OBJECTIVES:
To describe and compare survival among patients with out-of-hospital cardiac arrest as a function of their status for coronavirus disease 2019.
DESIGN:
We performed an observational study of out-of-hospital cardiac arrest patients between March 2020 and December 2020. Coronavirus disease 2019 status (confirmed, suspected, or negative) was defined according to the World Health Organization’s criteria.
SETTING:
Information on the patients and their care was extracted from the French national out-of-hospital cardiac arrest registry. The French prehospital emergency medical system has two tiers: the fire department intervenes rapidly to provide basic life support, and mobile ICUs provide advanced life support. The study data (including each patient’s coronavirus disease 2019 status) were collected by 95 mobile ICUs throughout France.
PATIENTS:
We included 6,624 out-of-hospital cardiac arrest patients: 127 cases with confirmed coronavirus disease 2019, 473 with suspected coronavirus disease 2019, and 6,024 negative for coronavirus disease 2019.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
The “confirmed” and “suspected” groups of coronavirus disease 2019 patients had similar characteristics and were more likely to have suffered an out-of-hospital cardiac arrest with a respiratory cause (confirmed: 53.7%, suspected coronavirus disease 2019: 56.5%; p = 0.472) than noncoronavirus disease 2019 patients (14.0%; p < 0.001 vs confirmed coronavirus disease 2019 patients). Advanced life support was initiated for 57.5% of the confirmed coronavirus disease 2019 patients, compared with 64.5% of the suspected coronavirus disease 2019 patients (p = 0.149) and 70.6% of the noncoronavirus disease 2019 ones (p = 0.002). The survival rate at 30-day postout-of-hospital cardiac arrest was 0% in the confirmed coronavirus disease 2019 group, 0.9% in the suspected coronavirus disease 2019 group (p = 0.583 vs confirmed), and 3.5% (p = 0.023) in the noncoronavirus disease 2019 group.
CONCLUSIONS:
Our results highlighted a zero survival rate in out-of-hospital cardiac arrest patients with confirmed coronavirus disease 2019. This finding raises important questions with regard to the futility of resuscitation for coronavirus disease 2019 patients and the management of the associated risks.
Keywords: coronavirus disease 2019, mobile intensive care units, out-of-hospital cardiac arrest, registry, resuscitation, zero survival
The past year has resulted in the pandemic (COVID-19) having both a direct and an indirect impact on health outcomes. These include morbidity, increase in severity of chronic diseases, increase in psychiatric illnesses (1, 2), and an increase in out-of-hospital arrests (OHCAs) (3, 4). We have previously reported that some post-OHCA deaths are directly related to COVID-19 (5).
The survival rate 30 days after an OHCA is typically very low—10.3% in Europe, for example (6, 7). We have previously reported that the survival rate in France fell during the COVID-19 pandemic (from 5.3% to 3.1%) (5). To date, published studies of COVID-19 and OHCA pooled confirmed and suspected cases of COVID-19 or compared prepandemic and per-pandemic cohorts (5, 8). Furthermore, none of the studies described the survival rate and other characteristics in a specific cohort of OHCA patients with confirmed COVID-19.
In this context, our primary objective of the present study was to describe the survival rate 30 days after OHCA among confirmed COVID-19 patients. Our secondary objective was to compare the confirmed COVID-19 patients with suspected COVID-19 patients and non-COVID-19 patients having experienced OHCA during the same period.
MATERIALS AND METHODS
Study Setting
Data were extracted from the French National OHCA Registry (RéAC). The RéAC records OHCAs managed by mobile ICUs (MICUs) in France and has been described elsewhere (9). The French prehospital emergency medical system has two tiers: the fire department acts as the first professional responder and intervenes rapidly to provide basic life support (BLS), whereas MICUs provide advanced life support (ALS). An MICU comprises at minimum an ambulance driver, a nurse, and a senior emergency medicine physician. The RéAC data entry form meets the requirements of the French emergency medical services and complies with the Utstein Resuscitation Registry’s template (10).
