Abstract
Filarial diseases like lymphatic filariasis and onchocerciasis belong to the Neglected Tropical Diseases and remain a public health problem in endemic countries. Lymphatic filariasis and onchocerciasis can lead to stigmatizing pathologies and present a socio-economic burden for affected people and their endemic countries. Current treatment recommendations by the WHO include mass drug administration with ivermectin for the treatment of onchocerciasis and a combination of ivermectin, albendazole and diethylcarbamazine (DEC) for the treatment of lymphatic filariasis in areas that are not co-endemic for onchocerciasis or loiasis. Limitations of these treatment strategies are due to potential severe adverse events in onchocerciasis and loiasis patients following DEC or ivermectin treatment, respectively, the lack of a macrofilaricidal efficacy of those drugs and the risk of drug resistance development. Thus, to achieve the elimination of transmission of onchocerciasis and the elimination of lymphatic filariasis as a public health problem by 2030, the WHO defined in its roadmap that new alternative treatment strategies with macrofilaricidal compounds are required. Within a collaboration of the non-profit organizations Drugs for Neglected Diseases initiative (DNDi), the Bill & Melinda Gates Foundation, and partners from academia and industry, several new promising macrofilaricidal drug candidates were identified, which will be discussed in this review.
Keywords: filariae, onchocerciasis, Wolbachia, doxycycline, ABBV-4083, emodepside, oxfendazole, rifampicine, Litomosoides sigmodontis, Onchocerca volvulus
Filariasis
Filarial nematodes can cause debilitating diseases like lymphatic filariasis (LF) and onchocerciasis. LF is caused by Wuchereria bancrofti, Brugia malayi or Brugia timori, which can lead to lymphedema in the extremities (elephantiasis) and/or hydrocele in the scrotum of men [1], [2]. The nocturnal mosquito vector (Mansonia, Anopheles, Culex, Aedes) transmits infective L3 larvae to humans, which migrate to the lymphatics and mold into adult worms. The progeny, so-called microfilariae (MF), are released into the peripheral blood, where they can be taken up again by the mosquito. LF is mainly found in sub-Saharan Africa and South-East Asia and it is estimated that in 2017, 65 million people were infected with LF, while 19.42 million people suffered from hydrocele, and 16.68 million people from lymphedema [3], [4].
The causative agent for onchocerciasis is Onchocerca volvulus, and the disease can lead to vision impairment and blindness as well as severe dermatitis. Thus, onchocerciasis is often referred to as river blindness; and the disease is mainly found in sub-Saharan Africa; and remaining foci in Yemen, Venezuela and Brazil exist [2], [5], [6]. The infective L3 larvae are transmitted by black flies (Simulium), and the adult worms reside in subcutaneous nodules, while the MF migrate through the skin and occasionally the cornea [2]. In 2017, onchocerciasis affected about 21 million people with 14.6 million people presenting skin diseases and 1.15 million people suffering from vision impairment [3], [4], [6].
The pathology in those diseases is induced through different mechanisms. While lymphedema initially occurs as an immunological consequence to the adult worms, which leads to the dilatation of the lymphatics and a leakage of the endothelial cell-cell junctions, skin manifestations and vision impairment in onchocerciasis are a result of an inflammatory immune response to the dying MF [7], [8]. Most human-pathogenic filarial nematodes live in an endosymbiotic state with Wolbachia bacteria, which provide important factors for worm development, growth and reproduction [9]. Release of these Wolbachia from dying MF provokes inflammation in the skin leading to rashes, itching, lesions in the skin or the cornea of the eye, and thus over time to vision impairment in onchocerciasis patients [10], [11], [12].
Current treatment strategies and their limitations
Standard drugs used for mass drug administration (MDA) include ivermectin (IVM), albendazole (ALB), and diethylcarbamazine citrate (DEC) [1], [7]. IVM is a macrocyclic lactone with a microfilaricidal effect that temporarily inhibits the embryogenesis of adult female worms, which interrupts microfilaremia for up to 6–12 months and thus limits the transmission of the diseases [13]. Similarly, the piperazin derivate DEC also targets the MF, leading to a temporary inhibition of the embryogenesis of female worms. The carbamate benzimidazole ALB is another drug used in combination for MDA. Its mode of action is the inhibition of the polymerization of β-tubulin and microtubule formation in helminths. Thus, this broad-spectrum anti-helminthic drug is not specifically used to treat filariasis but is active against other nematodes and cestodes [14], [15]. On its own, ALB has only little effect on MF and adult filariae [16].
For the control of onchocerciasis, the WHO recommends MDA of IVM on an annual or bi-annual basis. Treatment of LF is done with a combination of IVM and ALB in sub-Saharan Africa in areas that are co-endemic for onchocerciasis and with a triple therapy of DEC, IVM, plus ALB in regions non-endemic for onchocerciasis and loiasis [17], [18], [19]. MDA programs that have existed for up to 40 years now, have reduced the prevalence of LF. Seventeen countries have achieved elimination, and five additional countries have stopped MDAs and are now under surveillance of having eliminated LF, but 50 countries are still endemic for LF and require further MDA treatments [20]. Large-scale treatments in Latin America already successfully led to elimination of onchocerciasis in Colombia and Ecuador in 2013 and 2014, respectively. Furthermore, onchocerciasis transmission was stopped in Mexico and Guatemala in 2011. Thus, 11 out of 13 foci in the Americas have stopped MDA, while Brazil and Venezuela still require MDA treatment in few foci [21].
However, there are certain limitations for the current treatment strategies against onchocerciasis. The triple therapy (IVM, ALB, and DEC) used to treat LF may cause serious adverse events in patients of loiasis, another filarial disease caused by Loa loa, and onchocerciasis patients [5], [22], [23], [24], [25], [26], impairing the implementation of the triple therapy in areas co-endemic of those diseases. Furthermore, current treatment strategies are restricted to temporarily inhibiting the embryogenesis of adult female worms and having a microfilaricidal effect. Thus, the chemotherapeutics used lack a pronounced macrofilaricidal, i.e. adult worm killing, efficacy. Therefore, repeated annual or bi-annual drug administrations are required for the reproductive life-span of the adult worms, which is up to five years for LF and up to 15 years for onchocerciasis [1]. Moreover, modeling studies suggest that the triple therapy is in particular valid in clearing filariasis in areas with high prevalence, while it loses its cost efficiency in areas with low prevalence [17]. The WHO roadmap on Neglected Tropical Diseases 2021–2030 defined as a main target the elimination of LF as a public health problem and to stop the transmission of onchocerciasis by 2030 via mass drug administrations (MDA) and vector control [27], [28], [29], [30].
Recently, the FDA approved moxidectin as a treatment for onchocerciasis. Moxidectin belongs to the same milbemycin class of macrocyclic lactone as IVM. Similar to IVM, moxidectin is a potent microfilaricide and inhibits the filarial embryogenesis. However, inhibitory effects of moxidectin are superior to IVM, providing a complete clearance of MF, which is maintained for a longer period of time compared to IVM [31], [32].
Thus, a clinical study has shown that a single moxidectin treatment reduced the skin MF to 0.6 per mg skin after 1 year, in comparison to a single IVM treatment which resulted in 4.5 MF/mg of skin. Moreover, the proportion of patients without detectable skin MF was higher (38%) in the group treated with moxidectin than in the group receiving IVM (2%). Importantly, 98% of patients treated with moxidectin had no detectable MF within the eyes at 18 months post treatment. IVM treatment resulted in no detectable eye MF in 90% of the patients after 18 months [32]. This reduced MF load in moxidectin-treated patients is suggested to be the result of an enhanced embryostatic effect [33]. Moxidectin’s safety profile was comparable to IVM, and rapid MF death can result in adverse events after moxidectin as well as after IVM treatment [31], [32]. Due to moxidectin’s superior activity against MF in comparison to IVM, it may accelerate elimination of onchocerciasis, and modeling studies suggest that annual moxidectin administration could replace bi-annual IVM MDA in areas with persistent transmission [33]. However, IVM entails the risk for severe adverse events in patients with heavy L. loa microfilarial loads and thus, implementation is limited in L. loa co-endemic areas. Even though no clinical trials to evaluate the safety of moxidectin treatment in loiasis co-endemic areas have been conducted yet, it is expected that, similar to IVM, moxidectin treatment could have the same limitation. Thus, moxidectin could replace IVM treatment and reduce transmission as well as infection rates. However, it remains to be determined whether a microfilaricidal drug that lacks a strong macrofilaricidal efficacy is sufficient to achieve the goals of the WHO roadmap to stop the transmission of onchocerciasis by 2030. IVM MDA has been applied for almost 40 years and led to significant achievements in reducing onchocerciasis transmission. This success of IVM is closely linked to the commitment of Merck (MSD) to provide IVM free of charge, which is not the case for moxidectin, and will therefore challenge its broader use and success in endemic regions.
Thus, the identification of an effective macrofilaricide, which can be administered over a short period of time, could support the elimination of filariasis by mopping up residual foci and for case management [34], [35].
Endosymbiotic Wolbachia bacteria as targets for anti-filarial therapy
Screening drugs against the Wolbachia endosymbionts of filariae is a validated approach to identify new macrofilaricidal compounds [36]. Most human-pathogenic filariae, such as W. bancrofti [37], B. malayi [38], B. timori [39], O. volvulus [9], Mansonella perstans [40], [41], and Mansonella ozzardi [42] contain endosymbiotic Wolbachia, while L. loa lacks Wolbachia bacteria [43].
Wolbachia bacteria have also been found in filarial nematodes of animals, including filariae infecting cattle (Onchocerca ochengi, Onchocerca gutturosa and Onchocerca lienalis) [44], [45], [46], cats (Brugia pahangi) [47], [48], dogs (Dirofilaria immitis [47], [49], Dirofilaria repens [50]), and rodents (Litomosoides sigmodontis) [51]. Furthermore, in some animal filariae Wolbachia are absent, like in the rodent filaria Acanthocheilonema viteae [51]. Wolbachia are rickettsia-like endobacteria and are transmitted transovarially to the next generation. Thus, they are found in oocytes, all larval stages, the lateral chord and hypodermis of adult worms, but never in the male genitals [52].
The endosymbiotic relationship between Wolbachia and filariae is created through the exchange of certain proteins, which are essential for growth, survival and reproduction of the filariae, and allow the treatment of Wolbachia-containing filariae with antibiotics [53].
For B. malayi and their endosymbionts (wBM) it was shown that wBM had a highly reduced genome. wBM are able to synthesize purines and pyrimidines de novo, but lack genes for the synthesis of other amino acids except for meso-diaminopimelate, an amino acid required to produce peptidoglycan [38], [54], [55]. Moreover, the wBm genome encodes for the synthesis of riboflavin, flavin adenine dinucleotide, and heme [38]. However, these genes are only partly or completely absent in the nematode genome and thus, Wolbachia may provide the nematode with heme [56], riboflavin, flavin adenine dinucleotides, as well as nucleotides [57], and may also be a source of ATP during energy-intensive larval-stage development with high cell division such as development and embryogenesis [58].
Due to the close relationship and the dependency of nematode and endosymbiont, targeting Wolbachia by antibiotics results in the inhibition of worm development and fertility.
