Abstract
Introduction
Emerging evidence indicates that the COVID-19 pandemic, and the responses it has generated, have had disproportionate impacts on lesbian, gay, bisexual, transgender and queer (LGBTQ+) communities. This study seeks to build on existing information and provide regional insight.
Methods
In response, a cross-sectional survey was administered to a global sample of LGBTQ+ individuals (n=13 358) between 16 April and 20 May 2020 via the social networking application Hornet. The survey contained questions that characterise the impact of COVID-19 and associated mitigation strategies on economics, employment, mental health and access to healthcare.
Results
5191 (43.9%) individuals indicated they were somewhat, slightly or unable to meet basic needs with their current income, while 2827 (24.1%) and 4710 (40.1%) felt physically or emotionally unsafe in their living environment, respectively. 2202 individuals (24.7%) stated they are at risk for losing health insurance coverage. 2685 (22.7%) persons reported having skipped or cut meals as there was not enough money.
Conclusion
Many LGBTQ+persons who responded reported adverse consequences to mental health, economics, interruptions to care and lack of support from their government. This data is part of ongoing analyses but accentuates the unique needs of LGBTQ+ communities that will require targeted, ameliorative approaches.
Keywords: epidemiology, health policy, public health, respiratory infections
Strengths and limitations of this study.
Large, global sample of lesbian, gay, bisexual, transgender and queer (LGBTQ+) persons regarding the impact of COVID-19 - likely one of, if not the first of, its kind.
Considers the immediate and secondary effects of COVID-19 on the LGBTQ+ community.
Led by a multisector, collaborative research working group.
Convenience sample of individuals who have resources, including the liberty to use networking applications such as Hornet.
Underscores the need for improved monitoring and continued data collection to guide future programmes and policies.
Introduction
COVID-19 continues to sweep across the globe, with over 173 million confirmed cases and 3.7 million deaths.1 lesbian, gay, bisexual, transgender and queer (LGBTQ+) communities continue to be particularly vulnerable, with all stages of the continuum of care and prevention being disrupted.2–4 There has been significant heterogeneity in the burden of COVID-19 and the stringency of prevention and mitigation measures around the world.5 The ability to rapidly adjust implementation strategies to maintain physical distancing and adherence to guidelines has likely varied based on underlying infrastructure and resources, including aspects such as population density, crowded housing, use of public transportation, rates of incarceration or other group or closed housing settings and structural barriers like stigma, homophobia and racism. While these efforts have helped to curb the growth of new cases, they have had vast social, economic and health consequences.6–8
Socioeconomic status, and the ability to self-isolate, telecommute and practice good hygiene have emerged as social determinants of COVID-19 outcomes. Many vulnerable groups have suffered disproportionately, including migrant workers in many contexts, undocumented migrants, ethnic/racial minorities, prisoners and detainees, and others at the margins of societies.9–11 Reports also indicate the unique concerns and challenges experienced by members of the LGBTQ+ community resulting from antigay backlash and community crackdown under false pretexts.12–14 Moreover, many members of the LGBTQ+ community are at increased risk for food insecurity, unemployment and unstable housing, thereby making them more vulnerable to the economic and health impacts from COVID-19.7 15–18
COVID-19 may also amplify existing barriers to HIV prevention, testing and care, which could also slow efforts to achieve global HIV targets.19 Members of the LGBTQ+ community are among those at highest risk for HIV, with gay men and other MSM being 22 times more likely to acquire HIV than the worldwide general population.20 Reductions in access to HIV testing, condoms, pre-exposure prophylaxis (PrEP), and postexposure prophylaxis (PEP) put this community at higher risk for seroconversion.21–26 These interruptions also have wide-ranging implications for those who do seroconvert, or who are already living with HIV, such as increased viral load, increased transmission, and even drug resistance27–29 Highlighting the impact of COVID-19 on the HIV care continuum will be of crucial importance both during and beyond the pandemic. Collectively, gaps of varying intensity have emerged around the world, likely reinforcing underlying health and other disparities and inequities. For members of the LGTBQ+ community, existing structural vulnerabilities demand a unique and targeted response to COVID-10 to ameliorate its impacts. Additionally, given the wide variation in sociopolitical climates and responses to COVID-19 in countries around the world, regional analyses will be critical to examine how subpopulations are being disproportionately affected, including racial/ethnic minorities, immigrants, sex workers and socioeconomically disadvantaged groups. To assess the socioeconomic and health impacts of the current crisis on LGBTQ+ individuals around the world, a rapid, application-based survey was developed to collect additional evidence.
Methods
This cross-sectional study was conducted based on data collected from the COVID-19 disparities survey implemented by the gay social networking application, Hornet. The app is a free, smart phone based ‘Gay Social Networking’ application with over 25 million users worldwide and has previously been used for conducting research with LGBTQ+ communities worldwide. The data presented here was collected between 16 April 2020 and 4 May 2020, when Hornet users were invited to participate in a brief questionnaire with 58 questions regarding demographics and the impact of COVID-19 on economic vulnerability, access to care and mental health. Any Hornet user who was over the age of 18 and able to provide consent were eligible. The survey was made available in English, Arabic, Spanish, French, Russian, Portuguese, Italian, Simplified and Traditional Chinese, Malay, Thai, Indonesian, Farsi and Turkish. Only descriptive analysis were conducted on the full sample in order to characterise the impact on the full, global LGBTQ+ community that the sample represented. There is wide variation in the acceptance and marginalisation of LGBTQ+ people around the world, and to control for such differences, individual responses were stratified and analysed by WHO regions. The aim of this descriptive analysis was to lay a foundation and fill in data gaps on the economic and health impact of COVID-19 on LGBTQ+ communities around the world, creating an opportunity for researchers who are more familiar with such differences to expand on and further contextualise the results presented here. Given the nature of convenience sampling and the subsequent descriptive analysis outlined here, sensitivity analyses and controlling for confounding was deemed not necessary.
To ensure the equality of our sample, duplicates were screened out based on IP address, and searched for identical responses to randomly selected variables, but found none. In order to minimise bias between outcomes, each outcome was analysed individually with the respective number of individuals who responded.
Measures
Eligible, consenting individuals responded to general demographic questions on age, country of origin, sex assigned at birth, gender identity and sexual orientation. Participants were also asked about their HIV serostatus. The questionnaire was designed by combining validated instruments with newly created indicators specific to the impacts of COVID-19 on the following areas: (1) mental health; (2) economics and employment and (3) access to care.
Patient and public involvement
Amidst the ongoing COVID-19 pandemic, efforts were undertaken to characterise the continued impact on members of the LGBTQ+ community. Given the nature of inequities often faced by LGBTQ+ persons, special consideration was given to economics, mental health, and access to care during research question, outcome and survey development. While the public was not directly involved in development, the unique needs of the global LGBTQ+ community were centred in the design, translation and implementation of this research. Furthermore, there is a significant representation of LGBTQ+ identifying individuals within the COVID-19 Disparities Working Group. With clear plans for dissemination of any and all results to the entirety of the Hornet user base.
Demographic measures
Individuals self-reported their age, country of origin, socioeconomic status, history of sex work, years of education, ethnic minority and immigration status, and access to mask. To increase the power of our analyses, sexual orientation was collapsed into three groups: gay, bisexual, other (lesbian, heterosexual, asexual, pansexual, questioning and I don’t know). Individuals also self-reported gender identity from the following options: gender nonbinary, transgender woman, transgender man, woman or man.