Study Population and Data
We analyzed cases of OHCA recorded in the RéAC between March 1, 2020, and December 31, 2020. Data were gathered by 95 centers in France. The investigating physicians filled out the patients’ COVID-19 status in the RéAC database. We excluded patients with prolonged downtime and unwitnessed arrest with signs of rigor mortis and those whose COVID-19 status was not known. We separated the OHCA study population into three groups (confirmed COVID-19, suspected COVID-19, and non-COVID-19), according to the World Health Organization (WHO)’s definition. Hence, confirmed cases were defined as patients with laboratory-confirmed COVID-19 (after inhospital or outpatient screening) and who were allowed to return home or remain at home (because of nonseverity). Suspected cases in our study were defined as patients who: 1) had consulted a family physician before the OHCA, 2) were suspect cases according to the WHO definitions A, B, or C, and 3) did not have a laboratory confirmation of COVID-19 (11).
Statistical Analysis
The normality of the data distribution for categorical variables was assessed using the Kolmogorov-Smirnov test. Quantitative variables were described as the median and first and third quartiles (Q1–Q3). Qualitative variables were described as the frequency (percentage), and 95% CIs were computed. Bivariate analyses were assessed using Pearson chi-square test or Fisher exact test for categorical variables and the nonparametric Mann-Whitney test for continuous variables. All tests were two-sided, and the threshold for statistical significance was set to p < 0.05.
Ethics
The study was approved by the French Advisory Committee on Information Processing in Material Research in the Field of Health (“Comité Consultatif sur le Traitement de l’Information en Matière de Recherche dans le Domaine de la Santé”) and registered with the French National Data Protection Commission (“Commission Nationale de l’Informatique et des Libertés”: reference number: 910946).
RESULTS
Population
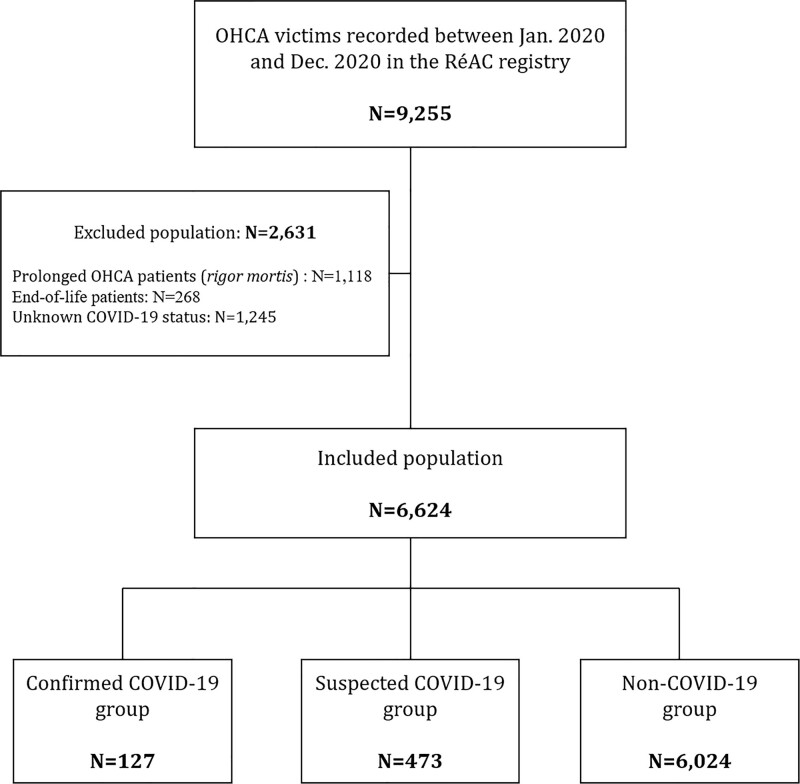
Between March 1, 2020, and December 31, 2020, the participating MICUs registered 9,255 patients in the RéAC registry. A total of 6,624 of these patients were included in our study (Fig. 1). There were 127 (1.9%) confirmed cases of COVID-19, 473 (7.1%) suspected cases, and 6,024 (90.9%) non-COVID-19 patients.
