Background:
Fine particulate matter (PM2.5) is a known risk factor for cardiovascular disease (CVD). Neighborhood walkability and greenness may also be associated with CVD, but there is limited evidence on their joint or interacting effects with PM2.5.
Methods:
Cox proportional hazard models were used to estimate the risk of CVD mortality among adults with a history of acute myocardial infarction and/or stroke living in Northern California. We assessed the independent and joint effects of walkability, greenness (Normalized Differentiated Vegetation Index [NDVI]), and PM2.5 at residential addresses, controlling for age, sex, race/ethnicity, comorbidities, BMI, smoking, revascularization, medications, and socioeconomic status.
Results:
Greenness had a nonlinear association with CVD mortality (P = 0.038), with notably protective effects (HR = 0.87 [95% confidence interval {CI} = 0.78, 0.97]) at higher greenness levels (NDVI ≥ 0.3) and moderate attenuation after adjusting for PM2.5 (HR = 0.92 [95% CI = 0.82, 1.03]) per 0.1 increase in NDVI. Walkability had no independent effect on CVD mortality. PM2.5 had a strong independent effect in models adjusted for greenness and walkability (HR = 1.20 [95% CI = 1.08, 1.33)) per 10 μg/m3 increase in PM2.5. There was an interaction between walkability and PM2.5 (P = 0.037), where PM2.5 had slightly stronger associations in more walkable than less walkable neighborhoods (HR = 1.23 [95% CI = 1.06, 1.42] vs. 1.17 [95% CI = 1.04, 1.32]) per 10 μg/m3 increase in PM2.5. Greenness had no interaction with PM2.5 (P = 0.768) nor walkability (P = 0.385).
Conclusions:
High greenness may be protective of CVD mortality among adults with CVD history. PM2.5 associated CVD mortality risk varies slightly by level of neighborhood walkability, though these small differences may not be clinically meaningful.
Keywords: National Walkability Index, Green space, Air pollutants, Effect modification, Susceptibility
What this study adds
There is insufficient evidence on the joint effects of PM2.5, greenness, and neighborhood walkability on cardiovascular (CVD) events, despite these factors being interrelated and associated with CVD health. No studies have been among a vulnerable population with CVD history. We found that higher neighborhood greenness levels may protect against CVD mortality risk, although that effect was attenuated when accounting for PM2.5 exposure. We also discovered that the PM2.5 effect was slightly stronger in more walkable than less walkable neighborhoods, suggesting that the cardiovascular health benefits of more walkable environments may be counteracted by the deleterious effects of air pollution.
Introduction
There is strong evidence of a causal relation between fine particulate matter less than 2.5 μm in diameter (PM2.5) exposure and cardiovascular (CVD) morbidity and mortality, with long-term (1 year or more) exposures inducing more risk than short-term exposures.1–3 Elevations of long-term PM2.5 exposure can reduce life expectancy by as much as a few years, and this reduction is most likely attributed to excess CVD mortality.1 Individuals with a history of CVD events may have a greater risk of CVD mortality4 and may be more susceptible to the harmful effects of air pollution.5–7
Both neighborhood walkability and residential greenness may be independently beneficial for cardiovascular health.8–11 However, air pollution is interrelated with these environmental factors. Although highly walkable neighborhoods are associated with increased walking and physical activity,12–18 they are also associated with greater exposure to air pollution.19–22 High levels of residential greenness have been associated with decreased exposure to air pollution and also with lower neighborhood walkability.23–25
Evidence on the joint or interacting effects of these three environmental factors on cardiovascular outcomes is limited and mixed.26 Several studies have reported no or only moderate effect modification by neighborhood walkability or greenness on cardiovascular outcomes associated with particulate matter.21,27–29 However, three studies reported evidence of greater effects of air pollution on CVD health risks in areas with higher walkability and lower greenness.22,30,31
Individuals with a history of acute myocardial infarction (AMI) or stroke are one of the highest risk groups for further coronary and cerebral events32 and may greatly benefit from community-level interventions that promote healthier living environments. To our knowledge, no studies have looked at the effect modification of walkability or greenness on the association between long-term PM2.5 and CVD mortality in this vulnerable population. Among a population of adults with AMI and/or stroke history, we aim to determine the (1) independent effects of walkability and greenness on CVD mortality risk and (2) joint effects of walkability, greenness, and PM2.5. Our goal is to understand how these interrelated environmental factors jointly affect CVD mortality risk among adults with a history of CVD events.
Methods
Study subjects
This retrospective cohort study includes adults with a documented medical history of AMI and/or stroke in the Kaiser Permanente Northern California (KPNC) electronic health record (EHR). KPNC is a large, integrated healthcare system that provides comprehensive medical services to over four million members who are broadly representative of Northern California’s diverse population.33–35 The study cohort has been described in detail previously.36 Briefly, subjects had to be KPNC members for at least one year, had at least one outpatient (nonemergency) visit, and lived in the 35 county study region for at least 1 year at an address that was successfully geocoded and linked to the air pollution, walkability, and Normalized Differentiated Vegetation Index (NDVI) data (see eFigure 1; http://links.lww.com/EE/A179 for study region). Study follow-up began on 1 January 2007 and ended on 31 December 2016. Each subject was followed to the first of the following dates: death, end of KPNC membership, moving away from study start address, or 31 December 2016. The institutional review board of the Kaiser Foundation Research Institute approved this study and no informed consent was required.
National Walkability Index
We assessed walkability by the National Walkability Index, which was developed by the US Environmental Protection Agency,37 and has been validated with self-reported walking data from the 2015 National Health Interview Survey.16 The Walkability Index is based on a weighted score of four urban planning indicators: intersection density, proximity to transit stops, employment types, and household types. Census 2010 block groups were ranked by each of these factors to determine the overall Walkability Index, which ranges from 0 (least walkable) to 20 (most walkable). We linked geocoded residential addresses of cohort members to the Walkability Index at the Census block-group level.
