac arrest (endotracheal tube, tracheostomy, or laryngeal mask airway), if the presence of an invasive airway before the arrest was unknown, if there were missing data regarding the placement of an endotracheal tube during the arrest, or if timing data for intubation and other arrest metrics were missing or inconsistent (e.g., the “end of the resuscitation” time occurred before the “onset of pulselessness” time).
Outcomes
The primary outcome was the rate of intra-arrest intubation from 2001-2018, tabulated annually. Intra-arrest intubation was defined as the successful insertion of an endotracheal or tracheostomy tube during the cardiac arrest. An intubation occurring after the time of return of spontaneous circulation was not included as an intra-arrest intubation.
For patients who were intubated, we also assessed the timing of intubation within the broader resuscitation attempt. The time to intubation was defined as the length of time (in whole minutes) from the onset of pulselessness to intubation. If intubation occurred during the same whole minute that pulses were lost, this was recorded as a time to intubation of 0 minutes, whereas a time of 1 minute indicated that intubation occurred within the next whole minute after loss of pulses. The timing of intubation relative to other arrest metrics was calculated similarly. For metrics where intubation could have occurred either before or after that measure (e.g., timing of first epinephrine dose), the time could have either a positive or negative value (e.g., with “−1” indicating that intubation occurred one minute before the first epinephrine dose was given, and “1” indicating that intubation occurred in the first minute after the epinephrine dose was given).
Statistical Analysis
Descriptive tests of association were used to characterize the study population, reporting continuous variables as medians with interquartile ranges and categorical variables as counts with frequencies, with categorical outcomes compared using Chi squared tests and continuous outcomes compared using Welch’s t-tests for unequal variance. The rate of intra-arrest intubation and the median time from onset of pulselessness to intubation were tabulated annually from 2001 to 2018. To evaluate changes over time, we performed a nonparametric test of trend across ordered groups. We additionally assessed the timing of intubation with respect to the onset of chest compressions in all arrests, as well as with respect to first defibrillation in arrests with initial shockable rhythms (e.g., ventricular fibrillation, ventricular tachycardia) and first epinephrine dose in patients with initial non-shockable rhythms. We additionally performed a pre-planned sensitivity analysis to evaluate for changes in intubation rates based upon resuscitation duration.
To further assess whether intubation rates changed over time independent of other arrest factors, we constructed multivariable regression models with generalized estimating equations (GEE) with clustering at the level of hospital for the entire cohort and stratified based upon the initial rhythm. Our model adjusted for hospital characteristics, patient characteristics (including age, sex, race, and pre-existing conditions), and case characteristics including pre-existing interventions, with variables chosen by the authors and based on prior literature (Supplemental Table 1) (11). Calendar year was the independent variable for these analyses and was calculated as a categorical variable, with 2001 as the reference year. Unadjusted analyses and analyses after the application of the GEE model above are presented.
Given our hypothesis that changes in the 2010 American Heart Association (AHA) BLS and ACLS algorithms would have an effect on intubation rates and intubation timing, we performed an interrupted time series analysis using segmented linear regression. This model included estimations of the trend before and after the guideline change. Given that the updated guidelines were released in October 2010, the first three quarters of 2010 (January-September) were included in the pre-guideline period, and the last quarter (October-December) was included in the post-guideline period.
All statistical analyses were conducting using STATA 16.1 (StataCorp, College Station, TX). All tests were two-sided, with significance set at p ≤ 0.05.
Results:
Study Sample Characteristics
Over the 18 year study period, 166,849 patients from 797 hospitals met inclusion criteria (Supplemental Figure 1), with a progressive increase in the number of patients and hospitals included over the years (Supplemental Table 2). The median age was 69 years (IQR 58-79 years) and 58% were male (Table 1). Patients were hospitalized throughout all areas of the country (14% Northeast, 27% Southeast, 20% Midwest, 19% Southwest, 15% West), and most (81%) were located in academic hospitals (Supplemental Table 3). Most events had an initial non-shockable rhythm (76%). The median length of resuscitation was 16 minutes (IQR 8-27 minutes); this decreased over time from 17 minutes (IQR 10-27 minutes, years 2001-2010) to 14 minutes (IQR 6-27 minutes, years 2011-2018) (p <0.001).
