Abstract
Objective:
To comprehensively characterize blast exposure across the lifespan and relationship to TBI.
Participants:
Post-deployment veterans and service members (N = 287).
Design:
Prospective cohort recruitment.
Main Measures:
Salisbury Blast Interview (SBI).
Results:
94.4% of participants reported at least one blast event, 75% reported a pressure gradient during a blast event. Participants reported an average of 337.7 (SD = 984.0) blast events (range 0–4857), 64.8% occurring during combat. Across participants, 19.7% reported experiencing a traumatic brain injury (TBI) during a blast event. Subjective ratings of blast characteristics (wind, debris, ground shaking, pressure, temperature, sound) were significantly higher when TBI was experienced and significantly lower when behind cover. Pressure had the strongest association with resulting TBI (AUC = 0.751). Pressure rating of 3 had the best sensitivity (.54)/specificity (.87) with TBI. Logistic regression demonstrated pressure, temperature and distance were the best predictors of TBI, and pressure was the best predictor of primary blast TBI.
Conclusion:
Results demonstrate the ubiquitous nature of blast events and provide insight into blast characteristics most associated with resulting TBI (pressure, temperature, distance). The SBI provides comprehensive characterization of blast events across the lifespan including the environment, protective factors, blast characteristics and estimates of distance and munition.
Keywords: Explosion, traumatic brain injury, military, assessment
Introduction
Military service often results in exposure to a multitude of different blast forces throughout training, deployment and combat (1,2). Many service members deployed to combat zones in support of Operations Enduring Freedom (OEF), Iraqi Freedom (OIF) and New Dawn (OND) have been exposed to blasts or explosions, often without symptoms of traumatic brain injury (TBI) at the time of exposure (3). In the instance of TBI, exposure to blasts accounts for roughly 78% of wounded-in-action cases in OEF/OIF/OND service members and veterans (4). Given the high prevalence of exposure to blasts and explosions, it is important to understand the potential sequelae of such exposures and the circumstances that most likely lead to negative outcomes.
Currently, no well-accepted, standardized criteria exist to identify and characterize an individual’s experience of blasts or explosive events such as those that exist for TBI (5,6). The myriad variables present during a blast event make characterization and standardization difficult (3). These include the source (e.g., rocket, mortar, improvised explosive device, heavy weapons), magnitude and distance of the blast, as well as the presence of environmental factors (e.g., protective gear, reflective surfaces) that can alter the generated forces. Despite this limitation, several studies have assessed sequelae of blast exposure using a variety of methods.
A few longitudinal studies have reported detrimental acute effects of blast exposure in a portion of military personnel undergoing breacher training (7,8), heavy weapons training (9), and with subconcussive blast exposures during deployment (10). Cross-sectional studies have reported higher levels of self-reported symptoms associated with blast exposures during deployment (3) and in personnel with repeated exposures to low-level blasts (e.g., breachers, operators of heavy weapons) (11). These results have been observed in individuals without history of TBI. For example, Mac Donald et al. (2017) found elevated symptom burden in blast-exposed combat veterans without TBI compared to those without a history of either TBI or blast exposure (12). Close-range (<10 m) blast exposure has been demonstrated to alter functional connectivity within the default mode network (13,14). Effects of blast exposure on white matter integrity have repeatedly been demonstrated in the absence of TBI (15–18). Grande et al. (2018) demonstrated deficits in verbal memory associated with close-range blast exposure and with greater number of exposures at any distance (19). Together, these studies support blast exposure as an important factor in post-deployment outcomes independent of TBI. Further, these studies demonstrate that blast exposure is potentially associated with alterations in brain function and structure months to years later, even when individuals do not experience TBI associated with the event.
A significant weakness in the body of work investigating blast exposure is the heterogeneity in methods used to characterize blast exposure across studies, limiting the generalizability and translational potential of this work. Most studies of blast exposure in humans have relied on some form of retrospective self-report elicited by either questionnaires or structured interviews. These assessments typically focus on the presence or absence of blast exposure, with no quantification of frequency or severity (13,14,16,19). The two published measures evaluating blast exposure are the Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L (20)) and the Virginia Commonwealth University (VCU) Retrospective Concussion Diagnostic Interview, Blast Version (VCU rCDI-B (4)). Both of these measures were developed and validated to assess TBI, with no published psychometric studies of the blast aspects of the instruments. The BAT-L obtains limited details about the three most severe exposures to blast. For any remaining blasts, only estimates of distance from the blast are obtained. The VCU rCDI-B evaluates only the single worst blast exposure. The BAT-L and VCU rCDI-B share two common limitations for characterizing lifetime blast exposure, stemming directly from the fact that they are TBI interviews. First, a restricted sample (between 1 and 3) of blast events are evaluated. This does not allow investigations into how the number of exposures might relate to outcomes and prognosis. This is a significant weakness given the growing evidence suggesting that a higher number of exposures to even subconcussive events (i.e., in the absence of TBI) is associated with increasing risk of detrimental outcomes (3,11,19). Second, the instruments obtain a limited characterization of each event. This is particularly important in a nascent field. Without a full characterization of events (including protective factors, environmental factors and forces present) important contributing factors cannot be investigated and may be overlooked. The lack of instruments dedicated to fully characterizing blast exposure across the lifespan of an individual is a significant limitation when attempting to evaluate the sequelae or the specific characteristics of blast exposure that are important for understanding outcomes.
The Salisbury Blast Interview (SBI) was developed to address these identified issues with currently used, but unvalidated measures and provide a mechanism to improve understanding of blast exposure and sequelae. The SBI is a structured interview that characterizes blast events across the lifespan, independent from TBI (12,15–18). The interview gathers data regarding several aspects of each blast event. As noted above, a true validation study against clinical criteria or clinical judgment is not possible due to the lack of an accepted definition operationalizing what constitutes blast exposure. Instead, this manuscript evaluates how aspects of the blast exposure and the experience of the blast are altered by environmental and protective factors. We also demonstrate how distinct aspects of blast events are related to subsequent outcomes, including psychiatric symptoms, psychiatric disorders and TBI, among other functional outcomes. The goal of developing this interview is to provide a systematic way to collect data about an individual’s exposure to blasts and explosions of all types and severities to more fully understand the specific characteristics that may be associated with negative outcomes.
Materials and methods
Participants
Participants were 287 combat-exposed individuals (14% female) in the US Armed Forces (9.9% active duty) who deployed in support of OEF/OIF/OND. Data were gathered as part of a larger neuroimaging project. Inclusion criteria for the study were: deployment in support of the wars in Iraq or Afghanistan after September 11, 2001; combat exposure defined as a score of 18 or greater on the Deployment Risk and Resiliency Inventory-2 (DRRI-2 section D (21)); English speaking; 18 years of age or older, and ability to provide informed consent. Exclusion criteria were: lifetime history of moderate or severe TBI or penetrating head injury; TBI outside of deployment with loss of consciousness (LOC); history of major neurologic disorder such as stroke, seizure, or spinal cord injury; history of serious mental illness (e.g., bipolar disorder, schizophrenia); current presence of dementia, substance use disorder, or psychosis. Additional exclusion criteria related to neuroimaging activities were pregnancy, inability to tolerate an enclosed space for magnetic resonance imaging (MRI), or presence of ferrous metal other than dental fillings.