Figure 1.
Study flowchart. COVID-19 = coronavirus disease 2019, MICU = mobile ICU, OHCA = out-of-hospital cardiac arrest, RéAC = French National Out-of-Hospital Cardiac Arrest registry.
Intergroup Comparisons
The confirmed and suspected COVID-19 groups did not differ significantly with regard to sex, age, location of the OHCA, medical history, OHCA etiology, receipt of BLS, receipt of ALS (if a European Resuscitation Council ALS algorithm was implemented), the time between the call to emergency services and the arrival of the first professional responder, “no-flow” status, and “low-flow” status (Table 1). In the confirmed COVID-19 group, as soon as an ALS was implemented, intubation was performed. No difference was observed between the confirmed and suspected COVID-19 patients regarding intubation (p = 0.085). The median (Q1–Q3) time between the emergency call and the MICU’s arrival was shorter in the confirmed COVID-19 group (19 min [12–25 min]) than that in the suspected COVID-19 group (20 min [14–30 min]; p = 0.026).
TABLE 1.
Comparison of the Confirmed Coronavirus Disease 2019, Suspected Coronavirus Disease 2019, and Noncoronavirus Disease 2019 Groups
| Variables | COVID-19 Status | p (vs Confirmed COVID-19) | |||
|---|---|---|---|---|---|
| Confirmed (n = 127) | Suspected (n = 473) | Non-COVID-19 (n = 6,024) | Suspected | Non-COVID-19 | |
| Sex (% men) | 76 (59.8) | 292 (61.7) | 4,092 (67.9) | 0.758 | 0.153 |
| Age | 70 (60–84) | 71 (59–82) | 68 (55–80) | 0.541 | 0.024 |
| Location of OHCA | |||||
| Home | 102 (86.5) | 418 (89.9) | 4,372 (77.9) | 0.059 | 0.006 |
| Public place | 5 (4.2) | 28 (6.0) | 820 (14.7) | ||
| Other location | 11 (9.3) | 19 (4.1) | 417 (7.4) | ||
| Medical history | |||||
| Cardiovascular disease | 54 (42.5) | 214 (45.2) | 2,549 (42.3) | 0.616 | 0.999 |
| Respiratory disease | 26 (20.5) | 107 (22.6) | 738 (12.3) | 0.633 | 0.009 |
| Diabetes | 21 (16.5) | 84 (17.8) | 786 (13.0) | 0.794 | 0.234 |
| Other disease | 39 (30.7) | 146 (30.9) | 1,705 (28.3) | 0.999 | 0.551 |
| No disease | 6 (4.7) | 22 (4.7) | 451 (7.5) | 0.999 | 0.304 |
| Etiology of the OHCA | < 0.001 | ||||
| Medical | 121 (95.3) | 463 (97.9) | 4,918 (81.6) | 0.103 | |
| If medical, % respiratory | 65 (53.7) | 266 (56.5) | 690 (14.0) | 0.472 | < 0.001 |
| Traumatic | 0 (0.0) | 2 (0.4) | 479 (8.0) | ||
| Other | 6 (4.7) | 8 (1.7) | 627 (10.4) | ||
| BLS | |||||
| Witness to the patient’s collapse | 84 (66.1) | 304 (64.3) | 3,656 (60.7) | 0.754 | 0.233 |
| BLS by the witness: | 0.349 | 0.192 | |||
| CC only | 44 (34.6) | 142 (30.0) | 2,233 (37.1) | ||
| CC + ventilation | 17 (13.4) | 85 (18.0) | 906 (13.5) | ||
| No BLS | 66 (52.0) | 246 (52.0) | 2,975 (49.4) | ||
| BLS by the first responder | 104 (81.9) | 401 (84.8) | 5,126 (85.1) | 0.415 | 0.315 |
