Abstract
Background:
Black women living with HIV account for a higher proportion of new HIV diagnoses than other groups. These women experience restricted access to reproductive services and inadequate support from healthcare providers because their position in society is based on their sexual health and social identity in the context of this stigmatizing chronic disease. By recognizing the analytical relevance of intersectionality, the reproductive decision-making of Black women can be explored as a social phenomenon of society with varied positionality.
Objective:
The purpose of this review was to synthesize the evidence about the reproductive decision-making of Black women living with HIV in high-income countries from the beginning of the HIV epidemic to the present.
Methods:
This systematic review was guided by the JBI evidence synthesis recommendations. Searches were completed in seven databases from 1985 to 2021, and the review protocol was registered with PROSPERO (CRD420180919).
Results:
Of 3503 records, 22 studies were chosen for synthesis, including 19 observational and three qualitative designs. Nearly, all studies originated from the United States; the earliest was reported in 1995. Few studies provided detailed sociodemographic data or subgroup analysis focused on race or ethnicity. Influencing factors for reproductive decision-making were organized into the following seven categories: ethnicity, race, and pregnancy; religion and spirituality; attitudes and beliefs about antiretroviral therapy; supportive people; motherhood and fulfillment; reproductive planning; and health and wellness.
Conclusion:
No major differences were identified in the reproductive decision-making of Black women living with HIV. Even though Black women were the largest group of women living with HIV, no studies reported a subgroup analysis, and few studies detailed sociodemographic information specific to Black women. In the future, institutional review boards should require a subgroup analysis for Black women when they are included as participants in larger studies of women living with HIV.
Keywords: Blacks, contraception, decision-making, developed countries, high-income countries, HIV, organization for economic co-operation and development, racial groups, reproduction, reproductive behavior, systematic review, women’s health
Introduction
Women living with HIV encounter different challenges than men in their daily lives because of their role in reproductive health. For most women, motherhood is an important social identity 1 that gives meaning to life. 2 Reproductive decision-making for women has been described as passive, 3 implicit, 4 automatic, 5 or something that just happens. 6 However, the decision to have a child is heavily influenced by societal norms and community expectations. Hadley 7 suggested the pronatal norm is firmly rooted in sociocultural structures, where motherhood is an inevitable decision for women. As such, motherhood is considered part of the normal course of heterosexual life.3,8–10
Decisions about pregnancy for women living with HIV are often complex. 11 For instance, HIV impacts maternal mortality during pregnancy by increasing the risk of complications and the potential for adverse perinatal outcomes, such as postpartum hemorrhage and puerperal sepsis. In general, pregnant women are also more susceptible to infections.12–14 At the same time, women living with HIV have to cope with stigma and discrimination from their families, social networks, and the larger community, 15 mostly because misinformation and prejudice persist in healthcare institutions.16–18 Consequently, women living with HIV and contemplating pregnancy have additional concerns about their baby being born with HIV, their health during the pregnancy, and their potential death before their child becomes an adult.14,19
Because of increased access to safe contraceptive methods, nearly, 80% 20 of women living with HIV of childbearing age have the choice to avoid pregnancy. 21 Furthermore, more effective antiretroviral therapies can maintain an undetectable viral load, so women living with HIV can choose pregnancy and have a less than a 1% risk of mother-to-child transmission. 22 The availability and access to effective antiretroviral therapies in high-income countries allows women living with HIV to have safe and successful pregnancies. 23 For this reason, these women require guidance from their healthcare providers about reproductive health that is tailored to their reality of living with HIV.
Healthcare providers generally avoid managing the sexual health of patients during primary care visits. 24 In the case of women living with HIV, psychosocial aspects of clinical care are rarely addressed by providers during conversations about reproductive desires and sexual health needs.25–29 Furthermore, women living with HIV report reproductive coercion from healthcare institutions, 30 being advised to avoid pregnancy,31,32 be sterilized,32–34 or have an elective abortion.32,35,36 Despite decades of work to develop women-centered approaches to care for women living with HIV,37,38 stigma remains a major problem in most healthcare settings.39,40 This situation is even more complex since women living with HIV have to concurrently manage family pressures and community expectations when engaging in reproductive decision-making.41,42
Background
The HIV epidemic disproportionately affects some populations of women more than others as evidenced by differences in race, ethnicity, sexual orientation, and socioeconomic characteristics. 43 For example, Black women account for a higher proportion of new HIV diagnoses than other races.44,45 In the United States, Black women living with HIV represent about 13% of the female population but account for 55% of female HIV diagnoses. 46 Similarly, Black women of African ethnicity in the United Kingdom represent 66% of female HIV diagnoses; White women represent only 21% of diagnoses. 47 In addition to managing their HIV infection, Black women must also navigate issues related to racism and discrimination, 48 which contribute to their heightened feeling of stigma. 49 Therefore, Black women living with HIV are more likely to experience depression, posttraumatic stress disorder, and substance abuse. 50
Healthcare experiences are shaped by interconnected and interdependent social conditions. 51 For decades, discrimination has caused an inequitable distribution of healthcare resources 52 that continues to disadvantage Black women living with HIV. 53 Because they encounter restricted access to reproductive services and inadequate support from healthcare providers when making reproductive decisions, 48 these women often access healthcare later or with less frequency for pregnancy-related care. For Black women, race also intersects with other social characteristics that generate oppression with power gradients.54,55 As such, oppression has resulted in involuntary sterilization of Black women living with HIV.56,57 In addition, gendered racism has relegated Black women to the background of HIV research, specifically in relation to reproductive decision-making. 58 As a result, the research literature perpetuates the privilege of being a White, heterosexual, educated, and upper-middle-class woman.
Intersectionality
Black women living with HIV are positioned in society in relation to their sexual health, and their social identity is often contextualized by a stigmatizing chronic disease. 59 However, their social identity also includes multiple sources of oppression, such as race, ethnicity, gender, income, education, health status, and other factors60,61 related to “racialized and gendered subjects” marginalized by power structures. 59 Intersectionality offers a lens to see where this “power comes and collides, where it interlocks and intersects.” 62 Within the narrow context of reproductive justice, 63 power structures can oppress decision-making 64 and marginalize people living with HIV. 65 For these reasons, intersectionality has analytical relevance for sensitive topics, such as reproductive health,66,67 that can be synthesized from the literature to identify the social experiences resulting in marginalization 68 and the positional variability within and between groups 69 causing health inequities. 70
Rationale for the review
The majority of reproductive decision-making literature focuses on women living with HIV without reporting the experiences of Black women living with HIV in high-income countries, such as Canada, 71 the United Kingdom, 72 and the United States. 73 Although the experiences of Black women included in this review are described by their shared social context of living with HIV, 69 the intersection of their different social identities are largely unknown in the reproductive health literature. As such, the findings of this study may guide new areas of research, improve clinical practice, inform health policy, and advance the theoretical development of reproductive decision-making.
Objectives
The purpose of this review was to synthesize the evidence about the reproductive decision-making of Black women living with HIV in high-income countries from the beginning of the HIV epidemic to the present. The principal objective was to describe the factors that influence reproductive decision-making of Black women living with HIV. Key questions guiding this review included the following: (a) Since the beginning of the HIV epidemic, how has the evidence for reproductive decision-making of Black women living with HIV evolved? (b) In studies reporting data for women of different races and ethnicities, how do influencing factors compare in subgroup analyses? (c) What is the relationship between Black women living with HIV and their reproductive intentions across cultures and countries? (d) What are the barriers and facilitators for reproductive decision-making? and (e) How has the advancement of antiretroviral therapy impacted decisions about pregnancy?
Methods
This systematic review of the scientific literature was guided by the Joanna Briggs Institute evidence synthesis recommendations.74,75 The reporting criteria followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, 76 and the protocol guiding this review was registered with PROSPERO (CRD42018091971), the International Prospective Register of Systematic Reviews. 77
Research studies with quantitative, qualitative, and mixed-methods designs published in peer-reviewed scientific journals that addressed reproductive decisions in women living with HIV were included in this review. Studies reporting any type of literature review were excluded, except when the review included a meta-synthesis or meta-analysis reporting data specific to Black women living with HIV. Review papers and graduate dissertations and theses were excluded, but their reference lists were assessed for studies meeting the inclusion criteria. Editorials and commentaries, guidelines, reports, and narrative policy papers were also excluded from the review. Randomized control trials focused exclusively on the efficacy of antiretroviral drugs and epidemiological studies not focused on the reproductive decision-making process were excluded as well.
