Abstract
Background:
Erythema nodosum-like sarcoid lesion is a specific form of cutaneous sarcoidosis sometimes observed in Japanese patients, with a female predominance, involving the lower extremities. By contrast, erythema nodosum as a non-specific cutaneous manifestation associated with sarcoidosis is rare in Japan. Erythema nodosum-like sarcoid lesion resembles erythema nodosum only in appearance, but histologically shows sarcoid granulomas.
Objectives:
To determine the clinical characteristics of erythema nodosum-like sarcoid lesion.
Methods:
We examined the clinical characteristics of erythema nodosum-like sarcoid lesion in our patients with sarcoidosis. Clinical charts were retrospectively examined from 2000 to 2019. The patients’ data, such as age, gender, types of cutaneous lesion, serum levels of angiotensin-converting enzyme, and extracutaneous organ involvement, were evaluated. We also reviewed cases of erythema nodosum-like sarcoid lesion reported in previous literature.
Results:
Among 101 cutaneous sarcoidosis patients, eight were diagnosed as having erythema nodosum-like sarcoid lesion in our department. The patients were one male and seven females, and their ages ranged from 30 to 74 years old. All cases involved the lower extremities. The serum angiotensin-converting enzyme level was elevated in five cases. Lung sarcoidosis was observed in all cases, and ocular sarcoidosis was observed in six cases, whereas no patients had cardiac sarcoidosis.
Conclusions:
Although erythema nodosum-like sarcoid lesion may not be major skin manifestation of sarcoidosis, erythema nodosum-like sarcoid lesion frequently accompanies lung and ocular sarcoidosis. Thus, we should pay much attention to erythema nodosum-like sarcoid lesion for early identification of patients needing workup for systemic illness.
Keywords: cutaneous sarcoidosis, erythema nodosum-like lesion, specific lesion, erythema nodosum, ocular sarcoidosis, lower sarcoidosis
Introduction
Cutaneous sarcoidosis presents with various clinical features, and the associated skin lesions are classified as either specific or non-specific. Erythema nodosum is characterized by painful erythematous lesions, which usually occur in the lower extremities and show septal panniculitis histologically. It is a common skin lesion of sarcoidosis; however, it is classified as a non-specific skin lesion because it usually does not show sarcoid granulomas histologically. Erythema nodosum may represent a delayed hypersensitivity reaction to various antigens in sarcoidosis patients, who may show aberrant immune responses to unknown antigenic triggers (1).
On the other hand, erythema nodosum-like sarcoid lesion (ENLS) is a rare specific form of cutaneous sarcoidosis, which resembles erythema nodosum only in appearance, but histologically presents with sarcoid granulomas. This type is rare in Western countries, and only a few cases have been reported, as an atypical form of cutaneous sarcoidosis (2). By contrast, in Japanese patients with sarcoidosis, ENLS is sometimes observed (3–5), whereas erythema nodosum is rarely seen (6). To determine the clinical characteristics of ENLS, we examined the cases in our department and reviewed previously published Japanese cases of sarcoidosis presenting with ENLS.
Materials and methods
All enrolled patients were diagnosed with cutaneous sarcoidosis based on histological findings of non-caseating epithelioid cell granulomas, using the pathology database from the Department of Dermatology of Fukushima Medical University from 2000 to 2019. Other granulomatous diseases, such as tuberculosis, deep fungal infection, necrobiosis lipoidica, or granuloma annulare, were excluded. Clinical charts were retrospectively examined, and the patients’ data, such as age, gender, types of cutaneous lesion, serum levels of angiotensin-converting enzyme (ACE), and extracutaneous organ involvement, were evaluated. Clinical characteristics were compared between ENLS patients and non-ENLS patients by the Mann-Whitney U test for quantitative parameters and the χ2 test or Fisher exact test for qualitative parameters. Values of P < 0.05 were considered statistically significant. These statistical analyses were performed with the Bell Curve for Excel software (version 3.21; Social Survey Research Information Co., Ltd., Tokyo, Japan). This study was approved by the institutional review board of Fukushima Medical University (No.3326).
