Key Points
Hematologic toxicity was observed in ∼20% of patients receiving anti-CD19 CAR T-cell therapy.
Higher CRS severity and CRS-related cytokine levels and lower prelymphodepletion platelet count predicted hematologic toxicity.
Visual Abstract
Abstract
CD19-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated remarkable efficacy in patients with relapsed/refractory B-cell malignancies; however, it is associated with toxicities including cytokine release syndrome (CRS), neurotoxicity, and impaired hematopoietic recovery. The latter is associated with high-grade cytopenias requiring extended growth factor or transfusional support, potentially leading to additional complications such as infection or hemorrhage. To date, the factors independently associated with hematologic toxicity have not been well characterized. To address this deficit, we retrospectively analyzed 173 patients who received defined-composition CD19 CAR T-cell therapy in a phase 1/2 clinical trial (https://clinicaltrials.gov; NCT01865617), with primary end points of absolute neutrophil count and platelet count at day-28 after CAR T-cell infusion. We observed cumulative incidences of neutrophil and platelet recovery of 81% and 75%, respectively, at 28 days after infusion. Hematologic toxicity was noted in a significant subset of patients, with persistent neutropenia in 9% and thrombocytopenia in 14% at last follow-up. Using debiased least absolute shrinkage selector and operator regression analysis for high-dimensional modeling and considering patient-, disease-, and treatment-related variables, we identified increased CRS severity as an independent predictor for decreased platelet count and lower prelymphodepletion platelet count as an independent predictor of both decreased neutrophil and platelet counts after CD19 CAR T-cell infusion. Furthermore, multivariable models including CRS-related cytokines identified associations between higher peak serum concentrations of interleukin-6 and lower day-28 cell counts; in contrast, higher serum concentrations of transforming growth factor-β1 were associated with higher counts. Our findings suggest that patient selection and improved CRS management may improve hematopoietic recovery after CD19 CAR T-cell therapy.
Introduction
CD19-targeted chimeric antigen receptor (CD19 CAR) T-cell therapy has demonstrated promising efficacy in patients with relapsed or refractory (R/R) B-cell malignancies with high objective or overall response rate (ORR) and complete response/remission (CR) or CR with incomplete hematologic recovery rates in acute lymphoblastic leukemia1 (ALL; 68% to 93% CR), chronic lymphocytic leukemia (CLL; 57% to 74% ORR; 21% CR),2,3 mantle cell lymphoma4 (59% CR), and large B-cell lymphoma5-9 (LBCL; 52% to 88% ORR; 40% to 59% CR), the latter including patients with diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, and transformed follicular lymphoma.10 A subset of these patients has demonstrated durable responses, with CR of >2 years without the need for further treatment.5,7 Consequently, the US Food and Drug Administration approved 4 CD19 CAR T-cell products: axicabtagene ciloleucel (Yescarta) for the treatment of R/R LBCL and primary mediastinal B-cell lymphoma; tisagenlecleucel (Kymriah) for R/R LBCL and ALL in children and young adults; and, most recently, brexucabtagene autoleucel (Tecartus) for the treatment of R/R mantle cell lymphoma and lisocabtagene maraleucel (Breyanzi) for R/R LBCL.
CD19 CAR T-cell therapy, however, is associated with significant toxicities that impede its development and wide dissemination: cytokine release syndrome (CRS), immune effector cell–associated neurotoxicity syndrome (ICANS), B-cell aplasia, and early and late infections.11-13 Furthermore, hematologic toxicity, including delayed hematopoietic recovery with persistent high-grade neutropenia, anemia, and thrombocytopenia, has been observed in a subset of patients who undergo CAR T-cell therapies targeting CD195,7,9,11,14 and other antigens.15,16 We have reported prolonged cytopenia requiring transfusions or growth factor support in a phase 1/2 trial of defined-composition CD19 CAR T-cell therapy, either starting or persisting beyond 90 days after CAR T-cell infusion in 16% of patients in CR for at least 1 year and without myelodysplastic syndrome after treatment.11 In the ZUMA15 and ELIANA17 studies, investigators reported 17% of patients with grade ≥3 cytopenia at ≥3 months after CAR T-cell infusion in the former study and grade ≥3 neutropenia (11%) and thrombocytopenia (12%) at a median follow-up of 13.1 months in the latter. Prolonged cytopenias were also noted in the recent TRANSCEND NHL 001 study,9 with 37% of evaluable patients with grade ≥3 cytopenia at day-29, and prolonged neutropenia (7%), thrombocytopenia (26%), and anemia (9%) by day-180.
Prolonged cytopenia may result in increased frequency of infections,13,18 hemorrhagic events, extended growth factor administration, and blood product transfusions. Persistent transfusion requirements are associated with risks of iron overload, transfusion-associated reactions, circulatory overload, and lung injury. These adverse effects may ultimately contribute to treatment-related morbidity and mortality, increased use of resources, and impaired quality of life.
Results of studies by our group19 and others20 have suggested an association between the severity of CRS and lower hematologic nadirs, delayed hematopoietic recovery, and increased dependence on transfusion. Yet, the factors that independently influence hematopoietic recovery after CD19 CAR T-cell therapy remain poorly understood; recent analyses have been limited by small cohort sizes leading to low statistical power that precludes robust multivariable modeling. In addition, the methodology used in these studies did not account for competing events.14,20-22 We performed a retrospective analysis of a cohort of 173 patients treated at our institution in a phase 1/2 clinical trial of defined-composition CD19 CAR T-cell therapy for B-cell malignancies. By applying the debiased LASSO (least absolute shrinkage and selection operator) to draw inference of the effects of multiple variables, we identified key factors independently associated with prolonged hematopoietic toxicity after CD19 CAR T-cell therapy.
Methods
Patients and study design
We performed a retrospective analysis of patients with R/R B-cell malignancies, including ALL, non-Hodgkin lymphoma (NHL), and CLL, who were treated with CD19-targeted CAR T-cells in a phase 1/2 clinical trial at our institution (https://clinicaltrials.gov, NCT01865617).1,2,8 The CAR construct comprised a CD19-targeting single-chain variable fragment (scFv) derived from the FMC63 monoclonal antibody fused to an immunoglobulin-G4 (IgG4) hinge region, a CD28 transmembrane domain, a 4-1BB costimulatory domain, and a CD3ζ signaling sequence. The CAR construct was separated by a T2A ribosomal skip sequence from a truncated human epidermal growth factor receptor (EGFRt), which served as a marker of transgene expression, as previously described.1,8 Patients received lymphodepleting chemotherapy with cyclophosphamide and fludarabine at high (60 mg/kg or >1500 mg/m2 cyclophosphamide with 75-125 mg/m2 fludarabine) or low (30 mg/kg or ≤1500 mg/m2 cyclophosphamide with 75-90 mg/m2 fludarabine) intensities or other regimens (supplemental Table 2). Lymphodepletion was followed 2 to 4 days later by infusion of CD19 CAR T-cells formulated in a 1:1 ratio of CD4+:CD8+ CAR T-cells at 1 of 3 dose levels: DL1, 2 × 105 EGFRt+ cells/kg; DL2, 2 × 106 EGFRt+cells/kg; or DL3, 2 × 107 EGFRt+ cells/kg.