Participants completed a brief telephone screening and were not scheduled if they reported any exclusion criteria. Participants then completed an assessment visit to provide thorough characterization and fully evaluate eligibility criteria prior to enrollment in neuroimaging. Current data were obtained from the assessment visit; therefore, some participants may have met exclusion criteria listed above.
Measures
All measures were administered in a standardized manner by licensed psychologists, neuropsychologists, as well as trained and supervised research staff and post-doctoral fellows.
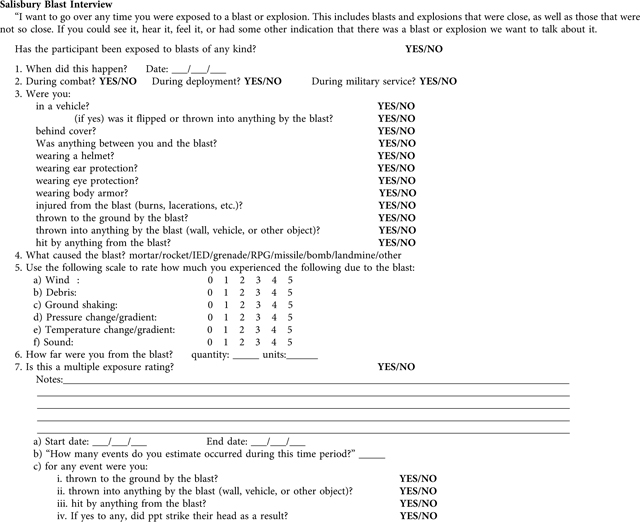
The Salisbury Blast Interview (SBI).
The Salisbury Blast Interview (SBI) is a structured interview evaluating events involving blasts or explosions across the lifespan (see Appendix A). Participants are asked about lifetime history of exposure to blasts or explosions regardless of the source, with events categorized according to military, deployment and/or civilian setting. The interview can be used alone, or accompanied by other measures and interviews. In the current study, additional questions were added to the SBI, the structured TBI interview, and the CAPS-5 to allow events to be cross-referenced. For example, the TBI interview confirmed which TBIs occurred during blast events. The SBI was developed to be applicable to both veterans and active duty service members, but could be easily utilized with other populations.
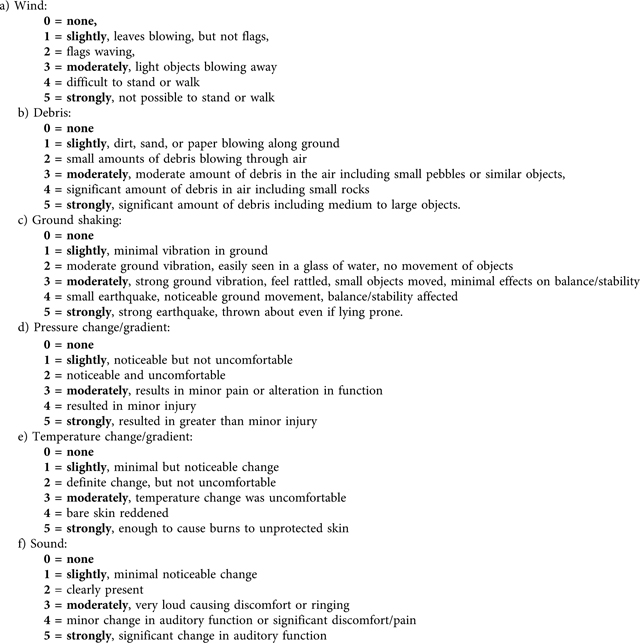
The initial query is purposefully broad to encourage reporting of any and all blast or explosive events, regardless of distance or severity. Because there is no agreed-upon or empirically supported definition of what constitutes a blast exposure, the interview is designed to gather information on as many events as possible (e.g., an IED detonating 5 feet away, or a rocket detonating 500 yards away). This allows the comparison of various definitions of blast exposure to be applied to the data, evaluating how different definitions may relate to outcomes. The date of each event is recorded and the environment is noted (combat, deployment, military service, or nonmilitary related). Circumstances (e.g., in a vehicle, wearing protective gear, behind cover), effects (e.g., thrown to the ground), blast event characteristics (e.g., wind, ground shaking, pressure change), distance, and other information about each event are collected. A distinguishing aspect of the interview is the provision of ratings by participants of their own experience across six blast event characteristics: wind, debris, ground shaking, pressure change, temperature change and sound (see Appendix B for behavioral anchors). Behavioral anchors standardize ratings across participants that may have experienced a blast or explosion across a variety of environments, munition types and/or distances.
Due to the potential for a large number of blast events in the OEF/OIF/OND population, a mechanism to capture multiple, highly similar events was included. For example, if the participant regularly engaged in route clearance or munition disposal they may report many blast events of a very similar nature under very similar circumstances. In these situations, a single rating is made representing a typical event, then the number of events and the time frame in which they occurred is recorded. This mechanism substantially reduces the time required to complete the interview. Manualized instructions for the interview are available by request from the corresponding author.
Several other interviews were administered to characterize participants. The Structured Clinical Interview for DSM-IV Diagnosis (SCID (22)) was used to determine the presence or absence of any Axis I psychiatric diagnosis. The Clinician Administered PTSD Scale − 5 (CAPS-5 (23)) was used to determine the presence or absence of current and lifetime PTSD. The Mid-Atlantic MIRECC Assessment of TBI (MMA-TBI) (unpublished; available upon request from the corresponding author) is a structured interview developed at the Mid-Atlantic Mental Illness Research, Education and Clinical Center (MIRECC). This interview provides a comprehensive assessment of brain injuries occurring across the lifespan. The cause, duration of LOC, alteration of consciousness (AOC) and post-traumatic amnesia (PTA), as well as symptoms immediately following each occurrence (e.g., headache, balance problems, vision problems), are evaluated. TBI severity was assigned based on VA/DoD consensus criteria (6).
Self-report measures were also included to evaluate current PTSD symptoms (PTSD Checklist – 5; PCL-5 (24)), postconcussive symptoms (The Neurobehavioral Symptom Inventory (25)), and combat exposure (The Deployment Risk and Resiliency Inventory, Version 2, Combat Experiences; DRRI-2 module D (21)). The Structured Inventory of Malingered Symptomatology (SIMS) (26) evaluated the validity of symptom presentation. Cutoff scores for a variety of populations have been developed; however, none are specific to service members or veterans (27). Therefore, a lenient cutoff score of 24 was selected for comparisons adjusting for symptom validity.