For this study, high-income countries were determined by membership in the Organization for Economic Co-operation and Development (OECD). 42 The 35 member countries of the OECD 78 have similar compliance with international laws, adherence to human rights conventions, and adoption of evidence-based clinical practice guidelines for HIV/AIDS.79–81 Their health systems are mostly uniform in structure, provide a higher complexity of services, and offer access to good quality services across the population. Evidence of disparities between health systems in higher- and lower-income countries is represented by the differences in maternal and infant mortality and morbidity rates. 82
Publication language for the reviewed studies was limited to English and Spanish. Age was not limited, but an upper demarcation of 55 years was set for reproductive age when assessing data that included age groups from later years.
Information sources
Multiple electronic databases were searched from January 1985 to August 2021, including CINAHL, Embase, MEDLINE (through PubMed), Scopus, Social Sciences Citation Index, Cochrane Library, and PsycINFO. The publication date range was chosen so all studies for the entire HIV epidemic would be included.
Search strategy
The keywords for this review were guided by systematic reviews in related areas and defined by the research team after consultation with a reference librarian. Specifically, the keywords were HIV, AIDS, pregnancy, reproduction, and decision-making. In addition to the keywords, Boolean operators were tailored for each database search. The search was not limited by race or ethnicity since most studies were expected to include data on Black women living with HIV. A hand search for references from documents such as systematic reviews focused on HIV and women was also completed during this process. The example search strategy is provided in Table 1.
Table 1.
Search strategy example.
| CINAHL | RESULTS |
|---|---|
| (Decision making OR attitudes OR beliefs OR meaning OR behavior OR behavior) AND (AIDS OR HIV OR seropositive OR serodiscordant) AND (pregnancy OR pregnant OR reproduction OR reproductive OR family planning OR contraception) NOT (screening or testing) Narrow by subject geographic: Mexico & Central / South America, Asia, Middle East, Australia & New Zealand, continental Europe, the United States, the United Kingdom and Ireland, Europe Narrow by subject age: middle-aged: 45–64 years, adult: 19–44 years Narrow by language: English, Spanish Search modes: Boolean/Phrase Narrow by sex: female Narrow by date from January 01, 2017 to August 30, 2021 |
213 |
Selection process
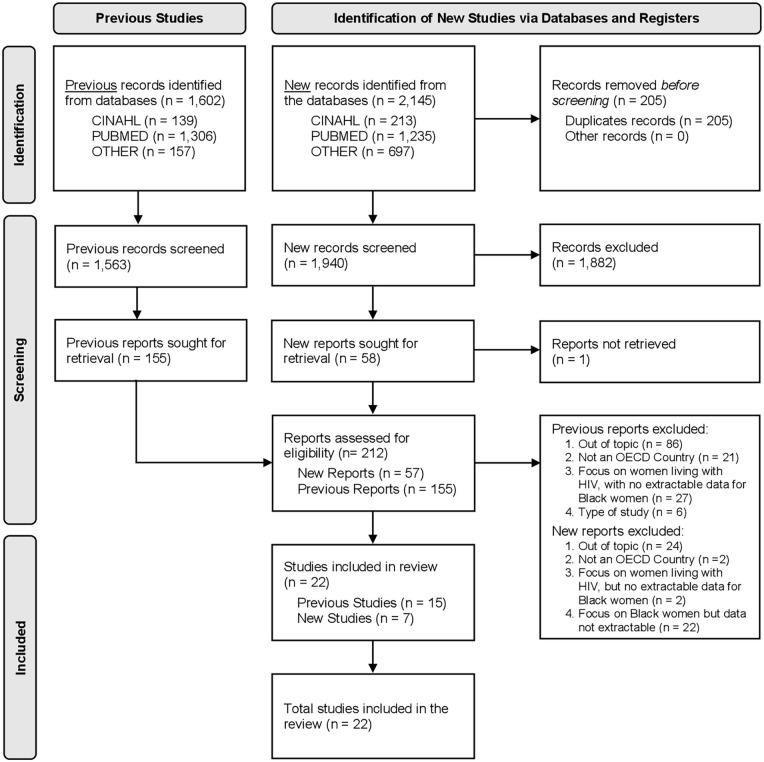
The selection process was divided into two phases. First, records (n = 1602) were identified from a previous systematic review 83 about the reproductive decision-making of women living with HIV. Next, new records (n = 2145) were identified through an updated search of the above databases for studies published between January 1, 2017, and July 31, 2021. All records from the searches were then merged for an initial screening that followed an established study selection process 84 with three review layers (title, abstract, and article). All record titles were independently screened by four paired teams of experienced reviewers to identify the studies that met inclusion criteria. The abstracts for the included titles were then reviewed, where each paired team assessed a different group of abstracts than the titles in the previous step. Finally, the paired teams screened the full text of the remaining reports, strictly applying the inclusion and exclusion criteria. During each round, a third reviewer checked the work of each paired team for discrepancies and errors. If there was disagreement between paired reviewers, the report was advanced to the next phase of the review process to limit deselection bias. The primary investigator checked the level of agreement between paired reviewers for the title and abstract phases; the predetermined 95% agreement was achieved in each round. The 2020 PRISMA flow diagram 76 details the results of the screening process.
Data collection
Data extraction for each study focused on the results and conclusion sections. All figures and tables were reviewed for data specific to Black women living with HIV. General data related to the review objectives were independently extracted line-by-line from the articles by two review authors (AH-Z and JL-M) and recorded in an Excel spreadsheet with a separate tab for each study. The review authors then organized the data by aim, setting, participants, study design, interview data (direct quotes), numerical data, and key findings. Data items of interest were assessments, measurements, experiences, and characteristics related to reproductive decision-making.
Risk of bias assessment
The studies included in the full-text review were independently reviewed by two review authors (AH-Z and JL-M) using established tools for risk and methodological quality assessment, specifically the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies 85 and the Critical Appraisal Skills Program for qualitative studies. 86 Any uncertainty or disagreement was discussed by the same two to achieve consensus followed by an independent review (PAP) of the decision.
Data synthesis
Once assessment was completed for each study, the data were organized in an Excel spreadsheet. Although a meta-analysis of the numerical data extracted from the studies was originally planned, this analysis was not possible because the studies lacked homogeneous data and had too many variations in observational study designs. Thus, a qualitative descriptive analysis was instead completed for the abstracted data. Results were then synthesized based on the research question, and findings were organized into defined decision-making influence categories 83 for women living with HIV but with minor modifications for this review. Organizing the findings in this manner highlighted the multiple similarities and contrasted the few differences. Selective reporting within studies was possible because of the lack of subgroup analysis for race and ethnicity.
Ethical considerations
For this review, ethics approval was not necessary since there were no human participants. All searches were conducted in publicly accessible databases. However, the studies included in the review were evaluated for appropriate ethical standards for research involving human participants, and they all reported approval by an ethics committee or institutional review board.
Results
After removing duplicate records, 3503 records were identified through the systematic database searches. The records included 1563 studies from a previous review 83 and 1940 from the current review. A full-text screening of 212 studies was completed, and 190 studies were excluded for various reasons. Of the final studies (n = 22) included in this review, most studies (n = 15) reported groups of women living with HIV and had extractable data relevant to the review criteria; only a few studies (n = 4) focused on Black women. All reviewed studies met the minimum risk and methodological assessment for quality. Results of the screening process are reported as a PRISMA flow diagram in Figure 1.
Figure 1.
PRISMA 2020 flow diagram.
Reference: Page et al. 87
For more information: http://www.prisma-statement.org/.
In terms of the publication years of the included studies, six were published between 1995 and 2000, six were published between 2001 and 2010, two were published between 2011 and 2015, and the remaining and eight were published after 2015. As summarized in Table 2, most studies (n = 18) were conducted in the United States, and the remainder were in Canada, France, and the United Kingdom. The studies were predominantly quantitative (n = 19) with observational designs (cross-sectional), but there were a few qualitative (n = 3) designs (descriptive, focus group, and phenomenology). Most studies included participants from urban settings who were mostly Black women of African ethnicity. The mean age of the women was 31.6 years. Most studies did not report information about education level (n = 8) or route of HIV infection (n = 7). For those studies that did report this information, most women had completed high school, and the route of infection was most often a sexual route.
Table 2.
