Abstract
Introduction
The COVID-19 pandemic has impacted healthcare on an unprecedented scale, with healthcare resources being channeled into managing the devastating effects of the outbreak. Healthcare provision for vulnerable older adults has also been affected by lockdowns and suspension of selected medical services worldwide. In our tertiary cancer center, the National University Cancer Institute, Singapore (NCIS), our Geriatric Oncology (GO) service for older adults with cancer was halted for five months. In this paper, we describe the adoption of a hybrid telemedicine model by our GO service to continue care provision for older adults in the midst of the pandemic.
Materials and Methods
Comprehensive geriatric assessments (CGA) were done via telemedicine and virtual multidisciplinary discussions were held prior to the patients' clinic visits. A hybrid telemedicine consultation allowed geriatricians and oncologists, segregated in different sites during the pandemic, to provide a hybrid physical and video geriatric oncology consultation. Scheduled phone follow ups by GO nurses helped to monitor patients for treatment-related toxicities and geriatric syndromes.
Results
Two hundred fifty patients were enrolled in the program from July 2020 to August 2021. All were assessed with a CGA, with 240 receiving interventions in the one-stop clinic.
The average amount of time spent per visit was shortened from four hours to two and a half hours with an average of three interventions on the same day, versus one previously.
Of the patients who received interventions, 84.8% were satisfied with the hybrid telemedicine model and 80.8% of them had reported a maintained or improved quality of life after being enrolled in the program.
Discussion
Telemedicine has been widely adopted during the pandemic, but older adults with limited digital literacy may find it a challenge. Our hybrid telemedicine model has allowed us to continue to provide cancer care, identify issues brought about by social isolation, and render timely assistance. It has become imperative to adapt, prepare and plan for the challenges we may face amid the ongoing COVID-19 pandemic and similar future outbreaks. Only by doing so can we remain agile and resilient, to continue providing quality care to our older patients with cancer.
Keywords: Geriatric oncology, COVID19, Telemedicine, Pandemic, Telehealth
1. Introduction
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic on 11 March 2020. To date, COVID-19 has affected more than 230 regions/countries, with more than 242 million confirmed cases, and close to five million deaths globally [1]. The impact of the disease is multifaceted and devastating on a global scale, with countries adopting varying strategies and approaches to management as the understanding of the disease evolves, and vaccinations and treatments become available.
Older adults with COVID-19 are at particularly risk of adverse outcomes including severe illness, hospitalization, and death [2,3]. Those who are frail or have underlying cancer or multimorbidity are more likely to develop critical illness [4]. Public health measures such as safe distancing, hand hygiene, and mask wearing are key to safeguarding this vulnerable population.
These measures are especially relevant for countries with rapidly aging populations like Singapore, a multi-ethnic independent city-state with the second densest population in the world. Leveraging prior experience following the Severe Acute Respiratory Syndrome (SARS) epidemic in 2003, Singapore entered the preparedness phase, which saw the development of communicable disease detection and surveillance programs, the planning of infrastructure including healthcare facilities that can cope with a major infectious disease outbreak, and the stockpiling of medications and personal protective equipment (PPE) [5]. This was followed by the readiness phase when the first guidance was distributed by the Ministry of Health (MOH) in January 2020, and various processes in the healthcare system were reviewed, with disease testing put in place when it became available. In early February 2020, Singapore entered the response phase with heightened surveillance, border control, containment protocols, and widespread contact tracing. A nationwide “Circuit Breaker” measure was implemented from 7 April 2020 to 1 June 2020 with shutdown of multiple services to further curb community transmission.
Our healthcare system had to actively reduce physical ambulatory clinic visits and turn to alternatives such as telemedicine. This led to a direct impact on our tertiary cancer center, the National University Cancer Institute, Singapore (NCIS), which is a comprehensive academic cancer center that manages 7000 adult and pediatric outpatients per month [6] While telemedicine is an effective solution to continuing medical care during the pandemic, there are also challenges with implementation given lower levels of digital literacy in a proportion of older adults. The resilience of our health system, which is the ability to prepare for and respond to crises by reorganizing systems to manage new conditions while maintaining core functions, was put to the test [6].
