Abstract
Mediastinal cysts are commonly an incidental finding simulating a benign or malignant diagnosis. Infection is a recognised complication of mediastinal cyst and therefore early surgical management is essential. Endobronchial ultrasound guided biopsy (EBUS) has been used to diagnose and manage mediastinal cyst. We present a case series of three patients who presented with sepsis following diagnostic EBUS of mediastinal cyst. We would recommend that EBUS guided biopsy be applied cautiously if there is a high suspicion of mediastinal cyst to avoid post procedural infection, which can thus complicate any future therapeutic options.
INTRODUCTION
Mediastinal bronchogenic cysts are rare congenital anomalies arising from malformations in the abnormal budding of the tracheobronchial tree during foetal development [1, 2]. They are often discovered as incidental findings in asymptomatic patients, but can produce common symptoms of cough, fever or dyspnoea [2–4]. They can also produce symptoms related to local expansion causing respiratory distress due to tracheal compression [5], vascular compression, airway fistulae and in a very small proportion of cases malignant transformation [2–4, 6]. The small risk of malignant transformation even in patients who are asymptomatic is one of the rationales for advocating surgical resection in this cohort of patients [7].
With the advancement of interventional and minimally invasive techniques, percutaneous, endobronchial and mediastinoscopic interventions have been described as valid alternative techniques [8–10]. The diagnosis of bronchogenic cysts is usually a combination of radiological and clinical features and is often based on computer tomography (CT) and magnetic resonance imaging (MRI) features suggestive of the diagnosis [4]. Endobronchial ultrasound (EBUS) is a useful diagnostic adjunct in confirming the diagnosis where there is clinical doubt [11].
The classic approach for large and complicated mediastinal cysts includes surgical drainage and resection. Furthermore, this is reported to prevent rupture and mediastinal and pleural contamination with infected contents [12]. An early study analysing differences between symptomatic and asymptomatic patients with bronchogenic cysts advocated surgical resection in both cohorts of patients to prevent future complications [1]. Pertaining to asymptomatic bronchogenic cysts there is contention as to whether surgical management may be appropriate, however, the general consensus is that surgical excision is indicated for infected bronchogenic cysts [2–4].
We describe our institution’s surgical and non-surgical management of three patients who presented with varying severity of infected bronchogenic cyst within 1 week following EBUS diagnostic biopsy.
CASE SERIES
Our first case was a 66-year-gentleman male with an incidental large subcarinal mass identified on contrast enhanced CT scan during pre-operative investigations for an infra-renal abdominal aortic aneurysm. He had previously undergone left thoracotomy and decortication following parapneumonic empyema 20 years ago. Contrast enhanced CT thorax revealed a 6 × 5 × 4-cm subcarinal mass measuring 65-Hounsfield unit and a 6-cm infrarenal aneurysm. He was referred to the respiratory physicians for further investigations of this mediastinal mass. Following discussion at the multidisciplinary meeting (MDT), there were concerns of mediastinal lymphadenopathy and he underwent EBUS, which showed a heterogeneous echogenic lesion in keeping with solid/semi-solid with multiple foci of calcium within it. EBUS guided biopsy revealed gel like material raising concerns of a suspicious mass. The infrarenal aneurysm was to be kept under surveillance. Five days following the procedure the patient presented to hospital in septic shock. Repeat CT imaging demonstrated an enlarged cyst 7.6 × 6.3 × 5.5-cm compressing the right pulmonary artery with a tense pericardium and pleural effusion (Fig. 1). The patient was haemodynamically unstable with cardiac tamponade and was admitted to intensive care for inotropic support and stabilisation prior to undergoing emergency surgery. Right posterolateral thoracotomy was performed, which revealed pyopericardium and purulent material with dense adhesions in the subcarinal region and its surrounding structures. The pericardium was opened, and the cavity irrigated with saline. The cyst was completely de-roofed and excised as much as possible. Copious washout was performed, and multiple drains were inserted. The patient returned in a stable condition to intensive care where he progressed satisfactorily and later recovered on the eventually discharged following completion of intravenous antibiotic therapy 21 days after admission. Histology demonstrated appearances consistent with infected bronchogenic cyst. Microbiology demonstrated pus cells with no growth on culture.
Figure 1.
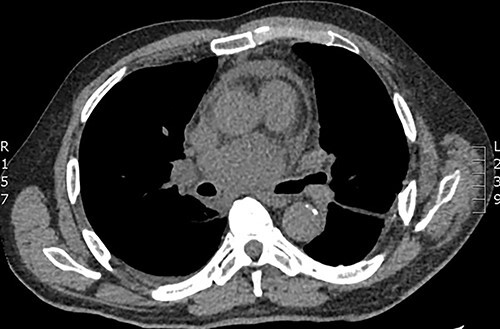
Axial CT demonstrating large subcarinal mass and pericardial effusion.