Table 1:
Trends in baseline characteristics in patients with an in-hospital cardiac arrest
| Variable | Overall (n=166,849) | 2001-2010 (n=75,892) | 2011-2018 (n=90,957) |
|---|---|---|---|
|
| |||
| Age, median (IQR) | 69 (58, 79) | 70 (58, 80) | 69 (58, 78) |
|
| |||
| Male sex | 58% | 58% | 59% |
|
| |||
| Race | |||
| White | 70% | 71% | 70% |
| Black | 21% | 19% | 22% |
| Asian | 1% | 1% | 2% |
| Other | 2% | 2% | 1% |
| Unknown | 6% | 6% | 6% |
|
| |||
| Pre-existing conditions | |||
| Respiratory insufficiency | 33% | 33% | 33% |
| Pneumonia | 12% | 12% | 12% |
| Septicemia | 13% | 12% | 14% |
| Hypotension | 19% | 21% | 18% |
| Renal insufficiency | 34% | 33% | 36% |
| Hepatic insufficiency | 7% | 6% | 7% |
| Acute CNS event | 7% | 7% | 6% |
| Metastatic malignancy | 12% | 13% | 11% |
| CHF (this admission) | 17% | 19% | 16% |
| MI (this admission) | 16% | 17% | 14% |
|
| |||
| Initial pulseless rhythm | |||
| Asystole | 31% | 37% | 27% |
| Pulseless Electrical Activity | 45% | 39% | 50% |
| Pulseless Ventricular Tachycardia | 7% | 7% | 7% |
| Ventricular Fibrillation | 11% | 13% | 9% |
| Unknown | 7% | 5% | 8% |
|
| |||
| Hospital location of arrest | |||
| Intensive Care Unit | 32% | 31% | 32% |
| Inpatient Ward | 50% | 51% | 48% |
| Emergency Department | 11% | 10% | 12% |
| Other | 8% | 7% | 8% |
|
| |||
| Arrest at night (11pm- 7am) | 33% | 34% | 32% |
|
| |||
| Resuscitation length, minutes (med, IQR) | 16 (8, 27) † | 17 (10, 27)† | 14 (6, 27) † |
|
| |||
| Witnessed arrest | 79% | 75% | 83% |
|
| |||
| ROSC achieved | 67% | 60% | 73% |
|
| |||
| Survival to hospital discharge | 26% | 22% | 30% |
= n is 163,957 for Overall, n is 74,739 for Group 1, n is 89,218 for Group 2
Return of spontaneous circulation was achieved in 67% of patients, with an increase over time from 60% (years 2001-2010) to 73% (years 2011-2018) (p<0.001). Twenty-six percent of patients survived to hospital discharge, with an increase over time from 22% (years 2001-2010) to 30% (years 2011-2018) (p<0.001).
Intubation Rates
Overall, 64% of patients were intubated during the arrest (Table 2). The percentage of patients intubated during an arrest decreased over time from 69% in 2001 to 55% in 2018 (p<0.001 for trend) (Figure 1). There was a similar decline in the percentage of patients intubated for both nonshockable rhythms and shockable rhythms, with a reduction from 73% in 2001 to 60% in 2018 for nonshockable rhythms (p<0.001 for trend) and from 58% in 2001 to 36% in 2018 for shockable rhythms (p<0.001 for trend). In the adjusted analysis, patients in 2018 had a 42% reduction in odds of intubation relative to patients in 2001 (aOR 0.58, 95% CI 0.51-0.66, p <0.001). This decrease remained significant when stratified by both shockable (aOR 0.37, 95% CI 0.31-0.45, p <0.001) and non-shockable initial rhythms (aOR 0.63, 95% CI 0.54-0.74, p<0.001). In the sensitivity analysis, intubation rates were lower in the 2011-2018 period as compared to the 2001-2010 period across all resuscitation durations (less than 5 minutes, 5-10 minutes, 11-15 minutes, and greater than 15 minutes) (Supplemental Table 4).
