Abstract
Introduction
As the global number of geriatric hip fracture cases continues to proliferate, a newly developed orthogeriatric co-management multidisciplinary care model has been implemented since November 2018 to meet further increases in demand. Our objective was to evaluate the effectiveness of the new pathway in improving the clinical outcomes of fragility hip fractures.
Methods
The data of geriatric hip fracture patients from 1 April 2018 till 30 October 2018 was collected as the conventional orthopaedic care model (pre-orthogeriatric care model) to compare with data from the orthogeriatric co-management model, 1 Feb 2019 till 31 August 2019. Clinical outcomes were analyzed between the groups, with the efficiency of the programme reflected in the total length of stay in acute and convalescent hospitals.
Results
194 patients were recruited to the conventional group and 207 were recruited to the orthogeriatric group, 290 patients (72.3%) were female. The mean (SD) patient age was 84.2 (7.9) years. The median length of stay in the acute and rehabilitation hospitals decreased by 1 day and 2 days, respectively (P=.001). The orthogeriatric group was associated with a higher Modified Barthel Index score on discharge from the rehabilitation hospital and more patients in the orthogeriatric collaboration group received osteoporosis medication prescription within one year after the index fracture. There was no difference in the 28-days unplanned readmission rate, complication rate, mortality rate or Elderly Mobility Scale scores on discharge from the rehabilitation hospital between the two groups.
Conclusion
Orthogeriatric collaboration has been proven to be effective in terms of a decreased length of stay in both the acute and the rehabilitation hospitals.
Keywords: orthogeriatric, multidisciplinary, hip, fracture, geriatric, intervention
Introduction
As the world’s population is ageing, geriatric hip fractures have truly become a worldwide health concern. In our territory with a population of over 7 million, approximately 5000 hip fractures are operated on each year. The trend is increasing in the past five years; a phenomenon also mirrored in other parts of the world. Even with aggressive surgical treatment, morbidities and complications are still common, showing the inadequacy of the present care model offered primarily by orthopaedic surgeons.
Solely fixing osteoporotic hip fractures is inadequate with regards to the standard of management in geriatric fragility fractures. To provide quality service to our older adult patients with proven cost-effectiveness, we must collaborate with the available expertise involved. The concept nowadays is not just multidisciplinary but interdisciplinary, focusing on collaboration, co-management and patient co-ownership.
There are works of literature in which the use of a multidisciplinary clinical pathway shortened hospital stay by 6.1 days in the acute setting with improved clinical outcomes, including pneumonia. 1 The average cost of manpower also decreased per hip fracture case. An ageing population presents with multiple comorbidities and polypharmacy problems following operation. These patients require considerable support both in the early postoperative period as well as after discharge, to prevent deterioration of their physical and mental health after hip fracture, as medical and surgical problems in the postoperative period can lead to repeated hospital readmissions and prolonged hospital stays.
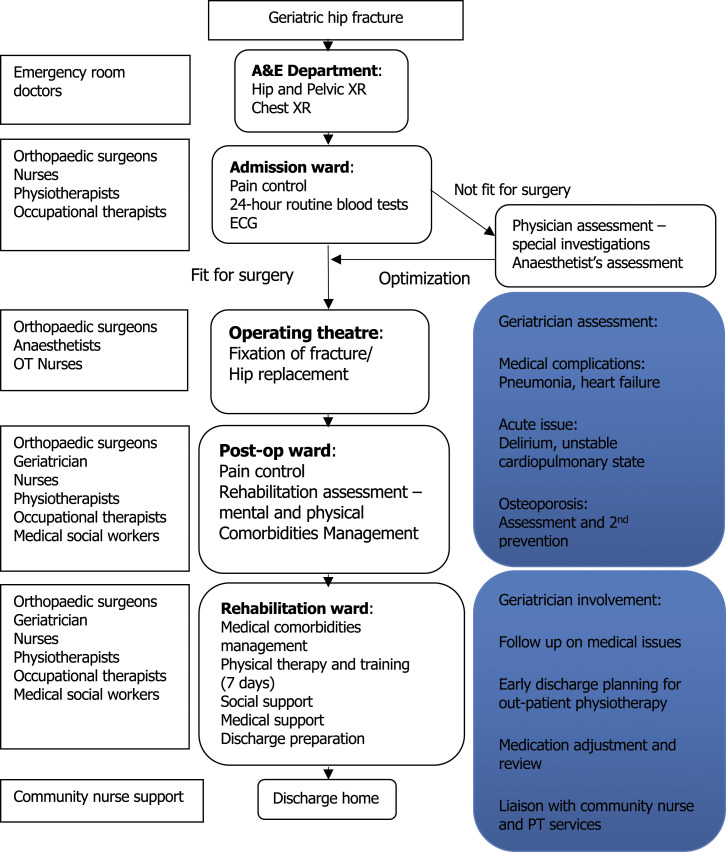
International guidance from organizations such as the British Orthopaedic Association, 2 National Institute for Health and Care Excellence (NICE), 3 National Osteoporosis Society, and Age UK 4 all suggest a model for hip fracture care would be best to start with orthogeriatric services focusing on achieving optimal recovery after hip fracture. Geriatrician input in the acute and rehabilitation phase becomes a logical and imminent step to improve the whole management process of hip fracture patients. The aim of the study was to evaluate the effectiveness of an orthogeriatric multidisciplinary care model in improving clinical outcomes for fragility hip fractures, implemented in late 2018. Through collaborative orthogeriatric care with active geriatrician involvement in daily management in both acute and rehabilitation phases (Figure 1), we hypothesized there to be an improvement in clinical and functional outcomes, such as mortality, complications and osteoporosis management, and a decrease in the length of hospitalization.
Figure 1.
Orthogeriatric collaboration clinical pathway flowchart.
Methodology
Study Design
This was a prospective cohort study looking into two groups of patients treated by the same orthopaedic trauma team before and after the implementation of an orthogeriatric co-management model. From November 2018 onwards, the orthogeriatric co-management model was implemented in our department, which consists of one acute hospital (Queen Mary Hospital) and two rehabilitation hospitals (Fung Yiu King Hospital and Maclehose Medical Rehabilitation Hospital). The data of geriatric hip fracture patients from 1 April 2018 till 30 October 2018 was collected as the conventional orthopaedic care model. After finalizing details of the co-management model and allowing for approximately one month of adjustment time, the data of the hip fracture patients from 1 Feb 2019 till 31 August 2019 was collected as the orthogeriatric collaboration cohort. The two data sets were then compared and analysed.
Ethical approval was sought and satisfied (HKU/HA HKW IRB Reference number: UW 16-301.