In this paper, we will describe how our Geriatric Oncology (GO) service was disrupted, and how we adapted our care model using a hybrid telemedicine workflow in order to remain agile and resilient in the pandemic, and continue to provide quality cancer care to our older patients with cancer. With more than 80% of the population now vaccinated against COVID-19 and the announcement on 9 October 2021 of Singapore heading towards COVID-resiliency through the streamlining of protocols in the healthcare system [7], we will also share our plans moving forward in order to provide a sustainable and effective service for older adults with cancer in the post-vaccination era.
2. The Geriatric Oncology Longitudinal End to eNd (GOLDEN) Program
The NCIS GO service is made up of a multidisciplinary team comprising geriatricians, oncologists, advanced nurse practitioner, nurses, care coordinators, pharmacists, medical social workers (MSW), physiotherapists (PT), occupational therapists (OT), and dietitians.
The Geriatric Oncology Longitudinal End to End (GOLDEN) Program was started in two restructured hospitals, NCIS and Ng Teng Fong General Hospital (NTFGH) in 2019. It is a service providing end-to-end clinical care from cancer diagnosis to treatment by the NCIS GO team.
The program comprises:
-
1.
A Comprehensive Geriatric Assessment (CGA) of an older patient's health status and fitness for cancer treatment,
-
2.
A Management and Innovation for Longevity in Elderly Surgical Patients (MILES) Surgical pre-rehabilitation program for patients planned for cancer surgery,
-
3.
Tailored interventions by a multidisciplinary team of geriatricians, oncologists, oncology nurses, care coordinators, medical social workers, dietitians, pharmacists, physiotherapists and occupational therapists,
-
4.
Transfer of care to the NCIS GO team post-surgery with a reassessment CGA post-surgery prior to initiation of chemotherapy or systemic therapy.
-
5.
Telemedicine follow-up by nurses on patients' health status and monitoring of treatment side effects during cancer treatment.
3. GOLDEN Workflow Prior to the Pandemic
All patients with cancer aged 65 years and above who were seen in either NCIS or NTFGH would be screened on their first visit with a Geriatric 8 (G8) questionnaire [8,9] to identify patients who might benefit from a CGA with directed interventions and care. An electronic memo would be sent to the primary oncologist (surgical oncology, medical oncology and radiation oncology) through the hospital's electronic medical records if the G8 score ≤ 14. Additionally, the primary oncologists could also directly refer their patients to the GO team for a geriatric oncology consultation.
Patients who were referred to the GOLDEN program would undergo a CGA during their initial visit to the NCIS and NTFGH GO Clinics.
-
1.
Patients and the accompanying next-of-kin or caregiver would be interviewed by the GO case manager or nurse on-site and undergo several screening assessments.
-
2.
This was followed by a medication review and reconciliation by the GO pharmacist.
-
3.
The patient would then proceed with a medical consultation with both an oncologist and a geriatrician.
-
4.
A referral would be made to the allied health professionals by the doctors if necessary, who would review the patient thereafter.
This entire process was time-consuming and tiring for the older person and their caregivers as each visit could last four hours or more. Consequently, a significant number of patients declined referrals to allied health, which were planned only after the doctors' consultation.
When the COVID-19 pandemic first broke out in 2020, NCIS had to adopt a segregated team workflow and cease inter-hospital staff movement to minimize transmission risk. The GOLDEN program had to be suspended for five months between January 2020 to June 2020 as a result. As these restrictions gradually lifted, the GOLDEN program in NUH and NTFGH resumed in July 2020.
Over the subsequent months, restrictions in inter-hospital movement of healthcare workers and segregation of healthcare teams within the hospital were intermittently imposed, depending on the epidemiological trend of COVID-19 infection nationwide. The GO multidisciplinary team had to be agile and continuously modified existing workflows to continue caring for the geriatric oncology population in two healthcare institutions amidst a changing landscape.