Summary of study findings in chronological order.
| Author(s) | Location (context) | Method (design) | Aims/purpose | Key findings |
|---|---|---|---|---|
| Kline et al. 88 | United States (urban) | Observational (cross-sectional) | Describe the profiles of women living with HIV becoming pregnant; understand the reasons for becoming pregnant; and examine pregnancy outcomes | Black women with pregnancy since HIV diagnosis (29.2%) was similar to White women (28.4%) but less than Hispanic women (42.3%). Associations between independent variables and women continuing pregnancy to term: Black (50.4%), White (37.9%), and Hispanic (41.6%). Few differences were statistically significant due to small sample size; but descriptively informative |
| Bedimo et al. 89 | United States (urban) | Qualitative (focus groups) | Explore the barriers to condom use among Black women living with HIV | Pregnancy gave women a societal status that entitled them to things they would not otherwise receive; pregnancy with HIV was a double burden, including concerns about their health, and possibility of having an infected baby |
| Bedimo et al. 90 | United States (urban) | Observational (cross-sectional) | Describe the characteristics of HIV positive women who became pregnant, chose sterilization, and elected abortion after diagnosis | Abortion among women pregnant after learning their HIV diagnosis was significantly associated with being White and non-single. Race was not associated with pregnancy after adjusting for age and sexual assault history |
| Smits et al. 91 | United States (urban) | Observational (cross-sectional) | Understand the relationship between knowledge of HIV infection and prenatal benefits of AZT, decisions about pregnancy planning, contraceptive use, and abortion | Race was not significantly related to subsequent pregnancy planning or termination (women without intravenous drug use living with HIV). Neither any contraceptive nor consistent contraceptive use was significantly associated with race |
| Sowell et al. 92 | United States (urban) | Observational (cross-sectional) | Identify the perception of Black women living with HIV about the risk for perinatal transmission; and examine the factors that influence their pregnancy decision | HIV status is not the most important influence for the reproductive decision-making of a Black woman; they identified significant others (husbands and sex partners) and family members as those more important influences for making the decision to have a child |
| Vitiello and Smeltzer 93 | United States (urban) | Observational (cross-sectional) | Assess the knowledge of women living with HIV about AZT use to reduce transmission during pregnancy and to understand their reproductive perspective | There were no relationships on chi-squared analysis between knowledge about AZT to reduce prenatal transmission during pregnancy by age or by ethnicity. Women living with HIV understanding the benefits of zidovudine were more likely to consider pregnancy (n = 192; p = 0.0001) than those not knowledgeable, without differences in knowledge by ethnicity |
| Chen et al. 94 | United States (n/a) |
Observational (cross-sectional) | Understand fertility and attitudes about contraception and behaviors of HIV positive men and women | All women living with HIV who desired children, 47% were Black; of the Black women 36% expected no children and 52% expected more than one child |
| Bedimo-Rung et al. 95 | United States (urban) | Observational (case–control) |
Describe factors related to reproductive decision-making before the use of HAART among African Americans living with HIV | Since HIV diagnosis, Black women with pregnancy 23.17% (n = 38); without pregnancy 26.83% (n = 44); surgical sterilization 21.34% (n = 35); and without sterilization 28.65% (n = 47) |
| Heard et al. 96 | France (n/a) |
Observational (cross-sectional) | Describe the sociodemographic and health-related factors influencing the desire to have a child among heterosexual individuals of reproductive age living with HIV | Status variables indicated being born in Africa was associated with the desire to have children. The desire to have children was two to six times higher among women born in sub-Saharan (OR 2.38, 95% CI (1.28, 4.43)) and North Africa than Europe (OR 5.73, 95% CI (1.74–18.85)) |
| Stanwood et al. 97 | United States (urban) | Observational (cross-sectional) | Examine the determinants of contraceptive use, desire for children, and sterilization regret among women living with HIV | Multivariate analysis, statistically significant predictors of desire for future childbearing were younger age, not being on HIV medication, higher current CD4 cell count, and relationship duration < 2 years. No association with race |
| Polzer et al. 98 | United States (n/a) | Qualitative (descriptive) | Describe how spirituality impacts African American mothers living with HIV in the context of coping | Perceived as a benevolent authority, God controls all aspects of their lives; power to heal; protects their baby from infection; and encourages them to avoid abortion |
| Loutfy et al. 99 | Canada (urban) |
Observational (cross-sectional) | Assess fertility desires, intentions, and actions of reproductive aged women living with HIV in Toronto, Canada | Women living with HIV intending to have children were more statistically likely to be African ethnicity, in univariate analysis. HIV-positive women in 20s or 30s, African descent, living in Toronto, and already given birth, would be most likely to intend to become pregnant |
| Cliffe et al. 100 | United Kingdom (urban) | Observational (cross-sectional) | Explore fertility intentions among women living with HIV, and to assess the effect of treatment and interventions for perinatal transmission on these intentions | There were no statistically significant differences in the effect of HIV diagnosis on fertility intentions by ethnicity (p = 0.08). Black African women were slightly more likely to report no change in fertility intentions, but 35% did not want children after HIV diagnosis. A lower proportion of non-London residents, Black African women, women over 29 years old, and those diagnosed for < 5 years changed their mind about not wanting children after learning the impact of improvements in treatment and interventions (not statistically significant) |
| Finger et al. 101 | United States (urban) | Observational (cross-sectional) | Determine in a population of young women with behaviorally acquired HIV, the association between desire for pregnancy, sociodemographic variables, and sexual risk behaviors | In young women with behaviorally acquired HIV infections (n = 130), 31.5% reported a desire for pregnancy in the next 6 months; desire for pregnancy was unrelated to ethnicity |
| Fletcher et al. 102 | United States (n/a) |
Qualitative (phenomenology) | Explore perspectives of reproduction and motherhood in African American women living with HIV of childbearing capacity; and the advice received from health care providers | Pregnancy fostered the sense of normalcy; motherhood was perceived to be transformative, inspirational, and purpose-filled; or a second chance. The advice of health care providers was either supportive or non-supportive |
| Raziano et al. 103 | United States (urban) | Observational (cross-sectional) | Identify the factors associated with sterilization among women living with HIV | Women living with HIV (n = 187), 88% Black or African American, with 41 women sterilized from which 33 were Black and eight White women. All other women (n = 146) used intrauterine device, implant, injection, pill, patch, ring, condom, withdrawal, and none. Differences in sterilization by ethnicity were not significant (p = 0.8) |
| Kaida et al. 104 | Canada (urban) | Observational (cross-sectional) | Measure the prevalence and correlates of effective contraceptive use among sexually active women living with HIV in Canada, and to assess the range of methods used, as well as method satisfaction and reasons for nonuse | Women living with HIV (n = 453), with 141 (31%) African American; Black women, 66.7% (n = 94), in the past 6 months used contraceptives, and 33.3% did not (n = 47). Overall, 73% of women in the prior 6 months used contraceptives. Greater proportions of women who had not used contraceptives than used them were African, Caribbean, or Black (39% vs. 29%); no association between Black race and contraceptive use (OR = 0.54, 95% CI (0.29, 1.03), AOR = 0.56, 95% CI (0.27, 1.15). |
| Polansky et al. 105 | United States (urban) | Observational (cross-sectional) | Determine whether pregnancy happiness was positively associated with pregnancy planning and wantedness, controlling for sociodemographic factors and HIV status | Black women living with HIV had higher mean prenatal depressive symptoms (M = 19.55, SD = 13.53) than all other women (M = 15.06, SD = 13.24) that was not statistically significant |
| Haddad et al. 106 | United States (urban) | Observational (cross-sectional) | Explore the reproductive health knowledge, attitudes, and practices among adolescents and young adults living with HIV receiving medical care at an HIV clinic in Atlanta | Women living with HIV (n = 103) with 92 (89.3%) Black from which 27 (29.3%) not sexually active, 26 (28.3%), used condoms, 16 (17.4%) used dual method, 13 (14.1%) used hormonal or intrauterine device, and 10 (10.9%) did not use a method at last coitus. Race not associated with increased odds of contraceptive use at last coitus |
| Tote et al. 107 | United States (urban) | Observational (cross-sectional) | Evaluate factors associated with women living with HIV method of contraceptive at last coitus defined as more effective (Tier 1 and 2 methods (T1/T2)) versus less effective (Tier 3 or no method (T3/none)). | Women living with HIV (n = 136) with 123 (90.6%) Black or African American. From all participants, 42 used T1/T2 from which 41 (97.6%) were Black, and 94 used T3/none, from which 82 (87.23%) were Black. Differences in race and ethnicity by contraception method used were not significant (p = 0.6) |
| Cohn et al. 108 | United States (urban) | Observational (cross-sectional) | Describe parenting desires among women, men who have sex with men, and men who have sex with women | In univariate analysis, factors significantly associated with parenting desires included being Black (this group included all participants) (OR = 2.04, 95% CI (1.60, 2.62)). For women living with HIV, being Black non-Hispanic was not significantly associated with parenting desires with (OR = 0.83, 95% CI (0.40, 1.73)). In multivariable analysis of all participants, Blacks had increased odds for considering children in the future (AOR = 2.20, 95% CI (1.45, 3.34)). For women living with HIV, being Black was not significantly associated with parenting desires (AOR = 0.93, 95% CI (0.31, 2.78)) |
| Gursahaney et al. 109 | United States (urban) | Observational (cross-sectional) | Evaluate factors associated with self-reported condom use in a cohort of adult, predominantly African American women receiving HIV care in Atlanta | Women living with HIV (n = 187). For Black women living with HIV, 108 (73%) used condoms in last coitus. During vaginal intercourse over the past 6 months, 82 (55%) used condoms. Race was not significantly associated with condom use |
OR: unadjusted odds ratio; AOR: adjusted odds ratio; IC: confidence interval.
