Abstract
Adoption of electronic health records (EHRs) and health information exchange (HIE) is a key tool to improving the quality of care in assisted living communities (ALC). We examined whether EHRs were being used in ALC to support HIE in 2010 and 2018. We found that adoption of EHR and HIE functions increased substantially over the study period. However, adoption of HIE functions lagged significantly behind EHR functions in both 2010 and 2018 and was accompanied by growing disparities in the adoption of EHR functions among smaller, nonchain, and for-profit communities. To improve the quality of care for this important and growing population, targeted policies are needed to support the adoption of both EHR and HIE functions in ALC.
Keywords: electronic health record, health information exchange, residential facilities, assisted living facilities
INTRODUCTION
Assisted living communities (ALCs) are long-term care settings that are becoming an increasingly popular residential option for older adults and people with disabilities. ALC (also known as residential care communities) offer residents a consumer-friendly approach to long-term residential care, and often feature private living quarters, a home-like environment, and more independence than nursing homes.1 The ALC population grew 25% from an estimated 733,300 residents in 2010 to 918,700 residents in 2018,2,3 compared with 1,246,079 nursing home residents in 2019.4 Like residents of other long-term care facilities, ALC residents are medically frail: nationally, over half of ALC residents need daily support to take medications, bathe, or walk,2,5 42% have a dementia diagnosis,5 and 70–90% have some form of cognitive impairment.6 ALC residents are more than twice as likely to suffer a hospitalization than age and gender-matched community-dwelling adults.7
Many ALC provide residents with a significant amount of direct care support including medication administration, dementia-specific care, hospice care, care management for chronic disease and primary care, and care coordination.8 Despite their popularity, there is very little federal government oversight of ALC, and therefore, little is known about the infrastructure that exists to support care delivery in ALC. Given the documented benefits of electronic health records (EHRs) in other healthcare settings such as hospitals and nursing homes,9–11 EHRs may be a critical tool to ensure quality of care in ALC. And because of the significant and complex medical needs of ALC residents, ALC may especially benefit from EHR functions that utilize electronic health information exchange (HIE) to facilitate communication with external medical providers and caregivers.12
The outsized impact of coronavirus disease 2019 on ALC has demonstrated the importance of exchanging up-to-date information such as lab results and discharge summaries electronically between ALC and other healthcare settings.13 Although EHR functions such as documentation of clinical notes, medication, and allergy lists are beneficial to care improvement efforts, HIE functions that use external data are potentially more valuable in ALC, as they can be used to ensure that everyone involved in a patient’s care has access to the same up-to-date information.14 However, ALC may face significant challenges to supporting HIE given the lack of policy incentives, resources, and infrastructure necessary to create data linkages with ALC.15 Little is known about how EHRs are currently being used in ALC, specifically whether EHRs are being used to support HIE functions. Although 1 study found that self-reported EHR and HIE adoption among ALC in the United States has risen between 2010 and 2016,16 this study did not examine adoption of individual EHR functions or their utilization of HIE.
In this article, we examine growth in 8 important health information technology (HIT) functions in ALC, comparing characteristics of ALC that are more likely to adopt EHR and HIE in 2010 and 2018.
DATA AND METHODS
Data
We use data from the 2010 National Survey of Residential Care Facilities (NSRCF) and the 2018 National Postacute and Long-term Care Study (NPALS). Both studies were conducted by the National Center for Health Statistics (NCHS) with the same eligibility criteria for inclusion. The 2018 sample size was lower than that of 2010 due to a lower number of eligible ALC and a lower response rate. Excluding 26 ALC that were missing 1 or more data points (9 from 2010 and 17 from 2019), the final analytic sample included 2293 ALC in 2010 and 486 ALC in 2018 for a weighted response rate of 81% and 30%, respectively (see Supplementary Material for details of sampling strategy and characteristics of ALC by year). We used survey weights to present nationally representative estimates with scaled variance to account for single-unit strata in our stratified analyses.