Table 2:
Trends in airway management in patients with an in-hospital cardiac arrest
| Variable | Overall (n=166,849) | Group 1: 2001-2010 (n=75,892) | Group 2: 2011-2018 (n=90,957) | P value (Group 1 vs Group 2) |
|---|---|---|---|---|
|
| ||||
| Intubated during arrest | 64% | 71% | 58% | ≤ 0.001 |
|
| ||||
| Airways used | ||||
| Laryngeal Mask Airway | 0.3% | 0.1% | 0.4% | ≤ 0.001 |
| Endotracheal Tube | 63% | 70% | 58% | ≤ 0.001 |
| Tracheostomy Tube | 0.4% | 0.2% | 0.5% | ≤ 0.001 |
|
| ||||
| Time to intubation from onset of pulselessness (minutes), median (IQR) | 5 (3, 9)^ | 5 (2, 8)^ | 6 (3, 9)^ | ≤ 0.001 |
|
| ||||
| Time to intubation from onset of chest compressions (minutes), median (IQR) | 5 (3, 8)† | 5 (2, 8)† | 6 (3, 9)† | ≤ 0.001 |
|
| ||||
| Time to intubation from first epinephrine (minutes), median (IQR) | 3 (0, 6)‡ | 2 (0, 5)‡ | 4 (1, 7)‡ | ≤ 0.001 |
|
| ||||
| Time to intubation from first shock (minutes), median (IQR) | 5 (2, 8)# | 4 (2, 8)# | 5 (2, 9)# | ≤ 0.001 |
n = 106,356 for “Overall,” n = 53,539 for “2001-2010,” n = 52,807 for “2011-2018”
n = 105,428 for “Overall,” n = 53,042 for “2001-2010,” n = 52,386 for “2011-2018”
n = 99,283 for “Overall,” n = 48,211 for “2001-2010,” n = 51,072 for “2011-2018;” only including patients with an initial non-shockable rhythm
n = 21,731 for “Overall,” n = 5,640 for “2001-2010,” n = 16,091 for “2011-2018;” only including patients with an initial shockable rhythm
Figure 1:
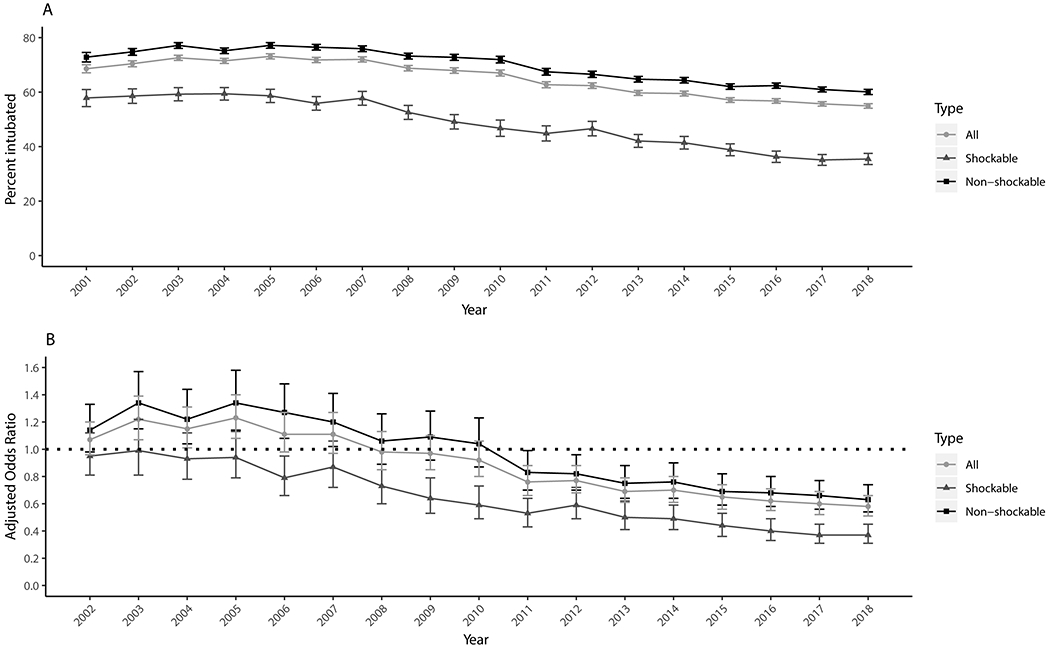
A: Percentage of patients intubated during an in-hospital cardiac arrest by calendar year. B: Adjusted odds ratio of being intubated each year with respect to the year 2001.
