Abstract
Introduction
Cerebral vasospasm (CVS) is the leading cause of mortality and morbidity following aneurysmal subarachnoid haemorrhage (aSAH). One of the recently implicated underlying mechanisms of CVS is inflammatory cascades. Specific feasibility objectives include determining the ability to recruit 30 participants over 24 months while at least 75% of them comply with at least 75% of the study protocol and being able to follow 85% of them for 3 months after discharge.
Methods and analysis
This is a feasibility study for a randomised controlled trial. Eligible participants are adult patients who are 18 years of age and older with an aSAH confirmed by a brain CT scan, and CT angiography, or magnetic resonance angiography, or digital subtraction angiography who admitted to the emergency department within 12 hours of the ictus. Eligible subjects will be randomised 1:1 for the administration of either ibuprofen or a placebo, while both groups will concomitantly be treated by the standard of care for 2 weeks. Care givers, patients, outcome assessors and data analysts will be blinded. This will be the first study to investigate the preventive effects of a short-acting non-steroidal anti-inflammatory drug on CVS and the key expected outcome of this pilot study is the feasibility and safety assessment of the administration of ibuprofen in patients with aSAH. The objectives of the definitive trial would be to assess the effect of ibuprofen relative to placebo on mortality, CVS, delayed cerebral ischaemia, and level of disability at 3-month follow-up.
Ethics and dissemination
This study is approved by Mashhad University of Medical Sciences ethical committee (IR.MUMS.MEDICAL.REC.1398.225). Results from the study will be submitted for publication regardless of whether or not there are significant findings.
Trial registration number
Keywords: Stroke, NEUROSURGERY, Clinical trials
Strengths and limitations of this study.
Rigorous trial protocol to evaluate the feasibility and safety of conducting a larger phase III trial to assess the preventive role of ibuprofen on cerebral vasospasm (CVS) secondary to aneurysmal subarachnoid haemorrhage (aSAH).
Based on this feasibility pilot trial, four critical outcomes will be evaluated in the definitive trial including mortality, CVS, delayed cerebral ischaemia and level of disability at 3-month follow-up.
Recruitment of eligible participants in a narrow time window (12-hour) after the occurrence of aSAH is a challenging inclusion criteria that may slow down the advancement of the trial.
To minimise any potential bias, blinding of healthcare providers (physicians, intensive care unit nurses, residents), patients, outcome assessors and data analysts to treatment allocation is being undertaken.
Example of a low cost trial due to using a repurposed Food and Drug Administration approved and affordable agent as prophylactic therapy.
Introduction
Background and rationale
Aneurysmal subarachnoid haemorrhage (aSAH) accounts for 5%–10% of all strokes worldwide, which approximately equals to a total of 600 000 new cases per year.1 Up to 44% of such cases will die,2 and almost 20% of the survived ones would become disabled and dependent.2 Cerebral vasospasm (CVS) following aSAH is the leading cause of mortality and morbidity.3–5
The exact mechanisms of the complex inflammatory cascade leading to CVS is not well understood, and usual treatments have no sufficient therapeutic effects.6–9 However, several studies support the hypothesis that local and systemic inflammatory responses may participate in the process of CVS and its consequent poor outcomes. Increased plasma and cerebrospinal fluid level of inflammatory markers, like tumour necrosis factor-α, and various interleukins during SAH is seen, and this increment is correlated with poor neurological outcomes.10–12 Moreover, the systemic inflammatory response syndrome (SIRS) is associated with poor outcomes after SAH and is presented in up to 63% of patients after SAH.13 14 This becomes an impetus to evaluate the possible effectiveness of anti-inflammatory medications after SAH.
