Abstract
A questionnaire was developed to evaluate the journey experienced by patients from identifying a need to see a community specialist in Israel's public healthcare system, through scheduling an appointment and attending. A telephone survey was conducted with a nationally representative group of 3751 adults, in 2019 to 2020. Fifty-seven percent needed to see a specialist in the last 6 months; among those, 82%, visited a specialist. Among the 3% who did not make an appointment, in 41 of 52 (79%) cases this was due to long waiting time. Younger and more educated patients were more likely to try to get an earlier appointment. Timeliness (55%) and wanting a specific physician (43%) were major considerations in scheduling. Reported need was greater in females, Jewish versus Arab respondents, more educated and those with chronic illness. Those who did not make an appointment sought private care, emergency treatment, or went untreated. Although a large percentage of respondents did eventually get an appointment, vulnerable patients may have more difficulty navigating the system. Following the patient journey can provide insights to help design services better suited to patients’ needs.
Keywords: patient preferences, appointment scheduling, specialists
Introduction
Patient experience is an important component of patient-centered care, influencing patient satisfaction and health. A systematic review of the evidence concluded that patient experience is associated with objectively measured health outcomes, preventive care, adherence to treatment, clinical effectiveness, and patient safety (1).
Patient experience comprises both functional aspects, such as timeliness and continuity of care; and relational aspects, which concern interpersonal aspects such as empathy of clinicians and involvement in decision-making (1). Patients’ experience, including satisfaction with the system, and perception of waiting times (WT), contribute to how long they are likely to wait in the public health system and whether and when they may leave the queue and choose alternatives, private treatment, or forgo treatment altogether. Beyond waiting times, other components of the process may be important within patient experience, for example, ease of communication and navigation through the system (2), or the option of choosing a specific physician. In primary care, the option to choose one's general practitioner (GP) was found to increase satisfaction with care (3).
Many factors may affect satisfaction with appointment scheduling including timeliness, location, and continuity of care. In a study of patients’ attitudes and open-access scheduling systems, risk-seeking characteristics were associated with choices when making appointments, regarding continuity of care (waiting for a specific, known physician) versus timeliness (preferring shorter wait time for another available physician). Risk-seeking patients were largely motivated by speed, and thus were more likely to prefer a quicker appointment with an unfamiliar physician, while for a serious condition they were more likely to prioritize a specific doctor (4).
Israel's public health system provides universal coverage through 4 competing Health Plans (HP) and guarantees the right of all citizens to receipt of healthcare “at a reasonable time, distance and quality” (5). Health Plan members have access to a statutory benefits package. Most specialist ambulatory care is provided in the community (6). Despite universal health coverage, private (“out of pocket”) expenditure on health remains around 34% to 35% of the national expenditure on health in 2018 (7). Most of the Israeli population (77%) holds complementary health insurance, mediated by the health plans, while around a third (35%) have private health insurance, sold through insurance companies, with some holding both types of insurance (6). Ownership of both insurance types is higher among the higher socioeconomic quintiles, and among Jews, compared with Arab citizens: Ownership of complementary health insurance was 86% and 38% among Jews and Arabs, respectively, and of private health insurance was 40% and 12% (8).
The “journey” of the patient in scheduling an appointment with a community-based specialist starts from the point of needing to see a specialist. Diverse factors throughout the process of trying to schedule, scheduling and finally attending the appointment might affect the decision to continue waiting or to leave the queue.
Patient experience in scheduling appointments is important since it might help identify reasons for not making or keeping an appointment, which may lead to avoidable emergency care, to seeking private treatment, or to forgoing care altogether. Insights gained about the patient journey might be used by decision makers to improve work processes in the healthcare system.
The aims of the current study were: (1) to evaluate patients’ experience during the process of scheduling and waiting for an appointment with a community specialist physician through the public healthcare system; (2) to evaluate disparities in the process of scheduling an appointment, and (3) to determine to what extent patients’ needs are being met.
Methods
A telephone survey was conducted by Myers-JDC-Brookdale Institute among a representative sample of Israeli adults aged 22 and over, between August 2019 and February 2020. The reason for excluding those aged less than 22 is that more than half of Israelis aged 18 to 21 serve in the army and have a separate health system for community-based care. Interviews were conducted in Hebrew, Arabic (the 2 official languages), Russian (the third most commonly spoken), or English according to the participants’ choice. A first call was made to explain the study, obtain consent and set a date for the telephone survey. Each questionnaire took around 20 min. A stratified hierarchical sampling was performed by population group in order to obtain a representative sample of all population subgroups with over sampling of the Arab minority. Both landlines and mobile phone numbers were included for better representation. The survey was anonymous with response rate of 55%.