Analyses
Analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). All statistical tests were conducted using an alpha value of 0.05, uncorrected for multiple comparisons. Analyses were conducted at the participant level, with a single outcome for each participant, as well as at the event level, where a single participant could have contributed multiple events. At the participant level (n = 287), group comparisons of outcome variables were conducted using ANOVA. Additionally, correlations among maximum reported blast event characteristic ratings and outcomes were conducted using Pearson’s r. At the event level, all individually rated blast events across participants were included (n = 867). Only individual ratings were used in comparisons of blast event characteristics (not data from multiple exposure ratings). This limited the influence of the small number of individuals with very high numbers of blast events on the outcomes, increasing generalizability to the majority of individuals with lower numbers of events. Correlations among ratings were conducted using Pearson’s r. Logistic regression evaluated the individual contribution of ratings and distance to the experience of a TBI during a blast event. All independent variables (blast event characteristic ratings of wind, debris, ground shaking, pressure, temperature, sound, and distance from the blast) were entered into a single step. The dependent variable was a binary indicator of the experience of a TBI during the blast event. Sensitivity and specificity of each blast event characteristic rating were calculated for the likelihood that a blast event resulted in a TBI. Area under the curve (AUC) was calculated for each rating in relation to the experience of a TBI during a blast event. To assess for effects of validity, analyses were calculated with all participants, and also after excluding participants who scored above cutoff on the SIMS. Removal of these participants (n = 39) did not alter results; therefore, presented results include the entire sample (n = 287 participants and n = 867 events). Next, analyses related to TBI were repeated after removing participants with any history of TBI involving forces other than primary blast (analysis conducted using n = 79 participants and n = 184 events). This allowed an examination of the experience of TBI due to blast forces alone. Finally, analyses were repeated after removing participants with any history of TBI at all (analyses conducted using n = 54) to allow examination of the effects of blast forces alone.
Results
All participants
Table 1 provides descriptive statistics for demographic and other characteristic variables for the sample. In the current sample, 94.4% of participants reported at least one blast event during their lifetime (M = 337.7, Mdn = 51.0, Mo = 1, SD = 984.0, min = 0, max = 11555). There was a wide range in the number of blast events reported, 25% of the sample reported 5 or fewer events, 50% of the sample reported 51 or fewer events, and 75% of the sample reported 221 or fewer events. Across all blast events, 15.9% occurred within 10 feet of the participant and 44.1% occurred within 100 feet of the participant. Participants reported that 98.8% of blast events occurred during military service, 88.4% during deployment, and 64.8% during combat (percentages are not mutually exclusive). Across participants, 19.7% reported experiencing a TBI during a blast event and 30.2% reported a blast event was the criterion A event for evaluation of PTSD.
Table 1.
Descriptive statistics of demographic and characteristic variables.
| Variable | Total sample |
|---|---|
|
| |
| n = 287 | |
| Age (years) | 41.7 (9.8) |
| Education (years) | 15.0 (2.2) |
| Number of Deployments | 2.7 (3.4) |
| Minority (%) | 45.6 |
| Sex (% male) | 86.2 |
| Veteran (%) | 92.9 |
| Number blast events | 337.7 (984.0) |
| Time since most recent | 3697.7 (1311.55) |
| Blast event (days) | |
| TBI history (%) | 80.0 |
| Deployment TBI history (%) | 50.5 |
| Number TBI | 2.4 (3.4) |
| Time since most | 4694.5 (3964.4) |
| Recent TBI (days)a | |
| Current PTSD (%) | 37.3 |
| Service branch (%) | |
| Army | 42.6 |
| Army national guard | 17.7 |
| Army reserves | 13.1 |
| Marine corps | 9.2 |
| Air force | 5.9 |
| Navy | 3.3 |
| Other | 11.2 |
Values are reported as Mean (Standard Deviation) unless otherwise specified.
n = 259 as participants without TBI history are not included. Time Since TBI and Time Since Blast Event represents the most recent occurrence. Current PTSD is based on the CAPS-5.
Event level analyses
Helmets were the protective factor most likely to be present during a blast event, followed closely by an object between the individual and the blast, and body armor (see Table 2). Few blast events involved forces other than primary blast, with 56 (6.5%) events reported to have an associated injury, 71 (8.2%) events involved being thrown to the ground, 87 (10.1%) being thrown into something, and 78 (9.0%) being hit by an object (percentages are not mutually exclusive).
Table 2.
Frequency of the presence of protective factors during blast events.
| Protective factor | Present | Absent |
|---|---|---|
|
| ||
| In a vehicle | 271 (31.3%) | 595 (68.7%) |
| Behind covera | 465 (53.7%) | 401 (46.3%) |
| Object between | 560 (64.6%) | 307 (35.4%) |
| Helmet | 569 (65.6%) | 298 (34.4%) |
| Ear protection | 309 (35.6%) | 558 (64.4%) |
| Eye protection | 427 (49.3%) | 440 (50.7%) |
| Body armor | 534 (61.6%) | 333 (38.4%) |
Data presented from 867 individually rated blast events across the entire sample.
n = 866 due to a missing data point.
Ratings of blast event characteristics spanned the full range of possible responses (see Table 3), but most fell toward the lower end of the rating scale. All characteristic ratings were significantly higher for blast events involving TBI and these events tended to be closer (see Table 4).
Table 3.
Descriptive statistics of blast event characteristic ratings.
| Variable | Minimum | Maximum | Median | Mean | Standard Deviation |
|---|---|---|---|---|---|
|
| |||||
| Wind | 0 | 5 | 1.00 | 1.30 | 1.5 |
| Debris | 0 | 5 | 1.00 | 1.64 | 1.6 |
| Ground shaking | 0 | 5 | 3.00 | 2.54 | 1.5 |
| Pressure | 0 | 5 | 1.00 | 1.39 | 1.4 |
| Temperature | 0 | 5 | 0.00 | 0.67 | 1.2 |
| Sound | 0 | 5 | 3.00 | 3.31 | 1.3 |
Data presented from 867 individually rated blast events across the entire sample.
Table 4.
Blast event characteristic ratings of all events compared across events involving TBI and not involving TBI, as well as for events involving individuals with primary blast TBI only and those without TBI history.
| All Eventsa | Primary Blast TBIb | |||
|---|---|---|---|---|
|
| ||||
| TBI Event (n = 169) | Non-TBI Event (n = 698) | Primary Blast TBI Event (n = 52) | Non-TBI Event (n = 133) | |
|
| ||||
| Windc,e | 2.01 (1.7) | 1.13 (1.4) | 1.94 (1.8) | 1.01 (1.3) |
| Debrisc,e | 2.64 (1.7) | 1.40 (1.5) | 2.77 (1.7) | 1.44 (1.6) |
| Ground Shakingc,e | 3.40 (1.4) | 2.33 (1.4) | 3.65 (1.3) | 2.44 (1.4) |
| Pressurec,e | 2.52 (1.5) | 1.12 (1.3) | 2.75 (1.4) | 1.00 (1.2) |
| Temperaturec,e | 1.41 (1.5) | 0.49 (1.0) | 1.71 (1.5) | 0.32 (0.7) |
| Soundc,e | 4.04 (1.2) | 3.13 (1.2) | 4.00 (1.1) | 3.07 (1.2) |
| Distance (feet)c,d | 81.34 (176.1) | 953.72 (2418.4) | 67.07 (195.3) | 766.31 (1970.8) |
Data presented from 867 individually rated blast events across the entire sample
Data presented from 185 individually rated blast events involving individuals with history of only Primary Blast TBI and individuals without TBI history; Data are presented as Mean (Standard Deviation)
TBI versus No TBI comparison significant at p < .001
Primary Blast TBI versus No TBI History comparison significant at p < .05
Primary Blast TBI versus No TBI History comparison significant at p < .001; TBI = traumatic brain injury.