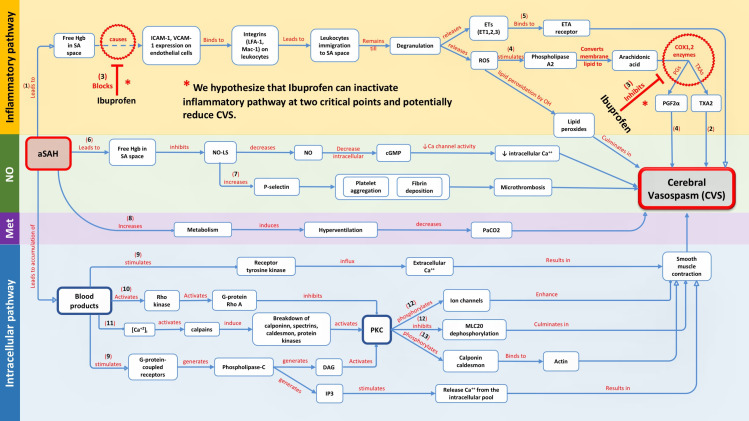
Ibuprofen is one of the non-steroidal anti-inflammatory drugs (NSAIDs) which inhibit cyclooxygenase enzymes in a non-specific manner. In addition to decreasing the level of cytokines and prostaglandins, this drug also prevents the expression of two specific cell adhesion molecules, intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 that belongs to the immunoglobulin superfamily. The immunoglobulin superfamily proteins are upregulated in patients who develop clinical vasospasm.11 Leucocyte integrins bind to these proteins on endothelial cells. The immunoglobulin superfamily proteins are necessary for leukocyte-endothelial cell adhesion and leucocyte migration15–17 (figure 1, online supplemental digital content, part 1).
Figure 1.
Concept map depicting four major pathways for the occurrence of CVS following aSAH. Inflammatory pathway is shown in yellow and explains how ibuprofen may act as a prophylactic agent in this scenario. Numbers in parentheses are representative of corresponding reference for that branch, all concept map references are available in online supplemental digital content, part 1. aSAH, aneurysmal subarachnoid haemorrhage; Ca++, Calcium ion; cGMP, cyclic guanosine monophosphate; COX, cyclooxygenase; DAG, diacylglycerol; ETA, endothelin A; ET, endothelin; Hgb, hemoglobin; ICAM-1, intercellular adhesion molecule-1; IP3, inositol trisphosphate; LFA-1, Lymphocyte function-associated antigen 1; Mac-1, macrophage-1 antigen; Met, metabolic; MLC 20, Myosin light chain 20; NO, nitric oxide; NO-LS, nitric oxide-like substance; PGF2α, prostaglandin F2 alpha; PGs, prostaglandins; PKC, protein kinase C; ROS, reactive oxygen species; SA, subarachnoid; TXAs, thromboxanes; TXA2, thromboxane A2; VCAM-1, vascular cell adhesion molecule-1.
bmjopen-2021-058895supp001.pdf (153.1KB, pdf)
Ibuprofen prevents inflammatory reactions caused by leucocytes with disrupting the process of migration.
Ibuprofen’s efficacy on CVS has been proven in an intracranial model of rabbits when its intracranial administration initiated within 6 hours after SAH, but no effect was observed when treatment is begun later than 12 hours.18 As the acute phase of inflammation starts 3–4 hours after the SAH,11 and ibuprofen is a fast-acting NSAID; it could prevent from binding of macrophages and neutrophils to the endothelial cells and entering the subarachnoid space; hence, reducing the intensity of acute phase inflammation. This inhibitory action, will decrease the number of trapped leucocytes dying and degranulating in the subarachnoid space in the next 2–4 days11, and subsequently may reduce or prevent chronic vasospasm in the upcoming days of admission. Thus, the early administration of ibuprofen considered in this study might be a key to shut off the inflammatory cascade at the initial step (figure 1). Furthermore, in terms of side effects, the potential of NSAIDs to induce haemorrhagic stroke has been heavily dismissed by self-reports, prescriptions databases and large multicentred studies.19
To date, we have found four clinical trials evaluating the efficacy of NSAIDs on vasospasm after aSAH, three of which were focused on the antiplatelet mechanism of aspirin.20–22 The fourth study was a placebo-controlled trial that assessed the preventive effects of meloxicam during 7 days after aSAH.23 However, no clinical data are available regarding the efficacy of a fast-acting oral NSAID for the administration in a narrow time interval after the occurrence of aSAH. In the current study, we sought to investigate the preventive role of ibuprofen on the CVS secondary to aSAH and its outcomes.
Objectives
The objective of the current pilot trial is to establish the feasibility of a larger trial by successfully recruiting 30 participants over a 24-month period and demonstrating adherence to our study protocol. Additionally, we will identify possible adverse events related to the administration of ibuprofen and determine whether its administration is superior to the standard treatment in terms of the prevention of CVS secondary to aSAH and its clinical outcomes.