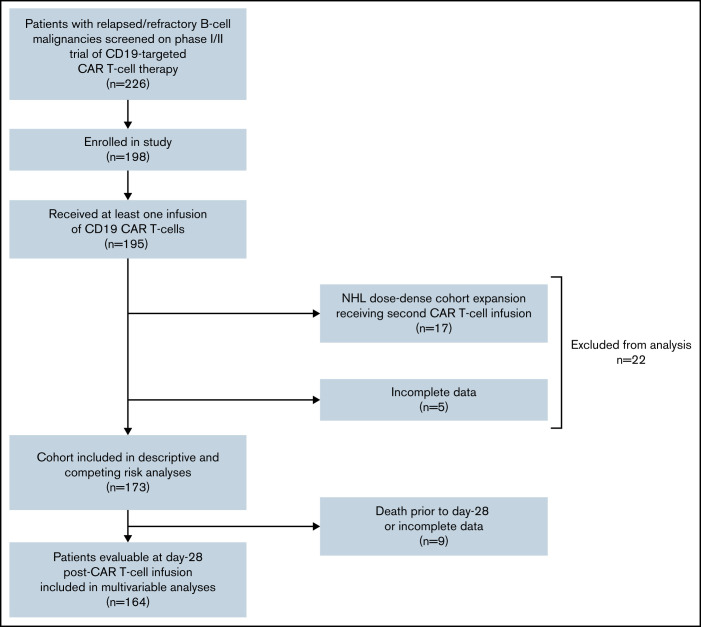
For this analysis, we included 173 of the 195 patients who received treatment after enrollment in the study (Figure 1). Five patients with missing or incomplete data were excluded, as were 17 patients with NHL treated in a pilot dose-dense cohort, who received a planned second CAR T-cell infusion without additional lymphodepleting therapy 15 days after the first infusion. The study was conducted according to the principles of the Declaration of Helsinki and with the approval of the Fred Hutchinson Cancer Research Center Institutional Review Board.
Figure 1.
Patient selection. Inclusion and exclusion criteria for analysis. Patients excluded from analysis at time of first competing event after CAR T-cell infusion, defined as relapse with marrow involvement, new cytotoxic therapy, second lymphodepletion or CAR T-cell infusion, death, or loss to follow-up.
Our primary end point for hematologic toxicity was absolute neutrophil count (ANC) and platelet count at day-28 after CAR T-cell infusion. As secondary end points, we assessed the cumulative incidence of hematopoietic recovery accounting for competing risks.
Evaluation of hematologic toxicity
Hematopoietic recovery.
Criteria for neutropenia, thrombocytopenia, and recovery of neutrophil and platelet counts were defined as per the established Center for International Blood and Marrow Transplant Research (CIBMTR)23 reporting guidelines for cellular therapy, with neutropenia, ANC ≤0.5 × 109/L; thrombocytopenia, platelet count ≤20 × 109/L; and neutrophil recovery, ANC >0.5 × 109/L, for 3 consecutive laboratory test results obtained on different days, irrespective of growth factor administration, and platelet recovery, platelet count >20 × 109/L for 3 consecutive results obtained on different days, in the absence of platelet transfusion for the preceding 7 days.
Grading of cytopenias.
Cytopenias were graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0.3, at a median of 14, 28, 60, 90, 120, and 180 days after CAR T-cell infusion (range, 13-17, 23-33, 55-65, 85-95, 110-130, and 160-200 days, respectively) in evaluable patients, with minimum ANC, hemoglobin level, or platelet count within each date range selected. To grade preinfusion cytopenia, the minimum result between the date of infusion and 7 days before infusion was selected.
Evaluation and grading of CRS and ICANS, serum biomarkers, cytokines, and additional clinical laboratory results
The severity of CRS was graded according to the 2014 Lee criteria.24 ICANS was graded according to the CTCAE 4.0.3 for neurologic adverse events, with the overall ICANS grade defined as the highest grade in each patient. Collection and analysis of serum biomarkers, cytokines, and additional laboratory parameters were performed as previously described.2,19 The following serum cytokines were evaluated in this study: transforming growth factor β1 (TGF-β); interferon-γ; interleukin 2 (IL-2), IL-5, IL-6, IL-7, IL-8, IL-10, IL-15, IL-18, IL-22, and IL-2Rα; and MCP-1, MIP-1β, Fas, IL-6R, soluble tumor necrosis factor receptor 1 (sTNFR1; p55), sTNFR1 (p75), TNFα, and TIM-3.
Statistical analysis
In evaluable patients, descriptive statistics excluded blood count data at time points after initiation of the subsequent antitumor therapy, a second CAR T-cell infusion, relapsed disease, or loss of the patient to follow-up.
Primary end point: day-28 ANC and platelet count.
For linear regression the primary end points were ANC and platelet count at day-28 after CAR T-cell infusion. With a window of ±7 days, 164 of the 173 patients were evaluable for this analysis (Figure 1). The following patient-, disease-, and treatment-related variables were considered for univariate and multivariable analyses: age, sex, disease type (ALL, CLL, or NHL), number of prior nontransplant treatments; prior autologous or allogeneic hematopoietic stem cell transplant (HSCT); CAR T-cell infusion dose level, CRS grade; prelymphodepletion (pre-LD) neutrophil, lymphocyte, and platelet counts; pre-LD D-dimer; prothrombin time; partial thromboplastin time; and ferritin, C-reactive protein, and fibrinogen levels.
A second analysis was performed to assess the contribution of CRS-related cytokines in which the CRS grade variable was replaced by each of the cytokines mentioned herein. For this analysis, we selected peak serum concentrations after CAR T-cell infusion, with the exception of TGF-β1, for which we used the trough serum concentration. This measure was determined by inspection of the serum concentration kinetics categorized by CRS grade after CAR T-cell infusion (supplemental Figure 1) and by applying a nonparametric smoother (locally weighted scatterplot smoothing) to the longitudinal data.
A univariate linear regression model was used to assess for each risk factor with neutrophil and platelet recovery. In the joint analysis, a novel debiased LASSO model was applied. First, regression coefficients were penalized by using the LASSO25 approach. Next, the penalized coefficient estimates were debiased to allow for statistical inference (confidence intervals [CIs] and null hypothesis testing). Multiple imputation using chained equations and predictive mean matching was used for selected variables that were missing for <25% of patients included in the analysis. We conducted univariate analysis of 3 variables (pre-LD C-reactive protein, fibrinogen, and D-dimer) with >25% missing values before and after imputation (number and proportion of patients with missing data are shown in supplemental Table 5). As none was statistically significant at the P = .05 level, these variables were removed from the covariate list. Regression beta coefficients are reported with 95% CIs.
Secondary end points: cumulative incidence of ANC and platelet recovery.
For our secondary end points, we chose a method of accounting for competing risks, because clinical events unrelated to CAR T-cells may preclude hematopoietic recovery after CD19 CAR T-cell therapy. An event was defined as neutrophil or platelet recovery by the CIBMTR criteria, as described in “Hematopoietic recovery,” whereas the following occurrences were considered to be competing events: death, new antitumor therapy, or disease relapse with marrow involvement in the absence of neutrophil or platelet recovery. As already noted, patients receiving a second CAR T-cell infusion as part of the dose-dense expansion cohort were excluded from the analysis. For patients included in the analysis who received more than 1 CAR T-cell infusion, second lymphodepletion (if administered) and second CAR T-cell infusion (if administered without second lymphodepletion) were also considered to be competing events. Patients who never met the CIBMTR criteria for neutropenia or thrombocytopenia were considered to have recovered at time 0. Median follow-up time was estimated by using the reverse Kaplan-Meier analysis.26 The cumulative incidences of neutrophil and platelet recovery were estimated using the Kalbfleisch and Prentice method,27 and univariate comparisons across categories were performed with Gray’s test.28,29
Data analysis was performed with R (version 3.6.3), RStudio (version 1.4.1106), and the following packages: cmprsk, ggplotly, ggpubr, gtsummary, hdi, mice, rms, scales, survival, survminer, and tidyverse.
Results
Patient characteristics
One hundred seventy-three patients with R/R B-cell malignancies (ALL, n = 62; CLL, n = 48; and NHL, n = 63) were included, with a median age of 55 years (range, 20-76). The patients were heavily pretreated with a median of 4 prior therapies (range, 1-11), and 61 (35%) underwent HSCT (autologous, 23 [13%]; allogeneic, 35 [20%]; or both autologous and allogeneic 3 [2%]). One hundred forty-six (85%) received a lymphodepletion regimen containing both cyclophosphamide and fludarabine at either high (80, 47%) or low (66, 39%) intensity, and 25 (15%) received an alternative regimen (supplemental Table 2). Median ANC and platelet counts before lymphodepletion were 2.41 × 109/L (range, 0-23) and 123 × 109/L (range, 7-448), respectively. Median pre-LD abnormal bone marrow B-cell percentage was 8% (range, 0% to 98%). Patients received CAR T-cells infused at 1 of 3 dose levels. Patient, disease, and treatment characteristics are summarized in Table 1.