Logistic regression was used to predict the occurrence of a TBI during a blast event from the blast event characteristic ratings and distance. Bivariate correlations indicated acceptable collinearity (r = 0.02−0.63), therefore all ratings and distance were retained in the analysis. Null hypothesis testing suggested that slopes were different from zero (Likelihood Ratio χ2(7) = 214.1, p < .001). Results indicated that pressure (χ2(1) = 16.92, p < .001, OR = 0.82) and distance (χ2 (1) = 21.69, p < .001, OR = 1.01) were the only significant independent predictors of resulting TBI, both in the expected direction. This relationship is displayed in Figure 1 (All Participants). Wind, debris, ground shaking, temperature and sound did not independently contribute to the model.
Figure 1.
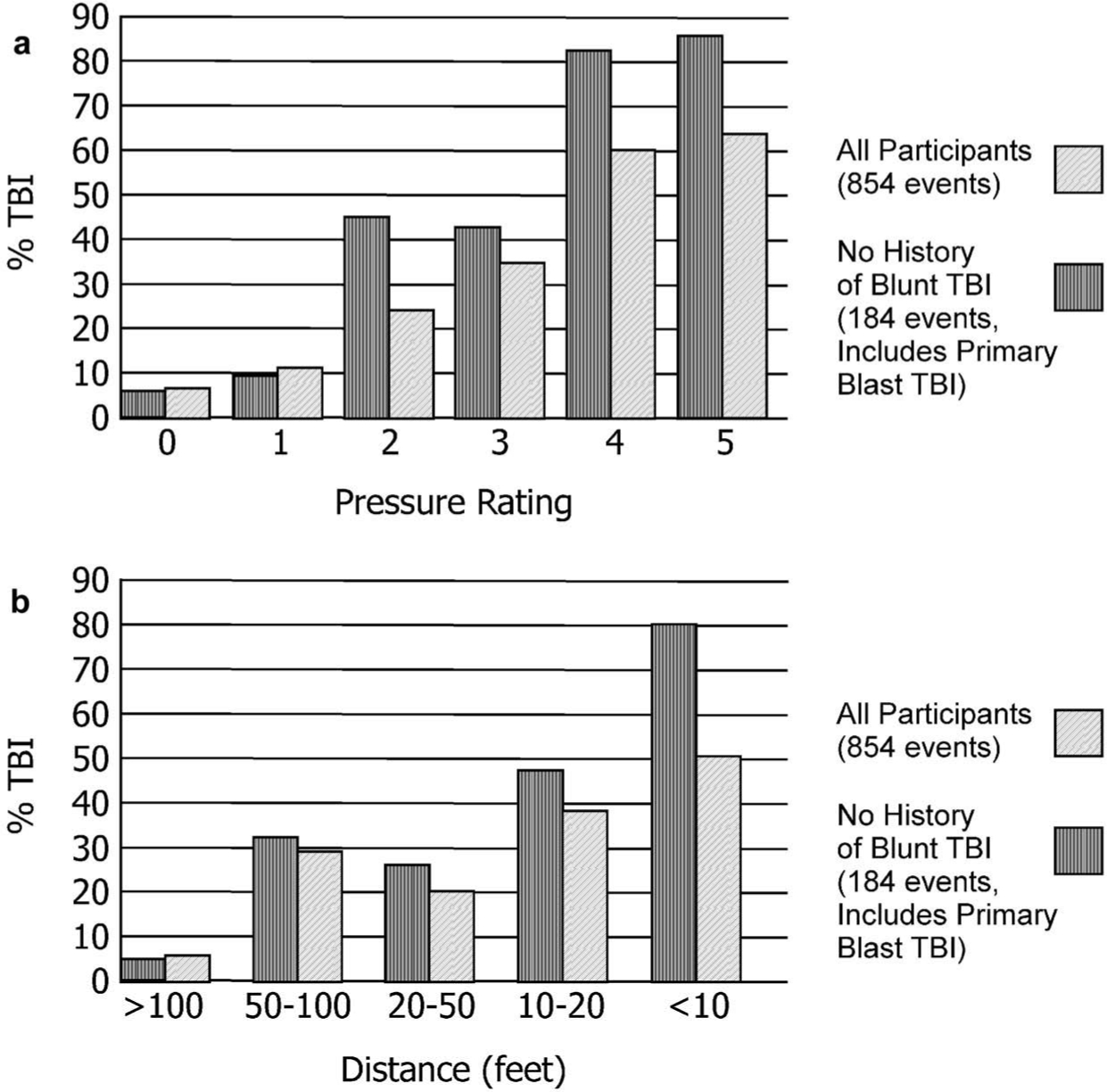
The likelihood of experiencing a TBI as a result of a blast event increased significantly as (a) the pressure rating increased and (b) the distance from the blast decreased. AUC for each characteristic rating and distance from the blast are presented in Table 5.
Table 5 shows the sensitivity and specificity of each level of blast event characteristic ratings for TBI occurring during a blast event. A pressure rating of 3 had the highest sensitivity while maintaining adequate specificity. A temperature rating of 2 had similar specificity but slightly lower sensitivity. AUC for associations between each rating and the occurrence of a TBI are also provided in Table 5. The highest AUC was associated with pressure, again suggesting this variable has the strongest relation to the occurrence of TBI during a blast event.
Table 5.
Sensitivity, specificity, and AUC of blast event characteristic ratings to the occurrence of TBI during the blast event.
| Characteristic rating | |||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | AUC | ||
|
| |||||||
| Wind | Sensitivity | 0.702 | 0.554 | 0.423 | 0.214 | 0.113 | 0.645 |
| Specificity | 0.478 | 0.678 | 0.808 | 0.936 | 0.977 | ||
| Debris | Sensitivity | 0.895 | 0.425 | 0.342 | 0.218 | 0.116 | 0.698 |
| Specificity | 0.492 | 0.527 | 0.688 | 0.855 | 0.959 | ||
| Ground | Sensitivity | 0.952 | 0.893 | 0.792 | 0.506 | 0.250 | 0.655 |
| Specificity | 0.117 | 0.318 | 0.510 | 0.780 | 0.943 | ||
| Pressure | Sensitivity | 0.857 | 0.762 | 0.512 | 0.250 | 0.125 | 0.752 |
| Specificity | 0.452 | 0.646 | 0.843 | 0.962 | 0.983 | ||
| Temperature | Sensitivity | 0.554 | 0.429 | 0.286 | 0.071 | 0.054 | 0.668 |
| Specificity | 0.733 | 0.860 | 0.934 | 0.981 | 0.994 | ||
| Sound | Sensitivity | 0.976 | 0.970 | 0.917 | 0.702 | 0.470 | 0.711 |
| Specificity | 0.010 | 0.063 | 0.341 | 0.662 | 0.797 | ||
Data presented from 867 individually rated blast events across the entire sample. AUC = area under the curve, TBI = traumatic brain injury. Underlined values represent the blast event characteristic rating with the best balance between sensitivity and specificity.
