Abstract
Objective
The COVID-19 pandemic has seen a rapid adoption of telehealth consultations, potentially creating new barriers to healthcare access for racial/ethnic minorities. This systematic review explored the use of telehealth consultations for people from racial/ethnic minority populations in relation to health outcomes, access to care, implementation facilitators and barriers, and satisfaction with care.
Materials and Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis and the Joanna Briggs Institute Manual for Evidence Synthesis. Five major databases were searched to identify relevant studies. Screening, full-text review, quality appraisal, and data extraction were all completed independently and in duplicate. A convergent integrated approach to data synthesis was applied with findings reported narratively.
Results
A total of 28 studies met the inclusion criteria. Telehealth-delivered interventions were mostly effective for the treatment/management of physical and mental health conditions including depression, diabetes, and hypertension. In several studies, telehealth improved access to care by providing financial and time benefits to patients. Technological difficulties were the main barriers to effective telehealth consultation, although overall satisfaction with telehealth-delivered care was high.
Discussion
Telehealth-delivered care for racial/ethnic minorities offers promise across a range of conditions and outcomes, particularly when delivered in the patient’s preferred language. However, telehealth may be problematic for some due to cost and limited digital and health literacy.
Conclusion
The development and implementation of guidelines, policies, and practices in relation to telehealth consultations for racial/ethnic minorities should consider the barriers and facilitators identified in this review to ensure existing health disparities are not exacerbated.
Keywords: telehealth, telemedicine, minority health, systematic review, racial/ethnic minorities
BACKGROUND AND SIGNIFICANCE
The global COVID-19 pandemic has seen a rapid adoption of telehealth in lieu of face-to-face consultations due to the need for social distancing and minimization of patient and healthcare provider physical contact.1–3 As a result, the use of telehealth to deliver healthcare services has become widespread.4 Implementation has been rapid with little evidence to guide such widespread adoption and insufficient attention to disparities and digital and health literacy. Consequently, there is a risk that quality of care could be compromised and new access barriers may emerge for underserved groups such as non-Indigenous racial and ethnic minorities who already experience health disparities.5,6
Telehealth consultations, including telemedicine, involve the use of telecommunication technologies between healthcare providers from any healthcare or social care discipline and patients in real time to transmit voice, images, and data for healthcare and health education.7 Using telehealth consultations, healthcare providers can deliver healthcare services and information directly to patients located elsewhere, enable patients to find providers who share their lived experiences and address access problems related to distance and transport, waiting times, cost, and limited patient and clinician time.7–10 Pre-COVID-19, telehealth consultations in Western countries were largely limited to rural and remote patients, psychiatry or niche subspecialties such as cancer genetics.11–14
Existing systematic reviews of telehealth have been conducted in various clinical settings with generally positive findings in relation to patient satisfaction outcomes and consultation effectiveness.15–17 In a review of quantitative studies, healthcare delivered by videoconferencing was effective in assessing and improving patients’ health conditions in 98% of included studies and telehealth improved treatment compliance and accountability for some participants.18 Additionally, telehealth services have been found to improve access to care, and communication and engagement with clinicians from patients’ and informal carers’ perspectives.16 However, telehealth services were not an effective means of psychosocial support in some studies and poor audio-visual quality limited patients’ satisfaction with healthcare.16
Other recent reviews have found telehealth to improve access to healthcare and be acceptable to Indigenous peoples.19–21 Barriers to telehealth services (eg, lack of technical skills) have been identified as well as important enablers such as engagement with Indigenous communities and consideration of local cultural beliefs.22 As First Nations peoples, Indigenous communities are the original inhabitants of their country. The history of attempted genocide and ongoing maltreatment experienced by many Indigenous communities has resulted in significant mistrust of mainstream healthcare services.22 The health needs of Indigenous peoples are unique due to colonization, dispossession, genocide, and forced removal from lands.23,24 Importantly, the strength, resilience, and advocacy of Indigenous peoples, as evident in community-controlled health services in some countries, has led to different healthcare systems and supports.24 These address the social determinants of health and political advocacy as well as clinical interventions to treat disease.19–22 Issues related to health equity experienced by Indigenous peoples and their community-based responses to these issues are therefore different from non-Indigenous racial/ethnic minorities.
Patients and communities from non-Indigenous racial/ethnic minorities are at risk of poorer health outcomes than the majority population because of structural inequities, including lack of access to health information in languages other than English, underutilization of interpreter services, lack of culturally appropriate services, and racism and discrimination.25–29 The use of telehealth consultations may further complicate healthcare access for patients from racial/ethnic minority backgrounds due to other structural issues such as health and digital literacy issues, and challenges in navigating mainstream healthcare systems.29,30 These access barriers are potentially heightened during the COVID-19 pandemic.7
Despite previous reviews of telehealth effectiveness for different patient populations such as older populations, rural and remote communities, and Indigenous peoples, no reviews have been undertaken of studies assessing telehealth consultations specifically for patients and communities from non-Indigenous racial/ethnic minority backgrounds. An evidence synthesis focused on patients and communities from non-Indigenous racial/ethnic minority groups would generate an evidence base for the tailoring of telehealth consultations to their diverse needs.
OBJECTIVE
The objective of this review was to explore the health outcomes, implementation facilitators and barriers, and satisfaction with care, in relation to telehealth consultations for racial/ethnic minority populations in order to make recommendations for practice and future research.
MATERIALS AND METHODS
The study design was a systematic review in accordance with the recommendations of the Joanna Briggs Institute (JBI).
Information sources and search strategy
The protocol for this systematic review was registered in the international register of systematic reviews PROSPERO (CRD 42020221017) and was conducted in accordance with the PRISMA guidelines.31 Studies were identified from a search of the following 5 electronic databases: Ovid Medline, Ovid PsycINFO, EMBASE, CINAHL via EBSCOhost and Scopus. The search was limited to studies published in English between January 1, 2005 and October 9, 2020. Reference lists of included studies were hand-searched for relevant studies.
A list of terms was formulated for the concepts: “telehealth” and “racial or ethnic minority.” These terms were mapped to subject headings (eg, Medical Subject Headings or equivalent) and keywords. Boolean operators were used to group subject headings and keywords to create a search strategy (Supplementary File). A medical research librarian provided input into the search strategy, and a “gold set” of key articles was used to check the comprehensiveness of the search strategy.
Eligibility criteria
To be included in the review the study had to meet the following inclusion criteria:
Sample population included patients of any age from racial/ethnic minorities, their carers or healthcare staff who provided care to racial/ethnic minorities, with study findings disaggregated by racial/ethnic minority group.
For this review, we describe the intervention as “telehealth consultation.” Telehealth consultations occurred instead of a face-to-face consultation (eg, via telephone, videoconferencing) to provide a health service such as a clinical assessment or diagnosis and/or management of a health condition (physical or mental).