Doxycycline as first anti-Wolbachial drug
Initial murine studies using the filarial nematode L. sigmodontis showed that tetracycline depletes Wolbachia bacteria from the filariae, which leads to female worm sterility, inhibited embryogenesis, and over time clearance of microfilaremia [51], [59]. Moreover, using O. ochengi, B. pahangi and D. immitis models, a macrofilaricidal effect for tetracycline was confirmed [45], [47]. Doxycycline, a second-generation tetracycline antibiotic, was subsequently used in first clinical studies. Administration of 100 mg doxycycline daily for 6 weeks resulted in the depletion of Wolbachia bacteria from O. volvulus, inhibition of the embryogenesis, long-term amicrofilaridermia, and killing of the adult worms [11]. Subsequent clinical trials demonstrated that doxycycline is also effective in depleting Wolbachia from bancroftian filariasis patients, leading to a 96% Wolbachia reduction and a 99% reduction in MF levels one year after treatment with 200 mg doxycycline for six weeks [60]. Combination therapy with doxycycline and a single dose of IVM resulted in a complete amicrofilaremia in bancroftian patients [60]. Further studies in LF patients showed that doxycycline regimens of 200 mg daily for 6 weeks followed by a single administration of IVM and ALB four months after doxycycline treatment not only reduced Wolbachia levels, but also had a macrofilaricidal effect of 89% after 24 months, determined by the absence of the filarial dance sign in the scrotum of male patients [61]. Lymphedema significantly improved after doxycycline administration already after 12 months [61]. Importantly, treatment duration of doxycycline could be reduced to 4 weeks with a single IVM dose 4 months after doxycycline regimen and still resulted in a macrofilaricidal activity of 83% after 24 months, which is comparable with the results of a 6-week doxycycline treatment [62]. Reduced treatment durations of three weeks with 200 mg doxycycline daily and a single DEC dose (6 mg/kg) were sufficient to completely ablate microfilaremia, but did not affect the adult worm burden [63].
For onchocerciasis it was shown that a 6-week doxycycline regimen with 100 mg daily resulted in a gradual decline of Wolbachia from month two to six following treatment, while the embryogenesis was inhibited by 6 months and MF declined by 11 months after treatment start. These effects were maintained for 18 months, whereas isolation of the adult worms through nodulectomy and collagenase digestion showed that only macrofilaricidal efficacy was observed at that time point and many worms were still viable [64]. A macrofilaricidal effect was observed for a 6-week therapy with 200 mg doxycycline after 20 and 27 months, resulting in the death of ~60% of the female adult worms as assessed by histological staining determining calcification, loss of body wall integrity, and absence of cathepsin D-like lysosomal aspartic protease of O. volvulus [65]. If newly acquired worms were subtracted, macrofilaricidal efficacy amounted to 70% [66]. Reducing treatment duration to 5 weeks and doxycycline concentration to 100 mg daily had a moderate macrofilaricidal effect with 51% viable adult female worms compared to 84% viable adult female worms in the control group, although the surviving female worms were not fertile [67]. Interestingly, combination treatment of doxycycline and IVM caused a quick decline in MF. However, unlike IVM treatment alone, the combination caused a permanent clearance of microfilarial loads in accordance with the inability of sterilized female worms to produce MF. Additional studies analyzing treatment duration and concentration revealed that 200 mg of doxycycline has to be given for four to six weeks, while two weeks treatment failed to deplete Wolbachia and MF [68]. Four- to six-week treatment with 200 mg doxycycline also resulted in a macrofilaricidal effect of 50 and 60%, respectively [65]. Moreover, a 6-week doxycycline treatment is also safe in areas co-endemic for loiasis, since L. loa has no Wolbachia bacteria, and doxycycline treatment does not bear the risk of life-threatening serious adverse events in L. loa patients with high microfilarial loads, unlike current MDA treatments with DEC and/or IVM [69], [70], [71].
Based on these results, it is recommended that doxycycline is given daily for 4 weeks at 200 mg [65], or for 5 weeks at 100 mg to achieve sustained sterilization of female adult worms and amicrofilaridermia in onchocerciasis patients [67]. To achieve the strongest macrofilaricidal effect, 200 mg doxycycline should be given daily for six weeks [72]. LF is treated with 200 mg doxycycline daily for four weeks to obtain a macrofilaricidal effect, while the reduction of lymphedema and hydrocele pathology can be achieved following a 6-week treatment of 200 mg doxycycline [73], [74].
In summary, these studies showed that doxycycline treatment depletes Wolbachia bacteria from the filariae causing LF and onchocerciasis, resulting in the inhibition of the embryogenesis, MF clearance over time, and a slow death of the adult worms. This is particularly advantageous since the treatment with doxycycline does not bear the risk of serious adverse events observed for onchocerciasis patients treated with DEC, or for loiasis patients with high MF loads treated with IVM, which is caused by the inflammation induced by the fast death of MF [70], [75], [76]. Thus, doxycycline administration is safe in areas co-endemic for those diseases overcoming the limitations of the current MDA. The results also show that the filariae causing LF (Brugia spp. and W. bancrofti) are more susceptible to the treatment with doxycycline compared to O. volvulus, since a 4-week treatment with doxycycline results in a long-lasting reduction in MF loads and adult worm removal in LF patients.
However, doxycycline treatment is contraindicated in pregnant and breast-feeding women, as well as children under the age of eight [74]. Furthermore, it requires daily treatments over several weeks and thus, it is rather used as an individual therapy. Doxycycline is administered by doctors in outpatient clinics in endemic countries with a health care system that provides individual care for filariasis, and in non-endemic countries like Europe and the US. Moreover, individual doxycycline treatment is recommended as an end-game strategy by the WHO to clear remaining onchocerciasis disease foci in Brazil and the Bolivarian Republic of Venezuela [77].
Next to human filariasis, canine heartworm disease caused by D. immitis is frequently treated with the standard monthly IVM (6 µg/kg), in combination with one round of doxycycline (10 mg/kg bi-daily) given for 4 weeks, followed by intramuscular injections with melarsomine (2.5 mg/kg) on day 60, 90 and 91 as recommended by the American Heartworm Society. This regimen leads to adult worm death, reduces MF loads, and prevents the aggravation of pulmonary damage in infected dogs [78].
New macrofilaricidal drugs in clinical studies
Drugs already tested in phase I clinical trials
High-dose rifampicin
Due to the limitations of doxycycline, additional antibiotics are under investigation for the treatment of filariasis. Rifampicin is of particular interest since it can be administered to children, and in initial preclinical tests, rifampicin depleted Wolbachia endosymbionts of L. sigmodontis, and reduced the filarial development and adult worm survival [79]. In first human clinical studies, 10 mg/kg/day rifampicin administered for two and four weeks to onchocerciasis patients resulted in impaired filarial embryogenesis and a Wolbachia reduction in female adult worms 18 months after treatment start. This was comparable to a 6-week treatment of doxycycline with 100 mg daily [80]. However, 78–100% of adult worms remained viable. Subsequent pharmacokinetic-pharmacodynamic (PK-PD) analysis of a dose-escalation study in B. malayi- and O. ochengi-infected mice showed that 10 mg/kg/day rifampicin (bioequivalent dose of 600 mg/day dose in humans) is suboptimal. Rather a bioequivalent human high-dose of 30–35 mg/kg/day is required to achieve a Wolbachia reduction of above 90% after 7 and 14 days in the B. malayi and O. ochengi model, respectively [81]. Thus, high-dose rifampicin has the potential to reduce the treatment duration to 1–2 weeks for human filariasis, and initial clinical studies for treatment of tuberculosis with rifampicin have shown that 20 and 35 mg/kg/day is safe and does not bear the risk of increasing toxicity in comparison to 10 mg/kg/day [82], [83], [84]. However, the number of patients in these studies is still limited, and larger patient cohorts with about 2000 patients will be required to ensure a sufficient safety profile, and are a prerequisite to be registered for filarial indication [85]. Additional phase II clinical studies using high-dose rifampicin to treat human filariasis are now under preparation and will investigate the safety profile of high-dose rifampicin in a larger study population [86], [87].
Of note, due to the short treatment duration of 1–2 weeks of rifampicin, drug resistance by Mycobacterium tuberculosis (TB) is not expected. However, possible risk for drug resistances in areas co-endemic for TB and filarial diseases cannot completely be excluded.
ABBV-4083
The Tylosin A analogue ABBV-4083 is a macrolide antibiotic with an improved pharmacokinetic profile with increased oral bioavailability and potency against Wolbachia [88], [89]. Using the B. malayi, L. sigmodontis, and O. ochengi animal models, ABBV-4083 showed a superior activity against Wolbachia compared to doxycycline. These preclinical studies demonstrated a Wolbachia depletion above 90% with blocked filarial embryogenesis and microfilarial release after treatment with ABBV-4083 for 1–2 weeks [88], [89]. Additional experiments in the L. sigmodontis rodent model showed that ABBV-4083 induced Wolbachia depletion as soon as 3 days after treatment start, and Wolbachia depletion continued in the following weeks after treatment ended [90]. Up to four missed treatments with ABBV-4083 did not impair the efficacy in depleting Wolbachia bacteria from L. sigmodontis, as long as the full regimen was subsequently completed [90]. Assessment of the safety of ABBV-4083 was done in preclinical and phase I clinical studies, which supports the progression of ABBV-4083 to phase II clinical studies [91], [92]. Thus, ABBV-4083 represents a next-generation macrofilaricidal oral drug candidate for the treatment of human filarial diseases, which may allow treatment regimens of 14 days or less. It has completed clinical phase I evaluation and phase II trials in onchocerciasis patients of the Democratic Republic of Congo begun in June 2021 [93].
In addition, in preclinical studies, using ABBV-4083 with ALB was tested in L. sigmodontis- and B. pahangi-infected jirds, and indicated that lower doses and shorter treatment durations of ABBV-4083 are possible when administered together with ALB [94]. Wolbachia depletion was improved by the combination therapy, which resulted in maintained clearance of peripheral MF loads compared to ALB and ABBV-4083 single treatments [94].
Oxfendazole as direct acting macrofilaricide
Oxfendazole belongs to the class of benzimidazoles, and is a broadspectrum anthelminthic veterinary drug that targets the β-tubulin of helminths. Thus, it was shown that oxfendazole is efficacious against Taenia solium in infected pigs [95]. Similar to flubendazole, oxfendazole has a high efficacy against adult worms when administered subcutaneously [96], [97], [98], [99], but unlike flubendazole, oxfendazole has an improved oral bioavailability [99], [100], [101]. However, flubendazole showed teratogenicity and aneugenicity [100], [102], which lead to the stop of further development of flubendazole as antifilarial drug in humans. For oxfendazole, indications of such a teratogenicity and aneugenicity were not reported, as oxfendazole exhibited no in vitro toxicity in the AMES assay, and the mouse lymphoma assay as well as in the in vivo rat micronucleus assay. Toxicity and behavioral studies in rats and cardiovascular studies in dogs further showed no safety concerns for oxfendazole [103]. Furthermore, a small study conducted in pregnant sows did not identify a risk of oxfendazole treatment on sows or the newborn pigs [104]. Subsequent first in human studies confirmed the safety of a multiple ascending dose [105], [106], [107]. However, since oxfendazole as well as ALB, which is currently used in MDA against LF, belong to the same chemical class as flubendazole, similar toxicity cannot be completely ruled out in humans and may require additional precautionary measures such as the exclusion of pregnant women and the usage of contraception for women of potential bearing age.