Intervention
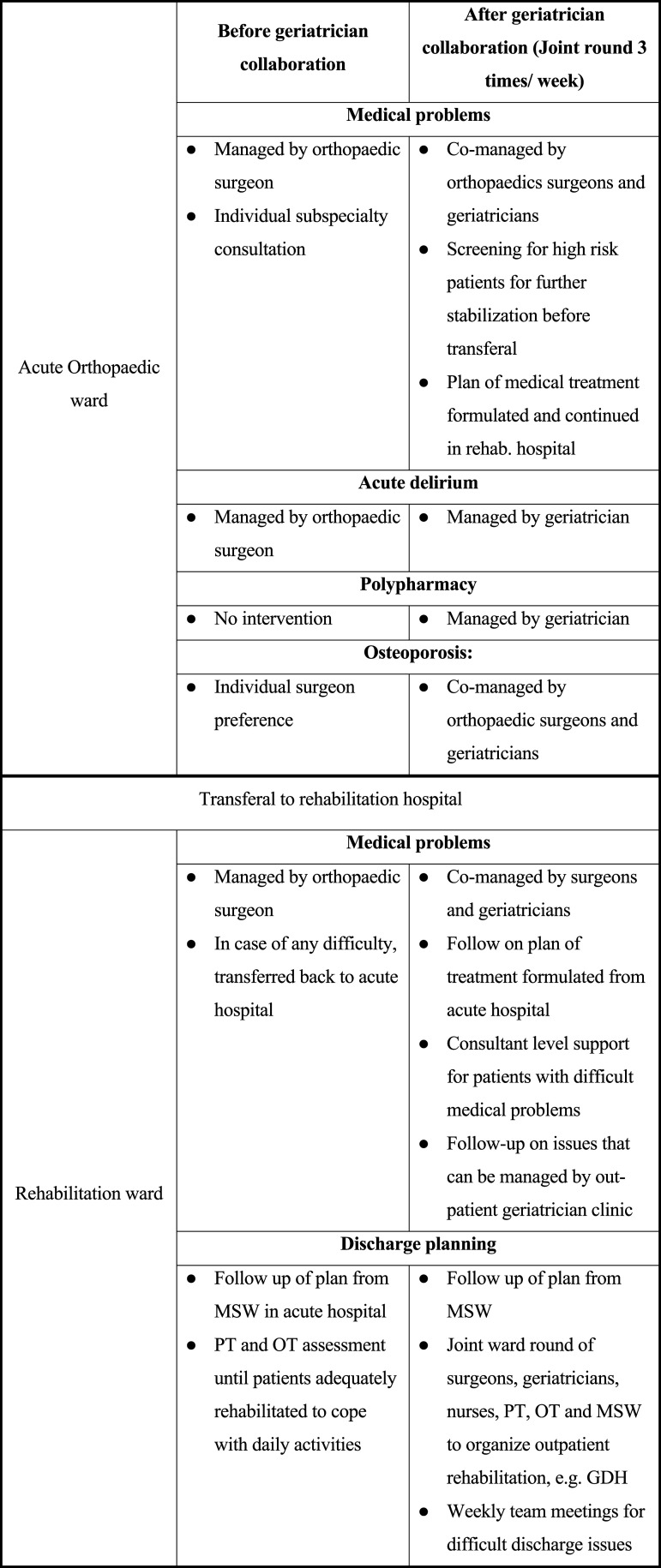
For a summary of the differences between the conventional and orthogeriatric care models, see Figure 2. In the conventional model, patients were admitted to an acute orthopaedic ward where an orthopaedic surgeon was responsible for managing care and treatment of all medical problems, including both orthopaedic and non-orthopaedic–related complications. Medical and geriatric input was only available upon ad hoc request and these interdisciplinary referrals occurred after the complications had already arisen. For semi-urgent referrals, the patients would be reviewed by the physician after 2 days, leading to delays in management and prolonged length of stay.
Figure 2.
Orthogeriatric co-management comparison.
The resources in the rehabilitation hospital were more limited than in the acute hospital in terms of nursing monitoring, medical support and laboratory support. Therefore, all patients needed to be optimized before transferral. This included stable respiratory status without supplemental oxygen support, stable haemodynamics and fluid status, near-normal electrolytes balance, and all acute medical problems needed to be thoroughly worked up, with care management plans in place. This created a delay between postoperation and patient discharge from the acute hospital to the rehabilitation hospital. In cases where patient health deteriorated in the rehabilitation hospital, the patient would be readmitted back to the acute hospital for closer monitoring, investigation and co-management with other subspecialities as required. 5
The interventional model differed in the addition of a geriatrician during the postoperative phase, who co-managed the patient in both the acute and rehabilitation hospital. An orthogeriatric speciality ward was set up and implemented in Nov 2018 to concentrate resources and manpower. The new system championed collaboration between the orthopaedic surgeons and the geriatricians. In the acute ward, cases were co-managed during combined ward rounds which occurred 3 times per week. The geriatrician actively reviewed all hip fracture patients to allow prompt diagnosis and management of medical complications, optimization of pain control and monitoring of comorbidities.
One important improvement with the new geriatrician support was that transferral of patients from the acute hospital to the rehabilitation hospital was more expedited and streamlined. Since this collaboration extended to our rehabilitation hospital where the same team of geriatricians continued follow-up, patients did not need to wait for all their medical problems to be solved before the transferral. The fitness for transferral was assessed by the geriatricians during their regular rounds in the acute hospital.
In the rehabilitation hospital, weekly orthogeriatric ward rounds allowed the orthopaedic surgeon and geriatrician to confer best care plans for the patients. Those with medical problems who did not require intensive nursing monitoring could be managed by the geriatrician in the rehabilitation hospital, instead of being transferred back to the acute hospital, to help decrease unnecessary readmissions. This contrasted with the conventional care model, where the patients received ad hoc geriatrician support only when medical complications had already occurred, and transferral of patients back to the acute hospital was common for medical consultations.
On discharge from the rehabilitation hospital, geriatric specialist clinic follow-up would be arranged for the patients. Osteoporosis medication prescriptions were continued by the geriatricians and monitored in the clinic follow-up.
Our orthogeriatric collaboration model did not involve preoperative optimization. Our existing geriatric hip fracture clinical pathway included a fast track preoperative cardiac assessment, as cardiac problems (eg incidental systolic heart murmur) were noted to be the main cause of delay for preoperative preparation in the past. 6
There was no change in pain management and deep vein thrombosis prophylaxis protocol between the two groups. Fascia iliaca compartment block was given to all eligible patients on admission. A multimodal analgesic regime was adopted which included regular acetaminophen, weak opioid, cox-2 inhibitors and strong opioid for breakthrough pain. Spinal anaesthesia was chosen for most patients to facilitate postoperative pain control. For deep vein thrombosis prophylaxis, patients are mobilized on day 1 post operation after drain removal with the help of the physiotherapists. Chemical deep vein thrombosis prophylaxis (subcutaneous enoxaparin) was used in high risk patients.