Table 1.
Patient and treatment characteristics by disease cohort
| Disease cohort (n, %) | ALL (n = 62; 36%) |
CLL (n = 48; 28%) |
NHL (n = 63; 36%) |
Total (N = 173) |
|---|---|---|---|---|
| Age (y), median (IQR) [range] | 40 (28, 54) [20-76] |
61 (55, 66) [40-73] |
58 (52, 64) [28-71] |
55 (43, 64) [20-76] |
|
Sex, n (%) Female Male |
26 (42) 36 (58) |
15 (31) 33 (69) |
17 (27) 46 (73) |
58 (34) 115 (66) |
|
Race, n (%) White Nonwhite Unknown |
50 (80.6) 12 (19.4) 0 (0) |
43 (90) 4 (8.3) 1 (2.1) |
58 (92) 5 (7.9) 0 (0) |
151 (87) 21 (12) 1 (0.6) |
| Prior therapies, median n (IQR) [range] |
3 (2, 4) [1-11] |
5 (4, 7) [1-10] |
4 (4, 6) [1-11] |
4 (3, 6) [1-11] |
|
Prior HSCT, n (%) Autologous Allogeneic Both None |
0 (0) 24 (39) 0 (0) 38 (61) |
1 (2) 7 (15) 0 (0) 40 (83) |
22 (35) 4 (6.3) 3 (4.8) 34 (54) |
23 (13) 35 (20) 3 (1.7) 112 (65) |
| Pre-LD marrow abnormal B-cells (%), median (IQR) [range] | 22.2 (1, 71) [0-98] |
52 (20, 74) [0-96] |
0 (0, 0) [0-92] |
8 (0, 57) [0-98] |
| Pre-LD ANCs (×109/L), median (IQR) [range] |
1.86 (0.88, 3.06) [0-7.62] |
2.13 (0.94, 4.30) [0-13.65] |
3.24 (1.98, 5.50) [0.23-23.17] |
2.41 (1.25, 4.23) [0-23.2] |
| Pre-LD ALCs (×109/L), median (IQR) [range] |
0.7 (0.4, 1.3) [0-5.1] |
1.9 (1.0, 7.6) [0.2-58.9] |
0.6 (0.4, 1.1) [0-8.8] |
0.9 (0.5, 1.7) [0-58.9] |
| Pre-LD hemoglobin (g/dL), median (IQR) [range] |
10.6 (9.8, 11.7) [7.3-14.8] |
10.6 (9.8, 12.35) [7.4-16] |
11.1 (9.8, 12.7) [7.2-15] |
10.8 (9.8, 12.2) [7.2-16] |
| Pre-LD platelets (×109/L), median (IQR) [range] |
110 (48, 200) [9-339] |
114 (86, 146) [7-434] |
143 (80, 214) [9-448] |
123 (64, 196) [7-448] |
|
Lymphodepletion, n (%) High-intensity CyFlu Low-intensity CyFlu Non-CyFlu |
31 (50) 19 (31) 12 (19) |
15 (31) 29 (60) 4 (8.3) |
34 (54) 18 (29) 11 (17) |
80 (46) 66 (38) 27 (16) |
|
CAR T-cell dose, n (%) DL1 DL2 DL3 |
38 (61) 22 (35) 2 (3.2) |
5 (10) 42 (88) 1 (2.1) |
4 (6) 50 (79) 9 (14) |
47 (27) 114 (66) 12 (6.9) |
|
CRS grade, n (%) 0 1 2 3-5 |
14 (23) 12 (19) 23 (37) 13 (21) |
8 (17) 15 (31) 18 (38) 7 (15) |
30 (48) 13 (21) 14 (22) 6 (9.5) |
52 (30) 40 (23) 55 (32) 26 (15) |
|
Neurotoxicity grade, n (%) 0-1 2-3 4-5 |
39 (63) 19 (31) 4 (6.5) |
32 (67) 15 (31) 1 (2.1) |
50 (79) 11 (17) 2 (3.2) |
121 (70) 45 (26.0) 7 (4.0) |
High-intensity CyFlu, cyclophosphamide (Cy) 60 mg/kg or >1500 mg/m2 with fludarabine (Flu) 75-125 mg/m2; low-intensity CyFlu, Cy 30 mg/kg or ≤1500 mg/m2 with Flu 75-90 mg/m2; Non-CyFlu, any conditioning regimen other than as noted above including single agent Cy or Flu. CAR T-cell dose level (DL): DL1 = 2 × 105 cells/kg, DL2 = 2 × 106 cells/kg, DL3 = 2 × 107 cells/kg. CRS grade as defined by Lee criteria.24 Neurotoxicity grade as defined by CTCAE 4.0.3. ALC, absolute lymphocyte count; IQR, interquartile range.
Hematologic toxicity after CD19 CAR T-cell therapy
Severity of hematologic toxicities.
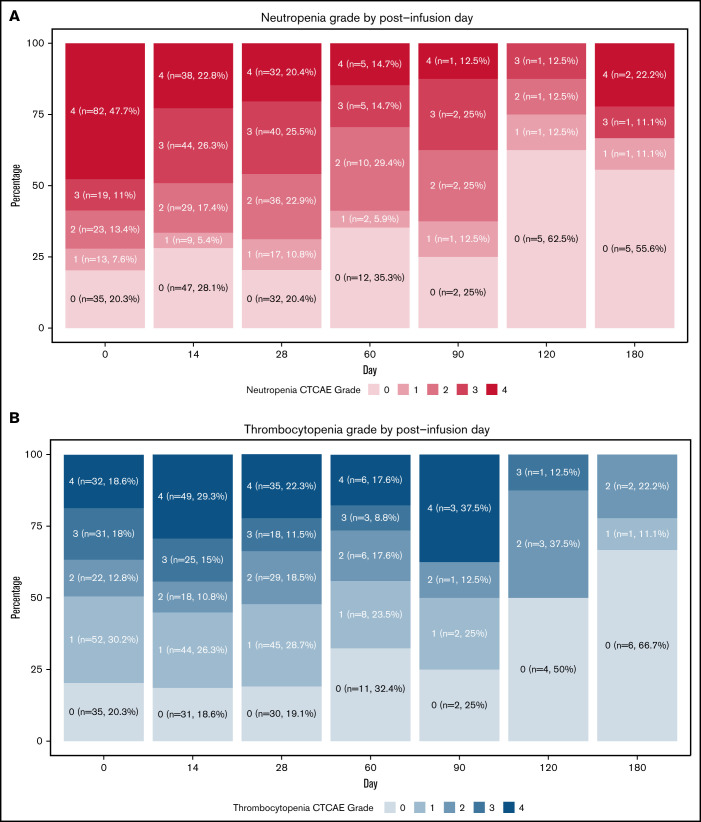
A significant proportion of patients presented with severe cytopenia after CAR T-cell therapy. We observed grade ≥3 neutropenia at days 0, 14, and 28 in 58.7% (95% CI, 51.0-66.1), 49.1% (95% CI, 41.3-56.9), and 45.9% (95% CI, 37.9-54.0), respectively (Figure 2A). We observed grade ≥3 thrombocytopenia at days 0, 14, and 28 in 36.6% (95% CI, 29.4-44.3), 44.3% (95% CI, 36.6-52.2), and 33.8% (95% CI, 26.4-41.7) of patients, respectively (Figure 2B). Grade 3 anemia was noted at days 0, 14, and 28 in 14.5% (95% CI, 9.6-20.7), 16.2% (95% CI, 10.9-22.6), and 14.6% (95% CI, 9.5-21.2) of patients, respectively (Figure 2C). The observed frequencies of cytopenia up to 180 days after CAR T-cell infusion are shown in Figure 2. As faster hematopoietic recovery could reflect response to treatment, we assessed the relationship between day-28 ANC and platelet count and response at first assessment in evaluable patients, typically performed at day-28 after CAR T-cell infusion. Patients were categorized as responders (complete remission, complete remission with minimal residual disease, or partial response) or nonresponders (stable disease or progression of disease). No statistically significant difference (Wilcoxon unpaired test) was noted for either ANC or platelet count (supplemental Figure 2A,C). When stratified by disease cohort, day-28 ANC was lower, with statistical significance in nonresponders within the ALL cohort (P = .037); however, no significant differences were noted in day-28 platelet count in ALL or for either measure in CLL and NHL cohorts (supplemental Figure 2B,D).