The second case was a 31-year-old gentleman otherwise fit and well was admitted to hospital with community acquired pneumonia and underwent intravenous antibiotic therapy. CT imaging demonstrated mediastinal lymphadenopathy and an incidental large subcarinal mass. The patient underwent EBUS biopsy of the subcarinal mass, which did not retrieve any tissue. Following discharge from hospital the patient represented 5 days later with pyrexia and chest pain. Repeat CT imaging demonstrated a rim enhancing lesion with cystic features and indenting the right pulmonary artery (Fig. 2). The patient was commenced on broad spectrum antibiotic therapy however remained pyrexial with rising inflammatory markers and was transferred to our institution for urgent surgery. The patient underwent urgent right posterolateral thoracotomy and deroofing of mediastinal cyst. Operative findings were that of an infected subcarinal cyst with pus within the cyst and dense adhesions to the surrounding structures. The cyst was excised from the surrounding structures and de-roofed. The patient returned to the high dependency unit in a stable condition and progressed satisfactorily eventually discharged from hospital 7 days following admission. Post-operative histology was consistent with an infected bronchogenic cyst and pus cells with no growth on culture.
Figure 2.

Axial CT scan demonstrating ring enhancing subcarinal mass.
The third patient was a 31-year-old female with no previous co-morbidities who presented with a 3-month history of night sweats and submental lymphadenitis. She has had previous exposure to tuberculosis infection and had recently travelled to Pakistan. Chest X-ray demonstrated right paratracheal mass and subsequent CT scan chest confirmed a solitary enlarged 3.4 × 2.6-cm subcarinal lymph node with no other mediastinal or hilar lymphadenopathy suspicious of being TB lymphadenopathy. She underwent EBUS, which showed a solid mass and diagnostic aspiration revealed small tissue material. She re-presented a week later with symptoms of fever and chest pain. CT chest confirmed the mass had enlarged measuring 4.9 × 3.6 cm and TB cultures and blood cultures were negative. She was commenced on intravenous antibiotics and as she had responded well, she was discharged home without surgical intervention.
At 1-year follow-up both surgical patients remained well with no evidence of cyst recurrence on imaging and no post-operative complications were noted. The non-surgical patient has remained well and repeat CT imaging has shown the cyst to have reduced in size. She is due to undergo elective surgical resection of this mediastinal cyst.
DISCUSSION
Bronchogenic cysts remain a challenge pertaining to their diagnosis and ensuing management. It is clear that in the case of complicated bronchogenic cyst and resultant symptoms that intervention is advised. This may occur in the form of non-surgical, minimally invasive or surgical approaches [7–10].
Conventional CT and MRI imaging modalities are not able to definitively differentiate cystic lesions from solid lesions solely on imaging appearances. Moreover, the contents of the cyst can vary and thus the Hounsfield unit value can vary from 0 to 20 Units and >30 Units for clear/serous fluid and mucoid/turbid fluid, respectively [11]. In the case of the latter the bronchogenic cysts with higher Hounsfield unit values often result in their appearance being indistinguishable from solid lesions. Pertaining to MRI, cysts tend to have high signal intensities on T2-weighted imaging irrespective of the nature of the cyst contents [13]. MRI with diffusion weighted imaging (DWI) may have a role in distinguishing cystic lesions from solid masses with signal suppression on high-b-value diffusion weighted images or high apparent diffusion coefficient (ADC) values of >2.5 × 10(−3) mm (2)/s [14].
EBUS is commonly used as a diagnostic adjunct if CT and MRI are not conclusive of a mediastinal cyst. It is known that EBUS can be a very useful diagnostic adjunct in distinguishing features consistent with a mediastinal cyst [15] and even in some cases as a therapeutic modality when performing aspiration [8]. Furthermore, EBUS facilitates further detailed assessment of masses adjacent to the tracheobronchial tree where is clinical suspicion of a solid composition. EBUS is able to detect the proximity or relation of the lesion to anatomical structures and is able to describe the intrinsic composition of the lesion according to its echogenicity. However, a caveat to this is when bronchogenic cysts contain hyperechoic areas, which may represent mucoid or viscous fluid collections within the cyst and in these cases heterogeneity of echogenicity can aid to establishing the diagnosis. Moreover, diagnosis aspiration usually reveals the diagnosis but carries an infective risk [16].
EBUS guided biopsy can also be performed if ultrasound features are equivocal however our case series exemplifies the potential complication of EBUS guided biopsy pertaining to mediastinal cysts. At our institution, the complication rate of infection following EBUS, and biopsy is ~3–4% for all biopsies. The fluid within the cyst is assumed sterile and the use of EBUS guided biopsy in theory would cause translocation of respiratory flora from the airway into a sterile cavity thus causing infection and ensuing sepsis.