Mental health
The survey asked individuals about the impact of the COVID-19 pandemic on their mental health. For indicators of mental health we used the 4-item Patient Health Questionnaire (PHQ-4) to screen for symptoms of depression and anxiety and overall category of psychological distress (none, mild, moderate and severe).30 Individuals were also asked how they feel about their current living environment (eg, ‘How do you feel about your current living environment?’) and whether it was emotionally and physically safe
Economics and employment
The impact of COVID-19 on economics and employment was assessed through questions regarding economic and employment status; type of work (eg, ‘What kind of work do you currently do?’); ability to miss work (eg, ‘Can you afford to miss work during COVID-19?’); ability to meet basic needs (eg, ‘How well are you able to meet your basic needs (eg, food, clothing, transportation, education, and healthcare) with your current income?’); financial support from work or government (eg, ‘Are you receiving any additional financial benefits from work or government because of the COVID-19 crisis?’); reductions in income (eg, ‘How much are you expecting your income to reduce because of the COVID-19 crisis?) and access to food (eg, ‘Since the COVID-19 crisis began, have you had to cut the size of your meals or skip meals because there was not enough money for food?’).
Access to care
Individuals were asked about healthcare coverage amid the COVID-19 pandemic, such as source of insurance (eg, ‘What is the primary source of healthcare coverage?’), which was trichotomised as government insurance, no insurance or private/employer/other; losing insurance (eg, ‘Do you expect to lose your health insurance coverage because of the COVID-19 crisis?; access to masks (eg, ‘Do you have access to masks for COVID-19 protection), which was then dichotomized into a positive sentiment (‘Yes’) and negative sentiment (‘No’). To further quantify access to care, individuals were asked whether COVID-19 had impacted their access to HIV prevention strategies, including condoms, testing, PrEP and PEP using Likert-type questions (eg, ‘Do you feel you have access to HIV prevention strategies during the COVID-19 crisis?’ with the following response options: ‘Definitely yes’, ‘“Probably yes’, ‘Might or might not’, ‘Probably not’, ‘Definitely not’).
Results
All individuals who consented to taking the survey were considered eligible, though not everyone responded to every question as it did not apply to them, or simply chose not to. The number of persons who responded to individual questions are reported as outcome events for each question.
Between 16 April 2020 and 4 May 2020, 13 358 individuals from 136 countries responded to the survey (table 1), ranging in age from under 18 to 85+. Most respondents were either younger than 30 years old (39.5%) or between the ages of 30 and 49 (49.8%). Twelve percent (n=1425) of respondents indicated that they were living with HIV, and 60.0% of these indicated that they were undetectable. Individuals were educated and living in metropolitan areas, with 50.0% having a university degree or more and 72.0% living in a large or capital city.
Table 1.
Demographics of LGBTQ+ individuals from the COVID-19 disparities survey distributed between 16 April 2020 and 4 May 2020, stratified by WHO region
| Variable | Overall (%) | Africa | Americas | Southeast Asia | Europe | Eastern Mediterranean | Western Pacific | P value* |
| Age | 13 557 | 103 | 1459 | 1262 | 9363 | 536 | 641 | 0.007† |
| >19 | 740 (5.5) | 9 (8.7) | 30 (2.1) | 61 (4.8) | 578 (6.2) | 29 (5.4) | 33 (5.2) | |
| 20–29 | 4534 (34.0) | 43 (41.8) | 349 (23.9) | 470 (37.2) | 3255 (34.7) | 207 (38.6) | 213 (33.2) | |
| 30–49 | 6659 (49.8) | 40 (38.8) | 736 (50.4) | 622 (49.3) | 4672 (49.9) | 377 (51.7) | 316 (49.3) | |
| 50+ | 1424 (10.7) | 11 (10.7) | 344 (23.6) | 109 (8.7) | 858 (9.2) | 23 (4.3) | 79 (12.3) | |
| Years of Education‡ | 90 | 1253 | 1057 | 8573 | 429 | 573 | 0.000§ | |
| Less than 6 years | 742 (6.2) | 18 (20.0) | 70 (5.6) | 198 (18.7) | 1259 (14.7) | 56 (13.1) | 61 (10.6) | |
| Between 6 and 12 years | 1661 (13.9) | 5 (5.6) | 8 (0.6) | 45 (4.3) | 661 (7.7) | 18 (4.2) | 5 (0.9) | |
| Some university but no degree | 2199 (18.4) | 19 (21.1) | 319 (25.5) | 160 (15.1) | 1564 (18.2) | 60 (14.0) | 78 (13.6) | |
| Trade school | 1387 (11.6) | 12 (13.3) | 99 (7.9) | 117 (11.0) | 1042 (12.2) | 43 (10.0) | 75 (13.1) | |
| University degree or more | 5981 (50.0) | 36 (40.0) | 757 (60.4) | 537 (50.8) | 4047 (47.2) | 252 (58.7) | 354 (61.8) | |
| Ethnic Minority‡ | 13 616 | 89 | 1248 | 1043 | 8547 | 423 | 570 | 0.08 |
| Yes | 2064 (15.2) | 36 (40.4) | 226 (18.1) | 247 (23.7) | 1320 (15.4) | 142 (33.6) | 93 (16.3) | |
| No | 9852 (72.4) | 37 (41.6) | 915 (73.3) | 517 (49.6) | 6093 (71.3) | 169 (39.9) | 423 (74.2) | |
| I don’t know/refuse | 1700 (12.5) | 16 (18.0) | 107 (8.6) | 279 (23.7) | 1134 (13.3) | 112 (26.5) | 54 (9.5) | |
| Immigration Status‡ | 11 040 | 83 | 1182 | 905 | 7978 | 358 | 537 | 0.27 |
| First generation | 547 (5.0) | 5 (6.0) | 70 (5.9) | 31 (3.4) | 382 (4.8) | 20 (5.6) | 39 (7.3) | |
| Immigrant | 1408 (12.8) | 24 (28.9) | 89 (7.5) | 151 (16.7) | 947 (11.9) | 106 (29.6) | 92 (1.3) | |
| Parents are native | 9085 (82.2) | 54 (65.1) | 1023 (86.6) | 723 (79.9) | 6649 (83.3) | 232 (64.8) | 406 (75.6) | |
| Urban/rural‡ | 11 932 | 90 | 1246 | 1048 | 8558 | 424 | 571 | 0.021† |
| A capital city | 3612 (30.3) | 34 (37.8) | 531 (42.6) | 367 (35.0) | 2345 (27.4) | 179 (42.2) | 158 (27.7) | |