No major differences were identified by race or ethnicity from previously reported categories of factors influencing the reproductive decision-making of women living with HIV. However, there were minor differences in some factors across categories related to mental health, religion, and relationships. For this reason, synthesis results were organized and reported by previously reported categories. Specifically, the seven categories were ethnicity, race, and pregnancy; religion and spirituality; attitudes and beliefs about antiretroviral therapy; supportive people; motherhood and fulfillment; reproductive planning; and health and wellness.
Ethnicity, race, and pregnancy
In earlier research from the United States, race was not related to planning or terminating a pregnancy. 91 For example, Kline et al. 88 reported 29.2% of Black women became pregnant after an HIV-positive diagnosis, which was similar to the 28.4% of White women who did. Regarding ethnicity, Hispanic women were more likely, at 42.3%, to become pregnant. In another study, 97 statistically significant predictors regarding the desire for childbearing were younger age, not currently on an HIV medication, higher current CD4 cell count, and a relationship duration of less than 2 years; race was not associated with a desire for children. Similarly, more recent studies reported the desire to become pregnant was unrelated to ethnicity.101,108 For women living with HIV, being a Black non-Hispanic woman was not significantly associated with the desire to have children (adjusted odds ratio (AOR) = 0.93, 95% confidence interval (CI) (0.31, 2.78)). 108
In other settings, Black women born in Africa but living in France were more likely than other groups to desire children. 96 The desire to have children was two to six times higher among women born in sub-Saharan (odds ratio (OR) = 2.38, 95% CI (1.28, 4.43)) and North Africa (OR 5.73, 95% CI (1.74, 18.85)) than among women born in Europe. 96 Similarly, Loutfy et al. 99 performed a univariate analysis of women living with HIV (n = 490) and found Black women of African ethnicity (n = 219) were more likely to have children and African ethnicity was a significant predictor (p < 0.0001) of fertility intention in their multivariable model. Finally, a study from the United Kingdom reported no statistically significant differences in the effect of HIV diagnosis on fertility intentions by ethnicity (p = 0.08) although Black women with African ethnicity were slightly more likely to report no change in fertility intentions. 100
Religion and spirituality
Religion and spirituality were important concepts for Black women living with HIV who were considering pregnancy. 98 Faith not only helped the women cope with everyday stresses related to their HIV-positive status, but also helped them manage daily living. Black women often underscored their ruminations about the risks of vertical transmission with the belief that God would protect their baby. 98 From their perspective, God had the power to heal and the power to decide the pregnancy outcome even when they contemplated an elective abortion.
Attitudes and beliefs about antiretroviral therapy
Given the variety of treatment options, women living with HIV can safely attempt pregnancy. In one study, 93 understanding the benefits of zidovudine made women living with HIV more likely to consider pregnancy (n = 192, p = 0.0001) than those who were not knowledgeable, and no differences were found by ethnicity regarding knowledge of zidovudine. Although results were not statistically significant, in another study, a lower proportion of non-London residents, Black women from African countries, women older than 29 years, and women more recently diagnosed with HIV (< 5 years) changed their decision to have children when they learned about improvements in treatments that safely facilitate pregnancy. 100
Supportive people
Healthcare providers have a key role in helping women living with HIV make informed reproductive decisions. However, when offered to women, reproductive counseling was reported as being poor and inconsistent across contexts and countries.110,111 Insufficient information about treatment advancements and reductions in transmission risks to the fetus resulted in women perceiving even greater stigmatization from healthcare providers. 102 Furthermore, HIV status was the most important influencing factor for Black women engaged in reproductive decision-making. Black women also named significant others (husbands and partners) and other family members as the most important people for consultation and guidance when making the decision to have a child. 112 The findings underscore the importance of family in childbearing decisions for Black women living with HIV. 92
Motherhood and fulfillment
Motherhood was reported to be a vital role that gave meaning to the lives of women living with HIV. The recognition of this role may have influenced some Black women living with HIV to try to become pregnant or, at the very least, to not try too hard to prevent it. 90 Motherhood was viewed as transformative, inspirational, and purposeful. Some Black women actively sought a second chance to responsibly care for children. Motherhood post-HIV diagnosis represented and reinforced life, hope, purpose, and normalcy. By extension, pregnancy was an opportunity for “a whole new second chance at life.” 102
Reproductive planning
Black women living with HIV used different birth control strategies to plan their pregnancy. During the late 1990s, abortion among women who became pregnant after their HIV diagnosis was significantly associated with being White and in a relationship. 113 In earlier studies, race was not associated with pregnancy after adjusting for age and sexual assault history. 90 Smits et al. 91 reported that not using or not consistently using contraceptives was significantly associated with race. In a later study, 103 elective sterilization was a common method to prevent pregnancies among women living with HIV. Another study reported 21% (n = 35) of Black women living with HIV had surgical sterilization after learning about their HIV-positive status; 29% (n = 47) were not sterilized. 95 Finally, involuntary 57 and nonconsensual 56 sterilizations are common among women living with HIV, but more problematic for racial and ethnic minorities. 57
Women living with HIV effectively used contraceptives to prevent unwanted pregnancies. In one study with open-ended responses, 73% of women living with HIV used contraceptives in the 6 months before the study. 104 Condoms were the most popular contraceptive for Black women living with HIV, and more than 70% of them used a condom during their last vaginal intercourse. However, race has not been reported as significantly associated with condom use. 109 A more recent study found 28% of Black women living with HIV used only condoms, 17% used dual methods, 14% used only hormonal contraception, and 11% did not use any method during their last vaginal intercourse. 106 Women who chose to not use contraception were significantly more likely to be Black (mostly African and Caribbean) than another race (39% vs 29%). However, there was no association between effective contraceptive use and Black women (OR 0.54, 95% CI (0.29, 1.03); OR 0.56, 95% CI (0.27, 1.15)). 104 Haddad et al. 106 found race was not associated with increased odds of contraceptive use during the last vaginal intercourse. Although not statistically significant, two other studies reported differences between ethnicity and contraceptive method (p = 0.06) 107 and sterilization status (p = 0.08). 103
Health and wellness
When considering a successful pregnancy, Black women living with HIV feared the possibility of mother-to-child transmission because they would need to care for an infected baby. 90 Some women believed totally avoiding pregnancy was the only way to prevent mother-to-child transmission. 102 For women living with HIV who became pregnant, Black women reported higher prenatal depressive symptoms than other women (M= 19.55, SD = 13.53 vs M= 15.06, SD = 13.24, p < 0.24). 105 Such symptoms may influence future reproductive decisions.
Discussion
This review synthesized the evidence about the reproductive decision-making of Black women living with HIV in high-income countries from the beginning of the HIV epidemic to the present. The categories previously identified as factors that influence the reproductive decision-making process for all women living with HIV 83 were remarkably similar to those identified for Black women. However, few studies in this review specifically focused on Black women living with HIV, and most did not provide subgroup analyses by race or ethnicity. Furthermore, the studies reported limited demographic characteristics of participants that could be synthesized by race or ethnicity. Because of this limited data for analysis, synthesis for intersectionality was not possible. However, three key areas related to the findings—reproductive intention, mental health, and research inequity—have implications for policy, practice, and future research.
