Text
Since February 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has been responsible for one of the major pandemic we have experienced in the last 100 years [1]. The most severe clinical presentation of COVID-19 is through acute respiratory distress syndrome (ARDS) classifying it as a respiratory illness. The presence of an underlying hypercoagulable state, associated to venous thrombotic events with a prevalence of 30%, was extensively reported worldwide in COVID-19 patients [2], [3], [4]. Moreover, several autopsy studies reported microvascular thromboses in lungs and most organs of deceased patients [5,6].
SARS-CoV-2 infection is thought to be responsible for a specific mechanism of thrombo-inflammation, called the “immunothrombosis model” [7]. The viral-mediated direct cellular damage and the immune response result in the release of proinflammatory cytokines. Cytokines determine the subsequent activation and dysfunction of the endothelium, which contributes to the establishment of an immuno-mediated hypercoagulable state [8]. The pro-thrombotic state is a condition that may precede morbidity and mortality.
According to Ciceri et al. [9], this atypical ARDS working hypothesis was named microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS). This syndrome is thought to be caused by alveolar endothelial damage, followed by progressive endothelial pulmonary involvement. Subsequently, the inflammation and the thrombotic milieu also affect the microcirculation of other organs, eventually leading to multiple organ failure (MOF) [10] and, in certain circumstances, also to a disseminated intravascular coagulation-like state. Among COVID-19 patients with normal angiographic studies, thromboinflammatory markers (D-dimer, C-reactive protein, ferritin, and interleukin 6) are often elevated [11], [12], [13] suggesting the presence of microvascular damage. Nailfold videocapillaroscopy performed on COVID-19 patients showed microvascular abnormalities, resembling acute and post-acute microvascular damage [14]. Furthermore, the COVID-19 radiological pattern is characterized by a unique distribution of pulmonary venous thromboses (PVTs) which overlaps with lung inflamed areas, confirming that in situ thromboses are not embolisms [2].
Several international guidelines recommend heparin-based anticoagulation therapy in all COVID-19 hospitalized patients [15], [16], [17], [18], [19], [20]. This recommendation is based on large observational studies [21,22] which support the efficacy of anticoagulation therapy, while randomized clinical trials (RCTs) comparing the use of heparin versus placebo are lacking. Advantages of heparin include its antithrombotic, anti-inflammatory, and likely antiviral effects [23]. Moreover, heparin has fewer pharmacologic interactions with experimental drugs used in COVID-19 patients, alike the other oral anticoagulants. Despite all of these recommendations, the proper dosage of anticoagulant therapy (prophylactic vs full dose) and the exact time to start anticoagulants remain uncertain [24].
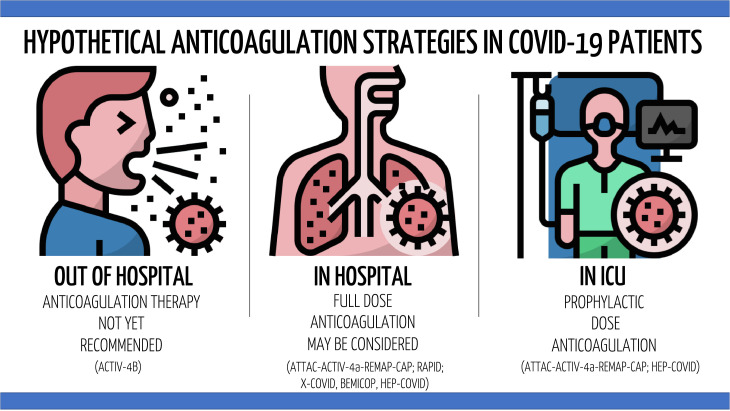
Large RCTs evaluated different anticoagulation strategies in critically ill (ATTAC-ACTIV-4a-REMAP-CAP, HEP-COVID) [25,26] and noncritically ill (ATTAC-ACTIV-4a-REMAP-CAP, RAPID, X-COVID, BEMICOP, HEP-COVID) [26], [27], [28], [29], [30] COVID-19 patients. According to these results, full dose anticoagulation (therapeutic dose) among non-critically ill patients may increase the probability of survival free of organ support, [27] the probability of 28-day survival, [28,30] and it may reduce the probability to developed venous thromboembolism (VTE) [29] with respect to prophylactic dose anticoagulation. However, these findings were not confirmed in patients treated in intensive care units (ICU) [25,26]. Although these RCTs did not include homogeneous populations and the mortality reduction was not confirmed in all studies, it is possible to hypothesize that the efficacy of the anticoagulation strategy may depend on the initiation time of the therapy with respect to the disease course.