Weighting was used in order to generalize to the adult Israeli population based on age group, geographic region, gender, and ethnic group (Arab/Jewish). In order to match the sample characteristics to population characteristics, a weight was given to each respondent according to the population groups they belonged to—sex (2 categories), ethnic group (Jewish or other vs Arabic), age (5 categories), and region (6 categories)—for a total of 120 groups. Weighting was then conducted to match the proportion of each group in the sample to the true proportion of that group in the population. All analyses used weighted data.
The survey tool was developed specifically for this study, as a collaboration of Myers-JDC-Brookdale Institute, the Ministry of Health, and the Gertner Institute. The questionnaire aimed to examine the patient experience of booking and waiting for a community specialist appointment and to learn about the patient's decision-making at various junctions throughout the process. The questionnaire was validated in the 4 study languages and pretesting conducted.
The survey aimed to evaluate the scheduling process within the publicly funded services, thus all questions referred to scheduling an appointment with a specialist working with the respondents’ health provider. Privately financed care, whether out of pocket or through private health insurance, (which is either supplementary ie, offered by the health plans, or commercial ie, from insurance companies) was excluded.
Participants were asked if they needed to see a specialist physician in the last 6 months. If they needed more than one specialist, they were asked to answer about the last need they experienced.
Survey Tool
Scheduling process variables
The English version of the full survey instrument is available in Supplementary Information. The scheduling journey was assessed from the point of the need to seek care (“in the last 6 months did you need to see a specialist physician?”) through the attempt to schedule an appointment—(“did you (or someone on your behalf) try to make an appointment with a specialist?”) to setting the appointment, and the actual appointment which took place.
At each stage, participants who responded in the negative (did not try to make an appointment, did not make an appointment, did not go to the appointment) were asked to indicate the reason and what they did instead. Patients who made an appointment were asked: “how long did you have to wait from the day you tried to make an appointment with a specialist until the appointment which was offered to you?.”
Other questions included outcome (“Did the problem resolve/ get worse?”) and no-show (“Why did you not go to the appointment you scheduled?”). Respondents who reported choosing the private option were asked for the reason.
Sociodemographic characteristics
Information was collected on age group, geographic region of residence, marital status, education, ethnic group, religiosity, income, employment status, country of birth, and possession of private health insurance.
Clinical variables
Information was collected on self-rated health and on the presence of chronic illness (respondents were asked if they suffer from any chronic disease such as hypertension, diabetes, or asthma) for which they take regular medications.
Statistical analysis
Descriptive statistics were performed to assess the number and proportion of participants at each junction. Logistic regressions were used (with the Firth logistic regression method used for rare events, since the logistic model suffers from small sample bias) (9) to assess which factors were associated with choosing a specific doctor; and to determine which factors were significantly associated with remaining in the queue or dropping out at junctions between the following milestones: need, trying, scheduling, and attending.
Results
A total of 4022 participants completed the survey, of which 271 were excluded for incomplete data, and 3751 were entered into the analysis. Tables 1 and 2 present details of the survey sample. The majority of respondents were between 22 and 74 years old, with only 2% of respondents aged 75+. Fifty-seven percent (n = 2124) of respondents reported needing to see a specialist in the last 6 months, the majority (70%), in one of the 5 most common specialties (orthopedics, dermatology, ophthalmology, gynecology, and otolaryngology [ENT]). Mean reported wait time for a specialist was 31 days; median reported wait time was 21 days. 53% of survey respondents considered the wait time offered to them to be reasonable.
Table 1.
Description of Survey Sample.
| Variable | Unweighted, N (%) | Weighted, N (%) |
|---|---|---|
| Age | ||
| 22-44 | 1321 (35%) | 49% |
| 45-64 | 1383 (37%) | 32% |
| 65+ | 982 (26%) | 19% |
| Missing data | 65 (2%) | - |
| Male | 1715 (46%) | 49% |
| Female | 2036 (54%) | 51% |
| Arab | 638 (17%) | 18% |
| Jewish | 3113 (83%) | 82% |
| Region of residence | ||
| North/Haifa | 1090 (29%) | 28% |
| Centre/Tel Aviv | 1717 (41%) | 43% |
| Jerusalem/Samaria | 524 (14%) | 15% |
| South | 420 (11%) | 14% |
| Chronic illness | 1386 (37%) | 30% |
Abbreviation: N, number of respondents.