Subjects
Participants were recruited from the Department of Orthopaedics and Traumatology, Queen Mary Hospital located in Hong Kong. All patients had hip fracture confirmed by pelvis and hip x-ray (anteroposterior and lateral view). The data of geriatric hip fracture patients for the two periods: 1 April 2018–30 October 2018 and 1 Feb 2019–31 August 2019 were collected prospectively.
Inclusion and Exclusion Criteria
Inclusion criteria were age more than or equal to 65; diagnosis of acute (time of injury within 14 days) isolated hip fracture patients from low energy trauma. Exclusion criteria included high-energy trauma, pathological fractures, multiple trauma, or old fractures that occurred more than 2 weeks ago.
Outcome Assessment and Data Collection
Demographics of the patients, including age, sex, original placement where the patients lived before admission, pre-morbid mobility and walking aids, were prospectively collected. Other data including the number of comorbidities, classification of the fractures, surgery types, Charlson comorbidity index, preoperative haemoglobin level, the postoperative requirement of blood transfusion and also placement arrangements were all collected.
The clinical outcomes that we used to compare the effectiveness of the pathway included:
- 1. Length of hospital stay
- a. Pre-operative waiting time
- b. Average and median of acute hospital length of stay
- c. Average and median of rehabilitation hospital length of stay
- d. Extended length of stay (either pre-operative waiting time >2 days OR postoperative length of stay >5days)
2. Mortality rates including 30-day mortality, 3-month mortality, 6-month mortality and 1-year mortality.
- 3. Functional recovery upon discharge from hospital:
- a. Elderly Mobility Scale (EMS)
- b. Modified Barthel Index (MBI)
4. Medical and surgical complication rates
- 5. Development of delirium state
- a. Diagnosed with CAM-score or clinically diagnosed in the chart at any time during admission
- 6. To evaluate the effect on rehabilitation
- a. Discharge destination
7. Prescription of anti-osteoporotic management
- 8. Unplanned hospital readmission rates
- a. Reasons for readmission
The hip fracture patients admitted under the orthogeriatric multidisciplinary care model were compared with those without this model. Based on the results of literature examining integrated orthogeriatric care and our local data, 1 we estimated a difference of 1.4 days in the length of stay between the intervention and the control group. The type-1 (alpha) error was set at .05 and type-II (beta) was set at .8. These data suggested that at least 170 patients should be recruited from each group. Since about 400 fragility hip fracture patients are admitted each year, expecting a drop-out rate of 5–10%, we allowed for 6–7 months to recruit for each group of hip fracture patients.
Statistical Analysis
The Shapiro–Wilk test was used to assess the assumption of normality, and data were expressed as mean (SD) or as median (interquartile range, IQR), according to their distribution. Percentages were compared using the chi-square test, and continuous data via the Student t-test or Mann–Whitney test, as appropriate.
The log-rank test was used to compare the Kaplan–Meier estimate curves for mortality. Adjusted analyses for the outcome of 1-month, 3-month, 6-month and 1-year mortality were performed using logistic regression models, considering sex, age, pre-operative waiting time, Charlson comorbidity Index scores (CCI), pre-operative haemoglobin level, pre-operative albumin level and pre-morbid residence as confounders. These confounders, all of which have been shown in previous literature as factors that may influence hip fracture mortality.7-13 Cox proportional hazard model of mortality was calculated taking into account the above covariates.
The log-rank test was used to compare the Kaplan–Meier time-to-event analysis for length of stay, with deaths being right-censored in the analysis.
Post hoc adjusted analyses for the outcome of length of stay were performed using Cox regression models to estimate hazard ratios (HRs) with corresponding 2-sided 95% CIs. Age, type of fracture (pertrochanteric fracture and neck of femur fracture), preoperative waiting time and Charlson comorbidity index scores (CCI) were listed as potential confounders, as these had been shown by Castelli et al. and Craigven et al. to potentially affect length of stay.14,15 Unstandardized coefficient (B) and 95% confidence intervals (95% CI) were estimated using the linear regression to adjust for possible baseline difference for discharge functional score, namely MBI and EMS. The covariates included rehabilitation hospital admission functional score and Abbreviated Mental Test score on admission to acute hospital (AMT). A logistic regression was performed to ascertain the effects of orthogeriatric group, age, sex and CCI on the likelihood that participants have any medical complications.
Results
Demographics
The demographics are summarized in Table 1. Of the 401 patients eligible for participation, 194 were recruited to the conventional group and 207 were recruited to the orthogeriatric group. The mean (SD) age of the patients was 84.2 (7.9) years. 290 patients (72.3%) were female. 219 cases in the study (54.6%) were femoral neck fractures and 182 (45.4%) were pertrochanteric fractures.
Table 1.
Demographics of geriatric fracture hip patients in the conventional and orthogeriatric groups.