Results
One hundred and one patients were diagnosed as having cutaneous sarcoidosis. Eight patients (one male and seven females) had developed ENLS, presenting with reddish to brownish erythematous lesions or erythematous plaques on the lower legs (Figure 1). Only one patient had developed ENLS as an initial manifestation of sarcoidosis. In six cases, the lesions spontaneously disappeared within six months (Figure 2), and among them, two cases showed transient enlargement of erythema showing livedoid changes. Histologically, the sarcoid granulomas were located in the dermis to subcutis (Figure 3). None of the patients had cardiac sarcoidosis; however, the lung was involved in all cases (100%), and ocular sarcoidosis was observed in six cases (75.0%). Serum levels of ACE were elevated in five cases (mean 41.2 ± 10.0 U/L: normal 7–25 U/L), whereas the levels were within normal ranges in the remaining three cases (mean 22.5 ± 1.5 U/L). The mean serum ACE level in the eight cases was 34.2 ± 12.0 U/L. The ENLS patient characteristics are summarized in Table 1.
Figure 1.
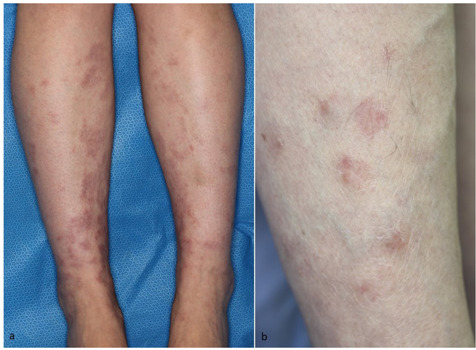
Clinical features of erythema nodosum-like sarcoid lesion. (a) Physical examination revealed bilateral erythematous lesions on the lower legs. (b) Close-up view reveals slightly infiltrated plaques.
Figure 2.
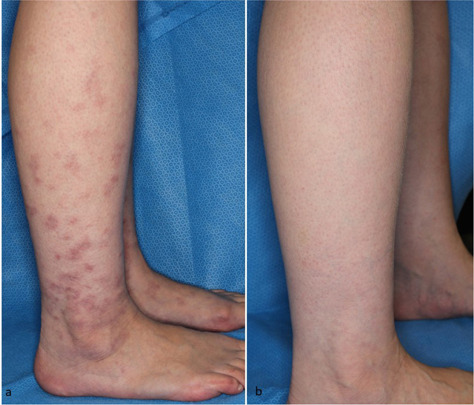
Spontaneous disappearance of erythema nodosum-like sarcoid lesions on the lateral aspects of the lower leg. (a) Clinical findings at the time of first examination. (b) Six months later.
Figure 3.
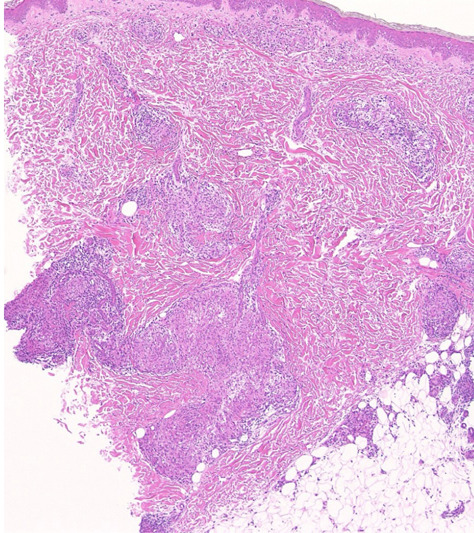
Histological features of the erythema nodosum-like sarcoid lesion showing epithelioid granulomas in the mid-dermis and subcutis (hematoxylin-eosin staining, original magnification × 40).
Table 1.
Characteristics of the ENLS patients
| Case | Age/Sex | Location | Other skin sarcoidosis | Pulmonary sarcoidosis | Ocular sarcoidosis | Serum ACE (U/L) |
|---|---|---|---|---|---|---|
| 1 | 65/F | Lower leg | - | + | - | 22.8 |
| 2 | 30/M | Lower legs | - | + | + | 33.7 |
| 3 | 46/F | Lower legs | Subcutaneous Scar sarcoidosis |
+ | + | 56.8 |
| 4 | 58/F | Lower legs | - | + | + | 24.2 |
| 5 | 39/F | Lower legs | Lupus pernio | + | + | 20.6 |
| 6 | 30/F | Lower leg | - | + | + | 45.3 |
| 7 | 74/F | Lower leg | Scar sarcoidosis | + | - | 42.2 |
| 8 | 36/F | Lower legs | - | + | + | 27.8 |
ENLS, erythema nodosum-like sarcoid lesion; ACE, angiotensin-converting enzyme.