Greenness
Greenness is the land that is partly or completely covered with grass, trees, shrubs, or other vegetation38 and is commonly measured within a defined area around a residential address.39 We measured greenness using the NDVI.40 During photosynthesis, chlorophyl in plants absorb visible light (0.4–0.7 μm) and their leaves reflect near-infrared light (0.7–1.1 μm), and satellite images provide information on these two measurements. NDVI calculates the ratio of the difference between the near-infrared region and red reflectance to the sum of these two measures. NDVI values range from −1.0 to 1.0, with higher values indicating more greenness. Continuous NDVI values were generated from NASA’s Landsat 8 satellite imagery (courtesy of the US Geological Survey) for the summer months (May to September) from 2003 to 2015 with a maximum cloud cover of fifteen percent for each scene and at a spatial resolution of 30 m × 30 m. Yearly NDVI averages were combined to create a 2003–2015 average of NDVI. Negative NDVI values were set to missing. Landsat image acquisition, processing, and NDVI conversion were performed using the Semi-Automatic Classification Plugin (Congedo 2016) for the QGIS program (www.qgis.org). We linked geocoded residential addresses to NDVI at 250 m, 500 m, and 1 km radii zones surrounding subjects’ residences. The primary measure was NDVI within 1 km because it captures a wider area of exposure within walking distance; NDVI within 250 m and 500 m buffers were used in sensitivity analyses. There were 152 subjects (0.18%) with missing NDVI data but who were successfully linked to PM2.5 data and walkability data; these subjects were excluded from the greenness analyses only.
Long-term PM2.5 exposure
PM2.5 exposure was estimated from a validated ensemble model that combined satellite data, land-use data, meteorological data, chemical transport model predictions data, and ground monitor data using machine learning algorithms.41 The model estimated daily average PM2.5 exposures at a resolution of 1 km × 1 km across the contiguous US from 2000 to 2016, with an R2 of 0.89 for 1-year PM2.5 predictions using 10-fold cross-validation.41 Using the daily PM2.5 exposures and the geocoded residential addresses of all cohort members at baseline, we constructed individual-level 1-year average PM2.5 exposures for each subject at baseline, defined as the year before study start date of each subject.
Cardiovascular mortality
Our primary outcome of interest was CVD mortality, defined by International Classification of Diseases codes42 for the underlying cause of death (ICD-10: I10.x-I70.x), based on previous studies of PM2.5 and CVD mortality.43–45 Cause of death data was obtained from the official state of California death certificate data, health plan inhospital mortality, and the National Death Index state death certificate data.
Covariates
Individual-level baseline covariates were extracted from EHRs and included age, sex, self-reported race/ethnicity (Non-Hispanic White, Hispanic White, Hispanic [any race], Black, American Indian/Alaska Native, Asian/Pacific Islander, Multiple Races), hypertension (HTN), hyperlipidemia, diabetes, CVD history (AMI only, stroke only, both AMI and stroke), body mass index (BMI), smoking status (never, former, current), revascularization procedures (percutaneous coronary intervention and coronary artery bypass graft), statin medication use, HTN medication use (only among those with a HTN diagnosis), and Medicaid insurance (indicator of socioeconomic status [SES]).36 Another indicator of SES measured at the block-group level from Census data included high school education attainment (percent with less than high school diploma). CVD history was defined as prior stroke or AMI compiled from inpatient and outpatient data recorded in the EHR.36 For the small percentage of subjects with missing data on sex (0.0024%), race/ethnicity (0.64%), smoking status (3.01%), and BMI (1.99%), we did single data imputation using the fully conditional method.46
Statistical analyses
Cox proportional hazards regression was used to model the associations between each exposure variable (greenness, walkability, PM2.5) and CVD mortality. We assessed departures from the proportional hazards assumption by interaction terms with the natural logarithm of the time variable. For all models, we used time on study as the time scale and stratified the baseline hazards by 5-year age groups, allowing each age category to have its own baseline hazard (Liao et al., 2021).36 Covariates we selected a priori based on previous epidemiologic studies of air pollution and CVD events.36,47–49 Correlations of continuous variables were computed using the Pearson correlation coefficient. We fit five different models to assess the influence of sequentially adding covariates and related environmental factors. Model 1 minimally adjusted for age, sex, and study start year. Model 2 adjusted for additional individual-level factors: race/ethnicity, BMI, smoking, relevant comorbidities (HTN, hyperlipidemia, diabetes), CVD history, revascularization (percutaneous coronary intervention and coronary artery bypass graft), and medications (statins and hypertensive medication). Model 3 (main model) added neighborhood-level and individual-level SES measures (neighborhood education and Medicaid insurance). Model 4 added PM2.5, and Model 5 included all individual-level, SES, and environmental factors (greenness, walkability, and PM2.5) simultaneously. Independent effects of greenness and PM2.5 are reported per 0.1 increase in NDVI and per 10 μg/m3 increase in PM2.5, respectively, consistent with other literature, and independent effects of walkability are reported per 5-unit increase in the National Walkability Index, approximate with its interquartile range (6.5). We assessed potential nonlinearity in the shape of each association using restricted cubic splines.
For our effect modification analyses, we assessed interactions between PM2.5, greenness, and walkability using two-way interaction terms. We first assessed these interactions using continuous variables, and then in categories since interactions between continuous variables can be difficult to interpret. Categories were as follows: PM2.5 (μg/m3) (low: ≤9, moderate: 9–12, high: >12) as previously defined,36 with concentrations above the state/federal regulation limit defined as high; walkability index (low: ≤6.67, moderate: 6.67–13.33, high: >13.33) using equal intervals16; and NDVI (low: ≤0.2, moderate: 0.2–0.3, high: >0.3) based on its distribution. We then estimated interactions for walkability/PM2.5, greenness/PM2.5, and greenness/walkability pairs. We also categorized walkability into quartiles to present the linear PM2.5 association by these quartiles. In sensitivity analyses, we looked at the pairwise combinations in a subset restricted to Census tracts with population densities ≥1,000 persons per square mile since more rural areas may have exceedingly higher greenness and lower walkability levels. In supplementary analyses, we analyzed three-way interactions between PM2.5, walkability, and neighborhood education. Analyses were conducted using SAS software, version 9.4 (SAS Institute) and RStudio, version 2021.09.0.
Results
Cohort characteristics
The study cohort included adults with a history of AMI and/or stroke. Cohort characteristics are displayed in Table 1. Most subjects (56%) had a history of stroke only, 33% had a history of AMI only, and 10% had a history of both AMI and stroke. There were more males (56%) and individuals over 65 years of age (67%). The cohort was very diverse, with 64% non-Hispanic White, 11% Hispanic (any race), 10% Asian/Pacific Islander, 8% Black, and 8% multiple races. In addition, 43% of subjects were former smokers, 16% were current smokers, 37% were overweight, and 33% were obese. Subjects had high rates of comorbidities: 82% had HTN, 81% had hyperlipidemia, and 31% had diabetes. The maximum follow-up time was 10 years (average follow-up time 5.1 years), with a total of 424,719 person–years and 8,820 CVD mortality events in the analyses.