Participant level analyses
As displayed in Figure 2, maximum reported blast event characteristic ratings were negatively correlated with distance, suggesting the farther an individual is from a blast event, the less severe their experience. Wind, pressure and temperature were positively correlated with the number of events, but debris, ground shaking and sound were not related (see Table 6, All events row). No rating was associated with the time since an event, suggesting the duration since an event did not affect how that event was rated. Maximum reported characteristic ratings, but not the number of events or distance from events, were positively correlated with report of current symptoms (see Figure 3 and Table 6 PCL Total and NSI Total). As expected, maximum reported characteristic ratings were also positively correlated with combat exposure (DRRI-2). In addition, environmental factors altered blast event ratings. Ratings for events during which an individual was behind cover were significantly lower for wind, F(1, 864) = 5.49, p = .019, ground shaking, F(1, 864) = 4.88, p = .027, pressure, F(1, 864) = 10.29, p = .001 and sound, F (1, 864) = 9.24, p = .002, but not for debris, temperature, or distance.
Figure 2.
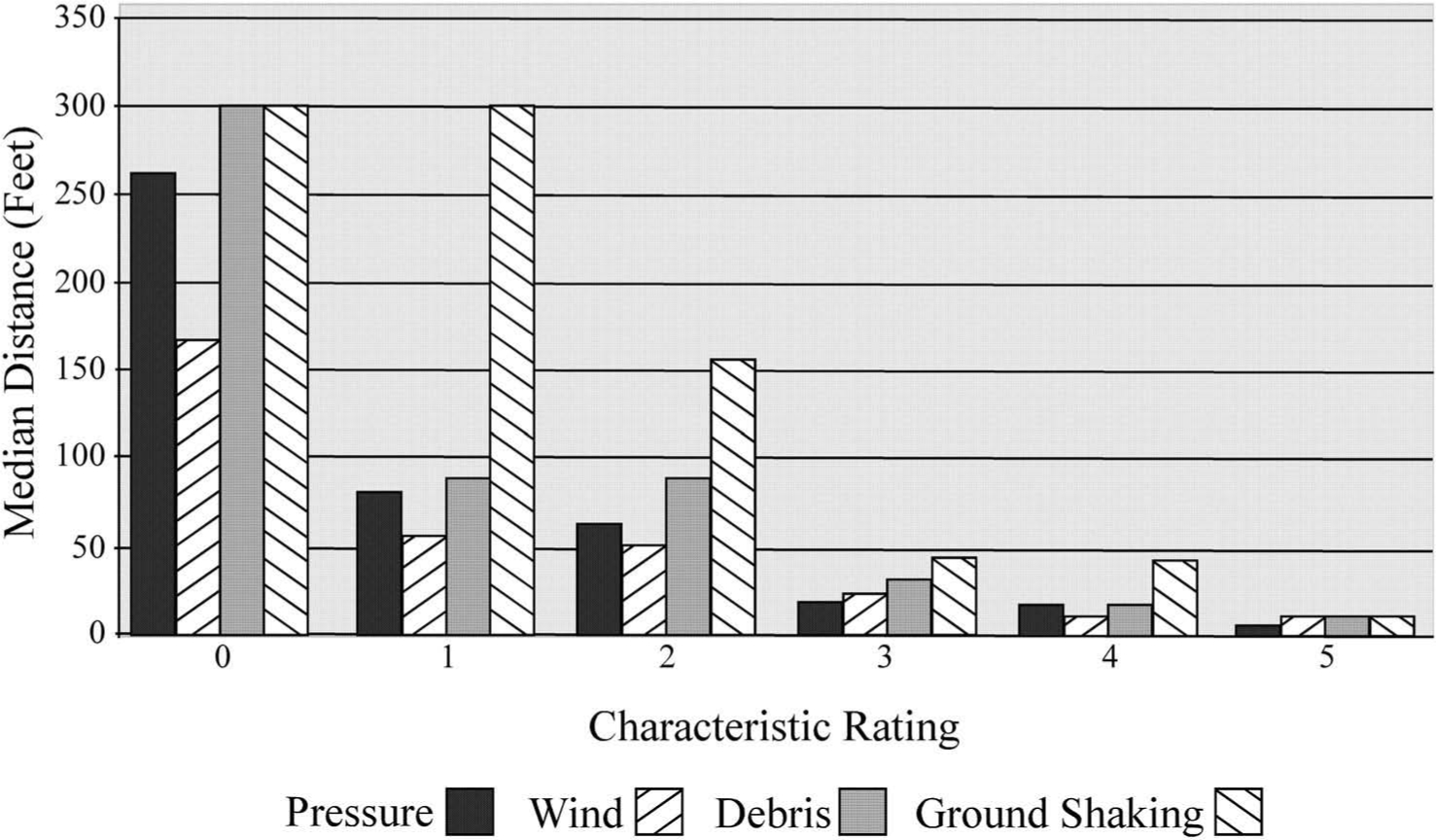
Median distance of blast events for each level of blast characteristic rating. All characteristic ratings were significantly negatively correlated with distance from the blast (presented in Table 6)
Table 6.
Correlations among blast event characteristic ratings and symptom reports for all participants, those with only a history of non-blunt force TBI, and those without TBI history.
| Minimum distance | Number of events | Time since event | DRRI-2-C | PCL Total | NSI Total | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Maximum wind | Alla | −.170** | .117* | −.014 | .406*** | .245*** | .230*** |
| Non-Blunt TBIb | −.264* | .054 | .066 | .464*** | .284* | .292** | |
| No TBIc | −.193 | .046 | .014 | .435*** | .271* | .269* | |
| Maximum debris | Alla | −.223*** | .081 | −.094 | .474*** | .269*** | .221** |
| Non-Blunt TBIb | −.429*** | .110 | −.048 | .518*** | .413*** | .390*** | |
| No TBIc | −.389** | .143 | −.101 | .507*** | .429** | .419** | |
| Maximum ground shake | Alla | −.166** | .052 | −.110 | .479*** | .327*** | .289*** |
| Non-Blunt TBIb | −.367*** | .193 | −.143 | .549*** | .438*** | .447*** | |
| No TBIc | −.264 | .223 | −.130 | .505*** | .402** | .401** | |
| Maximum pressure | Alla | −.134* | .134* | −.066 | .527*** | .346*** | .325*** |
| Non-Blunt TBIb | −.410*** | .100 | −.098 | .622*** | .497*** | .478*** | |
| No TBIc | −.335* | .195 | −.079 | .659*** | .392** | .365** | |
| Maximum temperature | Alla | −.127* | .141* | .029 | .468*** | .304*** | .274*** |
| Non-Blunt TBIb | −.276* | .173 | .022 | .635*** | .500*** | .492*** | |
| No TBIc | −.335* | .263 | −.031 | .556*** | .442*** | .343* | |
| Maximum sound | Alla | −.149* | .075 | −.035 | .414*** | .353** | .317** |
| Non-Blunt TBIb | −.458*** | .189 | −.009 | .481*** | .454*** | .422*** | |
| No TBIc | −.467*** | .160 | −.001 | .588*** | .434*** | .413** | |
| Minimum distance | Alla | 1.00 | −.027 | .139* | −.148* | −.025 | −.004 |
| Non-Blunt TBIb | 1.00 | −.057 | −.008 | −.332** | −.234* | −.276* | |
| No TBIc | 1.00 | −.126 | −.028 | −.195 | −.200 | −.246 | |
| Number of events | Alla | −.027 | 1.00 | −.054 | .074 | .086 | .037 |
| Non-Blunt TBIb | −.057 | 1.00 | −.078 | .133 | .121 | .105 | |
| No TBIc | −.126 | 1.00 | −.126 | .188 | .180 | .183 | |
n = 287
n = 79
n = 54
p < .05
p < .01
p < .001; all p values are uncorrected; DRRI-2-C = Deployment Risk and Resiliency Inventory – 2 – Combat Exposure, PCL = PTSD Checklist, NSI = Neurobehavioral Symptom Inventory.