| Conventional (n=194) | Orthogeriatric (n=207) | P | |
|---|---|---|---|
| Age, mean (SD), y | 84.8 (7.6) | 83.6 (8.2) | .17 |
| Sex, no. (%) | .70 | ||
| Men | 52 (26.8) | 59 (28.5) | |
| Women | 142 (73.2) | 148 (71.5) | |
| Abbreviated mental test on admission; median (IQR) | 5.1 (5.8) | 7 (8.1) | .08 |
| Rehabilitation hospital admission Modified Barthel Index; median (IQR) | 48 (24) | 49 (27) | .06 |
| Pre-morbid residence (%) | |||
| Old age home | 53 (27.3) | 38 (18.4) | .04 |
| Home | 141 (72.7) | 169 (81.6) | |
| Pre-morbid mobility (%) | |||
| Unaided | 61 (31.4) | 69 (33.3) | .58 |
| With aids | 121 (62.4) | 124 (59.9) | |
| Chairbound | 11 (5.7) | 10 (4.8) | |
| Bedbound | 1 (.5) | 4 (1.9) | |
| Fracture site; n (%) | .13 | ||
| Neck of femur | 97 (50.8) | 120 (58.8) | |
| Pertrochanteric | 94 (49.2) | 84 (41.2) | |
| Surgery performed; n (%) | |||
| Replacement | 65 (33.5) | 84 (40.6) | .15 |
| Fracture fixation | 129 (66.5) | 123 (59.4) | |
| Charlson comorbidity index; median (IQR) | 2 (5) | 2 (5) | .13 |
| Preoperative haemoglobin level (g/dL); mean +/− SD | 11.4 +/− 1.8 | 11.6 +/− 1.9 | .39 |
| Postoperative blood transfusion (number of packed cells); mean +/− SD | .7 +/− 1.0 | .5 +/− 0.9 | .02 |
Length of Stay
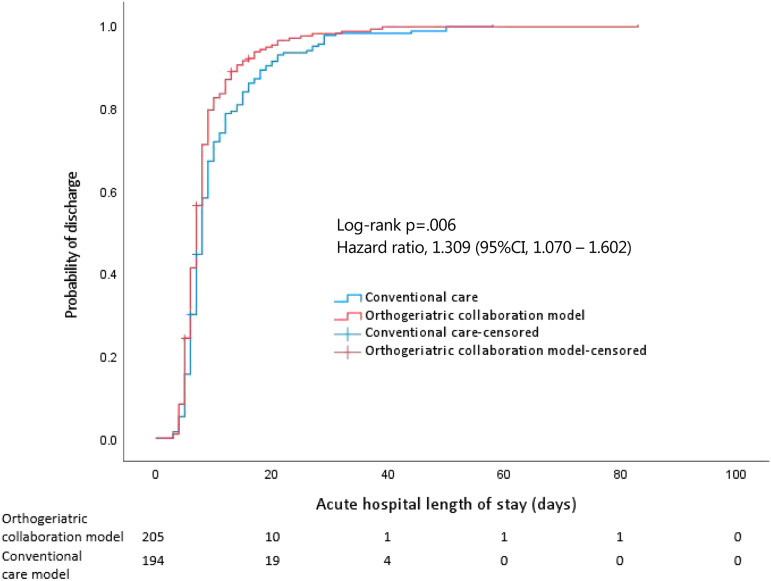
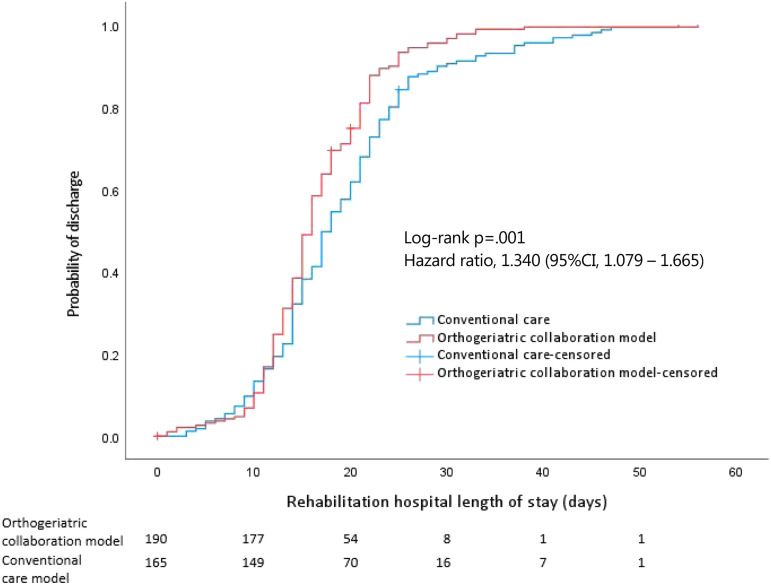
Extended LOS, defined as either preoperative LOS of more than 2 days, or postoperative LOS of more than 5 days, saw a dramatic significant reduction following implementation of the new care model. There were more patients with extended LOS in the conventional group vs orthogeriatric collaboration (64.4% vs 39.1%; difference 25.3% [95% CI, 15.838%–34.767%]; P<.001). Additionally, the new care model resulted in significant differences between both groups in the median (interquartile range [IQR]) acute hospital length of stay (LOS) (conventional group (8.0 [4–12] days) vs orthogeriatric collaboration group (7.0 [3–11] days)) (log-rank P=.001; unadjusted HR for hospital discharge, 1.284 [95% CI, 1.053–1.566]; P = .01; adjusted HR, 1.309 [95% CI,1.070–1.602]; P=.009) (Figure 3). Cox proportional hazards model of acute hospital LOS showed the effect of age (adjusted HR=.985, [95% CI, .972–.997]; P=.016) and preoperative waiting time (adjusted HR=.845, [95% CI, .741–.964]; P=.012) were significant. The median (IQR) rehabilitation hospital LOS was also significantly different between both groups (conventional group (18 [9–27] days) vs orthogeriatric collaboration group (16.0 [9–23] days)) (log-rank P=.001; unadjusted HR for hospital discharge, 1.391 [95% CI, 1.124–1.723]; P=.002; adjusted HR, 1.357 [95% CI, 1.095–1.682]; P=.005) (Figure 4). Cox proportional hazards model of rehabilitation hospital LOS showed trochanteric fracture was more likely in long-stayers (adjusted HR=1.340, [95% CI, 1.079–1.665]; P=.005). There was no significant difference between both groups for the median (IQR) of the preoperative LOS (1 [0–2] day vs 1 [0–2] day) (log-rank P=.38). The difference in acute hospital LOS between the two groups was a result of improvement in postoperative LOS. There was a significant difference between the median (IQR) of the postoperative LOS for conventional group (6.0 [2–10]) and orthogeriatric collaboration group (4.0 [1–7]) (log-rank P<.001).
Figure 3.
Kaplan–Meier survival curve of hospital discharge against length of stay in the acute hospital. Numbers below denote the number of patients ‘at risk’ in each group.
Figure 4.
Kaplan–Meier survival curve of hospital discharge against length of stay in the rehabilitation hospital. Numbers below denote the number of patients ‘at risk’ in each group.
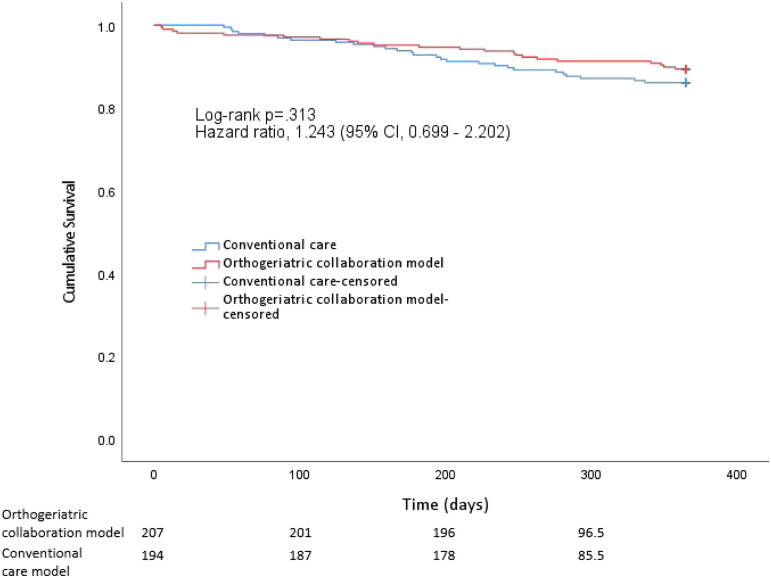
Mortality
An important clinical outcome that we measured is the mortality rate (Figure 5). There were no significant differences between the orthogeriatric collaboration group and conventional group in 30-day mortality (1.9% vs 0%; difference, 1.9% [95% CI, .0%–3.8%]; P=.99), 3-month mortality (2.9% vs 3.1%; difference, .2% [95% CI, −3.2% to 3.6%]; P=.56), 6-month mortality (4.8% vs 7.2%; difference, 2.4% [95% CI, −2.4%–7.3%]; P=.24), and 12-month mortality (10.6% vs 13.9%; difference, 3.3% [95% CI, −3.1%–9.7%]; P=.24) after adjusting for covariates.