| A farm or isolated house | 95 (0.8) | 0 (0.0) | 4 (0.3) | 16 (1.5) | 67 (0.8) | 6 (1.4) | 2 (0.3) | |
| A large city | 4631 (38.8) | 16 (17.8) | 368 (29.5) | 198 (18.9) | 3732 (43.6) | 123 (29.0) | 194 (34.0) | |
| A rural area or village | 646 (5.4) | 8 (8.9) | 17 (1.4) | 159 (15.2) | 402 (4.7) | 20 (4.7) | 41 (7.2) | |
| A small city or town | 1972 (16.5) | 16 (17.8) | 223 (17.9) | 133 (12.7) | 1448 (16.9) | 63 (14.9) | 91 (15.9) | |
| A suburb near large city | 976 (8.2) | 16 (17.8) | 103 (8.3) | 175 (16.7) | 564 (6.6) | 33 (7.8) | 85 (14.9) | |
| Sexual orientation‡ | 11 980 | 91 | 1252 | 1054 | 8586 | 430 | 572 | 0.13 |
| Gay | 8939 (74.6) | 12 (13.2) | 149 (11.9) | 195 (18.5) | 1513 (17.6) | 74 (17.2) | 66 (11.5) | |
| Bisexual | 2009 (16.7) | 57 (62.6) | 1048 (83.7) | 746 (70.8) | 6354 (74.0) | 254 (59.1) | 484 (84.6) | |
| Others (lesbian, heterosexual, asexual) | 1032 (8.6) | 22 (24.2) | 55 (4.4) | 113 (10.7) | 719 (8.4) | 102 (23.7) | 22 (3.9) | |
| Intersex | 132 | 2 | 2 | 65 | 35 | 21 | 7 | |
| Gender Identityঠ| 11 928 | 90 | 1250 | 1047 | 8569 | 429 | 572 | 0.39 |
| Gender nonbinary | 15 | 56 | 187 | 286 | 20 | 23 | ||
| Transgender woman | 5 | 4 | 21 | 94 | 35 | 6 | ||
| Transgender man | 3 | 8 | 31 | 48 | 9 | 6 | ||
| Man | 67 | 1151 | 807 | 7947 | 364 | 532 | ||
| Woman | 11 | 5 | 10 | 100 | 9 | 6 | ||
| I don’t know or I do not wish to answer | 10 | 51 | 110 | 384 | 46 | 23 | ||
| HIV Status‡ | 11 929 | 91 | 1251 | 1047 | 8554 | 420 | 572 | 0.11 |
| I don’t know | 15 (16.5) | 132 (10.5) | 233 (22.2) | 1217 (14.2) | 53 (12.6) | 78 (1.6) | ||
| I don’t want to answer | 3 (3.3) | 36 (2.9) | 97 (9.3) | 374 (4.4) | 20 (7.8) | 23 (4.0) | ||
| I’m HIV-Negative | 60 (65.9) | 779 (62.3) | 581 (55.5) | 6059 (70.8) | 324 (77.1) | 426 (74.5) | ||
| I’m HIV-Positive | 7 (7.7) | 96 (7.7) | 66 (6.3) | 372 (4.3) | 13 (3.1) | 9 (1.6) | ||
| I'm HIV-Positive and Undetectable | 6 (6.6) | 208 (16.6) | 70 (6.7) | 532 (6.3) | 10 (2.4) | 36 (6.3) | ||
| Sex work‡ | 11 787 | 87 | 1219 | 1027 | 8486 | 420 | 554 | 0.24 |
| I don’t know/refuse | 710 | 3 (3.5) | 32 (3.6) | 65 (6.3) | 552 (6.5) | 37 (8.8) | 22 (4.0) | |
| Never | 9564 | 63 (72.4) | 1041 (85.4) | 720 (70.1) | 6938 (81.8) | 304 (72.4) | 501 (90.4) | |
| Yes | 1513 | 21 (24.1) | 146 (12.0) | 242 (23.6) | 996 (11.7) | 79 (18.8) | 301 (5.6) | |
| Socioeconomic Status | 11 983 | 91 | 1254 | 1060 | 8580 | 430 | 573 | 0.007† |
| Lower | 1079 | 13 (14.3) | 111 (8.8) | 161 (15.2) | 688 (8.0) | 60 (14.0) | 47 (8.2) | |
| Lower middle | 4733 | 30 (32.0) | 574 (45.8) | 506 (47.7) | 3227 (37.6) | 166 (38.6) | 231 (40.3) | |
| Upper middle | 704 | 12 (13.2) | 70 (5.6) | 50 (4.7) | 520 (6.0) | 22 (5.1) | 31 (5.4) | |
| Upper | 5467 | 36 (39.5) | 499 (39.8) | 343 (32.4) | 4145 (48.3) | 182 (42.3) | 264 (46.1) | |
| Government restrictions‡ | 12 212 | 92 | 1282 | 1116 | 8657 | 433 | 582 | 0.045† |
| Complete restriction | 1087 (8.9) | 19 (20.6) | 84 (6.6) | 179 (16.6) | 743 (8.6) | 43 (9.9) | 19 (3.3) | |
| Somewhat restricted | 8093 (66.3) | 64 (69.6) | 1027 (80.1) | 780 (72.5) | 5643 (65.2) | 264 (61.0) | 225 (38.7) | |
| No restrictions | 3032 (24.8) | 9 (9.8) | 171 (13.3) | 117 (10.9) | 2271 (26.2) | 126 (29.1) | 338 (58.0) |
*P values were calculated using a one-way analysis of variance between WHO regions.
†Denotes p<0.05.
‡Denominators excluded individuals who did not respond.
§Denotes p<0.001.
¶Individuals who reported more than one gender identity were calculated by overall regional count.
LGBTQ, lesbian, gay, bisexual, transgender and queer.
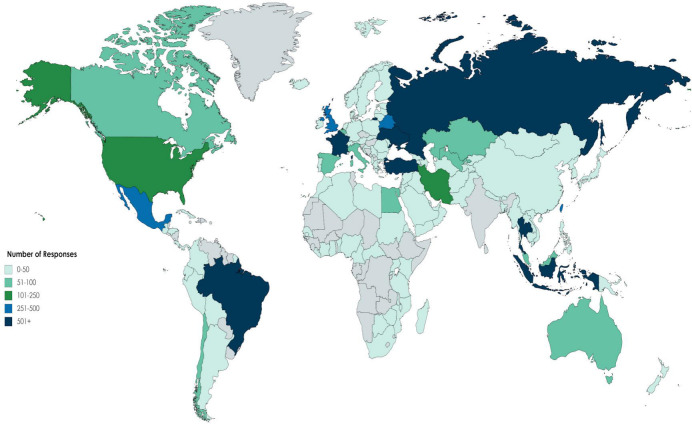
The data also represent samples individuals from some of the most COVID-affected countries globally, including Russia, Brazil, France and Mexico. Since only descriptive statistics were conducted on the data collected from an anonymous survey, no efforts to reduce potential sources of bias were undertaken. To account for economic, sociopolitical and geographical differences, responses were stratified by WHO region, but no further subgroup analyses were conducted in order to give a broad, descriptive overview of the impact of COVID-19 on the global LGBTQ+ community. Figure 1 highlights the geographical diversity captured by this survey, indicating the global impact of the crisis on members of this community. Majority of respondents were from Europe (70.1%), Americas (10.9%) and Southeast Asia (9.5%), generally reflecting Hornet’s user base. Hornet is used by a diverse community, with nearly 25% of users identifying as non-gay.
Figure 1.
Global distribution of individuals who particpated in the COVID Disparities Survey
Mental health
Given intersecting stigmas and minority stress, LGBTQ+ communities are well known to bear high burdens of mental health conditions.31–35 51.4% of individuals reported moderate to severe psychological distress as measured by the PHQ-4 scale (18.0% moderate, 31.4% severe) and there was a statistically significant difference between regions (F(5,18)=34.218), p=0.000). Based on the anxiety and depression subscales (table 2), 4003 individuals (36.4%) screened positive for anxiety, and 4639 individuals (41.6%) of individuals screen positive for depression. For both anxiety and depression screens, there was a statistically significant difference between WHO regions, as determined by one-way analysis of variance (ANOVA) tests (F(6,7)= 5.266, p=0.016 and F (6,7)=9.828 p=0.0004). Additionally, 40.1% of individuals reported that they felt emotionally unsafe in their current environment and 24.1% physically unsafe and the difference between regions was statistically significant (F (5,18)=43.822, p=0.000)
Table 2.