Figure 3.
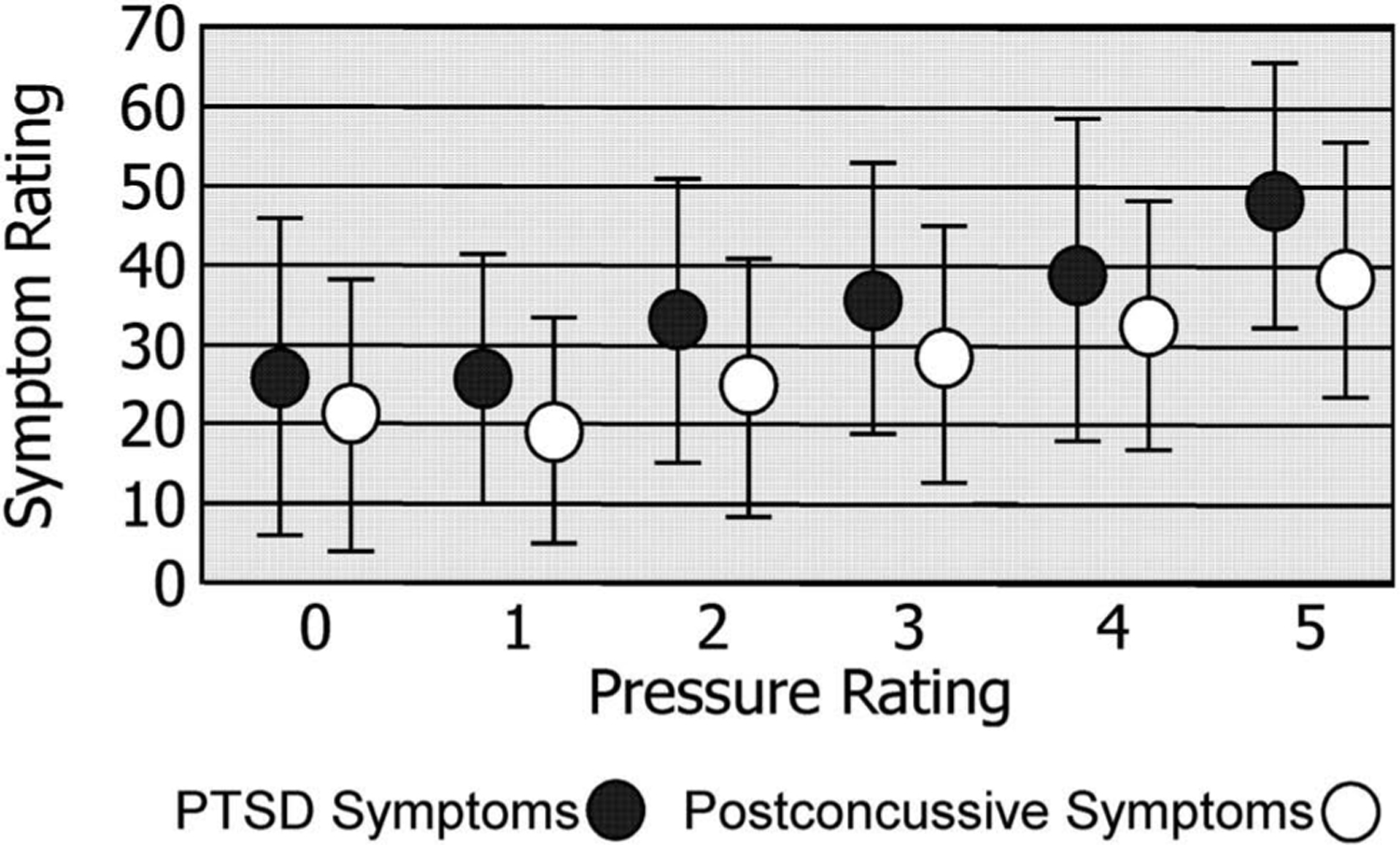
PTSD and postconcussive symptoms of participants presented at the maximum reported pressure across blast events. PTSD and postconcussive symptoms were significantly and positively correlated with the maximum pressure rating. Correlations among symptom report and characteristic ratings are presented in Table 6.
Results in participants without history of TBI involving blunt forces
Participants with lifetime history of TBI involving forces other than blast were removed from the sample for the following analyses (n = 79 participants and n = 184 events retained for analyses).
Event level analyses
Characteristic ratings were significantly higher for events resulting in primary blast TBI (see Table 4, Primary Blast TBI). Logistic regression was repeated predicting TBI resulting from a blast event from the characteristic ratings. Again, bivariate correlations among characteristic ratings indicated low collinearity. Null hypothesis testing suggested that slopes were different from zero (Likelihood Ratio χ2(7) = 86.47, p < .001). Pressure displayed the strongest relationship to TBI (χ2(1) = 10.24, p = .001, OR = 0.49), followed by temperature (χ2(1) = 7.97, p = .005, OR = 0.53) and distance (χ2 (1) = 4.69, p = .030, OR = 1.00). All associations were in the expected direction (see Figure 1, No History of Blunt TBI). No other variable had a chi-square value over 1. Sensitivity and specificity of subjective ratings were highly similar, with identical rating levels returning the best sensitivity while maintaining adequate specificity. Pressure again provided the best prediction of TBI at a rating of ‘3’ with specificity of 0.89 and sensitivity of 0.52.
Participant level analyses
Table 6 (Non-blunt TBI) demonstrates that bivariate correlations are highly similar between characteristic ratings and symptom presentation for the full sample and the non-blunt TBI sample.
Results in participants without history of TBI
Participant level analyses
Participants with lifetime history of TBI (regardless of the forces involved) were removed from the sample for the following analyses (n = 54 participants retained for analyses). Table 6 (No TBI) demonstrates that bivariate correlations were similar to those in the whole sample, with significant correlations between characteristic ratings and clinical outcomes. Differences were noted for maximum wind (correlations were not significant for distance) and ground shaking (correlations not significant for distance). Time since blast events remained unrelated to characteristic ratings. The number of blast events remained unrelated to clinical outcomes and was also no longer related to characteristic ratings.