Figure 2.
Severity of hematologic toxicities. Percentage of patients with neutropenia (A), thrombocytopenia (B), and anemia (C) by post-CAR T-cell infusion day, stratified by CTCAE grade. Because of the variability in collection dates, for day = n, the minimum cell count falling within an arbitrary range of n was selected for each patient (ie, day 0 = days −7 and 0, day 14 = days 12-16, day-28 = days 23-33, day 60 = days 55-65, day 90 = days 85-95, day 120 = days 110-130, and day 180 = days 160-200). Patients were no longer included in this analysis pending receipt of a subsequent line of therapy, second CAR T-cell infusion, or withdrawal from the study.
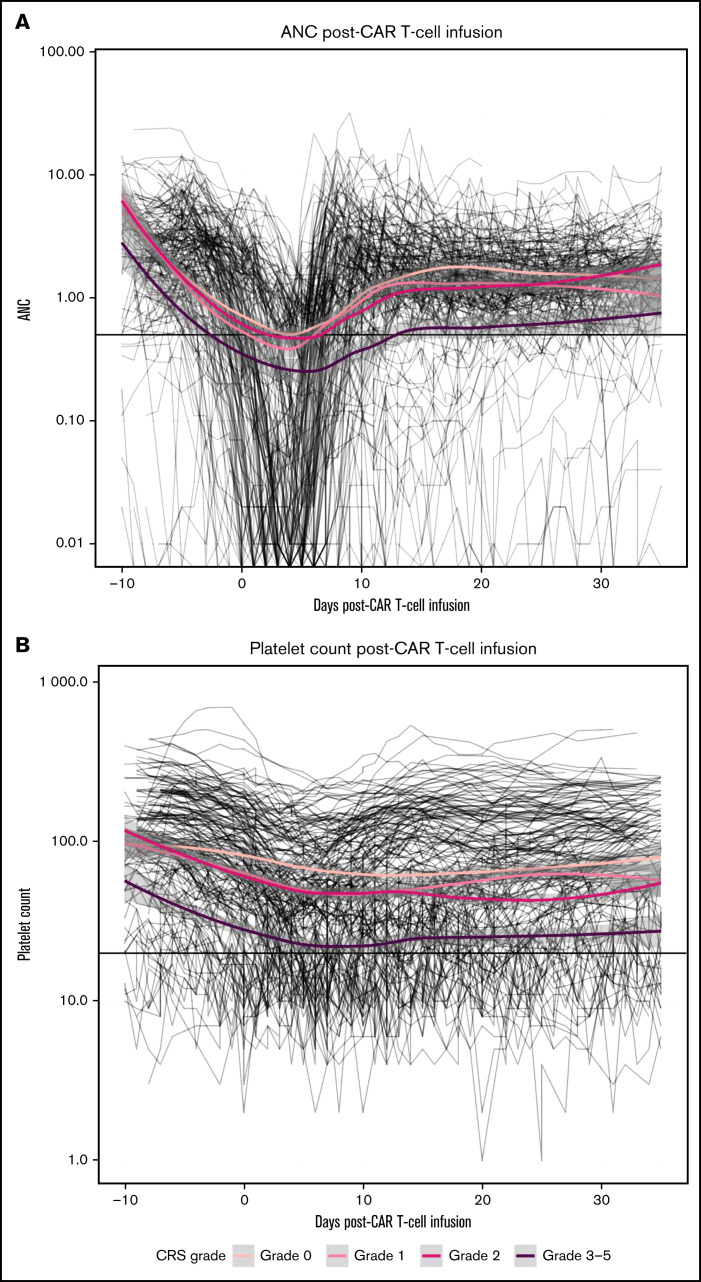
ANC and platelet kinetics after CAR T-cell infusion.
To visualize trends in ANC and platelet counts and to assess recovery at our primary end point of day-28 after CAR T-cell infusion, we applied a nonparametric smoother to longitudinal data (Figure 3) grouping subjects by CRS grade. Mean ANC (×109/L) at day-28 was 1.54, 1.21, 1.42, and 0.65 and mean platelet count (×109/L) was 70.8, 63.1, 44.7, and 26.1 for CRS grades 0, 1, 2, and 3-5 respectively. Mean time to ANC recovery by CRS grade was 4.2, 5.9, 6.5, and 12.8 days for CRS grades 0, 1, 2, and 3-5, respectively. ANC and platelet counts (median and interquartile range) at day-28 after CAR T-cell infusion in evaluable patients overall and by baseline characteristics are shown in Table 2, with continuous variables stratified by quartile.
Figure 3.
Kinetics of hematopoietic recovery. Longitudinal ANC (A) and platelet counts (log scale) (B) are depicted in spaghetti plots, with the application of a nonparametric smoother to subjects grouped by CRS grade.
Table 2.