4. Materials and Methods
4.1. Adopting Telemedicine for the GOLDEN Care Model during the COVID-19 Pandemic
4.1.1. Pre-Clinic Assessment and Medication Reconciliation conducted via Telemedicine
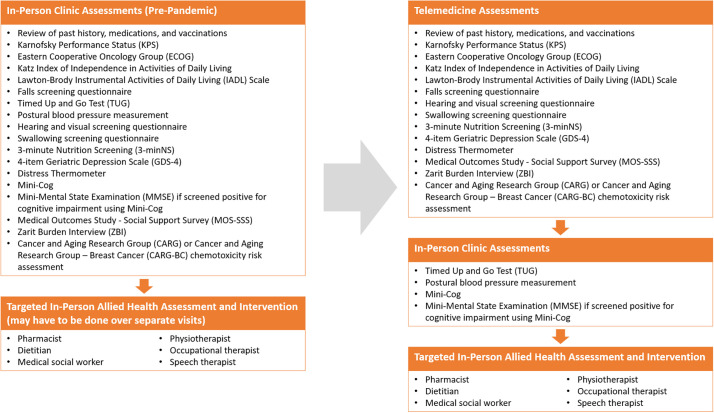
Telemedicine was adopted to minimize time spent by patients and their caregivers in the GO clinic (Fig. 1 ). In Singapore, telemedicine refers to the provision of healthcare services using information and communications technology across physically separate environments, and it includes the exchange of information for clinical purposes between healthcare providers and patients/caregivers over telephone, text messages, and video/audio platforms [10].
Fig. 1.
Change in clinic assessment workflow before (left) and after (right) telemedicine adoption.
A selected portion of the CGA was conducted remotely via a telephone or video call for selected patients by the GO nurse, coordinator and pharmacist up to two days prior to the GO clinic appointment. The GO coordinator contacted the patient prior to the teleconsult to arrange a suitable timing for the consult with the patients and their caregivers. Verbal consent was obtained and the patient/caregiver was interviewed on his/her medical comorbidities, adherence to medications, functional ability, nutritional and emotional status and social circumstances. This telemedicine pre-clinic evaluation took approximately 30 to 45 min to complete.
The GO pharmacist would also obtain the patient's active medication list and vaccination status from the National Electronic Health Records (NEHR), and check if the patient was taking the medications as prescribed.
With the information from the initial assessment, a patient's risk of chemotherapy related toxicities would be calculated using the Cancer and Aging Research (CARG) [11,12] or Cancer and Aging Research - Breast Cancer (CARG-BC) [13] chemotoxicity calculators.
Objective assessments that could only be done in person (e.g. cognitive assessments, timed up and go (TUG), postural blood pressure measurement) were performed on the day of the GO clinic consultation itself to complete the remainder of the CGA.
4.1.2. Virtual Pre-clinic GO Multidisciplinary Team discussion
A weekly multidisciplinary team meeting, using a secure online video communication platform, was held before every GO clinic session. The team discussed all patients who completed the pre-clinic telemedicine assessment and made preliminary plans for every patient before they were physically seen. After the initial assessment, the cases were again discussed in the virtual team meeting prior to their follow-up visit, which typically occurred within a month.
4.1.3. Hybrid Telemedicine Clinic Model
Originally, the doctors had to shuttle between sites to run GO clinics in two geographically separate healthcare institutions. During the pandemic, restrictions were imposed on the movement of healthcare workers between hospitals in Singapore to minimize transmission risk, which posed a significant challenge to the program.
A hybrid tele-consultation model was piloted and implemented to overcome this limitation. Instead of having both a geriatrician and an oncologist present physically on site, only one doctor was required to be physically present during the clinic consultation with the patient. The other doctor would join in the consultation remotely via a video communication platform set up concurrently in the physical clinic. The patient would hence be able to consult both the geriatrician and oncologist in the same clinic session and be involved in the joint decision-making process. In this way, this hybrid teleconsultation model allowed the GOLDEN program to continue supporting patients during the pandemic despite the movement restrictions imposed on healthcare workers between institutions.
4.1.4. Scheduled GO Nurse Phone follow-up on Treatment-Related Toxicities and Geriatric Syndromes
During the initial four months from the commencement of cancer therapy, the GO nurses performed follow-up phone calls every two weeks to assess for treatment-related toxicities graded with the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 [14]. The patients and caregivers were also assessed to ensure that they were coping well in the community. Each call lasted approximately twenty minutes.