Included telehealth consultations in healthcare settings (eg, hospitals, primary care clinics) and in any countries to ascertain the breadth of research internationally. If the provider is in a healthcare setting but the patient is located in a non-healthcare setting (eg, home), then the study is included.
Reported individual health outcomes (eg, physical health, mental health) that could be related to patients/health consumers and caregivers, and/or:
Reported health service outcomes (eg, readmission rates, barriers to implementation). Health service level outcomes may be related to access to care, service delivery, satisfaction with care, and cost-effectiveness.
Used quantitative, qualitative, or mixed methods study designs.
Published in a peer-reviewed journal.
Exclusion criteria were:
Studies did not include participants from racial/ethnic minorities or did not disaggregate findings by racial/ethnic background.
Support services provided as standard practice (eg, phone interpreting, telemonitoring without direct interaction with a healthcare provider) were excluded. Studies that primarily focused on delivery of health promotion and screening programs or health-related education via telehealth.
Publications that were opinion pieces, systematic reviews and meta-analyses, conference abstracts or proceedings, duplicate publications using the same sample and reporting the same outcomes.
Studies published in languages other than English.
The social determinants of health are different for Indigenous peoples compared with other racial/ethnic minorities due to colonization and dispossession. Reviews of telehealth consultations and healthcare for Indigenous peoples have been published.19–22,32 Thus, we did not include Indigenous peoples in the current review. For the purpose of exclusion, we accepted authors’ definitions of “Indigenous participants” as contained in their published reports. All studies, with the exception of one, met our inclusion criteria and only contained non-Indigenous racial/ethnic minority populations. One study, primarily focused on African American patients, had 1 (2.9%) participant who was identified as being American Indian.61
Our definition of “racial/ethnic minority” is based on the term “culturally and linguistically diverse” which is commonly used in Australia (where the authors are based) and refers to “groups and individuals of all genders and all ages who differ from the population in which they live according to race, language and ethnicity except those whose ancestry is Anglo-Saxon, Anglo-Celtic, Indigenous, Aboriginal or Torres Strait Islander.”33
Data screening and extraction
Search results were exported from the electronic databases into systematic review management platform Covidence (Veritas Health Innovation, 2021). Screening was undertaken in 2 phases. Following the removal of duplicates, studies were screened independently in duplicate by 2 reviewers on title and abstract. Conflicts were resolved by a third reviewer. In the second phase, full-text articles were screened independently in duplicate by 2 reviewers, and conflicts were resolved by a third reviewer.
Data extraction was performed by 2 reviewers using Covidence, with differences resolved by a third reviewer. Extracted data comprised the characteristics of each study: country of study, health setting, study aim, study design, sample size and participants’ characteristics (eg, gender, age, race/ethnicity/cultural background), health conditions, and the details of the telehealth intervention. Data were also extracted pertaining to study findings: health outcomes (eg, blood pressure, depression symptoms) and access to healthcare and delivery outcomes (eg, satisfaction with care, implementation barriers and facilitators).
Methodological quality assessment of studies
Risk of bias and critical appraisal were conducted independently in duplicate by 2 reviewers using the JBI Critical Appraisal tools.34 These tools assess the methodological quality of studies of various designs and the extent to which the risk of bias is addressed by authors. For each criterion assessed as “met” on the appropriate tool, a score of “1” was applied. Where criteria were assessed as “not met” or if it was “unclear” to the reviewer, a score of “0” was applied. The scores were then calculated for each study and converted to a final quality rating of “low,” “moderate,” or “high.” (See Supplementary File for JBI critical appraisal criteria for each study design.)
For mixed methods studies, we used 2 screening questions and 5 questions from the “mixed methods studies” section of the Mixed Methods Appraisal Tool,35 which are related to the rationale for using a mixed methods study design and level of interpretation and integration of the qualitative and quantitative components of the study.35
Synthesis of studies
Extracted data were exported from Covidence into a Microsoft Excel spreadsheet for analysis. A convergent integrated approach to data synthesis was taken in accordance with the JBI methodology for mixed methods systematic reviews.34 Due to the heterogeneity of study methodology, design, sample characteristics, and outcome measures, there was no opportunity to conduct a meta-analysis of quantitative studies or a meta-synthesis of qualitative studies. A narrative synthesis was thus conducted where both qualitative and quantitative data were tabulated together and categorized according to the 4 outcomes of interest: health outcomes, implementation barriers and facilitators to telehealth consultations, access to healthcare, and satisfaction with care. A descriptive comparison between studies reporting on the same outcome was performed, with similar and divergent findings reported. Study characteristics, such as country and setting, study methodology and design, sample sizes, and participant characteristics, were examined by calculating frequencies and proportions.
RESULTS
Study selection
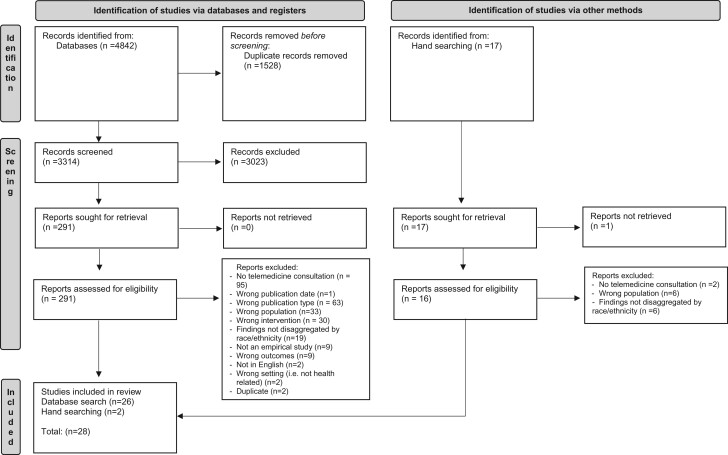
The combined searches from the 5 databases identified 3314 unique articles which were screened using the inclusion and exclusion criteria. A total of 28 articles met the inclusion criteria (Figure 1).
Figure 1.
Flow diagram of study selection. Adapted from PRISMA flow-chart.31
Study characteristics
Studies were published between 2005 and 2019 and comprised 4256 patients and 12 caregivers from racial/ethnic minorities, and 34 healthcare practitioners. Twenty-six (92.9%) studies examined adult populations and 2 focused on pediatric populations.36,37 The majority of studies (n = 23, 82.1%) examined groups located in the United States and utilized quantitative study designs (n = 19, 67.9%). The most common health conditions examined were mental health conditions (n = 17, 60.7%), of which 9 focused on depression. The most frequent study setting was community health centers (n = 8, 28.6%), followed by primary health clinics (n = 5, 17.9%), psychiatric or trauma treatment centers (n = 4, 14.3%), the general community (eg, churches) (n = 3, 10.7%) and HIV clinics (n = 2, 7.1%). The racial/ethnic minority populations included in the studies were predominantly Latino/a or Hispanic (n = 13, 46.4%) and African American (n = 7, 25.0%). Seven studies included Asian participants from Korean and Chinese communities, 3 studies included participants from refugee and immigrant backgrounds, and 1 study described their minority population as “non-white ethnic group.” Six studies included participants from more than 1 racial/ethnic group. Two studies included patients from both racial/ethnic minorities and the majority population and reported results disaggregated by race/ethnicity. Characteristics of included studies are presented in Table 1. (See Supplementary File for detailed information related to study characteristics.)