Reproductive intention
Although HIV status seems to have little impact on a woman’s decision to have children, cultural, and contextual factors make the decision-making process more complex. 114 Regardless of race and ethnicity, motherhood after an HIV diagnosis offers women living with HIV an opportunity for normalcy, achieved through a second chance at life with a family. 115 In this review, no relationship was found between race or ethnicity and planning or ending a pregnancy in the United States, but some studies from Europe reported Black women with African ethnicity were less likely to change their fertility intentions after an HIV diagnosis than European women. This finding may be related to the positive association between African cultural values and the importance of having children for Black women that was reported in an older study. 116 In a retrospective review of women living with HIV in Canada (n = 1165), 30% of the women identified as African/Caribbean/Black, almost 25% became pregnant after their HIV diagnosis with slightly more than 60% unintended. 117 However, none of the reported data was specific to race and ethnicity. Black women living with HIV usually want to continue their pregnancy, 118 but they also need to feel their baby is protected from HIV.119,120 For this reason, some Black women turn to their faith in God and pray for a good outcome. 119 However, involuntary 57 and nonconsensual 56 sterilizations are reported to eliminate reproductive decision-making for women living with HIV especially in the case of racial and ethnic minorities. 57 More research is needed to understand the reproductive intentions of Black women living with HIV and to support their reproductive decision-making and family planning in relation to their culture and context.
Mental health
In this review, significantly higher mean prenatal depressive symptoms were reported for Black women living with HIV than for other women. 105 Similarly, a systematic review of depression in HIV-infected African women reported a 23% mean weighted prevalence for antenatal (13 studies) and postnatal depression (10 studies); suspected depression was reported to be 43% and 31%, respectively. 121 Because symptoms in the studies were not explained by timing or etiology, depression may have been an underlying condition during the reproductive decision-making process. 122 Depressive symptoms for Black women are often missed or not clinically managed by providers. 123 For example, Black women are less likely to receive treatment for mental health problems than nearly all other racial and ethnic groups. 124 In the United States, White women are twice as likely to receive treatment for depression related to pregnancy than Black women. 125 Furthermore, most mental health research specific to pregnancy and to development of screening tools has focused on White women. More research is needed to understand mental health in all groups of women living with HIV, 126 most especially for depression experienced by Black women 127 engaging in reproductive decision-making.
Research inequity
For women living with HIV accessing health services worldwide, inadequate resources and lack of evidence-based clinical guidelines result in poor health outcomes 128 and high levels of marginalization. 129 Although Black women are disproportionately impacted by an HIV diagnosis,44,130 most reproductive decision-making research focuses on White women. 83 Studies that included Black women rarely reported subgroup analysis for race or ethnicity. One notable exception is a secondary data analysis 112 published nearly 20 years following the original data collection. 131 that examined the major influencers of Black mothers with HIV. As a result, the scientific literature has largely ignored Black women living with HIV despite their increased risk for adverse health outcomes, 132 problems with stigma and discrimination, 129 and barriers to accessing health services. Targeted funding is essential to increase the level of research and tailor clinical programs to address reproductive health. As a community, Black women living with HIV need to be prioritized as key stakeholders 133 in the development of new approaches that increase their access to women-centered care. 18
Limitations
This review had several limitations. Few studies reported data that could be extracted for synthesis specific to race or ethnicity. However, to our knowledge, this is the first systematic review focused on the reproductive decision-making of Black women living with HIV. Although most studies were conducted in urban areas of the United States, there were similarities with the few studies conducted in other countries. The lack of sociodemographic participant data and subgroup analysis for race and ethnicity from the reviewed studies limited the depth of analysis and prevented a robust review of intersectionality. Despite these limitations, major strengths of this review were the depth and breadth of the literature search, the longevity of the literature reviewed, the rigorous methods, and the quality assessment. Finally, the including criteria for OECD member countries can be considered a weakness as the literature specific to Black women of African ethnicity from other countries was not included in this review. However, the inclusion criteria can also be considered a strength as the OECD countries are more comparable in the socioeconomic and human rights conditions for women. This limitation is an important area for further research focused on the other countries.
Conclusion
Becoming a mother can be a transformative, inspirational, and purposeful experience for all groups of women. In this review, there were few differences in the reproductive decision-making process between Black women and other groups of women living with HIV. However, the desire to have children was more pronounced for Black women from Africa living with HIV in Europe. Also, prenatal depressive symptoms were more often observed among Black women. Furthermore, religion and spirituality helped Black women cope with their HIV infection and manage fears about vertical transmission. Unfortunately, dehumanizing behaviors and stigmatizing practices still exist in healthcare institutions.
Of the 35 OECD countries, studies from only four countries investigated the reproductive decision-making of Black women living with HIV. Despite the disproportionately larger number of Black women living with HIV, very few studies reported subgroup analysis for race or ethnicity. Therefore, institutional review boards should require subgroup analysis for Black women in larger studies of women living with HIV. Furthermore, clinical trials specifically focused on Black women are necessary to better understand the biopsychosocial factors associated with reproductive decision-making. As such, funding agencies should take a proactive role in promoting research that investigates Black women living with HIV.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057221090827 for Reproductive decision-making of Black women living with HIV: A systematic review by Ariadna Huertas-Zurriaga, Patrick A Palmieri, Mariela P Aguayo-Gonzalez, Karen A Dominguez-Cancino, Cristina Casanovas-Cuellar, Kara L Vander Linden, Sandra K Cesario, Joan E Edwards and Juan M Leyva-Moral in Women’s Health
Acknowledgments
The authors appreciate the continued guidance and support provided by the Joanna Briggs Institute (University of Adelaide) and the Evidence-Based Health Care South America: A JBI Affiliated Group. The authors also recongize thank Deborah Goggin, MA, ELS, scientific writer from the Department of Research Support at A.T. Still University, for her excellent editorial review. Finally, the authors are truly grateful to all the Black women living with HIV who took the time to share their experiences and to complete the surveys for the research studies included in this review.
Footnotes
Author contribution(s): Ariadna Huertas-Zurriaga: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Writing – original draft; Writing – review & editing.
Patrick A Palmieri: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing.
Mariela P Aguayo-Gonzalez: Data curation; Formal analysis; Writing – original draft.
Karen A Dominguez-Cancino: Data curation; Formal analysis; Writing – review & editing.
Cristina Casanovas-Cuellar: Data curation; Formal analysis; Writing – review & editing.
Kara L Vander Linden: Data curation; Formal analysis; Writing – review & editing.
Sandra K Cesario: Data curation; Formal analysis; Writing – review & editing.
Joan E Edwards: Data curation; Formal analysis; Writing – review & editing.
Juan M Leyva-Moral: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The dissemination of this study was funded by the Dirección de Desarrollo de la Investigación, Universidad Norbert Wiener (Grant number: VRI-D-2021-06-002-RDG). The funding agency had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. All authors had full access to the data for the study. The primary, corresponding, and last authors had the final responsibility for the decision to submit the manuscript for publication.
ORCID iDs: Patrick A Palmieri  https://orcid.org/0000-0002-0765-0239
https://orcid.org/0000-0002-0765-0239
Mariela P Aguayo-Gonzalez  https://orcid.org/0000-0002-5968-5214
https://orcid.org/0000-0002-5968-5214
Karen A Dominguez-Cancino  https://orcid.org/0000-0002-4264-8476
https://orcid.org/0000-0002-4264-8476
Cristina Casanovas-Cuellar  https://orcid.org/0000-0003-2077-1542
https://orcid.org/0000-0003-2077-1542
Sandra K Cesario  https://orcid.org/0000-0002-2804-0878
https://orcid.org/0000-0002-2804-0878
Juan M Leyva-Moral  https://orcid.org/0000-0003-4241-4992
https://orcid.org/0000-0003-4241-4992
Supplemental material: Supplemental material for this article is available online.