Outcome measures
We categorized 5 EHR functions into 2 categories based on whether they explicitly require information exchange with an external entity. Five “EHR Functions” included: resident demographics, individual service plans, clinical notes, problem list, medication, and allergy list. Three “HIE Functions” includes: prescription and/or lab test ordering, viewing laboratory and/or imaging results, and whether the ALCs report that their computerized system supports HIE with physicians or pharmacies. We chose these functions based on prior literature that examines EHR adoption and use in ALC.17
Organizational characteristics
Based on prior literature, we examined 6 ALC organizational characteristics: community size, chain membership, nonprofit status, Medicaid participation, any dementia care units, and years open.5,17
Statistical analysis
We started by calculating the percent of ALC that adopted each EHR function in each year and ran Chi-squared test to compare adoption across years. We next examined adoption by organizational characteristics by conducting stratified analyses, where we calculated the percent of ALC that adopted all 5 EHR and all 3 HIE functions by organizational characteristics, and ran Chi-squared tests to compare adoption across years. To identify organizational characteristics associated with adoption each year, we ran bivariate analyses comparing adoption within organization types across years using Chi-squared tests. We then ran pooled logistic regression models with the full set of organizational characteristics interacted with year to determine whether the difference in effect sizes were significantly different between years.
RESULTS
Prevalence of EHR and HIE adoption
In 2010, 8.7% of ALC reported having all 5 EHR functions, compared with 24.1% in 2018. In 2010, 2.4% of ALC reported having all 3 HIE functions, compared with 9.7% in 2018. The functions with the highest prevalence of adoption were medication and allergy lists (37.7% in 2010 and 51.0% in 2018), resident demographics (37.4% in 2010 and 45.5% in 2018), and individual service plans (34.4% in 2010 and 48.7% in 2018). The functions with the lowest prevalence of adoption were the 3 HIE functions: support for HIE with physician or pharmacy (10.5% in 2010 and 28.7% in 2018), ordering prescriptions (19.8% in 2010 and 27.7% in 2018), and viewing lab or imaging results (9.7% in 2010 and 24.1% in 2018; Table 1).
Table 1.
2010 and 2018 Adoption of electronic health record and health information exchange functions among assisted living communities, prevalence in percentage points
| 2010 (%) | 2018 (%) | Difference | |
|---|---|---|---|
| All functions (5 EHR and 3 HIE) | 1.1 | 6.4 | 5.3*** |
| EHR functions | |||
| All 5 EHR functions | 8.7 | 24.1 | 12.7*** |
| Medication and allergy lists | 37.7 | 51.0 | 15.4*** |
| Individual service plans | 34.4 | 48.7 | 14.3*** |
| Resident demographics | 37.4 | 45.5 | 8.1** |
| Resident problem list | 18.2 | 38.4 | 20.2*** |
| Clinical notes | 19.7 | 36.9 | 17.2*** |
| HIE functions | |||
| All 3 HIE functions | 2.4 | 9.7 | 7.3*** |
| Support HIE with physician or pharmacy | 10.5 | 28.7 | 18.2*** |
| Order prescriptions | 19.8 | 27.7 | 7.9** |
| Viewing lab or imaging results | 9.7 | 24.1 | 14.4*** |
Notes: The sample sizes were 2294 and 494 in 2010 and 2018, respectively. P values are based on Pearson’s Chi-squared statistic calculated with correction for the complex design. Components may not sum to total due to rounding.
P < .05, **P < .01, ***P < .001.
EHR: electronic health record; HIE: electronic health record.
Adoption of all 8 functions increased significantly over the study period. The 3 EHR functions with the greatest growth in adoption were: problem list (by 20.2 percentage points), supporting HIE with physician or pharmacy (by 18.2 percentage points), and clinical notes (by 17.2 percentage points). The capabilities that had the lowest growth in adoption over the study period were ordering prescriptions (by 7.9 percentage points), capturing resident demographics (by 8.1 percentage points), and individual service plans (by 14.3 percentage points; Table 1).
Bivariate analysis
Bivariate analysis suggests that the observed growth in EHR function adoption was driven primarily by larger ALC. EHR adoption grew significantly among large (26–100 beds) and very large (over 100 beds) ALC but not small (4–10 beds) and medium (11–25 beds) ALC. EHR function adoption increased among all organizational types but not at a uniform rate. Chain-owned, nonprofit, dementia care, non-Medicaid certified, and older (open more than 10 years) ALC adopted EHR functions faster than nonchain, for-profit, nondementia care, Medicaid-certified, and newer ALC (Table 2).