Table 1.
Characteristics of the walkability cohort at baseline.
| Characteristic | N = 83,560 | |
|---|---|---|
| N | % | |
| Sexa | ||
| Female | 36,898 | 44.2 |
| Male | 46,662 | 55.8 |
| Age (years) | ||
| 18 to 39 | 2,134 | 2.6 |
| 40 to 64 | 25,348 | 30.3 |
| ≥65 | 56,078 | 67.1 |
| Race/ethnicitya | ||
| White, non-Hispanic | 53,400 | 63.9 |
| Hispanic white | 7,417 | 8.9 |
| Black | 6,783 | 8.1 |
| American Indian/Alaska Native | 422 | 0.5 |
| Asian/Pacific Islander | 8,517 | 10.2 |
| Multiple races | 7,021 | 8.4 |
| Hispanic (any race) | 9,405 | 11.3 |
| Neighborhood education | Mean | SD |
| Percent with less than high school diploma | 13.8 | 12.3 |
| Medicaid insurance | ||
| Yes | 1,399 | 1.7 |
| No | 82,161 | 98.3 |
| Smokinga | ||
| Never | 34,952 | 41.8 |
| Former | 35,614 | 42.6 |
| Current | 12,994 | 15.6 |
| BMIa | ||
| Underweight (<18.5) | 1,709 | 2.1 |
| Normal (18.5–24.9) | 23,412 | 28.0 |
| Overweight (25.0–29.9) | 30,618 | 36.6 |
| Obese (≥30.0) | 27,821 | 33.3 |
| Comorbidities | ||
| HTN | 68,140 | 81.6 |
| Hyperlipidemia | 67,628 | 80.9 |
| Diabetes | 25,597 | 30.6 |
| Revascularization | ||
| PCI | 17,725 | 21.2 |
| CABG | 11,883 | 14.2 |
| Statin medication use | ||
| Yes | 66,232 | 79.3 |
| No | 17,328 | 20.7 |
| HTN medication use | ||
| Yes | 66,717 | 79.8 |
| No | 16,843 | 20.2 |
| History of CVD | ||
| AMI only | 27,872 | 33.4 |
| Stroke only | 46,972 | 56.2 |
| Both AMI and stroke | 8,716 | 10.4 |
| PM2.5 exposure (μg/m3) | Mean | SD |
| 1-year mean at baseline | 10.43 | 2.13 |
| Walkability | Mean | SD |
| National Walkability Index | 11.05 | 3.92 |
| Greenness | Mean | SD |
| NDVI 1 km | 0.32 | 0.08 |
CABG indicates coronary artery bypass graft; PCI, percutaneous coronary intervention.
aMissing data were imputed for unknown values of sex (N = 2, 0.0024%), race/ethnicity (N = 532, 0.64%), smoking status (N = 2,513, 3.01%), and BMI (N = 1,664, 1.99%).
Descriptions and correlations of environmental variables
Distributions of NDVI, walkability, and PM2.5 are displayed in eFigure 2; http://links.lww.com/EE/A179. NDVI within a 1km radius ranged from 0.03 to 0.53, with a median of 0.23. National Walkability Index values ranged from 1 to 20, with median of 11.00. PM2.5 exposures among study subjects at baseline ranged from 2.44 to 24.34 μg/m3, with a median of 10.2 μg/m3. Correlations between environmental variables were low to moderate. PM2.5 was slightly lower in areas of higher greenness (r = −0.21) and slightly higher in areas of higher walkability (r = 0.15). Walkability was lower in areas of higher greenness (r = −0.50). Areas with lower neighborhood education had slightly higher PM2.5 (r = 0.23), slightly lower greenness (r = −0.33), and slightly higher walkability (r = 0.16).
Main effects
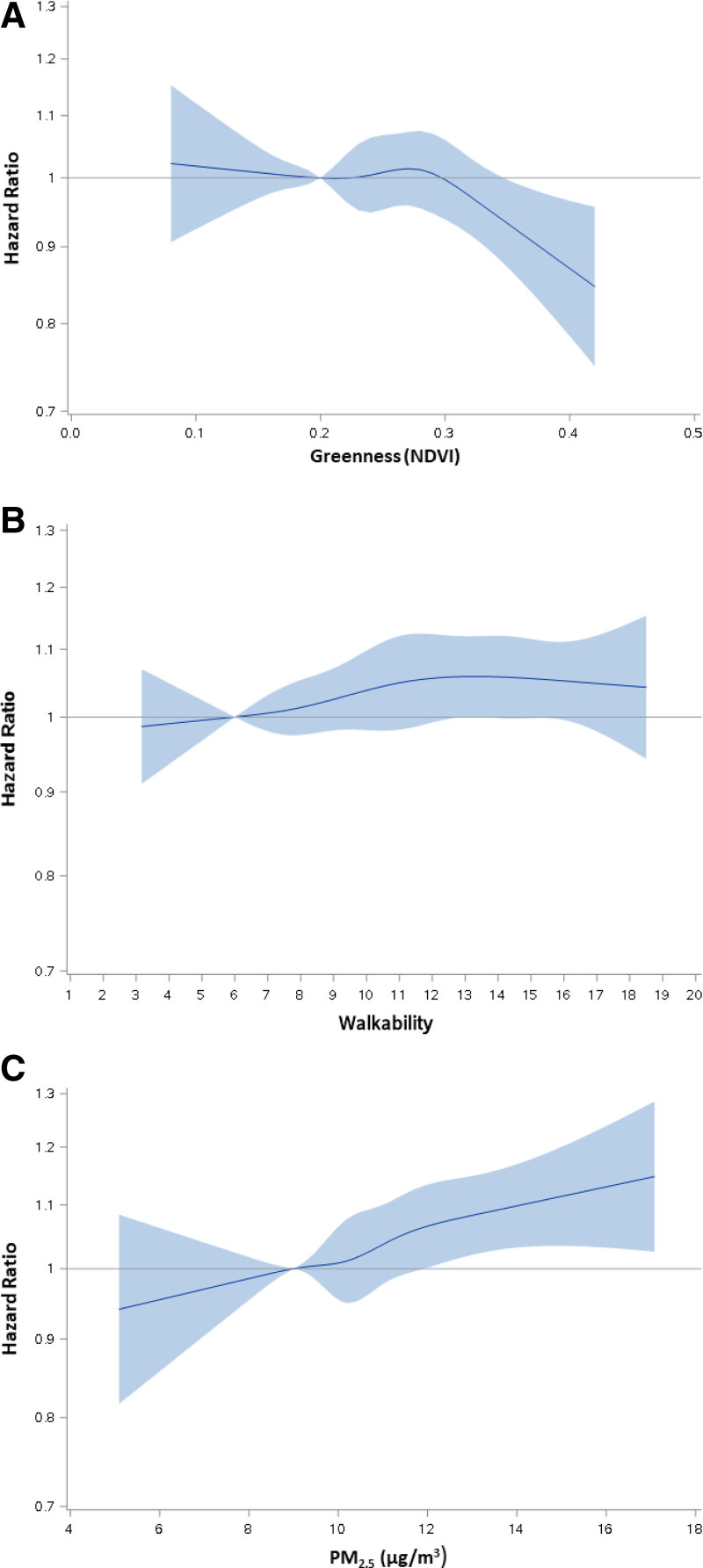
The main effects of greenness, walkability, and PM2.5 on CVD mortality are given in Table 2 and Figure 1. Greenness had a nonlinear association with CVD mortality (P = 0.038). Estimated risks seem null for NDVI < 0.3, and then decrease sharply thereafter. Based on the shape of association, we then estimated the linear effects above and below NDVI of 0.3 (Table 2, eFigure 3; http://links.lww.com/EE/A179). In model 3 (main model), greenness had a marked protective effect on CVD mortality risk at NDVI levels above 0.3 (HR = 0.87 [95% CI = 0.78, 0.97] per 0.1 increase) and no apparent effect at NDVI levels below 0.3 (HR = 1.00 [95% CI = 0.95, 1.04] per 0.1 increase). The protective effect at higher greenness levels was attenuated and no longer statistically significant when PM2.5 was added to the model (HR = 0.92 [95% CI = 0.82, 1.03] per 0.1 increase). In sensitivity analyses modeling NDVI within 250 m and 500 m buffers, associations were very similar (eTable 1; http://links.lww.com/EE/A179).