Table 1.
Summary of included telehealth articles (n = 28)
| n | % | ||
|---|---|---|---|
| Study location | United States | 23 | 82.1 |
| Australia | 1 | 3.6 | |
| Denmark | 1 | 3.6 | |
| Denmark and Sweden | 1 | 3.6 | |
| Korea, Vietnam, Cambodia, and Uzbekistan | 1 | 3.6 | |
| United Kingdom | 1 | 3.6 | |
| Year published | 2005–2009 | 3 | 10.7 |
| 2010–2014 | 16 | 57.1 | |
| 2015–2019 | 9 | 32.1 | |
| Study design | Randomized controlled trial | 11 | 39.3 |
| Cohort | 1 | 3.6 | |
| Quasi-experimental | 2 | 7.1 | |
| Cross-sectional | 4 | 14.3 | |
| Case series | 1 | 3.6 | |
| Mixed methods | 6 | 21.4 | |
| Qualitative | 3 | 10.7 | |
| Study setting | Community health center | 8 | 28.6 |
| Primary care clinic | 5 | 17.9 | |
| Psychiatric or trauma treatment center | 4 | 14.3 | |
| General community | 3 | 10.7 | |
| HIV clinic | 2 | 7.1 | |
| Other | 6 | 21.4 | |
| Health conditiona | Mental health | 17 | 60.7 |
| Cardiovascular related (eg, hypertension) | 8 | 28.6 | |
| Diabetes | 5 | 17.9 | |
| Infectious diseases (eg, HIV, Hepatitis C) | 2 | 7.1 | |
| Primary care | 1 | 3.6 | |
| Health counseling | 1 | 3.6 | |
| Racial/ethnic background of minority participantsb | Hispanic/Latino/a | 13 | 46.4 |
| African American | 7 | 25.0 | |
| Korean and Korean American | 5 | 17.9 | |
| Chinese American | 2 | 7.1 | |
| Other (eg, refugees, non-white ethnic group) | 4 | 14.3 |
Note: Percentages may not add up to 100 due to rounding.
Some studies included more than 1 health condition.
Some studies included participants from more than 1 racial/ethnic group.
Quality assessment
The quality of the included studies was varied with numerous studies not reporting sufficient information to replicate their methods (see Supplementary File). All 11 randomized controlled trials (RCTs) reported randomization of study participants. There was variation in the reporting of allocation concealment and differences in baseline characteristics between groups in some RCTs; however, most reported completion of follow-up assessments and an intent to treat approach to data analysis. As all RCT studies investigated a telehealth consultation between a practitioner and a patient, blinding of participant and practitioner was not possible. Accordingly, no RCT studies reported blinding of participants to intervention group or blinding of practitioners delivering the intervention to group allocation. The number of quality indicators for RCT studies reported ranged from 3/10 to 7/10. Each of the 2 quasi-experimental studies employed a pre/post design with small sample sizes and limited methodological rigor. The quality of reporting for the 1 study utilizing a cohort design and for the 1 study using a case series design was high. Overall, the quality of reporting for studies using cross-sectional, mixed methods, and qualitative designs was low to medium.
Telehealth consultations
Data pertaining to telehealth consultations are presented in Table 2. Across the included studies, telehealth consultations were primarily mental health consultations (n = 17, 60.7%) such as cognitive behavioral therapy (CBT) or psychiatry (telepsychiatry). Physical health consultations were related to chronic disease management (n = 9, 32.1%) and clinical monitoring (n = 2, 7.1%). Physical health diseases managed by telehealth included diabetes (n = 2, 7.1%), hypertension (n = 3, 11%), and infectious diseases (n = 2, 7.1%). Telehealth consultations were used to monitor patients’ clinical status in 2 studies. One study used a telephone triage system and computer-supported decision-making software to conduct a clinical assessment (eg, self-care advice from a clinician).38 (Telephone triage is an approach for handling requests for same-day doctor appointments; when a patient telephones a clinic to request a face-to-face appointment with a provider, their need for an appointment is assessed and the most appropriate management plan arranged.39) The other study monitored patients’ vital signs and other health related information “remotely,” and this was then used to inform virtual consultations by a nurse practitioner who discussed the patient’s medications and recent health data.40
Table 2.
Characteristics of included studies by study design
| First author, year | Country | Health condition | Sample size and participant race/ethnicity | Telemedicine intervention and comparison group | Relevant study outcomes and tools | Summary of results |
|---|---|---|---|---|---|---|
| Rando mized controlled trial | ||||||
| Alcántara 201664 | USA | Mental health (Depression) | Total n = 257; Latino |
|
- Worry symptoms (PSWQ) - Satisfaction with care |
Telephone ECLA significantly* reduced worry symptoms. |
| Chong 201249 | USA | Mental health (Depression) | Overall n = 167; Hispanic |
|
|
Telepsychiatry for depression was acceptable, less definite support for feasibility. |
| Dwight-Johnson 201159 | USA | Mental health (Depression) | Total n = 101; Latino |
|
- Depression (PHQ-9, SCL) | Telephone CBT resulted in significantly* lower depression scores at 6-month follow-up. |
| Han 201042 | USA | Hypertension | Total n = 360; Korean |
|
- Health behavior outcomes (self-report) | Telephone counseling resulted in improved hypertension management outcomes for both groups. |
| Himelhoch 201361 | USA | Mental health (Depression) | Total n = 34; AA = 32, AI = 1, other = 1, Hispanic = 2 |
|
|
Telephone CBT and usual care resulted in significant* decrease in depression. |
| Jackson 201243 | USA | Hypertension | Overall n = 573; AA = 284, white = 289 |
|
- Mean systolic and diastolic blood pressures |
|
| Kim 201144 | USA | Hypertension | Total n = 359; Korean |
|
|
Significant* improvement in BP for both groups over every 2-week period. |
| Moreno 201250 | USA | Mental health (Depression) | Overall n = 182; Hispanic |
|
|
Telepsychiatry resulted in significant* reduction in depression. |
| Vahia 201553 | USA | Mental health | Total n = 27, Latino |
|
- Neurocognition (MMSE, HVLT-revised, Digit Span subtest, BVMT-R) | No significant differences in test performance between control and intervention test. |
| Warren 201538 | United Kingdom | Primary care | Total n = 12 132; white = 11276, other ethnic = 476 | Telephone triage using computer-supported decision-making software by doctor or nurse. Comparison: usual care |
- Satisfaction and ease of accessing care | Patients from ethnic minorities reported higher satisfaction in GP triage compared to usual care, whereas white patients reported higher satisfaction with usual care. |