For filariae, in vitro studies have shown that oxfendazole inhibits motility of O. gutturosa adult worms, O. volvulus pre-adults (L5), and O. lienalis MF [99]. Preclinical studies provided further evidence that a five-day regimen of orally administered oxfendazole killed all adult worms in the L. sigmodontis mouse model [99]. Using the L. sigmodontis jird model, the effect on microfilaremia was analyzed. A 10-day regimen of oxfendazole inhibited filarial embryogenesis and resulted in a slow and continuous decline of peripheral MF, and finally to a complete clearance of MF [99]. Importantly, the decline in MF resulted from the inhibited embryogenesis rather than from a direct microfilaricidal effect [99]. Based on the animal pharmacokinetic studies, the human efficacious dose is predicted to range from 1.5–4.1 mg/kg [99]. A first human multiple ascending dose study with 3, 7.5, and 15 mg/kg oxfendazole daily for a total of five days has already been completed [105], [106] and has shown no adverse reactions [107]. Since the predicted human efficacious dose is within this tested and well-tolerated range, oxfendazole has the potential to be a potent drug candidate that could be used for case management and to treat remaining foci of onchocerciasis. Furthermore, as oxfendazole had no strong microfilaricidal efficacy in the L. sigmodontis model [99] and in mice infused with L. loa MF [108], it may also present a promising candidate for the treatment of loiasis. Thus, oxfendazole is currently under consideration for phase II clinical studies, and within the HELP consortium of the European Union’s Horizon 2020 activities [109], oxfendazole bioavailability studies and field-applicable tablet formulations are prepared [110]. However, it still has to be determined if oxfendazole is safe for treatment in neurocysticercosis patients, as the death of T. solium cysticerci in the brain following treatment with the benzimidazole ALB induces inflammatory responses and temporarily worsens neurological symptoms [111]. Since ALB or praziquantel therapy in general can provoke inflammatory responses upon dying cysts, co-administration of corticosteroids in neurocysticercosis patients are frequently required [112]. Therefore, onchocerciasis and cysticercosis co-endemic areas may require a test and treat strategy for oxfendazole treatment.
Emodepside
Repurposing of drugs which are already registered for animal health has been one of the focuses to identify new macrofilaricidal candidates against filariasis. Next to oxfendazole, emodepside is a drug frequently used in veterinary settings to treat parasitic gastrointestinal nematodes including roundworms, hookworms, and strongyloides [113], [114]. Emodepside belongs to the cyclooctadepsipeptides, and PF1022A is the first anthelminthic member recognized of this class, which is a compound isolated from the fungus Rosellinia spp. [115]. Emodepside acts on the Ca2+-gated K+-channel SLO-1 of nematodes [116]. In vitro studies have shown that emodepside paralyses the different larval stages of several filariae, including A. vitae, Brugia spp., D. immitis, L. sigmodontis, and Onchocerca spp. [117]. Importantly, adult worms seemed to have the highest in vitro sensitivity towards emodepside compared to the different larval stages [117]. Furthermore, emodepside was highly efficacious in rapidly decreasing microfilarial loads of L. sigmodontis, A. viteae, and B. malayi in infected Mastomys coucha in vivo. A single dose of 3.125 mg/kg (L. sigmodontis) and 6.25 mg/kg (B. malayi) reduced the microfilarial loads by more than 95% after 3 days already. Treatment with a single dose of 100 mg/kg and five treatments with 100 mg/kg emodepside caused a macrofilaricidal effect in A. vitae- and L. sigmodontis-infected animals, respectively, while no effect on adult worms was observed for B. malayi [118]. Even though Brugia spp. were least susceptible to emodepside, O. gutterosa and O. lienalis were paralyzed and killed even at low doses of emodepside [119]. A proof of principal study in O. ochengi-infected cattle confirmed that a 7-day emodepside treatment rapidly clears MF, inhibits filarial embryogenesis, and mediates a macrofilaricidal efficacy after 18 months [120]. Thus, emodepside targets multiple life-cycle stages of filariae, and due to the high susceptibility of adult worms of the Onchocerca spp., it is under investigation for the treatment of onchocerciasis [115]. First clinical human trials have demonstrated the safety of emodepside, and a phase II clinical trial in onchocerciasis patients in Ghana has started in January 2022 [121]. However, targeting several stages of the filariae including the MF stage could bear the risk for adverse events in patients with high MF loads, and may argue against its use in loiasis co-endemic areas. On the other hand, emodepside may also be active against intestinal helminths and may therefore present a pan-nematode candidate that tackles both filarial and intestinal helminth infections [115].
Auranofin
Another re-purposed drug to treat filarial diseases is auranofin (2,3,4,6-tetra-O-acetyl-1-thio-beta-D-glucopyranosato-S (triethylphosphine) gold), which is an FDA-approved drug used to treat rheumatoid arthritis in humans [122], [123]. Next to auranofin’s activity against Brugia spp. and O. ochengi MF, it showed an even higher activity against adult worms of Brugia spp. and O. ochengi, as well as against L3 larvae of O. volvulus in vitro. Since highest concentrations were required to inhibit L. loa MF, auranofin may provide a drug which can be administered in areas co-endemic for L. loa. In vivo, 28-day treatment with 5 mg/kg auranofin twice a day on weekdays reduced adult worm burden of B. malayi-infected jirds by 91% compared to the vehicle control group. Mode of action of auranofin is mediated through the inhibition of the thioredoxin reductase [124] and the related thioredoxin glutathione reductase [125]. A first phase I clinical trial was conducted, which reported auranofin’s safety [126].
Drugs in preparation for phase I clinical trials
Corallopyronin A
Corallopyronin A (Cor A) is an α-pyrone ring-containing natural product from Corallococcus coralloides [127], and it is a non-competitive inhibitor of bacterial DNA-dependent RNA polymerase by targeting the switch region rather than the active site [128], [129], [130], [131]. It is highly effective against Gram-positive bacteria including rifampicin-resistant Staphylococcus aureus, but has low efficacy against Gram-negative bacteria unless genes for the tolC or other efflux pumps are missing [130]. Even though Gram-negative bacteria are typically not susceptible, Cor A showed in vitro and in vivo activity against Wolbachia bacteria [132]. Since Wolbachia bacteria have a significant reduced genome, the efflux pump pathways are incomplete and they are unable to produce lipopolysaccharide, which renders them susceptible to Cor A [38].
In the L. sigmodontis model, Cor A significantly reduced Wolbachia bacteria, completely cleared microfilaremia and it has shown a robust reduction of adult worm burden when administered alone or in combination with ALB [133]. Safety and toxicity tests in vitro and in vivo suggest that Cor A is safe and non-toxic, and its progress towards first clinical studies, supported by the German Center for Infection Research (DZIF) and the EU Horizon 2020 HELP consortium, is under preparation.
AWZ1066S
A highly selective and potent anti-Wolbachia candidate is the azaquinazoline AWZ1066S, which showed a maximal clearance of Wolbachia within one day of in vitro drug exposure. Thus, Wolbachia clearance in vitro of AWZ1066S is much faster, and thus superior compared to doxycycline and rifampicin. AWZ1066S reduced more than 98% of Wolbachia in the B. malayi SCID mouse and L. sigmodontis gerbil model and inhibited embryogenesis in the latter [134]. Furthermore, beginning six weeks post AWZ1066S treatment in L. sigmodontis-infected gerbils, a continuous decline in peripheral MF was observed, and after 14 weeks post treatment start, MF were completely cleared. Similar to all anti-Wolbachials, AWZ1066S rather inhibits the embryogenesis than having a direct microfilaricidal effect [134]. Preclinical safety has already been proven, and human PK simulation predict a Wolbachia reduction by more than 90% in more than 90% of the patients after a 7-day regimen with 10 mg/kg AWZ1066S [134]. Due to this potent anti-Wolbachial efficacy and the early assessment of its safety, AWZ1066S fits the criteria for the target product profile for novel drug candidates for human filariasis, and first clinical studies to assess the safety of AWZ1066S are intended [135].
CC6166
CC6166 is a direct-acting compound developed by Celgene (now Bristol-Myers Squibb), which is supported by the DNDi, and it is currently under investigation for its macrofilaricidal activity [136], [137], [138].
Backup candidates on hold
AN11251
The boron-pleuromutilin AN11251 exhibited a solid potency against Wolbachia in vitro, and thus was targeted for further preclinical in vivo studies. Using the L. sigmodontis mouse model, AN11251 exhibited a good oral bioavailability, depleted more than 99% of Wolbachia after 10 to 14 days of treatment, and is thus superior to the human bioequivalent dose of doxycycline [139], [140]. Preliminary in vitro and in vivo safety assessment support further evaluation of AN11251 as a preclinical anti-Wolbachia candidate for human filarial diseases.
CBR417/CBR490
Further preclinical candidates on hold are the quinazolines CBR417 and CBR490, which showed a potent and selective anti-Wolbachia activity. Ex vivo assays demonstrated superior Wolbachia depletion by CBR417 and CBR490 from female B. pahangi ovaries compared to doxycycline. In vivo, these quinazolines rapidly cleared Wolbachia in the L. sigmodontis mouse model, and treatments as short as 4 days with 60 mg/kg/day eliminated more than 99% of Wolbachia in L. sigmodontis adult female worms. Even one single dose regimen or two doses within two weeks were sufficient to reduce more than 99% of Wolbachia [141]. Thus, these two new compounds highlight the potential of short-regiments using anti-Wolbachia drug candidates.
Summary and outlook
Current treatment strategies for onchocerciasis and LF face several limitations preventing the successful elimination of those diseases. The biggest challenge is still the lack of a macrofilaricidal drug that is safe and requires only short treatment durations, and thus would vastly accelerate the elimination of these debilitating diseases. By depleting Wolbachia bacteria, doxycycline was the first well-tolerated macrofilaricidal drug and paved the path for the identification of new anti-Wolbachial drugs with macrofilaricidal activity. Safety of high-dose rifampicin was provided in clinical studies for tuberculosis, and preclinical studies showed promising results for high-doses of rifampicin to be an effective anti-Wolbachial antibiotic with shorter treatment durations and a safe administration of rifampicin in children, thus overcoming two limitations of doxycycline. ABBV-4083, Cor A, and AWZ1066S are additional promising anti-Wolbachial drug candidates that could allow shorter treatment regimens. Based on preclinical modeling, suggested treatment regimens of 7 or 14 days are possible with ABBV-4083, which completed the clinical phase I and is currently under phase II evaluation. Cor A is the first published anti-Wolbachia candidate that significantly reduced the L. sigmodontis adult worm burden by depleting Wolbachia bacteria in preclinical studies. In vitro, AWZ1066S showed superior Wolbachia-depletion compared to doxycycline and rifampicin, and in vivo preclinical studies presented a very fast Wolbachia-reduction, which will enable short treatment durations predicted to be of 7 days or less.
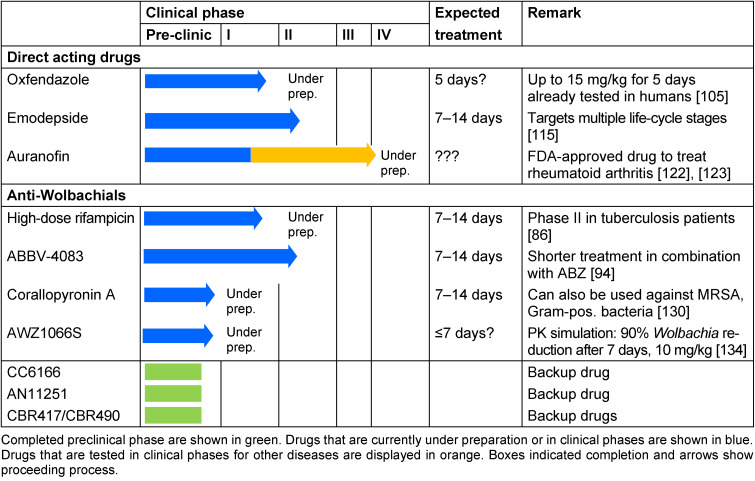
Promising direct-acting macrofilaricidal candidates currently under preparation for or in phase II clinical studies are oxfendazole and emodepside, respectively. Oxfendazole presented a robust macrofilaricidal but no strong microfilaricidal activity in preclinical studies with L. sigmodontis, and based on first human clinical trials, the predicted human efficacious dose for oxfendazole appears to be safe. Emodepside on the other hand targets multiple life-cycle stages of filariae, and first clinical human trails have demonstrated the safety of emodepside. Based on its broad activity against both filarial and intestinal nematodes, it is potentially useful for several nematode diseases [115], [117]. Next to emodepside, CC6166 is supported by the DNDi and currently investigated for its macrofilaricidal activity. Furthermore, several further candidates such as AN11251 and CBR417/CBR490 are currently on hold and serve as backup drugs (Table 1 (Tab. 1)).