Table 2.
Independent associations of greenness, walkability, and PM2.5 with CVD mortality.
| Model | Covariates | Greenness, NDVI < 0.3, HRa (95% CI) | Greenness, NDVI ≥ 0.3, HRa (95% CI) | Walkability HRb (95% CI) | PM2.5, HRc (95% CI) |
|---|---|---|---|---|---|
| 1 | Aged, sex, study start year | 0.94 (0.91, 0.98) | 0.83 (0.75, 0.92) | 1.04 (1.01, 1.07) | 1.34 (1.21, 1.48) |
| 2 | Model 1 + race, comorbidities, BMI, smoking, CVD history, revascularization, medication use | 0.96 (0.92, 1.00) | 0.85 (0.76, 0.94) | 1.04 (1.01, 1.07) | 1.30 (1.18, 1.44) |
| 3 | Model 2 + SES | 1.00 (0.95, 1.04) | 0.87 (0.78, 0.97) | 1.03 (1.00, 1.05) | 1.20 (1.08, 1.33) |
| 4e | Model 3 + PM2.5 | 0.99 (0.95, 1.03) | 0.92 (0.82, 1.03) | 1.02 (0.99, 1.05) | 1.20 (1.08, 1.33)f |
| 5g | Model 4 + (greenness or walkability) | 1.00 (0.95, 1.05) | 0.93 (0.83, 1.04) | 1.02 (0.98, 1.05) | 1.20 (1.08, 1.33)h |
N = 83,560 and 8,820 CVD mortality events for all models without NDVI.
N = 83,408 and 8,799 CVD mortality events for all models with NDVI.
aHazard ratios per 0.1 increase in NDVI 1 km.
bHazard ratios per 5-unit increase in the Walkability Index.
cHazard ratios per 10 μg/m3 increase in PM2.5.
dAdjusted for age using Cox models with age as strata.
eModel 4 includes 2 environmental factors simultaneously.
fFor PM2.5 independent effects, model 4 = model 3 + greenness.
gModel 5 includes 3 environmental factors simultaneously.
hFor PM2.5 independent effects, model 5 = model 4 + walkability.
Figure 1.
Independent associations of greenness, walkability, and PM2.5with CVD mortality using restricted cubic splines. (A) greenness (N = 83,408), (B) walkability (N = 83,560), and (C) PM2.5 (N = 83,560), in models adjusted for age, sex, study start year, race, comorbidities, BMI, smoking, CVD history, revascularization, medication use, and SES.
Walkability was associated with a suggestive, slightly increased risk of CVD mortality in the minimally adjusted model (model 1) (HR = 1.04 [95% CI = 1.01, 1.07] per 5-unit increase). In the main model (model 3), this effect was attenuated and no longer statistically significant (HR = 1.03 [95% CI = 1.00, 1.05] per 5-unit increase, P = 0.072), with further attenuation once PM2.5 was added to the model (HR = 1.02 [95% CI = 0.99, 1.05] per 5-unit increase, model 4). We found no evidence of nonlinearity for the association between walkability and CVD mortality (Figure 1B, P = 0.790 for test of nonlinearity).
There was substantial increased risk of CVD mortality associated with PM2.5 exposure (HR = 1.20 [95% CI = 1.08, 1.33] per 10 μg/m3 increase in 1-year average PM2.5) (model 3), as we have reported previously.36 Furthermore, we found no change in these harmful effects after adjusting for greenness and walkability (models 4–5). The shape of association between PM2.5 and CVD mortality appeared to be linear (Figure 1C, P = 0.950). We found no violations of the proportional hazards for walkability, greenness, or PM2.5.
Joint effects
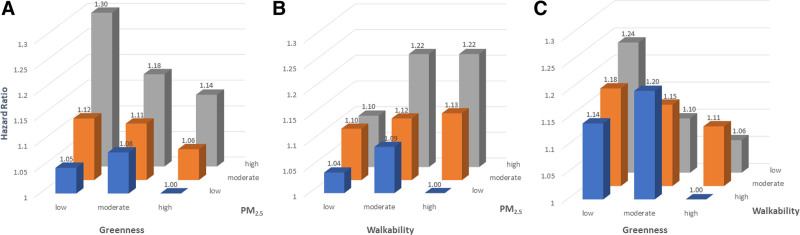
Joint effects of environmental variables are given in Figure 2 and eTable 2; http://links.lww.com/EE/A179. For the combined effects of PM2.5 and greenness, we found that living in an area of low greenness and high PM2.5 was associated with an increased risk of CVD mortality (HR = 1.30 [95% CI = 1.11, 1.52]) compared to living in an area of high greenness and low PM2.5 (Figure 2A and eTable 2; http://links.lww.com/EE/A179). We found no interaction between greenness and PM2.5 (P = 0.768), indicating that the combined effect of PM2.5 and greenness was driven by the strong independent effects of each environmental factor.