Table 2.
Reported Need of Specialists.
| N | % | |
|---|---|---|
| Orthopedics | 540 | 25.6 |
| Dermatology | 284 | 13.4 |
| Ophthalmology | 237 | 11.2 |
| Gynecology | 243 | 11.5 |
| Otolaryngology (ENT) | 175 | 8.3 |
| Cardiology | 79 | 3.7 |
| Gastroenterology | 88 | 4.2 |
| Neurology | 59 | 2.8 |
| Other | 408 | 19.3 |
Mapping the Appointment Scheduling Process
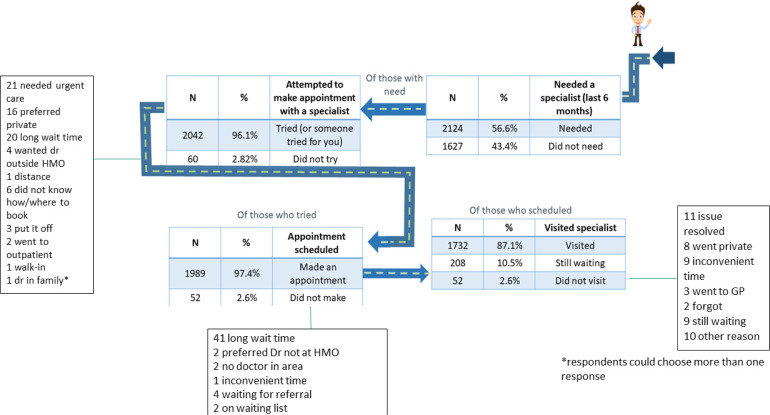
Figure 1 shows the percentage of respondents who expressed a need (56.6%), attempted to make an appointment or had someone try on their behalf (96.1% of those with need), made an appointment (97.4% of those who tried), and eventually visited a specialist (87.1% of those who scheduled, with a further 10.5% still waiting for their appointment). Just 2.6% failed to see a specialist despite scheduling an appointment (see Figure 1). The most common reasons for failing to see a specialist were inconvenient time (15%), the problem resolved (15%), or the patient went to a private doctor instead (7%).
Figure 1.
Flowchart showing the number and proportion of respondents at different stages of the appointment scheduling process and reasons for dropping out (numbers in the boxes represent the number of respondents choosing each reason).
Twenty-eight percent (561 respondents) of those who made an appointment, tried to get an earlier appointment than the one they were first offered, and 158 (28% of those that tried) succeeded in getting one. Younger and more educated patients were more likely to try to get an earlier appointment. Age, education, and population group were not related to succeeding in getting an earlier appointment, though men (34%) were more successful than women (24%) (P = .01). There was a higher likelihood of succeeding in getting an earlier appointment in ENT, gynecology, and orthopedics, and a lower chance for dermatology, cardiology, ophthalmology, and gastroenterology.
Considerations and Alternatives to Scheduling an Appointment
Major considerations when making an appointment were: timeliness (1126; 55%), wish to see a specific doctor (883; 43%), geographical proximity (733; 36%), and convenience of day/time (293; 14%). A further 3% (n = 70) were influenced by the gender of the doctor.
Of the small minority that expressed a need yet did not try to make an appointment (n = 60), the most common reason was needing an urgent appointment (35%), followed by a preference for a private doctor (27%). Alternatives for booking a specialist appointment included walk-ins, urgent care, GP, private doctor, calling the HP advice line, or not seeking any treatment. Of those who tried yet did not eventually make an appointment, in 79% (41/52) of cases this was due to long waiting time.