Figure 5.
Kaplan–Meier survival curve of 1-year mortality in each group. Numbers below denote the number of patients ‘at risk’ in each group.
Cox proportional hazard model of mortality showed the effect of CCI (adjusted HR=1.1, [95% CI, 1.1–1.2]; P<.001) and pre-operative albumin level (adjusted HR=.9, [95% CI, .8–1.0]; P=.001) were significant. For orthogeriatric co-management, there was no evidence of a benefit in survival (adjusted HR=.8, [95% CI, .5–1.4]; P=.81).
Functional Recovery
The median (IQR) MBI recorded before discharge from the rehabilitation hospital for the orthogeriatric collaboration and control group were 81 (27) and 63.5 (28), respectively, (P<.001). The median (IQR) of EMS recorded before discharge from the rehabilitation hospital for orthogeriatric collaboration and control group were 12 (8) and 9 (8), respectively, (P=.07).
Complications
Regarding adverse outcomes, there was a significant reduction in the number of chest infections in the orthogeriatric group (5.3% vs 10.8%, difference, 5.5% [95% CI, .2%–10.9%], P=.04). There were no statistically significant differences between the two groups in other complications or presence of any medical complications; however, wound complications and blood transfusions both saw decreases which reached near-significance (Table 2).
Table 2.
Analysis of adverse outcomes between the conventional and orthogeriatric group.
| Adverse Outcomes No. (%) | Conventional (n=194) | Orthogeriatric (n=207) | Total (n=401) | P | |
|---|---|---|---|---|---|
| Wound complications | |||||
| Yes | 14 (7.2) | 7 (3.4) | .09 a | ||
| No | |||||
| Surgical complications (except wound complications) | |||||
| Yes | 3 (1.5) | 5 (2.4) | .53 a | ||
| No | |||||
| Postoperative blood transfusion (D0-D5) | |||||
| Yes | 73 (37.6) | 61 (29.5) | 134 (33.4) | .08 a | |
| No | 121 (62.4) | 146 (70.5) | 267 (66.6) | ||
| Chest infection | |||||
| Yes | 21 (10.8) | 11 (5.3) | 32 (8) | .04 a | |
| No | 173 (89.2) | 196 (94.7) | 369 (92) | ||
| Urinary tract infection | |||||
| Yes | 41 (21.1) | 43 (20.8) | 84 (20.9) | .93 a | |
| No | 153 (78.9) | 164 (79.2) | 317 (79.1) | ||
| Acute retention of urine | |||||
| Yes | 34 (17.5) | 32 (15.5) | 66 (16.5) | .58 a | |
| No | 160 (82.5) | 175 (84.5) | 335 (83.5) | ||
| Delirium | |||||
| Yes | 35 (18.0) | 28 (13.5) | 63 (15.7) | .21 a | |
| No | 159 (82.0) | 179 (86.5) | 338 (84.3) | ||
| Gastrointestinal bleeding | |||||
| Yes | 0 (0) | 3 (1.4) | 3 (.7) | .09 a | |
| No | 194 (100) | 204 (98.6) | 398 (99.3) | ||
| Renal failure | |||||
| (Stage 2 or stage 3) 44 | |||||
| Yes | 19 (9.8) | 23 (11.1) | 42 (10.5) | .67 a | |
| No | 175 (90.2) | 184 (88.9) | 359 (89.5) | ||
| Any medical complications | |||||
| Yes | 72 (37.1) | 75 (36.2) | 147 (36.7) | .86 a | |
| No | 122 (62.9) | 132 (63.8) | 254 (63.3) | ||
aChi-Square Goodness of Fit Test.
Post hoc adjusted analysis with binary logistic regression model (dependent variable: presence of any medical complications; covariates: orthogeriatric group, age, sex and CCI) was statistically significant, χ2 (3) = 26.857, P< .001. Increasing age (Exp(B) .94 [95% CI, .91–.97], P<.001) and CCI (Exp(B) .94 [95% CI, .90–.98], P=.007) was associated with an increased likelihood of exhibiting medical complications, however, the orthogeriatric group was not associated with a likelihood of exhibiting medical complications (Exp(B) 1.06 [95% CI, .69–1.61], P=.81).
Osteoporosis
Enhanced secondary prevention of fracture is one of our goals in orthogeriatric collaboration. Bisphosphonate prescription saw a dramatic increase in the orthogeriatric group, from just 12.9%, to an overwhelming 66.7% (difference, 53.8% [95% CI, 45.8%–61.7%], P<.001) (Table 3). There was no difference in the number of subsequent fractures within 1 year of index fracture between the orthogeriatric group and conventional group (1.4% vs 3.1%, difference, 1.6% [95% CI, −1.3% to 4.6%], P=.27).
Table 3.
Osteoporosis medication prescription within one year from index fracture.
| Conventional (n=194) | Orthogeriatric (n=207) | Total (n=401) | P | ||
|---|---|---|---|---|---|
| Started bisphosphonate within 1 year of index fracture | |||||
| Yes | 25 (12.9) | 138 (66.7) | 163 (40.6) | <.001 a | |
| No | 169 (87.1) | 69 (33.3) | 238 (59.4) | ||
| Subsequent fracture within 1 year of index fracture | |||||
| Yes | 6 (3.1) | 3 (1.4) | 9 (2.2) | .27 a | |
| No | 188 (96.9) | 204 (98.6) | 392 (97.8) |
aChi-Square Goodness of Fit Test.
Discharge Destination From Rehabilitation Hospital
For the 246 patients who lived at home before the injury, there was no statistically significant difference between the orthogeriatric collaboration and the conventional group in the proportion of patients being able to go back to their original placement (69.1% vs 71.0%; difference, 2.0% [95% CI, −9.6 to 13.5]; P=.74) (Table 4).
