Abstract
Background
Intimate partner violence (IPV) during pregnancy is significantly associated with negative outcomes for both mother and child. Current evidence indicates an association between low levels of social support and IPV, however there is less evidence from low-and-middle income countries (LMIC) than high-income countries. Globally, the COVID-19 pandemic has radically altered how women can access social support. Hence since 2020, studies investigating IPV and pregnancy have occurred within the changing social context of the pandemic.
Objective
This scoping review summarizes the evidence from LMICs about the effects of IPV during pregnancy on maternal and child health. The review includes the impact of the COVID-19 pandemic on social support as mentioned in studies conducted since 2020.
Design
Library databases were used to identify papers from 2016 to 2021. These studies reported the maternal and child health outcomes of IPV during pregnancy, and described how social support during pregnancy, and the COVID-19 pandemic, were associated with rates of IPV during pregnancy. Observational study designs, qualitative and mixed methods studies were included.
Results
Twenty - six studies from 13 LMICs were included. Half (n = 13) were cross sectional studies which only collected data at one time-point. IPV during pregnancy was significantly associated with higher odds of postpartum depression, low birth weight, preterm birth and less breastfeeding in the year after birth. Lower levels of social support increased the odds of experiencing IPV during pregnancy, whilst higher levels of social support reduced antenatal anxiety and depression in women experiencing IPV during pregnancy. Of the four studies that investigated IPV during pregnancy throughout the COVID-19 pandemic, only one compared prevalence before and after the pandemic and unexpectedly reported a lower prevalence.
Conclusions
Further research on the impact of IPV during pregnancy on maternal and child outcomes in LMICs is required, especially evidence from longitudinal studies investigating a wider range of outcomes. To date, there is limited evidence on the impact of the COVID-19 pandemic on IPV during pregnancy in LMICs, and this should be prioritized as the pandemic continues to affect women’s access to social support globally.
Supplementary information
The online version contains supplementary material available at 10.1186/s12884-022-04604-3.
Background
Rationale
Intimate partner violence (IPV), the most common form of violence against women [1], is defined as “behaviour by an intimate partner that causes physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviours” [2]. Globally, it is estimated that nearly one in three women aged between 15 and 49 will suffer physical/sexual IPV at least once in their life [1]. IPV during pregnancy is associated with health consequences for both the mother and the expected child. In a systematic review of mainly high-income countries, longitudinal evidence revealed that exposure to IPV during pregnancy tripled the odds of postpartum depression [3]. In low- and middle-income countries (LMICs), perinatal common mental disorders (depression, anxiety, adjustment and somatic disorders) were more prevalent in women exposed to physical IPV during pregnancy or in the previous 12 months compared to unexposed women [4, 5]. IPV during pregnancy is also an established risk factor for antepartum hemorrhage [6], low birth weight [6, 7], intrauterine growth restriction [8], preterm delivery [6], and overall increased fetal morbidity [9]. Moreover, maternal exposure to IPV during pregnancy increases the level of stress hormones reaching the fetus [10], which may affect the behavioral development of the child [9]. Evidence suggests that the odds of both internalizing and externalizing behavioral problems in children whose mothers were exposed to violence during pregnancy were doubled compared to children whose mothers were not exposed to IPV [11]. Therefore, preventing IPV during pregnancy benefits the wellbeing of both mother and child.
Whilst IPV represents a relationship dynamic that is particularly associated with poor perinatal mental health outcomes [4], other forms of social support are also known to be vitally important to women’s wellbeing during the perinatal period. Globally, social distancing restrictions and lockdowns due to the COVID-19 pandemic have markedly affected family living and working arrangements, and access to face-to-face social support [12]. It is well established that pregnant women who have adequate social support (warm, supportive relationships with their partner, family, friends or significant others) are significantly less likely to experience physical or psychological abuse from their spouses [13]. Conversely, having little or no social support independently increases the odds of IPV during pregnancy [14, 15]. The direction of the relationship is unclear from quantitative evidence, but qualitative studies have established that controlling behaviour from an abusive partner can weaken women’s social networks and increase her social isolation [16, 17]. Emerging evidence since the pandemic begun in 2020 has consistently revealed that stay-at-home orders, interrupted access to support services and economic difficulties have worsened violence against women [18, 19]. However, specific information on violence against women who are/were pregnant during the pandemic is scarce. Therefore, this scoping review sought to re-evaluate the role of social support as a protective factor for perinatal mental health in light of this changing global context.
Before the pandemic (2010), an analysis of prevalence data from 19 countries revealed a higher prevalence of IPV during pregnancy in LMICs compared to high-income countries. Population – based research revealed that the prevalence of IPV during pregnancy was higher in African countries (3.8–13.5%), followed by Latin America countries (4.1–11.1%), then Asia (2–5%), while it was only 1.8% in Denmark and 2% in Australia [20]. In correspondence to this risk, the consequences of IPV during pregnancy for maternal and child health are expected to be more frequent in LMICs. However, since IPV was identified as a risk factor for perinatal common mental disorders in LMICs a systematic review by Fisher et al., [4], there has been no further systematic examination of the impact of IPV during pregnancy on both maternal and child health in these countries. Therefore, the purpose of this scoping review is to synthesize literature on IPV during pregnancy in LMICs from the previous five years (2016–2021), which includes research conducted during the COVID-19 pandemic.
Objectives
Three research questions informed this scoping review of the literature between 2016 and 2021: (1) What is the impact of IPV during pregnancy on maternal and child health in LMICs?, (2) What is the relationship between social support and IPV during pregnancy in LMICs? and (3) What is the impact of the COVID-19 pandemic on IPV during pregnancy in LMICs?
Methods
Protocol
As our main aim was to identify and map the literature available rather than to answer a clinical question or inform practice, a scoping review methodology was considered appropriate [21]. This review was conducted using the Joanna Briggs Institute’s updated methodological guidance for the conduct of scoping reviews [22]. The article search was limited to the past five years (2016–2021) to capture the recent literature. The protocol was revised by a researcher at the School of Health Sciences, College of Health, Massey University, New Zealand. Our study is presented according to the PRISMA Extension for Scoping Reviews: Checklist and Explanation (PRISMA-ScR) [23].
Eligibility criteria
The PCC (population, concept, and context) framework was used to select studies for this scoping review [22]. The population was defined as pregnant women (any time during pregnancy). The concept encompassed studies that reported at least one of the key measures of interest:
IPV during pregnancy.
Social support (search terms relating to partner support, and social/community support were included in the search string – see supplementary material for further information).
At least one of the key outcomes of interest (mother’s well – being, birth outcomes, child health and well-being).
The context was LMICs. As defined by the World Bank, low-income countries are those with a gross national income (GNI) per capita of $1,035 or less while middle income countries have GNI per capita between $1,036 and $12,535 [24]. In addition, it was noted that some eligible search results from 2020 to 2021 mentioned the context of the COVID-19 pandemic.