Table 2.
Electronic health record adoption of assisted living communities by organizational characteristics, prevalence in percentage points
| Organizational characteristics | 2010 (%) | 2018 (%) | Difference |
|---|---|---|---|
| Size | |||
| Small (4–10 beds) | 8 | 10 | 2 |
| Medium (11–25 beds) | 10 | 19 | 9 |
| Large (26–100 beds) | 9 | 39 | 30*** |
| Very large (over 100 beds) | 11 | 53 | 41*** |
| Chain membership | |||
| Chain membership | 9 | 29 | 20*** |
| Nonchain member | 8 | 16 | 8** |
| Ownership | |||
| Nonprofit | 11 | 44 | 33*** |
| For profit | 8 | 19 | 11*** |
| Dementia care | |||
| Offers dementia-specific care | 10 | 43 | 34*** |
| Does not offer dementia-specific care | 8 | 17 | 9*** |
| Medicaid certified | |||
| Medicaid certified | 10 | 25 | 15*** |
| Not medicaid Certified | 7 | 23 | 16 |
| Years open | |||
| Newer ALC (<10 years) | 8 | 21 | 13*** |
| Older ALC (10+ years) | 9 | 26 | 17*** |
Notes: The sample sizes were 2294 and 494 in 2010 and 2018, respectively. P values are based on Pearson’s Chi-squared statistic calculated with correction for the complex design. Components may not sum to total due to rounding.
P < .05, **P < .01, ***P < .001.
ALC: assisted living communities.
Similarly, HIE adoption grew significantly among medium (11–25 beds), large (26–100 beds) and very large (over 100 beds) ALC but not small (4–10 beds) ALC. HIE adoption increased among all other organizational types but not at a uniform rate. ALC that were part of a chain, nonprofit ALC, ALC that offer dementia care, non-Medicaid certified, and older ALC adopted HIE functions faster than nonchain, for-profit, nondementia care, Medicaid certified, and newer ALC (Table 3).
Table 3.
Health information exchange adoption of assisted living communities by organizational characteristics, prevalence in percentage points
| Organizational characteristics | 2010 (%) | 2018 (%) | Difference |
|---|---|---|---|
| Size | |||
| Small (4–10 beds) | 2 | 6 | 3 |
| Medium (11–25 beds) | 2 | 11 | 9** |
| Large (26–100 beds) | 2 | 13 | 11*** |
| Very large (over 100 beds) | 3 | 16 | 12*** |
| Chain membership | |||
| Chain member | 4 | 11 | 7*** |
| Nonchain member | 1 | 7 | 6*** |
| Ownership | |||
| Nonprofit | 3 | 15 | 13*** |
| For profit | 2 | 8 | 6*** |
| Dementia care | |||
| Offers dementia-specific care | 4 | 14 | 10*** |
| Does not offer dementia-specific care | 2 | 8 | 6*** |
| Medicaid certified | |||
| Medicaid certified | 3 | 8 | 6*** |
| Not medicaid certified | 2 | 11 | 9*** |
| Years open | |||
| Newer ALC (<10 years) | 2 | 7 | 5*** |
| Older ALC (10+ years) | 3 | 11 | 8*** |
Notes: The sample sizes were 2294 and 494 in 2010 and 2018, respectively. P values are based on Pearson’s Chi-squared statistic calculated with correction for the complex design. Components may not sum to total due to rounding.
P < .05, **P < .01, ***P < .001.
ALC: assisted living communities.