Trial design
This pilot trial is a single centre, parallel randomised 1:1, controlled, clinical trial. Healthcare providers (physicians, intensive care unit (ICU) nurses, residents), patients, outcome assessors and data analysts will be blinded to treatment allocation. We followed Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist to conduct this pilot clinical trial protocol.24
Methods
Subjects
Inclusion criteria
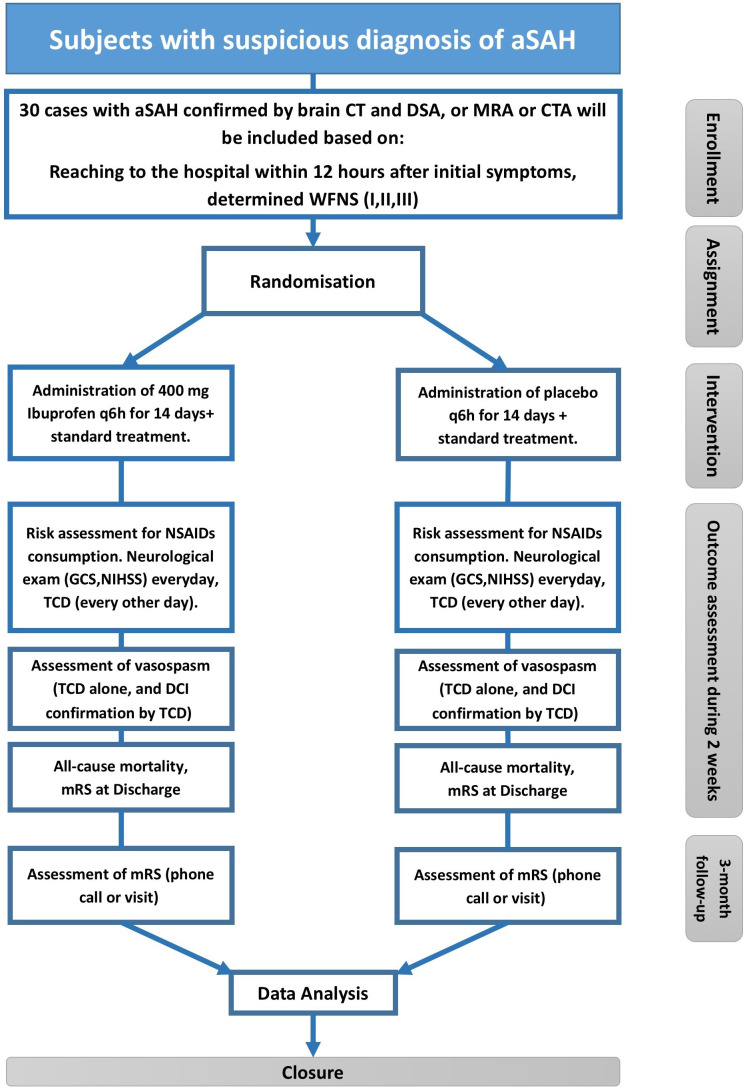
Adult patients who are 18 years of age and older with an aSAH confirmed by a brain CT scan, and CT angiography, or magnetic resonance angiography, or digital subtraction angiography (figure 2).
Admitted to the emergency department within 12 hours of the ictus.
Patients must have a World Federation of Neurological Surgeons score of I, II or III at the initial examination.
Figure 2.
Step-by-step flow diagram of the study. aSAH, aneurysmal subarachnoid haemorrhage; CTA, CT angiography; DCI, delayed cerebral ischaemia; DSA, digital subtraction angiography; GCS, Glasgow coma scale, MRA, magnetic resonance angiography; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; NSAIDs, non-steroidal anti-inflammatory drugs; q6h, every 6 hours; TCD, Transcranial Doppler; WFNS, World Federation of Neurological Surgeons.
Exclusion criteria
Patients who have hypersensitivity to aspirin, ibuprofen or other NSAIDs.
Previous and prolonged use of any type of NSAIDs.
History of aneurysmal re-bleeding, active bleeding of a gastrointestinal ulcer, haemodynamic instability, pregnancy, and current consumption of antiplatelet agents such as clopidogrel and aspirin.
Patients with history of myocardial infarction or percutaneous coronary interventions.