| Yeung 201655 | USA | Mental health | Total n = 190; Chinese |
|
|
Telepsychiatry resulted in significant* decreases in depression. |
| Cohort | ||||||
| Berg 200941 | USA | Diabetes | Total n = 980; Hispanic |
|
|
Intervention resulted in significant* reductions in inpatient bed days and higher rates of medicine use. |
| Quasi-experimental a | ||||||
| Jang 201462 | USA | Mental health (Depression) | n = 14; Korean |
|
|
Intervention resulted in reduced depressive symptoms at 3-month follow-up. |
| Mayes 201045 | USA | Diabetes | n = 16, Hispanic | Video-telehealth consultations assisted by Promotoras and primary care physician connecting to a medical specialist | - Weight, systolic and diastolic blood pressures, HbA1c |
|
| Cross-sectional a | ||||||
| Mucic 201051 | Denmark and Sweden | Mental health | n = 61; refugees = 45, asylum seekers = 12, migrants = 3, domestic = 1 | Video-telepsychiatry consultations | - Satisfaction with telehealth | Overall high level of satisfaction with video-telepsychiatry consultations. |
| Park 201946 | Korea, Vietnam, Cambodia, Uzbekistan | Health counseling | n = 442; Korean | Video-telehealth counseling | - Satisfaction with telehealth | Overall user satisfaction rates were 96.1% with telehealth. |
| Schulz 201448 | Australia | Infectious diseases |
|
Video-telehealth consultations |
|
Median distance patient travel distance saved was 494 km. Total saved = 54 000 km. |
| Yeung 200956 | USA | Mental health | n = 9; Chinese | Video-telehealth consultations |
|
Overall high satisfaction with telehealth among patients and nurses. |
| Case series a | ||||||
| Stewart 201736 | USA | Mental health | n = 4; Hispanic | Weekly video-telehealth TF-CBT sessions |
|
Positive feasibility outcomes (participants completed treatment and clinicians adhered to TF-CBT model). |
| Mixed methods | ||||||
| Bagchi 201840 | USA | Diabetes, hypertension | n = 10; AA | Video-telehealth consultations | - Satisfaction with telehealth | Overall high satisfaction with telehealth. |
| Glueckauf 201260 | USA | Mental health (Depression) | Total n = 12; AA caregivers |
|
|
Telephone and face-to-face CBT showed improvements in depression. |
| Mucic 200757 | Denmark | Mental health | n = 23; refugees | Video-telepsychiatry consultations | - Satisfaction with telehealth | Overall high satisfaction with telepsychiatry. |
| Stewart 201737 | USA | Mental health | n = 15; Hispanic = 7, AA = 6, white = 2 |
|
|
Intervention resulted in significant* reduction in posttraumatic stress disorder symptoms. |
| Uebelacker 201152 | USA | Mental health (Depression) | Total n = 38; Latino |
|
|
Trend for the intervention group to experience less depression in time. |
| Ye 201254 | USA | Mental health | n = 16; Korean | Video-telehealth consultations | - Feasibility of telepsychiatry | Overall, high level of acceptance with telehealth. |
| Qualitative a | ||||||
| Aisenberg 201258 | USA | Mental health (Depression) | Overall n = 56; Latino n = 5 doctors |
|
|
Overall high satisfaction among patients and providers. |
| Pekmezaris 201647 | USA | Heart failure | n = 4; AA, Hispanic |
|
- Barriers to implementation or usability | Two major themes related to improving equipment and participant engagement in future research. |
| Saberi 201363 | USA | HIV | n = 14; AA | Video-telehealth consultations | - Experiences with telehealth | Participants found telehealth to be convenient, efficient, and positive. |
AA: African American; AI: American Indian; BVMT-R: Brief Visuospatial Memory Test (revised); CBLC: Child Behavior Checklist; CBT: cognitive behavioral therapy; CGI-S: Clinical Global Impressions-Severity of Illness; CGSI-I: Clinical Global Impressions-Improvement; CSQ: Client Satisfaction Questionnaire; D-HELP: Depression Health Enhancement for Latino Patients; ECLA: Engagement and Counseling for Latinos intervention; HIV: Human Immunodeficiency Virus; HBCS: Hill-Bone Compliance Scale; HBP: high blood pressure; HBPM: home blood pressure monitoring; HDRS17: Hamilton Depression Rating Scale; HVLT-revised: Hopkins, Verbal Learning Test-Revised; KDSKA: Kim Depression Scale for Korean Americans; GP: general practitioner (ie, primary care physician); MADRS: Montgomery-Åsberg Depression Rating Scale; MMSE: Mini-Mental State Examination; PHQ-9: Personal Health Questionnaire-9; PSWQ: Penn State Worry Questionnaire; QID-R: Quick Inventory of Depression self-report; Q-LES-Q: Quality of Life Enjoyment and Satisfaction Questionnaire; SCARED: Screen for Children’s Anxiety Related Emotional Disorders, Child Version; SCL: Hopkins Symptom Checklist; SDS: Sheehan’s Disability Scale; SIMH: Satisfaction Index-Mental Health; SMFQ: Short Mood Feeling Questionnaire; T-CSCT: Telepsychiatry-based Culturally Sensitive Collaborative Treatment; TF-CBT: trauma-focused cognitive behavioral therapy; TSQ: Telehealth Satisfaction Questionnaire; UCLA PTSD RI: University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index for DSM-5; VSQ-9: Visit Specific Satisfaction Questionnaire.
Nil comparison group.
P < .5.
The telehealth consultations and interventions were delivered by a range of healthcare professionals including: nurses (n = 10, 35.7%)38,40–48; physicians (n = 13, 46.4%)38,43,45,46,48–57 including psychiatrists, primary care physicians, and specialists; allied health professionals (n = 9, 32.0%)36,37,52,58–63 such as social workers, counselors, and psychologists; and paraprofessional outreach workers in 1 study.45 In 18 studies (64%), the healthcare professionals delivering the telehealth intervention were bilingual. The mode used to deliver the telemedicine intervention was videoconferencing in 16 studies (57.1%) and telephone in 11 studies (39.3%); 1 study used both internet video and telephone communication.45
Health outcomes
In total, 14 studies measured health outcomes with evidence of effectiveness of telehealth on measures of mental health, cardiovascular health and diabetes related outcomes. Three RCTs focused on health outcomes related to treatment of depression, assessing the effect of a telehealth CBT intervention on depression severity compared with face-to-face CBT61,64 or compared with usual care.59 Among Latino patients, worry symptoms were reduced64 and depression symptoms were improved61 following the use of culturally adapted telephone-based CBT compared to face-to-face CBT. In the study by Dwight-Johnson et al,59 Latino patients receiving culturally adapted telephone-based CBT showed greater improvement in depression symptoms over 6 months compared to patients who received usual care.