References
- 1. Tubert S. Los ideales culturales de la feminidad y sus efectos sobre el cuerpo de las mujeres. Quaderns Psicol 2010; 12: 161–174. [Google Scholar]
- 2. Leyva-Moral JM. La dominación del cuerpo femenino: análisis feminista del climaterio y las prácticas de cuidado profesional. Ene 2014; 8, https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2014000100005 [Google Scholar]
- 3. Morison T. Heterosexual men and parenthood decision making in South Africa: attending to the invisible norm. J Family Iss 2013; 34: 1125–1144. [Google Scholar]
- 4. Rijken A, Knijn T. Couples’ decisions on having a first child: comparing pathways to early and late parenthood. Demograph Res 2009; 21: 765–802. [Google Scholar]
- 5. Meyers DT. The rush to motherhood: pronatalist discourse and women’s autonomy. Signs 2001; 26: 735–773. [Google Scholar]
- 6. Krause EL. “They just happened”: the curious case of the unplanned baby, Italian low fertility, and the “end” of rationality. Med Anthropol Q 2012; 26(3): 361–382. [DOI] [PubMed] [Google Scholar]
- 7. Hadley RA. “I’m missing out and I think I have something to give”: experiences of older involuntarily childless men. Work Older People 2018; 22: 83–92. [Google Scholar]
- 8. Riggs DW, Bartholomaeus C. “It’s just what you do”: Australian middle-class heterosexual couples negotiating compulsory parenthood. Femin Psychol 2018; 28: 373–389. [Google Scholar]
- 9. Riggs DW, Bartholomaeus C. The desire for a child among a sample of heterosexual Australian couples. J Reprod Infant Psychol 2016; 34: 442–450. [Google Scholar]
- 10. Overall C. Why have children? The ethical debate. Cambridge, MA: The MIT Press, 2013. [Google Scholar]
- 11. Liamputtong P. Women, motherhood and living with HIV/AIDS: A cross-cultural perspective. Cham: Springer, 2013. [Google Scholar]
- 12. Corrêa S, McIntyre P, Rodrigues C, et al. The population and reproductive health programme in Brazil 1990-2002: lessons learned. Reprod Health Matt 2005; 13(25): 72–80. [DOI] [PubMed] [Google Scholar]
- 13. Haberl A, Reitter A. How does HIV affect the reproductive choices of women of childbearing age. Antivir Ther 2013; 18(Suppl 2): 35–44. [DOI] [PubMed] [Google Scholar]
- 14. Mazzeo CI, Flanagan EH, Bobrow EA, et al. How the global call for elimination of pediatric HIV can support HIV-positive women to achieve their pregnancy intentions. Reprod Health Matters 2012; 20(39 Suppl): 90–102. [DOI] [PubMed] [Google Scholar]
- 15. Saleem HT, Narasimhan M, Denison JA, et al. Achieving pregnancy safely for HIV-serodiscordant couples: a social ecological approach. J Int AIDS Soc 2017; 20: 21331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Campero L, Kendall T, Caballero M, et al. El ejercicio de los derechos sexuales y reproductivos: Un estudio cualitativo de personas heterosexuales con VIH en México. Salud Pública de México 2010; 52: 61–69. [DOI] [PubMed] [Google Scholar]
- 17. Fransen-dos Santos R, Guarinieri M. Men living with HIV in serodiscordant relationships who desire a child/children. J Int AIDS Soc 2017; 20: 21749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O'Brien N, Greene S, Carter A, et al. Envisioning women-centered HIV care: perspectives from women living with HIV in Canada. Womens Health Iss 2017; 27(6): 721–730. [DOI] [PubMed] [Google Scholar]
- 19. Leyva-Moral JM, Piscoya-Angeles PN, Edwards JE, et al. The experience of pregnancy in women living with HIV: a meta-synthesis of qualitative evidence. J Assoc Nurses AIDS Care 2017; 28(4): 587–602 [DOI] [PubMed] [Google Scholar]
- 20. Joint United Nations Programme on HIV/AIDS. The gap report. Geneva: UNAIDS, 2014. [Google Scholar]
- 21. Brown JL, Haddad LB, Gause NK, et al. Examining the contraceptive decisions of young, HIV-infected women: a qualitative study. Women Health 2019; 59(3): 305–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mandelbrot L, Tubiana R, Le Chenadec J, et al. No perinatal HIV-1 transmission from women with effective antiretroviral therapy starting before conception. Clin Inf Dis 2015; 61: 1715–1725. [DOI] [PubMed] [Google Scholar]
- 23. American College of Obstertics Gynecology . Committee opinion 751: labor and delivery management of women with human immunodeficiency virus infection. Obstetr Gynecol 2018; 132: e131–e137. [DOI] [PubMed] [Google Scholar]
- 24. Leyva-Moral JM, Aguayo-Gonzalez M, Palmieri PA, et al. Attitudes and beliefs of nurses and physicians about managing sexual health in primary care: a multi-site cross-sectional comparative study. Nurs Open 2021; 8(1): 404–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barnes DB, Murphy S. Reproductive decisions for women with HIV: motherhood’s role in envisioning a future. Qual Health Res 2009; 19(4): 481–491. [DOI] [PubMed] [Google Scholar]
- 26. Carlsson-Lalloo E, Rusner M, Mellgren A, et al. Sexuality and reproduction in HIV-positive women: a meta-synthesis. AIDS Patient Care STDS 2016; 30(2): 56–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jean J, Coll A, Monda M, et al. Perspectives on safer conception practices and preconception counseling among women living with HIV. Health Care Women Int 2016; 37(10): 1096–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kelly C, Lohan M, Alderdice F, et al. Negotiation of risk in sexual relationships and reproductive decision-making amongst HIV sero-different couples. Cult Health Sex 2011; 13(7): 815–827. [DOI] [PubMed] [Google Scholar]
- 29. Kirshenbaum SB, Hirky AE, Correale J, et al. “Throwing the dice”: pregnancy decision-making among HIV-positive women in four U.S. Perspect Sex Reprod Health 2004; 36(3): 106–113. [DOI] [PubMed] [Google Scholar]
- 30. Park J, Nordstrom SK, Weber KM, et al. Reproductive coercion: uncloaking an imbalance of social power. Am J Obstet Gynecol 2016; 214(1): 74–78. [DOI] [PubMed] [Google Scholar]
- 31. Cuca YP, Rose CD. Social stigma and childbearing for women living with HIV/AIDS. Qual Health Res 2016; 26(11): 1508–1518. [DOI] [PubMed] [Google Scholar]
- 32. van Dijk MG, Wilson KS, Silva M, et al. Health care experiences of HIV-infected women with fertility desires in Mexico: a qualitative study. J Assoc Nurses AIDS Care 2014; 25(3): 224–232. [DOI] [PubMed] [Google Scholar]
- 33. Kumar S, Gruskin S, Khosla R, et al. Human rights and the sexual and reproductive health of women living with HIV—a literature review. J Int AIDS Soc 2015; 18(Suppl5): 20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gruskin S, Ferguson L, O'Malley J. Ensuring sexual and reproductive health for people living with HIV: an overview of key human rights, policy and health systems issues. Reprod Health Matters 2007; 15(29 Suppl): 4–26. [DOI] [PubMed] [Google Scholar]
- 35. O’Neill D. Abortion as a moral good? Lancet 2019; 394: 1323–1324. [DOI] [PubMed] [Google Scholar]
- 36. Watson K. Abortion as a moral good. Lancet 2019; 393: 1196–1197. [DOI] [PubMed] [Google Scholar]
- 37. Loutfy M, Tharao W, Kazemi M, et al. Development of the Canadian women-centred HIV care model using the knowledge-to-action framework. J Int Assoc Provid AIDS Care 2021; 20: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Medeiros P, Gupta M, Wong H, et al. Women-centred HIV care: a scoping review to understand the current state of service delivery for women living with HIV globally. AIDS Care 2021. DOI: 10.1080/09540121.2021.1948498. [DOI] [PubMed] [Google Scholar]
- 39. Chambers LA, Rueda S, Baker DN, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health 2015; 15: 848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Geter A, Herron AR, Sutton MY. HIV-Related stigma by healthcare providers in the United States: a systematic review. AIDS Patient Care STDS 2018; 32(10): 418–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Paudel V, Baral KP. Women living with HIV/AIDS (WLHA), battling stigma, discrimination and denial and the role of support groups as a coping strategy: a review of literature. Reproductive Health 2015; 12: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huertas-Zurriaga A, Palmieri PA, Edwards JE, et al. Motherhood and decision-making among women living with HIV in developed countries: a systematic review with qualitative research synthesis. Reproductive Health 2021; 18: 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pellowski JA, Kalichman SC, Matthews KA, et al. A pandemic of the poor: social disadvantage and the U.S. Am Psychol 2013; 68(4): 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Martin EG, Ansari B, Hart-Malloy R, et al. Racial and ethnic disparities in HIV diagnoses among heterosexually active persons in the United States nationally and by state, 2018. PLoS ONE 2021; 16(9): e0257583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bradley ELP, Williams AM, Green S, et al. Disparities incidence of human immunodeficiency virus infection among black and whitewomen—United States, 2010-2016. Morbid Mortal Wkly Rep 2019; 68: 416–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Centers for Disease Control Prevention. HIV surveillance report, 2019, https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- 47. Brown A, Rawson S, Kelly C, et al. Women and HIV in the United Kingdom: Data to end of December 2017. London: Public Health England, 2019. [Google Scholar]