On the other hand, among 93 cutaneous sarcoidosis patients who did not have ENLS, serum levels of ACE were elevated in 35 cases (mean 37.9 ± 11.8 U/L), and the mean serum ACE level in the 93 patients was 28.4 ± 13.0 U/L. Sixty-one patients had lung sarcoidosis (65.6%), and 29 patients had ocular sarcoidosis (31.2%). The comparison of clinical characteristics between ENLS patients and non-ENLS patients is summarized in Table 2.
Table 2.
Comparison of clinical characteristics between ENLS patients and non-ENLS patients
| ENLS (n=8) | Non-ENLS (n=93) | P-value | |
|---|---|---|---|
| Age (years), mean ± SD | 47.3 ± 15.6 | 58.3 ± 14.9 | 0.075 |
| Male : Female | 2 : 6 | 21 : 72 | 0.804 |
| Serum ACE, U/L ± SD | 34.2 ± 12.0 | 28.4 ± 13.0 | 0.145 |
| Pulmonary sarcoidosis, n (%) | 8 (100) | 61 (65.6) | 0.045* |
| Ocular sarcoidosis, n (%) | 6 (75.0) | 29 (31.2) | 0.013* |
| Cardiac sarcoidosis, n(%) | 0 (0) | 10 (10.8) | 0.329 |
*, P < 0.05, difference was statistically significant.
ENLS, erythema nodosum-like sarcoid lesion; ACE, angiotensin-converting enzyme.
Discussion
In Japan, cutaneous sarcoidosis is classified as 1) Cutaneous sarcoid (specific lesions), including nodular type, plaque type, lupus pernio, subcutaneous type as well as other types (lichenoid, erythema nodosum-like, ichthyosiform, other rare forms), 2) Infiltration of scars (scar infiltration), 3) Non-specific skin lesions (erythema nodosum) (7). ENLS is a rare specific form of cutaneous sarcoidosis, which resemble erythema nodosum only in appearance; however, skin biopsies reveal the presence of non-caseating epithelioid granuloma in the mid-dermis to subcutaneous tissues. Although ENLS involves the lower legs in almost all cases, patients with ENLS experience no pain or slight pain, if any, in contrast to erythema nodosum. In addition, the clinical symptoms, such as tenderness and subcutaneous induration, tend to be milder than those of non-specific erythema nodosum lesions.
ENLS may sometimes be observed in Asian patients with sarcoidosis. According to a review article of cutaneous sarcoidosis from Japan, there have been several clinicopathological studies of cutaneous sarcoidosis from Japanese institutions, and ENLS was observed in 24 out of 260 cases with cutaneous sarcoidosis (9.2%) (7). In our department, we observed 101 cases of cutaneous sarcoidosis, among which eight were ENLS (7.8%), suggesting that ENLS account for 5–10% of cutaneous sarcoidosis in Japanese patients. In addition, a report from Korea showed one case of ENLS among 17 patients with specific cutaneous sarcoidosis (8).
Moreover, from 2000 to 2019, we collected 12 solitary case reports of ENLS in Japanese patients. Eleven out of 12 were females (91.7%), and the ages ranged from 23 to 59 years old (mean age: 40.5 years old). Bilateral hilar lymphadenopathy was observed in all cases, and ophthalmic involvements were seen in eight patients (unknown: one patient). In our present study, ENLS patients were more frequently associated with pulmonary and ocular sarcoidosis than the patients with other types of cutaneous sarcoidosis (Table 2).
On the other hand, a case series study from England demonstrated that only two of 95 cases of cutaneous sarcoidosis showed erythema nodosum-like eruptions accompanied by histologically confirmed epithelioid granulomas (2.1%) (9). The author classified these two cases as erythema nodosum; however, we suggest that such cases should be regarded as ENLS. In order to distinguish between specific and non-specific skin lesions, lesions presenting with erythema nodosum-like eruptions accompanied by histologically confirmed epithelioid granuloma should be termed ENLS, not erythema nodosum.