| Automated external defibrillator used before the MICU’s arrival | 10 (7.9) | 48 (10.1) | 1,031 (17.1) | 0.503 | 0.004 |
| ALS | |||||
| First recorded rhythm | 0.947 | 0.286 | |||
| Asystole | 109 (85.8) | 409 (86.5) | 4,876 (80.9) | ||
| Pulseless electrical activity | 9 (7.1) | 33 (7.0) | 419 (7.0) | ||
| Ventricular fibrillation/ventricular tachycardia | 4 (3.1) | 17 (3.6) | 461 (7.7) | ||
| Return of spontaneous circulation due to BLS | 5 (3.9) | 14 (3.0) | 268 (4.4) | ||
| ALS initiated | 73 (57.5) | 305 (64.5) | 4,255 (70.6) | 0.149 | 0.002 |
| Intubation | 73 (57.5) | 284 (60.0) | 3,900 (64.7) | 0.085 | 0.002 |
| Times | |||||
| T0—first responder’s arrival | 10 (5–13) | 10 (5–16) | 10 (6–15) | 0.114 | 0.113 |
| T0—MICU’s arrival | 19 (12–25) | 20 (14–30) | 19 (13–27) | 0.026 | 0.282 |
| No flow | 10 (1–19) | 12 (3–20) | 11 (2–19) | 0.305 | 0.833 |
| Low flow | 27 (15–40) | 12 (3–20) | 28 (15–40) | 0.409 | 0.635 |
ALS = advanced life support, BLS = basic life support, CC = chest compression, MICU = mobile ICU, T0 = time of the call to the emergency services.
Data are quoted as the frequency (percentage) for qualitative variables or the median (first quartile–third quartile) for quantitative variables.
The confirmed COVID-19 patients and the non-COVID-19 patients did not differ significantly with regard to sex, diabetes, a history of cardiovascular disease, a history of another disease, and the provision of BLS (except for defibrillator use, which was less frequent in the confirmed COVID-19 group: 7.9%, versus 17.1% in the non-COVID-19 group; p = 0.009). No differences were observed with regard to the first cardiac rhythm recorded by the MICU or other timings. The confirmed COVID-19 patients were more likely to have a history of respiratory disease (20.5% versus 12.3% in the non-COVID-19 group; p = 0.009), and the OHCA was more likely to have a medical cause (cardiac, neurologic, respiratory, or other medical cause) (95.3% vs 81.6%; p < 0.001). More than half the OHCA with a medical cause in the confirmed COVID-19 group were due to respiratory disease (53.7%, vs 14.0% in the non-COVID-19 group; p < 0.001). ALS provision by the MICU was less frequent (57.5%, vs 70.6% in the non-COVID-19 group; p = 0.002). The intubation was also less frequent in the confirmed COVID-19 group compared with the non-COVID-19 one (57.5% vs 64.7%; p = 0.002).
Survival
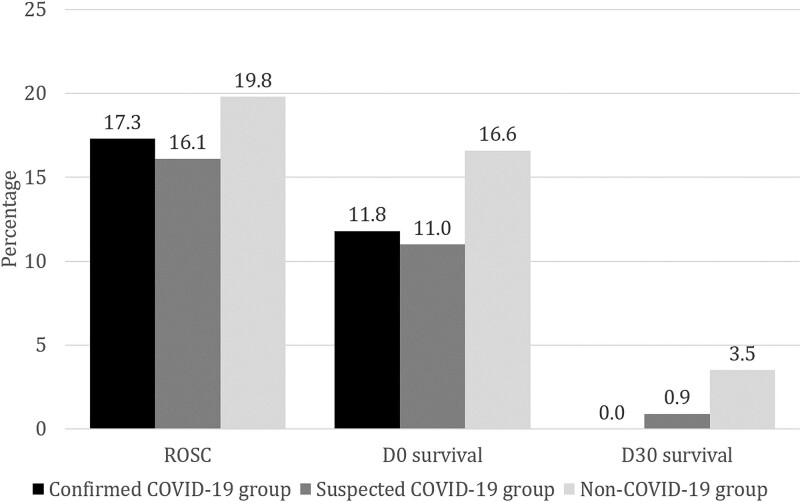
The D30 survival rate (95% CI) in the confirmed COVID-19 group was 0.00% (0.00–2.93), which was significantly lower than that in the non-COVID-19 group (3.5%; 95% CI [3.10–4.06]; p = 0.023) and lower (albeit not significantly) than in the suspected COVID-19 group (0.9%; 95% CI [0.34–2.20]; p = 0.583).