Table 1. Summary of new macrofilaricidal candidates and their current clinical status.
Recently, the FDA approved moxidectin as a treatment for onchocerciasis, and with its superior activity against MF in comparison to IVM, it may replace IVM, and thus reduce transmission and infection rates for onchocerciasis. Moxidectin could be especially effective in areas with persistent transmission despite high IVM coverage due to substantial inter-treatment transmission [142]. However, moxidectin still faces the same problems as the other microfilaricidal drug candidates. Moxidectin has the advantage that it only requires a single annual treatment, while the macrofilaricidal candidates are expected to require regimens of 7 to 14 days, and thus are more labor-intensive and expensive in comparison to moxidectin. However, selective macrofilaricides and anti-Wolbachials should be safe for treatment in areas co-endemic for loiasis, whereas moxidectin, similar to IVM, may cause severe adverse events in loiasis patients with high MF numbers. In particular, ABBV-4083 and oxfendazole are quite advanced in the development and may arise as good candidates to substantially eliminate onchocerciasis. However, registration of new macrofilaricidal drugs is planned but will not be done in the next few years, which reduces the time to reach the goals of the WHO roadmap. What will be more difficult is the distribution of the new drugs, since it will rely on a strong pharmaceutical partner. This partnership is lacking for all new macrofilaricidal drug candidates including moxidectin. Therefore, new drugs will require partnering for further development, and will mostly impact the outcome if onchocerciasis will be eliminated in the near future. Most candidates have been developed in collaboration with pharmaceutical companies, academia, and non-profit organizations. The research has been supported by programs such as the Bill & Melinda Gates foundation and TDR (Special Programme for Research and Training in Tropical Diseases), which recently have stopped the funding for additional preclinical development. Even though several candidates have been identified and tested in first clinical studies, Cor A, AWZ1066S, and CC6166 have not been tested in humans, and thus the safety profile is still preliminary. Therefore, these safety data could still pose the risk of a high attrition rate and limit the number of drugs in the pipeline for the treatment of onchocerciasis. Moreover, further development of the preclinical candidates AN11251 and CBR417/490 has been stopped and placed the candidates on hold due to lack of finance. Thus, due to the high attrition rate of drugs entering the first clinical phases and even among candidates that successfully cleared phase I clinical studies, a healthy drug pipeline is required. Despite the backup candidates that are currently on hold for the development, effective elimination of onchocerciasis should not be focused on a single candidate, but several drugs should be developed that address the specific need of the patients depending on its context. Such a pipeline could also be used to identify improved drugs that enable e.g. pediatric formulations, treatments for pregnant and lactating women, and a safe macrofilaricidal treatment for loiasis patients.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet. 2010 Oct;376(9747):1175–1185. doi: 10.1016/S0140-6736(10)60586-7. [DOI] [PubMed] [Google Scholar]
- 2.Simonsen PE. Filariases. In: Cook G, Zumla A, editors. Manson’s tropical diseases. London: Elsevier; 2009. pp. 1477–1513. [Google Scholar]
- 3.WHO. Global programme to eliminate lymphatic filariasis: progress report, 2015. Wkly Epidemiol Rec. 2015;39(91):441–560. [PubMed] [Google Scholar]
- 4.WHO. Lymphatic filariasis. [last updated 2022 Mar 16]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/lymphatic-filariasis.
- 5.WHO. Progress report on the elimination of human onchocerciasis, 2016–2017. Wkly Epidemiol Rec. 2017;92(45):681–700. [PubMed] [Google Scholar]
- 6.WHO. Onchocerciasis. [last updated 2022 Jan 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/onchocerciasis.
- 7.Hoerauf A. Onchocerciasis. In: Guerrant RL, Walker DH, Weller PF, editors. Tropical Infectious Diseases: Principles, Pathogens and Practice. Edinburgh: Elsevier; 2011. pp. 741–749. [Google Scholar]
- 8.Babu S, Nutman TB. Immunopathogenesis of lymphatic filarial disease. Semin Immunopathol. 2012 Nov;34(6):847–861. doi: 10.1007/s00281-012-0346-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor MJ, Bandi C, Hoerauf A. Wolbachia bacterial endosymbionts of filarial nematodes. Adv Parasitol. 2005;60:245–284. doi: 10.1016/S0065-308X(05)60004-8. [DOI] [PubMed] [Google Scholar]
- 10.Hoerauf A, Mand S, Adjei O, Fleischer B, Büttner DW. Depletion of wolbachia endobacteria in Onchocerca volvulus by doxycycline and microfilaridermia after ivermectin treatment. Lancet. 2001 May;357(9266):1415–1416. doi: 10.1016/S0140-6736(00)04581-5. [DOI] [PubMed] [Google Scholar]
- 11.Hoerauf A, Volkmann L, Hamelmann C, Adjei O, Autenrieth IB, Fleischer B, Büttner DW. Endosymbiotic bacteria in worms as targets for a novel chemotherapy in filariasis. Lancet. 2000 Apr;355(9211):1242–1243. doi: 10.1016/S0140-6736(00)02095-X. [DOI] [PubMed] [Google Scholar]
- 12.von Saint André A, Blackwell NM, Hall LR, Hoerauf A, Brattig NW, Volkmann L, Taylor MJ, Ford L, Hise AG, Lass JH, Diaconu E, Pearlman E. The role of endosymbiotic Wolbachia bacteria in the pathogenesis of river blindness. Science. 2002 Mar;295(5561):1892–1895. doi: 10.1126/science.1068732. [DOI] [PubMed] [Google Scholar]
- 13.Ette EI, Thomas WO, Achumba JI. Ivermectin: a long-acting microfilaricidal agent. DICP. 1990 Apr;24(4):426–433. doi: 10.1177/106002809002400417. [DOI] [PubMed] [Google Scholar]
- 14.Kwarteng A, Ahuno ST, Akoto FO. Killing filarial nematode parasites: role of treatment options and host immune response. Infect Dis Poverty. 2016 Oct;5(1):86. doi: 10.1186/s40249-016-0183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horton J. Albendazole: a review of anthelmintic efficacy and safety in humans. Parasitology. 2000;121 Suppl:S113–S132. doi: 10.1017/s0031182000007290. [DOI] [PubMed] [Google Scholar]
- 16.Macfarlane CL, Budhathoki SS, Johnson S, Richardson M, Garner P. Albendazole alone or in combination with microfilaricidal drugs for lymphatic filariasis. Cochrane Database Syst Rev. 2019 Jan;1:CD003753. doi: 10.1002/14651858.CD003753.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Irvine MA, Stolk WA, Smith ME, Subramanian S, Singh BK, Weil GJ, Michael E, Hollingsworth TD. Effectiveness of a triple-drug regimen for global elimination of lymphatic filariasis: a modelling study. Lancet Infect Dis. 2017 Apr;17(4):451–458. doi: 10.1016/S1473-3099(16)30467-4. [DOI] [PubMed] [Google Scholar]
- 18.Thomsen EK, Sanuku N, Baea M, Satofan S, Maki E, Lombore B, Schmidt MS, Siba PM, Weil GJ, Kazura JW, Fleckenstein LL, King CL. Efficacy, Safety, and Pharmacokinetics of Coadministered Diethylcarbamazine, Albendazole, and Ivermectin for Treatment of Bancroftian Filariasis. Clin Infect Dis. 2016 Feb;62(3):334–341. doi: 10.1093/cid/civ882. [DOI] [PubMed] [Google Scholar]
- 19.King CL, Suamani J, Sanuku N, Cheng YC, Satofan S, Mancuso B, Goss CW, Robinson LJ, Siba PM, Weil GJ, Kazura JW. A Trial of a Triple-Drug Treatment for Lymphatic Filariasis. N Engl J Med. 2018 Nov;379(19):1801–1810. doi: 10.1056/NEJMoa1706854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO. Global programme to eliminate lymphatic filariasis: progress report, 2019. Wkly Epidemiol Rec. 2020 Oct;95(43):509–523. [Google Scholar]
- 21.WHO. Progress in eliminating onchocerciasis in the WHO Region of the Americas: doxycycline treatment as an end-game strategy. Wkly Epidemiol Rec. 2019;37(94):415–419. [Google Scholar]
- 22.Taylor MJ, Awadzi K, Basáñez MG, Biritwum N, Boakye D, Boatin B, Bockarie M, Churcher TS, Debrah A, Edwards G, Hoerauf A, Mand S, Matthews G, Osei-Atweneboana M, Prichard RK, Wanji S, Adjei O. Onchocerciasis Control: Vision for the Future from a Ghanian perspective. Parasit Vectors. 2009 Jan;2(1):7. doi: 10.1186/1756-3305-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Francis H, Awadzi K, Ottesen EA. The Mazzotti reaction following treatment of onchocerciasis with diethylcarbamazine: clinical severity as a function of infection intensity. Am J Trop Med Hyg. 1985 May;34(3):529–536. doi: 10.4269/ajtmh.1985.34.529. [DOI] [PubMed] [Google Scholar]
- 24.Anderson J, Fuglsang H, de C Marshall TF. Effects of diethylcarbamazine on ocular onchocerciasis. Tropenmed Parasitol. 1976 Sep;27(3):263–278. [PubMed] [Google Scholar]
- 25.Pion SD, Filipe JA, Kamgno J, Gardon J, Basáñez MG, Boussinesq M. Microfilarial distribution of Loa loa in the human host: population dynamics and epidemiological implications. Parasitology. 2006 Jul;133(Pt 1):101–109. doi: 10.1017/S0031182006000035. [DOI] [PubMed] [Google Scholar]
- 26.Wanji S, Chounna Ndongmo WP, Fombad FF, Kengne-Ouafo JA, Njouendou AJ, Longang Tchounkeu YF, Koudou B, Bockarie M, Fobi G, Roungou JB, Enyong PA. Impact of repeated annual community directed treatment with ivermectin on loiasis parasitological indicators in Cameroon: Implications for onchocerciasis and lymphatic filariasis elimination in areas co-endemic with Loa loa in Africa. PLoS Negl Trop Dis. 2018 Sep;12(9):e0006750. doi: 10.1371/journal.pntd.0006750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO. Working to overcome the global impact of neglected tropical diseases – First WHO report on neglected tropical diseases. Geneva: WHO; 2010. [PubMed] [Google Scholar]
- 28.WHO. Elimination of human onchocerciasis: progress report, 2020. Wkly Epidemiol Rec. 2021 Nov 19;96(41):617–623. [Google Scholar]