Outcome measures and follow-up
The goal of the current pilot trial is to establish the feasibility of a larger trial by successfully recruiting 30 participants over a 24-month period and demonstrating adherence to our study protocol. Based on the effect estimates coming out of this pilot study, we will calculate a proper sample size for the definitive trial. Specific feasibility objectives include determining:
Our ability to recruit 30 participants over 24 months.
Our ability to follow 85% of participants for 3 months.
Whether at least 75% of participants comply with at least 75% of the study protocol.
Objectives for the definitive trial
The primary research objective is:
To determine the effects of ibuprofen versus placebo on the rate of all-cause mortality.
The secondary research objectives are:
To assess whether the administration of ibuprofen in patients with aSAH, could prevent the occurrence of CVS vs placebo.
To determine the effects of ibuprofen versus placebo on the occurrence of delayed cerebral ischaemia (DCI).
To elucidate the effects of ibuprofen versus placebo on the level of disability based on modified Rankin Scale at discharge and 3-month follow-up.
Study description
The patients will be hospitalised for at least 14 days because the maximum inflammation in the subarachnoid space occurs between days 9 and 14. Based on our institutional protocol for the management of SAH, nimodipine 60 mg every 4 hours for 21 days, appropriate fluid therapy and phenytoin will be administrated for all patients, and microsurgical aneurysmal clipping in patients presenting with large (>50 mL) intraparenchymal haematomas and middle cerebral artery aneurysms, or interventional coiling will be performed for elderly (>70 years of age) patients, in those presenting with poor-grade aSAH, and in those with aneurysms of the basilar apex.25
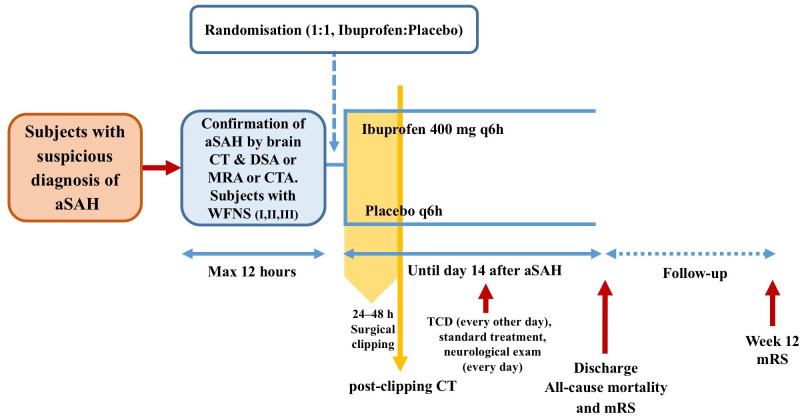
In the ibuprofen arm, eligible patients (online supplemental digital content, part 2) will receive ibuprofen capsules 400 mg/every 6 hours for 14 days, added to standard treatment (figure 3). Manufactured ibuprofen capsules will be administered orally in the intervention group. This dosage is an anti-inflammatory dose of ibuprofen and is placed in the middle of the therapeutic window of this drug. In the control group, placebo capsules that are manufactured identical to the ibuprofen capsules in terms of colour, size and shape; will be ordered in the same way as the intervention group. In subjects who are lethargic or have impaired consciousness, medication and placebo will be administered through enteral tube. The criteria for the evaluation of vasospasm and the scales used for assessing disability are discussed in online supplemental digital content, part 3.
Figure 3.
Timeline of the study. aSAH, aneurysmal subarachnoid haemorrhage; CTA, CT angiography; DSA, digital subtraction angiography; MRA, magnetic resonance angiography; mRS, modified Rankin Scale; q6h, every 6 hours; TCD, transcranial Doppler; WFNS, World Federation of Neurological Surgeons.
Randomisation and allocation
To protect the blinding and integrity of the study (online supplemental digital content, part 4), a statistician who is not affiliated to the research team develops the randomisation plan. The statistician will generate a permuted block randomisation table using an online random sequence generator with an allocation list in random order. The allocation ratio is 1:1. An independent investigator allocates participants into two groups. The allocator uses an online computer-based randomisation programme (http://www.randomization.com) to randomise permutation.26 In the first step, the statistician uses Randomization.com’s pseudo-random number generator of Wichmann and Hill (1982) as modified by McLeod to specify a treatment (A or B) to each participant file numbered 1–30. In the second step, an independent investigator will provide a random permutation of all of the integers from the smallest to the largest by the programme. The independent investigator gives a file to each participant by the order provided in the previous step. The allocator will pick up a covered, sealed envelope from a box in which sequentially numbered envelopes are shuffled. Patients will receive drug A or B according to the method of allocation mentioned above.