There were no significant differences between the confirmed and suspected COVID-19 patients in terms of return of spontaneous circulation (ROSC: 17.3% vs 16.1%, respectively; p = 0.787) and survival at hospital admission (D0 survival: 11.8% vs 11.0%; p = 0.753) (Fig. 2). Likewise, there were no significant differences between the confirmed COVID-19 patients and non-COVID-19 patients with regard to ROSC (17.3% vs 19.8%, respectively; p = 0.573) and D0 survival (11.8% vs 16.6, respectively; p = 0.183) (Fig. 2).
Figure 2.
Survival. D0 = at hospital admission, D30 = 30 d after out-of-hospital cardiac arrest or at hospital discharge, ROSC = return of spontaneous circulation.
DISCUSSION
To the best of our knowledge, the present study is the first to have specifically described patients with confirmed COVID-19 (according to the WHO definition [11]) having experienced OHCA. The study’s main finding was that none of the OHCA patients with confirmed COVID-19 were alive 30 days after the event.
In our study, we observed a difference in survival rates between the confirmed COVID-19 patients and non-COVID ones. Even though the post-OHCA survival rate has fallen markedly during the COVID-19 pandemic, survivors were always observed. It is extremely rare to observe a survival rate of zero (95% CI, 0.00–2.93) in a specific cohort of OHCA patients. However, researchers working in the state of Georgia (United States) did not observe any survivors among a cohort of 63 patients affected by the coronavirus who experienced inhospital cardiac arrest (survival rate [95% CI], 0.00% [0.00–5.69]) (12). This finding raises questions about the futility of resuscitation for confirmed COVID-19 patients.
In our study, we noticed that a low proportion (57.5%) of the patients known to have COVID-19 received ALS. This proportion is much lower than that for the non-COVID-19 patients in our study. This could partially explain the difference in survival. Overall, patients with suspected COVID-19 were treated in the same way as those with confirmed COVID-19. This lower level of ALS initiation during the COVID-19 era has been observed previously (5, 13). It has been suggested that resuscitation procedures can generate aerosols and, thus, risks for healthcare professionals, although the evidence has a very low degree of certainty (14). The WHO listed cardiopulmonary resuscitation (CPR) as an aerosol-generating procedure, and the international liaison committee on resuscitation confirmed this hypothesis (10). Initially, the scientific literature advised rescuers to consider their own safety before resuscitation or to change the ALS algorithm (15–17). International guidelines on resuscitation of COVID-19 patients came very late. The European Resuscitation Council COVID-19 guidelines suggested considering defibrillation before chest compression and ventilation while wearing personal protective equipment (PPE) (14). Professionals who provide ALS must take account of the patient’s context and medical history when assessing personal risks associated with treatment (14). Furthermore, the ethic in resuscitation suggests to take into account the prognostication of patient when to start ALS. Hence, regarding ethic, the futility of the resuscitation based on a zero survival rate is questioned. In this context, the high ALS initiation rate (57.5%) observed here with systematic intubation for each of the resuscitated patients testifies to MICU team members’ level of commitment.
We observed that medical OHCAs in confirmed COVID-19 patients were mainly due to respiratory distress (53.7%). Furthermore, confirmed COVID-19 patients were significantly more likely to have a history of respiratory disease than the other OHCA patients studied here. Hence, it is important to follow up COVID-19 patients carefully, especially when a history of respiratory disease is known or if the patients have few or only mild symptoms and have not been hospitalized. Indeed, acute respiratory distress syndrome (ARDS) can even occur in patients without comorbidities and who do not receive expert, individual medical follow-up. ARDS can rapidly lead to multiple organ failure and cardiac arrest (18).