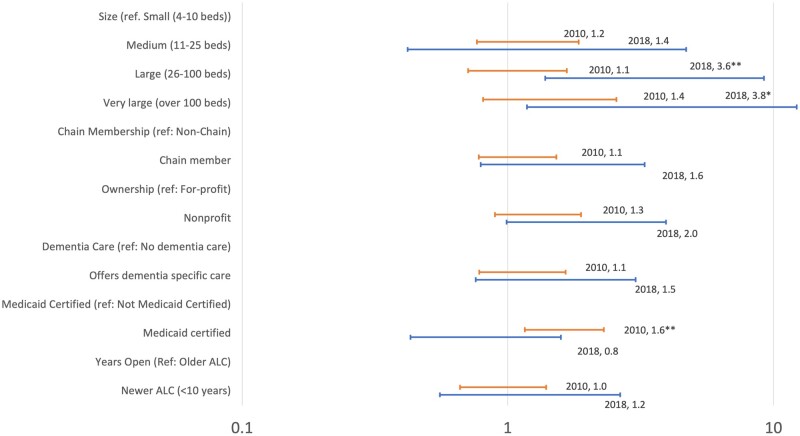
Logistic regression
Logistic regression results revealed that in 2010, Medicaid-certified ALC were significantly more likely to adopt all EHR functions than their non-Medicaid counterparts (OR, 1.6, 95% confidence interval [CI], [1.2, 2.3]). In 2018, large and very large communities were significantly more likely to adopt all EHR functions than their small counterparts (OR, 3.6 and 3.8; CI, [1.4, 9.2] and [1.2, 12.2], respectively). No significant difference in EHR function adoption was observed between newer and older ALC in either year (Figure 1).
Figure 1.
Adjusted odds ratios for adoption of all 5 electronic health record (EHR) functions by assisted living community characteristics, 2010 and 2018. Notes: Five EHR functions include: resident demographics, individual service plans, clinical notes, problem list, medication and allergy list; n = 2779 (2293 and 486 in 2010 and 2018, respectively). Odds ratios from logistic regression model with interaction terms for year. *P < .05, **P < .01, *** P < .001. Confidence intervals and P values estimated using survey weights.
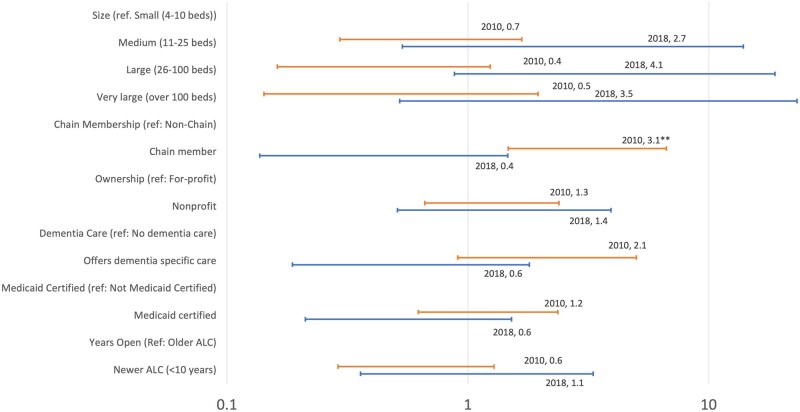
For HIE functions, we found that in 2010, ALC in chains were more likely than nonchain ALC to adopt all HIE functions (OR, 3.1; CI, [1.5, 6.7]). No significant difference in HIE adoption was observed in any other organizational characteristics in either year (Figure 2).
Figure 2.
Adjusted odds ratios for adoption of all 3 health information exchange (HIE) functions by assisted living community characteristics, 2010 and 2018. Notes: HIE functions include: prescription and/or lab test ordering, viewing laboratory and/or imaging results, and whether the assisted living communities report that their computerized system supports HIE with physicians or pharmacies; n = 2779 (2293 and 486 in 2010 and 2018, respectively). Odds ratios from logistic regression model with interaction terms for year. *P < .05, **P < .01, ***P < .001. Confidence intervals and P values estimated using survey weights.
DISCUSSION
This study fills an important gap in our understanding of EHR and HIE use in assisted living communities, a growing and understudied care setting. We find that adoption of EHR and HIE functions increased significantly among ALC from 2010 to 2018 with adoption of all EHR functions more than doubling from 8.7% to 24.1% and adoption of all HIE functions increasing over 4-fold from 2.4% to 9.7%. However, prevalence of EHR and HIE adoption still lags significantly behind that of other long-term care settings such as skilled nursing facilities (SNF), 66% of whom adopted EHRs and 48% of whom were able to access outside information via HIE in 2017.18 These findings align with the social model of care espoused by assisted living industry, which emphasizes aspects of a residential environment with support services (eg, medication management, individual care plans) over medical care.19 ALC might be less inclined to commit resources to EHR and HIE adoption than SNF, given this difference in the philosophy of care provided.