GO patients who developed grade 3 or higher toxicities and worsening frailty during the phone follow-ups would be identified by the GO nurses, who then informed their primary oncologists for an early review in the clinic. If patients had grade 1–2 toxicities, they were given advice on how to manage and red flags to watch out for. As there were no follow-up phone calls by the treating oncology team, it is crucial for our GO nurses to detect the grade 3 toxicities, as older adults have limited physiological reserves and may deteriorate rapidly if timely treatment is not instituted.
Patients who were deemed to be at a higher risk of grade 3–5 toxicities continued to be followed up by the GO nurses beyond the first four months of treatment.
Our nurses also evaluated patients' quality of life using the EORTC QLQ-C30 questionnaire [15] in the first and third month to ensure that they were coping appropriately and adapting well to any treatment-induced changes to their lifestyle. An overview of the GO hybrid telemedicine workflow is shown below in Fig. 2 .
Fig. 2.
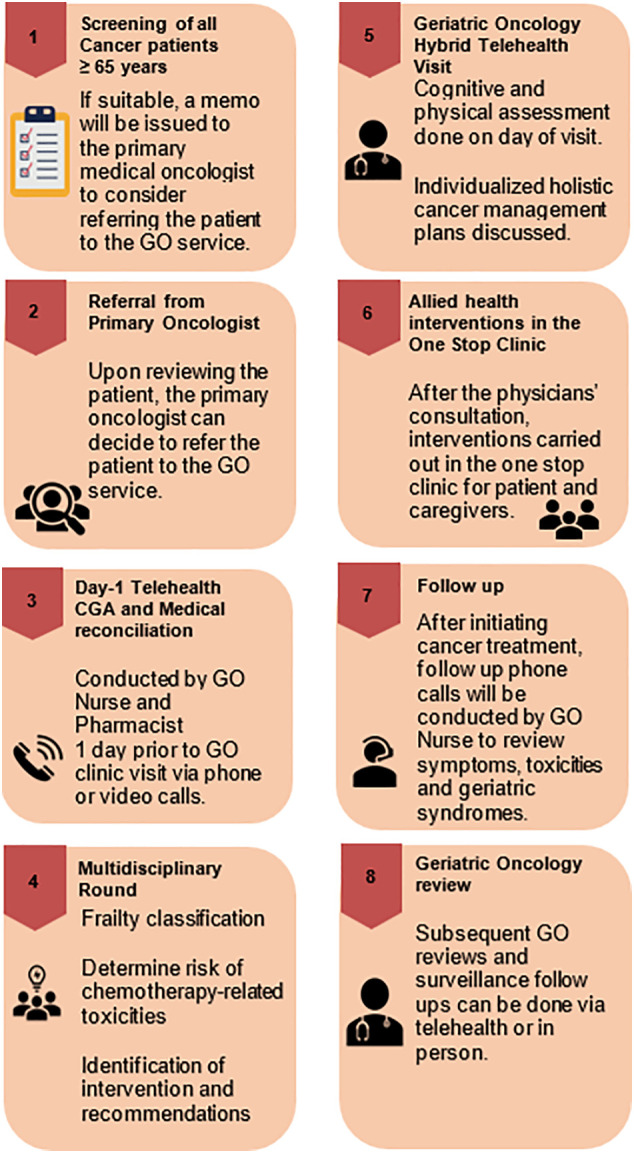
Overview of Geriatric Oncology Hybrid Telemedicine Clinic Visit and Follow-Up.
This study was approved by the National University Hospital (NUH) Institutional Ethics Review Board.
5. Results
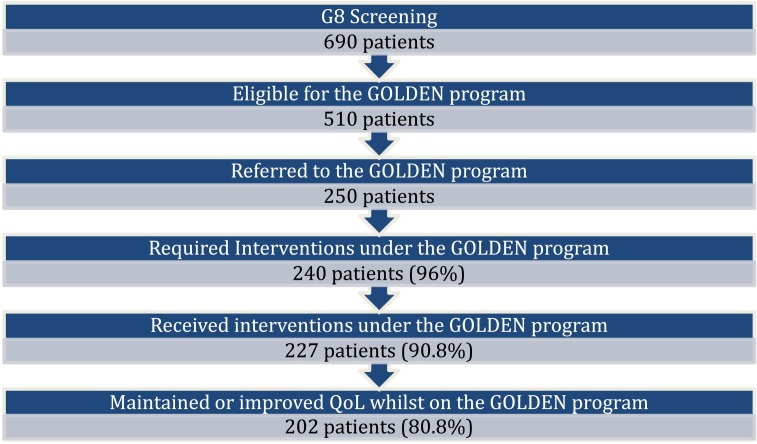
The GOLDEN program resumed in NCIS in July 2020 and in NTFGH in August 2020. Over a period of one year since resuming the program during the pandemic, 690 patients were screened with G8, of which 510 (73.9%) patients were eligible and 250 (36.2%) patients were referred to the GOLDEN program (Fig. 3 ).