- 29.WHO. Global programme to eliminate lymphatic filariasis: progress report, 2020. Wkly Epidemiol Rec. 2021 Oct 15;96(41):497–508. [Google Scholar]
- 30.WHO. Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization; 2020. [Google Scholar]
- 31.Awadzi K, Opoku NO, Attah SK, Lazdins-Helds J, Kuesel AC. A randomized, single-ascending-dose, ivermectin-controlled, double-blind study of moxidectin in Onchocerca volvulus infection. PLoS Negl Trop Dis. 2014 Jun;8(6):e2953. doi: 10.1371/journal.pntd.0002953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Opoku NO, Bakajika DK, Kanza EM, Howard H, Mambandu GL, Nyathirombo A, Nigo MM, Kasonia K, Masembe SL, Mumbere M, Kataliko K, Larbelee JP, Kpawor M, Bolay KM, Bolay F, Asare S, Attah SK, Olipoh G, Vaillant M, Halleux CM, Kuesel AC. Single dose moxidectin versus ivermectin for Onchocerca volvulus infection in Ghana, Liberia, and the Democratic Republic of the Congo: a randomised, controlled, double-blind phase 3 trial. Lancet. 2018 Oct;392(10154):1207–1216. doi: 10.1016/S0140-6736(17)32844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turner HC, Walker M, Attah SK, Opoku NO, Awadzi K, Kuesel AC, Basáñez MG. The potential impact of moxidectin on onchocerciasis elimination in Africa: an economic evaluation based on the Phase II clinical trial data. Parasit Vectors. 2015 Mar;8:167. doi: 10.1186/s13071-015-0779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dunn C, Callahan K, Katabarwa M, Richards F, Hopkins D, Withers PC, Jr, Buyon LE, McFarland D. The Contributions of Onchocerciasis Control and Elimination Programs toward the Achievement of the Millennium Development Goals. PLoS Negl Trop Dis. 2015 May;9(5):e0003703. doi: 10.1371/journal.pntd.0003703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Geary TG, Mackenzie CD. Progress and challenges in the discovery of macrofilaricidal drugs. Expert Rev Anti Infect Ther. 2011 Aug;9(8):681–695. doi: 10.1586/eri.11.76. [DOI] [PubMed] [Google Scholar]
- 36.Clare RH, Bardelle C, Harper P, Hong WD, Börjesson U, Johnston KL, Collier M, Myhill L, Cassidy A, Plant D, Plant H, Clark R, Cook DAN, Steven A, Archer J, McGillan P, Charoensutthivarakul S, Bibby J, Sharma R, Nixon GL, Slatko BE, Cantin L, Wu B, Turner J, Ford L, Rich K, Wigglesworth M, Berry NG, O’Neill PM, Taylor MJ, Ward SA. Industrial scale high-throughput screening delivers multiple fast acting macrofilaricides. Nat Commun. 2019 Jan;10(1):11. doi: 10.1038/s41467-018-07826-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor MJ, Makunde WH, McGarry HF, Turner JD, Mand S, Hoerauf A. Macrofilaricidal activity after doxycycline treatment of Wuchereria bancrofti: a double-blind, randomised placebo-controlled trial. Lancet. 2005 Jun 18-24;365(9477):2116–2121. doi: 10.1016/S0140-6736(05)66591-9. [DOI] [PubMed] [Google Scholar]
- 38.Foster J, Ganatra M, Kamal I, Ware J, Makarova K, Ivanova N, Bhattacharyya A, Kapatral V, Kumar S, Posfai J, Vincze T, Ingram J, Moran L, Lapidus A, Omelchenko M, Kyrpides N, Ghedin E, Wang S, Goltsman E, Joukov V, Ostrovskaya O, Tsukerman K, Mazur M, Comb D, Koonin E, Slatko B. The Wolbachia genome of Brugia malayi: endosymbiont evolution within a human pathogenic nematode. PLoS Biol. 2005 Apr;3(4):e121. doi: 10.1371/journal.pbio.0030121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fischer P, Wibowo H, Pischke S, Rückert P, Liebau E, Ismid IS, Supali T. PCR-based detection and identification of the filarial parasite Brugia timori from Alor Island, Indonesia. Ann Trop Med Parasitol. 2002 Dec;96(8):809–821. doi: 10.1179/000349802125002239. [DOI] [PubMed] [Google Scholar]
- 40.Batsa Debrah L, Phillips RO, Pfarr K, Klarmann-Schulz U, Opoku VS, Nausch N, Owusu W, Mubarik Y, Sander AL, Lämmer C, Ritter M, Layland LE, Jacobsen M, Debrah AY, Hoerauf A. The Efficacy of Doxycycline Treatment on Infection: An Open-Label, Randomized Trial in Ghana. Am J Trop Med Hyg. 2019 Jul;101(1):84–92. doi: 10.4269/ajtmh.18-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coulibaly YI, Dembele B, Diallo AA, Lipner EM, Doumbia SS, Coulibaly SY, Konate S, Diallo DA, Yalcouye D, Kubofcik J, Doumbo OK, Traore AK, Keita AD, Fay MP, Traore SF, Nutman TB, Klion AD. A randomized trial of doxycycline for Mansonella perstans infection. N Engl J Med. 2009 Oct;361(15):1448–1458. doi: 10.1056/NEJMoa0900863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Casiraghi M, Favia G, Cancrini G, Bartoloni A, Bandi C. Molecular identification of Wolbachia from the filarial nematode Mansonella ozzardi. Parasitol Res. 2001 May;87(5):417–420. doi: 10.1007/s004360000368. [DOI] [PubMed] [Google Scholar]
- 43.Büttner DW, Wanji S, Bazzocchi C, Bain O, Fischer P. Obligatory symbiotic Wolbachia endobacteria are absent from Loa loa. Filaria J. 2003 May;2(1):10. doi: 10.1186/1475-2883-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henkle-Dührsen K, Eckelt VH, Wildenburg G, Blaxter M, Walter RD. Gene structure, activity and localization of a catalase from intracellular bacteria in Onchocerca volvulus. Mol Biochem Parasitol. 1998 Oct;96(1-2):69–81. doi: 10.1016/s0166-6851(98)00109-1. [DOI] [PubMed] [Google Scholar]
- 45.Langworthy NG, Renz A, Mackenstedt U, Henkle-Dührsen K, de Bronsvoort MB, Tanya VN, Donnelly MJ, Trees AJ. Macrofilaricidal activity of tetracycline against the filarial nematode Onchocerca ochengi: elimination of Wolbachia precedes worm death and suggests a dependent relationship. Proc Biol Sci. 2000 Jun;267(1448):1063–1069. doi: 10.1098/rspb.2000.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Townson S, Hutton D, Siemienska J, Hollick L, Scanlon T, Tagboto SK, Taylor MJ. Antibiotics and Wolbachia in filarial nematodes: antifilarial activity of rifampicin, oxytetracycline and chloramphenicol against Onchocerca gutturosa, Onchocerca lienalis and Brugia pahangi. Ann Trop Med Parasitol. 2000 Dec;94(8):801–816. doi: 10.1080/00034980020027988. [DOI] [PubMed] [Google Scholar]
- 47.Bandi C, McCall JW, Genchi C, Corona S, Venco L, Sacchi L. Effects of tetracycline on the filarial worms Brugia pahangi and Dirofilaria immitis and their bacterial endosymbionts Wolbachia. Int J Parasitol. 1999 Feb;29(2):357–364. doi: 10.1016/s0020-7519(98)00200-8. [DOI] [PubMed] [Google Scholar]
- 48.Taylor MJ, Bilo K, Cross HF, Archer JP, Underwood AP. 16S rDNA phylogeny and ultrastructural characterization of Wolbachia intracellular bacteria of the filarial nematodes Brugia malayi, B. pahangi, and Wuchereria bancrofti. Exp Parasitol. 1999 Apr;91(4):356–361. doi: 10.1006/expr.1998.4383. [DOI] [PubMed] [Google Scholar]
- 49.Sironi M, Bandi C, Sacchi L, Di Sacco B, Damiani G, Genchi C. Molecular evidence for a close relative of the arthropod endosymbiont Wolbachia in a filarial worm. Mol Biochem Parasitol. 1995;74(2):223–227. doi: 10.1016/0166-6851(95)02494-8. [DOI] [PubMed] [Google Scholar]
- 50.Grandi G, Morchon R, Kramer L, Kartashev V, Simon F. Wolbachia in Dirofilaria repens, an agent causing human subcutaneous dirofilariasis. J Parasitol. 2008 Dec;94(6):1421–1423. doi: 10.1645/GE-1575.1. [DOI] [PubMed] [Google Scholar]
- 51.Hoerauf A, Nissen-Pähle K, Schmetz C, Henkle-Dührsen K, Blaxter ML, Büttner DW, Gallin MY, Al-Qaoud KM, Lucius R, Fleischer B. Tetracycline therapy targets intracellular bacteria in the filarial nematode Litomosoides sigmodontis and results in filarial infertility. J Clin Invest. 1999 Jan;103(1):11–18. doi: 10.1172/JCI4768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kozek WJ, Marroquin HF. Intracytoplasmic bacteria in Onchocerca volvulus. Am J Trop Med Hyg. 1977 Jul;26(4):663–678. doi: 10.4269/ajtmh.1977.26.663. [DOI] [PubMed] [Google Scholar]
- 53.Tamarozzi F, Halliday A, Gentil K, Hoerauf A, Pearlman E, Taylor MJ. Onchocerciasis: the role of Wolbachia bacterial endosymbionts in parasite biology, disease pathogenesis, and treatment. Clin Microbiol Rev. 2011 Jul;24(3):459–468. doi: 10.1128/CMR.00057-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ghedin E, Wang S, Foster JM, Slatko BE. First sequenced genome of a parasitic nematode. Trends Parasitol. 2004 Apr;20(4):151–153. doi: 10.1016/j.pt.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 55.Ghedin E, Wang S, Spiro D, Caler E, Zhao Q, Crabtree J, Allen JE, Delcher AL, Guiliano DB, Miranda-Saavedra D, Angiuoli SV, Creasy T, Amedeo P, Haas B, El-Sayed NM, Wortman JR, Feldblyum T, Tallon L, Schatz M, Shumway M, Koo H, Salzberg SL, Schobel S, Pertea M, Pop M, White O, Barton GJ, Carlow CK, Crawford MJ, Daub J, Dimmic MW, Estes CF, Foster JM, Ganatra M, Gregory WF, Johnson NM, Jin J, Komuniecki R, Korf I, Kumar S, Laney S, Li BW, Li W, Lindblom TH, Lustigman S, Ma D, Maina CV, Martin DM, McCarter JP, McReynolds L, Mitreva M, Nutman TB, Parkinson J, Peregrín-Alvarez JM, Poole C, Ren Q, Saunders L, Sluder AE, Smith K, Stanke M, Unnasch TR, Ware J, Wei AD, Weil G, Williams DJ, Zhang Y, Williams SA, Fraser-Liggett C, Slatko B, Blaxter ML, Scott AL. Draft genome of the filarial nematode parasite Brugia malayi. Science. 2007 Sep;317(5845):1756–1760. doi: 10.1126/science.1145406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu B, Novelli J, Foster J, Vaisvila R, Conway L, Ingram J, Ganatra M, Rao AU, Hamza I, Slatko B. The heme biosynthetic pathway of the obligate Wolbachia endosymbiont of Brugia malayi as a potential anti-filarial drug target. PLoS Negl Trop Dis. 2009 Jul;3(7):e475. doi: 10.1371/journal.pntd.0000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li Z, Carlow CK. Characterization of transcription factors that regulate the type IV secretion system and riboflavin biosynthesis in Wolbachia of Brugia malayi. PLoS One. 2012;7(12):e51597. doi: 10.1371/journal.pone.0051597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Strübing U, Lucius R, Hoerauf A, Pfarr KM. Mitochondrial genes for heme-dependent respiratory chain complexes are up-regulated after depletion of Wolbachia from filarial nematodes. Int J Parasitol. 2010 Aug;40(10):1193–1202. doi: 10.1016/j.ijpara.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 59.Hoerauf A, Volkmann L, Nissen-Paehle K, Schmetz C, Autenrieth I, Büttner DW, Fleischer B. Targeting of Wolbachia endobacteria in Litomosoides sigmodontis: comparison of tetracyclines with chloramphenicol, macrolides and ciprofloxacin. Trop Med Int Health. 2000 Apr;5(4):275–279. [PubMed] [Google Scholar]