Mental health indicators among LGBTQ+ individuals from the COVID-19 disparities survey distributed between 16 April 2020 and 4 May 2020, stratified by WHO region
| Indicator | Overall (%) | Africa | Americas | Southeast Asia | Europe | Eastern Mediterranean | Western Pacific | P value* |
| Total PHQ-4† | 10 939 | 79 | 1153 | 915 | 7874 | 379 | 539 | 0.000‡ |
| None | 3527 (32.2) | 21 (26.6) | 311 (27.0) | 245 (26.8) | 2645 (33.6) | 107 (28.2) | 198 (36.7) | |
| Mild | 2015 (18.4) | 15 (19.0) | 191 (16.5) | 143 (15.6) | 1512 (19.2) | 89 (23.5) | 65 (12.1) | |
| Moderate | 3431 (31.4) | 14 (17.7) | 440 (38.2) | 405 (44.3) | 2288 (29.0) | 59 (15.5) | 225 (41.7) | |
| Severe | 1966 (18.0) | 29 (36.7) | 211 (18.3) | 122 (13.3) | 1429 (18.1) | 124 (32.7) | 51 (9.5) | |
| Anxiety Screen† | 11 006 | 79 | 1169 | 918 | 7922 | 379 | 539 | 0.005§ |
| Positive | 4003 (36.4) | 43 (54.4) | 463 (39.6) | 274 (29.9) | 2885 (36.4) | 218 (57.5) | 120 (22.3) | |
| Negative | 7003 (63.6) | 36 (45.6) | 706 (60.4) | 644 (70.1) | 5037 (63.6) | 161 (42.5) | 419 (77.7) | |
| Depression Screen† | 11 153 | 82 | 1166 | 942 | 8031 | 386 | 546 | 0.001‡ |
| Positive | 4639 (41.6) | 48 (41.5) | 411 (35.3) | 316 (33.5) | 3490 (43.5) | 226 (41.5) | 148 (27.1) | |
| Negative | 6514 (58.4) | 34 (58.5) | 755 (64.7) | 626 (66.5) | 4541 (56.5) | 160 (58.5) | 398 (72.9) | |
| Current Environment†¶ | 11 741 | 103 | 1459 | 1262 | 9363 | 536 | 641 | 0.000§ |
| Physically unsafe | 25 | 244 | 156 | 2210 | 147 | 45 | ||
| Emotionally unsafe | 31 | 476 | 212 | 3665 | 207 | 120 | ||
| Physically safe | 38 | 663 | 542 | 3815 | 124 | 416 | ||
| Emotionally safe | 29 | 485 | 323 | 2533 | 82 | 344 | ||
| I don't know | 11 | 91 | 192 | 1271 | 71 | 52 |
*P values were calculated using a one-way analysis of variance between WHO regions.
†Denominators excluded individuals who did not respond.
‡Denotes p<0.001.
§Denotes p<0.05.
¶Question was select all that apply and were calculated by overall regional count.
LGBTQ, lesbian, gay, bisexual, transgender, and queer; PHQ-4, Patient Health Questionnaire.
Economics and employment
LGBTQ+ individuals are more likely to be employed in service, sales, and hospitality industries, all of which have been heavily impacted by the COVID-19 crisis.7 17 36 The significance of such employment demographics are reflected in the data collected (table 3), with 23.8% (3128/13115) of persons responding that they work in either the service or hospitality industries and 13.7% (1625/11 827) indicating that they already lost their job as a result of the COVID-19 crisis. Nearly 50.0% of individuals indicated that they were not able to completely meet their basic needs (eg, food, clothing, shelter, transportation, education and healthcare), which was significant between regions (F(5,24)=12.080, p=0.000). Furthermore, one out of every four individuals indicated that they have skipped or cut meals, although there was no significant difference between regions. Of those who responded, one in every three individuals expected at least a 30% reduction in income as a result of COVID-19, the difference of which between regions was significant (F(5,18)=59.1, p=0.000). Lastly, and perhaps most importantly, more than 80% of individuals responded that they had not received financial support from work or government, and one in two indicated that it was needed (F(5,18)=4.16, p=0.01).
Table 3.
Access to care indicators among LGBTQ+ individuals from the COVID-19 disparities survey distributed between 16 April 2020 and 4 May 2020, stratified by WHO region
| Indicator | Overall (%) | Africa | Americas | Southeast Asia | Europe | Eastern Mediterranean | Western Pacific | P value* |
| Access to masks† | 12 508 | 97 | 1296 | 1106 | 8976 | 444 | 589 | 0.176 |
| Yes | 10 301 (82.4) | 80 (82.5) | 1089 (84.0) | 1046 (95.0) | 7171 (79.9) | 371 (83.6) | 544 (92.0) | |
| No | 2207 (17.6) | 17 (17.5) | 207 (16.0) | 60 (5.0) | 1805 (20.1) | 73 (16.4) | 47 (8.0) | |
| Healthcare coverage | 11 827 | 89 | 1232 | 1030 | 8492 | 423 | 561 | 0.000‡ |
| Government insurance | 4486 (37.9) | 18 (20.2) | 385 (31.2) | 209 (20.3) | 3442 (40.5) | 111 (26.2) | 321 (57.2) | |
| No insurance | 1866 (15.8) | 33 (37.1) | 203 (16.5) | 272 (26.4) | 1192 (14.0) | 122 (28.8) | 44 (7.8) | |
| Private/employer/other | 5475 (46.3) | 38 (42.7) | 644 (52.3) | 549 (53.3) | 3858 (45.5) | 190 (44.9) | 196 (35.0) | |
| Lose Insurance† | 8902 | 50 | 996 | 681 | 6403 | 266 | 506 | 0.005§ |
| Definitely yes | 327 (3.6) | 0 (0.0) | 28 (2.8) | 67 (2.8) | 181 (13.8) | 20 (7.5) | 31 (6.1) | |
| Probably yes | 497 (5.7) | 5 (10.0) | 72 (7.2) | 83 (7.2) | 268 (4.2) | 24 (9.0) | 45 (9.0) | |
| Might or might not | 1378 (15.5) | 15 (30.0) | 170 (17.1) | 134 (17.1) | 889 (13.9) | 60 (22.6) | 110 (21.7) | |
| Probably not | 2511 (28.2) | 10 (20.0) | 299 (30.0) | 160 (30.0) | 1867 (29.2) | 67 (52.2) | 108 (21.3) | 0.000§ |
| Definitely not | 4189 (47.0) | 20 (40.0) | 427 (42.9) | 237 (42.9 | 3198 (49.9) | 95 (35.1) | 212 (41.9) |
*P values were calculated using a one-way analysis of variance between WHO regions.
†Denominators excluded individuals who did not respond.
‡Denotes p<0.001.
§Denotes p<0.05.
¶Question was select all that apply and were calculated by overall regional count.
LGBTQ, lesbian, gay, bisexual, transgender and queer.
Access to care
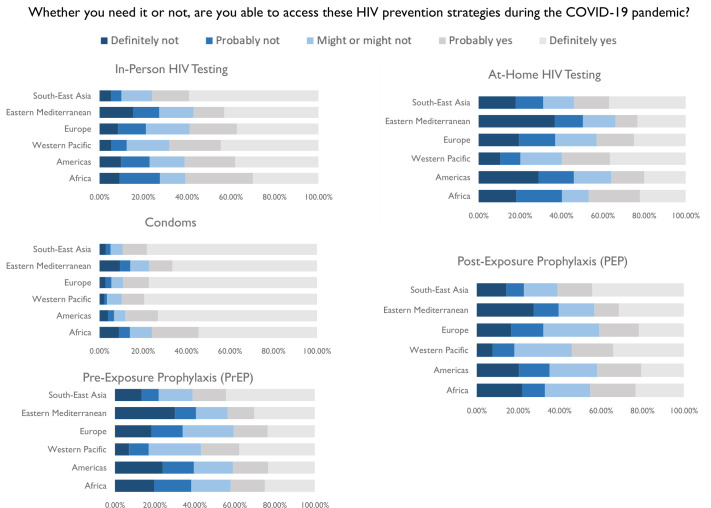
There are existing gaps in care for LGBTQ+ individuals, with many being underinsured or lacking insurance entirely.37–42 Those living in countries without a nationalised health programme are left at increased risk for both economic and health-related despair. The high cost of health services that are required when someone becomes infected with COVID-19 further adds to this already heavy burden.43–47 A majority of individuals indicated that they had access (84.8%) to masks (table 4). A total of 4486 (37.9%) individuals reported having government insurance, 1866 (15.8%) no insurance, and 5475 (46.3%) having insurance from private/employer/other. The differences in insurance between regions was statistically significant (F(5,12)=9.607, p=0.0007). One-quarter of individuals indicated that they may lose insurance, and the differences in expecting to lose insurance between regions was also significant according to a one-way ANOVA (F(4,20)=4.540, p=0.009). Access to HIV prevention methods (testing, condoms, PrEP, PEP) has also become more difficult because of the pandemic (figure 2).