If COVID-19 MicroCLOTS are similar to the immunothrombosis model, they are probably resistant to classical anticoagulants drugs. In this case, heparin may stop the progression of the coagulation cascade avoiding the increase in thrombi size, but is not able to dissolve clots. As a consequence, it may be reasonable to suggest that the rationale for the use of heparin would not be primary prevention, but secondary prevention and avoidance of thrombi progression and development of multisystemic thrombotic complications.
Within the context of mild-to-moderate respiratory illness, hospitalized SARS-CoV-2 infected patients may benefit from full-dose anticoagulation as secondary prevention. On the other hand, critically ill COVID-19 patients have probably already developed extensive lung thrombi. In this case, full-dose anticoagulation may not be able to reverse the established disease process. For these reasons, routine full-dose anticoagulation among ICU critically ill patients while not avoiding thrombotic complications can increase bleeding risk. Thus, anticoagulation therapy for critically ill COVID-19 patients should probably follow the same recommendation that are in place for critically ill non-COVID-19 patients.
Even if it reasonable to think that COVID-19 outpatients can benefit from (low dose) anticoagulants, a recent RCT showed no difference in clinical outcomes in patients treated with aspirin, apixaban, or placebo [31]. This might be attributed to the relatively low sample size of the study and/or to the use of drugs different from heparin. An observational large study also suggested that patients on chronic anticoagulants do not have reduced mortality if they develop COVID-19 [32].
As previously highlighted, Sars-CoV-2 exhibits a bidirectional crosstalk between inflammation and thrombosis, or immunothrombosis, and this unique mechanism of inducing coagulopathy paves the way to therapies including antithrombin supplementation, recombinant thrombomodulin, and multiple anti-inflammatory agents. Therefore, monoclonal antibodies targeting pro-inflammatory mediators have been proposed for the treatment of COVID-19 induced microvasculature injury and endothelial damage leading to thrombotic microangiopathy (TMA) [7,8]. Tocilizumab, an interleukin-6 inhibitor (IL-6), may reduce endothelial inflammation, microvascular thrombosis, and mortality [[33], [34], [35]].
Anakinra, an antagonist of interleukin 1 receptor, may dampen systemic inflammation, and reduce mortality [36] in COVID-19 patients, especially when administered early after hospitalization in moderate-to-severe patients outside the ICU. Future studies should investigate the concomitant use of therapeutic dose anticoagulation with anti-inflammatory drugs to prevent the development of critical illness and immunothrombosis.
Neutrophils extracellular traps (NETs) play a direct role in the immune-thrombotic process in COVID-19. Some experimental drugs, targeting NET formation, may limit endothelial damage and improve the prognosis [37]. Complement activation, secondary to endothelial injury, suggests the rational use of monoclonal antibodies against C5 and C3, such as Eculizumab and Ravulizumab (ClinicalTrials.gov Identifier: NCT04570397, NCT04288713, NCT04390464), for the treatment of COVID-19 associated thrombotic microangiopathy [38,39].
Summarizing all previous considerations, the hypercoagulable state associated with COVID-19 may be managed firstly by inhibiting the pro-inflammatory state and secondly by establishing anticoagulation at proper dosage, according to the disease course, to avoid the development or worsening of thrombotic complications.
In conclusion, our reasoning, which is supported by initial evidence, suggests that full anticoagulation maybe considered in non-ICU patients with COVID-19 at high risk of thrombosis progression and at low risk of bleeding. Other patients (eg ICU patients) might be routinely treated with prophylactic anticoagulants if not otherwise indicated. Further RCTs in homogeneous populations are needed to confirm these observations and to inform guidelines.
Fig. 1.
Anticoagulation therapy in COVID-19 according to the disease severity.