Fig. 3.
Screening and recruitment of patients into the GOLDEN program.
Table 1 shows the characteristics of the patients referred to the GOLDEN program. The mean age was 75.3 +/− 6.2 years. Most of the patients were Chinese (86.8%). Two-thirds of the patients had early stage cancer, with lower gastrointestinal cancers being the most commonly diagnosed tumor type. Almost three-quarters were pre-frail (72.8%), one-fifth were frail (19.2%) and the remainder were fit (8.0%). The median G8 score was 11 (range 2–16). About three-quarters of the patients (73.8%) received treatment, of which 134 (54.0%) were of curative intent and 49 (19.8%) were of palliative intent.
Table 1.
Patient characteristics.
| Characteristics | Patients referred to GOLDEN program (n = 250) |
|---|---|
| Age | |
| 65–69 years | 34 (13.6%) |
| 70–74 years | 93 (37.2%) |
| 74–79 years | 59 (23.6%) |
| 80–84 years | 47 (18.8%) |
| ≥ 85 years | 17 (6.8%) |
| Age, mean | 75.3 (±6.2 years) |
| Gender | |
| Female | 117 (46.8%) |
| Male | 133 (53.2%) |
| Ethnicity | |
| Chinese | 217 (86.8%) |
| Malay | 23 (9.2%) |
| Indian | 6 (2.4%) |
| Others | 4 (1.6%) |
| Tumor type | |
| Lower gastrointestinal | 102 (40.8%) |
| Hepatobiliary | 42 (16.8%) |
| Thoracic | 31 (12.4%) |
| Genitourinary | 20 (8.0%) |
| Breast | 17 (6.8%) |
| Head and neck | 13 (5.2%) |
| Upper gastrointestinal | 10 (4.1%) |
| Gynecological | 6 (2.4%) |
| Sarcoma | 5 (2.0%) |
| Others | 5 (2.0%) |
| Metastatic disease | |
| No | 171 (68.4%) |
| Yes | 79 (31.6%) |
| Level of education | |
| None | 31 (12.4%) |
| Primary | 116 (46.4%) |
| Secondary | 78 (31.2%) |
| Tertiary | 25 (10.0%) |
| Living arrangements | |
| Alone | 21 (8.4%) |
| With family | 221 (88.4) |
| With others | 8 (3.2%) |
| G8 score, mean (SD) | 11 (2.64) |
| Frailty state | |
| Fit | 20 (8.0%) |
| Pre-frail | 182 (72.8%) |
| Frail | 48 (19.2%) |
Abbreviations: G8: Geriatric 8 questionnaire, SD: standard deviation.
The majority of patients (96.0%) required upstream interventions by our multidisciplinary allied health team of pharmacists, medical social workers, physiotherapist, and occupational therapist as recommended in the one-stop GOLDEN clinic (Table 2 ).
Table 2.
Patients with interventions by allied health professionals in the GOLDEN program.
| Interventions | Allied health professionals | Patients (N = 250) |
|---|---|---|
| Medication reconciliation and review | Pharmacist | 237 (95.6%) |
| Psychosocial and financial support | Medical social worker | 162 (65.3%) |
| Nutrition advice | Dietician | 126 (50.8%) |
| Falls prevention and activity adaptation | Occupational therapist | 72 (29.0%) |
| Exercise recommendation | Physiotherapist | 70 (28.2%) |
| Swallowing assessment and management | Speech therapist | 4 (1.6%) |
The average amount of time spent in the hospital per visit was shortened from four hours to two and one-half hours, with an average of three interventions on the same day versus one intervention previously in the one-stop clinic.