Table 4.
Destination upon discharge from rehabilitation hospital
| Destination upon Discharge from Rehabilitation Hospital (Pre-Morbid Residence = Home) | Conventional (n=107) | Orthogeriatric (n=139) | Total (n=246) | P |
|---|---|---|---|---|
| Old aged home | 31 (29.0) | 43 (30.7) | 74 (30.1) | .74 |
| Home | 76 (71.0) | 96 (69.1) | 172 (69.9) |
Readmission Rates
Concerning hospital unplanned readmission rate, for the conventional group, the total 28-day readmission rate was 14.9%. This decreased to 12.6% in the orthogeriatric group. Moreover, readmission due to medical reasons decreased from 11.3% (within the conventional group) to 8.2% (within the orthogeriatric collaboration group), whereas readmission due to orthopaedic reasons increased slightly from 3.6% (within the conventional group) to 4.3% (within the orthogeriatric collaboration group). However, these changes did not reach statistical significance (P=.55).
Discussion
Geriatric fragility fractures are the major concern in our orthopaedics community nowadays, 16 with hip fractures making up a significant portion. In addition to the escalating number of hip fractures, the age of the average patient is also increasing year-on-year. The growing prevalence of osteoporotic bones not only gives rise to an increase in the technical difficulty of fixing the fractures, but also the number and severity of the comorbidities in advancing age presents a challenge to the anaesthetists and physicians before and after the surgical intervention. The urgency for improved management of geriatric fragility fractures has been internationally recognized, with several multidisciplinary care models involving geriatrician and orthopaedic surgeon co-management having been developed to address the need for higher standards of care for these patients. 17
Length of Stay
A key finding of our study is the decreased length of stay in both acute and rehabilitation hospitals. In the conventional model, the geriatric consultative service is on request of the in-charge orthopaedic surgeon, hence there is a time lag from sending the request, to the patient being seen by the geriatrician. This time lag is circumvented in the integrated care model as the patients are co-managed by both the orthopaedic surgeon and the geriatrician. As joint ward rounds are made up to 3 times weekly, the increased frequency allows for improved monitoring of patients, earlier detection of medical problems and timely intervention. Individual case needs are identified and met more quickly. Furthermore, the orthopaedic surgeon and geriatrician deliberate the optimal plan of medical treatment in unison, resulting in more consistency than compared to when individual orthopaedic surgeons were managing patient cases in isolation. Patients were transferred from acute hospital to rehabilitation hospital earlier because of the enhanced geriatrician support in the rehabilitation hospital. We also saw a significant improvement in extended LOS. The number of severe outliers was reduced due to the measures of the new orthogeriatric care model, allowing for more consistent quality of care to be provided to patients, while curbing excessive resource use.
Care must be taken regarding early patient discharge. Discharging patients prematurely would result in lower length of hospital stay, but may be detrimental to patient health. Therefore, it is important in this regard to ensure proper rehabilitation is achieved prior to patient discharge. However, as our results indicated non-significant differences in unplanned readmission rates and mortality between the conventional and interventional group, it is likely that the observed reductions in length of stay were in fact due to the new measures which eliminated unnecessary waiting, delays in decision making and streamlined the rehabilitation process.
Functional Recovery
Due to changes in the structure of society and better medical care, more people in advanced age are still active in their role in the family and even in society. The quality of life for these patients in the recent decade is no longer the same as those 30 years ago. These patients need a safe, quick, and efficient recovery to return to their normal lives after the injuries. With this upcoming challenge, a multidisciplinary management programme could help to cope with this efficiently, as shown in recent literature.6,18-20
We saw no difference in EMS scores, however there was a significant difference between the two groups for MBI scores. Other studies also saw improved functional outcomes following implementation of an orthogeriatric model. Adunsky et al. 21 saw statistically significant improvements to patient Functional Independence Measure (FIM) motor and cognitive scores, concluding that successful rehabilitation was twice as high in their interventional group. In their accelerated rehabilitation study, Cameron et al. saw increased ADL scores and a significant reduction in length of stay, 22 which is analogous to our own findings. In our model, the geriatrician facilitated transfer of patients to the rehabilitation hospitals, which significantly reduced length of stay. This helped to promote functional recovery, as prolonged bed rest and patient immobility is known to be associated with functional decline in ADL and increased complications and mortality.23-26 While the results differ within the wider literature,27-30 in our model, accelerated rehabilitation, monitoring and management of medical complications by the geriatrician and discharge planning during the rehabilitation phase all led to the observed significant increase in functional recovery for our patients.
Mortality
While we observed a decreasing trend for 3-, 6- and 12-month patient mortality between the conventional and interventional group, the results were not significant. Despite concerns that shortened length of stay may jeopardize the quality of patient care, this proved not to be true in our study, as it was noted that our 1-year mortality rate is not inferior to the conventional group and is also lower than reported data in the literature. 31 Jiang et al reported the clinical outcomes of 1057 geriatric hip fracture patients. Both the 30-day mortality (3% vs 1%) and 12-month mortality (14.4% vs 12%) were slightly higher than our cohorts. 32 There was an observed 1.9% increase in 30-day mortality for the orthogeriatric group. We attribute this non-significant difference to chance. Totalling 4 patients, the low incidence would cause the resulting percentage to seem a more concerning number than it is in context.
It is apparent from the wider literature that the effect an orthogeriatric pathway has on mortality remains unclear. In a literature review comparing 13 studies, Mukherjee et al. 33 concluded that while there was overall merit in favour of orthogeriatric care models, the effect on mortality in particular was inconsistent. Also, since our power analysis was calculated based on length of stay, we are unable to decisively conclude whether the study was too underpowered to detect changes in mortality, or whether there truly was no significant difference. However, our results match the sentiment in the wider literature; that the effect is ambiguous. While several papers confirm similar outcomes to our study, that is, no effect on mortality,34-37 other papers present a contrasting view,38-41 with some even reaching statistical significance. 41 The effect, if any, is usually more prevalent on short term mortality than long term, this may be due to patients no longer receiving the improved geriatric care after discharge, 42 and can be explained by improvements in the management of medical problems or due to shorter delays in surgery. In any case, all P values for differences in mortality in our study were not significant, nor were they largely divergent. There were also no significant differences in patient demographic between the groups.
Osteoporosis
A previously identified weakness in the conventional geriatric hip fracture programme was the lack of formal osteoporosis management in the pathway. A more holistic approach to patients with hip fractures is required and this has proven its value in the literature. 43 In the new orthogeriatric collaboration model, geriatricians evaluate and initiate osteoporosis treatment while the patient is still in the rehabilitation hospital. Patient follow-up of osteoporosis treatment is continued, following discharge to the geriatric clinic, where education programmes and fall prevention are initiated by the nurses. Although we saw positive effects in the reduction of subsequent fractures within 1 year of index fracture, this value did not reach significance. However, we anticipate the improvements that the increased osteoporosis management will bring to become more apparent over a longer time period.