ANC and platelet count at day-28 after CAR T-cell infusion
| Variable | ANCs (×109/L) median (IQR) |
Platelets (×109/L) median (IQR) |
|---|---|---|
|
Disease cohort Total (n = 164) ALL (n = 59) CLL (n = 46) NHL (n = 59) |
1.52 (0.87, 2.46) 1.27 (0.62, 2.02) 1.61 (0.88, 2.82) 1.64 (1.06, 2.51) |
82 (46, 149) 77 (32, 146) 84 (43, 121) 88 (60, 179) |
|
Sex Female (n = 52) Male (n = 112) |
1.50 (0.92, 2.20) 1.55 (0.84, 2.54) |
72 (42, 130) 91 (51, 153) |
|
Race, n (%) White (n = 143) Nonwhite (n = 20) Unknown (n = 1) |
1.53 (0.88, 2.41) 1.35 (0.84, 2.61) 3.60 (3.60, 3.60) |
79 (44, 150) 112 (58, 154) 140 (140, 140) |
|
Number of prior therapies <Q1 (1-2) Q1-Q2 (3-4) Q2-Q3 (5-6) >Q3 (7-11) |
1.71 (0.95, 2.23) 1.31 (1.07, 2.50) 1.41 (0.78, 3.10) 1.60 (0.54, 2.44) |
126 (51, 171) 78 (43, 162) 66 (46, 116) 78 (42, 114) |
|
Prior HSCT Autologous (n = 22) Allogeneic (n = 34) Both (n = 3) None (n = 105) |
1.42 (1.02, 2.34) 1.36 (0.49, 1.74) 3.91 (3.56, 4.96) 1.58 (0.91, 2.53) |
70 (58, 149) 76 (28, 112) 88 (80, 152) 94 (50, 155) |
|
Pre-LD marrow abnormal B-cells (%) <Q1 (0-0.006) Q1-Q2 (0.006-7.99) Q2-Q3 (8.00-60.0) >Q3 (60.1-98.5) |
1.61 (1.02, 2.58) 1.72 (1.22, 2.55) 1.68 (1.24, 2.65) 0.80 (0.26, 1.93) |
91 (61, 178) 104 (56, 149) 78 (49, 147) 55 (27, 115) |
|
Pre-LD ANC (×109/L) <Q1 (0-1.35) Q1-Q2 (1.36-2.43) Q2-Q3 (2.44-4.34) >Q3 (4.35-23.17) |
1.00 (0.43, 1.90) 1.47 (1.14, 2.13) 1.74 (1.10, 2.84) 2.14 (1.17, 3.20) |
50 (24, 90) 101 (60, 147) 128 (62, 156) 86 (49, 201) |
|
Pre-LD ALC (×109/L) <Q1 (0.00-0.51) Q1-Q2 (0.52-0.89) Q2-Q3 (0.90-1.94) >Q3 (1.95-58.92) |
1.58 (0.79, 2.00) 1.36 (0.93, 2.45) 1.77 (1.24, 2.48) 1.35 (0.72, 2.31) |
61 (42, 113) 116 (45, 174) 83 (60, 147) 100 (41, 133) |
|
Pre-LD hemoglobin (g/dL) <Q1 (7.2-9.8) Q1-Q2 (9.9-10.8) Q2-Q3 (10.9-12.1) >Q3 (12.2-16.0) |
1.37 (0.58, 2.51) 1.69 (0.56, 2.22) 1.52 (1.03, 2.20) 1.70 (1.24, 2.71) |
64 (32, 107) 74 (37, 143) 83 (52, 142) 137 (70, 188) |
|
Pre-LD platelet (×109/L) <Q1 (7-66) Q1-Q2 (67-126) Q2-Q3 (127-197) >Q3 (198-448) |
0.66 (0.24, 1.41) 1.53 (1.10, 2.84) 1.68 (1.17, 2.23) 2.20 (1.24, 3.32) |
33 (20, 64) 79 (55, 115) 125 (62, 164) 174 (76, 215) |
|
Lymphodepletion High-intensity CyFlu (n = 77) Low-intensity CyFlu (n = 61) Non-CyFlu (n = 26) |
1.58 (1.07, 2.53) 1.53 (0.82, 2.39) 1.23 (0.88, 2.09) |
107 (55, 161) 62 (31, 113) 104 (60, 196) |
|
CAR T-cell dose DL1 (n = 46) DL2 (n = 108) DL3 (n = 10) |
1.21 (0.46, 2.10) 1.63 (1.02, 2.70) 1.53 (1.03, 2.15) |
86 (36, 155) 80 (54, 138) 144 (61, 217) |
|
CRS grade 0 (n = 50) 1 (n = 39) 2 (n = 53) 3-5 (n = 22) |
1.62 (1.01, 2.31) 1.97 (1.12, 3.11) 1.27 (0.81, 2.14) 1.44 (0.42, 2.22) |
89 (57, 172) 105 (58, 144) 84 (32, 147) 50 (26, 98) |
|
Neurotoxicity grade, n (%) 0-1 (n = 117) 2-3 (n = 44) 4-5 (n = 3) |
1.64 (0.99, 2.55) 1.28 (0.76, 2.04) 1.68 (1.17, 3.35) |
82 (50, 155) 85 (48, 130) 29 (28, 47) |
High-intensity CyFlu, cyclophosphamide (Cy) 60 mg/kg or > 1500 mg/m2 with fludarabine (Flu) 75-125 mg/m2; low-intensity CyFlu, Cy 30 mg/kg or ≤1500 mg/m2 with Flu 75-90 mg/m2; Non-CyFlu, any conditioning regimen other than as noted above including single agent Cy or Flu. CAR T-cell dose level (DL): DL1 = 2 × 105 cells/kg, DL2 = 2 × 106 cells/kg, DL3 = 2 × 107 cells/kg. CRS grade as defined by Lee criteria.24 Neurotoxicity grade as defined by CTCAE 4.0.3. ALC, absolute lymphocyte count; IQR, interquartile range; LD, lymphodepletion; Q1, 25% quantile (1st quartile); Q2, 50% quantile (median); Q3, 75% quantile (3rd quartile).
Cumulative incidence of hematopoietic recovery.
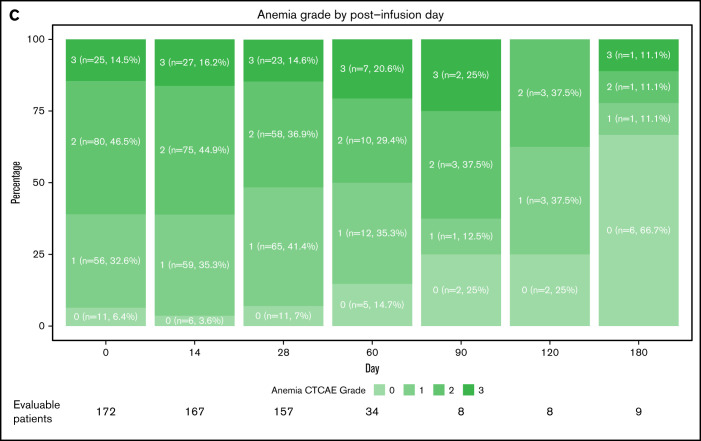
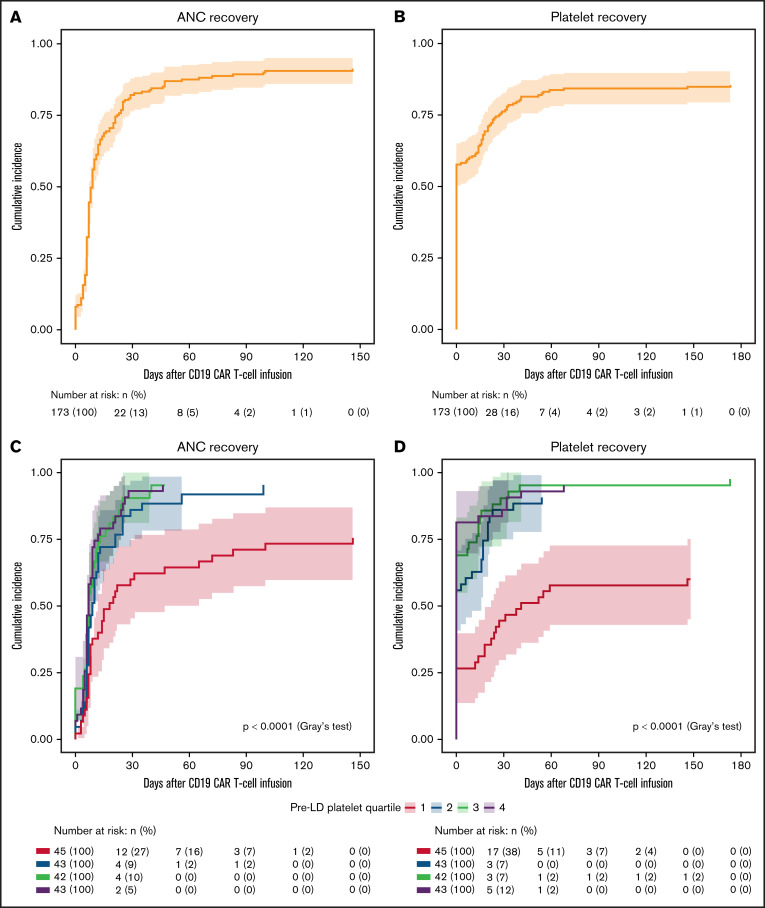
After a median follow-up time of 40.8 months (ALL, 45.7 months; CLL, 26.6 months; NHL, 47.3 months), the proportion of evaluable patients demonstrating ANC and platelet recovery according to the CIBMTR criteria after CD19 CAR T-cell therapy were 91% (ALL, 85%; CLL, 95%; NHL, 98%) and 86% (ALL, 82%; CLL, 83%; NHL, 90%), respectively. Median time to ANC recovery was 8 days (range, 0-146) and the cumulative incidence of ANC recovery at days 28, 60, and 90 were 81% (95% CI, 75-87), 88% (95% CI, 83-93), and 89% (95% CI, 85-94), respectively (Figure 4A). Median time to platelet recovery was 0 days (range, 0-173) and the cumulative incidence of platelet recovery on the day of CAR T-cell infusion was 58% (95% CI, 50-65); rising to 76% (95% CI, 69-82), 84% (95% CI, 78-89), and 84% (95% CI, 79-90) at days 28, 60, and 90, respectively (Figure 4B). When patients who never met the criteria for neutropenia or thrombocytopenia (supplemental Figure 3) were excluded, the median time to ANC recovery was 8.75 days (range, 1-146) and the median time to platelet recovery was 36.5 days (range, 3-173). The cumulative incidence of hematopoietic recovery stratified by disease type is shown in supplemental Figure 4.