Figure 2.
Joint effects of greenness, walkability, and PM2.5 on CVD mortality risk. (A) greenness and PM2.5 (N = 83,408), (B) walkability and PM2.5 (N = 83,560), and (C) greenness and walkability (N = 83,408), in models adjusted for age, sex, study start year, race, comorbidities, BMI, smoking, CVD history, revascularization, medication use, and SES.
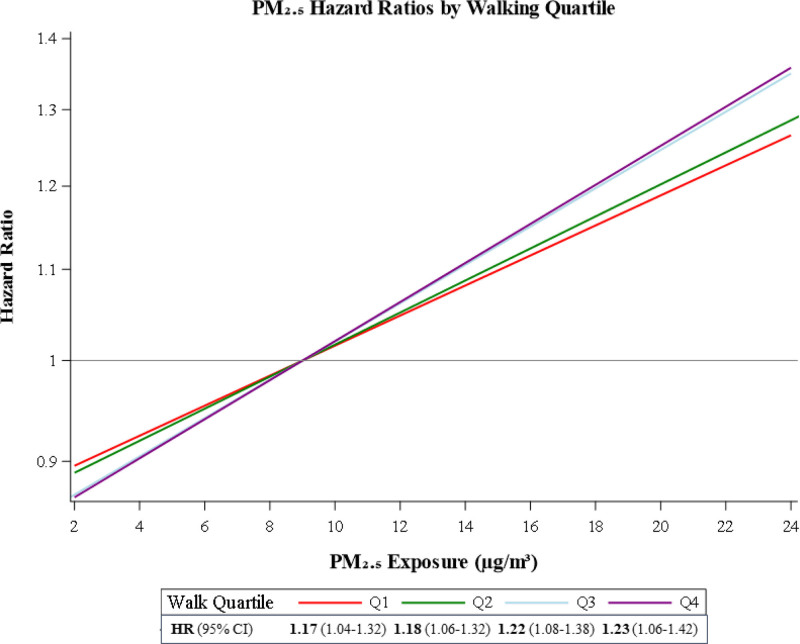
We found a statistically significant interaction between walkability and PM2.5 (P = 0.037). We highlight the very large difference in risk between living in a neighborhood with high walkability and high PM2.5 (HR = 1.22 [95% CI = 1.04, 1.43]) versus living in a neighborhood with high walkability and low PM2.5 (Figure 2B). To further illustrate this, we present the linear association between PM2.5 and CVD mortality by quartiles of walkability in Figure 3, since PM2.5 had a linear association with CVD mortality in the analyses of main effects. The deleterious effect of PM2.5 on CVD mortality was stronger in more walkable neighborhoods (HR = 1.23 [95% CI = 1.06, 1.42] for Q4) compared to less walkable neighborhoods (HR = 1.17 [95% CI = 1.04, 1.32] for Q1) per 10 μg/m3 increase in PM2.5. Results were very similar when additionally adjusting for greenness (eTable 3; http://links.lww.com/EE/A179). We found no interaction between greenness and walkability (P = 0.385). The number of subjects per category for joint effects is shown in eTable 4; http://links.lww.com/EE/A179. Sensitivity analyses restricted to people living in Census tracts with ≥1,000 persons per square mile showed little difference in effects, where the joint effect HRs of PM2.5/greenness and PM2.5/walkability were only slightly lower in areas with high greenness and high walkability (eTable 5; http://links.lww.com/EE/A179).
Figure 3.
Linear association of PM2.5 and CVD mortality by walkability quartile, in models adjusted for age, sex, study start year, race, comorbidities, BMI, smoking, CVD history, revascularization, medication use, and SES (N = 83,560). Overall PM2.5 hazard ratio = 1.19 (95% CI = 1.07, 1.32).
Although we found no evidence of a three-way interaction (P = 0.846) between walkability, PM2.5, and SES, the effect modification between walkability and PM2.5 appeared to be more pronounced in the lowest SES quartile. See the Supplement for further details (eTable 6; http://links.lww.com/EE/A179; eAppendix 1; http://links.lww.com/EE/A179).
Discussion
Among a susceptible population of adults with a history of prior stroke and/or AMI, we looked at the risk of CVD mortality and found strong protective effects of higher levels of greenness, with moderate attenuation of effects after adjusting for PM2.5 in models. We found no independent effect of walkability. We found a strong independent effect of PM2.5 that remained robust when controlling for greenness and walkability in models. In effect modification analyses, we found that increased risk of CVD mortality associated with PM2.5 varied by neighborhood walkability, where the harmful effects of long-term PM2.5 exposure were greater in more walkable settings. This suggests that highly walkable neighborhoods may not be as health fostering as we might expect after considering PM2.5 exposure in these settings.
Main effects
Previous research on the relation between greenness and CVD mortality is mixed.50 Some individual studies report no effect,51–54 while other studies report a decrease in risk per 0.1 increase in NDVI.55,56 Meta-analyses of the greenness–CVD mortality association have reported small pooled effect sizes10 or little to no effect.50,57 A recent review emphasizes that majority of the literature only looks at linear relationships between greenness and mortality and there is lack of data on the shape of the greenness–mortality relation.50 Our study discovered a nonlinear relation between greenness and CVD mortality, with prominent protective effects at higher levels of NDVI, and these associations could be overlooked in studies that only examine linear effects. Moreover, multiple studies have reported little change in effects on the greenness–CVD mortality association after adjusting for air pollution.10,51,55,58 The moderate attenuation in our study implies that PM2.5 may be a confounder of the greenness–CVD mortality association at higher greenness levels.
We found weak evidence of any association between walkability and CVD mortality. Similarly, two studies reported null associations between walkability indicators and CVD health measures, with small effect estimates in opposite directions.8,59 Other studies did found associations with other CVD outcomes, but in opposite directions as well. In more walkable neighborhoods, Hu et al. reported higher coronary artery calcium scores (a measure of atherosclerosis)25 and Yang et al reported lower risk of ischemic stroke.22 More research is needed to determine if there is an independent association between neighborhood walkability and CVD mortality.