CRediT authorship contribution statement
RS: study conception and design, data interpretation, manuscript drafting. MC: data interpretation, manuscript drafting. GL: study conception and design, critical review of the manuscript. LD: study conception and design, manuscript drafting. AZ: study conception and design, critical review of the manuscript. All Authors read and approved the final version of the manuscript.
Declaration of Competing Interest
The authors report no conflicts of interest.
Acknowledgments
Acknowledgement
Thanks to all the peer reviewers and editors for their opinions and suggestions.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.World Health Organization Coronavirus Disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10.
- 2.De Cobelli F, Palumbo D, Ciceri F, et al. Pulmonary Vascular Thrombosis in COVID-19 Pneumonia. J Cardiothorac Vasc Anesth. January 1, 2021 doi: 10.1053/j.jvca.2021.01.011. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roncon L, Zuin M, Barco S, et al. Incidence of acute pulmonary embolism in COVID-19 patients: Systematic review and meta-analysis. Eur J Intern Med. 2020;82:29–37. doi: 10.1016/j.ejim.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reichert G, Bunel V, Dreyfuss D, Saker L, Khalil A, Mal H. Prevalence of proximal deep vein thrombosis in hospitalized COVID-19 patients. Eur J Intern Med. 2021;89:118–120. doi: 10.1016/j.ejim.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carsana L, Sonzogni A, Nasr A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020;20(10):1135–1140. doi: 10.1016/S1473-3099(20)30434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wichmann D, Sperhake JP, Lütgehetmann M, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19. Ann Intern Med. 2020;173(4):268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L. The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management. Thromb Res. 2020;194:101–115. doi: 10.1016/j.thromres.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonaventura A, Vecchié A, Dagna L, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21(5):319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciceri F, Beretta L, Scandroglio AM, et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc J Australas Acad Crit Care Med. 2020;22(2):95–97. doi: 10.51893/2020.2.pov2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Renzi S, Landoni G, Zangrillo A, Ciceri F. MicroCLOTS pathophysiology in COVID 19. Korean J Intern Med. September 9, 2020 doi: 10.3904/kjim.2020.336. https://www.kjim.org/journal/view.php?doi=10.3904/kjim.2020.336 Published onlineAccessed September 22, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahat RK, Panda S, Rathore V, Swain S, Yadav L, Sah SP. The dynamics of inflammatory markers in coronavirus disease-2019 (COVID-19) patients: A systematic review and meta-analysis. Clin Epidemiol Glob Health. 2021;11 doi: 10.1016/j.cegh.2021.100727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed]
- 13.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost JTH. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Natalello G, De Luca G, Gigante L, et al. Nailfold capillaroscopy findings in patients with coronavirus disease 2019: Broadening the spectrum of COVID-19 microvascular involvement. Microvasc Res. 2021;133 doi: 10.1016/j.mvr.2020.104071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuker A, Tseng EK, Nieuwlaat R, et al. American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: May 2021 update on the use of intermediate intensity anticoagulation in critically ill patients. Blood Adv. 2021 doi: 10.1182/bloodadvances.2021005493. (bloodadvances.2021005493) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spyropoulos AC, Levy JH, Ageno W, et al. Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1859–1865. doi: 10.1111/jth.14929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barnes GD, Burnett A, Allen A, et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020;50(1):72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moores LK, Tritschler T, Brosnahan S, et al. Prevention, Diagnosis, and Treatment of VTE in Patients With Coronavirus Disease 2019. Chest. 2020;158(3):1143–1163. doi: 10.1016/j.chest.2020.05.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Information on COVID-19 Treatment, Prevention and Research. COVID-19 Treatment Guidelines. October 5, 2021 https://www.covid19treatmentguidelines.nih.gov/ Accessed. [Google Scholar]