Figure 4.
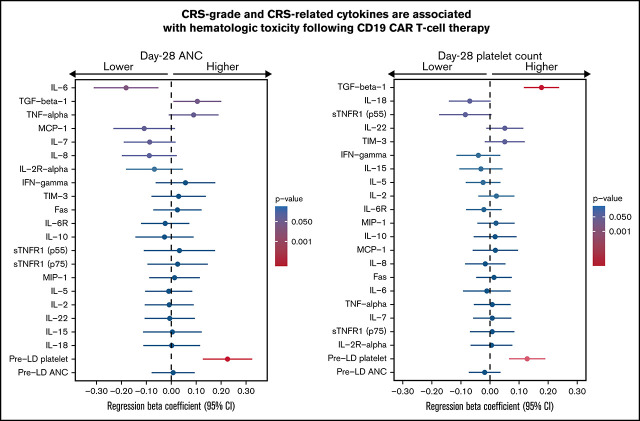
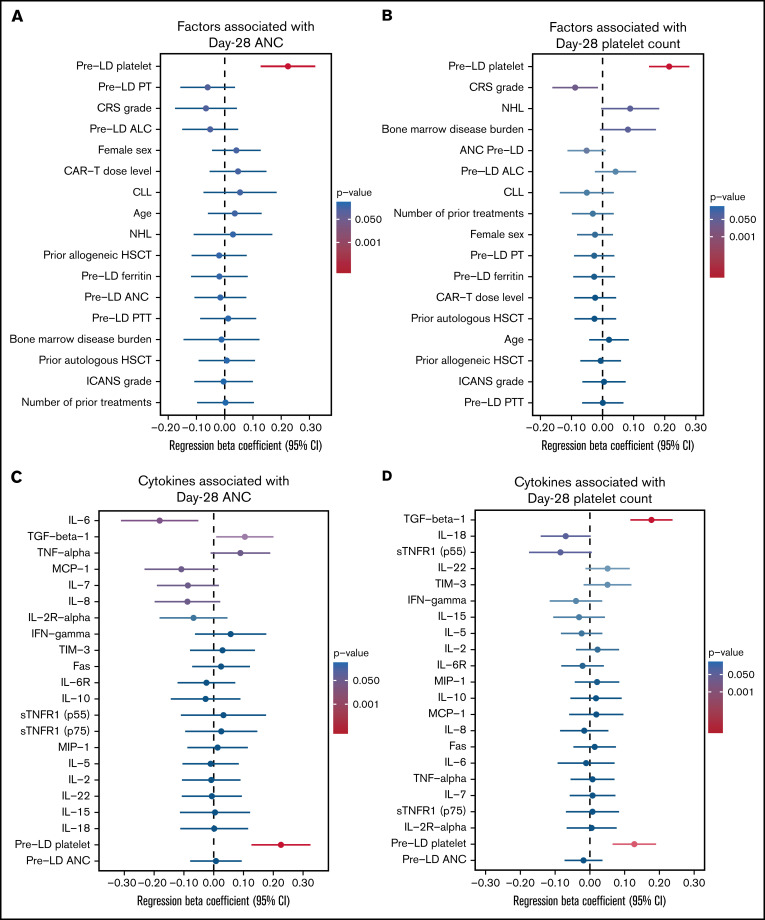
Multivariable analysis of factors associated with day-28 ANC and platelet counts. Forest plots of regression coefficients for day-28 neutrophil (A,C) or platelet (B,D) counts determined by high-dimensional inference for selected patient, disease, and treatment characteristics (A-B) or serum cytokine concentrations (C-D). Regression coefficient and associated 95% CI, denoted by circles and lines from a linear regression model, respectively. P-value of regression coefficient denoted by color gradient. CRS and ICANS variables are stratified by grade. Disease cohorts (CLL and NHL) and sex (female) are compared against a reference variable, ALL and male, respectively. All other variables are modeled as continuous variables. ALC, absolute lymphocyte count; IFN, interferon; MCP, monocyte chemoattractant protein; MIP, macrophage inflammatory protein; PT, prothrombin time; PTT, partial thromboplastin time, TIM, T-cell immunoglobulin and mucin domain-containing protein; TNF, tumor necrosis factor; sTNFR, soluble TNF-receptor.
Multivariable analyses of day-28 ANC and platelet count
We applied debiased LASSO in a high-dimension linear regression model to identify independent predictors of ANC (Figure 5A) and platelet (Figure 5B) recovery. We considered patient, disease, and treatment-related predictors in our models as described in “Methods.” Univariate analyses are shown in supplemental Table 2A-B).
Figure 5.
Cumulative incidence of hematopoietic recovery. Cumulative incidence of neutrophil (A,C) and platelet (B,D) recovery, as defined by CIBMTR criteria. Cumulative incidence estimated by the Kalbfleisch and Prentice method with univariate comparisons across categories according to Gray’s test and stratified by entire cohort (A-B) or by pre-LD platelet count (C-D, grouped by quartiles). Shaded areas represent 95% CIs.
A higher CRS grade was associated with a lower day-28 platelet count (β, −0.09 per CRS grade; 95% CI, − 0.16 to −0.014; P = .019) and suggested a similar trend for ANC, but we could not reject the null hypothesis with a similar but nonsignificant trend for ANC (β, −0.07; 95% CI, −0.17 to –0.04; P = .24). In contrast, higher pre-LD platelet count was associated with higher day-28 ANC (β, 0.22 per log10 platelet × 109/L; 95% CI, 0.127-0.32; P < .00001) and higher day-28 platelet count (β, 0.21 per log10 platelet × 109/L; 95% CI, 0.150-0.279). Confirming our observations, the univariate cumulative incidence of ANC recovery at day-28 by pre-LD platelet count was 58% (95% CI, 43-72), 84% (95% CI, 72-95), 90% (95% CI, 81-100), and 93% (95% CI, 85-100) for pre-LD platelet counts of 7-66, 67-124, 125-197, and 198-448 × 109/L, respectively (Figure 4C) and the univariate CI of platelet recovery at day-28 by pre-LD platelet count was 44% (95% CI, 30-59), 86% (95% CI, 75-97), 90% (95% CI, 81-100), and 84% (95% CI, 72-95) for the same quartiles, respectively (Figure 4D).
We could not confirm associations between several patient, disease, and treatment factors and hematopoietic recovery that were suggested in other studies. Notably, these included pre-LD bone marrow disease burden (ANC: β, −0.01; 95% CI, −0.145 to 0.123; P = .87; platelet: β, 0.08; 95% CI, −0.009 to 0.17; P = .08) and number of prior treatment regimens (ANC: β, 0.00 per additional treatment; 95% CI, −0.10 to 0.10; P = .96; platelet: β, −0.03; 95% CI, −0.099 to 0.036; P = .36). Similarly, the association between CAR T-cell dose level and hematopoietic recovery was undetermined (ANC: β, 0.05 per dose level; 95% CI, −0.053 to 0.148, P = .36; platelet: β, −0.02, 95% CI, −0.09 to 0.04; P = .49).