Study designs
As randomized controlled trials on IPV are ethically impossible [25], we included the studies with observational study designs (cohort, case control, cross – sectional, case series), as well as qualitative or mixed methods studies. Any study that included participants with a known diagnosis/treatment of mental health issues, overt psychosis or concurrent severe physical health problems was excluded.
Information sources
The search for relevant studies was conducted both electronically and manually. However, the criteria “low- and middle-income countries” was not used as a search term because many articles documented research taking place in an individual country. Therefore the locations of potentially eligible studies were checked against the list of the low- and middle-income countries provided by the World Bank [24].
An electronic search was conducted based on a comprehensive and reproducible strategy of four biomedical bibliographic databases MEDLINE (via Pubmed), Scopus, Web of Science, and PsychINFO. Searches in Google Scholar and Google were also performed to further capture publications from LMICs (grey literature). In addition, a manual search was conducted by going through the “Similar articles” section of an article or the reference lists of eligible studies.
Search
The search strategy is presented in the Supplementary material.
Selection of sources of evidence
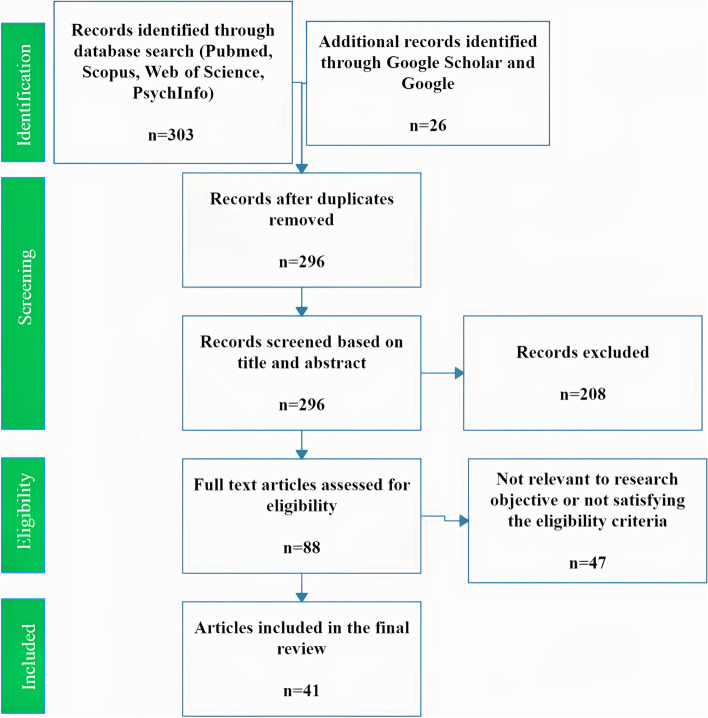
The search from the four main bibliographic databases yielded 303 studies while the Google/Google scholar search returned 26, resulting in a total of 329. All results were loaded into the online platform Picoportal (picoportal.org), and duplicates were removed, which resulted in 296 studies ready for screening. The criteria for screening studies were built and agreed upon by all authors prior to the selection process (Supplementary material).
Two reviewers independently screened the same 296 publications by checking the titles and abstracts. Eighty – eight studies were selected for full text screening. Finally, 26 studies were included in the scoping review. Any disagreement during the screening process was resolved through discussion between the co-authors (Fig. 1).
Fig. 1.
PRISMA flow chart of the study
Data charting process
Data from the eligible studies were independently extracted by two researchers using the template designed for this study (hosted in freeonlinesurveys.com). The template captured the relevant information on key study characteristics and detailed information on the aforementioned independent and outcome variables.
Data items
We extracted the data on article characteristics (e.g., title, first author, country of origin), study characteristics (e.g., objective, design, sample), and independent and dependent variables (as defined in the section on eligibility criteria) (the Supplementary material).
It is important to note that IPV during pregnancy is a type of perinatal IPV. Perinatal IPV is defined as the period of 12 months before the pregnancy, during the pregnancy and 12 months after childbirth [26]. As this scoping review focused only on IPV during pregnancy, data in the included studies which described perinatal IPV occurring outside of pregnancy was not included.
Synthesis of results
The results were grouped by the following themes:
Evidence about the effect of IPV during pregnancy on maternal and child health.
Evidence about social support and IPV during pregnancy.
Evidence about the COVID-19 pandemic and IPV during pregnancy.
Results
Characteristics of the included studies
Twenty - six studies were included (characteristics presented in Table 1). Most studies were cross sectional, facility – based, and from African nations, with sample sizes of between 180 and 500. The WHO’s domestic violence questionnaire was the most common tool used to detect IPV (Table 1). The prevalence of IPV during pregnancy was highly variable within and between countries and within research settings (facility/community) (see Supplementary material).
Table 1.
Characteristics of the 26 included studies
| Design | Number of studies |
|---|---|
| Prospective cohort | 5 [27–31] |
| Cross sectional | 13 [8, 32–43] |
| Quasi – experimental study | 1 [44] |
| Case control | 1 [45] |
| Baseline data of a quasi – experimental study | 1 [46] |
| Secondary analysis of data of a prospective cohort study | 1 [47] |
| Mixed method (quantitative and qualitative) | 1 [48] |
| Qualitative studies | 3 [49–51] |
| Number of studies using quantitative method | 23 [18–40] |
| Number of studies using qualitative method | 4 [48–51] |
| Setting (among 23 studies using quantitative method) | |
| Facility – based | 14 [8, 27, 28, 30, 32, 34, 36–40, 42, 47, 48] |
| Community – based | 9 [29, 31, 33, 35, 41, 43–46] |
| Sample size (among 23 studies using quantitative method) | |
| 180–500 | 9 [27, 28, 33, 36, 37, 39, 42, 44, 47] |
| 500–1,000 | 7 [8, 32, 34, 35, 40, 43, 48] |
| 1,000–1,400 | 6 [29–31, 38, 41, 43] |
| 4,680 | 1 [46] |
| Number of countries represented in this review | 13 |
| Locations of studies | |
| Eastern Africa | Ethiopia [35, 37, 42, 43, 45, 46], Tanzania [38, 51], Uganda [49] |
| Western Africa | Nigeria [36, 48] |
| Southern Africa | South Africa [32] |
| Southern Asia | Iran [28, 34, 39], India [44] |
| Southeastern Asia | Vietnam [29, 31, 41, 50], Malaysia [40] |
| Western Asia | Jordan [33] |
| Between Asia and Europe | Turkey [27] |
| Latin America | Brazil [8, 30], Mexico [47] |
| Tools to detect IPV during pregnancy | |
| WHO’s domestic violence questionnaire | 12 studies [28–31, 33, 35, 37–39, 42, 45, 50] |
| Abuse Assessment Screen | 2 studies [43, 44] |
| Conflict Tactics Scale | 1 study [36] |
| Revised Conflict Tactics Scale (CTS2) | 1 study [8] |
| Hurt, Insult, Threaten and Scream | 1 study [46] |
| Stressful Life Events Scale | 1 study [47] |
| Composite Abuse Scale - Short Form (CAS-SF) | 1 study [32] |
| Their own questionnaires | 6 studies [27, 34, 40, 41, 48, 49] |
Impact of IPV during pregnancy on maternal health
Only two studies using a prospective cohort design with adjustment of confounders were identified, and both evaluated postpartum depression as the outcome. Higher odds of postpartum depression were significantly associated with physical IPV [aOR = 2.75 (1.19–6.35)] and sexual IPV [aOR = 1.93 (1.01–3.73)] in Vietnam [31], while in Turkey, lower rates of postpartum depression [aOR = 0.056, (0.014–0.236)] were observed in women not exposed compared to those exposed to domestic violence during pregnancy [27].