The strong effects of PM2.5 on CVD mortality were unchanged after adjustment for walkability and greenness in models. Showing the cardiovascular health effects of PM2.5 with and without adjustment of these related environmental factors is an important contribution since review papers have found that there is a lack of air pollution studies that control for these variables in models.26,60 Our findings are consistent with four studies that found the independent effects of PM2.5 on CVD health risks remained robust or changed little after controlling for greenness and/or walkability.22,24,61,62
Joint effects
We found no evidence of effect modification by greenness on PM2.5 associated CVD mortality risk. Our finding is similar to a study in Korea that found no statistically significant interaction between long-term PM10 exposure and greenness on CVD mortality risk.28 However, two studies reported that in areas with more greenness, they found lower risk of cardiovascular hospitalization and all-cause mortality in association with short-term PM10 and long-term PM2.5, respectively, although PM particle size, time of exposure, and/or outcomes in these studies are different from ours.30,63 Additionally, another study found stronger associations between long-term PM2.5 and CVD hospitalization in areas with higher greenness, although they looked at hospitalizations and not deaths.64
We found a statistically significant interaction between neighborhood walkability and long-term PM2.5 exposure on CVD mortality risk, where the harmful effects of PM2.5 exposure were stronger in more walkable neighborhoods. Three other studies also found that more walkable neighborhoods were associated with higher CVD health risks as air pollution levels increased, though Hankey et al does not report a formal interaction and Howell et al. reported an interaction between NO2 and HTN and diabetes.21,22,31 On the contrary, one study analyzing short-term (2-day average) PM2.5 exposure and CVD mortality risk did not find evidence of effect modification by walkability.27 In comparison, our study looked at long-term (1-year average) PM2.5 exposure, which is identified as having stronger effects on CVD compared to short-term exposures,1 and this may be one factor influencing the difference in findings.
Mechanisms
Four proposed principal pathways by which greenness affects human health include: (1) improving air quality, (2) enhancing opportunities for physical activity, (3) reducing physiological stress, and (4) fostering greater social cohesion.10,65,66 Among individuals with existing CVD, residential greenness is associated with lower levels of sympathetic activation, reduced oxidative stress, and higher angiogenic capacity.67
We hypothesize that the higher PM2.5–associated CVD mortality risk observed in more walkable neighborhoods in our study may be due in part to increased exposure to PM2.5 during outdoor physical activity. Furthermore, the National Walkability Index is based partly on intersection density and proximity to transit stops where automobiles may be idling; thus, individuals walking in these areas may be exposed to higher air pollution. Mechanisms of the benefit–risk tradeoffs between increased outdoor exercise and increased exposure to air pollution have been researched among individuals with CVD.68,69 Physical activity in a less polluted area (park vs. street) can reduce arterial stiffness68 and have positive effects on stress levels and hemodynamic parameters.69 Thus, there are plausible mechanisms to support the effect modification by neighborhood walkability.
Strengths and limitations
We acknowledge several strengths of our study. To begin with, we have access to the large, highly detailed KPNC electronic health record which allows us to create a sizable cohort of individuals with previous CVD events and to control for numerous demographic, clinical, and lifestyle covariates in our analyses. Our large cohort size also enables us to achieve enough study power to conduct a variety of effect modification analyses. Another strength is our study design, a longitudinal retrospective cohort that follows subjects to time of CVD death or censored event, increasing the scientific rigor of our study. Furthermore, the availability of residential address data rather than only zip code-level data allowed individual-level linkage to high-resolution exposure data. Finally, our exposure data came from a sophisticated model for PM2.5 exposures with outstanding validation performance and a walkability index that has been previously validated with walking data.
We also acknowledge some limitations. First, although our study included residential location data on all participants, we did not have data on time spent at home, which could lead to exposure misclassification. However, adults in California have been shown to spend on average >65% of daily time at their home residence,70 and we would expect any exposure misclassification to be nondifferential. Second, although the National Walkability Index has been validated by walking data,16 it is based partly on intersection density and proximity to transit stops and may not be capturing some walking paths through greener, less dense areas. Third, our study did not include any individual-level data on physical activity or walking; therefore, we cannot rule out an ecologic association with neighborhood walkability. Fourth, we do not account for access to healthy food, neighborhood crime, sidewalk safety, physical activity facilities, or shade from street trees, all of which can influence the health effects of neighborhood walkability.71,72 Lastly, there are many causes of CVD and treatments for this disease, consequently our study population may not be representative of all different subjects with a prior AMI and/or stroke.
Conclusions
Air pollution, neighborhood walkability, and greenness are related to CVD, and their joint effects provide further insight into how interconnected environmental factors as a whole influence population health. In a population of adults with CVD history, we observed that high levels of greenness are associated with decreased CVD mortality risk, with some attenuation after controlling for PM2.5 exposure. PM2.5 had a strong association with increased risk of CVD mortality, and we found evidence of effect modification by neighborhood walkability but not greenness. Since the strength of the PM2.5 and CVD mortality association only varied slightly by level of neighborhood walkability, we note that although these small differences were statistically significant, they may not be clinically meaningful. Additional studies with individual-level physical activity data should be conducted to better understand this effect, since our study is based on neighborhood-level walkability only and does not include individual-level walking data. Urban planning decisions that increase the amount of greenness and decrease exposure to air pollution should be high public health priorities.
ACKNOWLEDGMENTS
Jun Shan from Kaiser Permanente Division of Research for linking geocoded residential addresses to NDVI data.
Conflicts of interest statement
The authors declare that they have no conflicts of interest with regard to the content of this report.
Supplementary Material
Footnotes
Published online 18 February 2022
Data sharing: Not available to protect patient confidentiality.