The present study had a number of strengths. It was based on a large, national registry fed by MICUs throughout France (including both rural and urban areas). However, participation by the MICUs was voluntary, and some French MICUs did not participate in the study. The study also had some limitations. First, this study might be not generalizable to some other countries. The present study population was predominantly Caucasian and had some specific characteristics that prevented us from generalizing our results further. In addition, this study was carried out on a “stay and play” emergency system model and then may be not fully generalizable to countries applying a “scoop and run” model. Second, some OHCAs may have been misclassified with regard to their COVID-19 status. Indeed, some of the “non-COVID-19” cases might have been false-negatives, and we did not have access to postmortem information. Furthermore, suspected cases of COVID-19 could have been misclassified. However, we did not observe significant differences in the characteristics of suspected COVID-19 patients and confirmed COVID-19 patients, and so the error level was probably low. Third, our knowledge of inhospital data was limited. Hence, some of these cares, as a withdrawal of care in the confirmed COVID-19 group, might explain the absence of difference in ROSC and D0 survival and the presence of difference at D30. Finally, we performed a cohort study and excluded 1,245 patients because their COVID-19 status was unknown. Thus, their COVID group and vital status were not observed, and this could have changed some results. However, we worked on a large sample of 6,624 patients, which allows us to observe some effects.
CONCLUSIONS
Our results highlighted a zero survival rate in OHCA patients with confirmed COVID-19. The current resuscitation guidelines suggest that professional emergency responders use PPE and assess the risk before to starting CPR in suspected or confirmed cases of COVID-19. The risk-benefit balance for resuscitating confirmed COVID-19 patients should be investigated. The survival of OHCA patients with confirmed COVID-19 should be analyzed in other countries.
ACKNOWLEDGMENTS
The members of the French National Out-of-Hospital Cardiac Arrest Registry (RéAC) study group are: Drs. Oganov Kirill, Babin Clement, Vasseur Laurene, Agostinucci Jean Marc, Pernot Thomas, Guery Carole, Fritsch Emmanuelle, Harel David, Guillon Alain, Lorge Sarah, Halbout Laurent, Levrard Pascaline, Narcisse Sophie, Hugenschmitt Delphine, Potriquier Stephane, Chassin Coralie, Deslais Benoit, Courcoux Hubert, Larcher Fanny, Bourg Arthur, Laot Melanie, Beaka Placido, De schlichting Marie Alix, Duperron Yann, Simeon Isabelle, Bargain Philippe, Morel Marechal Emanuel, Conio Alice, Le Beuan Celine, Dattin Alix, Andriamirado Florian, Dussoulier Sebastien, Cohen Rudy, Baina Anne, Morel Jean-Charles, Ballet Celine, Lafitte Blandine, Klimas Stephane, Robart Jean-Christophe, Simonnet Bruno, Busi Olivia, Maurel Marion, Decker Sandra, Remond Annabelle, Dubois Camille, Ahui Terence, Dubeaux Josephine, Ginoux Lucie, Sciacca Christelle, Fuseau Celine, Fiani Nasri, Aubert Raphael, Nenert Eloi, Prudor Florence, Goulvin Virginie, Bonhomme Cecile, Peixoto Brandon, Theurey Odile, Grave Eric, Marrakchi Faycal, Guillet Aline, Megard Marie fleur, Lamarche-Vadel Yacine, Sussat Myriam, Goulois Nathalie, Plenier Cecile, Montagnon