A proportion of the older adults were unable to participate in telehealth due to barriers such as impaired hearing, cognitive impairment, and limited digital literacy, but this was overcome by taking a corroborative history from their caregivers.
The majority of the patients who received interventions in the GOLDEN program (84.8%) were satisfied with the hybrid telemedicine model. The 227 patients who received interventions were followed up for quality of life (QOL) assessment using the EORTC QLQ-C30 questionnaire, of which 70 patients (33.9%) reported an overall improvement in their global health status, while 132 patients (58.1%) maintained their global health status after being enrolled in the GOLDEN program.
6. Discussion
The population of older adults with cancer is heterogeneous and requires a careful and tailored approach to care that considers frailty, a syndrome which in itself has been associated with an elevated risk of adverse outcomes [16,17]. The COVID-19 pandemic has disproportionately impacted older adults globally due to ageism, social isolation, loneliness, and higher threats of illness including mental health problems, leading to multiple unmet needs [18,19]. With safe distancing measures and restrictions on ambulatory healthcare and rehabilitation services, the pandemic also created barriers to geriatric oncology care by potentially leading to cancelled, missed, or delayed appointments, making the performance of comprehensive geriatric assessments challenging and causing treatment delays [18].
Our GOLDEN multidisciplinary team had to rapidly adopt a hybrid telemedicine model of care to overcome these barriers in order to continue providing our service to older adults with cancer during the pandemic. We have learnt that well-established geriatric oncology centers like the University of Rochester SO-CARE clinic had also adapted a telehealth geriatric assessment model in response to the COVID-19 pandemic. [20]
Despite screening all older adults in our cancer center for frailty with G8, only about half of the eligible patients were referred to the GOLDEN program. This could be attributed to the slow recognition of the need of a GO service by the primary physicians and patient factors, as many were reluctant to return for an additional visit to the hospital during the pandemic.
With a selected portion of the CGA done prior to the physical clinic visit, and with both geriatricians and oncologists co-consulting in the hybrid telemedicine model, the amount of time spent by the patients and their caregivers in the clinic was shortened. This minimized the potential exposure and infection risk to patients and caregivers. The time saved also allowed for additional tailored interventions by other allied health professionals to be carried out in the same visit to the one-stop clinic. This saved the patients and their caregivers direct and indirect costs of multiple visits for assessments by allied health professionals, leading to improved value driven outcomes.
Anxiety, while a normal response to a perceived threat, has been shown to be prevalent in older adults with cancer and is known to rise in response to additional threats such as surgery and disease progression [21,22]. In the context of COVID-19, with potential delays in diagnosis and initiation of treatment, disruptions in ongoing treatment and supportive care, this issue has become all the more relevant [23]. By engaging with patients and their caregivers earlier in the treatment journey starting with a telephone or video call, the GO team members were able to establish rapport earlier and elicit and address their concerns sooner. We have observed more than half of our patients reporting an improvement in their quality of life, though we are unable to make positive associations due to limitations of our study.
While we have found some success with our hybrid telemedicine model for the GOLDEN program in terms of reduction of time spent in clinic and cost, and a high level of patient satisfaction, we also faced some limitations. Some older adults found it difficult to comprehend some of the interview questions that were posed over telemedicine owing to barriers such as impaired hearing and vision, cognitive impairment, and limited digital literacy. We overcame these limitations as best as we could by engaging family members and caregivers who could assist our older patients during telemedicine sessions.Our study was also not designed to investigate how these barriers affected participation in telemedicine in our population, and this should be looked at in future studies.
Of note, digital literacy remains a significant challenge amongst older adults globally, with the proportion of older adults using digital technology being less than younger adults, though it is rising exponentially [24]. According to a 2019 survey by the Infocomm Media Development and Authority (IMDA), which is a statutory board under the Singaporean government, 58% of Singaporean residents aged 60 and above were internet users compared to 89% for all residents [25]. These figures are comparable to the findings of the Organization for Economic Cooperation and Development (OECD), with 63% of internet users being aged 55–74 years compared to 97% in 16–24-year-olds [26].