- 60.Hoerauf A, Mand S, Fischer K, Kruppa T, Marfo-Debrekyei Y, Debrah AY, Pfarr KM, Adjei O, Büttner DW. Doxycycline as a novel strategy against bancroftian filariasis-depletion of Wolbachia endosymbionts from Wuchereria bancrofti and stop of microfilaria production. Med Microbiol Immunol. 2003 Nov;192(4):211–216. doi: 10.1007/s00430-002-0174-6. [DOI] [PubMed] [Google Scholar]
- 61.Debrah AY, Mand S, Specht S, Marfo-Debrekyei Y, Batsa L, Pfarr K, Larbi J, Lawson B, Taylor M, Adjei O, Hoerauf A. Doxycycline reduces plasma VEGF-C/sVEGFR-3 and improves pathology in lymphatic filariasis. PLoS Pathog. 2006 Sep;2(9):e92. doi: 10.1371/journal.ppat.0020092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Debrah AY, Mand S, Marfo-Debrekyei Y, Batsa L, Pfarr K, Buttner M, Adjei O, Buttner D, Hoerauf A. Macrofilaricidal effect of 4 weeks of treatment with doxycycline on Wuchereria bancrofti. Trop Med Int Health. 2007 Dec;12(12):1433–1441. doi: 10.1111/j.1365-3156.2007.01949.x. [DOI] [PubMed] [Google Scholar]
- 63.Turner JD, Mand S, Debrah AY, Muehlfeld J, Pfarr K, McGarry HF, Adjei O, Taylor MJ, Hoerauf A. A randomized, double-blind clinical trial of a 3-week course of doxycycline plus albendazole and ivermectin for the treatment of Wuchereria bancrofti infection. Clin Infect Dis. 2006 Apr;42(8):1081–1089. doi: 10.1086/501351. [DOI] [PubMed] [Google Scholar]
- 64.Hoerauf A, Mand S, Volkmann L, Büttner M, Marfo-Debrekyei Y, Taylor M, Adjei O, Büttner DW. Doxycycline in the treatment of human onchocerciasis: Kinetics of Wolbachia endobacteria reduction and of inhibition of embryogenesis in female Onchocerca worms. Microbes Infect. 2003 Apr;5(4):261–273. doi: 10.1016/s1286-4579(03)00026-1. [DOI] [PubMed] [Google Scholar]
- 65.Hoerauf A, Specht S, Büttner M, Pfarr K, Mand S, Fimmers R, Marfo-Debrekyei Y, Konadu P, Debrah AY, Bandi C, Brattig N, Albers A, Larbi J, Batsa L, Taylor MJ, Adjei O, Büttner DW. Wolbachia endobacteria depletion by doxycycline as antifilarial therapy has macrofilaricidal activity in onchocerciasis: a randomized placebo-controlled study. Med Microbiol Immunol. 2008 Sep;197(3):335. doi: 10.1007/s00430-007-0072-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Specht S, Hoerauf A, Adjei O, Debrah A, Büttner DW. Newly acquired Onchocerca volvulus filariae after doxycycline treatment. Parasitol Res. 2009 Dec;106(1):23–31. doi: 10.1007/s00436-009-1624-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hoerauf A, Specht S, Marfo-Debrekyei Y, Büttner M, Debrah AY, Mand S, Batsa L, Brattig N, Konadu P, Bandi C, Fimmers R, Adjei O, Büttner DW. Efficacy of 5-week doxycycline treatment on adult Onchocerca volvulus. Parasitol Res. 2009 Jan;104(2):437–447. doi: 10.1007/s00436-008-1217-8. [DOI] [PubMed] [Google Scholar]
- 68.Debrah AY, Mand S, Marfo-Debrekyei Y, Larbi J, Adjei O, Hoerauf A. Assessment of microfilarial loads in the skin of onchocerciasis patients after treatment with different regimens of doxycycline plus ivermectin. Filaria J. 2006 Feb;5:1. doi: 10.1186/1475-2883-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Turner JD, Tendongfor N, Esum M, Johnston KL, Langley RS, Ford L, Faragher B, Specht S, Mand S, Hoerauf A, Enyong P, Wanji S, Taylor MJ. Macrofilaricidal activity after doxycycline only treatment of Onchocerca volvulus in an area of Loa loa co-endemicity: a randomized controlled trial. PLoS Negl Trop Dis. 2010;4(4):e660. doi: 10.1371/journal.pntd.0000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gardon J, Gardon-Wendel N, Demanga N, Kamgno J, Chippaux JP, Boussinesq M. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997;350(9070):18–22. doi: 10.1016/S0140-6736(96)11094-1. [DOI] [PubMed] [Google Scholar]
- 71.Wanji S, Tendongfor N, Nji T, Esum M, Che JN, Nkwescheu A, Alassa F, Kamnang G, Enyong PA, Taylor MJ, Hoerauf A, Taylor DW. Community-directed delivery of doxycycline for the treatment of onchocerciasis in areas of co-endemicity with loiasis in Cameroon. Parasit Vectors. 2009 Aug;2(1):39. doi: 10.1186/1756-3305-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.CDC. Parasites – Onchocerciasis (also known as River Blindness) [last updated 2021 Nov 10]. Available from: https://www.cdc.gov/parasites/onchocerciasis/health_professionals/index.html.
- 73.Mand S, Debrah AY, Klarmann U, Batsa L, Marfo-Debrekyei Y, Kwarteng A, Specht S, Belda-Domene A, Fimmers R, Taylor M, Adjei O, Hoerauf A. Doxycycline improves filarial lymphedema independent of active filarial infection: a randomized controlled trial. Clin Infect Dis. 2012 Sep;55(5):621–630. doi: 10.1093/cid/cis486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoerauf A. Filariasis: new drugs and new opportunities for lymphatic filariasis and onchocerciasis. Curr Opin Infect Dis. 2008 Dec;21(6):673–681. doi: 10.1097/QCO.0b013e328315cde7. [DOI] [PubMed] [Google Scholar]
- 75.Dadzie KY, Remme J, Rolland A, Thylefors B. Ocular onchocerciasis and intensity of infection in the community. II. West African rainforest foci of the vector Simulium yahense. Trop Med Parasitol. 1989 Sep;40(3):348–354. [PubMed] [Google Scholar]
- 76.Haselow NJ, Akame J, Evini C, Akongo S. Programmatic and Communication Issues in Relation to Serious Adverse Events Following Ivermectin Treatment in areas Co-endemic for Onchocerciasis and Loiasis. Filaria J. 2003 Oct;2 Suppl 1:S10. doi: 10.1186/1475-2883-2-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.WHO. Progress in eliminating onchocerciasis in the WHO Region of the Americas: doxycycline treatment as an end-game strategy. Wkly Epidemiol Rec. 2019;94(37):415–419. [Google Scholar]
- 78.Serrano-Parreño B, Carretón E, Caro-Vadillo A, Falcón-Cordón S, Falcón-Cordón Y, Montoya-Alonso JA. Pulmonary hypertension in dogs with heartworm before and after the adulticide protocol recommended by the American Heartworm Society. Vet Parasitol. 2017 Mar;236:34–37. doi: 10.1016/j.vetpar.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 79.Volkmann L, Fischer K, Taylor M, Hoerauf A. Antibiotic therapy in murine filariasis (Litomosoides sigmodontis): comparative effects of doxycycline and rifampicin on Wolbachia and filarial viability. Trop Med Int Health. 2003 May;8(5):392–401. doi: 10.1046/j.1365-3156.2003.01040.x. [DOI] [PubMed] [Google Scholar]
- 80.Specht S, Mand S, Marfo-Debrekyei Y, Debrah AY, Konadu P, Adjei O, Büttner DW, Hoerauf A. Efficacy of 2- and 4-week rifampicin treatment on the Wolbachia of Onchocerca volvulus. Parasitol Res. 2008 Nov;103(6):1303–1309. doi: 10.1007/s00436-008-1133-y. [DOI] [PubMed] [Google Scholar]
- 81.Aljayyoussi G, Tyrer HE, Ford L, Sjoberg H, Pionnier N, Waterhouse D, Davies J, Gamble J, Metuge H, Cook DAN, Steven A, Sharma R, Guimaraes AF, Clare RH, Cassidy A, Johnston KL, Myhill L, Hayward L, Wanji S, Turner JD, Taylor MJ, Ward SA. Short-Course, High-Dose Rifampicin Achieves Wolbachia Depletion Predictive of Curative Outcomes in Preclinical Models of Lymphatic Filariasis and Onchocerciasis. Sci Rep. 2017 Mar;7(1):210. doi: 10.1038/s41598-017-00322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Boeree MJ, Diacon AH, Dawson R, Narunsky K, du Bois J, Venter A, Phillips PP, Gillespie SH, McHugh TD, Hoelscher M, Heinrich N, Rehal S, van Soolingen D, van Ingen J, Magis-Escurra C, Burger D, Plemper van Balen G, Aarnoutse RE PanACEA Consortium. A dose-ranging trial to optimize the dose of rifampin in the treatment of tuberculosis. Am J Respir Crit Care Med. 2015 May;191(9):1058–1065. doi: 10.1164/rccm.201407-1264OC. [DOI] [PubMed] [Google Scholar]
- 83.Boeree MJ, Heinrich N, Aarnoutse R, Diacon AH, Dawson R, Rehal S, Kibiki GS, Churchyard G, Sanne I, Ntinginya NE, Minja LT, Hunt RD, Charalambous S, Hanekom M, Semvua HH, Mpagama SG, Manyama C, Mtafya B, Reither K, Wallis RS, Venter A, Narunsky K, Mekota A, Henne S, Colbers A, van Balen GP, Gillespie SH, Phillips PPJ, Hoelscher M PanACEA consortium. High-dose rifampicin, moxifloxacin, and SQ109 for treating tuberculosis: a multi-arm, multi-stage randomised controlled trial. Lancet Infect Dis. 2017 Jan;17(1):39–49. doi: 10.1016/S1473-3099(16)30274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Velásquez GE, Brooks MB, Coit JM, Pertinez H, Vargas Vásquez D, Sánchez Garavito E, Calderón RI, Jiménez J, Tintaya K, Peloquin CA, Osso E, Tierney DB, Seung KJ, Lecca L, Davies GR, Mitnick CD. Efficacy and Safety of High-Dose Rifampin in Pulmonary Tuberculosis. A Randomized Controlled Trial. Am J Respir Crit Care Med. 2018 Sep;198(5):657–666. doi: 10.1164/rccm.201712-2524OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.U.S. Department of Health and Human Services Food and Drug Administration. Determining the Extent of Safety Data Collection Needed in Late-Stage Premarket and Postapproval Clinical Investigations. Silver Spring: FDA; 2016. Available from: https://www.fda.gov/media/82664/download. [Google Scholar]
- 86.Grüneberg RN, Emmerson AM, Cremer AW. Rifampicin for non-tuberculous infections? Chemotherapy. 1985;31(4):324–328. doi: 10.1159/000238355. [DOI] [PubMed] [Google Scholar]
- 87.ISRCTN38954299 – The efficacy of rifampicin plus albendazole against river blindness (onchocerciasis) in Cameroon. ISRCTN registry. 2021. [last updated 2021 Dec 10]. Available from: https://www.isrctn.com/ISRCTN38954299.