Complications
There were no significant differences between the two groups in the occurrence of adverse outcomes, except for chest infections. Incidences of postoperative blood transfusion was found to be insignificant between the groups, however the mean number of packed cells for each transfusion saw a significant reduction. This can be explained by increasing awareness of blood management principles, whereby a more restrictive approach to transfusion was advocated to decrease unnecessary transfusion.
A reduction in wound complications was observed but not reaching statistical significance. From the inclusion of a geriatrician in the interventional model, both the detection and overall management of medical problems may be improved. However, we postulate that the occurrence of these complications is more related to underlying patient factors such as age, sex and presence of comorbidities, and less by patient treatment pathways. This was confirmed by post hoc regression analysis that showed only age and CCI were associated with the likelihood of the presence of medical complications.
Limitations
There are several limitations to our study. Firstly, this study is a prospective cohort study without randomization, thus there are confounding factors present that cannot be eliminated. Nevertheless, the patients in the 2 cohorts are comparable concerning their basic demographics. Another limitation is that both cohorts consist of only half-year data. The collection of more data would allow for better comparison between the two models, especially for the secondary outcomes.
When recruiting for our study sample, only hip fracture patients who had received surgical intervention were included. The majority of patients in our centre undergo operative treatment; however, non-operative treatment is a known risk factor for increased complications, mortality and length of stay. Hence, we did not include patients treated conservatively in our study, which may have affected the results.
Finally, the statistics obtained for medical complications such as UTI, delirium and pneumonia rely on medical notes being systematically documented, which may be lost to the turbulence of the hospital environment, resulting in understated values for these factors.
Conclusions
Geriatric hip fractures are increasing and they will become the major burden to our health care system. A multidisciplinary orthogeriatric collaboration hip fracture clinical pathway is effective in managing this problem. The pathway not only shortens the total length of stay in acute and rehabilitation hospitals, but it also improves the functional outcomes of the patients.
Acknowledgements
The authors would like to express their special thanks of gratitude to the Performance Office and Finance Division of Queen Mary Hospital who have contributed and made a tremendous effort on data capturing and processing. We would also like to extend our gratitude to the case manager of the Geriatric Hip Fracture Clinical Pathway, who has also spent a lot of effort in keeping the clinical pathway smooth and providing accurate data auditing.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) disclose receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Health and Medical Research Fund [grant number 15162751].
Ethical Approval: Ethical approval was sought and satisfied (HKU/HA HKW IRB Reference number: UW 16-301).
ORCID iDs
Dennis King Hang Yee https://orcid.org/0000-0002-6738-3670
Frankie Leung https://orcid.org/0000-0002-5215-1615
References
- 1.Lau TW, Fang C, Leung F. The effectiveness of a multidisciplinary hip fracture care model in improving the clinical outcome and the average cost of manpower. Osteoporos Int. March 2017;28(3):791-798. doi: 10.1007/s00198-016-3845-7 [DOI] [PubMed] [Google Scholar]
- 2.British Orthopaedic Association . The care of patients with fragility fracture. https://www.bgs.org.uk/resources/care-of-patients-with-fragility-fracture-blue-book Accessed June 14, 2021.
- 3.National Institute for Health and Care Excellence . Hip fracture: management. https://www.nice.org.uk/guidance/cg124 Accessed June 14, 2021. [PubMed]
- 4.Age UK . Report to the minister of state for care services, breaking through: building better falls and fracture services in England, 2012. https://www.nos.org.uk/documentdoc?id=987 Accessed June 14, 2021.
- 5.Pioli G, Giusti A, Barone A. Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res. April 2008;20(2):113-122. doi: 10.1007/BF03324757 [DOI] [PubMed] [Google Scholar]
- 6.Lau TW, Leung F, Siu D, Wong G, Luk KD. Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int. December 2010;21(suppl 4):S627-S636. doi: 10.1007/s00198-010-1387-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu SK, Ho AW, Wong SH. Early surgery for Hong Kong Chinese elderly patients with hip fracture reduces short-term and long-term mortality. Hong Kong Med J. August 2017;23(4):374-380. doi: 10.12809/hkmj165005 [DOI] [PubMed] [Google Scholar]
- 8.Gundel O, Thygesen LC, Gogenur I, Ekeloef S. Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop. February 2020;91(1):58-62. doi: 10.1080/17453674.2019.1680485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. June 2012;43(6):676-685. doi: 10.1016/j.injury.2011.05.017 [DOI] [PubMed] [Google Scholar]
- 10.Wei J, Zeng L, Li S, Luo F, Xiang Z, Ding Q. Relationship between comorbidities and treatment decision-making in elderly hip fracture patients. Aging Clin Exp Res. December 2019;31(12):1735-1741. doi: 10.1007/s40520-019-01134-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M, Fantini MP. Hip fracture: effectiveness of early surgery to prevent 30-day mortality. Int Orthop. March 2011;35(3):419-424. doi: 10.1007/s00264-010-1004-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kovar FM, Endler G, Wagner OF, Jaindl M. Basal haemoglobin levels as prognostic factor for early death in elderly patients with a hip fracture- -A twenty year observation study. Injury. 2015;46(6):1018-1022. doi: 10.1016/j.injury.2015.01.010 [DOI] [PubMed] [Google Scholar]
- 13.Yombi JC, Putineanu DC, Cornu O, Lavand'homme P, Cornette P, Castanares-Zapatero D. Low haemoglobin at admission is associated with mortality after hip fractures in elderly patients. Bone Joint Lett J. September 2019;101-B(9):1122-1128. doi: 10.1302/0301-620X.101B9.BJJ-2019-0526.R1 [DOI] [PubMed] [Google Scholar]
- 14.Castelli A, Daidone S, Jacobs R, Kasteridis P, Street AD. The Determinants of Costs and Length of Stay for Hip Fracture Patients. PLoS One. 2015;10(7):e0133545. doi: 10.1371/journal.pone.0133545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craigven SHS, Rehena S, Kenny TXK, Howe CY, Howe TS, Joyce KSB. Shorter acute hospital length of stay in hip fracture patients after surgery predicted by early surgery and mobilization. Arch Osteoporos. October 31 2021;16(1):162. doi: 10.1007/s11657-021-01027-z [DOI] [PubMed] [Google Scholar]