There has been a nationwide push to strengthen digital literacy across all age groups through the Digital Media and Information Literacy Framework as part of Singapore's Digital Readiness vision to be a Smart Nation, which has accelerated due to the pandemic [27]. The IMDA launched a “Seniors Go Digital” initiative at the height of the pandemic in May 2020 to equip older adults with skills such as using digital tools for video calls, with digital ambassadors being made readily available for them to do so [28], which will hopefully help them to overcome the barrier of digital illiteracy in the future. As part of the “Seniors Go Digital” initiative, a “Mobile Access for Seniors” scheme has also been put in place to provide subsidized smartphone and mobile plans to older adults who wish to go digital but are unable to afford them [29]. As we have begun to see the benefits of our hybrid telemedicine model during this pandemic, we perceive these initiatives to be an important step in the development of a pandemic-resilient healthcare system.
Our hybrid telemedicine model shows promise in terms of improving patient satisfaction and efficiency of the clinic consult and will continue to evolve in the post-vaccination era as the population becomes more familiar with telemedicine. Factors that have been previously described, such as the provision of an overarching architecture and infrastructure, strong program management, and a thorough needs analysis, will be key to success leading to a sustainable model of care [30].
7. Conclusion
It has become imperative to adapt, prepare, and plan for the challenges that we may face amid the ongoing COVID-19 pandemic and similar future outbreaks. The GOLDEN program has been able to continue caring for our patients with the implementation of the hybrid teleconsultation model during this period. Our model of care will continue to evolve and be sustainable in the post-vaccination era as the use of telemedicine gains traction in our population.
Ethnics Approval
This study was approved by the National University Hospital (NUH) Institutional Ethnics Review Board.
Consent for Publication
Yes. Author Contribution Form as attached.
Availability of Data and Materials
Yes.
Authors' Contribution
Conception and design: Angela Pang and Matthew Chen.
Data collection: Ng Yean Shin, Chun Meiling, Yao Yao and Eng Wan Nghee.
Analysis and interpretation of data: Angela Pang, Matthew Chen, Nydia Camelia and Yao Yao.
Manuscript writing: Angela Pang, Matthew Chen, Nydia Camelia, Natalie Ling, Francis Ho, Noorhanah Binte Mohammad, Yao Yao and Beatriz Korc-Grodzicki.
Declaration of Competing Interest
The authors indicated no potential conflicts of interest.
Acknowledgements
The GOLDEN program is funded by the Jurong Health Fund Grant.
References
- 1.World Health Organisation WHO Coronavirus (COVID-19) Dashboard. 2021. https://COVID-19.who.int/ URL: Accessed 25 October 2021.
- 2.Shahid Z., Kalayanamitra R., McClafferty B., et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–929. doi: 10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singhal S., Kumar P., Singh S., Saha S., Dey A.B. Clinical features and outcomes of COVID-19 in older adults: a systematic review and meta-analysis. BMC Geriatr. 2021;21(1):321. doi: 10.1186/s12877-021-02261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cavalcanti I.D.L., Soares J.C.S. Impact of COVID-19 on cancer patients: a review. Asia-Pac J Clin Oncol. 2021;17:186–192. doi: 10.1111/ajco.13445. [DOI] [PubMed] [Google Scholar]
- 5.Fisher D., Mak K. Exiting the pandemic: Singapore style. BMC Med. 2021;19:238. doi: 10.1186/s12916-021-02117-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nuzzo J.B., Meyer D., Snyder M., et al. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health. 2019;19:1310. doi: 10.1186/s12889-019-7707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government of Singapore Updates on the COVID-19 situation in Singapore. 2021. https://www.gov.sg/features/covid-19 URL: Accessed 25 October 2021.