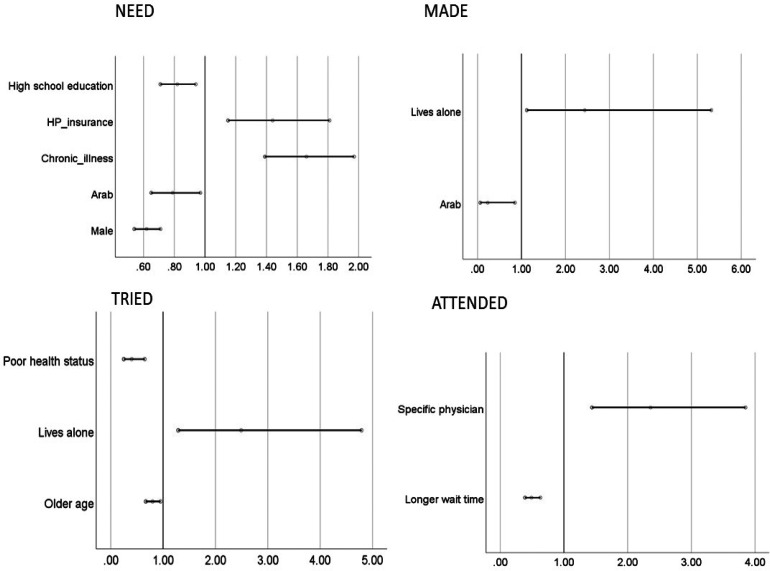
Characteristics of Individuals Reporting Need, Attempt, Scheduling, and Attending the Appointment
Needing a Specialist
Logistic regression demonstrated that respondents who reported a need to see a specialist in the last 6 months were more likely to be female, more educated, have complementary health insurance, be Jewish, and to suffer from some chronic illness (Figure 2), and more likely to reside in the central Tel Aviv region than Jerusalem or the Southern periphery (not shown). A sensitivity analysis was conducted excluding gynecology appointments, to assess the relationship between gender and need. Although the gender gap in need was reduced, it remained significant, with men still less likely to report the need for a specialist (P = .02).
Figure 2.
Odds ratios (95% CI) for variables significantly related to the 4 junctions: needed a specialist, tried to schedule, made an appointment, attended. HP-insurance = supplementary health insurance via the health plan.
Looking at specialty, Arab respondents reported more need of orthopedic physician compared to Jewish respondents and less need for dermatologists and ophthalmologists. The percentage of patients needing gynecologists and ENT specialists was similar between population groups. Indeed, when comparing regions and the need for different specialties, the Northern region showed the lowest percentage of all regions with regard to the need for dermatology.
Respondents with chronic illness were more likely to need an ophthalmologist or cardiologist than those without, and less likely to need a gynecologist, orthopedist, or ENT specialist.
Tried to book an appointment
Older respondents were less likely to try to make an appointment. Poor health status was also associated with a lower likelihood of trying to make an appointment. The highest rate of reporting a need but not attempting to schedule an appointment in the public system was reported for neurology (9%), cardiology (4%), and orthopedics (4%), with much lower rates in other specialties (ENT 0%, gynecology 0%, dermatology 2%, and ophthalmology 2%).
Made an appointment
Arab respondents were less likely to schedule an appointment than Jewish respondents. Respondents living alone were more likely to make an appointment. Of those who did not schedule an appointment, the highest percentage was for orthopedics (34%), followed by ENT (13%), dermatology (11%), gastro (8%), gynecology (4%), and ophthalmology and cardiology (2% each).
Attended appointment
Patients who booked a specific (rather than any) doctor were more likely to attend (OR 2.36), and a longer wait time lowered the chance of attending (OR 0.49).
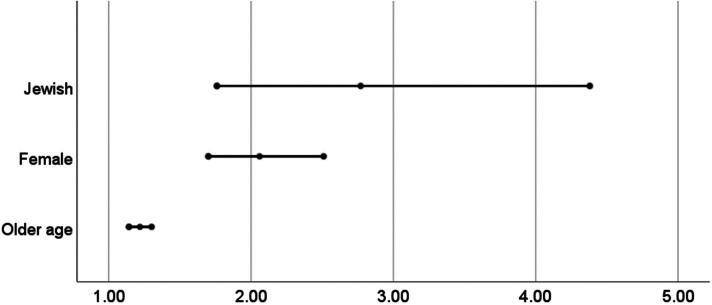
Choice of Physician
Of those who tried to make an appointment, slightly more than half (53%) wanted a specific, named physician, while 48% did not have a preference. Requesting a specific physician was associated with older age (OR 1.219 for increasing age, 95% CI: 1.142-1.301), higher income (44% of those with a household income up to 6400 NIS vs 68% of those with monthly household income over 47 000 NIS), female sex (OR 2.06; 95% CI: 1.70-2.51), and Jewish compared to Arab ethnicity (OR 2.77; 95% CI: 1.76-4.38) (Figure 3). Requests for a specific doctor were most common in the field of gynecology (79%), compared to other specialties (40%-50%).