Sample size
Our sample size is based on the confidence interval (CI) around the proportion of complete follow-up. We will consider the pilot successful if we achieved at least 85% follow-up at 3 months for our primary trial outcomes. If 29/30 participants achieve successful follow-up, the lower boundary of the 95% CI will be above 85%, and we will consider the trial feasible. If less than 22/30 achieve complete follow-up, the upper boundary of the CI will be below 85%, and we will consider the trial unfeasible. Therefore, if between 22 and 29 out of 30 patients complete a 3-month follow-up, the feasibility of the trial will remain uncertain; however, we will consider this satisfactory.
Data management and statistical analysis
The analysis and reporting of results will follow the Consolidated Standards of Reporting Trials (CONSORT) guidelines for reporting of randomised pilot and feasibility trials.27 Data will be collected on forms and archived in a password-protected encrypted electronic database. All recruited and randomised patients will be included in the analysis. Data analysis will be performed by a blinded investigator with treatment groups coded as A and B. All data collected will be summarised for reporting purposes using descriptive statistics.
Feasibility analysis (primary)
Data will be collected on forms and archived in a password-protected encrypted electronic database. Point estimates of recruitment and feasibility events, including adherence to protocol and follow-up rate at 3 months, will be presented as proportions with 95% CIs. The pilot study results will be evaluated to identify recruitment issues, data management issues and inform anticipated follow-up rates.
Efficacy analysis for definitive study (secondary)
We plan to include the data from our pilot in the definitive trial if we can demonstrate feasibility, assuming no important changes to our patient population, intervention or outcome measures. All patients enrolled in the trial and randomised will be included in the analysis, regardless of the level of adherence to the intervention or any other deviation from the protocol. Due to the low power of the pilot study, we will report the descriptive results for all efficacy-related and harm-related outcomes. We will not complete any subgroup, sensitivity or interim analysis due to the small sample size.
Quality assurance
The principal investigator along with a member of institutional ethics committee will systematically monitor and evaluate the various aspects of project to ensure standards of quality are met. Standards of quality include Good Clinical Practice Guidelines, Ethical Conduct for Research, study protocol and institutional policies. All investigators will participate in a training session before the commencement of the study to ensure about the consistency of data collection and study procedures. Data will be managed in a secured computer system by a dedicated neurosurgery resident under the supervision of the principal investigator. In case of any doubt or uncertainty about data forms, the site investigators will be informed.
Also, for further assurance, multiple checkpoints are defined during the trial, including the presence of signed informed consents obtained by the neurosurgery residents, respect of the inclusion and exclusion criteria, appropriate and instant reporting of any adverse events and the monitoring of all steps of the follow-up. All the files and data will be sealed and archived in a secure place at the end of the trial, once the final analysis is completed.
Trial status
The trial is in the recruitment phase and patient enrolment is planned to be completed in April 2022, and the last recruited patient will be due for final outcome assessment in July 2022.
Safety considerations
Concerning complications of NSAIDs, patients are classified into three categories: low, moderate and high risk.28 Low-risk patients are younger than 65 years without any cardiovascular risk factors. Moderate-risk patients are those 65 years of age or older without a history of gastrointestinal ulcer and had mild cardiovascular risk factors. Patients who are over 65 years old who have kidney or liver diseases or hypertension, having a history of a gastrointestinal ulcer or multiple gastrointestinal risk factors, history of cardiovascular diseases, as well as having a history of heart failure are considered as a high-risk patient.28 In the first group, routine care will be provided. Pantoprazole is administered in the moderate-risk and high-risk group along with ibuprofen. We strictly monitor blood pressure as a part of our routine management of all patients in ICU. Moreover, urea, creatinine and electrolytes (sodium and potassium) of moderate-risk patients will be measured every 3 days, while the same tests will be requested for the high-risk group every day.28 Administration of the study drug ceases if any serious adverse events happen or adverse effects prevent the tolerability of the ibuprofen (online supplemental digital content, parts 5 and 6) or the patient wishes to withdraw the consent before the study ends.