Our finding that EHR and HIE adoption in ALC is low highlights the lack of policy incentives and resources available for ALC to adopt and use HIT. In particular, ALC and other long-term care providers are ineligible to receive incentives through the Medicare and Medicaid EHR Incentive Programs, now known as the Promoting Interoperability Program. Continued low levels of HIE adoption might frustrate ongoing efforts to integrate health and long-term care services as well as efforts to improve primary care delivery to ALC residents in ALC.20 On the other hand, early evidence suggests that as payment reform programs that incentivize care coordination across care settings gain traction, the return on investment of HIE adoption in ALC may improve, leading to greater adoption.21
We also find evidence of growing disparities in the adoption of EHR functions. In particular, consistent with prior research on US hospitals, we find that large and very large communities (26 beds or more) were 3.6 and 3.8 times more likely to adopt EHR functions than small ones.22,23 This may be due to increased resource availability and benefits from economies of scale. However, unlike hospitals, small and medium ALC (<25 beds) make up the majority (65%) of the ALC market.5 Taken together this finding suggests that the majority of ALC will need additional support and incentives to adopt EHR and HIE.
Finally, we find that chain-owned communities were more likely to adopt all HIE functions compared with nonchain communities. This may be because chain-owned communities can pool resources to invest in HIE efforts such as IT expertise and capital, while also benefiting more from economies of scale. At the same time, chain-ownership may also drive market concentration, leading to increased willingness of ALC to share information.24 Chain-ownership among ALC has increased rapidly in recent years, suggesting that chain-ownership may be a critical driver of HIE adoption in the ALC market.20
Results must be interpreted with several limitations in mind. First, because community-level identifiers were not available in this dataset, we were unable to match ALC in both years, limiting our ability to draw inferences about growth in adoption in individual facilities over time. Second, EHR and HIE adoption measures were based on self-report and may not be accurate measures of EHR use. For example, an ALC may have reported that it had the capability to use HIE with physicians and hospitals, but may only do so for a small percentage of patients or use cases (eg, emailing a provider for follow-up questions vs automated transmission of transition of care summaries following a hospitalization). Finally, our results are associational and not meant to draw causal inferences; in other words, we were unable to determine whether changes in EHR adoption were caused by changes in ALC characteristics.
In conclusion, our findings suggest that targeted policies are needed to support the adoption of HIE functions in ALC, especially among smaller communities, which comprise 65% of ALC in the United States.5 Coupled with evidence that ALC residents are more likely to experience unnecessary hospitalizations and have increasing care coordination needs,7,12 our findings suggest that supporting HIE adoption among ALC ought to be a health policy priority to improve the quality of care for this growing population.
AUTHOR CONTRIBUTIONS
SCL and OT conceived the idea, designed the analysis, conducted the analysis, and drafted and revised the article.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article are available from the National Center for Health Statistics, at: https://www.cdc.gov/nchs/npals/index.htm.
Supplementary Material
Contributor Information
Sunny C Lin, Center for Population Health Informatics, Institute for Informatics, Washington University School of Medicine in St. Louis, Saint Louis, Missouri, USA; Center for Health Economics & Policy, Institute for Public Health, Washington University School of Medicine in St. Louis, Saint Louis, Missouri, USA; Department of Medicine, Washington University School of Medicine in St. Louis, Saint Louis, Missouri, USA.
Ozcan Tunalilar, Nohad A. Toulan School of Urban Studies and Planning, Portland State University, Portland, Oregon, USA; Institute on Aging, Portland State University, Portland, Oregon, USA.
REFERENCES
- 1. Zimmerman S, Gruber-Baldini AL, Sloane PD, et al. Assisted living and nursing homes: apples and oranges? Gerontologist 2003; 43 (suppl_2): 107–17. [DOI] [PubMed] [Google Scholar]
- 2. Khatutsky G, Ormond C, Wiener JM, et al. Residential care communities and their residents in 2010: A national portrait. DHHS Publication No. 2016-1041. Hyattsville, MD: National Center for Health Statistics; 2016.