By contrast, erythema nodosum is a representative non-specific cutaneous eruption occasionally associated with sarcoidosis. However, in Japan, erythema nodosum in association with sarcoidosis is rare. Okamoto reported two cases of erythema nodosum among 114 cases with cutaneous sarcoidosis (1.8%) (6). We found two cases of erythema nodosum among 93 cases of cutaneous sarcoidosis from 2000 to 2019 in our department (2.2%). In addition, we histologically diagnosed 59 patients with erythema nodosum in the same study period, among whom two patients had sarcoidosis (3.4%), suggesting that sarcoidosis is also rare as a background disease in Japanese erythema nodosum patients.
Cases presenting with erythema nodosum, bilateral hilar lymphadenopathy and arthritis with acute onset of sarcoidosis, are called Löfgren’s syndrome. HLA-DRB1*03 is strongly associated with symptoms observed in Löfgren’s syndrome, such as erythema nodosum and arthritis (10), and a recent study reported an association with CCR2 haplotype (11). Löfgren’s syndrome is also rare in Japanese sarcoidosis patients, probably due to the differing genetic backgrounds between Japanese people and those of other ethnicities.
Conclusion
ENLS is a specific form of cutaneous sarcoidosis that is occasionally observed in Japanese patients, with a female predominance, and frequently accompanies lung and ocular sarcoidosis. Although ENLS may not be major skin manifestation of sarcoidosis, we should pay much attention to ENLS for early identification of patients needing workup for systemic illness.
Conflict of interest:
None declared
References
- 1.Sakthivel P, Bruder D. Mechanism of granuloma formation in sarcoidosis. Curr Opin Hematol. 2017;24:59–65. doi: 10.1097/MOH.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 2.Rados J, Lipozencić J, Celić D, Loncarić D. Löfgren’s syndrome presenting with erythema nodosum-like eruption. Acta Dermatovenerol Croat. 2007;15:249–253. [PubMed] [Google Scholar]
- 3.Okamoto H, Mizuno K, Imamura S, Nagai S, Izumi T. Erythema nodosum-like eruption in sarcoidosis. Clin Exp Dermatol. 1994;19:507–510. doi: 10.1111/j.1365-2230.1994.tb01259.x. [DOI] [PubMed] [Google Scholar]
- 4.Takenoshita H, Yamamoto T. Erythema nodosum-like cutaneous lesions of sarcoidosis showing livedoid changes in a patient with sarcoidosis and Sjogren syndrome. Eur J Dermatol. 2010;20:640–641. doi: 10.1684/ejd.2010.1034. [DOI] [PubMed] [Google Scholar]
- 5.Endo M, Yamamoto T, Chen KR. Sarcoid vasculitis presenting with erythema nodosum-like lesions. Sarcoidosis Vasc Diffuse Lung Dis. 2021;38:e2021013. doi: 10.36141/SVDLD.V38I1.11277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okamoto H. Cutaneous sarcoidosis. Nihon Rinsho. 2002;60:1801–1806. (in Japanese) [PubMed] [Google Scholar]
- 7.Yamamoto T. Characteristics of cutaneous sarcoid lesions in Japanese patients. Pract Dermatol. 2018;40:766–770. (in Japanese) [Google Scholar]
- 8.Jung YJ, Roh MR. Clinical and histopathological analysis of specific lesions of cutaneous sarcoidosis in Korean patients. J Dermatol Treat. 2011;22:11–17. doi: 10.3109/09546630903440098. [DOI] [PubMed] [Google Scholar]
- 9.James DG. Dermatological aspects of sarcoidosis. Q J Med. 1959;28:108–124. [PubMed] [Google Scholar]
- 10.Grunewald J, Eklund A. Löfgren’s syndrome: human leukocyte antigen strongly influences the disease course. Am J Respir Crit Care Med. 2009;179:307–312. doi: 10.1164/rccm.200807-1082OC. [DOI] [PubMed] [Google Scholar]
- 11.Spagnolo P, Sato H, Grunewald J, et al. A common haplotype of the C-C chemokine receptor 2 gene and HLA-DRB1*0301 are independent genetic risk factors for Löfgren’s syndrome. J Intern Med. 2008;264:433–441. doi: 10.1111/j.1365-2796.2008.01984.x. [DOI] [PubMed] [Google Scholar]