Figure 3.
Odds ratios (95% CI) for preference for a specific physician.
Seeking Private Care and Satisfaction With the Public System
A small number of respondents (n = 97; 6%) made an appointment with a private specialist in addition to making an appointment through the HP, for the same problem. Of these, the majority (82%) visited the private doctor (either instead of or in addition to the HP doctor). Jewish patients were more likely to double-book than Arab patients (16% vs 8%); and this difference remained significant in logistic regression analysis (P = .02); age, region, income, and HP were not significantly related to double booking. Fifteen percent of respondents (556 people) reported that they had considered switching HPs due to long wait times for specialist care.
Discussion
More than half (57%) of respondents in a random representative survey of Israeli adults reported the need to see a specialist in the last 6 months. This is consistent with the 59% of respondents who reported visiting a specialist in a 2018 Israeli survey (10) and is similar to the 60% of patients who had seen a specialist in the last 2 years in a Canadian patient survey (11). The vast majority of respondents (82%) in the current survey who expressed a need were able to get an appointment and had seen a physician by the time of the survey. A further 10% were still on the waiting list at the time of the survey. Mean reported wait time for a specialist was 31 days and median wait time was 21 days. These figures are slightly longer than those reported in administrative data which showed median wait time varying between 10 and 17 days depending on specialty for the same period (12).
However, disadvantaged sectors of society—older patients, and those with poorer health—were less likely to try to book an appointment when in need, and members of the Arab minority were less likely to actually schedule an appointment. Younger patients were more likely to try to get an earlier appointment than the first one offered. This may be because they are more adept at navigating the system, especially by digital means which are more convenient and allow one to schedule an appointment 24/7 and skip waiting for the call center response (13,14). Health providers may need to adapt their systems to improve accessibility for more vulnerable populations (eg, keeping waiting lists, offering earlier slots by default when there are cancellations, instead of telling patients to call and ask for them).
Less need for specialist care was expressed among men, among the Arab minority, and among those without complementary health insurance, suggesting different patterns of help-seeking behavior. This is reflected in the literature where women seek healthcare more frequently than men (15), and men are more likely to delay help-seeking (16), sometimes resulting in later diagnosis and consequently poorer outcomes. However, when men did report a need and attempted to make an appointment, they were more successful than women in getting an earlier appointment, perhaps demonstrating greater assertiveness in navigating the system. It should be noted that one of the 5 most frequent specialties included here was gynecology, increasing the chance of women needing a visit over men. However, even when excluding this specialty from the analysis, the same pattern was maintained, though slightly weakened.
Living alone was also related to a greater likelihood of making a specialist appointment. This fits with the findings that elderly people living alone have generally poorer physical and emotional health, compared with those living with relatives (17), and that loneliness among older populations has been shown to be related to greater use of primary care services (18,19).
Ethnic minorities are overrepresented in the global burden of disease, with for example higher incidence of diabetes (20), kidney disease (21), and cardiovascular disease (22). Similarly, diabetes is more prevalent in the Arab Israeli minority, compared to the general Israeli population (23). Less need of specialist care reported in the current survey among Arabs is thus surprising. It is, however, consistent with survey data from 2007 which found that Arabs visited their GP more often, but that Arab women saw specialists less frequently than Jewish women (OR = 0.7) (24). It is also consistent with a more recent survey in which Muslim Arabs reported lower rates of visiting specialists within the last year (31% among Muslims compared to 57% among Jews) (25). Patients without supplementary health insurance were also less likely to report need of a specialist in our survey. Within the framework of universal health coverage, additional insurance is not required to see a specialist in the community, since all specialist consultations are covered within the benefit package of services. However, supplementary health insurance can help to shorten long waiting times by allowing access to semiprivate specialists, offered by the health plans to members with this kind of insurance, at a subsidized rate.