Time to Intubation
During the arrest, the observed time until intubation increased over time, with a median time from onset of pulselessness to intubation of 5 minutes in 2001 (IQR 2-8 minutes) compared to 6 minutes in 2018 (IQR 4-10 minutes) (Figure 2). There was a significant prolongation of the median time to intubation over the entire study period when measured annually (p<0.001 for trend). The time from CPR initiation to intubation also increased over time, with a median time of 4 minutes in 2001 (IQR 2-7 minutes) to 6 minutes in 2018 (IQR 4-10 minutes) (p<0.001 for trend). For non-shockable rhythms, the median time from the first epinephrine dose to intubation also increased over time from 1 minute in 2001 (IQR 0-4 minutes) to 4 minutes in 2018 (IQR 2-7 minutes) (p<0.001 for trend). For shockable rhythms, the median time from first defibrillation to intubation also increased from 2 minutes in 2001 (IQR 0-5 minutes) to 5 minutes in 2018 (IQR 2-9 minutes) (p<0.001 for trend).
Figure 2:
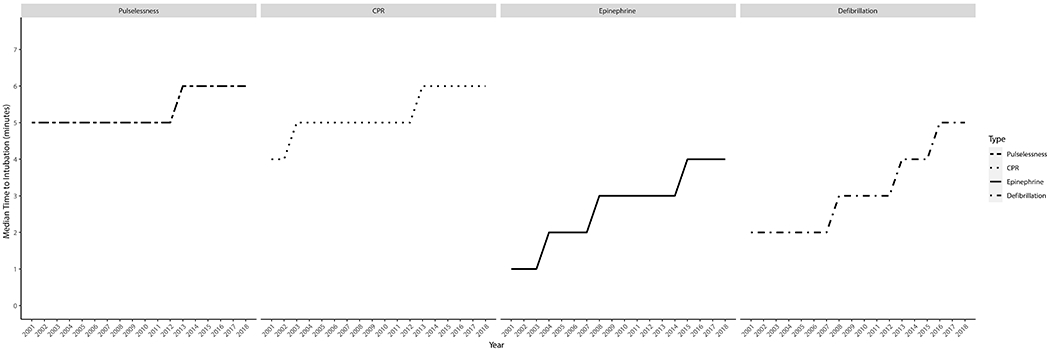
Time to intubation (in minutes) from the onset of pulselessness, CPR, first epinephrine (in non-shockable rhythms), and first defibrillation (in shockable rhythms), over time
In contrast, the observed time from onset of pulselessness to CPR initiation did not change over time (0 minutes in 2001, IQR 0-0 minutes, and 0 minutes in 2018, IQR 0-0 minutes, p = 0.74 for trend) (Supplemental Figure 2). Similarly, for non-shockable rhythms, the time from pulselessness to the first epinephrine dose did not change significantly over time (3 minutes in 2001, IQR 1-5 minutes, versus 2 minutes in 2018, IQR 1-3 minutes, p = 0.29 for trend). Finally, for shockable rhythms, the time from pulselessness to defibrillation also did not change over time (1 minute in 2001, IQR 0-4 minutes, and 1 minute in 2018, IQR 0-3 minutes, p = 0.04 for trend).
Time-Series Analysis
The interrupted time-series analysis showed a significant downward step change in the intercept and downward slope change when comparing the pre- and post-intervention periods (Figure 3). Prior to the second half of 2010, there was no significant change over time in intubation rates (mean difference per half-year 0.0%, 95% CI 0.0%, 0.0%, p=0.5). In the first year of the intervention, there was a significant decrease in intubation rates of −5.8% (95% CI 0.0%, −8.4%, p<0.001). This drop was followed by a significant decrease over time in the rate of intubation as compared to the pre-intervention period (mean decrease per half-year of −1.0%, 95% CI 0.0%, −1.0%, p<0.001).