Discussion
These results demonstrate the ubiquitous nature of blast events for individuals deployed in support of OEF/OIF/OND, with over 94% of the sample reporting at least one blast event, regardless of distance or severity. Further, 75% of the sample reported experiencing a minimum level of pressure gradient from at least one blast event (pressure rating > 0). Should these rates generalize to the OEF/OIF/OND population more broadly, blast events involving a reported pressure gradient would be one of the most prevalent deployment-related conditions. Despite this, few studies have investigated the unique effects of blast events on outcomes, as most studies focus on TBI resulting from forces including blast rather than on the experience of blast itself.
Though many service members and veterans experience blasts and explosions during military service, there is no standardized assessment tool to fully characterize these experiences. Without standardized methods to measure and characterize blast events, it remains difficult to evaluate and understand their role in the subsequent physical and mental health of service members and veterans. Current methods obtain limited characterization of blast events and only fully evaluate a small number of the total events experienced by service members. With increasing reports of the effects of blast on brain structure and function (13,14,16–18) as well as cognitive function (19), a standardized method for evaluating and characterizing such events is critical.
The SBI is a structured interview that allows comprehensive characterization of exposure to blasts and explosions across the lifespan. It is purposefully inclusive across all events, regardless of distance or severity. It can be administered independently, or in conjunction with other measures such as structured interviews for TBI or psychiatric diagnoses. The SBI captures multiple aspects of blast events including the environment, protective factors, ratings of event characteristics, as well as estimates of distance and type of munition. These data are easily related to outcomes of interest including TBI, mental health diagnoses and functional outcomes, as well as demographic and psychosocial factors. The current results serve to demonstrate the questions that can be answered using the SBI and the unique characteristics of the data.
Blast event characteristic ratings are a distinguishing aspect of the SBI. These ratings allow individual characterization of blasts events beyond distance, to include wind, debris, ground shaking, pressure gradient, temperature gradient and sound. One limitation of previous assessment methods is the reliance on report of munitions and distance to estimate the severity of the event regarding pressure and likelihood of injury (4,20). This approach is complicated by the many protective and agonistic factors that can be present, as well as a low likelihood of an individual having accurate knowledge of the munitions outside of controlled environments. Instead, the SBI obtains ratings of what an individual actually experienced using behaviorally anchored Likert scales in an interview format to reduce the ambiguity of ratings. Like other instruments, the SBI relies on self-report, which is the accepted standard for all research and clinical evaluations of TBI and psychiatric diagnoses in the OEF/OIF/OND population.
These results provide support for the experience of a pressure gradient as an important factor associated with TBI resulting from a blast event (Tables 4 and 5, Figure 3). Though all ratings were significantly higher when an individual experienced a TBI (Table 4), logistic regression demonstrated that pressure, temperature and distance were the three factors contributing the most unique explanatory power. Sensitivity/specificity and AUC results demonstrated that pressure had the strongest association and the best predictive power (Table 5). Further, when TBI due to primary blast forces only was examined (removing participants with TBI due to forces other than blast), pressure was again the strongest contributor to the experience of TBI. These results are consistent with current literature on the potential mechanisms of injury in primary blast TBI (28). These analyses could not be conducted using any other currently available method of quantifying and characterizing blast events.
As expected, characteristic ratings varied with the presence of protective factors. Participants behind cover reported lower levels of wind, ground shaking, pressure gradient and sound. Ratings for debris and temperature were qualitatively lower but did not reach significance, whereas distance was qualitatively higher without reaching significance. This pattern suggests participants behind cover experienced lower severity of several blast characteristics, likely due to the protective factors of cover as well as being farther away. Further, the likelihood of a TBI resulting from a blast event increased as the pressure rating increased and the distance decreased (Table 5, Figure 3). This provides support for the validity of these ratings as measures of the participants’ experience during a blast event.
Correlations revealed significant relationships between blast characteristic ratings and clinical outcome variables including PTSD symptoms and neurobehavioral symptoms (Table 6). Higher characteristic ratings were also associated with higher levels of combat exposure, as would be expected. However, combat exposure and characteristic ratings only shared between 16.5% and 27.7% of variance, suggesting characteristic ratings are not simply proxy measures of combat exposure. These relationships remained relatively stable when participants with TBI due to blunt forces were removed from analyses, and also when participants with lifetime history of any TBI were removed from analyses. This suggests characteristic ratings are also not proxy measures of TBI and that blast exposure in the absence of acute symptoms of TBI remains associated with detriemental outcomes. Finally, no characteristic rating was associated with the time since a blast event, suggesting ratings did not vary systematically and were not biased by the duration of time since an event. Similarly, only wind, pressure and temperature showed any association with the number of reported events, with increasing number of events associated with a small increase in the maximum rating for those respective characteristics.
Limitations of the SBI include a reliance on self-report retrospective data. Similar to evaluations of TBI, it is highly unlikely that researchers or clinicians will have access to individuals immediately following a blast event. Further, prospective studies of blast exposure in humans are not possible outside of highly specialized military occupations such as breachers. The SBI focuses on blasts and explosions; therefore, refinement of prompts may be necessary to capture effects of events not typically considered a blast or explosion, such as firing shoulder mounted weapons. The lack of a generally accepted definition of a blast exposure or a blast event precludes the development of concise outcomes or a scoring algorithm.
Overall, these results demonstrate the utility of the SBI, highlight the distinct types of data that can be extracted, and illustrate the unique questions that can be answered. Presented results are consistent with current literature regarding mechanisms of injury from blast exposures, suggesting report of the pressure gradient is the best predictor of TBI due to a blast event. Ratings of blast event characteristics on average were low, as would be expected when including assessments of any blast event regardless of severity or distance. These ratings varied in logical patterns across various environmental circumstances (e.g., being behind cover, increasing distance) and were related to reported symptom levels. The SBI is a demonstrably reliable method to comprehensively characterize blast events, particularly in military populations.
Acknowledgments
We would like to thank the veterans and service members who participated in this research. We would also like to thank Mary Peoples, David J. Curry, MSW, Alana M. Higgins, MA, Christine Sortino, MS, and G. Melissa Evans, MA, for their contributions to this project.
Funding
This research was supported by grant funding from Department of Defense, Chronic Effects of Neurotrauma Consortium (CENC) Award [W81XWH-13-2-0095] and Department of Veterans Affairs CENC Award I01 CX001135-01 [I01RX002172-01]. This research was also supported by the Salisbury VA Health Care System and Mid-Atlantic (VISN 6) Mental Illness Research, Education, and Clinical Center (MIRECC).
Appendix A
Appendix B
Footnotes
Declaration Statement
The authors declare no conflicts of interest, financial or otherwise. No competing financial interests exist.