The effects of telepsychiatry consultations or remote management on improving depression outcomes were reported in 3 RCTs.49,52,55 In a study of Hispanic patients with depression, monthly telepsychiatry consultations and usual care were equally effective in reducing depression scores after 6 months.49 In another pilot RCT,52 telephone-based depression care management plus usual care was compared with the usual care only group. Findings showed a trend for lower levels of depression in the intervention group over time compared with the control group.52 In another study, the effectiveness of culturally sensitive telepsychiatry treatment and care management was compared to usual care for Chinese Americans with depression.55 This study found greater improvement in depressive symptoms following telepsychiatry compared with usual care.55 In a single group pretest posttest design with Korean immigrants, weekly sessions of telepsychiatry for 4 weeks significantly reduced depression scores at immediate follow-up and at 3-month follow-up.62 In a pilot study using a pre-post 2 group design focusing on African American caregivers of older adults with dementia, telephone-based and face-to-face CBT interventions were equally effective in reducing depression scores.60
Three studies assessed the effects of telehealth on cardiovascular and diabetes health outcomes.43–45 In 1 RCT study of patients with hypertension from Korea, biweekly and monthly hypertension-related telephone counseling, and 12-month home monitoring of BP were effective in improving long-term BP outcomes.44 The second study assessed the effectiveness of a telemedicine intervention emphasizing medication management and home BP monitoring with African American patients living with hypertension.43 It found significant improvement in mean systolic blood pressure at 12 months and at 18 months following the intervention compared with usual care, but there were no analogous differences for white patients.43 A study of Hispanic patients living with type 2 diabetes found that telehealth monitoring significantly improved participants’ blood glucose regulation.45 In summary, telehealth was found to have contributed to reduced depression symptoms and improved blood pressure and blood glucose management.
Barriers and facilitators to implementation of telehealth
The majority of studies (n = 17, 60.1%) provided technology access and support to participants (eg, patients were provided with videoconferencing equipment, patients attended digital health centers or primary health clinics with specialized telehealth equipment) as part of their telehealth intervention.36,37,40,42,44–46,48–50,53–57,62,63 Three studies identified technology as a barrier to the implementation of telehealth, which was not unique to a health condition or study design. A mixed method study involving African Americans and Hispanics with mental health conditions identified initial issues with patients logging into the videoconferencing software and technical problems with the equipment.37 In a cross-sectional study involving refugees with infectious diseases, technical difficulties as rated by medical specialists were reported in a quarter of the first telehealth consultations, although this significantly improved with experience.48 A qualitative study involving African Americans and Hispanics with heart failure found that patients had initial concerns with using the equipment, but these dissipated with use.47 This study also reported issues with internet connection, patients managing the intervention alone at home, and concerns with patient literacy. The combined use of audio and text in the telemonitoring program assisted patients’ understanding.47
Factors facilitating use of telehealth were not unique to a health condition or racial/ethnic background. Telehealth consultations using videoconferencing supported health professionals to provide education to patients with mental health conditions by sharing PowerPoint presentations and other written material.36,37 Telehealth permitted caregiver engagement and could be delivered in a language of the patient and caregiver’s preference.36,37 Strategies to assist with telehealth consultations included: face-to-face meetings prior to establishing telehealth to build relationships37 and use of a telemonitoring program with text and audio to help patients understand the instructions.47 In summary, barriers to telehealth were mostly due to technology-related issues, and various strategies were used to facilitate telehealth use such as prior face-to-face meetings and providing text and audio materials.
Access to healthcare
Telehealth improved access to healthcare in a variety of areas. Patients from ethnic minorities reported ease of access to medical help through the GP telephone triage system (vs. usual care) compared with white patients; however, patients from ethnic minorities appeared to report poorer absolute scores than white patients across all 3 trial arms (nurse triage, GP triage, usual care).38 Patients with HIV reported that telehealth allowed quick access to their providers, was more convenient and comfortable in comparison to routine clinic visits, and reduced the need for travel which increased their likelihood of attending appointments.63 Patients with diabetes and hypertension gave favorable ratings to the accessibility of telehealth, specifically ability and time to be seen.40
Satisfaction with telehealth consultations
Overall, 16 studies (57.1%) explored satisfaction with telehealth consultations. Of these, 9 were quantitative studies,38,46,49,51,56,59,61,62,64 5 studies were mixed methods,37,40,52,54,57 and 2 studies used qualitative methods.58,63 Results across the 16 studies were mixed, with the majority of studies (n = 11, 68.8%) reporting high levels of satisfaction with telehealth among patients, carers, and health professionals.37,40,46,49,51,56–59,62,63 Patients’ reasons for satisfaction with telehealth included increased efficiency and convenience, enhanced privacy, and reduced need for travel compared to in-person face-to-face consultations. Physicians saw improvements in their clients with depression,58 and carers found the level of rapport with the therapist was as good as in-person visits.36 Some studies found no discernible differences in levels of satisfaction between telehealth groups and comparison groups (ie, usual care or face-to-face interventions),52,61,64 and patients in 1 study gave mixed feedback about telepsychiatry.54 In a study examining telephone triage, patients from ethnic minorities reported higher satisfaction in the GP triage arm compared to usual care but lower satisfaction compared with white patients overall.38 Thus, the majority of studies found that patients, carers, and providers were satisfied with telehealth consultations.
DISCUSSION
Findings from this systematic review indicate that telehealth for mental health and some physical health conditions between healthcare practitioners and patients from racial/ethnic minorities offer promise across a range of outcomes and healthcare settings and can result in high levels of patient satisfaction. However, it is yet to be determined whether this translates to other healthcare settings, different health conditions, and other racial/ethnic minority populations (particularly in countries outside the United States). Of the 28 included studies, only 2 studies included participants from racial/ethnic minorities and the majority population and reported findings disaggregated by racial/ethnic background. From these 2 studies, it can be ascertained that telehealth did not result in worse outcomes for racial/ethnic minority groups.
Despite the overall positive impact of telehealth consultations for patients from racial/ethnic minority backgrounds, some barriers and challenges were identified by the studies. Technology required to implement telehealth consultations may be problematic for some patients from racial/ethnic minorities because of the cost of equipment, limited understanding of the use of equipment, and limited digital literacy. This concurs with findings from previous reviews of telehealth consultations, including those with Indigenous peoples.15,16,18,22 Additionally, there may be unique and unanticipated challenges to telehealth consultation delivery for some racial/ethnic communities; for example, some may experience anxiety regarding telecommunication including telehealth because of a perceived risk of fraudulent use of telecommunication or because of their fear of contact from immigration authorities.52 Any barriers and challenges to use of telehealth are likely to be further exacerbated by factors related to English language proficiency, cultural factors, lack of familiarity with mainstream health systems, and other existing structural barriers to care (eg, socio-economic conditions, health insurance coverage). This includes awareness of changes in government subsidies related to medical care and advice delivered via telehealth.65
Other literature notes that limited English proficiency can be a significant barrier to health service access and utilization for racial/ethnic minorities, including via telehealth consultations. Among the studies48,51,57 in our review that included refugees, language barriers were not key issues as healthcare providers spoke patients’ native languages or interpreters were used. A recent survey by Rodriguez et al66 found that patients with limited English proficiency had lower rates of telehealth use compared with proficient English speakers. In English-speaking countries, patients with limited English language proficiency may experience substantial difficulties with the use of telehealth and information technology equipment, suggesting that these patients are at greater risk of receiving poorer quality healthcare when engaging in telehealth. Addressing structural (eg, technology and internet broadband) and system (eg, language capabilities and access to support services) barriers to telehealth use will improve the accessibility and equity of health systems and increase engagement among racial/ethnic minority groups and other underserved groups.67 This is particularly urgent in light of the rapid and widespread shift to telehealth consultations during the COVID-19 pandemic which will likely compound disparities in health outcomes for African Americans in particular.