Table 4.
Economic and indicators among LGBTQ+ individuals from the COVID-19 disparities survey distributed between 16 April 2020 and 4 May 2020, stratified by WHO region
| Indicator | Overall (%) | Africa | Americas | Southeast Asia | Europe | Eastern Mediterranean | Western Pacific | P value* |
| Occupation‡¶ | 13 115 | 102 | 1262 | 1255 | 9322 | 533 | 641 | 0.000† |
| Services and sales | 19 | 253 | 243 | 1874 | 69 | 165 | ||
| Skilled agriculture | 3 | 8 | 35 | 117 | 11 | 9 | ||
| Crafts | 7 | 21 | 35 | 232 | 21 | 12 | ||
| Manufacturing plant | 6 | 20 | 66 | 471 | 23 | 36 | ||
| Domestic work | 11 | 17 | 19 | 79 | 7 | 10 | ||
| Informal | 6 | 39 | 26 | 334 | 8 | 9 | ||
| Underground | 5 | 8 | 4 | 32 | 4 | 2 | ||
| Hospitality | 6 | 44 | 82 | 320 | 23 | 31 | ||
| Professional | 23 | 438 | 147 | 2042 | 109 | 136 | ||
| Artistic | 7 | 91 | 36 | 650 | 28 | 23 | ||
| Armed forced | 4 | 8 | 8 | 97 | 21 | 17 | ||
| Freelance | 6 | 105 | 103 | 283 | 53 | 33 | ||
| Unemployed | 13 | 129 | 97 | 1113 | 64 | 47 | ||
| Other | 17 | 193 | 208 | 1264 | 61 | 78 | 0.08 | |
| Not applicable | 20 | 123 | 79 | 889 | 38 | 61 | ||
| Afford to miss work‡¶ | 11 805 | 89 | 920 | 1030 | 8478 | 421 | 562 | 0.000† |
| I already lost my job | 10 (11.2) | 98 (8.0) | 168 (16.3) | 846 (10.0) | 51 (12.1) | 41 (7.3) | ||
| I am on paid leave | 3 (3.4) | 81 (6.6) | 61 (5.9) | 605 (7.1) | 19 (4.5) | 25 (4.4) | ||
| I telecommute (work from home) | 13 (14.6) | 342 (27.8) | 166 (16.1) | 1950 (23.0) | 55 (13.1) | 72 (12.8) | ||
| I was not working before COVID-19 | 11 (12.4) | 104 (8.5) | 77 (7.5) | 733 (8.6) | 43 (10.2) | 39 (7.0) | ||
| No, but I am following the confinement measure | 22 (24.7) | 258 (21.0) | 182 (17.7) | 1894 (22.3) | 110 (26.1) | 146 (26.0) | ||
| No, I need to work to survive and cannot stay at home, regardless of COVID-19 | 10 (11.2) | 129 (10.5) | 285 (27.7) | 1211 (27.7) | 82 (19.5) | 129 (23.0) | ||
| Not applicable | 20 (22.5) | 218 (17.7) | 91 (8.8) | 1239 (8.8) | 61 (14.5) | 110 (19.6) | ||
| Lost job due to COVID‡ | 11 827 | 88 | 1225 | 1032 | 8499 | 420 | 563 | 0.297 |
| Yes | 1625 (13.7) | 74 (15.9) | 1071 (87.4) | 187 (18.1) | 1164 (13.7) | 65 (15.5) | 41 (7.23) | |
| No | 10 197 (86.3) | 14 (84.1) | 154 (12.6) | 845 (81.9) | 7335 (86.3) | 355 (84.5) | 522 (92.3 | |
| Meet basic needs‡ | 11 821 | 90 | 1229 | 1029 | 8496 | 417 | 560 | 0.000§ |
| Not at all | 497 (4.2) | 5 (5.6) | 37 (3.0) | 38 (3.7) | 352 (4.1) | 32 (7.7) | 33 (5.9) | |
| Slightly | 1699 (14.4) | 19 (21.1) | 86 (7.0) | 148 (14.4) | 1309 (15.4) | 86 (20.6) | 51 (9.1) | |
| Somewhat | 2995 (25.3) | 21 (23.3) | 228 (18.5) | 213 (20.7) | 2249 (26.5) | 95 (22.8) | 189 (3.8) | |
| Fairly well | 4037 (34.2) | 25 (27.8) | 425 (34.6) | 346 (33.6) | 2975 (35.0) | 114 (27.3) | 152 (27.1) | |
| Very well | 2593 (21.9) | 20 (22.2) | 453 (36.9) | 284 (27.6) | 1611 (19.0) | 90 (21.6) | 135 (24.1) | |
| Skipped meals‡ | 11 828 | 89 | 1222 | 1035 | 8505 | 422 | 555 | 0.136 |
| I don't know | 565 (4.8) | 5 (5.6) | 33 (2.7) | 50 (4.8) | 407 (4.8) | 44 (10.4) | 26 (4.7) | |
| No | 8578 (72.5) | 47 (52.8) | 987 (80.8) | 589 (56.9) | 6313 (74.2) | 227 (53.8) | 415 (74.8) | 0.39 |
| Yes | 2685 (22.7) | 37 (41.6) | 202 (16.5) | 396 (38.3) | 1785 (21.0) | 151 (35.8) | 114 (20.5) | |
| Income reduction‡ | 11 692 | 86 | 1219 | 1030 | 8395 | 407 | 555 | 0.000§ |
| 0% | 3691 (31.6) | 24 (27.9) | 378 (31.0) | 188 (18.2) | 2813 (33.5) | 106 (26.2) | 182 (32.8) | |
| 1%–29% | 2854 (24.4) | 11 (12.8) | 264 (21.7) | 260 (25.2) | 2045 (24.3) | 86 (21.1) | 188 (33.9) | |
| 30%–59% | 2479 (21.2) | 22 (25.6) | 309 (25.3) | 233 (22.6) | 1703 (20.2) | 105 (25.7) | 107 (19.3) | |
| 60%–100% | 2668 (22.8) | 29 (33.7) | 268 (22.0) | 349 (34.0) | 1834 (22.0) | 110 (27.0) | 78 (14.0) | |
| Receive benefits‡ | 9610 | 76 | 1095 | 863 | 6759 | 322 | 495 | 0.01† |
| No, but it is needed | 4808 (50.0) | 41 (54.0) | 403 (36.8) | 423 (49.0) | 3531 (52.2) | 181 (56.2) | 229 (46.3) | |
| No, it is not needed | 3121 (32.5) | 20 (26.3) | 447 (40.8) | 148 (17.1) | 2263 (33.5) | 88 (27.3) | 155 (31.1) | |
| Yes, but it is not needed | 280 (2.9) | 0 (0.0) | 36 (3.3) | 17 (2.0) | 189 (2.8) | 13 (4.1) | 25 (5.0) | |
| Yes, it is needed | 1401 (14.6) | 15 (19.7) | 209 (19.1) | 275 (31.9) | 776 (11.5) | 40 (12.4) | 86 (17.6) |
*P values were calculated using a one-way analysis of variance between WHO regions.
†Denotes p<0.05.
‡Denominators excluded individuals who did not respond.
§Denotes p<0.001.
¶Question was select all that apply and were calculated by overall regional count.