Figure 3:
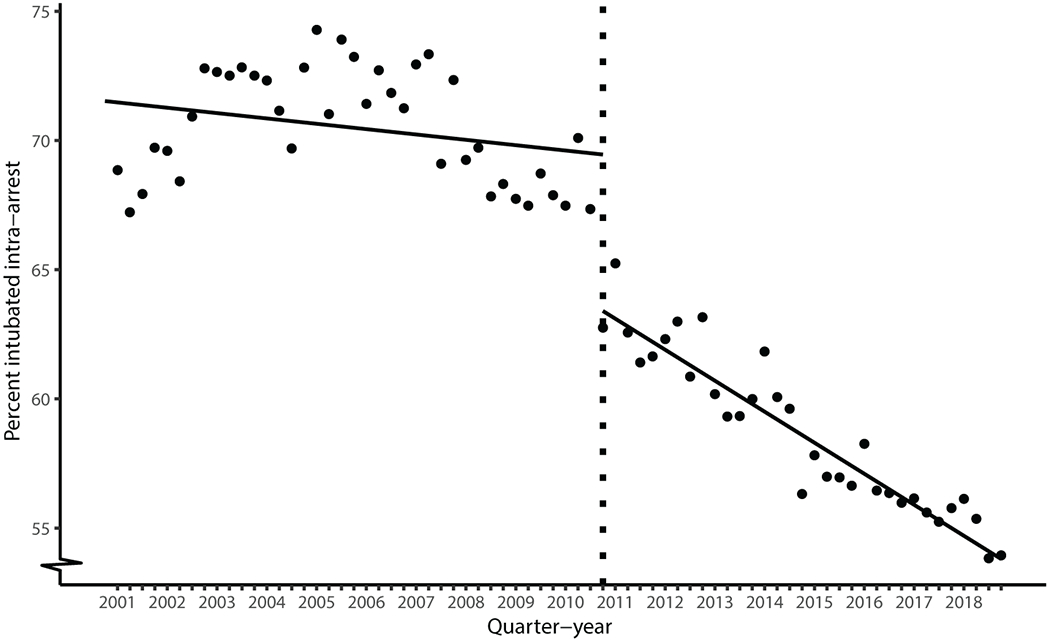
Interrupted time-series analysis of intubation rates over time
Discussion:
Our multicenter observational study, which represents the largest longitudinal report of IHCA intubation trends in the United States, reveals that endotracheal intubation rates during IHCA have declined substantially over time. When intubation occurs, it happens later in the arrest. As temporal trends in IHCA intubation rates have never been previously reported to this extent, these conclusions have important implications for understanding current practice and guiding future updates.
In our study, we found a decline in intubation that coincided with the release of the updated 2010 AHA guideline recommendations, which prioritized chest compressions over airway management during IHCA. It is notable that this increased flexibility in the timing of airway management led to a decrease in the use of ETI. This suggests that practitioners are both attuned to and responsive to national guideline changes. A recent study of temporal trends in medication administration during IHCA similarly showed significant practitioner responsiveness to pharmacotherapy guideline changes (11). Explanations for the responsiveness to AHA guideline changes may include the widespread accessibility of the internet and the relative ease with which knowledge can now be rapidly disseminated, the crisis-type nature of IHCA decision-making that thus favors an algorithm-based response, and the AHA’s training model, which requires practitioner recertification at regular intervals.
In addition to the substantial decrease in intubation rates over time, we also found that intubation, when performed, occurs later in the arrest. During the early arrest period, optimization of the chest compression fraction, early defibrillation in shockable rhythms, and epinephrine administration in nonshockable rhythms have been shown to be important predictors of survival (12–14). The increased lag time to intubation over the years may imply that practitioners are becoming increasingly focused on these other interventions during the early resuscitation period. Although the optimal timing and modality of airway management during IHCA remains unknown, it is possible that early endotracheal intubation may hinder the team’s ability to comply with these evidence-based interventions.