Furthermore, providing culturally appropriate healthcare is also important for racial/ethnic minorities.68 In our review, some of the studies included culturally adapted materials in their telehealth consultations and used bilingual staff or interpreters which are likely to have contributed to the overall positive findings across the included studies. The cultural appropriateness and acceptability of telehealth consultations and development of cultural frameworks to guide telehealth use should be considered more broadly, particularly if services are being delivered transnationally.69,70
Overcoming barriers and challenges to telehealth should address the need for digital literacy and linguistically appropriate online information. Digital literacy refers to a person’s ability to use digital tools (eg, health applications, patient portals, appointment booking) to access, understand, and analyze information and communicate with others.71,72 Although the use of bilingual staff or interpreters to deliver a telehealth consultation may mitigate some of the challenges experienced by racial/ethnic minorities when using telehealth, patients may still face significant barriers due to poor digital literacy and eHealth literacy skills. E-health literacy is the ability to search, understand, and evaluate health information from electronic sources and apply the knowledge in healthcare contexts.73 Previous studies suggest low digital literacy to be a contributing factor to racial/ethnic disparities among telehealth users.74,75
Limitations of the current evidence-base and areas for further research
This review identified key limitations of existing research. Given the more widespread adoption of telehealth consultations across the health system, it is important to understand its impact for patients from racial/ethnic minority groups to ensure equity of healthcare access and utilization. A recent study of telemedicine use during COVID-19 has already identified disparities in telemedicine access for African American patients compared to white patients.6 Future research should explore aspects of telehealth technologies and whether additional supports are required to facilitate its use in racial/ethnic minority populations, particularly for those with low digital literacy and language barriers. Additionally, studies could also examine the impacts of telehealth on underserved populations when technology access, supports, and skills are absent.
Further research is required in other areas such as acute and chronic disease management and in other care settings for racial/ethnic minorities such as cancer care, kidney disease, emergency department admissions, critical care, and pediatrics. Studies should also include patients from various racial/ethnic groups to examine whether there are differences in outcomes between racial/ethnic groups within the same healthcare setting. In this review, studies with African American populations are underrepresented relative to other minorities, potentially reflecting a greater focus on issues related to language by existing research. African American populations may experience other unique barriers to telehealth use which could be investigated in future research. In addition, studies should assess the effectiveness of telehealth on minority patients compared with majority patients and whether different barriers and facilitators are experienced by racial/ethnic minorities compared with the majority population. Healthcare organizations should monitor use of telehealth consultations across patient demographics, including language and racial/ethnic background, to measure the impact on health equity. Although our search strategy identified studies conducted in non-English-speaking countries, most studies were based in the United States. Additional studies are required in other countries with underserved populations who may have less access to information technologies and where the structure and function of the healthcare system may present different enabling and constraining factors.
Included studies were also limited by a lack of methodological rigor across most study designs, resulting in a significant gap in the evidence base. The majority of studies did not have a comparison group, and among the few where a comparison group was present, 1 study38 had a disproportionately larger sample for the white group compared with the “other ethnic” group. Longitudinal studies are needed to determine whether, and to what extent, telehealth consultations affect health-related outcomes over time for racial/ethnic minorities. In particular, the effects of telehealth on early identification of disease and on the long-term management of chronic health conditions are required to maximize long-term health outcomes for racial/ethnic minorities.
Patients from marginalized racial/ethnic minority groups such as refugees were only specifically studied in 3 of the 28 studies.48,51,57 Issues related to caregiver support and the optimal mode of telehealth consultation delivery (ie, telephone vs. videoconferencing) should also be explored in future research. Additionally, future research should also investigate the impact of social determinants such as residential segregation, economic circumstances, and education on telehealth use.
Limitations of the review
Our review has several limitations. Only articles published in English were included; therefore, there is risk of publication bias. Additionally, the search period of January 1, 2005 to October 9, 2020 may have omitted earlier relevant studies. However, information technology enabling telehealth consultation has evolved considerably since the early 21st century. We anticipate that studies published prior to 2005 would have limited relevance. Our screening and search strategy emphasized “racial and ethnic minorities.” This may have excluded studies where efforts were not made to provide inclusive care such as studies which did not include providers who spoke the first language of racial and ethnic minority patients. This may have influenced the generally positive results identified in the review. Our decision to exclude studies focused on Indigenous peoples may have omitted important studies about racial and ethnic minorities. However, a number of recent reviews of Indigenous peoples and telehealth have been undertaken.19–22 Additionally, and in agreement with Stanley et al,23 we argue that Indigenous health requires a specific focus because of the subtle differences in health equity for First Nations peoples.
CONCLUSION
This review has shown telehealth consultations to be mostly positive and beneficial to patients from racial/ethnic minority groups in terms of health outcomes, satisfaction with healthcare, and accessibility of health services. Telehealth delivered to patients in their preferred language or by bilingual health providers contributed to positive outcomes. Challenges to implementation of telehealth consultations across racial/ethnic minority populations were also identified and should be considered in the development and implementation of guidelines, policies, and practices in relation to the use of telehealth across the healthcare system. Further research is needed to understand the long-term impacts of telehealth use to ensure health disparities are not worsened.
AUTHOR CONTRIBUTIONS
All authors contributed to the study conception and design. MT and OC developed the protocol and search strategy with input from LY. All authors contributed to study screening and selection, data extraction, and quality assessment. Data synthesis was conducted by MT, LY, PW, KC, and JA. MT led the writing of the manuscript, with contributions from all coauthors. All authors reviewed and approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICTS OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article are available in the article and in its online supplementary material.
Supplementary Material
Contributor Information
Mandy Truong, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
Ladan Yeganeh, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
Olivia Cook, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
Kimberley Crawford, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
Pauline Wong, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
Jacqueline Allen, Monash Nursing and Midwifery, Monash University, Clayton, Victoria, Australia.