In a cross-sectional study from Iran, IPV during pregnancy was significantly associated with postpartum depression in bivariate analysis, but this association became insignificant when adjusted for congenital abnormalities in the child and history of postpartum depression [34]. Another two cross-sectional studies reported a significant association between IPV during pregnancy and antenatal depression [35, 38] (Table 5, Additional file 1).
Qualitative studies revealed how physical IPV during pregnancy resulted in a variety of physical injuries to mothers (swollen reddish face and eyes, burns from hot iron and hot water, open wounds, vaginal tears and bleeding as a result of marital rape), miscarriages and unwanted pregnancy [40]. Depression, suicidal ideation and self-harm were described in association with psychological IPV during pregnancy [42]. One study from Uganda reported the negative impact of IPV during pregnancy on women’ on physical health and financial stability for mothers with HIV, as their husbands prohibited them from picking up HIV medications or going to work [49].
Impact of IPV during pregnancy on child health
The findings of the seven studies which described the impact of IPV during pregnancy are summarized in Table 2. Three studies, which all used a prospective cohort design with adjustment of confounders evaluated child health outcomes such as low birthweight [28, 29], preterm birth [29] and inadequate breast feeding [30]. Once again, IPV was significantly associated with higher odds of these outcomes.
Table 2.
Studies reporting associations between IPV during pregnancy and child health (with adjustment of confounders)
| Author and year | Country | Sample size (n) and setting | Outcome | Association with outcome |
|---|---|---|---|---|
| Prospective cohort studies | ||||
| Dolatian, Mahmoodi [28] | Iran | 400 | Birthweight |
IPV has indirect effect on birthweight in the path analysis of the model: B= − 0.016 |
| Nguyen, Ngo [29] | Vietnam | 1,276 | Low birthweight and gestational age |
• Physical IPV significantly associated with higher odd of preterm birth: aOR = 5.5 (2.1–14.1). • Physical IPV significantly associated with higher odd of low birth weight: aOR = 5.7 (2.2–14.9). |
| Ribeiro, Batista [30] | Brazil | 1,146 | Breastfeeding |
The higher HR of not being breastfed within the first year of life was significantly associated with: • Violence (by partners/family members) before/during pregnancy increased: HR = 1.39 (1.03–1.88) • Recurrent physical/emotional/sexual violence during pregnancy: HR = 1.46 (1.11–1.92) |
| Cross sectional studies | ||||
| Laelago, Belachew [37] | Ethiopia |
183 Inpatient |
Low birth weight | All IPV: aOR = 14.3 (5.1–40.7) |
| Lobato, Reichenheim [8] | Brazil |
810 Outpatient |
Intrauterine growth restriction | Psychological IPV: aOR = 1.15 (1.07–1.23) |
| Kana, Safiyan [36] | Nigeria |
293 Outpatient |
Low birth weight | Physical, psychological and sexual IPV were all significantly associated to higher risk. |
| Case control study | ||||
| Wondimye, Bezatu [45] | Ethiopia |
103 cases and 412 controls Community-based |
Neonatal mortality |
• Sexual violence during pregnancy increased the risk of outcome: aOR = 3.20 (1.09–9.33). • Psychological and physical violence during pregnancy were not significantly associated. |
aOR adjusted odd ratio, HR hazard ratio. The range of aOR or HR in the parenthesis in the 95% CI of the aOR or HR
Findings from the cross-sectional studies suggested that IPV was significantly associated with higher odds of low birth weight [36, 37] or intrauterine growth restriction [8]. One case control study revealed sexual violence during pregnancy (but not psychological or physical violence) increased the odds of neonatal mortality [45].
The relationship between social support on IPV during pregnancy
The studies investigating IPV during pregnancy and social support are summarized in Table 3, and most were cross-sectional in nature. One study from Vietnam suggested that a lack of support during pregnancy tripled the odds of experiencing IPV during pregnancy [41]. Social support also seemed to moderate the impact of IPV during pregnancy. For example, it significantly reduced antenatal depression in Malaysia [40] and both antenatal depression and anxiety in Mexico [47].
Table 3.
Studies on the impact of social support on IPV during pregnancy (with adjustment of confounders)
| Author and year | Country | Sample size (n) and setting | Outcome | Association with risk of outcome |
|---|---|---|---|---|
| Quasi-experimental study | ||||
| Bhushan, Krupp [44] |
India, community - based |
480 Quasi-experimental study |
Antenatal anxiety |
Home visit or accompaniment to antenatal care by ASHAa significantly associated with lower odds of outcome. • Home visits: aPR = 0.90 (0.76–0.98). • Accompaniment to antenatal care: aPR = 0.86 (0.78–0.95). |
| Cross sectional and other studies | ||||
| Manongi, Rogathi [38] |
Tanzania, outpatient |
1,116 Cross sectional |
Antenatal depression | Emotional support from outside family significantly associated with higher odd of outcome: [aOR = 2.25 (1.26, 4.02)] compared with emotional support from inside family. |
| Woldetensay, Belachew [46] | Ethiopia |
4,680 Community – based Baseline data from a prospective, quasi-experimental cohort study |
Antenatal depressive symptoms | Poor social support from friends, families and husband significantly associated with higher odds of outcome: aOR = 1.63 (1.31–2.02). |
| Nguyen, Ngo [41] | Vietnam |
1309 Community – based Cross-sectional study nested within a larger prospective cohort study |
IPV during pregnancy |
Lack of social support significantly associated with higher odds of: • One - time IPV: aOR = 3.1 (2.4–3.9). • Multiple times: aOR = 2.9 (2.2–3.8). |
| Nasreen, Rahman [40] |
Malaysia, outpatient |
904 Cross sectional |
Antenatal depression and anxiety |
Moderate support [aOR = 0.16 (0.03–0.73)] and high support [aOR = 0.13 (0.03–0.59)] significantly associated with lower odds of depression. Anxiety: family support significantly associated with higher odds: aOR = 1.07 (1.03–1.13). |
| Woldetsadik, Ayele [43] |
Ethiopia, community - based |
743 Cross sectional |
Antenatal common mental disorders | No significant association between social support or husband support and the outcome. |
| Navarrete, Nieto [47] | Mexico |
210 Outpatient |
Antenatal depressive and anxiety symptoms |
When social support was introduced into the regression model, the impact of IPV during pregnancy was nullified (odd of depression) or reduced (odd of anxiety)b. |
aOR adjusted odd ratio, aPR adjusted prevalence ratio, The range of aOR/aPR in the parenthesis in the 95% CI of the aOR/aPR
aAccredited Social Health Activists. bThis research is a prospective cohort study but only cross-sectional data obtained during pregnancy is used in this review
In a qualitative study conducted on the Chaga and Pare tribes (northern Tanzania) where wives must live with their partners’ families and children are considered to be the property of male partners, IPV victims could receive emotional or financial support from their own families but were usually not welcome back home [44]. They were often asked to stay in their marriages in the children’s interest. In some instances, families acted as mediators between the women and their partners. However, some family members did advise the victims to leave the relationship [51].