- 88.Taylor MJ, von Geldern TW, Ford L, Hübner MP, Marsh K, Johnston KL, Sjoberg HT, Specht S, Pionnier N, Tyrer HE, Clare RH, Cook DAN, Murphy E, Steven A, Archer J, Bloemker D, Lenz F, Koschel M, Ehrens A, Metuge HM, Chunda VC, Ndongmo Chounna PW, Njouendou AJ, Fombad FF, Carr R, Morton HE, Aljayyoussi G, Hoerauf A, Wanji S, Kempf DJ, Turner JD, Ward SA. Preclinical development of an oral anti-macrolide drug for the treatment of lymphatic filariasis and onchocerciasis. Sci Transl Med. 2019 Mar;11(483):eaau2086. doi: 10.1126/scitranslmed.aau2086. [DOI] [PubMed] [Google Scholar]
- 89.von Geldern TW, Morton HE, Clark RF, Brown BS, Johnston KL, Ford L, Specht S, Carr RA, Stolarik DF, Ma J, Rieser MJ, Struever D, Frohberger SJ, Koschel M, Ehrens A, Turner JD, Hübner MP, Hoerauf A, Taylor MJ, Ward SA, Marsh K, Kempf DJ. Discovery of ABBV-4083, a novel analog of Tylosin A that has potent anti-Wolbachia and anti-filarial activity. PLoS Negl Trop Dis. 2019 Feb 28;13(2):e0007159. doi: 10.1371/journal.pntd.0007159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hübner MP, Koschel M, Struever D, Nikolov V, Frohberger SJ, Ehrens A, Fendler M, Johannes I, von Geldern TW, Marsh K, Turner JD, Taylor MJ, Ward SA, Pfarr K, Kempf DJ, Hoerauf A. In vivo kinetics of Wolbachia depletion by ABBV-4083 in L. sigmodontis adult worms and microfilariae. PLoS Negl Trop Dis. 2019 Aug 5;13(8):e0007636. doi: 10.1371/journal.pntd.0007636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Drugs for Neglected Diseases Initiative (DNDi) Filaria: river blindness – Tylamac (ABBV-4083) 2015. [last updated 2022 Mar 1]. Available from: https://www.dndi.org/diseases-projects/portfolio/abbv-4083/
- 92.Alami NN, Carter DC, Kwatra NV, Zhao W, Snodgrass L, Porcalla AR, Klein CE, Cohen DE, Gallenberg LA, Carr RA, Marsh KC, Kempf DJ. Anti-Wolbachia Candidate ABBV-4083: Phase 1 Safety and Pharmacokinetics Clinical Trial in healthy Adults. 68th Annual Meeting of the American Society for Tropical Medicine and Hygiene; National Harbor, MD, USA; 2019 Nov 20–24. Abstract 1280 [Google Scholar]
- 93.Study to Assess Adverse Events, Change in Disease Activity and How Oral ABBV-4083 Capsules When Given Alone or In Combination With Albendazole Capsules Moves in The Body of Adult Participants With Onchocerca Volvulus Infection. NCT04913610. ClinicalTrials.gov. 2021. [last updated 2021 Jun 25]. Available from: https://clinicaltrials.gov/ct2/show/NCT04913610.
- 94.Hübner MP, Von Geldern TW, Marsh K, Specht S, Koschel M, Ehrens A, Frohberger SJ, Gunderson E, Bulman C, Lim KC, Taylor MJ, Turner JD, Ward SA, Sakanari J, Kempf D, Hoerauf A. Preclincial efficacy of the novel macrofilaricidal drug candidate ABBV-4083. 68th Annual Meeting of the American Society for Tropical Medicine and Hygiene; National Harbor, MD, USA; 2019 Nov 20–24. Abstract 1281 [Google Scholar]
- 95.Gonzalez AE, Bustos JA, Jimenez JA, Rodriguez ML, Ramirez MG, Gilman RH, Garcia HH Cysticercosis Working Group in Peru. Efficacy of diverse antiparasitic treatments for cysticercosis in the pig model. Am J Trop Med Hyg. 2012 Aug;87(2):292–296. doi: 10.4269/ajtmh.2012.11-0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hübner MP, Ehrens A, Koschel M, Dubben B, Lenz F, Frohberger SJ, Specht S, Quirynen L, Lachau-Durand S, Tekle F, Baeten B, Engelen M, Mackenzie CD, Hoerauf A. Macrofilaricidal efficacy of single and repeated oral and subcutaneous doses of flubendazole in Litomosoides sigmodontis infected jirds. PLoS Negl Trop Dis. 2019 Jan;13(1):e0006320. doi: 10.1371/journal.pntd.0006320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Reddy AB, Rao UR, Chandrashekar R, Shrivastava R, Subrahmanyam D. Comparative efficacy of some benzimidazoles and amoscanate (Go.9333) against experimental filarial infections. Tropenmed Parasitol. 1983 Dec;34(4):259–262. [PubMed] [Google Scholar]
- 98.Surin J, Denham DA. Comparative susceptibility to anthelmintics of Brugia pahangi in jirds infected by different methods. J Helminthol. 1990 Sep;64(3):232–238. doi: 10.1017/s0022149x00012219. [DOI] [PubMed] [Google Scholar]
- 99.Hübner MP, Martin C, Specht S, Koschel M, Dubben B, Frohberger SJ, Ehrens A, Fendler M, Struever D, Mitre E, Vallarino-Lhermitte N, Gokool S, Lustigman S, Schneider M, Townson S, Hoerauf A, Scandale I. Oxfendazole mediates macrofilaricidal efficacy against the filarial nematode Litomosoides sigmodontis in vivo and inhibits Onchocerca spec. motility in vitro. PLoS Negl Trop Dis. 2020 Jul;14(7):e0008427. doi: 10.1371/journal.pntd.0008427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lachau-Durand S, Lammens L, van der Leede BJ, Van Gompel J, Bailey G, Engelen M, Lampo A. Preclinical toxicity and pharmacokinetics of a new orally bioavailable flubendazole formulation and the impact for clinical trials and risk/benefit to patients. PLoS Negl Trop Dis. 2019 Jan;13(1):e0007026. doi: 10.1371/journal.pntd.0007026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Russell GJ, Gill JH, Lacey E. Binding of [3H]benzimidazole carbamates to mammalian brain tubulin and the mechanism of selective toxicity of the benzimidazole anthelmintics. Biochem Pharmacol. 1992;43(5):1095–1100. doi: 10.1016/0006-2952(92)90617-r. [DOI] [PubMed] [Google Scholar]
- 102.Tweats DJ, Johnson GE, Scandale I, Whitwell J, Evans DB. Genotoxicity of flubendazole and its metabolites in vitro and the impact of a new formulation on in vivo aneugenicity. Mutagenesis. 2016 May;31(3):309–321. doi: 10.1093/mutage/gev070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Codd EE, Ng HH, McFarlane C, Riccio ES, Doppalapudi R, Mirsalis JC, Horton RJ, Gonzalez AE, Garcia HH, Gilman RH Cysticercosis Working Group in Peru. Preclinical studies on the pharmacokinetics, safety, and toxicology of oxfendazole: toward first in human studies. Int J Toxicol. 2015 Mar-Apr;34(2):129–137. doi: 10.1177/1091581815569582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Morgan DW. Toxicity study of oxfendazole in pregnant sows. Vet Rec. 1982 Aug;111(8):161–163. doi: 10.1136/vr.111.8.161. [DOI] [PubMed] [Google Scholar]
- 105.Multiple Ascending Dose Study of Oxfendazole in Healthy Adult Volunteers. NCT03035760. ClinicalTrials.gov. 2017. [last updated 2019 Dec 17]. Available from: https://clinicaltrials.gov/ct2/show/NCT03035760.
- 106.Bach T, Galbiati S, Kennedy JK, Deye G, Nomicos EYH, Codd EE, Garcia HH, Horton J, Gilman RH, Gonzalez AE, Winokur P, An G. Pharmacokinetics, Safety, and Tolerability of Oxfendazole in Healthy Adults in an Open-Label Phase 1 Multiple Ascending Dose and Food Effect Study. Antimicrob Agents Chemother. 2020 Oct 20;64(11):e01018–e01020. doi: 10.1128/AAC.01018-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.An G, Murry DJ, Gajurel K, Bach T, Deye G, Stebounova LV, Codd EE, Horton J, Gonzalez AE, Garcia HH, Ince D, Hodgson-Zingman D, Nomicos EYH, Conrad T, Kennedy J, Jones W, Gilman RH, Winokur P. Pharmacokinetics, Safety, and Tolerability of Oxfendazole in Healthy Volunteers: a Randomized, Placebo-Controlled First-in-Human Single-Dose Escalation Study. Antimicrob Agents Chemother. 2019 Apr;63(4):e02255–e02218. doi: 10.1128/AAC.02255-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pionnier NP, Sjoberg H, Chunda VC, Fombad FF, Chounna PW, Njouendou AJ, Metuge HM, Ndzeshang BL, Gandjui NV, Akumtoh DN, Tayong DB, Taylor MJ, Wanji S, Turner JD. Mouse models of Loa loa. Nat Commun. 2019 Mar;10(1):1429. doi: 10.1038/s41467-019-09442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Helminth Elimination Platform (HELP) Developing new drugs for infections caused by parasitic worms. [last accessed 2022 Mar 22]. Available from: https://eliminateworms.org/
- 110.Helminth Elimination Platform (HELP) River blindness (Onchocerciasis) [last accessed 2022 Mar 22]. Available from: https://eliminateworms.org/diseases/river-blindness/
- 111.García HH, Evans CA, Nash TE, Takayanagui OM, White AC, Jr, Botero D, Rajshekhar V, Tsang VC, Schantz PM, Allan JC, Flisser A, Correa D, Sarti E, Friedland JS, Martinez SM, Gonzalez AE, Gilman RH, Del Brutto OH. Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002 Oct;15(4):747–756. doi: 10.1128/CMR.15.4.747-756.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.CDC. Parasites – Cysticercosis: Resources for Health Professionals. [last reviewed 2020 Oct 22]. Available from: https://www.cdc.gov/parasites/cysticercosis/health_professionals/index.html.