This work was supported by the National Institute of Environmental Health Sciences (NIEHS) grant R01 ES029557 Particulate Air pollution, Cardiovascular Events, and Susceptibility factors (PACES). The air pollution model development was supported by the U.S. Environmental Protection Agency grant RD 835872.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
References
- 1.Brook RD, Rajagopalan S, Pope CA, 3rd, et al.; American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. [DOI] [PubMed] [Google Scholar]
- 2.Agency USEP. U.S. EPA. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, 2019). EPA/600/R-19/188. 2019. [Google Scholar]
- 3.Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med. 2021;385:1881–1892. [DOI] [PubMed] [Google Scholar]
- 4.Chen H, Burnett RT, Copes R, et al. Ambient fine particulate matter and mortality among survivors of myocardial infarction: population-based cohort study. Environ Health Perspect. 2016;124:1421–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tonne C, Wilkinson P. Long-term exposure to air pollution is associated with survival following acute coronary syndrome. Eur Heart J. 2013;34:1306–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desikan A, Crichton S, Hoang U, et al. Effect of exhaust- and nonexhaust-related components of particulate matter on long-term survival after stroke. Stroke. 2016;47:2916–2922. [DOI] [PubMed] [Google Scholar]
- 7.Zanobetti A, Schwartz J. Particulate air pollution, progression, and survival after myocardial infarction. Environ Health Perspect. 2007;115:769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howell NA, Tu JV, Moineddin R, Chu A, Booth GL. Association between neighborhood walkability and predicted 10-year cardiovascular disease risk: the CANHEART (Cardiovascular Health in Ambulatory Care Research Team) Cohort. J Am Heart Assoc. 2019;8:e013146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seo S, Choi S, Kim K, Kim SM, Park SM. Association between urban green space and the risk of cardiovascular disease: a longitudinal study in seven Korean metropolitan areas. Environ Int. 2019;125:51–57. [DOI] [PubMed] [Google Scholar]
- 10.Gascon M, Triguero-Mas M, Martínez D, et al. Residential green spaces and mortality: a systematic review. Environ Int. 2016;86:60–67. [DOI] [PubMed] [Google Scholar]
- 11.Nieuwenhuijsen MJ. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat Rev Cardiol. 2018;15:432–438. [DOI] [PubMed] [Google Scholar]
- 12.Hirsch JA, Moore KA, Clarke PJ, et al. Changes in the built environment and changes in the amount of walking over time: longitudinal results from the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2014;180:799–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sallis JF, Cerin E, Conway TL, et al. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet. 2016;387:2207–2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thielman J, Manson H, Chiu M, Copes R, Rosella LC. Residents of highly walkable neighbourhoods in Canadian urban areas do substantially more physical activity: a cross-sectional analysis. CMAJ Open. 2016;4:E720–E728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rundle AG, Chen Y, Quinn JW, et al. Development of a neighborhood walkability index for studying neighborhood physical activity contexts in communities across the U.S. over the past three decades. J Urban Health. 2019;96:583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watson KB, Whitfield GP, Thomas JV, Berrigan D, Fulton JE, Carlson SA. Associations between the National Walkability Index and walking among US Adults - National Health Interview Survey, 2015. Prev Med. 2020;137:106122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith M, Hosking J, Woodward A, et al. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saelens BE, Handy SL. Built environment correlates of walking: a review. Med Sci Sports Exerc. 2008;40(7 Suppl):S550–S566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.James P, Hart JE, Laden F. Neighborhood walkability and particulate air pollution in a nationwide cohort of women. Environ Res. 2015;142:703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marshall JD, Brauer M, Frank LD. Healthy neighborhoods: walkability and air pollution. Environ Health Perspect. 2009;117:1752–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hankey S, Marshall JD, Brauer M. Health impacts of the built environment: within-urban variability in physical inactivity, air pollution, and ischemic heart disease mortality. Environ Health Perspect. 2012;120:247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang Z, Wu M, Lu J, et al. Interaction between walkability and fine particulate matter on risk of ischemic stroke: a prospective cohort study in China. Environ Pollut. 2022;292(Pt B):118482. [DOI] [PubMed] [Google Scholar]
- 23.Shuvo FK, Mazumdar S, Labib SM. Walkability and greenness do not walk together: investigating associations between greenness and walkability in a large metropolitan city context. Int J Environ Res Public Health. 2021;18:4429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark C, Sbihi H, Tamburic L, Brauer M, Frank LD, Davies HW. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: a prospective cohort study. Environ Health Perspect. 2017;125:087025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu HB, Hou ZH, Huang CH, LaMonte MJ, Wang M, Lu B. Associations of exposure to residential green space and neighborhood walkability with coronary atherosclerosis in Chinese adults. Environ Pollut. 2022;292(Pt A):118347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rugel EJ, Brauer M. Quiet, clean, green, and active: a Navigation Guide systematic review of the impacts of spatially correlated urban exposures on a range of physical health outcomes. Environ Res. 2020;185:109388. [DOI] [PubMed] [Google Scholar]
- 27.Yitshak-Sade M, James P, Kloog I, et al. Neighborhood greenness attenuates the adverse effect of PM2.5 on cardiovascular mortality in neighborhoods of lower socioeconomic status. Int J Environ Res Public Health. 2019;16:E814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim S, Kim H, Lee JT. Interactions between ambient air particles and greenness on cause-specific mortality in seven Korean metropolitan cities, 2008-2016. Int J Environ Res Public Health. 2019;16:1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vivanco-Hidalgo RM, Wellenius GA, Basagaña X, et al. Short-term exposure to traffic-related air pollution and ischemic stroke onset in Barcelona, Spain. Environ Res. 2018;162:160–165. [DOI] [PubMed] [Google Scholar]
- 30.Heo S, Bell ML. The influence of green space on the short-term effects of particulate matter on hospitalization in the U.S. for 2000-2013. Environ Res. 2019;174:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Howell NA, Tu JV, Moineddin R, et al. Interaction between neighborhood walkability and traffic-related air pollution on hypertension and diabetes: the CANHEART cohort. Environ Int. 2019;132:104799. [DOI] [PubMed] [Google Scholar]
- 32.Organization WH. Prevention of Recurrences of Myocardial Infarction and Stroke Study. World Health Organization. Updated 2020. Available at: https://www.who.int/cardiovascular_diseases/priorities/secondary_prevention/country/en/index1.html. Accessed June 1, 2020. [Google Scholar]
- 33.Gordon N. Similarity of adult Kaiser Permanente members to the adult population in Kaiser Permanente’s Northern California service area: Comparisons based on the 2017/2018 cycle of the California Health Interview Survey. Research KPDo; 2020. November 8, 2020. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/compare_kp_ncal_chis2017-18.pdf [Google Scholar]