Impact of COVID-19 pandemic on IPV during pregnancy
As our library searches captured articles up to April 2021, the retrieved studies included those conducted during the COVID-19 pandemic in its first year. Specifically, four studies from April to November 2020 (see Table 4). Two studies were online or telephone surveys, reflecting the impact of lockdowns or social distancing on feasible research methods. The other two were facility – based.
Table 4.
Studies on the impact of COVID-19 on IPV during pregnancy
| Author and year | Country | Sample size (n) and setting | Setting and timing | What the study wants to determine | Association between outcome and social support |
|---|---|---|---|---|---|
| Naghizadeh, Mirghafourvand [39] | Iran |
250 Cross sectional |
Outpatient 5–8/2020 |
The prevalence of domestic violence and its relationship with the quality of life of pregnant women during the COVID-19 pandemic |
• About 1 in 3 women experienced domestic violence. • Violence victims had significant lower quality of life in the mental health compared to unaffected women: β = 9.3 (3.5 to 15.0), P = 0.002) |
| Teshome, Gudu [42] | Ethiopia |
464 Cross sectional |
Outpatient 8–11/2020 |
The incidence and predictors of IPV during pregnancy during the COVID-19 pandemic |
• 7.1% women experienced IPV during pregnancy • IPV during pregnancy was more reported among women who husbands consume Khat [aOR = 3.27 (1.45–7.38)] or alcohol [aOR = 1.52 (1.01–2.28)] |
| Abujilban, Mrayan [33] | Jordan |
215 Cross sectional (online survey) |
Community 4/2020 |
The change in the incidence of IPV during pregnancy before and during the COVID-19 pandemic | The pre-pandemic level of IPV during pregnancy was higher than that during the pandemic (Before: 65.1%, 30.7%, and 15.3%, for psychological, physical, and sexual violence, respectively. During: 50.2%, 13%, 11.2%, respectively). |
| Abrahams, Boisits [32] | South Africa |
885 Cross sectional (Telephone interview) |
Outpatient 6–7/2020 |
The relationship between common mental disorders, food insecurity and IPV during pregnancy during the COVID-19 pandemic |
Higher odds of common mental disorders were associated with IPV during pregnancy during the pandemic: • Psychological IPV: aOR = 2.50 (1.32–4.72) • Sexual IPV: 2.70 (1.07–6.80) |
aOR adjusted odd ratio. The range of aOR in the parenthesis in the 95% CI of the aOR
The prevalence of domestic violence during pregnancy during the pandemic was 35.2% in Iran [39], and 7.1% in Ethiopia [42]. Only one study from Jordan compared the prevalence of IPV during pregnancy before the pandemic with that during the pandemic, finding that the prevalence before the pandemic was actually higher. Specifically, before the pandemic, the prevalence was 65.1%, 30.7%, and 15.3%, for psychological, physical, and sexual violence, respectively, while it was 50.2%, 13%, and 11.2% during the pandemic [33].
During the pandemic, IPV during pregnancy was found to lower the quality of life in Iran [39], and increase the odds of common mental disorders in South Africa [32]. In Ethiopia, IPV during pregnancy was associated with husband’s alcohol or khat consumption during the pandemic [42].
Discussion
This scoping review consolidates existing knowledge regarding the impact of IPV during pregnancy on maternal and child health in LMICs, and identifies how social support and the COVID-19 pandemic may affect IPV during pregnancy in LMICs. Our findings confirm the well-established association between IPV during pregnancy and postpartum depression [4] and identifies additional evidence of the association between IPV during pregnancy and low birth weight, preterm birth and less breastfeeding in the year after birth [28, 30, 52]. The previously recognized protective effect of social support for women experiencing IPV during pregnancy was reflected by the findings of quantitative studies, highlighting the potential of social support interventions for improving perinatal mental health outcomes. However, qualitative evidence revealed that in contexts where proprietal attitudes towards women were common, wider social networks may encourage pregnant women to remain in violent relationships [44]. The number of studies exploring IPV during pregnancy during the COVID-19 pandemic is still small, though a negative impact of the pandemic on the quality of life and the mental health of pregnant women was found in the available literature.
Impact of IPV during pregnancy on maternal health
In their work on the link between IPV during pregnancy and maternal mental health, Halim et al. suggested that prospective cohort designs with adjustment of confounders are optimal for determining causality [5]. In our scoping review, two such studies reported that physical/sexual IPV and domestic violence during pregnancy were significantly associated with a higher risk of postpartum depression [27, 31]. Generally, our data is congruent with the literature before 2016. A prospective cohort study in 2010 from Brazil found a significant association between psychological IPV during pregnancy and postpartum depression [53] while another prospective cohort study conducted in 2015 in Tanzania revealed a similar finding between any IPV during pregnancy and postpartum depression [54]. There is consistent evidence from LMICs supporting the association between IPV during pregnancy and postpartum depression [55, 56]. The two more recent studies in our review only followed up women until eight [19] or twelve [23] weeks after birth, which is similar to existing literature from before 2016. Whilst it is intensive to continue cohort studies further into the postpartum period, there appears to very little research about the length and severity of depressive episodes during the first year postpartum, or if IPV continues during the postpartum period. Antenatal depression occurs concurrently with IPV during pregnancy, and this association has been identified in studies with cross-sectional designs. The finding of a significant association between IPV during pregnancy and antenatal depression in our review is also aligned with previous literature [57, 58].
Previous literature has identified a range of other maternal health issues associated with IPV during pregnancy [3, 5, 59–62]. For pregnancy outcomes (abortion, hemorrhage, placenta abruption, preeclampsia, vaginal delivery vs. cesarean), only premature rupture of membranes was found to be significantly associated with physical/psychological IPV in the studies using prospective cohort designs with adjustment of confounders [63, 64].
Impact of IPV during pregnancy on child health
For preterm birth, a study from Vietnam in our review identified a significant association between physical IPV during pregnancy and preterm birth [29]. In the previous literature, psychological IPV during pregnancy was not significantly associated with premature birth in a prospective cohort study from Iran in 2014 [64] or South Africa in HIV – infected mothers in 2017 [65]. Domestic violence of any form during pregnancy was also not associated with this outcome in another prospective cohort study from Brazil in 2008 [66]. These findings, including the association between preterm birth and IPV from the more recent study in Vietnam, can be used to inform interventions to protect maternal and child health in LMICs.