Our cases have demonstrated the varying severity in patients presenting following EBUS biopsy of mediastinal cyst. This includes symptoms of enlargement of the cyst to severe cases with associated pyopericardium. In addition, we have also demonstrated the management options of conservative and surgical management based on the severity of presentation and the patient’s response to antibiotic therapy. Therefore, we would recommend that EBUS is used as a diagnostic tool and EBUS guided biopsies should be avoided in lesions that appear cystic. This will prevent post procedural infection and avoid any complications that will limit future therapeutic options in managing the cyst.
Contributor Information
Saifullah Mohamed, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK.
Akshay J Patel, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK; College of Medical and Dental Sciences, Institute of Immunology and Immunotherapy, University of Birmingham, Birmingham, UK.
Rana Mehdi, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK.
Ashvini Menon, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK.
Richard Steyn, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK.
Ehab Bishay, Department of Thoracic Surgery, University Hospitals Birmingham, Birmingham, UK.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- [1]. Patel SR, Meeker DP, Biscotti CV, Kirby TJ, Rice TW. Presentation and management of bronchogenic cysts in the adult. Chest 1994;106:79–85. [DOI] [PubMed] [Google Scholar]
- [2]. Sarper A, Ayten A, Golbasi I, Demircan A, Isin E. Bronchogenic cyst. Tex Heart Inst J 2003;30:105–8. [PMC free article] [PubMed] [Google Scholar]
- [3]. St-Georges R, Deslauriers J, Duranceau A, Vaillancourt R, Deschamps C, Beauchamp G, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg 1991;52:6–13. [DOI] [PubMed] [Google Scholar]
- [4]. Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest 2003;124:125–32. [DOI] [PubMed] [Google Scholar]
- [5]. Nakajima T, Yasufuku K, Shibuya K, Fujisawa T. Endobronchial ultrasound-guided transbronchial needle aspiration for the treatment of central airway stenosis caused by a mediastinal cyst. Eur J Cardiothorac Surg 2007;32:538–40. [DOI] [PubMed] [Google Scholar]
- [6]. Bolton JWR, Shahian DM. Asymptomatic bronchogenic cysts: what is the best management? Ann Thorac Surg 1992;53:1134–7. [DOI] [PubMed] [Google Scholar]
- [7]. Ponn RB. Simple mediastinal cysts: resect them all? Chest 2003;124:4–6. [DOI] [PubMed] [Google Scholar]
- [8]. Sugarbaker DJ. Thoracoscopy in the management of anterior mediastinal masses. Ann Thorac Surg 1993;56:653–6. [DOI] [PubMed] [Google Scholar]
- [9]. Urschel JD, Horan TA. Mediastinoscopic treatment of mediastinal cysts. Ann Thorac Surg 1994;58:1698–700. [DOI] [PubMed] [Google Scholar]
- [10]. Kuo C-H, Chung F-T, Kuo H-P. Infected bronchogenic cyst diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration. J Formos Med Assoc 2013;112:436–7. [DOI] [PubMed] [Google Scholar]
- [11]. Mendelson DS, Rose JS, Efremidis SC, Kirschner PA, Cohen BA. Bronchogenic cysts with high CT numbers. AJR Am J Roentgenol 1983;140:463–5. [DOI] [PubMed] [Google Scholar]
- [12]. Rajmane R, Adams AM, Rajmane O. Cyst rupture after endobronchial ultrasound-guided transbronchial needle aspiration. J Bronchol Interv Pulmonol 2016;23:e20–2. [DOI] [PubMed] [Google Scholar]
- [13]. Jeung M-Y, Gasser B, Gangi A, Bogorin A, Charneau D, Wihlm JM, et al. Imaging of cystic masses of the mediastinum. Radiographics 2002;22:S79–93. [DOI] [PubMed] [Google Scholar]
- [14]. Shin KE, Yi CA, Kim TS, Lee HY, Choi YS, Kim HK, et al. Diffusion-weighted MRI for distinguishing non-neoplastic cysts from solid masses in the mediastinum: problem-solving in mediastinal masses of indeterminate internal characteristics on CT. Eur Radiol 2014;24:677–84. [DOI] [PubMed] [Google Scholar]
- [15]. Anantham D, Phua G-C, Low S-Y, Koh M-S. Role of endobronchial ultrasound in the diagnosis of bronchogenic cysts. Diagn Ther Endosc 2011;2011:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Katsenos S, Rojas-Solano J, Becker HD. Endobronchial ultrasound: a useful tool in the diagnosis of bronchogenic cyst. J Clin Imaging Sci 2013;3:57. [DOI] [PMC free article] [PubMed] [Google Scholar]