Cytokine levels and day-28 ANC and platelet count
Because our findings suggested that the CRS grade is a key factor in hematopoietic recovery, we included a panel of selected CRS-related cytokines in our high-dimensional linear regression models, in addition to cytokines known to have a role in hematopoiesis (Figures 5C-D), and retaining key baseline variables, preinfusion ANC, and platelet counts.
Discussion
CAR T-cell therapy has been associated with significant cytopenia responsible for prolonged transfusion requirements and with increased risk of infection and bleeding. Because this complication remains poorly characterized, we studied the kinetics of hematopoietic recovery and the factors associated with hematologic toxicity after CD19 CAR T-cell therapy in a large cohort of 173 patients.
Importantly, the day-28 cumulative incidences of neutrophil and platelet recovery in all patients were 81% and 89%, respectively, indicating that a significant proportion of patients had impaired hematopoiesis after CD19 CAR T-cell therapy. Using the debiased LASSO for high-dimensional linear regression modeling, we identified key factors independently associated with hematopoietic recovery. Our approach achieves robust variable selection in multivariable analysis, as it can account for large numbers of covariates and highly correlated covariates. Importantly, it provides statistical inference, with robust estimates for coefficients, and allows for the computation of confidence intervals for all coefficients, which cannot be achieved by other approaches, such as stepwise regression or linear regression using nondebiased LASSO.30 The severity of CRS was independently predictive of day-28 platelet count and the pre-LD platelet count was an independent predictor of both day-28 ANC and platelet count, although prior work from our group also noted an association between baseline platelet count and severity of subsequent CRS.19 The identification of pre-LD platelet count suggests that poor bone marrow reserve or treatment-related bone marrow injuries may be key factors associated with impaired hematopoietic recovery after CD19 CAR T-cell therapy. Results in other studies have suggested that the intensity of the lymphodepletion regimen31 and prior treatment regimens affect hematopoietic recovery after CAR T-cell therapy. Our study did not determine an association with either the number of prior treatment regimens or the status of prior autologous or allogeneic transplant and the day-28 ANC or platelet count. Because the selection of lymphodepletion regimen intensity was influenced by patients’ pretreatment baseline counts and the disease type, we did not include this variable in our analysis.
Because our multivariable modeling suggested a strong detrimental effect of CRS severity on hematopoietic recovery, we sought to investigate the impact of 20 serum cytokines associated with CRS on ANC and platelet recovery. Higher peak serum concentration of IL-6, known to be strongly associated with CRS severity,19 was independently associated with impaired hematopoietic recovery in our multivariable analysis, whereas a higher peak concentration of TGF-β was associated with improved recovery.
In our study, we noted an association between higher peak IL-6 serum concentration and slower hematopoietic recovery. IL-6 is a cytokine known to have pleiotropic effects on the hematologic system, including megakaryocytic maturation and platelet release from the bone marrow, myeloid differentiation during neutropenia, T-cell differentiation, and stimulation of antibody production from B-cells.32-35 Further studies are needed to clarify the role of IL-6 in hematologic toxicity after CAR T-cell therapy. We hypothesize that high IL-6 serum concentrations reflect a homeostatic increase that stimulates hematopoiesis in response to cytopenia, although we acknowledge that IL-6 serum concentrations in the bone marrow were not measured in our study. Furthermore, the effects of a therapeutic IL-6R blockade with tocilizumab on hematopoietic precursors and its contribution to hematologic toxicities of CAR T-cells remain unknown. We did not identify an independent association between the use of tocilizumab and hematopoietic recovery (supplemental Table 4).
Higher serum concentrations of TGF-β were associated with improved hematopoietic recovery. TGF-β is a pleiotropic cytokine expressed in a variety of tissues and stored in high concentrations within the α-granules of platelets.36 TGF-β has complex effects on the hematopoietic system, on both mature cells37 and stem cell progenitors.38 Although it is known to mediate cell cycle arrest in CD34+ cells, more recent evidence suggest differential response to TGF-β signaling by different subsets of HSCs, with proliferation of myeloid-producing HSCs and inhibition of lymphoid-producing HSCs,39 and our findings may reflect this activity. Alternatively, lower TGF-β serum concentrations may be reflective of decreased platelet production or CRS-related platelet consumption; we and other groups have shown that severe CRS is associated with consumptive coagulopathy.19,40,41 Maintenance of higher TGF-β serum concentrations may also reflect its homeostatic immunomodulatory effects during CAR T-cell activation.37
Although further studies are needed to characterize the biological effects of CRS-related cytokines under these conditions on hematopoiesis, our findings suggest interventions that may have immediate clinical impact. In our cohort, patients with pre-LD platelet counts falling into the lowest quartile exhibit prolonged hematopoietic recovery. This result suggests that risk stratification taking pre-LD platelet count into consideration when enrolling patients in CAR T-cell clinical trials, selecting lymphodepletion regimen intensity, number of CAR T-cell infusions, or CAR T-cell dose may be beneficial. The identification of CRS and CRS-related cytokines as predictors of delayed hematopoietic recovery in our study suggests that both early identification, through frequent monitoring of cytokines and inflammatory markers, and early interventions, to prevent high-grade CRS, may be beneficial to mitigate hematopoietic toxicity.
In summary, we characterized the kinetics and pattern of hematopoietic recovery in 173 patients treated with CD19 CAR T-cell therapy for R/R B-cell malignancies. Pre-LD blood counts, CRS severity and CRS-related cytokines independently affected hematopoietic recovery after CD19 CAR T-cell therapy. Our study suggests that both patient selection and advancing CRS management may improve hematopoietic recovery after CD19 CAR T-cell therapy.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank the Fred Hutchinson Cancer Research Center Cell Processing Facility, the Seattle Cancer Care Alliance Cell Therapy Laboratory, and the staff of the Program in Immunology and Seattle Cancer Care Alliance Immunotherapy Clinic for assistance.
This work was supported by National Institutes of Health, National Cancer Institute grants R01CA136551, R35CA197734, and P30CA015704; NIH National Institute of Diabetes and Digestive and Kidney Diseases grant P30DK56465; the Life Science Discovery Fund; the Bezos Family Foundation; The Anderson Family; the Innovation in Cancer Informatics (ICI) Fund; and Juno Therapeutics, a Bristol-Myers Squibb company. The NIH National Heart, Lung, and Blood Institute funded the National Gene Vector Biorepository at Indiana University (Contract 75N92019D00018), K.R.J. is supported by University of Washington, Division of Hematology Training Grant NIH NIHLB T32HL007093. J.G. acknowledges the Cancer Center Support Grant Clinical Scholar award (NCI P30CA015704).
Authorship
Contribution: K.R.J., M.B., and J.G. conceived of and designed the study; K.R.J., J.G., J.V., and Q.V.W. collected and assembled the data; K.R.J., M.B., J.G., J.V., and Q.V.W. analyzed and interpreted the data; and all authors participated in writing and approving the manuscript and are accountable for all aspects of the work.
Conflict-of-interest disclosure: A.V.H. received honoraria from Bristol Myers Squibb and Novartis and research support from Juno Therapeutics, a Bristol Myers Squibb company. D.G.M. received research funding from Kite Pharma, Juno Therapeutics, a Celgene company, and Celgene and honoraria for participation on advisory boards for Kite Pharma, Gilead, Genentech, Novartis, and Eureka. C.J.T. receives research funding from Juno Therapeutics, Nektar Therapeutics, Minerva, TCR2, and AstraZeneca; serves on scientific advisory boards and has options in Precision Biosciences, Eureka Therapeutics, Caribou Biosciences, Myeloid Therapeutics, and ArsenalBio; serves on scientific advisory boards for T-CURX and Century Therapeutics; has served on advisory boards for Nektar Therapeutics, Allogene, Kite/Gilead, Novartis, Humanigen, PACT Pharma, Amgen, and Astra Zeneca; and has patents licensed to Juno Therapeutics. J.G. has received honoraria from Larvol, Eusapharma, JMP, and Multerra Bio; has received research support from Juno Therapeutics, a Bristol Myers Squibb company, and Sobi; and has served on an advisory board for JNJ/Legend Biotech. The remaining authors declare no competing financial interests.