Regarding low birth weight, any IPV for the study from Iran [28], and physical IPV for the study from Vietnam [29] were found to be significantly associated. Our findings are consistent prospective cohort studies from Brazil in 2010 (physical IPV during pregnancy, alone or together with psychological IPV) [67] and Iran (physical/sexual IPV) in 2015 [63]. Interestingly, psychological IPV alone during pregnancy was not significantly associated with low birth weight in the previous studies from Iran [64] and South Africa [65]. However, as few prospective cohort studies are available, further research on this association is required.
In terms of breastfeeding, high odds of not being breastfed in the first year of life was reported for babies whose mother had been exposed to violence (by partners/family members) before/during pregnancy compared to unexposed mothers [30]. This finding is in keeping with a prospective cohort study from Tanzania which suggests exposure to IPV during either pregnancy or the postpartum period increased the odds of breastfeeding cessation before the child turned 6 months old [68].
We investigated other child outcomes explored in the previous literature [11, 61, 62, 69–71]. However, only one study from China was identified [72] in which the children of the mothers exposed to domestic violence during pregnancy were later found to have poorer behavioral development at 10 months of age (weaker rhythmicity, more negative mood, withdrawn behaviour, and poorer development of motor skills). The findings of this scoping review suggest that little is still known about the long-term effects of IPV during pregnancy on child health and development in LMIC settings.
Impact of social support during pregnancy on IPV during pregnancy
In our review, the association between a lack of social support and IPV during pregnancy is in keeping with the existing literature [13–15]. Social support also seemed to buffer the maternal health impacts of IPV during pregnancy (such as depression and anxiety). However, findings from cross sectional studies should be interpreted with caution due to the inability to conclude on the direction of the association. For example, in our review, the study by Nasreen et al. [40] showed that social support was significantly associated with lower odds of depression, but also with higher odds of anxiety. Further context specific qualitative research is required to understand how different forms of social support can be protective to women in violent relationships during pregnancy in LMIC. It is important to distinguish social support (support from a partner, family or friends [38, 40, 41, 43, 46, 47]) from social support interventions (such as home visits or accompaniment to antenatal care [44]), because the latter are sometimes called “social support” in the literature. For instance, to deliver efficient social support interventions for a pregnant woman experiencing IPV, health professionals should first find out about how much support she has from her partner, family or friends [73]. In India, there are also promising interventions suggesting that social support in the form of home visitors or accompaniment to antenatal care can decrease anxiety [37]. It is acknowledged that globally, the feasibility of such interventions have been seriously disrupted by the COVID-19 pandemic.
Impact of COVID-19 pandemic on IPV during pregnancy
Evidence from high income countries suggests that the COVID-19 pandemic has worsened the mental health of the general population [74] and also increased the incidence of violence against women [75]. There is currently very little evidence describing how IPV during pregnancy was/is experienced during the pandemic. Surprisingly, in our review, the only study providing a pre and during - pandemic comparison found that the prevalence of IPV during pregnancy throughout the pandemic was lower than that before the pandemic in [33]. Two other studies provided prevalence without such comparison [39, 42]. However, if their figures are compared with the existing data in the literature, the same trend is observed. Specifically, in Iran, the prevalence of domestic violence during pregnancy during the pandemic was 35.2% in our review [39], much lower than the prevalence of 67–70% found in a 2020 study in the same city [76]. In Ethiopia, while the prevalence of IPV during pregnancy was 7.1% in our review, it was as high as 20–35% in other recent studies from this country [35, 77].
Whether this downward trend reflects the true situation during the pandemic or is an artefact of nonrepresentative data (e.g. due to selection bias from online recruitment data collection [33], facility – based sampling [42], urban vs. rural setting [42] or economic and sociocultural differences [39]) is still to be determined. Nevertheless, evidence also suggests that different the pandemic situations in individual countries and the local measures available to combat violence will result in differences in prevalence of violence against women. To date, reports of the rates of domestic violence during the pandemic have been inconsistent, and it is well known that violence against women is underreported in most contexts [17]. According to one multi-country study, domestic violence increased in Austria, Belgium, France, Ireland, Spain and UK, decreased in Italy and Portugal and stayed the same in The Netherlands and Switzerland [78].
The scarcity of research on IPV during pregnancy during the COVID-19 pandemic in LMICs suggests that more research is required to illuminate the needs of pregnant women during this time. Such research is urgently needed due to the serious impact of IPV on pregnant women and their children [32, 39]. Also, whilst social support was found to be protective for women experiencing IPV in pregnancy, globally, lockdown orders and social distancing measures have created changes to maternity care that have resulted in barriers to such support being accessed. In addition, while our review describes the pandemic in 2020, new variants with more serious consequences and/or higher rates of infection [79, 80] mean that women suffering IPV during pregnancy in LMICs will continue to experience the context of the pandemic from 2021 into the future.
Conclusions
By looking specifically at prospective cohort studies with adjustment of confounders in this review and similar previous reviews, we conclude that high quality literature from LMICs is still limited. The scarcity of research is evident in both the number of studies and types of outcomes evaluated. The following recommendations are thus made as below:
More longitudinal primary studies with appropriate statistical techniques and longer postpartum timeframes should be conducted to gather more reliable data. Systematic reviews and meta – analysis in this area are unlikely to add new information at this stage.
Context specific qualitative research is required for nuanced understanding about what types of social support can be protective for pregnant women experiencing IPV.
Efforts should be made to standardize tools to detect IPV during pregnancy, screening practice and methodology to allow more comparable research.
The small number of LMICs in our review and others raises the possibility that relevant work might been published in languages other than English. For instance, one review included a few primary studies published in Portuguese [61]. As this possibility is highly true, the need to understand this topic in English literature will require collaboration from authors of LMICs to capture relevant research.
We believe that different COVID-19 variants are and will be creating diverse impacts on IPV during pregnancy in various stages of the ongoing pandemic and parts of the world. Therefore, scoping reviews are regularly required to inform on the literature available.
Social support interventions that are feasible during pandemic restrictions in LMIC should be trialed and evaluated, as these are imperative to the wellbeing of pregnant women.
Supplementary Information
Acknowledgements
The authors would like to thank Associate Professor Andy Towers for reviewing our manuscript before submission.
Abbreviations
- IPV
intimate partner violence
- LMICs
low- and middle-income countries
- GNI
gross national income
Authors' contributions
CT and LM screened articles, conducted analysis and prepared manuscript. VVT assisted with analysis and preparing manuscript.
Funding
No external funding obtained.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics and approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None declared.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. Geneva; 2021.