- 16.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. March 2005;16 suppl 2:S3-S7. doi: 10.1007/s00198-004-1702-6 [DOI] [PubMed] [Google Scholar]
- 17.Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service- -a literature review comparing different models. Osteoporos Int. December 2010;21(suppl 4):S637-S646. doi: 10.1007/s00198-010-1396-x [DOI] [PubMed] [Google Scholar]
- 18.Gholve PA, Kosygan KP, Sturdee SW, Faraj AA. Multidisciplinary integrated care pathway for fractured neck of femur. A prospective trial with improved outcome. Injury. January 2005;36(1):93-98; discussion 99. doi: 10.1016/j.injury.2004.02.007 [DOI] [PubMed] [Google Scholar]
- 19.Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. July 2008;56(7):1349-1356. doi: 10.1111/j.1532-5415.2008.01770.x [DOI] [PubMed] [Google Scholar]
- 20.Beaupre LA, Cinats JG, Senthilselvan A, et al. Reduced morbidity for elderly patients with a hip fracture after implementation of a perioperative evidence-based clinical pathway. Qual Saf Health Care. October 2006;15(5):375-379. doi: 10.1136/qshc.2005.017095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adunsky A, Lusky A, Arad M, Heruti RJ. A comparative study of rehabilitation outcomes of elderly hip fracture patients: the advantage of a comprehensive orthogeriatric approach. J Gerontol A Biol Sci Med Sci. June 2003;58(6):542-547. doi: 10.1093/gerona/58.6.m542 [DOI] [PubMed] [Google Scholar]
- 22.Cameron ID, Lyle DM, Quine S. Accelerated rehabilitation after proximal femoral fracture: a randomized controlled trial. Disabil Rehabil. January-March 1993;15(1):29-34. doi: 10.3109/09638289309165866 [DOI] [PubMed] [Google Scholar]
- 23.Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med. April 10 2006;166(7):766-771. doi: 10.1001/archinte.166.7.766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. November 3 2004;292(17):2115-2124. doi: 10.1001/jama.292.17.2115 [DOI] [PubMed] [Google Scholar]
- 25.Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. August 2004;52(8):1263-1270. doi: 10.1111/j.1532-5415.2004.52354.x [DOI] [PubMed] [Google Scholar]
- 26.Wu X, Li Z, Cao J, et al. The association between major complications of immobility during hospitalization and quality of life among bedridden patients: A 3 month prospective multi-center study. PLoS One. 2018;13(10):e0205729. doi: 10.1371/journal.pone.0205729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forch S, Kretschmer R, Haufe T, Plath J, Mayr E. Orthogeriatric Combined Management of Elderly Patients With Proximal Femoral Fracture: Results of a 1-Year Follow-Up. Geriatr Orthop Surg Rehabil. June 2017;8(2):109-114. doi: 10.1177/2151458517698536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dakhil S, Thingstad P, Frihagen F, et al. Orthogeriatrics prevents functional decline in hip fracture patients: report from two randomized controlled trials. BMC Geriatr. March 25 2021;21(1):208. doi: 10.1186/s12877-021-02152-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stenvall M, Olofsson B, Nyberg L, Lundstrom M, Gustafson Y. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med. 2007;39(3):232-238. doi: 10.2340/16501977-0045 [DOI] [PubMed] [Google Scholar]
- 30.Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ (Can Med Assoc J). July 9 2002;167(1):25-32. [PMC free article] [PubMed] [Google Scholar]
- 31.Morri M, Ambrosi E, Chiari P, et al. One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. December 10 2019;9(1):18718. doi: 10.1038/s41598-019-55196-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jiang L, Chou ACC, Nadkarni N, et al. Charlson Comorbidity Index Predicts 5-Year Survivorship of Surgically Treated Hip Fracture Patients. Geriatr Orthop Surg Rehabil. 2018;9:2151459318806442. doi: 10.1177/2151459318806442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mukherjee K, Brooks SE, Barraco RD, et al. Elderly adults with isolated hip fractures- orthogeriatric care versus standard care: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. February 2020;88(2):266-278. doi: 10.1097/TA.0000000000002482 [DOI] [PubMed] [Google Scholar]
- 34.Elliot JR, Wilkinson TJ, Hanger HC, et al. The added effectiveness of early geriatrician involvement on acute orthopaedic wards to orthogeriatric rehabilitation. N Z Med J. March 8 1996;109(1017):72-73. [PubMed] [Google Scholar]
- 35.Zuckerman JD, Sakales SR, Fabian DR, Frankel VH. Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program. Clin Orthop Relat Res. January 1992;274:213-225. [PubMed] [Google Scholar]
- 36.Gregersen M, Morch MM, Hougaard K, Damsgaard EM. Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Inj Violence Res. July 2012;4(2):45-51. doi: 10.5249/jivr.v4i2.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan R, Fernandez C, Kashifl F, Shedden R, Diggory P. Combined orthogeriatric care in the management of hip fractures: a prospective study. Ann R Coll Surg Engl. March 2002;84(2):122-124. [PMC free article] [PubMed] [Google Scholar]
- 38.Antonelli Incalzi R, Gemma A, Capparella O, Bernabei R, Sanguinetti C, Carbonin PU. Continuous geriatric care in orthopedic wards: a valuable alternative to orthogeriatric units. Aging (Milano). June 1993;5(3):207-216. doi: 10.1007/BF03324157 [DOI] [PubMed] [Google Scholar]
- 39.Hogan DB, Fox RA, Badley BW, Mann OE. Effect of a geriatric consultation service on management of patients in an acute care hospital. CMAJ (Can Med Assoc J). April 1 1987;136(7):713-717. [PMC free article] [PubMed] [Google Scholar]
- 40.Cogan L, Martin AJ, Kelly LA, Duggan J, Hynes D, Power D. An audit of hip fracture services in the Mater Hospital Dublin 2001 compared with 2006. Ir J Med Sci. March 2010;179(1):51-55. doi: 10.1007/s11845-009-0377-6 [DOI] [PubMed] [Google Scholar]
- 41.Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res. August 2004;425:72-81. doi: 10.1097/01.blo.0000132266.59787.d2 [DOI] [PubMed] [Google Scholar]
- 42.Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. September 2005;53(9):1476-1482. doi: 10.1111/j.1532-5415.2005.53466.x [DOI] [PubMed] [Google Scholar]
- 43.Fergus L, Cutfield G, Harris R. Auckland City Hospital's ortho-geriatric service: an audit of patients aged over 65 with fractured neck of femur. N Z Med J. June 24 2011;124(1337):40-54. [PubMed] [Google Scholar]
- 44.Hilton R. Defining acute renal failure. CMAJ (Can Med Assoc J). July 12 2011;183(10):1167-1169. doi: 10.1503/cmaj.081170. [DOI] [PMC free article] [PubMed] [Google Scholar]