A systematic review of health service use in ethnic minorities found potential barriers at 3 levels: patient (including sociodemographics and health beliefs), provider (skills and attitude), and system (organizational) level (26). An Israeli study reported structural barriers related to access as the main obstacle to help-seeking in the Arab minority population (27). Further research may be required to examine different patterns of healthcare use and the reasons for the lower use of specialist services in this minority group.
Are Patient Preferences Being Met?
The fact that the vast majority (87%) of respondents got an appointment with a specialist suggests that needs are being met. However, only around half of respondents considered the wait time offered to them to be reasonable. Waiting time is an important factor in patients’ decision-making process regarding making an appointment to see a specialist physician, and willingness to remain in the queue. Desire to see a specific doctor, and geographical proximity also play an important role in making and choosing an appointment. Older and wealthier respondents tended to have a preference for a specific doctor rather than any doctor in the field, with no difference by ethnic group. Although a small percentage of overall respondents, those who did not ultimately succeed in scheduling an appointment through the HP often resorted to private care.
Following a first visit in the public system, patients often seek out a private doctor for a second opinion. In a survey conducted in Israel, two-thirds of respondents who sought a second opinion did so in private practice, with the main reason being a belief that private physicians are more professional (28). Importantly, patients who did obtain a second opinion from a private practitioner did not report greater improvement in perceived clinical outcomes compared to those who did not.
A study in Hong Kong found that elderly patients were less willing to pay for private care, and a higher willingness to pay was reported by healthier and more affluent patients (29). In our study, age was not related to the likelihood of making an appointment with a private specialist.
Another important issue that arose in the survey is double-booking, with almost a hundred respondents reporting that they made a private appointment in parallel to the public system appointment; this may lead to missed appointments and lower efficiency in the public system. Nonattendance after scheduling was highest for gastroenterology, neurology, and dermatology, specialties with long waiting lists. In our survey, Jewish patients were more likely to double-book than Arab patients, likely related to the fact that Jews are more likely to have complementary or private health insurance, compared with Arabs. Since the survey question asked about double booking in both the public and private sector, it seems that those with additional options to schedule a specialist appointment (via the semiprivate subsidized or the private options) reported a higher rate of double-booking.
Other respondents turned to emergency services, putting added pressure on already oversubscribed EDs (30). Indeed, a US study that reported greater use of ED in patients without a regular medical care provider, proposed open-access scheduling—whereby patients can schedule their own appointment online—as a means to remove barriers to primary care, and thus reduce emergency care use (30). In the current survey, 11% of respondents who did not eventually make an appointment with a specialist reported seeking emergency care, which is similar to the results of a British study, where 13% who did not take the appointment with a GP they were offered, went to the ED (31).
Methods of Communication—Scheduling Systems
Self-scheduling, for example via an app or website, can improve the patient experience by allowing patients to have more control over which appointment they choose, and precludes the need to wait on the phone for a long time, or make multiple phone calls. Around 30% of respondents in the survey reported using these methods to make an appointment. Older patients were less likely to self-schedule, and more likely to make a phone call, have the GP make the appointment, or walk-in without an appointment. A US survey showed that many patients would like the option to book online, and the ability to book outside office hours (32). Although online scheduling exists in the Israeli system, it is not available for all healthcare providers, and could be broadened.
Limitations
Survey respondents may tend to recall events where they eventually saw a doctor, more than events where in the end they did not see a doctor. Therefore, there may be a bias toward reports of having made an appointment, which may result in the under-reporting of those who dropped out during the queueing process, especially those who did not attend after scheduling.
The survey was conducted by telephone, which may exclude some people, including those in institutions or those requiring care who may not answer the phone themselves. This method may miss some of the oldest and frailest patients who may be “super-users” of health services. Furthermore, participants were asked about appointments made in the public health system through official channels—it is possible that some people or groups approach a specialist through informal channels, either turning up at the clinic without an appointment or consulting with an acquaintance or family member.
Conclusion
The study aimed to evaluate patients’ experience in scheduling appointments for specialists within the public healthcare system, evaluate disparities, and determine to what extent patients’ needs are being met. The vast majority of respondents succeeded in making an appointment, though some groups experienced longer waits.