- 48. Prather C, Fuller TR, Marshall KJ, et al. The impact of racism on the sexual and reproductive health of African American women. J Womens Health (Larchmt) 2016; 25(7): 664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sengupta S, Banks B, Jonas D, et al. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav 2011; 15(6): 1075–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Brownley JR, Fallot RD, Wolfson Berley R, et al. Trauma history in African-American women living with HIV: effects on psychiatric symptom severity and religious coping. AIDS Care 2015; 27(8): 964–971. [DOI] [PubMed] [Google Scholar]
- 51. Brucker MC. Social determinants of health. Nurs Women’s Health 2017; 21: 7–8. [DOI] [PubMed] [Google Scholar]
- 52. Riley AR. Advancing the study of health inequality: fundamental causes as systems of exposure. SSM Popul Health 2020; 10: 100555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Earnshaw VA, Bogart LM, Dovidio JF, et al. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol 2013; 68(4): 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Crenshaw KW. On intersectionality: Essential writings. New York: The New York Press, 2017. [Google Scholar]
- 55. Hill Collins P. Intersectionality as critical social theory. Durham, NC: Duke University Press, 2019. [Google Scholar]
- 56. Rowlands S, Amy JJ. Non-consensual sterilization of women living with HIV. Int J STD AIDS 2018; 29(9): 917–924. [DOI] [PubMed] [Google Scholar]
- 57. Sifris R. Involuntary sterilization of HIV-positive women: an example of intersectional discrimination. Hum Rights Quart 2015; 37: 464–491. [Google Scholar]
- 58. Rosenthal L, Lobel M. Gendered racism and the sexual and reproductive health of Black and Latina Women. Ethn Health 2020; 25(3): 367–392. [DOI] [PubMed] [Google Scholar]
- 59. Serrant L. Silenced knowing: an intersectional framework for exploring Black women’s health and diasporic identities. Front Sociol 2020; 5: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanf Law Rev 1991; 43: 1241–1299. [Google Scholar]
- 61. McCall L. The complexity of intersectionality. Signs 2005; 30: 1771–1800. [Google Scholar]
- 62. Crenshaw KW. Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum 1989; 1989: 1. [Google Scholar]
- 63. Leath S, Wright P, Charity-Parker B, et al. Exploring Black women’s pathways to motherhood within a reproductive justice framework. Qual Health Res 2022; 32: 694–709. [DOI] [PubMed] [Google Scholar]
- 64. Collins PH. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. New York: Routledge, 1990. [Google Scholar]
- 65. Algarin AB, Zhou Z, Cook CL, et al. Age, sex, race, ethnicity, sexual orientation: intersectionality of marginalized-group identities and enacted HIV-related stigma among people living with HIV in Florida. AIDS Behav 2019; 23(11): 2992–3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Nyashanu M, Serrant L. Engaging black sub-Saharan African communities and their gatekeepers in HIV prevention programs: challenges and strategies from England. Family Med Commun Health 2016; 4: 22–29. [Google Scholar]
- 67. Greaves L. Women, gender, and health research. In: Armstrong P, Pederson A. (eds) Women’s health: Intersections of policy research and practice. 2nd ed. Toronto, ON, Canada: Women’s Press, 2015, pp .9–30. [Google Scholar]
- 68. Serrant-Green L. The sound of ‘silence’: a framework for researching sensitive issues or marginalised perspectives in health. J Res Nurs 2011; 16: 347–360. [Google Scholar]
- 69. Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med 2012; 75(12): 2099–2106. [DOI] [PubMed] [Google Scholar]
- 70. Prather C, Fuller TR, Jeffries WL, 4th, et al. Racism, African American women, and their sexual and reproductive health: a review of historical and contemporary evidence and implications for health equity. Health Eq 2018; 2(1): 249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Skerritt L, Kaida A, O’Brien N, et al. Patterns of changing pregnancy intentions among women living with HIV in Canada. BMC Women’s Health 2021; 21: 350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Tariq S, Elford J, Cortina-Borja M, et al. The association between ethnicity and late presentation to antenatal care among pregnant women living with HIV in the UK and Ireland. AIDS Care 2012; 24(8): 978–985. [DOI] [PubMed] [Google Scholar]
- 73. Fletcher FE, Amutah-Onukagha N, Attys J, et al. How can the experiences of black women living with HIV inform equitable and respectful reproductive health care delivery? AMA J Ethics 2021; 23: E156–E165. [DOI] [PubMed] [Google Scholar]
- 74. Aromataris E, Munn Z. JBI manual for evidence synthesis. Adelaide, SA, Australia: Joanna Briggs Institute, 2020. [Google Scholar]
- 75. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021; 18: e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Huertas-Zurriaga A, Palmieri PA, Casanovas C, et al. Reproductive decision making in black women living with HIV. Int J Nurs Stud 2018; 77: 207–221. [DOI] [PubMed] [Google Scholar]
- 78. Organization for Economic Co-operation Development. Secretary general’s report to ministers. Paris: OECD Publishing, 2018. [Google Scholar]
- 79. Hickey MD, Odeny TA, Petersen M, et al. Specification of implementation interventions to address the cascade of HIV care and treatment in resource-limited settings: a systematic review. Implement Sci 2017; 12: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Mepham S, Bland R, Newell ML. Prevention of mother-to-child transmission of HIV in resource-rich and -poor settings. BJOG 2011; 118(2): 202–218. [DOI] [PubMed] [Google Scholar]
- 81. Tudor Car L, van Velthoven M, Brusamento S, et al. Integrating prevention of mother-to-child HIV transmission (PMTCT) programmes with other health services for preventing HIV infection and improving HIV outcomes in developing countries. Cochrane Database Syst Rev 2011; 6: CD008741. [DOI] [PubMed] [Google Scholar]
- 82. Ramakrishnan R, Rao S, He JR, Perinatal health predictors using artificial intelligence: a review. Womens Health (Lond) 2021; 17: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Leyva-Moral JM, Palmieri PA, Feijoo-Cid M, et al. Reproductive decision-making in women living with human immunodeficiency virus: a systematic review. Int J Nurs Stud 2018; 77: 207–221. [DOI] [PubMed] [Google Scholar]
- 84. Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs 2014; 114(6): 47–52. [DOI] [PubMed] [Google Scholar]
- 85. National Heart Lung Blood Institute. Quality assessment tool for observational cohort and cross-sectional studies, 2014, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 86. Critical Appraisals Skills Programme. CASP qualitative studies checklist, 2018, https://casp-uk.net/casp-tools-checklists/
- 87. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kline A, Strickler J, Kempf J. Factors associated with pregnancy and pregnancy resolution in HIV seropositive women. Soc Sci Med 1995; 40(11): 1539–1547. [DOI] [PubMed] [Google Scholar]
- 89. Bedimo AL, Bennett M, Kissinger P, et al. Understanding barriers to condom usage among HIV-infected African American women. J Assoc Nurses AIDS Care 1998; 9(3): 48–58. 10.1016/S1055-3290(98)80019-8 [DOI] [PubMed] [Google Scholar]
- 90. Bedimo AL, Bessinger R, Kissinger P. Reproductive choices among HIV-positive women. Soc Sci Med 1998; 46(2): 171–179. [DOI] [PubMed] [Google Scholar]
- 91. Smits AK, Goergen CA, Delaney JA, et al. Contraceptive use and pregnancy decision making among women with HIV. AIDS Patient Care STDS 1999; 13(12): 739–746. [DOI] [PubMed] [Google Scholar]
- 92. Sowell RL, Phillips KD, Misener TR. HIV-infected women and motivation to add children to their families. J Family Nurs 1999; 5: 316–331. [Google Scholar]