- 2.WHO. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. 2013. [PubMed]
- 3.Howard LM, Oram S, Galley H, Trevillion K, Feder G. Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis. PLoS Med. 2013;10(5):e1001452. doi: 10.1371/journal.pmed.1001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139G-49G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halim N, Beard J, Mesic A, Patel A, Henderson D, Hibberd P. Intimate partner violence during pregnancy and perinatal mental disorders in low and lower middle income countries: A systematic review of literature, 1990–2017. Clin Psychol Rev. 2018;66:117–35. doi: 10.1016/j.cpr.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Dahlen HG, Munoz AM, Schmied V, Thornton C. The relationship between intimate partner violence reported at the first antenatal booking visit and obstetric and perinatal outcomes in an ethnically diverse group of Australian pregnant women: a population-based study over 10 years. BMJ Open. 2018;8(4):e019566-e. doi: 10.1136/bmjopen-2017-019566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sigalla GN, Mushi D, Meyrowitsch DW, Manongi R, Rogathi JJ, Gammeltoft T, et al. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: A prospective cohort study. PLoS One. 2017;12(2):e0172540. doi: 10.1371/journal.pone.0172540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lobato G, Reichenheim ME, Moraes CL, Peixoto-Filho FM, Migowski LS. Psychologic intimate partner violence and the risk of intrauterine growth restriction in Rio de Janeiro. Int J Gynecol Obstetr. 2018;143(1):77–83. doi: 10.1002/ijgo.12393. [DOI] [PubMed] [Google Scholar]
- 9.Mueller I, Tronick E. Early Life Exposure to Violence: Developmental Consequences on Brain and Behavior. Front Behav Neurosci. 2019;13:156. doi: 10.3389/fnbeh.2019.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boeckel MG, Viola TW, Daruy-Filho L, Martinez M, Grassi-Oliveira R. Intimate partner violence is associated with increased maternal hair cortisol in mother–child dyads. Compr Psychiatry. 2017;72:18–24. doi: 10.1016/j.comppsych.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Silva E, Lemos A, Andrade C, Ludermir A. Intimate partner violence during pregnancy and behavioral problems in children and adolescents: a meta-analysis. J de Pediatria. 2018;94(5):471–82. doi: 10.1016/j.jped.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Fisher J, Languilaire J-C, Lawthom R, Nieuwenhuis R, Petts RJ, Runswick-Cole K, et al. Community, work, and family in times of COVID-19. Community. Work Fam. 2020;23(3):247–52. doi: 10.1080/13668803.2020.1756568. [DOI] [Google Scholar]
- 13.Farid M, Saleem S, Karim MS, Hatcher J. Spousal abuse during pregnancy in Karachi, Pakistan. Int J Gynecol Obstetr. 2008;101(2):141–5. doi: 10.1016/j.ijgo.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 14.Peedicayil A, Sadowski LS, Jeyaseelan L, Shankar V, Jain D, Suresh S, et al. Spousal physical violence against women during pregnancy. BJOG. 2004;111(7):682–7. doi: 10.1111/j.1471-0528.2004.00151.x. [DOI] [PubMed] [Google Scholar]
- 15.Doi S, Fujiwara T, Isumi A. Development of the Intimate Partner Violence During Pregnancy Instrument (IPVPI) Front Public Health. 2019;7:43. doi: 10.3389/fpubh.2019.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray L, Warr D, Chen J, Block K, Murdolo A, Quiazon R, et al. Between ‘here’ and ‘there’: family violence against immigrant and refugee women in urban and rural Southern Australia. Gender Place Culture. 2019;26(1):91–110. doi: 10.1080/0966369X.2018.1553862. [DOI] [Google Scholar]
- 17.Smyth C, Cullen P, Breckenridge J, Cortis N, Valentine K. COVID-19 lockdowns, intimate partner violence and coercive control. Aust J Soc Issues. 2021 doi: 10.1002/ajs4.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans ML, Lindauer M, Farrell ME. A Pandemic within a Pandemic — Intimate Partner Violence during Covid-19. New England J Med. 2020;383(24):2302–4. doi: 10.1056/NEJMp2024046. [DOI] [PubMed] [Google Scholar]
- 19.Uzobo E, Ayinmoro AD. Trapped Between Two Pandemics: Domestic Violence Cases Under COVID-19 Pandemic Lockdown: A Scoping Review. International Quarterly of Community Health Education. 2021:0272684 × 211022121. [DOI] [PMC free article] [PubMed]
- 20.Devries KM, Kishor S, Johnson H, Stöckl H, Bacchus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. 2010;18(36):158–70. doi: 10.1016/S0968-8080(10)36533-5. [DOI] [PubMed] [Google Scholar]
- 21.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18(10). [DOI] [PubMed]
- 23.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Internal Med. 2018;169(7):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 24.World Bank. World Bank Country and Lending Groups 2021 [Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 25.Ellsberg M, Heise L, Peña R, Agurto S, Winkvist A. Researching Domestic Violence Against Women: Methodological and Ethical Considerations. Stud Fam Plan. 2001;32(1):1–16. doi: 10.1111/j.1728-4465.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 26.Hahn CK, Gilmore AK, Aguayo RO, Rheingold AA. Perinatal Intimate Partner Violence. Obstet Gynecol Clin North Am. 2018;45(3):535–47. doi: 10.1016/j.ogc.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Çankaya S. The effect of psychosocial risk factors on postpartum depression in antenatal period: A prospective study. Arch Psychiatric Nurs. 2020;34(3):176–83. doi: 10.1016/j.apnu.2020.04.007. [DOI] [PubMed] [Google Scholar]
- 28.Dolatian M, Mahmoodi Z, Alavi-Majd H, Moafi F, Ghorbani M, Mirabzadeh A. Psychosocial factors in pregnancy and birthweight: Path analysis. J Obstetr Gynaecol Res. 2016;42(7):822–30. doi: 10.1111/jog.12991. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen HT, Ngo VT, Gammeltoft T, Meyrowitsch W, Nguyen D, Rasch TTH. Association between Intimate Partner Violence during Pregnancy and Adverse Pregnancy Outcomes in Vietnam: A Prospective Cohort Study. PloS one. 2016;11(9):e0162844-e. doi: 10.1371/journal.pone.0162844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ribeiro MRC, Batista RFL, Schraiber LB, Pinheiro FS, Santos AMd, Simões VMF, et al. Recurrent Violence, Violence with Complications, and Intimate Partner Violence Against Pregnant Women and Breastfeeding Duration. J Women’s Health. 2020. [DOI] [PubMed]
- 31.Tran TN, Nguyen TTH, Nguyen DH, Ngo VT, Gammeltoft T, Rasch V, et al. Intimate Partner Violence among Pregnant Women and Postpartum Depression in Vietnam: A Longitudinal Study. BioMed Res Int. 2019;2019:4717485. doi: 10.1155/2019/4717485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abrahams Z, Boisits S, Schneider M, Prince M, Lund C. Domestic violence, food insecurity and mental health of pregnant women in the COVID-19 lockdown in Cape Town, South Africa: Research Square; 2021 [Available from: 10.21203/rs.3.rs-102205/v1. [DOI] [PMC free article] [PubMed]