To the best of our knowledge, this study is unique in examining the patient journey of scheduling an appointment, starting at the point of needing to see a physician, and examining further junctions along the pathway. This information is important in identifying which patients are most at risk of missing out on treatment. In the Israeli public healthcare system, the majority of patients needing to see a community specialist were able to make an appointment. However, the most at-risk populations—older patients, ethnic minorities and those with chronic illness, may be less likely to seek treatment or to get an appointment. The most common reason for not making an appointment within the public system was long wait times, indeed around half of respondents considered the waiting time unreasonable, and 15% would consider switching health providers.
In order to truly understand the patient experience, we need to follow the whole journey from a holistic point of view, as was done in this study, starting with the need to see a specialist, and to ask the right questions along the journey about trying to schedule an appointment, making an appointment and attending. This tool could also be used to gain a better understanding of the patient experience of the appointment scheduling process in other health services, such as elective surgical procedures.
The insights gained in this study could be used to better understand the user (patient) experience in interactions with the healthcare system, in order to design services that would better suit patients’ needs and expectations.
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735221092547 for Factors Affecting the Patient Journey in Scheduling a Specialist Appointment in a Public Healthcare System by Osnat Luxenburg, Vicki Myers, Arnona Ziv, Ilya Novikov, Irena Gimpelevitch, Mor Saban, Shuli Brammli-Greenberg and Rachel Wilf-Miron in Journal of Patient Experience
Acknowledgments
With thanks to Irit Elroy and Elinore Avni, who worked at Myers-JDC-Brookdale Institute at the time of the study, for preparing and conducting the survey, and for the initial analysis of the data.
Authors’ Note: Shuli Brammli-Greenberg and Rachel Wilf-Miron contributed equally. OL, SBG, AZ, and RWM conceptualized and designed the survey, contributed to data interpretation, and reviewed and revised the manuscript; the survey was conducted under the supervision of SBG; VM performed analyses, data interpretation and wrote the first draft; IN and IG performed data management and statistical analyses; MS contributed to data interpretation and reviewed and revised the manuscript for critical content. All authors read and approved the final manuscript. The survey received ethical approval from the Myers-JDC-Brookdale Institute ethics committee. The data are available on request. Informed consent was obtained from the survey respondents for the publication of anonymized survey results.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the Ministry of Health and Myers-JDC-Brookdale Institute.
ORCID iDs: Vicki Myers https://orcid.org/0000-0001-5866-3948
Arnona Ziv https://orcid.org/0000-0003-1147-8686
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shryock T, Lee TH. Why patient experience matters more than ever [Internet]. Vol. 2020. https://www.medicaleconomics.com/view/why-patient-experience-matters-more-ever
- 3.Schmittdiel J, Selby VJ, Grumbach K, Quesenberry CP. Choice of a personal physician and patient satisfaction in a health maintenance organization. JAMA. 1997;278:1596. [PubMed] [Google Scholar]
- 4.Finkelstein SR, Liu N, Rosenthal D, Poghosyan L. When open access might not work: understanding patient attitudes in appointment scheduling. Health Care Manag Rev. 2018;43:348. [DOI] [PubMed] [Google Scholar]
- 5.Israel Ministry of Health. Rights of the insured under the National Health Insurance Law. Accessed March, 2022. https://www.health.gov.il/English/Topics/RightsInsured/RightsUnderLaw/Pages/default.aspx
- 6.Rosen B, Waitzberg R, Merkur S. Israel: Health System Review, in Health Systems in Transition. World Health Organization; 2015. [PubMed] [Google Scholar]
- 7.Central Bureau of Statistics (CBS). National expenditure on Health [Internet]. Vol. 2020. 2018. https://www.cbs.gov.il/he/mediarelease/DocLib/2019/252/08_19_252b.pdf
- 8.CBS. Selected data on health insurance and health information [Internet]. Vol. 2020. 2019. https://www.cbs.gov.il/he/publications/doclib/2018/7.%20shnatonsocietyandwelfare/st07_15x.pdf
- 9.Heinze G. A comparative investigation of methods for logistic regression with separated or nearly separated data. Stat Med. 2006;25:4216-26. [DOI] [PubMed] [Google Scholar]