- 93. Vitiello MA, Smeltzer SC. HIV, pregnancy, and zidovudine: what do women know. J Assoc Nurses AIDS Care 1999; 10(4): 41–47. [DOI] [PubMed] [Google Scholar]
- 94. Chen JL, Phillips KA, Kanouse DE, et al. Fertility desires and intentions of HIV-positive men and women. Fam Plan Perspect 2001; 33(4): 144–165. 10.2307/2673717 [DOI] [PubMed] [Google Scholar]
- 95. Bedimo-Rung AL, Clark AR, Dumestre J, et al. Reproductive decision-making among HIV-Infected women. J Natl Med Assoc 2005; 97: 1403–1410. [PMC free article] [PubMed] [Google Scholar]
- 96. Heard I, Sitta R, Lert F, et al. Reproductive choice in men and women living with HIV: evidence from a large representative sample of outpatients attending French hospitals (ANRS-EN12-VESPA Study). AIDS 2007; 21(Suppl 1): S77–S82. [DOI] [PubMed] [Google Scholar]
- 97. Stanwood NL, Cohn SE, Heiser JR, et al. Contraception and fertility plans in a cohort of HIV-positive women in care. Contraception 2007; 75(4): 294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Polzer Casarez RL, Miles MS. Spirituality: a cultural strength for African American mothers with HIV. Clin Nurs Res 2008; 17(2): 118–132. [DOI] [PubMed] [Google Scholar]
- 99. Loutfy MR, Hart TA, Mohammed SS, et al. Fertility desires and intentions of HIV-positive women of reproductive age in Ontario, Canada: a cross-sectional study. PLoS ONE 2009; 4: e7925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Cliffe S, Townsend CL, Cortina-Borja M, et al. Fertility intentions of HIV-infected women in the United Kingdom. AIDS Care 2011; 23(9): 1093–1101. [DOI] [PubMed] [Google Scholar]
- 101. Finger JL, Clum GA, Trent ME, et al. Desire for pregnancy and risk behavior in young HIV-positive women. AIDS Pat Care STDS 2012; 26(3): 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Fletcher FE, Ingram LA, Kerr J, et al. “Out of all of this mess, I got a blessing”: perceptions and experiences of reproduction and motherhood in African American women living with HIV. J Assoc Nurses AIDS Care 2016; 27(4): 381–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Raziano VT, Smoots AN, Haddad LB, et al. Factors associated with sterilization among HIV-positive US women in an urban outpatient clinic. AIDS Care 2017; 29(5): 612–617. [DOI] [PubMed] [Google Scholar]
- 104. Kaida A, Patterson S, Carter A, et al. Contraceptive choice and use of dual protection among women living with HIV in Canada: priorities for integrated care. Perspect Sex Reprod Health 2017; 49(4): 223–236. [DOI] [PubMed] [Google Scholar]
- 105. Polansky M, Singh H, Gao Y, et al. Pregnancy planning, timing, happiness and depressive symptoms among low-income women living with and without HIV. J Reprod Infant Psychol 2018; 36(3): 222–234. [DOI] [PubMed] [Google Scholar]
- 106. Haddad LB, Brown JL, King C, et al. Contraceptive, condom and dual method use at last coitus among perinatally and horizontally HIV-infected young women in Atlanta, Georgia. PLoS ONE 2018; 13(9): e0202946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Tote KM, Raziano VT, Wall KM, et al. Contraceptive method use among HIV-positive women in a US urban outpatient clinic: an exploratory cross-sectional study. Contraception 2018; 98(6): 492–497. [DOI] [PubMed] [Google Scholar]
- 108. Cohn SE, Haddad LB, Sheth AN, et al. Parenting desires among individuals living with human immunodeficiency virus in the United States. Open Forum Infect Dis 2018; 5(10): ofy232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Gursahaney PR, Cordes S, Ofotokun I, et al. Factors associated with condom use among HIV-positive women living in Atlanta, Georgia. PLoS ONE 2019; 14(12): e0225406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Dehlendorf C, Rodriguez MI, Levy K, et al. Disparities in family planning. Am J Obstet Gynecol 2010; 202: 214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ippoliti NB, Nanda G, Wilcher R. Meeting the reproductive health needs of female key populations affected by HIV in low- and middle-income countries: a review of the evidence. Stud Fam Plann 2017; 48(2): 121–151. [DOI] [PubMed] [Google Scholar]
- 112. Amutah NN, Gifuni J, Wesley Y. Shaping the conversation: a secondary analysis of reproductive decision-making among Black mothers with HIV. Clin Med Insights Womens Health 2016; 9(Suppl1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Levine C, Dubler NN. Uncertain risks and bitter realities: the reproductive choices of HIV-infected women. Milbank Q 1990; 68(3): 321–351. [PubMed] [Google Scholar]
- 114. Craft SM, Delaney RO, Bautista DT, et al. Pregnancy decisions among women with HIV. AIDS and Behavior 2007; 11: 927–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Fletcher FE, Ingram LA, Kerr J, et al. “She told them, oh that bitch got AIDS”: experiences of multilevel HIV/AIDS-related stigma among African American women living with HIV/AIDS in the South. AIDS Patient Care STDS 2016; 30(7): 349–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Pivnick A, Jacobson A, Eric K, et al. Reproductive decisions among HIV-infected, drug-using women: the importance of mother-child coresidence. Med Anthropol Quart 1991; 5: 153–169. [Google Scholar]
- 117. Salters K, Loutfy M, de Pokomandy A, et al. Pregnancy incidence and intention after HIV diagnosis among women living with HIV in Canada. PLoS ONE 2017; 12(7): e0180524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Maccarthy S, Rasanathan JJ, Crawford-Roberts A, et al. Contemplating abortion: HIV-positive women’s decision to terminate pregnancy. Cult Health Sex 2014; 16(2): 190–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Njie-Carr V, Sharps P, Campbell D, et al. Experiences of HIV-positive African-American and African Caribbean childbearing women: a qualitative study. J Natl Black Nurses Assoc 2012; 23(1): 21–28. [PMC free article] [PubMed] [Google Scholar]
- 120. de Bruyn M. Safe abortion for HIV-Positive women with unwanted pregnancy: a reproductive right. Reprod Health Matters 2003; 11(22): 152–161. [DOI] [PubMed] [Google Scholar]
- 121. Sowa NA, Cholera R, Pence BW, et al. Perinatal depression in HIV-infected African women: a systematic review. J Clin Psychiatry 2015; 76(10): 1385–1396. [DOI] [PubMed] [Google Scholar]
- 122. Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Frontiers in Psychology 2015; 6: 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Liao KY-H, Wei M, Yin M. The misunderstood schema of the strong black woman: exploring its mental health consequences and coping responses among African American women. Psychol Women Quart 2020; 44: 84–104. [Google Scholar]
- 124. National Alliance on Mental Illness. Black/African American, https://nami.org/Your-Journey/Identity-and-Cultural-Dimensions/Black-African-American (2021, accessed 16 June 2021).
- 125. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv 2011; 62(6): 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Waldron EM, Burnett-Zeigler I, Wee V, et al. Mental health in women living with HIV: the unique and unmet needs. J Int Assoc Provid AIDS Care 2021; 20: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Ward EC, Heidrich SM. African American women’s beliefs about mental illness, stigma, and preferred coping behaviors. Res Nurs Health 2009; 32(5): 480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. World Health Organization. Maintaining and improving quality of care within HIV clinical services. Geneva: WHO Press, 2019. [Google Scholar]
- 129. Rice WS, Logie CH, Napoles TM, et al. Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med 2018; 208: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Aziz M, Smith KY. Challenges and successes in linking HIV-infected women to care in the United States. Clin Infect Dis 2011; 52: S231–S237. [DOI] [PubMed] [Google Scholar]
- 131. Wesley Y, Smeltzer SC, Redeker NS, et al. Reproductive decision making in mothers with HIV-1. Health Care Women Int 2000; 21(4): 291–304. [DOI] [PubMed] [Google Scholar]
- 132. Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open 2016; 6: e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Barr D, Odetoyinbo M, Mworeko L, et al. The leadership of communities in HIV service delivery. AIDS 2015; 29(Suppl. 2): S121–S127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057221090827 for Reproductive decision-making of Black women living with HIV: A systematic review by Ariadna Huertas-Zurriaga, Patrick A Palmieri, Mariela P Aguayo-Gonzalez, Karen A Dominguez-Cancino, Cristina Casanovas-Cuellar, Kara L Vander Linden, Sandra K Cesario, Joan E Edwards and Juan M Leyva-Moral in Women’s Health