- 33.Abujilban S, Mrayan L, Hamaideh S, Obeisat S, Damra J. Intimate Partner Violence Against Pregnant Jordanian Women at the Time of COVID-19 Pandemic’s Quarantine. J Interpersonal Violence. 2021:0886260520984259. [DOI] [PubMed]
- 34.Afshari P, Tadayon M, Abedi P, Yazdizadeh S. Prevalence and related factors of postpartum depression among reproductive aged women in Ahvaz, Iran. Health Care Women Int. 2020;41(3). [DOI] [PubMed]
- 35.Belay S, Astatkie A, Emmelin M, Hinderaker SG. Intimate partner violence and maternal depression during pregnancy: A community-based cross-sectional study in Ethiopia. PloS one. 2019;14(7):e0220003-e. doi: 10.1371/journal.pone.0220003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kana MA, Safiyan H, Yusuf HE, Musa ASM, Richards-Barber M, Harmon QE, et al. Association of intimate partner violence during pregnancy and birth weight among term births: a cross-sectional study in Kaduna, Northwestern Nigeria. BMJ Open. 2020;10(12):e036320. doi: 10.1136/bmjopen-2019-036320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laelago T, Belachew T, Tamrat M. Effect of intimate partner violence on birth outcomes. Afr Health Sci. 2017;17(3):681–9. doi: 10.4314/ahs.v17i3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manongi R, Rogathi J, Sigalla G, Mushi D, Rasch V, Gammeltoft T, et al. The Association Between Intimate Partner Violence and Signs of Depression During Pregnancy in Kilimanjaro Region, Northern Tanzania. J Interpersonal Violence. 2017;35(23–24):5797–811. doi: 10.1177/0886260517724256. [DOI] [PubMed] [Google Scholar]
- 39.Naghizadeh S, Mirghafourvand M, Mohammadirad R. Domestic violence and its relationship with quality of life in pregnant women during the outbreak of COVID-19 disease. BMC Pregnancy Childbirth. 2021;21(1):88. doi: 10.1186/s12884-021-03579-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nasreen HE, Rahman JA, Rus RM, Kartiwi M, Sutan R, Edhborg M. Prevalence and determinants of antepartum depressive and anxiety symptoms in expectant mothers and fathers: results from a perinatal psychiatric morbidity cohort study in the east and west coasts of Malaysia. BMC Psychiatry. 2018;18(1):195. doi: 10.1186/s12888-018-1781-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen TH, Ngo TV, Nguyen VD, Nguyen HD, Nguyen HTT, Gammeltoft T, et al. Intimate partner violence during pregnancy in Vietnam: prevalence, risk factors and the role of social support. Global Health Action. 2018;11(sup3):1638052. doi: 10.1080/16549716.2019.1638052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teshome A, Gudu W, Bekele D, Asfaw M, Enyew R, Compton SD. Intimate partner violence among prenatal care attendees amidst the COVID-19 crisis: The incidence in Ethiopia. Int J Gynecol Obstetr. 2021;153(1):45–50. doi: 10.1002/ijgo.13566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Woldetsadik AM, Ayele AN, Roba AE, Haile GF, Mubashir K. Prevalence of common mental disorder and associated factors among pregnant women in South-East Ethiopia, 2017: a community based cross-sectional study. Reprod Health. 2019;16(1):173. doi: 10.1186/s12978-019-0834-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhushan NA-O, Krupp K, Jaykrishna P, Ravi K, Khan A, Shidhaye R, et al. The association between social support through contacts with Accredited Social Health Activists (ASHAs) and antenatal anxiety among women in Mysore, India: a cross-sectional study. 2020(1433–9285 (Electronic)). [DOI] [PMC free article] [PubMed]
- 45.Wondimye A, Bezatu M, Gudina E, Yemane B. Intimate partner violence during pregnancy and neonatal mortality in Eastern Ethiopia: A population based matched case-control study. Res Square. 2021. https://www.researchsquare.com/article/rs-58851/v1.
- 46.Woldetensay YK, Belachew T, Biesalski HK, Ghosh S, Lacruz ME, Scherbaum V, et al. The role of nutrition, intimate partner violence and social support in prenatal depressive symptoms in rural Ethiopia: community based birth cohort study. BMC Pregnancy Childbirth. 2018;18(1):374. doi: 10.1186/s12884-018-2009-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Navarrete L, Nieto L, Lara MA. Intimate partner violence and perinatal depression and anxiety: Social support as moderator among Mexican women. Sex Reprod Healthcare. 2021;27:100569. doi: 10.1016/j.srhc.2020.100569. [DOI] [PubMed] [Google Scholar]
- 48.Ezeudu CC, Akpa O, Waziri NE, Oladimeji A, Adedire E, Saude I, et al. Prevalence and correlates of intimate partner violence, before and during pregnancy among attendees of maternal and child health services, Enugu, Nigeria: mixed method approach, January 2015. Pan Afr Med J. 2019;32(Suppl 1):14. doi: 10.11604/pamj.supp.2019.32.1.13287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ashaba S, Kaida A, Coleman JN, Burns BF, Dunkley E, O’Neil K, et al. Psychosocial challenges facing women living with HIV during the perinatal period in rural Uganda. PloS One. 2017;12(5):e0176256-e. doi: 10.1371/journal.pone.0176256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nhị TT, Hạnh NTT, Gammeltoft TM. Emotional violence and maternal mental health: a qualitative study among women in northern Vietnam. BMC Women’s Health. 2018;18(1):58. doi: 10.1186/s12905-018-0553-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sigalla GN, Mushi D, Gammeltoft T. "Staying for the children”: The role of natal relatives in supporting women experiencing intimate partner violence during pregnancy in northern Tanzania - A qualitative study. PloS One. 2018;13(6):e0198098-e. doi: 10.1371/journal.pone.0198098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nguyen ANT, Nguyen LH. The study on situation of exclusive breast feeding for the first 6 months in Hoi An. J Med Pharm Hue Univ Med Pharm. 2016;6(3):36–42. [Google Scholar]
- 53.Ludermir AB, Lewis G, Valongueiro SA, de Araújo TVB, Araya R. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet. 2010;376(9744):903–10. doi: 10.1016/S0140-6736(10)60887-2. [DOI] [PubMed] [Google Scholar]
- 54.Rogathi JJ, Manongi R, Mushi D, Rasch V, Sigalla GN, Gammeltoft T, et al. Postpartum depression among women who have experienced intimate partner violence: A prospective cohort study at Moshi, Tanzania. J Affect Disord. 2017;218:238–45. doi: 10.1016/j.jad.2017.04.063. [DOI] [PubMed] [Google Scholar]