- 10.Brammli-Greenberg S, Yaari I. National Consumer Health Survey 2018 [Internet]. Brookdale. 2019. https://brookdale.jdc.org.il/publication/national-consumer-health-survey-2018/
- 11.Haggerty J. Room for improvement: patients’ experiences of primary care in Quebec before major reforms. Can Fam Physician. 2007;53:1057. [PMC free article] [PubMed] [Google Scholar]
- 12.Wilf-Miron R, Novikov I, Ziv A, Mandelbaum A, Ritov Y, Luxenburg O. A novel methodology to measure waiting times for community-based specialist care in a public healthcare system. Health Policy (New York). 2020;124:805. [DOI] [PubMed] [Google Scholar]
- 13.Azzopardi-Muscat N, Sørensen K. Towards an equitable digital public health era: promoting equity through a health literacy perspective. Eur J Public Health. 2019;29:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganguli I, Orav J, Lupo C, Metlay JP, Sequist TD. Patient and visit characteristics associated with use of direct scheduling in primary care practices. JAMA. 2020;3:e209637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147-52. [PubMed] [Google Scholar]
- 16.Cameron E, Bernardes J. Gender and disadvantage in health: men’s health for a change. Sociol Health Illn. 1998;20:673. [Google Scholar]
- 17.Rendall MS, Weden MM, Favreault M, Waldron H. The protective effect of marriage for survival: a review and update. Demography. 2011;48:481-506. [DOI] [PubMed] [Google Scholar]
- 18.Sirois FM, Owens J. A meta-analysis of loneliness and use of primary health care. Health Psychol Rev. 2021;1. [DOI] [PubMed] [Google Scholar]
- 19.Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. 2015;105:1013-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meeks KAC, Freitas-Da-Silva D, Adeyemo A, Beune EJAJ, Modesti PA, Stronks K, et al. Disparities in type 2 diabetes prevalence among ethnic minority groups resident in Europe: a systematic review and meta-analysis. Intern Emerg Med. 2016;11:327-40. [DOI] [PubMed] [Google Scholar]
- 21.Garcia-Garcia G, Jha V. Chronic kidney disease in disadvantaged populations. Transplantation. 2015;99:13. [DOI] [PubMed] [Google Scholar]
- 22.Liu L, Núṅez AE, An Y, Liu H, Chen M, Ma J, et al. Burden of cardiovascular disease among multi-racial and ethnic populations in the United States: an update from the National Health Interview Surveys. Front Cardiovasc Med. 2014;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jaffe A, Giveon S, Wulffhart L, Oberman B, Baidousi M, Ziv A, et al. Adult Arabs have higher risk for diabetes mellitus than Jews in Israel. PLoS One. 2017;12:e0176661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baron-Epel O, Garty N, Green MS. Inequalities in use of health services among Jews and Arabs in Israel. Health Serv Res. 2007;42:1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chernichovsky D, Basharat B, Bevers L, Sharon C. Health of the Arab Population in Israel. Taub Center; 2017. [Google Scholar]
- 26.Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23:325-48. [DOI] [PubMed] [Google Scholar]
- 27.Daeem R, Mansbach-Kleinfeld I, Farbstein I. Barriers to help-seeking in Israeli Arab minority adolescents with mental health problems: results from the Galilee study. Isr J Heal Policy Res. 2019;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shmueli L, Davidovitch N, Pliskin JS, Hekselman I, Balicer RD, Greenfield G. Reasons, perceived outcomes and characteristics of second-opinion seekers: are there differences in private vs. public settings? BMC Health Serv Res. 2019;19:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu S, Yam CHK, Huang OHY, Griffiths SM. Willingness to pay for private primary care services in Hong Kong: are elderly ready to move from the public sector? Health Policy Plan. 2013;28:717-29. [DOI] [PubMed] [Google Scholar]
- 30.Rust G, Ye J, Baltrus O, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access impact on adult use of emergency department services. Arch Intern Med. 2008;168:1705-10. [DOI] [PubMed] [Google Scholar]
- 31.NHS. GP patient survey [Internet]. Vol. 2020. 2020. https://www.gp-patient.co.uk/analysistool
- 32.Patient Pop. Survey reveals patients want online appointment booking [Internet]. Vol. 2020. https://www.patientpop.com/blog/healthcare-website/online-scheduling-statistics-healthcare/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735221092547 for Factors Affecting the Patient Journey in Scheduling a Specialist Appointment in a Public Healthcare System by Osnat Luxenburg, Vicki Myers, Arnona Ziv, Ilya Novikov, Irena Gimpelevitch, Mor Saban, Shuli Brammli-Greenberg and Rachel Wilf-Miron in Journal of Patient Experience