References
- 1.Moore DF, Jaffee MS. Military traumatic brain injury and blast. NeuroRehabilitation. 2010;26:179–81. doi: 10.3233/NRE-2010-0553. [DOI] [PubMed] [Google Scholar]
- 2.Davenport ND. The chaos of combat: an overview of challenges in military mild traumatic brain injury research. Front Psychiatry. 2016;7:85. doi: 10.3389/fpsyt.2016.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsao JW, Stentz LA, Rouhanian M, Howard RS, Perry BN, Haran FJ, Pasquina PF, Wolde M, Taylor CE, Lizardo R, et al. Effect of concussion and blast exposure on symptoms after military deployment. Neurology. 2017;89:2010–16. doi: 10.1212/WNL.0000000000004616. [DOI] [PubMed] [Google Scholar]
- 4.Walker W, Cifu DX, Hudak AM, Goldberg G, Kunz RD, Sima AP. Structured interview for mild TBI after military blast Exposure: interrater agreement and development of diagnositic algorithm. Arch Phys Med Rehabiliation. 2014;95: 464–73. [DOI] [PubMed] [Google Scholar]
- 5.Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91:1637–40. doi: 10.1016/j.apmr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 6.Management of Concussion/mTBI Working Group. VA/DoD clinical practice guideline for management of concussion/mild Traumatic Brain Injury (mTBI). J Rehabiliatation Res Dev. 2009;46:CP1. doi: 10.1682/JRRD.2008.03.0038. [DOI] [Google Scholar]
- 7.Tate CM, Wang KKW, Eonta S, Zhang Y, Carr W, Tortella FC, Hayes RL, Kamimori GH. Serum brain biomarker level, neurocognitive performance, and self-reported symptom changes in soldiers repeatedly exposed to low-level blast: A breacher pilot study. J Neurotrauma. 2013;30:1–11. doi: 10.1089/neu.2012.2683. [DOI] [PubMed] [Google Scholar]
- 8.Kamimori GH, LaValle CR, Eonta SE, Carr W, Tate C, Wang KKW. Longitudinal investigation of neurotrauma serum biomarkers, behavioral characterization, and brain imaging in soldiers following repeated low-level blast exposure (New Zealand Breacher Study). Mil Med. 2018;183:28–33. doi: 10.1093/milmed/usx186. [DOI] [PubMed] [Google Scholar]
- 9.Rhea CK, Kuznetsov NA, Ross SE, Long B, Jakiela JT, Bailie JM, Yanagi MA, Haran FJ, Wright WG, Robins RK, et al. Development of a portable tool for screening neuromotor sequelae from repetitive low-level blast exposure. Mil Med. 2017;182:147–54. doi: 10.7205/MILMED-D-16-00140. [DOI] [PubMed] [Google Scholar]
- 10.Haran FJ, Handy JD, Servatius RJ, Rhea CK, Tsao JW. Acute neurocognitive deficits in active duty service members following subconcussive blast exposure. Appl Neuropsychology Adult. 2019;Jul 3:1–13. doi: 10.1080/23279095.2019.1630627Epub Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 11.Carr W, Polejaeva E, Grome A, Crandall B, LaValle C, Eonta SE, Young LA. Relation of repeated low-level blast exposure with symptomology similar to concussion. J Head Trauma Rehabil. 2015;30:47–55. doi: 10.1097/HTR.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 12.Mac Donald CL, Johnson AM, Wierzechowski L, Kassner E, Stewart T, Nelson EC, Werner NJ, Adam OR, Rivet DJ, Flaherty SF, et al. Outcome trends after US military concussive traumatic brain injury. J Neurotrauma. 2017;34:2206–19. doi: 10.1089/neu.2016.4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson ME, Clark DC, Milberg WP, McGlinchey RE, Salat DH. Characterization of differences in functional connectivity associated with close-range blast exposure. J Neurotrauma. 2017;34: S53–61. doi: 10.1089/neu.2016.4709. [DOI] [PubMed] [Google Scholar]
- 14.Robinson ME, Lindemer ER, Fonda JR, Milberg WP, McGlinchey RE, Salat DH. Close-range blast exposure is associated with altered functional connectivity in veterans independent of concussion symptoms at time of exposure. Hum Brain Mapp. 2015;36:911–22. doi: 10.1002/hbm.v36.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bazarian JJ, Donnelly K, Peterson DR, Warner GC, Zhu T, Zhong J. The relation between posttraumatic stress disorder and mild traumatic brain injury acquired during Operations Enduring Freedom and Iraqi Freedom. J Head Trauma Rehabil. 2013;28:1–12. doi: 10.1097/HTR.0b013e318256d3d3. [DOI] [PubMed] [Google Scholar]
- 16.Trotter BB, Robinson ME, Milberg WP, McGlinchey RE, Salat DH. Military blast exposure, ageing and white matter integrity. Brain. 2015;138:2278–92. doi: 10.1093/brain/awv139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taber KH, Hurley RA, Haswell CC, Rowland JA, Hurt SD, Lamar CD, Morey RA. White matter compromise in veterans exposed to primary blast forces. J Head Trauma Rehabil. 2015;30:E15–25. doi: 10.1097/HTR.0000000000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ivanov I, Fernandez C, Mitsis EM, Dickstein DL, Wong E, Tang CY, Simantov J, Bang C, Moshier E, Sano M, et al. Blast exposure, white matter integrity, and cognitive function in Iraq and Afghanistan combat veterans. Front Neurol. 2017;8:127. doi: 10.3389/fneur.2017.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grande LJ, Robinson ME, Radigan LJ, Levin LK, Fortier CB, Milberg WP, McGlinchey RE. Verbal memory deficits in OEF/OIF/OND veterans exposed to blasts at close range. J Int Neuropsychological Soc. 2018;24:466–75. doi: 10.1017/S1355617717001242. [DOI] [PubMed] [Google Scholar]
- 20.Fortier CB, Amick MM, Grande L, McGlynn S, Kenna A, Morra L, Clark A, Milberg WP, McGlinchey RE. The Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L) semistructured interview: evidence of research utility and validity. J Head Trauma Rehabil. 2014;29:89–98. doi: 10.1097/HTR.0b013e3182865859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. Deployment Risk and Resilience Inventory-2 (DRRI-2): an updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J Trauma Stress. 2013;26:710–17. doi: 10.1002/jts.2013.26.issue-6. [DOI] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV-TR Axis I disorders. Washington, D.C: American Psychiatric Press, Inc.; 1996. [Google Scholar]
- 23.Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, Marx BP. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol Assess. 2018. Mar;30(3):383–395. doi: 10.1037/pas0000486.Epub 2017 May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–98.doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 25.Cicerone KD, Kalmar K. Persistent postconcussion syndrome: the structure of subjective complaints after mild traumatic brain injury. J Head Trauma Rehabilitation. 1995;10(3): 1–17. [Google Scholar]
- 26.Smith GP, Burger GK. Detection of malingering: validation of the Structured Inventory of Malingered Symptomatology (SIMS). J Am Acad Psychiatry Law. 1997;25:183–89. [PubMed] [Google Scholar]
- 27.van Impelen A, Merckelbach H, Jelicic M, Merten T. The Structured Inventory of Malingered Symptomatology (SIMS): a systematic review and meta-analysis. Clin Neuropsychol. 2014;28:1336–65. doi: 10.1080/13854046.2014.984763. [DOI] [PubMed] [Google Scholar]
- 28.Cernak I Understanding blast-induced neurotrauma: how far have we come? Concussion. 2017;2:CNC42. doi: 10.2217/cnc-2017-0006 [DOI] [PMC free article] [PubMed] [Google Scholar]