LGBTQ, lesbian, gay, bisexual, transgender and queer.
Figure 2.
Access to HIV prevention strategies for LGBTQ+ persons from from the COVID-19 Disparities Survey distributed between April 16 and May 4, 2020, stratified by WHO region.
Discussion
COVID-19 has rapidly emerged as a major public health threat, causing significant global disruption. Growing evidence indicates that the incidence of COVID-19 is higher in communities of lower socioeconomic status, in which LGBTQ+ individuals are over-represented given their long history of economic marginalisation.48–51 Additionally, higher burdens of mental health and infectious diseases—due to the intersection of upstream determinants such as stigma, criminalisation of same-sex practices and sex work, and continued limited investment in these communities—place LGBTQ+ individuals at even higher risk.2 13 16 Such compounding vulnerabilities result in earlier disruptions to health services, leading to prolonged periods without access to care, especially during global crises.31 These impacts are felt more strongly among those further marginalised by society, such as sex workers, racial/ethnic minorities, immigrants, and those lacking access to healthcare. These realities will undoubtedly reinforce the intersectional vulnerabilities that existed before the COVID-19 pandemic.
This descriptive analysis highlights the severe impacts to mental health, access to care and socioeconomics that members of the LGBTQ+ community are experiencing. Be it the nearly one-quarter of individuals experiencing food insecurity, or the one-half of individuals who have yet to receive financial benefits, despite need. The inability to meet basic needs will likely be exacerbated further for individuals who are unemployed or working in industries most directly impacted by COVID-19.52 Even among those who have remained employed during the pandemic, reductions in income will likely put additional strain on individuals during an already difficult period.
While most individuals who participated in the survey reported having access to masks, at least one in five of individuals were unsure if they would continue to have insurance. Condoms as a means of HIV prevention remained largely accessible despite the pandemic, while at-home HIV testing, PrEP and PEP were the prevention methods that became more difficult to access during the COVID-19 crisis. This is particularly alarming because members of the LGBTQ+ continue to be disproportionately impacted by HIV globally,20 so these disparities in access to prevention strategies may lead to heightened vulnerability to HIV, especially among minorities, immigrants and others who may have been forced to engage in sex work due to the pandemic.53–56 This also has major implications for rates of HIV transmission throughout the duration of the crisis, where changes in income and employment have been shown to increase HIV risk.57 58 Furthermore, while this analysis did not examine the impact of COVID-19 on those living with HIV, it’s been shown that interruptions to the HIV care continuum may have impacts on community transmission, treatment, and mortality.59–62 Unless efforts are undertaken to address these disparities in access to methods of prevention, decades of progress may be lost.
Given the wide variation in healthcare coverage around the world, it should not be forgotten that one in six individuals indicated having no insurance at all. This is of particular importance within the context of the 50.0% of individuals who reported having moderate and severe psychological distress, as well as those who screened positive for anxiety and/or depression. While there has been a large international focus on the clinical manifestations and treatment for COVID-19, it is worth noting that there is likely an even bigger crisis brewing just under the surface as people continue to experience the psychological distress associated with the response to COVID-19, and our data indicate that members of the LGBTQ+ community are no different. With efforts to mitigate this growing mental health crisis, there is a continued need to not only characterise its parameters, but implement targeted solutions with the utmost urgency.
These findings highlight important considerations in the wake of this pandemic. It is evident that there is a growing need to mitigate the impacts of this crisis by circumventing traditional models of care to ensure continuity and achieve long-term health outcomes. Telemedicine continues to show promise as a way to ensure individuals have continued care, allowing for patient–provider interactions while minimising the risk of new COVID-19 transmission events.63–66 Additionally, mHealth strategies will become even more important to keep in touch and regularly check-in with patients now that in-person contact is largely discouraged.67 68 While access to in-person HIV testing remains moderately accessible according to our analysis, moving forward it will be crucial to implement strategies that limit the need to travel and possible interactions with the general public, such as delivery of at-home testing kits, drop-off testing, or even mobile testing. Even if improvements in the use of technology for care continue, without addressing the digital divide that persists in many communities around the world, it is likely that the most vulnerable among us will remain increasingly vulnerable and may even further exacerbate existing disparities.69–71 Additionally, these findings indicate the need to develop more robust and targeted approaches for regional differences and sub-populations. Economic support, HIV prevention and mental health services will remain pivotal moving forward, and while targeted and tailored, individual-level interventions are necessary, they will likely not be enough. Structural and policy changes which prioritise public health and address the systemic barriers that individuals in this community continue to face are necessary to ensure economic and health equity long term.
For countries where there is higher acceptability of LGBTQ+ people, this may begin with disaggregating data by sexual orientation and gender identity at the local, subnational and national levels. In many countries around the world, no data are collected on these communities, and short of researchers using novel methods to estimate population size these individuals would otherwise, ‘not count’.72 73 For countries with less favourable views, it will require recognition of this community, eliminating criminalising policies on same-sex behaviour and sex work, extending the right to marry for same-sex couples and establishing laws that bestow legal protection to members of this marginalised community throughout society.13 74 75
Notably, there are some limitations of this study. Individuals must be users of Hornet in order to participate in the survey, and thus must have internet and smartphone access, limiting generalisability of the findings to a target population of interest. Additionally, emerging evidence indicates that COVID-19 is having a larger impact on those of lower socioeconomic status (ie, without internet or smartphone access); therefore, it is possible that this underestimates the true magnitude of the pandemic on more marginalised individuals in these communities. Even so, prior studies have documented the success of using social networking platforms to reach hidden and stigmatised populations. It is also possible that barriers such as language or stigma, led particular subgroups to not participate or complete the survey in its entirety, resulting in non-response bias. To mitigate this, we plan to translate later iterations of the study into additional languages. Meaning that further studies, including but not limited to qualitative interviews, will be required to characterise the impact of the COVID-19 crisis further. As well, this is a convenience sample and cross-sectional in nature, so may not be representative of the whole LGBTQ+ community and precludes our ability to examine temporality in the outcomes we analysed.
Despite these limitations, the novel use of a rapid survey among users of a social network application provides insight into the effects felt by the LGBTQ+ community in real time, when it may otherwise be infeasible to collect such information as scale. Collectively, these results reflect the impact that the pandemic will have on the LGBTQ+ community, and the need for continued monitoring and policy action as the COVID-19 crisis progresses.
Conclusion
These findings represent individuals from 136 countries and highlight the clear immediate and secondary effects of COVID-19 on LGBTQ+ communities around the world, while emphasising the need for additional data to guide future programmes and policies. If not for surveys of this kind, which leveraged a global social network and app-based technology, we would be unable to obtain this quantity of accurate, and real-time information on how marginalised communities are being impacted by the pandemic, nor at this level of granularity. This novel, technology-based approach highlights the profoundly detrimental impact that COVID-19 is having and will continue to have on LGBTQ+ communities, thereby underscoring the need for a data driven and timely response, both immediately, and in the wake of this crisis.
Supplementary Material
Acknowledgments
We would like to acknowledge the following language translators: Ana Cara-Linda, Anna Yakusik, Carol Strong, Damiano Cerasuolo, Ezgi Ayeser, Henrique Vicentim, Howie Lim, Ibu Ketty, Jose Garcia, Junming Wu, Ketty Rosenfeld, Luana Araujo, Mariano Ruiz, Maso, Panyaphon Phiphatkunarnon, Pedro Moreno, Poyao Huang, Souad Orhan, Stephane Ku, Tanat Chinbunchorn, Teak Sowaprux, Top Medping, and Yalda Toofan
Footnotes
Twitter: @BrotherAdamson
Collaborators: COVID-19 Disparities Working Group: Omar Cherkaoui, Angelica Lopez-Hernandez, Edward Sutanto
Contributors: TA and MH conducted analyses and drafted figures and tables. TA, MH, SW, SB, CB and SH contributed to the initial drafting of this manuscript. All authors contributed opinions and feedback based on their individual expertise and the policies of their centres critically reviewed the manuscript. All authors agreed to submit the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. No additional data available currently.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Study procedures were reviewed by the Johns Hopkins School of Public Health Institutional Review Board, which determined that the protocol qualified for exempt status under category 4.