Despite the decrease in intubation rates over time, our study found that intubation remains the most common airway management technique during IHCA, with 55% of patients in 2018 undergoing intubation. As our study was not designed to evaluate the relationship between airway management and outcomes, future studies are needed to evaluate if and how these intra-arrest airway management decisions affect both immediate survival and longer term disability in survivors. While previous single center studies from the IHCA realm have reached differing conclusions regarding the benefit of intubation (15–17), two recently-published large national database studies have suggested that intubation may be associated with harm (8,9). In these observational studies, early IHCA intubation was found to worsen the chance of survival as compared to bag-mask ventilation at the individual patient level (8), and intubation rates at the hospital level were found to be strongly inversely associated with rates of survival to discharge (9). Further, while no randomized trials have been performed in the IHCA setting, randomized trials in the out-of-hospital setting have failed to show superiority of endotracheal intubation to alternative airway modalities (5–7), with one trial even suggesting inferiority when compared to laryngeal mask airway placement (5). As these conclusions may not apply to in-hospital settings where expert airway technicians are more available, however, future randomized studies in the IHCA realm are needed.
In light of the current pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), it will be additionally instructive to see how these intubation trends continue over time. SARS-CoV-2 spreads via aerosolization, with intubation ranking among the highest risk procedures for healthcare worker infection (18–20). Cardiopulmonary resuscitation places multiple providers in close proximity to the nose and mouth and may represent an additional threat for aerosolization (21,22). This has led many to advocate for reconsideration of hospital resuscitation policies (23). The extent to which these concerns will impact practice remains unknown.
Limitations of our study include generalizability, as our analysis only included hospitals participating in our registry. These hospitals may be more responsive to AHA guideline changes than non-participating hospitals. Further, as the number of contributing hospitals increased over time, it is possible that baseline differences between the included hospitals in each time period contributed to the observed practice changes over time (though this was adjusted for in the hierarchical analysis). In addition, our registry does not include data on the cause of the arrest, which may limit our understanding of temporal trends for predominately respiratory arrests. Nevertheless, our models adjusted for pre-existing conditions such as respiratory insufficiency and pneumonia, and the subgroup analysis for non-shockable rhythms showed similar findings to the total cohort. Finally, though missing data is always a concern in large registry analyses, missing data was relatively uncommon in our report, with <10% missing data for each of the variables included in our multivariable analysis.
In conclusion, in our large, multicenter, retrospective observational 18-year study, we found that the rate of intubation during IHCA has decreased over time and that changes to the AHA guidelines coincided with this decline. Future studies should further investigate the optimal timing and modality of airway management during IHCA.
Supplementary Material
Acknowledgements:
The authors acknowledge the AHA-GWTG Adult Research Task Force members: Anne Grossestreuer PhD; Ari Moskowitz MD; Dana Edelson MD MS; Joseph Ornato MD; Mary Ann Peberdy MD; Matthew Churpek MD MPH PhD; Michael Kurz MD MS-HES; Monique Anderson Starks MD MHS; Paul Chan MD MSc; Saket Girotra MBBS SM; Sarah Perman MD MSCE; Zachary Goldberger MD MS.
Financial Disclosures:
No financial support was used for the study.
Conflicts of Interest and Sources of Funding:
Dr. Schwab, Mr. Balaji, and Dr Lee report nothing to disclose. Dr. Buhr reports personal consulting fees from GlaxoSmithKline and Mylan/Theravance Biopharma, not related to this work. Dr. Buhr is employed part-time by the Veterans Health Administration. This work does not necessarily represent the views and opinions of the Department of Veterans Affairs. Dr. Buhr is funded by a grant from the National Institutes of Health (KL2TR001882). Dr. Moskowitz is funded by a grant from the National Institutes of Health (K23GM128005). Dr. Moskowitz and Dr Grossetreuer are volunteer members of the American Heart Association Get With The Guidelines – Resuscitation research task force.