Francois-Xavier, Laborne Francois xavier, Piboule Ludovic, Grua David, Thibaud Eric, Jeanmasson Yoann, Sauvaget Geraldine, Muteaud Margaux, Guillaumee Frederic, Jaeger Deborah, Genuyt Benoit, Naud Julien, Baudin Marine, Abarrategui Diego, Altervain Yohan, Gay Julien, Maroteix Paul, Weyer Claire Marie, Thiriez Sylvain, Ramaherison Thierry, Mesli Adil, Massacrier Sylvie, Ovtcharenko Mariane, Duchier Caroline, Gaillard Nancy, Ursat Cecile, Jardel Benoit, Suhas Pauline, Rallu Martin, Picot Jessica, Pancher Agathe, Handwerk Tom, Bardelay Romain, Lagadec Steven, Lespiaucq Christine, Joliet Geraldine, Maigre Olivier, Mur Sebastien, Longo Celine, Li Crapi Raffaello, Barberis Christophe, Ngoyi Natacha, Serre Patrice, Mansouri Nadia, Leroy Antoine, Sanchez Caroline, Chevrier Guillaume, Jonquet Sebastien, Boutin Celia, Vanderstraeten Carine, Colson Camille, Barbery Adele, Meunier Juliette, Bertrand Philippe, Watrelot Olivier, Hiller Pascale, Guinard Sollweig, Javaudin Francois, Lepeve Alexandra, Labarrere Franck, Pes Philippe, Fromont Isaure, Carle Olivier, Crusoe Clarysse, Bernigaud Emmanuel, Dubernat Manon, Hoff Julie, Garcia Carolina, Huet Loic, Petitprez Martin, Lambert Julia, Trouvain Helene, Jung Mathilde, Gentilhomme Angelie, Durieux Emilie, Kamara Mariam, Agbemebia Fabrice, David Sandy, Savu Alexandru, Outrequin Maud, Garcia Lea, Delprat Adrien, Segard Lionel, Sebai Salim, Leduc Aurelien, Orange Rodolphe, Le Pennetier Olivier, Arnaudet Idriss, Prouve Christina, Boulanger Chloe, Trogoff Bruno, Nicolats Ophelie, Rouet Christelle, Guenier Pierre-Alban, Branche Fabienne, Ferreira Justine, Carruesco Chloe, Letur Gregory, Parsis Pierre, Hebrard Manon, Vermersch Celine, Yvetot Quentin, Besserve Paulin, Dyani Mohamed, Bujon Cecile, Loquet Lea, Le Normand Thomas, Miquelestorena Julie, Costa Aurelie, Hsing Priscilia, Desclefs Jean-Philippe, Roucaud Nicolas, Negrello Florian, Lafay Marina, Jubert Ignasi, Jeziorny Alexandre, Besnier Sylvie, Alba Pierre, Bouilleau Guillem, Tellier Eric, Hamdan David, Roux Nicolas, Pradeau Catherine, Petitdemange Olivia, Yahiaoui Samraa, Pradignac Nicolas, Torreton Florian, Goldstein Adrien, Letourneur Emilie, Bouhey Emmanuel, Dumont Nathalie, Marinoni Heloise, Mozzi Valerie, Verge Guillaume, Galtier Veronique, Nussbaum Camille, Lamourere Charles, Majour Gilles, Gevrey Vincent, Chatrenet Arthur, Laville Edouard, Gress Gauthier, Simon Benoit, Pascalon Clemence, Vara Paul, Basty-Ghuysen Marielle, Tabary Romain, Chesnoy Marine, Majoufre Gwenaelle, Lougnon Jean-Paul, Antouard Jerome, Pic Daniel, Noel Magaly, Bokobza Romain, Clauw Emmelyne, Robert Helene, Guerin Magali, Blain Stephane, Charney Alexandre, Durand Sandrine, Rakotonirina Jean-Louis, Lafon Jean, Pretalli Jean-Baptiste, Guigon Victor, Lory Thomas, Evain Yoann, Emonet Anne, Capuano Elvira, Macabre Yannick, Moine Linda, Foudi Lahcene, Andre Antoine, Bertille Hedi, Oliveira Larissa, Gornet Marion, Laggia Kelly, Edange Claire, Martinage Arnaud, Leroux Pierre, Bonnet Lucie, Rojas Jerome, Beunas Veronique, Millot Audrey, Beayni Zaher, Robert Frederique, Masson Loic, Segard Julien, Lannes Mathilde, Billier Laurianne, Barandiaran Patrick, Ferri Anne Laure, Parisot Sarah, Mazzoldi Margherita, Roudiak Nathalie, Laboure Anne, Lucas Remy, Chomono Hendricks, Metzger Jacques, Rapp Jocelyn, Ferquel Martin, Sylvie Roux, Echeikh Malek, Lamazou Elisa, Lahmar Sana, Herpin Aurelien, and Viratelle Clelia.