Based on the recommendation of extension of the CONSORT statement on better reporting of harms in randomised trials,27 29 we will collect and appropriately report all good and bad events and outcomes so that they may be compared across treatment groups. Also, according to the same statement, the balance of benefits and harm will be discussed in the final publication of the pilot trial. In addition, for assessing the severity of adverse events (including clinical and laboratory abnormalities) and grading them among the participants, we will use the Table for Grading the Severity of Adult and Pediatric Adverse Events.30 Four comprehensive sections regarding the management and reporting adverse events are provided in the online supplemental digital content, parts 5, 6, 7 and 8.
Follow-up
The clinical team will do in person follow-up with the patients every day for any adverse events during initial admission and weekly for the first 3 weeks if discharged. A 3-month in-person visit or phone interview is arranged for the assessment of disability outcomes and possible adverse events. Contact information will be available for the enrolled patients for questions or possible adverse event reports during the study period.
Expected outcomes of the study
The key expected result of this pilot study is the feasibility and safety assessment of the administration of ibuprofen in patients with aSAH. The objectives of the definitive trial are mentioned in the methods section. During the pilot trial, we will collect information on all outcomes for the definitive trial.
Duration of the project
This project is scheduled to last 24 months. The first patient recruited in June 2020 and the last one is planned to be included by April 2022, the end of the follow-up period for the last patient would be in July 2022.
Project management
Principal investigator: Oversight of all study procedures and managing the relations with the source of funding.
Research scientist: Study design, drafting of the proposal, randomised controlled trial registration and drafting of the manuscript.
Study coordinator: Blinding, randomisation of the participants, organising datasheets and coordinating members of the team.
Neurosurgery residents: Check patients’ eligibility, consenting, assessing clinical DCI, diagnosing and managing of the adverse events, order Transcranial Doppler (TCD), and ibuprofen.
Neurologist: A clinical stroke fellow will do the TCD.
Statistician: Assistance regarding study design, revising the manuscript and data analysis.
Ethics and dissemination
This study is approved by Mashhad University of Medical Sciences (MUMS) ethical committee (IR.MUMS.MEDICAL.REC.1398.225). Written informed consent will be obtained from the eligible patients or next of kin for enrollment to the study.
Dissemination policy
Results from the study will be submitted for publication regardless of whether or not there are significant findings. Every attempt will be made to ensure that the amount of time between completing data collection and the release of study findings is minimised. The Methods Centre will also be responsible for reporting required results on the ISRCTN registry.
Patient and public involvement
Patients and public were not involved in this study.
Discussion
CVS is a common devastating complication of the aSAH. Pharmacological management of this clinical problem is still a controversial issue.
We have found some pieces of evidence through in vitro,31 animal18 32 and human33 34 studies indicating that some NSAIDs might be a promising choice to be used as a repurposing approved agent for the prevention of CVS secondary to aSAH.
In a propensity score-matched analysis study by Nassiri et al,33 consumption of NSAIDs with various therapeutic indications was assessed in patients with aSAH. Results demonstrated a reduction in mortality and improved functional outcomes.24 These effects were independent of the development of DCI or vasospasm. Furthermore, patients treated with NSAIDs had reduced ICU and hospital stay. The authors hypothesised that inflammation may have a critical role in development of poor outcomes (disability and death) after aSAH and patients with aSAH may find some benefit from NSAIDs.
A large, high-quality trial is needed to establish whether adding ibuprofen to standard treatment effectively reduces vasospasm after aSAH. Such a trial poses fundamental challenges for methodological design as well as complexities of execution. Thus, a prerequisite pilot trial is required to justify if the preliminary plan can be implemented in a larger definitive trial.
Ibuprofen is a Food and Drug Administration-approved anti-inflammatory medication; however, using it in a new clinical condition as a repurposing approved agent to prevent CVS requires further evaluation. Since there is no previous phase III trial for this purpose, we planned to run feasibility pilot study before the definitive trial.
Supplementary Material
Acknowledgments
We appreciate the deputy of research at Mashhad University of Medical Sciences for the financial support of this project.
Footnotes
Contributors: SZ and MD conceptualised the study. MD, EMM, VA and BS designed the study, EMM and MJY coordinated the administrative tasks. EMM and MD did the literature search, and drafted the initial version of the manuscript. MD designed the concept map and all figures. JG, NG and SZ and all authors critically reviewed and approved the final manuscript as submitted.