- 3. Caffrey C, Sengupta M, Melekin A. Residential care community resident characteristics: United States. NCHS Data Brief 2018; 2021 (404): 1–8. [CVOCROSSCVO] [PubMed] [Google Scholar]
- 4.KFF’s State Health Facts. Data Source: KFF Analysis of Certification and Survey Provider Enhanced Reports (CASPER) Data, Total Number of Residents in Certified Nursing Facilities; 2019.
- 5. Harris-Kojetin LD, Sengupta M, Lendon JP, Rome V, Valverde R, Caffrey C. Long-term care providers and services users in the United States, 2015–2016. National Center for Health Statistics. Vital Health Stat 2019; 3 (43). [PubMed]
- 6. Zimmerman S, Sloane PD, Reed D. Dementia prevalence and care in assisted living. Health Aff (Millwood) 2014; 33 (4): 658–66. [DOI] [PubMed] [Google Scholar]
- 7. Bartley M, Bartley M, Quigg S, Chandra A, Takahashi PY. Health outcomes from assisted living facilities: a cohort study of a primary care practice. J Am Med Dir Assoc 2018; 19 (3): B26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zimmerman S, Gruber-Baldini AL, Sloane PD, et al. Assisted living and nursing homes. Gerontologist 2003; 43(Spec No 2): 107–17. [DOI] [PubMed] [Google Scholar]
- 9. Menachemi N, Collum TH. Benefits and drawbacks of electronic health. Risk Manag Healthc Policy 2011; 4: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kruse CS, Mileski M, Vijaykumar AG, Viswanathan SV, Suskandla U, Chidambaram Y. Impact of electronic health records on long-term care facilities: systematic review. JMIR Med Inform 2017; 5 (3): e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen M, Guo S, Tan X. Does health information exchange improve patient outcomes? Empirical evidence from Florida hospitals. Health Aff (Millwood) 2019; 38 (2): 197–204. [DOI] [PubMed] [Google Scholar]
- 12. Dys S, Smith L, Tunalilar O, Carder P. Revisiting the role of physicians in assisted living and residential care settings. Gerontol Geriatr Med 2020; 6: 2333721420979840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jenq GY, Mills JP, Malani PN. Preventing COVID-19 in assisted living facilities—a balancing act. JAMA Intern Med 2020; 180 (8): 1106–7. [DOI] [PubMed] [Google Scholar]
- 14. Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc 2010; 17 (3): 288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Adler-Milstein J, Garg A, Zhao W, Patel V. A survey of health information exchange organizations in advance of a nationwide connectivity framework. Health Aff (Millwood) 2021; 40 (5): 736–44. [DOI] [PubMed] [Google Scholar]
- 16. Caffrey C, Cairns C, Rome V. Trends in electronic health record use among residential care communities: United States, 2012, 2014, and 2016. National Health Statistics Reports; no. 140. Hyattsville, MD: National Center for Health Statistics; 2020. [PubMed]
- 17. Holup AA, Dobbs D, Meng H, Hyer K. Facility characteristics associated with the use of electronic health records in residential care facilities. J Am Med Inform Assoc 2013; 20 (4): 787–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Henry J, Pylypchuk Y, Patel V. Electronic Health Record Adoption and Interoperability among U.S. Skilled Nursing Facilities in 2017. ONC Data Brief, no. 41. Washington, DC: Office of the National Coordinator for Health Information Technology; 2018.
- 19. Carder PC. The social world of assisted living. J Aging Stud 2002; 16 (1): 1–18. [Google Scholar]
- 20. Zimmerman S, Carder P, Schwartz L, et al. The imperative to reimagine assisted living. J Am Med Dir Assoc 2022; 23(2): 225–35. [CVOCROSSCVO] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities. J Am Med Dir Assoc 2017; 18 (1): 30–4. [DOI] [PubMed] [Google Scholar]
- 22. Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff (Millwood) 2015; 34 (12): 2174–80. [DOI] [PubMed] [Google Scholar]
- 23. Lin SC, Everson J, Adler-Milstein J. Technology, incentives, or both? Factors related to level of hospital health information exchange. Health Serv Res 2018; 53 (5): 3285–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lin SC, Adler-Milstein J. The relationship between hospital and EHR vendor market dynamics on health information organization presence and participation. BMC Med Inform Decis Mak 2018; 18 (1): 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available from the National Center for Health Statistics, at: https://www.cdc.gov/nchs/npals/index.htm.