- 55.Fisher J, Tran T, La BT, Kriitmaa K, Rosenthal D, Tran T. Common perinatal mental disorders in northern Viet Nam: community prevalence and health care use. Bull World Health Organ. 2010;88(10):737–45. doi: 10.2471/BLT.09.067066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Murray L, Dunne MP, Van Vo T, Anh PNT, Khawaja NG, Cao TN. Postnatal depressive symptoms amongst women in Central Vietnam: a cross-sectional study investigating prevalence and associations with social, cultural and infant factors. BMC Pregnancy Childbirth. 2015;15(1):234. doi: 10.1186/s12884-015-0662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mahenge B, Likindikoki S, Stöckl H, Mbwambo J. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in Tanzania: a cross-sectional study. BJOG. 2013;120(8):940–7. doi: 10.1111/1471-0528.12185. [DOI] [PubMed] [Google Scholar]
- 58.Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: A population based study in rural Bangladesh. BMC Women’s Health. 2011;11(1):22. doi: 10.1186/1472-6874-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Oliveira Fonseca-Machado M, Camargo Alves L, Scotini Freitas P, dos Santos Monteiro JC, Gomes-Sponholz F. Mental health of women who suffer intimate partner violence during pregnancy. Investigación y Educación en Enfermería. 2014;32:291–305. doi: 10.17533/udea.iee.v32n2a12. [DOI] [PubMed] [Google Scholar]
- 60.Jamieson B. Exposure to Interpersonal Violence During Pregnancy and Its Association With Women’s Prenatal Care Utilization: A Meta-Analytic Review. Trauma Violence Abuse. 2018;21(5):904–21. doi: 10.1177/1524838018806511. [DOI] [PubMed] [Google Scholar]
- 61.Lafaurie M. Intimate partner violence against women during pregnancy: a critical reading from a gender perspective. Rev Colomb Enferm. 2015;10(10):64–77. doi: 10.18270/rce.v10i10.581. [DOI] [Google Scholar]
- 62.Pastor-Moreno G, Ruiz-Pérez I, Henares-Montiel J, Escribà-Agüir V, Higueras-Callejón C, Ricci-Cabello I. Intimate partner violence and perinatal health: a systematic review. BJOG. 2020;127(5):537–47. doi: 10.1111/1471-0528.16084. [DOI] [PubMed] [Google Scholar]
- 63.Abdollahi F, Abhari FR, Delavar MA, Charati JY. Physical violence against pregnant women by an intimate partner, and adverse pregnancy outcomes in Mazandaran Province, Iran. J Family Community Med. 2015;22(1):13–8. doi: 10.4103/2230-8229.149577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abdollahi F, Rezaie Abhari F, Yazdani Charati J, Rouhani S. Impact of psychological violence on pregnancy outcomes in a prospective study. Iran J Psychiatry Behav Sci. 2014;8(3):22–7. [PMC free article] [PubMed] [Google Scholar]
- 65.Sania A, Brittain K, Phillips TK, Zerbe A, Ronan A, Myer L, et al. Effect of alcohol consumption and psychosocial stressors on preterm and small-for-gestational-age births in HIV-infected women in South Africa: a cohort study. BMJ Open. 2017;7(3):e014293-e. doi: 10.1136/bmjopen-2016-014293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Audi CA, Corrêa Am Fau - Latorre MdRDdO, Latorre Mdo R Fau - Santiago SM, Santiago SM. The association between domestic violence during pregnancy and low birth weight or prematurity. J Pediatr (Rio J). 2008;84(1):60–7. [DOI] [PubMed]
- 67.Nunes M, Camey S, Ferri C, Manzolli P, Manenti C, Schmidt M. Violence during pregnancy and newborn outcomes: A cohort study in a disadvantaged population in Brazil. Eur J Public Health. 2010;21(1):92–7. doi: 10.1093/eurpub/ckp241. [DOI] [PubMed] [Google Scholar]
- 68.Kjerulff Madsen F, Holm-Larsen CE, Wu C, Rogathi J, Manongi R, Mushi D, et al. Intimate partner violence and subsequent premature termination of exclusive breastfeeding: A cohort study. PLoS One. 2019;14(6):e0217479. doi: 10.1371/journal.pone.0217479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pastor-Moreno G, Ruiz-Pérez I, Henares-Montiel J, Petrova D. Intimate partner violence during pregnancy and risk of fetal and neonatal death: a meta-analysis with socioeconomic context indicators. Am J Obstetr Gynecol. 2020;222(2):123–33.e5. doi: 10.1016/j.ajog.2019.07.045. [DOI] [PubMed] [Google Scholar]
- 70.Hill A, Pallitto C, McCleary-Sills J, Garcia-Moreno C. A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int J Gynecol Obstetr. 2016;133(3):269–76. doi: 10.1016/j.ijgo.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 71.Donovan BM, Spracklen CN, Schweizer ML, Ryckman KK, Saftlas AF. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG. 2016;123(8):1289–99. doi: 10.1111/1471-0528.13928. [DOI] [PubMed] [Google Scholar]
- 72.Zou S, Zhang Y, Cao Y, Zhang Y. Correlation of maternal abuse during pregnancy with infant temperament and development. Arch Dis Childhood. 2015;100(10):938. doi: 10.1136/archdischild-2013-305450. [DOI] [PubMed] [Google Scholar]
- 73.Bhandari S, Bullock LFC, Bair-Merritt M, Rose L, Marcantonio K, Campbell JC, et al. Pregnant women experiencing IPV: impact of supportive and non-supportive relationships with their mothers and other supportive adults on perinatal depression: a mixed methods analysis. Issues Ment Health Nurs. 2012;33(12):827–37. doi: 10.3109/01612840.2012.712628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fisher JRW, Tran TD, Hammarberg K, Sastry J, Nguyen H, Rowe H, et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust. 2020;213(10):458–64. doi: 10.5694/mja2.50831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mendoza OTB, Meza Díaz R, Carbajal M. Feminicide Violence Before and During the COVID-19 Health Emergency. Violence Gender. 2021;9(1). 10.1089/vio.2021.0032.
- 76.Bahrami-Vazir E, Mohammad-Alizadeh-Charandabi S, Ghelichkhani F, Mohammadi A, Mirghafourvand M. Intimate partner abuse among couples during pregnancy and its predictors as reported by pregnant women visiting governmental health care centres in Tabriz, Iran. J Biosoc Sci. 2020;52(3):400–11. doi: 10.1017/S002193201900052X. [DOI] [PubMed] [Google Scholar]
- 77.Gashaw BT, Schei B, Magnus JH. Social ecological factors and intimate partner violence in pregnancy. PloS one. 2018;13(3):e0194681-e. doi: 10.1371/journal.pone.0194681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brink J, Cullen P, Beek K, Peters SAE. Intimate partner violence during the COVID-19 pandemic in Western and Southern European countries. Eur J Public Health. 2021;31(5):1058–63. 10.1093/eurpub/ckab093. [DOI] [PMC free article] [PubMed]
- 79.Saha S, Tanmoy AM, Tanni AA, Goswami S, Sium SMA, Saha S, et al. New waves, new variants, old inequity: a continuing COVID-19 crisis. BMJ Glob Health. 2021;6(8):e007031. doi: 10.1136/bmjgh-2021-007031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Khedar RS, Mittal K, Ambaliya HC, Mathur A, Gupta JB, Sharma KK, et al. Greater Covid-19 Severity and Mortality in Hospitalized Patients in Second (Delta Variant) Wave Compared to the First: Single Centre Prospective Study in India. medRxiv. 2021:2021.09.03.21263091.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.