References
- 1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Santos G-M, Ackerman B, Rao A, et al. Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of Cisgender gay men and other men who have sex with men. AIDS Behav 2021;25:311–21. 10.1007/s10461-020-02969-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jarrett BA, Peitzmeier SM, Restar A, et al. Gender-affirming care, mental health, and economic stability in the time of COVID-19: a global cross-sectional study of transgender and non-binary people. medRxiv 2020. 10.1101/2020.11.02.20224709. [Epub ahead of print: 04 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hall KS, Samari G, Garbers S, et al. Centring sexual and reproductive health and justice in the global COVID-19 response. Lancet 2020;395:1175–7. 10.1016/S0140-6736(20)30801-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hale T, Webster S. Oxford COVID-19 government response tracker, 2020. Available: https://apo.org.au/node/303043 [DOI] [PubMed]
- 6. DeMulder J, Kraus-Perrotta C, Zaidi H. Sexual and gender minority adolescents must be prioritised during the global COVID-19 public health response. Sex Reprod Health Matters 2020;28:1804717. 10.1080/26410397.2020.1804717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry 2020;7:389–90. 10.1016/S2215-0366(20)30141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV 2020;7:e308–9. 10.1016/S2352-3018(20)30105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Poteat TC, Reisner SL, Miller M, et al. COVID-19 vulnerability of transgender women with and without HIV infection in the eastern and southern U.S. medRxiv 2020. 10.1101/2020.07.21.20159327. [Epub ahead of print: 24 Jul 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barnert E, Ahalt C, Williams B. Prisons: amplifiers of the COVID-19 pandemic hiding in plain sight. Am J Public Health 2020;110:964–6. 10.2105/AJPH.2020.305713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koh D. Migrant workers and COVID-19. Occup Environ Med 2020;77:634. 10.1136/oemed-2020-106626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kline NS. Rethinking COVID-19 vulnerability: a call for LGTBQ+ Im/migrant health equity in the United States during and after a pandemic. Health Equity 2020;4:239–42. 10.1089/heq.2020.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wallach S, Garner A, Howell S, et al. Address exacerbated health disparities and risks to LGBTQ+ individuals during COVID-19. Health Hum Rights 2020;22:313–6. [PMC free article] [PubMed] [Google Scholar]
- 14. Banerjee D, Rao TSS, Sexuality RTSS. Sexuality, sexual well being, and intimacy during COVID-19 pandemic: an advocacy perspective. Indian J Psychiatry 2020;62:418–26. 10.4103/psychiatry.IndianJPsychiatry_484_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fraser B, Pierse N, Chisholm E, et al. LGBTIQ+ homelessness: a review of the literature. Int J Environ Res Public Health 2019;16:2677. 10.3390/ijerph16152677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hutchcraft ML, Teferra AA, Montemorano L, et al. Differences in health-related quality of life and health behaviors among Lesbian, bisexual, and heterosexual women surviving cancer from the 2013 to 2018 National health interview survey. LGBT Health 2021;8:68–78. 10.1089/lgbt.2020.0185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Raifman J, Bor J, Venkataramani A. Unemployment insurance and food insecurity among people who lost employment in the wake of COVID-19. medRxiv 2020. 10.1101/2020.07.28.20163618. [Epub ahead of print: 30 Jul 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Salerno JP, Williams ND, Gattamorta KA. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychol Trauma 2020;12:S239–42. 10.1037/tra0000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hogan AB, Jewell BL, Sherrard-Smith E, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e1132–41. 10.1016/S2214-109X(20)30288-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. UNAIDS data, 2019. Available: https://www.unaids.org/en/resources/documents/2019/2019-UNAIDS-data [Accessed 1 Feb 2021].
- 21. Jewell BL, Mudimu E, Stover J, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. Lancet HIV 2020;7:e629–40. 10.1016/S2352-3018(20)30211-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The Lancet Hiv . When pandemics collide. Lancet HIV 2020;7:e301. 10.1016/S2352-3018(20)30113-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Logie CH, Lacombe-Duncan A, Brien N, et al. Barriers and facilitators to HIV testing among young men who have sex with men and transgender women in Kingston, Jamaica: a qualitative study. J Int AIDS Soc 2017;20:21385. 10.7448/IAS.20.1.21385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Agénor M, Pérez AE, Koma JW, et al. Sexual orientation identity, Race/Ethnicity, and lifetime HIV testing in a national probability sample of U.S. women and men: an intersectional approach. LGBT Health 2019;6:306–18. 10.1089/lgbt.2019.0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rael CT, Martinez M, Giguere R, et al. Barriers and facilitators to oral PreP use among transgender women in New York City. AIDS Behav 2018;22:3627–36. 10.1007/s10461-018-2102-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Duffus WA, Davis HT, Byrd MD, et al. Hiv testing in women: missed opportunities. J Womens Health 2012;21:170–8. 10.1089/jwh.2010.2655 [DOI] [PubMed] [Google Scholar]
- 27. Schweighardt B, Ortiz GM, Grant RM. Emergence of drug-resistant HIV-1 variants in patients undergoing structured treatment interruptions. AIDS, 2002. Available: https://journals.lww.com/aidsonline/Fulltext/2002/11220/Emergence_of_drug_resistant_HIV_1_variants_in.18.aspx [DOI] [PubMed]
- 28. Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med 2016;375:830–9. 10.1056/NEJMoa1600693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Strategies for Management of Antiretroviral Therapy (SMART) Study Group, El-Sadr WM, Lundgren JD, et al. Cd4+ count-guided interruption of antiretroviral treatment. N Engl J Med 2006;355:2283-96. 10.1056/NEJMoa062360 [DOI] [PubMed] [Google Scholar]
- 30. Kroenke K, Spitzer RL, Williams JBW, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613–21. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 31. Fredriksen-Goldsen KI, Simoni JM, Kim H-J, et al. The health equity promotion model: reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. Am J Orthopsychiatry 2014;84:653–63. 10.1037/ort0000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bockting WO, Miner MH, Swinburne Romine RE, et al. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health 2013;103:943–51. 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Feinstein BA, Goldfried MR, Davila J. The relationship between experiences of discrimination and mental health among lesbians and gay men: an examination of internalized homonegativity and rejection sensitivity as potential mechanisms. J Consult Clin Psychol 2012;80:917–27. 10.1037/a0029425 [DOI] [PubMed] [Google Scholar]
- 34. Balsam KF, Molina Y, Beadnell B, et al. Measuring multiple minority stress: the LGBT people of color Microaggressions scale. Cultur Divers Ethnic Minor Psychol 2011;17:163–74. 10.1037/a0023244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fredriksen-Goldsen KI, Emlet CA, Kim H-J, et al. The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: the role of key health indicators and risk and protective factors. Gerontologist 2013;53:664–75. 10.1093/geront/gns123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. The economic impact of COVID-19 on the LGBTQ community. HRC. Available: https://www.hrc.org/resources/the-economic-impact-of-covid-19-on-the-lgbtq-community [Accessed 4 Feb 2021].