Footnotes
*See also p. 883.
The French National Out-of-Hospital Cardiac Arrest Registry (RéAC) study group are listed in the Acknowledgments.
The French National Cardiac Arrest Registry is supported by the French Society of Emergency Medicine; a patient foundation, the Fédération Française de Cardiologie; the Mutuelle Générale de l’Education Nationale, and Lille University. The registry is funded by the Hauts-de-France Regional Council and the European Union via the European Regional Development Fund.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Guessoum SB, Lachal J, Radjack R, et al. : Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020; 291:113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li LZ, Wang S: Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020; 291:113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baldi E, Sechi GM, Mare C, et al. ; Lombardia CARe researchers: COVID-19 kills at home: The close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020; 41:3045–3054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hubert H, Baert V, Beuscart JB, et al. : Use of out-of-hospital cardiac arrest registries to assess COVID-19 home mortality. BMC Med Res Methodol. 2020; 20:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baert V, Jaeger D, Hubert H, et al. ; GR-RéAC: Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: Registry-based study. Scand J Trauma Resusc Emerg Med. 2020; 28:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berdowski J, Berg RA, Tijssen JG, et al. : Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010; 81:1479–1487 [DOI] [PubMed] [Google Scholar]
- 7.Gräsner JT, Wnent J, Herlitz J, et al. : Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa TWO study. Resuscitation. 2020; 148:218–226 [DOI] [PubMed] [Google Scholar]
- 8.Sultanian P, Lundgren P, Strömsöe A, et al. : Cardiac arrest in COVID-19: Characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J. 2021;42:1094–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Javaudin F, Penverne Y, Montassier E: Organisation of prehospital care: The French experience. Eur J Emerg Med. 2020; 27:404–405 [DOI] [PubMed] [Google Scholar]
- 10.Perkins GD, Jacobs IG, Nadkarni VM, et al. ; Utstein Collaborators: Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015; 132:1286–1300 [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization: Global Surveillance for COVID-19 Caused by Human Infection With COVID-19 Virus: Interim Guidance, 20 March 2020. Geneva, Switzerland, World Health Organization. 2020. Available at: https://apps.who.int/iris/handle/10665/331506. Accessed May 28, 2021 [Google Scholar]
- 12.Shah P, Smith H, Olarewaju A, et al. : Is cardiopulmonary resuscitation futile in coronavirus disease 2019 patients experiencing in-hospital cardiac arrest? Crit Care Med. 2021; 49:201–208 [DOI] [PubMed] [Google Scholar]
- 13.Fothergill RT, Smith AL, Wrigley F, et al. : Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc Plus. 2021; 5:100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nolan JP, Monsieurs KG, Bossaert L, et al. ; European Resuscitation Council COVID-Guideline Writing Groups: European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation. 2020; 153:45–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edelson DP, Sasson C, Chan PS, et al. ; American Heart Association ECC Interim COVID Guidance Authors: Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: From the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020; 141:e933–e943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kapoor I, Prabhakar H, Mahajan C: Cardiopulmonary resuscitation in COVID-19 patients - To do or not to? J Clin Anesth. 2020; 65:109879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malysz M, Dabrowski M, Böttiger BW, et al. : Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: A randomized multicenter crossover simulation trial. Cardiol J. 2020; 27:497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhont S, Derom E, Van Braeckel E, et al. : The pathophysiology of ‘happy’ hypoxemia in COVID-19. Respir Res. 2020; 21:198. [DOI] [PMC free article] [PubMed] [Google Scholar]