REFERENCES
- 1. Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020; 6 (2): e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. El-Shakankery KH, Kefas J, Crusz SM. Caring for our cancer patients in the wake of COVID-19. Br J Cancer 2020; 123 (1): 3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26 (5): 309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wong MYZ, Gunasekeran DV, Nusinovici S, et al. Telehealth demand trends during the COVID-19 pandemic in the top 50 most affected countries: infodemiological evaluation. JMIR Public Health Surveill 2021; 7 (2): e24445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Delivery 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123. Accessed July 14, 2021. [Google Scholar]
- 6. Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc 2021; 28 (1): 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Global Strategy on Digital Health 2020-2025. Geneva: World Health Organization; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Polinski JM, Barker T, Gagliano N, et al. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med 2016; 31 (3): 269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care 2019; 25 (1): 40–4. [PubMed] [Google Scholar]
- 10. Cox A, Lucas G, Marcu A, et al. Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res 2017; 19 (1): e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thota R, Gill DM, Brant JL, et al. Telehealth is a sustainable population health strategy to lower costs and increase quality of health care in rural Utah. JCO Oncol Pract 2020; 16 (7): e557–62. [DOI] [PubMed] [Google Scholar]
- 12. Zilliacus E, Meiser B, Lobb E, et al. The virtual consultation: practitioners’ experiences of genetic counseling by videoconferencing in Australia. Telemed J E Health 2010; 16 (3): 350–7. [DOI] [PubMed] [Google Scholar]
- 13. Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J Psychiatry 2015; 5 (3): 286–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sabesan S, Kelly J, Evans R, Larkins S. A tele-oncology model replacing face-to-face specialist cancer care: perspectives of patients in North Queensland. J Telemed Telecare 2014; 20 (4): 207–11. [DOI] [PubMed] [Google Scholar]
- 15. Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implementation Sci 2016; 11 (1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PloS One 2019; 14 (8): e0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kruse CS, Krowski N, Rodriguez B, Tran L, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017; 7 (8): e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Almathami HKY, Win KT, Vlahu-Gjorgievska E. Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res 2020; 22 (2): e16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Caffery LJ, Bradford NK, Wickramasinghe SI, Hayman N, Smith AC. Outcomes of using telehealth for the provision of healthcare to Aboriginal and Torres Strait Islander people: a systematic review. Aust N Z J Public Health 2017; 41 (1): 48–53. [DOI] [PubMed] [Google Scholar]
- 20. Kruse CS, Bouffard S, Dougherty M, Parro JS. Telemedicine use in rural Native American communities in the era of the ACA: a systematic literature review. J Med Syst 2016; 40 (6): 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fraser S, Mackean T, Grant J, Hunter K, Towers K, Ivers R. Use of telehealth for health care of Indigenous peoples with chronic conditions: a systematic review. Rural Remote Health 2017; 17 (3): 4205. [DOI] [PubMed] [Google Scholar]
- 22. Wickramasinghe SI, Caffery LJ, Bradford NK, Smith AC. Enablers and barriers in providing telediabetes services for Indigenous communities: a systematic review. J Telemed Telecare 2016; 22 (8): 465–71. [DOI] [PubMed] [Google Scholar]
- 23. Stanley LR, Swaim RC, Kaholokula JKa, Kelly KJ, Belcourt A, Allen J. The imperative for research to promote health equity in Indigenous communities. Prev Sci 2020; 21 (Suppl 1): 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Commonwealth of Australia. Bringing Them Home. National Inquiry into the Separation of Aboriginal and Torres Strait Islander Children from Their Families. Sydney: Human Rights and Equal Opportunity Commission; 1997. [Google Scholar]
- 25. Suphanchaimat R, Kantamaturapoj K, Putthasri W, Prakongsai P. Challenges in the provision of healthcare services for migrants: a systematic review through providers’ lens. BMC Health Serv Res 2015; 15 (1): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bastos JL, Harnois CE, Paradies Y. Health care barriers, racism, and intersectionality in Australia. Soc Sci Med 2018; 199: 209–18. [DOI] [PubMed] [Google Scholar]
- 27. Greenwood N, Habibi R, Smith R, Manthorpe J. Barriers to access and minority ethnic carers’ satisfaction with social care services in the community: a systematic review of qualitative and quantitative literature. Health Soc Care Community 2015; 23 (1): 64–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pangas J, Ogunsiji O, Elmir R, et al. Refugee women’s experiences negotiating motherhood and maternity care in a new country: a meta-ethnographic review. Int J Nurs Stud 2019; 90: 31–45. [DOI] [PubMed] [Google Scholar]
- 29. Kerrigan V, McGrath SY, Majoni SW, et al. From “stuck” to satisfied: aboriginal people’s experience of culturally safe care with interpreters in a Northern Territory hospital. BMC Health Serv Res 2021; 21 (1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ortega G, Rodriguez JA, Maurer LR, et al. Telemedicine, COVID-19, and disparities: policy implications. Health Policy Technol 2020; 9 (3): 368–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dawson AZ, Walker RJ, Campbell JA, et al. Telehealth and indigenous populations around the world: a systematic review on current modalities for physical and mental health. Mhealth 2020; 6: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Goris J, Komaric N, Guandalini A, Francis D, Hawes E. Effectiveness of multicultural health workers in chronic disease prevention and self-management in culturally and linguistically diverse populations: a systematic literature review. Aust J Prim Health 2013; 19 (1): 14–37. [DOI] [PubMed] [Google Scholar]
- 34. Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. Adelaide: Joanna Briggs Institute; 2020.