- 34.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NP G. Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011-12 California Health Interview Survey. 2015. June 2015. http://www.dor.kaiser.org/external/chis_non_kp_2011/
- 36.Liao NS, Sidney S, Deosaransingh K, Van Den Eeden SK, Schwartz J, Alexeeff SE. Particulate air pollution and risk of cardiovascular events among adults with a history of stroke or acute myocardial infarction. J Am Heart Assoc. 2021;10:e019758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agency USEP. Walkability Index. United States Environmental Protection Agency. 2021. Available at: https://edg.epa.gov/metadata/catalog/search/resource/details.page?uuid=%7B251AFDD9-23A7-4068-9B27-A3048A7E6012%7D. Accessed March 1, 2021. [Google Scholar]
- 38.Agency USEP. What is Open Space/Green Space? United States Environmental Protection Agency. Updated April 10, 2017. 2022. Available at: https://www3.epa.gov/region1/eco/uep/openspace.html. Accessed January 7, 2022. [Google Scholar]
- 39.Fong KC, Hart JE, James P. A Review of Epidemiologic Studies on Greenness and Health: Updated Literature Through 2017. Curr Environ Health Rep. 2018;5:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Observatory NE. Normalized Difference Vegetation Index (NDVI). NASA. Updated August 30, 2020. 2022. Available at: https://earthobservatory.nasa.gov/features/MeasuringVegetation/measuring_vegetation_2.php. Accessed January 6, 2022. [Google Scholar]
- 41.Di Q, Amini H, Shi L, et al. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ Int. 2019;130:104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Statistics CNCfH. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). CDC. Updated December 16, 2021. 2021. https://www.cdc.gov/nchs/icd/icd10cm.htm. [Google Scholar]
- 43.Weichenthal S, Villeneuve PJ, Burnett RT, et al. Long-term exposure to fine particulate matter: association with nonaccidental and cardiovascular mortality in the agricultural health study cohort. Environ Health Perspect. 2014;122:609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turner MC, Cohen A, Burnett RT, et al. Interactions between cigarette smoking and ambient PM2.5 for cardiovascular mortality. Environ Res. 2017;154:304–310. [DOI] [PubMed] [Google Scholar]
- 45.Lipsett MJ, Ostro BD, Reynolds P, et al. Long-term exposure to air pollution and cardiorespiratory disease in the California teachers study cohort. Am J Respir Crit Care Med. 2011;184:828–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. [DOI] [PubMed] [Google Scholar]
- 47.Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–458. [DOI] [PubMed] [Google Scholar]
- 48.Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology. 2013;24:44–53. [DOI] [PubMed] [Google Scholar]
- 49.Hoffmann B, Weinmayr G, Hennig F, et al. Air quality, stroke, and coronary events: results of the Heinz Nixdorf Recall study from the Ruhr region. Dtsch Arztebl Int. 2015;112:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bertrand C, Pascal M, Médina S. Do we know enough to quantify the impact of urban green spaces on mortality? An analysis of the current knowledge. Public Health. 2021;200:91–98. [DOI] [PubMed] [Google Scholar]
- 51.Villeneuve PJ, Jerrett M, Su JG, et al. A cohort study relating urban green space with mortality in Ontario, Canada. Environ Res. 2012;115:51–58. [DOI] [PubMed] [Google Scholar]
- 52.Mitchell R, Popham F. Effect of exposure to natural environment on health inequalities: an observational population study. Lancet. 2008;372:1655–1660. [DOI] [PubMed] [Google Scholar]
- 53.James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124:1344–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lachowycz K, Jones AP. Does walking explain associations between access to greenspace and lower mortality? Soc Sci Med. 2014;107:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vienneau D, de Hoogh K, Faeh D, Kaufmann M, Wunderli JM, Röösli M; SNC Study Group. More than clean air and tranquillity: residential green is independently associated with decreasing mortality. Environ Int. 2017;108:176–184. [DOI] [PubMed] [Google Scholar]
- 56.Wang D, Lau KK, Yu R, Wong SYS, Kwok TTY, Woo J. Neighbouring green space and mortality in community-dwelling elderly Hong Kong Chinese: a cohort study. BMJ Open. 2017;7:e015794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yuan Y, Huang F, Lin F, Zhu P, Zhu P. Green space exposure on mortality and cardiovascular outcomes in older adults: a systematic review and meta-analysis of observational studies. Aging Clin Exp Res. 2021;33:1783–1797. [DOI] [PubMed] [Google Scholar]
- 58.Chen H, Burnett RT, Bai L, et al. Residential greenness and cardiovascular disease incidence, readmission, and mortality. Environ Health Perspect. 2020;128:87005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Griffin BA, Eibner C, Bird CE, et al. The relationship between urban sprawl and coronary heart disease in women. Health Place. 2013;20:51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alexeeff SE, Liao NS, Liu X, Van Den Eeden SK, Sidney S. Long-term PM2.5 exposure and risks of ischemic heart disease and stroke events: review and meta-analysis. J Am Heart Assoc. 2021;10:e016890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Crouse DL, Pinault L, Balram A, et al. Complex relationships between greenness, air pollution, and mortality in a population-based Canadian cohort. Environ Int. 2019;128:292–300. [DOI] [PubMed] [Google Scholar]
- 62.Klompmaker JO, Janssen NAH, Bloemsma LD, et al. Associations of combined exposures to surrounding green, air pollution, and road traffic noise with cardiometabolic diseases. Environ Health Perspect. 2019;127:87003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Son JY, Sabath MB, Lane KJ, et al. Long-term exposure to PM2.5 and mortality for the older population: effect modification by residential greenness. Epidemiology. 2021;32:477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Klompmaker JO, Hart JE, James P, et al. Air pollution and cardiovascular disease hospitalization - are associations modified by greenness, temperature and humidity? Environ Int. 2021;156:106715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Europe CWROf. Urban green spaces and health. 2016. https://www.euro.who.int/__data/assets/pdf_file/0005/321971/Urban-green-spaces-and-health-review-evidence.pdf
- 66.Markevych I, Schoierer J, Hartig T, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301–317. [DOI] [PubMed] [Google Scholar]
- 67.Yeager R, Riggs DW, DeJarnett N, et al. Association between residential greenness and cardiovascular disease risk. J Am Heart Assoc. 2018;7:e009117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sinharay R, Gong J, Barratt B, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study. Lancet. 2018;391:339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grazuleviciene R, Vencloviene J, Kubilius R, et al. Tracking restoration of park and urban street settings in coronary artery disease patients. Int J Environ Res Public Health. 2016;13:E550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Klepeis NE, Nelson WC, Ott WR, et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001;11:231–252. [DOI] [PubMed] [Google Scholar]
- 71.Paulo Dos Anjos Souza Barbosa J, Henrique Guerra P, de Oliveira Santos C, de Oliveira Barbosa Nunes AP, Turrell G, Antonio Florindo A. Walkability, overweight, and obesity in adults: a systematic review of observational studies. Int J Environ Res Public Health. 2019;16:E3135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stangl P. The US pedestrian plan: linking practice and research. Plan Pract Res. 2011;26:289–305. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.