- 21.Paranjpe I, Fuster V, Lala A, et al. Association of Treatment Dose Anticoagulation With In-Hospital Survival Among Hospitalized Patients With COVID-19. J Am Coll Cardiol. 2020;76(1):122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rentsch CT, Beckman JA, Tomlinson L, et al. Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the United States: cohort study. BMJ. 2021;372:n311. doi: 10.1136/bmj.n311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buijsers B, Yanginlar C, Maciej-Hulme ML, de Mast Q, der Vlag J van. Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients. EBioMedicine. 2020:59. doi: 10.1016/j.ebiom.2020.102969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giannis D, Douketis JD, Spyropoulos AC. Anticoagulant therapy for COVID-19: What we have learned and what are the unanswered questions? Eur J Intern Med. 2022;96:13–16. doi: 10.1016/j.ejim.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.REMAP-CAP Investigators, ACTIV-4a Investigators, ATTACC Investigators Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med. 2021;385(9):777–789. doi: 10.1056/NEJMoa2103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spyropoulos AC, Goldin M, Giannis D, et al. Efficacy and Safety of Therapeutic-Dose Heparin vs Standard Prophylactic or Intermediate-Dose Heparins for Thromboprophylaxis in High-risk Hospitalized Patients With COVID-19: The HEP-COVID Randomized Clinical Trial. JAMA Intern Med. 2021;181(12):1612–1620. doi: 10.1001/jamainternmed.2021.6203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ATTACC Investigators, ACTIV-4a Investigators, REMAP-CAP Investigators Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med. 2021;385(9):790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sholzberg M, Tang GH, Rahhal H, et al. Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with covid-19 admitted to hospital: RAPID randomised clinical trial. BMJ. 2021;375:n2400. doi: 10.1136/bmj.n2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morici N, Podda G, Birocchi S, et al. Enoxaparin for thromboprophylaxis in hospitalized COVID-19 patients: The X-COVID-19 Randomized Trial. Eur J Clin Invest. n/a(n/a):e13735. doi: 10.1111/eci.13735. [DOI] [PubMed]
- 30.Marcos-Jubilar M, Carmona-Torre F, Vidal R, et al. Therapeutic versus Prophylactic Bemiparin in Hospitalized Patients with Nonsevere COVID-19 Pneumonia (BEMICOP Study): An Open-Label, Multicenter, Randomized, Controlled Trial. Thromb Haemost. 2021;12 doi: 10.1055/a-1667-7534. Published online October. [DOI] [PubMed] [Google Scholar]
- 31.Connors JM, Brooks MM, Sciurba FC, et al. Effect of Antithrombotic Therapy on Clinical Outcomes in Outpatients With Clinically Stable Symptomatic COVID-19: The ACTIV-4B Randomized Clinical Trial. JAMA. 2021;326(17):1703–1712. doi: 10.1001/jama.2021.17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montorfano M, Leoni O, Andreassi A, et al. Chronic anticoagulant treatment and risk of mortality in SARS-Cov2 patients: a large population-based study. Minerva Med. Published online February 2022. doi: 10.23736/S0026-4806.22.07797-7. [DOI] [PubMed]
- 33.Levi M. Tocilizumab in severe COVID-19: A promise fulfilled. Eur J Intern Med. 2022;95:38–39. doi: 10.1016/j.ejim.2021.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campochiaro C, Tomelleri A, Matucci-Cerinic M, Dagna L. One year later: The case of tocilizumab in COVID-19. Eur J Intern Med. 2022;95:5–6. doi: 10.1016/j.ejim.2021.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Belletti A, Campochiaro C, Marmiere M, et al. Efficacy and safety of IL-6 inhibitors in patients with COVID-19 pneumonia: a systematic review and meta-analysis of multicentre, randomized trials. Ann Intensive Care. 2021;11(1):152. doi: 10.1186/s13613-021-00941-2. [DOI] [PMC free article] [PubMed]
- 36.Cavalli G, De Luca G, Campochiaro C, et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;2(6):e325–e331. doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barnes BJ, Adrover JM, Baxter-Stoltzfus A, et al. Targeting potential drivers of COVID-19: Neutrophil extracellular trapsNeutrophil extracellular traps in COVID-19. J Exp Med. 2020;217(6) doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Annane D, Heming N, Grimaldi-Bensouda L, et al. Eculizumab as an emergency treatment for adult patients with severe COVID-19 in the intensive care unit: A proof-of-concept study. eClinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mastellos DC, Pires da Silva BGP, Fonseca BAL, et al. Complement C3 vs C5 inhibition in severe COVID-19: Early clinical findings reveal differential biological efficacy. Clin Immunol Orlando Fla. 2020;220 doi: 10.1016/j.clim.2020.108598. [DOI] [PMC free article] [PubMed] [Google Scholar]