Funding: This study was funded by Mashhad University of Medical Sciences, Deputy of Research, Grant No.971587.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Feigin VL, Lawes CMM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355–69. 10.1016/S1474-4422(09)70025-0 [DOI] [PubMed] [Google Scholar]
- 2.Nieuwkamp DJ, Setz LE, Algra A, et al. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol 2009;8:635–42. 10.1016/S1474-4422(09)70126-7 [DOI] [PubMed] [Google Scholar]
- 3.Mayberg MR. Cerebral vasospasm. Neurosurg Clin N Am 1998;9:615–27. 10.1016/S1042-3680(18)30256-0 [DOI] [PubMed] [Google Scholar]
- 4.Claassen J, Bernardini GL, Kreiter K, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke 2001;32:2012–20. 10.1161/hs0901.095677 [DOI] [PubMed] [Google Scholar]
- 5.Kreiter KT, Copeland D, Bernardini GL, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke 2002;33:200–9. 10.1161/hs0102.101080 [DOI] [PubMed] [Google Scholar]
- 6.Mocco J, Zacharia BE, Komotar RJ, et al. A review of current and future medical therapies for cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Neurosurg Focus 2006;21:1–7. 10.3171/foc.2006.21.3.9 [DOI] [PubMed] [Google Scholar]
- 7.Belen D, Besalti O, Yiğitkanli K, et al. Leflunomide prevents vasospasm secondary to subarachnoid haemorrhage. Acta Neurochir 2007;149:1041–8. 10.1007/s00701-007-1275-1 [DOI] [PubMed] [Google Scholar]
- 8.Vural M, Cosan TE, Ozbek Z, et al. Digoxin may provide protection against vasospasm in subarachnoid haemorrhage. Acta Neurochir 2009;151:1135–41. 10.1007/s00701-009-0391-5 [DOI] [PubMed] [Google Scholar]
- 9.Günaldi O, Tuğcu B, Cöllüoğlu B, et al. Morphometric analysis of the influence of selenium over vasospastic femoral artery in rats. Acta Neurochir 2010;152:855–60. 10.1007/s00701-010-0599-4 [DOI] [PubMed] [Google Scholar]
- 10.Polin RS, Bavbek M, Shaffrey ME, et al. Detection of soluble E-selectin, ICAM-1, VCAM-1, and L-selectin in the cerebrospinal fluid of patients after subarachnoid hemorrhage. J Neurosurg 1998;89:559–67. 10.3171/jns.1998.89.4.0559 [DOI] [PubMed] [Google Scholar]
- 11.Chaichana KL, Pradilla G, Huang J, et al. Role of inflammation (leukocyte-endothelial cell interactions) in vasospasm after subarachnoid hemorrhage. World Neurosurg 2010;73:22–41. 10.1016/j.surneu.2009.05.027 [DOI] [PubMed] [Google Scholar]
- 12.Muroi C, Hugelshofer M, Seule M, et al. Correlation among systemic inflammatory parameter, occurrence of delayed neurological deficits, and outcome after aneurysmal subarachnoid hemorrhage. Neurosurgery 2013;72:367–75. 10.1227/NEU.0b013e31828048ce [DOI] [PubMed] [Google Scholar]
- 13.Tam AKH, Ilodigwe D, Mocco J, et al. Impact of systemic inflammatory response syndrome on vasospasm, cerebral infarction, and outcome after subarachnoid hemorrhage: exploratory analysis of CONSCIOUS-1 database. Neurocrit Care 2010;13:182–9. 10.1007/s12028-010-9402-x [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim GM, Morgan BR, Macdonald RL. Patient phenotypes associated with outcomes after aneurysmal subarachnoid hemorrhage: a principal component analysis. Stroke 2014;45:670–6. 10.1161/STROKEAHA.113.003078 [DOI] [PubMed] [Google Scholar]
- 15.Larson RS, Springer TA. Structure and function of leukocyte integrins. Immunol Rev 1990;114:181–217. 10.1111/j.1600-065X.1990.tb00565.x [DOI] [PubMed] [Google Scholar]
- 16.de Fougerolles AR, Stacker SA, Schwarting R, et al. Characterization of ICAM-2 and evidence for a third counter-receptor for LFA-1. J Exp Med 1991;174:253–67. 10.1084/jem.174.1.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lollo BA, Chan KW, Hanson EM, et al. Direct evidence for two affinity states for lymphocyte function-associated antigen 1 on activated T cells. J Biol Chem 1993;268:21693–700. 10.1016/S0021-9258(20)80597-3 [DOI] [PubMed] [Google Scholar]