Correspondence: Jordan Gauthier, Clinical Research Division, Fred Hutchinson Cancer Research Center, 1100 Fairview Ave N, Seattle, WA 98109; e-mail: jgauthier@fredhutch.org.
References
- 1.Turtle CJ, Hanafi LA, Berger C, et al. CD19 CAR-T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J Clin Invest. 2016;126(6):2123-2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turtle CJ, Hay KA, Hanafi LA, et al. Durable Molecular Remissions in Chronic Lymphocytic Leukemia Treated With CD19-Specific Chimeric Antigen Receptor-Modified T Cells After Failure of Ibrutinib. J Clin Oncol. 2017;35(26):3010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porter DL, Hwang WT, Frey NV, et al. Chimeric antigen receptor T cells persist and induce sustained remissions in relapsed refractory chronic lymphocytic leukemia. Sci Transl Med. 2015;7(303):303ra139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang M, Munoz J, Goy A, et al. KTE-X19 CAR T-Cell Therapy in Relapsed or Refractory Mantle-Cell Lymphoma. N Engl J Med. 2020;382(14):1331-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Locke FL, Ghobadi A, Jacobson CA, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20(1):31-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N Engl J Med. 2017;377(26):2531-2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schuster SJ, Bishop MR, Tam CS, et al. ; JULIET Investigators . Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med. 2019;380(1):45-56. [DOI] [PubMed] [Google Scholar]
- 8.Turtle CJ, Hanafi LA, Berger C, et al. Immunotherapy of non-Hodgkin’s lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells. Sci Transl Med. 2016;8(355):355ra116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839-852. [DOI] [PubMed] [Google Scholar]
- 10.Hirayama AV, Gauthier J, Hay KA, et al. High rate of durable complete remission in follicular lymphoma after CD19 CAR-T cell immunotherapy. Blood. 2019;134(7):636-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cordeiro A, Bezerra ED, Hirayama AV, et al. Late Events after Treatment with CD19-Targeted Chimeric Antigen Receptor Modified T Cells. Biol Blood Marrow Transplant. 2020;26(1):26-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirayama AV, Turtle CJ. Toxicities of CD19 CAR-T cell immunotherapy. Am J Hematol. 2019;94(S1):S42-S49. [DOI] [PubMed] [Google Scholar]
- 13.Hill JA, Li D, Hay KA, et al. Infectious complications of CD19-targeted chimeric antigen receptor-modified T-cell immunotherapy. Blood. 2018; 131(1):121-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Logue JM, Zucchetti E, Bachmeier CA, et al. Immune reconstitution and associated infections following axicabtagene ciloleucel in relapsed or refractory large B-cell lymphoma. Haematologica. 2021;106(4)978-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brudno JN, Maric I, Hartman SD, et al. T Cells Genetically Modified to Express an Anti-B-Cell Maturation Antigen Chimeric Antigen Receptor Cause Remissions of Poor-Prognosis Relapsed Multiple Myeloma. J Clin Oncol. 2018;36(22):2267-2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shalabi H, Shah NN, Fry TJ, Yates B, Delbrook C. Chimeric antigen receptor induced cytopenia differs from chemotherapy induced myelosuppression [abstract]. Blood. 2017;130(suppl 1). Abstract 5048. [Google Scholar]
- 17.Maude SL, Laetsch TW, Buechner J, et al. Tisagenlecleucel in Children and Young Adults with B-Cell Lymphoblastic Leukemia. N Engl J Med. 2018;378(5):439-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wudhikarn K, Palomba ML, Pennisi M, et al. Infection during the first year in patients treated with CD19 CAR T cells for diffuse large B cell lymphoma. Blood Cancer J. 2020;10(8):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hay KA, Hanafi LA, Li D, et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor-modified T-cell therapy. Blood. 2017;130(21):2295-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fried S, Avigdor A, Bielorai B, et al. Early and late hematologic toxicity following CD19 CAR-T cells. Bone Marrow Transplant. 2019;54(10):1643-1650. [DOI] [PubMed] [Google Scholar]
- 21.Nahas GR, Komanduri KV, Pereira D, et al. Incidence and risk factors associated with a syndrome of persistent cytopenias after CAR-T cell therapy (PCTT). Leuk Lymphoma. 2020;61(4):940-943. [DOI] [PubMed] [Google Scholar]
- 22.Jain T, Knezevic A, Pennisi M, et al. Hematopoietic recovery in patients receiving chimeric antigen receptor T-cell therapy for hematologic malignancies. Blood Adv. 2020;4(15):3776-3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Center for International Blood & Marrow Transplant Research. Cellular Therapy Manuals: Peripheral Blood Count Recovery. Milwaukee, WI: CIBMTR; Last modified 22 January 2021. Available at: https://www.cibmtr.org/manuals/fim/1/en/topic/4100q17-20/. [Google Scholar]
- 24.Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome [published correction appears in Blood. 2015;126(8):1048]. Blood. 2014;124(2):188-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tibshirani R. Regression Shrinkage and Selection via the Lasso. J R Stat Soc B. 1996;58(1):267-288. [Google Scholar]
- 26.Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17(4):343-346. [DOI] [PubMed] [Google Scholar]
- 27.Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. New York: John Wiley & Sons, Inc.; 1980. [Google Scholar]
- 28.Fine JP, Gray RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J Am Stat Assoc. 1999;94(446):496-509. [Google Scholar]
- 29.Gray RJ. A Class of $K$-Sample Tests for Comparing the Cumulative Incidence of a Competing Risk. Ann Stat. 1988;16(3):1141-1154. [Google Scholar]
- 30.Fu Z, Parikh CR, Zhou B. Penalized variable selection in competing risks regression. Lifetime Data Anal. 2017;23(3):353-376. [DOI] [PubMed] [Google Scholar]
- 31.Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321-3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodríguez MdC, Bernad A, Aracil M. Interleukin-6 deficiency affects bone marrow stromal precursors, resulting in defective hematopoietic support. Blood. 2004;103(9):3349-3354. [DOI] [PubMed] [Google Scholar]
- 33.Feng X, Scheinberg P, Wu CO, et al. Cytokine signature profiles in acquired aplastic anemia and myelodysplastic syndromes. Haematologica. 2011;96(4):602-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tie R, Li H, Cai S, et al. Interleukin-6 signaling regulates hematopoietic stem cell emergence. Exp Mol Med. 2019;51(10):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao JL, Ma C, O’Connell RM, et al. Conversion of danger signals into cytokine signals by hematopoietic stem and progenitor cells for regulation of stress-induced hematopoiesis. Cell Stem Cell. 2014;14(4):445-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Assoian RK, Komoriya A, Meyers CA, Miller DM, Sporn MB. Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J Biol Chem. 1983;258(11):7155-7160. [PubMed] [Google Scholar]
- 37.Oh SA, Li MO. TGF-β: guardian of T cell function. J Immunol. 2013;191(8):3973-3979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blank U, Karlsson S. TGF-β signaling in the control of hematopoietic stem cells. Blood. 2015;125(23):3542-3550. [DOI] [PubMed] [Google Scholar]
- 39.Challen GA, Boles NC, Chambers SM, Goodell MA. Distinct hematopoietic stem cell subtypes are differentially regulated by TGF-beta1. Cell Stem Cell. 2010;6(3):265-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santomasso BD, Park JH, Salloum D, et al. Clinical and Biological Correlates of Neurotoxicity Associated with CAR T-cell Therapy in Patients with B-cell Acute Lymphoblastic Leukemia. Cancer Discov. 2018;8(8):958-971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teachey DT, Lacey SF, Shaw PA, et al. Identification of Predictive Biomarkers for Cytokine Release Syndrome after Chimeric Antigen Receptor T-cell Therapy for Acute Lymphoblastic Leukemia. Cancer Discov. 2016;6(6):664-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.