- 35. Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 2018; 34 (4): 285–91. [Google Scholar]
- 36. Stewart RW, Orengo-Aguayo RE, Gilmore AK, de Arellano M. Addressing barriers to care among Hispanic youth: telehealth delivery of trauma-focused cognitive behavioral therapy. Behav Ther (N Y N Y) 2017; 40 (3): 112–8. [PMC free article] [PubMed] [Google Scholar]
- 37. Stewart RW, Orengo-Aguayo RE, Cohen JA, et al. A pilot study of trauma-focused cognitive–behavioral therapy delivered via telehealth technology. Child Maltreat 2017; 22 (4): 324–33. [DOI] [PubMed] [Google Scholar]
- 38. Warren FC, Calitri R, Fletcher E, et al. Exploring demographic and lifestyle associations with patient experience following telephone triage by a primary care doctor or nurse: secondary analyses from a cluster randomised controlled trial. BMJ Qual Saf 2015; 24 (9): 572–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Holt TA, Fletcher E, Warren F, et al. Telephone triage systems in UK general practice: analysis of consultation duration during the index day in a pragmatic randomised controlled trial. Br J Gen Pract 2016; 66 (644): e214–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bagchi AD, Melamed B, Yeniyurt S, et al. Telemedicine delivery for urban seniors with low computer literacy: a pilot study. Online J Nurs Inform 2018; 22 (2): 1–13. [Google Scholar]
- 41. Berg GD, Wadhwa S. Diabetes disease management results in Hispanic Medicaid patients. J Health Care Poor Underserved 2009; 20 (2): 432–43. [DOI] [PubMed] [Google Scholar]
- 42. Han H-R, Kim J, Kim KB, et al. Implementation and success of nurse telephone counseling in linguistically isolated Korean American patients with high blood pressure. Patient Educ Couns 2010; 80 (1): 130–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jackson GL, Oddone EZ, Olsen MK, et al. Racial differences in the effect of a telephone-delivered hypertension disease management program. J Gen Intern Med 2012; 27 (12): 1682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim MT, Han HR, Hedlin H, et al. Teletransmitted monitoring of blood pressure and bilingual nurse counseling–sustained improvements in blood pressure control during 12 months in hypertensive Korean Americans. J Clin Hypertens 2011; 13 (8): 605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mayes P, Silvers A, Prendergast J. Paraprofessional outreach workers backed by an expert medical team. Telemed J E Health 2010; 16 (3): 358–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Park HY, Kim JY, Koo HY, et al. Evaluation of a telehealth counseling program for expatriates. Telemed J E Health 2019; 25 (8): 693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pekmezaris R, Schwartz RM, Taylor TN, et al. A qualitative analysis to optimize a telemonitoring intervention for heart failure patients from disparity communities. BMC Med Inform Decis Mak 2016; 16: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schulz TR, Richards M, Gasko H, Lohrey J, et al. Telehealth: experience of the first 120 consultations delivered from a new refugee telehealth clinic. Intern Med J 2014; 44 (10): 981–85. [DOI] [PubMed] [Google Scholar]
- 49. Chong J, Moreno F. Feasibility and acceptability of clinic-based telepsychiatry for low-income Hispanic primary care patients. Telemed J E Health 2012; 18 (4): 297–304. [DOI] [PubMed] [Google Scholar]
- 50. Moreno FA, Chong J, Dumbauld J, et al. Use of standard Webcam and Internet equipment for telepsychiatry treatment of depression among underserved Hispanics. Psychiat Serv 2012; 63 (12): 1213–7. [DOI] [PubMed] [Google Scholar]
- 51. Mucic D. Transcultural telepsychiatry and its impact on patient satisfaction. J Telemed Telecare 2010; 16 (5): 237–42. [DOI] [PubMed] [Google Scholar]
- 52. Uebelacker LA, Marootian BA, Tigue P, et al. Telephone depression care management for latino medicaid health plan members: a pilot randomized controlled trial. J Nerv Ment Dis 2011; 199 (9): 678–83. [DOI] [PubMed] [Google Scholar]
- 53. Vahia IV, Ng B, Camacho A, et al. Telepsychiatry for neurocognitive testing in older rural Latino adults. Am J Geriatr Psychiatry 2015; 23 (7): 666–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ye J, Shim R, Lukaszewski T, et al. Telepsychiatry services for Korean immigrants. Telemed J E Health 2012; 18 (10): 797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yeung A, Martinson M, Baer L, et al. The effectiveness of telepsychiatry-based culturally sensitive collaborative treatment for depressed Chinese American immigrants: a randomized controlled trial. J Clin Psychiatry 2016; 77 (8): e996–1002. [DOI] [PubMed] [Google Scholar]
- 56. Yeung A, Johnson DP, Trinh N-H, et al. Feasibility and effectiveness of telepsychiatry services for Chinese immigrants in a nursing home. Telemed J E Health 2009; 15 (4): 336–41. [DOI] [PubMed] [Google Scholar]
- 57. Mucic D. Telepsychiatry pilot-project in Denmark. World Cult Psychiatry Res Rev 2007; 2: 3–9. [Google Scholar]
- 58. Aisenberg E, Dwight-Johnson M, O’Brien M, et al. Building a community-academic partnership: implementing a community-based trial of telephone cognitive behavioral therapy for rural Latinos. Depress Res Treat 2012; 2012: 257858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Dwight-Johnson M, Aisenberg E, Golinelli D, et al. Telephone-based cognitive-behavioral therapy for Latino patients living in rural areas: a randomized pilot study. Psychiat Serv 2011; 62 (8): 936–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Glueckauf RL, Davis WS, Willis F, et al. Telephone-based, cognitive-behavioral therapy for African American dementia caregivers with depression: initial findings. Rehabil Psychol 2012; 57 (2): 124–39. [DOI] [PubMed] [Google Scholar]
- 61. Himelhoch S, Medoff D, Maxfield J, et al. Telephone based cognitive behavioral therapy targeting major depression among urban dwelling, low income people living with HIV/AIDS: results of a randomized controlled trial. AIDS Behav 2013; 17 (8): 2756–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Jang Y, Chiriboga DA, Molinari V, et al. Telecounseling for the linguistically isolated: a pilot study with older Korean immigrants. Gerontologist 2014; 54 (2): 290–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Saberi P, Yuan P, John M, et al. A pilot study to engage and counsel HIV-positive African American youth via telehealth technology. AIDS Patient Care STDs 2013; 27 (9): 529–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Alcántara C, Li X, Wang Y, et al. Treatment moderators and effectiveness of Engagement and Counseling for Latinos intervention on worry reduction in a low-income primary care sample. J Consult Clin Psychol 2016; 84 (11): 1016–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. O’Mara B, Monani D, Carey G. Telehealth, COVID-19 and refugees and migrants in Australia: policy and related barriers and opportunities for more inclusive health and technology systems. Int J Health Policy Manag 2021; 1–5. doi: 10.34172/ijhpm.2021.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood) 2021; 40 (3): 487–95. [DOI] [PubMed] [Google Scholar]
- 67. Anaya YBM, Hernandez GD, Hernandez SA, Hayes-Bautista DE. Meeting them where they are on the web: addressing structural barriers for Latinos in telehealth care. J Am Med Inform Assoc 2021; 28 (10): 2301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Leung AYM, Bo A, Hsiao H-Y, Wang SS, Chi I. Health literacy issues in the care of Chinese American immigrants with diabetes: a qualitative study. BMJ Open 2014; 4 (11): e005294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sivaraman M, Fahmie TA. A systematic review of cultural adaptations in the global application of ABA-based telehealth services. J Appl Behav Anal 2020; 53 (4): 1838–55. [DOI] [PubMed] [Google Scholar]
- 70. Hilty DM, Crawford A, Teshima J, et al. Mobile health and cultural competencies as a foundation for telehealth care: scoping review. J Technol Behav Sci 2021; 6 (2): 197–230. [Google Scholar]
- 71. Martin A, Grudziecki J. DigEuLit: concepts and tools for digital literacy development. Innovation in Teaching and Learning in Information and Computer Sciences 2006; 5 (4): 249–67. [Google Scholar]
- 72. Reddy P, Sharma B, Chaudhary K. Digital literacy: a review of literature. Int J Technoethics 2020; 11 (2): 65–94. [Google Scholar]
- 73. Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006; 8 (2): e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open 2021; 4 (3): ooab056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Goel MS, Brown TL, Williams A, et al. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26 (10): 1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.