- 8.Bellera C., Rainfray M., Mathoulin-Pélissier S., et al. Screening older cancer patients: first evaluation of the G-8 geriatric screening tool. Ann Oncol. 2012 Aug;23(8):2166–2172. doi: 10.1093/annonc/mdr587. [DOI] [PubMed] [Google Scholar]
- 9.Soubeyran P., Bellera C., Goyard J., et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PLoS One. 2014;9(12) doi: 10.1371/journal.pone.0115060. Published 2014 Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health Singapore . 2015. National Telemedicine Guidelines. [Google Scholar]
- 11.Hurria A., Togawa K., Mohile S., et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective 500 patient multi-center study. J Clin Oncol. 2011;29(25):3457–3465. doi: 10.1200/JCO.2011.34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hurria A., Mohile S.G., Gajra A., et al. Validation of a prediction tool for chemotherapy toxicity in older adults with cancer. J Clin Oncol. 2016;34(20):2366–2371. doi: 10.1200/JCO.2015.65.4327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magnuson A., Sedrak M., Gross C., et al. Development and validation of a risk tool for predicting severe toxicity in older adults receiving chemotherapy for early-stage breast cancer. J Clin Oncol. 2021;39(6):608–618. doi: 10.1200/JCO.20.02063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Cancer Institute, National Institutes of Health, US Department of Health and Human Services . 2010. Common terminology criteria for adverse events (CTCAE), Version 4.0. NIH publication 09–7473. Published May 29, 2009. Revised June 14. [Google Scholar]
- 15.Aaronson N.K., Ahmedzai S., Bergman B., Bullinger M., Cull A., Duez N.J., et al. The European Organisation for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 16.Clegg A., Young J., Iliffe S., et al. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Handforth C., Clegg A., Young C., et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. 2015;26(6):1091–1101. doi: 10.1093/annonc/mdu540. [DOI] [PubMed] [Google Scholar]
- 18.Van Jaarsveld G. The effects of COVID-19 among the elderly population: a case for closing the digital divide. Front Psych. 2020;11:1211. doi: 10.3389/fpsyt.2020.577427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lebrasseur A., Fortin-Bédard N., Lettre J., et al. Impact of the COVID-19 pandemic on older adults: rapid review. JMIR Aging. 2021;4(2) doi: 10.2196/26474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiGiovanni G., Mousaw K., Lloyd T., et al. Development of a telehealth geriatric assessment model in response to the COVID-19 pandemic. J Geriatr Oncol. 2020;11(5):761–763. doi: 10.1016/j.jgo.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trevino K.M., Saracino R.M., Roth A.J. Symptomatology, assessment, and treatment of anxiety in older adults with cancer. J Geriatr Oncol. 2021;12(2):316–319. doi: 10.1016/j.jgo.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stark D.P., House A. Anxiety in cancer patients. Br J Cancer. 2000;83(10):1261–1267. doi: 10.1054/bjoc.2000.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Büntzel J., Klein M., Keinki C., et al. Oncology services in corona times: a flash interview among German cancer patients and their physicians. J Cancer Res Clin Oncol. 2020;1–3 doi: 10.1007/s00432-020-03249-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oh S.S., Kim K.A., Kim M., et al. Measurement of Digital Literacy Among Older Adults: Systematic Review [published correction appears in J Med Internet Res. 2021 Mar 3;23(3):e28211] [published correction appears in J Med Internet Res. 2021 Jun 15;23(6):e30828] J Med Internet Res. 2021;23(2) Published 2021 Feb 3. [Google Scholar]
- 25.Infocomm Media Development and Authority. Annual survey on infocomm usage in households and by individuals for 2019. URL: https://www.imda.gov.sg/-/media/Imda/Files/Infocomm-Media-Landscape/Research-and-Statistics/Survey-Report/2019-HH-Public-Report_09032020.pdf. Assessed 1 December 2021.
- 26.OECD Secretariat OECD Digital Economy Outlook 2017. Organisation for economic cooperation and development (OECD) 2017 Oct 11. https://www.oecd.org/digital/oecd-digital-economy-outlook-2017-9789264276284-en.htm URL:
- 27.Ministry of Communications and Information Digital media and information literacy framework. 2021. https://www.mci.gov.sg/literacy URL: Assessed 1 December 2021.
- 28.Infocomm Media Development and Authority Seniors Go Digital. 2021. https://www.imda.gov.sg/digitalforlife/About-Us URL:
- 29.Infocomm Media Development and Authority Mobile access for seniors. 2021. https://www.imda.gov.sg/ma URL:
- 30.Moehr J.R., Schaafsma J., Anglin C., et al. Success factors for telehealth--a case study. Int J Med Inform. 2006 Oct-Nov;75(10−11):755–763. doi: 10.1016/j.ijmedinf.2005.11.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Yes.