- 37. Dahlhamer JM, Galinsky AM, Joestl SS, et al. Barriers to health care among adults identifying as sexual minorities: a US national study. Am J Public Health 2016;106:1116–22. 10.2105/AJPH.2016.303049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health 2010;100:489–95. 10.2105/AJPH.2009.160804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Radix A, Maingi S. LGBT cultural competence and interventions to help oncology nurses and other health care providers. Semin Oncol Nurs 2018;34:80–9. 10.1016/j.soncn.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 40. Macapagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse Lesbian, gay, bisexual, transgender, and Questioning emerging adults. LGBT Health 2016;3:434–42. 10.1089/lgbt.2015.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Qureshi RI, Zha P, Kim S, et al. Health care needs and care utilization among Lesbian, gay, bisexual, and transgender populations in New Jersey. J Homosex 2018;65:167–80. 10.1080/00918369.2017.1311555 [DOI] [PubMed] [Google Scholar]
- 42. Injustice at every turn: a report of the National transgender discrimination survey. National LGBTQ Task force, 2011. Available: https://www.thetaskforce.org/injustice-every-turn-report-national-transgender-discrimination-survey/ [Accessed 4 Feb 2021].
- 43. Yamin M. Counting the cost of COVID-19. Int J Inf Technol 2020:311–7. 10.1007/s41870-020-00466-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bartsch SM, Ferguson MC, McKinnell JA, et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff 2020;39:927–35. 10.1377/hlthaff.2020.00426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liu Y, Lee JM, Lee C. The challenges and opportunities of a global health crisis: the management and business implications of COVID-19 from an Asian perspective. Asian Bus Manage 2020;19:277–97. 10.1057/s41291-020-00119-x [DOI] [Google Scholar]
- 46. Khan JR, Awan N, Islam MM, et al. Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: a global analysis. Front Public Health 2020;8:347. 10.3389/fpubh.2020.00347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tan-Torres Edejer T, Hanssen O, Mirelman A, et al. Projected health-care resource needs for an effective response to COVID-19 in 73 low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e1372–9. 10.1016/S2214-109X(20)30383-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Emlet CA, Social ECA. Social, economic, and health disparities among LGBT older adults. Generations 2016;40:16–22. [PMC free article] [PubMed] [Google Scholar]
- 49. Patel JA, Nielsen FBH, Badiani AA, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health 2020;183:110–1. 10.1016/j.puhe.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Corburn J, Vlahov D, Mberu B, et al. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J Urban Health 2020;97:348–57. 10.1007/s11524-020-00438-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8:659–61. 10.1016/S2213-2600(20)30234-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Charlton BM, Gordon AR, Reisner SL, et al. Sexual orientation-related disparities in employment, health insurance, healthcare access and health-related quality of life: a cohort study of US male and female adolescents and young adults. BMJ Open 2018;8:e020418. 10.1136/bmjopen-2017-020418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Baral SD, Friedman MR, Geibel S, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet 2015;385:260–73. 10.1016/S0140-6736(14)60801-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Santos G-M, Makofane K, Arreola S, et al. Reductions in access to HIV prevention and care services are associated with arrest and convictions in a global survey of men who have sex with men. Sex Transm Infect 2017;93:62–4. 10.1136/sextrans-2015-052386 [DOI] [PubMed] [Google Scholar]
- 55. Santos G-M, Do T, Beck J, et al. Syndemic conditions associated with increased HIV risk in a global sample of men who have sex with men. Sex Transm Infect 2014;90:250–3. 10.1136/sextrans-2013-051318 [DOI] [PubMed] [Google Scholar]
- 56. Martinez O, Brady KA, Levine E, et al. Using Syndemics theory to examine HIV sexual risk among Latinx men who have sex with men in Philadelphia, PA: findings from the National HIV behavioral surveillance. EHQUIDAD 2020;13:217–36. 10.15257/ehquidad.2020.0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Maulsby CH, Ratnayake A, Hesson D, et al. A scoping review of employment and HIV. AIDS Behav 2020;24:2942–55. 10.1007/s10461-020-02845-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Delpierre C, Cuzin L, Lauwers-Cances V, et al. Unemployment as a risk factor for AIDS and death for HIV-infected patients in the era of highly active antiretroviral therapy. Sex Transm Infect 2008;84:183–6. 10.1136/sti.2007.027961 [DOI] [PubMed] [Google Scholar]
- 59. Chenneville T, Gabbidon K, Hanson P, et al. The impact of COVID-19 on HIV treatment and research: a call to action. Int J Environ Res Public Health 2020;17:4548. 10.3390/ijerph17124548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mitchell KM, Dimitrov D, Silhol R, et al. Estimating the potential impact of COVID-19-related disruptions on HIV incidence and mortality among men who have sex with men in the United States: a modelling study. medRxiv 2020. 10.1101/2020.10.30.20222893. [Epub ahead of print: 03 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pinto RM, Park S. COVID-19 pandemic disrupts HIV continuum of care and prevention: implications for research and practice concerning community-based organizations and frontline providers. AIDS Behav 2020;24:2486–9. 10.1007/s10461-020-02893-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Prabhu S, Poongulali S, Kumarasamy N. Impact of COVID-19 on people living with HIV: a review. J Virus Erad 2020;6:100019. 10.1016/j.jve.2020.100019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mgbako O, Miller EH, Santoro AF, et al. COVID-19, telemedicine, and patient Empowerment in HIV care and research. AIDS Behav 2020;24:1990–3. 10.1007/s10461-020-02926-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Touger R, Wood BR. A review of telehealth innovations for HIV pre-exposure prophylaxis (PreP). Curr HIV/AIDS Rep 2019;16:113–9. 10.1007/s11904-019-00430-z [DOI] [PubMed] [Google Scholar]
- 65. Rogers BG, Coats CS, Adams E, et al. Development of Telemedicine Infrastructure at an LGBTQ+ Clinic to Support HIV Prevention and Care in Response to COVID-19, Providence, RI. AIDS Behav 2020;24:2743–7. 10.1007/s10461-020-02895-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Langarizadeh M, Tabatabaei MS, Tavakol K, et al. Telemental health care, an effective alternative to conventional mental care: a systematic review. Acta Inform Med 2017;25:240–6. 10.5455/aim.2017.25.240-246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wong KYK, Stafylis C, Klausner JD. Telemedicine: a solution to disparities in human immunodeficiency virus prevention and pre-exposure prophylaxis uptake, and a framework to scalability and equity. Mhealth 2020;6:21. 10.21037/mhealth.2019.12.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Catalani C, Philbrick W, Fraser H, et al. mHealth for HIV treatment & prevention: a systematic review of the literature. Open AIDS J 2013;7:17–41. 10.2174/1874613620130812003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Blandford A, Wesson J, Amalberti R, et al. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob Health 2020;8:e1364–5. 10.1016/S2214-109X(20)30362-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Campbell BR, Ingersoll KS, Flickinger TE, et al. Bridging the digital health divide: toward equitable global access to mobile health interventions for people living with HIV. Expert Rev Anti Infect Ther 2019;17:141–4. 10.1080/14787210.2019.1578649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: How COVID-19's telemedicine expansion could exacerbate disparities. J Am Acad Dermatol 2020;83:e345–6. 10.1016/j.jaad.2020.07.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Baral S, Turner RM, Lyons CE, et al. Population size estimation of gay and bisexual men and other men who have sex with men using social Media-Based platforms. JMIR Public Health Surveill 2018;4:e15. 10.2196/publichealth.9321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Cahill SR, Makadon HJ. If they don’t count us, we don’t count: trump administration rolls back sexual orientation and gender identity data collection. LGBT Health 2017;4:171–3. 10.1089/lgbt.2017.0073 [DOI] [PubMed] [Google Scholar]
- 74. Beyrer C. Pushback: the current wave of anti-homosexuality laws and impacts on health. PLoS Med 2014;11:e1001658. 10.1371/journal.pmed.1001658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Marks SM. Global recognition of human rights for lesbian, gay, bisexual, and transgender people. Health Hum Rights 2006;9:33–42. 10.2307/4065388 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. No additional data available currently.