Copyright Form Disclosure:
Dr. Buhr’s institution received funding from the National Institutes of Health (NIH) and the National Center for Advancing Translational Sciences (NCATS); he received funding from Mylan/Theravance Biopharma, GlaxoSmithKline, the NIH, NCATS, the National Heart, Lung, and Blood Institute, and the University of California Office of the President; he disclosed he is employed by the Veterans Health Administration; he received support for article research from the NIH. Dr. Balaji disclosed work for hire. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References:
- 1.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; [DOI] [PubMed] [Google Scholar]
- 2.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010. [DOI] [PubMed] [Google Scholar]
- 3.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; [DOI] [PubMed] [Google Scholar]
- 4.Benoit JL, Prince DK, Wang HE. Mechanisms linking advanced airway management and cardiac arrest outcomes. Resuscitation. 2015; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang HE, Schmicker RH, Daya MR, Stephens SW, Idris AH, Carlson JN, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest a randomized clinical trial. JAMA - J Am Med Assoc. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benger JR, Kirby K, Black S, Brett SJ, Clout M, Lazaroo MJ, et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome the AIRWAYS-2 randomized clinical trial. JAMA - J Am Med Assoc. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabre P, Penaloza A, Pinero D, Duchateau FX, Borron SW, Javaudin F, et al. Effect of bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after out-of-hospital cardiorespiratory arrest a randomized clinical trial. JAMA - J Am Med Assoc. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersen LW, Granfeldt A, Callaway CW, Bradley SM, Soar J, Nolan JP, et al. Association between tracheal intubation during adult in-hospital cardiac arrest and survival. JAMA - J Am Med Assoc. 2017; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradley SM, Zhou Y, Ramachandran SK, Engoren M, Donnino M, Girotra S. Retrospective cohort study of hospital variation in airway management during in-hospital cardiac arrest and the association with patient survival: insights from Get With The Guidelines-Resuscitation. Crit Care. 2019; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA - J Am Med Assoc. 2008; [DOI] [PubMed] [Google Scholar]
- 11.Moskowitz A, Ross CE, Andersen LW, Grossestreuer AV, Berg KM, Donnino MW. Trends Over Time in Drug Administration During Adult In-Hospital Cardiac Arrest. Crit Care Med. 2019; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan PS, Krumholz HM, Nichol G, Nallamothu BK, Nichol G, Mancini M, et al. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008; [DOI] [PubMed] [Google Scholar]
- 14.Donnino MW, Salciccioli JD, Howell MD, Cocchi MN, Giberson B, Berg K, et al. Time To administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: Retrospective analysis of large in-hospital data registry. BMJ. 2014; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tortolani AJ, Risucci DA, Rosati RJ, Dixon R. In-hospital cardiopulmonary resuscitation: patient, arrest and resuscitation factors associated with survival. Resuscitation. 1990; [DOI] [PubMed] [Google Scholar]
- 16.Dumot JA, Burval DJ, Sprung J, Waters JH, Mraovic B, Karafa MT, et al. Outcome of adult cardiopulmonary resuscitations at a Tertiary Referral Center including results of “limited” resuscitations. Arch Intern Med. 2001; [DOI] [PubMed] [Google Scholar]
- 17.Wang CH, Chen WJ, Chang WT, Tsai MS, Yu PH, Wu YW, et al. The association between timing of tracheal intubation and outcomes of adult in-hospital cardiac arrest: A retrospective cohort study. Resuscitation. 2016; [DOI] [PubMed] [Google Scholar]
- 18.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS ONE. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID -19. Anaesthesia. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weissman DN, De Perio MA, Radonovich LJ. COVID-19 and Risks Posed to Personnel during Endotracheal Intubation. JAMA - Journal of the American Medical Association. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Couper K, Taylor-Phillips S, Grove A, Freeman K, Osokogu O, Court R, et al. COVID-19 in cardiac arrest and infection risk to rescuers: A systematic review. Resuscitation. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization W. Modes of transmission of virus causing COVID-19 : implications for IPC precaution recommendations. Sci Br. 2020; [Google Scholar]
- 23.Chan PS, Berg RA, Nadkarni VM. Code Blue during the COVID-19 Pandemic. Circulation: Cardiovascular Quality and Outcomes. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