- 113.Krücken J, Harder A, Jeschke P, Holden-Dye L, O’Connor V, Welz C, von Samson-Himmelstjerna G. Anthelmintic cyclcooctadepsipeptides: complex in structure and mode of action. Trends Parasitol. 2012 Sep;28(9):385–394. doi: 10.1016/j.pt.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 114.von Samson-Himmelstjerna G, Harder A, Sangster NC, Coles GC. Efficacy of two cyclooctadepsipeptides, PF1022A and emodepside, against anthelmintic-resistant nematodes in sheep and cattle. Parasitology. 2005 Mar;130(Pt 3):343–347. doi: 10.1017/s0031182004006523. [DOI] [PubMed] [Google Scholar]
- 115.Krücken J, Holden-Dye L, Keiser J, Prichard RK, Townson S, Makepeace BL, Hübner MP, Hahnel SR, Scandale I, Harder A, Kulke D. Development of emodepside as a possible adulticidal treatment for human onchocerciasis – The fruit of a successful industrial-academic collaboration. PLoS Pathog. 2021 Jul;17(7):e1009682. doi: 10.1371/journal.ppat.1009682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kulke D, von Samson-Himmelstjerna G, Miltsch SM, Wolstenholme AJ, Jex AR, Gasser RB, Ballesteros C, Geary TG, Keiser J, Townson S, Harder A, Krücken J. Characterization of the Ca2+-gated and voltage-dependent K+-channel Slo-1 of nematodes and its interaction with emodepside. PLoS Negl Trop Dis. 2014 Dec;8(12):e3401. doi: 10.1371/journal.pntd.0003401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hübner MP, Townson S, Gokool S, Tagboto S, Maclean MJ, Verocai GG, Wolstenholme AJ, Frohberger SJ, Hoerauf A, Specht S, Scandale I, Harder A, Glenschek-Sieberth M, Hahnel SR, Kulke D. Evaluation of the in vitro susceptibility of various filarial nematodes to emodepside. Int J Parasitol Drugs Drug Resist. 2021 Dec;17:27–35. doi: 10.1016/j.ijpddr.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zahner H, Taubert A, Harder A, von Samson-Himmelstjerna G. Filaricidal efficacy of anthelmintically active cyclodepsipeptides. Int J Parasitol. 2001 Nov;31(13):1515–1522. doi: 10.1016/s0020-7519(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 119.Townson S, Freeman A, Harris A, Harder A. Activity of the Cyclooctadepsipeptide Emodepside against Onchocerca guttorosa, Onchocerca lienalis and Brugia pahangi. American Society of Tropical Medicine and Hygiene 54th Annual Meeting; Washington, DC, USA; 2005 Dec 11-15. [Google Scholar]
- 120.Bah GS, Schneckener S, Hahnel SR, Bayang NH, Fieseler H, Schmuck GM, Krebber R, Sarr A, Terjung C, Ngangyung HF, Ekale DD, Mfopit YM, Rufener L, Graham-Brown J, Tanya VN, Glenschek-Sieberth M, Kulke D, Makepeace BL. Emodepside targets SLO-1 channels of Onchocerca ochengi and induces broad anthelmintic effects in a bovine model of onchocerciasis. PLoS Pathog. 2021 Jun 2;17(6):e1009601. doi: 10.1371/journal.ppat.1009601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.DNDi. R&D Portfolio Update February 2019: DNDi Filarial diseases programme. Feb 21, 2019. Available from: https://dndi.org/news/2019/filaria-rnd-status-2019/
- 122.Finkelstein AE, Walz DT, Batista V, Mizraji M, Roisman F, Misher A. Auranofin. New oral gold compound for treatment of rheumatoid arthritis. Ann Rheum Dis. 1976;35(3):251–257. doi: 10.1136/ard.35.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Katz WA, Alexander S, Bland JH, Blechman W, Bluhm GB, Bonebrake RA, Falbo A, Greenwald RA, Hartman S, Hobbs T, Indenbaum S, Lergier JE, Lanier BG, Lightfoot RW, Jr, Phelps P, Sheon RP, Torretti D, Wenger ME, Wilske K. The efficacy and safety of auranofin compared to placebo in rheumatoid arthritis. J Rheumatol Suppl. 1982 Jul-Aug;8:173–178. [PubMed] [Google Scholar]
- 124.Bulman CA, Bidlow CM, Lustigman S, Cho-Ngwa F, Williams D, Rascón AA, Jr, Tricoche N, Samje M, Bell A, Suzuki B, Lim KC, Supakorndej N, Supakorndej P, Wolfe AR, Knudsen GM, Chen S, Wilson C, Ang KH, Arkin M, Gut J, Franklin C, Marcellino C, McKerrow JH, Debnath A, Sakanari JA. Repurposing auranofin as a lead candidate for treatment of lymphatic filariasis and onchocerciasis. PLoS Negl Trop Dis. 2015 Feb;9(2):e0003534. doi: 10.1371/journal.pntd.0003534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Song L, Li J, Xie S, Qian C, Wang J, Zhang W, Yin X, Hua Z, Yu C. Thioredoxin glutathione reductase as a novel drug target: evidence from Schistosoma japonicum. PLoS One. 2012;7(2):e31456. doi: 10.1371/journal.pone.0031456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Capparelli EV, Bricker-Ford R, Rogers MJ, McKerrow JH, Reed SL. Phase I Clinical Trial Results of Auranofin, a Novel Antiparasitic Agent. Antimicrob Agents Chemother. 2016 Dec 27;61(1):e01947–e01916. doi: 10.1128/AAC.01947-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Schäberle TF, Schmitz A, Zocher G, Schiefer A, Kehraus S, Neu E, Roth M, Vassylyev DG, Stehle T, Bierbaum G, Hoerauf A, Pfarr K, König GM. Insights into Structure-Activity Relationships of Bacterial RNA Polymerase Inhibiting Corallopyronin Derivatives. J Nat Prod. 2015 Oct;78(10):2505–2509. doi: 10.1021/acs.jnatprod.5b00175. [DOI] [PubMed] [Google Scholar]
- 128.Belogurov GA, Vassylyeva MN, Sevostyanova A, Appleman JR, Xiang AX, Lira R, Webber SE, Klyuyev S, Nudler E, Artsimovitch I, Vassylyev DG. Transcription inactivation through local refolding of the RNA polymerase structure. Nature. 2009 Jan;457(7227):332–335. doi: 10.1038/nature07510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mukhopadhyay J, Das K, Ismail S, Koppstein D, Jang M, Hudson B, Sarafianos S, Tuske S, Patel J, Jansen R, Irschik H, Arnold E, Ebright RH. The RNA polymerase “switch region” is a target for inhibitors. Cell. 2008 Oct;135(2):295–307. doi: 10.1016/j.cell.2008.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Irschik H, Jansen R, Höfle G, Gerth K, Reichenbach H. The corallopyronins, new inhibitors of bacterial RNA synthesis from Myxobacteria. J Antibiot (Tokyo) 1985 Feb;38(2):145–152. doi: 10.7164/antibiotics.38.145. [DOI] [PubMed] [Google Scholar]
- 131.Rentsch A, Kalesse M. The total synthesis of corallopyronin A and myxopyronin B. Angew Chem Int Ed Engl. 2012 Nov 5;51(45):11381–11384. doi: 10.1002/anie.201206560. [DOI] [PubMed] [Google Scholar]
- 132.Schiefer A, Schmitz A, Schäberle TF, Specht S, Lämmer C, Johnston KL, Vassylyev DG, König GM, Hoerauf A, Pfarr K. Corallopyronin A specifically targets and depletes essential obligate Wolbachia endobacteria from filarial nematodes in vivo. J Infect Dis. 2012 Jul;206(2):249–257. doi: 10.1093/infdis/jis341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Schiefer A, Hübner MP, Krome A, Lämmer C, Ehrens A, Aden T, Koschel M, Neufeld H, Chaverra-Muñoz L, Jansen R, Kehraus S, König GM, Pogorevc D, Müller R, Stadler M, Hüttel S, Hesterkamp T, Wagner K, Pfarr K, Hoerauf A. Corallopyronin A for short-course anti-wolbachial, macrofilaricidal treatment of filarial infections. PLoS Negl Trop Dis. 2020 Dec;14(12):e0008930. doi: 10.1371/journal.pntd.0008930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hong WD, Benayoud F, Nixon GL, Ford L, Johnston KL, Clare RH, Cassidy A, Cook DAN, Siu A, Shiotani M, Webborn PJH, Kavanagh S, Aljayyoussi G, Murphy E, Steven A, Archer J, Struever D, Frohberger SJ, Ehrens A, Hübner MP, Hoerauf A, Roberts AP, Hubbard ATM, Tate EW, Serwa RA, Leung SC, Qie L, Berry NG, Gusovsky F, Hemingway J, Turner JD, Taylor MJ, Ward SA, O’Neill PM. AWZ1066S, a highly specific anti-Wolbachia drug candidate for a short-course treatment of filariasis. Proc Natl Acad Sci U S A. 2019 Jan;116(4):1414–1419. doi: 10.1073/pnas.1816585116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Development of AWZ1066S, a Small Molecule Anti-Wolbachia Candidate Macrofilaricide Drug (AWOL). NCT05084560. ClinicalTrials.gov. 2021. [last updated 2021 Oct 20]. Available from: https://clinicaltrials.gov/ct2/show/NCT05084560.
- 136.Drugs for Neglected Diseases Initiative (DNDi) Filaria: river blindness – CC6166. 2016. [last updated 2021 Jun 1]. Available from: https://dndi.org/research-development/portfolio/cc6166/
- 137.Hübner MP, Hoerauf A, Blömker D, Townson S, Gokool S, Martin C, Vallarino-Lhermitte N, Chojnowski A, Kreiss T, Prorok M, Siekierka J, Khetani V, Camardo J, Canan S, Scandale I, Hawryluk N. Identification of potential clinical candidates with macrofilaricidal efficacy for the treatment of onchocerciasis. 66th Annual Meeting of the American Society for Tropical Medicine and Hygiene; Baltimore, Maryland, USA; 2017 Nov 5-9. [Google Scholar]
- 138.Hübner MP, Hoerauf A, Townson S, Gokool S, Martin C, Chojnowsk A, Kreiss T, Prorok M, Siekierka J, Zeldis J, Canan S, Khetani V, Scandal I, Hawryluk NA. Identification of new Macrofilaricidal Compounds for Treatment of Onchocerciasis. 66th Annual Meeting of the American Society for Tropical Medicine and Hygiene; Baltimore, Maryland, USA; 2017 Nov 5-9. [Google Scholar]
- 139.Jacobs RT, Lunde CS, Freund YR, Hernandez V, Li X, Xia Y, Carter DS, Berry PW, Halladay J, Rock F, Stefanakis R, Easom E, Plattner JJ, Ford L, Johnston KL, Cook DAN, Clare R, Cassidy A, Myhill L, Tyrer H, Gamble J, Guimaraes AF, Steven A, Lenz F, Ehrens A, Frohberger SJ, Koschel M, Hoerauf A, Hübner MP, McNamara CW, Bakowski MA, Turner JD, Taylor MJ, Ward SA. Boron-Pleuromutilins as Anti-Wolbachia Agents with Potential for Treatment of Onchocerciasis and Lymphatic Filariasis. J Med Chem. 2019 Mar;62(5):2521–2540. doi: 10.1021/acs.jmedchem.8b01854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ehrens A, Lunde CS, Jacobs RT, Struever D, Koschel M, Frohberger SJ, Lenz F, Fendler M, Turner JD, Ward SA, Taylor MJ, Freund YR, Stefanakis R, Easom E, Li X, Plattner JJ, Hoerauf A, Hübner MP. In vivo efficacy of the boron-pleuromutilin AN11251 against Wolbachia of the rodent filarial nematode Litomosoides sigmodontis. PLoS Negl Trop Dis. 2020 Jan;14(1):e0007957. doi: 10.1371/journal.pntd.0007957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bakowski MA, Shiroodi RK, Liu R, Olejniczak J, Yang B, Gagaring K, Guo H, White PM, Chappell L, Debec A, Landmann F, Dubben B, Lenz F, Struever D, Ehrens A, Frohberger SJ, Sjoberg H, Pionnier N, Murphy E, Archer J, Steven A, Chunda VC, Fombad FF, Chounna PW, Njouendou AJ, Metuge HM, Ndzeshang BL, Gandjui NV, Akumtoh DN, Kwenti TDB, Woods AK, Joseph SB, Hull MV, Xiong W, Kuhen KL, Taylor MJ, Wanji S, Turner JD, Hübner MP, Hoerauf A, Chatterjee AK, Roland J, Tremblay MS, Schultz PG, Sullivan W, Chu XJ, Petrassi HM, McNamara CW. Discovery of short-course antiwolbachial quinazolines for elimination of filarial worm infections. Sci Transl Med. 2019 May;11(491):eaav3523. doi: 10.1126/scitranslmed.aav3523. [DOI] [PubMed] [Google Scholar]
- 142.Milton P, Hamley JID, Walker M, Basáñez MG. Moxidectin: an oral treatment for human onchocerciasis. Expert Rev Anti Infect Ther. 2020 Nov;18(11):1067–1081. doi: 10.1080/14787210.2020.1792772. [DOI] [PubMed] [Google Scholar]