- 18.Frazier JL, Pradilla G, Wang PP, et al. Inhibition of cerebral vasospasm by intracranial delivery of ibuprofen from a controlled-release polymer in a rabbit model of subarachnoid hemorrhage. J Neurosurg 2004;101:93–8. 10.3171/jns.2004.101.1.0093 [DOI] [PubMed] [Google Scholar]
- 19.Young AMH, Karri SK, Ogilvy CS. Non-steroidal anti-inflammatory drugs used as a treatment modality in subarachnoid hemorrhage. Curr Drug Saf 2012;7:197–201. 10.2174/157488612803251342 [DOI] [PubMed] [Google Scholar]
- 20.Mendelow AD, Stockdill G, Steers AJ, et al. Double-blind trial of aspirin in patient receiving tranexamic acid for subarachnoid hemorrhage. Acta Neurochir 1982;62:195–202. 10.1007/BF01403624 [DOI] [PubMed] [Google Scholar]
- 21.Hop JW, Rinkel GJ, Algra A, et al. Randomized pilot trial of postoperative aspirin in subarachnoid hemorrhage. Neurology 2000;54:872–8. 10.1212/WNL.54.4.872 [DOI] [PubMed] [Google Scholar]
- 22.van den Bergh WM, Algra A, et al. , MASH Study Group . Randomized controlled trial of acetylsalicylic acid in aneurysmal subarachnoid hemorrhage: the mash study. Stroke 2006;37:2326–30. 10.1161/01.STR.0000236841.16055.0f [DOI] [PubMed] [Google Scholar]
- 23.Ghodsi SM, Mohebbi N, Naderi S, et al. Comparative efficacy of meloxicam and placebo in vasospasm of patients with subarachnoid hemorrhage. Iran J Pharm Res 2015;14:125–30. [PMC free article] [PubMed] [Google Scholar]
- 24.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart Association/american stroke association. Stroke 2012;43:1711–37. 10.1161/STR.0b013e3182587839 [DOI] [PubMed] [Google Scholar]
- 26.Lachin JM, Matts JP, Wei LJ. Randomization in clinical trials: conclusions and recommendations. Control Clin Trials 1988;9:365–74. 10.1016/0197-2456(88)90049-9 [DOI] [PubMed] [Google Scholar]
- 27.Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355:i5239. 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther 2013;15(Suppl 3):S2. 10.1186/ar4174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ioannidis JPA, Evans SJW, Gøtzsche PC, et al. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med 2004;141:781–8. 10.7326/0003-4819-141-10-200411160-00009 [DOI] [PubMed] [Google Scholar]
- 30.National Institute of Allergy and Infectious Diseases, National Institutes of Health . Division of AIDS (DAIDS) table for grading the severity of adult and pediatric adverse events. Corrected version 2.1 ed. United States, 2017. [Google Scholar]
- 31.Kapiotis S, Sengoelge G, Sperr WR, et al. Ibuprofen inhibits pyrogen-dependent expression of VCAM-1 and ICAM-1 on human endothelial cells. Life Sci 1996;58:2167–81. 10.1016/0024-3205(96)00210-X [DOI] [PubMed] [Google Scholar]
- 32.White RP, Robertson JT. Comparison of piroxicam, meclofenamate, ibuprofen, aspirin, and prostacyclin efficacy in a chronic model of cerebral vasospasm. Neurosurgery 1983;12:40–6. 10.1227/00006123-198301000-00008 [DOI] [PubMed] [Google Scholar]
- 33.Nassiri F, Ibrahim GM, Badhiwala JH, et al. A propensity score-matched study of the use of non-steroidal anti-inflammatory agents following aneurysmal subarachnoid hemorrhage. Neurocrit Care 2016;25:351–8. 10.1007/s12028-016-0266-6 [DOI] [PubMed] [Google Scholar]
- 34.Muroi C, Hugelshofer M, Seule M, et al. The impact of nonsteroidal anti-inflammatory drugs on inflammatory response after aneurysmal subarachnoid hemorrhage. Neurocrit Care 2014;20:240–6. 10.1007/s12028-013-9930-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058895supp001.pdf (153.1KB, pdf)